- 1Masonic Institute for the Developing Brain, University of Minnesota, Minneapolis, MN, United States
- 2Department of Population and Public Health Sciences, University of Southern California, Los Angeles, CA, United States
- 3Mallinckrodt Institute of Radiology, Washington University School of Medicine, St. Louis, MO, United States
- 4Neuroimaging Labs Research Center, Washington University School of Medicine, St. Louis, MO, United States
- 5Department of Psychiatry, Washington University School of Medicine, St. Louis, MO, United States
- 6AI Institute for Health, Washington University School of Medicine, St. Louis, MO, United States
- 7Department of Pediatrics, University of Minnesota, Minneapolis, MN, United States
Racism is embedded in the fabric of society at structural, disciplinary, hegemonic, and interpersonal levels, working as a mechanism that drives health disparities. In particular, stigmatized views of substance use get entangled with racialization, serving as a tool to uphold oppressive systems. While national health institutions have made commitments to dismantle these systems in the United States, anti-racism has not been integrated into biomedical research practice. The ways in which substance use researchers use and interpret race data—without engaging in structural racism as a mechanism of health inequity—can only be described as inadequate. Drawing upon concepts from the Public Health Critical Race praxis, QuantCrit, and an anti-racism research framework, we recommend a set of guidelines to help biomedical researchers conceptualize and engage with race more responsibly in substance use research.
1 Introduction
Since the 1950s, substance use has been medically defined as a psychopathology (1). While early definitions once categorized addiction as a “sociopathic personality disturbance” (2), distinct substance abuse and substance dependence labels have existed since 1980 with the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-III) (1, 3). Despite the establishment of a biomedical model of substance use, views of substance use as a personal moral failing have persisted in both the public and medical spheres (4). The moral rhetoric against individuals with substance use disorders (SUDs) goes hand in hand with perceptions that substance use warrants punishment; when paired with prejudice and animosity, these beliefs lay the foundation to target groups of people with the selective enforcement of drug laws, as seen with the US War on Drugs (5). Policies that ignore public health recommendations and employ racism—such as Nixon’s refusal to deschedule and decriminalize cannabis in the 1970s—mold “moral failings” into systemic tools of oppression (6). Hence, it is vital to reject unfounded beliefs about individuals with SUDs that get entangled with racism, which must begin with the scientific community.
Unfortunately, biomedical researchers often report race-related findings without critically considering the systems driving their observations (7–11). Social epidemiologist Dr. Nancy Krieger describes this dilemma as a two-edged sword, where the omission of race data from investigations ignores existing injustice, and the mishandling of race data exacerbates further injustice, reinforcing harmful beliefs about marginalized groups (12, 13). Investigators fall short by not incorporating anti-racist, equity-focused frameworks into their work, such as Critical Race Theory (CRT). Originally a framework for legal analysis, CRT underscores the relationship between race, racism, and power and denotes many ways in which oppression manifests across all forms of expression (14), providing language to examine how social, political, and historical forces give race meaning as a construct (see Table 1 for CRT tenets and principles). Frameworks like CRT can be used to recognize structural racism and racialization as the drivers of differential health outcomes, not race. This gets at a fundamental limitation of the biomedical model of substance use: the model minimizes the impact of psychosocial factors on SUDs (17); in turn, this risks positioning race as a biological driver of SUDs.
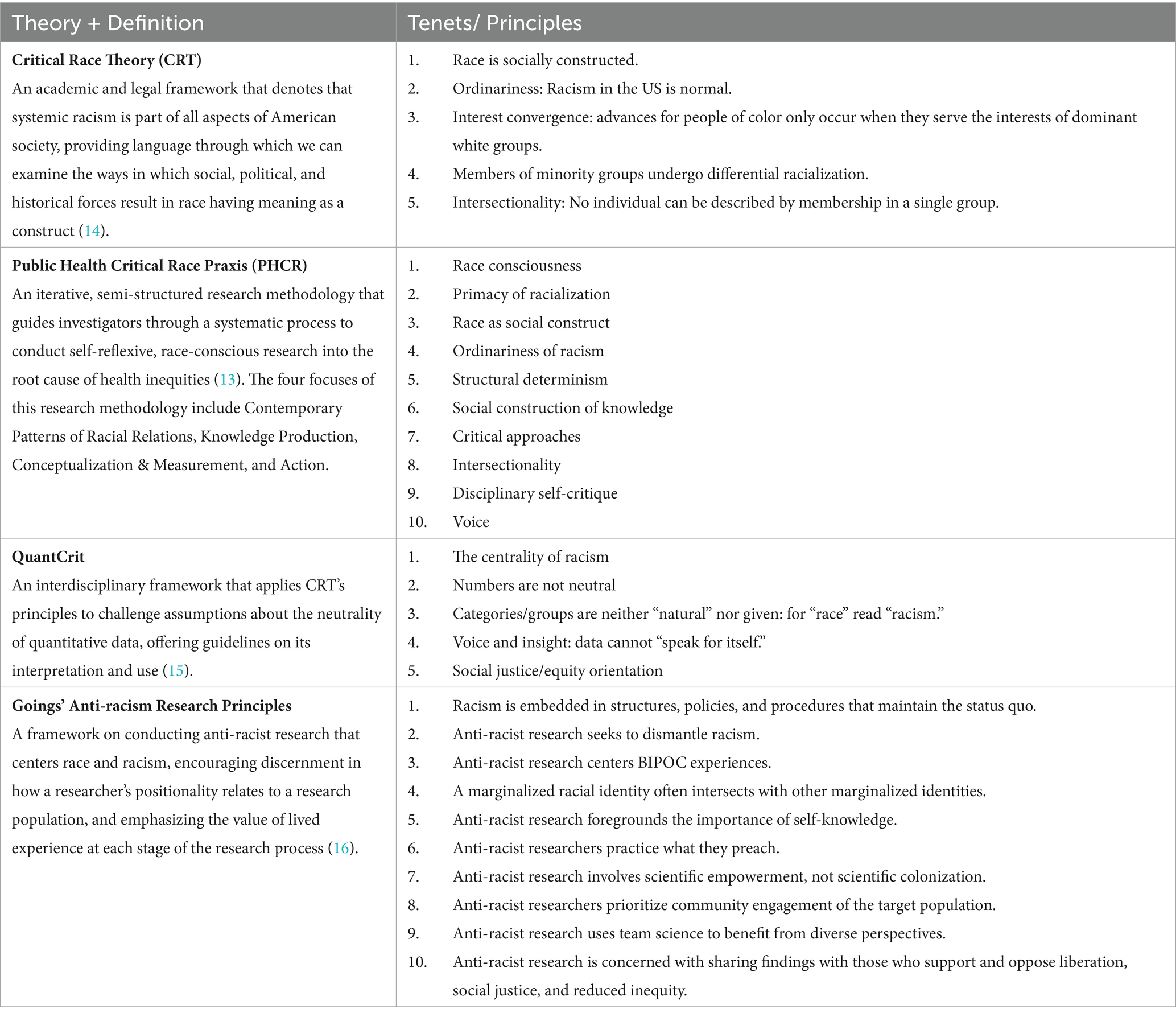
Table 1. Definitions and major tenets/principles of the anti-racist, equity-focused frameworks that influenced this article’s suggested guidelines for biomedical SUR.
Therefore, in order to engage with race data with diligence, substance use researchers must employ anti-racist praxes in their investigations. Given that many research institutions have been created and maintained through white supremacy, anti-racist progress requires transformative action driven by the perspectives and priorities of minoritized communities (18). Drawing on concepts from the Public Health Critical Race praxis (PHCR) (13), QuantCrit (15), and an anti-racism research framework from Goings and colleagues (16), we recommend a set of guidelines to help biomedical researchers conceptualize and engage with race more responsibly in substance use research (SUR).
2 Mishandling race in health disparities and substance use research
The use of race as a broad proxy for structural racism can be extremely harmful to minoritized groups, thereby reinforcing racialized stigma and perpetuating biological determinism (7). Whether explicit or implicit, any use of biological determinism has no place in published literature (7). Across biomedical SUR literature, few studies systematically evaluate whether substance use researchers appropriately define race or report race data. In a recent scoping review of studies from 2000 to 2020 involving maternal–infant dyads with Opioid Use Disorder, investigators found that of the 63 identified quantitative studies that used race/ethnicity in their statistical analyses, only 17 mentioned race/ethnicity in their discussion sections (8). None of the included studies defined race as a social construct, leaving the authors to conclude that SUR “can benefit from a reckoning with how poorly race data have been incorporated to date” (8).
While there are limited critical evaluations of anti-racism in SUR, publications in adjacent health sciences fields highlight a concerning pattern. For example, a systematic review of 329 epidemiology studies published in five prominent journals from 1995 to 2018 found that 61% of studies failed to justify using race or ethnicity data (9). In more recent publications from 2020 to 2021, a review of 192 epidemiology studies revealed that only 23% of articles discussed systemic mechanisms that might drive observed racial health disparities (10). Perhaps even more concerning, three of the identified articles considered biological mechanisms as reasons for racial disparities (10). Similar trends are seen across both public health and medical journals; with broad failures to discuss the role of structural racism in driving health disparities, suggesting that these practices are not outliers but instead the norm (11, 19).
3 Guidelines on conducting anti-racist substance use research
The direct link between intersectional oppression and racial health inequity has been recently recognized as a public health crisis (20–22). While institutions like the National Institutes of Health have proposed direct commitments to address racial health inequity in research moving forward (19, 23), such commitments have not yet translated into tangible changes in published biomedical research. Anti-racist research frameworks are especially needed for biomedical SUR, where (1) racism is deeply intertwined with the moralization of substance use, and (2) research findings shape public perceptions, institutional norms, federal policies, and biases from medical providers (4, 24). To this end, we outline a foundational set of guidelines on conducting anti-racist research in the following sections, drawing on principles from PHCR (13), QuantCrit (15), and a framework on conducting anti-racist research (16) (see Table 1 for definitions and tenets/ principles of these frameworks).
3.1 Study design considerations
Guideline 1 : Employ mixed methods study designs to help contextualize and supplement quantitative findings.
As previously discussed, the biomedical model of substance use disregards the role psychosocial factors play in SUDs (17), omitting the lived experiences of black, indigenous, and other people of color (BIPOC); these experiences are central to understanding the relationship between structural racism and quantitative findings (13, 15, 16). Considering that addiction neuroscience literature often refrains from engaging with social determinants of health relevant to their study samples (25), it is all the more prudent to seek out additional forms of knowledge and forms of knowing (26). This can be accomplished with mixed methods study designs, where quantitative findings can be contextualized using qualitative representations of lived experience (13, 27, 28). Furthermore, qualitative data from mixed-methods studies can provide information that could not otherwise be captured with quantitative methods, like identifying unexplored manifestations of structural racism (22, 29). These methodologies can be strengthened by applying a community-based participatory research (CBPR) paradigm, which integrates community voice, ownership, and decision making at each stage of the research process (30).
As an example of a mixed-methods research project that employs CBPR, the University of Minnesota’s Randolph Lab is conducting an ongoing comprehensive needs assessment on mental health and substance use in Minnesota youth. This initiative—the Minnesota Youth Needs Assessment (MYNA)—draws on a community of practice model to bring together a network of youth and outreach organizations to collaboratively address the incidence of mental health and substance use among youth aged 12–24 (31, 32). Bringing these stakeholders together allowed us to draw on their experiential knowledge to co-design this study, centering the comfort of youth when broaching certain topics, using unbiased language in study materials, and understanding that youth are the experts of their own experiences. These conversations provided social validity for the study prior to data collection, ensuring that the study methods and aims were aligned with the priorities of, and were accepted by, the community (33, 34). The assessment included a mixture of quantitative and qualitative methods, allowing for an eventual triangulation of data elements to represent a comprehensive picture of the youths’ lived experiences. Although our study is ongoing, we aim to use social context to highlight the systematic factors that are driving mental health and substance use concerns in youth.
Guideline 2 : Ensure that samples are not only representative of the minoritized populations being investigated, but also large enough to draw valid conclusions concerning these groups.
A pivotal goal in human neuroscience—including substance use neuroscience—is building models that are reproducible and generalizable; however, this field has historically relied on small convenience samples from populations that are western, educated, industrialized, rich, and democratic (WEIRD) (35). Although there has been a recent emphasis on larger sample sizes for improved reproducibility of brain-behavior linkages (36), larger samples alone do not guarantee generalizability of brain-based models across individuals from diverse backgrounds. While it may be difficult to find representative samples of certain minoritized groups, it would be inappropriate to draw conclusions using non-representative samples (37). However, representative samples do not guarantee the validity of a model stratified by race, as insufficient sample sizes in stratified groups can result in invalid, harmful findings (37–39).
3.2 Diverse, interdisciplinary research teams
Guideline 3 : Examine one’s own positionality in relation to a target population, recognizing the limitations of one’s perspectives and embracing diverse, equitable collaborations.
The social distance between a researcher and a research population is a fundamental consideration factor in ensuring an investigation does not perpetuate scientific racism, stemming from limitations in a researcher’s lived experience (13, 16, 40). Dr. Krieger notes that data does not speak for itself, instead, it is “always produced by people, out of what they observe, fail to see, or suppress in the world in which they live” (12). To this end, biases can determine what research questions get asked, how data are collected and analyzed, how findings are interpreted, and what findings are reported (13, 15, 16, 40). Therefore, it is critical that researchers seek out diverse, equitable collaborations with both fellow scholars and with community stakeholders through CBPR to draw on the wisdom of lived experience.
Guideline 4 : Because of how embedded racism is in society, anti-racist research requires a breadth of interdisciplinary expertise.
Similar to how lived experiences provide socio-contextual expertise to anti-racism research, interdisciplinary teams are necessary to develop robust, comprehensive solutions that address structural racism. Anti-racist research benefits from a range of “unique perspectives, expertise, and approaches” that are drawn from various disciplines, improving the impact, novelty, and reach of research publications (16, 41). Because racism and racialization permeate all aspects of society, specialized (e.g., mixed method), interdisciplinary teams are needed to adequately address health inequity (16, 18, 27, 42).
3.3 Use and interpretation of race data
Guideline 5 : Whenever possible, measure structural racism directly instead of using race as a proxy for racism or racialization. When analyzing race data, racism or racialization should be framed as risk factors for group differences, not race.
Since researchers operate under the structures and policies of academic institutions, they are subject to systems that uphold structural racism (13, 16, 18). It is clear that biomedical researchers have not done enough to embrace anti-racism in their work and must move beyond solely documenting inequality (8–11, 13, 19). Therefore it is paramount for researchers to acknowledge structural racism as a driver of health disparities by measuring it directly whenever possible (e.g., racialized economic segregation) (43), rather than using race as a proxy for racism or racialization (7, 13, 16, 44). This shift is needed to eliminate any possibility of erroneous interpretation that racial health disparities are a result of inherent differences or deficiencies (7, 15, 44–46). However, there are circumstances where using race data is required or appropriate, including in identifying populations that are at risk for specific racism exposures (13). Therefore, in these scenarios, researchers must frame racism and racialization as risk factors for outcome differences, not race.
4 Discussion
As scientists, our paradigms must reflect the consensus that systemic oppression and social conditions are the drivers of health inequity, otherwise scientific racism persists (7). The many factors that contribute to health disparities (e.g., neighborhood disadvantage) often go unmeasured and ignored with typological thinking in epidemiological studies related to substance use (47); letting researchers “off the hook” from identifying the structural and political forces that give rise to racial social stratification (48). Even when studies do consider some social conditions like the impact of social class on health, they still sidestep addressing structural racism by placing class and race as independent and mutually exclusive of one another, rather than acknowledging their intersectional relationship (38, 49). When researchers omit systemic context, BIPOC populations bear the consequences of structural racism, like lower rates of opioid medication receipt following inpatient admissions compared to white populations, and widening overdose rates (50–52). Hence, it is critical to dismantle the systems that sustain racism and racialization through the use of anti-racist, CRT-informed approaches in SUR.
An interconnection between theory and practice toward social justice must be at the forefront of SUR, from project ideation to implementation. Although there are challenges to integrating anti-racist research into practice that require further attention (e.g., securing funding for community engagement, balancing time-intensive methodologies with systemic pressures for frequent publications), it is nonetheless crucial that we redefine institutional norms to disrupt oppressive systems (16, 53). This includes moving beyond the biomedical model of substance use and shifting the focus of health inequity from race to racism (13, 15–17). While this paper aims to help substance use researchers engage with race more responsibly, we are not the first to make such a call to biomedical researchers, nor are the guidelines presented here exhaustive [e.g., (see 38) for considerations on how researchers can operationalize race and ethnicity]. However, given the scarcity of publications systematically examining how the field of SUR handles race, it is necessary to have ongoing, evolving discussions about what anti-racist practices look like within SUR, as seen in adjacent fields [(see 10, 13, 15, 16, 38, 54)]. In addition to conducting future systematic reviews, the field must also work to place a greater emphasis on the collective uplift of historically marginalized communities, especially concerning the applicability, acceptability, and community usability of research findings. As noted by race, gender, and law scholar Dorothy Roberts, “Race persists neither because it is scientifically valid nor because its invalidity remains to be proven. Race persists because it continues to be politically useful” (55). It is therefore our duty as substance use researchers to integrate anti-racism into our work in efforts to disentangle racialization from the moralization of substance use, thereby disarming structural racism as a tool of oppression.
Positionality statement
This manuscript was collaboratively written by a group of early-career researchers whose backgrounds span a spectrum of lived experience and expertise. As a collective, our identities—Mexican, Honduran, Latinx, White, Black, and African—shape our perspectives and our work. Our understanding of SUR as a field stems from our multidisciplinary specializations, including substance use neuroscience, cognitive neuroscience, prenatal substance exposure, pediatric neuroimaging, structural and social determinants of health, community engaged research, sociology, and reproductive justice. Through our engagement and interaction with communities, our perspectives are further informed by community voice. Overall, our outlooks represent a collection of cultural knowledge, expertise, anti-racism scholarship, and community engagement.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding author.
Author contributions
JL: Conceptualization, Writing – original draft, Writing – review & editing. DB: Writing – original draft, Writing – review & editing, Conceptualization. AM: Writing – original draft, Writing – review & editing, Conceptualization. CC-I: Writing – original draft, Writing – review & editing, Conceptualization. SM: Writing – original draft, Writing – review & editing. AR: Writing – original draft, Writing – review & editing, Conceptualization, Supervision.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fitzgerald, B, and Morgan, BD. DSM-5 changes on the horizon: substance use disorders. Issues Ment Health Nurs. (2012) 33:605–12. doi: 10.3109/01612840.2012.704131
2. American Psychiatric Association. Diagnostic and Statistical Manual: Mental Disorders. 1st ed American Psychiatric Association Mental Hospital Service, Washington, D.C., USA (1952).
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. American Psychiatric Association, Washington, D.C., USA (1980). 512 p.
4. Lawrence, RE, Rasinski, KA, Yoon, JD, and Curlin, FA. Physicians’ beliefs about the nature of addiction: a survey of primary care physicians and psychiatrists. Am J Addict. (2013) 22:255–60. doi: 10.1111/j.1521-0391.2012.00332.x
5. Earp, BD, and Lewis, J. Hart CL, with bioethicists and allied professionals for drug policy reform. Racial justice requires ending the war on drugs. Am J Bioeth. (2021) 21:4–19. doi: 10.1080/15265161.2020.1861364
6. Miron, J, and Partin, E. Ending the war on drugs is an essential step toward racial justice. Am J Bioeth. (2021) 21:1–3. doi: 10.1080/15265161.2021.1895590
7. Perry, MJ, Arrington, S, Freisthler, MS, Ibe, IN, McCray, NL, Neumann, LM, et al. Pervasive structural racism in environmental epidemiology. Environ Health. (2021) 20:119. doi: 10.1186/s12940-021-00801-3
8. Schiff, DM, Work, EC, Foley, B, Applewhite, R, Diop, H, Goullaud, L, et al. Perinatal opioid use disorder research, race, and racism: a scoping review. Pediatr Int. (2022) 149:27–35. doi: 10.1542/peds.2021-052368
9. Martinez, RAM, Andrabi, N, Goodwin, AN, Wilbur, RE, Smith, NR, and Zivich, PN. Conceptualization, operationalization, and utilization of race and ethnicity in major epidemiology journals, 1995-2018: a systematic review. Am J Epidemiol. (2023) 192:483–96. doi: 10.1093/aje/kwac146
10. Swilley-Martinez, ME, Coles, SA, Miller, VE, Alam, IZ, Fitch, KV, Cruz, TH, et al. “We adjusted for race”: now what? A systematic review of utilization and reporting of race in American Journal of Epidemiology and Epidemiology, 2020-2021. Epidemiol Rev. (2023) 45:15–31. doi: 10.1093/epirev/mxad010
11. Hardeman, RR, Murphy, KA, Karbeah, J, and Kozhimannil, KB. Naming institutionalized racism in the public health literature: a systematic literature review. Public Health Rep. (2018) 133:240–9. doi: 10.1177/0033354918760574
12. Krieger, N. Structural racism, health inequities, and the two-edged sword of data: structural problems require structural solutions. Front Public Health. (2021) 9:655447. doi: 10.3389/fpubh.2021.655447
13. Ford, CL, and Airhihenbuwa, CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. (2010) 71:1390–8. doi: 10.1016/j.socscimed.2010.07.030
14. Delgado, R, and Stefancic, J. Critical Race Theory (Third Edition): An Introduction NYU Press, New York, USA (2017). 199 p.
15. Gillborn, D, Warmington, P, and Demack, S. QuantCrit: education, policy, ‘big data’ and principles for a critical race theory of statistics. Race Ethn Educ. (2018) 21:158–79. doi: 10.1080/13613324.2017.1377417
16. Goings, TC, Belgrave, FZ, Mosavel, M, and Evans, CBR. An antiracist research framework: principles, challenges, and recommendations for dismantling racism through research. J Soc Soc Work Res. (2023) 14:101–28. doi: 10.1086/720983
17. Deacon, BJ. The biomedical model of mental disorder: a critical analysis of its validity, utility, and effects on psychotherapy research. Clin Psychol Rev. (2013) 33:846–61. doi: 10.1016/j.cpr.2012.09.007
18. Bowleg, L. “The Master’s tools will never dismantle the Master’s house”: ten critical lessons for black and other health equity researchers of color. Health Educ Behav. (2021) 48:237–49. doi: 10.1177/10901981211007402
19. Krieger, N, Boyd, RW, De Maio, F, and Maybank, A (2021). Medicine’s privileged gatekeepers: producing harmful ignorance about racism and health. Health Affairs Forefront. Available at: https://www.healthaffairs.org/content/forefront/medicine-s-privileged-gatekeepers-producing-harmful-ignorance-racism-and-health
20. Ghasemi, E, Majdzadeh, R, Rajabi, F, Vedadhir, A, Negarandeh, R, Jamshidi, E, et al. Applying intersectionality in designing and implementing health interventions: a scoping review. BMC Public Health. (2021) 21:1407. doi: 10.1186/s12889-021-11449-6
21. Bowleg, L. The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. (2012) 102:1267–73. doi: 10.2105/AJPH.2012.300750
22. Hardeman, RR, Homan, PA, Chantarat, T, Davis, BA, and Brown, TH. Improving the measurement of structural racism to achieve antiracist health policy. Health Aff. (2022) 41:179–86. doi: 10.1377/hlthaff.2021.01489
23. Compton, WM, Einstein, EB, Wargo, EM, Crump, AD, and Aklin, WM. Racial inequities and addiction research. Drug Alcohol Depend. (2023) 251:110940. doi: 10.1016/j.drugalcdep.2023.110940
24. Jackson, DS, Nguemeni Tiako, MJ, and Jordan, A. Disparities in addiction treatment: learning from the past to forge an equitable future. Med Clin North Am. (2022) 106:29–41. doi: 10.1016/j.mcna.2021.08.008
25. Netherland, J, and Hansen, H. White opioids: pharmaceutical race and the war on drugs that wasn’t. BioSocieties. (2017) 12:217–38. doi: 10.1057/biosoc.2015.46
26. Coleman, G. Core issues in modern epistemology for action researchers: dancing between knower and known In Bradbury H. editor. Sage Handbook of Action Research, Thousand Oaks, California, USA (2015). 392–400.
27. Mertens, DM. Research and Evaluation in Education and Psychology: Integrating Diversity With Quantitative, Qualitative, and Mixed Methods SAGE Publications, Thousand Oaks, California, USA (2023). 544 p.
28. Mertens, DM. Transformative paradigm: mixed methods and social justice. J Mixed Methods Res. (2007) 1:212–25. doi: 10.1177/1558689807302811
29. Chantarat, T, Van Riper, DC, and Hardeman, RR. The intricacy of structural racism measurement: a pilot development of a latent-class multidimensional measure. EClinicalMedicine. (2021) 40:101092. doi: 10.1016/j.eclinm.2021.101092
30. Key, KD, Furr-Holden, D, Lewis, EY, Cunningham, R, Zimmerman, MA, Johnson-Lawrence, V, et al. The continuum of community engagement in research: a roadmap for understanding and assessing progress. Prog Community Health Partnersh. (2019) 13:427–34. doi: 10.1353/cpr.2019.0064
31. Watson-Thompson, J, Collie-Akers, V, Woods, N, Anderson-Carpenter, KD, Jones, MD, and Taylor, EL. (first Edition) Participatory approaches for conducting community needs and resources assessments. Scott, V C and Wolfe, S M editors. Community Psychology. SAGE Publications, Thousand Oaks, California, USA (2015):157–88. doi: 10.4135/9781483398150.n6
32. Anderson-Carpenter, KD, Watson-Thompson, J, Jones, M, and Chaney, L. Using communities of practice to support implementation of evidence-based prevention strategies. J Community Pract. (2014) 22:176–88. doi: 10.1080/10705422.2014.901268
33. Snodgrass, MR, Chung, MY, Kretzer, JM, and Biggs, EE. Rigorous assessment of social validity: a scoping review of a 40-year conversation. Remedial Spec Educ. (2022) 43:114–30. doi: 10.1177/07419325211017295
34. Francisco, VT, and Butterfoss, FD. Social validation of goals, procedures, and effects in public health. Health Promot Pract. (2007) 8:128–33. doi: 10.1177/1524839906298495
35. Ricard, JA, Parker, TC, Dhamala, E, Kwasa, J, Allsop, A, and Holmes, AJ. Confronting racially exclusionary practices in the acquisition and analyses of neuroimaging data. Nat Neurosci. (2022) 26:4–11. doi: 10.1038/s41593-022-01218-y
36. Marek, S, Tervo-Clemmens, B, Calabro, FJ, Montez, DF, Kay, BP, Hatoum, AS, et al. Reproducible brain-wide association studies require thousands of individuals. Nature. (2022) 603:654–60. doi: 10.1038/s41586-022-04492-9
37. Sue, S, and Dhindsa, MK. Ethnic and racial health disparities research: issues and problems. Health Educ Behav. (2006) 33:459–69. doi: 10.1177/1090198106287922
38. Cardenas-Iniguez, C, and Gonzalez, MR. Recommendations for the responsible use and communication of race and ethnicity in neuroimaging research. Nat Neurosci. (2024) 27:615–28. doi: 10.1038/s41593-024-01608-4
39. Tervo-Clemmens, B, Marek, S, and Barch, DM. Tailoring psychiatric neuroimaging to translational goals. JAMA Psychiatry. (2023) 80:765–6. doi: 10.1001/jamapsychiatry.2023.1416
40. Rebello, V, and Uban, KA. A call to leverage a health equity lens to accelerate human neuroscience research. Front Integr Neurosci. (2023) 17:1035597. doi: 10.3389/fnint.2023.1035597
41. Cooke, NJ, and Hilton, ML (2015). Committee on the science of team science, board on behavioral, cognitive, and sensory sciences, division of behavioral and social sciences and…. Enhancing the effectiveness of team science.
42. Cooper, SM, Hurd, NM, and Loyd, AB. Advancing scholarship on anti-racism within developmental science: reflections on the special section and recommendations for future research. Child Dev. (2022) 93:619–32. doi: 10.1111/cdev.13783
43. Furtado, K, Rao, N, Payton, M, Brown, K, Balu, R, and Dubay, L (2023). Measuring structural racism. Available at: https://www.urban.org/sites/default/files/2023-08/Measuring%20Structural%20Racism%20Approaches%20from%20the%20Health%20Literature.pdf
44. Boyd, RW, Lindo, EG, Weeks, LD, and McLemore, M.R. (2020). On racism: a new standard for publishing on racial health inequities. Health Affairs Forefront. Available at: https://www.healthaffairs.org/content/forefront/racism-new-standard-publishing-racial-health-inequities (Accessed February 8, 2024).
45. Matsui, EC, Perry, TT, and Adamson, AS. An antiracist framework for racial and ethnic health disparities research. Pediatr Int. (2020) 146:1–3. doi: 10.1542/peds.2020-018572
46. Bryant, BE, Jordan, A, and Clark, US. Race as a social construct in psychiatry research and practice. JAMA Psychiatry. (2022) 79:93–4. doi: 10.1001/jamapsychiatry.2021.2877
47. Webb, EK, Cardenas-Iniguez, C, and Douglas, R. Radically reframing studies on neurobiology and socioeconomic circumstances: a call for social justice-oriented neuroscience. Front Integr Neurosci. (2022) 16:958545. doi: 10.3389/fnint.2022.958545
48. Krieger, N, and Davey, SG. The tale wagged by the DAG: broadening the scope of causal inference and explanation for epidemiology. Int J Epidemiol. (2016) 45:1787–808. doi: 10.1093/ije/dyw114
49. Cardenas-Iniguez, C, Schachner, JN, Ip, KI, Schertz, KE, Gonzalez, MR, Abad, S, et al. Building towards an adolescent neural urbanome: expanding environmental measures using linked external data (LED) in the ABCD study. Dev Cogn Neurosci. (2024) 65:101338. doi: 10.1016/j.dcn.2023.101338
50. Barnett, ML, Meara, E, Lewinson, T, Hardy, B, Chyn, D, Onsando, M, et al. Racial inequality in receipt of medications for opioid use disorder. N Engl J Med. (2023) 388:1779–89. doi: 10.1056/NEJMsa2212412
51. Kariisa, M, Davis, NL, Kumar, S, Seth, P, Mattson, CL, Chowdhury, F, et al. Vital signs: drug overdose deaths, by selected sociodemographic and social determinants of health characteristics—25 states and the District of Columbia, 2019-2020. MMWR Morb Mortal Wkly Rep. (2022) 71:940–7. doi: 10.15585/mmwr.mm7129e2
52. Larochelle, MR, Slavova, S, Root, ED, Feaster, DJ, Ward, PJ, Selk, SC, et al. Disparities in opioid overdose death trends by race/ethnicity, 2018-2019, from the HEALing communities study. Am J Public Health. (2021) 111:1851–4. doi: 10.2105/AJPH.2021.306431
53. Holzer, J, and Kass, N. Understanding the supports of and challenges to community engagement in the CTSAs. Clin Transl Sci. (2015) 8:116–22. doi: 10.1111/cts.12205
54. Jones, CP. Invited commentary: “race,” racism, and the practice of epidemiology. Am J Epidemiol. (2001) 154:357–65. doi: 10.1093/aje/154.4.357
Keywords: antiracism, research, J-DEI, equity, substance use, critical race theory (CRT), racialization, racism
Citation: Lehman J, Balangoy D, Mejia AP, Cardenas-Iniguez C, Marek S and Randolph AC (2024) Negligence in biomedical research: an anti-racist approach for substance use researchers. Front. Public Health. 12:1401221. doi: 10.3389/fpubh.2024.1401221
Edited by:
Shabbar I. Ranapurwala, University of North Carolina at Chapel Hill, United StatesReviewed by:
M. Barton Laws, Brown University, United StatesCopyright © 2024 Lehman, Balangoy, Mejia, Cardenas-Iniguez, Marek and Randolph. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jonathan Lehman, bGVobWEzMjlAdW1uLmVkdQ==: Danniella Balangoy, YmFsYW4wMTdAdW1uLmVkdQ==
†These authors have contributed equally to this work and share first authorship
 Jonathan Lehman
Jonathan Lehman Danniella Balangoy
Danniella Balangoy Angie P. Mejia
Angie P. Mejia Carlos Cardenas-Iniguez
Carlos Cardenas-Iniguez Scott Marek
Scott Marek Anita C. Randolph
Anita C. Randolph