- 1Key Laboratory of Environmental Medicine Engineering of Ministry of Education, Department of Epidemiology and Health Statistics, School of Public Health, Southeast University, Nanjing, China
- 2Jiangsu Provincial Center for Disease Control and Prevention, Nanjing, China
Objective: This meta-analysis aims to evaluate the global prevalence of mental disorders among young people living with HIV.
Methods: A comprehensive search was conducted of the PubMed, Embase, and Cochrane Library databases for articles relevant to the study, published between January 2013 and June 2023. To identify sources of heterogeneity and compare prevalence estimates among various groups, subgroup analyses were conducted. Study heterogeneity was assessed using Cochran’s Q and the I2 tests. The robustness of the findings was ascertained through sensitivity analyses, while publication bias was evaluated with funnel plots and Egger’s test.
Results: Sixty studies were included in this meta-analysis. It revealed that approximately one-quarter of YLWH experience depression, with a prevalence of 24.6% (95% CI: 21.1–28.2%). The prevalence of anxiety was found to be 17.0% (95% CI: 11.4–22.6%). Regarding suicidality, the prevalence of suicidal ideation and lifetime suicidal ideation in YLWH was 16.8% (95% CI: 11.3–22.4%) and 29.7% (95% CI: 23.7–35.7%), respectively. Additionally, the prevalence rates for suicidal attempts and lifetime suicidal attempts were 9.7% (95% CI: 4.0–15.4%) and 12.9% (95% CI: 2.8–23.1%), respectively. The prevalence of Post-Traumatic Stress Disorder and Attention Deficit Hyperactivity Disorder was identified as 10.5% (95% CI: 5.8–15.2%) and 5.0% (95% CI: 3.1–7.0%), respectively.
Conclusion: The findings indicate a heightened risk of mental disorders among YLWH, underscoring the necessity for targeted intervention strategies to mitigate their suffering and potentially diminish the adverse impacts.
Systematic Review Registration: PROSPERO, identifier CRD42023470050, https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023470050.
Introduction
According to the World Health Organization (WHO), individuals aged 10–24 years constitute the young demographic (1). HIV persists as a major global health challenge, affecting approximately 39.0 million people worldwide in 2022, with a significant concentration in the WHO African Region (2). Alarmingly, the incidence of HIV is increasingly prevalent among young people, as evidenced by 480,000 new cases in this age group in 2022 alone (3).
Contemporary research indicates that individuals with HIV are more prone to mental health disorders than their non-infected counterparts (4, 5), a trend also observed in young people living with HIV (YLWH). Depression and anxiety are particularly prevalent mental health issues among YLWH. Research also indicates a significant prevalence of suicide, Post-Traumatic Stress Disorder (PTSD), and Attention-deficit hyperactivity disorder (ADHD) within this demographic (6, 7). The past decade has seen an escalation in research focusing on the mental health of YLWH. However, the global variation in reported mental disorder rates among YLWH underscores the need for more systematic research and thorough analysis. For example, the prevalence of anxiety among YLWH ranges from 2.2% in Indonesia to 56.7% in South Africa (8, 9), and for depression, it ranges from 3.3 to 52.6%, with both studies conducted in Kenya (10, 11). This variance can be attributed to factors such as diverse study population characteristics, disease stages, geographical locations, and the use of different standardized measurement tools. Additionally, research has linked mental health disorders with suboptimal adherence to antiretroviral therapy (ART), resulting in poor virologic control, drug resistance, and heightened HIV morbidity and mortality (12, 13). Therefore, comprehending the worldwide prevalence of mental disorders among young people living with HIV is of paramount importance and urgency.
Prior systematic reviews and meta-analyses have primarily focused on adolescents, with less emphasis on young adults. Our systematic review and meta-analysis extend the age range to encompass YLWH aged 10–24. This study is, to the best of our knowledge, the first to offer a comprehensive global synthesis of data regarding the prevalence of mental disorders among this demographic. The findings will offer critical insights into the prevalence of mental health conditions within this group, thus facilitating the creation of timely and impactful interventions.
Methods
The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guideline was used to guide this review’s design and reporting (14). Registration of the study was completed under the identifier CRD42023470050 with the International Prospective Register of Systematic Reviews (PROSPERO).
Search strategy and study eligibility
We conducted searches in PubMed, Embase, and the Cochrane Library from June 20, 2023, to June 30, 2023, for cross-sectional studies, longitudinal studies, and case–control studies on the prevalence of depression, anxiety, suicidality, PTSD, and ADHD YLWH aged 10 to 24 years, published between January 2013 and June 2023. The keywords and their combinations include HIV and all the synonyms; mental disorders, depression, anxiety, suicide, PTSD, ADHD and all their synonyms; adolescents and young people and all the synonyms (The full search strategy see Supplementary material 2 Table S1). The retrieved papers were included in this review if they met the following inclusion and exclusion criteria.
Inclusion criteria: (1) The study population was YLWH aged 10–24 years old; (2) Provide data on the prevalence of any or multiple mental disorders among the following: depression, anxiety, suicidality, PTSD, and ADHD. (3) Cross-sectional studies, longitudinal studies and case–control studies.
Exclusion criteria: (1) Case studies, reviews, comments, conference abstracts, case reports and letters; (2) Not English articles; (3) No data on the prevalence of any of the mental disorders including depression, anxiety, suicidality, PTSD, and ADHD were provided; (4) Age range of the study population is not specified; (5) The study population is not YLWH aged 10–24 years old.
Screening and data extraction
Following the search strategy, the retrieved articles were imported into Endnote X9, and duplicates were removed. Two researchers (SZ and WZ) independently screened the titles and abstracts for initial selection and then independently read the full texts for secondary screening. Studies to be included were determined based on the inclusion and exclusion criteria. Any discrepancies were adjudicated by a third researcher (FO).
Data extraction was conducted independently by two researchers (SZ and WZ), encompassing various study parameters: (1) Article’s first author and publication year; (2) Country; (3) Study design; (4) ART status; (5) Sample size; (6) Male ratio; (7) Age range; (8) Mean or median age of participants; (9) Period of survey execution; (10) Instruments used for measurement; (11) Cut-off score; (12) Validation information for the measurement tools; (13) Prevalence of depression, anxiety, suicidality, PTSD, and ADHD. Specifically for suicide, separate assessments were made for suicidal ideation, lifetime suicidal ideation, suicidal attempts, and lifetime suicidal attempts. In the case of longitudinal studies, only baseline data were considered.
Quality assessment
For quality assessment, the Agency for Healthcare Research and Quality (AHRQ) cross-sectional study quality evaluation list, comprising 11 items, was utilized (15). Each item rated “yes” referring value “1” was summed giving a range of a possible total score between 0 and 11 on the checklist. Studies were classified based on quality into three categories: low (0–3 points), medium (4–7 points), and high (8–11 points). The evaluation was conducted by two researchers (SZ and WZ), using the AHRQ criteria. In cases of inconsistent evaluations, a third reviewer (FO) was consulted for reassessment.
Data analysis
We employed the R4.2.3 software for calculating the aggregated prevalence of various mental disorders. The fixed effect model was applied in cases where the I2 heterogeneity test indicated moderate or low heterogeneity (I2 < 50%); conversely, for substantial heterogeneity (I2 ≥ 50%), the random effect model was utilized. The resultant composite findings were represented through forest plots. We conducted subgroup analyses to explore the sources of heterogeneity. To verify the reliability of our findings, we performed sensitivity analyses on mental disorders featured in over 10 studies to assess the impact of individual studies on the overall results. To address publication bias, we constructed funnel plots and applied Egger’s test to mental disorder categories with at least 10 estimates (16).
Results
Search results
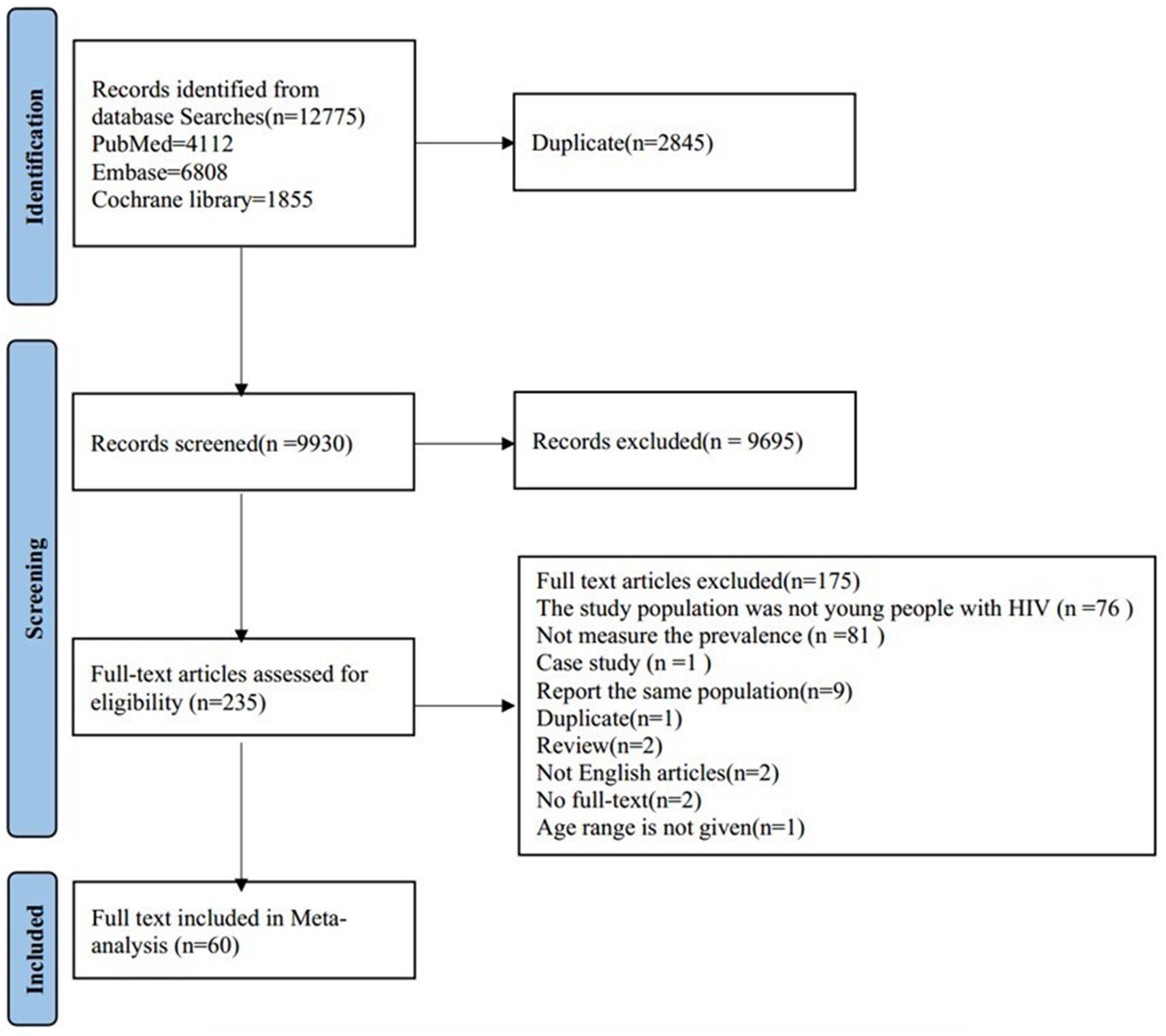
We conducted a search across PubMed (4,112 articles), Embase (6,808 articles), and the Cochrane Library (1,855 articles), totaling 12,775 articles. After excluding 2,845 duplicate articles, we reviewed the titles and abstracts of the remaining 9,930 articles, of which 235 articles underwent full-text eligibility screening. Among these, 175 articles were excluded, and ultimately, 60 articles were included in our meta-analysis. The selection process and reasons for exclusion were illustrated in Figure 1.
Study characteristics
The final 60 studies included in this systematic review and meta-analysis were published in years ranging from 2014 to 2023, with the highest number of studies published in 2020, with 10 studies. The included studies were from 26 countries, of which 15 were from African countries, 7 from Asian countries, 2 from European countries, 1 from North American countries, and 1 from South American countries. The number of studies conducted in Africa, Asia, North America, Europe, and South America was 44, 7, 6, 2, and 1, respectively. Among the 60 studies included, 54 adopted a cross-sectional design, with the remaining comprising 1 case–control and 5 longitudinal studies. Among the 44 studies reporting ART status, 32 had populations on ART, 11 had majorities on ART with over 85% uptake, and only 1 had a population not on ART. Of the 46 studies that reported the survey time, the period of investigation ranged from June 2005 to March 2022 (see Supplementary material 1 Table S1). Among the 60 observational studies, 13 were of high quality, 47 were rated as medium quality, and none were classified as low quality (see Supplementary material 1 Table S2).
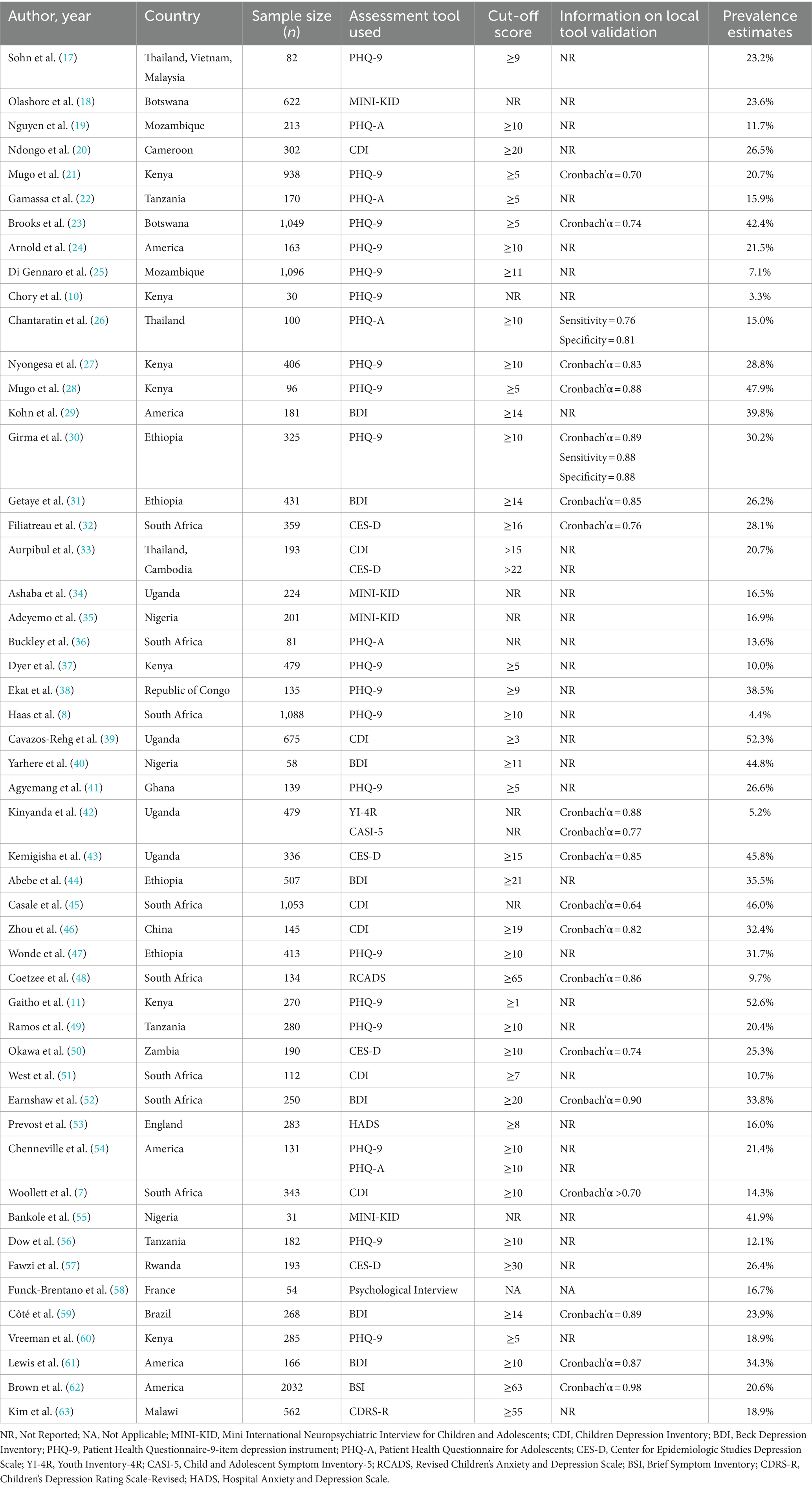
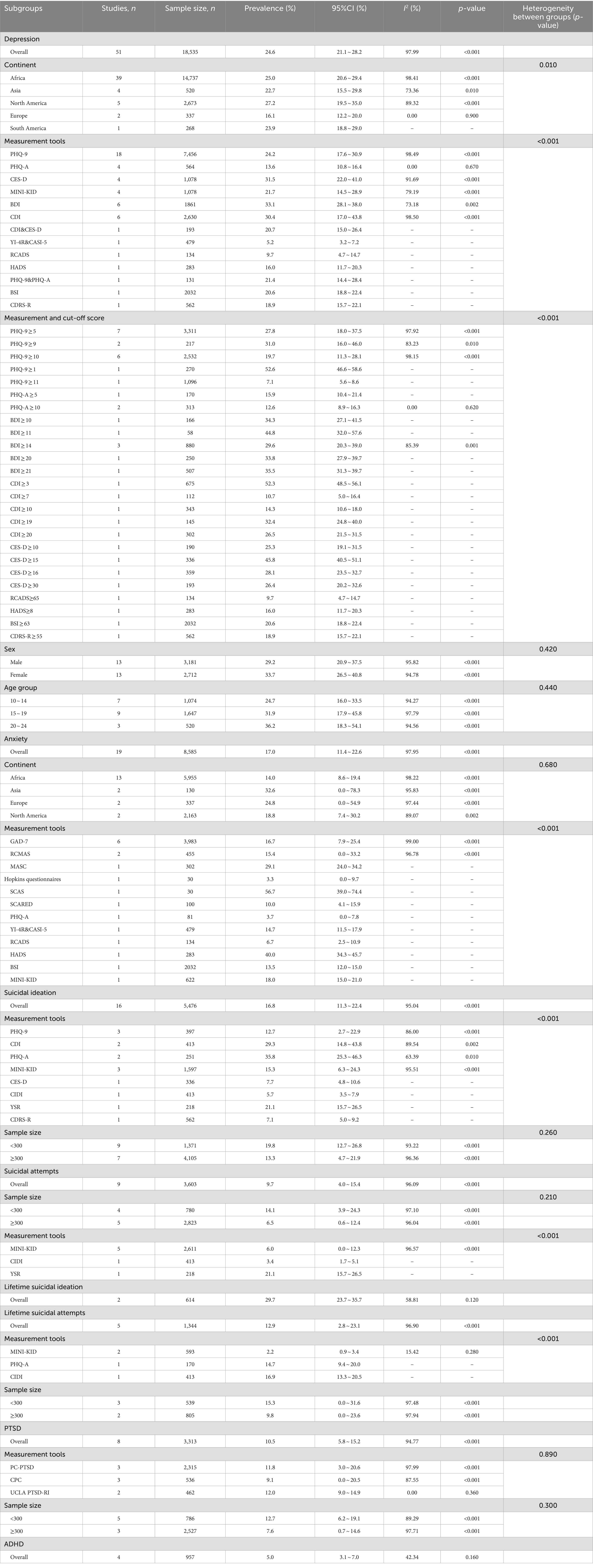
Depression
In this meta-analysis, a total of 51 studies reported on the prevalence of depression in YLWH, as outlined in Table 1. These studies encompassed a collective sample size of 18,535 participants, revealing a pooled prevalence of depression at 24.6% (95% CI: 21.1–28.2%). Notably, there was substantial heterogeneity observed among the studies (I2 = 98.03%, p < 0.001). The majority of these studies were conducted in Africa, accounting for 39 of the total, while South America contributed the least, with only one study. The measurement tools for depression were diverse, with the Patient Health Questionnaire-9 (PHQ-9) being used in 18 studies, the Beck Depression Inventory (BDI) and Child Depression Inventory (CDI) in 6 studies, and Patient Health Questionnaire for Adolescents (PHQ-A), Center for Epidemiologic Studies Depression Scale (CES-D), and Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) in 4 studies. Furthermore, 7 studies utilized different measurement tools, and 3 studies employed two tools concurrently.
The subgroup analysis of depression, as presented in Table 2, revealed variations in depression prevalence attributed to the measurement tools employed, yielding statistically significant differences among the groups (p < 0.001). Studies utilizing MINI-KID, PHQ-A, and BDI demonstrated reduced heterogeneity, particularly among those using PHQ-A (I2 = 0%, p = 0.67). Intriguingly, depression prevalence as determined by the PHQ-9 with a cut-off score of 5 was significantly higher (27.8, 95% CI: 18.0 to 37.5%) compared to a cut-off score of 10 (19.7, 95% CI: 11.3 to 28.1%). Similarly, the depression prevalence assessed by the PHQ-9 (cut-off score of 5) closely mirrored that assessed by the BDI (cut-off score of 14).
The prevalence of depression also demonstrated significant geographic variation. The highest pooled prevalence was observed in North America (27.2, 95% CI: 19.5–35.0%), and the lowest in Europe (16.1, 95% CI: 12.2–20.0%). Notably, heterogeneity was considerably reduced in studies from Asia, North America, and Europe, with respective I2 values of 73.36, 89.32, and 0%. Gender and age-based Subgroup analyses showed that the prevalence of depression in females (33.7, 95% CI: 26.5–40.8%) was higher than in males (29.2, 95% CI: 20.9–37.5%), but the difference did not reach statistical significance (p = 0.42). Additionally, higher prevalence rates were observed in older youth, with the 20–24 age group showing a prevalence of 36.2% (95% CI: 18.3–54.1%) and the 15–19 age group (31.9, 95% CI: 17.9–45.8%), compared to the 10–14 age group (24.7, 95% CI: 16.0–33.5%); However, these differences did not achieve statistical significance either (p = 0.44).
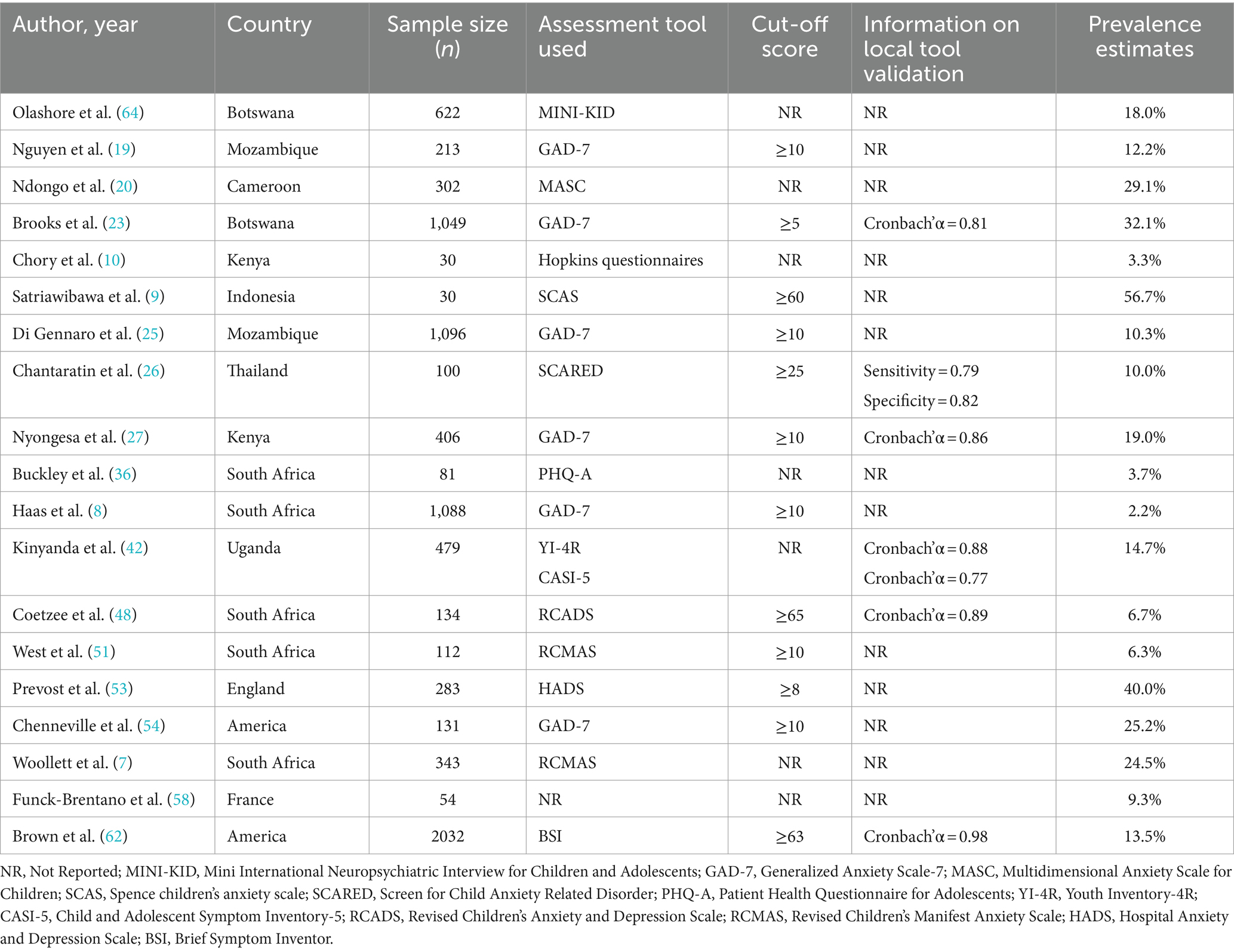
Anxiety
The meta-analytic synthesis of anxiety prevalence, conducted across 19 studies as delineated in Table 3, revealed a summary prevalence of 17.0% (95% CI: 11.4–22.6%) from a collective sample of 8,585 participants. This analysis uncovered considerable heterogeneity across studies (I2 = 97.95%, p < 0.001). Samples were sourced from a variety of geographic regions: Asia (n = 2), Africa (n = 13), North America (n = 2), and Europe (n = 2). Six studies predominantly utilized the Generalized Anxiety Disorder-7 (GAD-7) scale with a threshold of 10, whereas the Revised Children’s Manifest Anxiety Scale (RCMAS) was used in 2 studies. Notably, 1 study did not specify the measurement tool employed, another utilized two different tools concurrently, and the remaining 10 studies incorporated various other instruments.
In the stratified meta-analyses by continent and assessment instruments (Table 2), we explored the factors contributing to the observed heterogeneity and detailed the anxiety prevalence across continents. The pooled prevalence of anxiety in YLWH varied considerably, ranging from 14.0% in Africa (95% CI: 8.6–19.4%) to 32.6% in Asia (95% CI: 0.0–78.3%); however, these intercontinental differences did not reach statistical significance (p = 0.68). Subgroup analyses further revealed variations in anxiety prevalence depending on the measurement tools used, with significant differences detected (p < 0.001). The overall pooled prevalence and the prevalence determined using the GAD-7 (16.7, 95% CI: 7.9–25.4%) exhibited similarity.
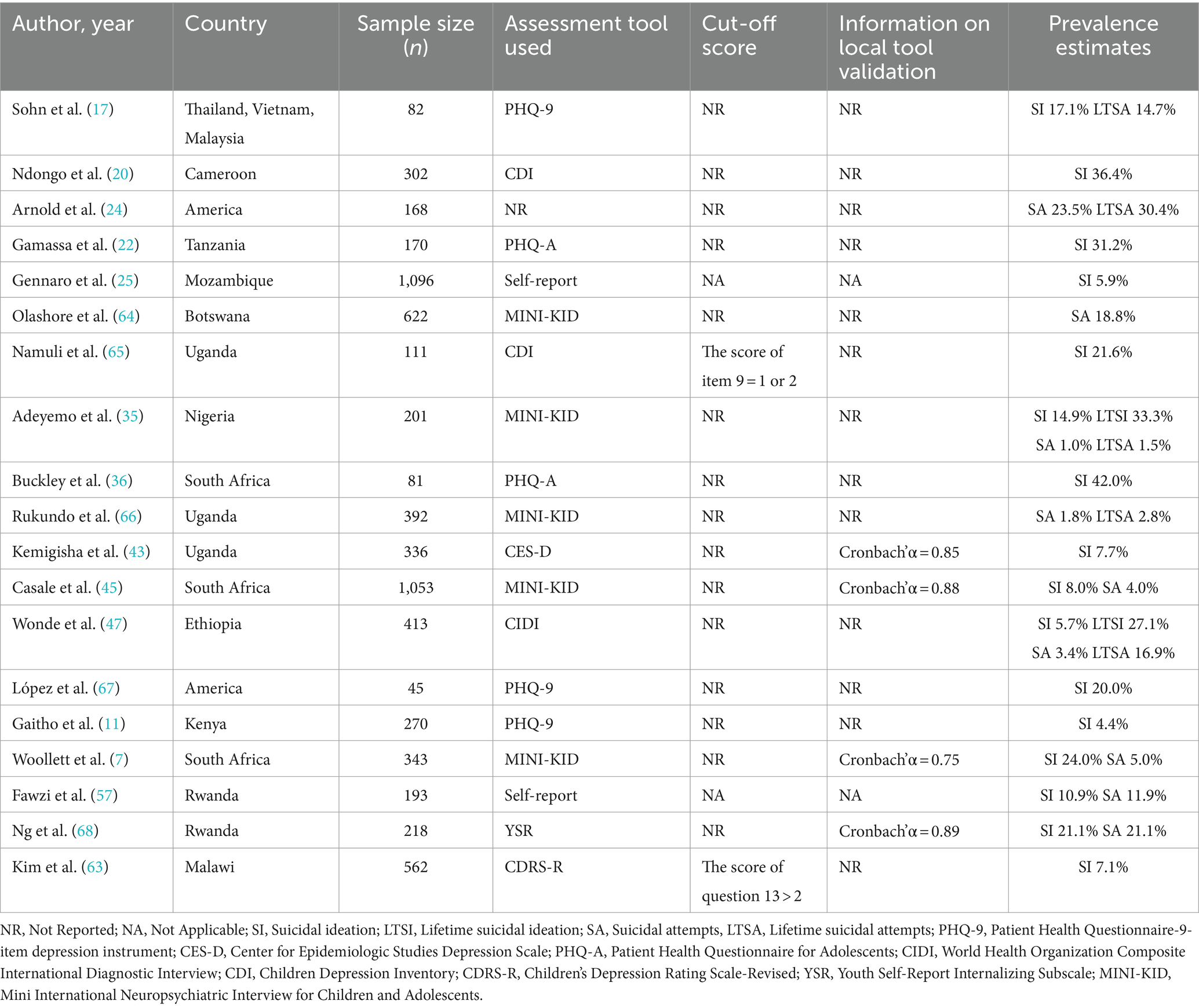
Suicidality
A total of 5,476 participants from 16 studies assessed suicidal ideation, while 614 participants from 2 studies evaluated lifetime suicidal ideation, as noted in Table 4. Regarding suicide attempts, 9 studies (totaling 3,603 participants) reported on suicide attempt prevalence, and 5 studies (with 1,344 participants) on lifetime suicide attempt prevalence (Table 4). As shown in Table 2, random effect prevalence estimates varied from 9.7% (95% CI: 4.0–15.4%) for lifetime attempts to 29.7% (95% CI: 23.7–35.7%) for suicidal ideation prevalence. Heterogeneity measures were notably high across all outcomes, with I2 ranging from 58.81 to 96.90%.
Subgroup analysis revealed significant differences in suicidal ideation prevalence when measured with the PHQ-A (35.8, 95%CI: 25.3–46.3%) and CDI (29.3, 95%CI: 14.8–43.8%), compared to the MINI-KID (15.3, 95%CI: 6.3–24.3%) and PHQ-9 (12.7, 95%CI: 2.7–22.8%). Additionally, marked differences were noted in the prevalence of suicidal and lifetime suicide attempts across measurement tools (p < 0.001). Analysis stratified by sample size revealed that studies with smaller sample sizes (<300) indicated higher rates of suicidal ideation, attempts, and lifetime attempts compared to those with larger sample sizes (≥300).
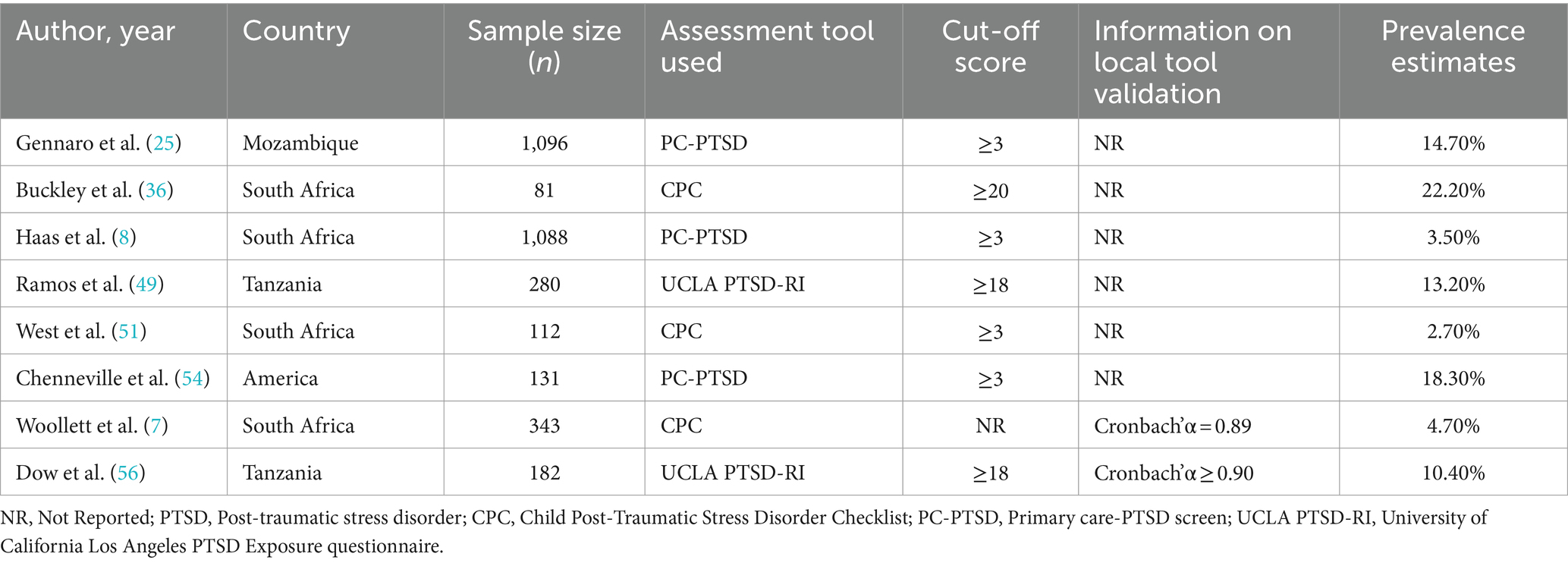
PTSD and ADHD
Eight studies reported on the prevalence of PTSD, as indicated in Table 5, encompassing a combined sample size of 3,313 participants. There was a notable variation in the reported prevalence of PTSD, with substantial heterogeneity observed (I2 = 94.77%, p < 0.001). Consequently, a random effects model was employed to aggregate the prevalence rates, yielding an overall prevalence of 10.5% (95% CI: 5.8–15.2%). Across the included studies, a total of three different measurement tools were utilized, with three studies employing both the Primary care-PTSD screen (PC-PTSD) and Child Post-Traumatic Stress Disorder Checklist (CPC), while the remaining two studies utilized the University of California Los Angeles PTSD Exposure questionnaire (UCLA PTSD-RI) for assessment.
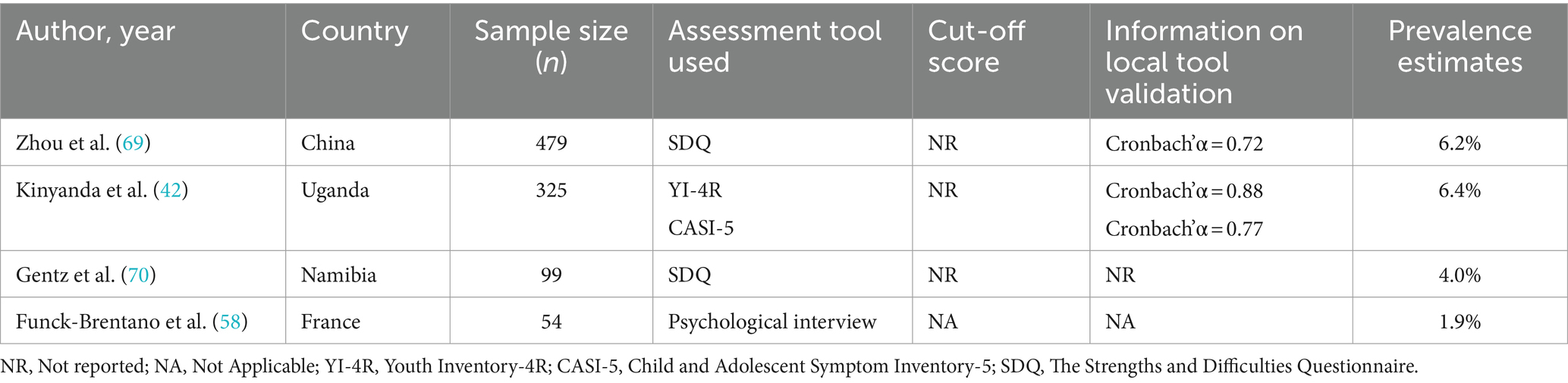
Table 6 displays the ADHD prevalence rates from all studies included. Heterogeneity testing yielded low to moderate levels (I2 = 42.34%, p = 0.16), necessitating the use of a fixed effects model for the analysis. ADHD prevalence in YLWH was determined to be 5.0% (95% CI: 3.1–7.0%).
Additionally, subgroup analysis presented in Table 2, which focused on the measurement tools for PTSD, showed that the prevalence rates assessed by different tools were comparable, with no statistically significant variations found across groups (p = 0.22). It was noted that studies with smaller sample sizes (<300) reported higher prevalence rates compared to those with larger sample sizes (≥300), though these differences were not statistically significant (p = 0.30).
Sensitivity analysis and publication bias
The sensitivity analysis revealed that no individual study significantly influenced the aggregated prevalence rates of depression, anxiety, or suicidal ideation, indicating a stable overall outcome (see Supplementary material 2 Figures S3, S4, S6). Funnel plots for depression, anxiety and suicidal ideation showed significant asymmetry (see Supplementary material 2 Figures S12–S14). Egger’s test indicated a significant risk of publication bias in the pooled prevalence rates of depression, anxiety, and suicidal ideation (p < 0.05).
Discussion
This systematic review and meta-analysis included a total of 60 studies from 26 different countries, focusing on the mental disorders among YLWH. In general, the prevalence of depression, anxiety, suicidal ideation, lifetime suicidal ideation, suicidal attempts, lifetime suicidal attempts, PTSD, and ADHD was assessed. To our knowledge, this is the first systematic evaluation of mental disorders in YLWH globally.
The meta-analysis revealed that depression and anxiety are the predominant mental disorders among YLWH, with the pooled prevalence rates being 24.6% (95% CI: 21.1–28.2%) for depression and 17.0% (95% CI: 11.4–22.6%) for anxiety, respectively (71, 72). Compared to general young people, depression and anxiety are 2.34 and 2.62 times more prevalent in YLWH in the current study, respectively. Considering the large number of YLWH worldwide, depression and anxiety issues should be the major health priorities for this population. The greater prevalence of depression in YLWH could be attributed to several factors. The first is the release of monoamines and increased levels of cytokines that promote inflammation (73). Additionally, depression’s start is significantly linked to psychosocial stigma-related factors (74). Similarly, there is proof that stigma connected to HIV and anxiety are strongly correlated (75). Consistent with the reported rates of depression in the general young population, our meta-analysis found that depression is more prevalent among female YLWH than their male counterparts, and higher among older youth compared to their younger peers (76, 77). The gender disparity in depression prevalence may stem from differing societal expectations and moral standards for men and women, alongside varying degrees of social discrimination and psychological stress. Our study found that depression prevalence varied from 16.1 to 27.2%, while anxiety prevalence ranged from 14.0 to 32.6% across different continents. Instead of being only due to changes in geography, these disparities could also be ascribed to variations in social level, religious affiliation, and cultural diversity. The included studies use a variety of measurement tools to measure depression and anxiety, and most of these measurement tools had unclear sensitivity and accuracy. We therefore conducted subgroup analyses of depression and anxiety based on measurement tools. Surprisingly, the prevalence of depression and anxiety measured by different measurement tools and even the prevalence of depression measured using the same measurement tools but with different cut-off scores varied considerably. So it is important to use validated assessment methods carefully because doing otherwise can lead to inaccurate or misleading results (78).
While antiretroviral therapy offers considerable benefits, the issue of suicidality among HIV/AIDS patients continues to pose a significant public health challenge, especially in developing countries (79, 80). The meta-analysis showed that 16.8% of young people living with HIV experienced suicidal ideation, and 9.7% attempted suicide, rates significantly exceeding those in the general population (81). However, a recent review on suicidal ideation in Chinese adults with HIV found the incidence to be 30.6% (82). This may be because in many countries, adults and middle-aged individuals, who bear significant economic and family responsibilities, face high social pressures and are at greater risk of suicide. Our analysis of the available data revealed that 29.7% of young people living with HIV (YLWH) reported experiencing lifetime suicidal ideation, while 12.9% reported lifetime suicide attempts. Previous research indicates that both physiological factors (HIV infection status, low CD4 cell counts, opportunistic infections, adverse reactions to antiretroviral therapy) and psychosocial factors (depression, high stress, low social support, violence, discrimination exposure) significantly contribute to suicidality risk in individuals with HIV (83–85). Among YLWH, studies have shown a higher prevalence of opportunistic infections and a greater risk of stigma and discrimination (74, 86). Therefore, suicidality among YLWH should require urgent attention in terms of prevention and treatment.
This meta-analysis offers, to the best of our knowledge, the first global assessment of PTSD and ADHD among YLWH. Data from 8 studies were combined to evaluate the prevalence of PTSD in YLWH in the current meta-analysis. The prevalence of PTSD from the 2 studies was merged in a meta-analysis examining psychiatric disorders in HIV-infected individuals less than 19 years of age in sub-Saharan Africa (SSA), and the resuls was 3.0% (87), which is substantially lower than what we measured (10.5%). However, a different meta-analysis with adult HIV-infected patients as the research group found that the prevalence of PTSD was 2.40 times greater than ours (88). There is one rationale why this might be the case. According to a study conducted on HIV-infected patients, PTSD is linked to HIV infection duration (89). The fact that young people have had an HIV diagnosis for a shorter amount of time may thus account for this difference. Despite this, YLWH still has a much higher prevalence of PTSD than the general population (3.9%) (90) and other vulnerable groups, such as cancer patients (5.1%) (91). Our meta-analysis revealed that 5.0% of YLWH had ADHD, which was less than what was previously reported in kids and adolescents with HIV in the prior review (92). This may be a result of the beneficial effects of early ART on the developing brain (93), in comparison to the pre-ART era, the introduction of ART both prenatally and postnatally may have considerably reduced the rate of ADHD among YLWH.
Identifying several limitations in this meta-analysis is crucial. Firstly, because there were variations in the research populations, study designs, measurement tools, and their cutoff values, there was a considerable degree of heterogeneity among the included studies. Secondly, the majority of the prevalence of mental disorders found in this study was derived from research conducted in African nations, which may limit the applicability of our findings elsewhere. And more excellent research from other continents is anticipated to be available in the future, which will allow us to update our findings even further.
Conclusion
This systematic review and meta-analysis found a significantly higher prevalence of mental disorders among YLWH, highlighting the benefits of early screening and intervention, particularly for females. More high-quality longitudinal studies are required to explore the reasons behind the increased prevalence of mental disorders in this group. Additionally, research into improved screening, prevention, and intervention methods for these issues is necessary.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SZ: Writing – original draft, Writing – review & editing. FO: Writing – review & editing. WZ: Writing – review & editing. HY: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We are delighted to acknowledge all the authors from the included studies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1392872/full#supplementary-material
Abbreviations
YLWH, Young people living with HIV; WHO, World Health Organization; PTSD, Post-traumatic stress disorder; ADHD, Attention-deficit hyperactivity disorder; ART, Antiretroviral therapy; AHRQ, Agency for Healthcare Research and Quality list; PHQ-9, Patient Health Questionnaire-9; BDI, Beck Depression Inventory; CDI, Child Depression Inventory; PHQ-A, Patient Health Questionnaire for Adolescents; CES-D, Center for Epidemiologic Studies Depression Scale; MINI-KID, Mini International Neuropsychiatric Interview for Children and Adolescents; GAD-7, Generalized Anxiety Disorder-7; RCMAS, Revised Children’s Manifest Anxiety Scale; PC-PTSD, Primary care-PTSD screen; CPC, Child Post-Traumatic Stress Disorder Checklist; UCLA PTSD-RI, University of California Los Angeles PTSD Exposure questionnaire; SSA, Sub-Saharan Africa.
References
1. World Health Organization . Orientation Programme on Adolescent Health for Health-care Providers. (2006). Available at: https://iris.who.int/bitstream/handle/10665/42868/9241591269_Guide_eng.pdf?sequence=1 (Accessed 20 December 2023).
2. World Health Organization . Global HIV Programme. (2023). Available at: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/strategic-information/hiv-data-and-statistics (Accessed 24 December 2023).
3. UNICEF . Adolescent HIV prevention. (2023). Available at: https://data.unicef.org/topic/hivaids/adolescents-young-people/ (Accessed 24 December 2023).
4. Lofgren, SM, Bond, DJ, Nakasujja, N, and Boulware, DR. Burden of depression in outpatient HIV-infected adults in sub-Saharan Africa; systematic review and Meta-analysis. AIDS Behav. (2020) 24:1752–64. doi: 10.1007/s10461-019-02706-2
5. Verhey, R, Gibson, L, Brakarsh, J, Chibanda, D, and Seedat, S. Prevalence and correlates of probable post-traumatic stress disorder and common mental disorders in a population with a high prevalence of HIV in Zimbabwe. Eur J Psychotraumatol. (2018) 9:1536286. doi: 10.1080/20008198.2018.1536286
6. Pao, M, Lyon, M, D’Angelo, LJ, Schuman, WB, Tipnis, T, and Mrazek, DA. Psychiatric diagnoses in adolescents seropositive for the human immunodeficiency virus. Arch Pediatr Adolesc Med. (2000) 154:240–4. doi: 10.1001/archpedi.154.3.240
7. Woollett, N, Cluver, L, Bandeira, M, and Brahmbhatt, H. Identifying risks for mental health problems in HIV positive adolescents accessing HIV treatment in Johannesburg. J Child Adolesc Ment Health. (2017) 29:11–26. doi: 10.2989/17280583.2017.1283320
8. Haas, AD, Technau, KG, Pahad, S, Braithwaite, K, Madzivhandila, M, Sorour, G, et al. Mental health, substance use and viral suppression in adolescents receiving ART at a paediatric HIV clinic in South Africa. J Int AIDS Soc. (2020) 23:e25644. doi: 10.1002/jia2.25644
9. Satriawibawa, IW, Wati, K, Windiani, IG, Adnyana, IGA, Vedaswari, PD, and Sutawan, IB. Factors associated with anxiety in children and adolescents with HIV infection. HIV AIDS Rev. (2022) 21:137–43. doi: 10.5114/hivar.2022.115828
10. Chory, A, Callen, G, Nyandiko, W, Njoroge, T, Ashimosi, C, Aluoch, J, et al. A pilot study of a Mobile intervention to support mental health and adherence among adolescents living with HIV in Western Kenya. AIDS Behav. (2022) 26:232–42. doi: 10.1007/s10461-021-03376-9
11. Gaitho, D, Kumar, M, Wamalwa, D, Wambua, GN, and Nduati, R. Understanding mental health difficulties and associated psychosocial outcomes in adolescents in the HIV clinic at Kenyatta National Hospital. Kenya Ann Gen Psychiatry. (2018) 17:29. doi: 10.1186/s12991-018-0200-8
12. Mutumba, M, Musiime, V, Lepkwoski, JM, Harper, GW, Snow, RC, Resnicow, K, et al. Examining the relationship between psychological distress and adherence to anti-retroviral therapy among Ugandan adolescents living with HIV. AIDS Care. (2016) 28:807–15. doi: 10.1080/09540121.2015.1131966
13. Rosenstein, LD . ADHD as a potential risk factor in poor antiretroviral adherence rates in HIV: a brief narrative review and suggestions for future research. Neuropsychol Rev. (2021) 31:683–8. doi: 10.1007/s11065-021-09483-7
14. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
15. Rostom, A, Dubé, C, and Cranney, A. Celiac disease. Rockville (MD): Agency for Healthcare Research and Quality (US). (2004). Available at: https://www.ncbi.nlm.nih.gov/books/NBK35156/ (Accessed 26 May 2024).
16. Higgins, JPT, and Green, S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, (2011). Available at: https://training.cochrane.org/handbook (Accessed 26 May 2024).
17. Sohn, AH, Singtoroj, T, Chokephaibulkit, K, Lumbiganon, P, Hansudewechakul, R, Gani, YM, et al. Long-Term Post-Transition Outcomes of Adolescents and Young Adults Living With Perinatally and Non-perinatally Acquired HIV in Southeast Asia. J Adolesc Health. (2023) 72:471–9. doi: 10.1016/j.jadohealth.2022.10.021
18. Olashore, AA, Paruk, S, Akanni, OO, and Chiliza, B. Psychiatric disorders in adolescents living with HIV in Botswana. AIDS Res Ther. (2023) 20:2. doi: 10.1186/s12981-022-00490-z
19. Nguyen, N, Lovero, KL, Falcao, J, Brittain, K, Zerbe, A, Wilson, IB, et al. Mental health and ART adherence among adolescents living with HIV in Mozambique. AIDS Care. (2023) 35:182–90. doi: 10.1080/09540121.2022.2032574
20. Ndongo, FA, Kana, R, Nono, MT, Noah, JPYA, Ndzie, P, Tejiokem, MC, et al. Mental health troubles among Cameroonian adolescents perinatally infected with Human Immunodeficiency Virus. Rev Epidemiol Sante Publique. (2023) 71:101422. doi: 10.1016/j.respe.2022.101422
21. Mugo, C, Kohler, P, Kumar, M, Badia, J, Kibugi, J, Wamalwa, DC, et al. Effect of HIV stigma on depressive symptoms, treatment adherence, and viral suppression among youth with HIV. AIDS. (2023) 37:813–21. doi: 10.1097/QAD.0000000000003473
22. Gamassa, E, Steven, E, Mtei, R, and Kaaya, S. Prevalence of Depression and Suicidal Ideation and Associated Risk Factors in Adolescents Receiving Care and Treatment for Hiv/Aids at a Tertiary Health Facility in Kilimanjaro Region, Tanzania. Res Square. (2023) 28:2534893. doi: 10.21203/rs.3.rs-2534893/v1
23. Brooks, M, Burmen, B, Olashore, A, Gezmu, AM, Molebatsi, K, Tshume, O, et al. Symptoms of depression, anxiety, and thoughts of suicide/self-injury in adolescents and young adults living with HIV in Botswana. Afr J AIDS Res. (2023) 22:54–62. doi: 10.2989/16085906.2023.2186252
24. Arnold, EM, Yalch, MM, Christodoulou, J, Murphy, DA, Swendeman, D, Rotheram-Borus, MJ, et al. Rumination influences the relationship between trauma and depression over time among youth living with HIV. J Affect Disord. (2023) 322:9–14. doi: 10.1016/j.jad.2022.11.010
25. Di Gennaro, F, Marotta, C, Ramirez, L, Cardoso, H, Alamo, C, Cinturao, V, et al. High prevalence of mental health disorders in adolescents and youth living with HIV: an observational study from eight health services in Sofala Province, Mozambique. AIDS Patient Care STDs. (2022) 36:123–9. doi: 10.1089/apc.2022.0007
26. Chantaratin, S, Trimetha, K, Werarak, P, Lapphra, K, Maleesatharn, A, Rungmaitree, S, et al. Depression and anxiety in youth and young adults living with HIV: frequency and associated factors in Thai setting. J Int Assoc Phys AIDS Care. (2022) 21:23259582221101811. doi: 10.1177/23259582221101811
27. Nyongesa, MK, Mwangi, P, Kinuthia, M, Hassan, AS, Koot, HM, Cuijpers, P, et al. Prevalence, risk and protective indicators of common mental disorders among young people living with HIV compared to their uninfected peers from the Kenyan coast: a cross-sectional study. BMC Psychiatry. (2021) 21:1–17. doi: 10.1186/s12888-021-03079-4
28. Mugo, C, Seeh, D, Guthrie, B, Moreno, M, Kumar, M, John-Stewart, G, et al. Association of experienced and internalized stigma with self-disclosure of HIV status by youth living with HIV. AIDS Behav. (2021) 25:2084–93. doi: 10.1007/s10461-020-03137-0
29. Kohn, JN, Loop, MS, Kim-Chang, JJ, Garvie, PA, Sleasman, JW, Fischer, B, et al. Trajectories of depressive symptoms, neurocognitive function and viral suppression with antiretroviral therapy among youth with HIV over 36 months. J Acq Immune Deficiency Syndromes. (2021) 87:851–9. doi: 10.1097/QAI.0000000000002653
30. Girma, D, Assegid, S, and Gezahegn, Y. Depression and associated factors among HIV-positive youths attending antiretroviral therapy clinics in Jimma town, southwest Ethiopia. PLoS One. (2021) 16:e0244879. doi: 10.1371/journal.pone.0244879
31. Getaye, A, Cherie, N, Bazie, GW, and Gebremeskel, AT. Proportion of depression and its associated factors among youth HIV/AIDS clients attending ART clinic in Dessie town government health facilities, Northeast Ethiopia. J Multidisciplin Healthc. (2021) 14:197–205. doi: 10.2147/JMDH.S296849
32. Filiatreau, LM, Pettifor, A, Edwards, JK, Masilela, N, Twine, R, Xavier Gómez-Olivé, F, et al. Associations between key psychosocial stressors and viral suppression and retention in care among youth with HIV in rural South Africa. AIDS Behav. (2021) 25:2358–68. doi: 10.1007/s10461-021-03198-9
33. Aurpibul, L, Sophonphan, J, Malee, K, Kerr, SJ, Sun, LP, Ounchanum, P, et al. HIV-related enacted stigma and increase frequency of depressive symptoms among Thai and Cambodian adolescents and young adults with perinatal HIV. Int J STD AIDS. (2021) 32:246–56. doi: 10.1177/0956462420960602
34. Ashaba, S, Cooper-Vince, CE, Maling, S, Satinsky, EN, Baguma, C, Akena, D, et al. Childhood trauma, major depressive disorder, suicidality, and the modifying role of social support among adolescents living with HIV in rural Uganda. J Affect Disord Rep. (2021) 4:100094. doi: 10.1016/j.jadr.2021.100094
35. Adeyemo, S, Adeosun, II, Ogun, OC, Adewuya, A, David, AN, Adegbohun, AA, et al. Depression and suicidality among adolescents living with human immunodeficiency virus in Lagos, Nigeria. Child Adolesc Psychiatry Mental Health. (2020) 14:1–10. doi: 10.1186/s13034-020-00337-3
36. Buckley, J, Otwombe, K, Joyce, C, Leshabane, G, Hornschuh, S, Hlongwane, K, et al. Mental health of adolescents in the era of antiretroviral therapy: is there a difference between HIV-infected and uninfected youth in South Africa? J Adolesc Health. (2020) 67:76–83. doi: 10.1016/j.jadohealth.2020.01.010
37. Dyer, J, Wilson, K, Badia, J, Agot, K, Neary, J, Njuguna, I, et al. The psychosocial effects of the COVID-19 pandemic on youth living with HIV in Western Kenya. AIDS Behav. (2021) 25:68–72. doi: 10.1007/s10461-020-03005-x
38. Ekat, MH, Yotebieng, M, Leroy, V, Mpody, C, Diafouka, M, Loubaki, G, et al. Association between depressive symptoms and adherence among adolescents living with HIV in the Republic of Congo: a cross sectional study. Medicine. (2020) 99:606. doi: 10.1097/MD.0000000000021606
39. Cavazos-Rehg, P, Xu, C, Kasson, E, Byansi, W, Bahar, OS, and Ssewamala, FM. Social and economic equity and family cohesion as potential protective factors from depression among adolescents living with HIV in Uganda. AIDS Behav. (2020) 24:2546–54. doi: 10.1007/s10461-020-02812-6
40. Yarhere, IE, and Jaja, T. Beck Depression Inventory scores for children with some chronic diseases (Type I diabetes mellitus, Sickle cell anaemia, and AIDS) on management in University of Port Harcourt Teaching Hospital. Afric J Diabetes Med. (2020) 28
41. Agyemang, EO, Dapaah, JM, Osei, FA, Appiah, SCY, Mensah, NK, Odoom, SF, et al. Self-esteem assessment among adolescents living with HIV and seeking healthcare at Komfo Anokye Teaching Hospital-Kumasi, Ghana. J Int Assoc Providers AIDS Care. (2020) 19:2325958220976828. doi: 10.1177/2325958220976828
42. Kinyanda, E, Salisbury, TT, Levin, J, Nakasujja, N, Mpango, RS, Abbo, C, et al. Rates, types and co-occurrence of emotional and behavioural disorders among perinatally HIV-infected youth in Uganda: the CHAKA study. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:415–25. doi: 10.1007/s00127-019-01675-0
43. Kemigisha, E, Zanoni, B, Bruce, K, Menjivar, R, Kadengye, D, Atwine, D, et al. Prevalence of depressive symptoms and associated factors among adolescents living with HIV/AIDS in South Western Uganda. AIDS care. (2019) 31:1297. doi: 10.1080/09540121.2019.1566511
44. Abebe, H, Shumet, S, Nassir, Z, Agidew, M, and Abebaw, D. Prevalence of depressive symptoms and associated factors among HIV-positive youth attending ART follow-up in Addis Ababa, Ethiopia. AIDS Res Treat. (2019) 2019:4610458. doi: 10.1155/2019/4610458
45. Casale, M, Boyes, M, Pantelic, M, Toska, E, and Cluver, L. Suicidal thoughts and behaviour among South African adolescents living with HIV: Can social support buffer the impact of stigma? J Affect Disord. (2019) 245:82–90. doi: 10.1016/j.jad.2018.10.102
46. Zhou, E, Qiao, Z, Cheng, Y, Zhou, J, Wang, W, Zhao, M, et al. Factors associated with depression among HIV/AIDS children in China. Int J Mental Health Syst. (2019) 13:1–9. doi: 10.1186/s13033-019-0263-1
47. Wonde, M, Mulat, H, Birhanu, A, Biru, A, Kassew, T, and Shumet, S. The magnitude of suicidal ideation, attempts and associated factors of HIV positive youth attending ART follow ups at St. Paul’s hospital Millennium Medical College and St. Peter’s specialized hospital, Addis Ababa, Ethiopia, 2018. PloS one. (2019) 14:e0224371. doi: 10.1371/journal.pone.0224371
48. Coetzee, BJ, Loades, ME, Du Toit, S, and Kagee, A. Correlates of fatigue among South African adolescents living with HIV and receiving antiretroviral therapy. AIDS Behav. (2019) 23:602–8. doi: 10.1007/s10461-018-02384-6
49. Ramos, JV, Mmbaga, BT, Turner, EL, Rugalabamu, LL, Luhanga, S, Cunningham, CK, et al. Modality of primary HIV disclosure and association with mental health, stigma, and antiretroviral therapy adherence in Tanzanian youth living with HIV. AIDS Patient Care STDs. (2018) 32:31–7. doi: 10.1089/apc.2017.0196
50. Okawa, S, Mwanza Kabaghe, S, Mwiya, M, Kikuchi, K, Jimba, M, Kankasa, C, et al. Psychological well-being and adherence to antiretroviral therapy among adolescents living with HIV in Zambia. AIDS care. (2018) 30:634–42. doi: 10.1080/09540121.2018.1425364
51. West, N, Schwartz, S, Mudavanhu, M, Hanrahan, C, France, H, Nel, J, et al. Mental health in South African adolescents living with HIV. AIDS Care. (2019) 31:117–24. doi: 10.1080/09540121.2018.1533222
52. Earnshaw, VA, Kidman, RC, and Violari, A. Stigma, depression, and substance use problems among perinatally HIV-infected youth in South Africa. AIDS Behavior. (2018) 22:3892–6. doi: 10.1007/s10461-018-2201-7
53. Le Prevost, M, Arenas-Pinto, A, Melvin, D, Parrott, F, Foster, C, Ford, D, et al. Anxiety and depression symptoms in young people with perinatally acquired HIV and HIV affected young people in England. AIDS Care. (2018) 30:1040–9. doi: 10.1080/09540121.2018.1441972
54. Chenneville, T, Gabbidon, K, Lynn, C, and Rodriguez, C. Psychological factors related to resilience and vulnerability among youth with HIV in an integrated care setting. AIDS Care. (2018) 30:5–11. doi: 10.1080/09540121.2018.1488032
55. Bankole, KO, Bakare, MO, Edet, BE, Igwe, MN, Ewa, AU, Bankole, IA, et al. Psychological complications associated with HIV/AIDS infection among children in South-South Nigeria, sub-Saharan Africa. Cogent Med. (2017) 4:1372869. doi: 10.1080/2331205X.2017.1372869
56. Dow, DE, Turner, EL, Shayo, AM, Mmbaga, B, Cunningham, CK, and O’Donnell, K. Evaluating mental health difficulties and associated outcomes among HIV-positive adolescents in Tanzania. AIDS Care. (2016) 28:825–33. doi: 10.1080/09540121.2016.1139043
57. Smith Fawzi, MC, Ng, L, Kanyanganzi, F, Kirk, C, Bizimana, J, Cyamatare, F, et al. Mental health and antiretroviral adherence among youth living with HIV in Rwanda. Pediatrics. (2016) 138:3235. doi: 10.1542/peds.2015-3235
58. Funck-Brentano, I, Assoumou, L, Veber, F, Moshous, D, Frange, P, and Blanche, S. Resilience and life expectations of perinatally HIV-1 infected adolescents in France. Open AIDS J. (2016) 10:209. doi: 10.2174/1874613601610010209
59. Côté, J, Delmas, P, de Menezes Succi, RC, Galano, E, Auger, P, Sylvain, H, et al. Predictors and evolution of antiretroviral therapy adherence among perinatally HIV-infected adolescents in Brazil. J Adolesc Health. (2016) 59:305–410. doi: 10.1016/j.jadohealth.2016.05.004
60. Vreeman, RC, Scanlon, ML, Marete, I, Mwangi, A, Inui, TS, McAteer, CI, et al. Characteristics of HIV-infected adolescents enrolled in a disclosure intervention trial in western Kenya. AIDS Care. (2015) 27:6–17. doi: 10.1080/09540121.2015.1026307
61. Lewis, J, Abramowitz, S, Koenig, L, Chandwani, S, and Orban, L. Negative life events and depression in adolescents with HIV: a stress and coping analysis. AIDS Care. (2015) 27:1265–74. doi: 10.1080/09540121.2015.1050984
62. Brown, LK, Whiteley, L, Harper, GW, Nichols, S, and Nieves, A. Interventions A 086 PT for TAMTN for H. Psychological symptoms among 2032 youth living with HIV: a multisite study. AIDS Patient Care STDs. (2015) 29:212–9. doi: 10.1089/apc.2014.0113
63. Kim, MH, Mazenga, AC, Devandra, A, Ahmed, S, Kazembe, PN, Yu, X, et al. Prevalence of depression and validation of the Beck Depression Inventory-II and the Children’s Depression Inventory-Short amongst HIV-positive adolescents in Malawi. J Int AIDS Soc. (2014) 17:18965. doi: 10.7448/IAS.17.1.1896
64. Olashore, AA, Paruk, S, Tshume, O, and Chiliza, B. Depression and suicidal behavior among adolescents living with HIV in Botswana: a cross-sectional study. Child Adolesc Psychiatry Mental Health. (2022) 16:62. doi: 10.1186/s13034-022-00492-9
65. Namuli, JD, Nalugya, JS, Bangirana, P, and Nakimuli-Mpungu, E. Prevalence and factors associated with suicidal ideation among children and adolescents attending a pediatric HIV clinic in Uganda. Front Sociol. (2021) 6:656739. doi: 10.3389/fsoc.2021.656739
66. Rukundo, GZ, Mpango, RS, Ssembajjwe, W, Gadow, KD, Patel, V, and Kinyanda, E. Prevalence and risk factors for youth suicidality among perinatally infected youths living with HIV/AIDS in Uganda: the CHAKA study. Child Adolesc Psychiatry Mental Health. (2020) 14:1–9. doi: 10.1186/s13034-020-00348-0
67. López, J, Shacham, E, and Brown, T. Suicidal ideation persists among individuals engaged in HIV care in the era of antiretroviral therapy. AIDS Behavior. (2018) 22:800–5. doi: 10.1007/s10461-016-1666-5
68. Ng, LC, Kirk, CM, Kanyanganzi, F, Fawzi, MCS, Sezibera, V, Shema, E, et al. Risk and protective factors for suicidal ideation and behaviour in Rwandan children. Br J Psychiatry. (2015) 207:262–8. doi: 10.1192/bjp.bp.114.154591
69. Zhou, Y, Tang, K, Lu, H, Chen, H, Xie, H, Li, Z, et al. Behavioral and emotional difficulties and HIV treatment outcomes among HIV-infected children in rural southwestern China. Child Adolesc Psychiatry Mental Health. (2023) 17:1–10. doi: 10.1186/s13034-023-00601-2
70. Gentz, SG, Calonge Romano, I, Martínez-Arias, R, and Ruiz-Casares, M. Predictors of mental health problems in adolescents living with HIV in Namibia. Child Adolesc Mental Health. (2017) 22:179–85. doi: 10.1111/camh.12247
71. Balázs, J, Miklósi, M, Keresztény, A, Hoven, CW, Carli, V, Wasserman, C, et al. Adolescent subthreshold-depression and anxiety: psychopathology, functional impairment and increased suicide risk. J Child Psychol Psychiatry. (2013) 54:670–7. doi: 10.1111/jcpp.12016
72. Polanczyk, GV, Salum, GA, Sugaya, LS, Caye, A, and Rohde, LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. (2015) 56:345–65. doi: 10.1111/jcpp.12381
73. Rivera-Rivera, Y, Vázquez-Santiago, FJ, Albino, E, Sánchez, MDC, and Rivera-Amill, V. Impact of depression and inflammation on the progression of HIV disease. J Clin Cell Immunol. (2016) 7:423. doi: 10.4172/2155-9899.1000423
74. Kimera, E, Vindevogel, S, Reynaert, D, Justice, KM, Rubaihayo, J, De Maeyer, J, et al. Experiences and effects of HIV-related stigma among youth living with HIV/AIDS in Western Uganda: a photovoice study. PLoS One. (2020) 15:e0232359. doi: 10.1371/journal.pone.0232359
75. Durteste, M, Kyselyova, G, Volokha, A, Judd, A, Thorne, C, Cortina-Borja, M, et al. Anxiety symptoms and felt stigma among young people living with perinatally or behaviourally-acquired HIV in Ukraine: a cross-sectional survey. PLoS One. (2019) 14:e0210412. doi: 10.1371/journal.pone.0210412
76. Khesht-Masjedi, MF, Shokrgozar, S, Abdollahi, E, Golshahi, M, and Sharif-Ghaziani, Z. Comparing depressive symptoms in teenage boys and girls. J Family Med Prim Care. (2017) 6:775–9. doi: 10.4103/jfmpc.jfmpc_129_17
77. Piccinelli, M, and Wilkinson, G. Gender differences in depression: critical review. Br J Psychiatry. (2000) 177:486–92. doi: 10.1192/bjp.177.6.486
78. Vreeman, RC, McCoy, BM, and Lee, S. Mental health challenges among adolescents living with HIV. J Int AIDS Soc. (2017) 20:21497. doi: 10.7448/IAS.20.4.21497
79. Carrico, AW . Elevated suicide rate among HIV-positive persons despite benefits of antiretroviral therapy: implications for a stress and coping model of suicide. Am J Psychiatry. (2010) 167:117–9. doi: 10.1176/appi.ajp.2009.09111565
80. Schlebusch, L, and Govender, RD. Elevated risk of suicidal ideation in HIV-positive persons. Depress Res Treat. (2015) 2015:609172:1–6. doi: 10.1155/2015/609172
81. Cao, XL, Zhong, BL, Xiang, YT, Ungvari, GS, Lai, KYC, Chiu, HFK, et al. Prevalence of suicidal ideation and suicide attempts in the general population of China: a meta-analysis. Int J Psychiatry Med. (2015) 49:296–308. doi: 10.1177/0091217415589306
82. Li, S, Yu, S, Yang, Q, Yin, J, Zhu, H, Jiang, Y, et al. Prevalence of suicide ideation among HIV/AIDS patients in China: a systematic review and meta-analysis. Front Public Health. (2023) 11:1082521. doi: 10.3389/fpubh.2023.1082521
83. Tsai, YT, K M, SP, Ku, HC, Wu, YL, and Ko, NY. Global overview of suicidal behavior and associated risk factors among people living with human immunodeficiency virus: a scoping review. PLoS One. (2023) 18:e0269489. doi: 10.1371/journal.pone.0269489
84. Kinyanda, E, Hoskins, S, Nakku, J, Nawaz, S, and Patel, V. The prevalence and characteristics of suicidality in HIV/AIDS as seen in an African population in Entebbe district, Uganda. BMC Psychiatry. (2012) 12:63. doi: 10.1186/1471-244X-12-63
85. Keiser, O, Spoerri, A, Brinkhof, MWG, Hasse, B, Gayet-Ageron, A, Tissot, F, et al. Suicide in HIV-infected individuals and the general population in Switzerland, 1988-2008. Am J Psychiatry. (2010) 167:143–50. doi: 10.1176/appi.ajp.2009.09050651
86. Tesfaw, G, Ayano, G, Awoke, T, Assefa, D, Birhanu, Z, Miheretie, G, et al. Prevalence and correlates of depression and anxiety among patients with HIV on-follow up at alert hospital, Addis Ababa, Ethiopia. BMC Psychiatry. (2016) 16:368. doi: 10.1186/s12888-016-1037-9
87. Olashore, AA, Paruk, S, Akanni, OO, Tomita, A, and Chiliza, B. Psychiatric disorders in adolescents living with HIV and association with antiretroviral therapy adherence in sub-Saharan Africa: a systematic review and Meta-analysis. AIDS Behav. (2021) 25:1711–28. doi: 10.1007/s10461-020-03100-z
88. Ayano, G, Duko, B, and Bedaso, A. The prevalence of post-traumatic stress disorder among people living with HIV/AIDS: a systematic review and Meta-analysis. Psychiatry Q. (2020) 91:1317–32. doi: 10.1007/s11126-020-09849-9
89. Rzeszutek, M, Oniszczenko, W, Żebrowska, M, and Firląg-Burkacka, E. HIV infection duration, social support and the level of trauma symptoms in a sample of HIV-positive polish individuals. AIDS Care. (2015) 27:363–9. doi: 10.1080/09540121.2014.963018
90. Koenen, KC, Ratanatharathorn, A, Ng, L, McLaughlin, KA, Bromet, EJ, Stein, DJ, et al. Posttraumatic stress disorder in the world mental health surveys. Psychol Med. (2017) 47:2260–74. doi: 10.1017/S0033291717000708
91. Siqveland, J, Hussain, A, Lindstrøm, JC, Ruud, T, and Hauff, E. Prevalence of posttraumatic stress disorder in persons with chronic pain: a meta-analysis. Front Psych. (2017) 8:164. doi: 10.3389/fpsyt.2017.00164
92. Scharko, AM . DSM psychiatric disorders in the context of pediatric HIV/AIDS. AIDS Care. (2006) 18:441–5. doi: 10.1080/09540120500213487
Keywords: young people, HIV, depression, anxiety, mental disorders, meta-analysis
Citation: Zhan S, Ouyang F, Zhai W and Yang H (2024) Prevalence of mental disorders among young people living with HIV: a systematic review and meta-analysis. Front. Public Health. 12:1392872. doi: 10.3389/fpubh.2024.1392872
Edited by:
Getinet Ayano, Curtin University, AustraliaReviewed by:
Emmanuel Kumah, University of Education, Winneba, GhanaSiaw Leng Chan, Universiti Putra Malaysia Bintulu Sarawak Campus, Malaysia
Copyright © 2024 Zhan, Ouyang, Zhai and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haitao Yang, eWh0QGpzY2RjLmNu
 Shenao Zhan
Shenao Zhan Fei Ouyang
Fei Ouyang Wenjing Zhai
Wenjing Zhai Haitao Yang1,2*
Haitao Yang1,2*