- Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, China
Introduction: In recent years, China has been carrying out the Diagnosis Related Groups (DRGs) payment reform, which has an impact not only on payment methods and medical expenses, but also on the behaviors of medical staff. Some of these behaviors are unexpected by policymakers, such as turning away critically ill patients, disaggregating hospitalization costs, setting up disease groups with higher points, and so on. This phenomenon attracted the attention of some scholars, who put forward a few positive intervention measures, mainly including policy advocacy and system improvement. The scholars believed that the former was more feasible. However, there is a lack of research on the effects and influencing processes of these interventions. Therefore, this study aims to explore the influence of policy advocacy and education on medical staff’s adaptation to DRGs payment reform in China and the role of policy cognition in this process, in order to provide experiences for the smooth implementation and sustainable development of DRGs payment system.
Methods: A questionnaire survey was conducted among 650 medical staff in five large general hospitals in Zhejiang Province, China, to understand their participation and feedback on policy advocacy and education, their adaptation to the current DRGs payment reform, and their cognition of relevant policies. After descriptive statistical analysis, partial correlation analysis, multiple linear regression models and bias correction Bootstrap sampling method were used to analyze the mediating effect of policy cognition factors.
Results: All respondents had participated in organized collective policy advocacy and education activities in the past year, but the degree of satisfaction and recognition was not very high. 59.5 percent said their adaptation to the DRGs payment reform was average. Nearly half did not regularly pay attention to and participate in the management of the medical costs of patients with DRGs through compliance. And they had a low understanding of the specific rules of DRGs payment and did not form a high policy identity. The mediating effect values of policy cognition were 0.148, 0.152, 0.108, and 0.057, respectively, when the frequency and quality of policy advocacy and education influenced medical staff’s adaptive perception and adaptive behaviors.
Discussion: The organized collective policy advocacy and education can promote medical staff’s adaptation to DRGs payment reform by improving their policy cognition, and the action paths are diverse. Policymakers and hospital managers need pay attention to this phenomenon, and formulate demand-centered, value-oriented whole-process advocacy and education strategies while constantly improving the DRGs payment system. All of these provided a basis for further research and practice of positive intervention in DRGs payment reform.
1 Introduction
1.1 The origin and development of DRGs
Diagnosis Related Groups is a tool to measure the quality and efficiency of medical services or measure the amount paid by the health insurance fund. It is a case cluster statistical method for hospital management, considering the diagnosis of disease, treatment, complications, comorbidities, as well as the age of patients, resource consumption, and other factors (1, 2). Diagnosis Related Groups-Prospective Payment System (DRG-PPS) is to apply the above method to group the cases, in advance to establish the payment standard for each patient group, according to which the medical expenses are paid. This is a new medical insurance fund payment method that is different from the traditional payment by service item or capitation (3). DRGs was first developed by Yale University in 1969. After many practices and adjustments proved that its fee control effect was significant, and the national uniform rate standard was achieved in 1987, so far, several versions of Medicare Severity-Diagnosis Related Groups (MS-DRG) have been issued (4, 5). Since then, Australia, Germany, France, Japan, and other developed countries in order to control the rise of medical costs and improve the efficiency of medical services, have explored the implementation of a DRGs payment system and made a series of adjustments according to their respective situations, and achieved good results (6–8). At the same time, the reform of DRGs had also promoted the unification of their domestic International Classification of Diseases (ICD) versions, medical service prices, and medical insurance payment standards, and strengthened their assessment and supervision of medical institutions (9–11). However, there were also some problems in this process, such as the unreasonable disease grouping, the insufficiently friendly compensation mechanism of new clinical technology, the emergence of negative behaviors of doctors, and so on (12–14).
1.2 DRGs payment reform in China
In recent years, in order to deal with the chain problems of the aging population, excessive medical treatment, rapid growth of medical expenditure, and increasing pressure on medical insurance funds, many developing countries have also begun to reform the DRGs payment system (15). Among them, China, as a populous country, the above problems are particularly severe, and it is urgent to reform the payment method of medical insurance (16, 17). In fact, as early as the 1980s, China began to explore the feasibility of implementing DRGs at the theoretical level. In 2008, the construction of the first DRGs grouping device in the Chinese Mainland was completed, and from 2011 to 2017, the DRGs payment reform pilot work was carried out in Beijing, Shenzhen, Sanming, and other places, during which multiple DRGs grouping schemes were used, including BJ-DRG, CN-DRG, and C-DRG (2, 18). Since the establishment of the National Healthcare Security Administration in 2018, the national general grouping standard (China Healthcare Security-Diagnosis Related Groups, CHS-DRG) has been formulated based on the previous different grouping schemes, and the pilot scope of reform has been continuously expanded, requiring all eligible medical institutions to complete the reforms related to DRGs payment method by the end of 2025 (19). It is worth noting that in September 2020, Zhejiang Province became the first province in China except Taiwan Province to implement DRGs payment reform in the whole province, and it had its characteristic grouping scheme (ZJ-DRG), and was currently in a critical period of transition to CHS-DRG (20).
1.3 Research questions and objectives
Based on relevant studies and reports, we found that although China’s DRGs payment reform had played a certain role in fee control and improved the efficiency of medical services, it had also brought about a series of problems (10). These problems were mainly manifested in the medical staff in the process of reform to turn away critically ill patients, disaggregate hospitalization costs, discharge the patient early, set up disease groups with higher points, and other unexpected behaviors (13, 21). Although these behaviors were considered to be the reasonable feedback of stakeholders’ mutual game under the combined influence of reform enforcement and system defects (13). However, these behaviors are contrary to the goals of the reform and are non-compliant fee control behaviors. If there is no effective intervention, it will not only hinder the sustainable development of the reform but also affect the quality of medical services. From the point of view of system theory and social ecology, medical staff with such adverse stress reactions had not adapted to the changes in the current medical insurance payment system, and they were not coordinated with the operation of the new system (22, 23). Without proper control and guidance, they could affect the balance and development of the system. Therefore, even though there are still some defects in the new payment system, the mandatory and dynamic development of the reform is undeniable, so how to improve the adaptation of stakeholders to the complex system is the key issue.
At present, more and more scholars have begun to pay attention to the impact of DRGs payment reform on medical staff, and their research has gradually shifted from macro policy evaluation to micro policy impact (13, 21, 24). Most of these studies focused on the investigation of cognition and behavior and explored the relationship between the two. Among them, in addition to improving the defects of the system itself, some active intervention measures had been proposed, among which the priority of policy advocacy and education was higher, but there was a lack of further research on its effect and action process (25, 26). To sum up, this study aims to explore the influence of policy advocacy and education on adaptation to DRGs payment reform and its action process from the perspective of medical staff combining multidisciplinary theories. Based on this, we can propose some more scientific and effective action plans, which will not only make up for the shortcomings of relevant research fields but also provide a basis for those countries or regions that are undergoing DRGs payment reform to formulate effective interventions to promote the smooth implementation and sustainable development of the new payment system.
2 Theoretical basis and research hypothesis
The word “adaptation” first appeared in Darwin’s “Origin of Species,” his theory of evolution pointed out “natural selection, survival of the fittest,” emphasizing that adapting to environmental changes is the nature of organisms (27). Later, ecosystem theory and ecological balance theory specified the importance of adapting to the environment and harmonious coexistence, and the relationship between individuals and the environment will not only affect the survival of individuals, but also affect the sustainable development of the whole system (28). The derived social ecosystem theory divided the interaction between individual development and the social environment into three major systems: micro, meso, and macro (29). These theories illustrated the importance and complexity of the relationship between human beings and social environment. With the concept of “social adaptation” put forward by Herbert Spencer, it was clear that it was a process of an individual’s response to the social environmental stimuli in line with norms, and finally reached the state of accepting the existing social norms, including both psychological and behavioral dimensions (30). Subsequently, many scholars focused on the measurement and intervention of people’s social adaptability, especially in the fields of social support and health education (31–33). However, there was no unified concept or scale of adaptation to policy reform, so this study combined Merton’s adaptation typology and Yanyan Chi’s research on the adaptability of rural disabled people to medical security and considered the mandatory and binding nature of DRGs payment reform (34, 35), it is believed that the real ideal state of adaptation should be that the goals and contents of autonomous actions meet the requirements of reform, that is, medical staff take the initiative to achieve the goal of cost control and efficiency improvement through compliance.
According to the above definition of adaptation state in the face of reform, this is not only the behavior manifestation of policy internalization at the highest level of policy acceptance response in public policy science, but also the final internalization state in Kelman’s three-process theory of attitude change (36, 37). It can be seen that good policy awareness and policy identity which can be collectively referred to as policy cognition are important factors affecting whether the adaptation to reform can be successfully achieved (38). This is also consistent with the knowledge-attitude-practice theory on the process of people’s behavior change (39). Then, policy advocacy and education is precisely considered as an information intervention means for policymakers to improve the compliance and implementation effect of policies and improve the awareness and identity of policies by target groups through various ways (40, 41). The advantage of this method is that, on the one hand, compared with punishment, threat, and other means, it can induce spontaneous behavior changes by changing people’s cognition, which is a non-coercive long-term intervention at the psychological level, and can reduce the subordination or rebellion of policy implementors (42, 43). On the other hand, compared with all kinds of regulatory measures, it belongs to the pre-intervention in the early stage of policy implementation, which has better controllability and higher cost performance (44). Long-term practice and research results have also verified the feasibility and importance of policy advocacy and education, which can help people quickly and correctly understand policies, reduce the resistance in the process of policy implementation, and contribute to the development and improvement of policies (40, 44, 45). However, in order to reduce the confusion of the research and facilitate the investigation, the policy advocacy and education in this study specifically referred to the organized collective training, lectures, or meetings on the DRGs payment system that medical staff participate in, excluding informal or personal information acquisition forms, such as through friends, personal browsing of the web, reading posters, reading books, etc.
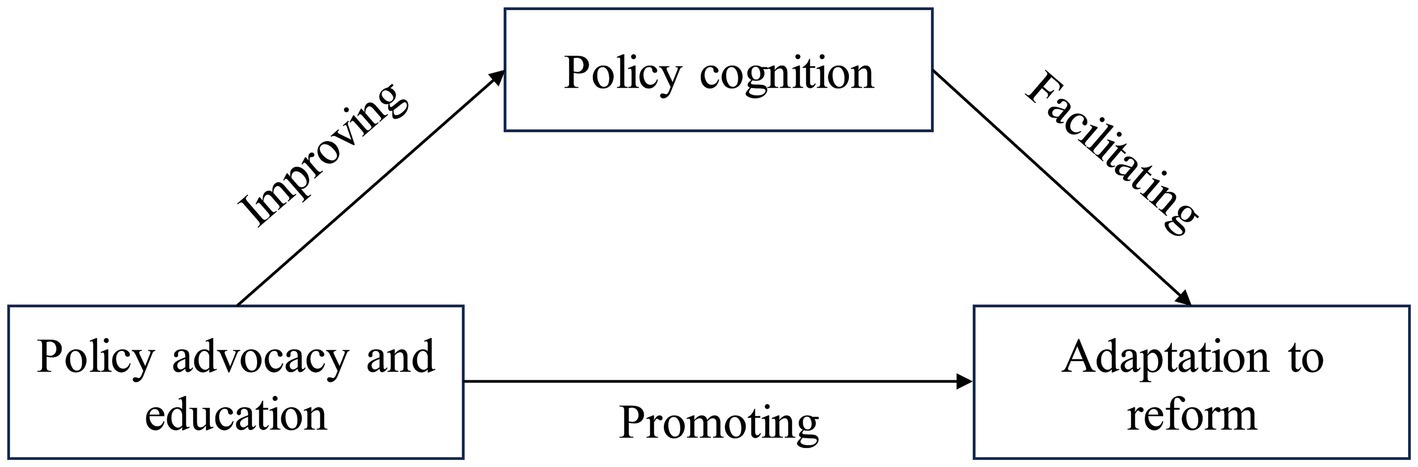
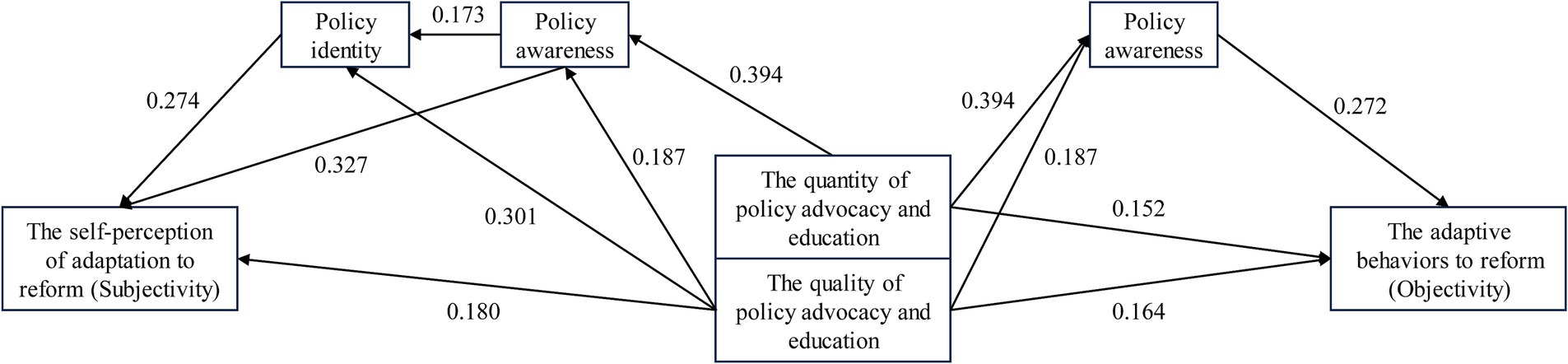
Based on the above related theories and concepts, this study put forward the following three hypotheses, the relationship of which is shown in Figure 1. Among them, policy cognition was the intermediary variable of policy advocacy and education influencing adaptation to reform.
H1: Policy advocacy and education could promote medical staff’s adaptation to the DRGs payment reform.
H2: Policy advocacy and education could improve medical staff’s cognition of DRGs payment policy.
H3: Policy advocacy and education could help medical staff adapt to DGRs payment reform by improving their policy cognition.
3 Materials and methods
3.1 Respondents
Considering the representativeness and feasibility of the questionnaire survey, this study selected medical staff from five large Grade III and A hospitals in Hangzhou, Zhejiang Province as the respondents. In particular, it should be noted that the number of medical staff in the five hospitals ranked among the top 10 in the province, and they have implemented the DRGs payment reform earlier and more standardized. Meanwhile, their medical insurance offices were relatively mature and have conducted a lot of medical insurance policy advocacy and education.
3.2 Survey methods
This study collected data through field questionnaire survey. Firstly, we reasonably estimated the sample size and proportion of each hospital, occupational type (doctors, nurses, and medical technicians) and clinical department according to the difference in the number of medical staff in each hospital and the distribution of their occupational types and departments. Then experienced investigators carried questionnaires to each department for convenient sampling investigation according to the calculated quantity distribution. Meanwhile, to ensure the timeliness and accuracy of the survey results, the survey was conducted from October 15 to 30, 2023, and each questionnaire was filled out independently under the supervision of the investigator. In addition, to improve the efficiency of survey, the questionnaire was made into an electronic two-dimensional code and filled in by scanning the code on site. Finally, we sent out a total of 650 questionnaires. After data entry and elimination, the effective response rate was 97%. For details on the data collection and processing program, see the Supplementary File 1.
3.3 Questionnaire design
Based on the above hypothesis, this study combined literature research, case analysis, expert consultation and brainstorming methods to design the questionnaire. Besides the basic information of the respondents, it mainly included three parts: DRGs payment policy advocacy and education for medical staff, their adaptation to DRGs payment reform, and their cognition of the policy. The specific survey contents were detailed in the questionnaire section of the Supplementary File 2.
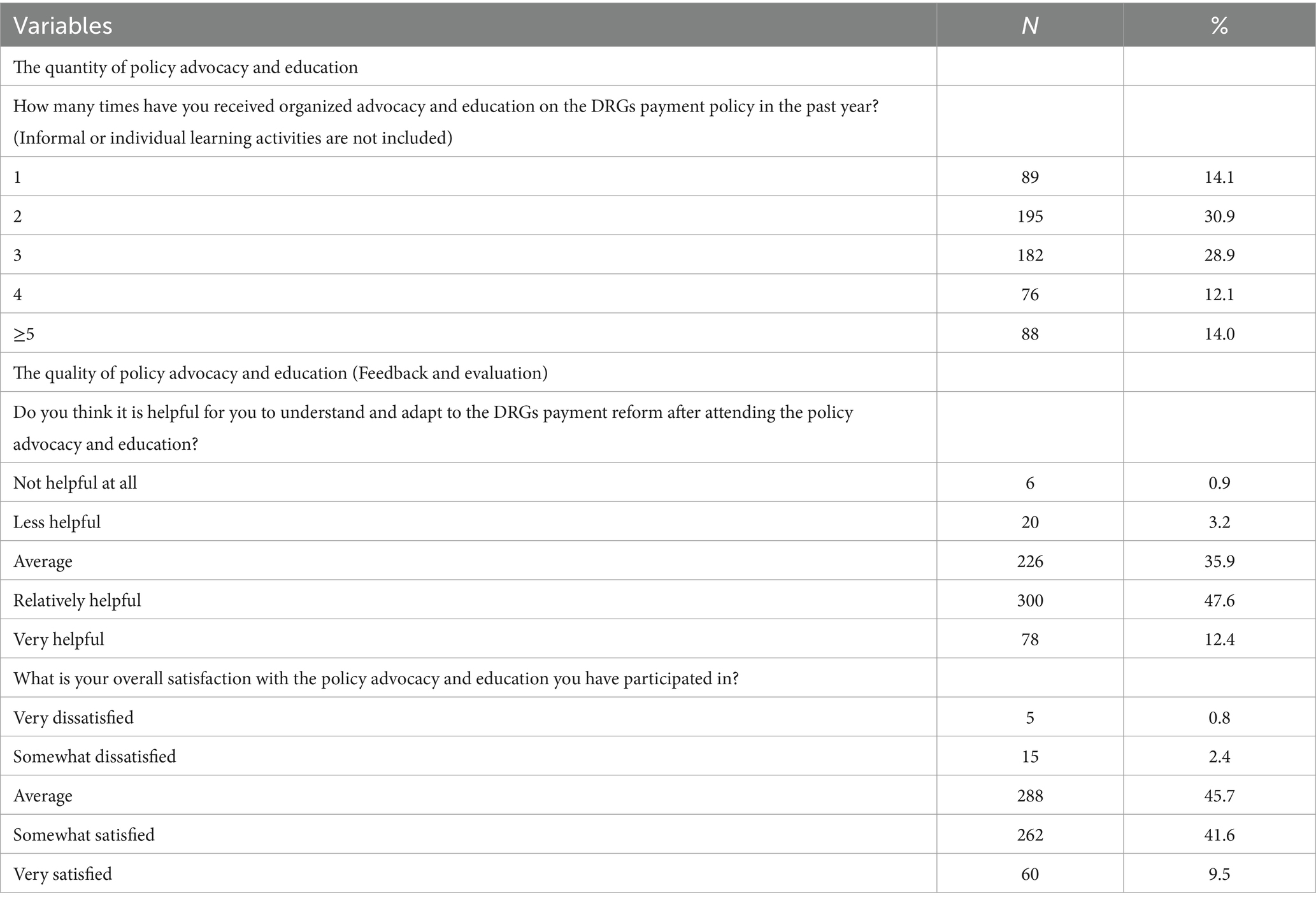
The survey of policy advocacy and education was divided into two parts: quantity and quality. The quantity was represented by the number of participants, and the quality was reflected by the feedback evaluation of the participants. It was worth noting that for the need for variable substitution in sensitivity analysis, this study set up two similar questions (recognition and satisfaction) for feedback evaluation surveys. In addition, this study also conducted a supplementary investigation on the access of medical staff to policy information and the need for policy advocacy and education content.
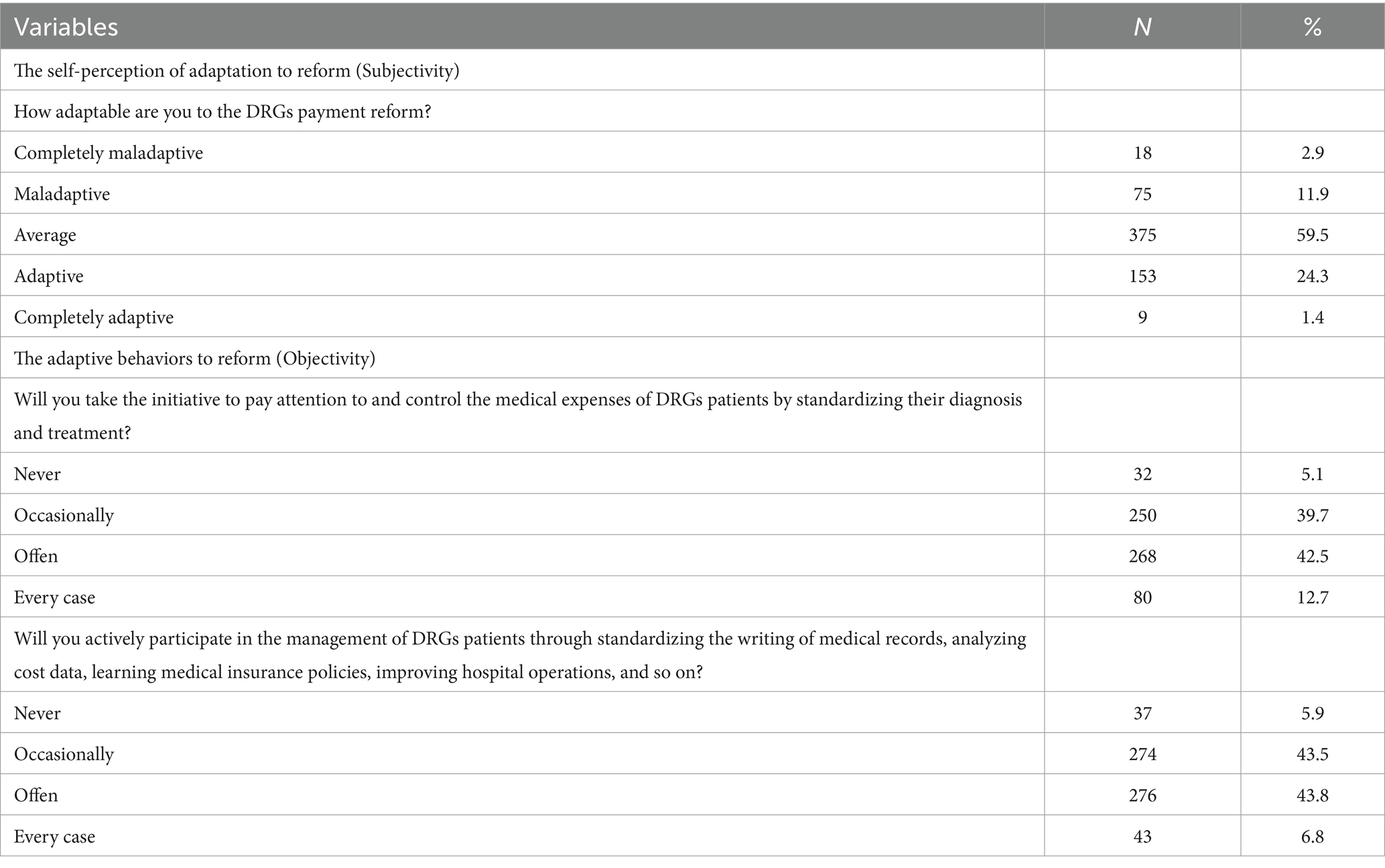
The survey of adaptation was also divided into two parts: self-perception (varying degrees from low to high) and objective behaviors (varying frequencies from low to high). The latter was further divided into medical behaviors (mainly including standardizing diagnosis and treatment) and non-medical management behaviors (such as standardizing the writing of medical records, analyzing cost data, learning medical insurance policies, and improving hospital operations) according to the above definition of adaptive behaviors.
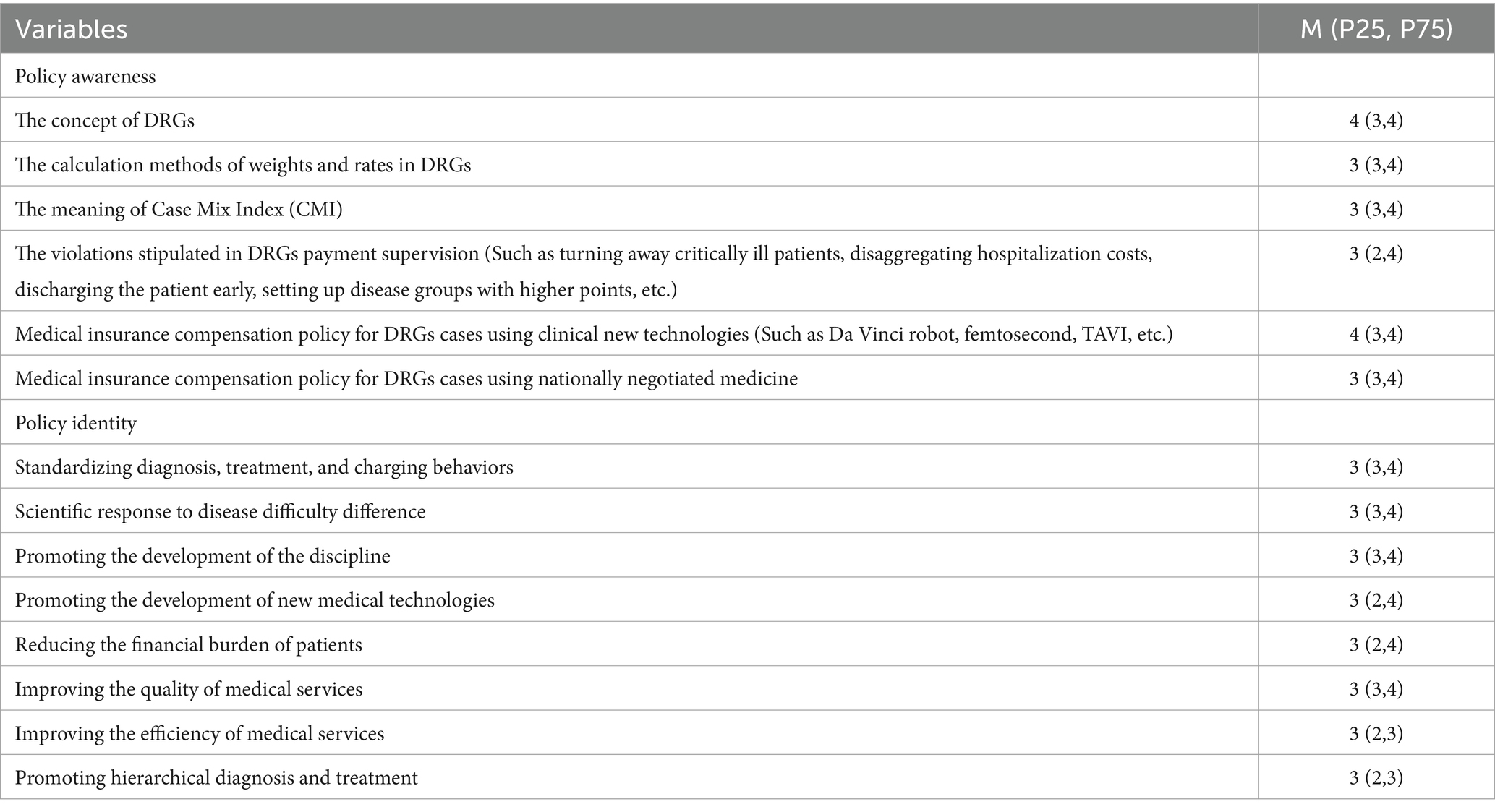
The survey of policy cognition was divided into two dimensions: policy awareness and policy identity. Each dimension included multiple questions from different perspectives, and scores 1–5 according to the degree.
3.4 Statistical methods
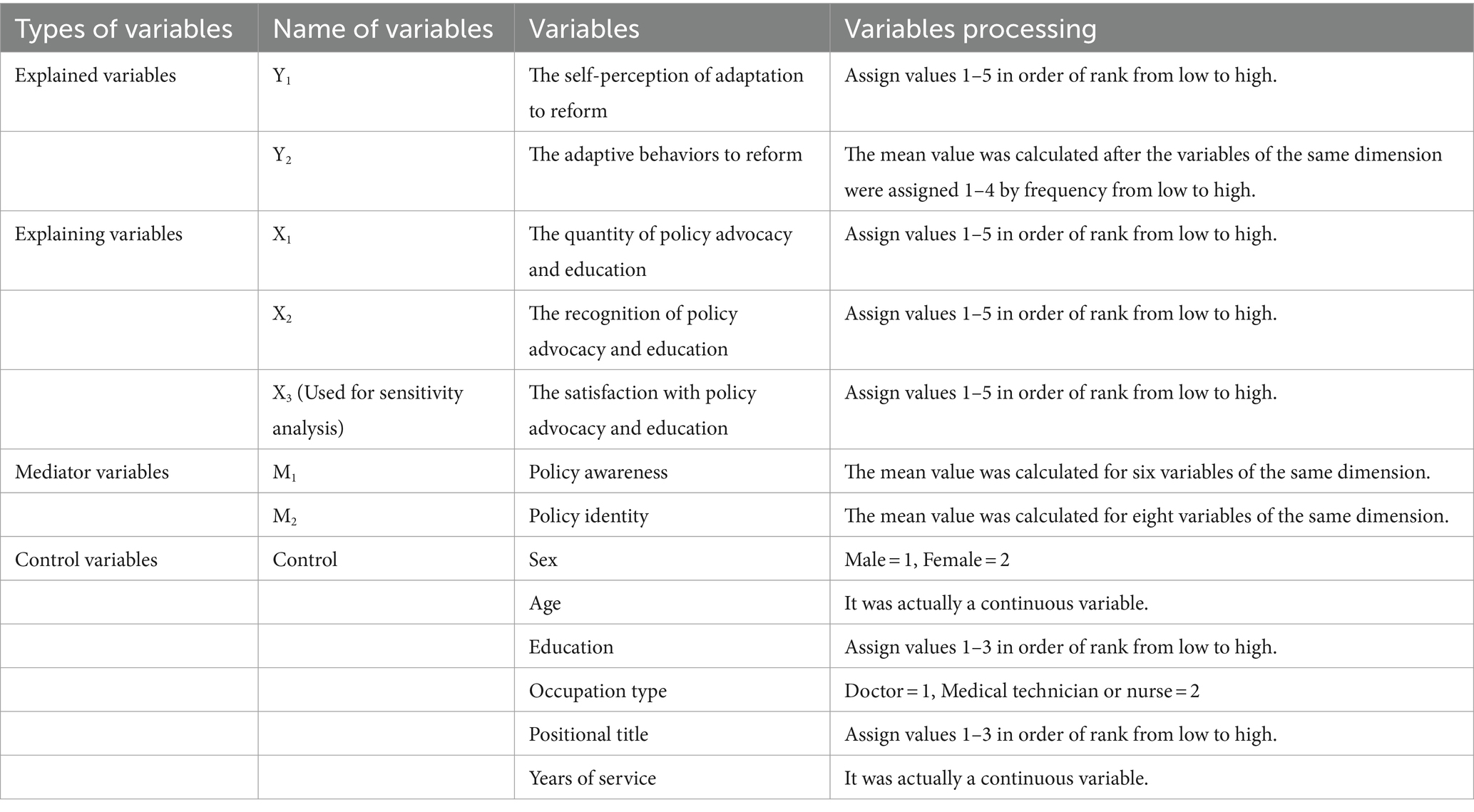
3.4.1 Variables processing and pre-test
In this study, the minimum dimension data containing more than two variables in the questionnaire were tested for reliability and validity. In the reliability test, the overall standardized Cronbach’s alpha was 0.89, indicating good reliability, and the Component Indicator of Total Credibility (CITC) value of each variable was greater than 0.4, indicating good correlation of variables in the same dimension. In the validity test, the Kaiser-Meyer-Olkin (KMO) value was greater than 0.9, and the Bartlett test was passed (p < 0.05). Meanwhile, four common factors were given, which was consistent with the questionnaire design, and the cumulative variance explanation rate after rotation was 76%, indicating that the questionnaire validity was good. On this basis, the variables (especially categorical variables) were named, assigned, and consolidated, to be included in the following statistical analysis, as shown in Table 1.
Then, the correlation between the core variables except the basic information was verified by partial correlation analysis, which was the premise of the mediating effect test. At the same time, they were incorporated into the multiple linear regression model, and the validity and collinearity of the model were explored by the F test and Variance Inflation Factor (VIF) value. Finally, to improve the accuracy of the research results, the mediation effect test was carried out after all variables were standardized.
3.4.2 Models design
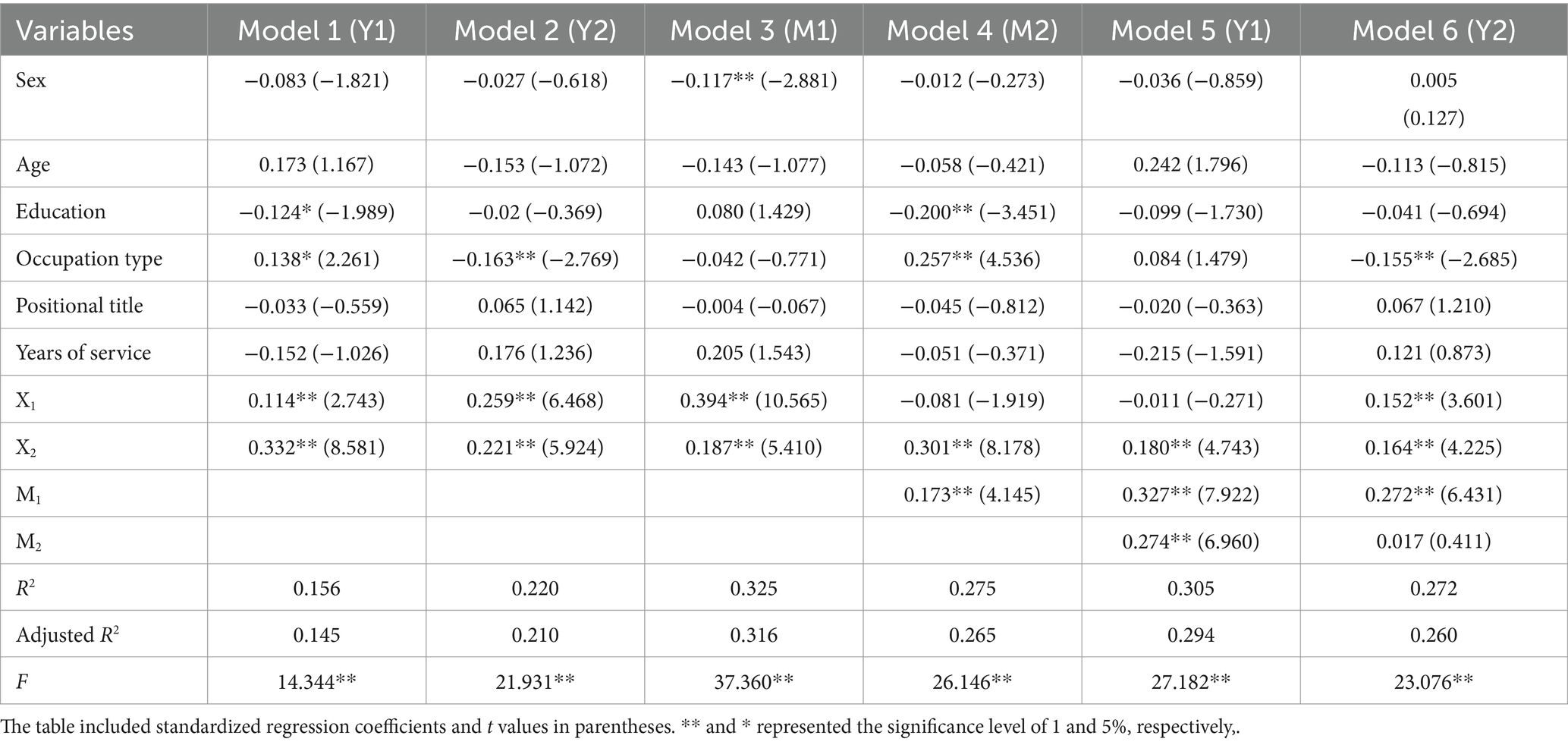
According to the research hypothesis and variable processing results, the following mediation effect test models were designed.
Total effect test:
Y1 = β0 + β1X1 + β2X2 + β3Control + ε Model 1.
Y2 = β0 + β1X1 + β2X2 + β3Control + ε Model 2.
Intermediate path test:
M1 = β0 + β1X1 + β2X2 + β3Control + ε Model 3.
M2 = β0 + β1X1 + β2X2 + β3M1 + β4Control + ε Model 4.
Direct effect and intermediate effect test:
Y1 = β0 + β1X1 + β2X2 + β3M1 + β4M2 + β5Control + ε Model 5.
Y2 = β0 + β1X1 + β2X2 + β3M1 + β4M2 + β5Control + ε Model 6.
In the above models, β0, Control, and ε represented the constant term, the set of control variables, and the random error term, respectively, and β1–β5 were regression coefficients. Under standardized conditions, β1 and β2 in Model 1 and Model 2 represented the total effect value, β1 and β2 in Model 3 and Model 4 represented the influence of independent variables on intermediary variables, β3 in Model 4 represented the influence of intermediary variables M1 on M2, β1 and β2 in Model 5 and Model 6 were the direct effect values, and the cross-multiplicative values of β1–β4 in Model 3–6 were the intermediary effect values of different paths.
3.4.3 Bootstrap sampling method
The Bootstrap sampling method was first proposed by Efron in 1977. It is a method to infer the population distribution of complex statistics by using the resampling technique with retracting (46). Meanwhile, it tests the significance of the intermediary effect value based on the results of multiple linear regression analysis. Compared with the traditional hierarchical regression method and the later Sobel test method, it has a higher test efficiency, which neither covers up the real intermediary effect nor is limited by the type of data distribution (47, 48). In order to further improve the accuracy and stability of research results, this study used the SPSS PROCESS tool to conduct Bootstrap sampling (5,000 times) to test the mediation effect.
4 Results
4.1 Basic information
As shown in Table 2, among the 630 valid survey subjects, the ratio of male to female was about 1:2, most of them were under 40 years old, 48.4% were doctors, half of them had obtained master’s or doctoral degrees, and 59.4% had obtained intermediate or above professional titles.
4.2 Policy advocacy and education about DRGs payment
As shown in Table 3, all respondents had participated in organized formal advocacy and education activities on DRGs payment policies in the past year, but only about 60% of them found them helpful or satisfactory. In addition, we also found through the investigation that medical staff mainly obtained policy information through the intensive training, lectures or meetings organized by the hospital medical insurance office or superior departments, but less obtained policy information through friends, browsing the web, looking at posters, reading books, and other ways. In terms of advocacy and education content, they had the greatest demand for basic policy knowledge and the use of cost management software. In terms of the number of advocacy and education, they suggested once every quarter or half a year, not too frequently.
4.3 Adaptation to the DRGs payment reform
As shown in Table 4, 59.5 percent said their adaptation to the DRGs payment reform was average. Nearly half did not regularly pay attention to and participate in the management of the medical costs of patients with DRGs through compliance.
4.4 Cognition of DRGs payment policy
As shown in Table 5, according to the scores of the respondents, their knowledge level of DRGs payment policy was generally medium to above, with a relatively high understanding of basic knowledge, but an average understanding of more specific rules and systems. Meanwhile, their identity of the instrumental value, economic value, and social value of the DRGs payment policy was average.
4.5 Pre-test results
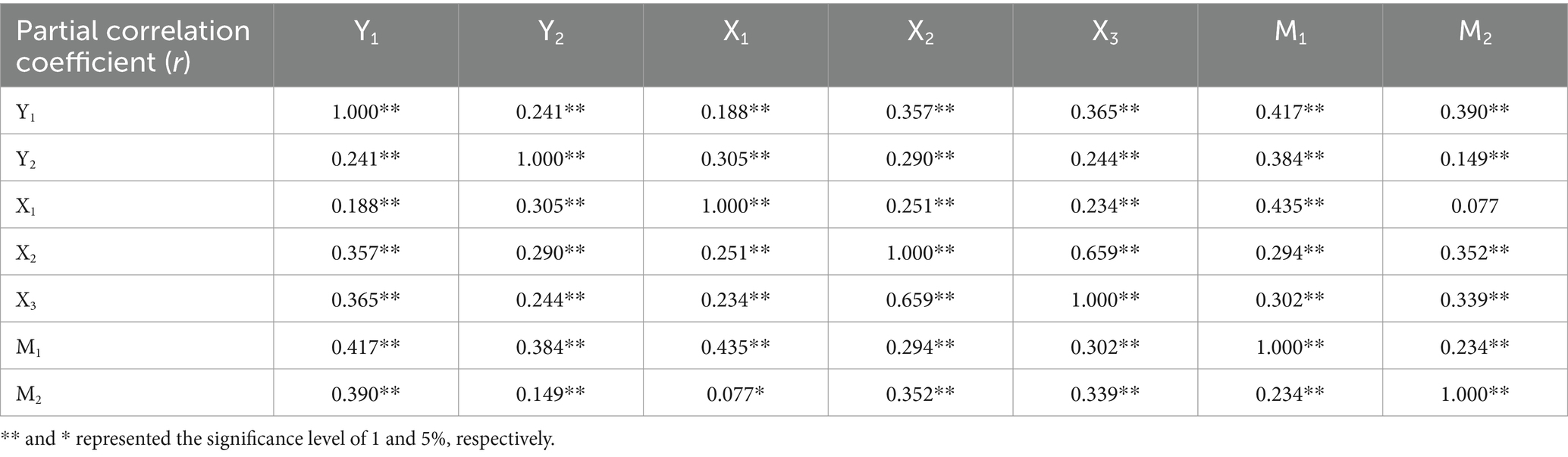
Under the condition of controlling age, gender, position, and other basic characteristic factors, the results of partial correlation regression analysis among core variables showed that there was a certain correlation between them, as shown in Table 6. Subsequently, the core variables were included in the multiple linear regression model successively according to the research requirements, and the F-test results all showed that the model had statistical significance as a whole (p < 0.05), and the VIF value of each variable was less than 10, which proved that there was no collinearity problem.
4.6 Intermediate effect test
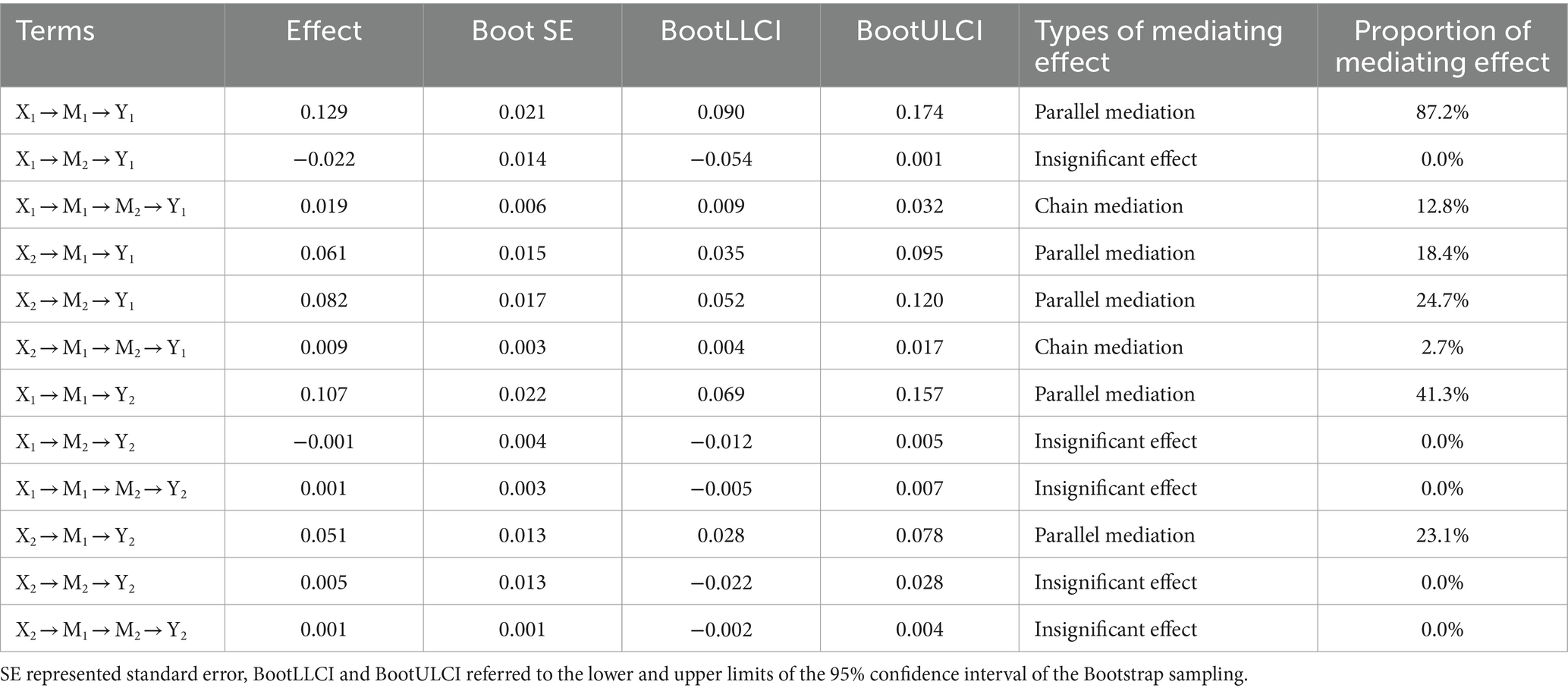
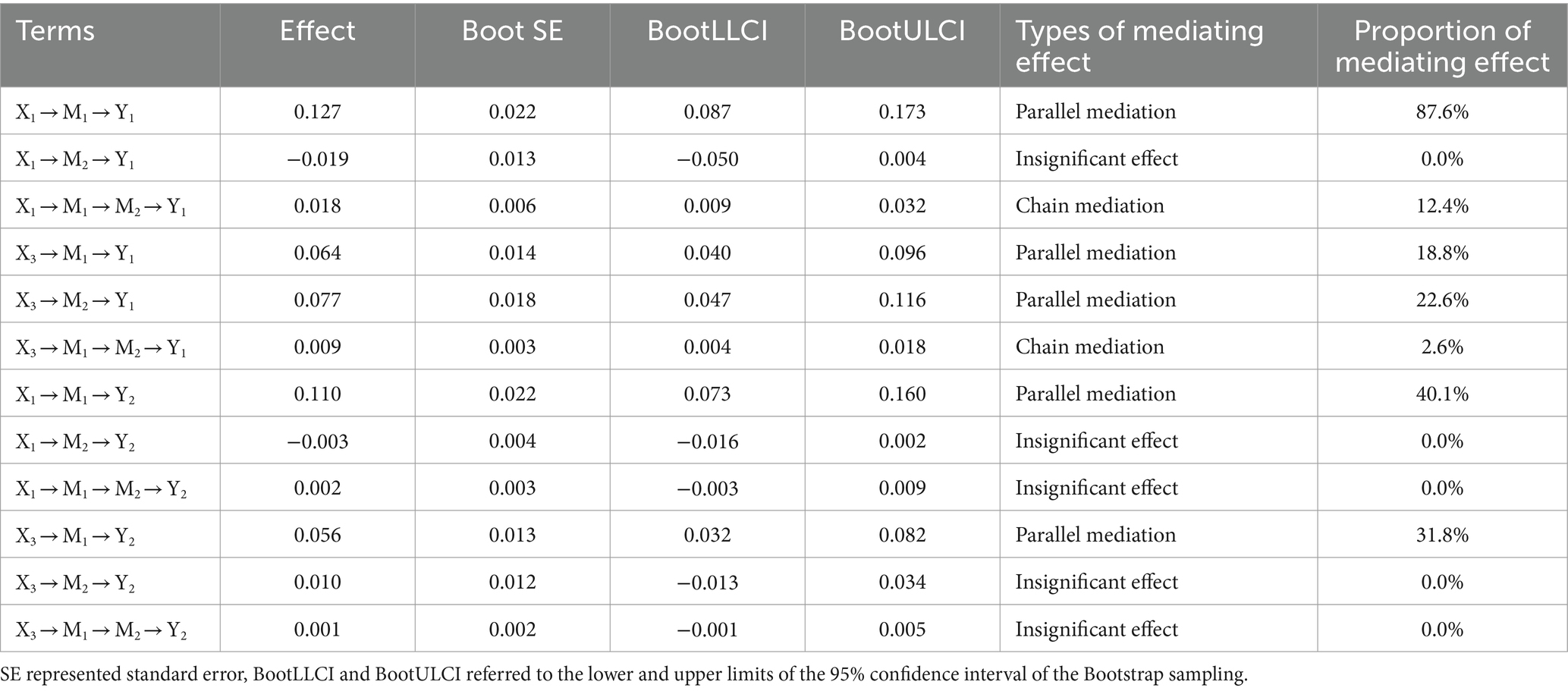
Combined with the analysis results in Tables 7, 8, it was shown that policy cognition had seven effective mediating paths in the process of policy advocacy and education promoting medical staff to adapt to the DRGs payment reform because the 95% confidence interval of Bootstrap sampling of their mediating effect value did not contain zero. These pathways included both parallel mediation and chain mediation, as well as partial mediation and complete mediation, among which the largest mediation effect value was 0.129, and the proportion of its effect (the ratio of mediating effect to total effect) was 87.2%, and the total mediation effect value of policy cognition was 0.148, 0.152, 0.108, and 0.057, respectively. At the same time, we found that the mediating effect of policy awareness was relatively larger than that of policy identity, and the chain mediating effect formed by the two was relatively smaller than that of the separate parallel mediating effect. Therefore, this study also drew the mediating effect paths diagram to better display and understand the research results, as shown in Figure 2.
4.7 Sensitivity analysis
To ensure the reliability of the research results, we applied the variable substitution method to carry out the sensitivity analysis, that is, the independent variable X2 was replaced by X3, and the intermediary effect analysis was carried out according to the steps above. The results were shown in Tables 9, 10, and the mediating action path, effect value, and effect proportion had basically not changed, which indicated that the research results had a certain credibility.
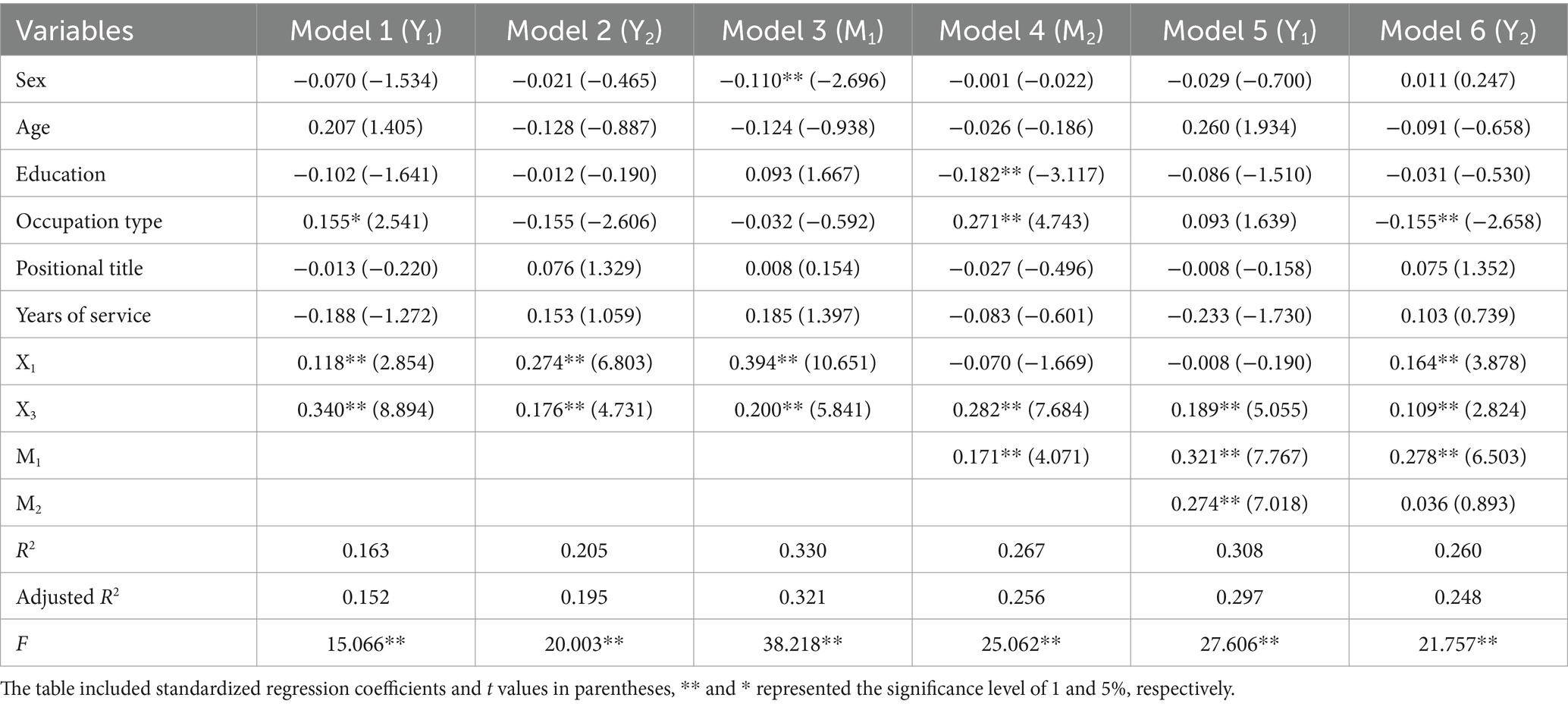
Table 9. Sensitivity analysis of the models in Table 7.
5 Discussion
The research results showed that organized and focused policy advocacy and education could promote the adaptation of medical staff to the DRGs payment reform by improving their cognition of the policy. Although this conclusion was the first to be proposed, many similar research conclusions that could be used as evidence. On the one hand, many practices and studies have confirmed that policy advocacy and education have an effective effect on people’s cognition and behavior, especially in the field of health intervention of health policy (40, 41). In addition, Doaty, Sarah and others also put forward more specific advocacy and education action plans (45). On the other hand, a large number of studies have shown that policy cognition could have an important impact on the public’s behavioral intention and results, including consumption behavior, health behavior, production behavior, and other fields (49–52). In addition, Zhou, Lingyi, Beasley, Lisa, and others also conducted a series of studies on the connotation of policy cognition and how it affected the adaptation to reform (38, 43). On this basis, this study suggested that it was no accident that policy advocacy and education could help medical staff adapt to health insurance reforms. This was because medical staff, although they were direct stakeholders in the DRGs payment reform, had a greater information asymmetry compared with policymakers, which made the enforcement of reform and their inherent cognition and behavior habits have a fierce collision, the phenomenon of maladaptation or superficial adaptation brought about by passive obedience was widespread (13, 21, 24). However, timely and accurate policy advocacy and education could just make up for their cognitive deficiencies, reduce misunderstanding and even resistance, and promote them to make correct behavioral responses to achieve real adaptation (44).
At the same time, we found that the mediating effects of policy awareness and policy identity were both chain and parallel, that is, there were ideal mediating paths from policy awareness to policy identity and non-ideal paths that only directly affected through policy awareness or policy identity, and the latter effect accounted for a relatively large proportion. The diversity of intermediary paths showed the complexity of policy advocacy and education influence process and also indicated that there were some problems on its own (43). The ideal action path conforms to both the knowledge-attitude-practice theory and the process of policy acceptance response from low to high, but the action path lacking policy awareness or policy identity often represents blind identification or passive obedience (25, 39), which belongs to the surface adaptation state and is not stable. Although this phenomenon is related to the differences in cognitive ability and social environment of medical staff (53), the universality and pertinence of policy advocacy and education still cannot be ignored.
The results also showed that the more times the medical staff participated in the policy advocacy and education activities or the better the feedback evaluation of them could promote their adaptation to the reform. However, there were differences in their action paths. The former must be based on improving the level of policy awareness to have an impact, and the overall effect of paths was relatively large. The latter could directly influence the adaptation to reform through various paths, but the overall effect is relatively small. This indicated that in the early stage of the reform, the information gap among medical staff was large, and a lot of policy advocacy and education could quickly improve their cognition, and then promote their response to new things, and finally achieve the state of adaptation. It is worth noting that this process of causing qualitative change through quantitative change will consume a lot of time so that the intervention efficiency is low (54). Therefore, improving the quality of advocacy and education is the long-term means to promote the adaptation to reform, which requires the organizers to pay attention to the feedback of medical staff promptly, formulate targeted advocacy and education strategies that meet the needs, and enrich the value connotation of it, so as to play a positive role in the cultivation of medical staff (55, 56).
In addition, we also found that medical staff’s self-perception and behavioral performance of adaptive state were affected by different paths, the former had a more extensive influence path and relatively large mediating effect, while the latter only promoted the generation of adaptive behaviors by improving the level of policy awareness. This indicated that the influence of policy advocacy and education had not realized the ideal mechanism of the knowledge-attitude-practice theory among the respondents, which once again confirmed the existence of the phenomenon of passive obedience. It is not hard to understand, on the one hand, due to the compulsory and dynamic nature of the reform, medical staff had to make adaptive responses in a short period to reduce conflicts of interest, such as choosing more cost-effective diagnosis and treatment plans, regulating fees, writing medical records more carefully, and introducing DRGs-related indicators for performance assessment, which conflicted with their perception under the old medicare payment system (29, 57). On the other hand, the new payment method itself was not perfect, such as unreasonable disease grouping, unscientific calculation method of payment standard, imperfect compensation mechanism, etc. (58, 59), coupled with insufficient policy advocacy and education, medical staff did not agree with the DRGs payment reform, and even conflict, thus forming a surface adaptation state with only objective behavior but no subjective perception.
6 Limitations
Firstly, although the questionnaire has passed the reliability and validity test, the design of the questionnaire is still subjective and has not been widely used before, and its universality needs to be further verified. Secondly, the sampling scope of this study is limited, and the sampling method is only approximate stratified sampling and convenience sampling, which is not completely random, which will cause some confusion or bias in the research results. In addition, due to the fact that there are currently few literatures related to the content of this study, although the innovativeness of the article is proved, the discussion section has relatively little literature basis.
7 Practical implications and theoretical implications
In terms of practical implications, this study provided a basis for policymakers and hospital managers to develop interventions to promote medical staff to adapt to DRGs payment reform, including constantly improving the DRGs payment system, increasing the number of organized collective policy advocacy and education, paying attention to the needs and feedback of medical staff, formulating targeted, timely and accurate policy advocacy and education content, highlighting the value connotation of DRGs payment reform, etc.
In terms of theoretical implications, this study combined the multidisciplinary theory to define the state of adaptation to reform, and designed the survey dimensions and questions accordingly, which provided a framework for investigation and research in related fields. Meanwhile, this study also revealed the complexity of the influence path of policy advocacy and education on cognition and behavior, and the process was affected by multiple factors, which did not necessarily fully conform to the traditional theory of knowledge-attitude-practice theory.
8 Conclusion and suggestion
Policy advocacy and education can promote medical staff’s adaptation to DRGs payment reform by improving their policy cognition, and the action paths are diverse. Policymakers and hospital managers should pay attention to this phenomenon, and formulate demand-centered, value-oriented whole-process advocacy and education strategies while constantly improving the DRGs payment system, so as to enable medical staff to adapt to the current reform faster and better. These also provided a basis for further research and practice of positive intervention in DRGs payment reform.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
Z-YN: Conceptualization, Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Writing – original draft. B-KZ: Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft. LS: Data curation, Investigation, Project administration, Software, Writing – original draft, Writing – review & editing. Z-YZ: Data curation, Methodology, Resources, Writing – original draft. HY: Conceptualization, Formal analysis, Investigation, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the General project of Education Department of Zhejiang Province, China (Grant No. YI22020037).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1375739/full#supplementary-material
References
1. Yu, L, and Lang, J. Diagnosis-related groups (DRG) pricing and payment policy in China: where are we? Hepatobil Surg Nutr. (2020) 9:771–3. doi: 10.21037/hbsn-2020-8
2. Liu, R, Shi, J, Yang, B, Jin, C, Sun, P, Wu, L, et al. Charting a path forward: policy analysis of China’s evolved DRG-based hospital payment system. Int Health. (2017) 9:317–24. doi: 10.1093/inthealth/ihx030
3. Sakurai, R. Pilot trial of the diagnosis related group and prospective payment system (DRG-PPS) in Japan. No.14, in series of articles: controversy and reform proposals concerning insured medical care in neurosurgery. Neurol Surg. (2003) 31:339–42.
4. Chilingerian, J In: JR Kimberly, G DePouvourville, and T Daunno, editors. Origins of DRGs in the United States: A Technical, Political and Cultural Story. Cambridge: Cambridge Univ Press (2008). 30 p.
5. Baum, GR, Stricsek, G, Kumarasamy, MA, Thirunavu, V, Esper, GJ, Boden, SD, et al. CPT-based procedure categorization enhances cost prediction of MS-DRG in spine surgery. Spine. (2020) 46:391–400. doi: 10.1097/BRS.0000000000003801
6. Kienapfel, H, Griss, P, and Hinrichs, F. DRG based development of revenues in orthopaedic surgery. A comparison of the development of cost weights and average lengths of hospital stay in Germany (G-DRG V1.0) and in Australian teaching hospitals (AR-DRG 4.1). Z Orthop Grenzg. (2003) 141:261–71. doi: 10.1055/s-2003-40082
7. Annear, PL, Kwon, S, Lorenzoni, L, Duckett, S, Huntington, D, Langenbrunner, JC, et al. Pathways to DRG-based hospital payment systems in Japan, Korea, and Thailand. Health Policy. (2018) 122:707–13. doi: 10.1016/j.healthpol.2018.04.013
8. Or, Z. Implementation of DRG payment in France: issues and recent developments. Health Policy. (2014) 117:146–50. doi: 10.1016/j.healthpol.2014.05.006
9. Coimbra, C, Esteves, M, Miranda, F, Portela, F, Santos, M, Machado, J, et al. (2017). Improving diagnosis-related groups with a computerized clinical coding tool for ICD-9-CM codification. Available online at: https://www.zhangqiaokeyan.com/academic-conference-foreign_meeting-260209_thesis/0705014085659.html (Accessed January 10, 2024)
10. Li, Q, Fan, X, and Jian, W. Impact of diagnosis-related-group (DRG) payment on variation in hospitalization expenditure: evidence from China. BMC Health Serv Res. (2023) 23:688. doi: 10.1186/s12913-023-09686-z
11. Peiling, W, Jie, Z, and Fanghong, JHospital Y, University CM. Status quo and countermeasures of diagnosis related groups-based payment for treatment of diseases in Beijing:analysis based on questionnaire survey among experts. Chin J Soc Med. (2019) 36:528–31. doi: 10.3969/j.issn.1673-5625.2019.05.023
12. Health Affairs (2024). Experience With Medicare’s New Technology Add-On Payment Program. Available online at: https://www.healthaffairs.org/doi/10.1377/hlthaff.27.6.1632 (Accessed January 10, 2024).
13. Chang, W-F, Yan, X-Y, Ling, H, Liu, T, and Luo, A-J. A study of the types and manifestations of physicians’ unintended behaviors in the DRG payment system. Front Public Health. (2023) 11:1141981. doi: 10.3389/fpubh.2023.1141981
14. Reinecke, H, Bunzmeier, H, Fürstenberg, T, Rothenburger, M, Böcker, D, Scheld, HH, et al. Evaluating the first German diagnosis-related groups (G-DRG) in cardiological patients: problems in the correct medical and economic grouping. Z Kardiol. (2003) 92:581–94. doi: 10.1007/s00392-003-0957-9
15. Pongpirul, K, Walker, DG, Rahman, H, and Robinson, C. DRG coding practice: a nationwide hospital survey in Thailand. BMC Health Serv Res. (2011) 11:290. doi: 10.1186/1472-6963-11-290
16. Fu, J, Huang, C, Li, S, and Xia, Y. Evolutionary game analysis of rural public-private partnership older adult care project in the context of population aging in China. Front Public Health. (2023) 11:1110082. doi: 10.3389/fpubh.2023.1110082
17. Li, J, and Feng, XL. Health care-seeking behaviours and health expenditures in adults aged 45 years and older in China, 2011-2013. Trop Med Int Health. (2017) 22:638–54. doi: 10.1111/tmi.12865
18. Jian, W, Lu, M, Liu, G, Chan, KY, and Poon, AN. Beijing’s diagnosis-related group payment reform pilot: impact on quality of acute myocardial infarction care. Soc Sci Med. (2019) 243:112590. doi: 10.1016/j.socscimed.2019.112590
19. Xu, K, Guo, Q, Zhou, C, Zhao, G, and Li, X. Study on the direct economic burden of hospital – acquired infection patients under CHS–DRG payment. J Clin Exp Med. (2023) 22:2458–62. doi: 10.3969/j.issn.1671-4695.2023.22.029
20. Gu, X, Lv, B, Zhao, M, and Zhang, P. The building of DRG-based payment system in Zhejiang: an “important window” for National Strategy of medical insurance provider-payment reform. China Health Insur. (2021) 6:39–45. doi: 10.19546/j.issn.1674–3830.2021.6.014
21. Zhang, L, and Sun, L. Impacts of diagnosis-related groups payment on the healthcare providers’ behavior in China: a cross-sectional study among physicians. RMHP. (2021) 14:2263–76. doi: 10.2147/RMHP.S308183
22. Guangrong, Z. On the restriction of nature to human with the viewpoint of systems theory. J Syst Dialect. (1998) 6:36–9.
23. Browning, CR, and Jackson, AL. The social ecology of public space: active streets and violent crime in URBAN neighborhoods. Criminology. (2013) 51:1009–43. doi: 10.1111/1745-9125.12026
24. Li, X, Zhang, Y, Zhang, X, Li, X, Lin, X, and Han, Y. Effects of fee-for-service, diagnosis-related-group, and mixed payment systems on physicians’ medical service behavior: experimental evidence. BMC Health Serv Res. (2022) 22:870–12. doi: 10.1186/s12913-022-08218-5
25. Liu, W, Peng, M, Li, J, Wu, J, Yu, L, Liu, X, et al. Investigation on clinicians' knowledge,belief and practice of DRG payment reform. Mod Hosp. (2023) 23:912–6. doi: 10.3969/j.issn.1671-332X.2023.06.024
26. Li, R, Li, Z, and Su, X. Investigation and analysis of medical staff's cognition of DRG. Jiangsu Healthcare Administr. (2023) 34:1099–102.
27. Schemske, DW. Adaptation and the origin of species. Am Nat. (2010) 176:S4–S25. doi: 10.1086/657060
28. Walter, GH. Individuals, populations and the balance of nature: the question of persistence in ecology. Biol Philos. (2008) 23:417–38. doi: 10.1007/s10539-007-9106-6
29. Peng, X, Li, Z, Zhang, C, Liu, R, Jiang, Y, Chen, J, et al. Determinants of physicians’ online medical services uptake: a cross-sectional study applying social ecosystem theory. BMJ Open. (2021) 11:e048851. doi: 10.1136/bmjopen-2021-048851
30. Leslie, JC. Herbert Spencer’s contributions to behavior analysis: a retrospective review of principles of psychology. J Exp Anal Behav. (2006) 86:123–9. doi: 10.1901/jeab.2006.04-06
31. Holliman, AJ, Waldeck, D, Jay, B, Murphy, S, Atkinson, E, Collie, RJ, et al. Adaptability and social support: examining links with psychological wellbeing among UK students and non-students. Front Psychol. (2021) 12:636520. doi: 10.3389/fpsyg.2021.636520
32. Li, F (2015). “Training of Student’s social adaptability by physical education teaching of higher vocational College” in Proceedings of the International Conference on Education, Management, Commerce and Society. Advances in Social Science Education and Humanities Research. eds. Yingying S, Guiran C, Zhen L; Atlantis Press, Paris. p. 328–332. Available online at: https://www.webofscience.com/wos/woscc/full-record/WOS:000358533200066 (Accessed January 10, 2024).
33. Goldfarb-Rumyantzev, A, Barenbaum, A, Rodrigue, J, Rout, P, Isaacs, R, and Mukamal, K. New social adaptability index predicts overall mortality. Arch Med Sci. (2011) 4:720–7. doi: 10.5114/aoms.2011.24145
34. Pan-Shi, W, and Xiang, Z. A study on social adaptation mode of minority residents. J Xingyi Norm Univ Nat. (2014) 1:94–7.
35. Chi, Y. Research on rural disabled People's adaptive behavior to medical security. Shandong Univ. (2021). doi: 10.27272/d.cnki.gshdu.2021.003017
36. Cao, G. The change from tradition to modern: the change of farmers' fertility view in 30 years of reform and opening up. J Hunan Administr Instit. (2008) 6:39–42. doi: 10.16480/j.cnki.cn43-1326/c.2008.06.027
37. Xin-Ping, WU. College ideological and political education from the perspective of the three processes of attitude change. J Yunmeng. (2011) 32:118–22.
38. Zhou, L, Dai, D, Ren, J, Chen, X, and Chen, S. What is policy content and how is the public’s policy support? A policy cognition study based on natural language processing and social psychology. Front Psychol. (2022) 13:941762. doi: 10.3389/fpsyg.2022.941762
39. Ahmed, B, Rehman, HM, Javaid, S, and Binyamin, M. Knowledge, attitude, practice and risk assessment of frontline healthcare professionals related to Covid-19 in Lahore. Biosci Res. (2022) 19:210–21.
40. Thompson, RL, Belokas, J, Johnson, K, and Williams, AL. The public policy advocacy actions checklist: success stories from three states. Behav Anal Pract. (2023). doi: 10.1007/s40617-023-00874-1
41. Amini, H, Wells, AJ, Boynton, JR, Guo, X, and Ni, A. Oral health advocacy education impacts future engagement: exploration at a Midwestern US dental school. Front Oral Health. (2021) 2:714199. doi: 10.3389/froh.2021.714199
42. Sardell, A In: M Halliwell and SA Jones, editors. US Children’s Health Insurance: Policy Advocacy and Ideological Conflict. Edinburgh: Edinburgh Univ Press (2022). 17 p.
43. Beasley, L, Grace, S, and Horstmanshof, L. Responding and adapting to change: an allied health perspective. Leadersh Health Serv. (2020) 33:339–49. doi: 10.1108/LHS-07-2019-0050
44. Molina, Y, San Miguel, C, Sanz, S, San Miguel, L, Rankin, K, and Handler, A. Adapting to a shifting health care landscape: Illinois breast and cervical cancer program Lead agencies’ perspectives. Health Promot Pract. (2019) 20:600–7. doi: 10.1177/1524839918776012
45. Doaty, S, Bitencourt, N, Harvey, W, Kolasinski, S, and Solow, EB. Advocacy 101: engaging rheumatology fellows in health policy and advocacy. Arthritis Care Res. (2019) 71:1141–5. doi: 10.1002/acr.23749
46. Jimenez-Gamero, MD, Munoz-Garcia, J, Munoz-Reyes, A, and Pino-Mejias, R. On Efron’s method II with identification of outlier bootstrap samples. Comput Stat. (1998) 13:301–18.
47. Levy, JA, Landerman, LR, and Davis, LL. Advances in mediation analysis can facilitate nursing research. Nurs Res. (2011) 60:333–9. doi: 10.1097/NNR.0b013e318227efca
48. Zhang, Z. Monte Carlo based statistical power analysis for mediation models: methods and software. Behav Res Methods. (2014) 46:1184–98. doi: 10.3758/s13428-013-0424-0
49. Wang, J, Liu, H, and Yin, H (2012). “How the personal cognition affect the health insurance reform-based on the empirical analysis of residents’ health and medical demands” in Proceedings of 2012 International Conference on Public Administration (8th), Vol III. (eds.) Zhu XN, Zhao SR Univ Electronic Science & Technology China Press, Chengdu. p. 135–153. Available online at: https://www.webofscience.com/wos/woscc/summary/24be62ff-2322-43fd-8292-07d9bd1db3f4-c4612c9b/relevance/1 (Accessed January 11, 2024)
50. Xiong, Y, and Wang, L. Policy cognition of potential consumers of new energy vehicles and its sensitivity to purchase willingness. J Clean Prod. (2020) 261:121032. doi: 10.1016/j.jclepro.2020.121032
51. Yingying, N, Junfeng, D, Kai, Z, and Jingjing, S. The influence of farmers’ policy cognition on their cultivated land protection (CLP) behavior in Huaxian County in Henan. J Henan Agric Univ. (2018) 52:648–56. doi: 10.16445/j.cnki.1000-2340.2018.04.026
52. Wang, Z, Sun, Y, and Wang, B. Policy cognition is more effective than step tariff in promoting electricity saving behaviour of residents. Energy Policy. (2020) 139:111338. doi: 10.1016/j.enpol.2020.111338
53. Shi, L, and Qian, S-R (2016). “Maletzke model of mass communication in the network education” in 2016 2nd International Conference On Modern Education And Social Science (MESS 2016). Destech Publications, Inc., Lancaster. p. 743–745. Available online at: https://www.webofscience.com/wos/woscc/summary/0a150bf6-a33d-45aa-aa89-08733101267d-c499d3e5/relevance/1 (Accessed January 12, 2024).
54. Shu, W. From "quantitative change" to "qualitative change" the internet of things still has a long way to go. Commun World. (2022) 18:1. doi: 10.13571/j.cnki.cww.2022.18.014
55. Salwen, MB (1993). Communication models for the study of mass communication, second edition (book). World Communication. Available online at: http://connection.ebscohost.com/c/book-reviews/10959863/communication-models-study-mass-communication-second-edition-book (Accessed January 11, 2024).
56. Shah, Z, Chu, J, Ghani, U, Qaisar, S, and Hassan, Z. Media and altruistic behaviors: the mediating role of fear of victimization in cultivation theory perspective. Int J Disaster Risk Reduct. (2020) 42:101336. doi: 10.1016/j.ijdrr.2019.101336
57. Ma, X, and Wang, Y. Application of Grey relational entropy weight method in DRG performance evaluation of inpatient departments. Contrast Media Mol Imag. (2022) 2022:1–9. doi: 10.1155/2022/7348985
58. Liu, X, Fang, C, Wu, C, Yu, J, and Zhao, Q. DRG grouping by machine learning: from expert-oriented to data-based method. BMC Med Inform Decis Mak. (2021) 21:312. doi: 10.1186/s12911-021-01676-7
Keywords: DRGs payment reform, policy advocacy and education, policy cognition, adaptation, mediating effect
Citation: Ni Z-Y, Zhang B-K, Song L, Zang Z-Y and Yu H (2024) The influence of policy advocacy and education on medical staff’s adaptation to diagnosis related groups payment reform in China: an analysis of the mediating effect of policy cognition. Front. Public Health. 12:1375739. doi: 10.3389/fpubh.2024.1375739
Edited by:
Alexandre Morais Nunes, University of Lisbon, PortugalReviewed by:
Habib Nawaz Khan, University of Science and Technology, Bannu, PakistanAna Moreira, University Institute of Psychological, Social and Life Sciences (ISPA), Portugal
Copyright © 2024 Ni, Zhang, Song, Zang and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Yu, Ymx1ZXl1MDAwQHpqdS5lZHUuY24=
†These authors have contributed equally to this work
 Zhi-Ying Ni†
Zhi-Ying Ni† Bo-Kai Zhang
Bo-Kai Zhang Hong Yu
Hong Yu