
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 04 September 2024
Sec. Aging and Public Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1387550
Background: Anxiety and depression are serious psychological and public health issues among the older adults. Currently, there is a lack of understanding of the relationship between Body Mass Index (BMI) and anxiety or depression symptoms in the older adult population in China. Therefore, the purpose of this study is to investigate the impact of BMI on anxiety and depression through correlation analysis in different subgroups and to examine the potential chain mediating effects of Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) between BMI and symptoms of anxiety and depression.
Methods: From the CLHLS database conducted in 2017–2018, data regarding height, weight, anxiety symptoms, depression symptoms, as well as demographic, socioeconomic, behavioral, and health-related characteristics were collected. Multivariate logistic regression analysis was used to explore the impact of BMI on anxiety and depression symptoms. Finally, the SPSS macro process was utilized to test the multiple mediating effects of ADL and IADL between BMI and anxiety or depression symptoms.
Results: After screening, a final sample of 9,098 Chinese older adult individuals aged 65 and above was selected. Among them, 1,074 cases (11.8%) exhibited anxiety symptoms, 1,458 cases (16.0%) exhibited depressive symptoms. Compared to normal BMI, the adjusted analysis showed that underweight in Chinese older adult individuals was significantly associated with anxiety (OR = 1.316, p = 0.004) and depression (OR = 1.232, p = 0.013). This relationship was found to be more significant in males, individuals aged 80 and above, unmarried individuals, and those residing in town. ADL and IADL played a chain-mediated role between BMI and anxiety symptoms in the older adult. BMI not only had a direct effect on anxiety symptoms in the older adult (effect = −0.0159; SE = 0.0066; 95%CI: LL = −0.0288, UL = −0.0031), but also influenced them indirectly through two pathways: the independent mediating role of IADL (effect = −0.0010; SE = 0.0005; 95%CI: LL = −0.0018, UL = −0.0003) and the chain-mediated role of ADL and IADL (effect = −0.0012; SE = 0.0004; 95%CI: LL = −0.0020, UL = −0.0006).
Conclusion: In the older adult individuals in China, underweight is associated with an increased risk of anxiety and depression symptoms. Improving the underweight condition of Chinese older adult individuals can reduce their ADL and IADL limitations, thereby benefiting their mental health.
Anxiety and depression are prevalent among older adults, posing significant psychological and public health challenges for this age group and being leading causes of disability in the older adult worldwide (1–3). Epidemiological studies have revealed that anxiety and depression are linked to a range of adverse health outcomes, including coronary heart diseases, stroke, and even all-cause mortality (4–6). Moreover, these mental health disorders can induce neuropathic symptoms, diminish interest in daily activities, and impair memory (7, 8). However, owing to insufficient attention given to precursors of mental health issues, such as anxiety and depression, psychological disorders among the older adult population are frequently overlooked and underdiagnosed.
In recent years, research on the relationship between Body Mass Index (BMI) and mental health has attracted widespread attention (9). A systematic review shows that there exists a bidirectional association between a higher BMI and depression. Elevated BMI serves as a predictor for depression onset, while depression exacerbates the risk of overweight and obesity (10). On the other hand, obesity/overweight individuals exhibit a higher frequency of anxiety episodes compared to those of normal weight (11). Furthermore, obesity-Induced cellular senescence drives anxiety (12). Similarly, underweight individuals are more likely to experience depressive/anxiety symptoms compared to those of a normal weight. Previous studies have indicated that abnormal BMI (including obesity and underweight) is associated with an increased risk of psychological disorders such as depression and anxiety. However, the conclusions drawn from various studies remain inconsistent (13–16). A meta-analysis shows that overweight in males is associated with a reduced incidence of depression, whereas in females, this relationship exhibits a trend towards increased risk (13). Additionally, a study observed a U-shaped relationship between anxiety and BMI among whites. Blacks showed a strong association between anxiety and obesity, whereas no such association was found among Asians or Hispanics (15). In summary, this suggests that factors such as gender, race, culture, and social background may influence the relationship between BMI and depression and anxiety. Another possible explanation lies in the existence of potential mediating variables in the relationship between BMI and anxiety/depression symptoms.
A meta-analysis indicates that an increase in BMI is associated with limitations in Activities of Daily Living (ADL) (17). Numerous studies have also found a significant correlation between older adults’ ADL and Instrumental Activities of Daily Living (IADL) with symptoms of anxiety and depression (18–20). According to the stress process theory, when the BMI of older adult individuals is either excessively high or low, it can lead to a decline in their ADL and IADL abilities. The resulting stress may then contribute to cognitive impairment-related diseases, such as depression (21). Therefore, ADL and IADL can be viewed as a type of mediating variable. A study has demonstrated that ADL and IADL impairments mediate the relationship between cognitive impairments, depressive symptoms, and the physical component score (22). Additionally, ADL also mediates the relationship between BMI and life satisfaction (23). However, as of now, there’s no hard evidence indicating that ADL and IADL serve as mediators between BMI and the symptoms of anxiety and depression. Hence, we hypothesize that ADL and IADL play a certain role in the relationship between BMI and the manifestations of anxiety and depression.
Previous studies have already demonstrated the impact of abnormal BMI on anxiety and depression symptoms, and several investigations have also examined disparities within genders and age groups. Despite this, the specific dynamics of this relationship within the older adult population in China still await comprehensive exploration. Furthermore, whether ADL and IADL mediate this effect remains unexplored. Meanwhile, due to the complexity of psychological issues faced by the older adult, which are often influenced by multiple factors, it is imperative to conduct research discussing the relevant influencing factors and mechanisms to promote their mental health. Based on these compelling reasons, our study aims to investigate the impact of BMI on anxiety and depression symptoms, while also exploring the differences in different subgroups, and furthermore, investigating the potential chain mediating effects of ADL and IADL between BMI and symptoms of anxiety and depression.
The dataset utilized in this study was derived from the China Longitudinal Healthy Longevity Survey (CLHLS), a nationally representative survey conducted by the Center for Healthy Aging and Development at Peking University. The survey, which began in 1998 and has conducted 8 surveys with follow-ups every 3–4 years, used a multi-stage cluster random sampling method, covering more than half of the country’s regions (23 provinces/cities/autonomous regions). Face-to-face interviews were conducted with older adults aged 65 and above. Questions that could not be reliably answered by the oldest participants due to potential limitations such as low educational levels and/or poor hearing and vision were excluded from the survey (24). All participating respondents voluntarily signed the informed consent form during the survey. For older adult individuals unable to sign, family members signed the informed consent form on their behalf. To represent the current conditions among older individuals, we utilized the dataset from the 2017–2018 CLHLS, encompassing 15,874 participants. We excluded participants who did not complete the 10-item Center for Epidemiologic Studies Depression Scale (CES-D-10) and the 7-item Chinese Generalized Anxiety Disorder (GAD-7) scale, as well as those with missing or extreme values for height and weight data. Concurrently, after excluding individuals with incomplete data on pertinent covariates, we finalized a sample size of 9,098 older adults for our study. The specific screening steps are illustrated in Figure 1.
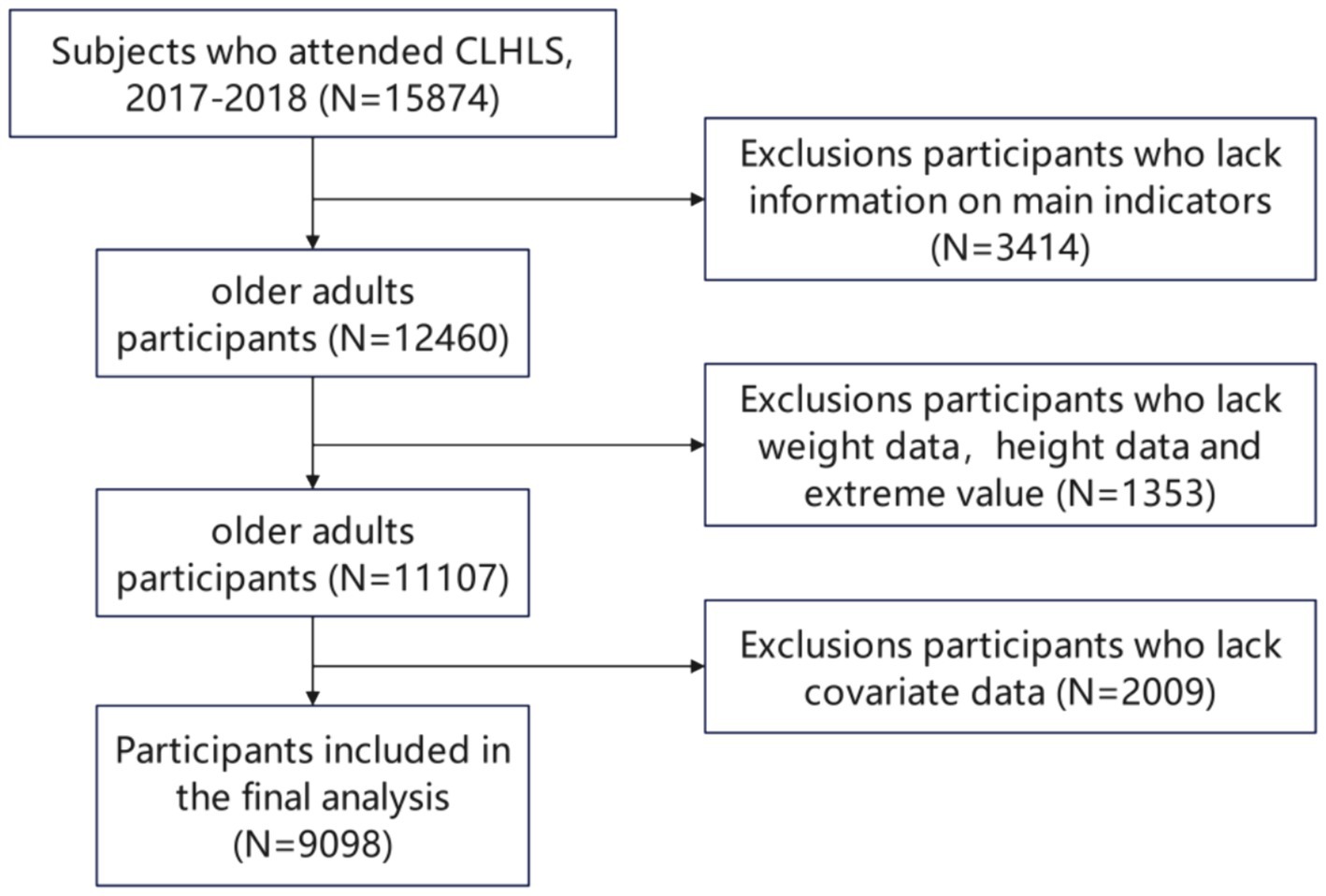
Figure 1. CLHLS database research participants screening flow chart.(DATA screening from top to bottom as indicated by the arrow).
The CLHLS study adopted the CES-D-10 questionnaire to assess depressive symptoms experienced by respondents during the previous week. This questionnaire has been validated for use among older adult individuals in China, demonstrating good reliability with a Cronbach α coefficient of 0.78–0.79 (25). The CES-D-10 scale comprises 10 questions targeting specific emotions or behaviors. Points are assigned according to the reported duration of negative emotions or behaviors: 0 points if lasting less than a day, 1 point for 1 to 2 days, 2 points for 3 to 4 days, 3 points for 5 to 6 days, and 4 points for a full week. Notably, for questions 5, 7, and 10, the scoring pattern is inverted. Based on the application research of CES-D-10 in Chinese older adult individuals (26), we defined the dichotomous depression variable with a cutoff score of 12 or above.
In the CLHLS questionnaire, anxiety was assessed using the GAD-7 scale, focusing on symptoms experienced over the past 2 weeks. The GAD-7 showed excellent internal consistency (Cronbach’s α = 0.92) and good test–retest reliability (intraclass correlation = 0.83) (27). The GAD-7 scale comprises seven items, each scored on a four-point Likert scale: never (0), several days (1), more than half the days (2), and almost every day (3). The total score, ranging from 0 to 21, reflects the severity of anxiety, with higher scores indicating greater anxiety. Consistent with prior research, a GAD-7 score of 5 or above indicates the presence of anxiety.
Based on Chinese standards (28), BMI was calculated for each participant using the formula: BMI = weight (kg) / (height (m))^2. The participants were then divided into four BMI classes according to their calculated BMI values: underweight (BMI < 18.5), normal weight (18.5 ≤ BMI < 24), overweight (24 ≤ BMI < 28), and obesity (BMI ≥ 28).
ADL disability was assessed using Katz index scale, which is evaluated based on six items: bathing, dressing, indoor transfer, toileting, eating, and continence. The IADL scales assessment includes the following eight items: visiting neighbors, shopping, cooking, washing clothes, walking for 2 kilometers continuously, lifting 5 kilograms, squatting three times continuously, and taking public transportation alone. Previous evidence has shown that ADL and IADL can be used as independent indicators for effectively predicting functional disability in the older adult (29, 30). If the respondent “can complete it by themselves,” it is coded as 1, “with some difficulty” is coded as 2, and “cannot” is coded as 3; the scoring range for ADL is 0–18, and for IADL it is 0–24.
We controlled for the following confounding factors (16, 31–36): sociodemographic characteristics (age (65–79/ ≥ 80), gender (female/male), residence area (city/town/rural), co-residence (with family/alone/nursing room), marital status (married/others), education (no school education/≥1 year), income source (pensions/family/others) and economics status (higher/medium/lower), lifestyle (tea consumption (everyday/often/hardly), smoking (yes/no), drinking (yes/no), exercise (yes/no)), chronic disease (none/1/≥2)).
We classified education as no formal education or more than 1 year of education. Current marital status was classified as married or other (divorced/widowed/never married). Subjects were categorized as current smoker or non-current smoker and current drinker or non-current drinker. Current participation in purposive fitness activities was classified as regular exercise. The number of chronic diseases (such as Hypertension, Diabetes, Heart disease, Stroke, cerebrovascular disease, Bronchitis, asthma, pneumonia, Pulmonary tuberculosis, Cancer, and Others) was recorded through self-reporting.
Frequency with percentage was used to describe categorical variables. The baseline characteristics were summarized based on depressive and anxiety symptoms, and the differences between participants with and without depressive or anxiety symptoms were analyzed using the chi-square test.
To examine the association between BMI and symptoms of anxiety and depression, logistic regression models were used to calculate odds ratio (OR) with 95% confidence interval (CI). We constructed three logistic models: the unadjusted model (Model 1); Model 1 adjusted for age, gender, residence area, co-residence, marital status, education, income source, and economic status (Model 2); Model 2 with additional adjustment for tea consumption, alcohol, smoking, exercise, and the number of chronic diseases (Model 3). We performed a set of subgroup analyses to explore whether associations varied by gender, age, marital status, and residence area.
To demonstrate whether there exist a series of multiple mediation effects of BMI and symptoms of anxiety or depression between ADL and IADL, we used SPSS macro PROCESS program (Model 6) designed by (37) for data analysis. A p-value <0.05 was considered statistically significant. We set the bootstrap confidence interval at 95% with a bootstrap sample size of 5,000. If zero was not included in the interval of 95% CI, it indicated a significant mediation effect.
Among the 9,098 participants, 1,074 cases (11.8%) exhibited anxiety symptoms, of whom 541 were classed as underweight according to their BMI. Similarly, 1,458 cases (16.0%) exhibited depressive symptoms, of whom 749 were classed as underweight according to their BMI. Factors such as BMI, age, gender, residence area, co-residence, education, income source, economic status, tea consumption, alcohol, smoking, exercise, and chronic diseases were significant determinants of anxiety and depression symptoms (p < 0.05). Marital status was a significant determinant of depression only (p < 0.05). Refer to Table 1 for further details.
As shown in Tables 2, 3, Model 1 indicates that, in comparison to individuals with normal BMI, underweight is a significant factor of anxiety and depression symptoms (OR = 1.361, p < 0.001; OR = 1.382, p < 0.001). After controlling for demographic and socioeconomic characteristics (Model 2), underweight remains a significant influencing factor affecting anxiety and depression symptoms (OR = 1.257, p = 0.014; OR = 1.180, p = 0.045). In the fully adjusted model (Model 3), underweight remains a significant influencing factor affecting anxiety and depression symptoms (OR = 1.316, p = 0.004; OR = 1.232, p = 0.013).
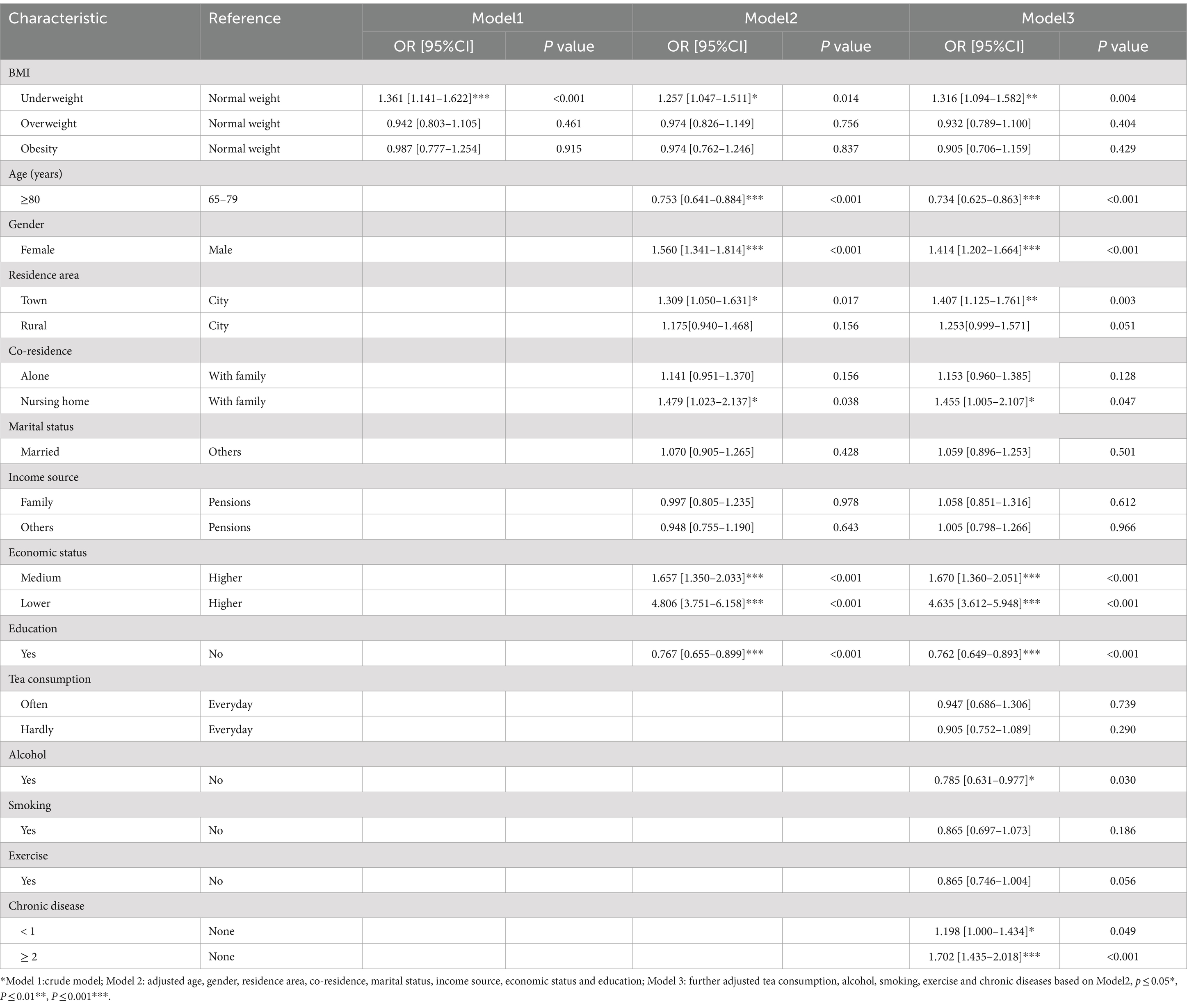
Table 2. Multivariate logistic regression analysis of the association between BMI and anxiety symptoms.
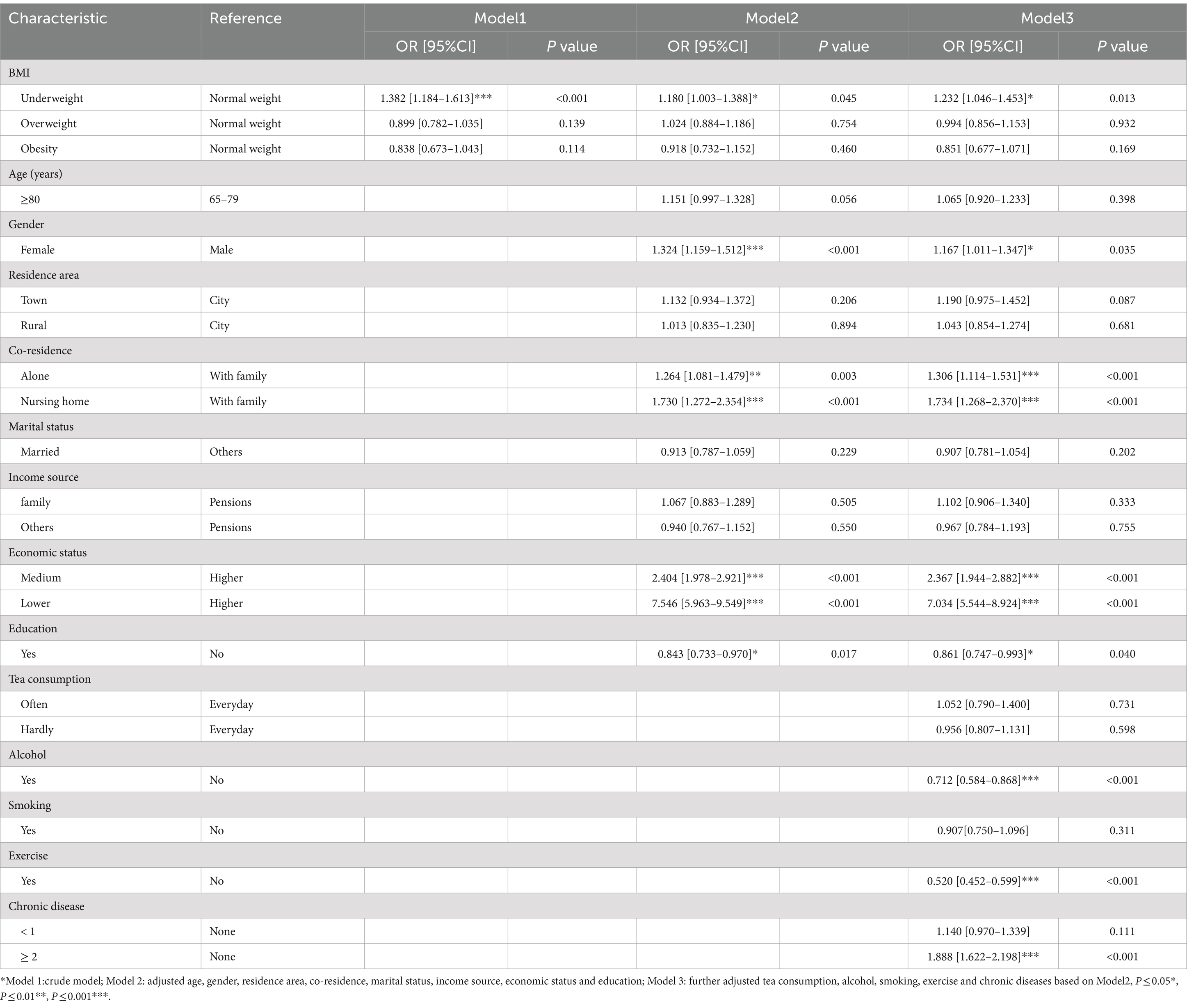
Table 3. Multivariate logistic regression analysis of the association between BMI and depression symptoms.
As shown in Tables 4, 5, in different subgroups, underweight remains a significant influencing factor affecting anxiety and depression symptoms. Among older adult individuals with underweight, males (OR = 1.565; OR = 1.554), those aged 80 and above (OR = 1.366; OR = 1.296), unmarried individuals (OR = 1.227; OR = 1.316), and those residing in town (OR = 1.526; OR = 1.427) exhibited a higher risk.
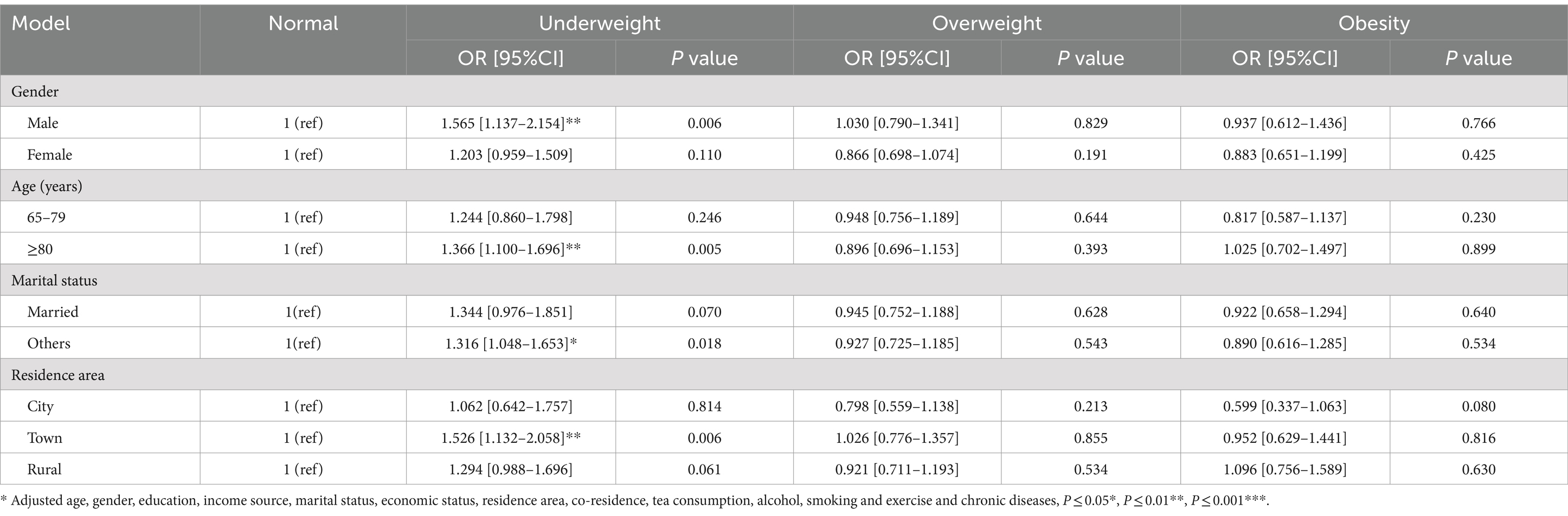
Table 4. Multivariate logistic regression analysis of the association between BMI and anxiety symptoms in different subgroups.
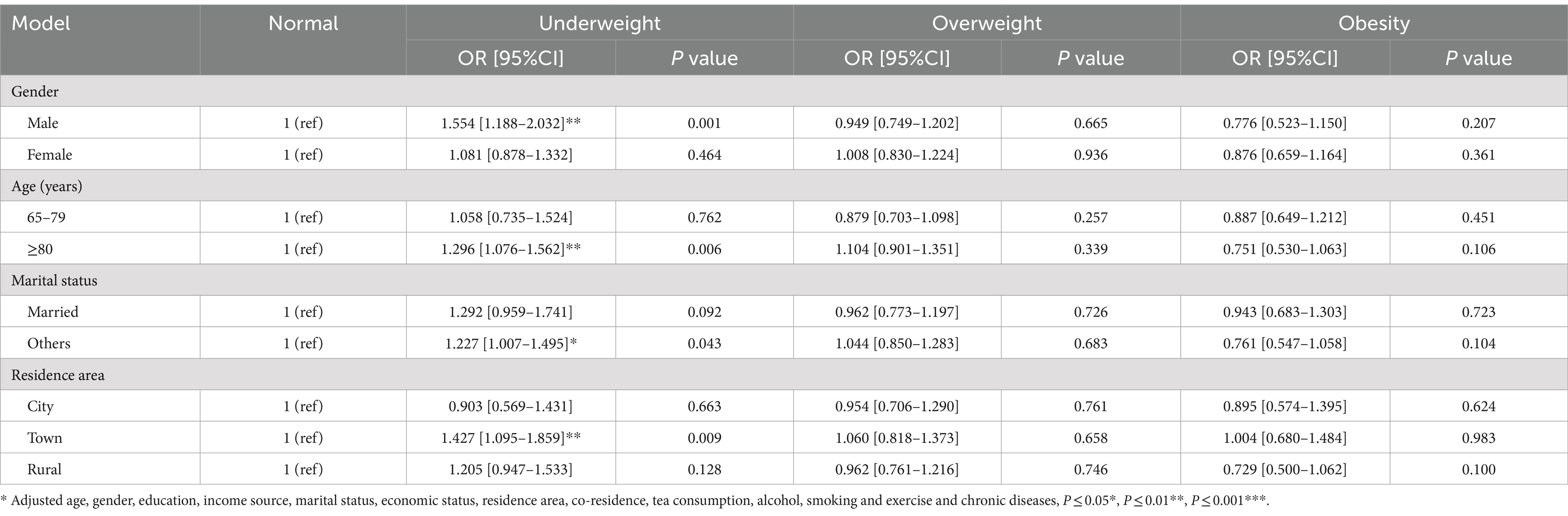
Table 5. Multivariate logistic regression analysis of the association between BMI and depression symptoms in different subgroups.
After controlling for covariates, ADL and IADL played a chain-mediated role between BMI and anxiety symptoms in the older adult. BMI not only had a direct effect on anxiety symptoms in the older adult (effect = −0.0159; SE = 0.0066; 95%CI: LL = −0.0288, UL = −0.0031), but also influenced them indirectly through two pathways: the independent mediating role of IADL (effect = −0.0010; SE = 0.0005; 95%CI: LL = −0.0018, UL = −0.0003) and the chain-mediated role of ADL and IADL (effect = −0.0012; SE = 0.0004; 95%CI: LL = −0.0020, UL = −0.0006). The detailed mediation analysis is shown in Table 6 and Figure 2. ADL and IADL do not mediate the relationship between BMI and depressive symptoms in older adult individuals is shown in Table 7 and Figure 3.
The main purpose of this study was to explore the relationship between BMI and anxiety or depression symptoms among the older adult in China, as well as investigate whether ADL (activities of daily living) and IADL (instrumental activities of daily living) can moderate the relationship between BMI and anxiety/depression symptoms. First, our research results showed a significant association between underweight and anxiety/depression symptoms. Second, among older adult individuals with underweight, males, those aged 80 and above, unmarried individuals, and those residing in urban areas exhibited a higher risk. Third, ADL and IADL played a chained mediating role in the relationship between BMI and anxiety symptoms among the older adult.
This study found that among the older adult population in China, underweight is an independent predictor of symptoms of depression and anxiety. Unlike some overseas studies (13, 36), the effect of overweight and obesity on depression and anxiety was not statistically significant compared with normal BMI. In other words, BMI levels did not show a U-shaped relationship with anxiety and depression among the older adult population in China. There is an old Chinese saying that “a broad mind brings a plump body,” which means that a person with a good mood will look calm and thus gain weight. A British survey study has proved this point, showing that the possibility of depression and anxiety is lower for the older adult as BMI increases (38). On the other hand, people with better diet quality that is rich in vegetables, lean meat, fish, and whole grains are less likely to suffer from emotional disorders or anxiety (39, 40). In addition, another possible explanation is response shift (41), which means that obese people may have adapted to their condition and begun to positively evaluate their mental health.
The study results indicate that among older adult individuals with underweight, males, those aged 80 and above, unmarried individuals, and those residing in urban areas exhibit a higher risk compared to those with a normal BMI. Older adult males are more likely to experience symptoms of anxiety and depression when they lose weight, a phenomenon that has also been reported in other studies (42–44). This may be related to the traditional Chinese concept that obesity represents a good social and economic status (45), On the other hand, it could also be associated with dieting, as unhealthy eating patterns are more likely to cause anxiety and depression (46, 47). In our study, there was no significant correlation between underweight or obesity among female participants. This is contrary to the findings of studies in Japan and Korea (48, 49), which may be related to social status (50). Married women tend to shoulder more family responsibilities (51), and work–family conflicts or interference are more likely to lead to psychological distress (52), ultimately resulting in anxiety and depression.
In terms of age, older adult individuals over the age of 80 are more prone to psychological issues, which may be related to their self-care abilities and emotional well-being. Research has shown that older adults require more financial support, daily care, and emotional support as they age (53).
In terms of marital status, consistent with previous studies (54–56), single and unmarried older adult individuals are more likely to experience symptoms of anxiety and depression. Single older adult individuals generally lack social interactions, and spouses are the primary source of support for the older adult (47). Receiving care from spouses can reduce the risk of depression among the older adult (57).
In our study, living in urban areas is more likely to lead to anxiety and depression symptoms, possibly because of the relatively stable economic level and abundant social resources in cities (58). Meanwhile, the living environment in rural areas can effectively reduce stress (59). Conversely, people living in urban areas are more likely to be affected by issues related to social resources, resulting in anxiety (35).
The study revealed that ADL and IADL play a chain-mediated role between BMI and anxiety symptoms among the older adult. Specifically, BMI is first negatively correlated with ADL, which then leads to increased limitations in IADL, ultimately exacerbating the risk of anxiety. Prior research has shown that weight loss is associated with a decrease in bone mineral content and bone density, which increases the risk of osteoporosis and fractures, resulting in ADL limitations among the older adult (60). On the other hand, underweight also leads to muscle loss and reduced muscle strength, which are significant factors contributing to ADL limitations among the older adult (61). There is also a negative correlation between underweight and IADL, as a higher BMI represents a better living standard, potentially leading to better access to medical resources, which may be beneficial for IADL function (62). Firstly, limitations in IADL increase dependence on others, thereby leading to increased anxiety in daily life (63). On the other hand, ADL and IADL impairments restrict social activities among the older adult. Previous studies have shown that more social activities can help older adult individuals achieve better mental health (64). Participating in social activities not only provides positive interpersonal interaction opportunities for the older adult, but also enriches their social life and greatly enhances their confidence in obtaining support when needed. This interpersonal interaction can effectively prevent and alleviate interpersonal issues, while an enhanced sense of support makes the older adult more resilient in the face of life adversities, reducing sensitivity to negative experiences (65), ultimately lowering their risk of anxiety (66).
Moreover, ADL/IADL impairments also have a significant impact on the participation of older adult individuals in physical activities. Regular participation in physical activities can lead to positive emotional experiences (64), thereby reducing mental health problems, which is also one of the strategies for treating anxiety and depression (67, 68).
This study possesses numerous strengths, among them a considerable and nationally representative sample of community-dwelling older Chinese adults, distinguished by a significant inclusion of the oldest-old demographic. Moreover, the CLHLS, encompassing 23 provinces or municipalities across China, covers regions that display a wide range of geographical, economic, public resource, and health characteristics, thereby offering a robust and comprehensive representation of the Chinese population. The questionnaire design that is based on international standards while also being adapted to the cultural and social context of China. Furthermore, our study adds to the limited literature on the relationship between BMI and anxiety/depression symptoms among older adult individuals in China.
However, this study also has some limitations. Firstly, our research design was a cross-sectional study, which cannot determine the causal relationship between variables. Secondly, it would be better to explore the impact of BMI on anxiety and depression among older adult individuals across different subgroups in future studies. Thirdly, other potential mediating or moderating factors could also be further studied. Finally, although some studies have shown that the data we used has good reliability, these results mainly rely on the self-evaluation of the respondents.
In conclusion, despite some limitations in our study, it still provides guidance on current health issues among the older adult. The findings indicate a significant correlation between underweight and anxiety/depression symptoms among Chinese older adult individuals. This suggests that relevant departments can take measures to reduce emaciation among the older adult, such as nutritional support, daily care, financial assistance and psychological support. These measures can further prevent ADL and IADL limitations among the older adult and ultimately reduce their risk of developing anxiety and depression symptoms.
Publicly available datasets were analyzed in this study. This data can be found here: https://opendata.pku.edu.cn/dataverse/CHADS.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the biomedical ethics committee of Peking University (IRB00001052–13074).
ZQ: Writing – original draft, Writing – review & editing. ZW: Data curation, Formal analysis, Writing – original draft. JQ: Supervision, Writing – review & editing. JZ: Project administration, Resources, Writing – review & editing. WC: Funding acquisition, Project administration, Resources, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to thank the Center for Healthy Aging and Development Studies of National School of Development at Peking University for the approval to use the 2018 CLHLS data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Allan, CE, Valkanova, V, and Ebmeier, KP. Depression in older people is underdiagnosed. Practitioner. (2014) 258:2–3.
2. Friedrich, MJ. Depression is the leading cause of disability around the world. JAMA. (2017) 317:1517. doi: 10.1001/jama.2017.3826
3. Baxter, AJ, Vos, T, Scott, KM, Ferrari, AJ, and Whiteford, HA. The global burden of anxiety disorders in 2010. Psychol Med. (2014) 44:2363–74. doi: 10.1017/S0033291713003243
4. Kozela, M, Bobak, M, Besala, A, Micek, A, Kubinova, R, Malyutina, S, et al. The association of depressive symptoms with cardiovascular and all-cause mortality in central and eastern europe: prospective results of the hapiee study. Eur J Prev Cardiol. (2016) 23:1839–47. doi: 10.1177/2047487316649493
5. Allgulander, C. Anxiety as a risk factor in cardiovascular disease. Curr Opin Psychiatry. (2016) 29:13–7. doi: 10.1097/YCO.0000000000000217
6. Cohen, BE, Edmondson, D, and Kronish, IM. State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens. (2015) 28:1295–302. doi: 10.1093/ajh/hpv047
7. Malhi, GS, and Mann, JJ. Depression. Lancet. (2018) 392:2299–312. doi: 10.1016/S0140-6736(18)31948-2
8. Su, D, Zhang, X, He, K, and Chen, Y. Use of machine learning approach to predict depression in the elderly in China: a longitudinal study. J Affect Disord. (2021) 282:289–98. doi: 10.1016/j.jad.2020.12.160
9. Scott, KM, Bruffaerts, R, Simon, GE, Alonso, J, Angermeyer, M, de Girolamo, G, et al. Obesity and mental disorders in the general population: results from the world mental health surveys. Int J Obes. (2008) 32:192–200. doi: 10.1038/sj.ijo.0803701
10. Luppino, FS, de Wit, LM, Bouvy, PF, Stijnen, T, Cuijpers, P, Penninx, BWJH, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. (2010) 67:220–9. doi: 10.1001/archgenpsychiatry.2010.2
11. Amiri, S, and Behnezhad, S. Obesity and anxiety symptoms: a systematic review and meta-analysis. Neuropsychiatrie. (2019) 33:72–89. doi: 10.1007/s40211-019-0302-9
12. Ogrodnik, M, Zhu, Y, Langhi, LGP, Tchkonia, T, Krüger, P, Fielder, E, et al. Obesity-induced cellular senescence drives anxiety and impairs neurogenesis. Cell Metab. (2019) 29:1061–1077.e8. doi: 10.1016/j.cmet.2018.12.008
13. Jung, SJ, Woo, H-T, Cho, S, Park, K, Jeong, S, Lee, YJ, et al. Association between body size, weight change and depression: systematic review and meta-analysis. Br J Psychiatry. (2017) 211:14–21. doi: 10.1192/bjp.bp.116.186726
14. de Wit, LM, van Straten, A, van Herten, M, Penninx, BWJH, and Cuijpers, P. Depression and body mass index, a u-shaped association. BMC Public Health. (2009) 9:14. doi: 10.1186/1471-2458-9-14
15. DeJesus, RS, Breitkopf, CR, Ebbert, JO, Rutten, LJF, Jacobson, RM, Jacobson, DJ, et al. Associations between anxiety disorder diagnoses and body mass index differ by age, sex and race: a population based study. Clin Pract Epidemiol Ment Health. (2016) 12:67–74. doi: 10.2174/1745017901612010067
16. Lee, J-H, Park, SK, Ryoo, J-H, Oh, C-M, Choi, J-M, McIntyre, RS, et al. U-shaped relationship between depression and body mass index in the Korean adults. Eur Psychiatry. (2017) 45:72–80. doi: 10.1016/j.eurpsy.2017.05.025
17. Backholer, K, Wong, E, Freak-Poli, R, Walls, HL, and Peeters, A. Increasing body weight and risk of limitations in activities of daily living: a systematic review and meta-analysis. Obes Rev. (2012) 13:456–68. doi: 10.1111/j.1467-789X.2011.00970.x
18. Maier, A, Riedel-Heller, SG, Pabst, A, and Luppa, M. Risk factors and protective factors of depression in older people 65 a systematic review. PLoS One. (2021) 16:e0251326. doi: 10.1371/journal.pone.0251326
19. Yan, Y, Du, Y, Li, X, Ping, W, and Chang, Y. Physical function, ADL, and depressive symptoms in Chinese elderly: evidence from the CHARLS. Front Public Health. (2023) 11:1017689. doi: 10.3389/fpubh.2023.1017689
20. Cavusoglu, C, Ileri, I, Tuna Dogrul, R, Ozsurekci, C, Caliskan, H, Cemal Kizilarslanoglu, M, et al. Relationship between psychological pain and death anxiety with comprehensive geriatric assessment in older adults. Geriatr Gerontol Int. (2020) 20:1056–60. doi: 10.1111/ggi.14045
21. Pearlin, LI. The stress process revisited: reflections on concepts and their interrelationships In: CS Aneshensel and JC Phelan, editors. The handbook of sociology of mental health. Boston, MA: Kluwer Academic Publishers (1999). 395–415.
22. Liang, Y, Yang, Y, Yang, T, Li, M, Ruan, Y, Jiang, Y, et al. Effects of cognitive impairment and depressive symptoms on health-related quality of life in community-dwelling older adults: the mediating role of disability in the activities of daily living and the instrumental activities of daily living. Health Soc Care Community. (2022) 30:e5848–62. doi: 10.1111/hsc.14016
23. Liu, Z, Huang, J, Qian, D, Chen, F, Xu, J, Li, S, et al. Does low body mass index matter? Relationship between body mass index and subjective well-being among long-lived women over 95 years of age. J Nutr Health Aging. (2016) 20:99–105. doi: 10.1007/s12603-015-0556-2
24. Zeng, Y, Poston, DL, and Vlosky, DA. Healthy longevity in China:demographic, socioeconomic, and psychological dimensions. (2008) Available at: https://link.springer.com/book/10.1007/978-1-4020-6752-5 (Accessed January 3, 2024).
25. Boey, KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. (1999) 14:608–17. doi: 10.1002/(sici)1099-1166(199908)14:8<608::aid-gps991>3.0.co;2-z
26. Cheng, S-T, and Chan, ACM. Detecting depression in Chinese adults with mild dementia: findings with two versions of the Center for Epidemiologic Studies Depression Scale. Psychiatry Res. (2008) 159:44–9. doi: 10.1016/j.psychres.2007.06.023
27. Spitzer, RL, Kroenke, K, Williams, JBW, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
28. Chinese Nutrition Society Obesity Prevention and Control Section, Chinese Nutrition Society Clinical Nutrition Section. Expert consensus on obesity prevention and treatment in China. Chin J Prevent Med. (2022) 23:321–39. doi: 10.16506/j.1009-6639.2022.05.001
29. Zhang, Y, Xiong, Y, Yu, Q, Shen, S, Chen, L, and Lei, X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. (2021) 21:30. doi: 10.1186/s12877-020-01986-x
30. Zhang, Q, Wu, Y, Han, T, and Liu, E. Changes in cognitive function and risk factors for cognitive impairment of the elderly in China: 2005-2014. Int J Environ Res Public Health. (2019) 16:2847. doi: 10.3390/ijerph16162847
31. Pei, Z, Zhang, J, Qin, W, Hu, F, Zhao, Y, Zhang, X, et al. Association between dietary patterns and depression in Chinese older adults: a longitudinal study based on CLHLS. Nutrients. (2022) 14:5230. doi: 10.3390/nu14245230
32. Li, W, Sun, H, Xu, W, Ma, W, Yuan, X, Wu, H, et al. Leisure activity and cognitive function among Chinese old adults: the multiple mediation effect of anxiety and loneliness. J Affect Disord. (2021) 294:137–42. doi: 10.1016/j.jad.2021.07.051
33. Chan, S-P, Yong, PZ, Sun, Y, Mahendran, R, Wong, JCM, Qiu, C, et al. Associations of long-term tea consumption with depressive and anxiety symptoms in community-living elderly: findings from the diet and healthy aging study. J Prev Alzheimers Dis. (2018) 5:21–5. doi: 10.14283/jpad.2017.20
34. Wang, M, and Pan, Q. Analysis of urban-rural differences in anxiety status and influencing factors among the elderly in China. Chin Gene Pract Med. (2021) 24:3963–70. doi: 10.12114/j.issn.1007-9572.2021.00.294
35. Rotărescu, VS, Matei, DB, Mircea, IA, Mirescu, AM, Nedelescu, BG, Nedelea, DG, et al. How anxious did you feel during lockdown? The roles resilience, living environment, and gender play on the level of anxiety state during pandemic isolation. Res Psychother. (2021) 23:496. doi: 10.4081/ripppo.2020.496
36. Herhaus, B, Kersting, A, Brähler, E, and Petrowski, K. Depression, anxiety and health status across different BMI classes: a representative study in Germany. J Affect Disord. (2020) 276:45–52. doi: 10.1016/j.jad.2020.07.020
37. Hayes, AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press. (2013).
38. McCrea, RL, Berger, YG, and King, MB. Body mass index and common mental disorders: exploring the shape of the association and its moderation by age, gender and education. Int J Obes. (2012) 36:414–21. doi: 10.1038/ijo.2011.65
39. Jacka, FN, Pasco, JA, Mykletun, A, Williams, LJ, Hodge, AM, O’Reilly, SL, et al. Association of western and traditional diets with depression and anxiety in women. Am J Psychiatry. (2010) 167:305–11. doi: 10.1176/appi.ajp.2009.09060881
40. Jacka, FN, Kremer, PJ, Berk, M, de Silva-Sanigorski, AM, Moodie, M, Leslie, ER, et al. A prospective study of diet quality and mental health in adolescents. PLoS One. (2011) 6:e24805. doi: 10.1371/journal.pone.0024805
41. Sprangers, MA, and Schwartz, CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med. (1999) 48:1507–15. doi: 10.1016/s0277-9536(99)00045-3
42. Dey, M, Gmel, G, and Mohler-Kuo, M. Body mass index and health-related quality of life among young Swiss men. BMC Public Health. (2013) 13:1028. doi: 10.1186/1471-2458-13-1028
43. Hopman, WM, Berger, C, Joseph, L, Barr, SI, Gao, Y, Prior, JC, et al. The association between body mass index and health-related quality of life: data from CaMos, a stratified population study. Qual Life Res. (2007) 16:1595–603. doi: 10.1007/s11136-007-9273-6
44. López-García, E, Banegas Banegas, JR, Gutiérrez-Fisac, JL, Pérez-Regadera, AG, Gañán, LD, and Rodríguez-Artalejo, F. Relation between body weight and health-related quality of life among the elderly in Spain. Int J Obes Relat Metab Disord. (2003) 27:701–9. doi: 10.1038/sj.ijo.0802275
45. Li, ZB, Ho, SY, Chan, WM, Ho, KS, Li, MP, Leung, GM, et al. Obesity and depressive symptoms in Chinese elderly. Int J Geriatr Psychiatry. (2004) 19:68–74. doi: 10.1002/gps.1040
46. Aucoin, M, LaChance, L, Naidoo, U, Remy, D, Shekdar, T, Sayar, N, et al. Diet and anxiety: a scoping review. Nutrients. (2021) 13:4418. doi: 10.3390/nu13124418
47. Marx, W, Lane, M, Hockey, M, Aslam, H, Berk, M, Walder, K, et al. Diet and depression: exploring the biological mechanisms of action. Mol Psychiatry. (2021) 26:134–50. doi: 10.1038/s41380-020-00925-x
48. Tiedt, AD. The gender gap in depressive symptoms among Japanese elders: evaluating social support and health as mediating factors. J Cross Cult Gerontol. (2010) 25:239–56. doi: 10.1007/s10823-010-9122-x
49. Hong, SM, and Hur, Y-I. Relationship between obesity and depression in Korean adults: Korea National Health and nutrition examination survey 2014. Medicine. (2017) 96:e9478. doi: 10.1097/MD.0000000000009478
50. Park, M, Jang, J, Joo, HJ, Kim, GR, and Park, EC. Association between unequal division of caregiving work and south Korean married Women’s depressive symptoms. Front Public Health. (2022) 10:739477. doi: 10.3389/fpubh.2022.739477
51. Munn, SL, and Chaudhuri, S. Work-life balance: a cross-cultural review of dual-earner couples in India and the United States. Adv Dev Hum Resour. (2016) 18:54–68. doi: 10.1177/1523422315616342
52. Grzywacz, JG, and Marks, NF. Reconceptualizing the work-family interface: an ecological perspective on the correlates of positive and negative spillover between work and family. J Occup Health Psychol. (2000) 5:111–26. doi: 10.1037/1076-8998.5.1.111
53. Cai, Y, Qiu, P, He, Y, Wang, C, Wu, Y, and Yang, Y. Age-varying relationships between family support and depressive symptoms in Chinese community-dwelling older adults. J Affect Disord. (2023) 333:94–101. doi: 10.1016/j.jad.2023.04.045
54. Fan, X, Guo, X, Ren, Z, Li, X, He, M, Shi, H, et al. The prevalence of depressive symptoms and associated factors in middle-aged and elderly Chinese people. J Affect Disord. (2021) 293:222–8. doi: 10.1016/j.jad.2021.06.044
55. Yu, J, Kahana, E, Kahana, B, and Han, C. Depressive symptoms among elderly men and women who transition to widowhood: comparisons with long term married and long term widowed over a 10-year period. J Women Aging. (2021) 33:231–46. doi: 10.1080/08952841.2019.1685855
56. Fatima, M, Sehar, A, Ali, M, Iqbal, A, and Shaukat, F. Incidence of depression among community dwelling healthy elderly and the predisposing socio-environmental factors. Cureus. (2019) 11:e4292. doi: 10.7759/cureus.4292
57. Han, SH, Kim, K, and Burr, JA. Activity limitations and depressive symptoms among older couples: the moderating role of spousal care. J Gerontol B Psychol Sci Soc Sci. (2021) 76:360–9. doi: 10.1093/geronb/gbz161
58. National Bureau of statistics. National annual statistical bulletin (2023). Available at: https://www.stats.gov.cn/sj/tjgb/ndtjgb/ (Accessed March 2, 2024).
59. Thompson, CW, Roe, J, Aspinall, P, Mitchell, R, Clow, A, and Miller, D. More green space is linked to less stress in deprived communities: evidence from salivary cortisol patterns. Landsc Urban Plan. (2012) 105:221–9. doi: 10.1016/j.landurbplan.2011.12.015
60. Coin, A, Sergi, G, Benincà, P, Lupoli, L, Cinti, G, Ferrara, L, et al. Bone mineral density and body composition in underweight and normal elderly subjects. Osteoporos Int. (2000) 11:1043–50. doi: 10.1007/s001980070026
61. Janssen, I, Heymsfield, SB, and Ross, R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. (2002) 50:889–96. doi: 10.1046/j.1532-5415.2002.50216.x
62. Bahat, G, Tufan, F, Saka, B, Akin, S, Ozkaya, H, Yucel, N, et al. Which body mass index (BMI) is better in the elderly for functional status? Arch Gerontol Geriatr. (2012) 54:78–81. doi: 10.1016/j.archger.2011.04.019
63. Demirkol, M, Namlı, Z, and Tamam, L. Psychological pain. Psikiyatride Guncel Yaklasimlar. (2019) 11:205–13. doi: 10.18863/pgy.444006
64. Chao, S-F. Changes in leisure activities and dimensions of depressive symptoms in later life: a 12-year follow-up. Gerontologist. (2016) 56:397–407. doi: 10.1093/geront/gnu052
65. Simone, PM, and Haas, AL. Frailty, leisure activity and functional status in older adults: relationship with subjective well being. Clin Gerontol. (2013) 36:275–93. doi: 10.1080/07317115.2013.788114
66. Hoffman, YSG, Grossman, ES, Bergman, YS, and Bodner, E. The link between social anxiety and intimate loneliness is stronger for older adults than for younger adults. Aging Ment Health. (2021) 25:1246–53. doi: 10.1080/13607863.2020.1774741
67. Ensari, I, Greenlee, TA, Motl, RW, and Petruzzello, SJ. META-analysis of acute exercise effects on STATE anxiety: an update of randomized controlled trials OVER the past 25 years. Depress Anxiety. (2015) 32:624–34. doi: 10.1002/da.22370
Keywords: BMI, depressive symptoms, anxiety symptoms, mediation effect, ADL, IADL
Citation: Qiao Z, Wang Z, Qiu J, Zhang J and Cao W (2024) Analysis of the effect of BMI on depression and anxiety among older adults in China: the mediating role of ADL and IADL. Front. Public Health. 12:1387550. doi: 10.3389/fpubh.2024.1387550
Received: 18 February 2024; Accepted: 26 August 2024;
Published: 04 September 2024.
Edited by:
Duarte Miguel Henriques-Neto, University of Maia, PortugalReviewed by:
Viskasari P. Kalanjati, Airlangga University, IndonesiaCopyright © 2024 Qiao, Wang, Qiu, Zhang and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiyi Cao, MTIxMDcxMDA3MEBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.