- 1School of Public Health, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan Teferi, Ethiopia
- 2School of Medicine, Faculty of Health, Deakin University, Waurn Ponds, VIC, Australia
- 3Department of Emergency Medicine, Mizan-Aman College of Health Sciences, Mizan Teferi, Ethiopia
- 4Department of Medical Laboratory Science, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan Teferi, Ethiopia
- 5School of Exercise and Nutrition Sciences, Institute for Physical Activity and Nutrition, Deakin University, Melbourne, VIC, Australia
- 6Division of Public Health Sciences, Department of Surgery, Washington University School of Medicine, St Louis, MO, United States
- 7School of Public Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
Background: Abdominal obesity, excess fat around the abdomen, is more harmful than other fat types and is a key diagnostic criterion for metabolic syndrome. It poses a growing global public health concern. This study aimed to assess the prevalence of and determinants of abdominal obesity among adults in southwest Ethiopia.
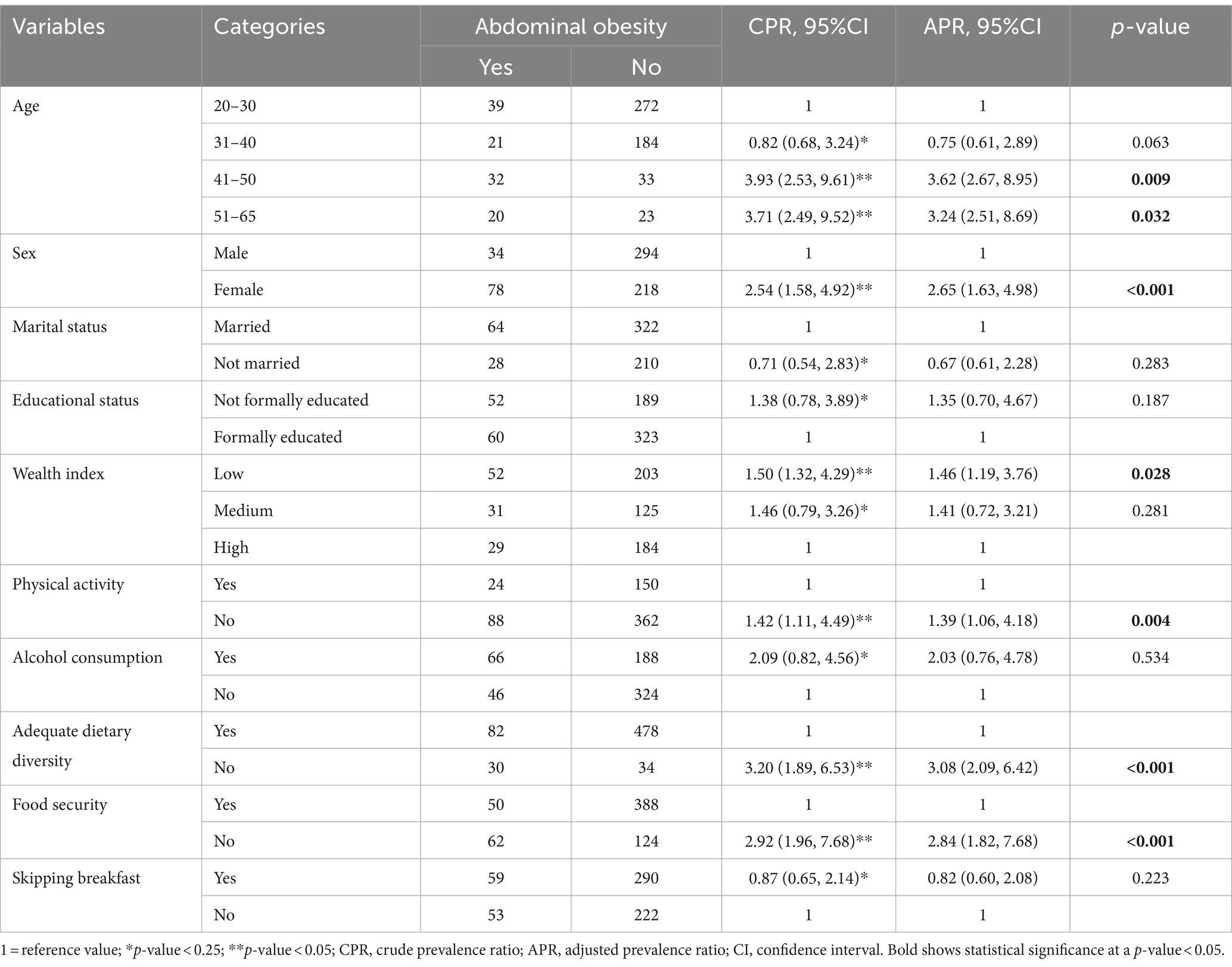
Methods: A cross-sectional study involving 624 adults in Semen Bench district, southwest Ethiopia was conducted from May 23 to June 23, 2022. The data was gathered using questionnaires and anthropometric measurements. The data were analyzed using Stata version 18. A robust Poisson regression was used due to the abdominal obesity prevalence exceeding 10%. Variables with p-values < 0.25 in the bivariate analysis were included in the multivariable analysis. The adjusted prevalence ratio (APR) and 95% confidence interval were reported to indicate statistical significance and the strength of associations.
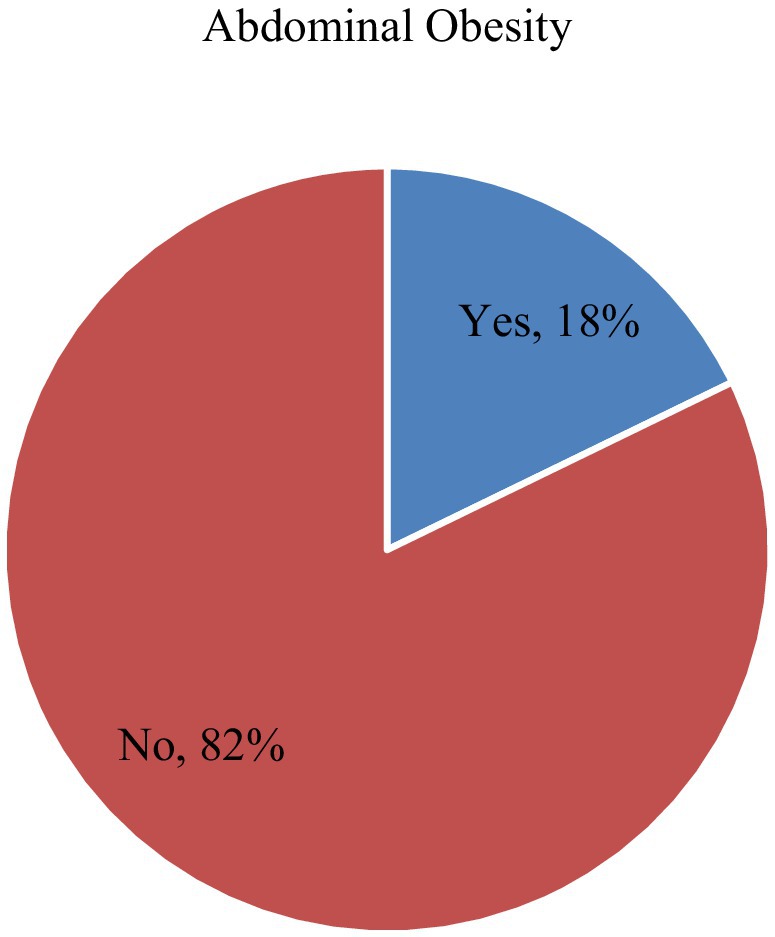
Results: The prevalence of abdominal obesity was 18% (95% CI: 15–21%). After adjusting for confounding variables, the determinants of abdominal obesity included participants aged 31–50 (APR = 3.62, 95% CI: 2.67–8.95) and 51–65 (APR = 3.24, 95% CI: 2.51–8.69), being female (APR = 2.65, 95% CI: 1.63–4.98), having a low wealth index (APR = 1.46, 95% CI: 1.19–3.76), physical inactivity (APR = 1.39, 95% CI: 1.06–4.18), lack of adequate dietary diversity (APR = 3.08, 95% CI: 2.09–6.42), and food insecurity (APR = 2.84, 95% CI: 1.82–7.68).
Conclusion: The research revealed that 18% of the participants exhibited abdominal obesity. Factors such as advanced age, being female, having a low wealth index, physical inactivity, insufficient dietary diversity, and food insecurity were identified as contributors to abdominal obesity. Therefore, it is crucial to develop targeted interventions to address modifiable factors, as this can also help prevent the onset of non-communicable chronic diseases associated with abdominal obesity.
Introduction
The World Health Organization (WHO) states that obesity is one of the most prevalent public health issues. Yet, it remains one of the most overlooked, affecting both developed and developing countries (1). Obesity is the excessive fat buildup that can impair overall health (2). Obesity has become a major global health problem, with its prevalence more than doubling since 1980 (1). Obesity, once considered an issue exclusive to high-income countries, has rapidly increased in low- and middle-income nations over the past 30 years (3). In low and middle-income countries, a significant portion of the adult population, particularly in urban areas, is affected by overweight and obesity (4, 5).
Obesity can be classified as general or abdominal. General obesity is defined by body mass index (BMI). Abdominal obesity is determined by waist circumference (WC) or waist-to-hip ratio (WHR) (6). Abdominal obesity, characterized by the accumulation of fat in the abdominal area, has risen markedly in recent years, leading to increased health risks (7). This type of fat is particularly detrimental compared to others and serves as a crucial indicator in diagnosing metabolic syndrome (8). Abdominal obesity is known to harm health, increasing the risk of diabetes, hypertension, dyslipidemia, cardiovascular disease, stroke, and cancer (9). Abdominal obesity is notably associated with increased mortality in all weight categories (10).
In Sub-Saharan Africa, abdominal obesity is increasing, with higher rates in urban areas compared to rural ones. It is often viewed as a sign of affluence and respect (11). Multiple studies in West Africa have reported abdominal obesity prevalence rates ranging from 22.5 to 50.8% (12–14). Several studies in East Africa have revealed that the prevalence of abdominal obesity ranges from 11.8 to 67.8% (15–19).
Overeating energy-dense foods increases the risk of abdominal obesity, common in sedentary modern lifestyles (20). Various factors contributing to abdominal obesity include sociodemographic aspects like age (13, 17, 21–24), gender (21, 25), wealth index (21, 23–25), marital (22–24), and educational status (15, 23), and place of residence (15, 22, 26). Behavioral factors such as sedentary lifestyles (22, 26), alcohol use and smoking habits (26, 27), fast food consumption (24), reduced physical activity (21, 25, 26), dietary diversity (23, 25), low intake of fruits and vegetables, and higher consumption of processed foods (28), and snacking habits (23) also play significant roles. Additionally, comorbidities such as hypertension (13, 15, 21), overweight, obesity (13, 21), and knowledge about obesity (24) contribute to this condition across different studies.
Ethiopia is experiencing a significant rise in obesity rates (29). Abdominal obesity, specifically, is becoming more common across the country, with reported prevalence rates ranging from 16.5 to 28.4% (23–25). However, specific evidence regarding this issue in the study area is currently lacking. Thus, this study aimed to determine the prevalence of abdominal obesity and explore its determinants among adults in southwest Ethiopia.
Methods
Study setting, design, and period
A community-based cross-sectional survey was conducted among adults residing in the Semen Bench district, Bench Sheko zone in southwest Ethiopia from May 23 to June 23, 2022. Semen Bench district is one of the 10 decentralized districts in the Bench Sheko zone. It is located 17 km from the zonal administration town of Mizan-Aman and 568 km southwest of Ethiopia’s capital, Addis Ababa. The residents primarily rely on crop cultivation and livestock breeding for their livelihoods.
Populations
The source population included all adults aged ≥18 years in the Semen Bench district, while the study population consisted of randomly selected adults who had lived there for at least 6 months during data collection. Exclusions included women who gave birth in the last 6 months, and adults with abdominal distension, severe illness, communication barriers, or physical deformities affecting measurement.
Sample size determination and sampling technique
The sample size was calculated using the formula for a single population proportion, assuming a 95% confidence level and a 5% margin of error, with a prevalence of abdominal obesity at 24.4% (25). Adjustments were made for a 10% non-response rate and a design effect of 2. The final sample size was 624. A stratified sampling technique was used, dividing the district into urban, semi-urban, and rural kebeles. One-third of kebeles from urban and semi-urban were randomly selected. The total households in each kebele were divided by the allocated sample sizes to determine sampling intervals (k). A random start was chosen by lottery, and every kth household from the random start was included until the required sample size was reached.
Data collection tools, and procedures
The study used a modified questionnaire adapted from the WHO-STEP approach for chronic non-communicable diseases (30). All participants underwent interviews, and multiple anthropometric measurements were conducted, with recorded averages. Waist and hip circumference were measured to the nearest 0.1 cm using a tape measuring, and the waist-to-hip ratio was then calculated. Principal component analysis was used to compute the household wealth index. The wealth index was divided into higher, medium, and lower categories (31). The study used the Household Food Insecurity Access Scale (HFIAS) to assess household food insecurity. Participants answered nine questions about their household’s food experiences in the past 30 days, focusing on worry about food access (1 question), food quality (3 questions), and inadequate food intake and its effects (5 questions). Responses were scored from 0 to 3 based on frequency: 0 for never, 1 for rarely (once or twice), 2 for sometimes (three to 10 times), and 3 for often (more than 10 times). A score of 27 indicates severe food insecurity, while lower scores indicate greater food security (32). The Food Frequency Questionnaire (FFQ) assessed participants’ dietary habits across eight categories: meat, eggs, fish, fat-rich foods, vegetables, fruits, dairy products, and sweets. Consuming four or more food categories within 24 h in households indicates sufficient dietary diversity, whereas consuming fewer than four food types within the same timeframe suggests insufficient diversity (33). A pretest involving 5% of the sample was conducted in Mizan Aman town before data collection. Additionally, comprehensive training was provided to data collectors and supervisors to ensure the questionnaire was administered consistently and clearly.
Study variables
The study considered abdominal obesity as the dependent variable. Independent variables included sociodemographic factors (age, sex, marital status, education, occupation, family size, wealth index, and place of residence), behavioral characteristics (alcohol consumption, cigarette smoking, khat chewing, and physical activity), and nutritional factors (dietary diversity, household food security, dining out of home, skipping breakfast, snacking habits, fruit and vegetable intake).
Operational definitions
A waist-to-hip ratio above 0.85 for women and 0.90 for men indicates abdominal obesity (34). Alcohol drinkers: those who drink alcohol (beer, local beer or areke, tella, or tej) daily or every other day (35, 36). Cigarette smokers: those who smoke daily, regardless of the number (35–37).
Khat (Catha edulis) is a stimulant derived from the fresh leaves of the Catha edulis shrub, native to East Africa and southern Arabia. Khat chewers: those who chew khat at least once per week (35, 36). Physically active: participants with 3+ days of physical activity (walking, running, bicycling, and stretching exercises such as sit-ups and pull-ups) (30 min/day) per week (36). A snack was characterized as consuming extra food items such as dabo kolo (small pieces of baked bread resembling pretzels), kolo (roasted barley, sometimes mixed with other local grains), sambusas (fried or baked pastries filled with lentils, meat, or vegetables), as well as bread and fruits (such as mangoes, papayas, and bananas), between the three main meals of the day, regardless of quantity (38).
Statistical analysis
The data were analyzed using Stata version 18 (Stata Corp. 2023. Stata Statistical Software: Release 18. College Station, TX: Stata Corp LLC). Continuous variables were assessed for normality, normally distributed variables were summarized using means and standard deviations (SD), while non-normally distributed variables were summarized using medians and interquartile ranges (IQR). Categorical variables were summarized using frequencies and percentages. This research utilized a cross-sectional design and identified that the prevalence of abdominal obesity was over 10%. Given that the odds ratio could overstate the relationship between abdominal obesity and the independent variables in such instances, the prevalence ratio was deemed a more accurate measure of association. To determine the predictors of abdominal obesity, a Poisson regression with robust variance was applied. Variables with a p-value < 0.25 in the initial bivariate analysis were included in the multivariable model. The model’s fit was evaluated using deviance, and the model with the lowest deviance was selected as the best fit. The study reported the Adjusted Prevalence Ratio (APR) along with its 95% confidence interval (CI), and considered variables with a p-value < 0.05 in the multivariable analysis as significant predictors of abdominal obesity.
Results
Sociodemographic and economic characteristics
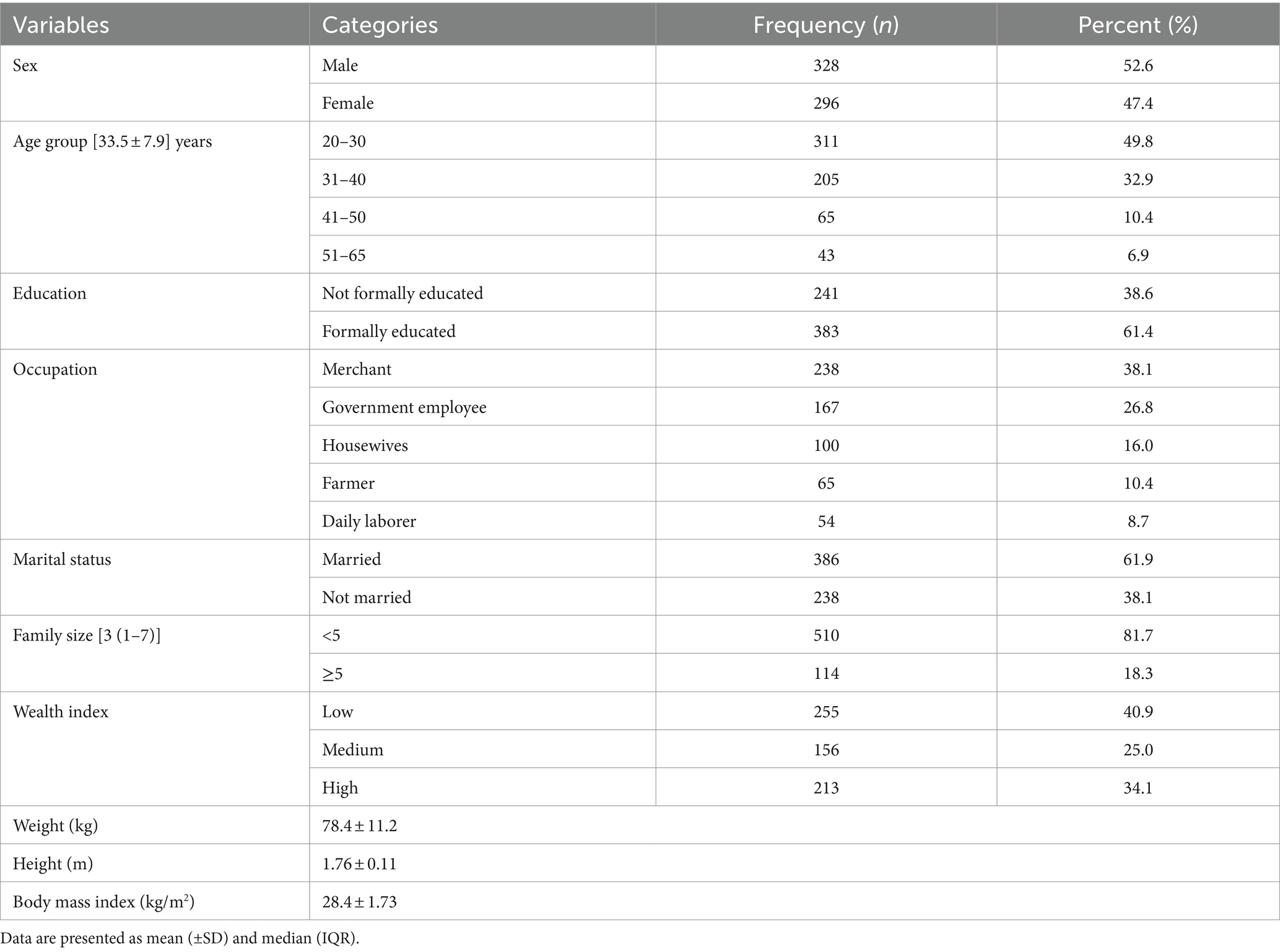
All respondents participated in the study, achieving a 100% response rate. Of 624 participants, 47.4% were female. The average age of participants was 33.5 (SD ± 7.9) years, with half falling between 20 and 30 years old. The median family size was 3 (IQR 1–7). Additionally, 18.3% of participants lived in households with five or more members. Out of the participants, 383 (61.4%) had formal education, and 255 (40.9%) were categorized as having a low wealth index (Table 1).
Behavioral, nutrition-related characteristics and prevalence of abdominal obesity
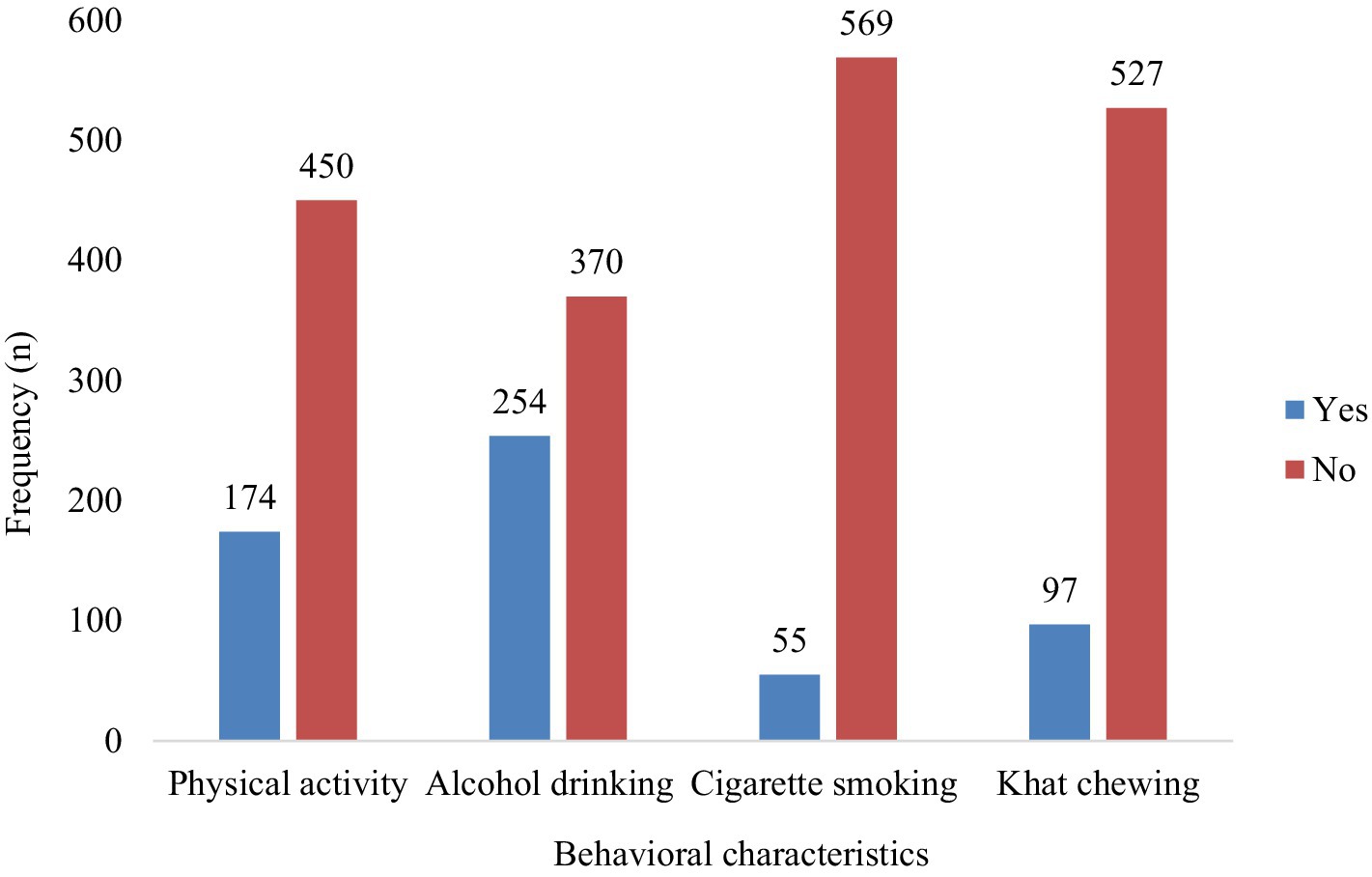
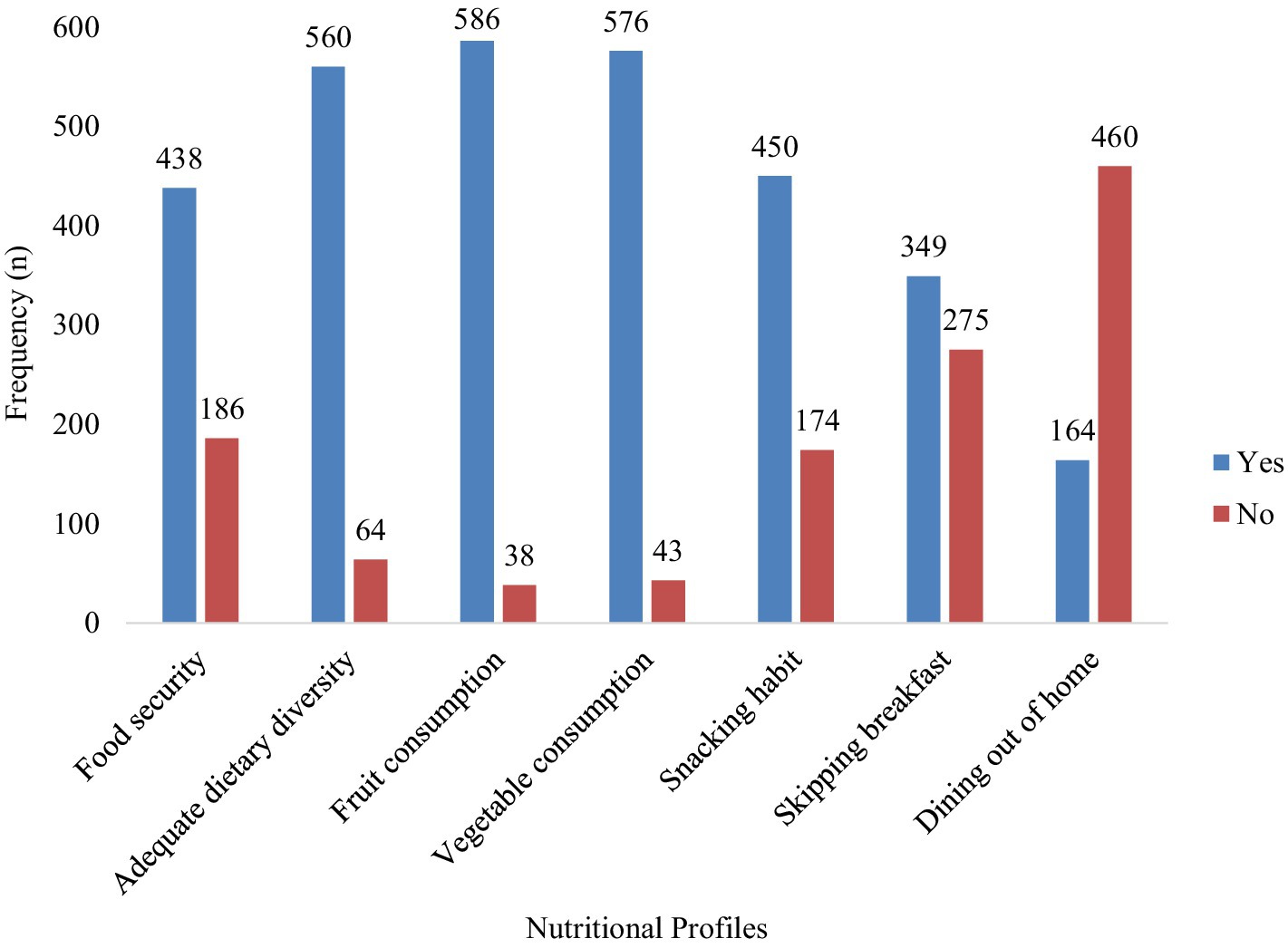
Among participants, 40.7% reported drinking alcohol, 8.8% smoked cigarettes, 15.6% chewed khat, and 27.9% engaged in physical activity (Figure 1). In the study, 70.2% of the participants were from food-secure households. Additionally, 72.1% had a snacking habit, 63.1% skipped breakfast, and the consumption rates for fruit, and vegetables were 93.9, and 92.3%, respectively (Figure 2). The prevalence of abdominal obesity was 18% (95% CI: 15–21%) (Figure 3).
Factors associated with abdominal obesity
After adjusting for confounding variables, the determinants of abdominal obesity included participants aged 31–50 (APR = 3.62, 95% CI: 2.67–8.95) and 51–65 (APR = 3.24, 95% CI: 2.51–8.69), being female (APR = 2.65, 95% CI: 1.63–4.98), having a low wealth index (APR = 1.46, 95% CI: 1.19–3.76), physical inactivity (APR = 1.39, 95% CI: 1.06–4.18), lack of adequate dietary diversity (APR = 3.08, 95% CI: 2.09–6.42), and food insecurity (APR = 2.84, 95% CI: 1.82–7.68) (Table 2).
Discussion
This study sought to assess the prevalence of abdominal obesity and its determinants among adults in the Semen Bench district, in southwest Ethiopia. The prevalence of abdominal obesity was 18% (95% CI: 15–21%). Factors associated with abdominal obesity included age, sex, wealth index, physical activity, dietary diversity, and food security.
The prevalence of abdominal obesity (18%) in this study aligned with findings from Woldia, Ethiopia (16.5%) (23). It was higher than rates reported in Uganda (11.8%) (15) but lower than those in Dilla (24.4%) (25), Nekemte (28.4%) (24), and Bale Zone (39.0%) (39) in Ethiopia, as well as Abia State, Nigeria (21.8%) (40), and Tanzania (24.9%) (22). Variations in abdominal obesity prevalence across studies stem from differences in sampled populations, methodological discrepancies like sample size and measurement techniques (24, 39), geographical and cultural influences on diet and physical activity, disparities in healthcare access and economic development, and evolving lifestyle behaviors and healthcare interventions targeting obesity.
The age of participants is significantly associated with abdominal obesity. Participants aged 41–50 and 51–65 years had increased prevalence of abdominal obesity compared to those aged 20–30 years. This finding was supported by other studies somewhere (13, 17, 21–24). This could be explained by the fact that advanced age is associated with abdominal obesity due to slower metabolism, muscle loss, hormonal changes, reduced physical activity, and fat redistribution to the abdominal region.
This study revealed a significant association between sex and abdominal obesity. Female participants had a higher prevalence of abdominal obesity compared to males, a finding supported by other studies elsewhere (21, 23, 25, 27, 41). This can be explained by the fact that females tend to develop abdominal obesity due to higher estrogen levels, sedentary lifestyles influenced by cultural roles, effects of pregnancy and childbirth, dietary habits that increase fat intake, and genetic predispositions to store abdominal fat (42). Traditional gender roles in Ethiopian culture often lead women to engage in less physically demanding activities than men.
Individuals with a low wealth index had a higher prevalence of abdominal obesity compared to those with a high wealth index, a finding supported by other studies (21, 23–25). Low wealth can lead to the consumption of inexpensive, unhealthy foods, increasing the risk of abdominal obesity. Lee et al. (43) found that poor-quality diets lacking nutrients may also contribute to abdominal fat accumulation.
Physical activity is significantly associated with abdominal obesity. Physically inactive participants were more likely to be abdominally obese compared to physically active participants. This finding was consistent with other studies elsewhere (21, 25, 26). Physical inactivity leads to abdominal obesity by reducing energy expenditure, metabolism, and insulin sensitivity while disrupting hormonal balance, promoting muscle loss, and increasing the risk of metabolic and cardiovascular diseases linked to abdominal fat accumulation (44). Exercise helps fight belly fat by burning calories and boosting metabolism.
Participants who were food-insecure had a higher prevalence of abdominal obesity compared to their counterparts. This finding was supported by other studies (45, 46). Food insecurity is linked to abdominal obesity due to irregular eating patterns and reliance on cheap, calorie-dense, nutrient-poor foods, leading to weight gain and abdominal fat (43, 47). Stress and anxiety from food insecurity can also cause overeating, further increasing obesity risk.
Participants with no dietary diversity were more likely to be abdominally obese compared to their counterparts. This finding was consistent with other studies (23, 25). A lack of dietary diversity is linked to abdominal obesity due to reliance on high-calorie, low-nutrient foods, leading to excess calorie intake and poor nutrition (43, 47). A diverse diet, rich in fruits, vegetables, whole grains, and lean proteins, helps maintain a healthy weight and prevent obesity.
Over 90% of participants in the area consumed fruits and vegetables, a higher rate than 67.87% in Jimma town (38). This difference may be attributed to the area’s abundant fruit and vegetable production, supported by year-round rainfall. Eating fruits and vegetables can reduce abdominal obesity by providing low-calorie, high-fiber, and nutrient-dense options that promote fullness and digestion. They also support overall health, improve metabolism and insulin sensitivity, and help decrease the intake of high-calorie, processed foods (48). Additionally, their high water content aids in hydration and satiety. Given these benefits, health education campaigns should be developed to raise community awareness about the importance of consuming fruits and vegetables to reduce the incidence of abdominal obesity.
Strength and limitations
This study stands out for its novelty as the first of its kind in the area, offering valuable insights and baseline data for informing future research and public health interventions. Additional strengths include using a modified standard tool, achieving a 100% response rate, and employing a random sampling method. However, its focus on a single area limits the generalization of the findings to other regions or populations. Additionally, the cross-sectionality of the study presents a limitation, as it captures data at a single point in time, making it difficult to establish causal relationships or temporal links between variables. Relying on self-reported data for physical activity, dietary diversity, and food insecurity may introduce recall bias and affect accuracy in assessing associations with abdominal obesity. Longitudinal studies would be needed to understand the dynamics and causation of the observed factors.
Conclusion
The study found that 18% of participants had abdominal obesity, influenced by factors such as advanced age, female gender, low wealth index, physical inactivity, inadequate dietary diversity, and food insecurity. Addressing the modifiable factors through targeted interventions is crucial to preventing non-communicable chronic diseases associated with abdominal obesity, including cardiovascular disorders, type 2 diabetes, and certain cancers. Promoting physical activity, improving dietary habits, and addressing socioeconomic disparities can significantly reduce the burden of abdominal obesity and enhance overall public health outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Mizan-Tepi University College of Medicine and Health Sciences research and community service review committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
TY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing. AS: Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – original draft, Writing – review and editing. ET: Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – original draft, Writing – review and editing. BS: Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – original draft, Writing – review and editing. BB: Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – original draft, Writing – review and editing. AT: Formal analysis, Investigation, Project administration, Software, Supervision, Visualization, Writing – original draft, Writing – review and editing. NS: Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ng, M, Fleming, T, Robinson, M, Thomson, B, Graetz, N, Margono, C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet. (2014) 384:766–81. doi: 10.1016/S0140-6736(14)60460-8
2. Ellulu, MS, Patimah, I, Khaza’ai, H, Rahmat, A, and Abed, Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. (2017) 4:851–63. doi: 10.5114/aoms.2016.58928
3. Ogden, CL, Fryar, CD, Hales, CM, Carroll, MD, Aoki, Y, and Freedman, DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA. (2018) 319:2410–8. doi: 10.1001/jama.2018.5158
4. Fikre, A, Shehmolo, M, BotiI, N, Oumer, B, Tenalem, B, Kibru, S, et al. Magnitude and risks of overweight/obesity among adults in Welkite town, southern Ethiopia: A community based cross-sectional study. PLoS One. (2022) 17:e0275014. doi: 10.1371/journal.pone.0275014
5. Ellulu, M, Abed, Y, Rahmat, A, Ranneh, Y, and Ali, F. Epidemiology of obesity in developing countries: challenges and prevention. Glob Epidemic Obes. (2014) 2:1–6. doi: 10.7243/2052-5966-2-2
6. Park, S, and Baek, KA. Association of General Obesity and Abdominal Obesity with the prevalence of urinary incontinence in women: cross-sectional secondary data analysis. Iran J Public Health. (2018) 47:830–7.
7. Dhawana, D, and Sharma, S. Abdominal obesity, Adipokines and non-communicable diseases. J Steroid Biochem Mol Biol. (2020) 203:105737. doi: 10.1016/j.jsbmb.2020.105737
8. Sahakyan, KR, Somers, VK, Rodriguez-Escudero, JP, Hodge, DO, Carter, RE, Sochor, O, et al. Normal-weight central obesity: implications for Total and cardiovascular mortality. Ann Intern Med. (2015) 163:827–35. doi: 10.7326/M14-2525
9. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects)Lu, Y, Hajifathalian, K, Ezzati, M, Woodward, M, Rimm, EB, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet (London, England). (2014) 383:970–83. doi: 10.1016/S0140-6736(13)61836-X,
10. Cerhan, JR, Moore, SC, Jacobs, EJ, Kitahara, CM, Rosenberg, PS, Adami, H-O, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin Proc. (2014) 89:335–45. doi: 10.1016/j.mayocp.2013.11.011
11. SNAIB, EJ. Increasing obesity in Ugandan women due to transition from rural to urban living conditions? A qualitative study on traditional body image, changed lifestyles and unawareness of risk for heart disease. J Res Obes. (2015) 2015:213083:1–13. doi: 10.5171/2015.213083
12. Cisse, K, Samadoulougou, S, Ouedraogo, M, Kouanda, S, and Kirakoya-Samadoulougou, F. Prevalence of abdominal obesity and its association with cardiovascular risk among the adult population in Burkina Faso: findings from a nationwide cross-sectional study. BMJ Open. (2021) 11:e049496. doi: 10.1136/bmjopen-2021-049496
13. Malik, SK, Kouame, J, Gbane, M, Coulibaly, M, Ake, MD, and Ake, O. Prevalence of abdominal obesity and its correlates among adults in a peri-urban population of West Africa. AIMS Public Health. (2019) 6:334–44. doi: 10.3934/publichealth.2019.3.334
14. Bashir, MAYA, Muhammad, M, Yusuf, AH, and Mukhtar, IG. Prevalence of central obesity in Nigeria: a systematic review and meta-analysis. Public Health. (2022) 206:87–93. doi: 10.1016/j.puhe.2022.02.020
15. Kabwama, SKB, Mutungi, G, Wesonga, R, and Bahendeka, SGD. BMC obesity, 5, 40. Prevalence and correlates of abdominal obesity among adults in Uganda: findings from a national cross-sectional, population based survey. BMC Obes. (2014) 5:40. doi: 10.1186/s40608-018-0217-1
16. Achila, OO, Araya, M, Berhe, AB, Haile, NH, Tsige, LK, Shifare, BY, et al. Metabolic syndrome, associated factors and optimal waist circumference cut points: findings from a cross-sectional community-based study in the elderly population in Asmara, Eritrea. BMJ Open. (2022) 12:e052296. doi: 10.1136/bmjopen-2021-052296
17. Mohamed, SFHT, Khayeka-Wandabwa, C, Muthuri, SK, and Kyobutungi, C. Magnitude and predictors of normal-weight central obesity- the AWI-gen study findings. Glob Health Action. (2019) 12:1685809. doi: 10.1080/16549716.2019.1685809
18. Omar, SM, Taha, Z, Hassan, AA, Al-Wutayd, O, and Adam, I. Prevalence and factors associated with overweight and central obesity among adults in the eastern Sudan. PLoS One. (2020) 15:e0232624. doi: 10.1371/journal.pone.0232624
19. Munyogwa, MJ, Ntalima, KS, and Kapalata, SN. Setting - based prevalence and correlates of central obesity: findings from a cross-sectional study among formal sector employees in Dodoma City, Central Tanzania. BMC Public Health. (2021) 21:97. doi: 10.1186/s12889-020-10142-4
20. Żukiewicz-Sobczak, W, Wróblewska, P, Zwoliński, J, Chmielewska-Badora, J, Adamczuk, P, Krasowska, E, et al. Obesity and poverty paradox in developed countries. Ann Agric Environ Med. (2014) 21:590–4. doi: 10.5604/12321966.1120608
21. Tegegne, KDWG, Gebeyehu, NA, Yirdaw, LT, Shewangashaw, NE, Mekonen, NA, and Kassaw, MW. Prevalence of central obesity and associated factors in Ethiopia: A systematic review and meta-analysis. Front Endocrinol (Lausanne). (2022) 13:983180. doi: 10.3389/fendo.2022.983180
22. Munyogwa, MJ, and Mtumwa, AH. The prevalence of abdominal obesity and its correlates among the adults in Dodoma region, Tanzania: A community-based cross-sectional study. Adv Med. (2018) 2018:1–8. doi: 10.1155/2018/6123156
23. Dagne, S, Menber, Y, Petrucka, P, and Wassihun, Y. Prevalence and associated factors of abdominal obesity among the adult population in Woldia town, Northeast Ethiopia, 2020: community-based cross-sectional study. PLoS One. (2021) 16:e0247960. doi: 10.1371/journal.pone.0247960
24. Biru, B, Tamiru, D, Taye, A, and Feyisa, BR. Central obesity and its predictors among adults in Nekemte town, West Ethiopia. SAGE Open Med. (2021) 9:205031212110549–9. doi: 10.1177/20503121211054988
25. Tesfaye, TS, Zeleke, TM, Alemu, W, Argaw, D, and Bedane, TK. Dietary diversity and physical activity as risk factors of abdominal obesity among adults in Dilla town, Ethiopia. PLoS One. (2020) 15:e0236671. doi: 10.1371/journal.pone.0236671
26. Jensen, MD, Ryan, DH, Apovian, CM, Ard, JD, Comuzzie, AG, Donato, KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Obesity Society. Circulation. (2014) 129:S102–38. doi: 10.1161/01.cir.0000437739.71477.ee
27. Raimi, TH, Odusan, O, and Fasanmade, O. High prevalence of central obesity in rural South-Western Nigeria: need for targeted prevention. J Diab Endocrinol. (2015) 6:12–8. doi: 10.5897/JDE2015.0084
28. Bosu, WK. An overview of the nutrition transition in West Africa: implications for non-communicable diseases. Proc Nutr Soc. (2015) 74:466–77. doi: 10.1017/S0029665114001669
29. Kassie, AM, Abate, BB, and Kassaw, MW. Prevalence of overweight/obesity among the adult population in Ethiopia: a systematic review and meta-analysis. BMJ Open. (2020) 10:e039200. doi: 10.1136/bmjopen-2020-039200
30. World Health Organization. Noncommunicable diseases and mental health cluster. WHO STEPS surveillance manual: The WHO STEPwise approach to chronic disease risk factor surveillance / noncommunicable diseases and mental health, World Health Organization World Health Organization (2005).
31. Central Statistical Agency. Ethiopian demographic and health survey, 2016. Addis Ababa: The DHS Program. Rockville, Maryland: ICF (2017).
32. Coates, J, Swindale, A, and Bilinsky, P. Household food insecurity access scale (HFIAS) for measurement of food access: indicator guide (v.3). Washington, DC: FHI 360/FANTA (2007).
33. Mekuria, G, Wubneh, Y, and Tewabe, T. Household dietary diversity and associated factors among residents of Finote Selam town, north West Ethiopia: a cross sectional study. BMC Nutr. (2017) 3:1–6. doi: 10.1186/s40795-017-0148-0
34. World Health Organization. Technical report series −854. Physiacl status: The use and interpretation of Antropmetery. (1995).
35. Yosef, T, Belachew, A, and Tefera, Y. Magnitude and contributing factors of low Back pain among long distance truck drivers at Modjo dry port, Ethiopia: A cross-sectional study. J Environ Public Health. (2019) 2019:1–7. doi: 10.1155/2019/6793090
36. Yosef, T. Prevalence and associated factors of chronic non-communicable diseases among cross-country truck drivers in Ethiopia. BMC Public Health. (2020) 20:1564. doi: 10.1186/s12889-020-09646-w
37. Yosef, T, Bogale, B, Destaw, A, and Weldu, A. The burden of overweight and obesity among long-distance truckers in Ethiopia. J Obes. (2020) 2020:1–6. doi: 10.1155/2020/4242789
38. Endale, F, Nigussie, A, Tamene, A, Habte, A, Ermias, D, Beyamo, A, et al. Abdominal obesity and associated factors among urban adults in Southwest Ethiopia: a communitybased cross-sectional study. Pan Afr Med J. (2024) 47:47. doi: 10.11604/pamj.2024.47.47.34746
39. Tekalegn, Y, Solomon, D, Sahiledengle, B, Assefa, T, Negash, W, Tahir, A, et al. Prevalence of central obesity and its associated risk factors among adults in Southeast Ethiopia: A community-based cross-sectional study. PLoS One. (2022) 17:e0265107. doi: 10.1371/journal.pone.0265107
40. Chukwuonye, II, Chuku, A, Onyeonoro, UU, Okpechi, IG, Madukwe, OO, Umeizudike, TI, et al. Prevalence of abdominal obesity in Abia state, Nigeria: results of a population-based house-to-house survey. Diab Metab Syndr Obes. (2013) 6:285–91. doi: 10.2147/DMSO.S43545
41. Eyitayo Omolara Owolabi DTGOVA. Central obesity and normal-weight central obesity among adults attending healthcare facilities in Buffalo City metropolitan municipality, South Africa. J Health Popul Nutr. (2017) 36:54. doi: 10.1186/s41043-017-0133-x
42. Barnes, AS. Obesity and sedentary lifestyles: risk for cardiovascular disease in women. Tex Heart Inst J. (2012) 39:224–7.
43. Lee, M-J, Yuanyuan, W, and Fried, SK. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Asp Med. (2013) 34:1–11. doi: 10.1016/j.mam.2012.10.001
44. Sanchez-Lastra, MA, Ding, D, Cruz, BDP, Dalene, KE, Ayán, C, Ekelund, U, et al. Joint associations of device-measured physical activity and abdominal obesity with incident cardiovascular disease: a prospective cohort study. Br J Sports Med. (2024) 58:196–203. doi: 10.1136/bjsports-2023-107252
45. Jafari, F, Ehsani, S, Nadjarzadeh, A, Esmaillzadeh, A, Noori-Shadkam, M, and Salehi-Abargouei, A. Household food insecurity is associated with abdominal but not general obesity among Iranian children. BMC Public Health. (2017) 17:350. doi: 10.1186/s12889-017-4262-3
46. Ponce-Alcala, RE, Luna, JLR-G, Shamah-Levy, T, and Melgar-Quiñonez, H. The association between household food insecurity and obesity in Mexico: a cross-sectional study of ENSANUT MC 2016. Public Health Nutr. (2021) 24:5826–36. doi: 10.1017/S1368980021003153
47. El-Jamal, S, Mziwira, M, Elfane, H, Sahel, K, Barakat, I, Kalili, A, et al. Association between food insecurity and obesity in an agricultural community of women from El Jadida, Morocco. AIMS Med Sci. (2021) 8:175–88. doi: 10.3934/medsci.2021016
Keywords: abdominal obesity, cross-sectional study, prevalence ratio, southwest Ethiopia, waist-to-hip ratio
Citation: Yosef T, Sebeta A, Tekalign E, Sisay BG, Bekele BB, Tesfaw A and Shifera N (2024) Assessment of abdominal obesity prevalence and determinants among adults in southwest Ethiopia: a cross-sectional study. Front. Public Health. 12:1400066. doi: 10.3389/fpubh.2024.1400066
Edited by:
Basil Nwaneri Okeahialam, University of Jos, NigeriaReviewed by:
Dewi Friska, University of Indonesia, IndonesiaShelly R. McFarlane, University of the West Indies, Mona, Jamaica
Copyright © 2024 Yosef, Sebeta, Tekalign, Sisay, Bekele, Tesfaw and Shifera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tewodros Yosef, dGV3b2Ryb3N5b3NlZjQ3QG10dS5lZHUuZXQ=
†ORCID: Tewodros Yosef, orcid.org/0000-0002-3173-6753
 Tewodros Yosef
Tewodros Yosef Asresash Sebeta3
Asresash Sebeta3