- 1Department of Family and Community Medicine, College of Medicine Jouf University, Sakaka, Saudi Arabia
- 2Department of Compliance, Ministry of Health, Arar, Saudi Arabia
- 3College of Medicine Jouf University, Sakaka, Saudi Arabia
- 4Family Medicine Resident, Ministry of Health, Tabuk, Saudi Arabia
Background and aim: The global healthcare system acknowledged the crucial role of disease knowledge in health outcomes and improving quality of life among patients with chronic disease. A lack of adequate knowledge and understanding of hypertension, its symptoms, and available treatments can lead to poor treatment outcomes. The present study aimed to determine the level of hypertension knowledge and associated factors among hypertensive patients. Furthermore, we evaluated the correlation between levels of knowledge and medication adherence among them.
Methods: The present study was carried out among 406 hypertensive patients attending different primary health centers in Hafr Al Batin, Saudi Arabia. Participants’ hypertension-related knowledge was evaluated using the validated hypertension knowledge–level scale, and adherence practice was evaluated using the medication adherence and refill scale. We categorized the knowledge score into low, medium, and high, according to Bloom’s criteria. We applied Spearman’s correlation test to find the strength and direction of the correlation between hypertension-related knowledge and medication adherence. Furthermore, we used binomial logistic regression analysis to find the associated factors of the low hypertension-related knowledge among the patients.
Results: Of the studied patients, only 10.3% demonstrated a high level of knowledge, and the highest knowledge levels were observed in the domains of complications (
Conclusion: The study findings highlight a moderate level of knowledge about hypertension among patients, with significant gaps in drug compliance understanding. The positive correlation between knowledge and medication adherence underscores the need for better hypertension education at primary health centers. Furthermore, it is recommended that future prospective studies be conducted within various cultural contexts.
1 Introduction
Hypertension is a chronic medical condition characterized by elevated blood pressure. The World Health Organization (WHO) has estimated that about 1.3 billion people suffer from hypertension worldwide, and nearly half of them are not aware of their hypertension status (1). Hence, it is increasingly emerging as a worldwide public health concern, encompassing a significant portion of public health financial allocations (2, 3). The prevalence of hypertension exhibits variation across different countries, with a notable upward trend observed in developing nations (4, 5). People with uncontrolled hypertension are at high risk of experiencing heart failure, renal failure, atherosclerosis, and stroke (6, 7). Hypertension, however, is preventable, treatable, and can be managed through medication (2, 8).
A higher risk of negative consequences, such as hospitalization and higher healthcare expenses due to problems, is seen in individuals with poor adherence to antihypertensive drugs compared to those with strong adherence. So, medication adherence is necessary to achieve blood pressure control. Medication adherence refers to the percentage of patients who take their prescribed medications as their treating physician recommends (9, 10). Peacock and Krousel-Wood report that only 50% of people with “chronic diseases medication,” for instance, hypertensive patients, adhere to their medication regimen as prescribed (11). Another research conducted in 2022 among hypertensive adult patients (18+ years) attending primary health centers (PHC) in the Kingdom of Saudi Arabia (KSA) shows that only 36% of the hypertensive patients had high adherence to the treatment (12). In contrast, a comprehensive survey conducted in the United States, including an extensive sample of 24 million individuals diagnosed with hypertension, has revealed that a notable proportion, specifically about one-third, exhibited nonadherence to their prescribed drug regimen (13).
The global healthcare system acknowledges the crucial role of disease knowledge in health outcomes and improving quality of life among patients with chronic disease. Health professionals should provide patients with information about the benefits of taking their drugs and how to ensure that they are taking them as prescribed, which is essential to help patients control their blood pressure in the long term and reduce the risk of developing complications of hypertension (14, 15). An integrated approach to managing hypertension and increasing literacy levels among hypertensive patients and healthcare professionals is essential. The physicians and other healthcare practitioners must then collaborate to ensure success in helping patients avoid complications related to high blood pressure (16, 17). One way to achieve this is through a shared decision-making (SDM) model. Shared decision-making refers to a collaborative decision-making process in which all involved in the decision-making process have a stake in the outcome. The SDM model is particularly effective in managing chronic conditions like hypertension, where long-term adherence to treatment plans is crucial. By involving patients in the decision-making process, they are more likely to understand the importance of their medication regimen, lifestyle modifications, and the potential consequences of nonadherence (18, 19). Educating hypertensive patients is necessary to make them aware of the condition and the available medications so that they can make informed decisions about their care (17, 20). This collaborative approach can improve patient satisfaction, adherence to treatment, and overall health outcomes (21, 22).
A lack of adequate knowledge, awareness, and understanding of hypertension, its symptoms, and available treatments can lead to poor treatment adherence. Furthermore, a good knowledge about disease improves self-management, which is critical for patients to self-manage their situations (23). Studies have consistently shown that a lack of knowledge is a significant factor associated with poor adherence, and patients with a lack of knowledge are more likely to discontinue medications for several reasons (24, 25). Moreover, some studies have shown that knowledge regarding hypertension is generally low among hypertensive patients in KSA. Among those with some knowledge, there was a significant correlation between knowledge level, blood pressure control, and medication adherence (26, 27).
In the KSA, healthcare is delivered at four levels: PHCs, general hospitals, specialty hospitals, and medical cities. PHCs are integral to the healthcare system and provide essential services, including the diagnosis, management, and follow-up of chronic diseases such as hypertension. Continuous monitoring of epidemiological characteristics related to hypertension, such as knowledge of hypertension in terms of risk factors, complications, treatment compliance, and lifestyle factors among the patients attending PHCs, is critical to planning and implementing an intervention program to address the knowledge gap, eventually to improve the medication adherence and health of the individuals with hypertension. Furthermore, the sociocultural and demographic characteristics of each region of KSA, including Eastern Province, differ highly. Hence, there is an absolute necessity for region-specific data and evaluation. Understanding the local context and challenges in this specific region can inform tailored interventions and improve hypertension management practices in this region. Considering these factors, we aimed to assess the level of hypertension knowledge and associated factors among the patients attending different PHCs of Hafr Al Batin. Furthermore, we assessed the correlation between levels of knowledge and medication adherence among them.
2 Participants and methods
2.1 Study design
The present study was an analytical cross-sectional study that was performed from June 2023 to December 2023.
2.2 Study setting
The present survey was conducted among the patients attending different PHCs of Hafr-Al Batin. Hafr Al-Batin is in the Eastern province of KSA, with a total population of approximately about 400,000. These centers are critical in diagnosing, treating, and educating patients about hypertension, thereby playing a crucial role in mitigating its complications and improving the overall health outcomes of the patients. There are 73 PHCs in this region, and the present study selected 10 PHCs randomly to recruit hypertensive patients for the current survey. In order to recruit hypertensive patients over a period of time, we restricted five patients per day in each PHC.
2.3 Sample size estimation and sampling method
We used the World Health Organization (WHO) sample size formula (n = z2pq /e2) to estimate the required number of adults to participate in the present survey. The WHO formula uses the principles of Cochran’s sample size calculation method, a commonly used method to calculate the minimum required sample size in a cross-sectional study (28). During estimation, we considered 50% of expected adequate knowledge (p), q = 1-p, 95% of the confidence interval (z = 1.96), and 5% of the margin of error (d). After carefully calculating the above-stated values, we concluded that 384 participants are required for the survey (rounded to 390). These required participants were selected from 10 randomly selected PHCs. In this study, we applied a non-probability consecutive sampling method, a type of convenience sampling where participants were consecutively selected based on their availability and meeting the inclusion criteria until the required sample size was achieved. Furthermore, we restricted our data collection per day to a maximum of 10 participants to ensure that the data is collected over a period of time.
2.4 Inclusion and exclusion criteria
We included all adult-confirmed hypertensive patients who were on antihypertensive medications for a minimum of 3 months and attended the outpatient clinics of the PHCs from the Hafr Al-Batin region. The 3 months duration was determined by the research team through a focus group discussion considering the guidelines of follow-up visit (29, 30). We excluded pediatric patients, pregnant women, patients from other regions, and patients who were unwilling to participate.
2.5 Data collection procedure
The present research followed the ethical principles of the Declaration of Helsinki during the entire study duration. We initiated the data collection after obtaining ethical clearance from the research committee, the Ministry of Health, Hafr Al-batin (approval no: 134), and other necessary approvals from the concerned authorities. After briefing the survey to the hypertensive patients and obtaining informed consent, we gave the participants the Arabic version of the data collection tool (Google form). This was on the day of their visit to the health center, and the data was filled in the data collectors’ electronic devices. The data collection tool is a standard, pretested, and validated tool adapted from previous literature (12, 31–33). The first section inquired about participants’ background and health-related aspects: age, gender, income, occupation, education, presence of other comorbidities, duration since the first diagnosis of hypertension, and the number of medications taken for hypertension. The second part asked about participants’ hypertension-related knowledge using the hypertension knowledge–level scale (HK-LS) (32, 34). The HK-LS consists of 22 items to investigate participants’ knowledge regarding six subscales, including definition (two items), medical treatment (four items), drug compliance (four items), lifestyle (five items), diet (two items), and complications (five items). The correct answer was given 1 point, and the wrong answer, not sure, was given zero. Participants’ overall knowledge was based on summing up the correct responses to these items. Therefore, the overall knowledge scores ranged between 0 and 22. We further categorized them into low (less than 60% of total score), medium (60 to 80% of total score), and high (more than 80% of total score). The research team determined these categories according to Bloom’s criteria, which is used in several studies (35–37). The final section inquired about medication adherence and refill practices among the selected participants and consisted of 10 questions (12, 31). Hypertensive patients responded with a range of answers, from never (score 4) to always (score 1). The scores of each item were summed up to get the total scores for further analysis. The higher scores indicate a higher adherence practice. Initially, we pretested the tool among 30 adult hypertensive patients. All pilot study patients were informed that the data collection tool was simple and easy to understand. The Cronbach alpha values for the knowledge and adherence sections that were obtained through pilot study were 0.79 and 0.83, respectively.
2.6 Statistical analysis
The research team downloaded the Excel sheet from Google Form and exported it to the Statistical Package for Social Sciences (SPSS) version 23.0 for data entry, coding, and analysis. We presented the descriptive data as frequency, proportion, mean/median, and standard deviation/interquartile range. The normality assumption of the data was analyzed through the Shapiro–Wilk test. The test revealed that both hypertension-related knowledge scores (statistical value = 0.971, p < 0.001) and medication adherence scores (statistical value = 0.982, p < 0.001) did not meet the normality assumption. Hence, we applied Spearnman’s correlation test (non-parametric test) to find the correlation between knowledge and medication adherence practice. Furthermore, we used the binary logistic regression analysis (enter method) to find the factors for the knowledge categories. In this regression model, we calculated the odds ratio with a 95% confidence interval after adjusting with other covariables of the study. A p-value less than 0.05 will be considered a statistically significant association.
3 Results
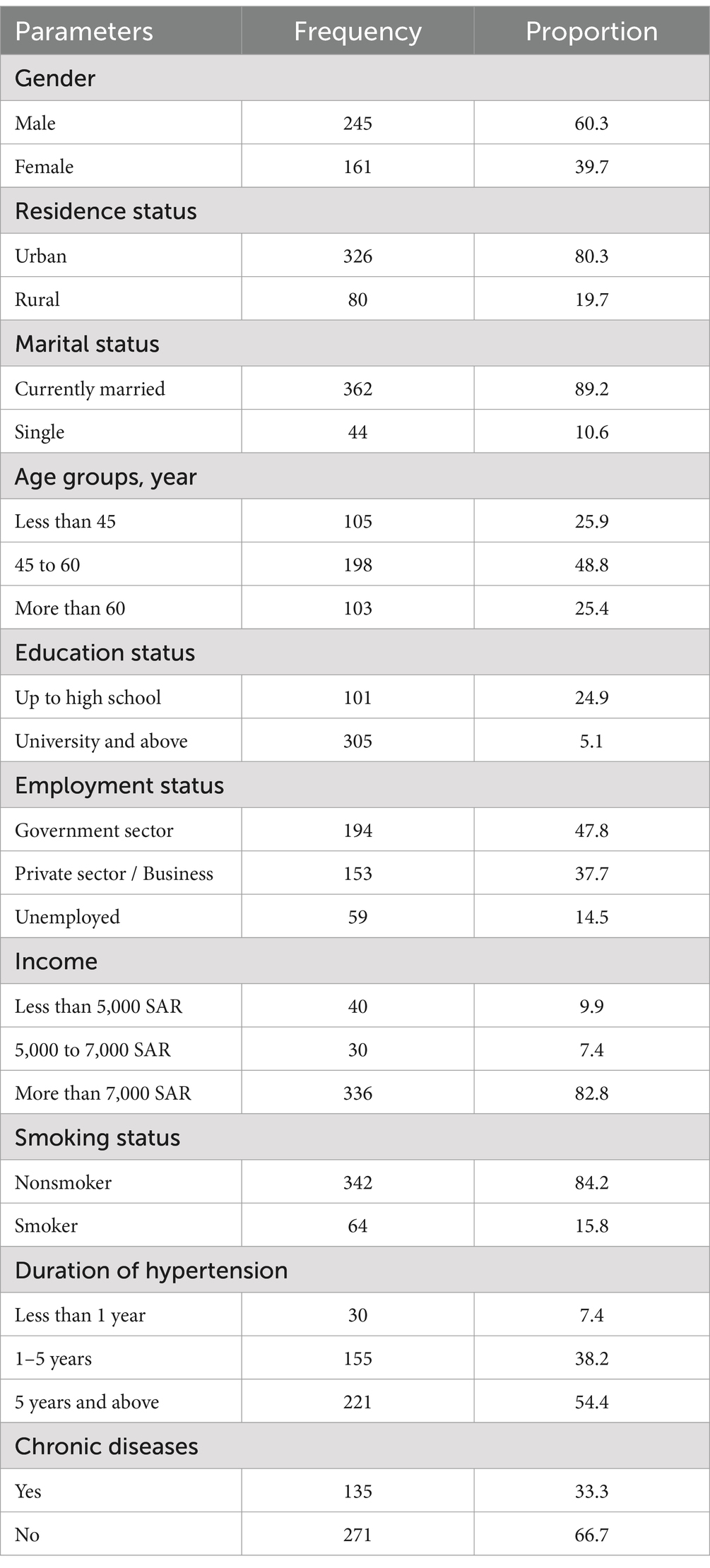
The majority of participants were male (60.3%), residing in urban areas (80.3%), and currently married (89.2%). Nearly half of the participants belonged to the age group of 45 to 60 years, comprising 48.8% of the total respondents. Most participants had a university degree or higher (75.1%). Almost half of the participants were employed in the government sector (47.8%). The vast majority of participants had an income exceeding 7,000 SAR (82.8%). Most participants were non-smokers (84.2%). Over half of the participants had hypertension for 5 years or above (54.4%). One-third of the participants reported having chronic diseases (33.3%; Table 1).
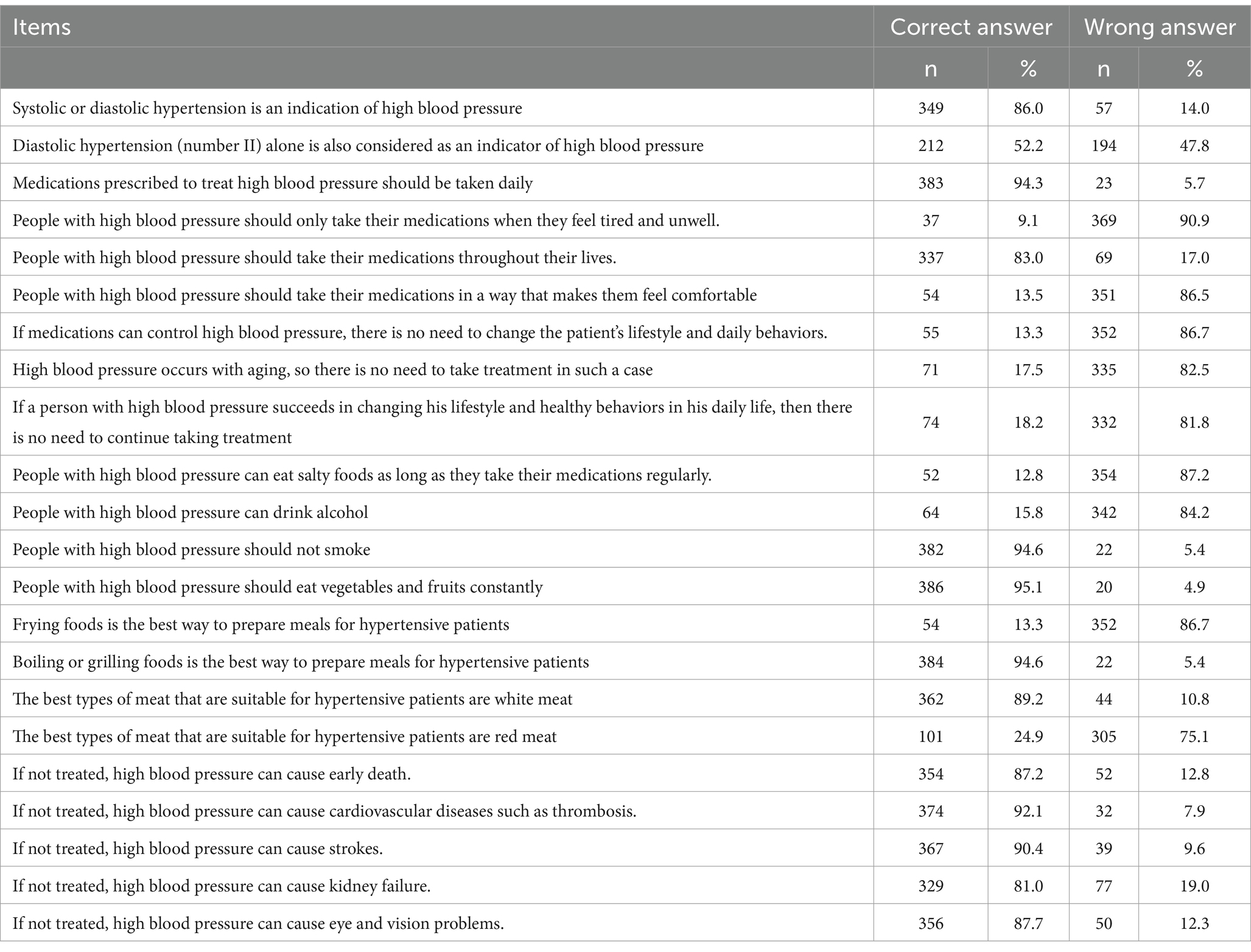
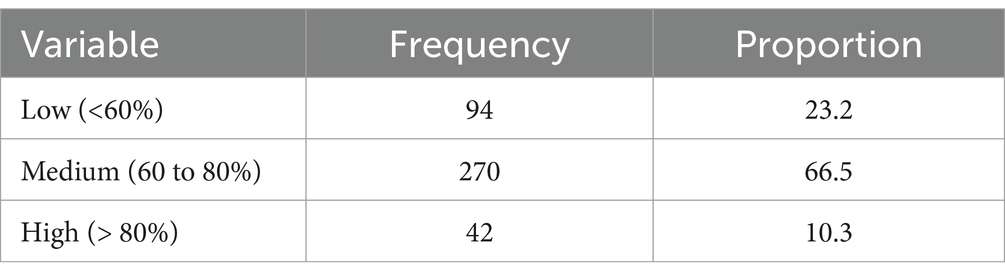
The study participants demonstrated a relatively high awareness of fundamental aspects of hypertension, such as the importance of daily medication intake (94.3%) and the necessity of lifelong medication adherence (83.0%). However, a considerable proportion of study participants believe that high blood pressure only occurs with aging (17.5%) and that lifestyle changes can negate the need for medication (18.2%). Moreover, there were notable gaps in knowledge regarding dietary habits, as a significant number thought it was permissible for hypertensive individuals to consume salty foods (12.8%) or drink alcohol (15.8%). Furthermore, the highest levels of wrong answers were observed on the knowledge of the statements: people with high blood pressure should only take their medications when they feel tired and unwell (90.9%), people with high blood pressure can eat salty foods as long as they take their medications regularly (87.2%), and type of food intake such as frying food (86.7%). The majority of participants have a medium level of knowledge (51 to 75%), and only 10.3% demonstrate a high level of knowledge (above 75%; Tables 2, 3).
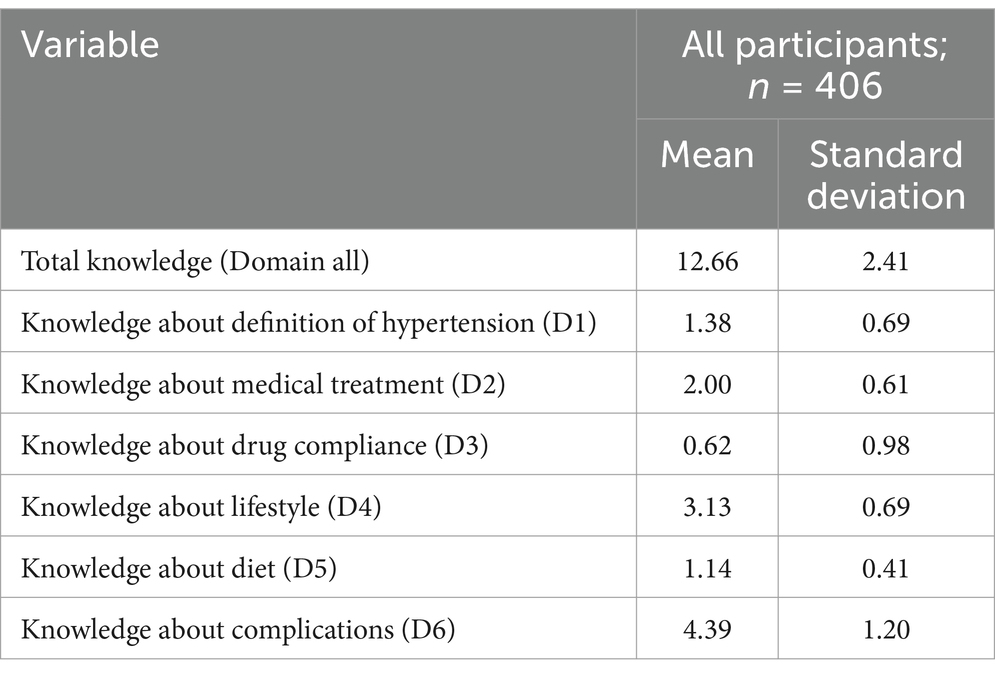
The overall mean knowledge score for hypertension among the 406 participants was 12.66 (SD = 2.41), indicating a moderate level of knowledge. Participants demonstrated the highest knowledge levels in the domains of complications ( = 4.39, SD = 1.20) and lifestyle ( = 3.13, SD = 0.69), while knowledge about drug compliance ( = 0.62, SD = 0.98) was the lowest (Table 4).
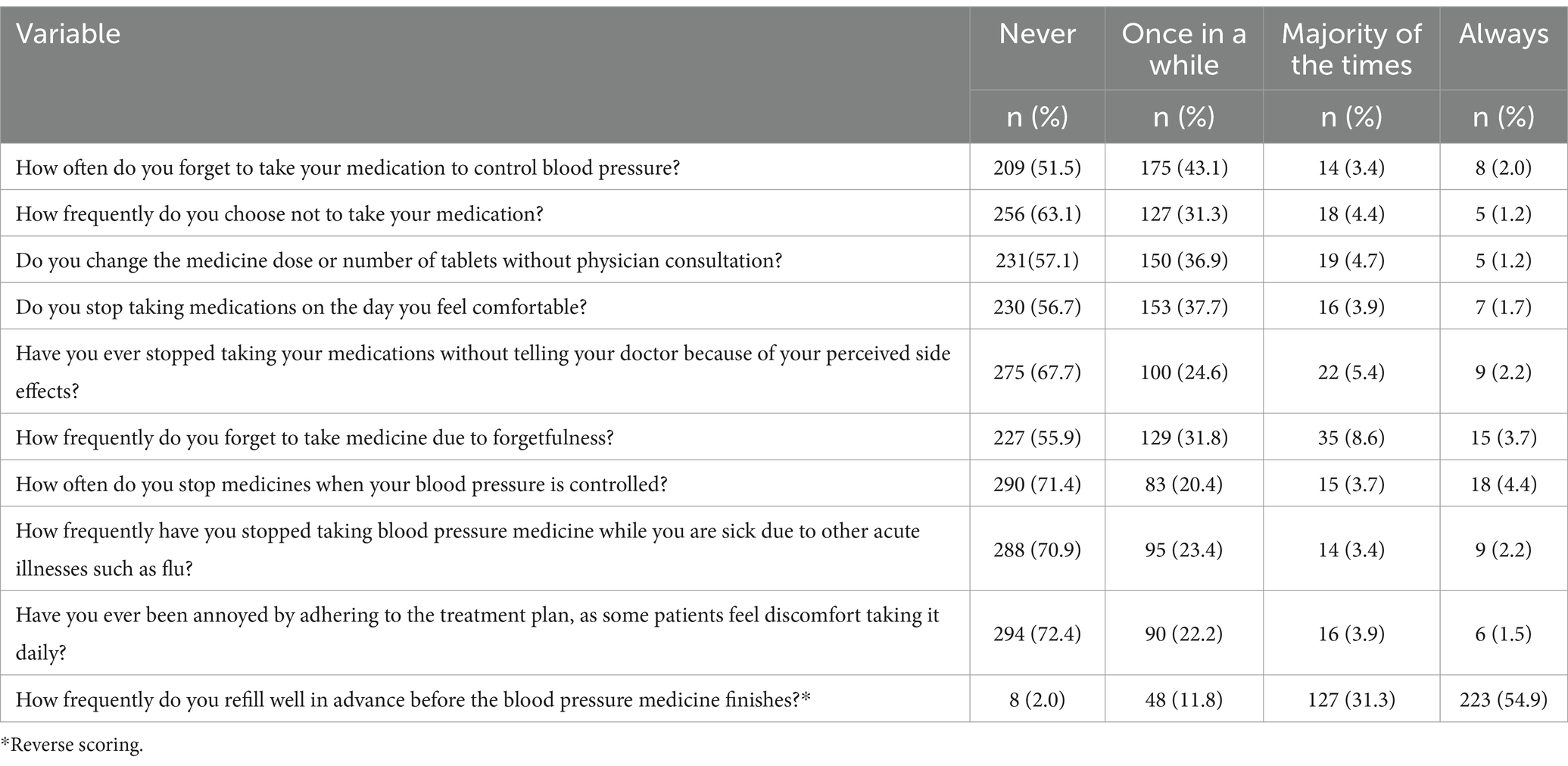
Regarding antihypertensive medication adherence, 51.5% of the patients never forget to take their medicines, and more than two-thirds (71.4%) of the patients never stopped their medicines even when their blood pressure is controlled. Similarly, about 55% of patients always refill their antihypertensive medications well in advance before they finish (Table 5).
A statistically significant positive correlation was observed between knowledge and adherence regarding hypertension (rho = 0.268, p = 0.001) among study participants (Table 6).
In the univariate analysis, several socio-demographic factors were identified as predictors of knowledge about hypertension. Participants aged 45 to 60 years (crude odds ratio [COR] = 0.339, 9% confidence interval [CI] = 0.180–0.639, p = 0.001), females (COR = 2.058, 95% CI = 1.290–3.282, p = 0.002), those residing in rural areas (COR = 4.687, 95% CI = 2.771–7.927, p = 0.001), employed in the private sector/business (COR = 2.206, 95% CI = 1.192–4.084, p = 0.012), unmarried individuals (COR = 6.245, 95% CI = 3.240–12.038, p = 0.001), those with high income, non-smokers (COR = 0.299, 95% CI = 0.124–0.716, p = 0.001), and those with 1 to 5 years of hypertension duration (COR = 0.224, 95% CI = 0.102–0.492, p = 0.001) were significantly associated with the hypertension related knowledge. After adjusting for confounding factors in the multivariate analysis, marital status (adjusted odds ratio [AOR] = 2.538, 95% CI = 1.086–5.932, p = 0.032), income (AOR = 0.364, 95% CI = 0.138–0.963, p = 0.042), and absence of chronic diseases (AOR = 0.491, 95% CI = 0.260–0.932, p = 0.001) remained significant predictors of knowledge about hypertension (Table 7).
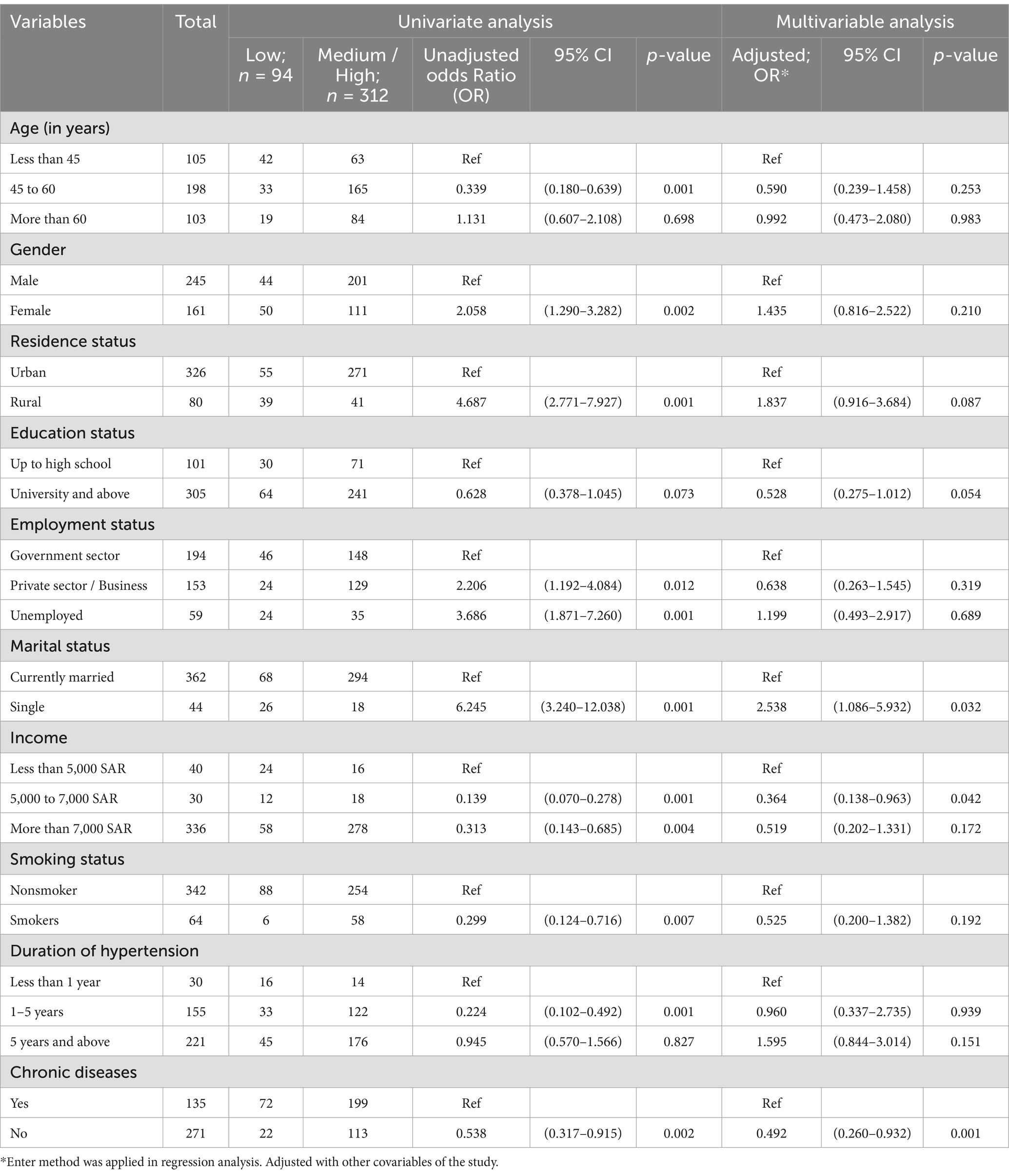
Table 7. Univariate and multivariate regression analysis for the predictors of knowledge regarding hypertension.
4 Discussion
Hypertension poses a significant public health burden worldwide. In KSA, its prevalence is alarming, with one in four adults estimated to have the condition (38). To effectively combat this challenge, understanding the knowledge about hypertension and adherence to hypertensive medication of hypertensive individuals is crucial. The present study delves into the knowledge and medication adherence landscape among patients attending various primary health centers in Saudi Arabia, offering valuable insights for tailored interventions and improved health outcomes. The findings from this study underscore the ongoing challenge of managing hypertension in Saudi Arabia, particularly in the Eastern region.
Overall, participants’ knowledge about hypertension was moderate (mean 2.66), which is similar to research conducted in Lebanon (39), Sri Lanka (24), Indonesia (25), and Pakistan (40). However, specific knowledge domains revealed notable disparities. Participants demonstrated a strong understanding of complications (mean 4.39) and lifestyle modifications (mean 3.13), aligning with the research findings of Buang NFB et al. (41) and Alshammari SA et al. (42). Conversely, a significant knowledge gap was identified in our study regarding drug compliance (mean 0.62), similar to the concerns raised in studies from India (43) and Pakistan (44). The current study highlights the persistent knowledge gaps that could contribute to suboptimal health outcomes.
The present study also reports that the participants have poor knowledge in the domains “definition and diet.” This finding is similar to the study done by Al Zahrani S et al. (26) and Jankowska-Polańska B et al. (45). Low scores in understanding definitions, diet, and drug compliance may be attributed to various factors. These could include unclear communication from healthcare providers, insufficient awareness of the significance of medication adherence, or cultural beliefs influencing medication use. Exploring these contributing factors can guide the development of targeted interventions. Tailored interventions like communication training for health care providers and behavioral change communication to the community will address these root causes and empower individuals and communities for improved health outcomes. The present study found several domains related to medication adherence and proper diet. These results emphasize the importance of the SDM model, as many patients were unaware of the importance of medication adherence even if they felt well and the importance of proper dietary methods. Furthermore, as a process of SDM, healthcare professionals must provide patients with comprehensive information about the benefits of medications even if the patients are feeling well, the role of lifestyle changes in managing hypertension, and the importance of regular monitoring and follow-up. Additionally, addressing patients’ concerns, preferences, and values is crucial in developing a personalized treatment plan that patients are more likely to follow (18, 46, 47).
In our study, about half of the participants responded as “always” in most of the medication adherence scale items. This aligns with recent findings by Amer M et al. (40), Lee EK et al. (48) Shi S et al. (49), and Gavrilova A et al. (50), high prevalence of nonadherence to antihypertensive medication globally with non-western countries showing even higher rates (48). These stark figures underscore the persistent challenge of medication nonadherence in chronic disease management, particularly in hypertension, affecting over 1.3 billion people globally, as highlighted by the World Health Organization in 2023 (51). This warrants further investigation into the specific factors influencing adherence patterns within low-adherence populations. Exploring modifiable factors, such as financial barriers, medication complexity, and patient-provider communication, could inform targeted interventions to improve adherence and ultimately optimize clinical outcomes, especially in the context of hypertension, where uncontrolled blood pressure can lead to devastating consequences like heart attacks and strokes. Our study provides specific insights into these gaps, such as the limited understanding of drug compliance and diet, which are crucial for effective hypertension management. These insights emphasize the need for targeted educational interventions at primary health centers to enhance patients’ knowledge and adherence to treatment regimens.
Similar to the research findings by Amer M (40) and Paczkowska A et al. (52), the present study shows that knowledge about hypertension was found to have a statistically significant positive correlation with medication adherence with a coefficient of 0.268, indicating a positive association between medication adherence and knowledge about hypertension. Patients with an adequate knowledge of hypertension may better perceive the need for regular drug adherence in managing their disease, resulting in a better dedication to following prescribed treatment regimens. Furthermore, the correlation coefficient of 0.268 suggests a positive relationship between hypertension awareness and medication adherence, highlighting the importance of patient education in improving positive health behaviors. This can lead to better blood pressure control and overall health outcomes, reducing the burden on the healthcare system due to complications arising from poorly managed hypertension.
We found that the knowledge level of the participants about hypertension is influenced by factors such as education, income, marital status, and the presence of chronic conditions. Individuals who are married, have chronic illnesses, have lower incomes, and are less educated are more likely to have a lack of knowledge about hypertension. These results are consistent with studies conducted in Poland (52), Malaysia (41), Saudi Arabia (38), and Lebanon (39). These warrants targeted intervention, especially for people of lower socio-economic status, to effectively manage this significant global health problem. Hence, we can decrease the associated complications and healthcare expenditure (53, 54). In agreement with recommendations from previous global studies, the present study offers a road map for creating proper interventions to increase awareness of hypertension and medication adherence. Culturally tailored health promotion activities that address specific knowledge gaps and target high-risk groups and include social aspects of health are vital. These programs must actively address the fears and myths surrounding the illness in addition to merely providing information. Furthermore, integrating community-based interventions and encouraging self-management abilities can enable people to take charge of their health and enhance long-term results worldwide. Additionally, integrating regular counseling sessions during follow-ups in PHCs could help reinforce the importance of medication adherence and lifestyle modifications.
We have carried out this survey with an adequate sample size and a validated Arabic questionnaire. Nonetheless, the readers should consider some of the essential constraints of this research findings. Firstly, we assessed the knowledge gap among hypertensive patients in a unique sociocultural setting. Hence, the conclusions assessed in this study may not be applicable to other regions. Secondly, the limitations of cross-sectional studies, such as the lack of ability to identify the causal association, need to be kept in mind. Next, the study faced limitations due to the non-probability consecutive sampling method, which may have introduced selection bias. Additionally, the higher proportion of male participants reflects sociocultural restrictions, affecting generalizability. Finally, some other biases, such as recall and self-report, cannot be ruled out.
5 Conclusion
We found that the majority of the participants had either low or medium knowledge of hypertension. Furthermore, a positive correlation was observed between hypertension-related knowledge and medication adherence. The results emphasize the need for better hypertension education at the primary health centers. It also emphasizes the need for culturally sensitive interventions that fill in knowledge gaps and provide people with the tools they need to take charge of their health. These issues can be effectively addressed by adopting targeted interventions for the high-risk population and the prevalence of hypertension in Saudi Arabia, enabling people to properly manage their health and enhance their quality of life. To contribute to a comprehensive understanding of this global challenge, it is recommended that future prospective studies be conducted to examine the factors influencing drug adherence, lifestyle modifications, and healthcare expenditure within a variety of cultural contexts.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by IRB, Directorate of Health Affairs, Hafr Al Batin, Saudi Arabia. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AA-H: Conceptualization, Data curation, Methodology, Software, Supervision, Validation, Writing – original draft, Funding acquisition, Resources. AMA: Conceptualization, Data curation, Formal analysis, Validation, Visualization, Writing – original draft, Methodology, Resources, Software. AT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Project administration, Software, Visualization, Writing – original draft, Methodology. NA: Conceptualization, Formal analysis, Funding acquisition, Methodology, Validation, Visualization, Writing – original draft, Investigation. MMA: Conceptualization, Data curation, Resources, Software, Validation, Writing – review & editing, Visualization. ASA: Conceptualization, Data curation, Methodology, Resources, Software, Validation, Writing – review & editing. MSA: Data curation, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing. AA: Conceptualization, Data curation, Formal analysis, Project administration, Visualization, Writing – review & editing, Resources, Software.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was funded by the Deanship of Graduate Studies and Scientific Research at Jouf University under grant no. (DGSSR-2023-01-02069).
Acknowledgments
We would like to thank the Hafr Al Batin health affairs for their immense support in data collection from the patients.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. Hypertension: fact sheets Geneva, Switzerland: World Health Organization. (2022). Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension (Accessed on 2023, 15 March)
2. Jaffe, MG, DiPette, DJ, Campbell, NRC, Angell, SY, and Ordunez, P. Developing population-based hypertension control programs. Rev Panam Salud Publica. (2022) 46:e153. doi: 10.26633/rpsp.2022.153
3. Lemogoum, D. Challenge for hypertension prevention and control worldwide: the time for action. J Clin Hypertens (Greenwich). (2014) 16:554–6. doi: 10.1111/jch.12373
4. Alenazi, AM, and Alqahtani, BA. National and regional prevalence rates of hypertension in Saudi Arabia: a descriptive analysis using the National Survey Data. Front Public Health. (2023) 11:1092905. doi: 10.3389/fpubh.2023.1092905
5. Mills, KT, Stefanescu, A, and He, J. The global epidemiology of hypertension. Nat Rev Nephrol. (2020) 16:223–37. doi: 10.1038/s41581-019-0244-2
6. Mamaghani, EA, Hasanpoor, E, Maghsoodi, E, and Soleimani, F. Barriers to medication adherence among hypertensive patients in deprived rural areas. Ethiop J Health Sci. (2020) 30:85–94. doi: 10.4314/ejhs.v30i1.11
7. Poznyak, AV, Sadykhov, NK, Kartuesov, AG, Borisov, EE, Melnichenko, AA, Grechko, AV, et al. Hypertension as a risk factor for atherosclerosis: cardiovascular risk assessment. Front Cardiovasc Med. (2022) 9:959285. doi: 10.3389/fcvm.2022.959285
8. Carey, RM, Muntner, P, Bosworth, HB, and Whelton, PK. Prevention and control of hypertension: Jacc health promotion series. J Am Coll Cardiol. (2018) 72:1278–93. doi: 10.1016/j.jacc.2018.07.008
9. Kengne, AP, Brière, J-B, Zhu, L, Li, J, Bhatia, MK, Atanasov, P, et al. Impact of poor medication adherence on clinical outcomes and health resource utilization in patients with hypertension and/or dyslipidemia: systematic review. Expert Rev Pharmacoecon Outcomes Res (2023) 24:1–12. doi: 10.1080/14737167.2023.2266135
10. Gebreyohannes, EA, Bhagavathula, AS, Abebe, TB, Tefera, YG, and Abegaz, TM. Adverse effects and non-adherence to antihypertensive medications in University of Gondar Comprehensive Specialized Hospital. Clin Hypertension. (2019) 25:1. doi: 10.1186/s40885-018-0104-6
11. Peacock, E, and Krousel-Wood, M. Adherence to antihypertensive therapy. Med Clin North Am. (2017) 101:229–45. doi: 10.1016/j.mcna.2016.08.005
12. Thirunavukkarasu, A, Naser Abdullah Alshahrani, A, Mazen Abdel-Salam, D, Homoud Al-Hazmi, A, Farhan, AB, Awad Alsaidan, A, et al. Medication adherence among hypertensive patients attending different primary health centers in Abha, Saudi Arabia: a cross-sectional study. Patient Prefer Adherence. (2022) 16:2835–44. doi: 10.2147/ppa.S388365
13. Chang, TE, Ritchey, MD, Park, S, Chang, A, Odom, EC, Durthaler, J, et al. National Rates of nonadherence to antihypertensive medications among insured adults with hypertension, 2015. Hypertension. (2019) 74:1324–32. doi: 10.1161/hypertensionaha.119.13616
14. Wieczorek, M, Meier, C, Vilpert, S, Reinecke, R, Borrat-Besson, C, Maurer, J, et al. Association between multiple chronic conditions and insufficient health literacy: cross-sectional evidence from a population-based sample of older adults living in Switzerland. BMC Public Health. (2023) 23:253. doi: 10.1186/s12889-023-15136-6
15. Liu, L, Qian, X, Chen, Z, and He, T. Health literacy and its effect on chronic disease prevention: evidence from China’s data. BMC Public Health. (2020) 20:690. doi: 10.1186/s12889-020-08804-4
16. Satriana, A, Kadar, KS, and Saleh, A. Effect of health literacy towards medication compliance on elderly with hypertension: an updated literature review. Enferm Clin. (2021) 31:S802–6. doi: 10.1016/j.enfcli.2021.07.034
17. Nam, HJ, and Yoon, JY. Linking health literacy to self-Care in Hypertensive Patients with physical disabilities: a path analysis using a multi-mediation model. Int J Environ Res Public Health. (2021) 18:e3363. doi: 10.3390/ijerph18073363
18. Montori, VM, Ruissen, MM, Hargraves, IG, Brito, JP, and Kunneman, M. Shared decision-making as a method of care. BMJ Evid Based Med. (2023) 28:213–7. doi: 10.1136/bmjebm-2022-112068
19. Simmons, L, Leavitt, L, Ray, A, Fosburgh, B, and Sepucha, K. Shared decision making in common chronic conditions: impact of a resident training workshop. Teach Learn Med. (2016) 28:202–9. doi: 10.1080/10401334.2016.1146600
20. Kurnia, AD, Melizza, N, Ruhyanudin, F, Masruroh, NL, Prasetyo, YB, Setyowati, CI, et al. The effect of educational program on hypertension management toward knowledge and attitude among uncontrolled hypertension patients in rural area of Indonesia. Community Health Equity Res Policy. (2020) 42:181–8. doi: 10.1177/0272684X20972846
21. Hu, Q, Feng, Z, Zong, Q, Wang, J, Zheng, Z, and Feng, D. Analysis of factors that promote the participation of patients with chronic diseases in shared decision making on medication: a cross-sectional survey in Hubei Province, China. BMC Public Health. (2023) 23:2440. doi: 10.1186/s12889-023-17099-0
22. Ward, J, Kalsi, D, Barnett, N, Fulford, B, and Handa, A. Shared decision making in chronic medication use: scenarios depicting exemplary care. Res Soc Adm Pharm. (2020) 16:108–10. doi: 10.1016/j.sapharm.2019.04.047
23. Centre for Health Protection, Department of Health. Hypertension - the Preventable and Treatable Silent Killer United Kingdom. (2023). Available from: https://www.chp.gov.hk/en/features/28272.html#:~:text=Hypertension%20is%20a%20chronic%20disease (Accessed on 2023, 15 June 2023)
24. Pirasath, S, and Sundaresan, T. Descriptive cross-sectional study on knowledge, awareness and adherence to medication among hypertensive patients in a tertiary care center. Eastern Sri Lanka SAGE Open Med. (2021) 9:20503121211012497. doi: 10.1177/20503121211012497
25. Pristianty, L, Hingis, ES, Priyandani, Y, and Rahem, A. Relationship between knowledge and adherence to hypertension treatment. J Public Health Afr. (2023) 14:2502. doi: 10.4081/jphia.2023.2502
26. Al Zahrani, S, Eid Alosaimi, M, Alamrim, A, Alotaibi, M, Almatar, EA, and Almanea, BA. Association between knowledge and drug adherence in patients with hypertension in Saudi Arabia. Arch Pharm Pract. (2019) 10:71–6.
27. Duraihim, HA, Alghamdi, G, AlNemer, M, Abdulaal, AE, and Sayyari, AA. Blood pressure control, lifestyle and disease awareness of Saudi hypertensive patients. Saudi J Kidney Dis Transpl. (2019) 30:33–8. doi: 10.4103/1319-2442.252930
29. Unger, T, Borghi, C, Charchar, F, Khan, NA, Poulter, NR, Prabhakaran, D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. (2020) 75:1334–57. doi: 10.1161/HYPERTENSIONAHA.120.15026
30. PAHO/WHO. Hearts in the Americas: Protocols and Medications - Paho/Who | Pan American Health Organization: Pan American Health Organization. (2021). Available from: https://www.paho.org/en/hearts-americas/hearts-americas-protocols-and-medications (Accessed on 2023, 15 May)
31. Alammari, G, Alhazzani, H, AlRajhi, N, Sales, I, Jamal, A, Almigbal, TH, et al. Validation of an Arabic version of the adherence to refills and medications scale (arms). Healthcare (Basel). (2021) 9:e1430. doi: 10.3390/healthcare9111430
32. Eshah, NF, and Al-daken, LI. Assessing publics’ knowledge about hypertension in a community-dwelling sample. J Cardiovasc Nurs. (2016) 31:158–65. doi: 10.1097/JCN.0000000000000227
33. Alsaidan, AA, Alotaibi, SF, and Thirunavukkarasu, A. Medication adherence and its associated factors among patients with type 2 diabetes mellitus attending primary health centers of Eastern Province, Saudi Arabia. Medicina (Kaunas). (2023) 59:e989. doi: 10.3390/medicina59050989
34. Erkoc, SB, Isikli, B, Metintas, S, and Kalyoncu, C. Hypertension knowledge-level scale (Hk-ls): a study on development, validity and reliability. Int J Environ Res Public Health. (2012) 9:1018–29. doi: 10.3390/ijerph9031018
35. Thirunavukkarasu, A, Alsaidan, AA, Al-Ruwaili, AM, Alanazi, RBS, and Alruwaili, AMB. Knowledge, attitude, and practice towards evidence-based medicine among northern Saudi primary care physicians: a cross-sectional study. Healthcare (Basel). (2022) 10: e2285. doi: 10.3390/healthcare10112285
36. Machaalani, M, Fakhry, B, Zwaideh, M, Mendelek, K, Mahmoud, N, Hammoud, T, et al. Knowledge, attitude, and practice toward cardiovascular diseases in the Lebanese population. Glob Heart. (2022) 17:47. doi: 10.5334/gh.1138
37. Yakut, S, Karagülle, B, Atçalı, T, Öztürk, Y, Açık, MN, and Çetinkaya, B. Knowledge, attitudes, practices and some characteristic features of people recovered from Covid-19 in Turkey. Medicina (Kaunas). (2021) 57:e431. doi: 10.3390/medicina57050431
38. Alshammari, SA, Alshammari, AS, Alshammari, HS, and Ahamed, SS. Overview of hypertension in Saudi Arabia: a systematic review and Meta-analysis. Saudi Med J. (2023) 44:951–64. doi: 10.15537/smj.2023.44.10.20230178
39. Machaalani, M, Seifeddine, H, Ali, A, Bitar, H, Briman, O, and Chahine, MN. Knowledge, attitude, and practice toward hypertension among hypertensive patients residing in Lebanon. Vasc Health Risk Manag. (2022) 18:541–53. doi: 10.2147/vhrm.S367187
40. Amer, M, Raza, A, Riaz, H, Sadeeqa, S, and Sultana, M. Hypertension-related knowledge, medication adherence and health-related quality of life (Hrqol) among hypertensive patients in Islamabad. Pakistan Tropical J Pharmaceutical Res. (2019) 18:1123–32. doi: 10.4314/tjpr.v18i5.30
41. Buang, NFB, Rahman, NAA, and Haque, M. Knowledge, attitude and practice regarding hypertension among residents in a housing area in Selangor. Malaysia Med Pharm Rep. (2019) 92:145–52. doi: 10.15386/mpr-1227
42. Alshammari, SA, Alshathri, AH, Alshathri, AH, Aleban, SA, Alabdullah, DW, Abukhlaled, JK, et al. Assessment of public knowledge of hypertension among the Saudi population. Cureus. (2023) 15:e37649. doi: 10.7759/cureus.37649
43. Shah, AJ, Singh, V, Patil, SP, Gadkari, MR, Ramchandani, V, and Doshi, KJ. Factors affecting compliance to antihypertensive treatment among adults in a tertiary Care Hospital in Mumbai. Indian J Community Med. (2018) 43:53–5. doi: 10.4103/ijcm.IJCM_40_17
44. Qasim, A, Qureshi, MI, Kumar, D, and Kashif, SM. Factors associated with compliance to antihypertensive therapy in patients visiting tertiary care hospital. Professional Med J. (2020) 27:1511–5. doi: 10.29309/TPMJ/2020.27.07.4552
45. Jankowska-Polańska, B, Uchmanowicz, I, Dudek, K, and Mazur, G. Relationship between Patients' knowledge and medication adherence among patients with hypertension. Patient Prefer Adherence. (2016) 10:2437–47. doi: 10.2147/ppa.S117269
46. Force, USPST. Collaboration and shared decision-making between patients and clinicians in preventive health care decisions and us preventive services task Force recommendations. JAMA. (2022) 327:1171–6. doi: 10.1001/jama.2022.3267
47. Merschel, M. What is shared decision-making, and how can it help patients? United States: American Heart Association (2023).
48. Lee, EKP, Poon, P, Yip, BHK, Bo, Y, Zhu, MT, Yu, CP, et al. Global burden, regional differences, trends, and health consequences of medication nonadherence for hypertension during 2010 to 2020: a Meta-analysis involving 27 million patients. J Am Heart Assoc. (2022) 11:e026582. doi: 10.1161/jaha.122.026582
49. Shi, S, Shen, Z, Duan, Y, Ding, S, and Zhong, Z. Association between medication literacy and medication adherence among patients with hypertension. Front Pharmacol. (2019) 10:822. doi: 10.3389/fphar.2019.00822
50. Gavrilova, A, Bandere, D, Rutkovska, I, Šmits, D, Mauriņa, B, and Poplavska, E. Urtāne AI knowledge about disease, medication therapy, and related medication adherence levels among patients with hypertension. Medicina (Kaunas). (2019) 55:e715. doi: 10.3390/medicina55110715
51. WHO. First who report details devastating impact of hypertension and ways to stop it. Geneva, Switzerland: World Health Organization (2023).
52. Paczkowska, A, Hoffmann, K, Kus, K, Kopciuch, D, Zaprutko, T, Ratajczak, P, et al. Impact of patient knowledge on hypertension treatment adherence and efficacy: a single-Centre study in Poland. Int J Med Sci. (2021) 18:852–60. doi: 10.7150/ijms.48139
53. Zhang, D, Wang, G, Zhang, P, Fang, J, and Ayala, C. Medical expenditures associated with hypertension in the U.S., 2000-2013. Am J Prev Med. (2017) 53:S164–71. doi: 10.1016/j.amepre.2017.05.014
Keywords: hypertension, knowledge, adherence, health center, complications, Saudi Arabia
Citation: Al-Hazmi AH, Alanazi ADM, Thirunavukkarasu A, Alriwely NS, Alrais MMF, Alruwaili ABS, Alnosairi MS and Alsirhani AI (2025) Evaluation of hypertension knowledge and its association with medication adherence among hypertensive patients attending primary health centers: a cross-sectional study from eastern Saudi Arabia. Front. Public Health. 12:1378561. doi: 10.3389/fpubh.2024.1378561
Edited by:
Xiaozhen Lai, Peking University, ChinaReviewed by:
Victoria Ramos Gonzalez, Carlos III Health Institute (ISCIII), SpainHuan-Keat Chan, Ministry of Health, Malaysia
Copyright © 2025 Al-Hazmi, Alanazi, Thirunavukkarasu, Alriwely, Alrais, Alruwaili, Alnosairi and Alsirhani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmad Homoud Al-Hazmi, YWhoYXptaUBqdS5lZHUuc2E=
†Present address: Nasser Saleh Alriwely, Department of Health Support Services, Ministry of Health, Riyadh, Saudi Arabia
 Ahmad Homoud Al-Hazmi1*
Ahmad Homoud Al-Hazmi1* Ashokkumar Thirunavukkarasu
Ashokkumar Thirunavukkarasu