- 1The School of Physical Education and Sports, Central China Normal University, Wuhan, China
- 2The School of Physical Education, Dali University, Yunnan, China
Objective: This study systematically evaluates the impact of different physical exercise modalities on vision health interventions for Chinese children and adolescents.
Methods: A comprehensive search was conducted in databases, including Web of Science, PubMed, EBSCO, MEDLINE, Embase, and CNKI. The focus was on randomized controlled trial (RCT) studies related to physical activity interventions for vision health in this demographic. The search covered literature from the inception of each database until May 1, 2023. Two researchers independently conducted literature screening, data extraction, and risk of bias assessment, adhering to pre-established inclusion and exclusion criteria. A network meta-analysis was performed using the “Network” package in Stata 14.2.
Results: The analysis encompassed 17 studies with 1,840 participants aged 7 to 18 years. Findings from the network meta-analysis revealed that badminton [MD = 0.23 (0.12, 0.33), p < 0.001] and table tennis [MD = 0.16 (0.09, 0.22), p < 0.001] exercises, along with health education [MD = 0.13 (0.03, 0.23), p = 0.013], were statistically significant in enhancing vision health compared to no intervention. According to the Surface Under the Cumulative Ranking (SUCRA) probability ranking, badminton (SUCRA = 96.7) and table tennis (SUCRA = 84.1) emerged as the most effective modalities for myopia intervention in children and adolescents, with health education (SUCRA = 73.2) following closely.
Conclusion: Physical exercise significantly contributes to the healthy development of vision in children and adolescents. Among various activities, badminton and table tennis are the most effective in improving visual health, highlighting the need for augmented promotion of visual health education. However, the quantity and quality of the included studies necessitate further high-quality intervention research to confirm these findings.
1 Introduction
In recent years, the global incidence of myopia has been steadily rising, with a notable surge among children and adolescents (1, 2). Projections indicate that by 2050, nearly half of the world’s population may be affected by varying degrees of myopia, with the prevalence among Chinese youth potentially exceeding 80% (3–6). The COVID-19 pandemic has further exacerbated this trend, as children and adolescents increasingly rely on electronic devices for extended periods for online learning (7, 8). The impairment of vision and the discomfort and pain caused by the damage to visual functions can lead to various psychological issues, including anxiety, worry, depression, and melancholy (9–11). Individuals with visual dysfunction often experience anxiety and tension in their daily lives due to the difficulty in perceiving their surroundings. Myopia patients may feel frustrated because they cannot see things clearly, leading to negative emotional experiences. The accumulation of long-term psychological stress may lead to the onset of depression, causing individuals to fall into states of emotional lowness and loss of interest. This emphasizes the critical impact of vision health on the physical development of China’s youth, necessitating urgent attention to finding effective strategies to mitigate myopia in this demographic.
Physical activity is known to play a crucial role in bolstering the physical health of young people and mitigating the spread of myopia (12–14). Research indicates that higher levels of physical activity correlate with a reduced risk of myopia development and a slower progression of the condition (15), Additionally, children with myopia tend to engage less in high-intensity physical activities (16). In essence, physical activity serves as a significant deterrent against myopia (17). The study (18) reviews the relationship between physical activity in children and adolescents and myopia and points out, there is no correlation between the duration of physical activity in children and adolescents with myopia and the progression of myopia, and it suggests that high-quality intervention studies are needed to verify its conclusions. Based on this, some independent studies have indicated that engaging in outdoor physical activities can reduce the incidence of myopia among children and adolescents (19). At the same time, there are also studies suggesting that yoga exercises can effectively prevent myopia in adolescents and improve symptoms of poor vision (20, 21). With the continuous increase in the number of intervention studies, research on the impact of physical activity on the progression of myopia in children and adolescents has entered the stage of systematic review. The study (22) conducted a meta-analysis of eight independent studies on the impact of table tennis on visual health and concluded that the physical exercise program of table tennis has a good effect on improving vision. Another study (23) pointed out through a meta-analysis of 30 independent studies that net sports can play a protective and preventive role in the visual health of children and adolescents against myopia. The sports interventions included in the study are table tennis, badminton, gymnastics, soccer, basketball, middle and long-distance running, and sports games, among others. Another meta-analysis (24) concluded through subgroup analysis of 11 studies that outdoor activities, table tennis, and badminton have significant results in improving the vision of primary and secondary school students. It can be seen that the impact of physical exercise on visual health is unquestionable, but the specific methods of physical exercise intervention have not been clarified. The comparative impact of various exercise forms and identifying the most beneficial type of physical exercise for myopia in children and adolescents remains unclear (1). Therefore, exploring more scientific and efficient physical activity methods to improve visual health in this demographic is a vital and ongoing area of research.
In this study, we employed different physical activity modalities as interventions for myopia in children and adolescents, conducting a comprehensive meta-analysis. Our goal was to assess and rank the effectiveness of these various physical activity modalities in managing myopia. This analysis aims to identify the optimal physical activity modality, providing a reference for devising precise exercise programs tailored to prevent myopia in young individuals and to enhance their overall physical development.
2 Methodology of the study
2.1 Inclusion and exclusion criteria
For this study, we adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to systematically evaluate the impact of physical activity on visual health (25, 26). Our inclusion and exclusion criteria were established based on the “PICOS” framework detailed in these guidelines, covering P (study population), I (intervention), C (comparator), O (outcome indicator), and S (study design).
2.1.1 Study population (P)
This included children and adolescents aged 7 to18 years, enrolled in primary and secondary schools across China (27).
2.1.2 Interventions (I)
We considered various physical activity modalities, ranging from individual sports to comprehensive physical activity programs.
2.1.3 Comparator (C)
Comparisons were made either with no intervention or with controlled studies involving non-physical activity interventions, such as health education programs.
2.1.4 Outcome indicator (O)
The primary outcome was naked eye vision (static vision) assessed using the Standard Logarithmic Visual Acuity Scale (SLVAS). We included both bilateral naked eye vision and separate assessments of left and right-eye vision.
2.1.5 Study type (S)
Eligible studies included randomized controlled trials (RCTs) and non-randomized controlled studies focusing on physical activity interventions for visual health in children and adolescents.
2.1.6 Exclusion criteria
Studies were excluded if: ① the full text was not accessible; ② the study population did not consist of the specified age group (7 to 18 years) or included individuals with pathological eye diseases; ③ the literature was in languages other than Chinese or English.
2.2 Literature search strategy
To ensure a comprehensive literature review, three researchers independently conducted searches across multiple databases, including Web of Science, PubMed, EBSCO, Embase, MEDLINE, and CNKI. The search spanned from the inception of each database to May 1, 2023, providing a thorough exploration of existing literature.
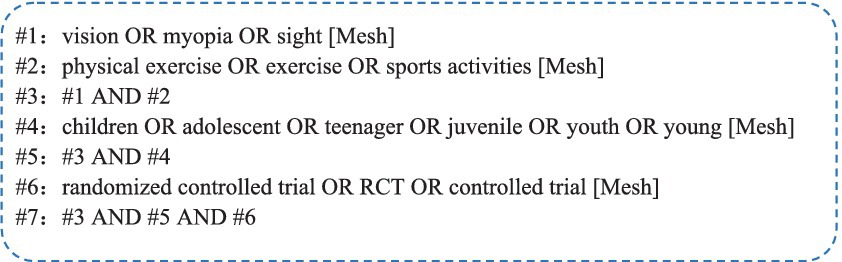
To enhance the study’s reliability and validity of our study, we implemented a meticulous primary literature search. Our search terms were extensive and included, encompassing both Chinese and English keywords. In Chinese, terms such as physical exercise, physical activities, sports, children, adolescents, vision, vision health and myopia were utilized. In English corresponding terms such as physical exercise, exercise, sports activities, children, adolescent, juvenile, vision, myopia, sight, youth, young, teenager were included. Compound search terms, as illustrated in Figure 1, were also employed.
Furthermore, we included references from the selected studies and relevant literature recommended by the databases, ensuring a comprehensive and scientifically rigorous search approach.
2.3 Literature screening and data extraction
Literature screening and data extraction were meticulously conducted by two researchers, strictly adhering to the predetermined inclusion and exclusion criteria. In cases of disagreement or inconsistency in the extracted data, discussions were facilitated with a third researcher to achieve a consensus. The extracted information included: ① Authors’ names, year of publication, and region.② Characteristics of the subject population, including age and sample size. ③ Details of interventions, such as the period, duration, and frequency; ④ A seven-point risk of bias evaluation. ⑤ Mean values, standard deviations, and standard errors of the outcome indicators for both the intervention and control groups in each study.
2.4 Literature quality assessment of included studies
The methodological quality of the included studies was appraised using the Physiotherapy Evidence Database (PEDro) scale, consisting 11 items. Items 2 to 11 being scored out of a possible 10 points. Studies scoring ≥6 were categorized as high quality, those with scores between 4 and 5 as moderate quality, and scores <4 as low quality. The quality assessment was independently conducted by two researchers, with any scoring discrepancies resolved through discussion with a third researcher.
2.5 Statistical analysis
We conducted a network meta-analysis using the “Network” package in Stata 14.2 software (28, 29), employing a frequentist approach. Visual acuity assessments, measured using a lightbox-type “E” shaped vision chart, were considered as continuous variables in the included studies. The mean difference (MD) served as the effect size, with a 95% confidence interval (CI) used for effect size evaluation. A MD’s 95% CI not including 0 was indicative of a statistically significant difference between interventions (equivalent to p < 0.05).
For inconsistency testing, nodal analysis was employed, where a p-value <0.05 suggested inconsistency between direct and indirect comparisons (30). Conversely, a p-value >0.05 indicated good consistency. Additionally, we utilized the node-splitting method for local inconsistency testing.
The study results were summarized using the Surface Under the Cumulative Ranking (SUCRA) indicator. A larger area under the curve denoted more effective interventions. SUCRA values, presented as percentages ranging from 0 to 100%, reflected the efficacy of a particular intervention, with higher percentages indicating greater efficacy (31).
3 Results
3.1 Literature screening process and results
We implemented our developed search strategy across six major international and domestic databases, resulting in the identification 2074 literature pieces relevant to our study’s theme. Additionally, two more pertinent articles were uncovered through alternative means. To streamline this extensive dataset, we utilized EndNote X9 software to remove duplicates and initiated an initial screening. Subsequently, we meticulously reviewed titles and abstracts to further assess relevance. A thorough examination of the full texts followed, allowing us to exclude any literature that did not meet our predefined inclusion and exclusion criteria. This rigorous process ultimately led to the selection of seventeen studies for our network meta-analysis. A detailed illustration of the search process and the results of the literature selection can be found in Figure 2.
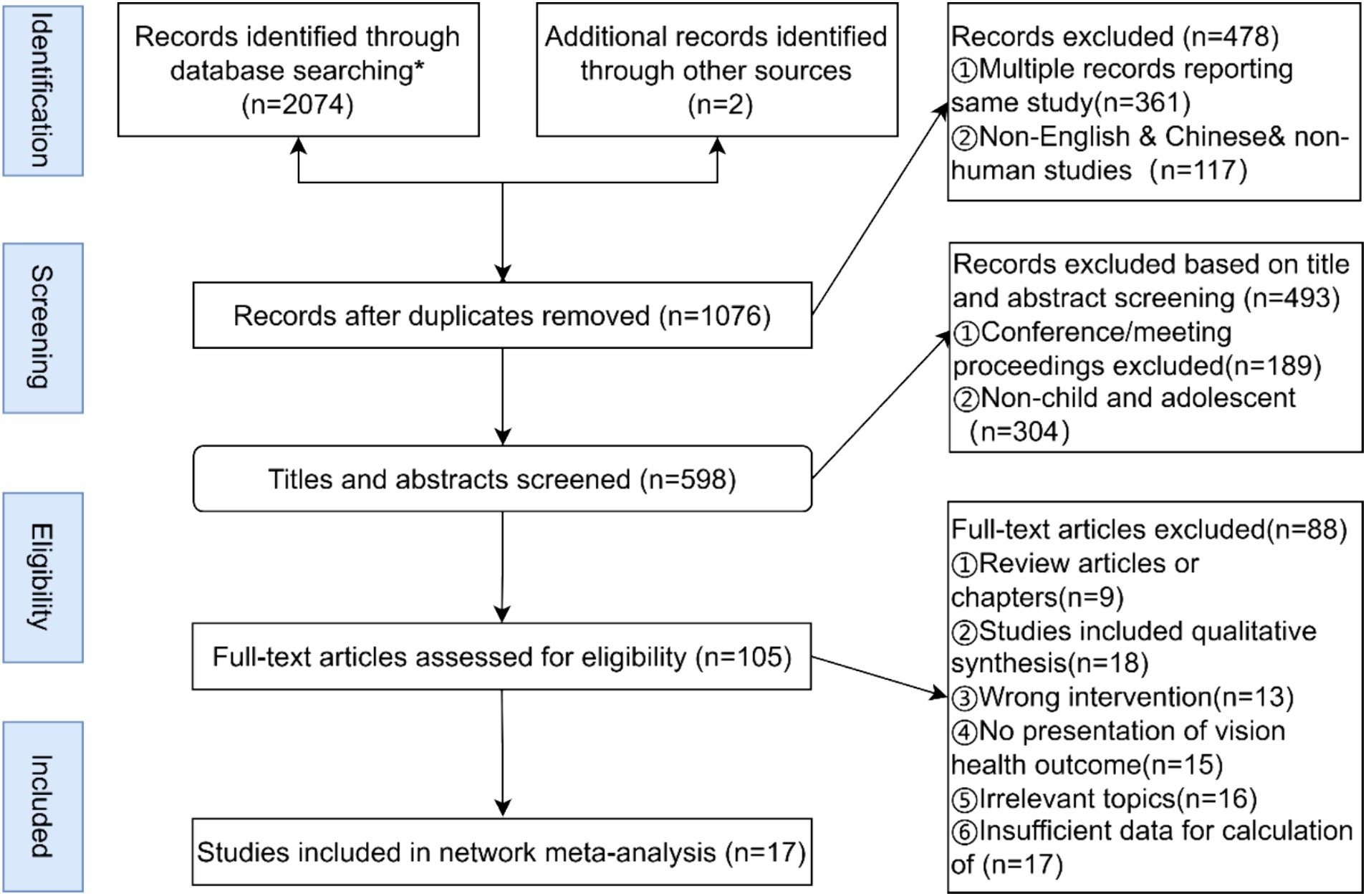
Figure 2. Literature screening process. *Results of specific searches in each database PubMed (n = 381), EBSCO (n = 327), web of science (n = 327), CNKI (n = 351), MEDLINE (n = 387), Embase (n = 301).
3.2 Basic characteristics of included studies
In this study, we selected seventeen studies for the network meta-analysis, involving a total of 1,840 participants aged between 7 to 18 years. Each study had an intervention period of at least 8 weeks. The primary outcome measure across all studies was naked eye vision (static vision). The fundamental characteristics of these studies are detailed in Table 1. Notably, three studies employed a three-arm experimental design, while the remaining utilized a two-arm approach.
The selected studies featured a diverse range of intervention modalities, including ball sports like table tennis, badminton, and basketball, track and field activities with a focus on long-distance running, and various related physical activities. These interventions encompassed physical games, sports activities, physical education classes (Gym class), dynamic visual physical activities, as well as health education and non-intervention controls.
Specifically, ‘sports games’ referred to activities that stimulate physical engagement, such as the game “tearing name tags.” ‘Gym class’, a mandatory course in China’s compulsory education system, aims to impart basic physical education and health care knowledge, develop students’ skills and athletic abilities, and contribute to their ideological and moral education. ‘Sports activities’ included various formats, either organized or informal, intended to provide relaxation and enjoyment for students. ‘Dynamic Visual Physical Activity’ involved integrating visual cognitive tasks into physical exercises, requiring participants to identify and report visual markers (such as pictures or letters) while engaged in sports like soccer, basketball, or track and field.
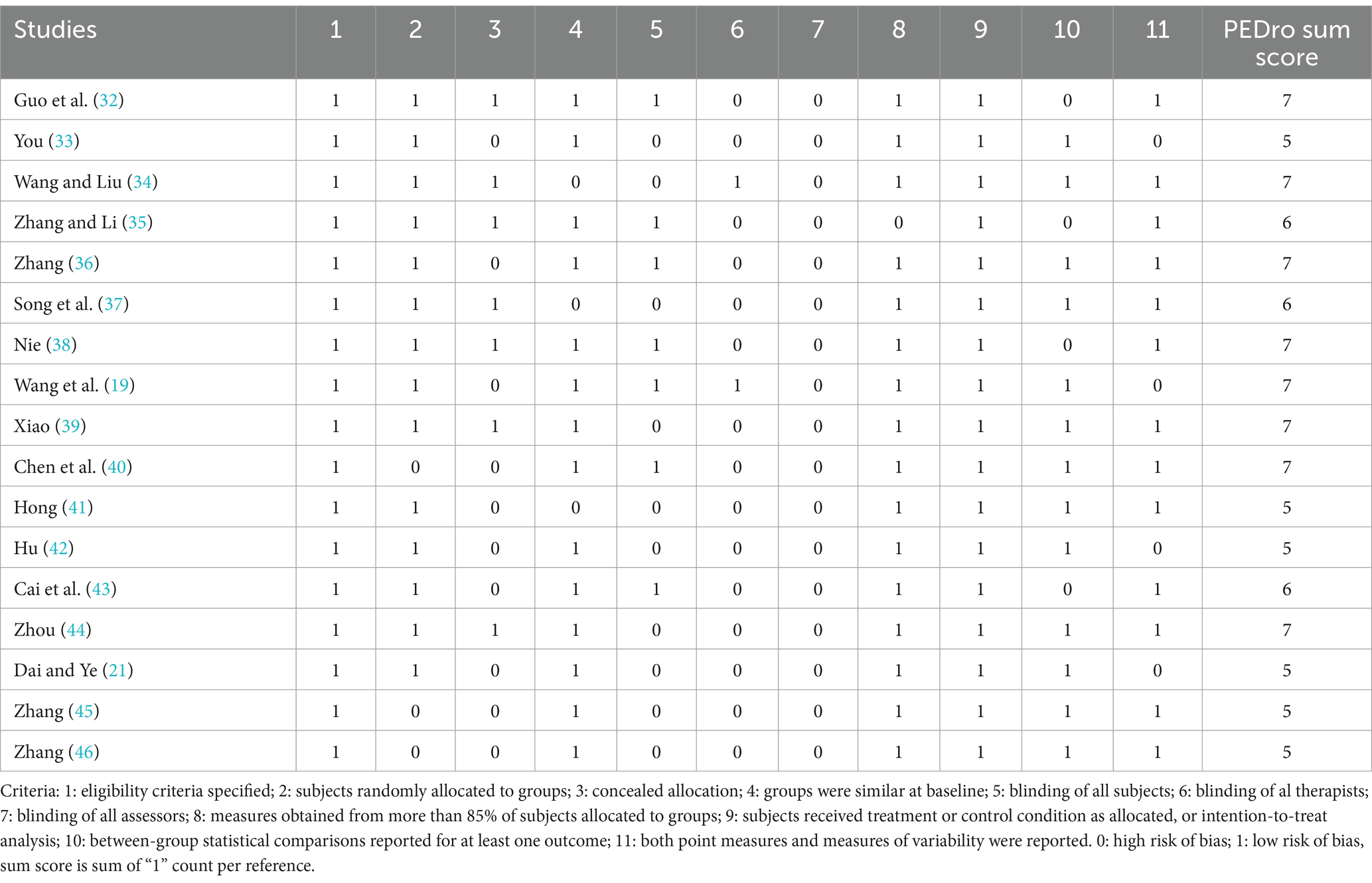
3.3 Literature quality assessment
The quality of the 17 studies included in our network meta-analysis underwent rigorously assessment. The average quality score for these papers was 6.12, indicating an overall high standard of literature quality. For detailed quality assessment results for each study, please refer to Table 2.
3.4 Network of included studies
Figure 3 illustrates the network of various physical activity modalities employed in myopia interventions for children and adolescents. In this graphical representation, the size of each node correlates with the sample size of each intervention type, where larger nodes indicate larger sample sizes. Furthermore, the thickness of the lines connecting the nodes signifies the number of studies that have compared the respective interventions. Consequently, thicker lines denote a greater number of comparative studies between two specific interventions.
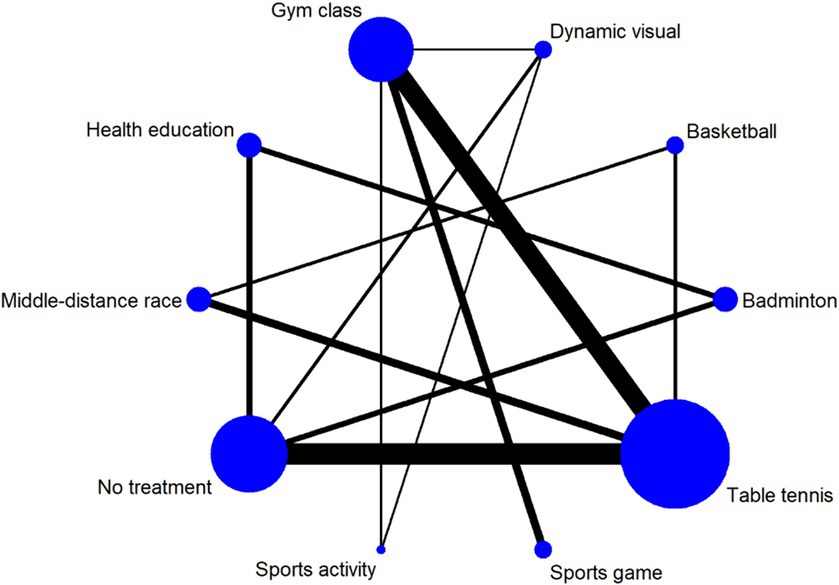
Figure 3. Meshwork of different physical activity modalities for myopia intervention in children and adolescents. Dynamic vision: dynamic vision sports activity.
3.5 Results of network meta-analysis
3.5.1 Inconsistency test
The nodal analysis model yielded a p-value of 0.83 (>0.05), indicating no significant inconsistency. This suggests that the results of both direct and indirect comparisons of the effectiveness of various interventions for myopia in children and adolescents are consistent, allowing for analysis using the consistency model.
3.5.2 Results of consistency analysis
The consistency analysis revealed that interventions such as table tennis [MD = 0.16, 95% CI (0.09, 0.22), p = 0.000], badminton [MD = 0.23, 95% CI (0.12, 0.33), p = 0.000], and health education [MD = 0.13, 95% CI (0.03, 0.23), p = 0.013] significantly outperformed no intervention, demonstrating notable effectiveness in vision health interventions for children and adolescents. Conversely, interventions like middle and long-distance running [MD = 0.06, 95% CI (−0.05, 0.18), p = 0.301], sports games [MD = 0.03, 95% CI (−0.10, 0.16), p = 0.681], basketball [MD = 0.07, 95% CI (−0.22, 0.07), p = 0.317], general physical activity [MD = 0.17, 95% CI (−0.14, 0.17), p = 0.832], and kinesthetic physical activity [MD = 0.10, 95% CI (−0.14, 0.21), p = 0.085], as well as regular physical education classes [MD = 0.001, 95% CI (−0.09, 0.09), p = 0.990], did not demonstrate significant effectiveness for vision health in children and adolescents.
3.5.3 Local inconsistency
The local inconsistency test, utilizing the node-splitting method, showed that all interventions had p-values greater than 0.05, signifying no local inconsistency. This confirms that the direct and indirect comparison results of each intervention are in alignment.
3.6 Ranking of network meta-analysis
The ranked results of the network meta-analysis interventions are displayed in Table 3. A higher SUCRA (Surface Under the Cumulative Ranking) percentage indicates greater intervention effectiveness. The rankings for different physical activities on myopia interventions in children and adolescents were as follows: badminton (SUCRA = 96.7) > table tennis (SUCRA = 84.1) > health education (SUCRA = 73.2) > kinesthetic physical activity (SUCRA = 65.2) > middle and long-distance running (SUCRA = 51.1) > sports games (SUCRA = 37.6) > general physical activities (SUCRA = 33.7) > regular physical education classes (SUCRA = 25.6) > basketball (SUCRA = 25.3) > no intervention (SUCRA = 7.5).
Comparative results for each intervention, based on SUCRA rankings, along with effect sizes and 95% confidence intervals (MD + 95% CI) for all comparisons, are presented in Table 4. A 95% CI not including 0 indicates significant comparisons.
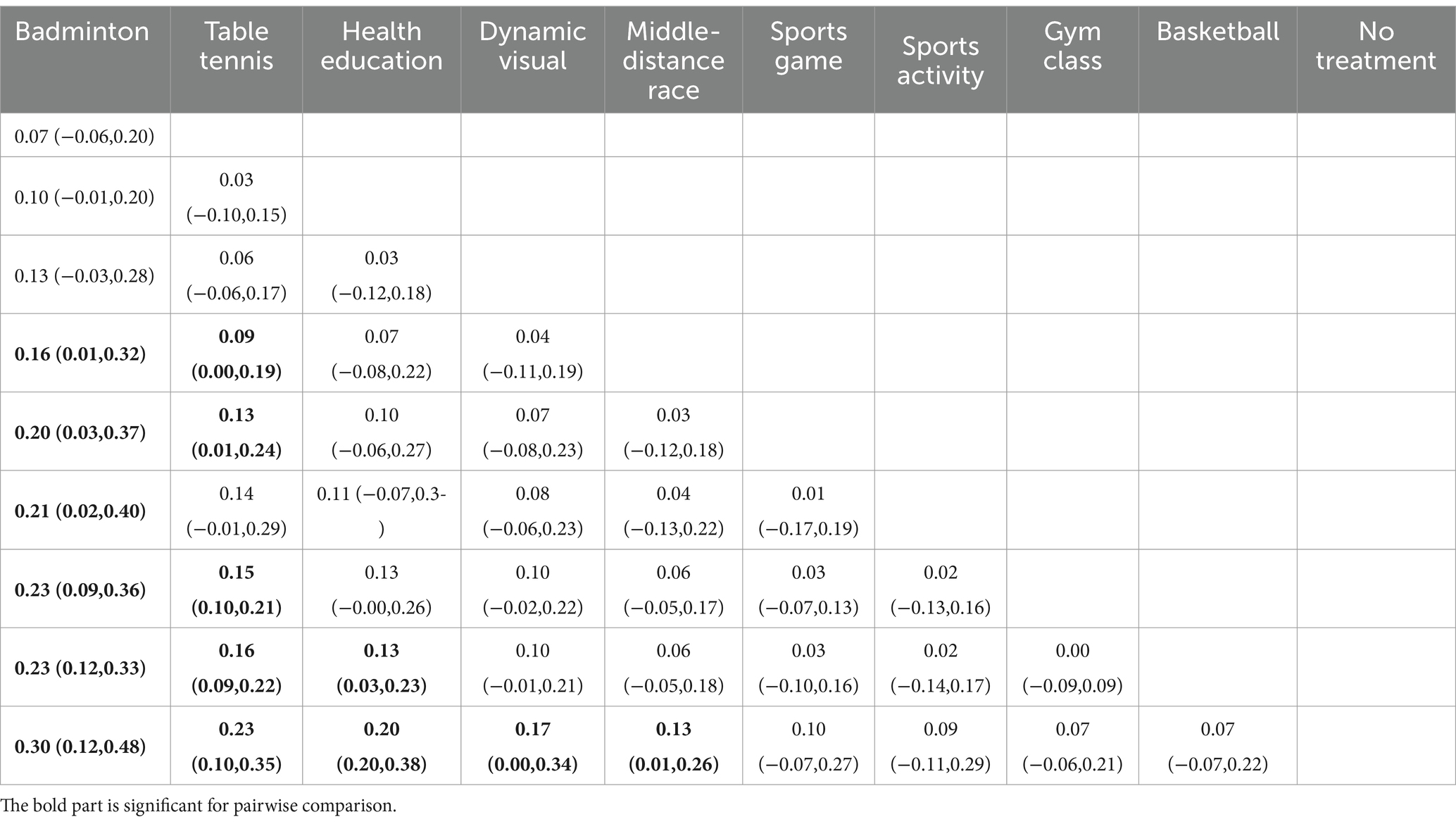
Table 4. League table reporting the comparative effects for all interventions for the vision health network (MD + 95%CI).
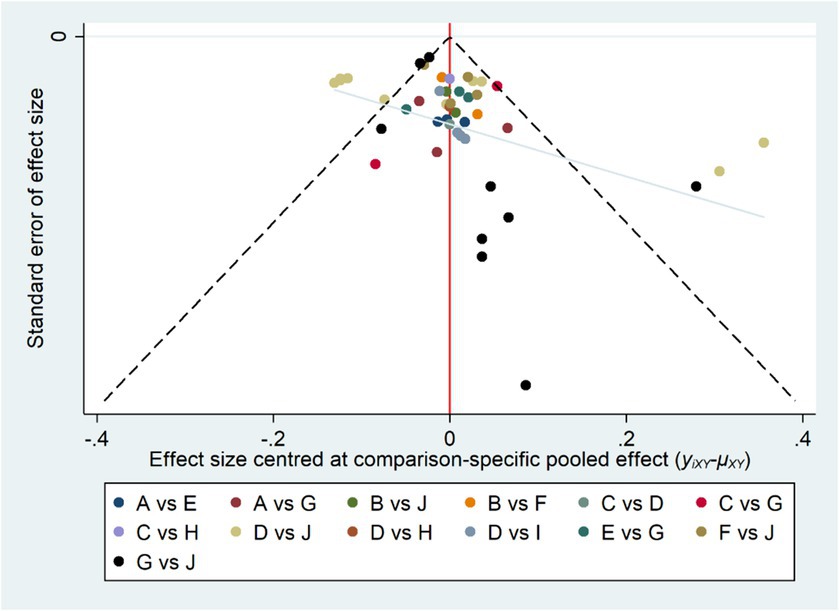
3.7 Publication bias test
To assess the presence of publication bias in the studies included in our analysis, we employed comparison-adjusted funnel plots (47). These plots utilized the effect of myopia intervention as the key effect indicator. As depicted in Figure 4, each point on the plot represents an individual study. The observed symmetry in the funnel plots suggests a lower likelihood of publication bias and small-sample effects among the included literature. This symmetry indicates a balanced and unbiased representation of study results, underscoring the reliability of our meta-analytical findings (see Figure 4).
4 Discussion
The primary aim of this study was to assess the impact of physical exercise on myopia intervention in children and adolescents through using a systematic review and network meta-analysis approach. The objective was to identify the most effective physical exercises for managing myopia in this demographic. The findings underscore the significant role of physical exercise in myopia intervention for children and adolescents, aligning with related studies (18). The most beneficial forms of physical activity identified for myopia intervention were badminton (95.3%) and table tennis (81.4%), with health education (74.8%) also deemed critical.
4.1 Effectiveness of physical exercise in vision health interventions
Myopia occurs when the axial length of the eye surpasses the focal length of the cornea and lens, leading to refractive error (48). Prolonged near vision and sustained focus are primary contributors to vision impairment (49). Continuous near vision induces strain on the ciliary muscles, potentially leading to spasms and pseudomyopia. If left unaddressed, this can accelerate the onset of myopia (49). Extended periods of near vision in children and adolescents can cause sustained contraction and eyestrain, hindering the ability of ciliary muscles to relax (50). Maintaining normal ciliary muscle function and alleviating eyestrain are effective strategies for preventing and controlling myopia.
Physical exercise serves as an active rest mechanism after prolonged near vision activities, alleviating eyestrain, relaxing the ciliary muscles, preventing pseudomyopia, and improving blood circulation around the eyes (51). Various physical exercise modalities, such as basketball (42), middle-distance running (39), and yoga (20), have proven effective in intervening in myopia development in children and adolescents.
The “light-dopamine” hypothesis supports the effectiveness of outdoor physical activities in mitigating myopia. The intensity of light significantly impacts visual acuity. Animal studies show that that visual deprivation leads to reduced retinal dopamine content (52–54). Bright light stimulates retinal dopamine synthesis and release, inhibiting eye axis growth (55, 56), thereby contributing to myopia prevention. This finding supports studies highlighting the effectiveness of outdoor physical exercises, such as comprehensive outdoor activities (19) and sports games (20), in preventing myopia in children and adolescents.
4.2 Effectiveness of badminton and table tennis exercises in vision health interventions for children and adolescents
The network meta-analysis, comparing nine different interventions directly and indirectly, revealed that badminton (95.3%) and table tennis (81.4%) exercises possess a significant advantage in myopia intervention for children and adolescents. Myopia development is intricately linked to ciliary muscle function, and dysregulation of these muscles can cause blurred retinal imaging, subsequently leading to myopia (57). Badminton and table tennis exercises not only mitigate eye fatigue and prevent the onset of pseudomyopia but also enhance ciliary muscle regulation more effectively than other sports exercises. These activities require rapid shifts between far and near vision, training the ciliary muscles to contract and relax swiftly, thereby enhancing their sensitivity and precision.
Existing research on improving myopia through ball sports is also mainly focused on small ball games such as table tennis and badminton, and there are relevant explanations in the mechanism research of improving visual health. In these types of sports, the ball moves quickly and changes direction frequently, requiring participants to closely watch the trajectory of the ball to make correct judgments. This provides excellent exercise for the adjustment of the eye’s refractive power and the contraction of the ciliary muscles. Compared to large ball sports, badminton and table tennis have relatively smaller ranges and amplitudes of physical activity, but the frequency of stimulation the eyes receive per unit of time is relatively higher. Large ball sports involve a larger range of physical activity, and large balls (such as basketballs and soccer balls) take relatively longer to roll with each movement, resulting in a relatively lower frequency of stimulation to the eyes per unit of time. This is also why relevant studies have shown that large ball sports (such as basketball, etc.) (42) have a certain effect on improving myopia, but compared to small ball sports, the effect is not significant. During badminton and table tennis play, the varying speeds and directions of the ball necessitate vigilant tracking and accurate judgment by the eyes. This dynamic environment fosters the training of alternating distant and near vision. When following the fast-moving ball, the ciliary muscles contract, relaxing the lens suspensory ligament, allowing the lens to increase its curvature and refractive index due to its elasticity. Conversely, when returning the ball, the process reverses. The long-range shots also aid in relaxing the ciliary muscle, alleviating any spasms. Thus, these sports exercises not only bolster blood circulation and metabolism in the eyes, alleviating fatigue, but also provide comprehensive training of the ciliary muscle, enhancing its regulatory ability.
Furthermore, badminton and table tennis exercises are advantageous over other sports due to their minimal requirements for venues, personnel, and technical skill levels. They enable children and adolescents to engage more readily and deeply in the exercise experience, thereby effectively improving ciliary muscle regulation.
4.3 Research limitations and prospects
The review found that there are some shortcomings in the existing studies on the intervention of physical exercise in the visual health of children and adolescents: (1) Most research consists of cohort and cross-sectional studies, with fewer dedicated intervention studies, leading to varied findings. Future research should address potential differences in confounding variables for a more accurate exercise prescription. (2) Studies have often conflated the effects of “physical exercise” with “outdoor activities.” Future studies should distinguish the specific influences of “outdoor factors” and “physical activity” in myopia management. Additionally, most research have focused on naked-eye visual acuity as the primary outcome measure, there is a paucity of research on dynamic visual acuity and related physiological indexes is needed. (3) The quality of independent intervention studies needs enhancement. Applying “blinding” techniques, implementing high-quality intervention studies, and controlling extraneous variables are crucial for scientifically robust evidence.
This review also has some limitations and deficiencies: (1) This study primarily focuses on the effects of physical exercise on visual health within the intervention period, but in reality, long-term follow-up data on participants would provide more compelling evidence for the sustained impact of physical activity on the visual health development of children and adolescents. (2) The included physical exercises encompass specific sports, outdoor activities, and physical training, and different types of physical exercises as well as the intensity of physical activity may all lead to content bias. (3) The number of studies on sports interventions for the progression of myopia in children and adolescents is relatively small, and there is an imbalance in the number of studies on different sports activities, which means that the conclusions drawn from the network meta-analysis require further validation by more high-quality research. (4) The data obtained all come from published literature, and some studies lack extractable data, which limits the number of studies included in the network meta-analysis. These deficiencies all need to be further explored and addressed in future research.
From the study results, it’s evident that, alongside physical activity, health education is pivotal intervention for the visual health of children and adolescents. Combining health education with physical activity interventions holds promise for future research in myopia interventions. The presence of publication bias and small sample effects may influence outcomes, requiring further high-quality intervention studies for validation.
5 Conclusion
The study’s findings highlight the effectiveness of physical activity as an intervention for enhancing the visual health of children and adolescents. Among various physical activities, badminton and table tennis stand out as the most beneficial modalities for achieving this purpose. Additionally, the study emphasizes the importance of enhancing education and awareness regarding visual health. Such efforts are crucial for raising awareness among children and adolescents about the importance of safeguarding their visual well-being.
However, the quality of the literature reviewed in this research underscores the need for additional high-quality intervention studies to validate and strengthen these conclusions. Future research endeavors should aim to provide more substantial and reliable evidence, further confirming the efficacy of physical activities in addressing visual health issues among children and adolescents.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
WL: Investigation, Conceptualization, Data curation, Methodology, Software, Writing – original draft. JL: Investigation, Writing – original draft, Writing – review & editing. DZ: Conceptualization, Investigation, Data curation, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was Supported by the Fundamental Research Funds for the Central Universities (CCNU24ZZ117).
Acknowledgments
We thank Professor Bin Wang (Central China Normal University) for stimulating discussions and Professor Jun Sun (Central China Normal University) for providing project support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhu, Z, Chen, Y, Tan, Z, Xiong, R, McGuinness, MB, and Müller, A. Interventions recommended for myopia prevention and control among children and adolescents in China: a systematic review. Br J Ophthalmol. (2023) 107:160–6. doi: 10.1136/bjophthalmol-2021-319306
2. Qi, ZY, Chen, J, and He, XG. Epidemiology of high myopia among children and adolescents in China. Zhonghua Yan Ke Za Zhi [Chin J Ophthalmol]. (2023) 59:138–45. doi: 10.3760/cma.j.cn112142-20220313-00105
3. Dong, L, Kang, YK, Li, Y, Wei, WB, and Jonas, JB. Prevalence and time trends of myopia in children and adolescents in china a systemic review and meta-analysis. Retina J Retinal Vitr Dis. (2020) 40:399–411. doi: 10.1097/iae.0000000000002590
4. Bruce, A. Re: Holden et al.: global prevalence of myopia and high myopia and temporal trends from 2000 through 2050 (ophthalmology 2016;123:1036-1042). Ophthalmology. (2017) 124:E24–e25. doi: 10.1016/j.ophtha.2016.06.066
5. Leo, S-W, and Young, TL. An evidence-based update on myopia and interventions to retard its progression. J AAPOS. (2011) 15:181–9. doi: 10.1016/j.jaapos.2010.09.020
6. Bourne, RRA, Stevens, GA, White, RA, Smith, JL, Flaxman, SR, Price, H, et al. Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Health. (2013) 1:e339–49. doi: 10.1016/S2214-109X(13)70113-X
7. Ku, P-W, Steptoe, A, Lai, Y-J, Hu, H-Y, Chu, D, Yen, Y-F, et al. The associations between near visual activity and incident myopia in children a Nationwide 4-year follow-up study. Ophthalmology. (2019) 126:214–20. doi: 10.1016/j.ophtha.2018.05.010
8. Zhou, X, Liu, T, Wu, A, Cheng, B, Chen, M, and Wang, K. Prevalence of myopia among senior students in Fenghua, eastern China, before and during the COVID-19 pandemic. Front Public Health. (2023) 11:1180800. doi: 10.3389/fpubh.2023.1180800
9. Fleckenstein, M, Schmitz-Valckenberg, S, and Chakravarthy, U. Age-related macular degeneration: a review. JAMA. (2024) 331:147–57. doi: 10.1001/jama.2023.26074
10. Buffenn, AN. The impact of strabismus on psychosocial heath and quality of life: a systematic review. Surv Ophthalmol. (2021) 66:1051–64. doi: 10.1016/j.survophthal.2021.03.005, Epub 2021 Mar 25
11. Mylona, I, Deres, ES, Dere, GS, Tsinopoulos, I, and Glynatsis, M. The impact of internet and Videogaming addiction on adolescent vision: a review of the literature. Front Public Health. (2020) 8:63. doi: 10.3389/fpubh.2020.00063
12. Zhao, X, and Zhang, Y. Degree of myopia and reduced physical activity in 3600 college students in China. Med Sci Monit Basic Res. (2022) 28:2325–6. doi: 10.12659/MSMBR.934807
13. Hansen, MH, Laigaard, PP, Olsen, EM, Skovgaard, AM, Larsen, M, Kessel, L, et al. Low physical activity and higher use of screen devices are associated with myopia at the age of 16-17 years in the CCC2000 eye study. Acta Ophthalmol. (2020) 98:315–21. doi: 10.1111/aos.14242
14. Theophanous, C, Modjtahedi, BS, Batech, M, Marlin, DS, Luong, TQ, and Fong, DS. Myopia prevalence and risk factors in children. Clin Ophthalmol. (2018) 12:1581–7. doi: 10.2147/OPTH.S164641
15. Jacobsen, N, Jensen, H, and Goldschmidt, E. Does the level of physical activity in university students influence development and progression of myopia?--a 2-year prospective cohort study. Invest Ophthalmol Vis Sci. (2008) 49:1322–7. doi: 10.1167/iovs.07-1144
16. Deere, K, Williams, C, Leary, S, Mattocks, C, Ness, A, Blair, SN, et al. Myopia and later physical activity in adolescence: a prospective study. Br J Sports Med. (2009) 43:542–4. doi: 10.1136/bjsm.2008.049288
17. Saw, SM, Nieto, FJ, Katz, J, Schein, OD, Levy, B, and Chew, SJ. Factors related to the progression of myopia in Singaporean children. Optomet Vision Sci. (2000) 77:549–54. doi: 10.1097/00006324-200010000-00009
18. Wang, BN, Wang, LJ, Chen, RZ, and Zhou, YL. The relationship between physical activity and myopia in children and adolescents: a systematic review and Meta-analysis. China Sport Sci. (2022) 58:62–72. doi: 10.16470/j.csst.2019160
19. Wang, SJ, Li, YF, Li, AH, and Wei, GX. Tracking intervention study on the impact of outdoor physical activities on primary school students' visual health. J Capital Univ Phys Educ Sports. (2021) 33:679–85. doi: 10.14036/j.cnki.cn11-4513.2021.06.013
20. Jadhav, RLN. Effect of yogic exercise on myopia of high school girls. Int Proc Econ Dev Res. (2013) 64:55–8. doi: 10.7763/ipedr
21. Dai, YY, and Ye, HH. Evaluation of the effect of badminton on poor vision intervention in children. J Xi'an Univ Arts Sci. (2020) 23:120–3.
22. Li, ZC, Li, SS, and Chen, ZC. Effects of physical exercises on the vision of students in China: a meta-analysis (2020) 20:551–5.
23. Yu, MM, Li, NC, Shi, G, and Ni, YN. Meta-analysis of effects of physical activity on visual acuity. Hubei sports science. (2021) 40:901–7.
24. Dong, YQ, He, Q, and Xiong, QQ. A Meta-analysis of the effect of exercise on vision. Fujian sports science and technology. (2022) 41:46–50.
25. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DGGroup P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
26. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. (2021) 18:e1003583. doi: 10.1371/journal.pmed.1003583
27. Zhang, X, Zhou, Y, Wang, Y, Du, W, and Yang, J. Trend of myopia through different interventions from 2010 to 2050: findings from eastern Chinese student surveillance study. Front Med. (2023) 9:9. doi: 10.3389/fmed.2022.1069649
28. Liu, Y, Wang, W, Zhang, A, Bai, X, and Zhang, S. Epley and Semont maneuvers for posterior canal benign paroxysmal positional vertigo: a network meta-analysis(article). Laryngoscope. (2016) 126:951–5. doi: 10.1002/lary.25688
29. Mutz, J, Vipulananthan, V, Carter, B, Hurlemann, R, Fu, CHY, and Young, AH. Comparative efficacy and acceptability of non-surgical brain stimulation for the acute treatment of major depressive episodes in adults: systematic review and network meta-analysis. BMJ. (2019) 364:l1079. doi: 10.1136/bmj.l1079
30. DoneganSarah, WP, D'Alessandro, U, and Tudur, SC. Assessing key assumptions of network meta-analysis: a review of methods. Res Synth Methods. (2013) 4:291–323. doi: 10.1002/jrsm.1085, Epub 2013 Aug 1
31. Ga, S, Aeb, A, and Jpaa, I. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
32. Guo, XP, Ge, SS, Liu, RH, and Hou, XL. Experimental study on the impact of table tennis on agility and vision in middle school students. Anhui Sports Sci. (2012) 33:87–9.
33. You, L. Experimental study on improving students' vision through table tennis. Sports Space. (2013) [Page numbers not provided]
34. Wang, WQ, and Liu, YL. Study on the effect of table tennis intervention on improving adolescents' physical fitness. J Zhangzhou Voc Techn Coll. (2013) 15:87–91. doi: 10.13908/j.cnki.issn1673-1417.2013.01.022
35. Zhang, JS, and Li, LX. The impact of table tennis on vision in children with pseudomyopia. J Tonghua Teach Coll. (2010) 31:54–5. doi: 10.13877/j.cnki.cn22-1284.2010.08.029
36. Zhang, ZY. Experimental study on the effect of table tennis practice on improving vision in myopic children. Shanxi Normal University (2014).
37. Song, SX, Wang, FY, and Li, YH. Comparative study on the impact of table tennis on vision in children and adolescents. China Sport Sci Technol. (2002) 11:19–20. doi: 10.16470/j.csst.2002.11.006
38. Nie, PF. Study on the impact of modified physical games on vision in middle school students. Soochow University (2020).
39. Xiao, BJ. Comparative study on the effect of table tennis and middle-long distance running on improving pseudomyopia in 7-8-year-old primary school students. Sci Technol Inform. (2012) 14:322–3.
40. Chen, YL, Linlin, LIU, and Nanjie, DING. Application and practice study of table tennis sports prescription in improving primary school students' vision. Sports World (Academic Edition). (2018) 11:194–5. doi: 10.16730/j.cnki.61-1019/g8.2018.11.133
41. Hong, YX. Practical analysis of table tennis in improving primary school students' vision. Questions Stud. (2019) 21:60.
42. Hu, CX. Comparative analysis of the impact of table tennis, basketball, and middle-long distance running on vision in children and adolescents. Contemp Sports Technol. (2015) 5:210–1. doi: 10.16655/j.cnki.2095-2813.2015.01.131
43. Cai, QF, Chen, J, Pan, JL, and Tan, Q. Experimental study on the maintenance of primary school students' vision through physical activities. Sports Sci. (2019) 40:32–4. doi: 10.14038/j.cnki.tykj.2019.06.012
44. Zhou, Q. Pedagogical study on the development of dynamic vision in primary second-year students through modern gaming devices in physical activities. Soochow University (2020).
45. Zhang, WS. Observation of the therapeutic effect of badminton and eye health education intervention on pseudomyopia in middle school students. Shanxi Normal University (2020).
46. Zhang, YZ. Study on the impact of physical activities with dynamic vision tasks on the vision of 7-8-year-old children. Soochow University (2020).
47. Chaimani, A, Higgins, JPT, Mavridis, D, Spyridonos, P, and Salanti, G. Graphical tools for network Meta-analysis in STATA. PLoS One. (2013) 8:e76654. doi: 10.1371/journal.pone.0076654
48. Baird, PN, Saw, SM, Lanca, C, Guggenheim, JA, Smith Iii, EL, Zhou, X, et al. Myopia. Nat Rev Dis Prim. (2020) 6:99. doi: 10.1038/s41572-020-00231-4
49. Hargrave, BK. Accommodation: the role of the external muscles of the eye: a consideration of refractive errors in relation to extraocular malfunction. Med Hypotheses. (2014) 83:607–13. doi: 10.1016/j.mehy.2014.08.006
50. Morgan, IG, Wu, PC, Ostrin, LA, Tideman, JWL, Yam, JC, Lan, W, et al. IMI risk factors for myopia. Invest Ophthalmol Vis Sci. (2021) 62:3. doi: 10.1167/iovs.62.5.3
51. Torii, H, Kurihara, T, Seko, Y, Negishi, K, Ohnuma, K, Inaba, T, et al. Violet light exposure can be a preventive strategy against myopia progression. EBioMedicine. (2017) 15:210–9. doi: 10.1016/j.ebiom.2016.12.007
52. Dong, F, Zhi, Z, Pan, M, Xie, R, Qin, X, Lu, R, et al. Inhibition of experimental myopia by a dopamine agonist: different effectiveness between form deprivation and hyperopic defocus in guinea pigs. Mol Vis. (2011) 17:2824–34.
53. McBrien, NA, Cottriall, CL, and Annies, R. Retinal acetylcholine content in normal and myopic eyes: a role in ocular growth control? Vis Neurosci. (2001) 18:571–80. doi: 10.1017/s0952523801184075
54. Papastergiou, GI, Schmid, GF, Laties, AM, Pendrak, K, Lin, T, and Stone, RA. Induction of axial eye elongation and myopic refractive shift in one-year-old chickens. Vis Res. (1998) 38:1883–8. doi: 10.1016/s0042-6989(97)00347-7
55. Feldkaemper, M, and Schaeffel, F. An updated view on the role of dopamine in myopia. Exp Eye Res. (2013) 114:106–19. doi: 10.1016/j.exer.2013.02.007
56. Nebbioso, M, Plateroti, AM, Pucci, B, and Pescosolido, N. Role of the dopaminergic system in the development of myopia in children and adolescents. J Child Neurol. (2014) 29:1739–46. doi: 10.1177/0883073814538666
Keywords: children, adolescents, vision health, myopia, physical activity, network meta-analysis
Citation: Liu J, Lan W and Zhang D (2024) Network meta-analysis of the efficacy of physical exercise interventions on vision health in children and adolescents. Front. Public Health. 12:1393909. doi: 10.3389/fpubh.2024.1393909
Edited by:
Vivek Podder, Baptist Hospital of Miami, United StatesReviewed by:
Mohammad Sarif Mohiuddin, New York University, United StatesXuejing Bi, Harbin Medical University, China
Copyright © 2024 Liu, Lan and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wencen Lan, bGFud2VuY2VuQDE2My5jb20=
 Jianming Liu
Jianming Liu Wencen Lan
Wencen Lan Danxuan Zhang1
Danxuan Zhang1