- Department of Statistics, Samara University, Semera, Ethiopia
Introduction: Breast milk is the ideal food for the infant and is associated with various public health benefits for both the infant and the mother. The recommended time for early initiation of breastfeeding is within one hour after birth. The prevalence of early initiation of breastfeeding was lower than the plan of the Ethiopian Ministry of Health Sector Development program. Thus, the main objective of this study was to identify individual and group-level factors associated with the early initiation of breastfeeding in Ethiopia.
Methods: Secondary data on children was obtained from the 2019 Ethiopia mini-demographic and health survey. The survey was a population-based cross-sectional study and was downloaded from the Measure Demographic and Health Survey website (http://www.measuredhs.com). The study included a random sample of 2,125 last-born infants who were born within 24 months before the survey. A multilevel binary logistic regression analysis was employed to identify the factors associated with the early initiation of breastfeeding in Ethiopia. Statistical data was analyzed using the Statistical Analysis System (SAS 9.4).
Results: The prevalence of early breastfeeding initiation was 72%. The higher preceding birth interval (AOR = 1.18, 95% CI: 1.1076, 1.5451), the higher gestational age of infants (AOR = 1.38, 95% CI: 1.2796, 1.4782), the higher number of antenatal care visits (AOR = 1.26, 95% CI: 1.2340, 1.2934), delivery at a health facility (AOR = 1.60, 95% CI: 1.4585, 1.7515), vaginal delivery (AOR = 1.11, 95% CI: 1.1019, 1.1123), mothers with primary education (AOR = 1.14, 95% CI: 1.0204, 1.2738), mothers with secondary education (AOR = 1.54, 95% CI: 1.4678, 1.6190), and mothers with higher education (AOR = 2.62, 95% CI: 2.2574, 3.0526) were associated with higher odds of early initiation of breastfeeding. Being a rural dweller (AOR = 0.63, 95% CI: 0.5684, 0.7038) and the age of mothers (AOR = 0.44, 95% CI: 0.3921, 0.4894) were associated with lower odds of early initiation of breastfeeding.
Conclusion: Since the prevalence of early initiation of breastfeeding was minimal among rural mothers who delivered their child by caesarean section, this study strongly suggests special supportive care for these mothers.
Introduction
Breast milk is the ideal food for the infant and is associated with lower neonatal mortality, prevents morbidities such as diarrhea, pneumonia, and neonatal sepsis, and may reduce obesity and diabetes later in life (1, 2). Recent World Health Organization (WHO) evaluations on the short- and long-term benefits of breastfeeding came to the conclusion that there is solid evidence for various public health benefits for the infant, the mother, the household, and the community as a whole (3). The benefits for the infant include improve cognitive development, a decreased rate of necrotizing enterocolitis, common childhood infections, and a decreased risk of sudden death. Breastfeeding helps the mother return to her pre-pregnancy weight, improves birth spacing, and decreases the rate of chronic illness and breast cancer (3, 4). Moreover, optimally breastfed children contribute to improved human capital through a reduction in expenses on infant formula and increased opportunities for a more sustainable future (5).
The World Health Organization’s (WHO) recommendation for starting breastfeeding is within one hour after birth (6). Moreover, the World Health Organization and the United Nations Children’s Fund (UNICEF) recommends exclusive breastfeeding (EBF) for the first 6 months of life and continued breastfeeding until the child is 2 years of age (7). Early initiation of breastfeeding can reduce neonatal mortality by 33% (8). Different studies indicate that the late initiation of breastfeeding leads to high neonatal morbidity and mortality. According to a systematic review study, infants who initiated breastfeeding after one hour were 33% at risk of neonatal mortality (9). Moreover, studies in different parts of the world revealed that delayed breastfeeding increases the risk of mental and physical problems at different stages of life (8). Neonatal morbidity and mortality in infants who did not feed breast milk within one hour are increased by threefold when compared to infants who fed breast milk within one hour of birth (10–12).
Even though the evidence on breastfeeding suggests the existence of variation around the world, it is clear that the prevalence of early initiation of breastfeeding was higher in high-income countries than low- and middle-income countries (13). More recently, the United Nations renewed its commitment to improving child nutrition (including breastfeeding outcomes) worldwide through the United Nations Decade of Action on Nutrition (2016–2025) and the Sustainable Development Goals (SDG-2.2) of ending all forms of malnutrition (14, 15). Moreover, the Sustainable Development Goals (SDG) target reducing neonatal deaths to 12 per 1,000 live births and under-five deaths to less than 25 per 1,000 live births through eliminating preventable child deaths by the year 2030 (16).
In low- and middle-income countries, where access to clean water, adequate sanitation, and basic health and social services is often limited, the lower prevalence of early initiation of breastfeeding may increase various health problems (5, 7, 17). For example, a recent study from Nigeria indicated that an estimated 23% of diarrhea deaths among children under five were attributable to late breastfeeding in 2016 (18).
In Ethiopia, many subnational reports indicated that the prevalence of early initiation of breastfeeding was about 66.5%, which is below the Ethiopian Health Sector Transformation Plan (HSTP) target of 90% (19). The government of Ethiopia created the National Nutrition Program (NNP) I (2008–2015) and the NNP II (2016–2020) with a strong focus on multi-sectoral coordination of nutrition activities to expedite reductions in malnutrition (20). The importance of early initiation of breastfeeding was recognized together with other nutrition programs through national reforms and strategies on infant and young child feeding practices, especially after the launch of the health promotion program in 2003 (21). Accordingly, the prevalence increased from 52% in 2011 to 74.3% in 2016, but still fell below the plan of the Ethiopian Ministry of Health Sector Development Program, which targeted the 92% prevalence of early initiation of breastfeeding (22). A systematic review of mostly subnational studies reported that a mother’s occupation, education level, receiving guidance and counseling from health care workers, place of delivery, and mode of delivery were common factors associated with the early initiation of breastfeeding in Ethiopia (16). According to various studies, the WHO and the concerned United Nations organizations (UN) report that the factors associated with breastfeeding practice differ with socioeconomic, demographic, behavioral, and cultural factors of mothers, place and mode of delivery, professional counseling on breastfeeding, and obstetric and health service-related factors (23–25). Identifying factors associated with breastfeeding practices is essential to increasing the prevalence of early breastfeeding. Despite the fact that a number of single-level and descriptive studies have been done to analyze the trend, factors, and prevalence of early initiation time, exclusive breastfeeding, and duration of breastfeeding in Ethiopia, the prevalence is below the plan of the Ethiopian health sector, and more work is needed. Thus, in view of the above literature, this study targeted identifying individual and group-level factors associated with early initiation of breastfeeding using the data from the 2019 Ethiopia Mini Demographic and Health Survey (EMDHS).
Materials and methods
Data source and study design
This paper uses secondary data from the children’s data set of the 2019 Ethiopia Mini Demographic and Health Survey (EMDHS). The survey was population-based cross-sectional, and the data was downloaded from the Measure DHS Website1 after reasonable request, and data use permission was obtained from the institutional review board of the International Classification of Functioning (ICF). The survey conducted from March 21 to June 28, 2019, was the second EMDHS and the fifth DHS implemented in Ethiopia. The Ethiopian Public Health Institute (EPHI) carried out this survey in partnership with the Central Statistical Agency (CSA) and the Federal Ministry of Health (FMoH), with technical assistance from the ICF and financial and technical support from development partners.
Sampling design
The sampling frame for the 2019 Ethiopia mini demographic and health survey was a complete list of the 149,093 enumeration areas (EAs), which was performed by the Central Statistical Agency (CSA). The average coverage for an enumeration area was 131 households. For the 2019 EMDHS, a two-stage stratified sampling design was used. Currently, Ethiopia is structured administratively into twelve nation-states and two city administrations. However, during the 2019 EMDHS exclusion, there were nine nation-states and two city administrations, which were then stratified into urban and rural areas except for Addis Ababa, which is entirely urban, to establish 21 sampling strata. To ensure the precision of sample selection, the allocation was done through an equal allocation where 25 EAs were selected from eight regions and each of the three main regions was assigned 35 EAs: Amhara, Oromia, and the Southern Nations, Nationalities, and Peoples’ Region (SNNPR). Among the 305 EAs selected in the primary stage, 93 were urban and 212 were rural, and in the second stage of selection, an equal probability systematic selection was used to select a fixed number of 30 families per cluster from the newly established household list. The survey interviewed 5,753 women of reproductive age (15–49) from a nationally representative sample of 8,663 households. In accordance with the denominator of early initiation of breastfeeding, the sample for this study was made up of last-born infants who were born within 24 months before the survey, which resulted in a total weighted sample of 2,125 infants.
Variables in the study
In this study, we have considered two types of variables, namely, response and explanatory variables.
Response variable
The response variable in this study was early initiation of breastfeeding using the recommended definition of children born within 24 months before the survey who were put to the breast within one hour after birth (25). The response variable was dichotomized as early breastfeeding when the mother starts breastfeeding within one hour after birth and delayed breastfeeding when it exceeds one hour.
Explanatory variables
The selection of explanatory variables was theoretically driven and supported by prior research with regard to factors influencing the early initiation of breastfeeding in Ethiopia. Therefore, the explanatory variables used in this study were the sex and gestational age of infants, which were potential infant-level predictors of early initiation of breastfeeding. Mother’s education level, age of mother, numbers of children ever born, preceding birth interval, mode of delivery, number of antenatal care visits, place of delivery, and wealth index were potential mother-level predictors of early initiation of breastfeeding, while residence was an enumeration-level predictor. The data was managed with SPSS 26 and analyzed using SAS 9.4. The data was weighted to take into account or adjust for disproportionate sampling and non-sampling responses and to increase the representativeness of the sample. Variable selection was made by the purposeful method, while a univariable analysis was made between a response variable and each predictor separately at a 25% level, then a multivariable analysis was performed at a 5% level between a response variable and all significant variables in the univariable analysis. The model selection was performed using deviance and log likelihood statistics due to the presence of nested models.
The generalized linear model
The selection of any statistical analysis depends on the nature of the response and the explanatory variables. The standard linear regression analysis assumes a continuous response variable with a normally distributed random error term, but there are conditions where this assumption is clearly violated. For instance, when the response variable has a nominal and ordinal scale, there is no way to think about the normal distribution (26). Thus, the methods called generalized linear models were introduced by Nelder and Wedderburn in 1972 and revised in 1989 by McCullagh and Nelder to generalize linear models by the general mean structures and more general distributions (27).
The multilevel binary logistic regression model
The binary logistic regression model is a generalized linear model where the outcome variables are measured on a binary scale. In most cases, those two categories of the response variable are noted as success and failure. If we define the binary response variable as
With the corresponding probabilities p(Y = 1) = π and p(Y = 0) = 1−π.
In this case, the response variable and the corresponding error term will assume a binomial distribution with a logit transformation rather than a normal distribution. If there are n such random variables , , , ………, with equal probability (π), then the random variable Y has the binomial (n, π) distribution as;
Thus, binary logistic regression analysis expresses individual probabilities of success as a function of predictor variables as follows;
Where the left hand side represents individual probability of success and the right hand side is the function of predictor variables. But the expressions on the left and right hand sides have different ranges; the left hand side has values between 0 and 1, while the right hand side assumes any real number. Thus, to overcome this problem, it is important to convert these probabilities into odds as follows;
then we can take logarithms to obtain the logit link function, which has the effect of removing the floor restriction.
Even though the above binary regression model provides us with the effect of several predictors on the response variable, due to the hierarchical nature of the data, where each infant is nested in a mother and each mother is nested in an enumeration area, the multilevel approach is recommended over the standard approach (28). If there are N predictors X at the child level, Q predictors Z at the mother level, and K predictors W at the enumeration area level, then the 3-level model for a binary outcome variable with a mean is;
Where, u0jk and u00k are the intercept variations at the mother and enumeration area level, respectively.
Results
Descriptive statistics
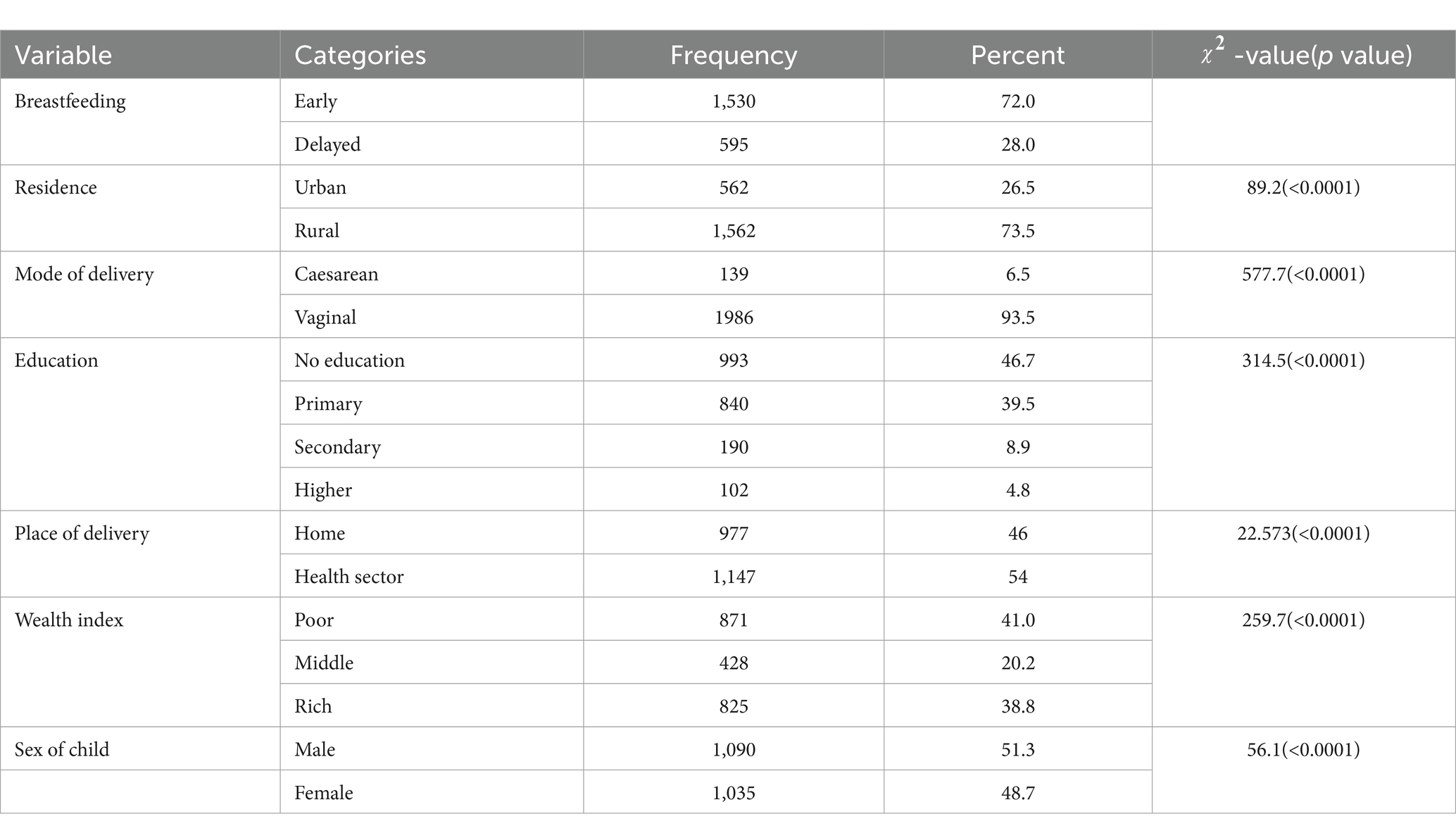
This study was conducted on the multilevel analysis of early initiation of breastfeeding among 2,125 infants who were born within 24 months before the 2019 Ethiopia mini demographic and health survey. Accordingly, the prevalence of early initiation of breastfeeding among the randomly sampled infants in the country was 72%. Among these randomly selected infants, 51.3% were male, and the remaining 48.7% were female. The average age of randomly selected mothers was 27.65 years, with minimum and maximum values of 15 and 49 years, respectively. Moreover, the average preceding birth interval, gestational age, and number of antenatal visits were 39.79 months, 33.6 weeks, and 3.08 visits, respectively. However, among these mothers, the majority (73.5%) belongs to rural residents, while the remaining 26.5% is urban residents. Most of the mothers (93.5%) used vaginal delivery. Regarding the place of delivery, the majority (54%) delivered their child in any of the health facilities. In addition, when compared to other categories of factors, the majority of these sampled mothers were illiterate unschooled (46.7%) and poor (41.0%). Moreover, the significance of the Chi Square value showed the existence of a significant association between the early initiation of breastfeeding and the corresponding predictors at a 5% level of significance (Table 1).
Model selection
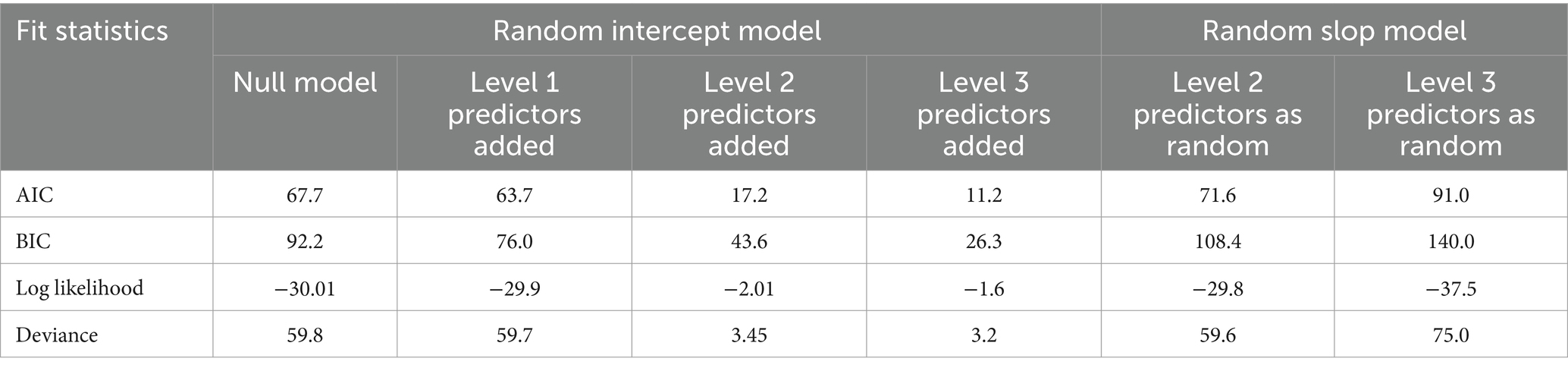
Model selection is the task of selecting the statistically best model that fits the statistical data among a series of candidate models. The intra-class correlation was computed from the intercept-only model for the purpose of identifying the proportion of variance explained by the grouping structure. Then the value demonstrated that the use of multilevel analysis, which takes into account the effect of such grouping structures, is more important than single-level analysis. Moreover, due to the hierarchical nature for the data, the presence of predictors at different levels in multilevel studies makes the model selection different from standard methods. Accordingly, different mixed-effects models were considered to analyse the early initiation of breastfeeding in Ethiopia. Due to the maximum value for log likelihood statistics and the minimum value for deviance, the random intercept model with fixed infant, mother, and enumeration area level predictors was the best fit to the data (Table 2).
The intercept-only model
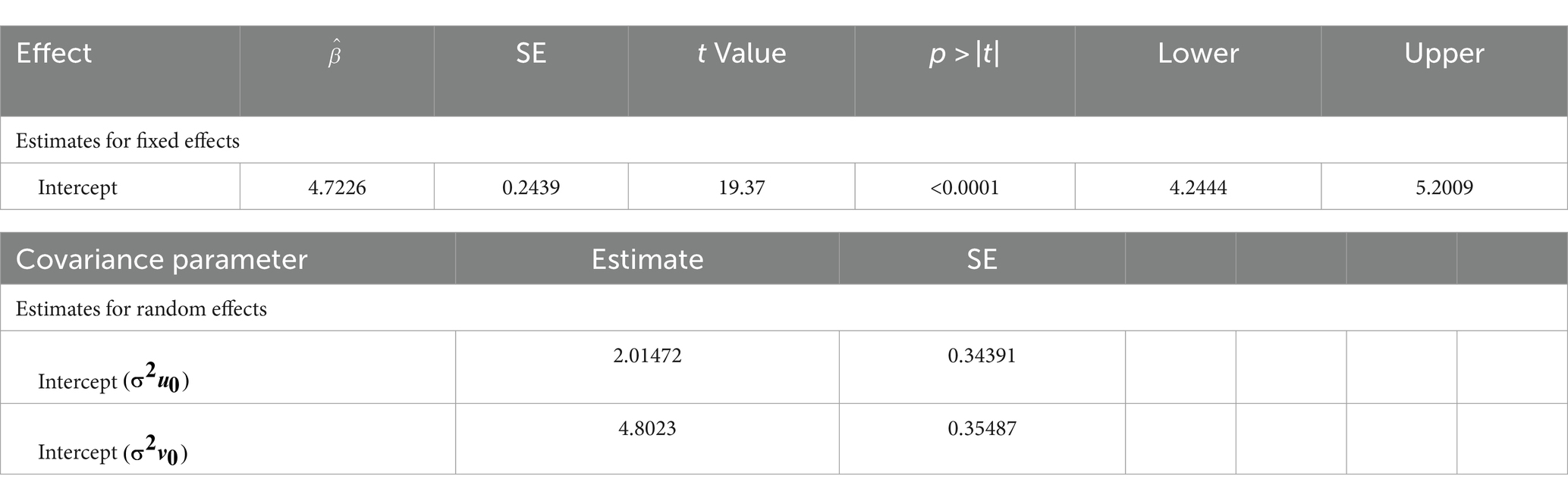
The intercept-only model is the model fitted without any predictor variables. In multilevel analysis, the random effect results from the intercept-only model are important to indicate the necessity of such an analysis. The residual error variance at the mother and enumeration area levels was estimated to be 2.01472 and 4.8023, respectively, as a result of the maximum mean pseudo-likelihood estimation. We can conclude that there is more variation among the different enumeration areas (2.4219) than within the enumeration areas (0.4534). In a logistic regression model without over-dispersion, the lower level (child level) variance is not reported in the result, and it is automatically constrained to . The proportion of variance explained by the grouping structure could be discussed further when we calculate the intra-class correlation ( ). In three-level models, the proportion of explained variance at the second and third levels can be identified by the intra-class correlation separately. Let the variances at the first, second, and third level are and respectively (29).
This result implies that 19.9% of the variation in early initiation of breastfeeding was at the mother’s level, 47.5% was at the enumeration area level, and the remaining 32.6% was at the infant’s level (Table 3).
Variable selection
When modeling with many independent variables, of which only a few are likely to be important, finding an appropriate subset of explanatory variables for the model is called variable selection.
Univariable analysis
The first step in a purposeful variable selection procedure is a univariable analysis. This step concerned the analysis of each predictor with the early initiation of breastfeeding at a 25% level to “screen” out potentially significant variables for consideration in the multivariable model. Based on this analysis, all the predictors except sex of infants and wealth index were statistically significant at a 25% level and not considered in multivariable analysis (Table 4).
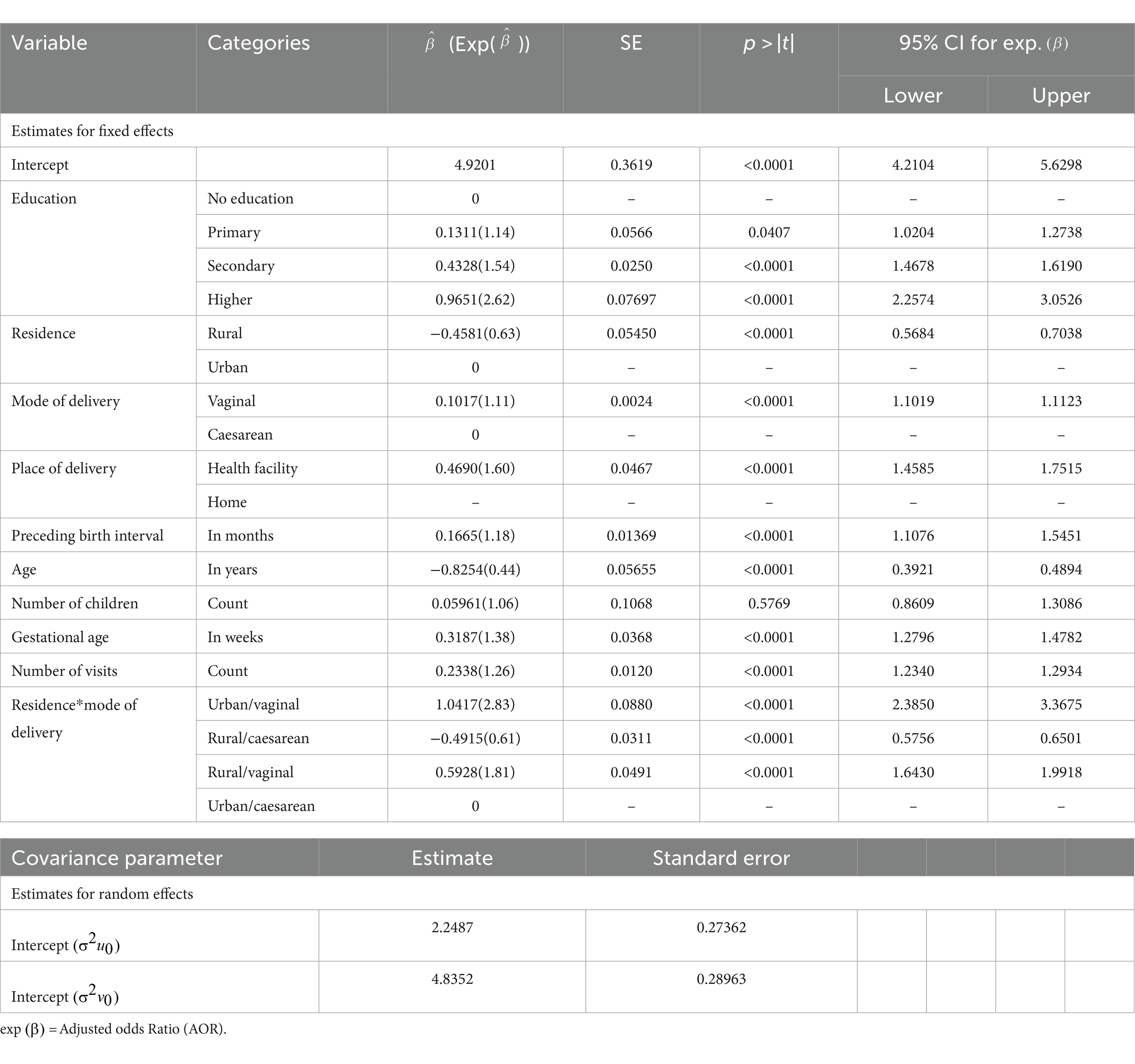
Multivariable analysis
This is the second step of the purposeful variable selection procedure, concerned with the analysis of all the significant predictors of early initiation of breastfeeding. Accordingly, results from the final multilevel binary logistic regression model revealed that age of mothers, place of residence, number of antenatal care visits, preceding birth interval, gestational age of infants, mother’s education level, mode of delivery, place of delivery, and the interaction of residence and mode of delivery were the significant predictors of early initiation of breastfeeding in Ethiopia. The random effect estimates revealed that there was more variation at higher levels (mothers and enumeration area) than at lower level (infants) (Table 5).
Discussion
This study was conducted based on secondary data obtained from randomly selected mothers across the country. The prevalence of early initiation of breastfeeding among infants within 24 months before the 2019 Ethiopia Mini Demographic and Health Survey was 72%. This proportion is below the plan of the Ethiopian Ministry of Health Sector Development Program, which targets the prevalence of early initiation of breastfeeding at 92% (22). Moreover, this prevalence is lower than the recently reported prevalence of early initiation of breastfeeding in Burundi (86.19%), Ruanda (80.57%), and Malawi (78.38%) (30). This variation might happen due to the differences in the demographic and socio-cultural characteristics of the countries, such as the mother’s educational attainment, age, place of residence, place of delivery, mode of delivery, number of antenatal care visits, preceding birth interval, and gestational age of infants.
The estimated adjusted odds ratio for the age of mothers was exp. (−0.8254) = 0.44, implying that a one-year increase in the age of mothers reduced the odds of early initiation of breastfeeding by 56% (95% CI: 0.3921, 0.4894), while all other variables remained constant. The result was consistent with refs. (30–32), where increasing the age of mothers was associated with a delayed initiation of breastfeeding.
The estimated adjusted odds ratio for the number of antenatal care visits was exp.(0.2338) = 1.26 (95% CI, 1.2340, 1.2934), implying that one more antenatal care visit was associated with a 26% increment in the odds of early initiation of breastfeeding among mothers in Ethiopia, while all other variables remained constant. The result was consistent with refs. (31, 33), where there is a direct relationship between the numbers of antenatal care visits and the prevalence of early initiation of breastfeeding.
The estimated adjusted odds ratio for the preceding birth interval was exp.(0.1665) = 1.18, implying that a one-month increase in the preceding birth interval increases the odds of early initiation of breastfeeding by 18% (95% CI, 1.1076, 1.5451), while all other variables remained constant. The result was consistent with refs. (31, 33), where an increasing preceding birth interval was associated with a higher prevalence of early initiation of breastfeeding.
The estimated adjusted odds ratio for the gestational age of a child was exp.(0.3187) = 1.38, implying that a one-week increase in gestational age increases the odds of early initiation of breastfeeding by 38% (95% CI, 1.2796, 1.4782), while all other variables remained constant. The result was consistent with refs. (34, 35), where increasing gestational age of an infant was associated with a higher prevalence of timely initiation of breastfeeding.
The estimated adjusted odds ratio of early initiation of breastfeeding among rural mothers compared to urban mothers was exp. (−0.4581) = 0.63, indicating that the odds of early initiation of breastfeeding among rural women were 37% (95% CI: 0.5684, 0.7038) lower than the odds of early initiation of breastfeeding among urban mothers, keeping all other variables constant. The result was consistent with refs. (33, 36–38), where rural residents were less likely to initiate timely breastfeeding than mothers in urban areas.
The estimated adjusted odds ratio of early initiation of breastfeeding among mothers with vaginal delivery as compared to those with caesarean section was exp. (0.1017) = 1.11, indicating that the odds of early initiation of breastfeeding among mothers with vaginal delivery were 11% (95% CI: 1.1019, 1.1123) higher than those with caesarean section, keeping all other variables constant. The result was consistent with refs. (6, 31, 34, 36–39), where giving birth by caesarean section is associated with a lower prevalence of early initiation of breastfeeding than vaginal delivery.
The estimated adjusted odds ratio of early initiation of breastfeeding among mothers who bear their child at a health facility as compared to those at home was exp. (0.4690) = 1.60, indicating that the odds of early initiation of breastfeeding among mothers who bear their child at a health facility were 60% (95% CI: 1.4585, 1.7515) higher than those at home, keeping all other variables constant. The result was consistent with refs. (31, 33, 36, 37), where mothers who delivered with the assistance of health professionals were associated with a higher prevalence of early initiation of breastfeeding. Moreover, where a dedicated psychologist and trained professionals in human lactation are present in hospitals to inform and support mothers immediately after childbirth, there will be a significant increment in the percentage of early onset and not abandonment of breastfeeding (40). The odds of early initiation of breastfeeding among mothers with primary, secondary, and higher education were 14, 54, and 162%, respectively, higher than the odds of early initiation of breastfeeding among mothers with no education, keeping all other variables constant. The result was consistent with refs. (31, 33, 38, 41), where educated mothers were more likely to initiate timely breastfeeding than illiterate mothers. In order to reach a higher overall percentage of breastfeeding, training should focus on women with lower levels of education. This subgroup is the one that could benefit the most from information from the staff in the hospital, taking into account the previous misinformation on the subject and reducing disadvantages coming from low education levels (42).
The odds of early initiation of breastfeeding among rural mothers with caesarean sections were 39% lower than the odds of early initiation of breastfeeding among urban mothers with caesarean sections, keeping all other variables constant. The odds of early initiation of breastfeeding among urban and rural mothers with vaginal delivery were 183 and 81%, respectively, higher than the odds of early initiation of breastfeeding among urban mothers with caesarean sections. The result was consistent with refs. (6, 38), where childbearing by caesarean section was significantly associated with delayed initiation of breastfeeding compared to vaginal delivery given urban or rural residents.
Strengths and weaknesses of the study
This study demonstrates how data collected through demographic surveys can be used. The methodology used to identify factors influencing early breastfeeding is correct and the results are in line with known results. However, the data must be integrated with the other variables that justify a delayed start of breastfeeding, which can however be collected by ad hoc surveys on clinical records.
Conclusion
This study aimed to identify factors associated with the early initiation of breastfeeding in Ethiopia using a framework of multilevel analysis of the 2019 Ethiopia Mini Demographic and Health Survey data. The prevalence of early initiation of breastfeeding was 72%, which is below the plan of the Ethiopian Ministry of Health Sector Development Program, and close monitoring of each mother during birth was important. As the result revealed, there was more variation due to the grouping structure than infant-level variation, so analysis of such data using a single-level approach may ignore such variation. Moreover, age of mothers, place of residence, number of antenatal care visits, preceding birth interval, gestational age of an infant, mother’s education level, mode of delivery, place of delivery, and the interaction of residence and mode of delivery were the significant predictors of early initiation of breastfeeding in Ethiopia. The federal and regional stakeholders should focus on infant feeding strategies, especially modifiable factors like place of delivery, mode of delivery, counselling during antenatal care visits, and socioeconomic characteristics of mothers. Moreover, sufficient supportive care, especially for rural mothers who undergo caesarean sections, is needed to improve the prevalence of early initiation of breastfeeding.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by International Classification of Functioning (ICF) institutional review board (IRB# 187138). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
NH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. TK: Data curation, Methodology, Writing – review & editing. GH: Methodology, Software, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank the Central Statistical Agency of Ethiopia for making the data freely available for research purposes. Moreover, we are very grateful to the institutional review board of the International Classification of Functioning (ICF) for their support in providing an ethical statement.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AIC, Akaike Information Criteria; BIC, Bayesian Information Criteria; CSA, Central Statistical Agency; EA, Enumeration Area; EMDHS, Ethiopia Mini Demographic and Health Survey; EPHI, Ethiopian Public Health Institute; FMoH, Federal Ministry of Health; HSTP, Health Sector Transformation Plan; ICF, International Classification of Functioning; NNP, National Nutrition Program,; SDG, Sustainable Development Goals; SNNPR, Southern Nations, Nationalities, and Peoples’ Region; UNICEF, United Nations Children’s Fund; WHO, World Health Organization.
Footnotes
References
1. Gilmour, S, and Shibuya, K. Simple steps to equity in child survival. BMC Med (2013);11:1–3, doi: 10.1186/1741-7015-11-261
2. Victora, CG, Bahl, R, Barros, AJ, França, GV, Horton, S, Krasevec, J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. (2016) 387:475–90. doi: 10.1016/S0140-6736(15)01024-7
3. Binns, C, Lee, M, and Low, WY. The long-term public health benefits of breastfeeding. Asia Pac J Public Health. (2016) 28:7–14. doi: 10.1177/1010539515624964
4. Mennella, JA, Yourshaw, LM, and Morgan, LK. Breastfeeding and smoking: short-term effects on infant feeding and sleep. Pediatrics. (2007) 120:497–502. doi: 10.1542/peds.2007-0488
5. Arts, M, Taqi, I, and Bégin, F. Improving the early initiation of breastfeeding: the WHO-UNICEF breastfeeding advocacy initiative. Breastfeed Med. (2017) 12:326–7. doi: 10.1089/bfm.2017.0047
6. Takahashi, K, Ganchimeg, T, Ota, E, Vogel, JP, Souza, JP, Laopaiboon, M, et al. Prevalence of early initiation of breastfeeding and determinants of delayed initiation of breastfeeding: secondary analysis of the WHO global survey. Sci Rep. (2017) 7:44868. doi: 10.1038/srep44868
7. Kamudoni, P, Maleta, K, Shi, Z, and Holmboe-Ottesen, G. Exclusive breastfeeding duration during the first 6 months of life is positively associated with length-for-age among infants 6–12 months old, in Mangochi district, Malawi. Eur J Clin Nutr. (2015) 69:96–101. doi: 10.1038/ejcn.2014.148
8. Mugadza, G, Zvinavashe, M, Gumbo, FZ, and Pedersen, BS. Early breastfeeding initiation and incidence of neonatal sepsis in Chipinge District Zimbabwe. Int J Contemp Pediatr. (2018) 5:1–5. doi: 10.18203/2349-3291.ijcp20175564
9. Smith, ER, Hurt, L, Chowdhury, R, Sinha, B, Fawzi, W, Edmond, KM, et al. Delayed breastfeeding initiation and infant survival: a systematic review and meta-analysis. PLoS One. (2017) 12:e0180722. doi: 10.1371/journal.pone.0180722
10. Berkat, S, and Sutan, R. The effect of early initiation of breastfeeding on neonatal mortality among low birth weight in Aceh Province, Indonesia: an unmatched case control study. Adv Epidemiol. (2014) 2014:1–7. doi: 10.1155/2014/358692
11. Group NS. Timing of initiation, patterns of breastfeeding, and infant survival: prospective analysis of pooled data from three randomised trials. Lancet Glob Health. (2016) 4:e266–75. doi: 10.1016/S2214-109X(16)00040-1
12. Du Plessis, L . Let's work together to make breastfeeding work! S Afr J Clin Nutr. (2015) 28:103–4. doi: 10.1080/16070658.2015.11734543
13. Hansstein, FV . The impact of breastfeeding on early childhood obesity: evidence from the National Survey of Children’s health. Am J Health Promot. (2016) 30:250–8. doi: 10.1177/0890117116639564
14. Barbier, EB, and Burgess, JC. Sustainable development goal indicators: analyzing trade-offs and complementarities. World Dev. (2019) 122:295–305. doi: 10.1016/j.worlddev.2019.05.026
15. UN Global Nutrition Agenda. Delivering on the commitment to eradicate malnutrition in all its forms: E role of the UN system. New York, NY, USA: UN Global Nutrition Agenda (2015).
16. Lee, BX, Kjaerulf, F, Turner, S, Cohen, L, Donnelly, PD, Muggah, R, et al. Transforming our world: implementing the 2030 agenda through sustainable development goal indicators. J Public Health Policy. (2016) 37:13–31. doi: 10.1057/s41271-016-0002-7
17. Qazi, S, Aboubaker, S, MacLean, R, Fontaine, O, Mantel, C, Goodman, T, et al. Ending preventable child deaths from pneumonia and diarrhoea by 2025. Development of the integrated global action plan for the prevention and control of pneumonia and diarrhoea. Arch Dis Child. (2015) 100:S23–8. doi: 10.1136/archdischild-2013-305429
18. Ogbo, FA, Okoro, A, Olusanya, BO, Olusanya, J, Ifegwu, IK, Awosemo, AO, et al. Diarrhoea deaths and disability-adjusted life years attributable to suboptimal breastfeeding practices in Nigeria: findings from the global burden of disease study 2016. Int Breastfeed J. (2019) 14:1–9. doi: 10.1186/s13006-019-0198-9
19. Assefa, Y, Van Damme, W, Williams, OD, and Hill, PS. Successes and challenges of the millennium development goals in Ethiopia: lessons for the sustainable development goals. BMJ Glob Health. (2017) 2:e000318. doi: 10.1136/bmjgh-2017-000318
20. Odhiambo, LK, Session, N, Shoham, J, and Dolan, C. Multi-sector programmes at the sub-national level: A case study of the Seqota declaration in Naedir Adet and Ebinat woredas in Ethiopia; (2019).
21. Abageda, M, Belachew, T, Mokonen, A, and Hamdela, B. Predictors of optimal breastfeeding practices among mothers who have less than 24 months of age children in Misha District, Hadiya zone, South Ethiopia. J Preg Child Health. 2:182. doi: 10.4172/2376-127X.1000182
22. Baschieri, A, and Hobson, J. Support for the Ethiopian health sector development Programme (Federal Ministry of Health MDG Performance Fund); (2013).
24. World Health Organization. Acceptable medical reasons for use of breast-Milk substitutes. Acceptable medical reasons for use of breast-milk substitutes; (2009): p. 12.
25. Daelmans, B, Dewey, K, and Arimond, M. New and updated indicators for assessing infant and young child feeding. Food Nutr Bull. (2009) 30:S256–S62.
26. Cleary, PD, and Angel, R. The analysis of relationships involving dichotomous dependent variables. J Health Soc Behav. (1984) 25:334. doi: 10.2307/2136429
28. Moliterno, TP, and Mahony, DM. Network theory of organization: a multilevel approach. J Manag. (2011) 37:443–67.
29. Davis, P, and Scott, A. The effect of interviewer variance on domain comparisons. Surv Methodol. (1995) 21:99–106.
30. Appiah, F, Ahinkorah, BO, Budu, E, Oduro, JK, Sambah, F, Baatiema, L, et al. Maternal and child factors associated with timely initiation of breastfeeding in sub-Saharan Africa. Int Breastfeed J. (2021) 16:1–11. doi: 10.1186/s13006-021-00402-3
31. John, JR, Mistry, SK, Kebede, G, Manohar, N, and Arora, A. Determinants of early initiation of breastfeeding in Ethiopia: a population-based study using the 2016 demographic and health survey data. BMC Pregnancy Childbirth. (2019) 19:1–10. doi: 10.1186/s12884-019-2211-0
32. Chien, LY, and Tai, CJ. Effect of delivery method and timing of breastfeeding initiation on breastfeeding outcomes in Taiwan. Birth. (2007) 34:123–30. doi: 10.1111/j.1523-536X.2007.00158.x
33. Senanayake, P, O’Connor, E, and Ogbo, FA. National and rural-urban prevalence and determinants of early initiation of breastfeeding in India. BMC Public Health. (2019) 19:1–13. doi: 10.1186/s12889-019-7246-7
34. Patel, A, Banerjee, A, and Kaletwad, A. Factors associated with prelacteal feeding and timely initiation of breastfeeding in hospital-delivered infants in India. J Hum Lact. (2013) 29:572–8. doi: 10.1177/0890334412474718
35. Örün, E, Yalçin, SS, Madendag, Y, Üstünyurt-Eras, Z, Kutluk, S, and Yurdakök, K. Factors associated with breastfeeding initiation time in a baby-friendly hospital. Turk J Pediatr. (2010) 52:10–6.
36. Ahmed, KY, Page, A, Arora, A, and Ogbo, FA. Trends and determinants of early initiation of breastfeeding and exclusive breastfeeding in Ethiopia from 2000 to 2016. Int Breastfeed J. (2019) 14:1–14. doi: 10.1186/s13006-019-0234-9
37. Woldeamanuel, BT . Trends and factors associated to early initiation of breastfeeding, exclusive breastfeeding and duration of breastfeeding in Ethiopia: evidence from the Ethiopia demographic and health survey 2016. Int Breastfeed J. (2020) 15:1–13. doi: 10.1186/s13006-019-0248-3
38. Liben, ML, and Yesuf, EM. Determinants of early initiation of breastfeeding in Amibara district, northeastern Ethiopia: a community based cross-sectional study. Int Breastfeed J. (2016) 11:1–7.
39. Tilahun, G, Degu, G, Azale, T, and Tigabu, A. Prevalence and associated factors of timely initiation of breastfeeding among mothers at Debre Berhan town, Ethiopia: a cross-sectional study. Int Breastfeed J (2016);11:1–29, 27, doi: 10.1186/s13006-016-0086-5
40. Ragusa, R, Marranzano, M, La Rosa, VL, Giorgianni, G, Commodari, E, Quattrocchi, R, et al. Factors influencing uptake of breastfeeding: the role of early promotion in the maternity hospital. Int J Environ Res Public Health. (2021) 18:4783. doi: 10.3390/ijerph18094783
41. Tariku, A, Biks, GA, Wassie, MM, Worku, AG, and Yenit, MK. Only half of the mothers practiced early initiation of breastfeeding in Northwest Ethiopia, 2015. BMC Res Notes. (2017) 10:1–7. doi: 10.1186/s13104-017-2823-2
Keywords: early initiation of breastfeeding, Ethiopia, demographic survey, regression analysis, public health
Citation: Hussen NM, Kassa TH and Habtie GM (2024) Multilevel analysis of early initiation of breastfeeding in Ethiopia. Front. Public Health. 12:1393496. doi: 10.3389/fpubh.2024.1393496
Edited by:
Satyajit Kundu, Griffith University, AustraliaReviewed by:
Melese Abate Reta, University of Pretoria, South AfricaRosalia Maria Ragusa, University Hospital Polyclinic Vittorio Emanuele, Italy
Copyright © 2024 Hussen, Kassa and Habtie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nuru Mohammed Hussen, bnVyZWRpaW41MTExQGdtYWlsLmNvbQ==
†ORCID: Nuru Mohammed Hussen, orcid.org/0000-0002-5423-65671
 Nuru Mohammed Hussen
Nuru Mohammed Hussen Tigabu Hailu Kassa
Tigabu Hailu Kassa Getnet Mamo Habtie
Getnet Mamo Habtie