- 1Department of Social Community and Health Education, School of Public Health, Xuzhou Medical University, Xuzhou, Jiangsu, China
- 2Huadong Research Institute for Medicine and Biotechniques, Nanjing, Jiangsu, China
- 3Department of psychiatry, Renmin Hospital of Wuhan University, Wuhan, Hubei, China
- 4Department of health management, School of Management, Xuzhou Medical University, Xuzhou, Jiangsu, China
Background: As population migration increases and the aging process accelerates, the number of migrant older adults is growing significantly. This trend presents a substantial challenge to urban health services in regions experiencing an influx of older adults individuals. Consequently, examining the healthcare service utilization of the migrant older adults population is crucial to promote healthy aging.
Methods: A multi-stage random sampling method was employed to select a study population of 568 migrant older adults individuals, aged 60 years and above, residing in urban Xuzhou City. Multivariate logistic regression analysis, based on Anderson’s model, was conducted to explore the factors influencing outpatient and inpatient health service utilization among this population.
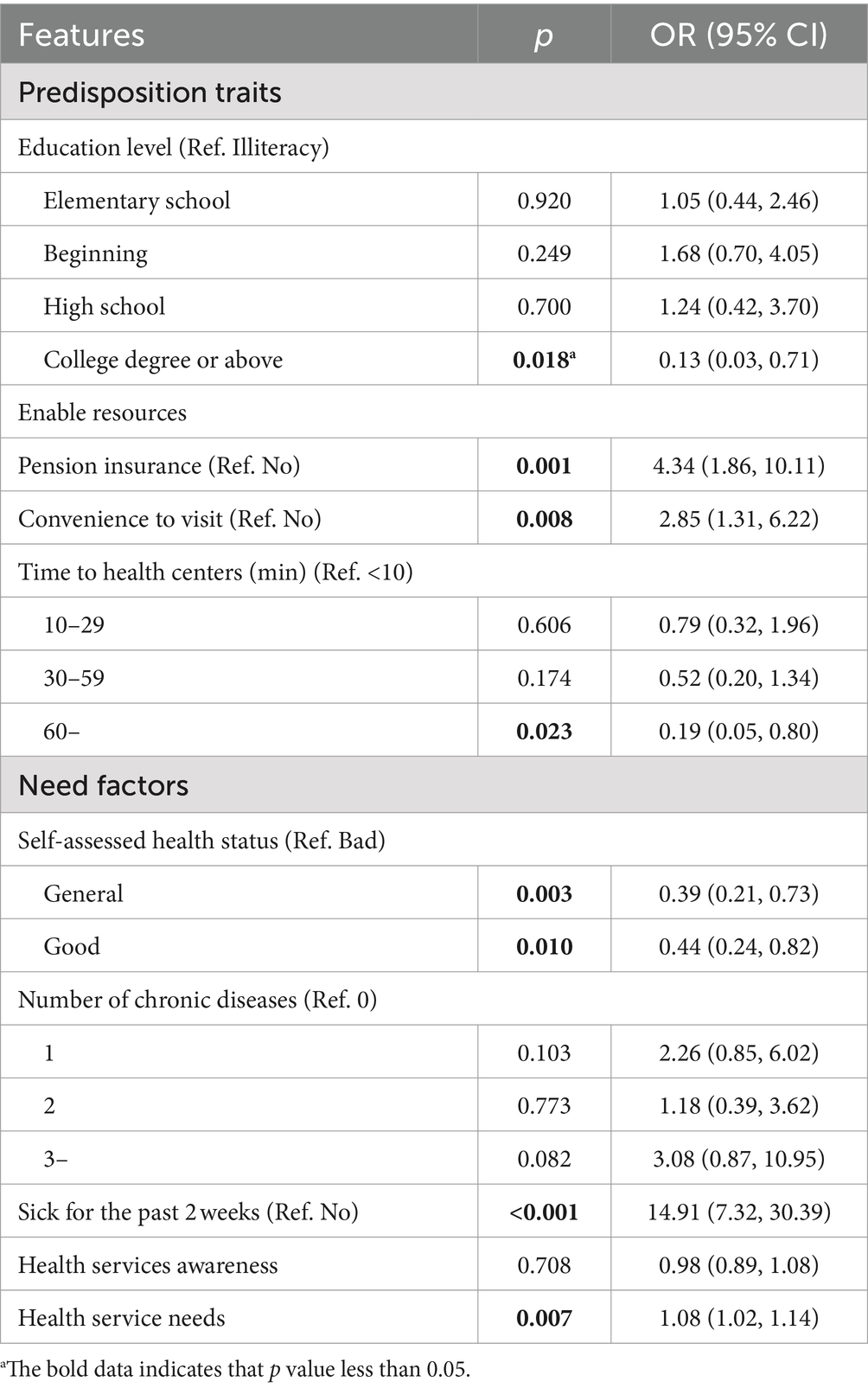
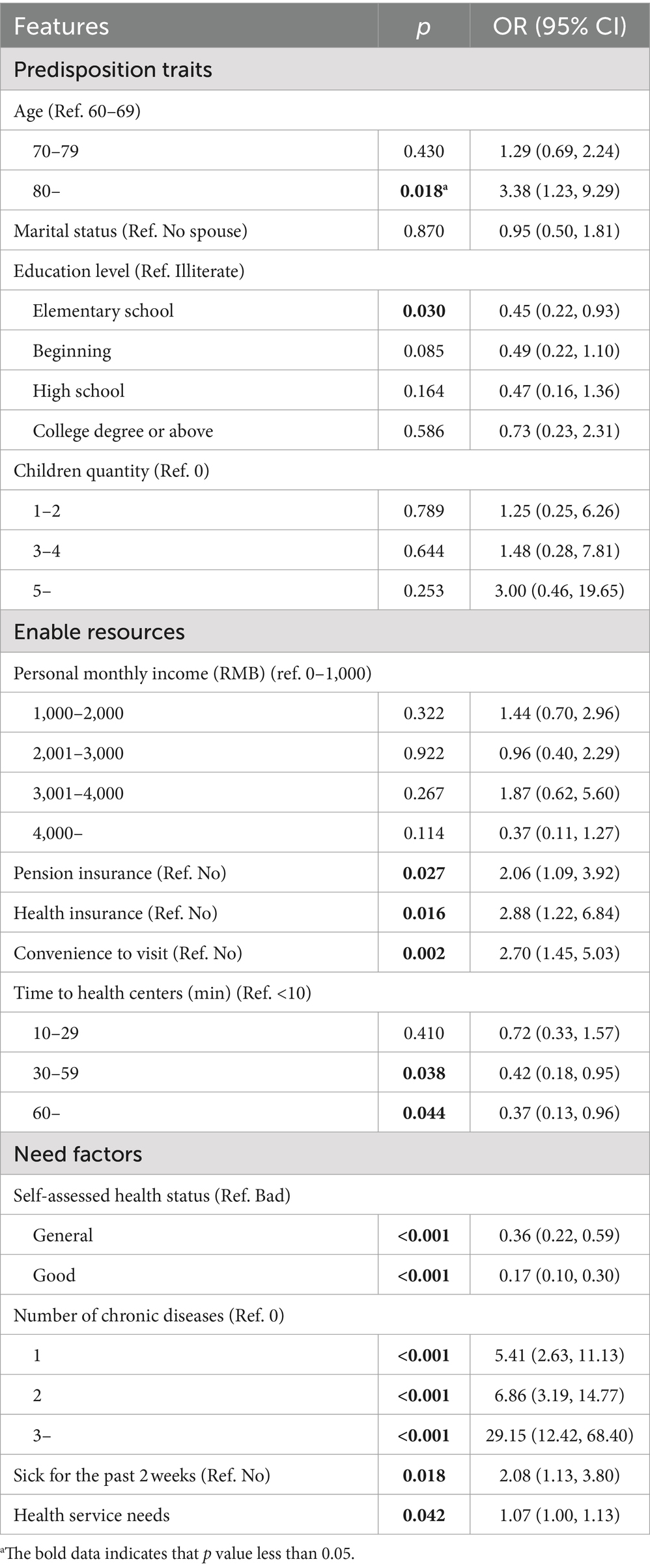
Results: Among the 568 migrants, 73 (12.9%) had received outpatient services within the past 2 weeks, while 109 (19.2%) had received inpatient services within the past year. Migrant older adults with education level, time to health centers, and self-assessed health status negatively influenced the outpatient services utilization among migrant older adults. Possession of pension insurance, convenience to visit, sick for the past 2 weeks, and health services need positively influenced the outpatient services utilization among migrant older adults. Furthermore, age, possession of pension insurance and health insurance, convenience to visit, number of chronic diseases, sick for the past 2 weeks, and healthcare service need positively influenced inpatient service utilization among migrant older adults. Education level, self-assessed health status, and time to health centers negatively influenced the inpatient services utilization among migrant older adults.
Conclusion: The overall utilization of healthcare services by migrant older adults in Xuzhou remains inadequate. Addressing this issue requires enhanced medical policy support and assistance, stronger health education initiatives, and improved social integration for the older adults. Additionally, efforts should be made to reduce their financial burdens and improve the accessibility of healthcare services.
1 Introduction
Health service utilization refers to the actual volume of healthcare services accessed by individuals, serving as a direct measure of the effectiveness and efficiency of delivering comprehensive care for the overall wellbeing of a population (1). The utilization of healthcare services is closely tied to the physical and mental health of migrants, often manifested in their behaviors related to outpatient or inpatient care when faced with discomfort, injuries, or physiological issues (2, 3). As a common metric, health service utilization reflects the societal and economic benefits of healthcare services and indicates the impact of these services on population health outcomes (4, 5). The provision of healthcare services in China is a complex system with multiple levels and channels, with the government taking the lead and medical institutions (including public hospitals, private hospitals and community health service organizations) as the mainstay in providing outpatient and inpatient services. Patients undertake the costs of health service utilization through individual payments, health insurance, and commercial insurance. And the term “underutilization of health services” describes a scenario where individuals or groups fail to make adequate or timely use of available health resources when needed, often resulting in a lack of access to preventive, diagnostic, therapeutic, or rehabilitative services aligned with their health needs.
China, in the past few decades, has experienced a unique challenge related to its internal migrant population due to rapid urbanization. The most commonly accepted definition of this population is from the Census 2000, which describes migrants as individuals residing in a new location for at least 1 year without local household registration. And China’s migrant population reached 376 million, accounting for approximately 26.7% of the total population, and continues to grow (6). Internal migrants often face barriers to accessing healthcare services in their new locations, such as unfamiliarity with local healthcare organizations, service delivery processes, and health insurance policies. Additionally, low health literacy, often due to limited education or language barriers, further complicates their ability to seek timely medical care, exacerbating health risks. As both population migration and the aging process accelerate, there has been a noticeable increase in both the size and proportion of older adults individuals within the migrant population (7, 8). The health challenges of this demographic pose significant pressure on urban management and public health services in regions experiencing an influx of older adults migrants (9). Moreover, addressing the health needs of this growing group is crucial for promoting equitable access to basic public services in urban areas (10). Therefore, it is vital to investigate the healthcare service utilization of migrant older adults to ensure the continued stability and development of urban healthcare services.
A significant portion of China’s internal migrants come from rural areas, and many, including the older adults, migrate to cities for work. These individuals often live-in poor conditions, with low levels of personal and family income, and their financial situation remains bleak. Migrant older adults populations face changes in their economic circumstances, living environments, and social roles (11, 12), and are often considered a vulnerable subgroup within the broader migrant community. They encounter numerous barriers in accessing essential healthcare services (13). Existing studies on healthcare service utilization among migrant older adults primarily rely on national data concerning health insurance, basic public health services, health education, and service satisfaction (14–17), etc. However, much of this research focuses on individual characteristics that are difficult to change, lacks systematic analysis, and often lacks strong theoretical foundations (18–20).
The Anderson model, first proposed by American scholar Ronald M. Andersen in 1968, is a widely used theoretical framework for understanding the factors influencing healthcare service utilization. The model helps researchers grasp the complex mechanisms affecting healthcare access and utilization and provides a basis for designing interventions aimed at improving the accessibility and equity of health services. Anderson’s model incorporates both societal and individual determinants in its analysis. According to the model, health service utilization—whether outpatient or inpatient—is influenced by three key components: predisposing traits, enabling resources, and need factors (PEN) (20). Predisposition traits include factors that exist before an individual seeks healthcare, which can influence a person’s tendency to utilize health services. Enabling resources refer to the conditions that facilitate or hinder access to healthcare, such as income, health insurance coverage, and geographic accessibility to healthcare facilities. Need factors reflect an individual’s health status and their perceived or actual need for healthcare services (21–23). Given its well-established theoretical foundation, Anderson’s model provides a robust framework for analyzing the factors affecting health service utilization, making it particularly useful for examining the healthcare behaviors of migrant older adults.
Xuzhou City, located at the intersection of Jiangsu, Shandong, Anhui, and Henan provinces, has a significant migrant population, including a growing and aging older adults demographic. As of the end of 2022, Xuzhou’s migrant population stood at approximately 1.33 million, with 19.8% aged 60 or older (24). This study aims to assess the current utilization of outpatient and inpatient healthcare services among the migrant older adults population in Xuzhou and to explore the factors influencing this utilization.
2 Materials and methods
2.1 Study design and participants
A multi-stage random sampling method was employed to select participants from the urban area of Xuzhou between October 2020 and May 2021, focusing on migrant older adults aged 60 years and above. In the first stage, 10 communities were randomly selected from each of the five administrative districts of Xuzhou: Tongshan District, Yunlong District, Gulou District, Quanshan District, and Jiawang District. In the second stage, 12 households were randomly chosen within each community. Finally, in the third stage, one migrant older adults individual was randomly selected from each household to participate in the offline questionnaire survey. A total of 600 questionnaires were distributed, of which 568 were deemed valid after careful scrutiny, yielding an effective response rate of 94.7%.
Inclusion criteria for participants were: migrant older adults aged 60 years and older, who had lived in the local area for at least 1 month, held foreign household registration, and provided informed consent to participate in the survey. Exclusion criteria included individuals in poor health, those with cognitive impairments, and those who were unwilling or unable to complete the questionnaire.
2.2 Measurements
According to the definition in social medicine and health management textbooks, outpatient service utilization was assessed by determining whether the respondent had used outpatient services at a health center in the past 2 weeks. Inpatient service utilization was measured by whether the respondent had been hospitalized in the past year. Data were collected through face-to-face questionnaires. Additionally, awareness of and needs for health services were measured across 11 categories, including physical examinations, auxiliary examinations, chronic disease management, health education, interpretation of physical examination results, health guidance, follow-up, and review etc. Both health service awareness and needs were scored on a binary scale (Yes = 1, No = 0), with total scores ranging from 0 to 11.
2.3 Variables based on Anderson’s model
The questionnaire was developed following Anderson’s Behavioral Model of Health Service Utilization and through a series of pre-surveys and team discussions. It included three main sections: (1) The first section was predisposition traits, mainly include gender, age, education level, marital status, children quantity, flow range and flow time among participants. (2) The second section was enabling resources, mainly include personal monthly income, pension insurance, access to healthcare services including health insurance availability and time to health centers. (3) The third section was need factors, mainly include self-assessed health status, the number of chronic diseases, sick for the past 2 weeks, their health services awareness, and their health needs.
2.4 Statistical analysis
Descriptive statistics were used to calculate the number and percentage of categorical variables, with proportions expressed as percentages for different classifications of each variable.
To explore the associations between various factors and healthcare service utilization, Chi-square tests were employed to assess the factors influencing health service utilization among migrant older adults. Multivariate logistic regressions were selected for analysis, which is particularly useful for identifying the associations between variables (25). Variables that demonstrated statistical significance in the univariate analysis were included in the logistic regression model to explore the determinants of healthcare utilization among the migrant older adults. For non-normally distributed data, such as health service awareness and health service needs, non-parametric tests were used, with results expressed in medians and quartiles. Statistical analyses were conducted using SPSS software (version 22.0), with a significance level of p < 0.05 (two-sided) considered statistically significant.
3 Results
3.1 Participant characteristics
Table 1 shows a balanced distribution in gender, among 568 migrant older adults, with 285 (50.2%) males and 283 (49.8%) females, spanning an age range of 60 and 86 years, with a mean age of (66.9 ± 6.2) years. Within the sample, 434 participants (76.4%) were married. The majority, 366 (64.4%) possessed pension insurance and 496 (87.3%) possessed health insurance.
3.2 Univariate analysis of healthcare services utilization
Table 1 also illustrates the healthcare service utilization among the 568 migrant older adults participants. A total of 73 participants (12.9%) reported using outpatient services at health centers in the past 2 weeks. The analysis revealed significant differences in outpatient service utilization based on several variables. In the predisposing traits category, only education level showed statistical significance. In the enabling resources category, factors such as pension insurance, convenience to visit, and time to health centers were significant. Finally, in the need factors category, self-assessed health status, the number of chronic diseases, sick for the past 2 weeks, and health service needs were all significantly associated with outpatient service utilization (p < 0.05).
Regarding inpatient services, 109 participants (19.2%) reported being hospitalized in the past year. The analysis showed significant differences in inpatient service utilization based on age, marital status, education level, and number of children in the predisposing traits category. In the enabling resources category, variables such as personal monthly income, pension insurance, health insurance, convenience to visit, and time to health centers were significantly associated with inpatient service utilization. The need factors of self-assessed health status, the number of chronic diseases, sick for the past 2 weeks, and health service needs also showed statistical significance (p < 0.05).
3.3 Multivariate logistic regression analysis
3.3.1 Factors influencing the outpatient services utilization
Table 2 demonstrates a notably diminished outpatient services utilization among highly educated migrant older adults (OR = 0.13, 95% CI: 0.03, 0.71) in compared to their counterparts with limited education levels in predisposing traits. Among the enabling resources, the likelihood of utilizing outpatient services was significantly higher for those with pension insurance (OR = 4.34, 95% CI: 1.86, 10.11) and those reporting high convenience to visit (OR = 2.85, 95% CI: 1.31, 6.22). Conversely, participants whose travel time to health centers was 60 min or more were significantly less likely to utilize outpatient services (OR = 0.19, 95% CI: 0.15, 0.80) compared to those with a travel time of less than 10 min. In terms of need factors, participants in good self-assessed health were significantly less likely to utilize outpatient services (OR = 0.44, 95% CI: 0.24, 0.82) compared to those with poorer self-assessed health. Conversely, those who had been sick in the past 2 weeks (OR = 14.91, 95% CI: 7.32, 30.39) and those with higher health service needs (OR = 1.08, 95% CI: 1.02, 1.14) were significantly more likely to utilize outpatient services.
3.3.2 Factors influencing the inpatient services utilization
Table 3 reveals that migrant older adults aged 80 and above demonstrated significantly elevated inpatient health services utilization (OR = 3.38, 95% CI: 1.23, 9.29) compared to their counterparts aged 60–69 years in predisposing traits. Among the enabling resources, pension insurance (OR = 2.06, 95% CI: 1.09, 3.92), health insurance coverage (OR = 2.88, 95% CI: 1.22, 6.84), and convenient access to visit (OR = 2.70, 95% CI: 1.45, 5.03) were significantly associated with higher inpatient service utilization. Conversely, those with travel times 60 min or more (OR = 0.37, 95% CI: 0.13–0.96) were significantly less likely to utilize inpatient services compared to those with shorter travel times. Regarding the need factors, participants in good self-assessed health (OR = 0.17, 95% CI: 0.10, 0.30) were significantly less likely to utilize inpatient services compared to those in poor self-assessed health. Conversely, those with three or more chronic diseases (OR = 29.15, 95% CI: 12.42, 68.40), those who had been sick in the past 2 weeks (OR = 2.08, 95% CI: 1.13, 3.80), and those with higher health service needs (OR = 1.07, 95% CI: 1.00, 1.13) were significantly more likely to utilize inpatient services.
4 Discussion
4.1 The rate of healthcare services utilization among the migrant older adults in Xuzhou is comparatively low and requires improvement
The study found that, among the 568 participants, only 73 individuals (12.9%) utilized outpatient services within the past 2 weeks. This rate is considerably lower than the average outpatient service utilization for migrant populations in the province (20.42%) (26, 27), and also below the national average for older adults populations (20.9%) (28, 29). In the past year, inpatient services were utilized by 109 migrant older adults (19.2%), which is again lower than the rates reported in most recent studies (29.9%) (30, 31). This discrepancy can be attributed to the fact that a large proportion of the sample (73.2%) consisted of migrant older adults aged 60–69, who generally enjoy relatively good health and exhibit fewer evident healthcare needs, thereby lowering their utilization rates (32).
Additionally, limited health awareness among the migrants and a lack of understanding of healthcare services at their destination may lead them to rely on purchasing medication from pharmacies or even avoid seeking medical attention when experiencing discomfort (33). These factors contribute to the relatively low healthcare service utilization observed in this study. The findings suggest, on one hand, a lack of disease knowledge and insufficient attention to personal health among the migrant older adults in Xuzhou, pointing to the need for improved health education. On the other hand, they highlight the limited understanding of available health services, underscoring the importance of strengthening health promotion efforts targeting migrant populations. Furthermore, it is recommended that migrant older adults be included in health management through community health service centers in order to promote more effective health services utilization.
4.2 Multiple factors influence the utilization of outpatient health services among migrant older adults
Among the three characteristics in Anderson’s model, enabling resources and need factors exert the most significant influence on outpatient service utilization among migrant older adults. Predisposing traits play a limited role, with one exception: migrant older adults with higher education levels (college or above) tend to develop a stronger sense of health awareness (34, 35), which correlates with a reduced likelihood of utilizing outpatient services. These individuals often possess basic medical knowledge and have a better understanding of their health conditions (16), leading them to prefer purchasing medications from pharmacies or using medicines brought from their hometowns to manage minor health issues (36).
At the enabling resources level, outpatient service utilization is higher among those with pension insurance and convenient access to healthcare services. Conversely, migrant older adults who need to travel more than 60 min to reach a health center show significantly lower utilization rates. Pension insurance plays a pivotal role in providing financial security, supporting basic healthcare needs (16), and promoting the utilization of outpatient services. However, the underutilization of outpatient services among those with long travel times highlights the critical impact of accessibility and convenience on healthcare utilization (21–23). The mobility of migrant older adults across provinces or regions introduces challenges such as varying medical policies, lifestyle differences, language barriers, and limited access to resources, prompting many to rely on self-medication or informal care for minor ailments (37, 38). Implementing comprehensive health management for migrant older adults could help ensure more equitable and efficient access to healthcare services.
Previous studies have also emphasized the predictive power of need factors in determining healthcare service utilization, particularly among the older adults (39–41). For outpatient services, good self-assessed health status is associated with lower utilization, while recent illness (within the past 2 weeks) increases the demand for healthcare services. Migrant older adults in good self-assessed health are less likely to engage with healthcare services, as their health status accurately reflects their overall wellbeing (42–44). Migrant older adults with poor self-assessed health status tend to have a subjective perception of their own health status (45), thereby increasing the likelihood of accepting outpatient medical services. Migrant older adults with high health service needs typically exhibit varying degrees of physical or mental impairment or are in a suboptimal state of health, leading to an increased inclination to utilize healthcare services (46). Moreover, the attribute of mobility can further exacerbate concerns about their health status among migrant older adults, potentially resulting in a psychological burden and consequently driving them toward seeking healthcare services (47). Consequently, the impact of the mental health and health awareness of migrant older adults people in the field of health can be targeted in subsequent research.
4.3 Multiple factors influence the utilization of inpatient health services among migrant older adults
In addition to outpatient services, predisposing traits significantly influence inpatient service utilization, particularly among migrant older adults aged 80 and above, who demonstrate much higher utilization rates than their younger counterparts (aged 60–69). This increase is likely due to the natural aging process and the associated decline in physiological functioning (48, 49) as well as the inverse relationship between age and overall health status (49, 50), leading to a greater demand for inpatient care (50, 51). With advancing age, the prevalence of chronic diseases rises (52, 53), further increasing the need for inpatient services. Previous research has documented the high prevalence of chronic diseases among the older adults in Xuzhou (54), and migrant older adults with multiple chronic conditions exhibit significantly higher utilization of inpatient services compared to those without such ailments (55). Chronic diseases such as hypertension and diabetes, which often lead to debilitating complications, profoundly affect the quality of life for migrant older adults and drive their reliance on inpatient care (56, 57).
Among enabling resources, limitations in Medicare coverage and pension income restrict the utilization of residential health services by migrant older adults. This study highlights the significant impact of health insurance coverage on healthcare utilization (58). The low reimbursement rates for hospitalization expenses at the destination, coupled with complex reimbursement procedures and limitations on eligible services, create barriers to inpatient healthcare access for migrant older adults (49, 59). Socioeconomic factors also contribute to disparities in healthcare utilization, as migrant older adults often face financial instability due to inconsistent incomes (60, 61). However, pension insurance can reduce reliance on offspring for healthcare costs, especially for hospitalization, which can incur substantial expenses (26). Conversely, migrant older adults without pension or health insurance are less likely to utilize healthcare services. To address these challenges, enhancing the development of medical insurance information systems is crucial for facilitating cross-regional medical expense settlements. Additionally, efforts should be made to promote commercial health insurance as a supplementary option for migrant older adults. Expanding the scope of reimbursement and increasing hospitalization coverage rates can alleviate financial burdens and ultimately improve healthcare utilization among this population (62).
4.4 Limitation
This study is subject to several limitations that should be acknowledged. First, the cross-sectional design limits the ability to establish causal relationships regarding healthcare service utilization among the migrant older adults. Second, this study’s geographic focus on Xuzhou City may introduce regional biases, as the findings are influenced by the specific characteristics and healthcare landscape of this area. Third, we did not collect data on key variables such as social integration, familiarity with the healthcare system in the destination, or the existence of personal health records, and their absence limits the depth of our analysis regarding the influences on healthcare services utilization. Despite these limitations, our study provides a foundation for future research and offers valuable insights for improving the utilization of healthcare services.
5 Conclusion
Overall, compared with the migrant population and the older adults in the non-migrant population, healthcare service utilization among the migrant older adults in Xuzhou is suboptimal. The study identified several key factors influencing healthcare service utilization, including age, education level, possession of pension and health insurance, ease of access to healthcare facilities, travel time to health centers, health status, recent illness (within the past 2 weeks), number of chronic diseases, and perceived need for healthcare services. To improve healthcare access for migrant older adults, it is essential to consider a multifaceted approach. This should include policy support and assistance, reducing the medical and economic burdens faced by this population, improving the accessibility and convenience of healthcare organizations, and prioritizing health education and promotion efforts. By addressing these factors, policymakers and healthcare providers can work toward enhancing the healthcare experiences and outcomes for migrant older adults populations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics statement
The studies involving humans were approved by The Research Ethics Committee of Xuzhou Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GL: Methodology, Visualization, Writing – review & editing. ZQ: Methodology, Visualization, Writing – review & editing. WYu: Methodology, Visualization, Writing – review & editing. QW: Conceptualization, Supervision, Validation, Writing – review & editing. HH: Data curation, Investigation, Writing – review & editing. CM: Conceptualization, Supervision, Writing – review & editing. WYan: Visualization, Writing – review & editing, Validation, Funding. XG: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Jiangsu Province Education Science 14th Five Year Plan Project (JS/2021/GH0106-07330).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Arueira Chaves, L, de Souza Serio dos Santos, DM, Rodrigues Campos, M, and Luiza, VL. Use of health outcome and health service utilization indicators as an outcome of access to medicines in Brazil: perspectives from a literature review. Public Health Rev. (2019) 40:5. doi: 10.1186/s40985-019-0115-1
2. Tepper, SJ, Fang, J, Vo, P, Shen, Y, Zhou, L, Abdrabboh, A, et al. Impact of erenumab on acute medication usage and health care resource utilization among migraine patients: a US claims database study. J Headache Pain. (2021) 22:27. doi: 10.1186/s10194-021-01238-2
3. Bastani, P, Mohammadpour, M, Samadbeik, M, Bastani, M, Rossi-Fedele, G, and Balasubramanian, M. Factors influencing access and utilization of health services among older people during the COVID-19 pandemic: a scoping review. Arch Public Health. (2021) 79:190. doi: 10.1186/s13690-021-00719-9
4. Chong, JL, Lim, KK, and Matchar, DB. Population segmentation based on healthcare needs: a systematic review. Syst Rev. (2019) 8:202. doi: 10.1186/s13643-019-1105-6
5. Zhao, Q, Xu, S, Aziz, N, He, J, and Wang, Y. Dialect culture and the utilization of public health service by rural migrants: insights from China. Front Public Health. (2022) 10:985343. doi: 10.3389/fpubh.2022.985343
6. Yan, L. Study on factors influencing the utilization of medical and health services by the mobile population - taking the Pearl River Delta region as an example. Acad Res. (2022) 12:79–83. doi: 10.3969/j.issn.1000-7326.2022.12.013
7. Cai, X, Yang, F, and Bian, Y. Gap analysis on hospitalized health service utilization in floating population covered by different medical insurances—case study from Jiangsu Province, China. Int J Equity Health. (2019) 18:84. doi: 10.1186/s12939-019-0992-4
8. Jarzebski, MP, Elmqvist, T, Gasparatos, A, Fukushi, K, Eckersten, S, Haase, D, et al. Ageing and population shrinking: implications for sustainability in the urban century. npj Urban Sustain. (2021) 1:17. doi: 10.1038/s42949-021-00023-z
9. Galea, S, and Vlahov, D. Urban health: evidence, challenges, and directions. Annu Rev Public Health. (2005) 26:341–65. doi: 10.1146/annurev.publhealth.26.021304.144708
10. Leider, JP, Meit, M, McCullough, JM, Resnick, B, Dekker, D, Alfonso, YN, et al. The state of rural public health: enduring needs in a new decade. Am J Public Health. (2020) 110:1283–90. doi: 10.2105/ajph.2020.305728
11. Preston, J, and Biddell, B. The physiology of ageing and how these changes affect older people. Medicine. (2021) 49:1–5. doi: 10.1016/j.mpmed.2020.10.011
12. Palmer, AK, and Jensen, MD. Metabolic changes in aging humans: current evidence and therapeutic strategies. J Clin Invest. (2022) 132:e158451. doi: 10.1172/JCI158451
13. Northridge, ME, Kumar, A, and Kaur, R. Disparities in access to oral health care. Annu Rev Public Health. (2020) 41:513–35. doi: 10.1146/annurev-publhealth-040119-094318
14. Mao, A-L, Tian, Y-K, and Li, Y-N. Can community health centers improve the self-rated health of migrants? Evidence from China. Front Public Health. (2022) 10:986201. doi: 10.3389/fpubh.2022.986201
15. Lin, Y, Wang, T, and Zhu, T. Do migration characteristics influence the utilization of basic public health services in internal elderly migrants in China? Front Public Health. (2021) 9:514687. doi: 10.3389/fpubh.2021.514687
16. Zeng, W, Wang, C, Chen, H, Tong, B, Li, D, Zou, Z, et al. Health status and public health education for internal older migrants in China: evidence from a nationally representative survey. Front Public Health. (2022) 10:937361. doi: 10.3389/fpubh.2022.937361
17. Lindberg, LG, Mundy, SS, Kristiansen, M, Johansen, KS, and Carlsson, J. Satisfaction with mental health treatment among patients with a non-western migrant background: a survey in a Danish specialized outpatient mental health clinic. Eur J Pub Health. (2019) 29:700–5. doi: 10.1093/eurpub/ckz090
18. Zhao, K, He, Y, Zeng, Q, and Ye, L. Factors of mental health service utilization by community-dwelling adults in Shanghai, China. Commun Ment Health J. (2019) 55:161–7. doi: 10.1007/s10597-018-0352-7
19. Min, R, Fang, Z, Zi, C, Tang, C, and Fang, P. Do migrant residents really achieve health equity by obtaining urban Hukou? A comparative study on health service utilization and urbanization in Central China. Front Public Health. (2022) 10:784066. doi: 10.3389/fpubh.2022.784066
20. Xin, Y, and Ren, X. Determinants of province-based health service utilization according to Andersen's behavioral model: a population-based spatial panel modeling study. BMC Public Health. (2023) 23:985. doi: 10.1186/s12889-023-15885-4
21. Full text of the Jiangsu Health and Wellness Yearbook (Volume 2022). Available at: https://wjw.jiangsu.gov.cn/art/2023/1/30/art_49262_10736693.html (Accessed December 15, 2023).
22. Schmidt, AF, and Finan, C. Linear regression and the normality assumption. J Clin Epidemiol. (2018) 98:146–51. doi: 10.1016/j.jclinepi.2017.12.006
23. Ji-Cheng, XU, and Ji-Yun, S. Research on demand and utilization of health services among urban elderly residents in Xuzhou. Chinese Health Resour. (2016) 19: 137–140. doi: 10.13688/j.cnki.chr.2016.15242
24. Zhang, K, You, H, Yu, L, Wu, Q, and Xu, X. Inequality of opportunity in outpatient expenditure among the elderly with multimorbidity: evidence from China. Int J Equity Health. (2023) 22:153. doi: 10.1186/s12939-023-01953-z
25. Mao, W, Zhang, Y, Xu, L, Miao, Z, Dong, D, and Tang, S. Does health insurance impact health service utilization among older adults in urban China? A nationwide cross-sectional study. BMC Health Serv Res. (2020) 20:630. doi: 10.1186/s12913-020-05489-8
26. Yan, P, Li, F, Nicholas, S, Maitland, E, Tan, J, Chen, C, et al. Impact of pension income on healthcare utilization of older adults in rural China. Int J Equity Health. (2023) 22:166. doi: 10.1186/s12939-023-01985-5
27. Jizhe, N. Main data of the seventh national population census news release. National Bureau of Statistics of China. (2021). Available at: https://www.stats.gov.cn/english/PressRelease/202105/t20210510_1817185.html (Accessed December 15, 2023).
28. Kong, D, Liu, S, Hong, Y, Chen, K, and Luo, Y. Perspectives on the popularization of smart senior care to meet the demands of older adults living alone in communities of Southwest China: a qualitative study. Front Public Health. (2023) 11:1094745. doi: 10.3389/fpubh.2023.1094745
29. Specht, S, Schwarzkopf, L, Braun-Michl, B, Seitz, N-N, Wildner, M, and Kraus, L. Age, period, and cohort effects on trends in outpatient addiction care utilization in the general Berlin population from 2008 to 2016. BMC Public Health. (2022) 22:320. doi: 10.1186/s12889-022-12744-6
30. Alarcon, FJ. The migrant crisis and access to health care. Delaware J Public Health. (2022) 8:20–5. doi: 10.32481/djph.2022.10.006
31. Flores, MJ. Aging and undocumented: the sociology of aging meets immigration status. Sociol Compass. (2021) 15:e12859. doi: 10.1111/soc4.12859
32. Anyanwu, FC, Akinsola, HA, Tugli, AK, and Obisie-Nmehielle, N. A qualitative assessment of the influence of family dynamics on adolescents' sexual risk behaviour in a migration-affected community. Int J Qual Stud Health Well Being. (2020) 15:1717322. doi: 10.1080/17482631.2020.1717322
33. Soboleva, MS, Loskutova, EE, and Kosova, IV. Problems of purchasing pharmacy products through online orders. J Adv Pharm Technol Res. (2022) 13:286–90. doi: 10.4103/japtr.japtr_454_22
34. Soleimanvandiazar, N, Kamal, H, Sajjadi, H, Ghaedamini Harouni, G, Karimi, S, Djalalinia, S, et al. Determinants of outpatient health service utilization according to Andersen's behavioral model: a systematic scoping review. Iranian. J Med Sci. (2020) 45:405–24. doi: 10.30476/ijms.2020.85028.1481
35. Hu, H, Jian, W, Fu, H, Zhang, H, Pan, J, and Yip, W. Health service underutilization and its associated factors for chronic diseases patients in poverty-stricken areas in China: a multilevel analysis. BMC Health Serv Res. (2021) 21:707. doi: 10.1186/s12913-021-06725-5
36. Rogus, S. Examining the influence of perceived and objective time constraints on the quality of household food purchases. Appetite. (2018) 130:268–73. doi: 10.1016/j.appet.2018.08.025
37. Gubernskaya, Z. Age at migration and self-rated health trajectories after age 50: understanding the older immigrant health paradox. J Gerontol Ser B. (2014) 70:279–90. doi: 10.1093/geronb/gbu049
38. Au, N, and Johnston, DW. Self-assessed health: what does it mean and what does it hide? Soc Sci Med. (1982) 121:21–8. doi: 10.1016/j.socscimed.2014.10.007
39. Paul, P, Nguemdjo, U, Kovtun, N, and Ventelou, B. Does self-assessed health reflect the true health state? Int J Environ Res Public Health. (2021) 18:111153. doi: 10.3390/ijerph182111153
40. Llorca, M, Rodriguez-Alvarez, A, and Jamasb, T. Objective vs. subjective fuel poverty and self-assessed health. Energy Econ. (2020) 87:104736. doi: 10.1016/j.eneco.2020.104736
41. Hawkins, MM, Holliday, DD, Weinhardt, LS, Florsheim, P, Ngui, E, and AbuZahra, T. Barriers and facilitators of health among older adult immigrants in the United States: an integrative review of 20 years of literature. BMC Public Health. (2022) 22:755. doi: 10.1186/s12889-022-13042-x
42. Si, X, and Chu, F-L. The impact of the public pension program on the elderly’s medical expenditures: a regression discontinuity approach. J Appl Econ. (2022) 25:178–96. doi: 10.1080/15140326.2021.2021748
43. Strauss, R, Pfeifer, C, Ulmer, H, Mühlberger, V, and Pfeiffer, KP. Spatial analysis of percutaneous transluminal coronary angioplasty (PTCA) in Austria. Eur J Epidemiol. (1999) 15:451–9. doi: 10.1023/a:1007577516433
44. Coste, M, and M-a-Q, B. Predicting health services utilization using a score of perceived barriers to medical care: evidence from rural Senegal. BMC Health Serv Res. (2023) 23:263. doi: 10.1186/s12913-023-09192-2
45. Jiang, M, Yang, G, Fang, L, Wan, J, Yang, Y, and Wang, Y. Factors associated with healthcare utilization among community-dwelling elderly in Shanghai, China. PLoS One. (2018) 13:e0207646. doi: 10.1371/journal.pone.0207646
46. Izquierdo, M, Duque, G, and Morley, JE. Physical activity guidelines for older people: knowledge gaps and future directions. Lancet Healthy Longev. (2021) 2:e380–3. doi: 10.1016/s2666-7568(21)00079-9
47. Musich, S, Wang, SS, Ruiz, J, Hawkins, K, and Wicker, E. The impact of mobility limitations on health outcomes among older adults. Geriatr Nurs. (2018) 39:162–9. doi: 10.1016/j.gerinurse.2017.08.002
48. Wu, N, Xie, X, Cai, M, Han, Y, and Wu, S. Trends in health service needs, utilization, and non-communicable chronic diseases burden of older adults in China: evidence from the 1993 to 2018 National Health Service Survey. Int J Equity Health. (2023) 22:169. doi: 10.1186/s12939-023-01983-7
49. Fulmer, T, Reuben, DB, Auerbach, J, Fick, DM, Galambos, C, and Johnson, KS. Actualizing better health and health care for older adults. Health Aff (Millwood). (2021) 40:219–25. doi: 10.1377/hlthaff.2020.01470
50. Cylus, J, and Al, TL. Health, an ageing labour force, and the economy: does health moderate the relationship between population age-structure and economic growth? Soc Sci Med. (1982) 287:114353. doi: 10.1016/j.socscimed.2021.114353
51. Fang, EF, Xie, C, Schenkel, JA, Wu, C, Long, Q, Cui, H, et al. A research agenda for ageing in China in the 21st century (2nd edition): focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. (2020) 64:101174. doi: 10.1016/j.arr.2020.101174
52. Cachioni, M, Cipolli, GC, Borim, FSA, Batistoni, SST, Yassuda, MS, Neri, AL, et al. Factors associated with positive self-rated health: comparing older adults in Brazil and in Portugal [original research]. Front Public Health. (2021) 9:650294. doi: 10.3389/fpubh.2021.650294
53. Ansah, JP, and Chiu, CT. Projecting the chronic disease burden among the adult population in the United States using a multi-state population model. Front Public Health. (2022) 10:1082183. doi: 10.3389/fpubh.2022.1082183
54. Wang, LM, Chen, ZH, Zhang, M, Zhao, ZP, Huang, ZJ, Zhang, X, et al. Study of the prevalence and disease burden of chronic disease in the elderly in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2019) 40:277–83. doi: 10.3760/cma.j.issn.0254-6450.2019.03.005
55. Zhang, L, Ma, L, Sun, F, Tang, Z, and Chan, P. A multicenter study of multimorbidity in older adult inpatients in China. J Nutr Health Aging. (2020) 24:269–76. doi: 10.1007/s12603-020-1311-x
56. Tsimihodimos, V, Gonzalez-Villalpando, C, Meigs, JB, and Ferrannini, E. Hypertension and diabetes mellitus: coprediction and time trajectories. Hypertension. (2018) 71:422–8. doi: 10.1161/hypertensionaha.117.10546
57. Petrie, JR, Guzik, TJ, and Touyz, RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol. (2018) 34:575–84. doi: 10.1016/j.cjca.2017.12.005
58. van Hees, SGM, O'Fallon, T, Hofker, M, Dekker, M, Polack, S, Banks, LM, et al. Leaving no one behind? Social inclusion of health insurance in low- and middle-income countries: a systematic review. Int J Equity Health. (2019) 18:134. doi: 10.1186/s12939-019-1040-0
59. Zhang, X, and Zhang, L. The impact of instant reimbursement of cross-regional medical services on hospitalization costs incurred by the floating population-evidence from China. Healthcare. (2022) 10:1099. doi: 10.3390/healthcare10061099
60. McMaughan, DJ, Oloruntoba, O, and Smith, ML. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Front Public Health. (2020) 8:231. doi: 10.3389/fpubh.2020.00231
61. Ryu, S, and Fan, L. The relationship between financial worries and psychological distress among U.S. Adults J Family Econ Iss. (2023) 44:16–33. doi: 10.1007/s10834-022-09820-9
Keywords: migrant older adults, outpatient services, inpatient services, Anderson’s model, influencing factors
Citation: Li G, Qi Z, Yu W, Wang Q, Hou H, Miao C, Yan W and Gao X (2024) Factors influencing utilization of healthcare services for internal migrant older adults in Xuzhou, China: based on Anderson’s model. Front. Public Health. 12:1378790. doi: 10.3389/fpubh.2024.1378790
Edited by:
Wei Zhou, Yunnan University of Finance and Economics, ChinaReviewed by:
Carol Galletly, Medical College of Wisconsin, United StatesM. Alvi Syahrin, Immigration Polytechnic, Indonesia
Copyright © 2024 Li, Qi, Yu, Wang, Hou, Miao, Yan and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiuyin Gao, MTAwMDAwNDAxMDA0QHh6aG11LmVkdS5jbg==
†These authors have contributed equally to this work
 Guiyuan Li
Guiyuan Li Zijian Qi1†
Zijian Qi1† Qingzhi Wang
Qingzhi Wang Hao Hou
Hao Hou Xiuyin Gao
Xiuyin Gao