- 1The Third Affiliated Hospital of Zhengzhou University, Zhengzhou, China
- 2School of Nursing and Health, Zhengzhou University, Zhengzhou, China
Aim: This study aims to assess the extent of social alienation in patients undergoing peritoneal dialysis and examine how personal mastery and perceived social support mediate the association between emotional intelligence and social alienation in this patient population.
Methods: This study adopts a cross-sectional survey design. A total of 192 patients were recruited from a tertiary hospital located in Henan Province, China, using a convenience sampling method. We have developed a structural equation model to investigate the mediating influence of personal mastery and perceived social support on the emotional intelligence and social alienation of patients undergoing Peritoneal dialysis.
Results: Peritoneal patients exhibited an social alienation score of 42.01 ± 3.15. Elevated EI levels (coefficient = −0.616, p < 0.001) were significantly correlated with reduced social alienation. The mediation model demonstrated that personal mastery and perceived social support fully mediated the impact of emotional intelligence on social alienation.
Conclusion: The social alienation of peritoneal dialysis patients is serious, and healthcare professionals should pay attention to patients’ social alienation, improve patients’ emotional intelligence through relevant interventions, increase personal mastery and perceived social support, and finally reduce social alienation.
Introduction
Chronic kidney disease (CKD) is a worldwide public health concern, affecting approximately 13.4% of the global population (1). Patients with chronic kidney disease face a threefold higher risk of heart failure and an increased susceptibility to urinary tract infections, gastrointestinal bleeding, hip fractures, and other related comorbidities (2). These complications significantly diminish patients’ quality of life. Progressive deterioration of kidney function ultimately leads to the development of end-stage renal disease (ESRD), necessitating renal replacement therapy for survival. Research indicates a projected increase in the number of patients requiring renal replacement therapy, expected to rise from 2,455,000 in 2016 to 5,439,000 by 2030 (3).
Peritoneal dialysis, as a modality of renal replacement therapy, has gained acceptance among patients and is utilized in various countries and regions due to its attributes, including the preservation of residual renal function, the option for home-based administration, and cost-effectiveness (4). Globally, 10–20% of patients are currently undergoing peritoneal dialysis treatment (5). Continuous Ambulatory Peritoneal Dialysis (CAPD) refers to patients exchanging dialysate 3–5 times per day, with each exchange volume of 1.5–2 L. Dialysate is left in the peritoneal cavity for 4–6 h/time during the daytime, and 10–12 h during the night. CAPD is the most dominant peritoneal dialysis modality, accounting for 90% of PD patients (6).
Regrettably, Dialysis fluid exchange at specific times and places restricts patients’ travel and the irreversible aggravation of their psychological burden by their kidneys, leading to the prominence of the phenomenon of “social alienation” (SA), such as peritoneal dialysis patients’ active avoidance of social interaction and the feeling of being alienated by others (7). SA is an objective phenomenon in which an individual is detached from social relationships, accompanied by emotional experiences such as loneliness and indifference, as well as avoidance and rejection of social activities (8). Qing-Er et al. (9) conducted a questionnaire survey involving 300 peritoneal dialysis patients, revealing that 70% of them exhibited deficits in social functioning. Tao Weiwei et al. (10) discovered that, following dialysis, 36.3% of patients experienced reduced interaction with family and community members, rarely engaging in group activities. Moreover, 14.6% of patients remained entirely homebound, with this figure escalating to 84.93% in rural regions. Cuevas-Budhart et al. (11) conducted in-depth interviews with 29 peritoneal dialysis patients across 13 hospitals in Mexico. Their findings indicated that patients’ experiences of family isolation and socioeconomic difficulties led to somatization of emotions, resulting in manifestations of sadness, anxiety, loneliness, and social abandonment.
The SA threatens peritoneal dialysis patients’ physical and mental health. Research has demonstrated that SA induces hypofunction of the hypothalamic–pituitary–adrenal (HPA) axis, subjecting patients to a pro-inflammatory milieu, thus exacerbating the inflammatory aspects of diseases like atherosclerosis, thereby becoming a significant risk factor for cardiovascular disease (11, 12). Furthermore, severe SA exhibits a substantial association with rapid renal failure in patients, serving as a prognostic indicator for the deterioration of renal function and the acceleration of disease progression (13).
Emotional intelligence (EI) is the ability of an individual to recognize and control his or her own emotions and those of others, and to be able to use emotions correctly to deal with and solve problems (14). Previous studies have found a correlation between EI and SA (15), enhancing emotional intelligence and promoting positive emotional expression in patients can help expand social networks and restore social functioning (16). However, how EI affects SA remains a black box that needs to be explored in further research. Understanding the mechanisms of influence will help healthcare professionals to develop targeted interventions to alleviate social alienation in peritoneal dialysis patients.
According to the Cascading Model, the association between EI and behavioral performance is not straightforward; instead, it is influenced by intervening variables (17). Consequently, it is reasonable to hypothesize the presence of mediating variables rather than direct mediators linking EI to SA. The Neurocognitive Processing Model of Emotional Intelligence suggests that emotional intelligence affects social relationships in a way that requires individuals to re-identify and increase their confidence, and that the effectiveness of emotional intelligence relies heavily on reliable feedback from the surrounding environment (18).
Personal mastery is the degree to which an individual perceives control over his or her life and surroundings, and reflects the patient’s self-confidence in life and disease management (19). Furthermore, mentioning the level of EI has been shown to enhance patient self-confidence and elevate self-efficacy, a pivotal factor influencing the personal master (20, 21). It was found that patients with a high personal mastery were more inclined to respond to changes in things with an open and inclusive mindset, actively engage in social interactions, and feel less SA during stressful situations (22, 23). Therefore, this study proposes the hypothesis that EI may improve SA by enhancing patients’ personal mastery.
Perceived social support is an individual perceives or appreciates material or emotional support from the outside world, which reflects the emotional response of the surrounding environment to the patient.
Emotional intelligence was positively correlated with perceived social support, with individuals with high EI subjectively perceiving more social support and utilizing it (24). According to the WHITE heuristic cognitive model of the cognitive theory of emotion, patients in a state of somatic vulnerability tend to actively detach themselves from social activities and persist in negative emotions if the perceived level of social support is low (25). Above all, this study again hypothesizes that EI influences the SA process in which perceived social support plays an important role.
To date, despite some studies examining the connections among EI, personal mastery, perceived social support, and SA, the precise nature of their interrelationships remains ambiguous. Consequently, this study seeks to explore the mediating functions of personal mastery and perceived social support in the relationship between EI and SA among peritoneal dialysis patients.
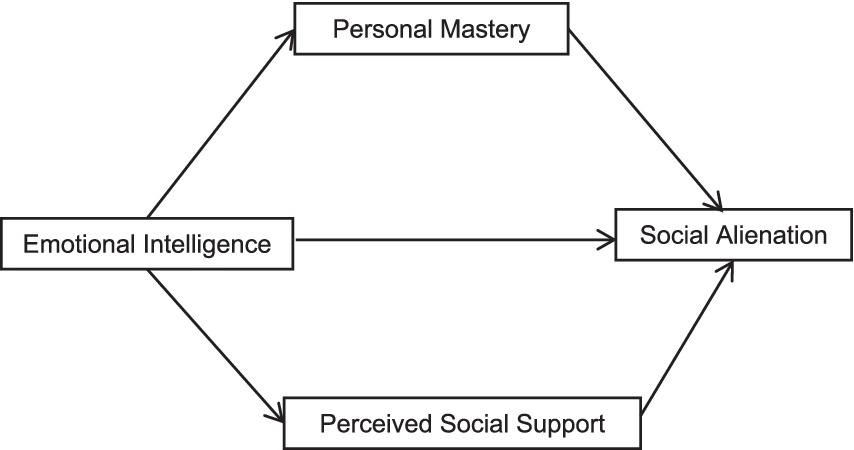
This endeavor aims to establish a theoretical foundation for intervention strategies aimed at mitigating social alienation within this patient population. Therefore, we developed a mediation model (see Figure 1) to explore the effects and mediating mechanisms of EI on SA in peritoneal dialysis patients, which outlines the hypotheses that (1) EI may affect SA in peritoneal dialysis patients (2) personal mastery and perceived social support mediate EI and SA in peritoneal dialysis patients.
Methods
Participants
This study was approved by the author’s university ethics review board and adhered to the principles outlined in the Declaration of Helsinki. This study employed a cross-sectional survey design, and it included peritoneal dialysis patients who met the predetermined inclusion and exclusion criteria. These patients were recruited from the Department of Nephrology at the First Affiliated Hospital of Zhengzhou University between December 2022 and March 2023, utilizing a convenience sampling approach. Inclusion criteria encompassed (a) undergoing peritoneal dialysis more than 1 month; (b) aged ≥18 years; (c) exhibiting stable vital signs; (d) ability to read and understand Chinese language; (e) willing to provide informed consent for active participation in the study.
Exclusion criteria comprised participants who underwent a change in their renal replacement therapy, including transitioning to hemodialysis or receiving a renal transplantation. A total of 202 questionnaires were distributed between December 2022 and March 2023. After eliminating invalid questionnaires, 192 responses were deemed eligible for inclusion.
Sample size
To ascertain the appropriate sample size, the researcher considered the guideline that the sample size for multiple linear regression analysis should be at least 5–10 times the number of study variables (26). Given the presence of 26 study variables, the sample size was calculated as 7 times this number, resulting in a preliminary sample size of 182. Additionally, to account for potential invalid questionnaires (estimated at 10%), the final sample size was determined to be 202. The study encompassed 202 participants, from whom 192 valid questionnaires were collected, resulting in an effective recovery rate of 95.0%. This high participation rate bolstered the study’s statistical power and ensured the accuracy of its findings.
Measures
General information about the patient
We employed a self-administered general information questionnaire to gather pertinent demographic data from the participants. This questionnaire comprised 13 items, encompassing gender, age, marital status, education, occupation, monthly family income (yuan), methods of medical expense payment, living arrangements, time of disease diagnosis (year), duration on dialysis (year), underlying disease etiology, comorbidity count, and biochemical values for calcium, phosphorus, urea nitrogen, and blood creatinine (to be filled out by the researcher after reviewing medical records).
Wong Law Emotional Intelligence Scale Chinese version (WLEIS-C)
The Wong Law Emotional Intelligence Scale (WLEIS) was developed by Wong and Kenneth in 2002 based on Gross’s theoretical model of emotion regulation (27). Later, Chinese scholars Yifei (28) revised the scale into a Chinese version. The scale comprises four dimensions: self-emotional assessment, emotional assessment of others, emotional control, and emotional use, featuring 16 items. This scale employs a 7-point Likert scale, with responses ranging from “Strongly Disagree” to “Strongly Agree,” yielding a total score between 0 and 96. A higher score indicates a higher level of EI. The WLEIS-C has been validated in a Chinese adult population, and the Cronbach’s alpha coefficient for this scale is 0.89, which is highly reliable.
General Alienation Scale Chinese version (GAS-C)
The General Alienation Scale (GAS) was developed by Safipour et al. (29) in 1977, and translated and revised into Chinese by Wu Shuang et al. (30). The GAS assesses feelings of alienation concerning personal roles, uncertainty regarding the significance of engagement in activities, and perceived alienation from others. It comprises 15 items organized into four dimensions: alienation from others, skepticism, self-alienation, and meaninglessness. Responses are recorded on a 4-point Likert scale, with each item ranging from 1 to 4, anchored by “strongly disagree” and “strongly agree.” Items 2, 5, and 13 are reverse-scored. The total score ranges from 15 to 60 points, with higher scores indicating a greater severity of SA. The Cronbach’s coefficient for GAS-C applied to peritoneal dialysis patients was 0.902, indicating acceptable reliability (31).
Personal Mastery Scale Chinese version (PMS-C)
Personal Mastery Scale was developed by Pearlin and Schooler (32), and translated into Chinese by Yu Yibing (33). The PMS assesses an individual’s sense of control over life events’ outcomes. This scale comprises seven items and employs a 5-point Likert scale, with each item scored from 1 (“not at all”) to 5 (“very much”). The total score ranges from 7 to 35 points, with higher scores denoting a stronger perception of individual control. PMS-C has been validated in Chinese peritoneal dialysis patients with reliable reliability (34).
Perceived Social Support Scale Chinese version (PSSS-C)
Perceived Social Support Scale was developed by Chinese scholars Qianjin (35). The PSSS assesses an individual’s self-awareness and their perceived level of social support. This scale comprises three dimensions: family support, friend support, and support from others, totaling 12 items. Responses are collected on a 7-point Likert scale, with each item spanning from “Strongly Disagree” to “Strongly Agree.” The total score ranges from 12 to 84 points, with higher scores signifying greater perceived social support. A higher score reflects an elevated level of social support comprehension. The scale exhibits strong reliability, as indicated by a Cronbach’s alpha coefficient for this scale applied to Chinese peritoneal dialysis patients of 0.880 (36).
Statistical analyses
The SPSS 25.0 and Amos 24.0 software were used for data entry and analysis. Continuous variables following a normal distribution were summarized using mean (M) and standard deviation (SD), and differences between groups were assessed via independent samples t-tests. Categorical variables were described using counts and percentages, and group differences were evaluated using chi-square (χ2) tests. Two independent samples t-tests and one-way ANOVA were employed to compare the SA scores of peritoneal dialysis patients with differing characteristics. Multiple stepwise regression analyses were conducted to identify significant predictors of social alienation in peritoneal dialysis patients. Additionally, Pearson correlation analysis was used to examine the relationships between patients’ demographic information, EI, personal mastery, perceived social support, and SA. Multiple linear regression analyses were performed to identify significant predictors of SA in peritoneal dialysis patients. Finally, structural equation models were developed using Amos 24.0, and mediation model testing was carried out utilizing the Bootstrap method, with 2,000 resampling iterations and a two-sided significance level of α = 0.05.
The researchers checked the collected data one by one, and entries with more than 20% missing items were deleted. Two researchers entered the data separately and then exchanged the results to ensure that the data were correct.
Results
Comparison of SA scores in peritoneal dialysis patients with different characteristics
Among the 192 patients, 98 were male and 94 were female. The mean age of the patients was (42.93 ± 12.64) years, calcium was (2.30 ± 0.39) mmol/L, phosphorus was (2.05 ± 0.52) mmol/L, urea nitrogen was (26.23 ± 6.67) mmol/L, and blood creatinine was (763.66 ± 345.05) μmol/L. Other specific data are shown in Table 1.
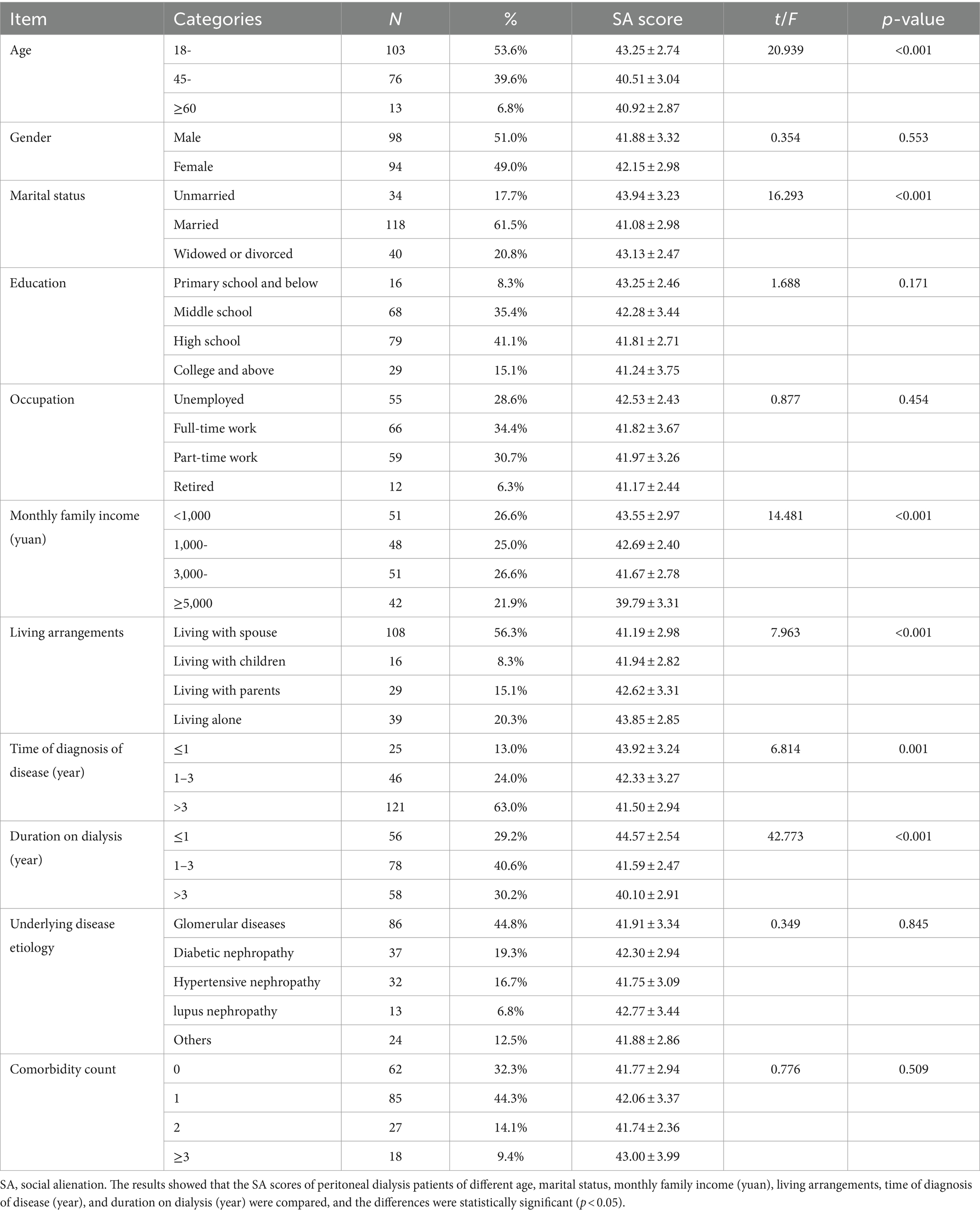
Table 1. Comparison of social alienation scores in peritoneal dialysis patients with different characteristics (n = 192, ±S).
Correlation analysis of EI, personal mastery, perceived social support and SA in peritoneal dialysis patients
As shown in Table 2, the total SA score of peritoneal dialysis patients was negatively correlated with the total EI score (r = −0.616, p < 0.001), with the total Personal Mastery score (r = −0.661, p < 0.001), and also with the Perceived Social Support score (r = −0.696, p < 0.001).
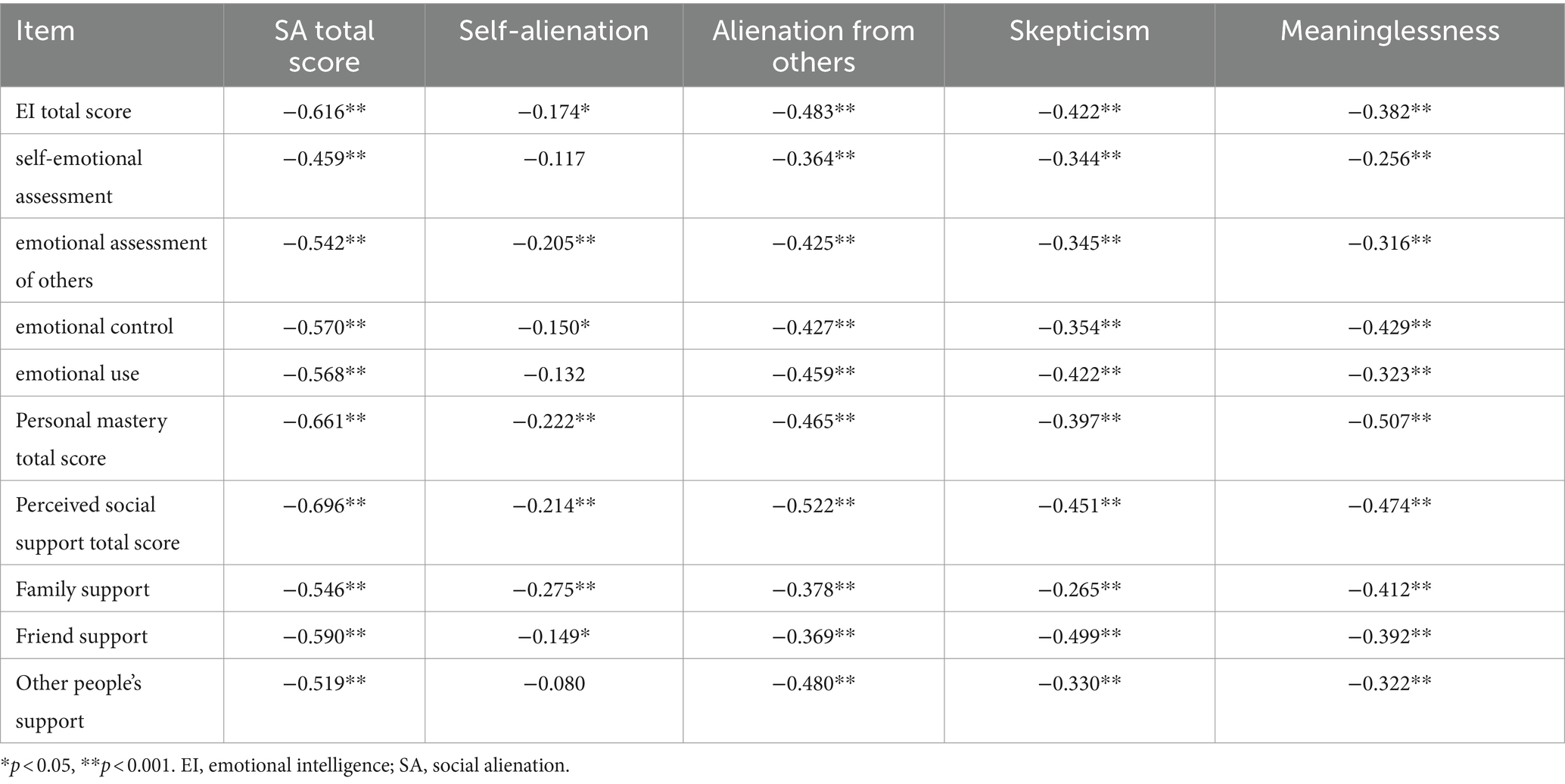
Table 2. Correlation analysis of EI, personal mastery, perceived social support and SA in peritoneal dialysis patients.
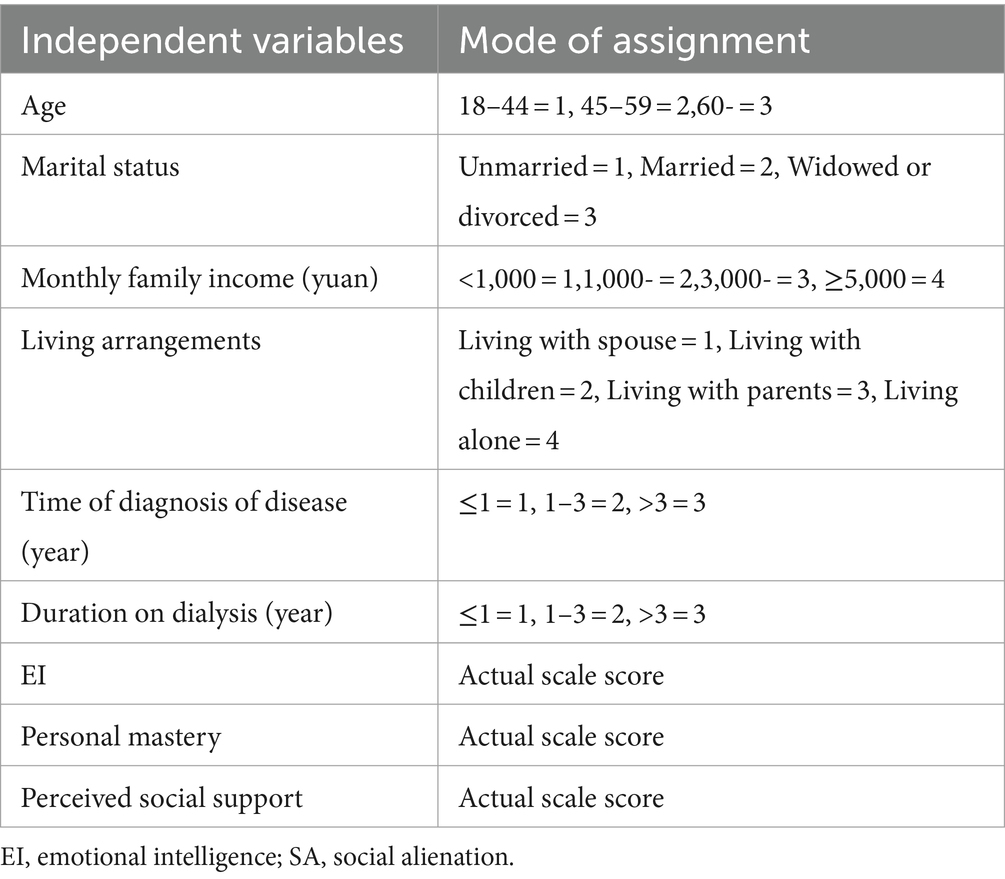
Multiple linear regression analyses of SA
The SA score was used as the dependent variable. Age, marital status, monthly family income (yuan), living arrangements, time of diagnosis of disease (year), and duration on dialysis (year), EI, personal mastery, and perceived social support were used as the independent variables, and the values assigned to the independent variables are shown in Table 3. The results showed that age, duration on dialysis (year), EI, personal mastery, and perceived social support were influential factors leading to SA in peritoneal dialysis patients (all p < 0.05), explaining a total of 66.1% of the total variance, as detailed in Table 4.

Table 4. Multiple linear regression analysis of factors influencing social alienation in peritoneal dialysis patients (n = 192).
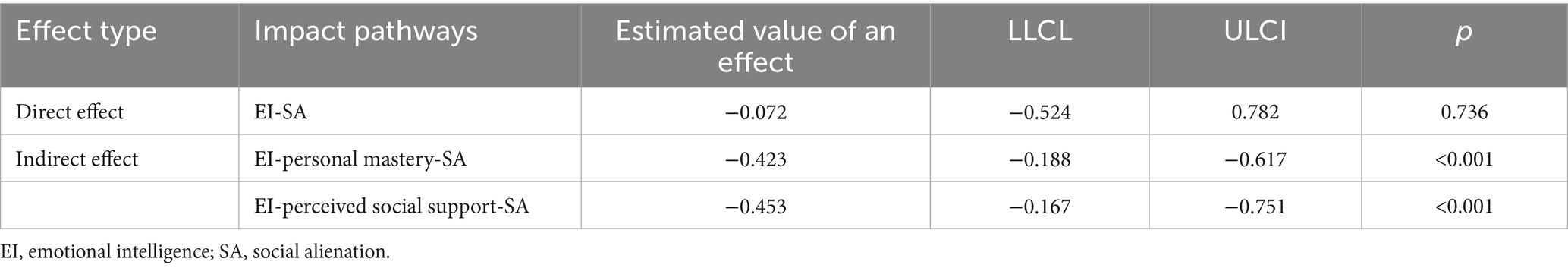
A model test of the relationship between EI, personal mastery, perceived social support and SA in peritoneal dialysis patients
A structural equation model was constructed to test the relationship between EI, Personal Mastery, Perceived Social Support and SA in peritoneal dialysis patients. The model fit indices were calculated using great likelihood estimation: χ2/df = 1.973(<3), CFI = 0.931(>0.9), GFI = 0. 902(>0.9), IFI = 0.933(>0.9), TLI = 0.909(>0.9), and RMSEA = 0.060(<0.08). The peritoneal dialysis patients’ structural equation models for EI, Personal Mastery, Perceived Social Support and SA are shown in Figure 2.
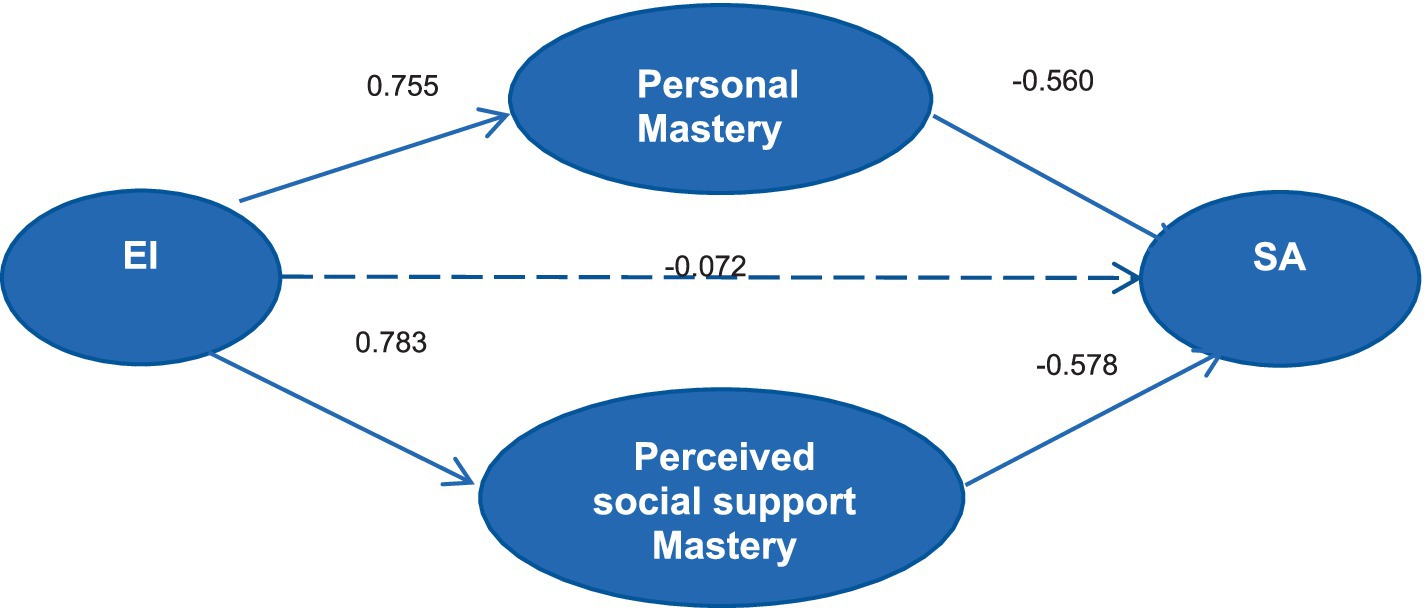
Figure 2. Structural equation modeling of peritoneal dialysis patients’ EI, personal mastery, perceived social support and SA. EI, emotional intelligence; SA, social alienation.
The results showed that the indirect effect of EI on SA was −0.876, with 95% confidence interval excluding 0, so the indirect effect of EI on SA was established, and since the direct effect of EI on SA was not significant and was not included in the model, the personal mastery and the perceives social support played a fully mediating role in EI and SA at this time. The mediating effect value of personal mastery was −0.423, accounting for 48.29% of the total mediating effect, and the mediating effect value of perceived social support was −0.453, accounting for 51.71% of the total mediating effect. The analysis of effects is shown in Table 5.
Discussion
Social alienation (SA) represents an inescapable challenge faced by peritoneal dialysis patients, profoundly impacting their mental well-being. Consequently, it is imperative to scrutinize the determinants of SA and to formulate tailored intervention strategies. In this investigation, the SA score among peritoneal dialysis patients averaged 42.01 ± 3.15, indicating a notably elevated level compared to the scale’s median total score of 37.50. These findings align closely with the scores reported by Xiaofang et al. (37) for lung cancer patients, though they slightly surpass scores observed in stroke patients (38). Several factors contribute to this discrepancy. Firstly, Zhao Cuicui (38) study encompassed a substantial proportion of older adult patients, the cognitive and physical functions of the older adult population are in a stage of decline, which, with increasing age, causes them to be socially inactive and thus aggravates SA. While this study predominantly enrolled young and middle-aged individuals who shoulder diverse family and occupational responsibilities, thus experiencing heightened demands for social engagement (39). Furthermore, the social role of supporting the older adult and caring for children compounds the burdens borne by these patients. Additionally, influenced by traditional Chinese cultural norms, individuals frequently refrain from sharing the impact of their illness with others, believing that such vulnerability does not align with societal expectations. This restraint fosters heightened anxiety, feelings of powerlessness, and a sense of detachment.
Simultaneously, our findings underscore the significance of age and duration on dialysis as pivotal determinants of SA in peritoneal dialysis patients. Surprisingly, our study revealed elevated SA scores among younger patients, a trend contrary to the findings of several previous investigations (40, 41). Notably, dialysis-related complications manifest as discernible alterations in patients’ physical appearance, encompassing generalized edema (42), melanosis (43) and characteristic hyperparathyroidism (44), etc. These conspicuous disease-related attributes are prone to create unfavorable impressions on others, further exacerbated by societal misconceptions and potential instances of social discrimination, thereby inducing psychological distress among patients (44, 45). Younger patients, in particular, grapple with the pronounced impact of these appearance-related changes, which can lead to challenges in pursuing marriage, forming new social connections, and realizing their socialization aspirations (46). Moreover, younger patients often exhibit reticence in sharing their emotions and experiences, ultimately isolating themselves from active engagement in social activities, thus fostering SA (47).
Furthermore, the study results indicate that peritoneal dialysis patients with a dialysis vintage of less than 1 year exhibited higher scores on social alienation, aligning with the findings of Xiaofang et al. (37). Peritoneal dialysis necessitates multiple daily fluid exchanges, meticulous monitoring of fluid balance, and the endurance of complications like pruritus and sleep disturbances (48, 49). For patients with a short dialysis history, striking a swift equilibrium between demanding self-care regimens and their pre-existing work commitments poses a formidable challenge. For patients who have been on peritoneal dialysis for a longer period of time, they have had a rich experience with nephrological care, better adapted to dialysis treatments, and have found the right place in their lives for dialysis, and therefore are less concerned about feeling alienated (50). Consequently, confronted with the stressors of dialysis, these patients often struggle to adapt to and redefine their roles, harboring numerous anxieties and reservations about their treatment. The amplification of psychological symptoms exacerbates their inclination toward social avoidance and SA (51). As a result, healthcare practitioners should direct their attention toward younger patients with shorter dialysis histories, proactively monitoring their emotional shifts. Collaborative interventions, such as patient support associations, can be instrumental in fostering positive emotional experiences, thereby establishing stable social bonds and mitigating their degree of social alienation.
The study’s findings reveal a negative association between higher levels of EI and lower levels of SA among peritoneal dialysis patients. These results align with previous research and contribute to a deeper understanding of the underlying mechanisms (52). Individuals with elevated EI exhibit a propensity to mitigate the impact of stress within their social environment through positive coping strategies, such as cognitive reappraisal. This serves as a protective factor against SA, in accordance with the stress buffer model (53). During this process, individuals tend to refrain from negative emotional expressions (self-containment and avoidance), increase positive emotional experiences, bolster resource development when facing stressful circumstances, and fulfill the prerequisites for social participation. These dynamics align with the extended construction theory (54). It was found that one feature of EI - affective differentiation – neutralizes neural responses to social rejection (i.e., dACC and forebrain insulae) (55), and from this perspective, EI creates conditions for patients to initiate social interactions. These findings lay the groundwork for further exploration of the interplay between personal mastery, perceived social support, EI, and SA among peritoneal dialysis patients.
Our study reveals that personal mastery acts as a complete mediator between EI and SA in peritoneal dialysis patients. According to the theory of limited self-control, self-control resources are finite, allowing individuals only short-term exertion of self-control. Externally stressful situations deplete these resources, diminishing self-control, and potentially resulting in emotional regulation failures (56). Peritoneal dialysis patients, grappling with the enduring burden of lifelong dialysis, job transitions, and life adjustments, often experience a significant erosion of self-worth, which profoundly affects their personal mastery. Moreover, personal mastery is cultivated through continuous social interactions. EI emerges from the amalgamation of self-cognitive processes and emotional management (57). In the realm of emotion regulation and control, patients employ self-beneficial coping strategies, facilitating the transformation of negative emotions into positive ones through cognitive reappraisal. The sustenance of positive emotions fosters self-management confidence, life optimism, and an ensuing personal mastery. Patients possessing high personal mastery exhibit superior disease-related stress coping mechanisms, and through positive outlooks, they confront adverse events related to their condition, thereby fostering improved societal engagement and lower levels of SA (23, 58).
Additionally, our study reveals that perceived social support fully mediates the relationship between EI and SA in peritoneal dialysis patients. Individuals with high EI excel at perceiving and effectively regulating emotions, fostering positive emotional states during social interactions. These positive emotions often extend to family members and friends, fostering positive social interactions, aligning with the concept of emotional contagion (59, 60). Moreover, high EI equips patients to harness valuable social resources effectively. Perceived social support enhances patients’ sense of belonging and identity, compensating for social roles lost due to illness and encouraging proactive engagement in social interactions, ultimately reducing SA (61).
Our study further demonstrates that personal mastery and perceived social support partially mediate the relationship between EI and SA in peritoneal dialysis patients. Notably, navigational social support plays a more substantial mediating role than personal mastery, suggesting that perceived social support may be a stronger predictor of SA. However, additional research is required to validate this hypothesis. This study offers a mechanistic examination of the EI-SA relationship, addressing a gap in previous research. Nevertheless, relevant studies remain limited, and the precise mechanisms require further validation through additional research. Several limitations should be acknowledged. Firstly, this study is cross-sectional, precluding the establishment of causal relationships among variables. Subsequent longitudinal investigations are warranted to validate these findings. Secondly, the study sample was drawn from a single province in China, limiting its generalizability to all peritoneal dialysis patients.
To delve deeper into these intricate connections, future research could explore them through longitudinal surveys and mixed-method studies, incorporating qualitative research components.
Conclusion
In summary, our study has revealed a pronounced level of SA in peritoneal dialysis patients, with a robust association with EI. Personal mastery and perceived social support emerge as crucial mediators in this relationship. Specifically, implementing an emotional intelligence management program has the potential to enhance patients’ personal mastery and perceived social support, resulting in a subsequent reduction in SA levels. These findings offer a substantive theoretical foundation for addressing SA among peritoneal dialysis patients, suggesting that future clinical practice should consider tailoring interventions, such as the development of an emotional intelligence management program, to augment patients’ personal mastery and perceived social support, ultimately mitigating SA.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Zhengzhou University Life Science Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KD: Conceptualization, Methodology, Writing – original draft. JW: Methodology, Writing – review & editing. YZ: Data curation, Methodology, Writing – original draft. YH: Data curation, Investigation, Writing – original draft. YS: Funding acquisition, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This project was supported by the Medical Science and Technology Tackling Program of Henan Province (SBGJ2018053).
Acknowledgments
We thank all the patients involved for their positive cooperation as well as the doctors and nurses at the hospital who helped, and all the faculty members who offered guidance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lv, JC, and Zhang, LX. Prevalence and disease burden of chronic kidney disease. Adv Exp Med Biol. (2019) 1165:3–15. doi: 10.1007/978-981-13-8871-2_1
2. Iwagami, M, Caplin, B, Smeeth, L, Tomlinson, LA, and Nitsch, D. Chronic kidney disease and cause-specific hospitalisation: a matched cohort study using primary and secondary care patient data. Br J Gen Pract. (2018) 68:E512–23. doi: 10.3399/Bjgp18x697973
3. Requena-Ibanez, JA, Santos-Gallego, CG, Zafar, MU, and Badimon, JJ. SGLT2-inhibitors on HFpEF patients. Role of Ejection Fraction. Cardiovasc Drugs Ther. (2022) 37:989–96. doi: 10.1007/S10557-022-07371-7
4. Mehrotra, R, Devuyst, O, Davies, SJ, and Johnson, DW. The current state of peritoneal Dialysis. J Am Soc Nephrol. (2016) 27:3238–52. doi: 10.1681/Asn.2016010112
5. Htay, H, Foo, MWY, Jayaballa, M, Lim, LWW, Oei, EL, Sim, MH, et al. Exploration of Patients' preference for modalities of care among peritoneal Dialysis patients in Singapore: a single-center experience. Int Urol Nephrol. (2023) 56:199–204. doi: 10.1007/S11255-023-03605-1
6. Brown, EA, Blake, PG, Boudville, N, Davies, S, De Arteaga, J, Dong, J, et al. International society for peritoneal Dialysis practice recommendations: prescribing high-quality goal-directed peritoneal Dialysis. Perit Dial Int. (2020) 40:244–53. doi: 10.1177/0896860819895364
7. Lambie, M, Zhao, J, Mccullough, K, Davies, SJ, Kawanishi, H, Johnson, DW, et al. Variation in peritoneal dialysis time on therapy by country: results from the peritoneal dialysis outcomes and practice patterns study. Clin J Am Soc Nephrol. (2022) 17:861–71. doi: 10.2215/Cjn.16341221
8. Hao Limin, HW, Huiqin, H, and Peishan, C. Status quo and influencing factors of social alienation in ovarian cancer patients accepting postoperative chemotherapy. Chin Nurs Res. (2023) 37:1713–8.
9. Qing-Er, W, Hui-Min, S, Ting-Ting, Z, Qing-Wen, X, Kai, Q, Shan-Shan, H, et al. Social function and its influencing factors of peritoneal dialysis patients. Chin J Nurs. (2016) 51:707–11. doi: 10.3761/j.issn.0254-1769.2016.06.015
10. Tao Weiwei, WL, and Yizhi, W. Survey on the social participation status of peritoneal dialysis patients and the factors affecting them. Chin J Nurs. (2007) 42:123–6.
11. Cuevas-Budhart, M, Celaya Pineda, IX, Perez Moran, D, Trejo Villeda, MA, Gomez Del Pulgar, M, Rodríguez Zamora, MC, et al. Patient experience in automated peritoneal dialysis with telemedicine monitoring during the COVID-19 pandemic in Mexico: qualitative study. Nurs Open. (2023) 10:1092–101. doi: 10.1002/Nop2.1377
12. Gafarov, VV, Panov, DO, Gromova, EA, Gagulin, IV, and Gafarova, AV. The influence of social support on risk of acute cardiovascular diseases in female population aged 25-64 in Russia. Int J Circumpolar Health. (2013) 72:21210. doi: 10.3402/Ijch.V72i0.21210
13. Zhou, W, Li, Y, Ning, Y, Gong, S, Song, N, Zhu, B, et al. Social isolation is associated with rapid kidney function decline and the development of chronic kidney diseases in middle-aged and elderly adults: findings from the China health and retirement longitudinal study (CHARLS). Front Med. (2021) 8:782624. doi: 10.3389/Fmed.2021.782624
14. Supramanian Kogila, RS, and Sekar, M. Shahruddin and M. Sekar, emotional intelligence using ability model in context of nursing and its impact on end-stage renal disease patients: a narrative review. Int J Curr Res Rev. (2021) 13:151–8. doi: 10.31782/IJCRR.2021.131609
15. Gan, X, Wang, P, Huang, C, Li, H, and Jin, X. Alienation from school and cyberbullying among Chinese middle school students: a moderated mediation model involving self-esteem and emotional intelligence. Front Public Health. (2022) 10:903206. doi: 10.3389/Fpubh.2022.903206
16. Gu Yanhong, SZ, Hua, L, Mengxue, Y, Qianyu, M, and Jingjing, Z. Application of the EIM-based emotion management Programme in patients with depressive episode of bipolar disorder. Chin Nurs Manag. (2022) 22:1009–14. doi: 10.3969/j.issn.1672-1756.2022.07.010
17. Dong Min-Ye, JZ-Y, Zhen-Su, S, and Guo-Hong, L. Influence of emotional intelligence on behavior performance in crisis intervention situations. J Shanghai Jiaotong Univ. (2020) 40:101–6. doi: 10.3969/j.issn.1674-8115.2020.01.016
18. Smith, R, Killgore, WDS, Alkozei, A, and Lane, RD. A neuro-cognitive process model of emotional intelligence. Biol Psychol. (2018) 139:131–51. doi: 10.1016/J.Biopsycho.2018.10.012
19. Skaff, MM, Pearlin, LI, and Mullan, JT. Transitions in the caregiving career: effects on sense of mastery. Psychol Aging. (1996) 11:247–57. doi: 10.1037/0882-7974.11.2.247
20. Li, HX, and Xia, N. The role of oxidative stress in cardiovascular disease caused by social isolation and loneliness. Redox Biol. (2020) 37:101585. doi: 10.1016/J.Redox.2020.101585
21. Zhao Jiming, FX, Qiao, M, Jing, Z, and Meixia, Z. Status and influencing factors of personal mastery in kidney transplant patients. Chin J Nurs. (2022) 57:1213–8. doi: 10.3761/j.issn.0254-1769.2022.10.009
22. Bonds Johnson, K, Brewster, GS, Cicero, E, Hepburn, K, Clevenger, CK, Daniel, G, et al. Promoting caregiver mastery in black American dementia caregivers. Gerontologist. (2022) 62:685–93. doi: 10.1093/Geront/Gnab147
23. Morris, ME, Slade, SC, Wittwer, JE, Blackberry, I, Haines, S, Hackney, ME, et al. Online dance therapy for people with Parkinson's disease: feasibility and impact on consumer engagement. Neurorehabil Neural Repair. (2021) 35:1076–87. doi: 10.1177/15459683211046254
24. Bruno, F, Lau, C, Tagliaferro, C, Marunic, G, Quilty, LC, Liuzza, MT, et al. Effects of Cancer severity on the relationship between emotional intelligence, perceived social support, and psychological distress in Italian women. Support Care Cancer. (2024) 32:142. doi: 10.1007/S00520-024-08346-0
25. White, CA . Body image dimensions and Cancer: a heuristic cognitive behavioural model. Psychooncology. (2000) 9:183–92. doi: 10.1002/1099-1611(200005/06)9:3<183::Aid-Pon446>3.0.Co;2-L
26. Jiqian, HYF . The introduce and usage of WHOQOL instrument in Chinese. Chin J Tissue Engineer Res. (2004) 4:1127–9. doi: 10.3321/j.issn:1673-8225.2000.08.002
27. Wong, C-S, and Law, KS. The effects of leader and follower emotional intelligence on performance and attitude: an exploratory study. Leadersh Q. (2002) 13:243–74. doi: 10.1016/S1048-9843(02)00099-1
28. Yefei, W . A reliability study of the Chinese version of the emotional intelligence scale. Ma Thesis: Central South University (2010).
29. Safipour, J, Tessma, MK, Higginbottom, G, and Emami, A. Measuring social alienation in adolescence: translation and validation of the Jessor and Jessor social alienation scale. Scand J Psychol. (2010) 51:517–24. doi: 10.1111/J.1467-9450.2010.00810.X
30. Wu Shuang, LY, Xiaolin, Z, Qi, D, Ling, D, and Siyi, G. Reliability and validity of the generalized social of alienation scale among the elderly. J Cheng Med College. (2010) 100:751–4. doi: 10.3969/j.issn.1674-2257.2015.06.031
31. Du Rongrong, LR, Yihuan, D, and Panpan, C. Mediating role of self-efficacy between Stiga and social alienation in peritoneal Dialysis patients. Mil Med Joint Logist. (2023) 37:1036–9. doi: 10.13730/j.issn.2097-2148.2023.12.010
32. Pearlin, LI, and Schooler, C. The structure of coping. J Health Soc Behav. (1978) 19:2–21. doi: 10.2307/2136319
33. Yu Yibing, ZH . A study on the development characteristics of the positive psychological qualities in migrant children. Chin J Spec Educ. (2008) 4:78–83. doi: 10.3969/j.issn.1007-3728.2008.04.016
34. Zhou Yue, SY, Li Yanan, D, Liping, CL, Tingting, J, Yajing, G, and Xinxin, J. Characteristics and influencing factors of mastery in young and middle-aged patients undergoing peritoneal Dialysis. Chin Nurs Manag. (2020) 20:378–82. doi: 10.3969/j.issn.1672-1756.2020.03.013
36. Zhou Rui, QS-W, Zhi, L, and Yuan-Qing, D. The present status and influencing factors of dietary compliance behaviors in peritoneal Dialysis patients. Chin J Blood Purificat. (2022) 21:926–30. doi: 10.3969/j.issn.1671-4091.2022.12.014
37. Xiaofang,, Wei, LYWLZ, and Qiugui, JLYH. Status of social isolation among lung Cancer survivors: the influencing factors. J Nurs Sci. (2021) 36:63–6. doi: 10.3870/j.issn.1001-4152.2021.15.063
38. Zhao Cuicui, XF . Study on the status quo and influencing factors of social alienation in patients with cerebral apoplexy in rehabilitation period. Nurs Res. (2021) 21:685–91. doi: 10.12102/j.issn.1009-6493.2022.05.014
39. Shao Lijiao, WJ, Tianrui, W, Yuhua, Z, Shuyi, G, and Ruixing, Z. Analysis of the current situation of social isolation of Enterostomal patients and the factors affecting it. J Nurs. (2022) 29:19–23. doi: 10.16460/j.issn1008-9969.2022.15.019
40. Beaumier, M, Calvar, E, Launay, L, Béchade, C, Lanot, A, Schauder, N, et al. Effect of social deprivation on peritoneal Dialysis uptake: a mediation analysis with the data of the REIN registry. Perit Dial Int. (2022) 42:361–9. doi: 10.1177/08968608211023268
41. Moore, S, Leung, B, Bates, A, and Ho, C. Social isolation: impact on treatment and survival in patients with advanced Cancer. J Clin Oncol. (2018) 36:156–6. doi: 10.1200/Jco.2018.36.34_Suppl.156
42. Tuchman, S, Khademian, ZP, and Mistry, K. Dialysis disequilibrium syndrome occurring during continuous renal replacement therapy. Clin Kidney J. (2013) 6:526–9. doi: 10.1093/Ckj/Sft087
43. Rachmin, I, Ostrowski, SM, Weng, QY, and Fisher, DE. Topical treatment strategies to manipulate human skin pigmentation. Adv Drug Deliv Rev. (2020) 153:65–71. doi: 10.1016/J.Addr.2020.02.002
44. Egan, CE, Qazi, M, Lee, J, Lee-Saxton, YJ, Greenberg, JA, Beninato, T, et al. Treatment of secondary hyperparathyroidism and post-transplant tertiary hyperparathyroidism. J Surg Res. (2023) 291:330–5. doi: 10.1016/J.Jss.2023.06.031
45. Li Ting, ZQ, Na, L, and Bai, L. Research on the relationship between body image and the feeling of self-value of patients with small area burns. Mil Nurs. (2014) 31:17–20. doi: 10.3969/j.issn.1008-9993.2014.16.005
46. King, G, Smart, E, Bowman, L, and Pinto, M. Social participation interventions targeting relational outcomes for young people with physical and developmental disabilities: an umbrella review and narrative synthesis. Disabil Rehabil. (2023) 45:2073–86. doi: 10.1080/09638288.2022.2085332
47. Hongxia, ZLZBL . Correlation between self-disclosure and social alienation, psychosocial adjustment in patients with psoriasis and its influencing factors analysis. China Med Herald. (2022) 19:94–7.
48. Lengton, R, Van Der Willik, EM, De Rooij, ENM, Meuleman, Y, Le Cessie, S, Michels, WM, et al. Effect of residual kidney function and Dialysis adequacy on chronic pruritus in Dialysis patients. Nephrol Dial Transplant. (2023) 38:1508–18. doi: 10.1093/Ndt/Gfac341
49. Li, H, Li, X, Feng, S, Zhang, G, Wang, W, and Wang, S. Sleep disorders and its related risk factors in patients undergoing chronic peritoneal Dialysis. Chin Med J. (2014) 127:1289–93. doi: 10.3760/cma.j.issn.0366-6999.20132428
50. Montalescot, L, Rascle, N, Combe, C, and Untas, A. Patients' experience one year after dialysis initiation: a lexicometric analysis. Health Psychol Behav Med. (2021) 9:380–97. doi: 10.1080/21642850.2021.1918552
51. Xu Haili, JY, Dujuan, N, and Zhiling, Z. Effect of disease uncertainty on disease adaptation in patients undergoing early peritoneal Dialysis. J Zheng Univ. (2018) 53:521–4. doi: 10.13705/j.issn.1671-6825.2018.01.123
52. Barberis, N, Cannavò, M, Trovato, M, and Verrastro, V. Pathways from trait emotional intelligence to factors of distress in Rosacea: the mediating role of social phobia and self-esteem. J Affect Disord. (2023) 331:362–8. doi: 10.1016/J.Jad.2023.03.003
53. Li, D, Li, X, Zhao, L, Zhou, Y, Sun, W, and Wang, Y. Linking multiple risk exposure profiles with adolescent internet addiction: insights from the person-centered approach. Comput Hum Behav. (2017) 75:236–44. doi: 10.1016/j.chb.2017.04.063
54. Fredrickson, BL . The role of positive emotions in positive psychology: the broaden-and-build theory of positive emotions. Am Psychol. (2001) 56:218–26. doi: 10.1037/0003-066X.56.3.218
55. Kashdan, TB, Dewall, CN, Masten, CL, Pond, RS Jr, Powell, C, Combs, D, et al. Who is Most vulnerable to social rejection? The toxic combination of low self-esteem and lack of negative emotion differentiation on neural responses to rejection. PLoS One. (2014) 9:E90651. doi: 10.1371/Journal.Pone.0090651
56. Muraven, M, and Baumeister, RF. Self-regulation and depletion of limited resources: does self-control resemble a muscle? Psychol Bull. (2000) 126:247–59. doi: 10.1037/0033-2909.126.2.247
57. Chen, X, and Cheng, L. Emotional intelligence and creative self-efficacy among gifted children: mediating effect of self-esteem and moderating effect of gender. J Intelligence. (2023) 11:17. doi: 10.3390/Jintelligence11010017
58. Chang, C-H, Ferris, DL, Johnson, RE, Rosen, CC, and Tan, JA. Core self-evaluations: a review and evaluation of the literature. J Manag. (2012) 38:81–128. doi: 10.1177/0149206311419661
59. Lidan, LZW . The causes and effects of emotional contagion of leaders. Leadership Sci. (2019) 52
60. Zhang, L, Roslan, S, Zaremohzzabieh, Z, Jiang, Y, Wu, S, and Chen, Y. Perceived stress, social support, emotional intelligence, and post-stress growth among Chinese left-behind children: a moderated mediation model. Int J Environ Res Public Health. (2022) 19:1851. doi: 10.3390/Ijerph19031851
Keywords: peritoneal dialysis, emotional intelligence, personal mastery, perceived social support, social alienation
Citation: Diao K, Wang J, Zhang Y, Huang Y and Shan Y (2024) The mediating effect of personal mastery and perceived social support between emotional intelligence and social alienation among patients receiving peritoneal dialysis. Front. Public Health. 12:1392224. doi: 10.3389/fpubh.2024.1392224
Edited by:
Steffen Schulz, Charité University Medicine Berlin, GermanyReviewed by:
Adnan Fateh, University of Central Punjab, PakistanNadeeka Chandraratne, University of Colombo, Sri Lanka
Copyright © 2024 Diao, Wang, Zhang, Huang and Shan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Shan, c3kxMTBAc2luYS5jb20=
 Keke Diao
Keke Diao Jiajia Wang1
Jiajia Wang1 Yijia Huang
Yijia Huang