- 1Dermatology Hospital, Southern Medical University, Guangzhou, China
- 2Institute for Global Health, Southern Medical University, Guangzhou, China
- 3School of Public Health, Southern Medical University, Guangzhou, China
Background: Seasonal influenza continues to pose a substantial public health challenge for older adults residing in rural areas worldwide. Vaccination remains the most efficacious means of preventing influenza. This study aimed to investigate the extent of influenza vaccine coverage and identify the factors influencing vaccine uptake among older adults in rural regions of south China.
Methods: A cross-sectional study utilizing convenience sampling was conducted in two rural sites in Guangdong Province. Individuals needed to meet specific inclusion criteria: (1) attainment of 60 years of age or older; (2) originating from rural households; (3) demonstrating a voluntary desire to partake in the survey, either through written or verbal informed consent. Data encompassed variables such as socio-demographic information, influenza infection and vaccination history, knowledge and attitudes toward influenza vaccination, and perceived beliefs regarding the influenza vaccine. Univariate and multivariable logistic regression analyses were employed to ascertain the factors associated with influenza vaccine utilization. In the multivariable model, adjustments were made for gender, age, legal marital status, highest educational attainment, and monthly income.
Results: A total of 423 participants were ultimately included in this study, with the majority falling within the age range of 60–75 years (81.3%). Only one-third of the participants had received an influenza vaccine in the past year (30.0%). Notably, nearly half of the older adults exhibited hesitancy toward influenza vaccination (45.1%). The multivariable analysis revealed that rural older people with a robust understanding of influenza vaccines and a positive attitude toward them (adjusted odds ratio [aOR] = 2.60, 95% confidence interval [CI]: 1.41–4.81), along with a high level of trust in vaccination service providers (aOR = 2.58, 95% CI: 1.01–6.63), were positively associated with receiving influenza vaccination in the past year.
Conclusion: This study reveals a low rate of influenza vaccine uptake among older adults residing in rural areas of south China. Given the limited adoption of influenza vaccination and the significant threat it poses, there is an urgent imperative to devise precise interventions aimed at enhancing the effectiveness of influenza vaccination programs.
Introduction
Seasonal influenza imposes a significant global health burden, annually resulting in a substantial toll of morbidity and mortality. Recent estimates indicate an alarming prevalence of severe illness, encompassing 3–5 million cases, alongside a staggering 290,000–650,000 annual respiratory-related fatalities (1). While influenza can affect individuals across all age groups, it is imperative to recognize that older adults, aged 60 and above, face a heightened susceptibility to hospitalization and mortality upon infection (2). This vulnerability stems from a weakened immune system compounded by the presence of chronic diseases (3). A study conducted in China, utilizing data from national influenza surveillance and cause-of-death surveillance, unveiled a disconcerting annual average of 88,100 excess deaths attributed to influenza-associated respiratory diseases during the seasons spanning from 2010–2011 to 2014–2015. Strikingly, older people accounted for a significant 80% of these fatalities (4).
Immunization is the paramount strategy for influenza prevention, substantially mitigating the risk of influenza-related hospitalization among older adults by an average of 40% (5). The World Health Organization (WHO) and the technical guidelines for influenza vaccination in China (2019–2020) both endorse prioritizing individuals aged 60 and above for influenza vaccination (6). Meanwhile, a review indicated that influenza vaccination in the old adult is also cost-effective from a societal perspective (7–9). Regrettably, influenza vaccine uptake in China remains distressingly low, standing at a mere 3.8%, in stark contrast to the United States (ranging from 59.6 to 75.2%) and Europe (35.5%) (10–12). Meanwhile, a study in Florida did not find an association between influenza vaccine use among rural and urban residence (13). Significantly, the influenza vaccine is not integrated into China’s national immunization program and is available only upon request, incurring out-of-pocket expenses for vaccination, typically around $21. Exceptions to this financial burden exist in the form of local government-subsidized influenza vaccine initiatives, which are limited to select metropolitan areas (14, 15). Consequently, accessibility to vaccines may be markedly restricted for older adults residing in remote or rural regions, particularly those who possess limited knowledge about influenza and are economically disadvantaged. Paying special attention to the older adults living in rural areas is of great significance to promote health equality. Although there were studies focused on the influenza vaccine coverage among older adults, most of them did research on the developed areas (such as Beijing, Shanghai, etc.) or only focused on urban populations and lacked the analysis of the overall status of the older adults in rural China (16–19).
In light of this knowledge gap, our study aimed to scrutinize the prevalence of influenza vaccine coverage and to elucidate the influencing factors that govern vaccination uptake among older adults inhabiting rural areas of south China.
Methods
Study sites
Guangdong, a subtropical province in southern China, serves as a vital hub for both domestic and international trade. With a population exceeding 120 million, the province faces year-round influenza prevalence. Guangdong is composed of 21 prefecture-level cities, each with distinct economic conditions and population profiles. At its center lies the Pearl River Delta, a cluster of nine highly developed cities that contribute 80% of the province’s gross domestic product. In contrast, the other 12 municipalities, which are less developed and resource-constrained, are spread across four cities in the east, four in the west, and four in the north.
Participants
A cross-sectional study was carried out in October 2023 at two rural sites, namely Yangcheng and Zhongluotan, both situated in Guangdong Province, China. Each site featured a single clinic that engaged in the recruitment of research participants. The choice of these clinics stemmed from their ample representation of older adults and medical personnel, including nurses and doctors, well-versed in influenza vaccination procedures. These clinics, serving as primary care facilities, catered to the healthcare needs of local residents, offering a spectrum of primary medical services. These services encompassed vaccinations, complimentary health check-ups for older people, and the dissemination of health-related information. The range of essential primary care services provided was consistent between the two clinics, encompassing the management of common medical conditions, chronic diseases, vaccination services, and other preventive public health initiatives. It is noteworthy that the majority of the study participants were regular visitors to these clinics.
To qualify for participation in the study, individuals needed to meet specific inclusion criteria: (1) attainment of 60 years of age or older; (2) originating from rural households; (3) demonstrating a voluntary desire to partake in the survey, either through written or verbal informed consent.
Data collection
Data collection for this study employed paper questionnaires, which were crafted in consultation with the study group, influenza vaccine experts, and personnel from the local Centers for Disease Control and Prevention (CDC). In order to ensure the survey’s validity, a pilot test was administered to 10 older adults to assess the questionnaire items. It is pertinent to note that the data obtained during the pilot phase were not integrated into the final analysis. Face-to-face survey interviews were administered by local medical staff or members of the research team to all eligible participants in the clinic setting. The survey required approximately 10 min to be completed in its entirety. It is imperative to emphasize that all survey data were treated with utmost anonymity and confidentiality, with written or verbal consent being procured prior to the initiation of the survey process. To express our gratitude for their participation, participants were provided with a moisturizing cream valued at 2 United States dollars upon concluding their involvement in the study.
Measurements
Social-demographic factors
The socio-demographic information gathered in this study included a range of variables such as age, gender, marital status, education, household size (including family members residing in the same home), and insurance status.
History of influenza infection and vaccination
The assessment of a participant’s history of influenza infection involved the use of two binary (yes/no) questions: ‘Have you experienced influenza or flu-like symptoms in the past year?’ and ‘Have you been hospitalized due to influenza or flu-like symptoms?’ The history of receiving the influenza vaccine was evaluated through the following question: ‘Did you receive the seasonal influenza vaccine in the previous year?’.
Knowledge and attitudes toward the influenza vaccine
The assessment of knowledge and attitudes toward the influenza vaccine involved the utilization of five items, each rated on a Likert-type scale ranging from 1 (completely agree) to 5 (completely disagree). These items covered areas related to the perceived importance, safety, and effectiveness of the vaccination. The total scores ranged from 5 to 25 with 3 categories: low (5–10), moderate (11–20), and high (21–25). The Cronbach’s α of knowledge and attitudes toward the influenza vaccine scale in this study was 0.869.
Perceived beliefs regarding the influenza vaccine
Participants’ perceived beliefs regarding the influenza vaccine encompassed several key aspects, namely their trust in healthcare providers’ guidance, self-perceived risk of infection, attitudes toward vaccination cost, and vaccine hesitancy.
Trust in healthcare providers’ advice was gauged through the employment of four items, self-perceived infection risk through four items, attitudes regarding vaccination cost through three items, and vaccine hesitancy through one item. Each of these items was rated on a Likert-type scale, spanning from 1 (completely agree/very hesitant) to 5 (completely disagree/not at all hesitant). All questionnaire items were adapted from a prior study on vaccine hesitancy among Chinese adults. Trust in healthcare providers’ advice ranged from 4 to 20 with 3 categories: low (4–12), moderate (13–15), and high (16–20). In a similar manner, self-perceived infection risk produced a total score ranging from 4 to 20, thus allowing for categorization as low (4–10), moderate (11–15), and high (16–20). Finally, attitudes toward vaccination costs generated a total score within the range of 3–15, with 3 categories: low (3–5), moderate (6–12), and high (13–15). The Cronbach’s α of trust in healthcare providers’ guidance scale was 0.877. The Cronbach’s α of self-perceived infection risk scale was 0.778. The Cronbach’s α of attitudes toward vaccination scale was 0.732.
Statistical analysis
A descriptive analysis was undertaken to furnish an overview of the sociodemographic attributes and the prevalence of influenza vaccine uptake. For comparing categorical variables, the χ2 test was employed. The differences in knowledge and attitudes between the subgroup of individuals who had received the influenza vaccine and those who had not in China were assessed using the t-test. To scrutinize the factors linked to the utilization of the influenza vaccine, univariate and multivariable logistic regression analyses were conducted. In the multivariable model, adjustments were made for gender, age, legal marital status, highest educational attainment, and monthly income. All data analyses were executed utilizing SAS 9.2 (SAS Institute Inc., Cary, NC).
Results
In its entirety, the survey encompassed 435 older individuals. Among this group, 9 participants were excluded due to being below 60 years of age, while 3 older people were ineligible for inclusion as they had not provided their consent. Consequently, a total of 423 (97.2%) participants were ultimately included in this study.
Sociodemographic characteristics
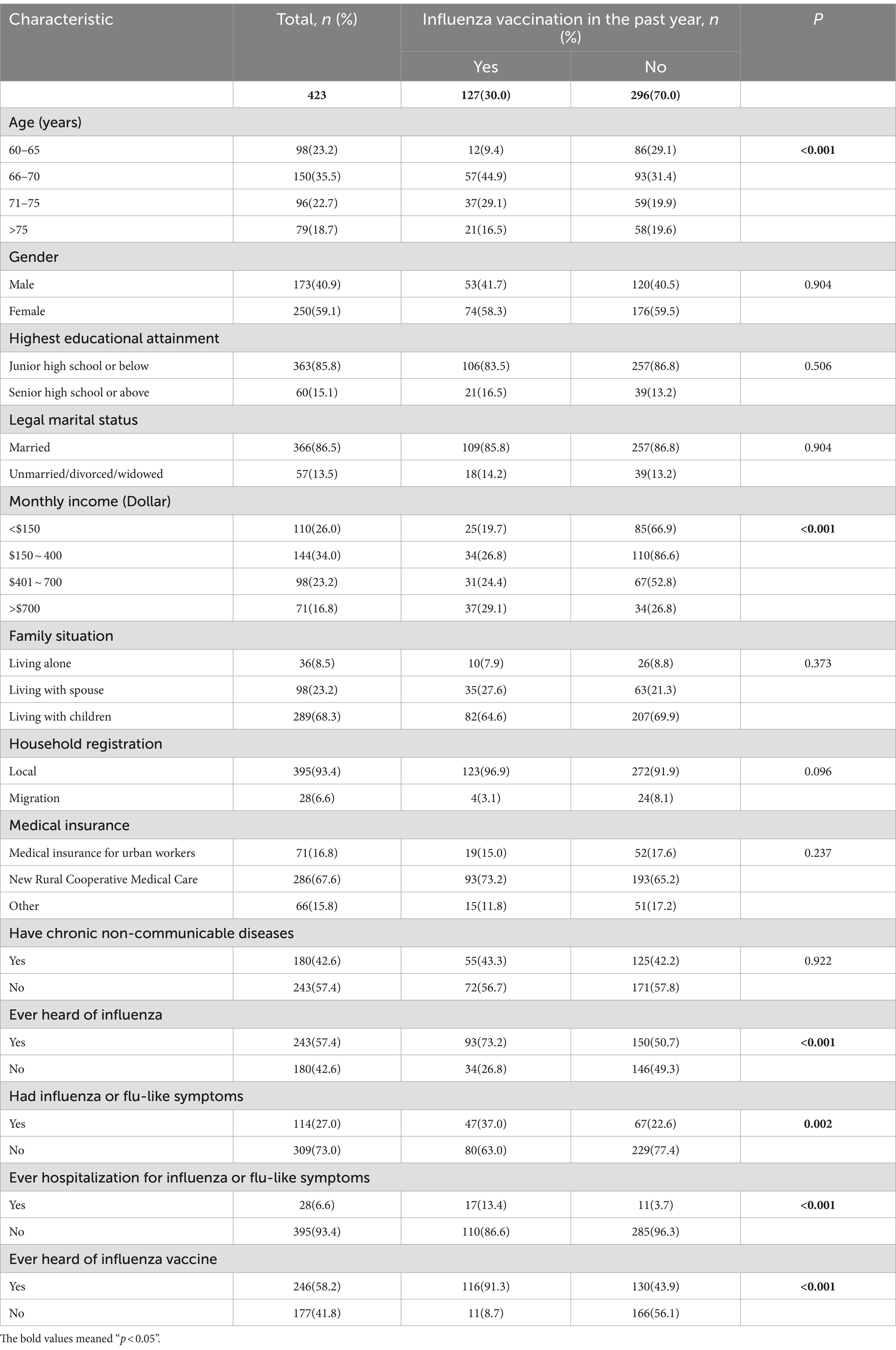
Among the 423 participants, the majority fell within the age range of 60–75 years (81.3%), were predominantly female (59.1%), married (86.5%), possessed an educational background of junior high school or below (85.8%), reported a monthly income of less than 700 US dollars (83.2%), resided with their children (68.3%), held local household registrations (93.4%), and nearly two-fifths of them had chronic non-communicable diseases (42.6%). Additionally, more than half of the participants had previous knowledge of influenza (57.4%), over one-fourth had experienced influenza or flu-like symptoms in the past year (27.0%), and less than one-tenth had a history of hospitalization due to influenza or flu-like symptoms (6.6%) (Table 1).
Vaccine characteristics
A mere one-third of the participants had received an influenza vaccine in the previous year (30.0%), while nearly half of the older adults exhibited hesitancy toward influenza vaccination (45.1%). Furthermore, more than half of the participants were already familiar with the concept of the influenza vaccine (58.2%). Additionally, a significant majority of the older population expressed willingness to accept free influenza vaccines donated by their peers (83.9%), as evidenced in Table 1.
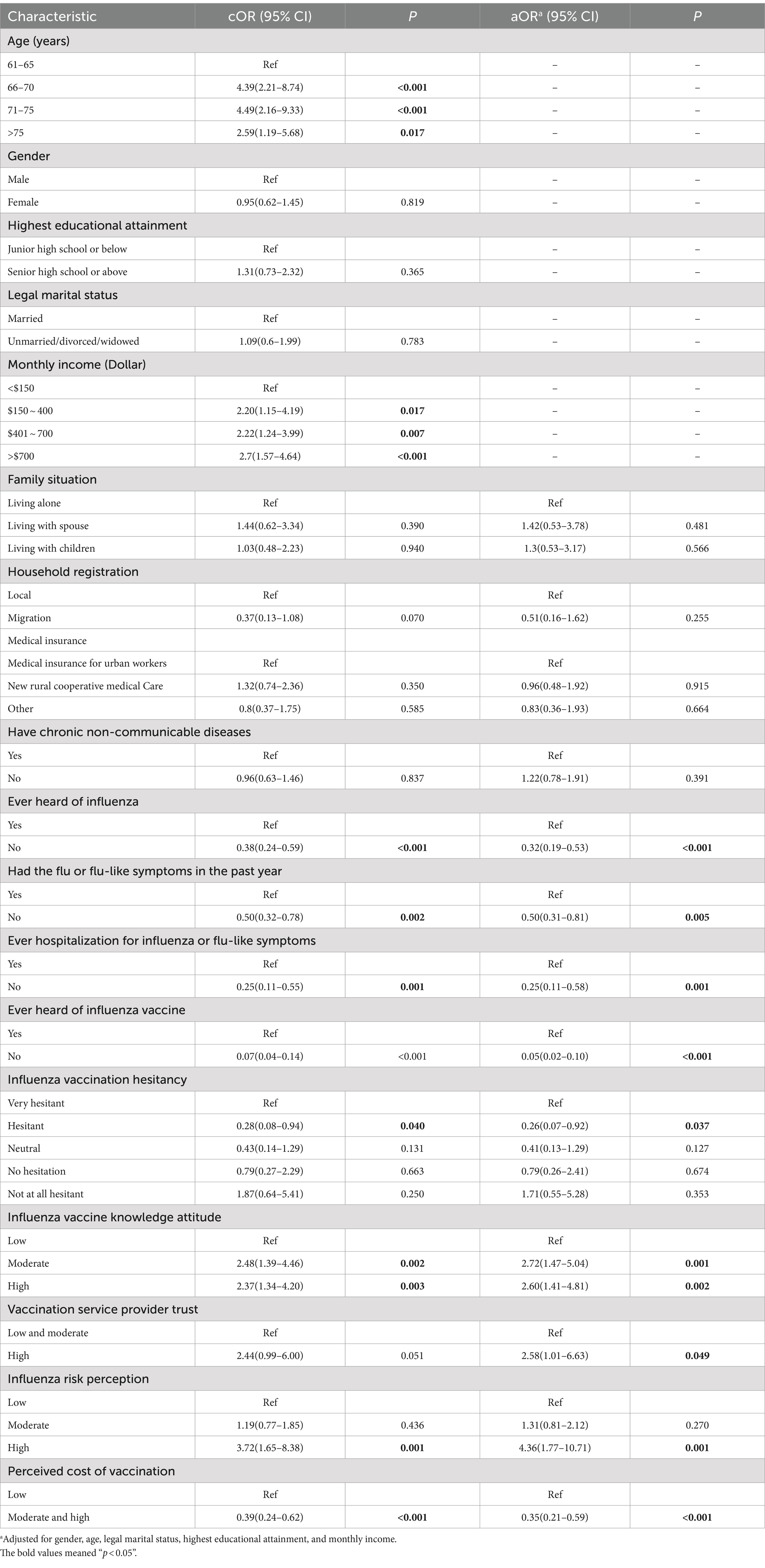
The analysis revealed that participants who had received an influenza vaccination in the past year were more likely to fall within the age bracket of 66 to 75 (41.6%), have a monthly income exceeding 700 dollars (52.1%), possess prior knowledge of influenza (38.3%), have experienced influenza or flu-like symptoms in the past year (41.2%), have a history of hospitalization due to influenza or flu-like symptoms (60.7%), possess knowledge of the influenza vaccine (47.2%), exhibit a high level of influenza vaccine knowledge and positive attitudes (38.5%), exhibit a high level of influenza risk (57.1%), perceive the cost of vaccination as low (46.9%), and have no hesitations whatsoever regarding influenza vaccination (50.5%). These associations were found to be statistically significant (p < 0.05), as elucidated in Tables 1, 2.
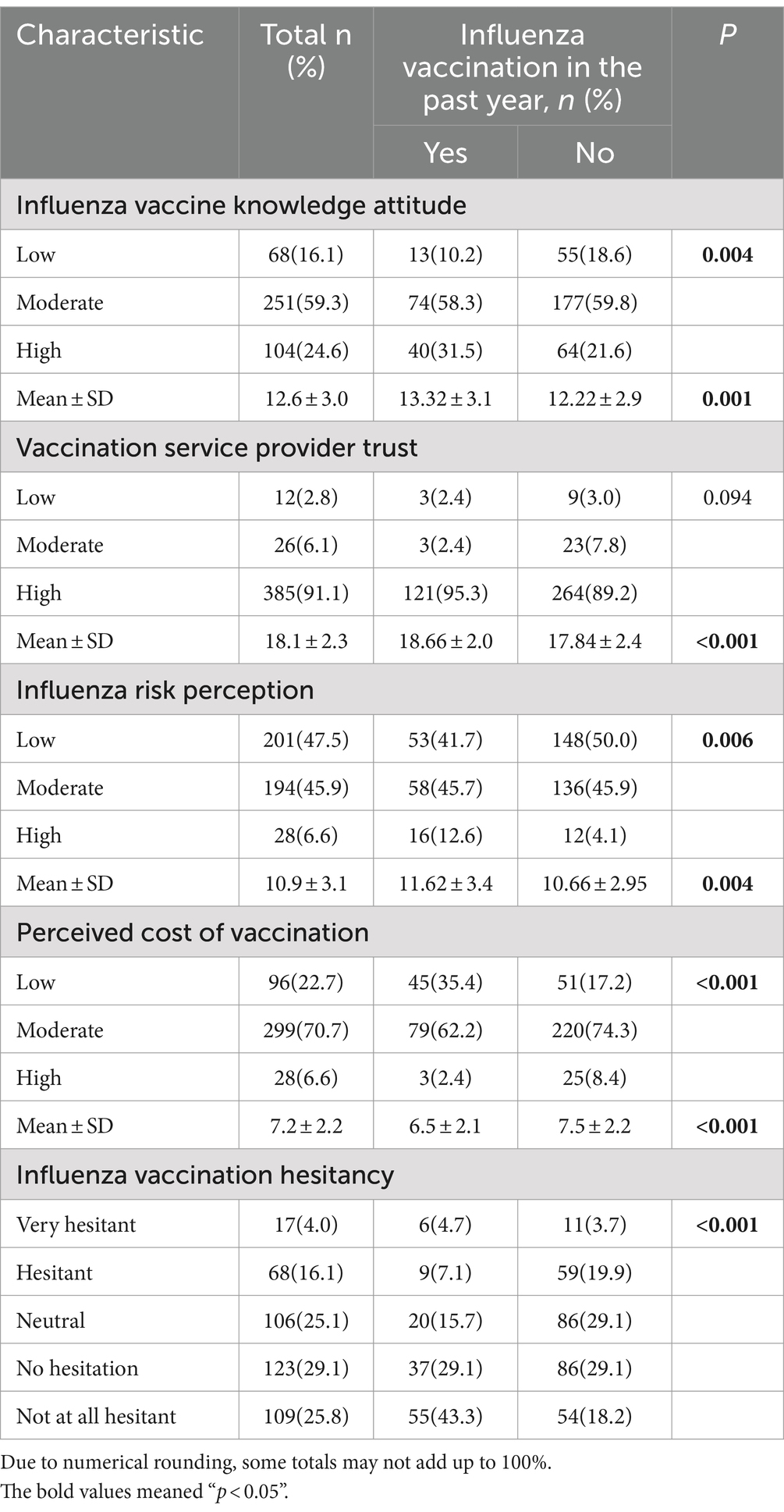
Table 2. Influenza vaccine knowledge, attitude, vaccination service provider trust, influenza risk perception, perceived cost of vaccination, and influenza vaccination hesitancy among Chinese older, 2023 (n = 423).
Factors correlated with receiving the influenza vaccine
In the multivariable model, adjusted for age, marital status, highest educational attainment, annual income, and gender, several factors were found to be significantly associated with influenza vaccination in the past year. Three factors demonstrated a positive correlation with influenza vaccination uptake: possessing high influenza vaccine knowledge and a positive attitude (adjusted odds ratio [aOR] = 2.60, 95% confidence interval [CI]: 1.41–4.81), having a high level of trust in vaccination service providers (aOR = 2.58, 95% CI: 1.01–6.63) and having a high level of influenza risk perception (aOR = 4.36, 95% CI: 1.77–10.71).
Conversely, five factors exhibited a negative correlation with influenza vaccination in the past year: never having heard of influenza (aOR = 0.32, 95% CI: 0.19–0.53), not experiencing flu-like symptoms in the past year (aOR = 0.50, 95% CI: 0.31–0.81), no history of hospitalization due to influenza or flu-like symptoms (aOR = 0.25, 95% CI: 0.11–0.58), never having heard of the influenza vaccine (aOR = 0.05, 95% CI: 0.02–0.10), and perceiving a high cost associated with vaccination (aOR = 0.35, 95% CI: 0.21–0.59). Refer to Table 3 for further details.
Discussion
Influenza remains a formidable global public health challenge. The most effective preventive measure against influenza is vaccination, with the older people being prioritized for such vaccination. Studies have indicated that influenza vaccination for the old adult is cost-effective (7–9). Our study reveals a notable deficiency in influenza vaccine coverage among older people in rural China. By focusing on this demographic, monitoring prevalence, and probing into the associated factors affecting vaccine coverage, our study contributes to the existing body of literature. The insights gleaned from this study hold the potential to bolster vaccination rates among the older people in China.
Our findings indicate a low rate of influenza vaccine uptake among rural older people in China, a trend that aligns with similar observations in previous Chinese studies, but is lower than vaccination rates in the United States and Canada (12, 20). However, the rate is higher than the COVID-19 vaccination rate in most high-income countries from a scoping review about COVID-19 vaccine hesitancy (21). Several factors may underlie this suboptimal vaccination rate. First and foremost, rural older people exhibit limited awareness of the influenza vaccine. Such low awareness, coupled with perceived disease risk, serves as a deterrent to vaccination. Additionally, older adults in rural areas of China encounter significant challenges in accessing influenza vaccination services, including geographic barriers, limited healthcare resources (22). Finally, the variation in vaccination programs and public health policy might contribute to the differences in vaccination rates. A review also clearly indicated gaps for evidence on system-based level or political strategies to improve vaccination uptake among older adults (23). Currently, only a few areas with budget surpluses in China are trying to integrate influenza vaccination into government financial subsidies or medical insurance reimbursement schemes, providing free vaccination for the older people. In contrast, in most regions, the older people must bear the cost of vaccination. Given the high cost-effectiveness of influenza vaccination for the old adult (7), developed countries such as the United States, the United Kingdom, and Australia have already incorporated influenza vaccination into national immunization programs, offering free vaccines to the older people (12, 24, 25). Considering the low coverage of influenza vaccination among the older people and the serious health threats posed by influenza, China urgently needs to devise effective strategies to promote vaccine uptake for older adults, such as expanding national immunization programs to include free vaccinations, establishing mobile vaccination units to reach older adults who have limited access to healthcare facilities in rural areas.
We found that approximately three-quarters of the rural older people exhibits a moderate and high level of perceived cost of vaccination. This may be primarily attributed to lower income levels among older people in rural areas (26). Our study found that approximately one-quarter of older people in rural areas have a monthly income below $150. However, previous studies and our findings have shown that older people with a higher level of perceived cost of vaccination are less likely to be vaccinated (26, 27). In the context of influenza vaccines being currently categorized as self-paid vaccines in China, many studies are exploring novel economic interventions to promote vaccine uptake among older people, such “pay it forward” initiatives (16, 28, 29), offering financial or social incentives to encourage older adults to get vaccinated and local free government influenza vaccination policy. Additionally, previous studies also suggest that launching public awareness campaigns to highlight the long-term cost benefits of flu vaccination, emphasizing potential savings on medical expenses, sick days, and productivity losses, can mitigate perceived cost risks associated with vaccination (30, 31). Hence, developing national-level public health campaigns to raise awareness about the benefits of influenza vaccination is necessary for older populations who are at higher risk of complications.
We found a low level of knowledge, attitude, and risk perception regarding influenza vaccine among older people, only one quarter of the older people possesses a high level of knowledge, attitude, and risk perception. We also found that older people with heightened knowledge and a greater perception of the risk associated with flu vaccines exhibit higher vaccination rates, which was consistent with other studies (32, 33). This finding was also similar with other studies about COVID-19, SARS and MERS pandemics (34). This phenomenon is primarily attributable to the fact that increased knowledge and heightened risk perception empower individuals to make proactive decisions to protect themselves and their communities against influenza, consequently leading to increased vaccination rates. Given the low level of influenza vaccine knowledge, it is imperative to initiate public health campaigns aimed at educating the older people on the significance of vaccinations and the potential risks associated with abstaining from vaccination. A combination of traditional and digital media channels, including television, radio, newspapers, social media, and online platforms, can be leveraged to reach a wide-ranging audience. Collaborations with local healthcare providers, community leaders, and influential figures can further facilitate the dissemination of information regarding vaccination’s importance (35).
It is important to acknowledge the limitations of our study. First, the data regarding influenza vaccine uptake were gathered via voluntary self-reporting, introducing the potential for information bias. Second, as this was a cross-sectional study, the observed correlations between influenza vaccine uptake and knowledge and attitudes should be interpreted as associations rather than causation. Third, while our study examined older adults in rural areas, the findings may not necessarily extrapolate to older adults in urban settings in China or those residing outside of China.
Conclusion
In this study, we found a low influenza vaccine uptake among older people residing in rural China. Notably, influenza vaccine utilization is positively associated with factors such as knowledge about influenza, positive attitudes toward vaccination, and an increased perception of the risks associated with the influenza virus. In light of the suboptimal vaccination rate and the considerable health risks posed by influenza, it is crucial to devise targeted interventions aimed at augmenting influenza vaccine coverage.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Dermatology Hospital of Southern Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
PZ: Conceptualization, Writing – original draft. WX: Writing – original draft. JW: Data curation, Writing – review & editing. PL: Writing – review & editing. HL: Writing – review & editing. CW: Conceptualization, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This publication was supported by Medical Scientific Research Foundation of Guangdong Province (B2022139).
Acknowledgments
We are very grateful to all the participants who participated in this study. We wish to acknowledge Yangcheng Town Health Service Center and Zhongluotan Town Health Service Center.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
WHO, World Health Organization; CDC, Centers for Disease Control and Prevention; aOR, Adjusted odds ratio; CI, Confidence interval.
References
1. Iuliano, AD, Roguski, KM, Chang, HH, Muscatello, DJ, Palekar, R, Tempia, S, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet. (2018) 391:1285–300. doi: 10.1016/S0140-6736(17)33293-2
2. Tanner, AR, Dorey, RB, Brendish, NJ, and Clark, TW. Influenza vaccination: protecting the most vulnerable. Eur Respir Rev. (2021) 30:200258. doi: 10.1183/16000617.0258-2020
3. Bartoszko, J, and Loeb, M. The burden of influenza in older adults: meeting the challenge. Aging Clin Exp Res. (2021) 33:711–7. doi: 10.1007/s40520-019-01279-3
4. Li, L, Liu, Y, Wu, P, Peng, Z, Wang, X, Chen, T, et al. Influenza-associated excess respiratory mortality in China, 2010–15: a population-based study. Lancet Public Health. (2019) 4:e473–81. doi: 10.1016/S2468-2667(19)30163-X
5. Rondy, M, el Omeiri, N, Thompson, MG, Levêque, A, Moren, A, and Sullivan, SG. Effectiveness of influenza vaccines in preventing severe influenza illness among adults: a systematic review and meta-analysis of test-negative design case-control studies. J Infect. (2017) 75:381–94. doi: 10.1016/j.jinf.2017.09.010
6. World Health Organization. Vaccines against influenza WHO position paper—November 2012. Weekly Epidemiol Rec. (2012) 87:461–76.
7. Dilokthornsakul, P, Lan, LM, Thakkinstian, A, Hutubessy, R, Lambach, P, and Chaiyakunapruk, N. Economic evaluation of seasonal influenza vaccination in elderly and health workers: a systematic review and meta-analysis. EClinicalMedicine. (2022) 47:101410. doi: 10.1016/j.eclinm.2022.101410
8. Newall, AT, Kelly, H, Harsley, S, and Scuffham, PA. Cost effectiveness of influenza vaccination in older adults: a critical review of economic evaluations for the 50-to 64-year age group. PharmacoEconomics. (2009) 27:439–50. doi: 10.2165/00019053-200927060-00001
9. Ting, EEK, Sander, B, and Ungar, WJ. Systematic review of the cost-effectiveness of influenza immunization programs. Vaccine. (2017) 35:1828–43. doi: 10.1016/j.vaccine.2017.02.044
10. Zhou, L, Su, Q, Xu, Z, Feng, A, Jin, H, Wang, S, et al. Seasonal influenza vaccination coverage rate of target groups in selected cities and provinces in China by season (2009/10 to 2011/12). PLoS One. (2013) 8:e73724. doi: 10.1371/journal.pone.0073724
11. Blank, PR, van Essen, GA, Ortiz de Lejarazu, R, Kyncl, J, Nitsch-Osuch, A, Kuchar, EP, et al. Impact of European vaccination policies on seasonal influenza vaccination coverage rates: an update seven years later. Hum Vaccin Immunother. (2018) 14:1–9. doi: 10.1080/21645515.2018.1489948
12. Centres for Disease Control and Prevention. Flu vaccination coverage, United States, 2021–22 influenza season. (2022). [cited 2023 September]; Available at https://www.cdc.gov/flu/fluvaxview/coverage-2022estimates.htm. (Accessed February 07, 2024).
13. Alalwan, AA. Influenza vaccine utilization: a comparison between urban and rural counties in Florida. Vaccine. (2022) 10:669. doi: 10.3390/vaccines10050669
14. Zheng, J, Zhou, Y, Wang, H, and Liang, X. The role of the China experts advisory committee on immunization program. Vaccine. (2010) 28:A84–7. doi: 10.1016/j.vaccine.2010.02.039
15. Yang, J, Atkins, KE, Feng, L, Pang, M, Zheng, Y, Liu, X, et al. Seasonal influenza vaccination in China: landscape of diverse regional reimbursement policy, and budget impact analysis. Vaccine. (2016) 34:5724–35. doi: 10.1016/j.vaccine.2016.10.013
16. Li, T, Lv, M, Lei, T, Wu, J, Pang, X, Deng, Y, et al. Who benefits most from influenza vaccination policy: a study among the elderly in Beijing, China. Int J Equity Health. (2016) 15:1–7. doi: 10.1186/s12939-016-0332-x
17. Zhang, D, Zhang, Y, Wang, Q, Lock, J, Pan, Y, Cui, S, et al. The effectiveness of influenza vaccination in preventing hospitalizations in elderly in Beijing, 2016–18. Vaccine. (2019) 37:1853–8. doi: 10.1016/j.vaccine.2019.02.013
18. Wu, S, Su, J, Yang, P, Zhang, H, Li, H, Chu, Y, et al. Factors associated with the uptake of seasonal influenza vaccination in older and younger adults: a large, population-based survey in Beijing, China. BMJ Open. (2017) 7:e017459. doi: 10.1136/bmjopen-2017-017459
19. Yan, S, Wang, Y, Zhu, W, Zhang, L, Gu, H, Liu, D, et al. Barriers to influenza vaccination among different populations in Shanghai. Hum Vaccin Immunother. (2021) 17:1403–11. doi: 10.1080/21645515.2020.1826250
20. Government of Canada. Seasonal influenza vaccination coverage in Canada, 2021–22. (2022) [cited 2023 November]; Available at: https://www.canada.ca/en/public-health/services/immunization-vaccines/vaccination-coverage/seasonal-influenza-survey-results-2021-2022/full-report.html (Accessed February 07, 2024).
21. Aw, J, Seng, JJB, Seah, SSY, and Low, LL. COVID-19 vaccine hesitancy—a scoping review of literature in high-income countries. Vaccine. (2021) 9:900. doi: 10.3390/vaccines9080900
22. Okoli, GN, Lam, OLT, Racovitan, F, Reddy, VK, Righolt, CH, Neilson, C, et al. Seasonal influenza vaccination in older people: a systematic review and meta-analysis of the determining factors. PLoS One. (2020) 15:e0234702. doi: 10.1371/journal.pone.0234702
23. Roller-Wirnsberger, R, Lindner, S, Kolosovski, L, Platzer, E, Dovjak, P, Flick, H, et al. The role of health determinants in the influenza vaccination uptake among older adults (65+): a scope review. Aging Clin Exp Res. (2021) 33:2123–32. doi: 10.1007/s40520-021-01793-3
24. European Centre for Disease Prevention and Control. seasonal influenza vaccination in Europe: Vaccination recommendations and coverage rates in the EU member states for eight influenza seasons 2007–2008 to 2014–2015. (2017) [cited 2023 September]. Available at: https://data.europa.eu/doi/. (Accessed February 07, 2024).
25. Trent, MJ, Salmon, DA, and MacIntyre, CR. Using the health belief model to identify barriers to seasonal influenza vaccination among Australian adults in 2019. Influenza Other Respir Viruses. (2021) 15:678–87. doi: 10.1111/irv.12843
26. Li, Q, Zhang, M, Chen, H, Wu, F, Xian, J, Zheng, L, et al. Influenza vaccination coverage among older adults with hypertension in Shenzhen, China: a cross-sectional survey during the COVID-19 pandemic. Vaccine. (2021) 9:1105. doi: 10.3390/vaccines9101105
27. Qin, C, Yan, W, Tao, L, Liu, M, and Liu, J. The association between risk perception and hesitancy toward the booster dose of COVID-19 vaccine among people aged 60 years and older in China. Vaccine. (2022) 10:1112. doi: 10.3390/vaccines10071112
28. Wu, D, Jin, C, Bessame, K, Tang, FFY, Ong, JJ, Wang, Z, et al. Effectiveness of a pay-it-forward intervention compared with user-paid vaccination to improve influenza vaccine uptake and community engagement among children and older adults in China: a quasi-experimental pragmatic trial. Lancet Infect Dis. (2022) 22:1484–92. doi: 10.1016/S1473-3099(22)00346-2
29. Yue, M, Wang, Y, Low, CK, Yoong, JSY, and Cook, AR. Optimal design of population-level financial incentives of influenza vaccination for the elderly. Value Health. (2020) 23:200–8. doi: 10.1016/j.jval.2019.08.006
30. Colombo, GL, Ferro, A, Vinci, M, Zordan, M, and Serra, G. Cost-benefit analysis of influenza vaccination in a public healthcare unit. Ther Clin Risk Manag. (2006) 2:219–26. doi: 10.2147/tcrm.2006.2.2.219
31. Centres for Disease Control and Prevention. New wild to mild campaign drives key message to tame flu and reset expectations. (2023). [cited 2023 November]; Available at: https://www.cdc.gov/flu/spotlights/2023-2024/new-campaign-wild-to-mild.htm (Accessed February 07, 2024).
32. Wei, Z, Sun, X, Yang, Y, Zhan, S, and Fu, C. Seasonal influenza vaccine hesitancy profiles and determinants among Chinese children’s guardians and the elderly. Expert Rev Vaccines. (2021) 20:601–10. doi: 10.1080/14760584.2021.1908134
33. Hou, Z, Guo, J, Lai, X, Zhang, H, Wang, J, Hu, S, et al. Influenza vaccination hesitancy and its determinants among elderly in China: a national cross-sectional study. Vaccine. (2022) 40:4806–15. doi: 10.1016/j.vaccine.2022.06.063
34. Seng, Jun Jie Benjamin, Yeam, ChengTeng, Huang, CalebWeihao, Tan, NgiapChuan, and Low, LianLeng, Pandemic-related health literacy: a systematic review of literature in COVID-19, SARS and MERS pandemics. Singapore Med J, (2023). [Epubh ahead of preprint]. doi: 10.4103/singaporemedj.SMJ-2021-026
Keywords: influenza vaccine, aged, rural population, factor, China
Citation: Zhao P, Xu W, Wang J, Liang P, Li H and Wang C (2024) Uptake and correlates of influenza vaccine among older adults residing in rural regions of south China: a cross-sectional study. Front. Public Health. 12:1383293. doi: 10.3389/fpubh.2024.1383293
Edited by:
Graça S. Carvalho, University of Minho, PortugalReviewed by:
Luminița-Smaranda Iancu, Grigore T. Popa University of Medicine and Pharmacy, RomaniaJun Jie Benjamin Seng, Ministry of Health, Singapore
Copyright © 2024 Zhao, Xu, Wang, Liang, Li and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng Wang, wangcheng090705@gmail.com
†These authors have contributed equally to this work
 Peizhen Zhao
Peizhen Zhao Wenqian Xu
Wenqian Xu Jinshen Wang
Jinshen Wang Peng Liang1,3
Peng Liang1,3 Cheng Wang
Cheng Wang