- 1School of Integrated Chinese and Western Medicine, Hunan University of Chinese Medicine, Changsha, Hunan, China
- 2Key Laboratory of Hunan Province for Integrated Traditional Chinese and Western Medicine on Prevention and Treatment of Cardio-Cerebral Diseases, College of Integrated Traditional Chinese and Western Medicine, Hunan University of Chinese Medicine, Changsha, Hunan, China
- 3School of Mechatronics and Energy Engineering, NingboTech University, Ningbo, China
- 4Nursing Department, Guizhou Provincial People's Hospital, Guiyang, Guizhou, China
- 5Department of Neurology, The Second Affiliated Hospital of Guizhou University of Chinese Medicine, Guiyang, Guizhou, China
Background: EPs pose significant challenges to individual health and quality of life, attracting attention in public health as a risk factor for diminished quality of life and healthy life expectancy in middle-aged and older adult populations. Therefore, in the context of global aging, meticulous exploration of the factors behind emotional issues becomes paramount. Whether ADL can serve as a potential marker for EPs remains unclear. This study aims to provide new evidence for ADL as an early predictor of EPs through statistical analysis and validation using machine learning algorithms.
Methods: Data from the 2018 China Health and Retirement Longitudinal Study (CHARLS) national baseline survey, comprising 9,766 samples aged 45 and above, were utilized. ADL was assessed using the BI, while the presence of EPs was evaluated based on the record of “Diagnosed with Emotional Problems by a Doctor” in CHARLS data. Statistical analyses including independent samples t-test, chi-square test, Pearson correlation analysis, and multiple linear regression were conducted using SPSS 25.0. Machine learning algorithms, including Support Vector Machine (SVM), Decision Tree (DT), and Logistic Regression (LR), were implemented using Python 3.10.2.
Results: Population demographic analysis revealed a significantly lower average BI score of 65.044 in the “Diagnosed with Emotional Problems by a Doctor” group compared to 85.128 in the “Not diagnosed with Emotional Problems by a Doctor” group. Pearson correlation analysis indicated a significant negative correlation between ADL and EPs (r = −0.165, p < 0.001). Iterative analysis using stratified multiple linear regression across three different models demonstrated the persistent statistical significance of the negative correlation between ADL and EPs (B = −0.002, β = −0.186, t = −16.476, 95% CI = −0.002, −0.001, p = 0.000), confirming its stability. Machine learning algorithms validated our findings from statistical analysis, confirming the predictive accuracy of ADL for EPs. The area under the curve (AUC) for the three models were SVM-AUC = 0.700, DT-AUC = 0.742, and LR-AUC = 0.711. In experiments using other covariates and other covariates + BI, the overall prediction level of machine learning algorithms improved after adding BI, emphasizing the positive effect of ADL on EPs prediction.
Conclusion: This study, employing various statistical methods, identified a negative correlation between ADL and EPs, with machine learning algorithms confirming this finding. Impaired ADL increases susceptibility to EPs.
1 Introduction
As the world’s population continues to age, projections indicate that the number of individuals aged 60 and above in developing nations will surge from 900 million to two billion between 2015 and 2050 (1). Among the older adult population, the activities of daily living (ADL) and emotional problems (EPs) have received widespread attention in the fields of medicine and public health research (2–6). EPs encompass a range of disorders such as panic disorder, generalized anxiety disorder, social phobia, specific phobia, obsessive-compulsive disorder, post-traumatic stress disorder, and depression (7). These EPs pose significant challenges to individual health and quality of life (8). Research has found that the overall prevalence of depression among older adults globally is 28.4% (9), and depression may accelerate the cellular aging process (10). Symptoms of depression, anxiety, and other emotional issues also manifest in the preclinical stages of Alzheimer’s disease (AD) (11). EPs greatly impact the health and lifespan of the older adult. Therefore, in the context of global aging, it is particularly important to meticulously explore the factors behind emotional issues.
EPs, characterized primarily by emotional disturbances such as depression, anxiety, mania, and feelings of loneliness, may also entail impulsive behavior, disruptions in sleep and diet, and even suicidal or self-harming thoughts (12). For middle-aged and older adult individuals, the pressures of work and family, or difficulties adjusting to life after retirement, coupled with disparities in social interaction and attention, can lead to emotional disruptions, resulting in a spectrum of EPs (13). In the prodromal stages of AD, which often coincide with gradual and insidious impairments in ADL, individuals may experience EPs, manifesting as depression or anxiety, yet these symptoms often go unnoticed, leading to exacerbation in later stages of AD (14, 15). During the recovery and sequelae phases of stroke, EPs are often present (16), with patients frequently experiencing difficulty in emotional regulation, thereby impacting stroke rehabilitation (17, 18). ADL encompasses a range of pertinent issues such as personal self-care, proficiency in functional tasks, and the ability to perform activities, serving as a cornerstone of an individual’s quality of life (19). Age-related impairments in ADL may render middle-aged and older adult individuals unable to accept declines in physical function and personal capabilities, thereby triggering EPs (20). Encouraging patients to improve their ADL is a crucial measure in the rehabilitation of EPs, as enhancing ADL can aid patients in returning to normal life and stabilizing their emotions (21). In stroke rehabilitation, as patients’ physical abilities improve, activities such as independent eating, walking, and climbing stairs can alleviate EPs resulting from stroke sequelae (22, 23).
Previous studies have hinted at the potential correlation between ADL and EPs. To elucidate this correlation further, the present study collected data from the China Health and Retirement Longitudinal Survey (CHARLS) in 2018 and employed various statistical methods for analysis, revealing a significant correlation between ADL and EPs. Additionally, three machine learning algorithms—Support Vector Machine (SVM), Decision Tree (DT), and Logistic Regression (LR)—were employed to validate our findings. The primary objective of this study is to elucidate the association between ADL and EPs, enhance the awareness of ADL among middle-aged and older adult individuals, and introduce novel avenues for non-pharmacological rehabilitation therapy for emotional issues in this demographic group.
2 Methods
2.1 Study population
This study collected data from the China Health and Retirement Longitudinal Study (CHARLS) baseline dataset, which is operated by the National School of Development at Peking University.1 CHARLS has established a high-quality open-access database encompassing various details regarding individuals, families, health status, and socio-economic aspects, including “Health Status and Functioning,” “Cognition,” “Work Retirement,” and “Family Information.” The study cohort comprised individuals aged 45 and above randomly selected from 150 counties or districts and 450 villages or urban areas across 28 provinces, representing the middle-aged and older adult population in China (24). Utilizing the 2018 CHARLS dataset, this study encompassed a total of 20,813 samples. Participants under 45 years old were excluded from the analysis, along with those with insufficient demographic or health data, resulting in a final sample size of 9,766 individuals.
2.2 Assessment of emotional problems
The assessment was conducted based on the records of emotional problems data “Diagnosed with Emotional Problems by a Doctor” in CHARLS. The samples were divided into two cohorts: those affirmed as “Diagnosed with Emotional Problems by a Doctor” and those negated as “Not diagnosed with Emotional Problems by a Doctor.”
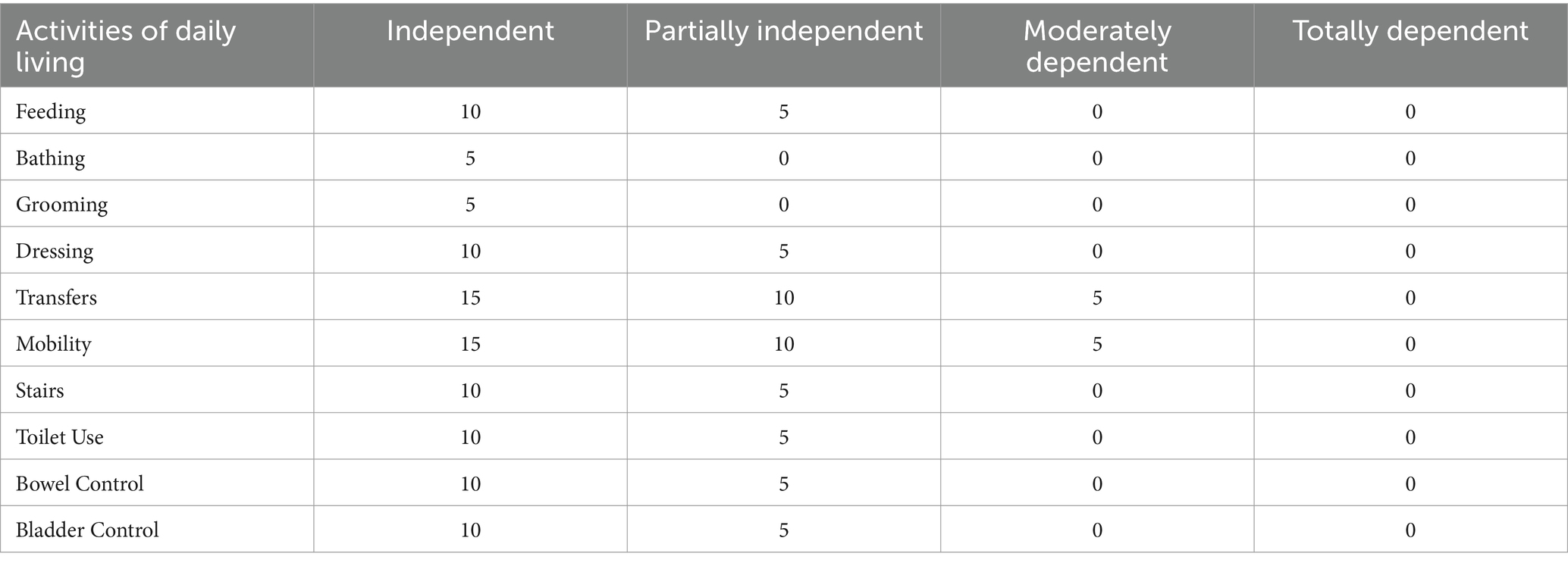
2.3 Assessment of ADL
The Barthel Index (BI) is a recognized method used to assess the level of ADL. In this study, the BI was employed to evaluate the ADL of all samples. The BI categorizes daily activities into 10 independent elements, including “Feeding,” “Bathing,” “Grooming,” “Dressing,” “Bowel Control,” “Bladder Control,” “Toilet Use,” “Transfers,” “Mobility,” and “Stairs,” each element being assessed with a score (Table 1), reflecting the individual’s ability and proficiency in completing the respective tasks. By assigning scores to each element and summarizing these scores, the BI is derived, ranging from 0 to 100. A higher BI score indicates greater autonomy and proficiency in performing daily life activities (6, 25–27).
2.4 Assessment of covariates
The covariates in this study were derived from the CHARLS dataset, encompassing variables such as age, gender (male, female), residence (Central of City/Town, Urban–Rural Integration Zone, Rural, Special Zone), education (ranging from No Formal Education (Illiterate) to Doctoral Degree/Ph.D.), smoking status (Still Smoke, Quit or No, Never Smoked), drinking status (Drink more than once a month, Drink but less than once a month, None), as well as hypertension, diabetes, and dyslipidemia. For age, middle-aged individuals were defined as those aged 45 to below 60 years, while older adult individuals were defined as those aged 60 years and above. Regarding hypertension, as per the 2010 Chinese Hypertension Guidelines, hypertension was diagnosed based on an average systolic blood pressure ≥ 140mmHg, and/or an average diastolic blood pressure ≥ 90mmHg, and/or self-reported use of antihypertensive medications within the past 2 weeks (28). Diabetes diagnosis criteria included a fasting blood glucose level ≥ 7.0 mmol/L or current treatment with antidiabetic medication. Dyslipidemia diagnosis criteria, following the 2016 Chinese Adult Dyslipidemia Guidelines, included total cholesterol level ≥ 240 mg/dL, high-density lipoprotein cholesterol level < 40 mg/dL, low-density lipoprotein cholesterol level > 160 mg/dL, or triglyceride level ≥ 200 mg/dL (29).
2.5 Statistical analysis
In the demographic characteristics analysis, continuous variables such as age and BI were summarized using mean and standard deviation (SD), while categorical variables like gender, residence, and education were represented as counts and percentages. To examine demographic characteristics, independent sample t-tests were employed for continuous variables to discern differences, while chi-square tests were utilized for categorical variables. Correlation analysis involved Pearson correlation tests to assess the relationship between independent variables, covariates, and dependent variables. Subsequently, a comprehensive evaluation of the relationship between ADL and EPs was conducted through hierarchical multiple linear regression analysis. This regression underwent three iterations with distinct models, incorporating dummy variables as references in each variable. Model 1 included three variables: age, gender, and ADL. Model 2 extended Model 1 by adding residence, education, smoking status, and drinking status, resulting in a total of seven variables. Model 3 further expanded upon Model 2 with the inclusion of hypertension, diabetes, and dyslipidemia, encompassing a total of 10 variables.
2.6 Machine learning algorithm
2.6.1 Parameter setup
The machine learning algorithms were implemented using the PyCharm 2023.1.2 integrated development environment and executed on a computer running the Windows 11 operating system. The software development process was conducted within the specified Anaconda development environment, utilizing Python version 3.10.2 for coding and analysis. A random seed number of 42 was set and maintained consistently across the entire process to ensure the reproducibility and consistency of results. The original dataset was partitioned into two distinct subsets: a training set and a testing set. The training set comprised 70% of the original data, while the remaining 30% was allocated to the testing set. The data was randomly shuffled, and the model’s performance was evaluated by examining the classification results generated from the testing dataset.
2.6.2 Experimental models
2.6.2.1 Support vector machine
The SVM stands out as a prominent supervised learning technique within the realm of machine learning, classified as a generalized linear classifier. Its core objective revolves around accurately classifying data points by discerning the maximum-margin hyperplane, which serves as the decision boundary for the training dataset. One of SVM’s distinguishing features is its adaptability in tackling nonlinear classification tasks, facilitated by the utilization of kernel functions. This capability underscores SVM’s pivotal role in kernel-based learning methodologies. Notably, SVM demonstrates remarkable efficacy in addressing high-dimensional problems, including those characterized by expansive feature spaces, and exhibits prowess in navigating intricate relationships among nonlinear features (30, 31).
2.6.2.2 Decision tree learning
DT, a widely used supervised technique in statistics, data mining, and machine learning, offers versatile classification and regression capabilities. These trees, fashioned as predictive models, derive insights from observational data. In classification, they serve as tree-based models for discrete target variable values, with terminal nodes denoting class labels and branches delineating feature combinations leading to these labels. In regression, decision trees adeptly handle continuous target variable values, typically real numbers. Their adaptability spans various data types, encompassing categorical sequences, thereby augmenting their versatility across diverse analytical domains. Known for their simplicity and interpretability, decision trees are valuable tools for transparent decision-making processes and are particularly useful in decision analysis and data mining applications, where they provide descriptive insights and aid in decision-making (32–34).
2.6.2.3 Logistic regression
LR (Equation 1), a widely embraced methodology in supervised learning within machine learning, is distinct from linear regression as it primarily tackles classification problems, even in multi-classification scenarios. During training, the model learns from a dataset comprising multiple groups, known as the training set, absorbing patterns crucial for classification decisions. After training, the model applies this acquired knowledge to classify one or more datasets, referred to as the test set, each characterized by various indicators contributing to the decision-making process. Logistic regression’s adaptability renders it indispensable in supervised learning, playing a foundational role in machine learning methodologies across scientific and medical domains (35–37).
Equation 1: Logistic regression.
2.6.3 Evaluating indicator
This study utilized accuracy, precision, recall, and F1-score as the selected evaluation metrics (38, 39). Accuracy assesses the proportion of correctly predicted labels to the total labels (Equation 2). Precision evaluates the proportion of true positive predictions among all positive predictions (Equation 3). Recall gauges the proportion of true positive predictions among all actual positive instances (Equation 4). F1-score reflects the robustness of the model, simultaneously considering precision and recall. A higher F1 value indicates better model performance (Equation 5).
Equation 2: Accuracy.
Equation 3: Precision.
Equation 4: Recall.
Equation 5: F1-score (TP, True Positive; FP, False Positive; FN, False Negative; TN, True Negative).
3 Results
3.1 Characteristics of samples
The study rigorously excluded ineligible subjects, namely those aged 45 and below, as well as individuals lacking adequate demographic or health data. Ultimately, the cohort comprised 9,766 participants, among whom 3,904 were male (39.98%) and 5862 were female (60.02%). Table 2 encapsulates the demographic characteristics of the study cohort, wherein 9539 individuals (97.68%) remained undiagnosed with EPs by medical professionals, while 227 individuals (2.32%) received EP diagnoses. Remarkably, those diagnosed with EPs demonstrated substantially lower average BI scores (65.044, standard deviation = 30.6421) compared to their undiagnosed counterparts (85.128, standard deviation = 17.6386), indicating a significant disparity (p < 0.001, t = 16.573) in ADL between the diagnosed and undiagnosed EP cohorts. Furthermore, significant differences (p < 0.001) were discerned between individuals diagnosed with EPs and those without in terms of gender (p = 0.015), smoking status (p = 0.005), alcohol consumption (p < 0.001), hypertension (p = 0.001), and dyslipidemia (p = 0.011). Analysis of the demographic features of the sample underscores the influence of ADL, gender, education, smoking and alcohol habits, as well as the presence of hypertension or dyslipidemia on the prevalence of EPs.
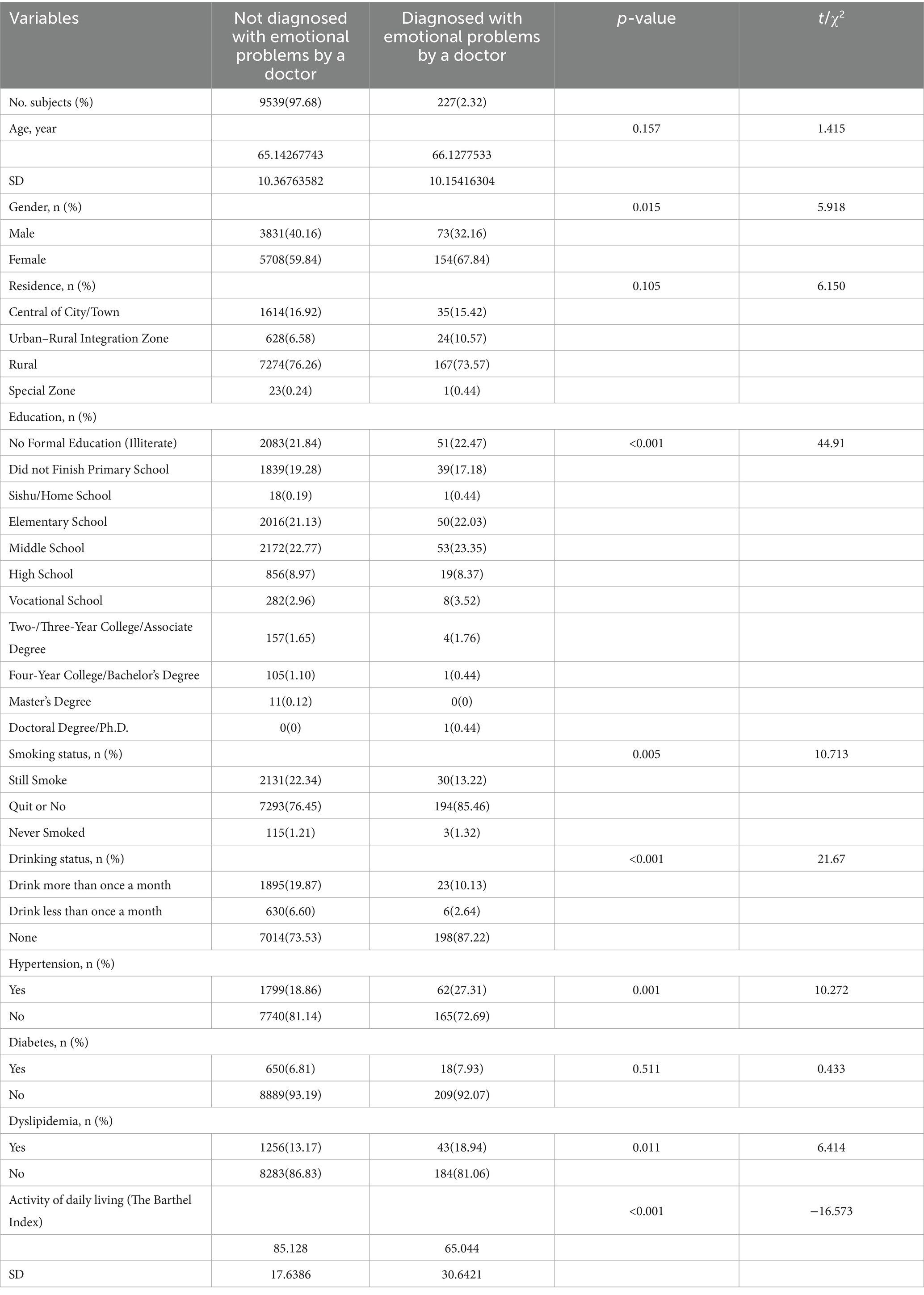
Table 2. Demographic characteristics of middle-aged and older adults Chinese with and without emotional problems by doctor.
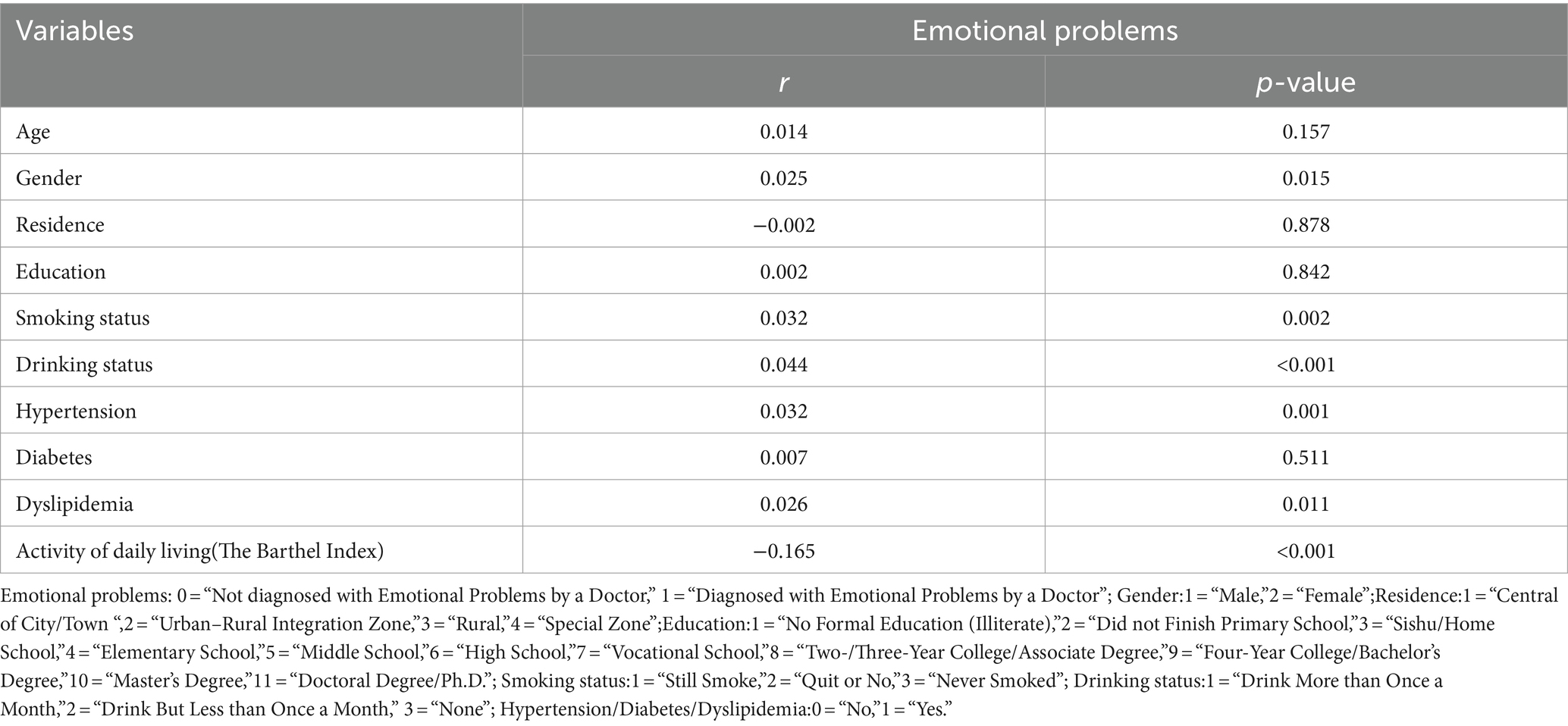
3.2 The correlation between variable and EPs
We employed Pearson correlation analysis to explore the relationship between EPs and both independent and covariate variables (Table 3). The results reveal a significant negative correlation between ADL and EPs (r = −0.165, p < 0.001), indicating an increased susceptibility to EPs among individuals with impaired ADL. Additionally, a slight yet significant positive correlation was observed between gender and EPs (r = 0.025, p = 0.015), suggesting a higher likelihood of females being diagnosed with EPs. Regarding smoking status, a significant positive correlation with EPs was found (r = 0.032, p = 0.002), implying a higher susceptibility to EPs among non-smokers. Similarly, a significant positive correlation was observed between alcohol consumption and EPs (r = 0.044, p < 0.001), indicating that individuals with lower alcohol consumption frequency are more likely to be diagnosed with EPs. Furthermore, hypertension (r = 0.032, p = 0.001) and dyslipidemia (r = 0.026, p = 0.011) exhibited significant positive correlations with EPs, suggesting a greater likelihood of individuals with hypertension or dyslipidemia being diagnosed with EPs.
3.3 Associations between ADL and EPs
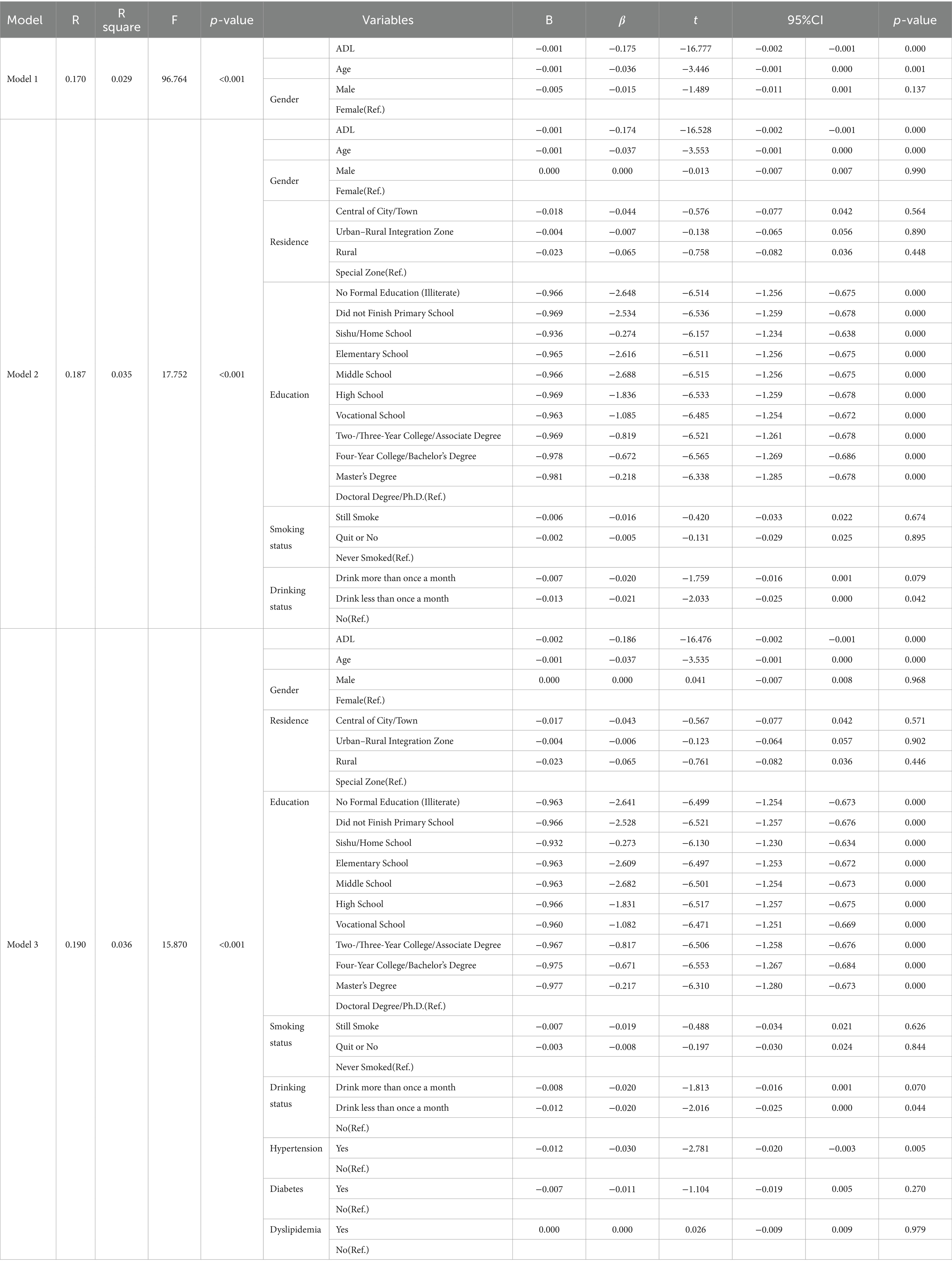
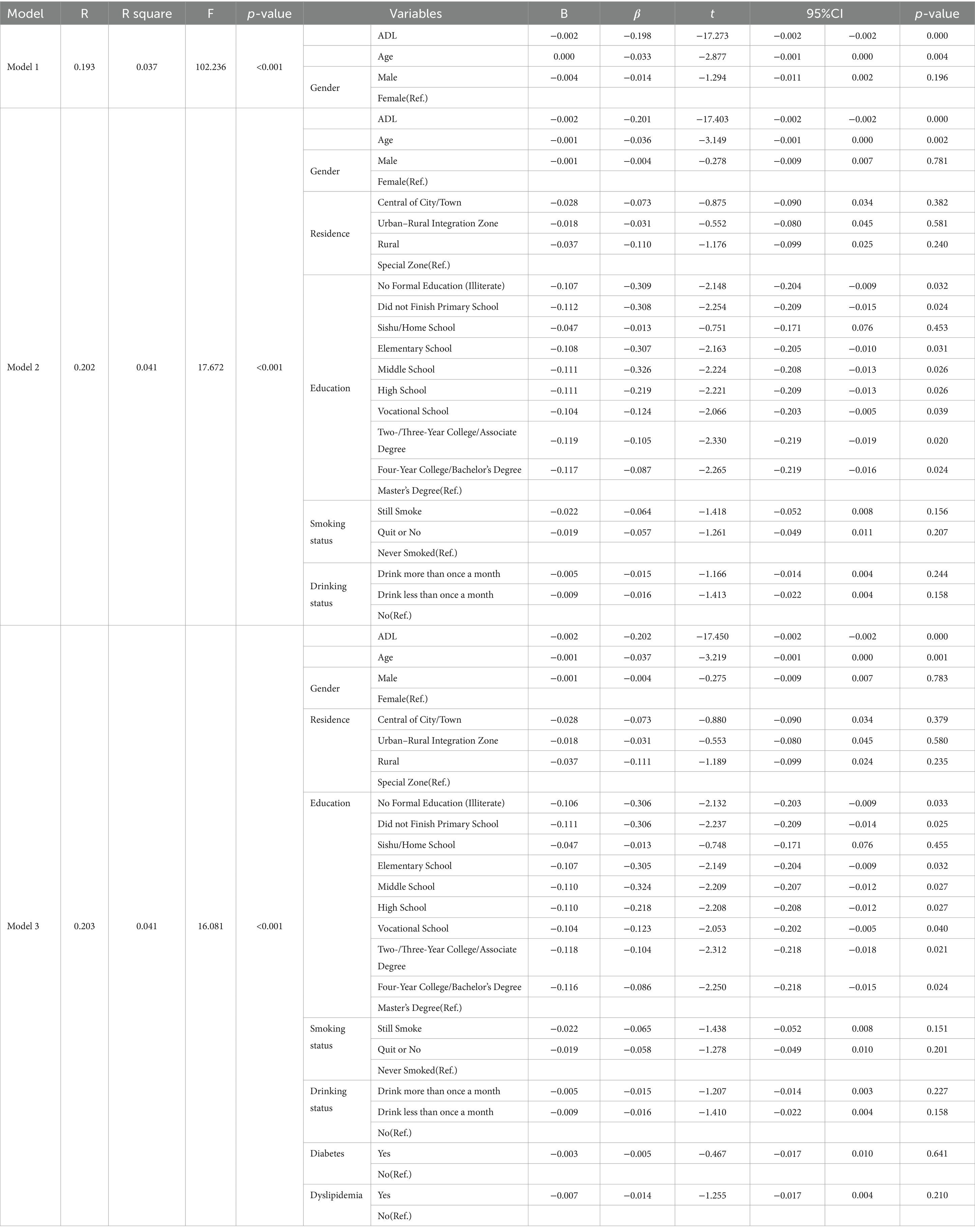
To delve deeper into the correlation between EPs and ADL, we employed hierarchical multiple linear regression to systematically investigate the association between the independent variables (ADL, age, gender, residence, smoking status, etc.) and the dependent variable EPs across three distinct models (Model 1, Model 2, Model 3; Table 4).
In Model 1, we included ADL, age, and gender (R = 0.170, R2 = 0.029, F = 96.764, p < 0.001). We observed a significant negative correlation between ADL and EPs (B = −0.001, β = −0.175, t = −16.777, 95% CI = −0.002, −0.001, p = 0.000), underscoring the heightened susceptibility to EPs among individuals with impaired daily living abilities. In Model 2, additional covariates were incorporated (residence, education, smoking, and drinking status), where ADL continued to exhibit a pronounced negative correlation with EPs (B = −0.001, β = −0.174, t = −16.528, 95% CI = −0.002, −0.001, p = 0.000), maintaining statistical significance. In the final iteration, Model 3 introduced hypertension, dyslipidemia, and diabetes, reaffirming the negative correlation between ADL and EPs (B = −0.002, β = −0.186, t = −16.476, 95% CI = −0.002, −0.001, p = 0.000), with an overall significant fit (R = 0.190, R2 = 0.036, F = 15.870, p < 0.001).
All three models demonstrated statistically significant associations between the independent and dependent variables (p < 0.001). The R value increased gradually from 0.170 in Model 1 to 0.190 in Model 3, indicating an enhanced ability to explain the variability of outcomes. Across all models, despite adjustments for covariates, our study consistently emphasized the significant association between declining ADL and increased susceptibility to EPs, while underscoring the robustness of this relationship.
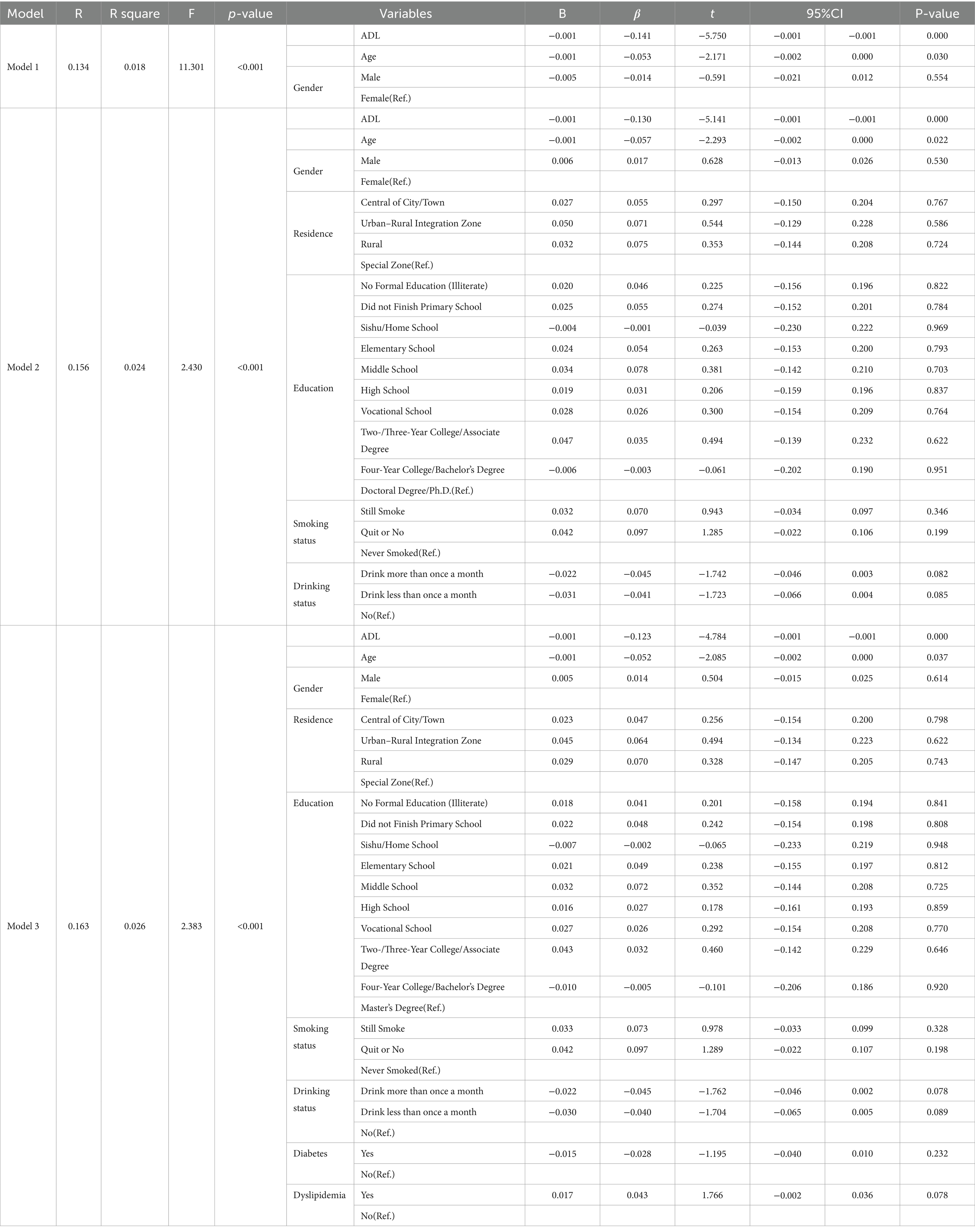
In our investigation, hypertension emerged as a consistent factor exhibiting correlation with EPs across all analyses, suggesting its potential role as a significant confounding factor in this study. To mitigate this confounding effect, we partitioned the entire sample into two cohorts: a hypertension group (Table 5) and a non-hypertension group (Table 6). Through this stratification, we aimed to delve into the relationship between ADL and EPs in detail.
Within the hypertension group, iterative modeling across three iterations continued to reveal a statistically significant negative correlation between ADL and EPs (B = −0.001, β = −0.123, t = −4.784, 95% CI = −0.001, −0.001, p = 0.000). Similarly, within the non-hypertension group, this negative correlation persisted (B = −0.002, β = −0.202, t = −17.450, 95% CI = −0.002, −0.002, p = 0.000). These findings underscore that irrespective of hypertension status and adjustments for covariates, ADL continues to influence susceptibility to EPs (p < 0.001).
3.4 Machine learning algorithm confirm the link between ADL and EPs
Through statistical analysis, we have identified a significant negative correlation between ADL and EPs, indicating that individuals with impaired daily living abilities are more susceptible to EPs. Moreover, employing hierarchical multiple linear regression, adjusting for and iterating covariates, we have established the stability of the negative correlation between ADL and EPs. Consequently, we employed three machine learning algorithms—SVM, DT, and LR—to validate the association between the two.
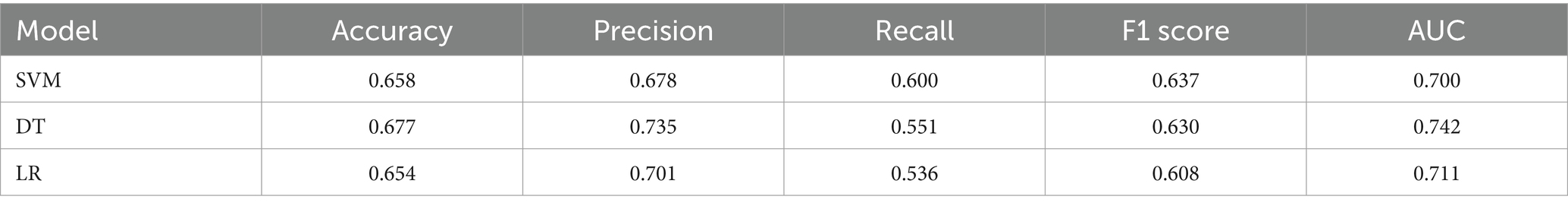
The results (see Figure 1A) demonstrate that the Area Under the Curve (AUC) values of SVM, DT, and LR exceeded the critical threshold of 0.7, reaching 0.700, 0.742, and 0.711, respectively, confirming the diagnostic capability of these models. Comprehensive evaluation of the three machine learning algorithms using Accuracy, Precision, Recall, and F1 Score metrics (see Figure 1B; Table 7) reveals that DT exhibited outstanding Accuracy (0.677) and Precision (0.735), while SVM demonstrated superiority in Recall (0.600) and F1 Score (0.637). The combined statistical analysis and machine learning algorithm validation affirm a substantial association between ADL and EPs, indicating that impaired daily living abilities increase susceptibility to emotional problems.
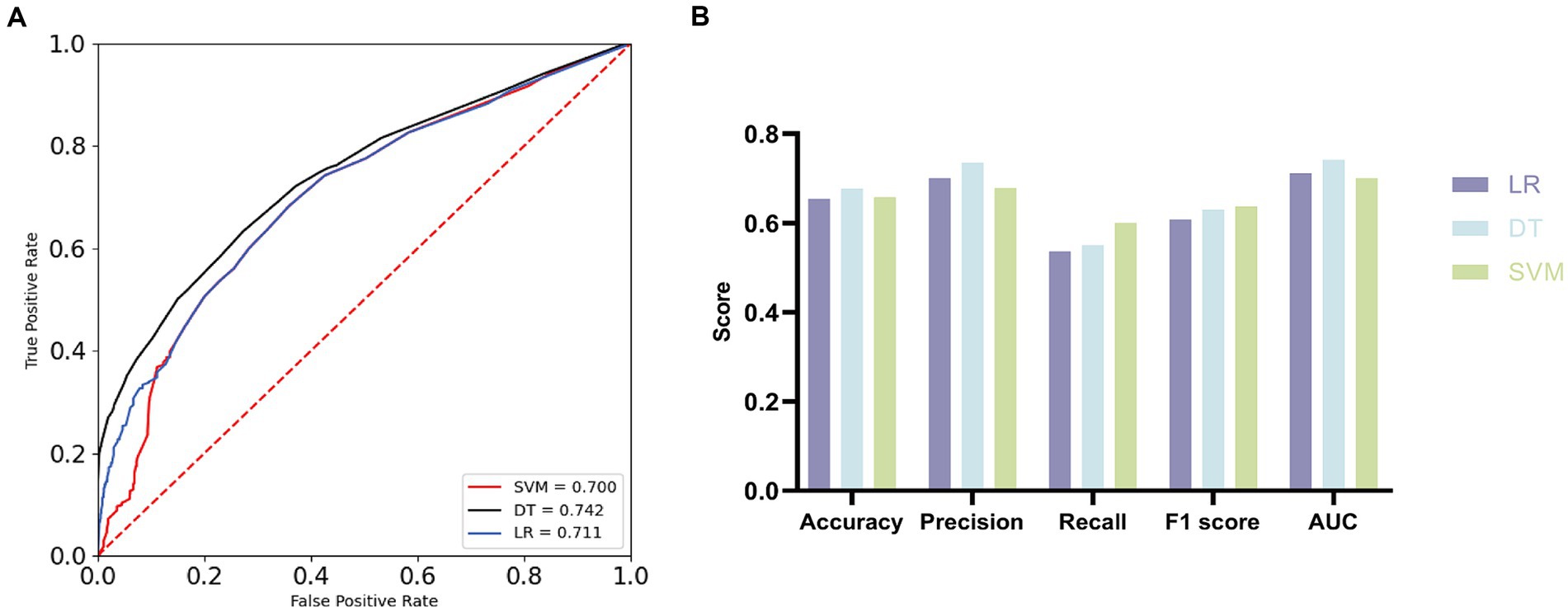
Figure 1. Receiver operating characteristic (ROC) curves and evaluation metrics. (A) ROC curves with AUC for the three machine learning algorithms. (B) Comparison of three machine learning algorithms.
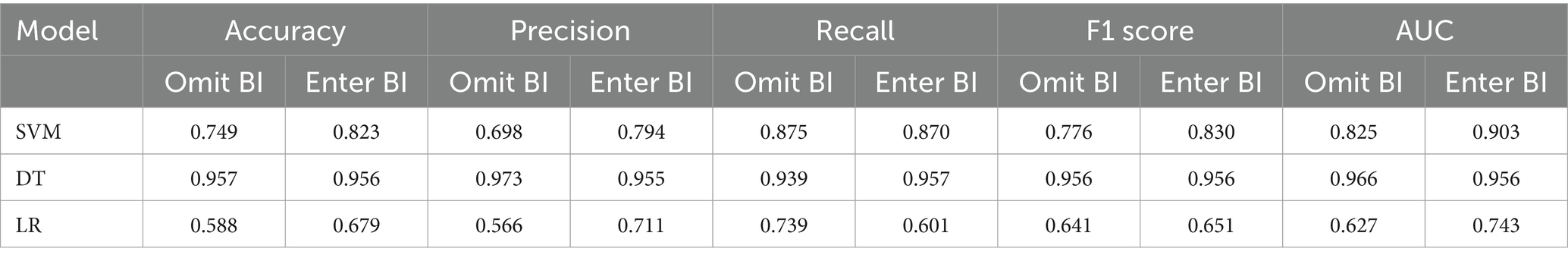
To enhance the credibility of the association between ADL and EPs and underscore the predictive role of ADL in EPs, we partitioned the dataset into two groups with distinct features. The first group included all covariates except for the Bath Index (BI), while the second group incorporated BI while retaining the same set of covariates. Machine learning algorithms rigorously validated these two data subsets. The results demonstrate that upon inclusion of BI, the AUC values of SVM and LR models increased from 0.825 and 0.627 to 0.903 and 0.743, respectively, whereas in the DT model, the AUC value decreased from 0.966 to 0.956. Overall, the addition of BI enhanced the predictive AUC values and improved model performance (see Figures 2A,B). Further analysis using Accuracy, Precision, Recall, and F1 Score metrics (see Figures 2C–E; Table 8) revealed that the SVM model exhibited the best performance, with Accuracy increasing from 0.749 to 0.823, Precision from 0.698 to 0.794, and F1 Score from 0.776 to 0.830, demonstrating robust overall performance.
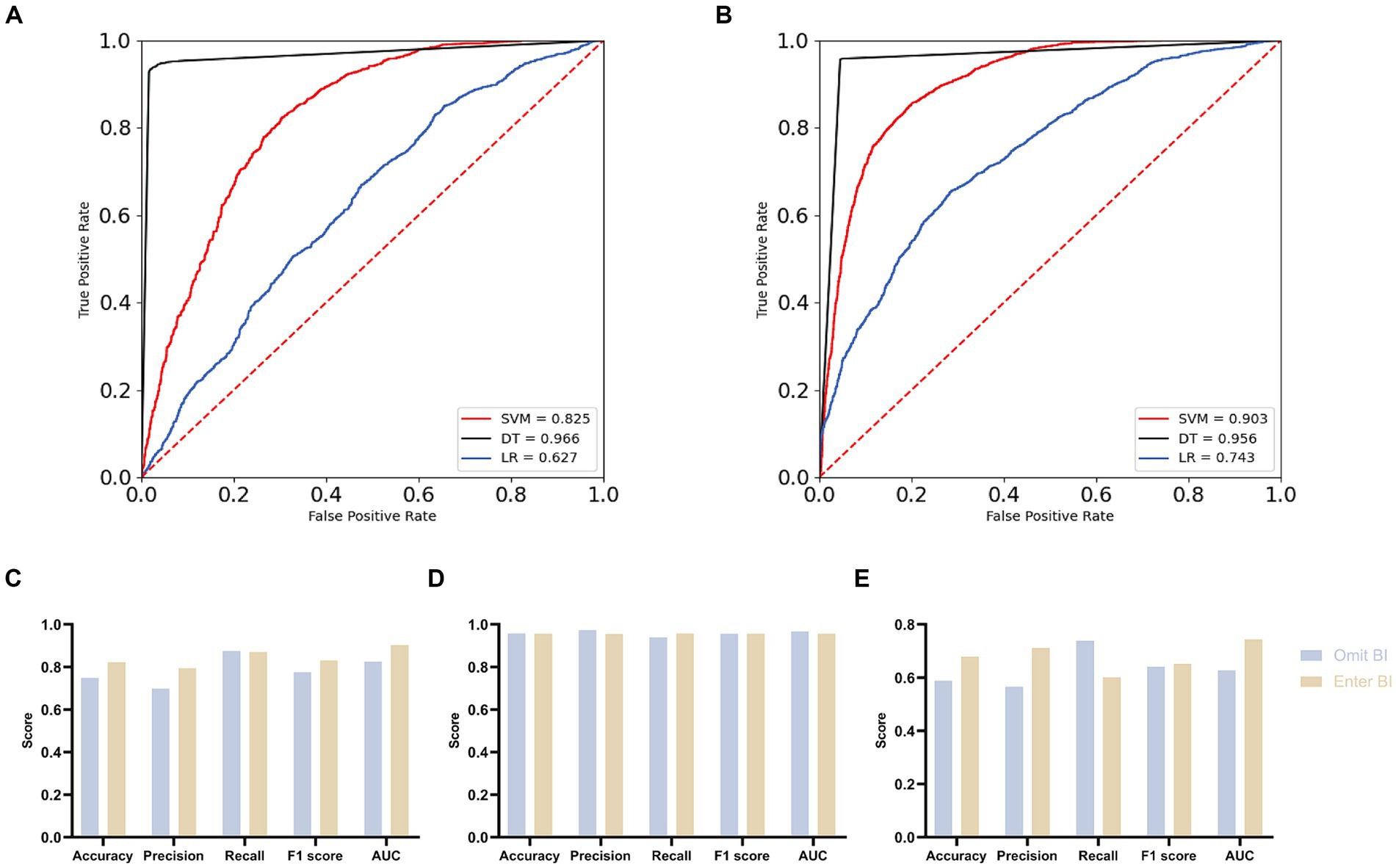
Figure 2. Comparison of overall effects of machine learning algorithms for two distinct datasets. (A) ROC curves with AUC for omit Barthel index group. (B) ROC curves with AUC for enter Barthel index group. (C) Contrasting the SVM model across the two groups. (D) Contrasting the DT model across the two groups. (E) Contrasting the LR model across the two groups.
All three machine learning algorithms verified the association between ADL and EPs and affirmed the positive role of BI in overall prediction, enhancing model performance. The validation of machine learning algorithms confirms our finding that impaired daily living abilities increase susceptibility to EPs.
4 Discussion
Amidst the ongoing global aging population phenomenon (40), the potential hazards of EPs among middle-aged and older adult individuals are gradually gaining attention. EPs may arise from psychological discrepancies associated with aging and are often concomitant with certain diseases (41). The exacerbation of global aging has led to increased feelings of loneliness among the older adult, coupled with the disregard for psychological well-being and emotional stability by individuals and families, thereby fostering the proliferation of EPs (42, 43). Hence, early detection and intervention for the complex factors contributing to EPs become particularly imperative.
In this study, we commenced by conducting demographic analyses of the individuals included in the research cohort. We observed disparities in the mean BI scores between cohorts afflicted with EPs and those without EPs, with the former exhibiting lower mean BI scores compared to the latter. Subsequently, utilizing Pearson correlation analysis, we established a negative correlation between ADL and EPs. Subsequent to this, employing iterative iterations of three distinct models, we conducted stratified multivariate linear regression. Even after controlling for covariates such as age, gender, residency, education, smoking and drinking status, and chronic diseases, a significant negative correlation between ADL and EPs persisted. Furthermore, machine learning algorithms validated our findings. In experiments utilizing solely BI data, the AUC scores of all three machine learning algorithms exceeded 0.7, indicating diagnostic value. In the subsequent experiments involving two groups—one with additional covariates and another with additional covariates plus BI—the inclusion of BI resulted in an overall enhancement of the predictive performance of machine learning algorithms. Particularly noteworthy was the notable improvement observed in the predictive performance of SVM when BI was added. This underscores the positive influence of BI on the predictive capabilities of machine learning algorithms, thus corroborating our findings that ADL impairment heightens susceptibility to EPs.
This study also conducted an analysis of other covariates. In the examination of demographic characteristics and Pearson correlation, gender, smoking and drinking status, hypertension, and dyslipidemia exhibited statistically significant differences between the EPs and non-EPs groups and were all significantly positively correlated with EPs. Specifically, females were more prone to EPs, while individuals with hypertension and dyslipidemia were also more susceptible to EPs, consistent with previous research findings (44–48). However, regarding smoking and drinking status, the results of this study showed that individuals who smoked less and drank less frequently were more susceptible to EPs, contradicting previous studies. We attribute this discrepancy to the higher proportion of female individuals in this study, as generally, fewer Chinese females have habits of smoking and drinking in daily life (49, 50). Additionally, studies have reported that acetylcholine contributes to regulating brain homeostasis and shaping synaptic neuron transmission and neurotransmitter levels (51). Nicotine may improve mood and alleviate anxiety by increasing acetylcholine release and the number of nicotinic receptors (52). As for other covariates such as residence and education level in this study, their definitions cannot be simply delineated through basic demographic characteristics and Pearson correlation analysis. These factors, as potential influencers of EPs, may require joint analysis with various socio-economic factors such as offspring support, retirement pensions, family migration, childhood experiences, etc., to derive more scientifically sound conclusions (53).
This study identified a significant negative correlation between ADL and EPs, which remained stable even after adjusting for other covariates, a relationship confirmed by machine learning algorithms. Therefore, emphasizing the importance of exercise for the older adults in daily life activities is crucial. Encouraging the older adults to improve ADL in community healthcare and home care settings serves as a preventive measure against EPs and ensures a better quality of life, forming the basis for quality longevity (54, 55). In the process of disease rehabilitation, such as stroke, timely restoration of ADL in patients is conducive to their psychological well-being post-illness and enhances their confidence in recovery (56, 57).
Nevertheless, this study has limitations. Its cross-sectional design precludes longitudinal exploration, hindering causal relationship establishment between ADL and EPs. Declining ADL may signify a symptom rather than a causative factor in EPs progression, inferring only a significant negative correlation between ADL and EPs. CHARLS data, collected annually, lacks precise diagnosis timings, constraining causal relationship determination. Future longitudinal studies are vital for robust evidence. Relying on “Diagnosed with Emotional Problems by a Doctor” in CHARLS, lacking detailed emotional problem classification such as Posttraumatic Stress Disorder (PTSD) and Generalized Anxiety Disorder (GAD), is another limitation. Enhancing understanding requires comprehensive emotional health assessments. Despite significant ADL-EPs correlation, predictive utility of ADL alone is limited; exploring sleep quality, social support, socioeconomic status, and chronic stress is needed to enhance predictive accuracy. Additionally, the small proportion (2.32%) of individuals diagnosed with EPs may introduce bias. Despite utilizing Synthetic Minority Over-sampling Technique(SMOTE) to address class imbalance, future studies should explore advanced techniques like stratified sampling or ensemble learning algorithms to improve result reliability. Although we examined three machine learning algorithms, further investigation is warranted for optimal predictive model identification. Nonetheless, our study’s predictive capacity remains significant (58, 59).. Furthermore, BI, derived from self-reported scales in the CHARLS dataset, differs from clinical assessments. However, literature supports the reliability of self-reported ADL assessments, validating our approach (60–62).
5 Conclusion
This study employs various statistical methods to reveal a negative correlation between ADL and EPs. Furthermore, the utilization of machine learning algorithms confirms this finding, indicating that impaired ADL heightens susceptibility to EPs.
5.1 Summary
Emotional Problems (EPs) have become a significant challenge affecting the quality of life in middle-aged and older adult populations, garnering increasing attention in public health. Early detection of potential EPs among middle-aged and older adults is crucial. This study explores the potential of Activities of Daily Living (ADL) as predictive indicators for EPs. Using data from the 2018 China Health and Retirement Longitudinal Study (CHARLS) national baseline survey, which includes 9,766 individuals aged 45 and above, we assessed ADL using the Barthel Index (BI). Statistical analyses were conducted to investigate the correlation between ADL and EPs, followed by validation using machine learning algorithms (Support Vector Machine, Decision Tree, and Logistic Regression) to elucidate the underlying relationship between ADL and EPs.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the National School of Development at Peking University (http://charls.pku.edu.cn). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
MG: Conceptualization, Data curation, Writing – original draft, Formal analysis, Investigation, Methodology. SX: Methodology, Software, Validation, Writing – original draft. XH: Data curation, Investigation, Supervision, Writing – original draft. JH: Methodology, Software, Validation, Writing – original draft. HY: Conceptualization, Formal analysis, Project administration, Resources, Writing – review & editing. LZ: Conceptualization, Formal analysis, Funding acquisition, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from National Natural Science Foundation of China (82060863), Science and technology projects of Guizhou Province (Qiankeheji-zk [2021] General 500), Research project of the Second Affiliated Hospital of Guizhou University of TCM GZEYK [2020]11, Research project of Guizhou University of Traditional Chinese Medicine [2019]20, Traditional Chinese Medicine and Ethnic Medicine Science and Technology Research Special Project of Guizhou Province (QZYY-2024-068).
Acknowledgments
I thank LZ for his helpful suggestion.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1391033/full#supplementary-material
Footnotes
References
1. Cheng, S-T, and Siankam, B. The impacts of the HIV/AIDS pandemic and socioeconomic development on the living arrangements of older persons in sub-Saharan Africa: a country-level analysis. Am J Community Psychol. (2009) 44:136–47. doi: 10.1007/s10464-009-9243-y
2. Diego, DL . Late-life suicide in an aging world. Nature aging. (2022) 2:7–12. doi: 10.1038/s43587-021-00160-1
3. Cai, H, Jin, Y, Liu, R, Zhang, Q, Su, Z, Ungvari, GS, et al. Global prevalence of depression in older adults: a systematic review and meta-analysis of epidemiological surveys. Asian J Psychiatr. (2023) 80:103417. doi: 10.1016/j.ajp.2022.103417
4. Zhao, J, Liu, YWJ, Tyrovolas, S, and Mutz, J. Exploring the concept of psychological frailty in older adults: a systematic scoping review. J Clin Epidemiol. (2023) 159:300–8. doi: 10.1016/j.jclinepi.2023.05.005
5. Jang, S, Numbers, K, Lam, BCP, Sachdev, PS, Brodaty, H, and Reppermund, S. Performance-based vs informant-reported instrumental activities of daily living in predicting dementia. J Am Med Dir Assoc. (2022) 23:1342–1347.e9. doi: 10.1016/j.jamda.2021.09.020
6. He, J, Wang, W, Wang, S, Guo, M, Song, Z, and Cheng, S. Taking precautions in advance: a lower level of activities of daily living may be associated with a higher likelihood of memory-related diseases. Front Public Health. (2023) 11:1293134. doi: 10.3389/fpubh.2023.1293134
7. Hill, NL, Mogle, J, Wion, R, Munoz, E, DePasquale, N, Yevchak, AM, et al. Subjective cognitive impairment and affective symptoms: a systematic review. The Gerontologist. (2016) 56:e109–27. doi: 10.1093/geront/gnw091
8. Fernandes, E, and Stéfani, C. Emotional problems and health-related quality of life: population-based study. Qual Life Res Int J Qual Life Asp Treat Care Rehab. (2019) 28:3037–46. doi: 10.1007/s11136-019-02230-9
9. Hu, T, Zhao, X, Wu, M, Li, Z, Luo, L, Yang, C, et al. Prevalence of depression in older adults: a systematic review and meta-analysis. Psychiatry Res. (2022) 311:114511. doi: 10.1016/j.psychres.2022.114511
10. Verhoeven, JE, Révész, D, Picard, M, Epel, EE, Wolkowitz, OM, Matthews, KA, et al. Depression, telomeres and mitochondrial DNA: between-and within-person associations from a 10-year longitudinal study. Mol Psychiatry. (2018) 23:850–7. doi: 10.1038/mp.2017.48
11. Bebbington, P . Losing the thread: experiences of cognitive decline in Alzheimer's disease. Br J Psychiatry J Ment Sci. (2023) 222:151–2. doi: 10.1192/bjp.2022.184
12. Patten, SB, Williams, JVA, Lavorato, DH, Wang, JL, Jetté, N, Sajobi, TT, et al. Patterns of association of chronic medical conditions and major depression. Epidemiol Psychiatr Sci. (2018) 27:42–50. doi: 10.1017/S204579601600072X
13. Surkalim, DL, Clare, PJ, Eres, R, Gebel, K, Bauman, A, and Ding, D. Have middle-aged and older Americans become lonelier? 20-year trends from the health and retirement study. J Gerontol B Psychol Sci Soc Sci. (2023) 78:1215–23. doi: 10.1093/geronb/gbad062
14. Pinz, MP, Vogt, AG, da Costa Rodrigues, K, dos Reis, AS, Duarte, LFB, Fronza, MG, et al. Effect of a purine derivative containing selenium to improve memory decline and anxiety through modulation of the cholinergic system and na+/K+-ATPase in an Alzheimer's disease model. Metab Brain Dis. (2021) 36:871–88. doi: 10.1007/s11011-021-00703-w
15. Prévot, T, and Sibille, E. Altered GABA-mediated information processing and cognitive dysfunctions in depression and other brain disorders. Mol Psychiatry. (2021) 26:151–67. doi: 10.1038/s41380-020-0727-3
16. Blomgren, C, Samuelsson, H, Blomstrand, C, Jern, C, Jood, K, and Claesson, L. Long-term performance of instrumental activities of daily living in young and middle-aged stroke survivors-impact of cognitive dysfunction, emotional problems and fatigue. PLoS One. (2019) 14:e0216822. doi: 10.1371/journal.pone.0216822
17. Empana, J-P, Boutouyrie, P, Lemogne, C, Jouven, X, and van Sloten, TT. Microvascular contribution to late-onset depression: mechanisms, current evidence, association with other brain diseases, and therapeutic perspectives. Biol Psychiatry. (2021) 90:214–25. doi: 10.1016/j.biopsych.2021.04.012
18. Gold, DA . An examination of instrumental activities of daily living assessment in older adults and mild cognitive impairment. J Clin Exp Neuropsychol. (2012) 34:11–34. doi: 10.1080/13803395.2011.614598
19. Gambaro, E, Gramaglia, C, Azzolina, D, Campani, D, Molin, AD, and Zeppegno, P. The complex associations between late life depression, fear of falling and risk of falls. A systematic review and meta-analysis. Ageing Res Rev. (2022) 73:101532. doi: 10.1016/j.arr.2021.101532
20. Xiao, S, Shi, L, Dong, F, Zheng, X, Xue, Y, Zhang, J, et al. The impact of chronic diseases on psychological distress among the older adults: the mediating and moderating role of activities of daily living and perceived social support. Aging Ment Health. (2022) 26:1798–804. doi: 10.1080/13607863.2021.1947965
21. Yu, DS-F, Li, P W-c, Lin, RS-Y, Kee, F, Chiu, A, and Wu, W. Effects of non-pharmacological interventions on loneliness among community-dwelling older adults: a systematic review, network meta-analysis, and meta-regression. Int J Nurs Stud. (2023) 144:104524. doi: 10.1016/j.ijnurstu.2023.104524
22. Li, J, Yang, L, Lv, R, Kuang, J, Zhou, K, and Xu, M. Mediating effect of post-stroke depression between activities of daily living and health-related quality of life: meta-analytic structural equation modeling. Qual Life Res Int J Qual Life Asp Treat Care Rehab. (2023) 32:331–8. doi: 10.1007/s11136-022-03225-9
23. Legg, LA, Lewis, SR, Schofield-Robinson, OJ, Drummond, A, and Langhorne, P. Occupational therapy for adults with problems in activities of daily living after stroke. Cochrane Database Syst Rev. (2023) 2017:CD003585. doi: 10.1002/14651858.CD003585.pub3
24. Zhao, Y, Hu, Y, Smith, JP, Strauss, J, and Yang, G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
25. Shah, S, Vanclay, F, and Cooper, B. Improving the sensitivity of the Barthel index for stroke rehabilitation. J Clin Epidemiol. (1989) 42:703–9. doi: 10.1016/0895-4356(89)90065-6
26. Wang, E, Liu, A, Wang, Z, Shang, X, Zhang, L, Jin, Y, et al. The prognostic value of the Barthel index for mortality in patients with COVID-19: a cross-sectional study. Front Public Health. (2023) 10:978237. doi: 10.3389/fpubh.2022.978237
27. Dos Santos, BV, Bassi-Dibai, D, Guedes, CLR, Morais, DN, Coutinho, SM, de Oliveira, SG, et al. Barthel index is a valid and reliable tool to measure the functional independence of cancer patients in palliative care. BMC Palliat Care. (2022) 21:124. doi: 10.1186/s12904-022-01017-z
28. Liu, LS . Writing group of 2010 Chinese guidelines for the Management of Hypertension. [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi. (2011) 39:579–615.
29. Joint committee issued Chinese guideline for the management of dyslipidemia in adults. Chinese guideline for the management of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi. (2016) 44:833–53. doi: 10.3760/cma.j.issn.0253-3758.2016.10.005
32. Luna, JM, Gennatas, ED, Ungar, LH, Eaton, E, Diffenderfer, ES, Jensen, ST, et al. Building more accurate decision trees with the additive tree. Proceeding National Acad of Sci United States of America. (2019) 116:19887–93. doi: 10.1073/pnas.1816748116
33. Shirali, GA, Noroozi, MV, and Malehi, AS. Predicting the outcome of occupational accidents by CART and CHAID methods at a steel factory in Iran. J Public Health Res. (2018) 7:1361. doi: 10.4081/jphr.2018.1361
34. Turcato, G, Zaboli, A, Pfeifer, N, Maccagnani, A, Tenci, A, Giudiceandrea, A, et al. Decision tree analysis to predict the risk of intracranial haemorrhage after mild traumatic brain injury in patients taking DOACs. Am J Emerg Med. (2021) 50:388–93. doi: 10.1016/j.ajem.2021.08.048
35. Bayman, EO, and Dexter, F. Multicollinearity in logistic regression models. Anesth Analg. (2021) 133:362–5. doi: 10.1213/ANE.0000000000005593
36. Meurer, WJ, and Tolles, J. Logistic regression diagnostics: understanding how well a model predicts outcomes. JAMA. (2017) 317:1068–9. doi: 10.1001/jama.2016.20441
37. LaValley, MP . Logistic regression. Circulation. (2008) 117:2395–9. doi: 10.1161/CIRCULATIONAHA.106.682658
38. Wang, J, Chen, H, Wang, H, Liu, W, Peng, D, Zhao, Q, et al. A risk prediction model for physical restraints among older Chinese adults in long-term care facilities: machine learning study. J Med Internet Res. (2023) 25:e43815. doi: 10.2196/43815
39. Luya, L . Deep Learning for Caries Detection and Classification. Diagnostics (Basel, Switzerland). (2021) 11:1672. doi: 10.3390/diagnostics11091672
40. Dogra, S, Dunstan, DW, Sugiyama, T, Stathi, A, Gardiner, PA, and Owen, N. Active aging and public health: evidence, implications, and opportunities. Annu Rev Public Health. (2022) 43:439–59. doi: 10.1146/annurev-publhealth-052620-091107
41. John, A, Patel, U, Rusted, J, Richards, M, and Gaysina, D. Affective problems and decline in cognitive state in older adults: a systematic review and meta-analysis. Psychol Med. (2019) 49:353–65. doi: 10.1017/S0033291718001137
42. Lee, SL, Pearce, E, Ajnakina, O, Johnson, S, Lewis, G, Mann, F, et al. The association between loneliness and depressive symptoms among adults aged 50 years and older: a 12-year population-based cohort study. Lancet Psychiatry. (2021) 8:48–57. doi: 10.1016/S2215-0366(20)30383-7
43. Steptoe, A, Shankar, A, Demakakos, P, and Wardle, J. Social isolation, loneliness, and all-cause mortality in older men and women. Proceed National Acad Sci United States of America. (2013) 110:5797–801. doi: 10.1073/pnas.1219686110
44. Sundström-Poromaa, I, Comasco, E, Sumner, R, and Luders, E. Progesterone-Friend or foe? Front Neuroendocrinol. (2020) 59:100856. doi: 10.1016/j.yfrne.2020.100856
45. Foster, KT, and Beltz, AM. Heterogeneity in affective complexity among men and women. Emotion (Washington, DC). (2022) 22:1815–27. doi: 10.1037/emo0000956
46. Cai, Y, Chen, M, Zhai, W, and Wang, C. Interaction between trouble sleeping and depression on hypertension in the NHANES 2005-2018. BMC Public Health. (2022) 22:481. doi: 10.1186/s12889-022-12942-2
47. Bergantin, LB . Depression rises the risk of hypertension incidence: discussing the link through the Ca2+/cAMP signalling. Curr Hypertens Rev. (2020) 16:73–8. doi: 10.2174/1573402115666190116095223
48. Xu, L, Wang, K, Wang, S, Liu, L, Lv, X, and Song, Y. Sex differences in the association between serum lipids and depressive symptoms: a longitudinal population-based study. J Affect Disord. (2021) 291:154–62. doi: 10.1016/j.jad.2021.05.011
50. Chen, H, Zhang, X, Feng, Q, and Zeng, Y. The effects of "diet-smoking-gender" three-way interactions on cognitive impairment among Chinese older adults. Nutrients. (2022) 14:2144. doi: 10.3390/nu14102144
51. Garofalo, S, Cocozza, G, Mormino, A, Bernardini, G, Russo, E, Ielpo, D, et al. Natural killer cells and innate lymphoid cells 1 tune anxiety-like behavior and memory in mice via interferon-γ and acetylcholine. Nat Commun. (2023) 14:3103. doi: 10.1038/s41467-023-38899-3
52. Terry, AV, and Callahan, PM. Nicotinic acetylcholine receptor ligands, cognitive function, and preclinical approaches to drug discovery. Nicotine Tob Res Off J Soc Res Nicotine Tob. (2019) 21:383–94. doi: 10.1093/ntr/nty166
53. Lebrusán, I, and Gómez, MV. The importance of place attachment in the understanding of ageing in place: "the stones know me". Int J Environ Res Public Health. (2022) 19:17052. doi: 10.3390/ijerph192417052
54. Almeida, OP, Yeap, BB, Hankey, GJ, Golledge, J, and Flicker, L. Association of depression with sexual and daily activities: a community study of octogenarian men. American J geriatric psychiatry: official J American Association for Geriatric Psychiatry. (2015) 23:234–42. doi: 10.1016/j.jagp.2013.09.007
55. Orgeta, V, Leung, P, del-Pino-Casado, R, Qazi, A, Orrell, M, Spector, AE, et al. Psychological treatments for depression and anxiety in dementia and mild cognitive impairment. Cochrane Database Syst Rev. (2022) 2022:CD009125. doi: 10.1002/14651858.CD009125.pub3
56. Haghgoo, HA, Pazuki, ES, Hosseini, AS, and Rassafiani, M. Depression, activities of daily living and quality of life in patients with stroke. J Neurol Sci. (2013) 328:87–91. doi: 10.1016/j.jns.2013.02.027
57. Zahuranec, DB, Skolarus, LE, Feng, C, Freedman, VA, and Burke, JF. Activity limitations and subjective well-being after stroke. Neurology. (2017) 89:944–50. doi: 10.1212/WNL.0000000000004286
58. Handelman, GS, Kok, HK, Chandra, RV, Razavi, AH, Lee, MJ, and Asadi, H. eDoctor: machine learning and the future of medicine. J Intern Med. (2018) 284:603–19. doi: 10.1111/joim.12822
59. Sohail, A, and Arif, F. Supervised and unsupervised algorithms for bioinformatics and data science. Prog Biophys Mol Biol. (2020) 151:14–22. doi: 10.1016/j.pbiomolbio.2019.11.012
60. O’Connell, J, Henman, MC, Burke, É, Donegan, C, McCallion, P, McCarron, M, et al. Association of Drug Burden Index with grip strength, timed up and go and Barthel index activities of daily living in older adults with intellectual disabilities: an observational cross-sectional study. BMC Geriatr. (2019) 19:173. doi: 10.1186/s12877-019-1190-3
61. Ma, Y, Deng, K, Liu, J, Ma, B, Mei, F, Hui, W, et al. The add-on effects of Danhong injection among patients with ischemic stroke receiving Western medicines: a systematic review and meta-analysis. Front Pharmacol. (2022) 13:937369. doi: 10.3389/fphar.2022.937369
Keywords: activities of daily living (ADL), emotional problems (EPs), machine learning algorithm, the China health and retirement longitudinal survey (CHARLS), Barthel index (BI), support vector machine (SVM), decision tree (DT), logistic regression (LR)
Citation: Guo M, Xu S, He X, He J, Yang H and Zhang L (2024) Decoding emotional resilience in aging: unveiling the interplay between daily functioning and emotional health. Front. Public Health. 12:1391033. doi: 10.3389/fpubh.2024.1391033
Edited by:
Yunhwan Lee, Ajou University, Republic of KoreaReviewed by:
Andrea C. Medina, National Autonomous University of Mexico, MexicoNeha Sinha, CHDI Foundation, United States
Copyright © 2024 Guo, Xu, He, He, Yang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lin Zhang, ZG9jdG9yemhhbmdsaW4wMUAxNjMuY29t; Hui Yang, eWh1aWh1aTIwMDRAMTYzLmNvbQ==
 Minhua Guo
Minhua Guo Songyang Xu
Songyang Xu Xiaofang He4
Xiaofang He4 Jiawei He
Jiawei He Lin Zhang
Lin Zhang