- 1School of Population and Health, Renmin University of China, Beijing, China
- 2Yichun Hospital of Traditional Chinese Medicine, Yichun, Jiangxi, China
Objective: The purpose of this study is to summarize the health system response to COVID-19 in four East Asian countries, analyze the effectiveness of their health system response, and provide lessons for other countries to control the epidemic and optimize their health system response.
Methods: This study investigated and summarized COVID-19 data and health system response in four East Asian countries, China, Japan, Mongolia, and South Korea from national governments and ministries of health, WHO country offices, and official websites of international organizations, to assess the effectiveness of health system measures.
Result: As of June 30, 2022, all four countries are in a declining portion of COVID-19. China has two waves, and new cases increased slowly, with the total cases per million remaining within 4, indicating a low level. Japan has experienced six waves, with case growth at an all-time high, total cases per million of 250.994. Mongolia started the epidemic later, but also experienced four waves, with total cases per million of 632.658, the highest of the four countries. South Korea has seen an increasing number of new cases per wave, with a total case per million of 473.759.
Conclusion: In containment strategies adopted by China and Mongolia, and mitigation strategies adopted by Japan and South Korea, health systems have played important roles in COVID-19 prevention and control. While promoting vaccination, countries should pay attention to non-pharmaceutical health system measures, as evidenced by: focusing on public information campaigns to lead public minds; strengthening detection capabilities for early detection and identification; using technical ways to participate in contact tracing, and promoting precise judging isolation.
1 Introduction
COVID-19 pandemic declared by the World Health Organization (WHO) in March 2020 has had far-reaching effects on people’s lives, health systems and wider society (1). As of June 30, 2022, the global cumulative number of confirmed cases exceeded 546.1 million for 546,100,990 cases and 6,333,828 deaths. Based on the United Nations Population Fund statistics of the global population, there are approximately 7,953.95 million people in 2022. With a mortality rate of over 1%, the average global diagnosis rate is 1 in 15 persons (2). Of these, a total of 258,324,223 cases have been diagnosed so far in 2022 alone, accounting for 47% of the cumulative new cases and 57% of the cumulative deaths in 2021 alone. On November 24, 2021, South Africa reported to the WHO the discovery of the omicron variant, in which infection speed and immune escape are very high (3, 4). Affected by the omicron variant, the global fourth wave began in 2022, and a new wave of COVID-19 began in various countries.
Since the first reported COVID-19 cases, countries have responded differently at different times and with different health system responses. China, Japan, Mongolia, and South Korea among East Asian countries were selected for this paper, and North Korea was not included in this study because the first COVID-19 case was reported on May 12, 2022. China is an upper-middle-income country, and effort to expand disease coverage in coming years adopted containment strategies with a strict blockade and proactive case management, makes full use of the unique advantages of traditional Chinese medicine. Japan and South Korea are high-income countries, generally have the highest spending on health care and the average percentage spending on health care is 5.5% of total GDP spent, adopted mitigation strategies to flatten the epidemic curve, targeting vulnerable populations and managing the seriously ill (5, 6). Japan is primarily managed by private organizations under universal health coverage (7). South Korea started “Living with the COVID-19” mode on November 1, 2021, and aims to implement universal health coverage; however, cost sharing is generally quite high, resulting in people still relying largely on private insurance. Mongolia, a lower-middle-income country, is on track to achieve universal health coverage by strengthening primary health care, and adopting containment strategies but had some problems with open borders and mitigating preventive and control measures.
Currently, 67.7% of the world population has received at least one dose of COVID-19 vaccines. 60.67% of the global population is fully vaccinated and 5.50% is incompletely vaccinated. China reached 90.75%, Japan reached 83.27%, Mongolia reached 67.90% (as of May 18, 2022) and South Korea reached 86.97% vaccination (8). Based on previous estimates of COVID-19 thresholds ranging from about 60–70%, current vaccination in many countries has exceeded this predicted herd immunity threshold, without taking into account previously confirmed cases (5, 9). Also, as with other seasonal coronaviruses, COVID-19 is capable of reinjecting people who already have the disease, but the frequency of reinfection is not known (10–12).
In this context, while promoting vaccination, we must pay attention to non-pharmacological interventions. The health system, as the main force in COVID-19 prevention and control, the health system undertakes the detection, identification, and treatment of cases; the health system undertakes the epidemiological investigation and management of cases, and so on (13, 14). Second, the ongoing management of the health system response to COVID-19 is not only about disease management but more importantly, about managing people. If not managed well, there will be significant psychological and social impacts that will have long-term effects on individuals and society (15). In addition, health system response is closely related to a country’s COVID-19 mortality rate. Given that COVID-19 is still in a global pandemic situation and poses a risk to people’s life safety and health, and also impacts the world economy. So, research on the health system’s response to COVID-19 is necessary. The purpose of this study is to summarize the health system response to COVID-19 in four East Asian countries, analyze the effectiveness of their health system response, and provide lessons for other countries to control the epidemic and optimize their health system response.
2 Methods
2.1 Statistic of COVID-19 data
This paper investigated new cases per million and total deaths per million in China, Japan, Mongolia, and South Korea from the first reported cases to June 30, 2022. Data on COVID-19 cases are from Coronavirus Resource Centre at Johns Hopkins University1 and WHO Coronavirus Dashboard.2 The inclusion criteria for confirmed cases of COVID-19 in China is based on the Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment published by the Chinese Health Commission. Classification of clinical manifestation was added in Hubei Province in February 2020, and it included suspected cases with imaging features of pneumonia to clinical diagnosis cases.
2.2 Health system measures in COVID-19
Health system measures were searched from the first reported cases around the world to June 30, 2022. The paper focused on COVID-19 measures used by national health system, thus we searched for health system measures in response to COVID-19 from national governments and ministries of health. Such as China’s Health Committee,3 Japan’s Ministry of Health, Labor and Welfare,4 Mongolia’s Ministry of Health,5 and South Korea’s Ministry of health and welfare.6 COVID-19 as a national public health emergency, some measures were directly issued by government departments, so the paper included national official websites in the search, such as China,7 Japan (see Footnote 4), Mongolia (see Footnote 5), and South Korea.8 The search used the following keywords: COVID-19, policy, response and strategy, and followed the inclusion–exclusion criteria: (1) The health system needs to play a role in measures, (2) Measure has a national scope, (3) Exclude duplication measures. After collecting data and health system measures, we mapped the national epidemic curve over time, sorted out through measures, and listed public information campaigns, testing policy, contact tracing, vaccination, isolation and quarantine policy.
3 Results
3.1 National measures to prevent and control COVID-19
China, Japan, Mongolia, and South Korea are the four East Asian countries that suffered from COVID-19 earlier and are the representative countries’ responses to COVID-19. Public health measures have played major roles in all COVID-19 stages. China has taken many measures in public health measures to achieve precise prevention and control and universal coverage. On January 1, 2020, a case of pneumonia of unknown cause was reported, and the epidemic information was released daily on the official website. China maintains a good public information campaign while keeping information open. The testing policy has been supported by people from all sectors of society. The testing cost continues to decrease, and the testing facilitation has been gradually promoted, with multiple rounds of testing conducted in cluster epidemics. China is using information technology and big data to contact tracing and isolate close contacts and is accelerating vaccination. In addition, China has issued multiple editions of COVID-19 Diagnosis and Treatment Plan, detailing treatment plans at various stages, not only adopting modern medicine and public health measures, but also traditional Chinese medicine theories and traditional Chinese medicine are widely used to deal with COVID-19.
Japan issued a level 1 risk warning on time, released a short video on COVID-19 prevention, and appealed to the public with “self-restraint.” Unlike in other countries, the decision to test in Japan is mainly made by physicians. Initially, testing was only available for symptomatic individuals, but later it became available for asymptomatic individuals when doctors deemed it necessary, and free Polymerase chain reaction (PCR) and antigen testing have become available for asymptomatic individuals. In contact tracing, Japan has adopted ‘cluster busting,’ which focuses on large tracking, clustered epidemics. On February 17, 2020, Japan officially vaccinated, with priority given to medical workers, the older adult, and those with pre-existing conditions. In addition, Japan advocates home isolation for mild, asymptomatic infections and hospitalization for severe cases.
Mongolia launched a one-month outbreak prevention and control operation in April 2020 and the highest level of national disaster preparedness on high alert in November. Citizens were called to pay attention to COVID-19 through official websites and the distribution of pamphlets. To facilitate testing for the public, testing centers are being established in all cities and specialized hospitals to provide drop-off-free testing services, and One Citizen-One Household is being launched. In March 2022, the traveler testing requirement was eliminated. Contact tracing in Mongolia is done with the help of scanning QR codes in public places, isolation of close contacts, and medical observation of sub-close contacts. On March 23, 2021, Mongolia officially launched vaccination with the same order of priority as Japan and suspended vaccination during the blockade. In response to COVID-19, Mongolia has lockdown several times. At various times, Mongolia requires quarantine for people entering the country from different regions. On March 14, 2022, Mongolia officially lifted its entry quarantine restrictions.
On January 27, 2020, South Korea raised the public alert level to orange and passed COVID-19 Three Act in February. On January 20, 2020,South Korea managed to get testing centers up and running, initially making testing available to suspected cases and patients under investigation, and then gradually liberalizing and simplifying the procedure for COVID-19 testing in March 2022 by recognizing rapid antigen-positive results. In February 2020, close contact tracing software was used to trace people within 100 meters of COVID-19 cases. In February 2021, South Korea officially started universal vaccination. A quarantine policy was adopted for confirmed patients, and inbound travelers were quarantined. After May 2021, travelers who have completed COVID-19 vaccination in South Korea were exempted from quarantine. Table 1 summarizes Core health system measures response to COVID-19 in China, Japan, Mongolia, and South Korea, including public information campaigns, testing policy, contact tracing, vaccination, isolation and quarantine policy.
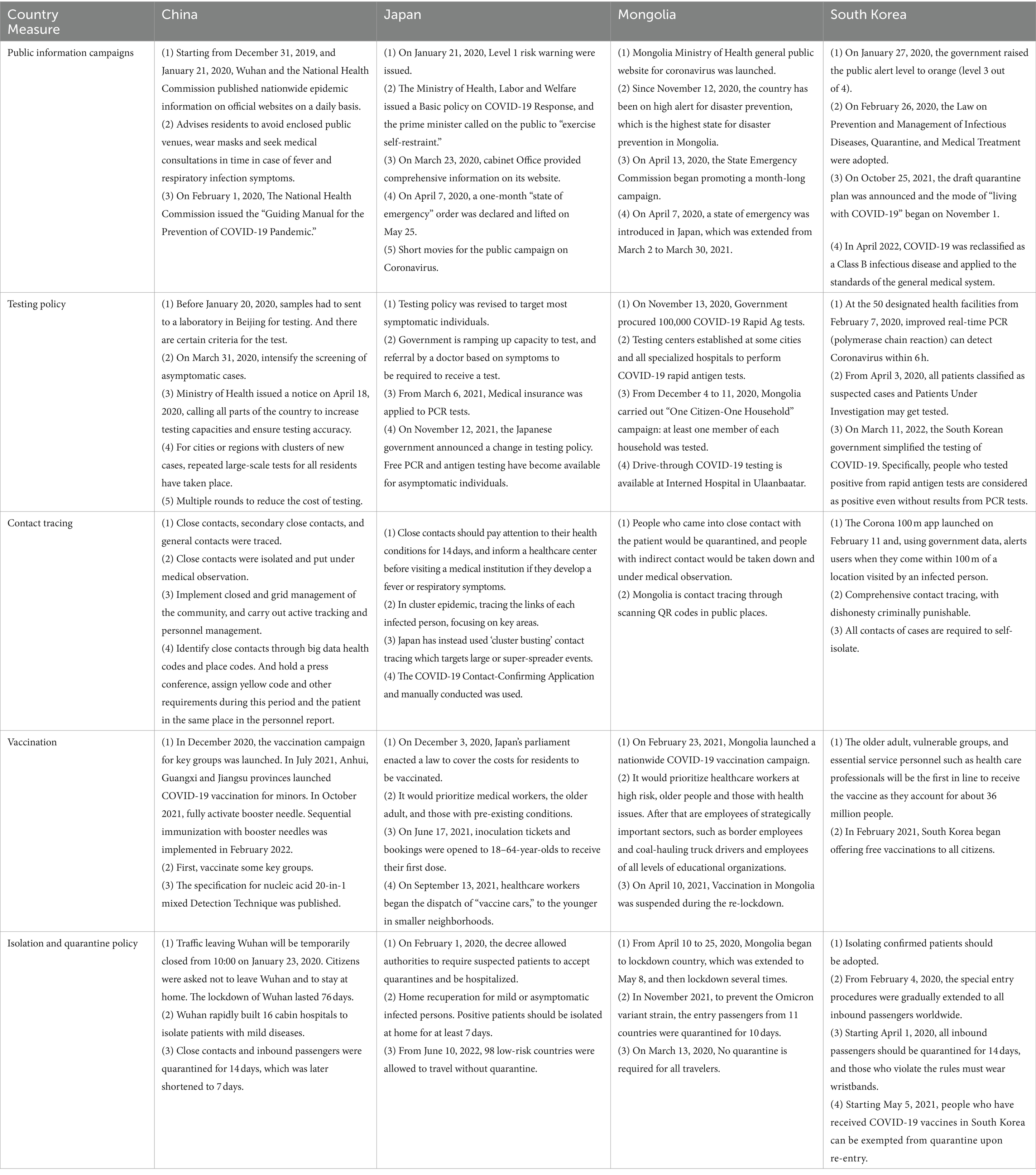
Table 1. Core health system measures response to COVID-19 in China, Japan, Mongolia, and South Korea.
3.2 COVID-19 trends
As shown in Figure 1, COVID-19 epidemic in China is divided into 3 periods: the outbreak period, normalized prevention and control period, and the second wave, which was cut off on May 8, 2020, and March 2022. After the first COVID-19 case was reported, China came into the outbreak period, and COVID-19 cases were increasing severely. On February 13, 2020, new cases per million reached 10.613, and then the growth of new cases gradually decreased. After the first death was reported on January 11 and reached a high point after the recount of cases on April 30. During the normalized prevention and control period, there was no nationwide epidemic, but cluster epidemics occurred sometimes. As we entered March 2022, the impact of the fourth global COVID-19 wave, coupled with the omicron characteristics, led to a marked increase in the frequency and scope of the epidemic, with new cases even surpassing the first wave. New cases per million peaked on April 14, 2022, showing a clear crest, while deaths. There is also an increase in the number of deaths.
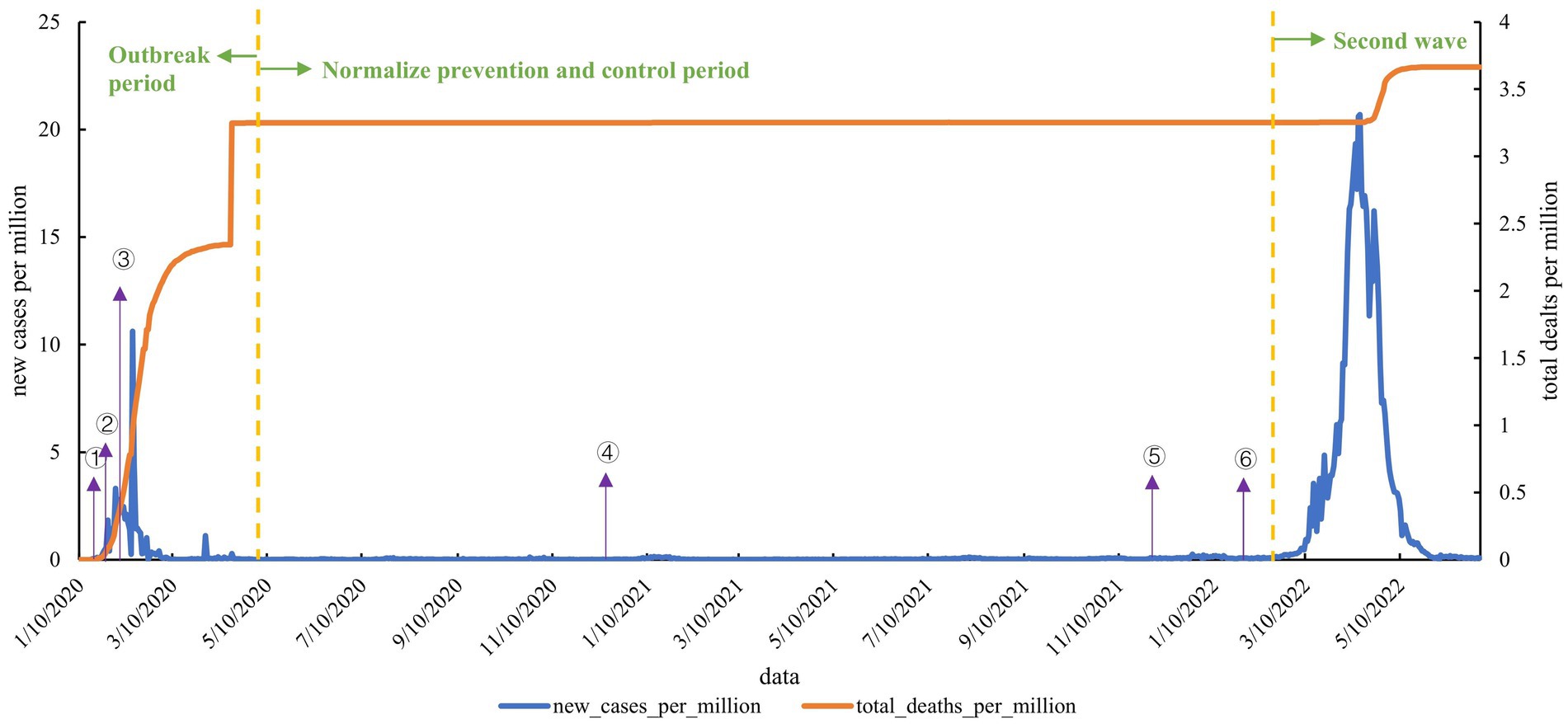
Figure 1. Epidemic curve of local cases of COVID-19 in China. (1) On January 21, 2020, the National Health Commission began issuing national outbreak information. (2) On January 23, 2020, lockdown Wuhan city. (3) On February 1, 2020, The National Health Commission issued the “Guiding Manual for the Prevention of COVID-19 Pandemic.” (4) In December 2020, vaccination of key populations began. (5) On December 7, 2021, the general strategy of “external prevention of importation and internal prevention of rebound” and the general policy of “dynamic clearance” were established. (6) In February 2022, booster vaccination was introduced. In February 2022, the booster vaccine was introduced.
As shown in Figure 2, the first COVID-19 case in Japan was reported on January 15, 2020. In February, there was a cluster epidemic on the Diamond Princess cruise ship. The first wave of COVID-19 began in March 2020, when Japan entered a state of emergency after a record-high number of new daily cases due to improved detection capabilities and many imported cases. In the first wave, the mortality rate was much higher than in the other waves, which remained largely above 0.1, and on May 11, the mortality rate exceeded 0.5. After a normalized period, the second wave broke out in June 2020. Entering late October 2020, with lower temperatures, Japan entered the third wave, which peaked on January 15, 2021, with new cases per million reaching 57.562 and total cases per million reaching 35.47. The fourth wave was quite similar to the third wave in terms of cycle and peak. Entering July 2021, the fifth wave dominated by the Delta followed, and in mid-August, the epidemic worsened, with more than 25,000 daily new cases. After entering October, new cases declined rapidly. Entering 2022 as in the other three countries, infections soared due to the omicron, and the speed and scale of infection far surpassed the previous five waves. As of June 30, 2022, the total cases per million in Japan reached 250.994.
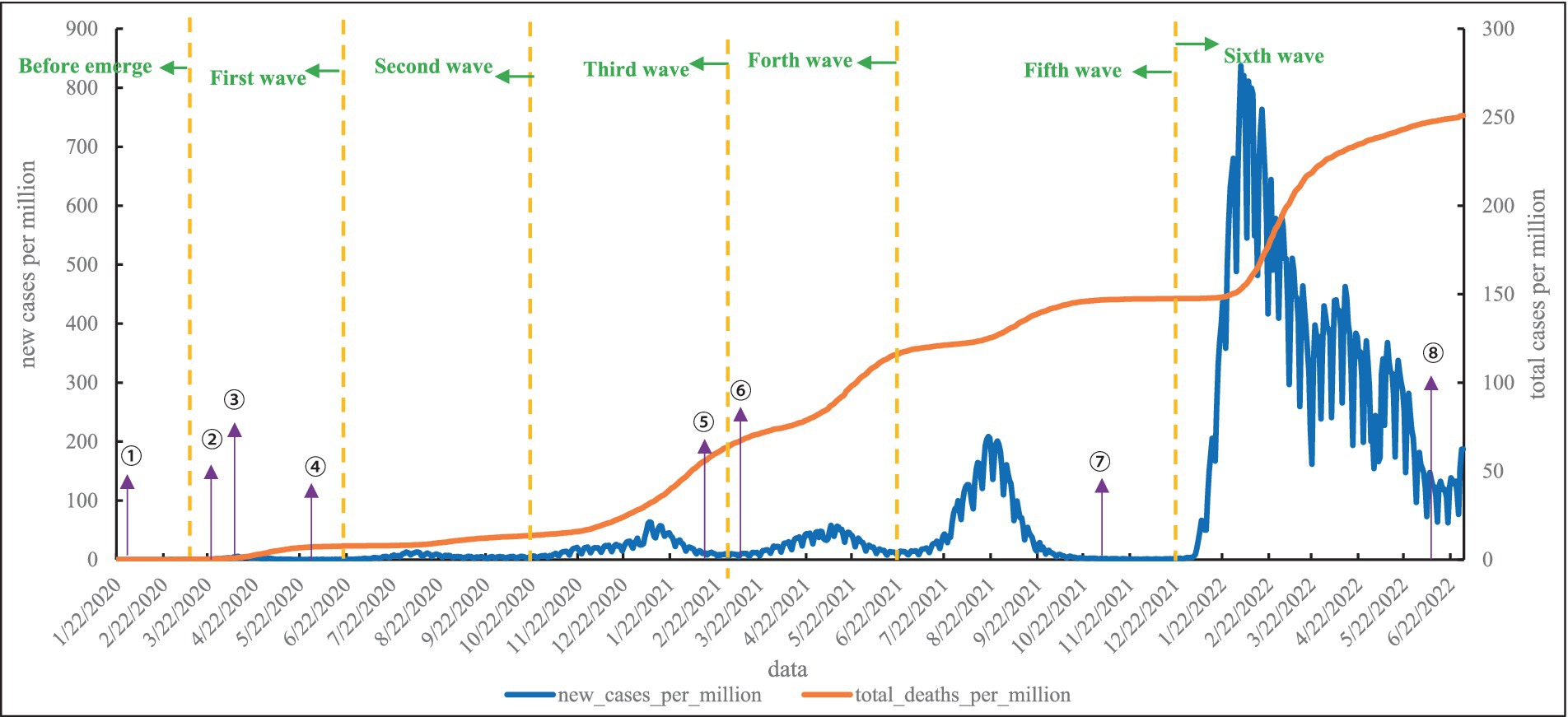
Figure 2. Epidemic curve of local cases of COVID-19 in Japan. (1) On February 1, 2020, the decree allowed authorities to require suspected patients to accept quarantines and be hospitalized. (2) On March 23, 2020, Binet Office provided comprehensive information on its website. (3) From April 7, 2020, a state of emergency was introduced in Japan. (4) On May 25, 2020, the state of emergency was lifted nationwide. (5) On February 17, 2021, Japan began vaccinating medical personnel with the COVID-19 vaccine. (6) From March 6, 2021, Medical insurance was applied to PCR tests. (7) On November 12, 2021, the government announced a change in testing policy, free PCR and antigen testing have become available for asymptomatic individuals. (8) On June 10, 2022, travel was opened to 98 countries with low risk, exempt from quarantine.
As shown in Figure 3, the first COVID-19 case was registered by French nationals on 10 March 2020, and subsequently, new cases spread rapidly after the first diagnosis (16). In addition, there were several peak points in the emerging stage. The first death case in Mongolia appeared on December 18, 2020, which was also the second wave. In the second wave, Mongolia was in an epidemic crisis, with new cases constantly showing a backlash tense, with constant ups and downs, and an increase in deaths. Compared to the second wave, the third wave came with a vengeance, and this was the wave with the most rapid increase in deaths. The third wave hits and the Delta spreads, on October 31, 2021, reaching a peak of 7335.006 new cases per million. With the accelerated global spread of omicron and a significant increase in the number of people entering and leaving Mongolia, the fourth wave was opened. Mongolia’s total cases per million are the highest of the four countries. As of June 30, 2022, Mongolia’s total cases per million reached 632.658.
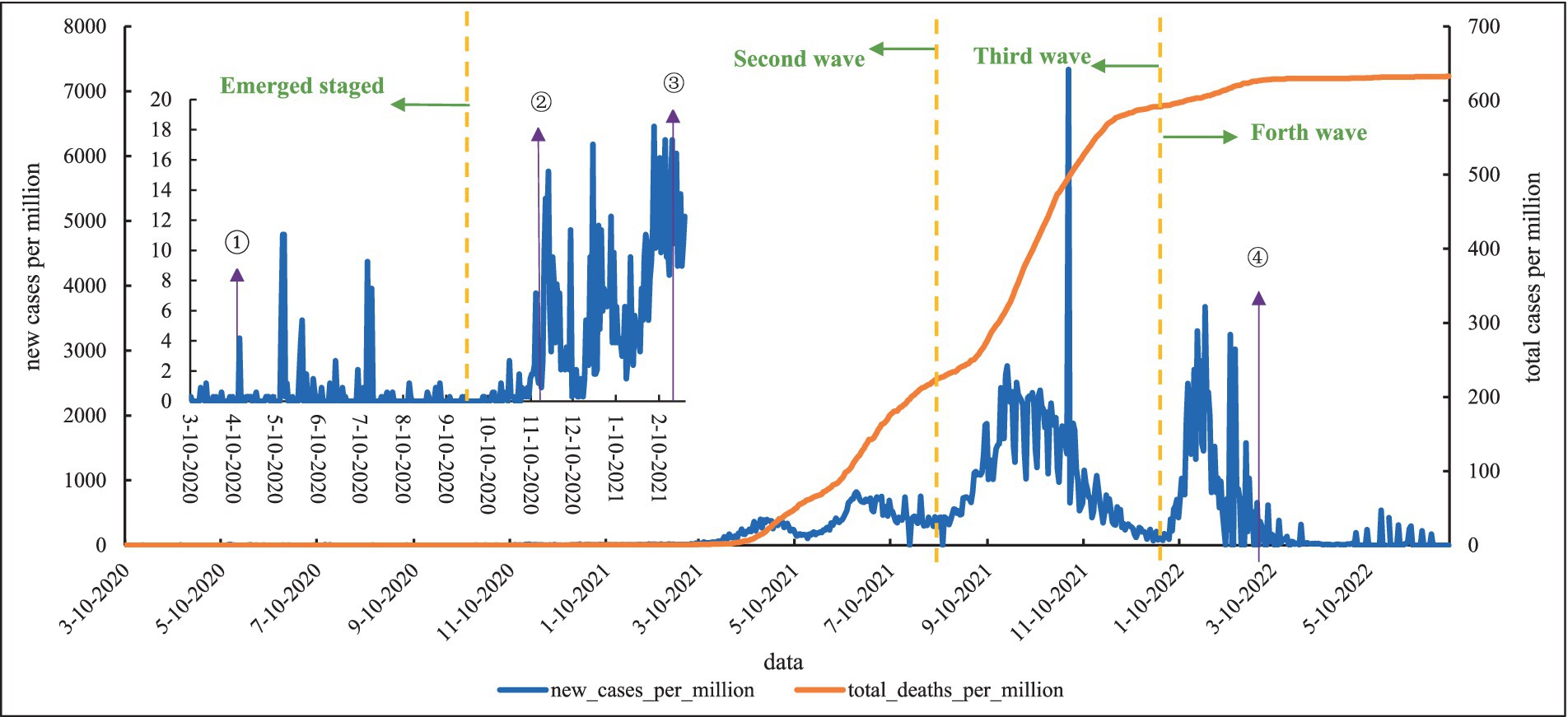
Figure 3. Epidemic curve of local cases of COVID-19 in Mongolia. (1) From April 10 to 25, 2020, Mongolia began to lockdown country, which was extended to May 8, and then lockdown several times. (2) From November 12, 2020, a state of high alert for national disaster preparedness was in effect. (3) From December 4 to 11, 2020, Mongolia carried out “One Citizen-One Household” campaign. (4) On February 23, 2021, Mongolia launched a nationwide COVID-19 vaccination campaign. (5) On March 14, 2022, all travelers do not need pre-travel tests max 72 h before departure.
As shown in Figure 4, there are five distinct peaks of COVID-19 in South Korea. The first COVID-19 case was reported on January 20, 2020, and the number of confirmed cases began to increase in February and reached the peak on February 29, which was associated with a religious group. From April to early August, new cases per million remained around 1, but in August, the second wave began in the metropolitan area churches and continued to spread, with frequent clusters in non-metropolitan areas and a nationwide multipoint spread. The interval between the second and third waves was shortened, and new cases rose again to more than 300 in a single day after 81 days since August 29, showing signs of a “third pandemic.” The fourth wave followed, and the deaths increased even more rapidly. On December 17, 2021, new cases per million reached 141.096, and by the 25th, total deaths per million exceeded 100. By 2022, the fifth wave was growing rapidly, with daily new cases per day reaching the highest in the world. At the peak of the fifth wave, on March 16, new cases per million reached 11,987.562, and by June 30, 2022, South Korea’s total cases per million reached 473.759.
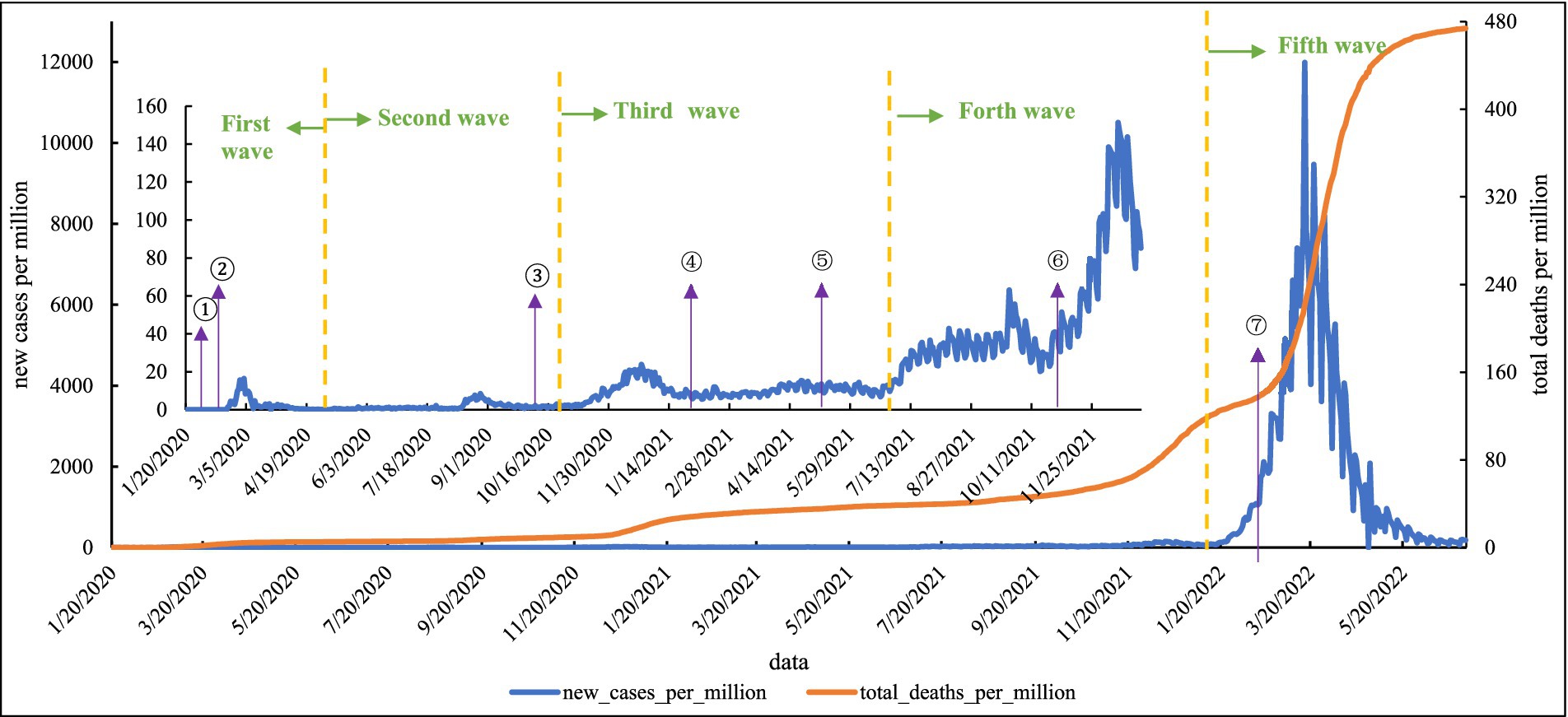
Figure 4. Epidemic curve of local cases of COVID-19 in South Korea. (1) On January 27, 2020, the government raised the public alert level to orange. (2) On February 26, 2020, the Amendment to the Infection Disease Prevention and Management Act, the Amendment to the Quarantine Act, and the Amendment to the Medical Treatment Act, the “COVID-19 Three Acts,” were passed in response to the COVID-19 outbreak. (3) From October 13, 2020, face masks are compulsory in public places. (4) On February 2021, South Korea began free vaccination. (5) From May 5, 2021, people who have received the COVID-19 vaccine within South Korea would be granted exemption from quarantine when re-entering from abroad. (6) On November 1, 2021, the South Korean government started the “Coexistence with Neosporin” model. (7) On March 11, 2022, the South Korean government simplified the testing of COVID-19.
4 Discussion
This study describes health systems measures used by the four East Asian countries – China, Japan, Mongolia, and South Korea – to respond to COVID-19 and their effectiveness in controlling new cases and deaths. China and Mongolia adopted containment strategies, adhered to a lockdown policy, adopted restrictions on social distance, strict public health measures, and proactive case detection and management. South Korea and Japan adopted mitigation strategies, recommending home isolation for mild cases in an attempt to flatten the policy curve and ease pressure on their healthcare systems (5).
Health system measures in response to COVID-19 include the following two main categories: first, policies to strengthen the health system capacity, such as new square cabin hospitals and coordination of medical resources; and second, policies to reduce people contracting the virus, such as wearing masks and isolating close contacts (17). This paper discusses the experiences and shortcomings of the response to COVID-19 in terms of five health system measures: public information campaigns, testing policy, contact tracing, vaccination, and isolation and quarantine policy.
4.1 Public information campaigns
Public information campaigns are the beacon of COVID-19 epidemic prevention and control, and the leader of people’s ideological trends, which are important policy tools used worldwide (18). Public information campaigns aiming at shaping beliefs, attitudes, Social norms, and actual behaviors in (a segment of) the mass public, and play an important role in educating people about COVID-19, promoting the acceptance and compliance of policies and measures, and promoting the implementation of policies (19). Public information campaigns are also considered one of the cost-effective intervention measures, which include promulgating policies and decrees, announcing risk levels and the state of country, releasing COVID-19-related public information, etc. (20).
All four countries have been publishing national epidemic information on their official websites to maintain the authority and reliability of the information. China continues to revise its “Guiding Manual for the Prevention of COVID-19 Pandemic” to inform the public about COVID-19 in various. China ranked first in the public perception survey of 19 countries severely affected by COVID-19, with high trust in government and much higher than average satisfaction with COVID-19 policies (21). The Japanese population exhibited higher self-regulation and health literacy. The suppression of the first COVID-19 wave is thought to be attributed to the increased risk perception of people after receiving information from government and media reports (22). In public information campaigns, people are only called for self-restraint, without coercion, punishment, or compensation. The new cases also maintain a relatively stable level in the early stages of the epidemic (23). Mongolia initially provided infection updates through the Ministry of Health’s daily briefings and currently provides infection updates through an online portal. However, due to its inadequate emergency management capacity and vulnerable health care resources, public confidence in the government’s ability to respond to a pandemic is lacking. Mongolia has repeatedly entered a state of emergency in an attempt to slow the outbreak through a blockade (24). South Korea’s public information campaigns guide the direction of its epidemic prevention, from the adoption of COVID-19 III law in 2020, with a strict contact tracing pathway, to the start of a coexistence model with COVID-19 in November 2021. Some studies show insufficient evidence for public information campaigns to prevent and control COVID-19 (25). The reason for this is that public information campaigns are a subtle process that is integrated into the compliance of other policies and public awareness. In COVID-19, public information campaigns were a link between the country’s mind and the population, and to strengthen confidence in the fight against the epidemic. In addition, public information campaigns also assumed the role of COVID-19 vaccination promotion.
4.2 Testing policy
Testing policy is the key policy of COVID-19, the basis of contact tracing and isolation policy, the key link to breaking the chain of COVID-19 transmission, and an important source of data to evaluate a country’s COVID-19 prevention and control policy (26). The testing policy depends on a country’s medical and human resources, as well as testing capacity. In COVID-19, testing patterns, testing prices, and so on are reflected.
China continues to improve testing capacity and reduce testing prices. And use the advantages of traditional Chinese medicine to reduce the symptoms of patients, shorten the course of disease and reduce the conversion rate of severe diseases to save medical resources. In cluster epidemics, multiple rounds of mass testing are started locally, using grouped testing to conserve testing resources. Test results are presented together in trip codes. Japan initially allowed only symptomatic individuals to take tests, but later shifted to testing based on physician judgment. After Japan continued to improve its testing capabilities, the testing strategy was changed so that asymptomatic infected individuals could be tested for free (27). During the lockdown period, the Mongolian government initiated a mass testing campaign, the so-called “One door-one test,” which at least one member of each household was tested (28). South Korea established a car-free testing site to facilitate testing for citizens. Post-approval of antigen testing as a positive indicator.
In the face of COVID-19 and the shortage of healthcare resources, four countries have taken measures to conserve medical resources. However, there are also some problems, large-scale testing tends to produce people gathering with the risk of cross-infection, which requires strengthening the popular testing science and personnel management, maintaining social distancing, and standardized sterilization training for medical staff to reduce the risk of cross-infection. Omicron is hidden and difficult to detect, requiring multiple rounds of testing (29, 30). This poses a new dilemma for both the sustainability of health systems and health resource allocation. Countries should strengthen their testing capacity, rationalize the allocation of health resources, and enhance the early detection and identification of symptomatic populations in the early stages.
4.3 Contact tracing
Both contact tracing and testing policies are well-known public health intervention tools that have the least impact on the lives of non-potentially infected individuals (25) and combined with operational data can develop an early warning system for COVID-19 hotspots, predicting the location of potential outbreaks (31). Contact tracing is a key step in the epidemiological investigation and one of the most important measures in containment strategies. Its purpose is to cut off the transmission route of the new crown transmission and reverse the basic aspects of finding the source of infection and containment transmission.
Chinese Center for Disease Control and Prevention at all levels is the main focus of contact tracing in China. China insists on early detection and early reporting in contact tracing. After confirming the trajectories of confirmed patients and close contacts’ movements, they are communicated to the whole society. To speed up the tracking and save health resources, the form of place code combined with health code is adopted to facilitate the identification of temporal and spatial closeness. Japan focuses on large events, and cluster epidemics, and relies on a large network of local health officials. They consider confined spaces, crowded places, and close contact environments as the main risk factors that may lead to the occurrence of clustered cases, and focus on identifying clustered cases and eliminating widespread transmission, rather than trying to track each case. In Mongolia, close contacts are identified through video, interview, and interrogation, and scanning QR codes in public places are also used (16). However health workers are overburdened, there is burnout with contact tracing, and public distrust of the health care system (24). South Korea uses technology to send alerts to people within 100 meters of the area involved in epidemics and advises them to take testing. The South Korean government publishes the whereabouts of confirmed cases on its official website to make it easier for residents to inquire about close contacts.
Contact tracing is labor-intensive and a resource-intensive, multi-step process, making current contact tracing suboptimal (32, 33). The incubation period and asymptomatic infections pose a challenge for contact tracing. In the face of human resource shortages, four countries have adopted some electronic information technology tools to assist in contact tracing, but the study realizes that their overall utilization is not high (34). There are many other issues to be noted, First, the difficulty of omicron detection, the need to extend the length of storage of electronic information systems to ensure access to contact information; Second, the protection of public privacy, contact tracing involves a large number of public personal information, strict prevention of data leakage and serious violations of digital privacy events; Third, the smartphone penetration rate of the older adult groups is not high, the existing electronic information technology tools for the protection of the older adult groups is low (34, 35). In addition, Japan’s focus on identifying clustered cases in contact tracing is worthy of being handled by Western countries in cluster epidemics. Moreover, countries need to pay attention to the demands of medical personnel, protect the rights and interests of frontline medical workers, and motivate them to participate in epidemic prevention efforts.
4.4 Vaccination
Vaccines are considered a key response to COVID-19 and the most effective tool to combat the spread of COVID-19, and several studies have shown that vaccines can prevent severe illness and death (36). Herd or community immunity occurs when most of the population in a community is naturally or artificially immune (37). Vaccination is the most effective strategy to ensure a robust and durable immune response to SARS-CoV-2 virus and its variants. Global vaccination has been accelerated since COVID-19 vaccination started in 2021.
Four countries have vaccination rates above the world average. China began a mass vaccination campaign in January 2021 and gradually expanded to people over 60 years of age and children. Japan lags far behind other developed countries in vaccination, due to the lack of domestically produced vaccines and its reliance on imports, and the strict approval process for Japanese vaccines. Mongolia has strengthened international cooperation and extensive vaccination campaigns with the World Bank, UNICEF, etc., and has achieved high vaccination rates among less developed countries (24). At the request of South Korean government, many private clinics have conducted COVID-19 testing and vaccinations to make vaccinations easily available. High vaccination rates in South Korea also played an important role in the third or fourth wave (38).
Despite favorable results and promising outcomes, vaccine efficacy or effectiveness decreases over time and the duration of immunity may be short-lived (39, 40). Increased transmissibility and infectivity, severity of associated diseases, and virus mutations can all affect vaccine effectiveness (41). Omicron reinfection rates were much higher in fully vaccinated or previously infected individuals than in earlier variant strains, and all COVID-19 vaccines were significantly less effective against omicron variants (36, 42). The emergence of breakthrough infections and mutant strains will be a great challenge for the COVID-19 vaccine against COVID-19 (43, 44). While stepping up vaccination efforts, we should recognize that vaccines alone will not get any country out of this crisis and that a broad range of protective interventions is needed for the evolving pandemic (45).
4.5 Isolation and quarantine policy
Before vaccination, Isolation policy, social distancing, blockade, isolation of confirmed cases, and isolation of their contacts are considered important measures to prevent and control COVID-19 (46). Studies showed that isolating confirmed or suspected cases prevented 44 to 81% of cases and 31 to 63% of deaths (47). Due to differences in healthcare capacity, countries have adopted different admission strategies. Countries with containment and mitigation strategies show very significant differences in the use of isolation policies.
China adhered to the strategy of all those who indeed are isolated. It imposed a 76-day-long closure of Wuhan and built a square cabin hospital as a temporary hospital to centralize the treatment of mildly ill patients. Localities also followed isolation requirements by building isolation hotels and adopting 14-day centralized isolation, which was later shortened to 7 days. Japan promotes the allocation of medical resources by adopting self-isolation at home for mildly ill patients and medical institutions only accepting seriously ill patients. Mongolia has taken several initiatives to lockdown countries and cities for isolation, accompanied by active infection surveillance and self-isolation recommendations. South Korea designed and implemented community treatment centers to ensure the safety of non-COVID-19 patients by segregating areas for respiratory and non-respiratory patients.
Isolation and quarantine policy is aimed at incoming persons and close contacts and is an important part of the control of incoming persons and a gateway to avoid the virus inboard. The implementation of mass isolation or systematic social isolation allows individuals to directly eliminate the possibility of infection due to low physical contact (48). Japan, Mongolia, and South Korea have relaxed or lifted the quarantine of incoming persons, which poses a great challenge to prevent and control COVID-19. In addition, some studies have concluded that Isolation and quarantine policy measures harm the mental health and economic and social development of the population, especially on vulnerable groups and those with poor housing conditions (49, 50). In this case, the family quarantine model helps to ease tensions and for countries to be more precise in judging quarantine and blockade events to ensure normal working life order while safeguarding the prevention and control COVID-19.
In addition, when dealing with pandemics, countries should give full play to their own characteristics and advantages, such as China’s advantages in using traditional Chinese medicine to alleviate symptoms, prevent disease deterioration and enhance people’s immunity, to save strained medical resources. Japan takes advantage of its people’s high health literacy; And Vietnam are participating in COVID-19 prevention and control through grassroots cross-sectoral organizations.
A limitation of our study is that new cases per million are used in this study to describe the epidemic trend, but different countries have different detection capabilities and reporting standards, resulting in a certain degree of error. And the data limitations make it difficult to retrieve COVID-19 data and core health system measures for North Korea. Another limitation is that health system measures. More attention is paid to the release of measures, and less consideration is given to the actual use of measures.
In future research, study looks at optimizing data collection and processing methods, as well as exploring in depth the practical application of health system measures, with a view to providing more effective policy recommendations and decision support for pandemic response. Firstly, adding control variables or correct data errors caused by differences in reporting standards; secondly, designing a system of indicators for evaluating the response of health system to epidemic and quantifying measures; in addition, collecting more detailed data through qualitative research methods, such as in-depth interviews or case studies.
5 Conclusion
In containment strategies adopted by China and Mongolia, and mitigation strategies adopted by Japan and South Korea, health systems have played an important role in COVID-19 prevention and control. While promoting vaccination, countries should pay attention to non-pharmaceutical health system measures, as evidenced by: focusing on public information campaigns to lead public minds; strengthening detection capabilities for early detection and identification; using technical means to participate in contact tracing, and promoting precise judging isolation.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
JJ: Writing – original draft. WC: Funding acquisition, Project administration, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by Jiangxi Provincial Training Program for Young and Middle-aged Backbone Talents in Traditional Chinese Medicine (NO. 360900228888020005282).
Acknowledgments
The authors gratefully acknowledge the study participants who have been involved and contributed to the manuscript. The authors gratefully acknowledge the financial supported by Jiangxi Provincial Training Program for Young and Middle-aged Backbone Talents in Traditional Chinese Medicine (NO. 360900228888020005282).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
WHO, the World Health Organization; PCR, Polymerase chain reaction.
Footnotes
1. ^https://coronavirus.jhu.edu/?from=groupmessage
2. ^https://covid19.who.int/table
4. ^https://www.mhlw.go.jp/index.html
6. ^https://www.mohw.go.kr/eng/index.jsp
References
1. Cucinotta, D, and Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
2. Population Data Portal . Available at: https://pdp.unfpa.org/?_ga=2.29710518.865667680.1662344878-1467124044.1662344878 (Accessed September 5, 2022).
3. Classification of omicron (B.1.1.529): SARS-CoV-2 variant of concern. Available at: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern (Accessed April 13, 2022).
4. Meo, SA, Meo, AS, Al-Jassir, FF, and Klonoff, DC. Omicron SARS-CoV-2 new variant: global prevalence and biological and clinical characteristics. Eur Rev Med Pharmacol Sci. (2021) 25:8012–8. doi: 10.26355/eurrev_202112_27652
5. Kwok, KO, Lai, F, Wei, WI, Wong, SYS, and Tang, JWT. Herd immunity – estimating the level required to halt the COVID-19 epidemics in affected countries. J Infect. (2020) 80:e32–3. doi: 10.1016/j.jinf.2020.03.027
6. Tham, TY, Tran, TL, Prueksaritanond, S, Isidro, JS, Setia, S, and Welluppillai, V. Integrated health care systems in Asia: an urgent necessity. Clin Interv Aging. (2018) 13:2527–38. doi: 10.2147/CIA.S185048
7. Japan health policy NOW – 4.1 overview of Japan’s healthcare delivery system. Available at: http://japanhpn.org/en/section-4-1/ (Accessed May 1, 2024).
8. Ritchie, H, Mathieu, E, Rodés-Guirao, L, Appel, C, Giattino, C, Ortiz-Ospina, E, et al. Coronavirus pandemic (COVID-19). Our World in Data (2020). Available at: https://ourworldindata.org/covid-vaccinations (Accessed September 5, 2022).
9. Kadkhoda, K . Herd immunity to COVID-19. Am J Clin Pathol. (2021) 155:471–2. doi: 10.1093/ajcp/aqaa272
10. Long COVID: let patients help define long-lasting COVID symptoms. Nature. (2020) 586:170–11. doi: 10.1038/d41586-020-02796-2
11. Ledford, H . Coronavirus reinfections: three questions scientists are asking. Nature. (2020) 585:168–9. doi: 10.1038/d41586-020-02506-y
12. Parry, J . Covid-19: Hong Kong scientists report first confirmed case of reinfection. BMJ. (2020) 370:m3340. doi: 10.1136/bmj.m3340
13. Vadlamannati, KC, Cooray, A, and de Soysa, I. Health-system equity, egalitarian democracy and COVID-19 outcomes: an empirical analysis. Scand J Public Health. (2021) 49:104–13. doi: 10.1177/1403494820982106
14. Chang, AY, Cullen, MR, Harrington, RA, and Barry, M. The impact of novel coronavirus COVID-19 on non-communicable disease patients and health systems: a review. J Intern Med. (2021) 289:450–62. doi: 10.1111/joim.13184
15. Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
16. Bayasgalan, T, Anuurad, E, and Byambaa, E. COVID-19 and public health efforts in Mongolia: a lesson maybe learned? J Clin Transl Sci. (2021) 5:e18. doi: 10.1017/cts.2020.510
17. Alfano, V, and Ercolano, S. The efficacy of lockdown against COVID-19: a cross-country panel analysis. Appl Health Econ Health Policy. (2020) 18:509–17. doi: 10.1007/s40258-020-00596-3
18. Weiss, JA, and Tschirhart, M. Public information campaigns as policy instruments. J Policy Anal Manage. (1994) 13:82–119. doi: 10.2307/3325092
19. Solovei, A, and Van Den, PB. The effects of five public information campaigns: the role of interpersonal communication. Communications. (2020) 45:586–602. doi: 10.1515/commun-2020-2089
20. Podolsky, MI, Present, I, Neumann, PJ, and Kim, DD. A systematic review of economic evaluations of COVID-19 interventions: considerations of non-health impacts and distributional issues. Value Health. (2022) 25:1298–306. doi: 10.1016/j.jval.2022.02.003
21. Lazarus, JV, Ratzan, S, Palayew, A, Billari, FC, Binagwaho, A, Kimball, S, et al. COVID-SCORE: a global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10). PLoS One. (2020) 15:e0240011. doi: 10.1371/journal.pone.0240011
22. Takahashi, H, Terada, I, Higuchi, T, Takada, D, Shin, J-H, Kunisawa, S, et al. The relationship between new PCR positive cases and going out in public during the COVID-19 epidemic in Japan. PLoS One. (2022) 17:e0266342. doi: 10.1371/journal.pone.0266342
23. Konishi, T . Effect of control measures on the pattern of COVID-19 epidemics in Japan. PeerJ. (2021) 9:e12215. doi: 10.7717/peerj.12215
24. Dagvadorj, A, Jantsansengee, B, Balogun, OO, Baasankhuu, T, and Lkhagvaa, B. Health emergency preparedness and response to the COVID-19 pandemic: lessons learnt from Mongolia. Lancet Reg Health West Pac. (2022) 21:100436. doi: 10.1016/j.lanwpc.2022.100436
25. Liu, Y, Morgenstern, C, Kelly, J, Lowe, R, Munday, J, Villabona-Arenas, CJ, et al. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC Med. (2021) 19:40. doi: 10.1186/s12916-020-01872-8
26. Kuster, AC, and Overgaard, HJ. A novel comprehensive metric to assess effectiveness of COVID-19 testing: inter-country comparison and association with geography, government, and policy response. PLoS One. (2021) 16:e0248176. doi: 10.1371/journal.pone.0248176
27. Kurihara, M, Kamata, K, Nakahara, S, Kitazawa, K, Koizumi, S, and Tokuda, Y. Healthcare use and RT-PCR testing during the first wave of the COVID-19 pandemic in Japan. J Gen Fam Med. (2021) 23:3–8. doi: 10.1002/jgf2.512
28. Dorjdagva, J, Batbaatar, E, and Kauhanen, J. Mass testing for COVID-19 in Ulaanbaatar, Mongolia: “one door-one test” approach. Lancet Reg Health West Pac. (2021) 9:100149. doi: 10.1016/j.lanwpc.2021.100149
29. Ferré, VM, Peiffer-Smadja, N, Visseaux, B, Descamps, D, Ghosn, J, and Charpentier, C. Omicron SARS-CoV-2 variant: what we know and what we don’t. Anaesth Crit care. Pain Med. (2021) 41:100998. doi: 10.1016/j.accpm.2021.100998
30. Chen, J, Wang, R, Gilby, NB, and Wei, G-W. Omicron variant (B.1.1.529): infectivity, vaccine breakthrough, and antibody resistance. J Chem Inf Model. (2022) 62:412–22. doi: 10.1021/acs.jcim.1c01451
31. Yabe, T, Tsubouchi, K, Sekimoto, Y, and Ukkusuri, SV. Early warning of COVID-19 hotspots using human mobility and web search query data. Comput Environ Urban Syst. (2022) 92:101747. doi: 10.1016/j.compenvurbsys.2021.101747
32. Lash, RR, Moonan, PK, Byers, BL, Bonacci, RA, Bonner, KE, Donahue, M, et al. COVID-19 case investigation and contact tracing in the US, 2020. JAMA Netw Open. (2021) 4:e2115850. doi: 10.1001/jamanetworkopen.2021.15850
33. CDC . Health departments. Centers for Disease Control and Prevention (2020). Available at: https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/overview.html (Accessed September 13, 2022).
34. He, Y, Yatsuya, H, Ota, A, and Tabuchi, T. The association of public trust with the utilization of digital contact tracing for COVID-19 in Japan. Public Health Pract. (2022) 4:100279. doi: 10.1016/j.puhip.2022.100279
35. Abeler, J, Bäcker, M, Buermeyer, U, and Zillessen, H. COVID-19 contact tracing and data protection can go together. JMIR Mhealth Uhealth. (2020) 8:e19359. doi: 10.2196/19359
36. Helmy, SA, El-Morsi, RM, Helmy, SAM, and El-Masry, SM. Towards novel nano-based vaccine platforms for SARS-CoV-2 and its variants of concern: advances, challenges and limitations. J Drug Deliv Sci Technol. (2022) 76:103762. doi: 10.1016/j.jddst.2022.103762
37. Neagu, M . The bumpy road to achieve herd immunity in COVID-19. J Immunoass Immunochem. (2020) 41:928–45. doi: 10.1080/15321819.2020.1833919
38. Jeon, J, Han, C, Kim, T, and Lee, S. Evolution of responses to COVID-19 and epidemiological characteristics in South Korea. Int J Environ Res Public Health. (2022) 19:4056. doi: 10.3390/ijerph19074056
39. Feikin, DR, Higdon, MM, Abu-Raddad, LJ, Andrews, N, Araos, R, Goldberg, Y, et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: results of a systematic review and meta-regression. Lancet. (2022) 399:924–44. doi: 10.1016/S0140-6736(22)00152-0
40. Anderson, RM, Vegvari, C, Truscott, J, and Collyer, BS. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. (2020) 396:1614–6. doi: 10.1016/S0140-6736(20)32318-7
41. Deng, X, Garcia-Knight, MA, Khalid, MM, Servellita, V, Wang, C, Morris, MK, et al. Transmission, infectivity, and neutralization of a spike L452R SARS-CoV-2 variant. Cell. (2021) 184:3426–3437.e8. doi: 10.1016/j.cell.2021.04.025
42. Mahase, E . Covid-19: omicron and the need for boosters. BMJ. (2021) 375:n3079. doi: 10.1136/bmj.n3079
43. Ferraz, MVF, Moreira, EG, Coêlho, DF, Wallau, GL, and Lins, RD. Immune evasion of SARS-CoV-2 variants of concern is driven by low affinity to neutralizing antibodies. Chem Commun. (2021) 57:6094–7. doi: 10.1039/D1CC01747K
44. Garcia-Beltran, WF, Lam, EC, St. Denis, K, Nitido, AD, Garcia, ZH, Hauser, BM, et al. Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity. Cell. (2021) 184:2372–2383.e9. doi: 10.1016/j.cell.2021.03.013
45. WHO director-General’s opening remarks at the media briefing on COVID-19 - 14 (2021). Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---14-december-2021 (Accessed April 11, 2022).
46. Lau, H, Khosrawipour, V, Kocbach, P, Mikolajczyk, A, Schubert, J, Bania, J, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. (2020) 27:taaa037. doi: 10.1093/jtm/taaa037
47. Nussbaumer-Streit, B, Mayr, V, Dobrescu, AI, Chapman, A, Persad, E, Klerings, I, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. (2020) 4:CD013574. doi: 10.1002/14651858.CD013574
48. Utsumi, S, Arefin, MR, Tatsukawa, Y, and Tanimoto, J. How and to what extent does the anti-social behavior of violating self-quarantine measures increase the spread of disease? Chaos, Solitons Fractals. (2022) 159:112178. doi: 10.1016/j.chaos.2022.112178
49. Haesebaert, F, Haesebaert, J, Zante, E, and Franck, N. Who maintains good mental health in a locked-down country? A French nationwide online survey of 11,391 participants. Health Place. (2020) 66:102440. doi: 10.1016/j.healthplace.2020.102440
Keywords: COVID-19, core health system, containment strategy, mitigation strategy, East Asia
Citation: Jiao J and Chen W (2024) Core health system measures response to COVID-19 among East Asian countries. Front. Public Health. 12:1385291. doi: 10.3389/fpubh.2024.1385291
Edited by:
Joao Soares Martins, National University of East Timor, Timor-LesteReviewed by:
Muslimah Ithnin, KPJ Healthcare University, MalaysiaCarla Sofia e Sá Farinha, New University of Lisbon, Portugal
Kei Shing Ng, The University of Hong Kong, Hong Kong SAR, China
Copyright © 2024 Jiao and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Chen, Q3c4NTAzMTFAMTYzLmNvbQ==
 Jun Jiao
Jun Jiao Wei Chen2*
Wei Chen2*