- Department of Community Health Sciences, School of Public Health, Boston University School of Public Health, Boston, MA, United States
Introduction: The Massachusetts Academic Health Department Consortium (AHD) established the Academic Public Health Volunteer Corps (APHVC) to support Local Health Departments (LHDs, n = 351) to meet rapidly emerging needs during the COVID-19 pandemic through engaging student volunteers. A program evaluation captured lessons learned and informed recommendations for sustainability and future replication.
Methods: The mixed-methods evaluation leveraged the Consolidated Framework for Implementation Research (CFIR). Data were stratified by LHD engagement with APHVC. Quantitative surveys informed probes for qualitative focus groups and interviews; findings were categorized into CFIR constructs using a deductive approach.
Results: One-fifth of LHDs (n = 76, 27 used APHVC services, 45 did not) completed the survey. Eleven employees participated in follow-up focus groups or interviews. APHVC filled resource gaps, built capacity, and provided high-quality deliverables. LHDs experienced issues with reliability and communication of volunteers and lacked time to train volunteers.
Conclusions: CFIR aided in evaluating APHVC in real time, producing actionable recommendations for best practices, dissemination, and future iterations of the program. Results are being used to enhance program effectiveness and sustainability, community health, and health equity across Massachusetts, and may help inform academic practice-based programs across the United States.
Introduction
Local health departments (LHDs) are governmental entities that play a central role in supporting the health of communities and address health areas ranging from infectious diseases to injury prevention to healthcare access (1, 2). There are over 2,800 LHDs (2) in the United States; they are consistently underfunded and understaffed (2, 3), hindering timely responses during public health emergencies like the COVID-19 pandemic.
LHD challenges were exacerbated during the pandemic, with 76% of LHDs reporting insufficient staffing and 47% reporting a lack of dedicated pandemic funding (4). They had inconsistent and inadequate guidelines and communication from federal and state governments (4, 5); a need for increased staff capacity in resource management, diversity and inclusion, and effective communication (6); and, a lack of data and community partnerships that added additional burdens (4). About 70% of LHDs expanded the provision of emergency preparedness and routine epidemiologic and surveillance services to respond to the pandemic (4, 7). This interfered with the provision of other key LHD services such as obesity prevention (75% of LHDs reduced services), high blood pressure screening (67%), blood lead screening (61%), environmental health inspections (48%), and immunizations (47%) (4, 7).
Massachusetts has 351 LHDs that are responsible for unique jurisdictions within the state, the highest number in the United States (4, 7). Due to this decentralized system, Massachusetts LHDs faced obstacles and inefficiencies in sharing resources and practices, despite reporting increased communication during the pandemic (8). LHDs reported that a centralized, regional approach to COVID-19 would have resulted in more streamlined efforts and resource-sharing, uniformity in messaging and policy implementation, and improved coordination and standardization of public health training (7).
Historically, academic-practice partnerships have proven beneficial in a variety of under-resourced contexts. For example, clinically-oriented partnerships pair nursing students and medical trainees with local hospitals (8–12), and non-clinical partnerships pair public health students or university researchers with LHDs (10, 13, 14). These alliances demonstrate benefits for all stakeholders; students and early career professionals gain valuable hands-on skills and infuse the workforce with innovative ideas, while organizations gain personnel, new perspectives, and support for infrastructure (15).
In response to pandemic-related challenges and building on the known benefits of practice-academic linkages, the Academic Health Department Consortium (AHD), which is comprised of the Massachusetts Department of Public Health and thirteen academic institutions, launched the Academic Public Health Volunteer Corps (APHVC) in March 2020 (16). APHVC paired public health students and alumni volunteers with LHDs seeking additional resources (17). This novel partnership was designed to benefit LHDs and early public health professionals alike (16).
APHVC underwent a mixed-methods evaluation (MME) guided by the Consolidated Framework for Implementation Research (CFIR) (18) to identify successes and areas for growth from the perspectives of Massachusetts LHDs that did and did not utilize APHVC. The program evaluation aims were to identify the diverse needs of LHDs during the COVID-19 pandemic and the extent to which APHVC fulfilled those needs; identify barriers to uptake of APHVC and future motivations for engagement among those who used and did not use APHVC; and, issue recommendations regarding sustainability, improvement, and replication to the APHVC implementing agencies. Evaluation findings ensure that future iterations of APHVC support LHDs in accessing resources and sustaining services.
Methods
Program description
In March 2020, the AHD established APHVC in response to the COVID-19 pandemic (16). The academic-practice based partnership aimed to leverage a large volunteer base of students and alumni to assist, enhance, and expand local health efforts (19). While APHVC initially focused on COVID-19 testing and community contact tracing (7), it quickly expanded to include additional response efforts, such as community outreach, message development, data collection, and analysis. For APHVC volunteers, the program's goal was to provide hands-on experience and exposure to LHD work, creating opportunities for career development, ultimately strengthening the public health workforce pipeline.
Conceptual framework
To understand the challenges and successes of APHVC, a mixed-methods evaluation (MME) was conducted according to the Consolidated Framework for Implementation Research (CFIR), which assists in providing insights into specific factors that influence program implementation of an intervention to encourage future effective enhancements (18). It is regularly used to systematically analyze and organize program implementation findings, particularly those with a large environmental influence.
This program evaluation was conducted before the current CFIR updates (20), and the established CFIR (18) was used to understand the perspectives of LHDs on APHVC, identify the factors that influenced APHVC program use or non-use, and present cohesive and actionable recommendations for future program iterations. This was accomplished through consideration of the five CFIR domains: characteristics of the intervention, outer/inner setting, implementation climate, characteristics of individuals, and process. Across those domains, there are nearly 40 constructs that represent different components of influence for implementation of a program like APHVC (18). Therefore, a menu of constructs approach was used (21) in which pre-determined constructs are used for the development of surveys and interview guides to assist in focusing data collection and analysis on the most relevant constructs.
Study design
The MME used quantitative and qualitative assessments to explore contexts and perspectives of LHDs. The authors collaborated with implementing agencies in the design, development, conduct, and execution of the evaluation. The quantitative results provided probes for the qualitative assessments. In addition to using CFIR to guide data collection and analysis, a logic model that was developed collaboratively by the implementing agencies and the evaluation team, further synthesized the practice-focused outcomes and guided recommendations for future application. The program evaluation received exempt approval from human subjects research review by the Boston University Medical Campus Institutional Review Board.
Study sample
The implementing agencies emailed a Qualtrics survey to contacts in all 351 Massachusetts LHDs, regardless of their engagement with APHVC. This allowed key LHD contacts to receive the evaluation invitation from a known and trusted sender. LHDs were given approximately three weeks to complete the survey with two reminders. Surveys were initiated by 118 respondents and completed by 72 LHDs (use = 27, non-use = 45).
Survey respondents who expressed interest in participating in a follow-up focus group or interviews were invited via email by the evaluation team to participate. Interviews were offered to those who could not join a focus group due to scheduling conflicts. Respondents were told responses were confidential. Participation was not incentivized. Focus groups and interviews were conducted over Zoom with two evaluation team members present. They facilitated discussions and transcribed the responses.
Respondents were categorized into use (worked for an LHD that used APHVC between March 2020 to August 2021) and non-use (worked for an LHD that did not used APHVC between March 2020 to August 2021) groups. Of the 72 LHD representatives that responded to the survey (use = 27, non-use = 45), 11 participated in focus groups and interviews (use = 5, non-use = 6).
Data collection
The survey took < 15 min to complete and assessed the characteristics of LHDs and communities served, the impact of COVID-19 on LHD efforts and resources, experiences working with APHVC volunteers (when applicable), and the benefits and challenges of APHVC utilization (when applicable). Survey questions, organized by the five CFIR domains, were developed using pre-existing publicly-available surveys (22) and aligned with the program outcomes. Certain questions were answered by all respondents; a subset of questions was completed based on APHVC use.
Subsequent qualitative data collection extracted findings from survey respondents and provided contexts on the needs and perspectives of LHDs. A focus group guide was developed using data from the quantitative surveys, aligning questions with the five CFIR domains and using quantitative results to generate probes. Each session lasted between 30–90 min, and focused on gaps in public health infrastructure before and during COVID-19, reasons for engaging or not engaging with APHVC, challenges working with APHVC students, and resources and supports that should be considered for future engagement with the APHVC.
Data analysis
Survey results were analyzed in SAS (version 9.2). Descriptive statistics were generated. For continuous data, means were calculated and chi-square tests and t-tests were performed to test for statistical significance (threshold set at p < 0.5). For categorical data, frequencies were used.
Stakeholder interviews were coded deductively, simultaneously line-by-line by two members of the evaluation team using a priori set of CFIR constructs (codes). Data were crossed referenced with CFIR domains and assessed for inclusion in the report of constructs, results, and recommendations. Coders determined if each code had a positive, negative, or neutral association with the implementation of APHVC. Discrepancies in categorization were discussed and resolved with a third member until consensus. After coding was complete, data were organized into analytic matrices for review and identifying implementation patterns, themes, and exemplar quotes (23).
Results
Survey findings
A total of 76 individuals completed the survey: 27 who used APHVC, 45 who did not, and 4 who were not sure.
Survey respondents had a variety of job functions as defined by the Department of Public Health (directors 37%, nurses 22%, health agents 17%, board of health members 12%, registered sanitarian 12%, health officers 8%, consultants 3%, and other 11%); years of service at that LHDs (36% >10 years, 25.3% 1–3 years, and 17.3% 6–10 years); and, number of staff employed at an LHD varied by community (mean = 6 individuals; std = 10.65, min = 0 max = 60; Table 1). Most survey respondents (60%) did not use APHVC. Those who did and those who did not were broadly distributed across the state, with higher reports of use in Eastern Massachusetts (Figure 1). Location of academic partners did not appear to influence the use of APHVC.
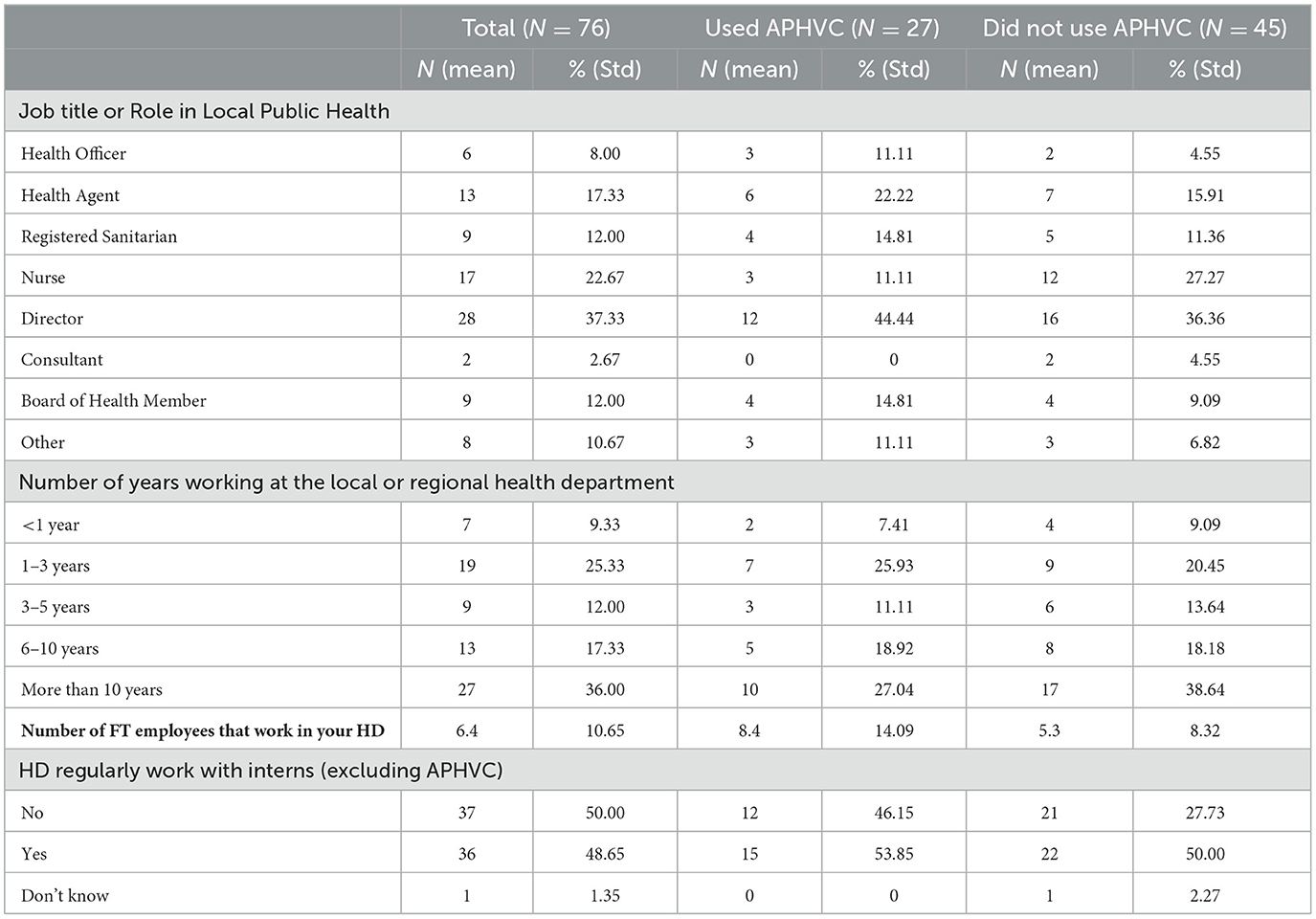
Table 1. Characteristics of Local Health Department Respondents across Massachusetts from 2020 to 2021.
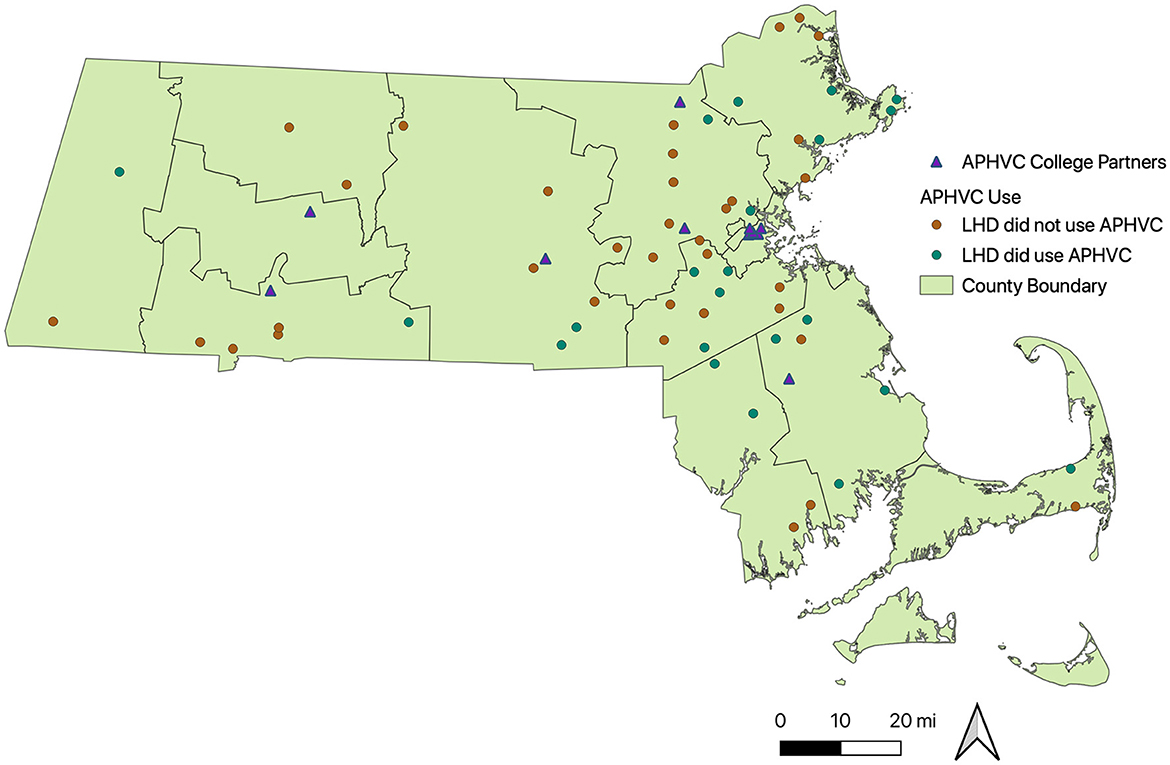
Figure 1. Locations of Academic Public Health Volunteer Corps Usage by Local Health Department (n = 351) and College Partners in Massachusetts between 2020–2021. Data sources: APHVC use—Survey data: Alyson Codner. College partnerships: https://academicpublichealthvolunteercorps.org/about/. Country Boundaries: https://www.mass.gov/info-details/massgis-data-counties#downloads-.
Among respondents who used APHVC, 71% reported that it was a useful asset for COVID-19-related activities, and 88% would use APHVC again. For non-COVID-19-related activities, 24% of respondents agreed there was a strong need for APHVC services. Many respondents (43%) indicated they somewhat agree that APHVC may support LHDs. Most respondents (71%) that used APHVC indicated that APHVC added value and filled gaps in work competencies lacking within their LHD.
Respondents who used APHVC (36%) reported being satisfied with services received; qualitative findings confirmed these responses. Data analysis, data visualization, infographics, and signage were identified as the most valuable services they used and should be kept in future versions of the program.
Respondents who did not use APHVC (60%) reported they tried to use APHVC but had a bad experience or faced various barriers; 44% noted they did not have time or resources to train and supervise volunteers, over 50% said they did not know why their LHD did not use APHVC, and 42% did not know how to engage and did not have enough information to use APHVC. Of respondents who did not use APHVC, 20% had concerns about quality of project/deliverables, 22% had concerns about students' readiness, 46% were concerned about the staff oversight requirements, and 40% reported having no concerns. Additionally, respondents reported that assistance with data analysis (69%), social media (66%), website content (60%), and grant writing (57%) would continue to be beneficial in the future; these responses were confirmed by the qualitative findings.
Qualitative findings
Eleven survey respondents (14%) participated in a focus group or interview. Findings are presented according to CFIR constructs and separated by APHVC use and non-use (Table 2).
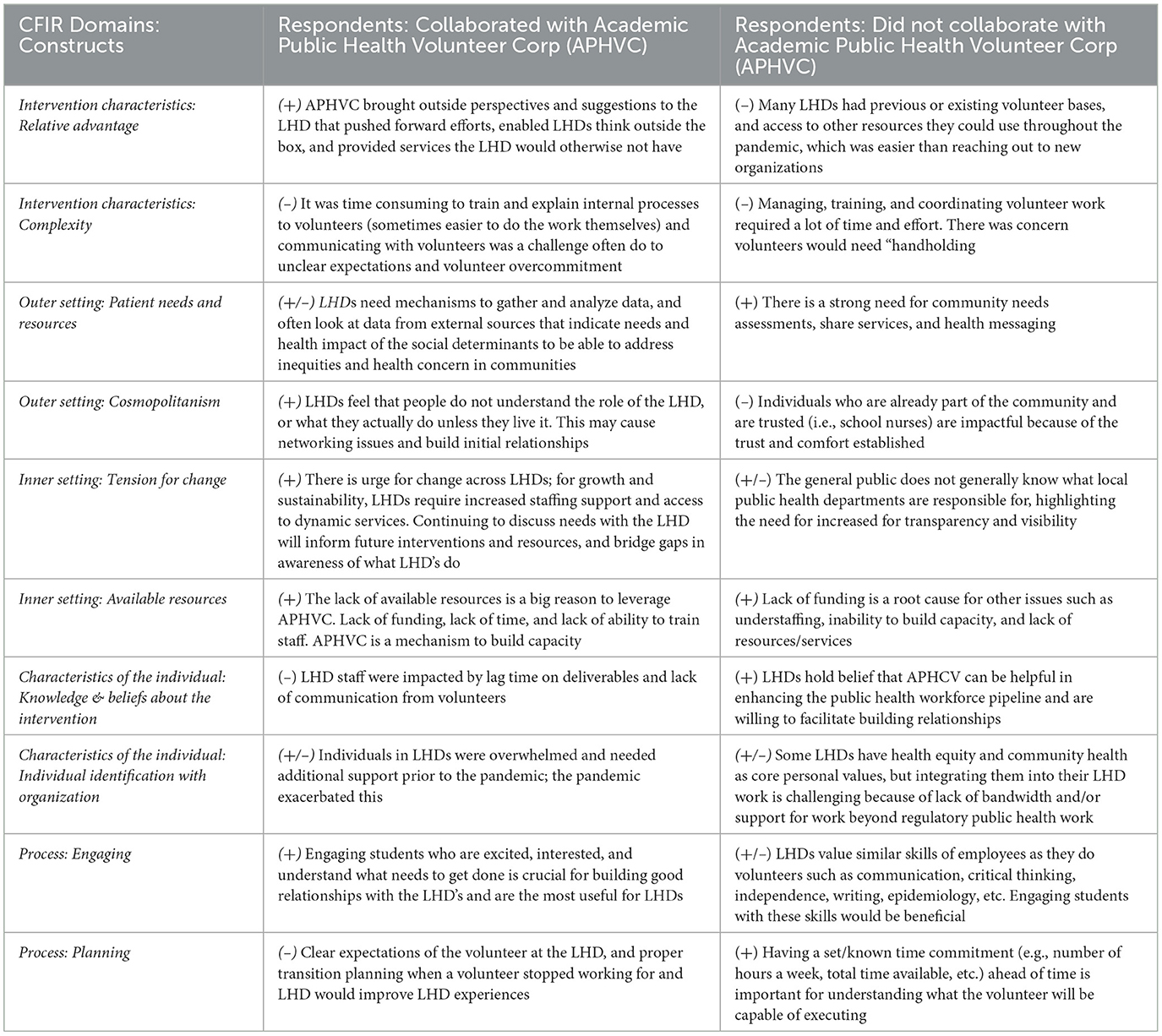
Table 2. Examples of Key Qualitative Themes from Local Health Department Respondents (n = 11) from 2020 to 2021 by the Consolidated Framework for Implementation Science Construct.
Intervention characteristics
The intervention characteristics domain identifies key attributes of the intervention that assists in identifying barriers and facilitators that impact the implementation success of the intervention including cost, complexity, and evidence strength.
APHVC use
Respondents recognized that volunteers provided high-quality deliverables, brought new perspectives, and encouraged LHDs to think more broadly about their programs. However, they noted that training and supervising volunteers often required more effort and work than if the LHD staff had completed certain projects or work themselves. Challenges included: time required to match, train and oversee a volunteer not familiar with the community; lag times for deliverables; gaps in communication; and, lack of a plan to address problems.
APHVC non-use
Those who did not collaborate with APHVC commented on their lack of knowledge of services offered or how to access the program. Many of them utilized pre-existing contract and volunteer services that were easier to access and offered skills beyond traditional public health. For direct community work, respondents indicated they needed people from within the community whom they already knew and trusted. Importantly, they noted having a minimum and standard time commitment from students, and a volunteer liaison would be helpful in training and supervising volunteers.
Outer setting
The outer setting refers to the environmental, social, political, and economic context outside of an implementation organization's control and plays a dynamic role with the inner setting. This domain addresses external factors such as policies and incentives, needs and resources, and competitive pressure to implement an intervention.
APHVC use
LHDs require data, specifically on health and social inequities within the population, to respond to community needs. During COVID-19, LHDs had access to some state and community-level data, but was not prepared for the rapid COVID-19 response and the need for additional staff and resources (e.g., community response services, mental health, wellness programs). Along with inconsistent COVID-19 communication and frequent changes in mandates, respondents reported that their health departments struggled to determine the best course of action for resolving these issues or addressing community needs.
APHVC non-use
Non-use LHDs lacked both awareness of community needs and capacity to conduct a rapid community needs assessment. Their representatives who responded to the survey believed working with trusted individuals within their community, as opposed to external APHVC volunteers, would enhance their COVID-19 response. Moreover, while grant funding would have been beneficial for them to acquire, they indicated it was difficult to seek APHVC assistance due to the rigid requirements for the process and that the service was shared across different jurisdictions.
Inner setting
The inner setting domain addresses organizational factors (e.g., available resources, networks and communication, culture, readiness for implementation) that respondents perceive directly impact the implementation.
APHVC use
Respondents reported that their LHDs lacked staff and recognized that APHVC volunteers could temporarily fill gaps and provide services that they could not do. Yet, some staff indicated they were unable to grow and develop new services as desired, and lacked staff to launch them. High staff turnover also impacted their capacity to train and supervise short-term volunteers. They were not able to prioritize volunteers over the needs of long-term staff.
APHVC non-use
Similarly, non-use LHDs reported limited time and resources as a common reason for not using APHVC; respondents indicated they wanted to conduct community assessments and acquire more funding, staff, data, and resources but were not able to. They noted their LHDs would have sought after APHVC support more if there had been greater compatibility between the services needed and APHVC services offered.
Characteristics of individuals
The characteristics of individuals domain address the perceptions, knowledge, confidence, and commitment to change of the individuals within the organization as related to an intervention's success.
APHVC use
Respondents reported that their LHD staff found APHVC to be an important learning opportunity for volunteers because they had similar valuable experiences in practice-based programs when they were students. Additionally, after using APHVC, many felt they knew how to best utilize volunteers' time and expertise if there were future iterations of the program. However, issues with deliverable lag time, communication, and limited time of volunteers were challenges associated with using APHVC. They disclosed being overwhelmed and burnt out with the numerous barriers to attracting new employees. They indicated that a valuable aspect of APHVC is its potential for recruiting volunteers to the LHD workforce.
APHVC non-use
Non-use LHDs discussed limited bandwidth and time to engage with new programs, highlighting needing to improve APHVC workflow to reduce burden. LHDs desire volunteers who work independently and collaboratively, are willing to learn, and have skills in writing and epidemiology.
Process
The process domain considers engagement strategies, delivery of the intervention, leadership roles, and feedback. This domain is important for understanding sustainability, program champions, leadership structure, and networks as well as program evaluation and reflection of processes and protocols.
APHVC use
Respondents connected student engagement, enthusiasm, and interest to building strong relationships, increasing the likelihood of ongoing program use. Likewise, clear expectations, volunteer skills, commitment, and ownership reduced their LHDs' burden. Inconsistent communication, commitment, and unrealistic expectations were attributed to negative experiences.
APHVC non-use
Respondents from non-use LHDs emphasized the need to have resources for health departments across the state, so they could tap into volunteers who have “valuable” skills (e.g., strong communication skills, ability to use social media to share information, epidemiologic skills, etc.) and/or a volunteer liaison (who can help supervise and train volunteers to facilitate stronger engagement of target communities).
Discussion
The COVID-19 pandemic exacerbated unmet needs across communities and exposed gaps in the public health infrastructure. Few who receive formal public health training are choosing to work in local public health (24) due to limited benefits, non-competitive wages, and few opportunities for development and advancement (25, 26), While there have been investments made to strengthen the public health workforce in the long-term (27), more rapid and innovative solutions are needed to reduce the current health burden faced by communities (4, 28). Academic-practice based partnerships may help address these needs.
This mixed-methods evaluation (MME) of Academic Public Health Volunteer Corps (APHVC) provided detailed insights into an academic-practice based partnership that informed sustainability and replication of the program. LHDs that utilized APHVC indicated that volunteers filled resource gaps, enhanced their capacity to meet community needs, and created high-quality deliverables. Those that did not engage with APHVC cited insufficient time, bandwidth, and staff to train and engage volunteers, highlighting the need to reduce program burdens. Because of the shortage in staffing and available resources across LHDs and with the potential for academic institutions to provide improved support, initiating partnerships like APHVC could represent a real world solution for helping improve and augment public health services during emergencies like COVID-19 and beyond.
Models like APHVC are well-suited to fill staffing gaps, and could potentially enable LHD staff to apply for grant funding to increase resources. Importantly, these partnerships provide high-quality and diverse services compatible with LHDs' needs and act as a mechanism to build capacity in the local public health workforce. These MME findings are similar to those for other academic and community partnerships that improved the efficiency of work when staffing is low, that increased the number of individuals working in public health, and that brought academic expertise to local public health (29, 30).
LHDs, however often lacked the staff and time to train, communicate with, and supervise short-term student volunteers. This is consistent with other findings in the literature, which confirmed that staffing and the time required to supervise students can be a significant challenge when organizations do not know if the collaboration will improve outcomes or result in return on investment (31). Comprehensive planning to operationalize volunteers (30) and the ability to mitigate time constraints through additional administrative support may be needed and should be encouraged in future iterations of programs.
There are other strategies and activities that APHVC or similar models could explore in the future to potentially optimize a program. While many LHDs expanded and modified services to respond to the pandemic, they also reduced many core functions such as various screening, prevention, and immunization services; services that could have directly impacted transmission, illness severity, comorbidities, and other health outcomes related to the pandemic. APHVC volunteers could have assisted in managing these pre-existing LHD services that were de-prioritized due to the pandemic. LHDs would not only benefit volunteers in learning about the functionality and impact of LHDs in communities, but also could facilitate provision of developed community services to improve community health and to provide a tertiary benefit of supporting pandemic related health outcomes.
Additionally, APHVC and similar model programs could support LHDs in applying different methods of community engagement as well as strategic communication, including using the latest science, techniques, and ideas, discussed in coursework to support and inform disease prevention guidance for target communities. Many LHDs relied heavily on expectations and federal and state authority to act and engage, often without robust outreach or messaging tailored to target audiences. APHVC volunteers could have brought innovative ideas and deep knowledge and skills in new technologies and engagement. Ultimately, volunteers could serve as an extra resource to support departments in modifying interventions so they better meet community needs, build trust, reinforce collaboration in developing and utilizing various modes of communication, and increase the depth of knowledge and services to inform public health policy and practice.
Despite existing barriers, LHDs and academic institutions can have a reciprocal relationship leading to quality improvements in the provision of public health services (32, 33). The MME findings suggest that LHDs could work with APHVC to enhance the public health workforce pipeline and increase the visibility of local public health while providing students with real-world experience. Public health workforce and infrastructure development are ongoing priorities for national government agencies (34), and the bi-directional relationship between LHDs and academic institutions could and should continue to help build capacity and provide further resources for the public health workforce.
Evaluating this mass mobilization of public health volunteers through an implementation science framework produced tangible recommendations (Table 3) for APHVC's implementing agency and for any institution seeking to support local public health infrastructure. The MME informed changes to the APHVC, which was redeveloped into the Academic Public Health Corps (APHC) in 2021 and has been formalized as an academic-practice base partnership work education program to support public health agencies across the state of Massachusetts. The APHC is currently undergoing a longer-term MME that seeks to build on the work presented herein. This longer-term MME will work to understand if the program is being implemented as intended, measuring impact on its target population, meeting program goals, and much more.
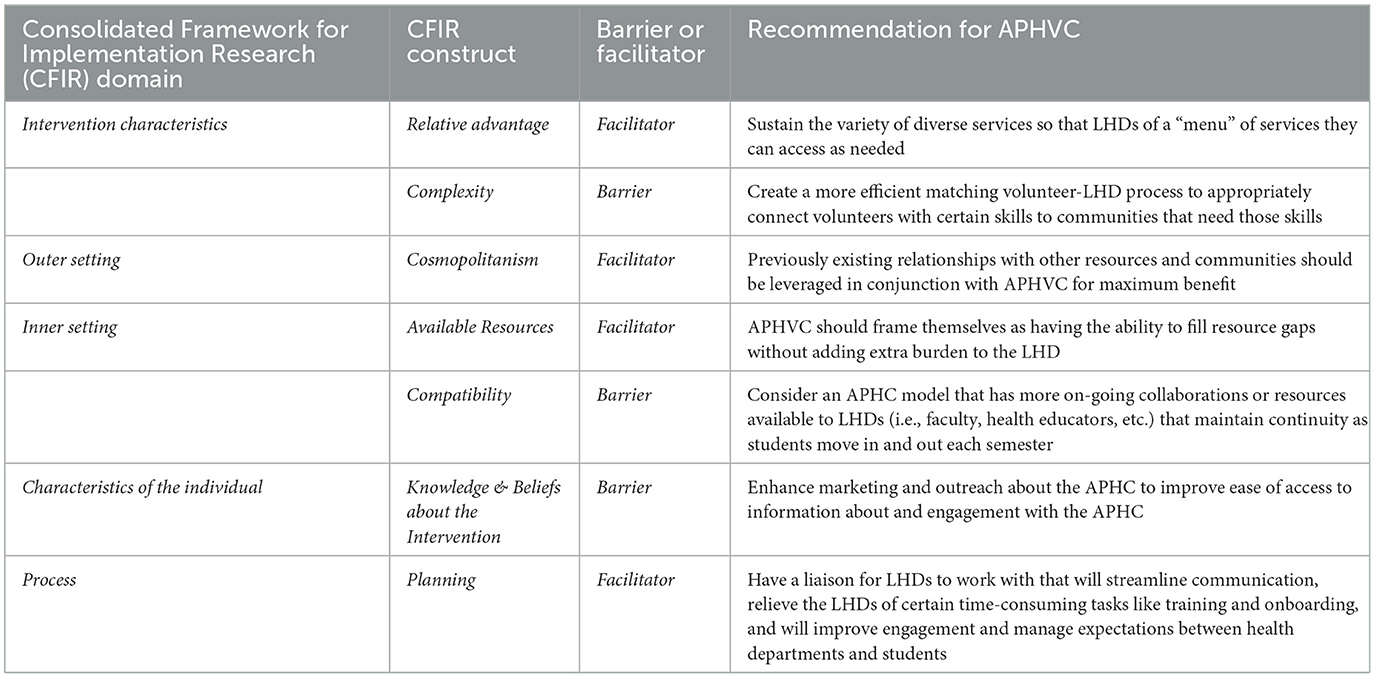
Table 3. Recommendations to the implementing agency in 2022 to Improve the Academic Public Health Volunteer Corps.
Strengths and limitations
To our knowledge, this particular academic-practice based partnership is unique among those found in the literature. APHVC is the first state-wide partnership available to any LHD, to public health students, and alumni from multiple universities, as compared to a specifically collaboration between a single LHD and a single university. To our knowledge, it is the only evaluated academic-practice based partnership developed during COVID-19 that mobilized public health students.
The MME has several limitations. First, the evaluation included students who previously volunteered for APHVC. While this provided greater insights into program operations from students, this nuanced aspect of the evaluation may have also biased the overall objectivity of the evaluation analyses. Second, LHD staff remained overstretched during the MME. Thus, the qualitative component of the evaluation was less robust (i.e., the program evaluation would have benefited from more participation of LHD stakeholders in the focus groups and interviews). Finally, findings and lessons learned may not be generalizable because health department structures and resources vary from state to state during the pandemic, often operating in a variable fashion, as a de-centralized system (such as in this case), as a centralized system, or as some combination of both.
Future research should expand the assessment of stakeholders to better understand their varying perspectives, their needs, and how to best prepare them for working with volunteers, so that APHVC experiences are mutually beneficial. Continual evaluation of model programs like APHVC will yield greater understanding of how they work and enable LHDs to make informed decisions and changes required to improved community health and individual health-related outcomes.
Public health implications
This MME encapsulates the multi-faceted dynamics of implementing a novel academic-practice based program that can be used to improve program operations on a local or national scale. The repercussions and health and social impacts caused by the COVID-19 pandemic endure, and local public health is more resource-constrained than ever before to address emerging and ongoing threats to the health of communities. Partnerships like APHVC can help strengthen the LHD workforce, mitigate the effects of a health crisis, and build LHD capacity to better meet community needs regardless of emergencies. Such programs are also beneficial to early public health professionals, who can practical skills and may join the public health workforce after graduating from school. With limited examples of these partnerships, working to understand them and improve existing partnerships through program evaluation will be key actions for enhancing public health preparedness and capacity to address public health core functions in the post COVID-19 recovery era.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Boston University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin because this study was approved as exempt. Verbal informed consent was obtained and approved.
Author contributions
SF: Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. PE: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing, Writing – original draft. AC: Data curation, Formal analysis, Writing – review & editing. HA: Data curation, Formal analysis, Project administration, Writing – original draft, Writing – review & editing. AC: Data curation, Formal analysis, Writing – review & editing. ZW: Data curation, Formal analysis, Writing – review & editing. JG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Boston University Clinical and Translational Science Institute through a grant from the NIH/NCATS UL1TR001430.
Acknowledgments
The authors acknowledge the members of local health departments who participated in our evaluation while serving their communities during the pandemic. We are grateful to our partners at the Academic Health Department Consortium, particularly Antonia Blinn with the Massachusetts Department of Public Health, Drs. Virginia Chomitz and Wenhui Feng with Tufts University, along with the Massachusetts Health Officers Association.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Glossary and Resources for the Local Health Department Strategy | HAI | CDC. (2023). Available online at: https://www.cdc.gov/hai/hai-ar-programs/resources/local-strategy/resources.html (accessed April 16, 2023).
2. NACCHO-2019-Profile-Study-Infographic.pdf. Available online at: https://www.naccho.org/uploads/downloadable-resources/NACCHO-2019-Profile-Study-Infographic.pdf (accessed October 11, 2022).
3. McKillop M, Lieberman DA, McIntyre K, Reavis B, Thomas C, West M. The Impact of Chronic Underfunding on America's Public Health System: Trends, Risks, and Recommendations, 2022. Trust for America's Health (2022). Available online at: https://www.tfah.org/wp-content/uploads/2022/07/2022PublicHealthFundingFINAL.pdf (accessed November 20, 2023).
4. Hall K, Brees K, McCall T, Cunningham M, Alford A. NACCHO 2020 Forces of Change Survey Report. National Association of County and City Health Official. Available online at: https://www.naccho.org/uploads/downloadable-resources/2020-Forces-of-Change-The-COVID-19-Edition.pdf (accessed August 27, 2023).
5. Wozniczka D, Demeke HB, Thompson-Paul AM, Ijeoma U, Williams TR, Taylor AW, et al. Real-time CDC consultation during the COVID-19 pandemic—United States, March–July, 2020. Int J Environ Res Public Health. (2021) 18:7251. doi: 10.3390/ijerph18147251
6. Zemmel DJ, Kulik PKG, Leider JP, Power LE. Public health workforce development during and beyond the COVID-19 pandemic: findings from a qualitative training needs assessment. J Public Health Manag Pract. (2022) 28(Supplement 5):S263–70. doi: 10.1097/PHH.0000000000001524
7. Mauzy S, Putney K, Baroni E, Dey A, Elangovan K, Ji G, et al. Lessons learned: the varied responses of Massachusetts' local health departments during the COVID-19 pandemic. J Public Health Manag Pract. (2022) 28:344–52. doi: 10.1097/PHH.0000000000001547
8. Zerwic JJ, Montgomery LA, Dawson C, Dolter KJ, Stineman A. Planning and implementing a practice/academic partnership during COVID-19. J Prof Nurs. (2021) 37:24–8. doi: 10.1016/j.profnurs.2020.11.007
9. Cygan HR, McNaughton D, Reising V, Reid B. An academic practice partnership: building capacity to meet sexual health education policy requirements of a public school system. Public Health Nurs. (2018) 35:414–9. doi: 10.1111/phn.12527
10. Davis RA, Travers Gustafson D. Academic-practice partnership in public health nursing: working with families in a village-based collaboration. Public Health Nurs. (2015) 32:327–38. doi: 10.1111/phn.12135
11. Gillett C, Mason S, Fleming L, Mayer DK, Bryant AL. An academic–practice partnership during COVID-19 pandemic: transitioning from a clinical to virtual fellowship. J Clin Nurs. (2022) 31:347–52. doi: 10.1111/jocn.15817
12. Akintobi TH, Dawood N, Blumenthal DS. An academic-public health department partnership for education, research, practice, and governance. J Public Health Manag Pract. (2014) 20:310–4. doi: 10.1097/PHH.0b013e31829dc256
13. Erwin PC, Brownson RC. The academic health department: aging gracefully? J Public Health Manag Pract. (2019) 25:32–3. doi: 10.1097/PHH.0000000000000924
14. Morgan IA, Tucker C, Urlaub DM, Shuler TO, Cilenti D. Leveraging an academic-practice partnership to improve maternal and child health outcomes in North Carolina. N C Med J. (2020) 81:5–13. doi: 10.18043/ncm.81.1.5
15. CEPH. Criteria & Procedures: Council on Education for Public Health. Available online at: https://ceph.org/about/org-info/criteria-procedures-documents/criteria-procedures/ (accessed May 5, 2023).
16. Academic Health Department — Academic Public Health Corps | Mass.gov. Available online at: https://www.mass.gov/info-details/academic-health-department-academic-public-health-corps (accessed April 16, 2023).
17. Boston 677 Huntington Avenue Ma 02115 +1495-1000. MA COVID-19 Academic Public Health Volunteer Corpsc. Field Education and Practice. (2020). Available online at: https://www.hsph.harvard.edu/public-health-practice-resources/covid-19-student-involvement-opportunities/covid-19-massashusetts-public-health-department-student-volunteers/ (accessed April 16, 2023).
18. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4:50. doi: 10.1186/1748-5908-4-50
19. Yasmin S, Haque R, Kadambaya K, Maliha M, Sheikh M. Exploring how public health partnerships with community-based organizations (CBOs) can be leveraged for health promotion and community health. Inq J Health Care Organ Provis Financ. (2022) 59:004695802211393. doi: 10.1177/00469580221139372
20. Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated consolidated framework for implementation research based on user feedback. Implement Sci. (2022) 17:75. doi: 10.1186/s13012-022-01245-0
21. Brehaut JC, Eva KW. Building theories of knowledge translation interventions: use the entire menu of constructs. Implement Sci. (2012) 7:114. doi: 10.1186/1748-5908-7-114
22. Alford A, Dekker D, Feeser K, Hall K, Newton S, Leider JP, et al. 2019 National Profile of Local Health Departments. National Association of County and City Health Official. Available online at: https://www.naccho.org/uploads/downloadable-resources/Programs/Public-Health-Infrastructure/NACCHO_2019_Profile_final.pdf (accessed August 27, 2023).
23. Keith RE, Crosson JC, O'Malley AS, Cromp D, Taylor EF. Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation. Implement Sci. (2017) 12:15. doi: 10.1186/s13012-017-0550-7
24. de Beaumont Foundation Association Association of State and Territorial Health Officials. Public Health Workforce Interests and Needs Survey: 2021 Dashboard. (2022). Available online at: https://debeaumont.org/wp-content/uploads/2022/11/1_States_2021_PH-WINS_Summary_Report.pdf (accessed September 14, 2023).
25. Locke R, McGinty M, Guerrero Ramirez G, Sellers K. attracting new talent to the governmental public health workforce: strategies for improved recruitment of public health graduates. J Public Health Manag Pract. (2022) 28:E235–43. doi: 10.1097/PHH.0000000000001336
26. Who Will Keep the Public Healthy?: Educating Public Health Professionals for the 21st Century. Washington, DC: National Academies Press (2003). Available online at: http://www.nap.edu/catalog/10542 (accessed May 6, 2023).
27. Administration (HRSA) HR and S. HHS.gov. With New American Rescue Plan Funding, HHS Expands and Strengthens the Community and Public Health Workforce. (2022). Available online at: https://www.hhs.gov/about/news/2022/09/30/new-american-rescue-plan-funding-hhs-expands-and-strengthens-community-and-public-health-workforce.html (accessed May 6, 2023).
28. Leider JP, McCullough JM, Singh SR, Sieger A, Robins M, Fisher JS, et al. Staffing Up and Sustaining the Public Health Workforce. J Public Health Manag Pract. (2023) 29:E100–7. doi: 10.1097/PHH.0000000000001614
29. Swain GR, Bennett N, Etkind P, Ransom J. Local health department and academic partnerships: education beyond the ivy walls. J Public Health Manag Pract. (2006) 12:33. doi: 10.1097/00124784-200601000-00008
30. Leser KA, Hay MC, Henebry B, Virden J, Patel M, Luttrell-Freeman J, et al. An academic–health department community partnership to expand disease investigation and contact tracing capacity and efficiency during the COVID-19 pandemic. J Public Health Manag Pract. (2022) 28:E16–22. doi: 10.1097/PHH.0000000000001379
31. Kegler MC, Lifflander A, Buehler J, Collins D, Wells J, Davidson H, et al. Multiple perspectives on collaboration between schools of public health and public health agencies. Public Health Rep. (2006) 121:634–9. doi: 10.1177/003335490612100522
32. Neri EM, Ballman MR, Lu H, Greenlund KJ, Grunbaum JA. Academic-health department collaborative relationships are reciprocal and strengthen public health practice: results from a study of academic research centers. J Public Health Manag Pract. (2014) 20:342–8. doi: 10.1097/PHH.0b013e3182a152c6
33. Erwin PC, Harris J, Wong R, Plepys CM, Brownson RC. The academic health department: academic–practice partnerships among accredited U.S. Schools and Programs of Public Health, 2015. Public Health Rep. (2016) 131:630–6. doi: 10.1177/0033354916662223
34. Public Health Infrastructure - Healthy People 2030 | health.gov. Available online at: https://health.gov/healthypeople/objectives-and-data/browse-objectives/public-health-infrastructure (accessed May 7, 2023).
Keywords: COVID-19, local public health, academic-practice partnerships, Consolidated Framework for Implementation Research (CFIR), mixed-methods program evaluation
Citation: Fielman S, Elliott PA, Codner A, Abousleiman H, Cogan A, Wangstrom Z and Greece JA (2024) Building capacity for local public health: lessons from a mixed-methods evaluation of an academic-public health partnership used in response to COVID-19. Front. Public Health 12:1387371. doi: 10.3389/fpubh.2024.1387371
Received: 17 February 2024; Accepted: 17 July 2024;
Published: 31 July 2024.
Edited by:
Christiane Stock, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, GermanyReviewed by:
John Pascoe, Wright State University, United StatesSairam Parthasarathy, University of Arizona, United States
Copyright © 2024 Fielman, Elliott, Codner, Abousleiman, Cogan, Wangstrom and Greece. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jacey A. Greece, amFibG9vbUBidS5lZHU=
 Sarah Fielman
Sarah Fielman Ally Cogan
Ally Cogan Jacey A. Greece
Jacey A. Greece