- 1Department of Health Policy, Planning and Management, School of Public Health, University of Ghana, Accra, Ghana
- 2Department of Biological, Environmental, and Occupational Health, School of Public Health, University of Ghana, Accra, Ghana
Background: Clinical studies, particularly in the context of HIV/AIDS, have utilized health-related quality of life (HRQoL) and health state utility values to assess both clinical and economic implications. Improvement in HIV management with antiretroviral therapy (ART) has coincided with an increased morbidity of chronic conditions such as diabetes and hypertension among people living with HIV. The study offers empirical evidence establishing a link between HIV, comorbidities like hypertension and diabetes, and their collective impact on HRQoL.
Methods: A cross-sectional quantitative study among 418 HIV patients in three regions of Ghana in the Savannah, Middle Belt, and Coastal belt. Face-to-face interviews were conducted using EuroQol-5 Dimensions-5 Levels (EQ-5D-5L) in combination with EuroQol-Visual Analog Scales (EQ-VAS). Ugandan EQ-5D-5L value set was used for computing the utility values. Patients' socio-demographic and clinical data were obtained from medical records and analyzed descriptively. Mann-Whitney U and Kruskal Wallis tests were used to evaluate the relationship between patient socio-demographic and clinical variables and health status.
Results: Overall median utility value was 0.93(IQR=0.79, 1.00) from the EQ-5D index and 90 (IQR = 80, 100) from the EQ-VAS scores. Prevalence of hypertension and diabetes were 9.1% and 2.4% respectively. There was significant difference in EQ-VAS score between HIV patients with hypertension and those without hypertension (z = 2.146 p = 0.032). There was also a significant difference in the EQ-VAS scores (z = 2.381, p = 0.017) of patients with diabetes and those without diabetes. Region, sex, age, education, marital status, employment status, place of residence, monthly income level, duration of infection, adherence to ART, and other illness were significantly associated with EQ-5D-5L utility and EQ-VAS scores at 0.05 significant level.
Conclusion: HRQoL among HIV positive individuals in Ghana was high. Comorbidities such as hypertension or diabetes had nuanced effects on perceived health status. A patient-centered, multidisciplinary approach to HIV care should be adopted considering regional differences and the presence of comorbidities.
Introduction
The concept of Quality of Life (QoL) which refers to an individual's total wellbeing is intricate, encompassing various contexts and influenced by factors such as personal perspectives, social interactions, environment, and both physical and mental health (1). Several studies have highlighted the impact of clinical considerations, cultural and personal values, as well as social context on the quality of life (1, 2). In situations where quality of life is considered in relation to health and illness, it is sometimes referred to as health-related quality of life (HRQoL) to distinguish it from other dimensions of quality of life such as social and environmental quality of life (3). HRQoL incorporates elements associated with the physical domains of the individual, in addition to factors pertaining to the individual's mental and social dimensions (4). When evaluating treatments for Human Immunodeficiency Virus (HIV) or acquired immunodeficiency syndrome (AIDS), both clinical and economic assessments are conducted, utilizing measures such as patient HRQoL and health state utility values (5). These evaluations provide a comprehensive understanding of the effectiveness of treatments, considering not only clinical outcomes but also the broader impact on individuals' wellbeing in various aspects of their lives.
The World Health Organization reports that HIV remains a serious global public health problem. It reported a death toll of about 42.3 million individuals with certain countries witnessing an alarming surge in newly reported cases following a period of steady decline (6). According to the Joint United Nations Programme on HIV/AIDS (UNAIDS), more people than ever now have advanced HIV infection, which is a factor in the global rise in AIDS prevalence (7). Availability of antiretroviral therapy (ART) has allowed people with HIV to live longer with a growing number of individuals aging with the virus. Hypertension and diabetes, two common chronic comorbidities, have gained prominence in this population since older individuals with HIV are at higher risks of developing comorbid conditions such as hypertension and diabetes (8, 9). These conditions, if not effectively managed, can lead to severe complications, including cardiovascular diseases, kidney disorders, and neurologic impairments (10, 11). The coexistence of HIV with hypertension and/or diabetes poses a multifaceted healthcare challenge, demanding an in-depth exploration of its impact on the overall wellbeing of affected individuals.
Sub-Saharan Africa (SSA) contributes to over 65% of the people living with HIV (PLHIV) (12). While countries in SSA grapple with infectious diseases such as HIV, Malaria, and Tuberculosis, there has been increasing incidence of non-communicable diseases (NCDs) (13). The most prevalent non-communicable diseases (NCDs) in Ghana include cardiovascular disease, cancer, chronic respiratory disorders, diabetes, and sickle cell disease (14). Studies report that cardiovascular diseases and diabetes contribute the largest national NCD burden in Ghana (15–17). NCDs account for about 65% of all fatalities in Ghana, and over 100,000 premature deaths and 10,500 lost of disability-adjusted life years (DALYs) for every 100,000 people in Ghana (15, 18).
In Ghana, the number of people with hypertensive heart disease and diabetes has increased significantly and features in the top 10 causes of death in all health facilities yearly (19). Ghana is experiencing epidemiological and demographic transition which means the incidence of NCDs will continue to rise in the coming years. Non-Communicable Diseases are anticipated to become the leading cause of death by 2030 in SSA including Ghana (14).
Many studies have evaluated the HRQoL of individuals living with HIV in several countries including Ethiopia (5), Columbia (20), and Nigeria (8). In Ethiopia, it was found that individuals living with HIV exhibit high HRQoL with median EQ-5D index and the EQ-VAS scores of 0.94 and 80 respectively. However, issues such as anxiety/depression and pain/discomfort were prevalent (5). EQ-5D-5L scores of 0.85 ± 0.21 and EQ-VAS score of 84 ± 14 were reported in Bogotá, Colombia among HIV patients receiving antiretroviral therapy (20). Although these studies reported high HRQoL, most of them were limited to solitary healthcare settings and comorbidities.
Despite the importance of QoL measurement and its usefulness in improving health outcomes and cumulative impact, it remains largely under-researched particularly in low and middle-income countries (LMICs). Notably, within the Ghanaian context, there is a dearth of studies assessing the HRQoL among patients dealing with the co-morbidities of HIV and conditions such as hypertension or diabetes.
This study seeks to address this gap by specifically investigating the HRQoL among individuals in Ghana who are simultaneously managing HIV and contending with the challenges of coexisting hypertension or diabetes. By focusing on this intersection of health concerns, the research aims to contribute valuable insights into the HRQoL of a population facing complex health conditions, ultimately fostering a better understanding of their unique needs and experiences.
Methods
Study design and setting
The study utilized a cross-sectional design with a quantitative approach to assess the HRQoL among HIV patients and investigate the prevalence of hypertension and diabetes. Cross-sectional studies offer a momentary depiction of outcomes and associated attributes at a specific point in time, making them suitable for capturing individual characteristics and desired outcomes concurrently (21). This design facilitated the examination of the relationship between individual characteristics and the targeted health outcomes. The study was conducted in three regions of Ghana, spanning the Savannah, middle belt, and coastal belt ecological zones, specifically in the Greater Accra, Ashanti, and Upper West regions. These regions were purposively selected due to the high prevalence of HIV cases in their respective ecological zones, as reported in the latest Ghana AIDS Commission fact sheets from 2019 (22). ART clinics in Madina Polyclinic, Kumasi South Hospital, and Wa Municipal Hospital were selected as survey sites. These ART clinics are well established healthcare facilities that provide antiretroviral therapy and other essential services like chronic care. Additionally, these facilities are situated within the capital of the selected regions and therefore have a large population of HIV patients and also serve as a referral point for ART services for other facilities within their respective regions.
Study population, sample size and sampling
The study population comprised individuals 18 years and above living with HIV/AIDS who visited the HIV treatment clinic at the selected facilities from August to September 2023. The sample size for this study was determined using the Cochran formula (23). The determination of the sample size for the study was derived from the prevalence of hypertension in individuals who are HIV positive. Considering hypertension being the most prevalent comorbidity of 30.8% as compared to diabetes (24). A convenience sampling technique was employed to select HIV patients who were eligible to partake in the study. Participants were recruited at the health facility level; thus, HIV treatment centers were purposively selected for recruiting potential respondents. PLHIV who were present and accessible at the HIV treatment center on each day of data collection during clinic hours (8am−4pm) were selected and each participant was given a unique identification code. Those individuals who met the stipulated criteria for inclusion and provided written informed consent were chosen to participate in the study until the minimum sample size was achieved. Given the sensitive nature of HIV and the significant stigma associated, respondents were selected based on their availability and willingness to participate at the time of data collection.
Data collection
The study employed the EuroQoL 5-dimension instrument (EQ-5D) to measure HRQoL, utilizing the 5-level EQ-5D (EQ-5D-5L) and the EuroQoL-visual analog scale (EQ-VAS). EQ-5D-5L, designed with five dimensions assessing mobility, self-care, usual activities, pain/discomfort, and anxiety/depression across five severity levels, allowed for a comprehensive evaluation of participants' health states. The VAS recorded overall health on a 20 cm vertical scale that features endpoints denoted as 0 (“the worst health you can imagine”) and 100 (“the best health you can imagine”) (25). The EQ-5D-5L has demonstrated good measurement properties, including reliability, validity, and responsiveness, when used in HIV/AIDS populations across various settings (26, 27). Additionally, as a preference-based instrument, the EQ-5D-5L provides utility scores that can be used for economic evaluations and cost-utility analyses (26, 28). The questionnaire which was administered in English and local dialects, collected socio-demographic and clinical characteristics data from medical records after obtaining written informed consent from respondents. Respondents self-reported the presence of hypertension and diabetes. Additionally, clinical characteristics data obtained from the medical records included the disease duration, duration on ART, CD4 count, blood pressure, viral load and other illnesses. Adherence to ART was self-reported by the respondents. A structured questionnaire with close-ended questions facilitated face-to-face data collection, administered by trained health workers who served as research assistants in about 10–15-min interviews. Data was collected from August to September 2023 with monthly income reflecting the 2023 currency year.
Data processing and analysis
Data collected was entered into Microsoft Excel 2016 by two research assistants, checked and cleaned by the researcher and then imported into STATA version 16 for analysis. Descriptive statistics such as frequency, percentage, mean, median, and standard deviation were used to present socio-demographic and clinical data, as well as EQ-5D-5L health profiles, EQ-VAS, and EQ-5D utility scores. The EQ-5D-5L value sets for Uganda were employed for the valuation of participants' health states due to the absence of value sets for Ghana at the time. Also, Uganda's cultural, socio-economic, and health system characteristics are similar to that of Ghana and offers a close approximation of HRQoL valuations. These similarities suggest that the health preferences and quality of life valuations of individuals from both countries might be more aligned. The value sets were applied by converting 5-digit health states to single summary index values using corresponding weights (29). HRQoL scores were determined, and normality tests revealed non-normal distribution for EQ-5D-5L utility and EQ-VAS scores. Non-parametric statistical analyses, including Mann-Whitney U and Kruskal Wallis tests, were utilized to assess associations between patient variables and health status (30). The outcome variables were EQ-5D utility scores and EQ-VAS scores. Independent variables included socio-demographic characteristics and respondents' clinical data (viral load, blood pressure, other illnesses). P-values <0.05 were considered statistically significant.
Ethical considerations
Ethical clearance was obtained from the Ghana Health Service Ethics Review Committee with reference number: GHS-ERC027/05/23. Written informed consent was obtained from all respondents before data collection.
Results
Participants' demographic and clinical characteristics
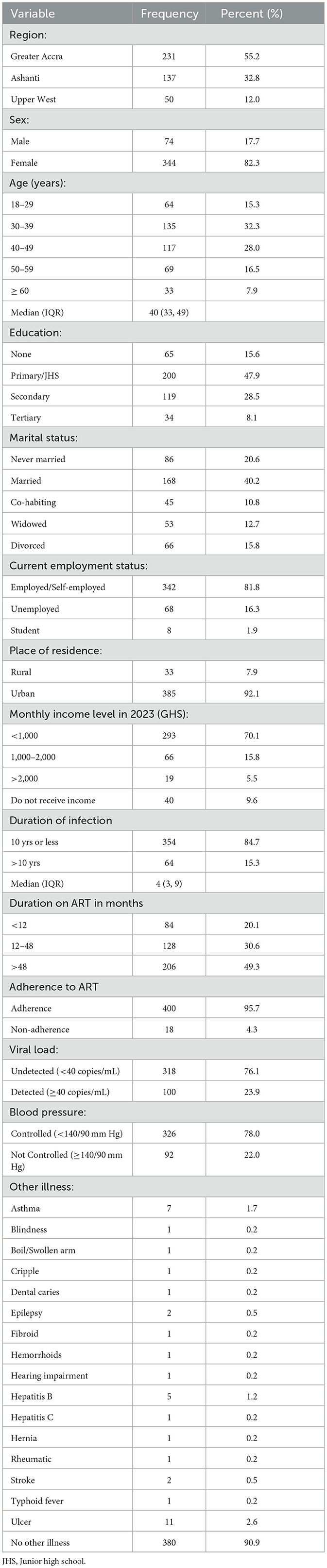
The study enrolled a total of 418 patients with wide-ranging demographic and clinical characteristics. From Table 1, majority of respondents 55.2% (n = 231) come from the Greater Accra region, followed by Ashanti 32.8% (n = 137) and Upper West 12.0% (n = 50). The patient population was predominantly female 82.3% (n = 344). The median age of the participants was 40 (IQR = 33, 49) years. The majority of the participants, 32.3% (n = 135), fell within the age group of 30–39 years.
Nearly half of the participants (47.9%, n = 200) had completed only Primary/JHS education, while just 8.1% (n = 34) had attained tertiary education. Also, the majority (40.2%, n = 168) of participants were married. The majority of respondents (81.8%, n = 342) were either employed or self-employed, whereas only 1.9% (n = 8) were students. Additionally, 92.1% (n = 385) of participants lived in urban areas. Furthermore, 70.1% (n = 293) had a monthly income less than GHS1,000, only 5.5% (n = 19) had monthly income more than GHS2,000 and 9.6% (n = 40) reported no monthly income. The median duration of HIV infection was 4 (IQR=3, 9) years with 84.7% (n = 354) of respondents reported to have been infected for 10 years or less. Moreover, almost half (49.3%, n = 206) of respondents reported being on ART for more than 48 months. The majority of respondents (95.7%, n = 400) were adherent to ART. Also, the majority (76.1%, n = 318) of participants had an undetected viral load and the majority had controlled blood pressure (78%, n = 326). In addition, 9.1% (n = 38) reported having other illnesses, with ulcers being the most reported illness followed by asthma.
Self-reported health profile of people living with HIV
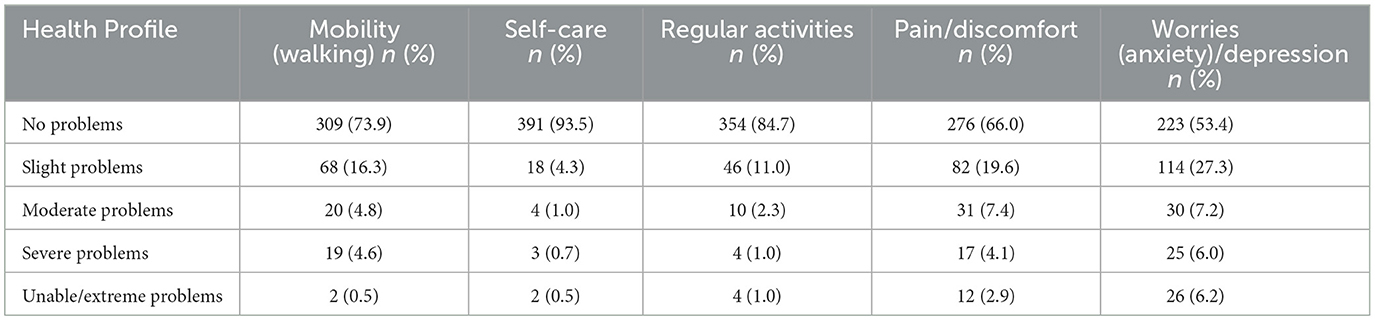
From Table 2, it can be observed that a considerable majority of the participants, specifically 73.9% (n = 309) had no problem with mobility. Additionally, the majority of respondents 93.5% (n = 391) reported no difficulties with self-care. The majority of respondents (84.7% n = 354) had no problems with regular activities. In relation to pain and discomfort, 66.0% (n = 276) reported no problems. A considerable percentage reported slight to extreme pain or discomfort (34%). More than half of respondents 53.4% (n = 223) reported not being worried or depressed. However, almost half (46.7%) reported slight to extreme levels of worry and depression.
Health-related quality of life score for people living with HIV
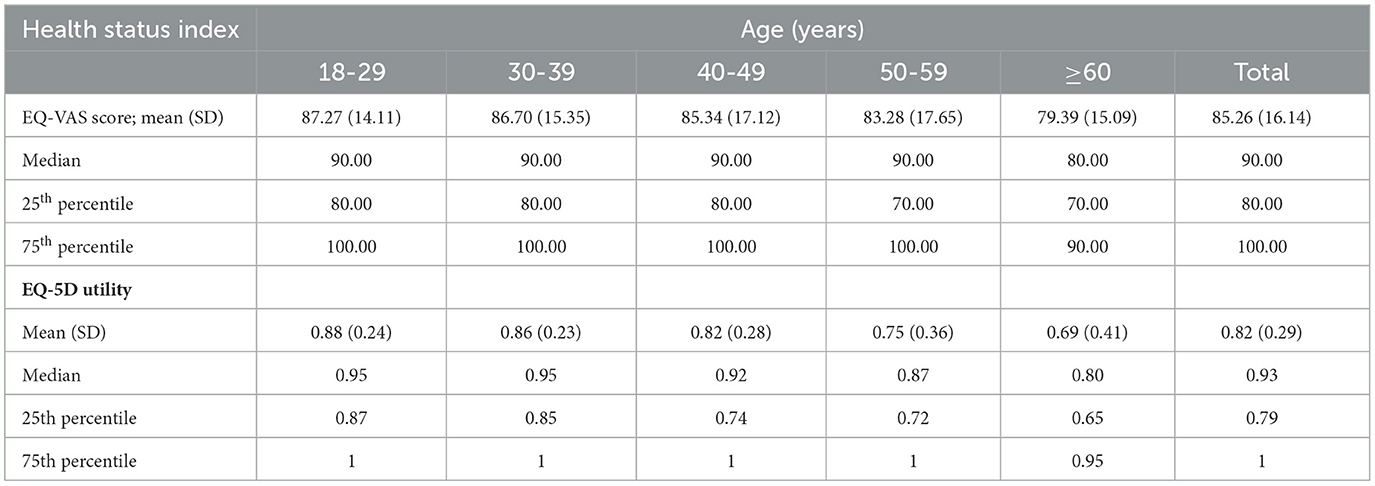
Table 3 indicates the health status indices for the total sample along with the values stratified by age. The median EQ-VAS score was 90.00 (IQR = 80.00, 100.00) and the median EQ-5D utility score was 0.93 (IQR=0.79, 1.00). Respondents within the age group of 18–29 years reported the highest EQ-VAS score and EQ-5D utility score of 87.27± 14.11 and 0.88± 0.24 respectively. On the other hand, participants within the age group ≥60 years reported the lowest mean EQ-VAS score and EQ-5D utility score of 79.39± 15.09 and 0.69± 0.41 respectively.
Prevalence of hypertension and diabetes among HIV patients
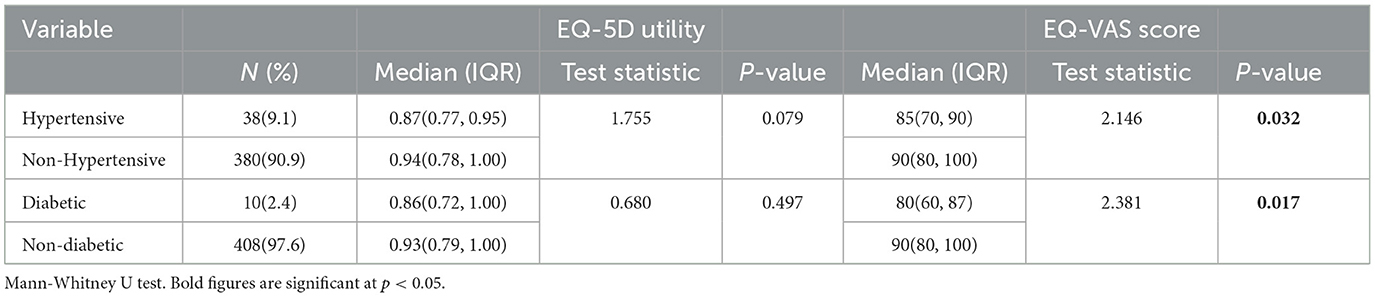
From Table 4, the prevalence of hypertension was 9.1%. The median EQ-5D utility score was 0.87 (IQR = 0.77, 0.95) for hypertensive patients and 0.94 (IQR = 0.78, 1.00) for non-hypertensive patients. The Mann-Whitney U test shows a test statistic of z=1.755 with a p-value of 0.079, indicating that there is no statistically significant difference in EQ-5D utility scores between the two groups. However, the median EQ-VAS score was 85 (IQR = 70, 90) for hypertensive patients and 90 (IQR = 80, 100) for non-hypertensive patients. The Mann-Whitney U test shows a test statistic of z=2.146 with a p-value of 0.032, which is significant at p < 0.05.
On the other hand, the prevalence of diabetes was 2.4%. The median EQ-5D utility score was 0.86 (IQR = 0.72, 1.00) for diabetic patients and 0.93 (IQR = 0.79, 1.00) for non-diabetic patients. The Mann-Whitney U test shows a test statistic of z = 0.680 with a p-value of 0.497, indicating that there is no statistically significant difference in EQ-5D utility scores between the two groups. However, the median EQ-VAS score was 80 (IQR = 60, 87) for diabetic patients and 90 (80,100) for non-diabetic patients. The Mann-Whitney U test shows a test statistic of z = 2.381 with a p-value of 0.017, which is statistically significant at p < 0.05.
Factors influencing HIV patients' HRQoL
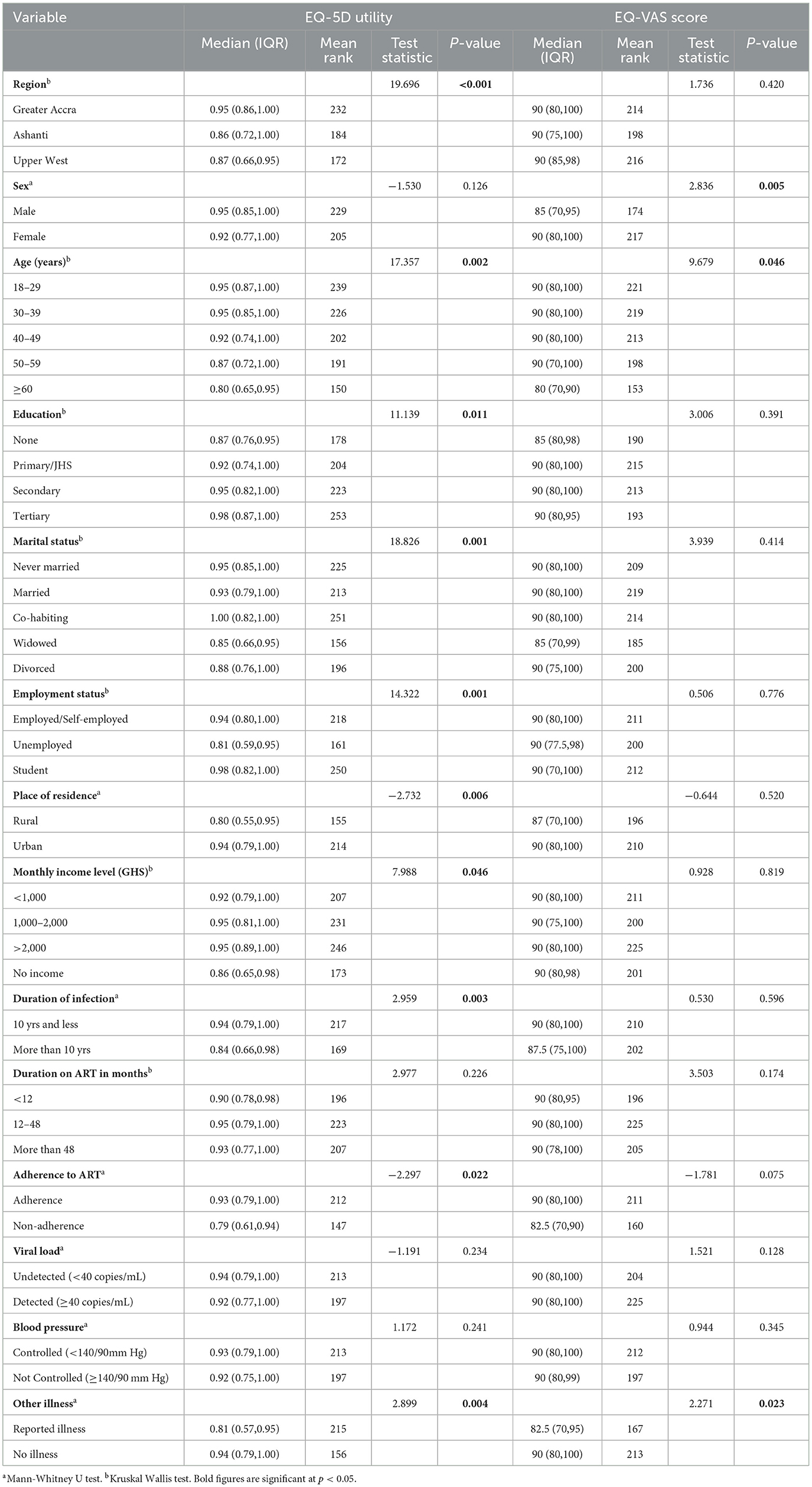
Table 5 reports the association of patients' characteristics with HRQoL. From the Kruskal Wallis test, there was a significant difference in EQ-5D utility score [χ2(2) =19.696, p < 0.001] among the three regions. No significant difference in EQ-VAS scores was observed among regions. The Mann-Whitney U test showed no significant difference in EQ-5D utility score between male and female, however, there was a significant difference in EQ-VAS scores (z = 2.836, p = 0.005). There was a significant difference in both EQ-5D utility [χ2(2) =17.357, p = 0.002] and EQ-VAS score [χ2(2) =9.679, p = 0.046] among age groups. Scores tend to decrease with increasing age, with the ≥60 age group displaying the lowest median score. Moreover, educational levels significantly influence EQ-5D utility scores [χ2(2) = 11.139, p = 0.011]. Tertiary-educated individuals reported higher EQ-5D utility scores compared to those with lower educational levels.
Also, there was a significant difference in EQ-5D utility scores [χ2(2) = 18.826, p = 0.001] among the marital status categories with those co-habiting reporting the highest EQ-D utility scores. Additionally, there was a significant difference in the EQ-5D utility scores [χ2(2) = 14.322, p = 0.001] among the employment status categories but no difference in the EQ-VAS score. Students reported higher EQ-5D utility scores compared to other employment categories. A significant difference was found in the EQ-5D utility score (z = −2.732, p = 0.006) between the two categories of place of residence, but no significant difference was observed in the EQ-VAS score. Urban residents reported higher EQ-5D utility scores compared to rural residents. Moreover, there was a marginally significant difference in the EQ-5D utility score [χ2(2) = 7.988, p = 0.046] across the various monthly income levels. Duration of infection significantly influences EQ-5D utility scores (z = 2.959, p = 0.003). Individuals with longer infection durations (>10 years) tend to have slightly lower EQ-5D utility scores. Furthermore, there was a significant difference in the EQ-5D utility scores among patients' adherence level, with those adhering to ART tending to have higher EQ-5D utility scores compared to non-adhering individuals. There is a significant difference in both the EQ-5D utility score (z = 2.899, p = 0.004) and EQ-VAS score (z = 2.271, p = 0.023) between HIV patients who reported other illness and patients who did not report any illness.
Discussion
The study included a diverse group of 418 HIV patients with representation across different ecological zones, this signifies a heterogeneous patient population. The majority of the participants were female, constituting 82.3% of the sample. This sex distribution reflects the global trend where women are disproportionately affected by HIV (31). In sub-Saharan Africa, about 62% of new HIV infections were among females of all ages. This corroborates the findings of this study. However, in some other jurisdictions, males of all ages experienced a proportionately higher incidence of HIV infections as of 2023 (31). The median age of the participants was 40 years, with a wide age range from 18 to 76 years. The self-reported health profiles of HIV/AIDS patients indicate varying degrees of challenges across different dimensions of health.
The prevalent challenges reported by respondents predominantly centered around the pain/discomfort and anxiety/depression dimensions of the EQ-5D-5L. Consistent with prior research conducted in Ethiopia, Nigeria, and Colombia, individuals living with HIV/AIDS exhibited a higher frequency of issues related to the anxiety/depression dimension compared to the general population (5, 8, 20). This underscores the necessity for an elevated standard of healthcare provision tailored to mitigate the health challenges faced by HIV/AIDS patients, with a particular emphasis on mental and palliative care. It is crucial to recognize that even mild levels of anxiety or depression can significantly impact an individual's overall wellbeing and quality of life, emphasizing the importance of addressing these concerns and offering appropriate psychological support.
The study's findings reveal a relatively high level of self-assessed HRQoL among HIV patients. Similar to a study conducted by Osei-Yeboal et al. (32) in the Volta region of Ghana, approximately 89% of PLHIV reported high HRQoL (32). This could be due to improvement in the access to ART and other support services, improvement in awareness and education, adequate psychosocial support including counseling and mental health resources, government initiatives and efforts by stakeholders, especially the non-governmental organizations (NGOs) to address HIV/AIDS. Although these scores align with those reported in Ethiopia (5) and England (33), they are comparatively lower than the findings of studies by Keaei et al. (20) in Colombia and Popping et al. (33) in the Netherlands. Additionally, it was observed that the perceived health status and overall quality of life of PLHIV tend to decline with increasing age. This underscores the significance of recognizing age-related disparities in healthcare planning and interventions. Consequently, acknowledging these differences becomes essential for the development of targeted interventions that focus on enhancing wellbeing and addressing the distinct needs of various age cohorts within the PLHIV community.
Only 9.1% of the survey respondents acknowledged having hypertension, a notably low prevalence considering that hypertension is a common comorbidity in individuals with HIV (34). In a prior study conducted in Ghana, the reported prevalence of hypertension was significantly higher at 30.8% (24). The unexpectedly lower prevalence observed in our study may be attributed to various factors, including underreporting of lack of awareness regarding one's health conditions. Also, the prevalence of diabetes among PLHIV was only 2.4%. This finding aligns with results from a study in Nigeria (8) and is lower than previous reports in Ghana (35, 36). Similar to hypertension, the surprisingly low prevalence of diabetes is noteworthy, given the increased risk of diabetes in HIV patients (37). This lower prevalence might be linked to underreporting or lack of awareness among the affected individuals. Alternatively, due to the high adherence rates to ART, HIV patients often engage in frequent interactions with healthcare personnel during routine follow-up appointments. This consistent contact facilitates the provision of education and counseling regarding the prevention of additional health conditions, such as NCDs, which may contribute to the observed lower prevalence rates of these conditions within this population. These outcomes emphasize the crucial need for regular health screenings, monitoring, and education for individuals with HIV who have comorbidities. The results suggest that a portion of the population may have undiagnosed or unreported hypertension and diabetes. Effective management of these comorbid conditions is paramount for ensuring the overall wellbeing of individuals living with HIV. The relatively low prevalence of these comorbidities also prompts further research to gain a deeper understanding of the factors contributing to their rarity in this specific population.
The study revealed a potential association between hypertension and a diminished HRQoL among HIV patients. While the difference in EQ-5D utility scores does not reach statistical significance, the EQ-VAS scores portray a meaningful disparity. Hypertensive individuals demonstrated lower median EQ-VAS scores, suggesting a potential impact on their perceived health and wellbeing compared to non-hypertensive peers. In the case of diabetes, though the difference in EQ-5D utility scores isn't statistically significant, a notable discrepancy emerges in EQ-VAS scores between diabetic and non-diabetic HIV patients. This discrepancy signifies a potential impact of diabetes on the subjective health perception of individuals, indicating a lower perceived health status among diabetic individuals.
These findings hold significance in clinical settings. Addressing hypertension and diabetes management among HIV patients might not only target the management of these conditions but also potentially improve their perceived health and overall wellbeing. It emphasizes the need for a holistic approach in healthcare interventions, considering not only the primary condition (HIV) but also comorbidities and their effects on the individual's HRQoL (38).
This study also delved into various patient-related factors that contribute to the perceived health status among individuals with HIV. Notably, regional disparities were observed, with significantly higher EQ-5D utility and EQ-VAS scores in Greater Accra compared to Ashanti and Upper West regions. These differences may indicate potential health disparities influenced by variations in healthcare infrastructure, accessibility, or socio-economic factors across these regions (39–41).
Moreover, gender emerged as a factor influencing perceived health status, as reflected in the EQ-VAS scores. While EQ-5D utility did not show gender disparity, females exhibited notably higher EQ-VAS scores. The reasons for this gender-based difference are likely multifaceted, involving biological, psychological, and sociocultural factors. This result aligns with the findings of Melaku et al. (42) but contrasts with studies conducted in Nigeria (8) and Ethiopia (5). Understanding these variations contributes to a more nuanced comprehension of how different factors may impact the perceived health status of HIV patients in diverse contexts.
Age emerges as a significant factor affecting health perception, with younger age groups reporting better health status compared to their older counterparts. This phenomenon may be attributed to the slower progression of diseases among younger individuals, bolstered immune systems, and robust social networks, including supportive family and friends. These networks contribute emotional and practical support, thereby positively impacting mental health and overall quality of life. This discovery corroborates with prior research findings (42, 43) and contrast with the conclusions drawn in Jackson et al. (8). Additionally, this underscores the imperative for age-specific interventions and support systems tailored to address the unique needs of older adult individuals living with HIV.
Educational attainment and employment status demonstrate a positive correlation with higher perceived health. Individuals with tertiary education, those employed or self-employed, and those with a monthly income exceeding GHS 1,000 tend to exhibit better health perception. This underscores the potential role of socio-economic empowerment in fostering improved health outcomes among individuals living with HIV, as evidenced by existing studies (39–41, 44). Other socio-demographic factors, including marital status and residence, were also identified as significant influences on the HRQoL of PLHIV. Understanding and addressing these factors are crucial in formulating comprehensive strategies to enhance the wellbeing of individuals by navigating the complexities of living with HIV.
The results derived from this study underscore the impact of infection duration on patients' HRQoL. Notably, individuals living with HIV for a period of 10 years or less reported higher HRQoL compared to those with more than 10 years of living with the virus. This disparity may be attributed to the progression of the disease over time, with prolonged exposure potentially leading to advanced stages and consequential effects on health status.
Moreover, the study revealed a significant correlation between adherence to ART and EQ-5D utility scores. This implies that individuals who adhere more closely to their antiretroviral treatment exhibit a higher HRQoL. These findings align with previous studies that have reported similar positive associations (43, 45, 46). The efficacy of ART is evident in its ability to suppress HIV replication, resulting in a substantial reduction in AIDS-related mortality, morbidity, and symptomatic experiences among PLHIV (1, 47, 48).
Additionally, a noteworthy discrepancy in HRQoL was observed among individuals living with HIV who disclosed the presence of other comorbidities in comparison to those who did not. This disparity suggests that the existence of additional illnesses is linked to a diminished state of HRQoL. Consistent with these findings, the study by Van Duin et al. (49) also highlighted a substantial association between the presence of multiple comorbidities and utility scores (49). This emphasizes the intricate relationship between the overall health status of individuals with HIV and the presence of concurrent health challenges, further highlighting the importance of a comprehensive approach to healthcare for this population.
Conclusion
The study revealed improved quality of life among HIV-positive individuals in Ghana. It underscores the effect of demographic, clinical, and socioeconomic factors on quality of life. However, regional differences significantly influenced health perceptions among HIV patients, with Greater Accra showing higher health scores compared to the Ashanti and Upper West regions. The significant disparities in HRQoL between regions and across different income levels highlight the need for targeted interventions to address these disparities. Additionally, the findings indicated that only a small proportion of these individuals reported coexisting hypertension or diabetes. Interestingly, hypertension and diabetes appeared to have nuanced effects on the perceived health status of individuals living with HIV. The higher HRQoL scores among individuals who are adherent to ART emphasize the importance of sustained treatment and adherence in managing HIV effectively.
In light of these observations, the study underscores the significance of adopting a patient-centered, multidisciplinary approach to HIV care. Recognizing the regional variations and the impact of co-morbidities on health perceptions emphasizes the need for tailored and comprehensive strategies to address the diverse needs of HIV-positive individuals, contributing to an improved quality of life and overall wellbeing. Future studies should focus on longitudinal studies to provide a comprehensive understanding and develop causal relationships to lay foundations for more effective policies and interventions.
Limitations and strengths
This study reports a few limitations that were observed. First, the study's cross-sectional nature might limit the ability to establish causality. Also, due to the low level of education of most of the HIV patients, it was necessary for skilled staff at the ART unit of the facilities to assist in comprehending the study questionnaire, originally intended to be self-administered. This might have introduced some biases in the responses. Lastly, there might be biases as patients self-reported their hypertension and diabetic status. The confinement of the EQ-5D-5L to 5 dimensions and 5 levels can limit the ability to capture subtle changes in health status. The EQ-VAS may be subject to subjective biases or may not be highly sensitive to detect small changes in health.
However, these tools have been widely used and validated for various populations. This study provided a robust and comprehensive assessment of HRQoL among HIV patients by conducting the study in three regions (Greater Accra, Ashanti, and Upper West) across three distinct ecological zones in Ghana. Thus, it offers insights into regional disparities in HRQoL, enhancing the generalizability of the findings within the country.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ghana Health Service Ethics Review Committee with reference number: GHS-ERC027/05/23. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
RO: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. EBK: Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. SAB: Conceptualization, Data curation, Funding acquisition, Project administration, Supervision, Writing – original draft, Writing – review & editing. DDO: Data curation, Writing – original draft, Writing – review & editing. JN: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study received funding from the Royal Society of Tropical Medicine and Hygiene. However, funder played no role in the manuscript writing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AIDs, Acquired Immunodeficiency Syndrome; ART, Antiretroviral therapy; DALYs, Disability Adjusted Life Years; EQ-5D, EuroQoL 5-dimension; EQ-VAS, EuroQoL-visual analog scale; HIV, Human Immunodeficiency Virus; HRQoL, Health Related Quality of Life; PLHIV, People Living with HIV; QoL, Quality of Life.
References
1. Joulaei H, Mousavi SG, Foroozanfar Z, Rakhshani T. Health-related quality of life in people living with HIV in Southwest Iran in 2018: a cross-sectional study. BioMed Res Int. (2021) 2021:9935175. doi: 10.1155/2021/9935175
2. Arjun BY, Unnikrishnan B, Ramapuram JT, Thapar R, Mithra P, Kumar N, et al. Factors influencing quality of life among people living with HIV in coastal South India. J Int Assoc Prov AIDS Care (JIAPAC). (2017) 16:247–53. doi: 10.1177/2325957415599213
3. Nigusso FT, Mavhandu-Mudzusi AH. Health-related quality of life of people living with HIV/AIDS: the role of social inequalities and disease-related factors. Health Qual Life Outcomes. (2021) 19:1–11. doi: 10.1186/s12955-021-01702-2
4. Hernández-Segura N, Marcos-Delgado A, Pinto-Carral A, Fernández-Villa T, Molina AJ. Health-related quality of life (HRQOL) instruments and mobility: a systematic review. Int J Environ Res Public Health. (2022) 19:16493. doi: 10.3390/ijerph192416493
5. Belay YB, Ali EE, Sander B, Gebretekle GB. Health-related quality of life of patients with HIV/AIDS at a tertiary care teaching hospital in Ethiopia. Health Qual Life Outcomes. (2021) 19:1–11. doi: 10.1186/s12955-021-01670-7
6. WHO. HIV and AIDS-Key Facts. (2023). Available at: https://www.who.int/news-room/fact-sheets/detail/hiv-aids (accessed December 02, 2023).
7. UNAIDS. 90-90-90: An Ambitious Treatment Target to Help End the AIDS Epidemic. Geneva: UNAIDS (2014).
8. Jackson IL, Igwe CN, Effiong DE, Ukwe CV. Health-related quality of life of HIV positive patients with hypertension: is there an association with blood pressure control? High Blood Press Cardiovasc Prevent. (2022) 29:393–400. doi: 10.1007/s40292-022-00527-4
9. Nguyen MH, Lim JK, Burak Ozbay A, Fraysse J, Liou I, Meyer N, et al. Advancing age and comorbidity in a US insured population-based cohort of patients with chronic hepatitis B. Hepatology. (2019) 69:959–73. doi: 10.1002/hep.30246
10. Monteiro A, Castro P, Pereira G, Ferreira C, Sorond F, Milstead A, et al. Neurovascular coupling is impaired in hypertensive and diabetic subjects without symptomatic cerebrovascular disease. Front Aging Neurosci. (2021) 13:728007. doi: 10.3389/fnagi.2021.728007
11. Raina SK, Chander V, Raina S, Kumar D, Grover A, Bhardwaj A. Hypertension and diabetes as risk factors for dementia: a secondary post-hoc analysis from north-west India. Ann Indian Acad Neurol. (2015) 18:63–5. doi: 10.4103/0972-2327.151045
13. Abdulai MA, Marable JK, Wadus A, Asante KP, A. qualitative analysis of factors influencing health-seeking behavior of people living with HIV, hypertension and diabetes in an urban area of Ghana. J Multimorb Comorb. (2022) 12:26335565221092664. doi: 10.1177/26335565221092664
14. WHO. Beating Noncommunicable Diseases Through Primary Healthcare. (2022). Available at: https://www.afro.who.int/countries/ghana/news/beating-noncommunicable-diseases-through-primary-healthcare (accessed November 203, 2023).
15. Boakye H, Atabila A, Hinneh T, Ackah M, Ojo-Benys F, Bello AI. The prevalence and determinants of non-communicable diseases among Ghanaian adults: A survey at a secondary healthcare level. PLoS ONE. (2023) 18:e0281310. doi: 10.1371/journal.pone.0281310
16. Ministry of Health. National Policy- Non-Communicable Diseases. Accra: Ministry of Health (2022). Available at: https://www.moh.gov.gh/wp-content/uploads/2022/05/Ghana-NCD-Policy-2022.pdfViewless (accessed November 12, 2023).
17. Ofori-Asenso R, Garcia D. Cardiovascular diseases in Ghana within the context of globalization. Cardiovasc Diagn Ther. (2016) 6:67.
18. Ministry of Health. Strategy for the Management, Prevention and Control of Chronic Non-Communicable Diseases in Ghana. (2012). Available at: https://extranet.who.int/countryplanningcycles/sites/default/files/country_docs/Ghana/ghana.pdf
19. Ghana Health Service. The Health Sector in Ghana: Facts and Figures 2018. Accra: Ghana Health Service (2018). Available at: https://open.africa/dataset/4176f749-cfa8-4e32-9418-86cef78f9db6/resource/0bcf9b54-3e35-4543-95cd-fd4de953edff/download/factsfigures_2018.pdf (accessed November 15, 2023).
20. Keaei M, Kuhlmann J, Conde R, Evers SM, Gonzalez J, Govers M, et al. Health-related quality of life of patients with HIV/AIDS in Bogotá, Colombia. Value in Health Region Issues. (2016) 11:68–72. doi: 10.1016/j.vhri.2016.05.001
21. Wang X, Cheng Z. Cross-sectional studies: strengths, weaknesses, and recommendations. Chest. (2020) 158:S65–71. doi: 10.1016/j.chest.2020.03.012
22. Ghana AIDS Commission. Ghana HIV Fact Sheet 2019. Accra: Ghana AIDS Commission (2019). Available at: https://gac3.reseauafrique.net/wp-content/uploads/2023/05/2019-FACT-SHEET-22-06-2020-revised11.pdf (accessed November 15, 2023).
24. Sarfo FS, Nichols M, Singh A, Hardy Y, Norman B, Mensah G, et al. Characteristics of hypertension among people living with HIV in Ghana: impact of new hypertension guideline. J Clini Hypert. (2019) 21:838–50. doi: 10.1111/jch.13561
25. Devlin NJ, Brooks R. EQ-5D and the EuroQol group: past, present and future. Appl Health Econ Health Policy. (2017) 15:127–37. doi: 10.1007/s40258-017-0310-5
26. Feng Y-S, Kohlmann T, Janssen MF, Buchholz I. Psychometric properties of the EQ-5D-5L: a systematic review of the literature. Qual Life Res. (2021) 30:647–73. doi: 10.1007/s11136-020-02688-y
27. Tran BX, Ohinmaa A, Nguyen LT. Quality of life profile and psychometric properties of the EQ-5D-5L in HIV/AIDS patients. Health Qual Life Outcomes. (2012) 10:1–8. doi: 10.1186/1477-7525-10-132
28. Wang X, Luo H, Yao E, Tang R, Dong W, Liu F, et al. Health utility measurement for people living with HIV/AIDS under combined antiretroviral therapy: a comparison of EQ-5D-5L and SF-6D. Medicine. (2022) 101:e31666. doi: 10.1097/MD.0000000000031666
29. Devlin N, Parkin D, Janssen B. Methods for Analysing and Reporting EQ-5D Data. Cham: Springer Nature (2020).
30. Nahm FS. Nonparametric statistical tests for the continuous data: the basic concept and the practical use. Korean J Anesthesiol. (2016) 69:8–14. doi: 10.4097/kjae.2016.69.1.8
31. UNAIDS. UNAIDS Data 2023. (2023). Available at: https://www.unaids.org/en/resources/documents/2023/2023_unaids_data (accessed December 11, 2023).
32. Osei-Yeboah J, Owiredu WK, Norgbe GK, Lokpo SY, Obirikorang C, Alote Allotey E, et al. Quality of life of people living with HIV/AIDS in the Ho municipality, Ghana: a cross-sectional study. AIDS Res Treat. (2017) 2017:6806951. doi: 10.1155/2017/6806951
33. Popping S, Kall M, Nichols BE, Stempher E, Versteegh L, van de Vijver DA, et al. Quality of life among people living with HIV in England and the Netherlands: a population-based study. Lancet Regional Health. (2021) 8:100177. doi: 10.1016/j.lanepe.2021.100177
34. Mutagonda RF, Siril H, Kaaya S, Amborose T, Haruna T, Mhalu A, et al. Prevalence and determinants of non-communicable diseases including depression among HIV patients on antiretroviral therapy in Dar es Salaam, Tanzania. Trop Med Int Health. (2022) 27:742–51. doi: 10.1111/tmi.13790
35. Appiah LT, Sarfo FS, Huffman MD, Nguah SB, Stiles JK. Cardiovascular risk factors among Ghanaian patients with HIV: a cross-sectional study. Clin Cardiol. (2019) 42:1195–201. doi: 10.1002/clc.23273
36. Sarfo FS, Norman B, Nichols M, Appiah L, Osei Assibey S, Tagge R, et al. Prevalence and incidence of pre-diabetes and diabetes mellitus among people living with HIV in Ghana: evidence from the EVERLAST Study. HIV Med. (2021) 22:231–43. doi: 10.1111/hiv.13007
37. Rajagopaul A, Naidoo M. Prevalence of diabetes mellitus and hypertension amongst the HIV-positive population at a district hospital in eThekwini, South Africa. African J Primary Health Care & Family Med. (2021) 13:2766. doi: 10.4102/phcfm.v13i1.2766
38. Boyd CM, Lucas GM. Patient-centered care for people living with multimorbidity. Curr Opin HIV AIDS. (2014) 9:419. doi: 10.1097/COH.0000000000000073
39. Kraft P, Kraft B. Explaining socioeconomic disparities in health behaviours: a review of biopsychological pathways involving stress and inflammation. Neurosci Biobehav Rev. (2021) 127:689–708. doi: 10.1016/j.neubiorev.2021.05.019
40. Organization WH. Health Inequities and Their Causes. (2018). Available fatrom: https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes (accessed December 11, 2023).
41. Riley WJ. Health disparities: gaps in access, quality and affordability of medical care. Trans Am Clin Climatol Assoc. (2012) 123:167.
42. Melaku T, Mamo G, Chelkeba L, Chanie T. Health-related quality of life among people living with human immunodeficiency virus on highly active antiretroviral therapy in Ethiopia: PROQOL-HIV based survey. Patient Relat Outcome Meas. (2020) 2020:73–86. doi: 10.2147/PROM.S239429
43. Ahmed A, Saqlain M, Bashir N, Dujaili J, Hashmi F, Mazhar F, et al. Health-related quality of life and its predictors among adults living with HIV/AIDS and receiving antiretroviral therapy in Pakistan. Qual Life Res. (2021) 30:1653–64. doi: 10.1007/s11136-021-02771-y
44. Ilinca S, Di Giorgio L, Salari P, Chuma J. Socio-economic inequality and inequity in use of health care services in Kenya: evidence from the fourth Kenya household health expenditure and utilization survey. Int J Equity Health. (2019) 18:1–13. doi: 10.1186/s12939-019-1106-z
45. Mwangi J, Ternent L, Ujiji POA, Were E, Ekström AM. Health related quality of life among pregnant women living with HIV in Kenya, results from comparing a patient generated index and the Euroqol 5 dimension 3 level. BMC Women's Health. (2022) 22:66. doi: 10.1186/s12905-022-01646-9
46. Tran BX. Quality of life outcomes of antiretroviral treatment for HIV/AIDS patients in Vietnam. PLoS ONE. (2012) 7:e41062. doi: 10.1371/journal.pone.0041062
47. Desta A, Biru TT, Kefale AT. Health related quality of life of people receiving highly active antiretroviral therapy in Southwest Ethiopia. PLoS ONE. (2020) 15:e0237013. doi: 10.1371/journal.pone.0237013
48. Yaya I, Djalogue L, Patassi AA, Landoh DE, Assindo A, Nambiema A, et al. Health-related quality of life among people living with HIV/AIDS in Togo: individuals and contextual effects. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4171-x
49. Van Duin MJ, Conde R, Wijnen B, Evers SM, Gonzalez-Rodriguez JL, Govers MJ, et al. The impact of comorbidities on costs, utilities and health-related quality of life among HIV patients in a clinical setting in Bogotá. Expert Rev Pharmacoecon Outcomes Res. (2017) 17:303–10. doi: 10.1080/14737167.2017.1246185
Keywords: HIV, health-related quality of life, Ghana, interventions, hypertension, diabetes, EQ-5D-5L
Citation: Owusu R, Kwarteng EB, Bawua SA, Otoo DD and Nonvignon J (2024) Health-related quality of life of HIV patients with comorbidities of hypertension or diabetes in Ghana. Front. Public Health 12:1383743. doi: 10.3389/fpubh.2024.1383743
Received: 07 February 2024; Accepted: 24 October 2024;
Published: 19 November 2024.
Edited by:
Chandan Kumar, TERI School of Advanced Studies (TERI SAS), IndiaReviewed by:
Julie Abimanyi-Ochom, Deakin University, AustraliaDaniel Edem Kpewou, University for Development Studies, Ghana
Copyright © 2024 Owusu, Kwarteng, Bawua, Otoo and Nonvignon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Richmond Owusu, cmlvd3VzdUB1Zy5lZHUuZ2g=
 Richmond Owusu
Richmond Owusu Emmanuel Bugyei Kwarteng1
Emmanuel Bugyei Kwarteng1 Serwaa Akoto Bawua
Serwaa Akoto Bawua Desmond Dzidzornu Otoo
Desmond Dzidzornu Otoo