
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Public Health , 17 May 2024
Sec. Substance Use Disorders and Behavioral Addictions
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1377688
This article is part of the Research Topic Substance Use Disorder: Above and Beyond Addiction, Volume II View all 27 articles
Background: Cannabis use may be increasing as countries legalize it and it becomes socially acceptable. A history of cannabis use may increase risk of complications after various kinds of surgery and compromise functional recovery. Here we systematically reviewed and meta-analyzed available evidence on how history of cannabis use affects recovery after hip or knee arthroplasty (THA/TKA).
Methods: The PubMed, EMBASE, and Web of Science databases were comprehensively searched and studies were selected and analyzed in accordance with the PRISMA guidelines. The methodological quality of included studies was assessed based on the Newcastle-Ottawa Scale, while quality of evidence was evaluated according to the “Grading of recommendations assessment, development, and evaluation” system. Data on various outcomes were pooled when appropriate and meta-analyzed.
Results: The systematic review included 16 cohort studies involving 5.91 million patients. Meta-analysis linked history of cannabis use to higher risk of the following outcomes: revision (RR 1.68, 95% CI 1.31–2.16), mechanical loosening (RR 1.77, 95% CI 1.52–2.07), periprosthetic fracture (RR 1.85, 95% CI 1.38–2.48), dislocation (RR 2.10, 95% CI 1.18–3.73), cardiovascular events (RR 2.49, 95% CI 1.22–5.08), cerebrovascular events (RR 3.15, 95% CI 2.54–3.91), pneumonia (RR 3.97, 95% CI 3.49–4.51), respiratory failure (RR 4.10, 95% CI 3.38–4.97), urinary tract infection (RR 2.46, 95% CI 1.84–3.28), acute kidney injury (RR 3.25, 95% CI 2.94–3.60), venous thromboembolism (RR 1.48, 95% CI 1.34–1.63), and deep vein thrombosis (RR 1.42, 95% CI 1.19–1.70). In addition, cannabis use was associated with significantly greater risk of postoperative transfusion (RR 2.23, 95% CI 1.83–2.71) as well as higher hospitalization costs.
Conclusion: History of cannabis use significantly increases the risk of numerous complications and transfusion after THA or TKA, leading to greater healthcare costs. Clinicians should consider these factors when treating cannabis users, and pre-surgical protocols should give special consideration to patients with history of cannbis use.
Cannabis, extracted from plants of the Cannabis genus, contains cannabinoids, which have been used in the traditional medicine of various countries against pain, inflammation, spasms, depression and asthma (1, 2). At the same time, cannabinoids can have wide-ranging effects on cognitive, cardiovascular, respiratory, nervous, and psychological functions, and they can induce addiction (3). As a growing number of countries legalize cannabis use, whether for recreation or specific medical purposes, concerns are growing about how history of cannabis use affects how people respond to medical treatments. For example, some studies have suggested that individuals with cannabis use disorder are at higher risk of various complications than other individuals after diverse elective surgeries (4, 5).
THA and TKA are the most successful surgeries for patients with severe painful, deformed, and damaged joints. In the United States, the annual demand for hip arthroplasty is expected to reach 710,000 and demand for knee arthroplasty to reach 1.2 million by 2040 (6). Several studies have linked history of cannabis use to increased risks of various postoperative complications such as cardiovascular events (7–9), pneumonia (7, 9), venous thromboembolism (7, 9, 10), and acute kidney injury following THA/TKA. Total joint arthroplasty patients with history of cannabis use may be also at higher risks of postoperative transfusion (7, 9) and morphine consumption (11–16). However, a comprehensive understanding of the associations between history of cannabis use with complications and poor outcomes after hip or knee arthroplasty is still lacking.
We are not aware of any published systematic review or meta-analysis in this field. Therefore, we systematically reviewed the available evidence on how history of cannabis use affects the following postoperative outcomes after THA/TKA: systemic complications, prosthetic complications, transfusion, morphine consumption, pain, and hospitalization costs. Our findings may help clinicians and patients predict prognosis after joint arthroplasty surgery, and they may guide future research on the effects of cannabis use on surgical outcomes more generally.
This systematic review and meta-analysis, whose protocol was registered on PROSPERO under accession number CRD42023472424, were performed and reported in accordance with the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) (17) and “Assessing the methodological quality of systematic reviews” (AMSTAR) (18) guidelines. Ethics approval was not sought because we retrospectively analyzed studies previously published in peer-reviewed journals.
Two researchers independently searched the databases of PUBMED, Embase, and Web of Science in August 2023 using combinations of MESH terms and keywords. The PUBMED search strategy were as follows: (“cannabis”[MeSH Terms] OR “cannabis”[All Fields] OR “marijuana”[All Fields]) AND (“arthroplasty, replacement”[MeSH Terms] OR “hip arthroplasty”[All Fields] OR “hip replacement”[All Fields] OR “knee arthroplasty”[All Fields] OR “knee replacement”[All Fields]).
To be eligible for inclusion, studies had to report original research comparing outcomes after THA/TKA between patients with or without a history of cannabis use, and the outcomes had to contain at least one of the following: systemic complications, prosthetic complications, transfusion, morphine consumption, pain, and hospitalization costs. Studies were excluded from the review if the control group involved any additional interventions, involved surgeries other than hip or knee arthroplasty, or did not report relevant outcomes. No restrictions were imposed on study design, language or publication date. References lists in potentially eligible studies were also searched manually in order to identify additional studies.
Potentially relevant studies were imported into Zotero 5.0,1 duplicate publications were removed, and two researchers independently screened studies based on titles and abstracts. They then reviewed the full texts of the remaining articles in order to decide on the final set. Discrepancies were resolved through discussion with a third author.
Two researchers independently extracted the following data from included studies: author names, publication year, study design, sample size, numbers of patients undergoing THA/TKA, how cannabis use was defined. Outcomes of interest included prosthetic complications, systemic complications, transfusions, postoperative morphine consumption, postoperative pain, and hospitalization costs. Discrepancies were resolved through discussion with a third author.
The methodological quality of included studies was assessed using the Newcastle-Ottawa Scale (19), which is a validated, widely used tool for evaluating the quality of observational studies with a total point of nine. The scoring items included (1) the methods used to select the study groups (0–4 points), (2) the comparability of cases and controls (0–2 points), and (3) the method used to ascertain the outcome of interest (0–3 points).
The overall quality of evidence for each outcome was categorized as high, moderate, low, or very low according to the “Grading of recommendations assessment, development, and evaluation” system (20).
Assessments were made independently by two researchers, and discrepancies were resolved through discussion with a third researcher.
Outcomes were synthesized qualitatively if data could not be directly compared across studies. Outcomes for comparable data were pooled between studies and meta-analyzed using a random-effects model in RevMan 5 software (The Cochrane Collaboration, Oxford, United Kingdom). Pooled results were reported as relative risks (RRs) for dichotomous outcomes or as weighted mean differences (WMDs) for continuous outcomes. In both cases, accompanying 95% confidence intervals (CIs) were also calculated. Heterogeneity across studies was assessed using the I2 test, with I2 > 50% defined as substantial heterogeneity (21).
Of 99 potentially relevant publications, 37 were first excluded because they were duplicates. Next, another 36 were excluded because they did not fulfill the inclusion criteria based on titles and abstracts (Figure 1). The remaining 26 publications were read in full, leading to the inclusion of 16 in the final review. Two of these were prospective (13, 22), while the others were retrospective (7–12, 14–16, 23–27). All studies were published in 2018 or later, and 10 were published in 2021 or later (7–9, 13–16, 25–27). These studies analyzed 42,602 individuals with history of cannabis use and 5,865,258 individuals who reported no cannabis use as a control group. Six studies analyzed patients who underwent either THA/TKA (11, 13, 14, 22, 24, 27), while five each examined patients after only one or the other type of surgery. Nine studies defined the history of cannabis use as “cannabis use” (12–16, 23–25, 27), five as “cannabis use disorder” (7–10, 26), one as “tetrahydrocannabinol use” (22) and one as “cannabinoid use” (11). The methodological quality of these studies ranged from 6 to 9 on the Newcastle-Ottawa Scale.
The detailed description of the study characteristics is shown in Table 1, and summary of outcomes data is shown in Table 2.
Three studies involving 2,991,581 individuals investigated the rate of revision (9, 23, 26). Meta-analysis associated history of cannabis use with significantly higher revision rate (RR 1.68, 95% CI 1.31–2.16; I2 = 85%; Figure 2). Similar results were obtained for incidence of mechanical loosening of prosthetic (RR 1.77, 95% CI 1.52–2.07; I2 = 57%) (7, 9, 23), incidence of periprosthetic fracture (7, 9, 23) (RR 1.85, 95% CI 1.38–2.48; I2 = 60%) and incidence of periprosthetic infection (RR 2.00, 95% CI 1.87–2.13; I2 = 0%), based on three studies involving 2,815,481 individuals (7, 9, 23).

Figure 2. Forest plot of the risk of prosthetic complications between patients with or without a history of cannabis use after total knee or hip arthroplasty. CI, confidence interval; M–H, Mantel–Haenszel; Random, random-effects model.
Meta-analysis of two studies (7, 9) involving 78,583 individuals linked history of cannabis use to significantly higher dislocation rate (RR 2.10, 95% CI 1.18–3.73; I2 = 94%).The evidence level was judged to be low for all these meta-analyses (Appendix 1).
Meta-analysis of three studies involving 2,917,324 individuals associated history of cannabis use with significantly higher incidence of cardiovascular complications (RR 2.49, 95% CI 1.22–5.08; I2 = 93%; Figure 3), for which the evidence level was low (Appendix 1). Meta-analysis of two studies (7, 9) involving 78,583 individuals linked cannabis use to significantly higher incidence of cerebrovascular complications (RR 3.15, 95% CI 2.54–3.91; I2 = 0%), for which the evidence level was moderate (Appendix 1).
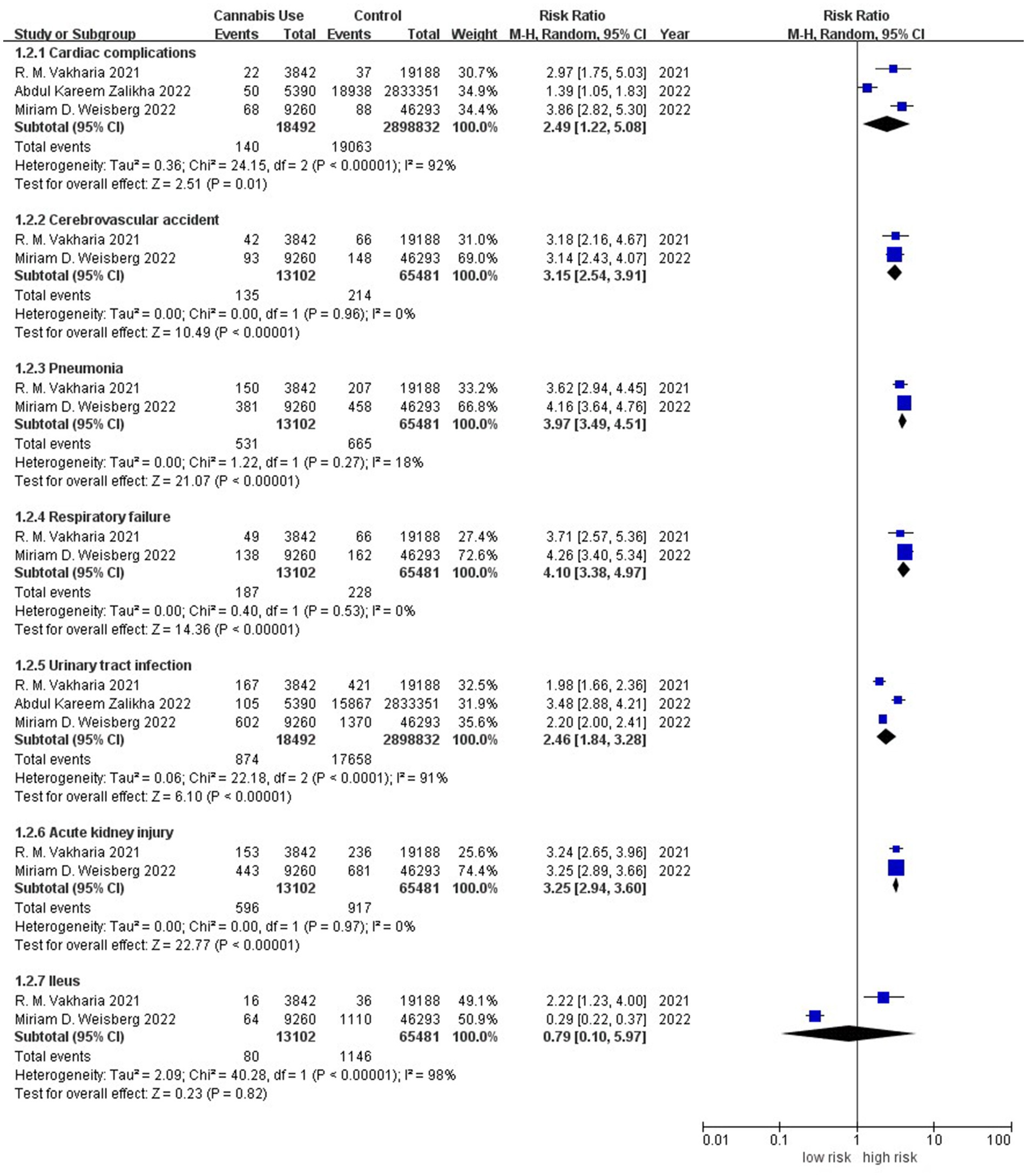
Figure 3. Forest plot of the risk of system complications between patients with or without a history of cannabis use after total knee or hip arthroplasty. CI, confidence interval; M–H, Mantel–Haenszel; Random, random-effects model.
Meta-analysis of two studies (7, 9) involving 78,583 individuals associated history of cannabis use with significantly higher incidence of postoperative pneumonia (RR 3.97, 95% CI 3.49–4.51; I2 = 18%) and postoperative respiratory failure (RR 4.10, 95% CI 3.38–4.97; I2 = 0%); the evidence level in both cases was moderate (Appendix 1). Meta-analysis of the same two studies (7, 9) linked cannabis use to significantly higher incidence of acute kidney injury (RR 3.25, 95% CI 2.94–3.60; I2 = 0%), for which the evidence level was moderate (Appendix 1); but it suggested no difference in incidence of postoperative ileus between patients (7, 9) with or without history of cannabis use (RR 0.79, 95% CI 0.10–5.97; I2 = 98%), though the evidence level for this outcome was very low (Appendix 1).
Meta-analysis of three studies (7–9) involving 2,917,324 individuals linked history of cannabis use to significantly higher incidence of urinary tract infection (RR 2.46, 95% CI 1.84–3.28; I2 = 93%), though the evidence level for this outcome was low (Appendix 1).
Meta-analysis of three studies (7, 9, 10) involving 96,971 individuals associated history of cannabis use with significantly higher incidence of venous thromboembolism (RR 1.48, 95% CI 1.34–1.63; I2 = 0%; Figure 4), and the evidence level was low (Appendix 1). Meta-analysis of four studies (7–10) involving 2,935,712 individuals linked cannabis use to significantly higher incidence of deep vein thrombosis (RR 1.42, 95% CI 1.19–1.70; I2 = 44%), for which the evidence level was low (Appendix 1); but it suggested no difference in incidence of postoperative pulmonary embolism between patients (7–10) with or without history of cannabis use (RR 1.14, 95% CI 0.77–1.68; I2 = 67%), though the evidence level was very low (Appendix 1).
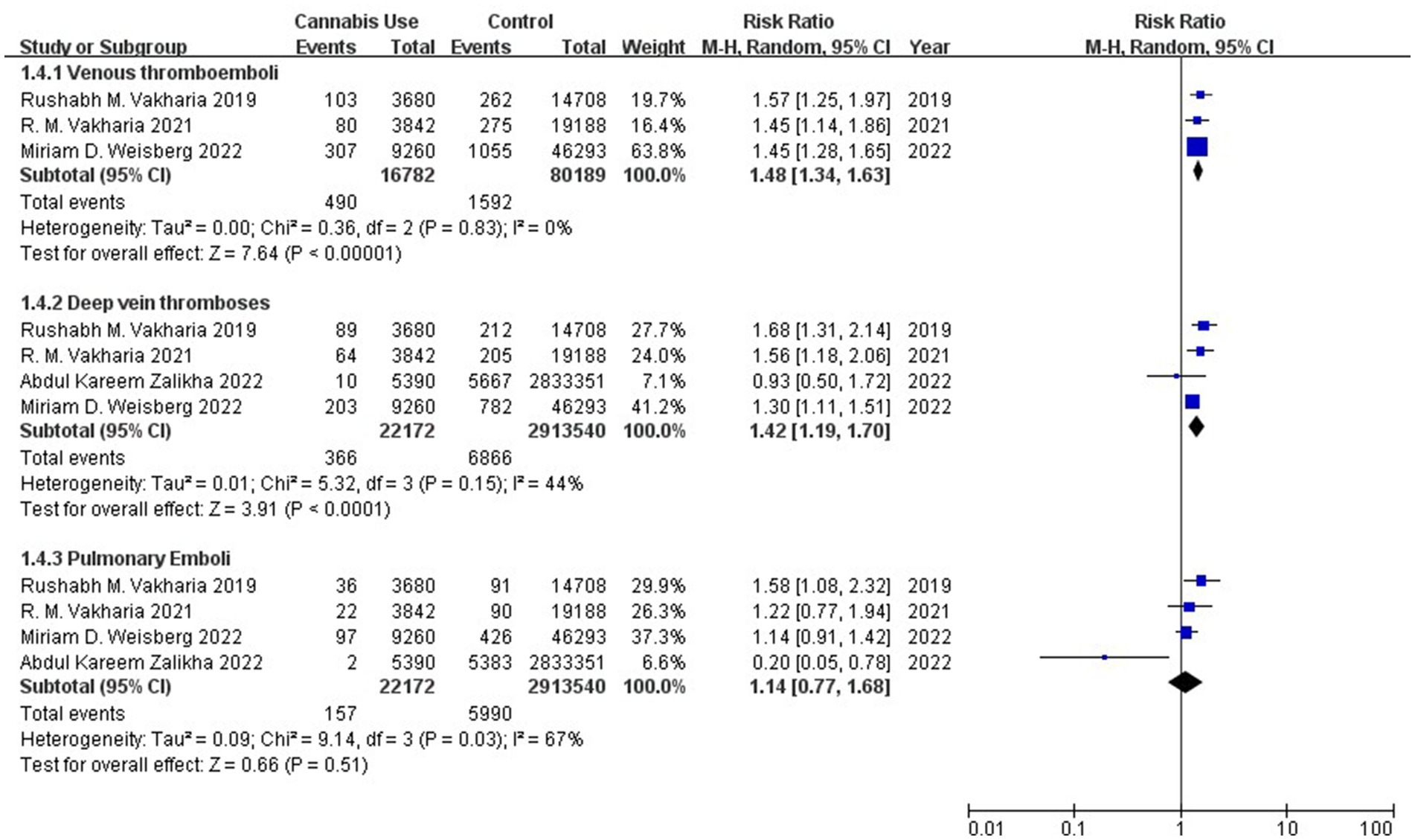
Figure 4. Forest plot of the risk of thromboembolic complications between patients with or without a history of cannabis use after total knee or hip arthroplasty. CI, confidence interval; M–H, Mantel–Haenszel; Random, random-effects model.
Meta-analysis of six studies (11–16) involving 2,137 patients did not detect a significant difference in postoperative morphine consumption between patients with or without history of cannabis use (WMD 3.71, 95% CI-4.14 to 11.55; I2 = 83%; Figure 5), although the evidence level was very low (Appendix 1).
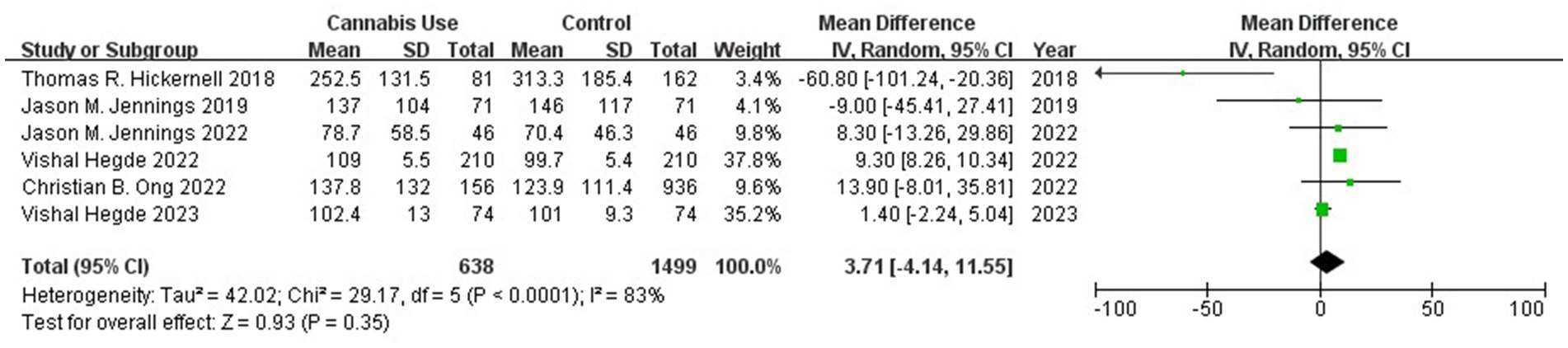
Figure 5. Forest plot of the mean difference of morphine consumption between patients with or without a history of cannabis use after total knee or hip arthroplasty. CI, confidence interval; Random, random-effects model.
We were unable to meta-analyze differences in self-reported postoperative pain scores across the five cohort studies (11, 13, 22, 24, 27) that reported such data, because the studies assessed pain at different time points. Three retrospective studies (11, 22, 27) and one prospective study (13), which together involved 727 participants, reported no significant difference in postoperative pain between patients with or without history of cannabis use, while one retrospective cohort study (24) involving 149 participants linked cannabis use to significantly higher pain.
Meta-analysis of two studies (7, 9) involving 78,583 individuals linked history of cannabis use to significantly higher rate of postoperative transfusion (RR 2.23, 95% CI 1.83–2.71; I2 = 54%; Figure 6), for which the evidence level was moderate (Appendix 1).

Figure 6. Forest plot of the risk of postoperative transfusion between patients with or without a history of cannabis use after total knee or hip arthroplasty. CI, confidence interval; M–H, Mantel–Haenszel; Random, random-effects model.
Five retrospective cohort studies (7–10, 25) involving 2,936,780 individuals reported hospitalization costs related to joint replacement, but we were unable to meta-analyze the comparison between patients with or without history of cannabis use because the studies assessed different types of costs and sometimes differed in how they defined the same cost. All five studies reported that history of cannabis use was associated with higher hospitalization costs, which ranged from 16,938 to 59,570 USD for cannabis users and from 16,023 to 53,316 USD for controls.
This systematic review and meta-analysis appears to be the first attempt to synthesize available evidence about whether and how history of cannabis use affects complications, pain control, and other aspects following THA/TKA. Our analyses suggest that cannabis use is associated with greater risk of a range of negative outcomes, implying the need for special preoperative preparation and postoperative management of such patients.
The tetrahydrocannabinol in cannabis can cause feelings of euphoria that lead to addiction (28), it exerts analgesic and sedative effects by activating cannabinoid receptors 1 and 2, and it exerts adverse cardiovascular effects by activating the endocannabinoid system in the central nervous and cardiovascular systems (29). Phytocannabinoids can exacerbate infections by inhibiting the proliferation of T cells in peripheral blood (30, 31). These diverse effects of phytocannabinoids may help explain the plant’s observed negative effects on patient recovery after not only total joint replacement but other types of surgery as well (5). The effects of phytocannabinoids on the central nervous system may help explain why cannabis use increases risk of prosthetic complications: the plant compounds may decrease proprioception and impair motor coordination (32), which may contribute to risk of revision, mechanical loosening, periprosthetic fractures, and joint dislocation. Phytocannabinoids may reduce bone density by affecting mesenchymal stem cells (33, 34), which may also contribute to the observed increase in fracture risk. The observed higher risk of infection with cannabis use in our meta-analysis may reflect the ability of phytocannabinoids and other compounds in canabis smoke to suppress immune responses, analogously to compounds in cigarette smoke (35–38).
Consistent with a study linking history of cannabis use to greater risk of thrombotic complications in trauma patients (39), our meta-analysis confirmed an association between cannabis use and higher risk of venous thromboembolism and deep vein thrombosis. This association can be attributed to the ability of phytocannabinoids, acting through cannabinoid receptor 1, to stimulate the sympathetic nervous system while inhibiting the parasympathetic nervous system. These simultaneous processes increase heart rate and myocardial oxygen demand, leading to endothelial dysfunction and oxidative stress, which in turn may increase risk of myocardial infarction and stroke (40, 41). In addition, tetrahydrocannabinol may increase risk of thrombotic complications by activating platelets (42). Nevertheless, the evidence level for the effects of cannabis use on venous thromboembolism and deep vein thrombosis is not strong, highlighting the need for further research into these complications. Such research should verify our finding of no association between cannabis use and risk of pulmonary embolism, and it should explore why cannabis use appears to increase risk of thrombotic complications in veins but not arteries (39).
Nearly all studies in our review found no significant difference in postoperative pain between patients with or without history of cannabis use, which may help explain why our meta-analysis indicated no significant difference in postoperative morphine consumption between the two groups. This pooled result contrasts with previous work suggesting that cannabis use can reduce postoperative morphine consumption (43, 44). Nevertheless, the evidence level for this pooled result was very low, highlighting the need for rigorous research into whether cannabis use can mitigate pain after arthroplasty or other surgical procedures.
Our finding of an association between history of cannabis use and significantly higher rate of postoperative transfusion may reflect the higher risk of certain complications, such as bleeding. The observed association of cannabis use with higher hospitalization costs likely reflects the higher risk of numerous complications requiring prolonged treatment and management in hospital.
Our results should be interpreted with caution in light of several limitations. One is the fact that nearly all studies in our review were retrospective, and another is heterogeneity in how studies defined “history of cannabis use,” which probably contributed to the heterogeneity in several meta-analyses and weakened the evidence level. Indeed, none of the included studies reported sufficient detail about duration and intensity of cannabis use to allow us to evaluate dose–response relationships or control for confounding factors.
Despite these limitations, our systematic review of a large number of patients provides strong evidence that a history of cannabis use significantly increases risk of prosthetic, systemic and thromboembolic complications after THA/TKA, which in turn increases risk of transfusion and makes hospitalization more expensive. Whether cannabis us helps reduce pain and the need for morphine after joint replacement remains unclear. Future research should verify and extend our findings, particularly those with a lower evidence level. Clinicians may wish to use our findings to optimize preoperative preparation and postoperative management for patients with a history of cannabis use.
GY: Conceptualization, Methodology, Writing – original draft. FL: Formal analysis, Investigation, Writing – review & editing. QW: Project administration, Data curation, Writing – review & editing. YL: Formal analysis, Funding acquisition, Writing – review & editing. JG: Funding acquisition, Project administration, Writing – review & editing. CY: Conceptualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The current project was supported by the “Traditional Chinese Medicine Evidence-Based Capacity Building Project (2019XZZX-GK004)” of the State Administration of Traditional Chinese Medicine.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1377688/full#supplementary-material
1. Balant, M, Gras, A, Ruz, M, Vallès, J, Vitales, D, and Garnatje, T. Traditional uses of Cannabis: an analysis of the CANNUSE database. J Ethnopharmacol. (2021) 279:114362. doi: 10.1016/j.jep.2021.114362
2. Deuel, LM, and Seeberger, LC. Complementary therapies in Parkinson disease: a review of acupuncture, tai chi, qi gong, yoga, and Cannabis. Neurotherapeutics. (2020) 17:1434–55. doi: 10.1007/s13311-020-00900-y
3. Cohen, K, Weizman, A, and Weinstein, A. Positive and negative effects of Cannabis and cannabinoids on health. Clin Pharmacol Ther. (2019) 105:1139–47. doi: 10.1002/cpt.1381
4. Connor, JP, Stjepanović, D, Le Foll, B, Hoch, E, Budney, AJ, and Hall, WD. Cannabis use and cannabis use disorder. Nat Rev Dis Primers. (2021) 7:16. doi: 10.1038/s41572-021-00247-4
5. McAfee, J, Boehnke, KF, Moser, SM, Brummett, CM, Waljee, JF, and Bonar, EE. Perioperative cannabis use: a longitudinal study of associated clinical characteristics and surgical outcomes. Reg Anesth Pain Med. (2021) 46:137–44. doi: 10.1136/rapm-2020-101812
6. Shichman, I, Roof, M, Askew, N, Nherera, L, Rozell, JC, Seyler, TM, et al. Projections and epidemiology of primary hip and knee arthroplasty in Medicare patients to 2040-2060. JB JS Open Access. (2023) 8:e22.00112. doi: 10.2106/JBJS.OA.22.00112
7. Weisberg, MD, Ng, MK, Magruder, ML, Vakharia, RM, Roche, MW, and Erez, O. The association of cannabis use disorder and perioperative complications after primary total knee arthroplasty. J Am Acad Orthop Surg. (2022) 30:313–20. doi: 10.5435/JAAOS-D-21-00703
8. Zalikha, AK, Rahmon, D, Mazur, M, Hussein, IH, and El-Othmani, MM. Cannabis use disorder in the setting of primary total hip arthroplasty: understanding the epidemiology, demographic characteristics, and inpatient postoperative outcomes. J Am Acad Orthop Surg. (2022) 30:321–8. doi: 10.5435/JAAOS-D-21-00976
9. Vakharia, RM, Mannino, A, Salem, HS, Roche, MW, Wong, CHJ, and Mont, MA. The association between cannabis use disorder and the outcome following primary total hip arthroplasty: analysis of a nationwide administrative claims database. Bone Joint J. (2021) 103-B:111–5. doi: 10.1302/0301-620X.103B7.BJJ-2020-2424.R1
10. Vakharia, RM, Sodhi, N, Anis, HK, Ehiorobo, JO, Mont, MA, and Roche, MW. Patients who have Cannabis use disorder have higher rates of venous Thromboemboli, readmission rates, and costs following primary total knee arthroplasty. J Arthroplast. (2020) 35:997–1002. doi: 10.1016/j.arth.2019.11.035
11. Hickernell, TR, Lakra, A, Berg, A, Cooper, HJ, Geller, JA, and Shah, RP. Should cannabinoids be added to multimodal pain regimens after total hip and knee arthroplasty? J Arthroplast. (2018) 33:3637–41. doi: 10.1016/j.arth.2018.07.027
12. Jennings, JM, Angerame, MR, Eschen, CL, Phocas, AJ, and Dennis, DA. Cannabis use does not affect outcomes after total knee arthroplasty. J Arthroplast. (2019) 34:1667–9. doi: 10.1016/j.arth.2019.04.015
13. Jennings, JM, McNabb, DC, Johnson, RM, Brady, AC, Kim, RH, and Dennis, DA. Use of Cannabis does not decrease opioid consumption in patients who underwent total joint arthroplasty. Arthroplast Today. (2022) 15:141–6. doi: 10.1016/j.artd.2022.03.018
14. Hegde, V, Bracey, DN, Johnson, RM, Farsad, YY, Dennis, DA, and Jennings, JM. Self-reported Cannabis use is associated with a lower rate of persistent opioid use after total joint arthroplasty. Arthroplast Today. (2022) 17:145–9. doi: 10.1016/j.artd.2022.07.014
15. Ong, CB, Puri, S, Lebowitz, J, Chiu, Y-F, Della Valle, AG, Sideris, A, et al. Preoperative cannabis use does not increase opioid utilization following primary total hip arthroplasty in a propensity matched analysis. Arch Orthop Trauma Surg. (2022) 143:3629–35. doi: 10.1007/s00402-022-04619-7
16. Hegde, V, Bracey, DN, Pollet, AK, Yazdani-Farsad, Y, Dennis, DA, and Jennings, JM. Cannabis use does not affect outcomes after total hip arthroplasty. J Arthroplast. (2023) 38:1808–11. doi: 10.1016/j.arth.2023.03.040
17. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
18. Shea, BJ, Reeves, BC, Wells, G, Thuku, M, Hamel, C, Moran, J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
19. Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
20. Guyatt, G, Oxman, AD, Akl, EA, Kunz, R, Vist, G, Brozek, J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. (2011) 64:383–94. doi: 10.1016/j.jclinepi.2010.04.026
21. Higgins, JPT, and Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
22. Runner, RP, Luu, AN, Nassif, NA, Scudday, TS, Patel, JJ, Barnett, SL, et al. Use of tetrahydrocannabinol and Cannabidiol products in the perioperative period around primary unilateral total hip and knee arthroplasty. J Arthroplast. (2020) 35:S138–43. doi: 10.1016/j.arth.2020.01.077
23. Law, TY, Kurowicki, J, Rosas, S, Sabeh, K, Summers, S, Hubbard, Z, et al. Cannabis use increases risk for revision after total knee arthroplasty. J Long-Term Eff Med Implants. (2018) 28:125–30. doi: 10.1615/JLongTermEffMedImplants.2018027401
24. Aleissa, MM, Ahern, KL, and Stern, GM. Peri-operative opioid and sedation requirements in patients who use marijuana and are undergoing total knee or total hip arthroplasty: a retrospective study. J Clin Anesth. (2020) 66:109953. doi: 10.1016/j.jclinane.2020.109953
25. Kirchner, GJ, Kim, A, Lieber, AM, Hines, SM, and Nikkel, LE. Cannabis use does not increase risk of perioperative complications following primary Total hip arthroplasty: a cohort-matched comparison. Cannabis Cannabinoid Res. (2022) 8:684–90. doi: 10.1089/can.2022.0042
26. Sambandam, S, Mounasamy, V, Selvaraj, S, and Wukich, D. Risk of revision surgery and manipulation under anesthesia in patients with Cannabis use disorder undergoing Total knee arthroplasty. Cureus. (2022) 14:e21016. doi: 10.7759/cureus.21016
27. Sharma, V, Laubach, L, Krumme, JW, and Satpathy, J. Cannabis use among lower-extremity arthroplasty patients does not lead to worse postoperative outcomes. Cureus. (2022) 14:e31964. doi: 10.7759/cureus.31964
28. Rezende, B, Alencar, AKN, de Bem, GF, Fontes-Dantas, FL, and Montes, GC. Endocannabinoid system: chemical characteristics and biological activity. Pharmaceuticals (Basel). (2023) 16:148. doi: 10.3390/ph16020148
29. Pacher, P, Steffens, S, Haskó, G, Schindler, TH, and Kunos, G. Cardiovascular effects of marijuana and synthetic cannabinoids: the good, the bad, and the ugly. Nat Rev Cardiol. (2018) 15:151–66. doi: 10.1038/nrcardio.2017.130
30. Robinson, RH, Meissler, JJ, Breslow-Deckman, JM, Gaughan, J, Adler, MW, and Eisenstein, TK. Cannabinoids inhibit T-cells via cannabinoid receptor 2 in an in vitro assay for graft rejection, the mixed lymphocyte reaction. J Neuroimmune Pharmacol. (2013) 8:1239–50. doi: 10.1007/s11481-013-9485-1
31. Yuan, M, Kiertscher, SM, Cheng, Q, Zoumalan, R, Tashkin, DP, and Roth, MD. Delta 9-tetrahydrocannabinol regulates Th1/Th2 cytokine balance in activated human T cells. J Neuroimmunol. (2002) 133:124–31. doi: 10.1016/s0165-5728(02)00370-3
32. Bolbecker, AR, Apthorp, D, Martin, AS, Tahayori, B, Moravec, L, Gomez, KL, et al. Disturbances of postural sway components in cannabis users. Drug Alcohol Depend. (2018) 190:54–61. doi: 10.1016/j.drugalcdep.2018.05.012
33. Gowran, A, McKayed, K, and Campbell, VA. The cannabinoid receptor type 1 is essential for mesenchymal stem cell survival and differentiation: implications for bone health. Stem Cells Int. (2013) 2013:796715:1–8. doi: 10.1155/2013/796715
34. Sophocleous, A, Robertson, R, Ferreira, NB, McKenzie, J, Fraser, WD, and Ralston, SH. Heavy Cannabis use is associated with low bone mineral density and an increased risk of fractures. Am J Med. (2017) 130:214–21. doi: 10.1016/j.amjmed.2016.07.034
35. Owen, KP, Sutter, ME, and Albertson, TE. Marijuana: respiratory tract effects. Clin Rev Allergy Immunol. (2014) 46:65–81. doi: 10.1007/s12016-013-8374-y
36. Roth, MD, Whittaker, K, Salehi, K, Tashkin, DP, and Baldwin, GC. Mechanisms for impaired effector function in alveolar macrophages from marijuana and cocaine smokers. J Neuroimmunol. (2004) 147:82–6. doi: 10.1016/j.jneuroim.2003.10.017
37. Bradley, SG, Munson, AE, Dewey, WL, and Harris, LS. Enhanced susceptibility of mice to combinations of delta 9-tetrahydrocannabinol and live or killed gram-negative bacteria. Infect Immun. (1977) 17:325–9. doi: 10.1128/iai.17.2.325-329.1977
38. Morahan, PS, Klykken, PC, Smith, SH, Harris, LS, and Munson, AE. Effects of cannabinoids on host resistance to listeria monocytogenes and herpes simplex virus. Infect Immun. (1979) 23:670–4. doi: 10.1128/iai.23.3.670-674.1979
39. Stupinski, J, Bible, L, Asmar, S, Chehab, M, Douglas, M, Ditillo, M, et al. Impact of marijuana on venous thromboembolic events: cannabinoids cause clots in trauma patients. J Trauma Acute Care Surg. (2020) 89:125–31. doi: 10.1097/TA.0000000000002667
40. Page, RL, Allen, LA, Kloner, RA, Carriker, CR, Martel, C, Morris, AA, et al. Medical marijuana, recreational Cannabis, and cardiovascular health: a scientific statement from the American Heart Association. Circulation. (2020) 142:e131–52. doi: 10.1161/CIR.0000000000000883
41. Hemachandra, D, McKetin, R, Cherbuin, N, and Anstey, KJ. Heavy cannabis users at elevated risk of stroke: evidence from a general population survey. Aust N Z J Public Health. (2016) 40:226–30. doi: 10.1111/1753-6405.12477
42. Deusch, E, Kress, HG, Kraft, B, and Kozek-Langenecker, SA. The procoagulatory effects of delta-9-tetrahydrocannabinol in human platelets. Anesth Analg. (2004) 99:1127–30. doi: 10.1213/01.ANE.0000131505.03006.74
43. Le Foll, B. Opioid-sparing effects of cannabinoids: myth or reality? Prog Neuro-Psychopharmacol Biol Psychiatry. (2021) 106:110065. doi: 10.1016/j.pnpbp.2020.110065
Keywords: Cannabis, total hip arthroplasty, total knee arthroplasty, postoperative outcomes, drug abuse and addiction
Citation: Yang G, Li F, Wang Q, Liu Y, Guo J and Yue C (2024) Association between history of cannabis use and outcomes after total hip or knee arthroplasty: a systematic review and meta-analysis. Front. Public Health. 12:1377688. doi: 10.3389/fpubh.2024.1377688
Received: 28 January 2024; Accepted: 25 April 2024;
Published: 17 May 2024.
Edited by:
Jaya Kumar, National University of Malaysia, MalaysiaReviewed by:
Robert J. Wellman, UMass Chan Medical School, United StatesCopyright © 2024 Yang, Li, Wang, Liu, Guo and Yue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiayi Guo, ZG9jdG9yZ3VvanlAb3V0bG9vay5jb20=; Chen Yue, b3J0aG9wZWRpY3MueXVlQG91dGxvb2suY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.