- 1Department of Epidemiology, The University of Texas MD Anderson Cancer Center, Houston, TX, United States
- 2Division of Cancer Prevention and Population Sciences, The University of Texas MD Anderson Cancer Center, Houston, TX, United States
- 3Department of Biostatistics, The University of Texas MD Anderson Cancer Center, Houston, TX, United States
Introduction: Evidence suggests that advice from health care professionals (HCP) increases the likelihood of quit attempts and successful quitting of tobacco use. However, previous studies primarily focussed on cigarette smoking and did not include all forms of tobacco products. This study aimed to investigate the prevalence and disparities in receiving HCP’s advice to quit tobacco use (combustible or noncombustible) in the US adult population.
Methods: Using the 2022 National Health Information Survey (NHIS) data, we examined 4,424 adults who reported (i) any tobacco product use within the past 12 months and (ii) having seen an HCP within the past 12 months. The outcome variable included the receipt of advice to quit tobacco use from an HCP, and predictors included sociodemographic variables. Weighted prevalence estimates were calculated, and multivariable regression analyses were conducted.
Results: Over 38% of tobacco users who visited an HCP were advised to quit. The odds of receiving such advice were lower among Hispanics (AOR: 0.625; 95% confidence interval (CI) [0.464–0.843];p = 0.002), males (AOR: 0.767; 95% CI [0.659–0.893], p = 0.001), those above the poverty level (AOR: 0.795; 95% CI [0.641–0.987];p = 0.037), foreign-born (AOR: 0.664; 95% CI [0.496–0.888]; p = 0.006), those with a bachelor’s degree or higher educational level (AOR: 0.477; 95% CI [0.349–0.653]; p < 0.001) and those aged less than 45 years (AOR: 0.404; 95% CI: [0.344–0.473]; p < 0.001).
Conclusion: The prevalence of receiving HCP’s advice to quit tobacco use remains suboptimal and disparate among sociodemographic groups. Our findings call for strategic implementation of the USPHS’s recommendation on treating tobacco use and taking further actions to equip HCPs with the training and resources needed to provide appropriate advice to quit tobacco.
1 Introduction
Tobacco use is a significant risk factor for several health conditions, such as cancer, cardiovascular disorders, chronic obstructive pulmonary diseases, and oral diseases (1–3). Commercial tobacco can be smoked as cigarettes, e-cigarettes, cigars, cigarillos, little filtered cigars, pipes, hookahs, etc.; consumed smokeless as snuff, loose leaf chewing tobacco, lozenges, etc. (4); or can be used in combination (poly use) (5–7). Despite its public health impact, tobacco use remains a serious health concern. In 2021, it was estimated that nearly 1 in 5 US adults (18.7%) were using any commercial tobacco product (5). Although the prevalence of cigarette smoking (which has been the primary target of most smoking cessation interventions so far) has decreased in the last decade in the US [from 18.0% in 2012 (8) to 11.5% in 2021 (5)], the use of other tobacco products (electronic cigarettes, cigars, cigarillos, little filtered cigars, pipes, and smokeless tobacco) has increased [from 7.3% in 2012 (8) to 11.0% in 2021 (5)].
In 2020, over half (53.9%) of US adults who smoked attempted to quit smoking, and only 8.5% were successful (9). Evidence suggests that advice from healthcare professionals (HCPs) increased the likelihood of quit attempts and successful quitting of tobacco use. Kastaun and colleagues found that patients who received advice from HCPs to quit smoking had 2-fold higher odds of quit attempts and also reported 2.22-fold higher odds of point prevalence abstinence at 26 weeks follow-up than those who did not receive such advice (10). In a systematic review of 42 trials, Stead and colleagues found that even brief advice from HCPs would likely increase quit smoking rates (11). In addition to doctors and other health professionals, tobacco cessation in oral health settings is effective and feasible (3). Yadav and colleagues found that individuals who received smoking cessation advice from a dental care professional reported 18% more quit attempts (12). In a systematic review, Holliday and colleagues found that brief advice from dental professionals increased quit rates for all tobacco use (13). Therefore, to increase tobacco use cessation rate, the United States Public Health Service (USPHS) clinical practice guidelines recommended that HCPs should use the 5A’s model (ask, advise, assess, assist, and arrange) to ask for tobacco use at every visit; advise to quit; assess willingness to quit; assist patients who are willing to make a quit attempt with counseling and pharmacotherapy; and arrange follow-up within the first week after the quit date (14). In the US, more than 80% of adults reported visiting an HCP, and more than 60% reported visiting a dentist at least once a year (15), which represents a unique opportunity for HCPs and dentists to ask about tobacco use and advise them to quit its use.
Previous studies have reported a 57.2% prevalence of medical advice to quit cigarette smoking, and sociodemographic characteristics such as Hispanic, younger age, male, and uninsured were found to be associated with a lower likelihood of receiving medical advice to quit smoking (10, 11, 16, 17). Furthermore, immigrants constitute 13.9% (18) of the US population and often experience challenges in receiving healthcare services due to cultural, social, and economic barriers (19–22). There is limited information on the prevalence of the receipt of medical advice to quit tobacco among immigrants in the US.
Although cigarette use has gradually decreased (5, 23), the emergence of a diverse landscape of combustible and noncombustible tobacco products and the observed increase in the consumption of these products (5, 8) may counterbalance the health, social, and economic benefits expected from the reduction of cigarette smoking. Therefore, it is essential to have a holistic approach in rendering medical advice to quit tobacco use. However, previous reports (10, 11, 16, 17, 24) have focused only on receiving advice to quit cigarette smoking, but not all forms of tobacco products. Furthermore, none of the previous reports included dentists as a source of medical advice to quit tobacco use (10, 11, 16, 17, 24).
To address these gaps, our study aimed to (1) investigate the prevalence of receiving advice to quit any form of tobacco products (cigarettes, e-cigarettes, cigars, cigarillos, little filtered cigars, pipes, and smokeless tobacco) from HCPs and dentists, and (2) examine disparities associated with receiving such advice among US adult tobacco users.
2 Methods
2.1 Study population and data collection
This was a cross-sectional study based on the data from NHIS 2022 (25), which collects health behavior and demographic information of US households every year. NHIS used a geographically clustered multistage sampling technique to select a sample of dwelling units. The data were collected between January 2022 and December 2022 using a computer-assisted face-to-face survey of adult household members in the non-institutionalized civilian population residing in the United States (26). Our study followed Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. Respondents to NHIS 2022 provided written informed consent, and the research ethics review board of the National Center for Health Statistics approved the survey (26). Our study was exempt from ethical approval since it was a secondary data analysis of publicly available and de-identified data.
In the NHIS 2022 survey, adults were asked questions about their visits to an HCP and tobacco use behavior in the past 12 months, which were the criteria used to determine our study population.
2.1.1 HCP visit
The visit to an HCP was measured using the questions: (1) “About how long has it been since you last saw a doctor or other health professional about your health?” and (2) “About how long has it been since you last had a dental examination or cleaning?” The response options for questions (1) and (2) were “Never,” “Within past year [anytime less than 12 months ago],” “Within last two years [1 year but less than 2 years ago],” “Within the last 3 years [2 years but less than 3 years ago],” “Within the last 5 years [3 years but less than 5 years ago],” “Within the last 10 years [5 years but less than 10 years ago],” and “10 years ago or more.”. Those who responded “Within past year [anytime less than 12 months ago]” to either (1) or (2) were included in this study.
2.1.2 Tobacco use
According to the NHIS report, “tobacco” refers to commercial tobacco products and not to tobacco used for medicinal and spiritual purposes by some American Indian communities (5). Thus, five tobacco products were assessed in this study: cigarettes, cigars (cigars, cigarillos, or little filtered cigars), pipes (regular pipes, water pipes, or hookahs), e-cigarettes, and smokeless tobacco. To determine tobacco use in the past 12 months, we used the following questions: (1) “Do you NOW smoke cigarettes every day, some days, or not at all?”; (2) “Do you NOW use e-cigarettes or other electronic vaping products every day, some days, or not at all?” (3) “Do you NOW smoke regular cigars, cigarillos, or little filtered cigars every day, some days, or not at all? (4) “Do you NOW smoke pipes filled with tobacco - either regular pipes, water pipes, or hookahs, every day, some days, or not at all?” (5) “Do you NOW use smokeless tobacco products every day, some days, or not at all?” The response options were “Every day,” “Some days,” and “Not at all.” Those who responded “Everyday” and “Somedays” to questions (1–5) were included in the study population. Those who responded “not at all” to question (1) were asked, “Enter time period for time since quit smoking.” The response was reported as either the number of “days,” “months,” or “years.” Those who responded >365 days, >52 weeks, >12 months, or > 1 year were excluded from the study. Therefore, our study sample consisted of 4,424 adults who reported using tobacco in the past 12 months and visiting an HCP in the past 12 months.
2.2 Measures
2.2.1 Study outcome
The dependent variable, medical advice to quit tobacco use, was measured using the survey questions, “In the past 12 months, has a medical doctor, dentist, or other health professional ADVISED you to quit smoking or to quit using other kinds of tobacco?” The response to this question was either “yes” or “no.”
2.2.2 Predictors
Selected predictors are included in Table 1. Age (recoded as <45 years/≥45 years) was chosen as a predictor because cancer risks increase after 45 due to life experiences and exposure to social and behavioral risk factors (27). Moreover, age was found to be significant in association with medical advice on quitting tobacco use in previous studies (16, 17, 24). We used sex (coded as female/male), ethnicity and race (coded as Non-Hispanic White/Non-Hispanic Black/Hispanic/Multiple/others), educational level (coded as high school or GED/less than high school/some college/bachelor’s or higher), poverty level (recoded as Below poverty level/Above poverty level), and insurance coverage (coded as covered/not covered) as predictors because they were found significant in previous studies (16, 17). The prevalence of tobacco use and quitting varies by urbanicity. Rural areas have a higher prevalence of the use of different types of tobacco products than urban areas (28, 29). However, individuals living in non-metropolitan areas were found to be less likely to receive medical advice for quitting cigarette smoking (16). Therefore, we used urbanicity (recoded as metropolitan/non-metropolitan) as a geographic predictor for our study. Furthermore, US immigrants experience challenges in healthcare service utilization due to language barriers and lack of preventive care practices (19–22). Therefore, we used place of birth (recoded as Foreign-born/US-born) as another predictor to investigate if individuals with foreign-born status experience differential outcomes in receiving medical advice to quit tobacco use.

Table 1. Characteristics of the adults who used tobacco products in the past 12 months in the study population stratified by the receipt of medical advice to quit tobacco usea by healthcare providers- National Household Information Survey, 2022.
2.3 Statistical analysis
Statistical analyses were conducted, incorporating sampling weights to account for two components of the NHIS surveys: that only a subset of the US population is selected to participate in the survey and non-response of the selected participants. The final weights are calculated in several steps: (1) each sampled individual receives a base weight, which is the inverse of the probability of being selected in the survey sample. In this initial step, households and persons within households that are more likely to be selected to participate in the survey receive lower weights. (2) Base weights are then adjusted for non-response, which can impact the representativeness of the sample. The non-response accounted weights are calibrated using iterative proportional raking, utilizing raking dimensions such as age stratified by sex, age in conjunction with race/ethnicity, levels of educational attainment, and geographical regions delineated by metropolitan statistical areas. The weighting approach ensures that the survey data is representative of the demographic distribution of the US population (30). We used weighted survey logistic regression to examine the association between medical advice to quit and several sociodemographic factors. Statistical analyses were performed using the R statistical software (Version 4.3.1), specifically utilizing the “survey” package to analyze survey data. A survey-weighted variance inflation factor greater than 10 was used as a criterion to establish any multicollinearity.
3 Results
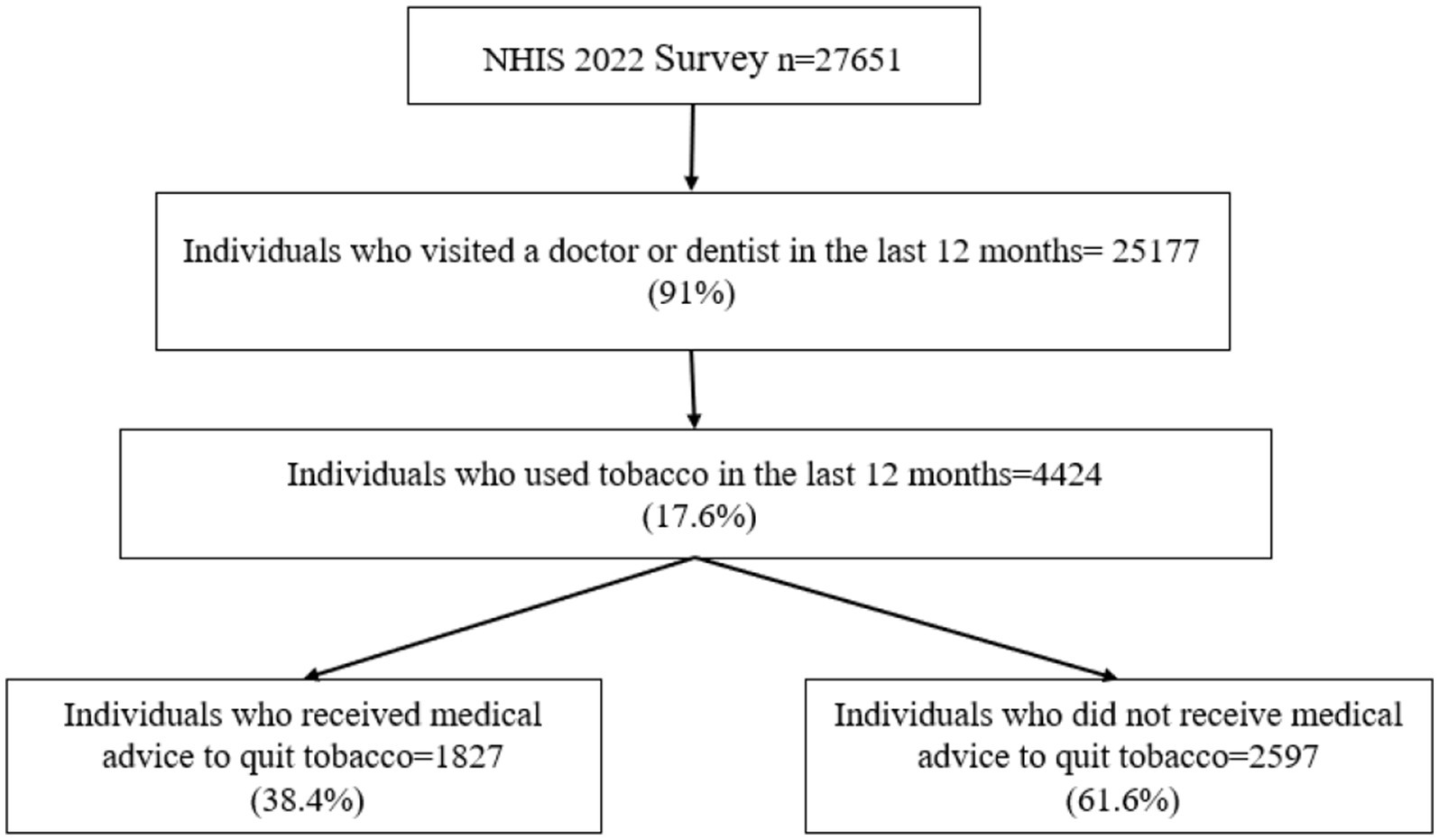
The NHIS 2022 dataset included 27,651 adult individuals, 91% of whom visited an HCP in the last 12 months. After screening for HCP visits and tobacco use in the past 12 months, the study sample included 4,424 individuals (Figure 1).
3.1 Characteristics of the study population
Over 70% of the study sample were Non-Hispanic White, 41.7% were females, 14% had a household income below the poverty level, 9.6% were foreign-born, 49.7% were younger than 45 years, 10.3% were individuals with less than a high school level of education, 9.5% had no health insurance coverage, and 19.3% were living in the non-metropolitan areas.
3.2 Prevalence of receiving HCP’s advice to quit tobacco
Overall, 38.4% (95% confidence interval [CI]: 36.7–40.1) of adult tobacco users received medical advice to quit. About 26% (95% CI: 21.1–31.2) of Hispanics, 35% (95% CI: 32.8–37.3) of males, 44.9% (95% CI: 40.2–49.6) of individuals living in households below the poverty level, 26% (95% CI: 21.4–31.1) of foreign-born, 27.1% (95% CI: 24.8–29.6) of individuals aged below 45 years, 27.8% [24.7–31.2] of individuals with education level of bachelor’s degree or higher, and 27.0% (95% CI: 21.8–33.0) of individuals without health insurance coverage received medical advice to quit tobacco use (Table 1).
3.3 Sociodemographic factors associated with receipt of advice to quit tobacco by HCPs
Using weighted survey logistic regression (Table 2), we found that Hispanics had 37.5% lower odds (AOR: 0.625, 95% CI: 0.464–0.843; p = 0.002) of receiving medical advice than Non-Hispanic White. Males had 23.3% lower odds (AOR: 0.767, 95% CI: 0.659–0.893, p = 0.001) of receiving medical advice to quit tobacco use than females. The odds of receiving medical advice among individuals living above the poverty level were 19.5% (AOR: 0.795, 95% CI: 0.641–0.987, p = 0.037) lower than those living below the poverty level. Foreign-born individuals had 33.6% lower odds (AOR: 0.664, 95% CI: 0.496–0.888, p = 0.006) of receiving HCPs’ advice to quit tobacco use than US-born individuals. Those younger than 45 years had 59.6% lower odds of receiving medical advice to quit tobacco use (AOR: 0.404, 95% CI: 0.344–0.473, p < 0.001) compared to individuals 45 years or older. Individuals with a bachelor’s degree or higher educational level had 52.3% lower odds (AOR: 0.477, 95% CI: 0.349–0.653; p < 0.001) of receiving medical advice to quit tobacco use than those with less than high school. The association of urbanicity and health insurance coverage with receiving medical advice for quitting was found statistically not significant.
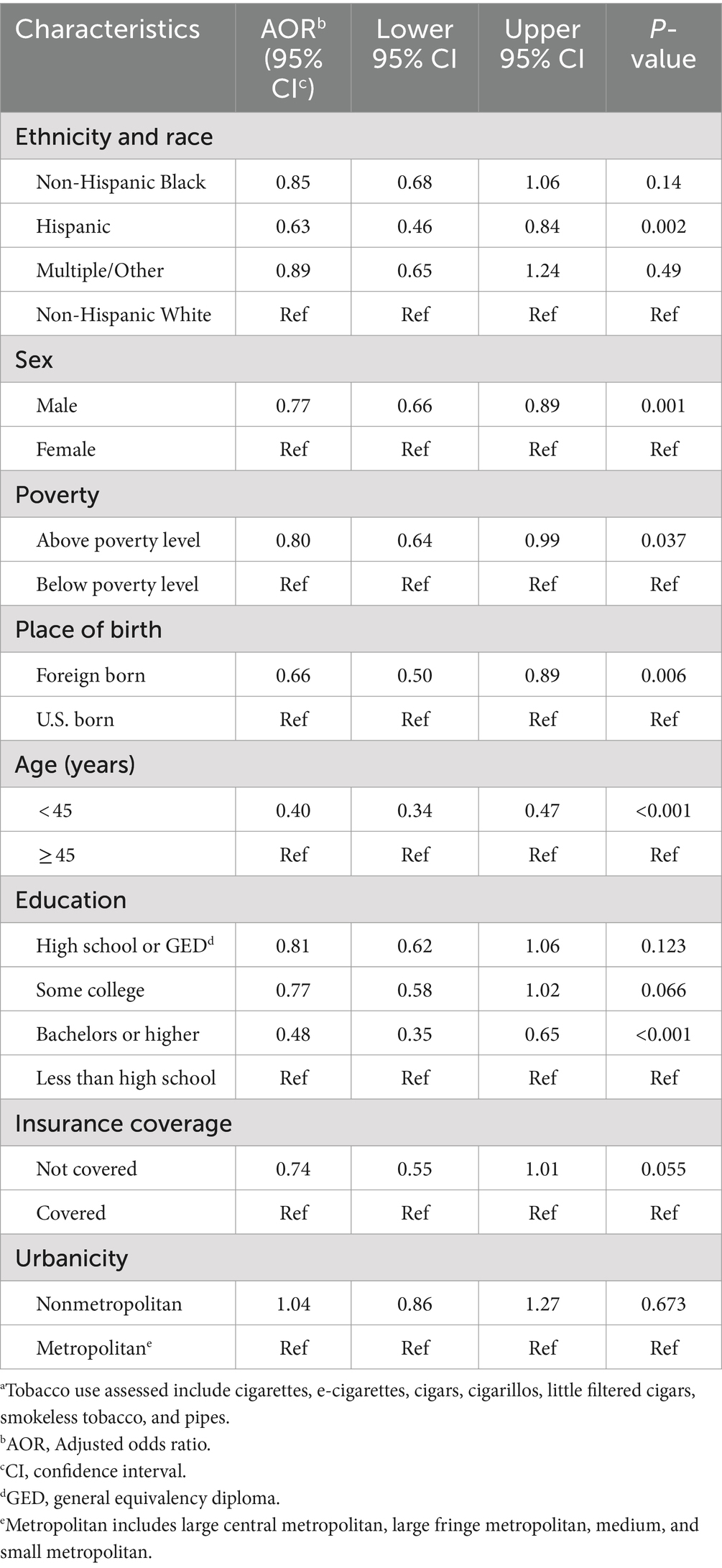
Table 2. Multivariable survey-weighted logistic regression analyses correlating factors associated with medical advice to quit tobacco usea: National Health Information Survey, 2022.
4 Discussion
In this nationally representative sample of the US adult population who used tobacco and visited an HCP in the last 12 months, 38.4% received medical advice to quit. Although medical advice to quit tobacco use is an effective intervention for tobacco use cessation (1, 10, 11, 31), our study suggests that almost two-thirds of adult tobacco users missed clinical opportunities to quit and remain at risk of tobacco-use-related diseases. The current literature on medical advice to quit tobacco use is mainly focused on cigarette smoking. However, in practice, cigarettes and other tobacco products such as e-cigarettes, cigars, pipes, and smokeless tobacco are used solo or in combination (32). With the growing consumption of other tobacco products (33) and the rising popularity of polysubstance use (34) in the US, it is of utmost importance that every tobacco user, regardless of the type of tobacco product used, receive advice and education from their HCPs on the harms associated with tobacco use.
In our study, race and ethnicity, sex, place of birth, age, and level of educational attainment were the major sociodemographic factors found to be significantly associated with the receipt of HCPs’ advice to quit all tobacco use. We found that Hispanics were less likely to receive medical advice to quit tobacco use, which is consistent with the existing literature on tobacco smoking (19, 24, 35, 36). Among other factors, the language barrier was found contributing to the lower odds of receipt of medical advice to quit tobacco use among Hispanics (20). Therefore, culturally competent interventions should be made available to HCPs to provide advice to Hispanics to quit tobacco use (19, 37, 38).
We also found that male tobacco users were less likely to receive medical advice to quit, corroborating the existing literature (17, 35). Females are more likely to receive medical advice because they tend to seek medical assistance to quit smoking and use recommended cessation resources more frequently than males (39). Since the prevalence of tobacco use is higher among males (40), lower odds of receiving medical advice to quit in males is alarming and calls for increased efforts to encourage men to seek medical assistance to quit tobacco use.
Interestingly, foreign-born US residents were less likely to receive medical advice to quit tobacco use compared to US-born individuals. Lower odds of receiving medical advice to quit tobacco use among foreign-born could be due to physicians’ limited access to culturally competent smoking cessation interventions and patient’s lack of access to care (19, 20). Moreover, studies have reported that foreign-born individuals have lower healthcare utilization and are less likely to use preventative care (21, 22). HCPs give priority to the patient’s primary complaint and usually do not focus on smoking cessation unless they present with a smoking-related disease (41). Since foreign-born individuals are more likely to visit an HCP only when they have a health complaint, and if the complaint is not associated with any smoking-related condition, it is less likely that they will receive any quit smoking advice from the HCP (41).
We found that individuals younger than 45 years were less likely to receive medical advice to quit tobacco use, which is congruent with other studies (17, 35). According to Frank and colleagues, a physician might not find advising healthy younger patients time-efficient due to lower perceived health risk; hence, physicians focus more on older patients as they present more frequently with smoking-related diseases (42). Moreover, El-Shahawy and colleagues found that physicians are inconsistent in advising users of newer tobacco products commonly used among the youth, such as e-cigarettes, because information on the potential harms and benefits are lacking or non-consensual, and there were beliefs supporting e-cigarette use as a safer alternative to combustible products and has benefits in smoking cessation (43, 44). The 2020 Surgeon General’s report indicates that the efficacy of e-cigarettes as a smoking cessation aid is inconclusive (1), and there are health risks associated with e-cigarette use, such as nicotine dependence, cancer, respiratory infections, and oral and gastrointestinal disorders (45, 46). Under such circumstances, the lower rate of HCP advice or inconsistent advice to quit all tobacco use among younger adults reflects a missed opportunity to prevent adverse tobacco-related health issues in the future.
We also found that individuals with tertiary education (bachelor’s degree or higher) were less likely to receive advice to quit tobacco use from HCPs. The existing literature has conflicting findings on this topic. While some studies supported our findings (24, 35, 36, 47), other studies suggested that individuals with a tertiary level of education were more likely to receive medical advice to quit smoking (48–50). After adjusting for education, we found that individuals living in households above the poverty level were less likely to receive medical advice to quit tobacco use. Like education, the relationship between poverty and medical advice to quit smoking was also inconsistent in the literature. While some reports state that high-income individuals are more likely to receive medical advice (48, 50), others found no significant association between income or poverty ratio (17, 49) and medical advice. Therefore, the role of patients’ education and income on medical advice to quit tobacco use needs further investigation. A plausible explanation of our finding is that individuals from middle or high socioeconomic status (here proxied by education and poverty ratio) have a low prevalence of tobacco use (5) and have lower comorbidities (51), high literacy (52), and better living conditions, which leads to HCPs having a low perceived threat of smoking-related diseases for these patients.
Despite recommendations from the Surgeon General and other professional medical associations, medical advice to quit tobacco use remains low in the US (1). Considering the critical role of HCPs in their patient’s decision to abstain from tobacco use, the suboptimal prevalence of medical advice indicates a missed clinical opportunity to promote quitting tobacco use. This is especially concerning because, in our data, about 91% of the US adult population had a clinical encounter(s) with a healthcare professional (HCP) or a dentist in the past 12 months, indicating a missed clinical opportunity to ask for tobacco use and advice to quit to a significant proportion of the US adult population. Individual and organization-level barriers may be accountable for suboptimal medical advice to quit tobacco. At the individual level, lower odds of medical advice to quit smoking could be driven by the HCPs’ lack of perceived health risks to patients (e.g., the patient has good health), a fear of damaging patient-provider relationship (41, 42), the lack of perceived effectiveness of counseling, perceived low patient motivation, and the lack of training in tobacco use cessation and effective counseling communication (53, 54).
At the organizational level, poor reimbursement, lack of tobacco use cessation resources, limited time for patient-provider communication, and lack of support services needed for smoking cessation could account for the low receipt of medical advice to stop tobacco use (36, 55). Therefore, training HCPs on quitting tobacco use and counseling skills and developing an integrated system of HCPs advice and a tiered system of support to quit tobacco use will help improve quitting (56).
To the best of our knowledge, this is the first study that included all tobacco products (and not just cigarettes) as the primary outcome and assessed disparities in receiving medical advice to quit all tobacco use. Holistic medical advice to quit any form of tobacco is especially important now, considering the rising use of other tobacco products, such as electronic cigarettes (57) and poly use (34). Considering the established effectiveness of tobacco use cessation by oral healthcare professionals (3, 12, 13), another novelty of this study is that in addition to HCP visits, we also accounted for dental visits as a criterion for the study population, unlike previous reports (16, 19). Additionally, we included foreign-born as a predictor, which was not included in the previous studies. Finding that foreign-born individuals are less likely to receive medical advice to quit smoking gives a new insight into healthcare disparities experienced by US immigrants and should be further investigated in greater depth. Moreover, our finding on disparate medical advice to individuals with tertiary education was unique and calls for further analysis to assess intersectionality for other factors such as race and sex. Another key strength of our study is that it uses the most updated (released June 2023) nationally representative large sample of the US population.
The study had some limitations. Given the cross-sectional design, the study could not establish a causal relationship between identified factors and advice to quit tobacco use. Therefore, longitudinal studies are needed to establish the causal relationship. The data was based on self-report; hence, recall bias could have affected participants’ responses. Further, because NHIS is limited to non-institutionalized US civilian populations, results are not generalizable to institutionalized populations or persons in the military.
The prevalence of receiving HCP advice to quit tobacco use in the US adult population remains suboptimal and disparate among sociodemographic groups. Our findings call for strategic implementation of USPHS’s guidelines through policy enforcement and resource allocation to improve the receipt of medical advice to quit tobacco use among Hispanics, males, foreign-born, young individuals, and those who are highly educated. Policies should be implemented to increase training on cessation for all forms of tobacco products in medical and dental schools, as well as practitioner licensing renewal curriculums, especially for primary care physicians and dentists. More resources should be allocated to equip the HCPs with culturally adapted counseling competencies. The other targeted systemic level changes could include increasing resources and funding towards college campus health clinics and community health clinics (especially in areas with a high presence of ethnic minorities and foreign-born) to improve quit smoking.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: https://www.cdc.gov/nchs/nhis/2022nhis.htm.
Ethics statement
The studies involving humans were approved by the Research ethics review board of the National Center for Health Statistics approved the study. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MC: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. RT: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. JF: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. SS: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the National Cancer Institute (P30CA016672 to S. Shete), the Betty B. Marcus Chair in Cancer Prevention (to S. Shete), and the Duncan Family Institute for Cancer Prevention and Risk Assessment (S. Shete). The funders were not involved in the study design, analysis, interpretation of data, or manuscript writing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. U.S. Department of Health and Human Services. Smoking cessation. A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health (2020).
2. Centers for Disease Control and Prevention. Smokeless tobacco: health effects 2020. Available at: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/smokeless/health_effects/index.htm.
3. Gajendra, S, McIntosh, S, and Ghosh, S. Effects of tobacco product use on oral health and the role of oral healthcare providers in cessation: a narrative review. Tob Induc Dis. (2023) 21:1–16. doi: 10.18332/tid/157203
4. Centers for Disease Control and Prevention. Smokeless tobacco: products and marketing (2021). Available at: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/smokeless/products_marketing/index.htm.
5. Cornelius, ME, Loretan, CG, Jamal, A, Davis Lynn, BC, Mayer, M, Alcantara, IC, et al. Tobacco product use among adults - United States, 2021. MMWR Morb Mortal Wkly Rep. (2023) 72:475–83. doi: 10.15585/mmwr.mm7218a1
6. Cohn, AM, Ehlke, SJ, Cobb, CO, and Soule, EK. Hookah tobacco smoking in a large urban sample of adult cigarette smokers: links with alcohol and poly-tobacco use. Addict Behav. (2017) 68:1–5. doi: 10.1016/j.addbeh.2016.12.012
7. Sterling, KL, Fryer, CS, Pagano, I, and Fagan, P. Little cigars and cigarillos use among young adult cigarette smokers in the United States: understanding risk of concomitant use subtypes. Nicotine Tob Res. (2016) 18:2234–42. doi: 10.1093/ntr/ntw170
8. Agaku, IT, King, BA, Husten, CG, Bunnell, R, Ambrose, BK, Hu, SS, et al. Tobacco product use among adults—United States, 2012–2013. Morb Mortal Wkly Rep. (2014) 63:542–47.
9. National Cancer Institute. Online summary of trends in US Cancer control measures: quitting smoking (2023). Available at: https://progressreport.cancer.gov/prevention/quitting_smoking#field_data_source.
10. Kastaun, S, Viechtbauer, W, Leve, V, Hildebrandt, J, Funke, C, Klosterhalfen, S, et al. Quit attempts and tobacco abstinence in primary care patients: follow-up of a pragmatic, two-arm cluster randomised controlled trial on brief stop-smoking advice - ABC versus 5As. ERJ Open Res. (2021) 7:00224-02021. doi: 10.1183/23120541.00224-2021
11. Stead, LF, Buitrago, D, Preciado, N, Sanchez, G, Hartmann-Boyce, J, and Lancaster, T. Physician advice for smoking cessation. Cochrane Database Syst Rev. (2013) 5:CD000165. doi: 10.1002/14651858.CD000165.pub4
12. Yadav, S, Lee, M, and Hong, Y-R. Smoking-cessation advice from dental care professionals and its association with smoking status: analysis of National Health and nutrition examination survey 2015-2018. J Am Dent Assoc. (2022) 153:15–22. doi: 10.1016/j.adaj.2021.07.009
13. Holliday, R, Hong, B, McColl, E, Livingstone-Banks, J, and Preshaw, PM. Interventions for tobacco cessation delivered by dental professionals. Cochrane Database Syst Rev. (2021) 2:CD005084. doi: 10.1002/14651858.CD005084.pub4
14. Tobacco Use and Dependence Guideline Panel. Treating tobacco use and dependence: 2008 update. Rockville, MD: US Department of Health and Human Services. (2008). Available at: https://www.ncbi.nlm.nih.gov/books/NBK63952/.
15. National Center for Health Statistics. Interactive summary health statistics for adults: National Health Interview Survey. (2023). Available at: https://wwwn.cdc.gov/NHISDataQueryTool/SHS_adult/index.html.
16. Maki, KG, and Volk, RJ. Disparities in receipt of smoking cessation assistance within the US. JAMA Netw Open. (2022) 5:e2215681. doi: 10.1001/jamanetworkopen.2022.15681
17. Babb, S, Malarcher, A, Schauer, G, Asman, K, and Jamal, A. Quitting smoking among adults—United States, 2000–2015. Morb Mortal Wkly Rep. (2017) 65:1457–64. doi: 10.15585/mmwr.mm6552a1
18. Shabnam Shenasi Azari, VJ, Hahn, Joyce, and Medina, Lauren. The foreign-born population in the United States: 2022. (2024). Available at: https://www.census.gov/library/publications/2024/acs/acsbr-019.html.
19. Babb, S. Disparities in cessation behaviors between Hispanic and non-Hispanic white adult cigarette smokers in the United States, 2000–2015. Prev Chronic Dis. (2020) 17:E10. doi: 10.5888/pcd17.190279
20. Carter-Pokras, OD, Feldman, RH, Kanamori, M, Rivera, I, Chen, L, Baezconde-Garbanati, L, et al. Barriers and facilitators to smoking cessation among Latino adults. J Natl Med Assoc. (2011) 103:423–31. doi: 10.1016/S0027-9684(15)30339-4
21. Xu, KT, and Borders, TF. Does being an immigrant make a difference in seeking physician services? J Health Care Poor Underserved. (2008) 19:380–90. doi: 10.1353/hpu.0.0001
22. Ye, J, Mack, D, Fry-Johnson, Y, and Parker, K. Health care access and utilization among US-born and foreign-born Asian Americans. J Immigr Minor Health. (2012) 14:731–7. doi: 10.1007/s10903-011-9543-9
23. Centers for Disease Control and Prevention. Tobacco use among adults- United States, 2005. (2006). Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5542a1.htm.
24. Azagba, S, and Shan, L. Disparities in the receipt of medical doctors' advice to quit smoking in the U.S., 1992-2019. Addict Behav. (2022) 125:107145. doi: 10.1016/j.addbeh.2021.107145
25. Center for Disease Control and Prevention. National health interview survey, 2022 (2023). Available at: https://www.cdc.gov/nchs/nhis/2022nhis.htm.
26. Zablotsky, B, Lessem, SE, Gindi, RM, Maitland, AK, Dahlhamer, JM, and Blumberg, SJ. Overview of the 2019 national health interview survey questionnaire redesign. Am J Public Health. (2023) 113:408–15. doi: 10.2105/AJPH.2022.307197
27. Ory, MG, Anderson, LA, Friedman, DB, Pulczinski, JC, Eugene, N, and Satariano, WA. Cancer prevention among adults aged 45–64 years: setting the stage. Am J Prev Med. (2014) 46:S1–6. doi: 10.1016/j.amepre.2013.10.027
28. Roberts, ME, Doogan, NJ, Kurti, AN, Redner, R, Gaalema, DE, Stanton, CA, et al. Rural tobacco use across the United States: how rural and urban areas differ, broken down by census regions and divisions. Health Place. (2016) 39:153–9. doi: 10.1016/j.healthplace.2016.04.001
29. Roberts, ME, Doogan, NJ, Stanton, CA, Quisenberry, AJ, Villanti, AC, Gaalema, DE, et al. Rural versus urban use of traditional and emerging tobacco products in the United States, 2013-2014. Am J Public Health. (2017) 107:1554–9. doi: 10.2105/AJPH.2017.303967
30. National Center for Health Statistics. National Health Interview Survey, 2022 survey description. (2023). Available at: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2022/srvydesc-508.pdf
31. Aveyard, P, Begh, R, Parsons, A, and West, R. Brief opportunistic smoking cessation interventions: a systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction. (2012) 107:1066–73. doi: 10.1111/j.1360-0443.2011.03770.x
32. Harrell, PT, Naqvi, SMH, Plunk, AD, Ji, M, and Martins, SS. Patterns of youth tobacco and polytobacco usage: the shift to alternative tobacco products. Am J Drug Alcohol Abuse. (2017) 43:694–702. doi: 10.1080/00952990.2016.1225072
33. Marshall, JR, Lotfipour, S, and Chakravarthy, B. Growing trend of alternative tobacco use among the Nation's youth: a new generation of addicts. West J Emerg Med. (2016) 17:139–42. doi: 10.5811/westjem.2016.1.29383
34. Agbonlahor, O, Mattingly, DT, Hart, JL, Rai, J, McLeish, AC, and Walker, KL. Differences in health care provider advice on abstaining from tobacco use: findings from the 2020 National Youth Tobacco Survey. Addict Behav. (2023) 144:107726. doi: 10.1016/j.addbeh.2023.107726
35. Kruger, J, Shaw, L, Kahende, J, and Frank, E. Health care providers' advice to quit smoking, National Health Interview Survey, 2000, 2005, and 2010. Prev Chronic Dis. (2012) 9:E130. doi: 10.5888/pcd9.110340
36. Mai, Y, and Soulakova, JN. Retrospective reports of former smokers: receiving doctor's advice to quit smoking and using behavioral interventions for smoking cessation in the United States. Prev Med Rep. (2018) 11:290–6. doi: 10.1016/j.pmedr.2018.07.012
37. Simmons, VN, Sutton, SK, Medina-Ramirez, P, Martinez, U, Brandon, KO, Byrne, MM, et al. Self-help smoking cessation intervention for Spanish-speaking Hispanics/Latinxs in the United States: a randomized controlled trial. Cancer. (2022) 128:984–94. doi: 10.1002/cncr.33986
38. Woodruff, SI, Talavera, GA, and Elder, JP. Evaluation of a culturally appropriate smoking cessation intervention for Latinos. Tob Control. (2002) 11:361–7. doi: 10.1136/tc.11.4.361
39. Jayakumar, N, Chaiton, M, Zhang, B, Selby, P, and Schwartz, R. Sex differences in use of smoking cessation services and resources: a real-world study. Tobacco Use Insights. (2020) 13:1179173X2090150. doi: 10.1177/1179173X20901500
40. Centers for Disease Control and Prevention. Current cigarette smoking among adults in the United States Atlanta, U.S.: Office of Smoking and Health, National Center for chronic disease prevention and health promotion (2023). Available at: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm.
41. Coleman, T, Murphy, E, and Cheater, F. Factors influencing discussion of smoking between general practitioners and patients who smoke: a qualitative study. Br J Gen Pract. (2000) 50:207–10.
42. Frank, E, Winkleby, MA, Altman, DG, Rockhill, B, and Fortmann, SP. Predictors of physicians' smoking cessation advice. JAMA. (1991) 266:3139–44. doi: 10.1001/jama.1991.03470220055026
43. El-Shahawy, O, Brown, R, and Elston, LJ. Primary care physicians’ beliefs and practices regarding e-cigarette use by patients who smoke: a qualitative assessment. Int J Environ Res Public Health. (2016) 13:445. doi: 10.3390/ijerph13050445
44. Warner, KE, Benowitz, NL, McNeill, A, and Rigotti, NA. Nicotine e-cigarettes as a tool for smoking cessation. Nat Med. (2023) 29:520–4. doi: 10.1038/s41591-022-02201-7
45. Seiler-Ramadas, R, Sandner, I, Haider, S, Grabovac, I, and Dorner, TE. Health effects of electronic cigarette (e-cigarette) use on organ systems and its implications for public health. Wien Klin Wochenschr. (2021) 133:1020–7. doi: 10.1007/s00508-020-01711-z
46. Mir, M, Rauf, I, Goksoy, S, Khedr, A, Jama, AB, Mushtaq, H, et al. Electronic cigarettes: are they smoking cessation aids or health hazards? Cureus. (2022) 14:e25330. doi: 10.7759/cureus.25330
47. Ramaswamy, AT, Toll, BA, Chagpar, AB, and Judson, BL. Smoking, cessation, and cessation counseling in patients with cancer: a population-based analysis. Cancer. (2016) 122:1247–53. doi: 10.1002/cncr.29851
48. Tibuakuu, M, Okunrintemi, V, Jirru, E, Echouffo Tcheugui, JB, Orimoloye, OA, Mehta, PK, et al. National Trends in cessation counseling, prescription medication use, and associated costs among US adult cigarette smokers. JAMA Netw Open. (2019) 2:e194585. doi: 10.1001/jamanetworkopen.2019.4585
49. Houston, TK, Scarinci, IC, Person, SD, and Greene, PG. Patient smoking cessation advice by health care providers: the role of ethnicity, socioeconomic status, and health. Am J Public Health. (2005) 95:1056–61. doi: 10.2105/AJPH.2004.039909
50. Kaplan, RM, Fang, Z, and Morgan, G. Providers' advice concerning smoking cessation: evidence from the medical expenditures panel survey. Prev Med. (2016) 91:32–6. doi: 10.1016/j.ypmed.2016.07.012
51. Weiser, JK, Tie, Y, Beer, L, Neblett Fanfair, R, and Shouse, RL. Racial/ethnic and income disparities in the prevalence of comorbidities that are associated with risk for severe COVID-19 among adults receiving HIV care, United States, 2014-2019. J Acquir Immune Defic Syndr. (2021) 86:297–304. doi: 10.1097/QAI.0000000000002592
52. Stormacq, C, Van den Broucke, S, and Wosinski, J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot Int. (2018) 34:e1–e17. doi: 10.1093/heapro/day062
53. Sherman, MD, and Hooker, SA. Family medicine physicians' confidence and perceived effectiveness in delivering health behaviour change interventions. Fam Pract. (2020) 37:493–8. doi: 10.1093/fampra/cmaa001
54. Chan, HL, Chan, AK, Chu, CH, and Tsang, YC. Smoking cessation in dental setting: a narrative review on dental professionals’ attitude, preparedness, practices and barriers. Front Oral Health. (2023) 4:1266467. doi: 10.3389/froh.2023.1266467
55. Bell, K, Bowers, M, McCullough, L, and Bell, J. Physician advice for smoking cessation in primary care: time for a paradigm shift? Crit Public Health. (2012) 22:9–24. doi: 10.1080/09581596.2011.572155
56. Bauld, L, Bell, K, McCullough, L, Richardson, L, and Greaves, L. The effectiveness of NHS smoking cessation services: a systematic review. J Public Health. (2010) 32:71–82. doi: 10.1093/pubmed/fdp074
Keywords: medical advice, tobacco cessation, tobacco use, disparities, health care professionals (HCPs)
Citation: Chandra M, Talluri R, Fokom Domgue J and Shete S (2024) Prevalence and disparities in receiving medical advice to quit tobacco use in the US adult population. Front. Public Health. 12:1383060. doi: 10.3389/fpubh.2024.1383060
Edited by:
Vaughan W. Rees, Harvard T.H. Chan School of Public Health, United StatesReviewed by:
Sonu Bhaskar, National Cerebral and Cardiovascular Center, JapanJeff Bolles, Francis Marion University, United States
Angela M. Goins, University of Houston–Downtown, United States
Copyright © 2024 Chandra, Talluri, Fokom Domgue and Shete. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sanjay Shete, c3NoZXRlQG1kYW5kZXJzb24ub3Jn
†These authors have contributed equally to this work and share first authorship
 Monalisa Chandra
Monalisa Chandra Rajesh Talluri
Rajesh Talluri Joel Fokom Domgue
Joel Fokom Domgue Sanjay Shete
Sanjay Shete