- 1Shandong Provincial Chronic Disease Hospital, Qingdao, China
- 2School of Public Health, Qingdao University, Qingdao, China
- 3Qilu Hospital, Shandong University, Jinan, China
- 4The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, International Healthcare Management Research and Development Centre (IHM-RDC), Jinan, China
- 5Henan Normal University, School of Social Affairs, Xinxiang, China
- 6Atlantica Instituto Universitario, Gestao em Saude, Oeiras, Portugal
- 7Qingdao University Archives, Qingdao, China
Objective: To ascertain the prevalence of asthma attacks among archivists and identify the associated occupational factors in this understudied professional population.
Methods: We conducted a cross-sectional, questionnaire-based study among 1,002 archival workers. A multiple logistic regression was conducted to identify the association between asthma attacks and occupational exposures. The Strobe Protocol was applied.
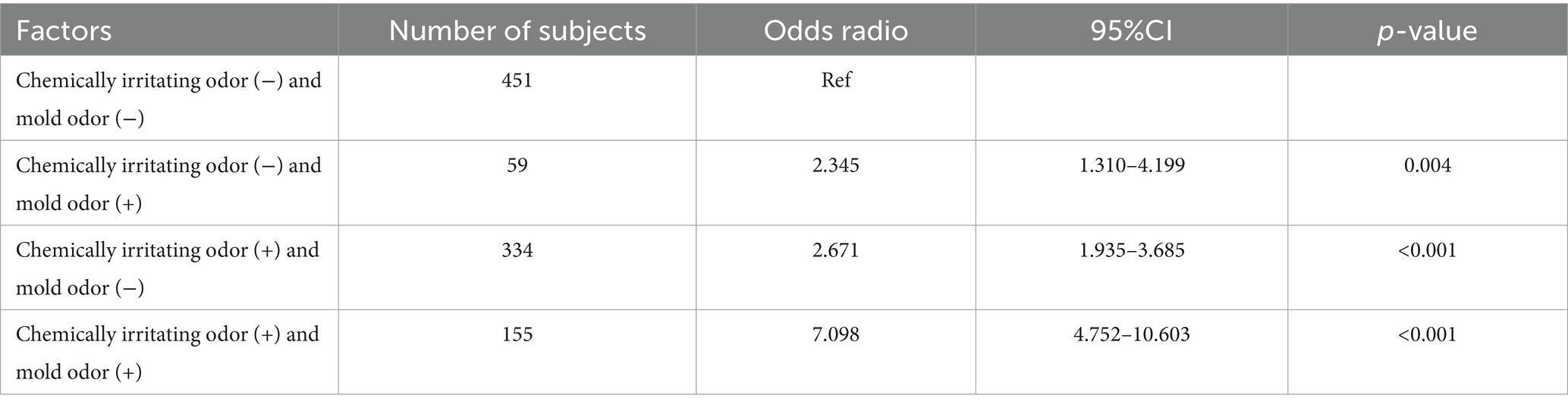
Results: 999 workers were included in the final analysis with the asthma prevalence of 33.3%. Main factors associated with asthma attacks (OR [95% CI]) were the presence of chemically irritating odors (2.152 [1.532–3.024]), mold odors (1.747 [1.148–2.658]), and insects (1.409[1.041–1.907]). A significant synergistic effect was observed between chemical irritants and mold, the odds ratio was 7.098 (95% CI, 4.752–10.603).
Conclusion: There was a high prevalence of asthma attacks among archival workers, an under-studied population. Chemical irritants, molds and insects were associated with their asthma attacks. Notably, this study’s data analysis has revealed a strong synergy (OR = 7.098) between chemical odors and molds in the workplace. While the existing international literature on this specific interaction remains somewhat limited, previous studies have already demonstrated the potential for chemical irritants, such as sulfur dioxide and ozone, to synergistically interact with inhalable allergens, including fungi, molds and dust mites. Consequently, this interaction seems to exacerbate asthma symptoms and perpetuate untreated exposure. Furthermore, in damp and damaged buildings, the presence of microbial components, such as cellular debris or spores released during fungal growth can trigger an inflammatory response, potentially served as a shared pathway for the development of asthma among individuals exposed to these hazardous factors.
1 Introduction
Asthma is a heterogeneous clinical syndrome that affects approximately 360 million people worldwide. Studies have found that up to 25% of adult asthma cases are work-related (1). The incidence does not appear to be decreasing (2), which leading to significant social and economic burdens. Recently, new cases of work related asthma due to workplace exposures in many sectors have been reported (3–5). Among all the workplaces, offices are not frequently associated with common agents for occupational asthma, office workers consequently remain a low risk of contracting occupational asthma (6, 7). Among all the workplaces, with relatively few exposure conditions associated with the incidence of occupational asthma, the risk of occupational asthma in the offices is low. However, A prevalence study conducted among office workers found totally 9.6% had doctor-diagnosed asthma (8). Anderson et al. (9) found that administrative support workers, including clerical workers and health service workers had significantly higher prevalence ratios (PR 1.5, 95%CI 1.2–1.9) of current asthma than prevalence in all industries. Thus, attention should be paid to the more specific occupational groups used to be simply classified as office workers.
Asthma can be triggered by factors such as exposure to allergens or irritants (10). A positive association between HDM allergens, dust, indoor air, mold, solvents and respiratory symptoms in office workers was reported (8, 11).
Related studies have shown a positive correlation between HDM allergens, dust, indoor air, mold, solvents and respiratory symptoms in office workers. The influencing factors of asthma are intricate, mainly attributed to genetic and environmental factors (12). Some researches have pointed out that there is also a certain amount of fungal pollution in different working environments, such as hospitals, nursing homes, museums and so on (13–15). When the fungus is exposed to a certain concentration it can cause asthma attacks in residents or staff (16, 17). Among them, archivists are susceptible to asthma due to the influence of working area and working mode.
Archive workers, a more specific occupational group as part of the office workers, besides dealing with relevant works in the office, closely expose to archive documents and document storage environment resulting. Most documents and files deposited in archives are made of paper, which are susceptible to chemical and biological damage. As a consequence of the exposed items degradation, VOCs can be formed from the paper itself (18), including acetic acid, formic acid, furfural, furfural, 4-hydroxy benzoic acid, 4-hydroxy acetophenone (19). Cladosporium, Aspergillus, and Penicillium species are almost ubiquitous in the archives (20), which induces allergic reactions and further developing of asthma (1, 21, 22). Exposure to biological allergens such as insect and microorganism is another crucial potential risk factor associated with incidence of asthma (23, 24). To the best of our knowledge, no studies have investigated asthma among archive workers.
Therefore, we sought to identify the prevalence and factors associated with asthma attacks in archival workers. In this study, a questionnaire-based study was conducted among archivists to investigate the associated factors concerning asthma attacks, and concurrently assessed potential interactions that may augment the risk of asthma attacks.
1.1 Contribution to the field
The evidence generated in this study suggests the need to further study and protect archivists as there is a strong synergy between chemical odors and molds in interaction with the potential of chemical irritants, such as sulfur dioxide and ozone, to synergistically interact with inhalable allergens, including fungi, molds and dust mites. Consequently, this interaction seems to exacerbate asthma symptom, perpetuate untreated exposure and trigger an inflammatory response potentially serving as a shared pathway for the development of asthma among individuals exposed to these hazardous factors (add here one more paragraph or two clarifying what can this paper contribute to knowledge and unknown aspects associated with the topic and the population under study, to be arranged in an independent section).
Additionally, the occupational health of archivists, who are the participants and executors of the preservation of important historical materials in countries and organizations, affects the sustainable development of archival undertakings. Archival workers often need to deal with all kinds of archival materials, including photo archives, physical archives and paper archives, etc., which plays a key role in the archives management work. These files may contain a variety of pathogenic microorganisms, such as bacteria, viruses, fungi and parasites, which may pose a potential risk of pathogenic infection to the archivists. A large number of occupational health studies have found that the human body will develop allergy symptoms, respiratory diseases and other health problems in the poor indoor environment.
At present, there are many studies based on the correlation between asthma and other occupations, but few studies on occupational risk factors for archivists, especially for the prevalence of asthma attacks in archivists, no evidence or correlation studies have been found. Therefore, the study of occupational hazard factors for archivists concerned in this study is a critical and ongoing topic, and its related research is of great significance for the protection of the health and safety of archival professionals.
2 Subjects and methods
2.1 Subjects
This cross-sectional, questionnaire-based study was conducted at the archives nationwide in China in a multi-center setting, including archives of enterprises and institutions (74.78%), national comprehensive archives (23.22%) and specialized archives (2.10%). Individuals who were currently employed in archive setting were included in the study. The questionnaire is available as Supplementary material.
2.1.1 Sample size calculation
The results of the total work-life microsimulation conducted by Laditka (25) showed that 14.9% (CI 13.4–16.3) of those with low trigger exposure risk reported asthma at least once. We classified archivists as having a low risk of triggering asthma exposure and considered the prevalence of asthma among archivists to be approximately 14.9%, calculated according to the PASS software. Based on α = 0.05, δ = 0.03, p = 0.149, the total sample size required was calculated to be 573 cases. Considering the possibility of invalid samples in the questionnaire, the final sample size required was calculated to be 717 cases.
2.2 Methods
2.2.1 Questionnaire
The questionnaires were sent to all eligible archivists in February 2022, and archivists were requested to fill out the questionnaires within 10 days. Here, we define “asthma attacks and exacerbation of asthma attacks among archivists after work” as asthma attacks. Data on the following personal factors were collected: sex (male, female), age (20–30 years, 31–40 years,41–50 years,51–65 years), education (below bachelor degree, bachelor, master’s degree or above), duration of employment (≤5 years,6–10 years,11–20 years, ≥21 years) and family history of the respiratory system. In order to explore archivists’ knowledge of occupational hazard factors, we also collected the data: whether knowing the effective protection measures to risk factors in the archival profession and well protection in work according to the professional protection files? The response to each is either “yes” or “no.” Furthermore, work-related factors were gathered: archivists’ average frequency of contacting paper files at work (times per day) ≤1, 1–2, 3–4, ≥5. And the strict separation of the working areas from archives warehouses, dampness in the working area, chemically irritating odor in working areas, mold odor in working areas, insects (roaches, ants, tobacco beetle and dust mite etc.) in working area. The answer options in each question are dichotomous (yes or no). To further adjust for confounding factors, the self-administered questionnaire asked about the protection to adverse factors related to archival work, i.e., legislation of protective measures of risk factors in the archival profession, having equipment for occupational protection, training on occupational protections of archives. Finally, subjects were asked to answer if they had asthma or more frequent asthma attacks at work (especially when in contact with archival entities), including questions about asthma symptoms, namely wheezing, chest tightness or shortness of breath which were questions in questionnaire. Responses range from always, frequently, occasionally, never. The data collected were conducted in an anonymous fashion. Ethical approval was obtained from XXX [Anonymized by request from JOEM]. Electronic informed consent was obtained for each participant.
2.3 Statistical analysis
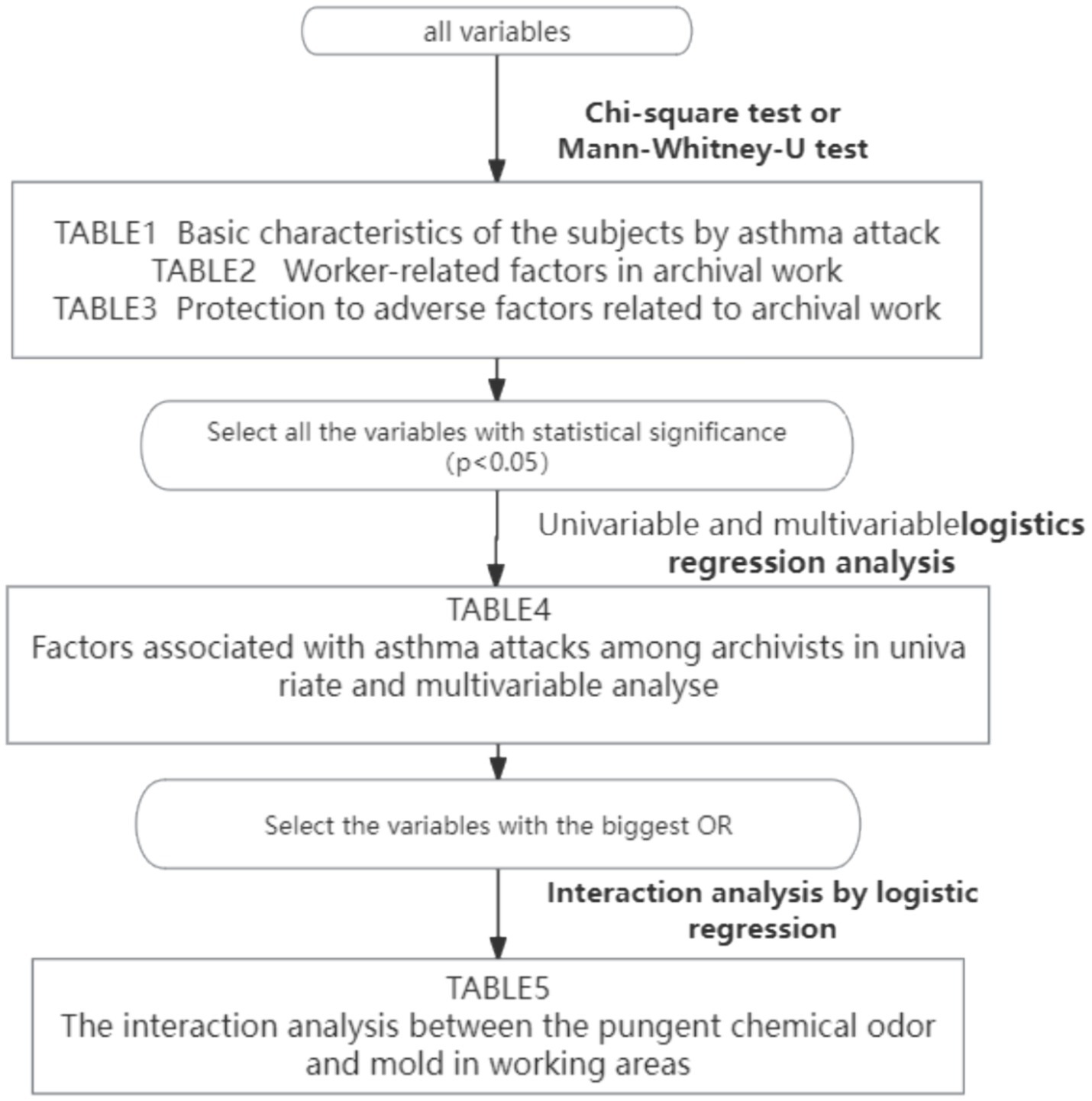
All statistical analysis was performed using SPSS 26.0. Initially, associations between personal factors (age, sex, duration of employment, family history) and asthma attacks were analyzed by Chi-square test or the Mann–Whitney-U test. Next, the association between the related factors in archival work, i.e., strict separation of working areas from archives warehouses, ventilation and its average time in warehouse, temperature and humidity of the warehouse in summer, chemically irritating odor, mold odor and insects (roaches, ants, tobacco beetle and dust mite etc) in working areas and asthma attacks were also assessed by Chi-square test. Thereby, logistic regression was conducted according to the p value. For the first selection of associated factors, univariate logistic regression analysis was performed. Subsequently, multiple logistic regression analysis was performed to assess independent association, in which the presence of asthma attacks was the objective variable and the associated factors that showed significant associations in the univariate analysis were the explanation variables. For the variables with a p value <0.05 in the univariable analysis were entered into the multiple logistic regression model. The interaction between the chemically irritating odors and mold odors was examined in the logistic regression model. Statistical significance was set at p < 0.05.
The Strobe Protocol for Cross-Sectional studies was applied.
3 Results
3.1 Basic characteristics of the subjects
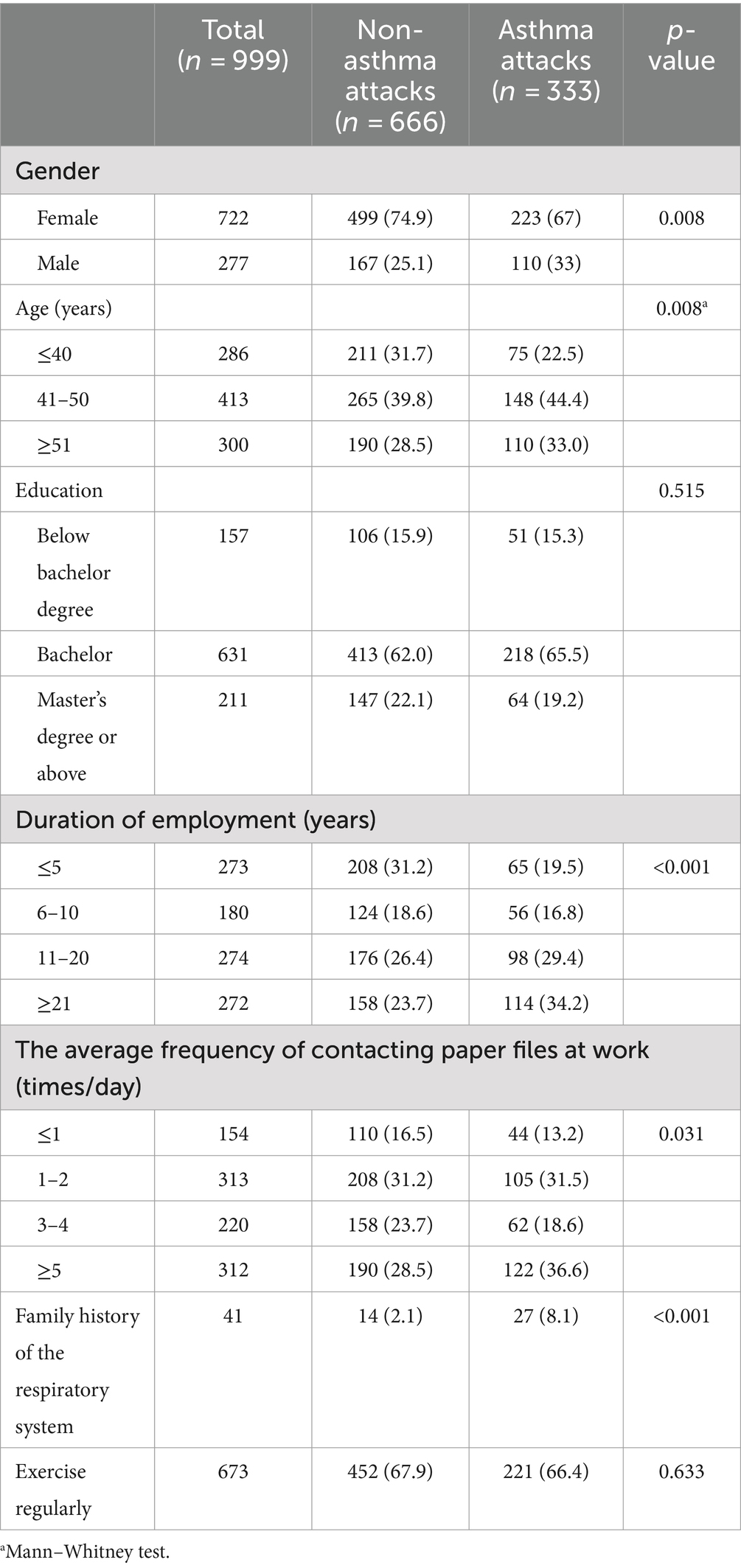
A total of 1,002 people submitted questionnaires, of which 999 were valid and included in the final analysis, with an effective rate of 99.7%. The gender, age, education, and duration of employment of the respondents substantially matched the statistics of the National Bureau of Statistics 2021. As shown in Table 1, individuals with asthma attacks accounted for 33%, of which 67% were female. Duration of employment were less than 10 years for 45% (n = 453) of subjects and 11 years or more for 55% (n = 556). Approximately 66% of those archivists with family history of the respiratory system had asthma attacks (Table 1).
3.2 Work-related factors
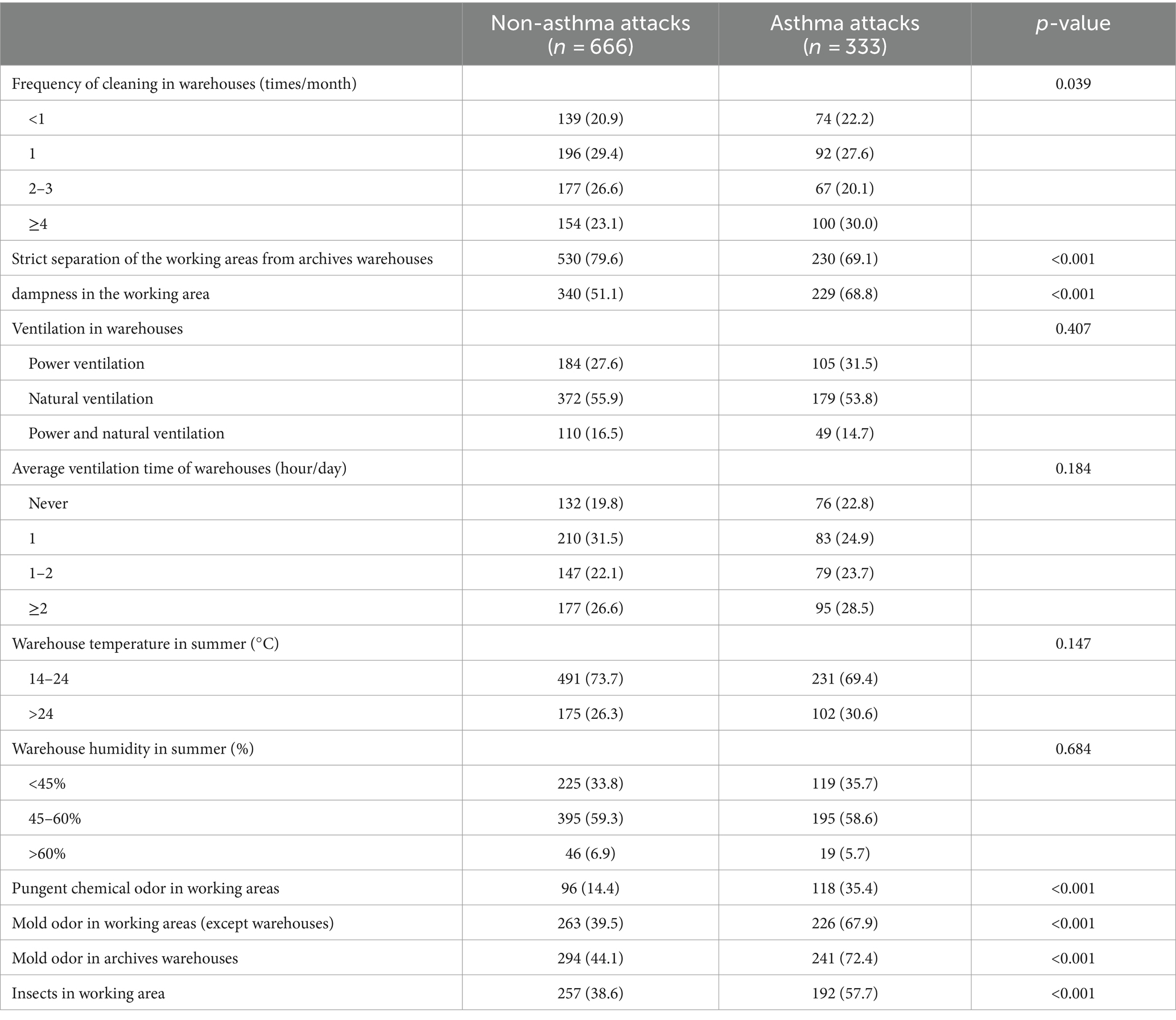
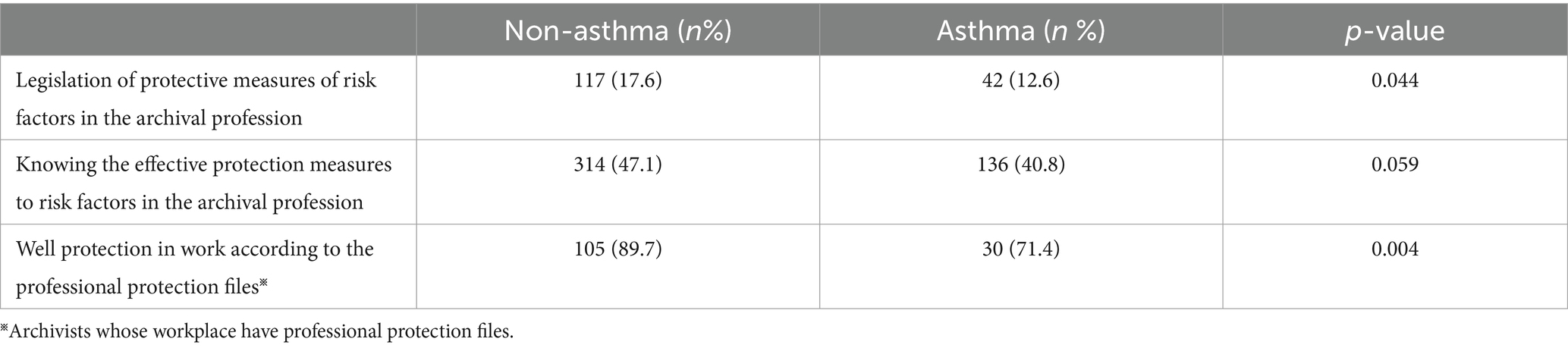
Archive’s daily sanitary measures and status in terms of asthma attacks in archivists are shown in Table 2. The archivists who have strict separation of the working areas from archives’ warehouses tended to respond that they suffered less asthma attacks, and many individuals respond that the occurrence of dampness, pungent chemical odor, mold odor as well as the harmful insects in the working area were significantly associated with the asthma attacks among them. Archives’ protective measures thought to be associated with asthma attacks were also assessed, the results of which were shown in Table 3. Those archivists having documentation of archival occupational risk factors in the workplace and achieving standardized protection at work were prone to have a lower prevalence of asthma attacks. As archival workers are exposed to various hazards in the workplace, it is essential for them to take appropriate protective measures. However, many archives fail to raise awareness of the dangers present in the workplace. Only 135 archivists participating in the study have had professional protection protocols in place. This study data indicates that chemically irritating odors, mold odors, and insects in the workplace are correlated with asthma attacks amongst the population studied. Therefore, it suggests that the workplace environment plays a key role in the occurrence of asthma attacks, and achieving standardized protection at work is prone to promote a lower prevalence of asthma attacks in the context studied.
3.3 Factors associated with asthma attacks
The univariate and multivariate analysis are summarized in Table 4. In the multivariate logistic regression analysis, sex, working years, strict separation of the working areas from archives, mold odor, chemically irritating odor and insects in the workplaces were significantly associated with the incidence of asthma attacks (p < 0.05). Workers who had work experiences≥21 years (OR, 95%CI: 2.116, 1.420 ~ 3.153) had the odds of developing asthma attacks 1.1 times more than workers who had work experiences between 6 and 10 years. Workers without strict separation of the working areas from archives warehouses were 0.522 times more likely to develop asthma attacks (OR, 95%CI: 1.522, 1.096 ~ 2.113). Workers who found mold odor in working areas as well as warehouses had a higher risk of developing asthma attacks (OR, 95%CI: 1.747, 1.148 ~ 2.658; 1.666, 1.084 ~ 2.561 separately). Workers who found chemically irritating odor in working areas were 1.152 times more likely to develop asthma attacks (OR, 95%CI: 2.152, 1.532 ~ 3.024). Workers who found insects in working areas were 0.409 times more likely to develop asthma attacks (OR, 95%CI: 1.409, 1.041 ~ 1.907).
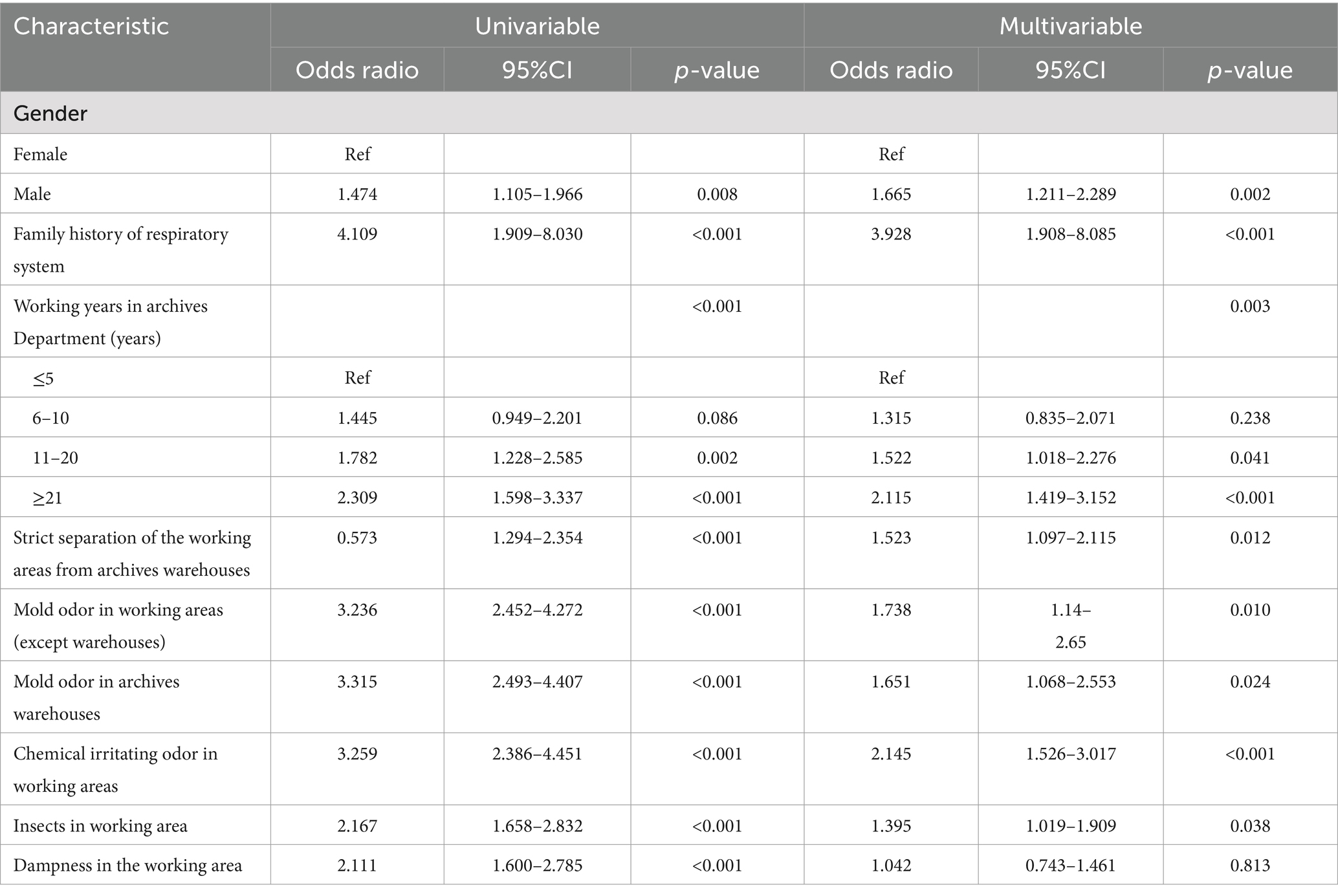
Table 4. Factors associated with asthma attacks among archivists in univariate and multivariable analyses.
Table 5 shows the results of analysis in which we tested for interactions between chemically irritating odor and mold odor in working areas for asthma attacks. A significant synergistic effect was observed between chemical irritants and molds, the odds ratio was 7.098 (95% CI, 4.752–10.603). A program flowchart is presented in Figure 1.
4 Discussion
This study found that the prevalence of asthma attacks was 33.3%, higher among male archivists. The existence of chemically irritating odors and moldy smells within the work environment were associated with higher asthma attacks. We also found a significant synergistic effect between the two risk factors. To the best of our knowledge, this is the first multicenter study focusing specifically on the risk factors related to asthma in archivists and provides a fresh perspective on occupational asthma.
The present study identified a significant association between the presence of chemically irritating odors in archival workplaces and high asthma attacks among archivists. Occupational hazards for archivists primarily stem from indoor air pollution, including conventional indoor chemical pollutants such as formaldehyde, sulfur dioxide, volatile organic compound (26). Additionally, there are archival-specific chemical pollutants such as acetic acid, hydrogen sulfide, ethylene oxide, sulfuryl fluoride, furfural, and other compounds (19). It has been reported that exposure to ozone and sulfur dioxide has deleterious effects on immune competent cells and airway responsiveness (27). Owing to its potential to sensitize airway inflammation, ozone exhibits a propensity to induce various respiratory ailments, encompassing coughing and wheezing (28). It has been extensively elucidated that elevated ozone levels have an inflammatory impact on the respiratory system, thereby contributing to the progression of asthma (29). Interestingly, a study revealed a negative correlation between low-to-moderate atmospheric ozone levels and hospital visits by asthma patients (30). However, the measured median ozone concentration in office environments is 9.04 μg/m3 (31), which were consistent with this study’s results. A noteworthy association between the frequency of printer usage (exceeding seven times per day) and the occurrence of asthma attack was demonstrated in our study. A study conducted in Estonia, with participation from over 50,000 adults, have revealed a significant association between exposure ranging from low to moderate levels of indoor air pollutants and asthma (OR = 1.88, 95%CI 1.48 ~ 2.37) (22). Inhalation of VOCs, in particular, has been implicated in various adverse health effects (32), and their role in triggering asthma is well-documented. VOCs can activate the immune system, cause oxidative stress, and interact with some allergens (33). Metabolites of VOCs have also been found to be correlated with markers of oxidative stress, which are associated with lung function parameters (33–35). Furthermore, multiple studies have reported a connection between exposure to formaldehyde and the development of asthma and asthma symptoms in adults. Formaldehyde, as a respiratory irritant, exerts its effects by inducing inflammation of the airway mucosa and eliciting an inflammatory response via cytokines produced by Th2 cells (34). Additionally, transient decreases in lung function have been attributed to formaldehyde exposure (36).
In addition, this study has indicated mold as an associated factor for asthma among archivists, exhibiting a correlated escalation of 65.1 and 73.8% in warehouses and workplaces, respectively. Molds, being a potent allergens, can trigger allergic reactions, provoke inflammatory responses and augment the susceptibility to asthma via the emission of VOCs (26). A study has revealed a pronounced elevation of Asthma-COPD Overlap Syndrome (ACOS) associated with occupational exposure to mold odor, with an odds ratio (OR) of 3.43(95%CI 1.04–11.29) (37). Although limited research has been conducted among office workers, previous studies have consistently reported a positive correlation between mold odor and adult individuals in residential settings (38–40). Furthermore, a heightened susceptibility to asthma was detected in relation to occupational exposure to mold odor, as opposed to exposure within the confines of one’s abode (37). This could be potentially elucidated by the more pervasive prevalence of mold issues in archives, coupled with a tendency for individuals to expeditiously remedy any mold-related problems within their own dwellings. Another biological factor encountered in the workplace, i.e., dust mites and cockroaches, may contribute to an elevated risk of asthma by 39.5%. A recent study revealed that dust mite allergen concentration of 10 μg g-1 has been proposed as the threshold for asthma development. While the levels of Der p 1 and Der f 1 allergens in dust samples collected from offices in Malaysia were found to be as high as 556 ng/g and 658 ng/g, respectively (8). Our findings align with the previous study, as we have observed an increased asthma attacks in connection with exposure to dust mites and cockroaches (41). Hence, it is crucial to accord primacy to the eradication of dust particles and the implementation of sterilization protocols within archival repositories.
Notably, our data analysis has revealed a strong synergy (OR = 7.098) between chemical odors and molds in the workplace. While the existing literature on this specific interaction remains somewhat limited, previous studies have already demonstrated the potential for chemical irritants, such as sulfur dioxide and ozone, to synergistically interact with inhalable allergens, including fungi, molds and dust mites. Consequently, this interaction serves to exacerbate asthma symptoms and perpetuate untreated exposure (42). Furthermore, in damp and damaged buildings, the presence of microbial components, such as cellular debris or spores released during fungal growth can trigger an inflammatory response, potentially served as a shared pathway for the development of asthma among individuals exposed to these hazardous factors.
Interestingly, contrary to findings from other studies that reported a higher prevalence of asthma among women than men, this study revealed that the prevalence of asthma among archivists was 1.28 times higher among male workers. Stratified analysis by gender demonstrates significantly higher odds ratios (ORs) for males in both chemical and biological factors. More precisely, the presence of chemically irritating odors and biological agents, such as molds and dust mites, in the archival work environment is more robustly correlated with declining pulmonary function in males. This finding in concordance with a previous study carried out in Italy (43).
In conclusion, this survey revealed that approximately one-third of archivists experienced asthma attacks. Chemically irritating odor, Mold odor and insects in the workplaces are associated with asthma attacks. Moreover, chemically irritating gases and molds in the archival workplace were highly associated with asthma attack, with a significant interaction between them. However, the health relevance and mechanism of the work-related exposure in archives need to be further explored by more detailed assessments.
4.1 Strengths and limitations
There are several strengths in this study. First, the participation of archivists from various types of archives nationwide, who exhibit higher levels of compliance and consistency in their education and job type, significantly enhances the credibility and generalizability of our findings. Consequently, it is reasonable to extrapolate the results to a broader population of office workers. Second, given the intricate compositions, relatively low concentrations and inherent difficulty in precise measurement of various factors within the work environment, pertinent information was gathered through the employment of a questionnaire-based approach. Hence, employing a questionnaire to gauge the overall extent of exposure among archivists represents a judicious methodology within this framework. The study revised and adopted recent trends in healthcare research and related challenges (44–68).
Also, there are some limitations. First, as was the case for most of the previous studies, this was a cross-sectional study. Therefore, the causality between the asthma attacks and the associated factors were not clarified in this study. Second, current study surveyed subjects via a self-administered questionnaire, but the reliability and validity of this questionnaire was not tested. Second, the lack of quantification pertaining to the exposures presents a notable challenge in elucidating potential mechanisms of action or dose–response relationships. Third, similar to other large-scale population-based surveys, the diagnosis of asthma was based mainly on a standardized questionnaire, which could potentially have led to the misclassification of some pulmonary diseases.
4.2 Further research
Current study surveyed subjects via a self-administered questionnaire, but the reliability and validity of this questionnaire were not tested, especially the diagnosis of asthma. Therefore, future research is expected to add some questions, such as the doctor diagnosed asthma, asthma medication, etc. In addition, as mentioned above, the causality between asthma attacks and the associated factors was not clarified in this study. Clearly, future longitudinal studies are necessary to address this issue. Finally, concerning measurement of exposure-related factors. Microorganisms, dust particles, etc. in the archive working environment can be measured using more accurate measurement techniques or culture methods.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
LY: Conceptualization, Investigation, Writing – original draft. CX: Methodology, Writing – original draft. ZA: Formal analysis, Writing – original draft. XR: Data curation, Writing – original draft. PM: Validation, Writing – review & editing. DM: Funding acquisition, Supervision, Validation, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Study on the correlation between multiple physical discomforts and working environment of archivists” (Project No: 2021-B-16) of the Science and Technology Project of the National Archives Administration of China. This work was supported by “Research on the Cultural Communication Strategies and Paths of Memory of the Archives: Based on the Oral Archives Construction” (Project No: QDSKL2301266) of Qingdao Planning Project for Philosophy and Social Sciences in 2023.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1397236/full#supplementary-material
References
1. Karvala, K, Toskala, E, Luukkonen, R, Lappalainen, S, Uitti, J, and Nordman, H. New-onset adult asthma in relation to damp and moldy workplaces. Int Arch Occup Environ Health. (2010) 83:855–65. doi: 10.1007/s00420-010-0507-5
2. Jo, W, Seo, KW, Jung, HS, Park, CY, Kang, BJ, Kang, HH, et al. Clinical importance of work-exacerbated asthma: findings from a prospective asthma cohort in a highly Industrialized City in Korea. Allergy Asthma Immunol Res. (2021) 13:256–70. doi: 10.4168/aair.2021.13.2.256
3. Reilly, MJ, Wang, L, and Rosenman, KD. The burden of work-related asthma in Michigan, 1988-2018. Ann Am Thorac Soc. (2020) 17:284–92. doi: 10.1513/AnnalsATS.201905-401OC
4. Jouneau, S, Chapron, A, Ropars, C, Marette, S, Robert, AM, Gouyet, T, et al. Prevalence and risk factors of asthma in dairy farmers: ancillary analysis of AIRBAg. Environ Res. (2022) 214:114145. doi: 10.1016/j.envres.2022.114145
5. Lagiso, ZA, Mekonnen, WT, Abaya, SW, Takele, AK, and Workneh, HM. Chronic respiratory symptoms, lung function and associated factors among flour mill factory workers in Hawassa city, southern Ethiopia: "comparative cross-sectional study". BMC Public Health. (2020) 20:909. doi: 10.1186/s12889-020-08950-9
6. Huntley, CC, Burge, PS, Moore, VC, Robertson, AS, and Walters, GI. Occupational asthma in office workers. Occup Med. (2022) 72:411–4. doi: 10.1093/occmed/kqac023
7. Wang, L, and Rosenman, K. Adverse health outcomes among industrial and occupational sectors in Michigan. Prev Chronic Dis. (2018) 15:E102. doi: 10.5888/pcd15.170487
8. Lim, FL, Hashim, Z, Than, LT, Md Said, S, Hisham Hashim, J, and Norbäck, D. Asthma, airway symptoms and rhinitis in Office Workers in Malaysia: associations with house dust mite (HDM) allergy, cat allergy and levels of house dust mite allergens in office dust. PLoS One. (2015) 10:e0124905. doi: 10.1371/journal.pone.0124905
9. Anderson, NJ, Fan, ZJ, Reeb-Whitaker, C, Bonauto, DK, and Rauser, E. Distribution of asthma by occupation: Washington state behavioral risk factor surveillance system data, 2006-2009. J Asthma. (2014) 51:1035–42. doi: 10.3109/02770903.2014.939282
10. Papi, A, Brightling, C, Pedersen, SE, and Reddel, HK. Asthma. Lancet. (2018) 391:783–800. doi: 10.1016/S0140-6736(17)33311-1
11. Fletcher, AM, London, MA, Gelberg, KH, and Grey, AJ. Characteristics of patients with work-related asthma seen in the New York state occupational health clinics. J Occup Environ Med. (2006) 48:1203–11. doi: 10.1097/01.jom.0000245920.87676.7b
12. Zhang, J. A study of the relationship between asthma and blood lipids. J Inner Mongol Med. (2016) 44:129–32. In Chinese
13. Gheith, S, Ranque, S, Bannour, W, Ben Youssef, Y, Khelif, A, Ben Said, M, et al. Hospital environment fungal contamination and aspergillosis risk in acute Leukaemia patients in Sousse (Tunisia). Mycoses. (2015) 58:337–42. doi: 10.1111/myc.12320
14. Lu, R, Tendal, K, Frederiksen, MW, Uhrbrand, K, Li, Y, and Madsen, AM. Strong variance in the inflammatory and cytotoxic potentials of Penicillium and aspergillus species from cleaning workers’ exposure in nursing homes. Sci Total Environ. (2020) 724:138231. doi: 10.1016/j.scitotenv.2020.138231
15. Awad, AHA, Saeed, Y, Shakour, AA, Abdellatif, NM, Ibrahim, YH, Elghanam, M, et al. Indoor air fungal pollution of a historical museum, Egypt: A case study. Aerobiologia. (2020) 36:197–209. doi: 10.1007/s10453-019-09623-w
16. Baxi, SN, Portnoy, JM, Larenas-Linnemann, D, Phipatanakul, W, and Workgroup, EA. Exposure and health effects of Fungi on humans. J Allergy Clin Immunol Pract. (2016) 4:396–404. doi: 10.1016/j.jaip.2016.01.008
17. Belizario, JA, Lopes, LG, and Pires, RH. Fungi in the indoor air of critical hospital areas: A review. Aerobiologia. (2021) 37:379–94. doi: 10.1007/s10453-021-09706-7
18. Cincinelli, A, Martellini, T, Amore, A, Dei, L, Marrazza, G, Carretti, E, et al. Measurement of volatile organic compounds (VOCs) in libraries and archives in Florence (Italy). Sci Total Environ. (2016) 572:333–9. doi: 10.1016/j.scitotenv.2016.07.201
19. Salthammer, T, Mentese, S, and Marutzky, R. Formaldehyde in the indoor environment. Chem Rev. (2010) 110:2536–72. doi: 10.1021/cr800399g
20. Pinheiro, AC, Sequeira, SO, and Macedo, MF. Fungi in archives, libraries, and museums: a review on paper conservation and human health. Crit Rev Microbiol. (2019) 45:686–700. doi: 10.1080/1040841X.2019.1690420
21. Peel, AM, Wilkinson, M, Sinha, A, Loke, YK, Fowler, SJ, and Wilson, AM. Volatile organic compounds associated with diagnosis and disease characteristics in asthma—A systematic review. Respir Med. (2020) 169:105984. doi: 10.1016/j.rmed.2020.105984
22. Maestrelli, P, Henneberger, PK, Tarlo, S, Mason, P, and Boschetto, P. Causes and phenotypes of work-related asthma. Int J Environ Res Public Health. (2020) 17:4713. doi: 10.3390/ijerph17134713
23. Savoldelli, S, Cattò, C, Villa, F, Saracchi, M, Troiano, F, Cortesi, P, et al. Biological risk assessment in the history and historical documentation library of the University of Milan. Sci Total Environ. (2021) 790:148204. doi: 10.1016/j.scitotenv.2021.148204
24. Baldacci, S, Maio, S, Cerrai, S, Sarno, G, Baïz, N, Simoni, M, et al. Allergy and asthma: effects of the exposure to particulate matter and biological allergens. Respir Med. (2015) 109:1089–104. doi: 10.1016/j.rmed.2015.05.017
25. Laditka, JN, Laditka, SB, Arif, AA, and Hoyle, JN. Work-related asthma in the USA: nationally representative estimates with extended follow-up. Occup Environ Med. (2020) 77:617–22. doi: 10.1136/oemed-2019-106121
26. Mu, L, Liu, L, Niu, R, Zhao, B, Shi, J, Li, Y, et al. Indoor air pollution and risk of lung cancer among Chinese female non-smokers. Cancer Causes Control. (2013) 24:439–50. doi: 10.1007/s10552-012-0130-8
27. Delfino, RJ, Chang, J, Wu, J, Ren, C, Tjoa, T, Nickerson, B, et al. Repeated hospital encounters for asthma in children and exposure to traffic-related air pollution near the home. Ann Allergy Asthma Immunol. (2009) 102:138–44. doi: 10.1016/S1081-1206(10)60244-X
28. Xu, F, Yan, S, Wu, M, Li, F, Xu, X, Song, W, et al. Ambient ozone pollution as a risk factor for skin disorders. Br J Dermatol. (2011) 165:224–5. doi: 10.1111/j.1365-2133.2011.10349.x
29. Paulin, LM, Gassett, AJ, Alexis, NE, Kirwa, K, Kanner, RE, Peters, S, et al. Association of Long-term Ambient Ozone Exposure with Respiratory Morbidity in smokers. JAMA Intern Med. (2020) 180:106. doi: 10.1001/jamainternmed.2019.5498
30. Lee, S, and Lee, M. Low-to-moderate atmospheric ozone levels are negatively correlated with hospital visits by asthma patients. Medicine. (2022) 101:e31737. doi: 10.1097/MD.0000000000031737
31. Salonen, H, Salthammer, T, and Morawska, L. Human exposure to ozone in school and office indoor environments. Environ Int. (2018) 119:503–14. doi: 10.1016/j.envint.2018.07.012
32. Maung, TZ, Bishop, JE, Holt, E, Turner, AM, and Pfrang, C. Indoor air pollution and the health of vulnerable groups: a systematic review focused on particulate matter (PM), volatile organic compounds (VOCs) and their effects on children and people with pre-existing lung disease. Int J Environ Res Public Health. (2022) 19:8752. doi: 10.3390/ijerph19148752
33. Tischer, C, Karvonen, AM, Kirjavainen, PV, Flexeder, C, Roponen, M, Hyvärinen, A, et al. Early age exposure to moisture and mould is related to FeNO at the age of 6 years. Pediatr Allergy Immunol. (2021) 32:1226–37. doi: 10.1111/pai.13526
34. Ren, B, Wu, Q, Muskhelishvili, L, Davis, K, Wang, Y, Rua, D, et al. Evaluating the sub-acute toxicity of formaldehyde fumes in an in vitro human airway epithelial tissue model. Int J Mol Sci. (2022) 23:2593. doi: 10.3390/ijms23052593
35. Yeatts, KB, el-Sadig, M, Leith, D, Kalsbeek, W, al-Maskari, F, Couper, D, et al. Indoor air pollutants and health in the United Arab Emirates. Environ Health Perspect. (2012) 120:687–94. doi: 10.1289/ehp.1104090
36. Herbert, FA, Hessel, PA, Melenka, LS, Yoshida, K, and Nakaza, M. Respiratory consequences of exposure to wood dust and formaldehyde of workers manufacturing oriented Strand board. Arch Environ Health. (1994) 49:465–70. doi: 10.1080/00039896.1994.9955002
37. Jaakkola, MS, Lajunen, TK, and Jaakkola, JJK. Indoor mold odor in the workplace increases the risk of asthma-COPD overlap syndrome: a population-based incident case–control study. Clin Transl Allergy. (2020) 10:3. doi: 10.1186/s13601-019-0307-2
38. Husman, T. Health effects of indoor-air microorganisms. Scand J Work Environ Health. (1996) 22:5–13. doi: 10.5271/sjweh.103
39. Shiue, I. Indoor mildew odour in old housing was associated with adult allergic symptoms, asthma, chronic bronchitis, vision, sleep and self-rated health: USA NHANES, 2005–2006. Environ Sci Pollut Res. (2015) 22:14234–40. doi: 10.1007/s11356-015-4671-8
40. Zhang, X, Norbäck, D, Fan, Q, Bai, X, Li, T, Zhang, Y, et al. Dampness and mold in homes across China: associations with rhinitis, ocular, throat and dermal symptoms, headache and fatigue among adults. Indoor Air. (2018) 29:30–42. doi: 10.1111/ina.12517
41. Ghaemmaghami, AM, and Shakib, F. Human T cells that have been conditioned by the proteolytic activity of the major dust mite allergen Der p 1 trigger enhanced immunoglobulin E synthesis by B cells. Clin Exp Allergy. (2002) 32:728–32. doi: 10.1046/j.1365-2222.2002.01374.x
42. Sokol, K, Sur, S, and Ameredes, BT. Inhaled environmental allergens and toxicants as determinants of the asthma phenotype. Heterogen Asthma. (2014):43–73. doi: 10.1007/978-1-4614-8603-9_4
43. Moscato, G, Apfelbacher, C, Brockow, K, Eberle, C, Genuneit, J, Mortz, CG, et al. Gender and occupational allergy: report from the task force of the EAACI environmental and occupational allergy interest group. Allergy. (2020) 75:2753–63. doi: 10.1111/all.14317
44. Antunes, V. On nursing research and evidence-based practice: topics for researchers and practitioners. Int Healthc Rev. (2022) 1:12. doi: 10.56226/ihr.v1i1.12
45. Chen, S, and Qin, Y. On ethics, biomedical education and health promotion: international and Chinese perspectives. Int Healthc Rev. (2023). doi: 10.56226/46
46. Chen, Y, Moreira, P, Liu, W, Monachino, M, Nguyen, TLH, and Wang, A. Is there a gap between artificial intelligence applications and priorities in health care and nursing management? J Nurs Manag. (2022) 30:3736–42. doi: 10.1111/jonm.13851
47. Dsouza, B. On sustainable health systems: a research emergency in pandemic times. Int Healthc Rev. (2022) 1. doi: 10.56226/ihr.v1i1.7
48. Dsouza, B, Prabhu, R, Unnikrishnan, B, Ballal, S, Mundkur, SC, Chandra Sekaran, V, et al. Effect of educational intervention on knowledge and level of adherence among hemodialysis patients: A randomized controlled trial. Glob Health Epidemiol Genom. (2023) 2023:4295613. doi: 10.1155/2023/4295613
49. Ferreira, J, Horta, P, and Geada, F. Internal audit process in eHealth: A case study. Int Healthc Rev. (2023). doi: 10.56226/50
50. Han, T, Han, M, Moreira, P, Song, H, Li, P, and Zhang, Z. Association between specific social activities and depressive symptoms among older adults: A study of urban-rural differences in China. Front Public Health. (2023) 11:1099260. doi: 10.3389/fpubh.2023.1099260
51. Jacennik, B, Zawadzka-Gosk, E, Moreira, JP, and Glinkowski, WM. Evaluating patients’ experiences with healthcare services: extracting domain and language-specific information from free-text narratives. Int J Environ Res Public Health. (2022) 19:10182. doi: 10.3390/ijerph191610182
52. Gao, Y, Zhang, S, Zhao, Y, Yang, T, Moreira, P, and Sun, G. Reduction of retinal vessel density in non-exudative macular neovascularization: a retrospective study. Front Med. (2024) 10:1219423. doi: 10.3389/fmed.2023.1219423
53. Jia, X, Tang, X, and Li, Y. And Paulo Moreira (2023) update of dialysis initiation timing in end stage kidney disease patients: is it a resolved question? A systematic literature review. BMC Nephrol. (2023) 24:162. doi: 10.1186/s12882-023-03184-4
54. Kehinde, O, Dixon-Lawson, K, and Mendelsohn, A. On community pharmacists and promotion of lifestyle modification in adults with hypertension: practice protocol. Int Healthc Rev. (2023). doi: 10.56226/49
55. Li, N, Guo, M, You, S, and Ji, H. On patient readiness for hospital discharge: an update on recent evidence. Int Healthc Rev. (2022). doi: 10.56226/ihr.v1i2.30
56. Lloyd Williams, D. On healthcare research priorities in the USA: from long COVID to precision health, what else is new? Int Healthc Rev. (2022) 1. doi: 10.56226/ihr.v1i1.14
57. Loureiro Pais Batista, SM, Pereira Gaspar, AC, Madeira dos Santos, B, da Cunha Silva, F, Fonseca Marta, F, Pinto Pedrosa, I, et al. Nurses’ knowledge of patients´’ swallowing ability: a cross sectional study in Portugal. Int Healthc Rev. (2023). doi: 10.56226/64
58. Monachino, M. On healthcare research for disease prevention: critical knowledge gaps in European public health. Int Healthc Rev. (2022) 1. doi: 10.56226/ihr.v1i1.6
59. Moreira, P. On new clinical research methods and technologies: from decentralised designs to artificial intelligence. Int Healthc Rev. (2022) 1. doi: 10.56226/ihr.v1i1.11
60. Nguyen, TLH. On improving healthcare with a world perspective: evidence for Global Health programs. Int Healthc Rev. (2022) 1. doi: 10.56226/ihr.v1i1.10
61. Niu, M. On planning and designing general hospitals in smart technology contexts. Int Healthc Rev. (2023). doi: 10.56226/59
62. Song, C, and Xie, H. On disparities in breast Cancer screening: an analysis of behavioral risk factor surveillance survey data related to racial/ ethnic characteristics. Int Healthc Rev. (2023). doi: 10.56226/53
63. Sun, P, Li, Z, Guo, W, and Moreira, P. Evidence on the need for early identification of asymptomatic true abdominal aortic aneurysm in pregnancy: A case report. SAGE Open Med Case Rep. (2023) 11:11. doi: 10.1177/2050313X231173789
64. Tian, M, Li, X, Zhou, F, Wang, Y, Wang, Q, Pan, N, et al. On the psychological experiences of hematopoietic stem cell donors: an update on international evidence. Int Healthc Rev. (2023). doi: 10.56226/31
65. Wei, L, and Xue, J. A longitudinal study on the emotional support mechanism of the mental health of empty nesters: recent evidence from China National Health and retirement survey. Int Healthc Rev. (2022). doi: 10.56226/37
66. Wang, M, Yang, Q, and Chen, Y. International comparison of the financing mechanism of basic medical insurance and its implications for China. Int Healthc Rev. (2024). doi: 10.56226/63
67. Zhang, B, Li, Y, Cao, M, and Xu, C. On workplace bullying in nursing: findings from a rapid review of the literature. Int Healthc Rev. (2023). doi: 10.56226/51
68. Zhang, L, Lei, J, Zhang, J, Yin, L, Chen, Y, Xi, Y, et al. Undiagnosed long COVID-19 in China among non-vaccinated individuals: identifying persistent symptoms and impacts on Patients' health-related quality of life. J Epidemiol Glob Health. (2022) 12:560–71. doi: 10.1007/s44197-022-00079-9
69. Wei, Y. Opportunities and challenges in cross-border healthcare: A case study based on the court of justice of the European Union. Int Healthc Rev. (2023). doi: 10.56226/65
Keywords: public health, asthma attacks, archival workers, chemical irritants, molds
Citation: Yang L, Xinting C, Aie Z, Ruiqi X, Moreira P and Mei D (2024) Insights into uncovered public health risks. The case of asthma attacks among archival workers: a cross-sectional study. Front. Public Health. 12:1397236. doi: 10.3389/fpubh.2024.1397236
Edited by:
João Cavaleiro Rufo, University Porto, PortugalCopyright © 2024 Yang, Xinting, Aie, Ruiqi, Moreira and Mei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paulo Moreira, anBtMjAzMEBvdXRsb29rLmNvbQ== Dou Mei ZG91bWVpQHFkdS5lZHUuY24=
†These authors share first authorship
 Liu Yang1†
Liu Yang1† Paulo Moreira
Paulo Moreira