- 1Department of Psychology, Stanford University, Stanford, CA, United States
- 2Department of Epidemiology and Population Health, Stanford University, Stanford, CA, United States
- 3University Hospital of Basel, Outpatient Medical Clinic, Basel, Switzerland
- 4Centre of Competence for Military and Disaster Medicine, Swiss Armed Forces, Bern, Switzerland
- 5Division of Diabetes, Endocrinology, Nutritional Medicine and Metabolism, University Hospital and University of Bern, Bern, Switzerland
- 6Psychiatric Hospital of the University of Basel, Basel, Switzerland
- 7Department of Psychology, Arizona State University, Tempe, AZ, United States
- 8Department of Psychology, Old Dominion University, Norfolk, VA, United States
- 9Psychiatric Hospital of the University of Basel, Center for Affective, Stress and Sleep Disorders, Basel, Switzerland
- 10Division of Sport Science and Psychosocial Health, Department of Sport, Exercise and Health, University of Basel, Basel, Switzerland
- 11Center of Military Disaster Psychiatry and Disaster Psychology, Psychiatric Hospital of the University of Basel, Basel, Switzerland
Background: Compared to civilians and non-medical personnel, military medical doctors are at increased risk for sleep disturbances and impaired psychological well-being. Despite their responsibility and workload, no research has examined sleep disturbances and psychological well-being among the medical doctors (MDs) of the Swiss Armed Forces (SAF). Thus, the aims of the proposed study are (1) to conduct a cross-sectional study (labeled ‘Survey-Study 1’) of sleep disturbances and psychological well-being among MDs of the SAF; (2) to identify MDs who report sleep disturbances (insomnia severity index >8), along with low psychological well-being such as symptoms of depression, anxiety and stress, but also emotion regulation, concentration, social life, strengths and difficulties, and mental toughness both in the private/professional and military context and (3) to offer those MDs with sleep disturbances an evidence-based and standardized online interventional group program of cognitive behavioral therapy for insomnia (eCBTi) over a time lapse of 6 weeks (labeled ‘Intervention-Study 2’).
Method: All MDs serving in the SAF (N = 480) will be contacted via the SAF-secured communication system to participate in a cross-sectional survey of sleep disturbances and psychological well-being (‘Survey-Study 1’). Those who consent will be provided a link to a secure online survey that assesses sleep disturbances and psychological well-being (depression, anxiety, stress, coping), including current working conditions, job-related quality of life, mental toughness, social context, family/couple functioning, substance use, and physical activity patterns. Baseline data will be screened to identify those MDs who report sleep disturbances (insomnia severity index >8); they will be re-contacted, consented, and randomly assigned either to the eCBTi or the active control condition (ACC) (‘Intervention-Study 2’). Individuals in the intervention condition will participate in an online standardized and evidence-based group intervention program of cognitive behavioral therapy for insomnia (eCBTi; once the week for six consecutive weeks; 60–70 min duration/session). Participants in the ACC will participate in an online group counseling (once the week for six consecutive weeks; 60–70 min duration/session), though, the ACC is not intended as a bona fide psychotherapeutic intervention. At the beginning of the intervention (baseline), at week 3, and at week 6 (post-intervention) participants complete a series of self-rating questionnaires as for the Survey-Study 1, though with additional questionnaires covering sleep-related cognitions, experiential avoidance, and dimensions of self-awareness.
Expected outcomes: Survey-Study 1: We expect to describe the prevalence rates of, and the associations between sleep disturbances (insomnia (sleep quality); sleep onset latency (SOL); awakenings after sleep onset (WASO)) and psychological well-being among MDs of the SAF; we further expect to identify specific dimensions of psychological well-being, which might be rather associated or non-associated with sleep disturbances.
Intervention-Study 2: We expect several significant condition-by-time-interactions. Such that participants in the eCBTi will report significantly greater improvement in sleep disturbances, symptoms of depression, anxiety, stress reduction both at work and at home (family related stress), and an improvement in the overall quality of life as compared to the ACC over the period of the study.
Conclusion: The study offers the opportunity to understand the prevalence of sleep disturbances, including factors of psychological well-being among MDs of the SAF. Further, based on the results of the Intervention-Study 2, and if supported, eCBTi may be a promising method to address sleep disturbances and psychological well-being among the specific context of MDs in the SAF.
1 Introduction
Findings from cross-sectional and longitudinal studies demonstrated that restorative sleep is associated with a broad variety of health benefits, including emotional and cognitive benefits and specifically, less impulsivity, enhanced driving behavior in traffic, and better social interactions. By contrast, poor sleep is associated with symptoms of depression and anxiety (1–12), low impulse control (13, 14), non-suicidal self-injury and suicidal behavior (10, 12, 15–20), impaired cognitive and emotional processing (21–36), reckless or aggressive driving behavior (37–44), and impaired social behavior (45, 46).
For short, findings from cross-sectional and longitudinal studies among children, adolescents, and adults and from non-clinical and clinical samples consistently demonstrated that impaired sleep is associated with a broad range of psychological issues on well-being, including cognitive, emotional, and social behavior problems.
1.1 Sleep disturbances and psychological well-being among medical doctors
Medical doctors (MDs) are at increased risk of mental health issues due to low sleep quality, irregular sleeping schedules, increased latency in falling asleep and increased frequency of sleep interruptions (47–51). These issues may lead to symptoms of depression, anxiety (47–54) and burnout (54–59). To explain such impairments among MDs, research has identified long and irregular working hours, irregular sleep schedules (52, 60, 61) and stress (48, 54, 58, 59, 62–64) as main drivers associated with sleep disturbances. Given these associations, in the present study, our focus is on sleep disturbances and psychological well-being among MDs, though, among MDs in the context of the Swiss military (Swiss Armed Forces).
1.2 Sleep disturbances among military personnel
There is sufficient evidence that compared to non-military personnel, military personnel report more sleep disturbances, in that military personnel have specific and unique work-related demands and work and life style patterns (65). Bai et al. (66) reported a number of factors that may increase sleep disturbances, especially during military operations. These include frequent involvement in high-risk activities (67), context-specific standards (65), misalignments of stable sleep–wake-rhythms, such as a disruptive sleep environment, concerns about family issues back home (68), sustained operations, excessive caffeine intake, along with the exposure to physical and psychological injuries (69). Mantua et al. (70) investigated the associations between sleep patterns and high-risk behavior among 2,296 deployed military personnel (mean age 24.7 years) and concluded that sufficient and restorative sleep may decrease poor or risky decision making in the context of military duty.
Bai et al. (66) conducted a systematic review and meta-analysis of 59 studies with a total of 28,100 participants (Ns = 14 to 8,481) involving military and veteran participants. Bai et al. (66) calculated that the overall pooled prevalence of sleep disturbances in military personnel and veterans was 69.00% (95% CI: 62.33–75.30%); pooled rates were 57.79% (95% CI: 49.88–65.50%) for active-duty personnel, and 82.88% (95% CI: 74.08–90.21%) for veterans. Further, a higher mean age, and the occurrence of symptoms of depression and posttraumatic stress disorder (PTSD) were associated with higher prevalence rates of impaired sleep. Crane et al. (71) investigated the professional and private re-integration of military personnel after their military deployment and identified adequate and restoring sleep as a key variable causally related to a favorable post-deployment process. Further factors conferring to a more successful post-deployment process were: Lower scores for shame, guilt, and negative cognitive appraisal, along with a higher motivation to deploy successfully predicted a favorable outcome in the post-deployment phase.
1.3 Sleep disturbances among medical doctors in the military context
Regarding sleep disturbances among military MDs, research is scarce, and consistent data are lacking. Hsu et al. (72) observed that among 1,003 US Army physicians just 25% of respondents were adherent to the recommended 8 h sleep per day. When following the recommended 8 h sleep per day, about 28.4% reported a positive response to this regimen. Better sleep was associated with being a staff physician (compared to being a physician in training), and working fewer hours/week.
In a systematic review (73) summarizing 14 publications on military physicians’ sleep and professional performance, it turned out that sleep deprivation in any ‘out-of-hours’ surgery had a significant impact on overall morbidity and mortality. Sleep deprivation in surgeons and surgical trainees did negatively impact on their cognitive performance, putting their own and patients’ health at risk. More specifically, forward surgical teams will become combat-ineffective after 48 h of continuous operations (73). In a simulation study with 77 medical personnel of the Air National Guard (a federal military reserve force of the United States Air Force) it turned out that participants’ sleep quantity significantly decreased from civilian to disaster-training periods, while their cognitive performance decreased in parallel (74). In a sample of 344 medical staff members deployed to Afghanistan, they reported significantly higher levels of burnout and stress, compared to other professions (75). Adler et al. (75) did not specifically assess sleep quality or quantity; however, based on previous studies on the relation between poor sleep and increased stress (48, 62, 71, 76), we may assume that these 344 medical staff members would have reported higher scores for sleep disturbances.
Last, the National Guard (NG) served as critical component of the US COVID-19 response. A total of 3,221 NG service members were surveyed after their service in response of the COVID-19 (mean duration: 18.6 weeks). Over one-third reported changes in usual sleep: 33% described poor sleep quality, and 21% had troubles falling or staying asleep (77). This study is important in that it described the sudden shift from civil life to military life, and such sudden shifts are often observed among personnel of the SAF, in general, and among MDs of the SAF, more specifically.
Given this background, one aim of the present study was to investigate the prevalence rates of sleep disturbances (insomnia; disrupted sleep continuity) among MDs of the Swiss Armed Forces (SAF; see details below).
1.4 Treatment of insomnia with cognitive behavioral therapy
To treat insomnia, specifically tailored CBT-interventions were established and standardized (CBTi). After a standardized and one-day long CBTi intervention, individuals with insomnia with no further mental health issues and randomly assigned to the intervention improved in their insomnia scores (78), compared to a wait-list condition. Results from meta-analyses (79–85) showed that compared to wait list or control conditions, CBTi delivered to clinical and non-clinical samples of children, adolescents and adults was always superior.
In the same vein, randomized clinical trials, and systematic review and meta-analyses evidenced that online-delivered CBTi programs (eCBTi) were as effective as ‘real’ and face-to-face CBTi interventions (86–92).
As for now, we are unaware of any eCBTi intervention to improve sleep disturbances among MDs in the military context. Given this, Intervention-Study 2 aims at investigating the feasibility and impact of a standardized eCBTi intervention on MDs of the SAF, compared to an active control condition (ACC).
1.5 The specific context of the Swiss Armed Forces
In Switzerland, military service is mandatory for men. After basic training the most skilled recruits continue on a voluntary basis their training as cadre. After training in the non-commissioned officers’ school, the 15 weeks long officers’ school (OS) begins. This is considered to be stressful and demanding, both physically and mentally. The cadets are pushed to their limits every day during the extraordinarily intensive training. Importantly, male and female Swiss MDs in particular are encouraged to pursue the military career as military physicians.
Next, a unique aspect of the SAF is the high permeability between military and civil life. More specifically, throughout the basic military training, officers’ school, and during their annual courses, exercise trainings and refresher courses military personnel usually return home for weekends. Further, once an officer has achieved her/his rankings, annual courses and exercise trainings lasting for several days to up to 4 weeks per year are possible. At a behavioral and practical level, this implies that military MDs may switch between their private/professional and military deployments throughout their military service. Thus, the boundaries between private/civil/professional life and military life might get blurred, with quick and sometimes unpredictable transitions from civil/private/professional life to military deployments and vice versa. Such sudden changes may add to sleep disturbances. Until this date, we are unaware of studies on sleep disturbances, along with psychological well-being among MDs of the SAF. Given this, the present study aims at filling this gap of knowledge. Please consider that for the present study, exclusively medical doctors after their final exam (master’s degree) at a university were included, while officers, who did not yet complete the university degree as medical doctors were not considered.
1.6 The concepts of the transdiagnostic approach and of allostatic load
Within the last decade two psychiatric and cognitive-behavioral concepts have gained increased attention as explanations for why the effective treatment of a specific psychiatric disorder leads to improvements in other psychiatric conditions. To illustrate, treating symptoms of insomnia also improved symptoms of depression (93), anxiety, and stress (94–99). To explain this phenomenon, the concept of the transdiagnostic approach (97, 100–109) reflects the observation that improvements in one dimension of psychological experiences are associated with improvements in further dimensions of psychological experiences. Moreover, a meta-analysis on the treatment of anxiety disorders did not observe systematic differences between a disorders-specific cognitive-behavioral therapy (CBT) and a transdiagnostic CBT (tCBT) (108). Further, no associations between the comorbidity rate and tCBT outcome were observed. Likewise, Brand et al. (110) showed that acute bouts of physical activity impacted positively on mood, social interaction, and rumination among inpatients with psychiatric impairments, fully irrespective from patients’ psychiatric diagnosis.
Next, the concept of allostatic load (111–114) may help explain the improvements of non-specific benefits of CBT. Allostatic load is understood as the cumulative effects of stressful experiences in daily life, and such an alostatic load may lead to both a physiological and psychological strain over time. Thus, it is conceivable that improvements in sleep disturbances may improve symptoms of depression, anxiety and stress, in parallel.
1.7 The present study
Overall, there is sufficient evidence that compared to non-military personnel, military personnel report more impaired sleep, along with more issues of psychological well-being. This holds particularly true for MDs in the military context, though, research on this topic is scarce. More specifically, for MDs of the SAF, no research is available on the prevalence and association of sleep disturbances, along with concomitant issues of psychological wellbeing.
Given this background, the present study has the following aims:
Survey-Study 1: (1) To investigate the prevalence of sleep disturbances (insomnia; disrupted sleep continuity), and concomitant issues of psychological well-being among MDs of the SAF. (2) To investigate the patterns of associtions between sleep disturbances and issues of psychological well-being; (3) to identify MDs who report sleep disturbances (insomnia severity index >8), along with further dimensions of psychological ill-being and well-being such as symptoms of depression, anxiety, stress, emotion regulation, concentration, social activity, strengths and difficulties and mental toughness.
Intervention-Study 2: (3) To offer a stanrdardized online CBT program for insomnia (eCBTi). To this end, MDs reporting sleep disturbances will be randomly assigned either to the internvention condition (see details below) or to the active control condition (see details below).
For the Survey-Study 1, the hypothesis is: Higher scores for sleep disturbances are associated with more issues of psychological wellbeing such as depression, anxiety, and stress, including also social behavior.
For the Intervention-Study 2, the hypothesis is: Compared to the baseline and to an ACC, at the end of the intervention participants of the eCBTi report improved sleep disturbances, along with improved psychological well-being, as mentioned above.
2 Methods
2.1 Participants
We expect that all 480 MDs of the SAF complete the survey. The inclusion criteria are: 1. Aged 18 years and older; 2. Master degree or higher in human medicine; 3. MD of the SAF; 3. Willing and able to comply with the study conditions; 4. Signed written informed consent. Exclusion criteria are: 1. Completing the questionnaires in an unreliable fashion (“clickthroughts”; answers are given clicking systematically on the right or left side or in the middle; questionnaires are completed within a couple of minutes). 2. A participant withdraws from the study. 3. Pregnancy or breastfeeding, as this may alter sleep and psychological well-being. 4. A participant leaves the SAF.
2.2 Procedure
For this cross-sctional and interventional study all MDs of the SAF will be contacted via the secure e-mail system of the SAF electronic platform. The invitation e-mail will explain the study aims, the approval process, the voluntary nature of participation, and the coded data handling. Further, participants will be informed that participation or non-participation will have no advantages or disadvantages for their professional and military career. The study will be conducted according to the seventh and current version (115) of the Declaration of Helsinki, and the study has been approved on March 28, 2024 by the local ethics committee (EKNZ; Ethikkommission Nordwest- und Zentralschweiz; Basel, Switzerland: register code: 2024–00258).
2.3 Survey-study 1; study design
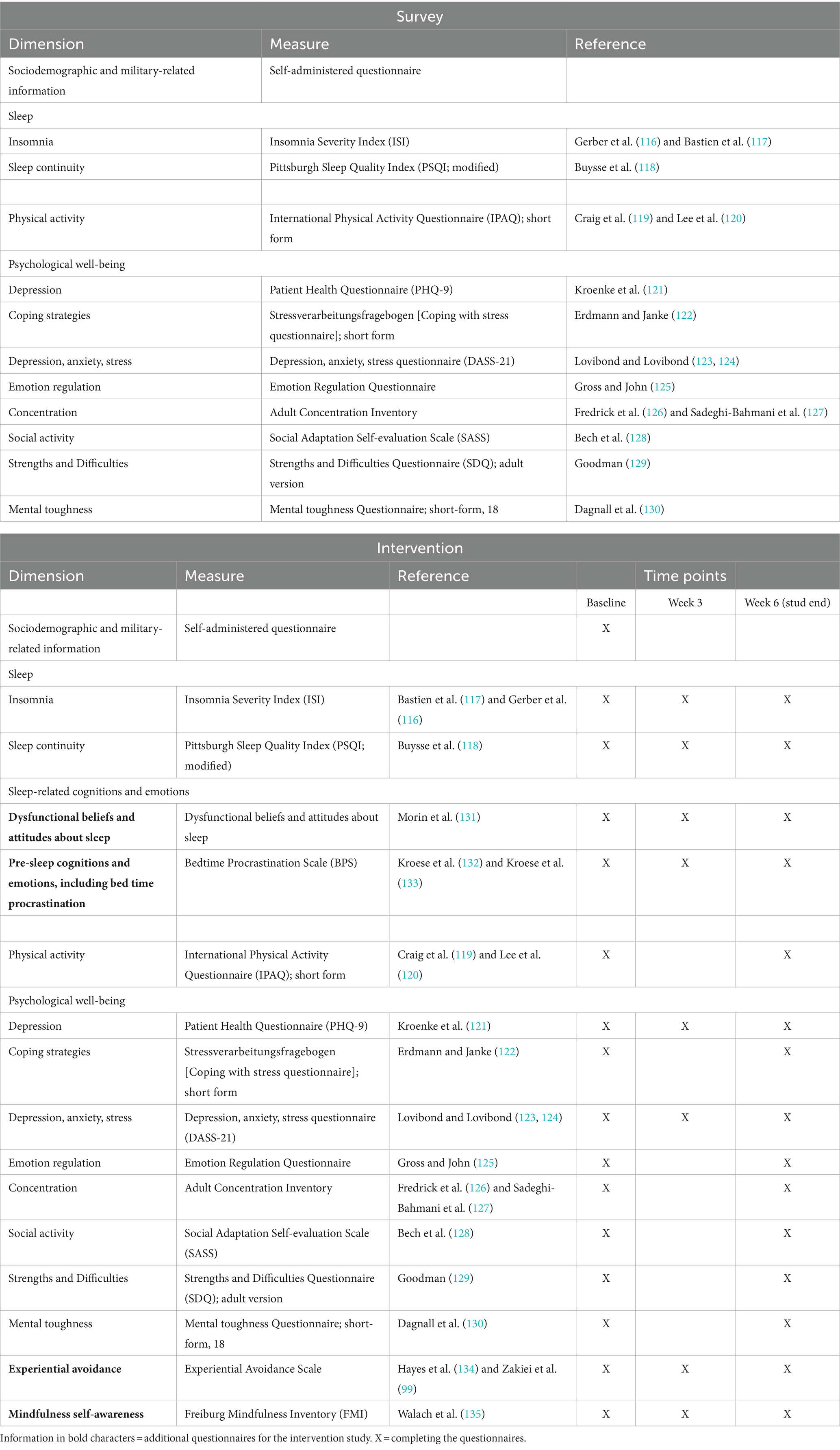
Participants who provide written informed consent will receive a survey link (see Table 1 for a description of the study measures). The baseline survey data will be analyzed to get a descriptive overview, including prevalence rates of participants’ sleep disturbances and psychological well-being. Next, those MDs with sleep disturbances along with issues of psychological well-being will be identified and are eligible for the Intervention-Study 2.
2.4 Intervention-study 2; study design
Medical doctors reporting sleep disturbances (see above) are contacted and invited to participate at the intervention of eCBTi. They are informed about the study design, the aims of the intervention study, the coded data handling, along with the information that participation or non-participation will have no advantages or disadvantages for their military career. Next, participants are randomly assigned either to the eCBTi condition (see details below) or to the ACC (see details below). All participants complete a series of self-rating questionnaires (see details below) at baseline, at week 3 (half time) and at week 6 (study end). At the end of the intervention, participants in the ACC can switch to the eCBTi condition.
2.5 Measures
Survey-Study 1: Table 1 provides the overview of the study measures. The primary outcome measures are sleep disturbances (insomnia; sleep onset latency (SOL); awakenings after sleep onset (WASO) = disrupted sleep continuity). Secondary outcomes are psychological ill-being and well-being, including depression, anxiety, stress, coping strategies, emotion regulation, concentration, social activity, strengths and difficulties, and mental toughness.
Intervention-Study 2: Table 2 provides the overview of the study measures. Primary outcomes are change in sleep disturbances (insomnia; disrupted sleep continuity). Secondary outcomes are psychological ill-being and well-being, including the dimensions metioned above, and additionally: Sleep-related cognitions, experiential avoidance, and mindfulness self-awareness (see also Table 1).
2.5.1 Online survey
Please consider that there will be a questionnaire for private/civil life and one for military deployment.
2.5.1.1 Sociodemographic and military-related information
Participants report on their age, sex at birth, current job position (residency status; specialty; position within a hospital or extra-hospital activity); current military ranking and duration of military service (years).
2.5.1.2 Sleep
To assess sleep dimensions, three questionnaires are used.
2.5.1.2.1 Insomnia
Participants complete the German version (116) of the Insomnia Severity Index [ISI; (117)]. The questionnaire consists of seven items that assess difficulty falling asleep, sleeping without interruption, feeling refreshed in the morning, and daytime performance, in the last 2 weeks. Participants rate how well each item describes themselves from: 0 (= not at all) to 4 (= almost always), with higher sum scores reflecting a higher degree of insomnia.
2.5.1.2.2 Sleep continuity
To assess sleep continuity of the last 2 weeks, participants will be administered the modified Pittsburgh Sleep Quality Inventory (PSQI (118):). The questionnaire assesses usual bedtime, sleep onset latency, the number of awakenings after sleep onset, and wake-up time.
2.5.1.2.3 Sleep-influencing factors and rituals
The self-administered questionnaire evaluates working and sleep time, factors influencing sleep such as pets, children, on-call service, co-sleeping, noise and similar. Typical pre-sleep rituals are reading books, physical activity, texting/messaging, using tablets or similar electronic devices, sex, substances such as alcohol, cannabis, medications. Items are answered “yes” (scored as 1) or “no” (scored as 0.), with higher sum scores reflecting more unfavorable sleep-influencing factors.
2.5.1.3 Physical activity
Participants complete the 7-item International Physical Activity Questionnaire-Short Form (119) to assess weekly sedentary life style, and light to moderate and vigorous physical activity patterns. An overall total physical activity MET-minutes/week score will be calculated, and according to the amount of physical activity the subjects will enter the category of low, moderate or high physical activity.
2.5.1.4 Depression
To assess symptoms of depression, participants will be asked to complete the PHQ-9 (122), a brief depression severity measure; higher overall summed scores indicate higher symptoms of depression (0–4 points indicate no depression, 5–9 mild depression, 10–14 moderate depression, 15–19 moderatly severe and 20–27 severe depression).
2.5.1.5 Coping strategies
To assess coping strategies, participants will be administered the short-form of the Stressverarbeitungsfragebogen 120 [Coping with stress questionnaire] (121). Favorable coping strategies are: Minimizing and trivializing, self-instructions, active problem solving. Unfavorable coping strategies are: Social withdrawal, catastrophizing, substance use. Higher summed scores reflect more pronounced favorable and unfavorable coping strategies.
2.5.1.6 Depression, anxiety, stress
Participants will complete the Depression, Anxiety, Stress-questionnaire [DASS-21; (123, 124)]. Higher summed scores indicate a higher degree of depression, anxiety and stress.
2.5.1.7 Emotion regulation
Participants will complete the Emotion Regulation Questionnaire (125), which focuses on cognitive reappraisal and emotion suppression. Item scores will be summed to create a total score; higher overall scores indicate more cognitive reappraisal and more emotion suppression.
2.5.1.8 Concentration
Participants complete the German version (Sadeghi-Bahmani and Brand, in preparation) of the Adult Concentration Inventory (126, 127); higher sum scores reflect more difficulties with concentration.
2.5.1.9 Social activity
Participants will complete the Social Adaptation Self-evaluation Scale [SASS; (128)]. Higher scores indicate higher social activity.
2.5.1.10 Strengths and difficulties
Participants will complete the Strength and Difficulties Questionnaire [SDQ; (129)] for adults. Dimensions are: Emotional problems, behavioral problems, hyperactivity, problems with peers and family members, and prosocial behavior.
2.5.1.11 Mental toughness
Participants complete the mental toughness short form [MTQ-18; (130, 136)], with higher scores reflecting a higher degree of mental toughness.
2.5.2 Measures for the eCBTi intervention and active control condition
The following questionnaires will be identical in both the initial survey and the intervention study: Sociodemographic and military-related information, sleep, physical activity, depression, coping strategies, depression, anxiety and stress, emotion regulation, social activity, strengths and difficulties, mental toughness (see Table 1).
In addition to the above mentioned questionnaires, the intervention study will also assess several additional psychological constructs with the following surveys:
2.5.2.1 Dysfunctional beliefs and attitudes about sleep
The Dysfunctional Beliefs and Attitudes about Sleep (DBAS; 16-items version) assesses cognitions and attitudes unfavorably impacting on sleep. Typical items are: “I need 8 h of sleep.,” or “It’s better taking sleeping pills.,” or “Sleep is unpredictable.” Answers are given on five-point Likert scales ranging from: 1 (= strongly disagree) to 5 (= strongly agree), with higher sum scores reflecting a more pronounced tendency to display dysfunctional beliefs and attitudes about sleep.
2.5.2.2 Pre-sleep cognitions and emotions, including bed time procrastination
The Bedtime Procrastination Scale [BPS (132, 133)] consists of nine items measuring subjective bedtime procrastination. Typical items are: “I easily get distracted by things when I actually would like to go to bed,” “I go to bed later than I had intended,” and “I want to go to bed on time but I just do not.” The response scale ranges from 1 (= almost never) to 5 (= almost always), with higher sum scores reflecting a higher tendency to delay to going to bed and to sleep.
2.5.2.3 Experiential avoidance
Participants will be administered the Experiential Avoidance Questionnaire [Hayes et al. (99, 137)]. It consists of 10 items, and typical items include: “I am afraid of my feelings.” or “My thoughts and feelings mess up my life.” Answers are given on 7-point Likert scales ranging from 1 (= never) to 7 (= always). Higher sum scores reflect a higher degree to accept also unpleasant experiences (emotions, cognitions), and accordingly, a lower degree of avoidance.
2.5.2.4 Mindfulness – self-awareness
Participants complete the Freiburg Mindfulness Inventory (FMI) (135). The short form consists of six items. Sample items are: “I perceive my feelings and emotions without having to react to them,” “I observe how my thoughts come and go,” “I accept unpleasant feelings,” and “I’m able to smile when I notice how I sometimes make life difficult.” Items are rated on a 4-point scale from 1 (= rarely) to 4 (= almost always), with higher sum scores reflecting a higher tendency of mindfulness and self-awareness.
2.6 Interventions
2.6.1 eCBTi
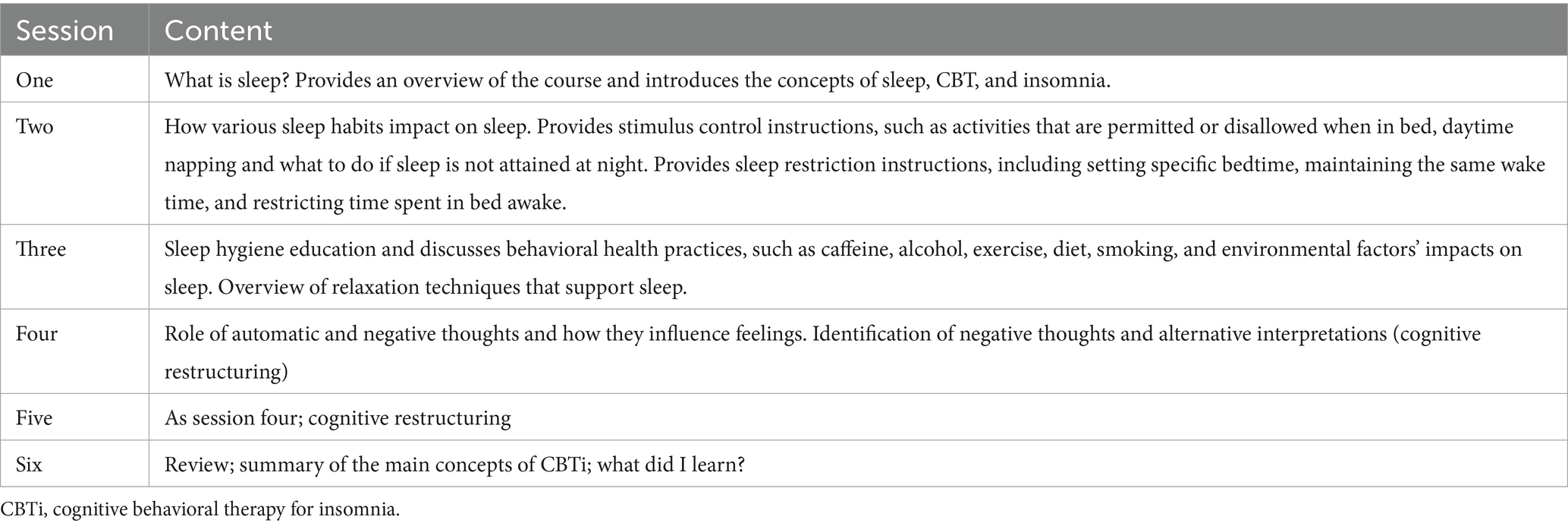
We follow the standardized and validated intervention protocol for eCBTi (87, 91, 92; see Table 2). The intervention lasts for six consecutive weeks, with one session per week; a session lasts between 60 min to 70 min. Weekly homeworks need about 60–90′ per week.
2.6.2 Active control condition
As described extensively elsewhere (99, 138–141) participants in the control condition will meet once a week for six consecutive weeks for about 70 min. Thus, frequency, duration, and intensity are identical to the intervention condition. For homework, participants are asked to journaling. The control condition could not be considered as a bona fide intervention, given that the sessions exclude treatment elements that are truly intended to be therapeutic (142). Rather, participants will have group discussions on daily activities and daily problems. Participants are encouraged to exchange daily life experiences. The active control condition is not intended to be an active therapy, but to control for possible placebo effects in the intervention condition.
Licensed and trained clinical psychologists are responsible for both the eCBTi and the ACC.
2.7 Sample size calculations
To calculate the sample size for the intervention study, we used the G*Power software (143). Based on previous studies on the efficacy of eCBTi (86–92), we expect a partial eta-squared of 0.08 (medium effect); alpha: 0.05; Power: 0.95; number of groups: 2; number of measurements: 3; total sample size: 32, that is, 16 per condition. To counterbalance possible drop-out, we assess 25 participants per condition.
2.8 Analytical plan
Survey-Study 1: We will examine the prevalence rates of insomnia (continuous and categorical dimensions), disrupted sleep continuity, physical activity, psychological well-being, including depression, anxiety, stress, coping with stress, emotion regulation, concentration, social activity, and mental toughness. A series of Pearson’s correlations are run to calculate the associations between the variables mentioned above. Chi-square-tests will be used to calculate the associations between categorical dimensions. To explore which psychological dimensions are statistically more strongly associated with insomnia, we run regression analyses; the minimum requirements are as follows (137, 144, 145): N = x > 100; predictors explain the dependent variables (R > 0.40, R2 > 30); the number of predictors x 10 should be < N; the Durbin–Watson coefficients should be between 1.5 and 2.5, indicating that the residuals of the predictors are independent. For the variances inflation factors (VIF): While there are no strict cut-off points to report the risk of multicollinearity, VIF < 1 and VIF > 10 indicate multicollinearity.
For t-tests, Cohen’s d effect sizes are reported with the following cut-off values: Trivial (ds: 0–0.19), small (ds: 0.20–0.49), medium (ds: 0.50–0.79) or large (ds: 0.80 and greater) (146–148).
2.8.1 Intervention
ANOVAs for repeated measures are run with the factors Group (eCBTi vs. ACC), Time (baseline, week 3, week 6), and the Group x Time-interaction; dependent variables as reported in Table 2. Post-hoc analyses after Bonferroni-Holm are used for p-corrections for multiple testing. Single mean comparisons are performed with Cohen’s d effect sizes, as proposed by Becker (149). In case of missing values, such missing data will be replaced with the means or medians of the sample (144, 145, 150, 151). For the intervention study: Statistical procedures are run both by protocol (that is: only available data observed at any time point from every participant are considered) and by intent-to-treat (ITT) with the last intervention carried forward (LOCF) (152). Further, we consider the following confounders, that is to say, we statistically calculate, whether the pattern of results might get biased in the same or opposite directions for the following confounders: Age, gender, working condition, including current full time or part time positions as medical doctors, including their subspeciality such as neurosurgeon, anesthesiologist, or emergency MD, to name but a few, and military rank, or time lapse between the assessment and the last deployment.
2.9 Assessment of safety
Survey: Completing the online survey has no risks of adverse effect. However, at the beginning, in the middle, and at the end of the booklet we provide websites, email-addresses and phone numbers of local emergency units for psychiatric issues.
Intervention: To our understanding, no adverse effects or risks are reported for eCBTi interventions. As such, also in previous studies CBTi interventions are considered as low-risk psychotherapeutic interventions (87, 92, 153).
2.10 Data protection
First, for both the Survey and the Internvention study, all participants sign the written informed consent, which clearly warrants full privacy and fully data protection. More specifically, neither the ranking officers of the SAF nor anybody else has access to the data. In line with this, the data are securely stored on a cluster of the server of the Psychiatric Hospital of the University of Basel (UPK, Basel, Switzerland). As such, no one except the study coordinator and some very specifically trained psychologists of the UPK who are by no means associated with the SAF, have access to the data set. Further, all data are coded, and the code-key is securely and separately stored from the data sheet. These circumstances warrant full anonymity and data protection, which are particularly important and delicate in organizations and systems such as the military.
2.11 Status and time line
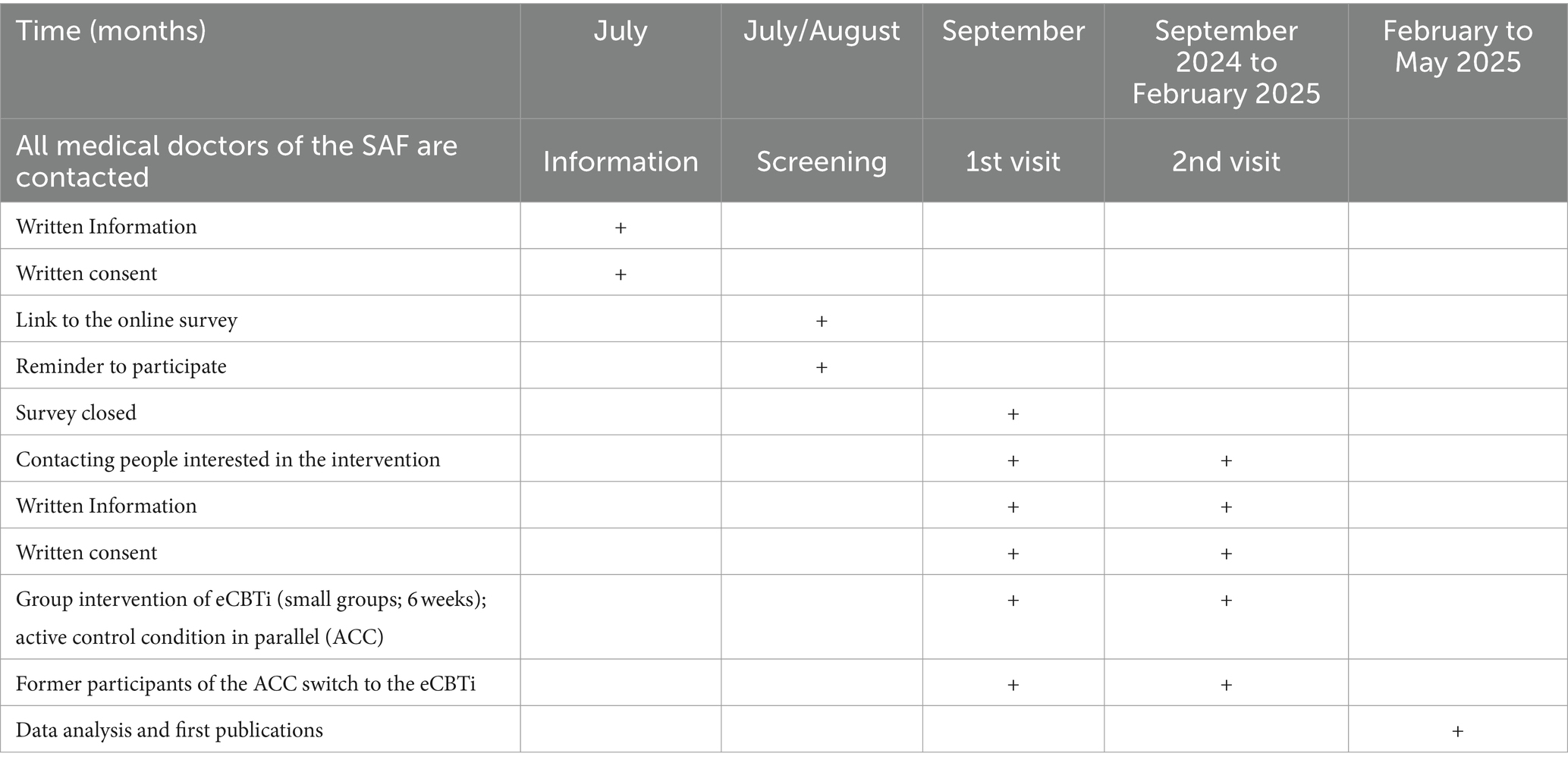
The present study protocol has been approved on March 28, 2024 by the local ethics committee (EKNZ; Ethikkommission Nordwest- und Zentralschweiz; Basel, Switzerland: register code: 2024–00258). The timeline is reported in Table 3.
3 Discussion
Sleep issues have become a major health concern in the general population. Further, compared to the general population, two subgroups are at increased risk to report poor sleep: Medical doctors (47–51), and military personnel (65, 66, 154). The logic is that military MDs should be at additional high risk to suffer from sleep issues. To our understanding, such data are missing in general, and for the Swiss Armed Forces (SAF), in specific. To counter this, the present study consists of two parts:
Survey-Study 1: The first part will be the survey with the aim to assess sleep disturbances (insomnia; disrupted sleep continuity), including dimensions of psychological well-being among military MDs of the SAF. Based on the results gathered during this survey, the second part starts, that is:
Intervention-Study 2: Participants reporting poor sleep (Insomnia Severity Index >8), including poor psychological well-being, and interested in undergoing a standardized and validated treatment for insomnia (eCBTi) (87, 91, 92) are randomly assigned either to the intervention condition (eCBTi) or to the active control condition (ACC). The interventions last six consecutive weeks, with weekly group sessions lasting for 60–70 min, plus weekly homework. At the end of the intervention, participants in the ACC have the possibility to switch to the eCBTi intervention.
3.1 Expected outcomes: survey-study 1
We expect to gather data on the prevalence of sleep disturbances among MDs of the SAF, both in their private/professional and military context. We further should understand, if and to what extent sleep disturbances are further associated with psychological dimenions of psychological well-being and ill-being, including depression, anxiety, stress, coping with stress, emotion regulation, concentration, social activity, strength and difficulties, and mental toughness. Last, we expect to indentify those MDs reporting sleep disturbances and being willing and able to undergo a standardized psychotherapeutic intervention of eCBTi.
3.1.1 Expected outcomes: intervention-study 2
We expect that compared to individuals in the ACC, and compared to the baseline, at the end of the intervention, individuals in the eCBTi condition report improved sleep disturbances, including dysfunctional cognitions impairing sleep, along with improvements for symptoms of depression, anxiety, coping with stress, emotion regulation, concentration, social activity, strength and difficulties, and mental toughness, and with improvements for experiential avoidance and mindfulness self-awareness. The intervention study should also help to understand possible improvements in sleep disturbances and psychological well-being both in the professional/private and in the military context.
3.2 Limitations
We are aware of the following study limitations. First, all data are self-reported, and as such, biases in the self-perception cannot be ruled-out. Ideally, psychiatrists and clinical psychologists would run clinical interviews to assess possible psychiatric disorders (155, 156). Second, we assess sleep disturbances, including psychological well-being both in a participants’ military and family/private/professional context: While the unique structure of SAF military service, including repeated regular training courses over several years, helps to keep an expert’s specific military skills high, the boundaries between civil/professional and military life might get blurred, with quick and sometimes unpredictable transitions from civil life to military deployments and vice versa. As such, it might be challenging to complete the questionnaires, while cognitively discerning between civil/professional and military life. Third, given the strictly voluntary character of both the survey and the intervention and considering a MD’s workload, it is not clear, how many military medical doctors will participate. Fourth, very similar to the literature on sleep disturbances among military personnel and military MDs (see Introduction section), we mainly assess insomnia and disrupted sleep continuity, while further sleep disturbances such as Restless Legs Syndrome (RLS), Obstructive Sleep Apnea (OSA), parasomnias, including night terrors and night mares are not considered. However, one paragraph in the survey asks more specifically about sleep-impairing events; as such, participants could report sleep-issues such as RLS, OSAs, and parasomnias. Fifth, we focused prevalently on sleep quality (insomnia), while sleep quantity (disrupted sleep continuity such as delayed sleep onset latency and awakenings after sleep onset) was regarded as less important (157).
Author contributions
DS-B: Conceptualization, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Data curation. VR: Conceptualization, Project administration, Writing – original draft, Writing – review & editing. ZS: Conceptualization, Writing – original draft, Writing – review & editing, Funding acquisition, Investigation, Methodology, Resources, Supervision. UL: Conceptualization, Methodology, Resources, Writing – original draft, Writing – review & editing. RB: Conceptualization, Methodology, Resources, Writing – original draft, Writing – review & editing, Supervision. MK: Conceptualization, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing. SB: Conceptualization, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing, Formal analysis, Funding acquisition, Investigation, Project administration, Software, Validation, Visualization.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The study is financially supported by internal fundings of the SAF, Bern Switzerland. The study was supported by the Center of Competence for Military and Disaster Medicine, Swiss Armed Forces, Bern, Switzerland. The Center of Competence for Military and Disaster Medicine of the Swiss Armed Forces has no influence on the content of the present manuscript.
Acknowledgments
The authors acknowledge the support of Major General Andreas Stettbacher, Surgeon General Swiss Armed Forces, Bern, Switzerland.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Baglioni, C, Nanovska, S, Regen, W, Spiegelhalder, K, Feige, B, Nissen, C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. (2016) 142:969–90. doi: 10.1037/bul0000053
2. Baglioni, C, Spiegelhalder, K, Lombardo, C, and Riemann, D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. (2010) 14:227–38. doi: 10.1016/j.smrv.2009.10.007
3. Baker, EK, Richdale, AL, Hazi, A, and Prendergast, LA. Assessing a hyperarousal hypothesis of insomnia in adults with autism spectrum disorder. Autism Res. (2019) 12:897–910. doi: 10.1002/aur.2094
4. Baum, KT, Desai, A, Field, J, Miller, LE, Rausch, J, and Beebe, DW. Sleep restriction worsens mood and emotion regulation in adolescents. J Child Psychol Psychiatry. (2014) 55:180–90. doi: 10.1111/jcpp.12125
5. Brand, S, Kirov, R, Kalak, N, Gerber, M, Schmidt, NB, Lemola, S, et al. Poor sleep is related to lower emotional competence among adolescents. Behav Sleep Med. (2016) 14:602–14. doi: 10.1080/15402002.2015.1048450
6. Cousins, JC, Whalen, DJ, Dahl, RE, Forbes, EE, Olino, TM, Ryan, ND, et al. The bidirectional association between daytime affect and nighttime sleep in youth with anxiety and depression. J Pediatr Psychol. (2011) 36:969–79. doi: 10.1093/jpepsy/jsr036
7. Goldstein, AN, and Walker, MP. The role of sleep in emotional brain function. Annu Rev Clin Psychol. (2014) 10:679–708. doi: 10.1146/annurev-clinpsy-032813-153716
8. Haghighi, M, Ludyga, S, Rahimi, B, Jahangard, L, Ahmadpanah, M, Torabian, S, et al. In patients suffering from major depressive disorders, quantitative EEG showed favorable changes in left and right prefrontal cortex. Psychiatry Res. (2017) 251:137–41. doi: 10.1016/j.psychres.2017.02.012
9. Manber, R, and Chambers, AS. Insomnia and depression: a multifaceted interplay. Curr Psychiatry Rep. (2009) 11:437–42. doi: 10.1007/s11920-009-0066-1
10. Pompili, M, Innamorati, M, Forte, A, Longo, L, Mazzetta, C, Erbuto, D, et al. Insomnia as a predictor of high-lethality suicide attempts. Int J Clin Pract. (2013) 67:1311–6. doi: 10.1111/ijcp.12211
11. Taylor, DJ, Lichstein, KL, Durrence, HH, Reidel, BW, and Bush, AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. (2005) 28:1457–64. doi: 10.1093/sleep/28.11.1457
12. Wang, X, Cheng, S, and Xu, H. Systematic review and meta-analysis of the relationship between sleep disorders and suicidal behaviour in patients with depression. BMC Psychiatry. (2019) 19:303. doi: 10.1186/s12888-019-2302-5
13. Acheson, A, Richards, JB, and de Wit, H. Effects of sleep deprivation on impulsive behaviors in men and women. Physiol Behav. (2007) 91:579–87. doi: 10.1016/j.physbeh.2007.03.020
14. Guarana, CL, Ryu, JW, O'Boyle, EH Jr, Lee, J, and Barnes, CM. Sleep and self-control: a systematic review and meta-analysis. Sleep Med Rev. (2021) 59:101514. doi: 10.1016/j.smrv.2021.101514
15. Liu, JW, Tu, YK, Lai, YF, Lee, HC, Tsai, PS, Chen, TJ, et al. Associations between sleep disturbances and suicidal ideation, plans, and attempts in adolescents: a systematic review and meta-analysis. Sleep. (2019) 42:54. doi: 10.1093/sleep/zsz054
16. Liu, RT, Steele, SJ, Hamilton, JL, Do, QBP, Furbish, K, Burke, TA, et al. Sleep and suicide: a systematic review and meta-analysis of longitudinal studies. Clin Psychol Rev. (2020) 81:101895. doi: 10.1016/j.cpr.2020.101895
17. Liu, X, Liu, ZZ, Chen, RH, Cheng, XZ, Bo, QG, Wang, ZY, et al. Nightmares are associated with future suicide attempt and non-suicidal self-injury in adolescents. J Clin Psychiatry. (2019) 80:12181. doi: 10.4088/JCP.18m12181
18. Russell, K, Allan, S, Beattie, L, Bohan, J, MacMahon, K, and Rasmussen, S. Sleep problem, suicide and self-harm in university students: a systematic review. Sleep Med Rev. (2019) 44:58–69. doi: 10.1016/j.smrv.2018.12.008
19. Wong, MM, and Brower, KJ. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of adolescent health. J Psychiatr Res. (2012) 46:953–9. doi: 10.1016/j.jpsychires.2012.04.008
20. Wong, MM, Brower, KJ, and Zucker, RA. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J Psychiatr Res. (2011) 45:505–11. doi: 10.1016/j.jpsychires.2010.09.005
21. Astill, RG, Van der Heijden, KB, Van Ijzendoorn, MH, and Van Someren, EJ. Sleep, cognition, and behavioral problems in school-age children: a century of research meta-analyzed. Psychol Bull. (2012) 138:1109–38. doi: 10.1037/a0028204
22. Ballesio, A, Aquino, M, Kyle, SD, Ferlazzo, F, and Lombardo, C. Executive functions in insomnia disorder: a systematic review and exploratory Meta-analysis. Front Psychol. (2019) 10:101. doi: 10.3389/fpsyg.2019.00101
23. Braley, TJ, Kratz, AL, Kaplish, N, and Chervin, RD. Sleep and cognitive function in multiple sclerosis. Sleep. (2016) 39:1525–33. doi: 10.5665/sleep.6012
24. Devore, EE, Grodstein, F, and Schernhammer, ES. Sleep duration in relation to cognitive function among older adults: a systematic review of observational studies. Neuroepidemiology. (2016) 46:57–78. doi: 10.1159/000442418
25. Dewald-Kaufmann, JF, Oort, FJ, and Meijer, AM. The effects of sleep extension on sleep and cognitive performance in adolescents with chronic sleep reduction: an experimental study. Sleep Med. (2013) 14:510–7. doi: 10.1016/j.sleep.2013.01.012
26. Harvey, AG. A cognitive model of insomnia. Behav Res Ther. (2002) 40:869–93. doi: 10.1016/S0005-7967(01)00061-4
27. Killgore, WD, Kahn-Greene, ET, Lipizzi, EL, Newman, RA, Kamimori, GH, and Balkin, TJ. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Med. (2008) 9:517–26. doi: 10.1016/j.sleep.2007.07.003
28. Krause, AJ, Simon, EB, Mander, BA, Greer, SM, Saletin, JM, Goldstein-Piekarski, AN, et al. The sleep-deprived human brain. Nat Rev Neurosci. (2017) 18:404–18. doi: 10.1038/nrn.2017.55
29. Lo, JC, Groeger, JA, Cheng, GH, Dijk, DJ, and Chee, MW. Self-reported sleep duration and cognitive performance in older adults: a systematic review and meta-analysis. Sleep Med. (2016) 17:87–98. doi: 10.1016/j.sleep.2015.08.021
30. Mahmood, Z, Hammond, A, Nunez, RA, Irwin, MR, and Thames, AD. Effects of sleep health on cognitive function in HIV+ and HIV-adults. J Int Neuropsychol Soc. (2018) 24:1038–46. doi: 10.1017/S1355617718000607
31. Stickgold, R. Sleep-dependent memory consolidation. Nature. (2005) 437:1272–8. doi: 10.1038/nature04286
32. van der Helm, E, Gujar, N, and Walker, MP. Sleep deprivation impairs the accurate recognition of human emotions. Sleep. (2010) 33:335–42. doi: 10.1093/sleep/33.3.335
33. Van Dongen, HP, Maislin, G, Mullington, JM, and Dinges, DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. (2003) 26:117–26. doi: 10.1093/sleep/26.2.117
34. Wardle-Pinkston, S, Slavish, DC, and Taylor, DJ. Insomnia and cognitive performance: a systematic review and meta-analysis. Sleep Med Rev. (2019) 48:101205. doi: 10.1016/j.smrv.2019.07.008
35. Wickens, CD, Hutchins, SD, Laux, L, and Sebok, A. The impact of sleep disruption on complex cognitive tasks: a meta-analysis. Hum Factors. (2015) 57:930–46. doi: 10.1177/0018720815571935
36. Wu, L, Sun, D, and Tan, Y. A systematic review and dose-response meta-analysis of sleep duration and the occurrence of cognitive disorders. Sleep Breath. (2018) 22:805–14. doi: 10.1007/s11325-017-1527-0
37. Abdoli, N, Bahmani, DS, Farnia, V, Alikhani, M, Golshani, S, Holsboer-Trachsler, E, et al. Among substance-abusing traffic offenders, poor sleep and poor general health predict lower driving skills but not slower reaction times. Psychol Res Behav Manag. (2018) 11:557–66. doi: 10.2147/PRBM.S173946
38. Bioulac, S, Franchi, JM, Arnaud, M, Sagaspe, P, Moore, N, Salvo, F, et al. Risk of motor vehicle accidents related to sleepiness at the wheel: a systematic review and Meta-analysis. Sleep. (2017) 40:134. doi: 10.1093/sleep/zsx134
39. Czeisler, CA, Wickwire, EM, Barger, LK, Dement, WC, Gamble, K, Hartenbaum, N, et al. Sleep-deprived motor vehicle operators are unfit to drive: a multidisciplinary expert consensus statement on drowsy driving. Sleep Health. (2016) 2:94–9. doi: 10.1016/j.sleh.2016.04.003
40. Garbarino, S, Magnavita, N, Guglielmi, O, Maestri, M, Dini, G, Bersi, FM, et al. Insomnia is associated with road accidents. Further evidence from a study on truck drivers. PLoS One. (2017) 12:e0187256. doi: 10.1371/journal.pone.0187256
41. Garbarino, S, Nobili, L, Beelke, M, De Carli, F, and Ferrillo, F. The contributing role of sleepiness in highway vehicle accidents. Sleep. (2001) 24:1–206. doi: 10.1093/sleep/24.2.1a
42. Goncalves, M, Amici, R, Lucas, R, Akerstedt, T, Cirignotta, F, Horne, J, et al. Sleepiness at the wheel across Europe: a survey of 19 countries. J Sleep Res. (2015) 24:242–53. doi: 10.1111/jsr.12267
43. Shekari Soleimanloo, S, White, MJ, Garcia-Hansen, V, and Smith, SS. The effects of sleep loss on young drivers' performance: a systematic review. PLoS One. (2017) 12:e0184002. doi: 10.1371/journal.pone.0184002
44. Strohl, KP, Brown, DB, Collop, N, George, C, Grunstein, R, Han, F, et al. An official American Thoracic Society clinical practice guideline: sleep apnea, sleepiness, and driving risk in noncommercial drivers. An update of a 1994 statement. Am J Respir Crit Care Med. (2013) 187:1259–66. doi: 10.1164/rccm.201304-0726ST
45. Ben Simon, E, and Walker, MP. Sleep loss causes social withdrawal and loneliness. Nat Commun. (2018) 9:3146. doi: 10.1038/s41467-018-05377-0
46. Dutcher, CD, Dowd, SM, Zalta, AK, Taylor, DJ, Rosenfield, D, Perrone, A, et al. Sleep quality and outcome of exposure therapy in adults with social anxiety disorder. Depress Anxiety. (2021) 38:1182–90. doi: 10.1002/da.23167
47. Melo, MCA, das Chagas Medeiros, F, Meireles Sales de Bruin, V, Pinheiro Santana, JA, Bastos Lima, A, and de Francesco Daher, E. Sleep quality among psychiatry residents. Can J Psychiatr. (2016) 61:44–9. doi: 10.1177/0706743715620410
48. de Mélo Silva Júnior, ML, Valença, MM, and Rocha-Filho, PAS. Individual and residency program factors related to depression, anxiety and burnout in physician residents - a Brazilian survey. BMC Psychiatry. (2022) 22:272. doi: 10.1186/s12888-022-03916-0
49. Jaradat, R, Lahlouh, A, Aldabbour, B, Saadeh, A, and Mustafa, M. The impact of duty hour limits on sleep quality of resident: a cross-sectional study. Oman Med J. (2022) 37:e403. doi: 10.5001/omj.2022.78
50. Jaradat, R, Lahlouh, A, and Mustafa, M. Sleep quality and health related problems of shift work among resident physicians: a cross-sectional study. Sleep Med. (2020) 66:201–6. doi: 10.1016/j.sleep.2019.11.1258
51. Magnavita, N, Di Prinzio, RR, Meraglia, I, Vacca, ME, Soave, PM, and Di Stasio, E. Sleep in residents: a comparison between anesthesiology and occupational medicine interns. Int J Environ Res Public Health. (2023) 20:356. doi: 10.3390/ijerph20032356
52. Bondagji, D, Fakeerh, M, Alwafi, H, and Khan, AA. The effects of long working hours on mental health among resident physicians in Saudi Arabia. Psychol Res Behav Manag. (2022) 15:1545–57. doi: 10.2147/PRBM.S370642
53. Hull, SK, DiLalla, LF, and Dorsey, JK. Prevalence of health-related behaviors among physicians and medical trainees. Acad Psychiatry. (2008) 32:31–8. doi: 10.1176/appi.ap.32.1.31
54. Lebensohn, P, Dodds, S, Benn, R, Brooks, AJ, Birch, M, Cook, P, et al. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med. (2013) 45:541–9.
55. Freedy, JR, Staley, C, Mims, LD, DeCastro, AO, Perkins, S, Berini, C, et al. Social, individual, and environmental characteristics of family medicine resident burnout: a CERA study. Fam Med. (2022) 54:270–6. doi: 10.22454/FamMed.2022.526799
56. Low, ZX, Yeo, KA, Sharma, VK, Leung, GK, McIntyre, RS, Guerrero, A, et al. Prevalence of burnout in medical and surgical residents: a Meta-analysis. Int J Environ Res Public Health. (2019) 16:1479. doi: 10.3390/ijerph16091479
57. Rodrigues, H, Cobucci, R, Oliveira, A, Cabral, JV, Medeiros, L, Gurgel, K, et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. (2018) 13:e0206840. doi: 10.1371/journal.pone.0206840
58. Simpkin, AL, Khan, A, West, DC, Garcia, BM, Sectish, TC, Spector, ND, et al. Stress from uncertainty and resilience among depressed and burned out residents: a cross-sectional study. Acad Pediatr. (2018) 18:698–704. doi: 10.1016/j.acap.2018.03.002
59. West, CP, Tan, AD, Habermann, TM, Sloan, JA, and Shanafelt, TD. Association of resident fatigue and distress with perceived medical errors. JAMA. (2009) 302:1294–300. doi: 10.1001/jama.2009.1389
60. Al-Maddah, EM, Al-Dabal, BK, and Khalil, MS. Prevalence of sleep deprivation and relation with depressive symptoms among medical residents in king Fahd university hospital, Saudi Arabia. Sultan Qaboos Univ Med J. (2015) 15:e78–84.
61. Alaska, YA, AlYahya, B, AlFakhri, L, AlHarbi, B, Alkattan, F, and Alhayaza, RM. Emergency medicine Personnel's preparation, performance and perception of their night shifts: a cross-sectional study from Saudi Arabia. Adv Med Educ Pract. (2022) 13:167–75. doi: 10.2147/AMEP.S339063
62. Kwok, C. Depression, stress, and perceived medical errors in Singapore psychiatry residents. Acad Psychiatry. (2021) 45:169–73. doi: 10.1007/s40596-020-01376-w
63. Lee, MJ, Nho, WY, Jung, H, Cho, JW, Seo, JS, Lee, HM, et al. High prevalence of depression and sleep-wake disorders among female emergency medicine residents in South Korea. Ann Med. (2022) 54:846–55. doi: 10.1080/07853890.2022.2053568
64. Ogawa, R, Seo, E, Maeno, T, Ito, M, Sanuki, M, and Maeno, T. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Educ. (2018) 18:50. doi: 10.1186/s12909-018-1171-9
65. Redmond, SA, Wilcox, SL, Campbell, S, Kim, A, Finney, K, Barr, K, et al. A brief introduction to the military workplace culture. Work. (2015) 50:9–20. doi: 10.3233/WOR-141987
66. Bai, W, Gui, Z, Chen, MY, Zhang, Q, Lam, MI, Si, TL, et al. Global prevalence of poor sleep quality in military personnel and veterans: a systematic review and meta-analysis of epidemiological studies. Sleep Med Rev. (2023) 71:101840. doi: 10.1016/j.smrv.2023.101840
67. Castro, CA, Adler, AB, McGurk, D, and Bliese, PD. Mental health training with soldiers four months after returning from Iraq: randomization by platoon. J Trauma Stress. (2012) 25:376–83. doi: 10.1002/jts.21721
68. Peterson, AL, Goodie, JL, Satterfield, WA, and Brim, WL. Sleep disturbance during military deployment. Mil Med. (2008) 173:230–5. doi: 10.7205/MILMED.173.3.230
69. Mysliwiec, V, Walter, RJ, Collen, J, and Wesensten, N. Military sleep management: an operational imperative. US Army Med Dep. (2016) J(2-16):128–34.
70. Mantua, J, Bessey, AF, Mickelson, CA, Choynowski, JJ, Noble, JJ, Burke, TM, et al. Sleep and high-risk behavior in military service members: a mega-analysis of four diverse US Army units. Sleep. (2021) 44:zsaa221. doi: 10.1093/sleep/zsaa221
71. Crane, MF, Hazel, G, Kunzelmann, A, Kho, M, Gucciardi, DF, Rigotti, T, et al. An exploratory domain analysis of deployment risks and protective features and their association to mental health, cognitive functioning and job performance in military personnel. Anxiety Stress Coping. (2023) 37:16–28. doi: 10.1080/10615806.2023.2228707
72. Hsu, DP, Hansen, SL, Roberts, TA, Murray, CK, and Mysliwiec, V. Predictors of wellness behaviors in US army physicians. Mil Med. (2018) 183:e641–e648.
73. Parker, RS, and Parker, P. The impact of sleep deprivation in military surgical teams: a systematic review. J R Army Med Corps. (2017) 163:158–63. doi: 10.1136/jramc-2016-000640
74. James, L, Smart, D, Odom-Maryon, T, Honn, K, and Rowan, S. Sleep deprivation in air National Guard medical personnel responding to simulated disaster-training exercises. Mil Psychol. (2019) 31:138–46. doi: 10.1080/08995605.2019.1565909
75. Adler, AB, Adrian, AL, Hemphill, M, Scaro, NH, Sipos, ML, and Thomas, JL. Professional stress and burnout in U.S. military medical personnel deployed to Afghanistan. Mil Med. (2017) 182:e1669–76. doi: 10.7205/MILMED-D-16-00154
76. Brand, S, Beck, J, Hatzinger, M, Harbaugh, A, Ruch, W, and Holsboer-Trachsler, E. Associations between satisfaction with life, burnout-related emotional and physical exhaustion, and sleep complaints. World J Biol Psychiatry. (2010) 11:744–54. doi: 10.3109/15622971003624205
77. Mash, HBH, Morganstein, JC, Fullerton, CS, and Ursano, RJ. COVID-19 pandemic responses among National Guard Service Members: stressors, coping strategies, sleep Difficultiesand substance use. Int J Environ Res Public Health. (2023) 20:731. doi: 10.3390/ijerph20095731
78. Swift, N, Stewart, R, Andiappan, M, Smith, A, Espie, CA, and Brown, JS. The effectiveness of community day-long CBT-I workshops for participants with insomnia symptoms: a randomised controlled trial. J Sleep Res. (2012) 21:270–80. doi: 10.1111/j.1365-2869.2011.00940.x
79. Alimoradi, Z, Jafari, E, Broström, A, Ohayon, MM, Lin, CY, Griffiths, MD, et al. Effects of cognitive behavioral therapy for insomnia (CBT-I) on quality of life: a systematic review and meta-analysis. Sleep Med Rev. (2022) 64:101646. doi: 10.1016/j.smrv.2022.101646
80. Baglioni, C, Espie, CA, Altena, E, Gavriloff, D, Jernelöv, S, Holzinger, B, et al. Cognitive behavioural therapy for insomnia disorder: extending the stepped care model. J Sleep Res. (2023) 32:e14016. doi: 10.1111/jsr.14016
81. He, D, Guo, Z, McClure, MA, Mu, Q, and Jiang, B. Cognitive-behavioral therapy for insomnia with objective short sleep duration phenotype: a systematic review with meta-analysis. Sleep Med Rev. (2023) 67:101736. doi: 10.1016/j.smrv.2022.101736
82. Hertenstein, E, Trinca, E, Wunderlin, M, Schneider, CL, Züst, MA, Fehér, KD, et al. Cognitive behavioral therapy for insomnia in patients with mental disorders and comorbid insomnia: a systematic review and meta-analysis. Sleep Med Rev. (2022) 62:101597. doi: 10.1016/j.smrv.2022.101597
83. Takano, Y, Ibata, R, Machida, N, Ubara, A, and Okajima, I. Effect of cognitive behavioral therapy for insomnia in workers: a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. (2023) 71:101839. doi: 10.1016/j.smrv.2023.101839
84. Trauer, JM, Qian, MY, Doyle, JS, Rajaratnam, SM, and Cunnington, D. Cognitive behavioral therapy for chronic insomnia: a systematic review and Meta-analysis. Ann Intern Med. (2015) 163:191–204. doi: 10.7326/M14-2841
85. van der Zweerde, T, Bisdounis, L, Kyle, SD, Lancee, J, and van Straten, A. Cognitive behavioral therapy for insomnia: a meta-analysis of long-term effects in controlled studies. Sleep Med Rev. (2019) 48:101208. doi: 10.1016/j.smrv.2019.08.002
86. Amidi, A, Buskbjerg, CR, Damholdt, MF, Dahlgaard, J, Thorndike, FP, Ritterband, L, et al. Changes in sleep following internet-delivered cognitive-behavioral therapy for insomnia in women treated for breast cancer: a 3-year follow-up assessment. Sleep Med. (2022) 96:35–41. doi: 10.1016/j.sleep.2022.04.020
87. Espie, CA, Kyle, SD, Williams, C, Ong, JC, Douglas, NJ, Hames, P, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. (2012) 35:769–81. doi: 10.5665/sleep.1872
88. Sharafkhaneh, A, Salari, N, Khazaie, S, Ghasemi, H, Darvishi, N, Hosseinian-Far, A, et al. Telemedicine and insomnia: a comprehensive systematic review and meta-analysis. Sleep Med. (2022) 90:117–30. doi: 10.1016/j.sleep.2022.01.016
89. Tsai, H-J, Yang, AC, Zhu, J-D, Hsu, Y-Y, Hsu, T-F, and Tsai, S-J. Effectiveness of digital cognitive behavioral therapy for insomnia in young people: preliminary findings from systematic review and Meta-analysis. J Pers Med. (2022) 12:481. doi: 10.3390/jpm12030481
90. Zachariae, R, Lyby, MS, Ritterband, LM, and O'Toole, MS. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia - a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. (2016) 30:1–10. doi: 10.1016/j.smrv.2015.10.004
91. Zhou, K, Kong, J, Wan, Y, Zhang, X, Liu, X, Qu, B, et al. Positive impacts of e-aid cognitive behavioural therapy on the sleep quality and mood of nurses on site during the COVID-19 pandemic. Sleep Breath. (2022) 26:1947–51. doi: 10.1007/s11325-021-02547-1
92. Zhu, Y, Stephenson, C, Moghimi, E, Jagayat, J, Nikjoo, N, Kumar, A, et al. Investigating the effectiveness of electronically delivered cognitive behavioural therapy (e-CBTi) compared to pharmaceutical interventions in treating insomnia: protocol for a randomized controlled trial. PLoS One. (2023) 18:e0285757. doi: 10.1371/journal.pone.0285757
93. Boland, EM, Goldschmied, JR, and Gehrman, PR. Does insomnia treatment prevent depression? Sleep. (2023) 46:104. doi: 10.1093/sleep/zsad104
94. Alvaro, PK, Roberts, RM, and Harris, JK. A systematic review assessing Bidirectionality between sleep disturbances, anxiety, and depression. Sleep. (2013) 36:1059–68. doi: 10.5665/sleep.2810
95. Ballesio, A, Aquino, M, Feige, B, Johann, AF, Kyle, SD, Spiegelhalder, K, et al. The effectiveness of behavioural and cognitive behavioural therapies for insomnia on depressive and fatigue symptoms: a systematic review and network meta-analysis. Sleep Med Rev. (2018) 37:114–29. doi: 10.1016/j.smrv.2017.01.006
96. Chen, TL, Chang, SC, Hsieh, HF, Huang, CY, Chuang, JH, and Wang, HH. Effects of mindfulness-based stress reduction on sleep quality and mental health for insomnia patients: a meta-analysis. J Psychosom Res. (2020) 135:110144. doi: 10.1016/j.jpsychores.2020.110144
97. Harvey, AG. A transdiagnostic approach to treating sleep disturbance in psychiatric disorders. Cogn Behav Ther. (2009) 38:35–42. doi: 10.1080/16506070903033825
98. Passos, GS, Poyares, D, Santana, MG, Teixeira, AA, Lira, FS, Youngstedt, SD, et al. Exercise improves immune function, antidepressive response, and sleep quality in patients with chronic primary insomnia. Biomed Res Int. (2014) 2014:498961:1–7. doi: 10.1155/2014/498961
99. Zakiei, A, Khazaie, H, Rostampour, M, Lemola, S, Esmaeili, M, Dürsteler, K, et al. Acceptance and commitment therapy (ACT) improves sleep quality, experiential avoidance, and emotion regulation in individuals with insomnia-results from a randomized interventional study. Life (Basel). (2021) 11:133. doi: 10.3390/life11020133
100. Andersen, P, Toner, P, Bland, M, and McMillan, D. Effectiveness of Transdiagnostic cognitive behaviour therapy for anxiety and depression in adults: a systematic review and Meta-analysis. Behav Cogn Psychother. (2016) 44:673–90. doi: 10.1017/S1352465816000229
101. Andersson, G, and Carlbring, P. Internet-assisted cognitive behavioral therapy. Psychiatr Clin North Am. (2017) 40:689–700. doi: 10.1016/j.psc.2017.08.004
102. Klimczak, KS, San Miguel, GG, Mukasa, MN, Twohig, MP, and Levin, ME. A systematic review and meta-analysis of self-guided online acceptance and commitment therapy as a transdiagnostic self-help intervention. Cogn Behav Ther. (2023) 52:269–94. doi: 10.1080/16506073.2023.2178498
103. Leventhal, AM, and Zvolensky, MJ. Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychol Bull. (2015) 141:176–212. doi: 10.1037/bul0000003
104. Mahoney, AE, and McEvoy, PM. A transdiagnostic examination of intolerance of uncertainty across anxiety and depressive disorders. Cogn Behav Ther. (2012) 41:212–22. doi: 10.1080/16506073.2011.622130
105. Norton, PJ, Barrera, TL, Mathew, AR, Chamberlain, LD, Szafranski, DD, Reddy, R, et al. Effect of transdiagnostic cbt for anxiety disorders on comorbid diagnoses. Depress Anxiety. (2013) 30:168–73. doi: 10.1002/da.22018
106. Norton, PJ, and Paulus, DJ. Toward a unified treatment for emotional disorders: update on the science and practice. Behav Ther. (2016) 47:854–68. doi: 10.1016/j.beth.2015.07.002
107. Norton, PJ, and Roberge, P. Transdiagnostic therapy. Psychiatr Clin North Am. (2017) 40:675–87. doi: 10.1016/j.psc.2017.08.003
108. Pearl, SB, and Norton, PJ. Transdiagnostic versus diagnosis specific cognitive behavioural therapies for anxiety: a meta-analysis. J Anxiety Disord. (2017) 46:11–24. doi: 10.1016/j.janxdis.2016.07.004
109. Reinholt, N, and Krogh, J. Efficacy of transdiagnostic cognitive behaviour therapy for anxiety disorders: a systematic review and meta-analysis of published outcome studies. Cogn Behav Ther. (2014) 43:171–84. doi: 10.1080/16506073.2014.897367
110. Brand, S, Colledge, F, Ludyga, S, Emmenegger, R, Kalak, N, Sadeghi Bahmani, D, et al. Acute bouts of exercising improved mood, rumination and social interaction in inpatients with mental disorders. Front Psychol. (2018) 9:249. doi: 10.3389/fpsyg.2018.00249
111. Fava, GA, McEwen, BS, Guidi, J, Gostoli, S, Offidani, E, and Sonino, N. Clinical characterization of allostatic overload. Psychoneuroendocrinology. (2019) 108:94–101. doi: 10.1016/j.psyneuen.2019.05.028
112. Guidi, J, and Fava, GA. The clinical science of Euthymia: a conceptual map. Psychother Psychosom. (2022) 91:156–67. doi: 10.1159/000524279
113. Guidi, J, Offidani, E, Rafanelli, C, Roncuzzi, R, Sonino, N, and Fava, GA. The assessment of allostatic overload in patients with congestive heart failure by Clinimetric criteria. Stress Health. (2016) 32:63–9. doi: 10.1002/smi.2579
114. Offidani, E, and Ruini, C. Psychobiological correlates of allostatic overload in a healthy population. Brain Behav Immun. (2012) 26:284–91. doi: 10.1016/j.bbi.2011.09.009
115. World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191–4. doi: 10.1001/jama.2013.281053
116. Gerber, M, Lang, C, Lemola, S, Colledge, F, Kalak, N, Holsboer-Trachsler, E, et al. Validation of the German version of the insomnia severity index in adolescents, young adults and adult workers: results from three cross-sectional studies. BMC Psychiatry. (2016) 16:174. doi: 10.1186/s12888-016-0876-8
117. Bastien, CH, Vallieres, A, and Morin, CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
118. Buysse, DJ, Reynolds, CF 3rd, Monk, TH, Berman, SR, and Kupfer, DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
119. Craig, CL, Marshall, AL, Sjöström, M, Bauman, AE, Booth, ML, Ainsworth, BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. (2003) 35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB
120. Lee, PH, Macfarlane, DJ, Lam, TH, and Stewart, SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. (2011) 8:115. doi: 10.1186/1479-5868-8-115
121. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
123. Lovibond, PF, and Lovibond, SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
124. Lovibond, PF, and Lovibond, SH. Depression anxiety stress scales (DASS-21). APA PsychTests. (1995).
125. Gross, JJ, and John, OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. (2003) 85:348–62. doi: 10.1037/0022-3514.85.2.348
126. Fredrick, JW, Burns, GL, Langberg, JM, and Becker, SP. Examining the structural and external validity of the adult concentration inventory for assessing sluggish cognitive tempo in adults. Assessment. (2022) 29:1742–55. doi: 10.1177/10731911211027224
127. Sadeghi-Bahmani, D, Parhoon, H, Esmaeili, M, Parhoon, K, Sadeghi Bahmani, L, Khazaie, H, et al. Validation of the Farsi version of the adult concentration inventory for assessing cognitive disengagement syndrome. J Clin Med. (2023) 12:4607. doi: 10.3390/jcm12144607
128. Bech, P, Lunde, M, and Unden, M. Social adaptation self-evaluation scale (SASS): psychometric analysis as outcome measure in the treatment of patients with major depression in the remission phase. Int J Psychiatry Clin Pract. (2002) 6:141–6. doi: 10.1080/136515002760276063
129. Goodman, R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. (1997) 38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x
130. Dagnall, N, Denovan, A, Papageorgiou, KA, Clough, PJ, Parker, A, and Drinkwater, KG. Psychometric assessment of shortened mental toughness questionnaires (MTQ): factor structure of the MTQ-18 and the MTQ-10. Front Psychol. (2019) 10:1933. doi: 10.3389/fpsyg.2019.01933
131. Morin, CM, Vallières, A, and Ivers, H. Dysfunctional beliefs and attitudes about sleep (DBAS): validation of a brief version (DBAS-16). Sleep. (2007) 30:1547–54. doi: 10.1093/sleep/30.11.1547
132. Kroese, FM, De Ridder, DTD, Evers, C, and Adriaanse, MA. Bedtime procrastination: introducing a new area of procrastination. Front Psychol. (2014) 5:611. doi: 10.3389/fpsyg.2014.00611
133. Kroese, FM, Evers, C, Adriaanse, MA, and de Ridder, DTD. Bedtime procrastination: a self-regulation perspective on sleep insufficiency in the general population. J Health Psychol. (2016) 21:853–62. doi: 10.1177/1359105314540014
134. Hayes, SC, Strosahl, K, Wilson, KG, Bissett, RT, Pistorello, J, Toarmino, D, et al. Measuring experiential avoidance: a preliminary test of a working model. Psychol Rec. (2004) 54:553–78. doi: 10.1007/BF03395492
135. Walach, H, Buchheld, N, Buttenmüller, V, Kleinknecht, N, and Schmidt, S. Measuring mindfulness—the Freiburg mindfulness inventory (FMI). Personal Individ Differ. (2006) 40:1543–55. doi: 10.1016/j.paid.2005.11.025
136. Clough, P, Earle, K, and Sewell, D. Mental toughness: the concept and its measurement In: I Cockerill, editor. Solutions in sport psychology. London: Thomson (2002). 32–43.
138. Jasbi, M, Sadeghi Bahmani, D, Karami, G, Omidbeygi, M, Peyravi, M, Panahi, A, et al. Influence of adjuvant mindfulness-based cognitive therapy (MBCT) on symptoms of post-traumatic stress disorder (PTSD) in veterans - results from a randomized control study. Cogn Behav Ther. (2018) 47:431–46. doi: 10.1080/16506073.2018.1445773
139. Kalak, N, Gerber, M, Kirov, R, Mikoteit, T, Yordanova, J, Puhse, U, et al. Daily morning running for 3 weeks improved sleep and psychological functioning in healthy adolescents compared with controls. J Adolesc Health. (2012) 51:615–22. doi: 10.1016/j.jadohealth.2012.02.020
140. Mousavi, E, Sadeghi-Bahmani, D, Khazaie, H, Brühl, AB, Stanga, Z, and Brand, S. The effect of a modified mindfulness-based stress reduction (MBSR) program on symptoms of stress and depression and on saliva cortisol and serum Creatine kinase among male wrestlers. Healthcare (Basel). (2023) 11:643. doi: 10.3390/healthcare11111643
141. Norouzi, E, Gerber, M, Masrur, F, Vaezmousavi, M, Pühse, U, and Brand, S. Implementation of a mindfulness-based stress reduction (MBSR) program to reduce stress, anxiety and depression and to improve psychological well-being among retired Iranian football players. Psychol Sport Exerc. (2019) 47:101636. doi: 10.1016/j.psychsport.2019.101636
142. Marcus, DK, O'Connell, D, Norris, AL, and Sawaqdeh, A. Is the dodo bird endangered in the 21st century? A meta-analysis of treatment comparison studies. Clin Psychol Rev. (2014) 34:519–30. doi: 10.1016/j.cpr.2014.08.001
143. Faul, F, Erdfelder, E, Lang, AG, and Buchner, A. G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39:175–91. doi: 10.3758/BF03193146
144. Brosius, F. SPSS; Umfassendes Handbuch zu Statistik und Datenanalyse-comprehensive textbook for statistics and data analysis. Frechen: mitp Verlags GmBH and Co. (2018).
145. Hair, JF, Black, CW, Babin, BJ, and Anderson, RE. Multivariate Data Analysis. 8th ed. Andover UK: Cengage Learning EMEA (2019).
146. Cohen, J. Statistical power analysis for the behavioral sciences. 2nd ed. Mahwah NJ: Lawrence Erlbaum Associates (1988).
148. Cohen, J. The earth is round (p < .05). Am Psychol. (1994) 49:997–1003. doi: 10.1037/0003-066X.49.12.997
149. Becker, BJ. Synthesizing standardized mean-change measures. Br J Math Stat Psychol. (1988) 41:257–78. doi: 10.1111/j.2044-8317.1988.tb00901.x
150. Harris, AH, Reeder, R, and Hyun, JK. Common statistical and research design problems in manuscripts submitted to high-impact psychiatry journals: what editors and reviewers want authors to know. J Psychiatr Res. (2009) 43:1231–4. doi: 10.1016/j.jpsychires.2009.04.007
151. Heymans, MW, and Twisk, JWR. Handling missing data in clinical research. J Clin Epidemiol. (2022) 151:185–8. doi: 10.1016/j.jclinepi.2022.08.016
152. Lachin, JM. Statistical considerations in the intent-to-treat principle. Control Clin Trials. (2000) 21:167–89. doi: 10.1016/S0197-2456(00)00046-5
153. Yang, Y, Luo, X, Paudel, D, Zhang, J, Li, SX, and Zhang, B. Effects of e-aid cognitive behavioural therapy for insomnia (eCBTI) to prevent the transition from acute insomnia to chronic insomnia: study protocol for a randomised controlled trial. BMJ Open. (2019) 9:e033457. doi: 10.1136/bmjopen-2019-033457
154. Hruby, A, Lieberman, HR, and Smith, TJ. Self-reported health behaviors, including sleep, correlate with doctor-informed medical conditions: data from the 2011 health related behaviors survey of U.S. active duty military personnel. BMC Public Health. (2018) 18:853. doi: 10.1186/s12889-018-5781-2
156. First, MB, Williams, JB, Benjamin, LS, and Spitzer, RL. User’s guide for the SCID-5-PD: Structured clinical interview for DSM-5 personality disorders. (2015).
157. Seow, LSE, Tan, XW, Chong, SA, Vaingankar, JA, Abdin, E, Shafie, S, et al. Independent and combined associations of sleep duration and sleep quality with common physical and mental disorders: results from a multi-ethnic population-based study. PLoS One. (2020) 15:e0235816. doi: 10.1371/journal.pone.0235816
Keywords: sleep disturbances, Swiss Armed Forces, psychological well-being, military medical doctors, eCBTI, active control condition
Citation: Sadeghi-Bahmani D, Rigotti V, Stanga Z, Lang UE, Blais RK, Kelley ML and Brand S (2024) Sleep disturbances and psychological well-being among military medical doctors of the Swiss Armed Forces: study protocol, rationale and development of a cross-sectional and longitudinal interventional study. Front. Public Health. 12:1390636. doi: 10.3389/fpubh.2024.1390636
Edited by:
Rudy Foddis, University of Pisa, ItalyReviewed by:
Sergio Garbarino, University of Genoa, ItalyAlessandro Fiorini, Italian Air Force Medical Service, Italy
Valeria Di Muzio, Aeronautica Militare, Italy
Copyright © 2024 Sadeghi-Bahmani, Rigotti, Stanga, Lang, Blais, Kelley and Brand. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Serge Brand, c2VyZ2UuYnJhbmRAdXBrLmNo
†These authors share first authorship
 Dena Sadeghi-Bahmani1,2†
Dena Sadeghi-Bahmani1,2† Viola Rigotti
Viola Rigotti Serge Brand
Serge Brand