- 1Academic Affairs, University of Arkansas for Medical Sciences, Little Rock, AR, United States
- 2Graduate School, University of Arkansas for Medical Sciences, Little Rock, AR, United States
- 3Biomedical Informatics, College of Medicine, University of Arkansas for Medical Sciences, Little Rock, AR, United States
- 4Department of Pediatrics, College of Medicine, University of Arkansas for Medical Sciences, Little Rock, AR, United States
- 5Department of Pharmaceutical Sciences, College of Pharmacy, University of Arkansas for Medical Sciences, Little Rock, AR, United States
Introduction: Diversity can enhance the agenda and quality of biomedical research, but a dearth of underrepresented minorities and women serve as biomedical researchers. The study purpose was to examine the impact of the a summer undergraduate research program on self-efficacy in research, scientific communication, and leadership as well as scientific identity, valuing objectives of the scientific community, and intent to pursue a biomedical research career.
Methods: Underrepresented minority and female undergraduate students participated in a mentored research experience in a rural, low-income state.
Results: Students' self-efficacy in research, scientific communication, and leadership as well as scientific identity, valuing objectives of the scientific community, and intent to pursue a biomedical research career increased post-program compared to pre-program.
Conclusion: This study supports implementation of a biomedical summer undergraduate research program for URM and women in a poor, rural, settings.
Introduction
Diversity in biomedical research can reduce health disparities (1). A diverse biomedical research workforce promotes a more comprehensive research agenda, including research on diseases with a disproportionate impact on underrepresented minorities (URM), primarily because researchers from populations with the greatest burden of disease tend to identify and apply solutions (2). Diversity can also enhance research quality. Ethnically or gender diverse research teams publish manuscripts in journals with higher impact factors and receive more citations, and peer reviewers perceive them as higher quality (3, 4). Yet, in many cases, biomedical researchers lack resemblance to the population they serve, because of a lack of diversity.
Indeed, a dearth of URM and women serve as biomedical researchers. Though URM make up 34.6% of the U.S. population, URM hold <6% of appointments among biomedical research faculty. African Americans constitute <3% of researchers with NIH research grants (5–7). Similarly, women hold less than one-third of tenured biomedical research faculty positions (8). A large gap exists in the number of URM and female biomedical researchers compared to their white and male counterparts. Reaching population parity may be an ideal goal, but there are many barriers to achieving parity including persistent incidents of discrimination, bias, stereotyping, and exclusion of minority students. These barriers collectively maintain the gap and result in low numbers of URM and women who pursue and attain a degree in science, technology, engineering, mathematics, and medicine (STEMM) (9).
Degree attainment in STEMM by URM and women is not narrowing this gap. Though URM students pursue STEMM majors at nearly the same rate as White and Asian students, unfortunately, the number who persist and graduate is low (10). African American and Hispanic STEMM students graduate at a rate of 34% and 43%, compared to much higher rates in White students (58%) (11). Indeed, African Americans earned only 9% and Hispanics 15% of STEMM bachelor degrees (12). Moreover, women earned 85% of health related degrees but less than one-fourth of the degrees for other sciences (13). A small pool of URM and female students are in a position to pursue graduate degrees in STEMM careers.
Pipeline programs for undergraduate students promote academic achievement and URM entry into STEMM and healthcare fields (14–16). The Survey of Undergraduate Research Experiences indicated most students had a sustained or increased interest in post-graduate studies after a summer research experience and reported an increase in their independence, motivation to learn, and undergraduate course participation (14). Further, pipeline programs for undergraduate students have reported improvement in research skills and increased matriculation into graduate biomedical research programs (15, 16). Still, observed gains are minor compared to the needs of URM and women in the population. A significant need exists for more interventions to improve diversity and inclusion in STEMM education and careers. Summer Undergraduate Research Programs exist throughout the country, including the rural south (17). For example, the University of Mississippi Medical Center offers the Summer Undergraduate Research Experience, which has many attributes similar to those of our Summer undergraduate Research Program (SURP) (18). In contrast, our SURP explicitly seeks to enroll URM and female students. Further, a scarcity of reports exist in the literature that report effective strategies, interventions, and evaluation outcomes in STEMM undergraduate pipeline programs in rural, impoverished southern states such as Arkansas, which account for 20% of Americans and where URM have less access to STEMM careers and chronic health disparities have the largest impact (19).
Arkansas is a rural, low-income southern state. It is the sixth most rural state, with 41% of the population living in rural areas compared to 14% nationally (20). Arkansas has the sixth highest poverty rate, with 17% of the population living below the poverty line compared to 13% nationally (21). Moreover, 37% of the Arkansas population is low-income, and 27% receive Medicaid coverage (22). In rural low-income households, many parents have little formal education. Thus, many of these parents lack expectations for children to pursue a STEMM education and career (23).
At the University of Arkansas for Medical Sciences (UAMS), <7% of the faculty are minorities, which constrains efforts to engage URM communities using URM faculty for direct advocate-to-community engagement. In particular, it constrains biomedical research domains with a focus on cardiovascular and blood disorders, as heart disease is the leading cause of death in the United States, including individuals of most racial and ethnic groups (24, 25). African Americans in Arkansas with reduced cardiovascular function have a significantly higher number of hospitalizations and readmissions than White Americans (26, 27). Further, prevalence of cardiovascular-related chronic conditions, such as congestive heart failure, and mortality risk are nearly twice the national average in many Arkansas counties where poverty persists. Thus, Arkansas is a fitting environment for assessing innovative biomedical training programs to address the complex health needs of its communities. UAMS, the only academic health center in Arkansas, implemented a SURP to increase the volume and quality of URM researchers with interests in cardiovascular, pulmonary, or hematologic research in the biomedical workforce pipeline.
SURP is a nine-week research experience, with the overarching goal to increase the percentage of URM students who pursue STEMM graduate degrees and careers in research or health professions. Specific aims were to: (a) Recruit a diverse group of academically talented and enthusiastic undergraduate students interested in pursuing careers in cardiovascular, pulmonary, or hematologic research, (b) Support and cultivate successful and rewarding mentor-mentee relationships, (c) Develop and promote student leadership and communication skills, (d) Stimulate underrepresented, minority, and disadvantaged students' interest in research and health-related careers, and (e) Evaluate the program and its activities to ensure student satisfaction and program effectiveness.
The purpose of this study was to examine the impact of the SURP on the students' self-efficacy in research, scientific communication, and leadership as well as impact on the extent they identified with science, valued objectives of the scientific community, and their intent to pursue a biomedical research career. We believed other academic health science centers in rural, low-income states could use our findings to help develop or enhance similar mentored research experiences for underrepresented minority undergraduate students.
Materials and methods
Setting
The setting was at UAMS, an academic health science medical center in a rural, low-income southern state.
Participants
The participants were URM, female, and first-generation undergraduate students enrolled in the 2022 and 2023 SURP.
Study design
The study design was a one-group, retrospective pre-post, and qualitative framework analysis.
Procedures
Each year, the SURP recruited and accepted up to 13 URM, female, or first-generation undergraduate students from colleges and universities throughout the U.S. The program has received an average of 70 applications per year. Program directors reviewed each application and selected participants based on several requirements. Participants were U.S. citizens who had completed at least 1 year of undergraduate studies with a minimum of 2.5 GPA. Applicants also answered questions about their research experience and career goals. In addition, applicants provided two letters of recommendation from faculty. Once accepted into the program, UAMS hired SURP participants as temporary student employees for 9-weeks during the summer.
Before the program began, based on the students' interest and background, SURP administrators paired each student with a faculty mentor, who supervised the students' summer research project and worked closely with the student throughout the summer. A SURP administrator had formal mentor training at the Center for the Improvement of Mentored Experiences in Research in Wisconsin and is currently participating in a campus wide effort to facilitate research mentor and mentee training at UAMS. The SURP program provided funding for research supplies. In mid-summer, students introduced their research project to other SURP participants and program staff. The research project culminated with each student delivering a research presentation in an open forum to all faculty mentors, program participants, and SURP administrators as well as invited faculty and family members.
In addition to the research project, students attended weekly research and professional development seminars. The seminars exposed students to various areas of research on the UAMS campus and sought to increase their knowledge about biomedical science and research careers. Students received a comprehensive tour of all of the research areas on the campus and had the opportunity to shadow health professionals who worked in the clinics and main hospital. At the conclusion of the program, students completed an evaluation. This manuscript presents the results of that evaluation.
Theoretical framework
The Tripartite Integration Model of Social Influence served as the theoretical framework for the program and the evaluation (28, 29). This framework helps explain how people socially integrate into a community. It features three social variables that influence the extent someone integrates into a community: (a) self-efficacy, (b) identity, and (c) values. In the context of this study, scientific self-efficacy refers to the extent the students believed in their ability to meet the challenges of planning, conducting and communicating about scientific experiments. Scientific identity was the extent the students had a gratifying definition of themselves as scientists. Scientific community values reflected how aligned the students were with the objectives of the scientific community. Together, scientific self-efficacy, science identity, and scientific community values can influence biomedical research career intention. Effective mentorship, a key component of our SURP, can promote self-efficacy, identity, and values (30, 31).
Measures
Demographic measures included undergraduate status, first-generation college student, gender, race, and ethnicity. We elicited the students' satisfaction with the program, including relevance, extent the SURP stimulated interest in a biomedical research career, quality, and recommending the SURP to other students.
The Mentoring Competency Assessment examines the competencies and skills of scientists who serve as research mentors (32). The instrument features a seven-point Likert scale (1 = Not at all skilled; 7 = Extremely skilled) to assess 26 skills needed for six competencies, including:: (a) Communication, (b) Alignment of expectations, (c) Assessment of understanding, (d) Fostering independence, (e) Addressing diversity, and (f) Promoting professional development. For example, skills for communication included active listening, providing constructive feedback, and developing a trusting relationship. Aligning expectations included setting goals and developing strategies to meet them. Assessing understanding included assessing the mentee's knowledge and ability. Fostering independence included motivating mentees, building their confidence, and stimulating creativity. Addressing diversity included accounting for different backgrounds. Promoting professional development included facilitating networking and setting career goals.
The investigators used a retrospective post then pre survey method for several measures. With this method, students made two separate sets of ratings, both post-SURP and pre-SURP, only after participating in the SURP. First, the students made post-SURP “NOW” or “AFTER” ratings about their knowledge, skills, attitude, or behaviors. Then, we asked the students to reflect back and rate the same knowledge, skills, attitude, or behaviors “BEFORE” the SURP. Previous research on survey methodology demonstrated that compared to conventional pre and post measures, the retrospective post then pre design reduced participants' overestimation of pre measures and, therefore, avoided underestimation of effect size (33, 34). Post then pre measures included self-efficacy in research competencies, scientific communication, and leadership as well as scientific identity, scientific values, and intention to pursue a research career in biomedical science (35–38). To compare post then pre outcomes for these constructs, the investigators totaled the score for each construct and divided each total by the number of possible points, to arrive at a score on a 100-point scale.
Additionally, students provided written reflections to qualitative inquiries about science identity and values as well as intention to pursue a biomedical research career. Seven open-ended questions assessed program strengths and weaknesses as well as how the program influenced career or academic choices.
Analysis
Descriptive statistics summarized data for demographics, satisfaction, mentoring competencies as well as self-efficacy in research competencies, scientific communication, leadership scientific identity, and scientific values. Median (Mdn) with interquartile ranges (IQR) expressed central tendency and the spread of the middle half of the nonparametric data.
The Wilcoxon rank sum test for nonparametric variables compared pre- and post- self-efficacy for research competencies, scientific communication, leadership scientific identity, scientific values, and intention to pursue a research career in biomedical science. The equation (r) = Z/square root of N estimated effect size. Alpha was p < 0.05.
For written responses to qualitative inquiries, the investigators used a conceptual analysis, with top-down deductive themes and inductive sub-themes. MAXQDA (2021) software analyzed qualitative data.
Ethics
The UAMS institutional review board determined this study was not human subject research.
Results
Participants
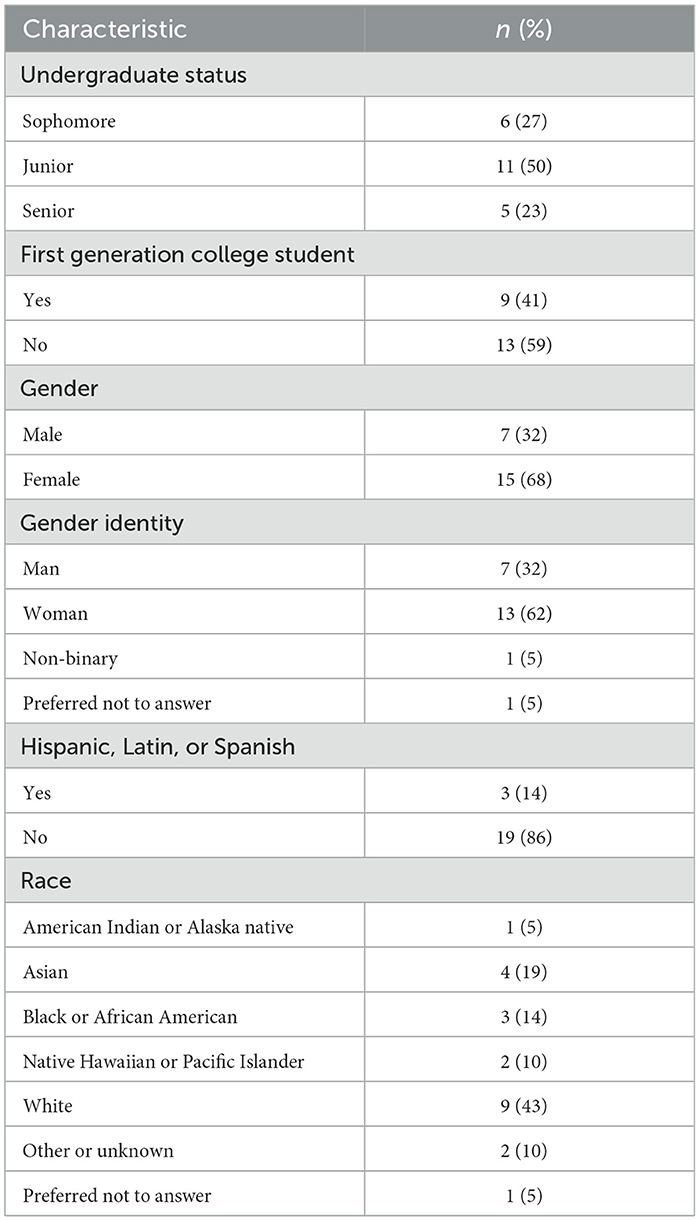
Twenty-two (N = 22) students participated, with 12 in 2022 and 10 in 2023. Ninety-five percent were URM, women, or first-generation college students (see Table 1).
Satisfaction
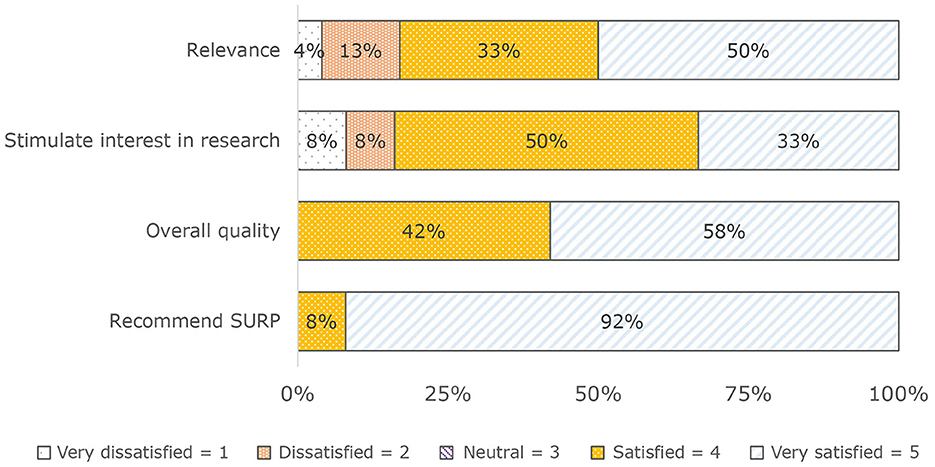
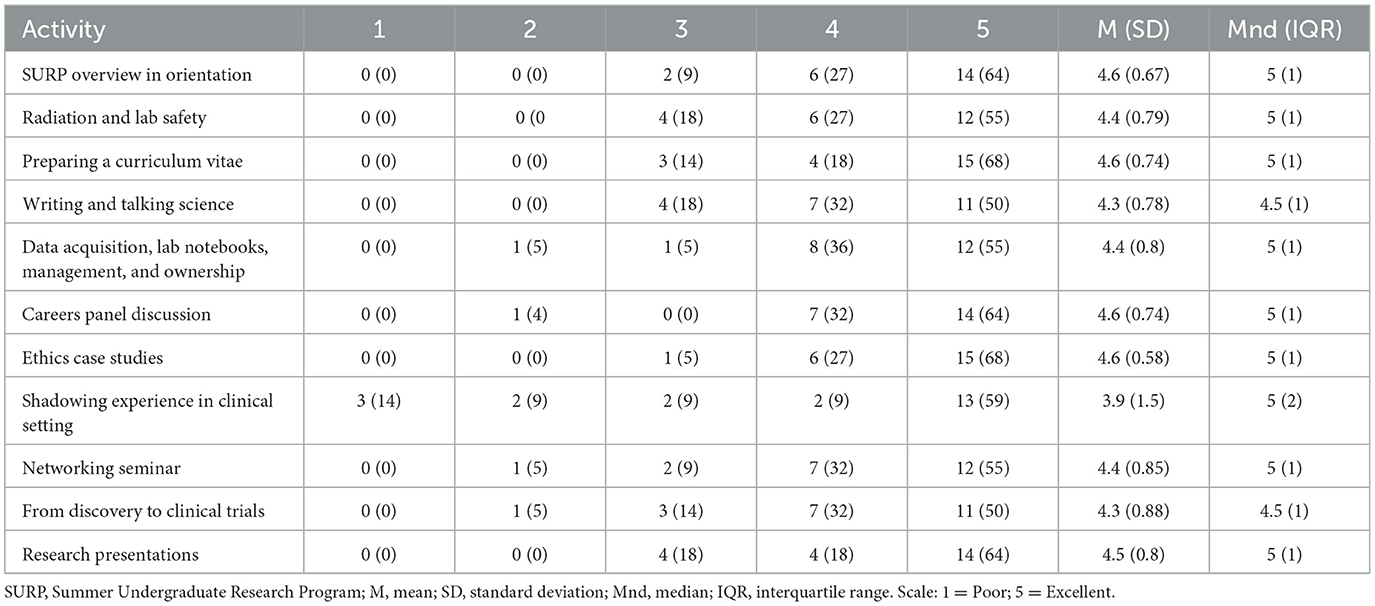
Students were satisfied with the SURP. They rated the SURP positively for: (a) Relevance (83%), (b) Extent the SURP stimulated interest in a biomedical research career (83%), (c) Quality (100%), and (d) Recommending the SURP to other students (100%) (see Figure 1). Similarly, with the exception of shadowing experiences in the clinical setting, most students were satisfied with each educational activity outside of their mentored research experience (Table 2).
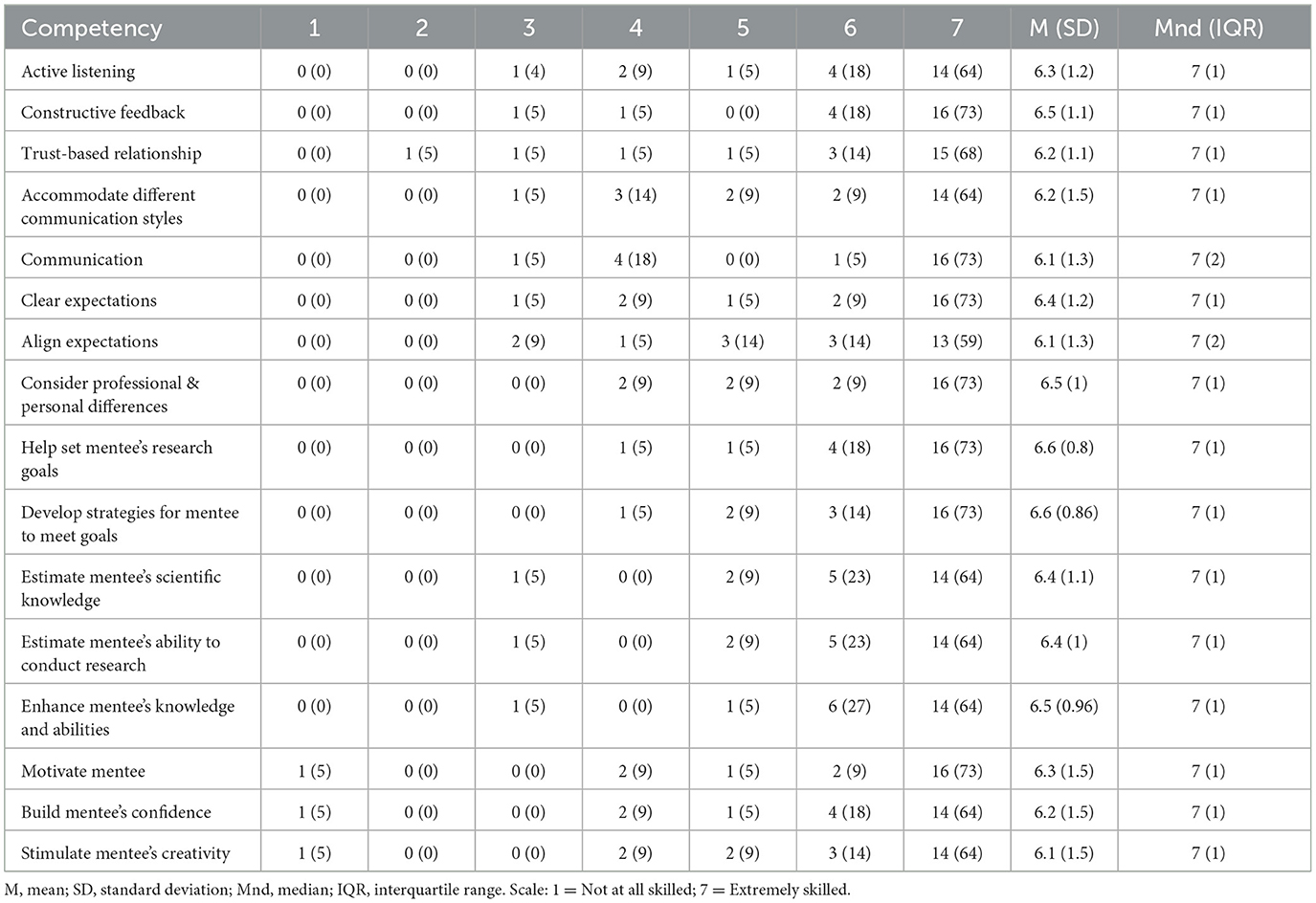
Mentorship
For the mentored research experiences, the students' median rating for all domains of the mentee-mentor relationship was 7, on a seven-point scale (see Table 3).
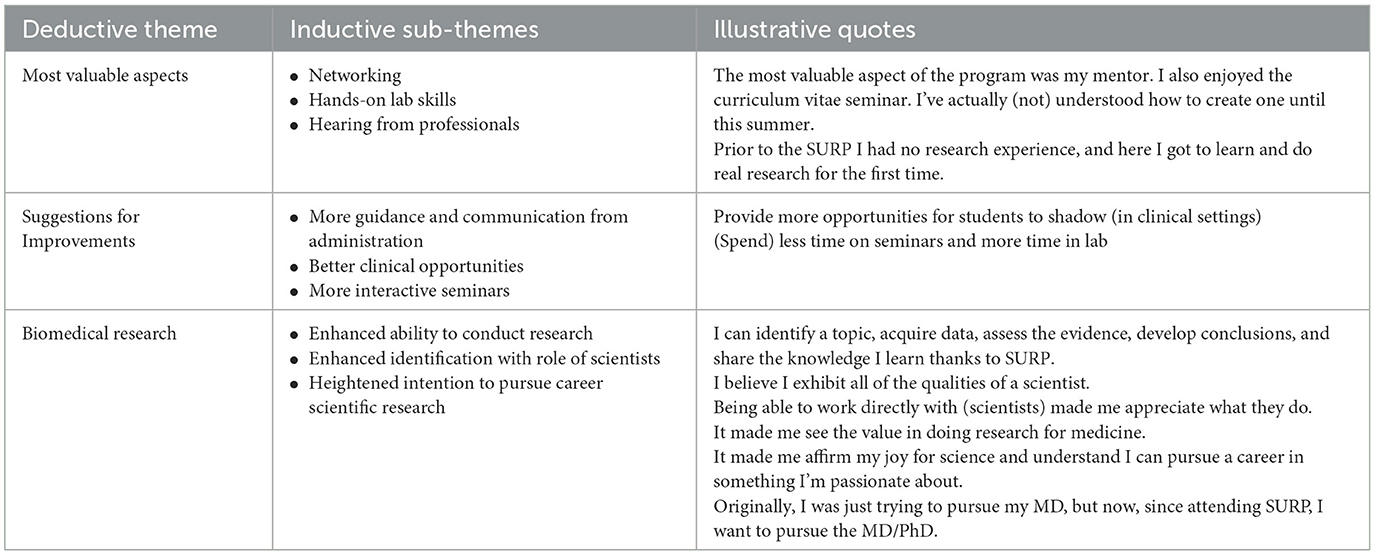
Qualitative inquiry
When asked to discuss the most valuable aspect(s) of the SURP, major themes were networking, hands-on lab training and skills, mentee-mentor relationships, and research experience (Table 4). The participants' suggestions for improving the SURP were: (a) Better pairing of mentees with mentors, (b) Fewer and more interactive seminars, and (c) More clinical and shadowing opportunities. We then asked participants to discuss how the SURP affected their ability to conduct research. Many indicated they had a better understanding of research, learned new lab techniques, and had more interest in research. We also wanted to know if the SURP affected how participants identified with the role of scientists. An overwhelming number of participants indicated they had a “better understanding of research and the role of a scientist.” The next question asked participants to discuss how the SURP affected how they value the objectives of the scientific community. Several participants mentioned more value and appreciation for the scientific community, including a better understanding of the importance of science in relation to medicine as well as more appreciation and respect for the scientific community. How the SURP affected the intent to pursue a science related research career received mixed responses. Some participants indicated the SURP confirmed their intent to pursue a science related research career, while others said it prompted their intent to pursue both an MD/PhD, and a few indicated it stimulated their interest in conducting clinical research as a physician.
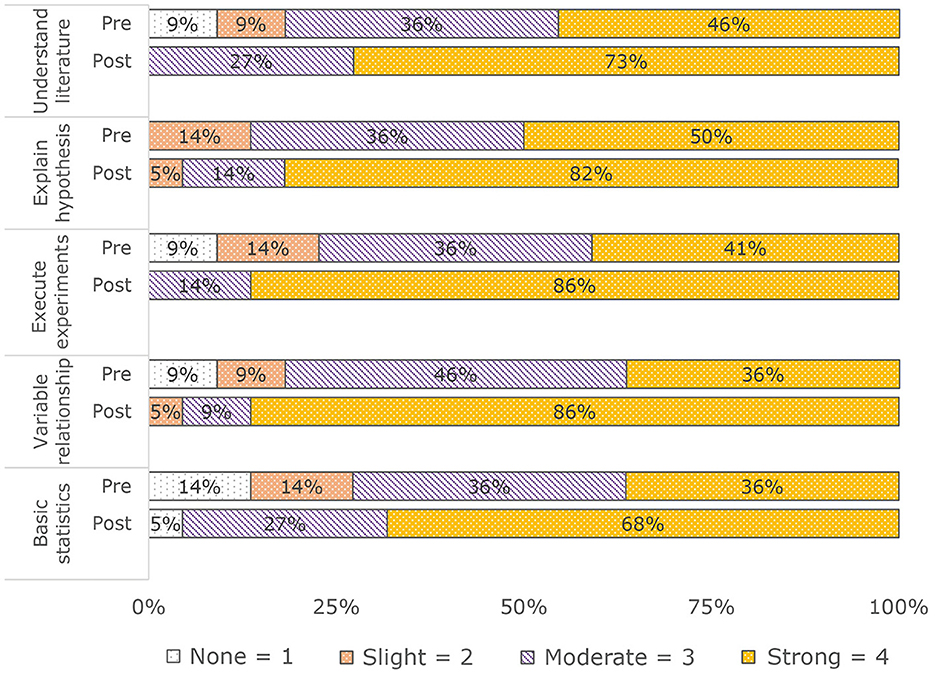
Self-efficacy in research competencies
Post-SURP, students reported higher self-efficacy score for each research competency: (a) Understand literature Pre: M (SD) = 3.2 (0.9); Mnd (IQR) = 3 (1); Post: M (SD) = 3.7 (0.5); Mnd (IQR) = 4 (1); (b) Explain hypothesis (Pre: M (SD) = 3.4 (0.7); Mnd (IQR) = 3.5 (1); Post: M (SD) = 3.8 (0.5); Mnd (IQR) = 4 (0); (c) Execute experiments: Pre: M (SD) = 3.1 (1); Mnd (IQR) = 3 (1); Post: M (SD) = 3.9 (0.4); Mnd (IQR) = 4 (0); (d) Variable relationship: Pre: M (SD) = 3.1 (0.9); Mnd (IQR) = 3 (1); Post: M (SD) = 3.8 (0.5); Mnd (IQR) = 4 (0); (e) Basic statistics: Pre: M (SD) = 3 (1); Mnd (IQR) = 3 (2); Post: M (SD) = 3.6 (0.7); Mnd (IQR) = 4 (1) (see Figure 2).
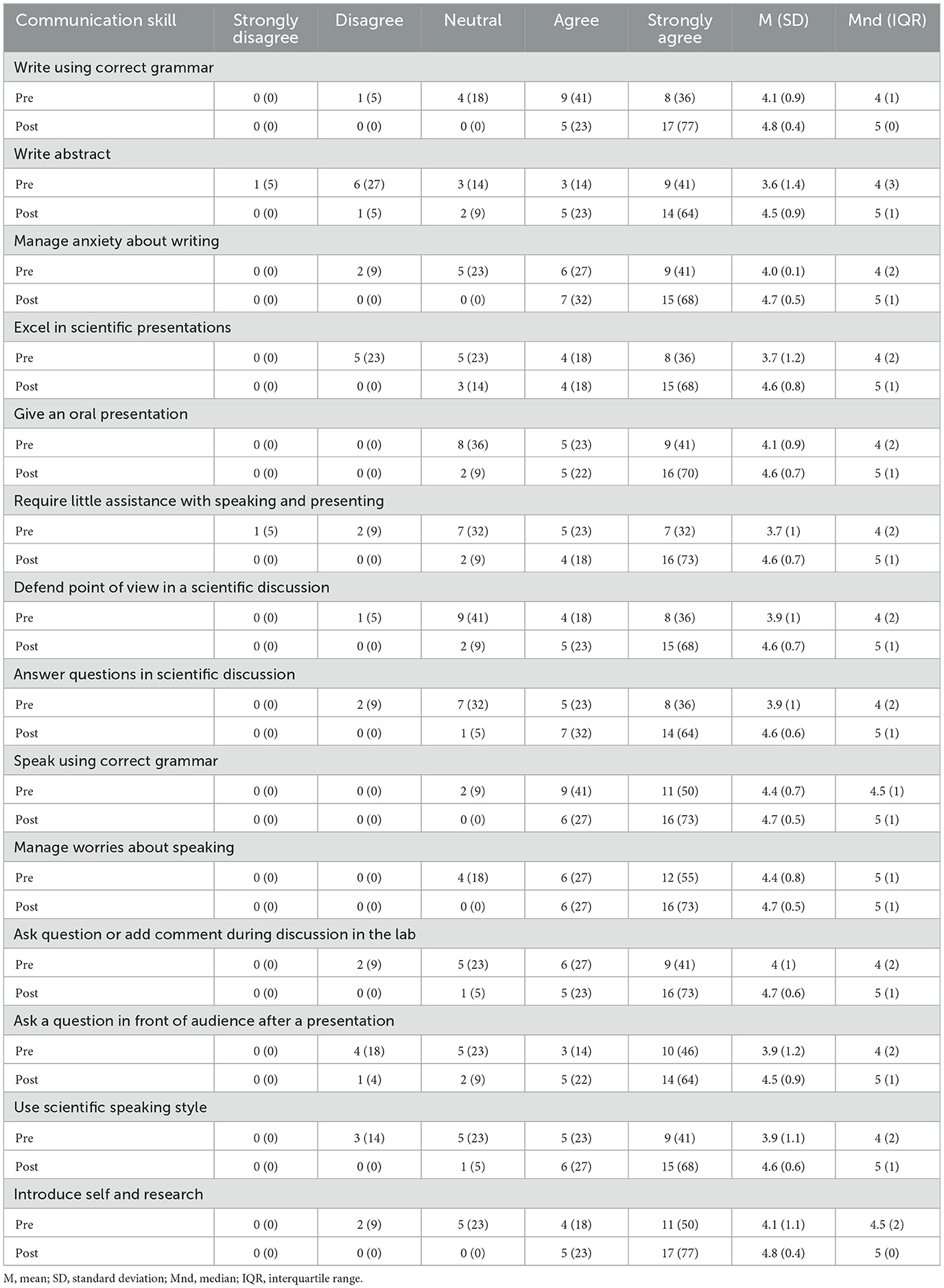
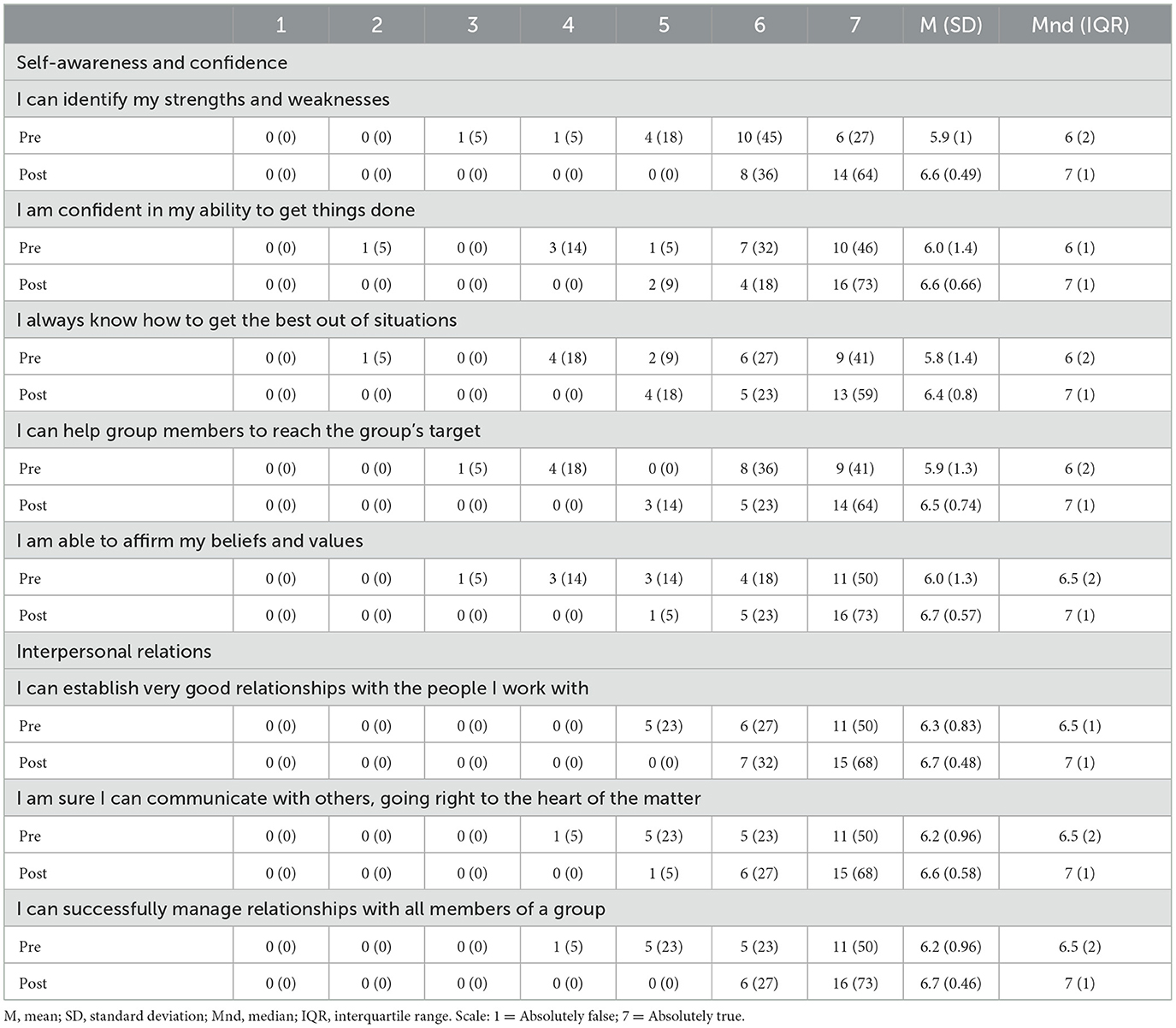
Self-efficacy in scientific communication and leadership
Post-SURP, students reported higher self-efficacy scores for each facet of scientific communication we measured as well as measures for internal and external leadership (see Tables 5, 6).
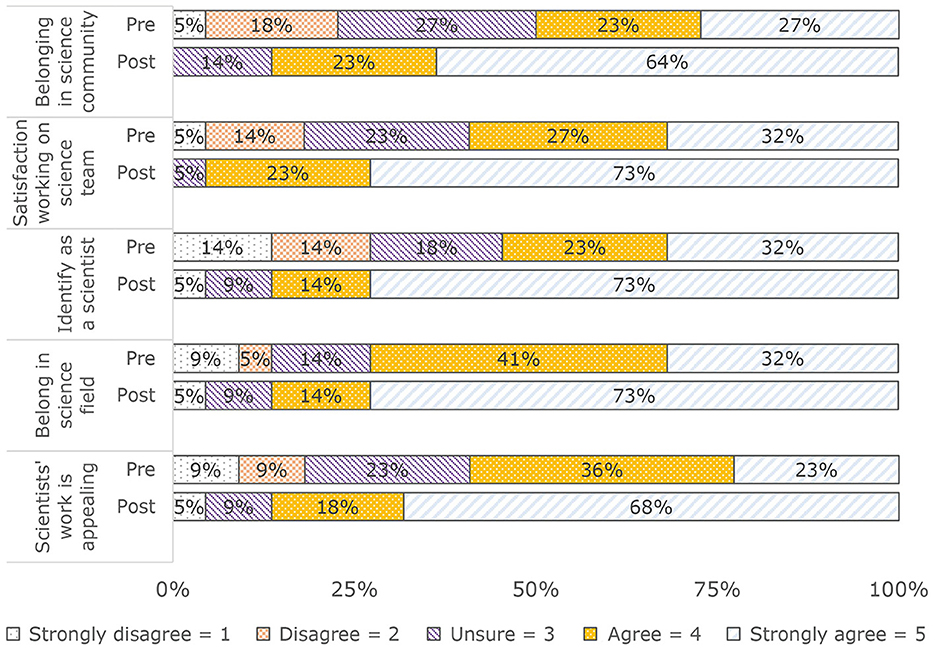
Science identity
Post-SURP, students reported higher scores for each facet of science identity: (a) Belonging in science community: Pre: M (SD) = 3.5 (1.2); Mnd (IQR) = 3.5 (2); Post: M (SD) = 4.5 (0.7); Mnd (IQR) = 5 (1); (b) Satisfaction working on science team: Pre: M (SD) = 3.2 (1.2); Mnd (IQR) = 4 (2); Post: M (SD) = 4.7 (0.6); Mnd (IQR) = 5 (1); (c) Identify as a scientist: Pre: M (SD) = 3.5 (1.4); Mnd (IQR) = 4 (3); Post: M (SD) = 4.7 (0.6); Mnd (IQR) = 5 (1); (d) Belonging in science field: Pre: M (SD) = 3.8 (1.2); Mnd (IQR) = 4 (2); Post: M (SD) = 4.5 (0.9); Mnd (IQR) = 5 (1); (e) Scientists' work is appealing: Pre: M (SD) = 3.6 (1.2); Mnd (IQR) =4 (1); Post: M (SD) = 4.5 (1); Mnd (IQR) = 5 (1) (see Figure 3).
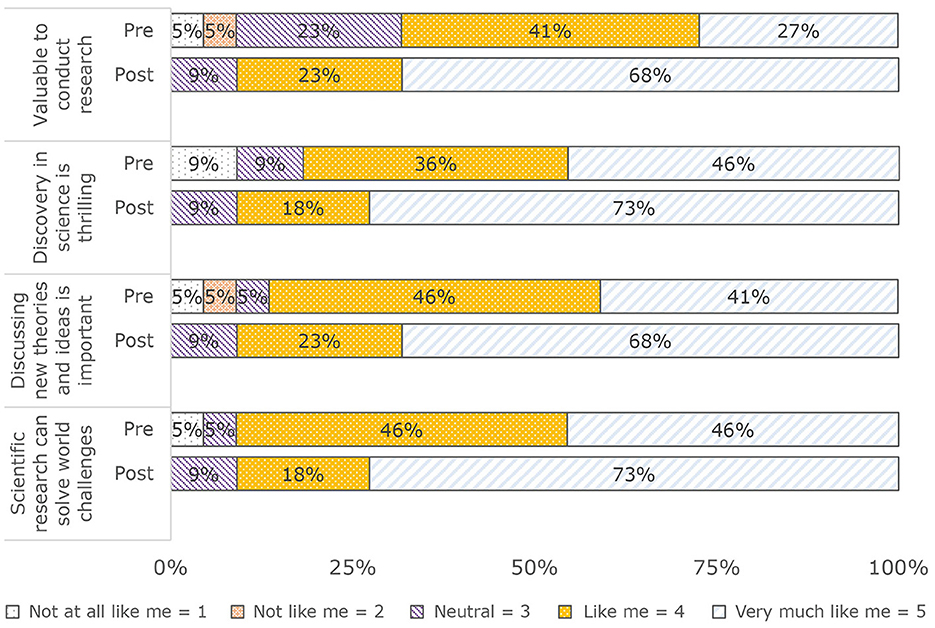
Valuing objectives of the scientific community
Post-SURP, students reported higher scores for each facet of valuing the objectives of the scientific community: (a) Valuable to conduct research: Pre: M (SD) = 3.8 (1); Mnd (IQR) = 4 (2); Post: M (SD) = 4.6 (0.7); Mnd (IQR) = 5 (1); (b) Discovery in science is thrilling: Pre: M (SD) = 4.2 (1); Mnd (IQR) = 4 (1); Post: M (SD) = 4.6 (0.7); Mnd (IQR) = 5 (1); (c) Discussing new theories and ideas is important: Pre: M (SD) = 4.1 (1); Mnd (IQR) = 4 (1); Post: M (SD) = 4.6 (0.7); Mnd (IQR) = 5 (1); (d) Scientific research can solve world challenges: Pre: M (SD) = 4.3 (0.9); Mnd (IQR) = 4 (1); Post: M (SD) = 4.6 (0.7); Mnd (IQR) = 5 (1) (see Figure 4).
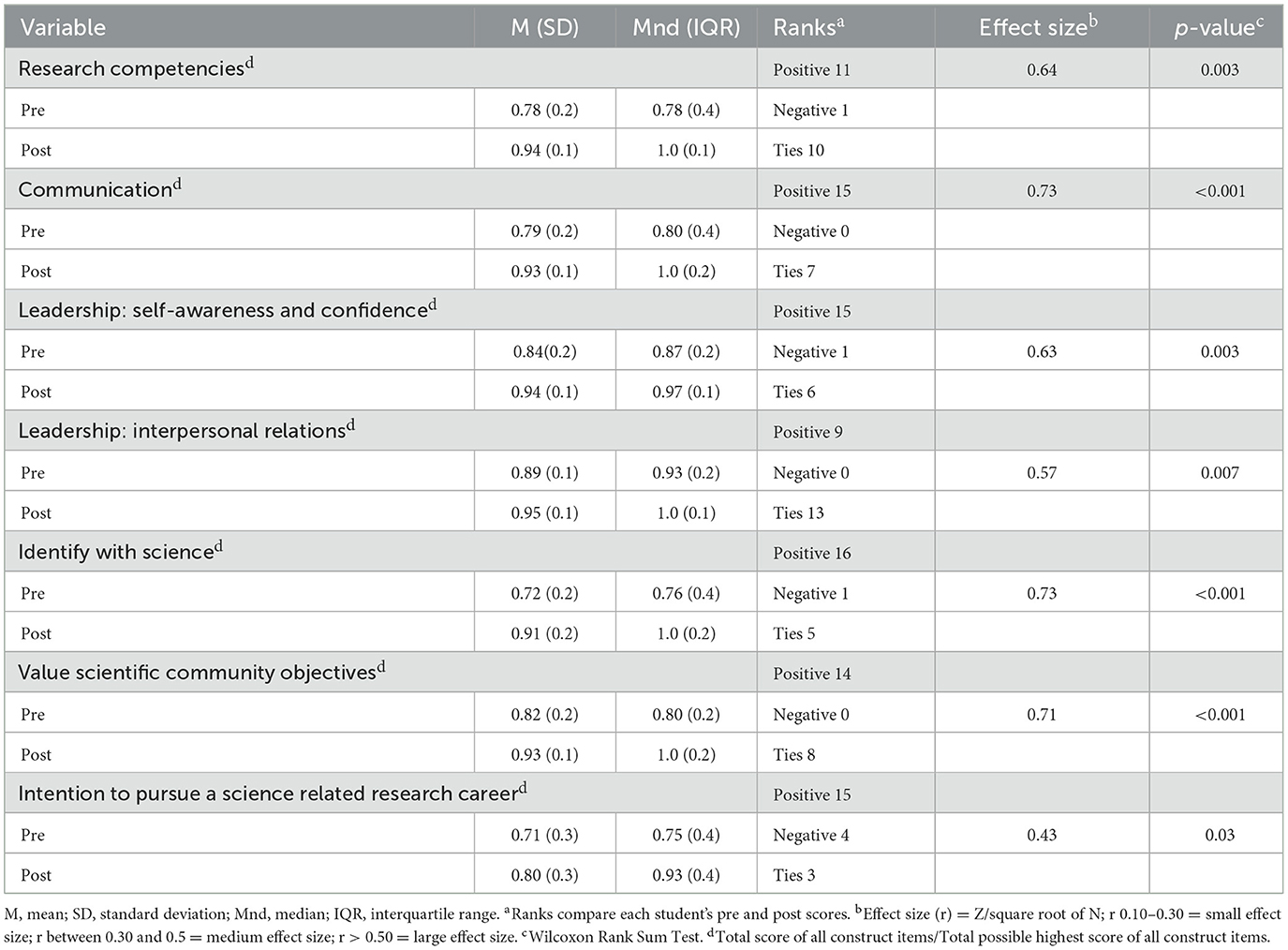
Comparison of pre- and post-outcomes for construct totals and intention to pursue biomedical research career
Compared to pre-SURP measures, post-SURP measures were significantly higher with medium or large effect sizes (see Table 7).
Discussion
Summary of the results
Study results demonstrated students were satisfied with the SURP and rated their mentee-mentor relationships highly. Compared to pre-SURP, self-efficacy in research, scientific communication, and leadership as well as increased science identity and valuing the objectives of the scientific community improved post-SURP. Further, compared to pre-SURP, post-SURP students indicated a stronger intention to pursue a career in biomedical research. Qualitative inquiry revealed the SURP encouraged students' to strongly identify with science, value the scientific community's objectives, and intend to pursue a biomedical research career.
Explanation of the results
The Tripartite Integration Model of Social Influence helps explain our findings (28, 29). The model provides a framework for explaining how a URM student orients to a scientific community/research environments (11). The model posits individuals socialize into a group through three processes: building scientific efficacy (i.e., following rules and norms for rewards, minimizing punishment), building scientific identity (i.e., developing a social identity that includes the environment), and internalizing scientific community values (i.e., embracing and sharing the values of the group/research (31)). Our results suggest: (a) The SURP contributed to the students' increased self-efficacy and (b) Increased self-efficacy generated by the SURP program may have influenced the students'intention to pursue a scientific career. Immersive mentored research projects and hands-on laboratory training help explain students' increased self-efficacy in research, scientific communication, and leadership. In turn, increased self-efficacy likely explains the students' increased science identity and valuing objectives of the scientific community, which may explain their enhanced intention to pursue a biomedical research career.
Comparison with other studies
Our results were consistent with that of other studies that demonstrated the influence of summer research programs on intention to pursue a career in the biomedical research workforce. A previous report about our SURP demonstrated students had positive and sustained interactions with mentors and the SURP influenced their career goals (39). The current study extends these results. Hernandez et al. (31) found development of science identity and values was associated with intention to pursue a STEMM career in undergraduates in several summer research programs. A qualitative study of the Arkansas IDeA Network of Biomedical Research Excellence Summer Research Fellowship found providing mentored research experiences for undergraduate students enhanced their interest in pursuing a career in the biomedical research workforce (40). A study in Idaho revealed improvements in science identity were associated with transitioning from summer undergraduate research to graduate school. The study found 91.4% of summer research students entered a scientific or healthcare related career, while 71% pursued graduate training, citing improved awareness of science as a cause of pursuing in the workforce pipeline (41). Similarly, the K-INBRE, a summer undergraduate research program in Kansas, identified career awareness as a critical component of program success, with 37% of students matriculating into graduate programs, 19% into medical school, and 12% into health-related professions (42). Yassa et al. (43) reported improvement in science self-efficacy and identity as well as visualization of a career as a scientist, in students predominantly from a Historically Black Universities after they participated in a mentored summer research program at the University of California. Both the Short-term Research Education Program to Increase Diversity in Health-Related Research Fellowships and the Integrative Organismal Systems Physiology Fellowships enrolled underrepresented students (44). However, none of the programs in these studies specifically targeted URM and female students in a rural, low-income southern state and reported outcomes that included science identity and alignment of values with the scientific community, which are components of the Tripartite Integration Model of Social Influence.
Summer research programs increased the probability of retaining students in the pipeline by expanding career awareness components of the programs beyond their common elements, such as lectures and lab exposure. This expansion could include a framework for career intention, such as the Tripartite Integration Model of Social Influence. Effective career awareness programs do the following: (a) Engage family, teachers, and friends of the students and (b) Use socialization initiatives to rebrand science, such as mitigating negative gender connotations (45). However, unlike the SURP, previous summer research programs do not universally integrate these strategies for enhancing career intention.
Limitations
This study had several limitations. Prominent among them was the use of self-reported data. Students could have provided inaccurate responses. However, the questions were anonymous, evidence exists for validity of the outcomes measures, and our findings were consistent with that of other studies. Additionally, the retrospective post then pre design could have introduced a recall bias. However, we used this design to help avoid response-shift bias seen with traditional pre-post measures, that is, students' pre-SURP self-evaluation overestimation of their self-efficacy, values, and intentions, which could result in underestimation of the SURP outcomes (31, 32).
Implications
Our study supports implementation of a biomedical research pipeline for URM and women in a poor, rural, and settings. Future studies should examine long-term academic and career outcomes and, ultimately, the impact on health disparities.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
MA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. LP: Data curation, Formal analysis, Funding acquisition, Project administration, Writing – original draft, Writing – review & editing. TW: Data curation, Funding acquisition, Writing – original draft, Writing – review & editing. RM: Funding acquisition, Project administration, Supervision, Writing – original draft, Writing – review & editing. BT: Funding acquisition, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. AA: Funding acquisition, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This program received support from the National Heart, Lung, and Blood Institute, Grant R25HL108825.
Acknowledgments
The authors acknowledge the guidance and support of the UAMS faculty members who served as mentors for the SURP students, the UAMS graduate school staff for providing administrative guidance to the SURP students and faculty, and Diane Mckinstry, Outreach Program Manager for the Arkansas IdeA Network for Biomedical Research Excellence, for collaborating with the SURP.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pittman P, Chen C, Erikson C, Salsberg E, Luo Q, Vichare A, et al. Health workforce for health equity. Med Care. (2021) 59:S405–8. doi: 10.1097/MLR.0000000000001609
2. Byrd K, Sege R. Developing a Racially Diverse Biomedical Research Workforce. Health Resources in Action. (2016). Available online at: https://hria.org/resources/developing-racially-diverse-biomedical-research-workfroce/ (accessed March 1, 2024).
3. Freeman RB, Huang W. Collaborating With People Like Me: Ethnic Co-Authorship Within The U.S. National Bureau of Economic Research. (2014). Available online at: https://www.nber.org/papers/w19905 (accessed February 28, 2024).
4. Campbell LG, Mehtani S, Dozier ME, Rinehart J. Gender-heterogeneous working groups produce higher quality science. PLoS ONE. (2013) 8:e79147. doi: 10.1371/journal.pone.0079147
5. United States Census Bureau. QuickFacts: United States. (2023). Available online at: https://www.census.gov/quickfacts/fact/table/US/PST045223 (accessed February 28, 2024).
6. Xierali IM, Nivet MA, Rayburn WF. Full-time faculty in clinical and basic science departments by sex and underrepresented in medicine status: a 40-year review. Acad Med. (2021) 96:568–75. doi: 10.1097/ACM.0000000000003925
7. National Institutes for Health. NIH Data Book. (2024). Available online at: https://report.nih.gov/nihdatabook/ (accessed February 28, 2024).
8. National Center for Science and Engineering Statistics. Survey of Earned Doctorates. National Science Foundation. (2020). Available online at: https://ncses.nsf.gov/pubs/nsf21320 (accessed March 1, 2024).
9. Hurtado S, Ruiz AA. Research Brief: Discrimination and Bias, Underrepresentation, and Sense of Belonging on Campus. Higher Education Research Institute. (2015). Available online at: https://www.heri.ucla.edu/PDFs/Discriminination-and-Bias-Underrepresentation-and-Sense-of-Belonging-on-Campus.pdf (accessed March 1, 2024).
10. Toven-Lindsey B, Levis-Fitzgerald M, Barber PH, Hasson T. Increasing persistence in undergraduate science majors: a model for institutional support of underrepresented students. CBE Life Sci Educ. (2015) 4:ar12. doi: 10.1187/cbe.14-05-0082
11. Hechinger Report: Covering Innovation and Inequality in Education. (2021). Available online at: https://hechingerreport.org/even-as-colleges-pledge-to-improve-share-of-engineering-graduates-who-are-black-declines/#:~:text=But%20the%20numbers%20diverge%20when,34%20percent%20of%20Black%20students (accessed February 29, 2024).
12. National Center for Education Statistics. Status and Trends in the Education of Racial and Ethnic Groups. (2020). Available online at: https://nces.ed.gov/programs/raceindicators/index.asp (accessed February 28, 2024).
13. Fry R, Kennedy B, Funk C. STEMM Jobs See Uneven Progress in Increasing Gender, Racial and Ethnic Diversity. PEW Research Center. (2021). Available online at: https://www.pewresearch.org/science/wp-content/uploads/sites/16/2021/03/PS_2021.04.01_diversity-in-STEMM_REPORT.pdf (accessed February 28, 2024).
14. Lopatto D. Undergraduate research experiences support science career decisions and active learning. CBE Life Sci Educ. (2007) 6:297–306. doi: 10.1187/cbe.07-06-0039
15. Stephenson-Hunter C, Strelnick AH, Rodriguez N, Stumpf LA, Spano H, Gonzalez CM, et al. Dreams realized: a long-term program evaluation of three summer diversity pipeline programs. Health Equity. (2021) 5:512–20. doi: 10.1089/heq.2020.0126
16. Bruthers CB, Matyas ML. Undergraduates from underrepresented groups gain research skills and career aspirations through summer research fellowship. Adv Physiol Educ. (2020) 4:525–39. doi: 10.1152/advan.00014.2020
17. Association of American Medical Colleges. Summer Undergraduate Research Programs. (2024). Available online at: https://www.aamc.org/career-development/affinity-groups/great/summer-undergrad-research-programs (accessed April 4, 2024).
18. University University of Mississippi Medical Center School School of Graduate Studies in the Health Sciences. Summer Undergraduate Research Experience. (2024). Available online at: https://www.umc.edu/graduateschool/SURE/SURE_Overview.html (accessed April 4, 2024).
19. Williams TB, Garza M, Lipchitz R, Powell T, Baghal A, Swindle T, et al. Cultivating informatics capacity for multimorbidity: a learning health systems use case. J Multimorb Comorb. (2022) 12:26335565221122017. doi: 10.1177/26335565221122017
20. U.S. Department of Agriculture. Rural America at a Glance. (2021). Available online at: https://www.ers.usda.gov/webdocs/publications/102576/eib-230.pdf?v=4409#:~:text=The%2046%20million%20U.S.%20residents,percent%20of%20the%20U.S.%20population (accessed March 1, 2024).
21. U.S. Census Bureau. American Community Survey. (2019). Available online at: https://www.census.gov/programs-surveys/acs (accessed February 28, 2024).
22. Kaiser Family Foundation. Medicaid in Arkansas. (2023). Available online at: https://files.kff.org/attachment/fact-sheet-medicaid-state-AR (accessed February 28, 2024).
23. Hill NE, Tyson DF. Parental involvement in middle school: a meta-analytic assessment of the strategies that promote achievement. Dev Psychol. (2009) 45:740–63. doi: 10.1037/a0015362
24. Centers for Disease Control and Prevention. Heart Disease Facts. (2023). Available online at: https://www.cdc.gov/heartdisease/facts.htm (accessed February 29, 2024).
25. Williams TB, Crump A, Garza MY, Parker N, Simmons S, Lipschitz R, et al. Care delivery team composition effect on hospitalization risk in African Americans with congestive heart failure. PLoS ONE. (2023) 18:e0286363. doi: 10.1371/journal.pone.0286363
26. Barnes JW, Massing M, Dugyala S, Cottoms N, Pursell IW. Design of a novel intervention model to address cardiovascular health disparities in the rural underserved community of Phillips County Arkansas. Health Equity. (2022) 6:248–53. doi: 10.1089/heq.2021.0175
27. Centers for Disease Control and Prevention. Interactive Atlas of Heart Disease and Stroke. (2024). Available online at: http://nccd.cdc.gov/DHDSPAtlas (accessed March 1, 2024).
28. Kelman H. Compliance, identification, and internalization: three processes of attitude change. Conf Res. (1958) 2:51–60. doi: 10.1177/002200275800200106
29. Estrada M, Woodcock A, Hernandez PR, Schultz PW. Toward a model of social influence that explains minority student integration into the scientific community. J Educ Psychol. (2011) 103:206–22. doi: 10.1037/a0020743
30. Crisp G, Cruz I. Mentoring college students: a critical review of the literature between 1990 and 2007. Res High Educ. (2009) 50:525–45. doi: 10.1007/s11162-009-9130-2
31. Hernandez PR, Hopkins PD, Masters K, Holland L, Mei BM, Richards-Babb M, et al. Student integration into STEMM careers and culture: a longitudinal examination of summer faculty mentors and project ownership. CBE Life Sci Educ. (2018) 7:ar50. doi: 10.1187/cbe.18-02-0022
32. Fleming M, House S, Shewkramani V, Yu L, Garbutt J, McGee R, et al. The mentoring competency assessment: validation of a new instrument to evaluate skills of research mentors. Acad Med. (2013) 88:1002–8. doi: 10.1097/ACM.0b013e318295e298
33. Drennan J, Hyde A. Controlling response shift bias: the use of the retrospective pre-test design in the evaluation of a master's programme. Assessm Eval Higher Educ. (2008) 33:699–709. doi: 10.1080/02602930701773026
34. Thomas EV, Wells R, Baumann SD, Graybill E, Roach A, Truscott SD, et al. Comparing traditional versus retrospective pre-/post-assessment in an interdisciplinary leadership training program. Matern Child Health J. (2019) 23:191–200. doi: 10.1007/s10995-018-2615-x
35. Estrada M, Hernandez PR, Schultz PW, A. longitudinal study of how quality mentorship and research experience integrate underrepresented minorities into STEMM Careers. CBE Life Sci Educ. (2018) 17:ar9. doi: 10.1187/cbe.17-04-0066
36. Verderame MF, Freedman VH, Kozlowski LM, McCormack WT. Competency-based assessment for the training of PhD students and early-career scientists. Elife. (2018) 7:e34801. doi: 10.7554/eLife.34801
37. Anderson CB, Lee HY, Byars-Winston A, Baldwin CD, Cameron C, Chang S. Assessment of scientific communication self-efficacy, interest, and outcome expectations for career development in academic medicine. J Career Assess. (2016) 24:182–96. doi: 10.1177/1069072714565780
38. Bobbio A, Manganelli AM. Leadership self-efficacy scale: a new multidimensional instrument. Testing Psychometr Methodol Appl Psychol. (2009) 16:3–24.
39. Prince LY, Williams TB, Allen AR, McGehee RE Jr, Thomas BR. Outcomes of the UAMS summer undergraduate research program to increase diversity in research and health professions. Adv Physiol Educ. (2023) 47:20–5. doi: 10.1152/advan.00201.2022
40. McSweeney JC, Hudson TJ, Prince L, Beneš H, Tackett AJ, Miller Robinson C, et al. Impact of the INBRE summer student mentored research program on undergraduate students in Arkansas. Adv Physiol Educ. (2018) 42:123–9. doi: 10.1152/advan.00127.2017
41. Heggland SJ, Hovde CJ, Minnich SA, Liou LE, Daniels RL. Building a biomedical pipeline: the impact of the Idaho IDeA INBRE summer research experience at a primarily undergraduate institution. Adv Physiol Educ. (2021) 45:786–96. doi: 10.1152/advan.00232.2020
42. Chapes SK, Velasquez SE. Assessment of the impact of the Kansas IDeA network of biomedical research excellence program on undergraduate participation in research. J Microbiol Biol Educ. (2013) 14:47–57. doi: 10.1128/jmbe.v14i1.492
43. Yassa M, Chen C. Outcomes and lessons learned from an intensive summer undergraduate research program in neuroscience. J Stem Outreach. (2023) 22:6. doi: 10.15695/jstem/v6i1.06
44. Bruthers CB, Hedman EL, Matyas ML. Undergraduate research programs build skills for diverse students. Adv Physiol Educ. (2021) 45:399–408. doi: 10.1152/advan.00165.2020
Keywords: minority groups, female, education, medical, undergraduate, biomedical research, mentors, surveys and questionnaires
Citation: Anders ME, Prince LY, Williams TB, McGehee RE Jr, Thomas BR and Allen AR (2024) Summer undergraduate biomedical research program for underrepresented minority students in a rural, low-income state. Front. Public Health 12:1395942. doi: 10.3389/fpubh.2024.1395942
Received: 04 March 2024; Accepted: 13 May 2024;
Published: 23 May 2024.
Edited by:
Tomas Nuno, University of Arizona, United StatesReviewed by:
Edgar Meyer, University of Mississippi Medical Center, United StatesSean Maurice, University of Northern British Columbia, Canada
Copyright © 2024 Anders, Prince, Williams, McGehee, Thomas and Allen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael E. Anders, YW5kZXJzbWljaGFlbGVAdWFtcy5lZHU=
 Michael E. Anders
Michael E. Anders Latrina Y. Prince2
Latrina Y. Prince2 Tremaine B. Williams
Tremaine B. Williams Billy R. Thomas
Billy R. Thomas