- 1Achutha Menon Centre for Health Science Studies, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, Kerala, India
- 2Manipal Academy of Higher Education, Manipal, Karnataka, India
- 3Amrita Institute of Medical Sciences, Kochi, Kerala, India
Background: Diabetes and hypertension are leading public health problems, particularly affecting low- and middle-income countries, with considerable variations in the care continuum between different age, socio-economic, and rural and urban groups. In this qualitative study, examining the factors affecting access to healthcare in Kerala, we aim to explore the healthcare-seeking pathways of people living with diabetes and hypertension.
Methods: We conducted 20 semi-structured interviews and one focus group discussion (FGD) on a purposive sample of people living with diabetes and hypertension. Participants were recruited at four primary care facilities in Malappuram district of Kerala. Interviews were transcribed and analyzed deductively and inductively using thematic analysis underpinned by Levesque et al.’s framework.
Results: The patient journey in managing diabetes and hypertension is complex, involving multiple entry and exit points within the healthcare system. Patients did not perceive Primary Health Centres (PHCs) as their initial points of access to healthcare, despite recognizing their value for specific services. Numerous social, cultural, economic, and health system determinants underpinned access to healthcare. These included limited patient knowledge of their condition, self-medication practices, lack of trust/support, high out-of-pocket expenditure, unavailability of medicines, physical distance to health facilities, and attitude of healthcare providers.
Conclusion: The study underscores the need to improve access to timely diagnosis, treatment, and ongoing care for diabetes and hypertension at the lower level of the healthcare system. Currently, primary healthcare services do not align with the “felt needs” of the community. Practical recommendations to address the social, cultural, economic, and health system determinants include enabling and empowering people with diabetes and hypertension and their families to engage in self-management, improving existing health information systems, ensuring the availability of diagnostics and first-line drug therapy for diabetes and hypertension, and encouraging the use of single-pill combination (SPC) medications to reduce pill burden. Ensuring equitable access to drugs may improve hypertension and diabetes control in most disadvantaged groups. Furthermore, a more comprehensive approach to healthcare policy that recognizes the interconnectedness of non-communicable diseases (NCDs) and their social determinants is essential.
1 Introduction
Noncommunicable diseases (NCDs), also known as chronic diseases, are a major global health challenge responsible for more than two-thirds (73%) of all-cause mortality (1). Furthermore, the majority of NCD deaths occur in low- and middle-income countries (LMICs) (2). Importantly, many NCD-related deaths are premature and preventable (2, 3). Even after a decade since the launch of the National Programme for Prevention & Control of Non-Communicable Diseases (NP-NCD) by the government of India, the prevalence, awareness, treatment, and control rates of diabetes and hypertension remain abysmally poor in primary care settings with notable variations across districts, age, and socio-economic groups (4–6).
Globally, primary health care is recognized as the cornerstone of developing a resilient health system approach to preventing and controlling NCDs (7, 8). Previous evidence suggests that an effective primary health care system contributes to NCD control by encouraging a healthy lifestyle, preventing the onset of NCDs, decreasing premature NCD-related deaths, improving the quality of care, and reducing hospital admissions related to NCDs (9–11). Additionally, Primary Health Centers (PHC) fosters community involvement in NCD prevention and control, ensuring equitable NCD care access (12). However, in India, health systems were initially designed to address acute communicable diseases and maternal and child health (13) but now grapple with the challenge of delivering care for chronic conditions (14, 15). The primary care system for NCDs remains weak with underfunding, fragmented service delivery, and poorly functioning referral systems and faces significant resource constraints, including limited health workforce, medicine, supplies, and infrastructure (16–19). Further, this situation is worsened by disparities of socio-economic class, caste, and gender, which manifest as health inequalities (20). Recently, the Government of India launched the National Health Protection Mission known as the Ayushman Bharat to bring a comprehensive range of services closer to communities by transforming PHCs and sub-centers into Health and wellness centers (HWCs) and achieve universal health coverage in India (21–24).
In parallel, the Government of Kerala initiated the “Aardram Mission” in 2017 to revitalize the PHCs, recognizing the importance of strengthening universal primary care (25). This transformation involved upgrading PHCs to Family Health Centers (FHCs), which aligned with the national model of HWCs, with additional healthcare providers, and a comprehensive package of primary care services (25). Furthermore, the services at PHCs were strategically restructured to address the current epidemiological situation, with a particular focus on NCDs (26, 27). The increasing prevalence of diabetes and hypertension is considered a primary driver of this epidemiological transition.
Despite the discourse in policies regarding the importance of comprehensive care for managing diabetes and hypertension, research on patient experience remains under-investigated. Evidence highlights the central role of patient experience in healthcare quality (28). Therefore, mapping the entire patient journey and understanding various factors that influence how people with diabetes and hypertension access the healthcare system when needed is the key to understanding the patient experience and identifying any existing gaps. Against this background, our study aimed to explore the experiences of persons living with diabetes and hypertension (PLWDH) regarding their access to primary health care services to manage these conditions and to examine if the community expectations from FHCs resonate with the above-proposed policy direction.
2 Methods
2.1 Study design
This study is an exploratory (29) descriptive (30) qualitative research involving data collection through semi-structured interviews and focus-group discussions conducted among persons with diabetes, hypertension, or both in outpatient settings in Malappuram, Kerala.
2.2 Study setting
We conducted this study in purposively selected four FHCs of Malappuram, Kerala, from September 2022 to March 2023. Notably, all these health centers underwent a transformation in the initial phase of the Aardram mission in 2017. Malappuram, a northern district in Kerala, has a population of 4,112,920 (31). Malappuram was among the first districts in Kerala where the National Program for NCDs was implemented, and the community-based palliative care model for NCD was piloted in 1996 (32). A recent study in the district reported an NCD-multimorbidity prevalence of 39.8% among people seeking care from FHCs. Notably, the prevalence was higher in men (42.6%) than in women (38.1%). Hypertension and diabetes were the predominant coexisting chronic conditions (33). Malappuram is divided into 15 health blocks, with 59 fully functional FHCs implementing the national program for preventing and controlling non-communicable diseases (NP-NCD) across these blocks (33).
FHCs provide a range of services--- including health promotion activities, screening, laboratory services, and outpatient management for patients with diabetes and hypertension under the NCD program. The state has recently initiated the population-based screening of NCDs and risk factors (26), facilitated by Accredited Social Health Activists (ASHAs) and (JPHN), and suspected cases are referred to medical officers at FHCs. Patients requiring specialized care are referred to NCD clinics in community health centers or district hospitals. Additionally, the program offers free medicines for diabetes and hypertension at these facilities, with patients receiving their prescribed medications every month following consultation at the FHCs. Electronic health records and information systems at the patient level are being introduced in these centers (34).
2.3 Study participants, sampling strategy
The study population included adult individuals living with confirmed diabetes/hypertension or both, regardless of the disease stage or control status, in four FHCs in the Malappuram district. Purposive sampling (35) was used to identify eligible participants, following inclusion criteria: adults (18 years of age and older) seeking healthcare from public facilities or both public and private healthcare facilities for a minimum of six months. The assistance of local community health workers facilitated the identification of participants.
2.4 Data collection
In the first phase, semi-structured interviews were conducted face-to-face (36) with twenty adult participants. RR conducted all interviews in Malayalam using topic guides (Supplementary material S1). Pre-testing of the topic guides was undertaken before data collection. Each selected respondent was interviewed in a calm setting within health facility premises. All interviews were audio-recorded, and their duration ranged from 20 to 60 minutes.
We conducted one focus group discussion (FGD) (37) with six adults in the study area during the second phase. A heterogeneous group was selected for the FGD with different control statuses – achieved, not achieved, and taking insulin/oral hypoglycaemics or both, diagnosed but did not initiate the treatment. An experienced social worker and a junior public health nurse identified and recruited eligible participants for FGD. A topic guide was used to introduce different themes during the discussion. Basic demographic details like age, gender, marital status, education, and occupation were collected from each participant. Topics encompassed patients’ experiences of living with a chronic illness, health care utilization, and challenges in accessing health care. The FGD was audio-recorded and lasted for 60 minutes.
RR translated and transcribed all the interviews. Transcripts were checked multiple times to minimize mistakes made during transcription. Participant recruitment concluded following thematic saturation (meaning the researchers collectively determined that additional interviews were unlikely to yield new insights or information on the subject) (38). In total, 26 people participated in the study.
2.5 Data analysis
The analysis of interview transcripts and fieldwork notes employed a thematic analysis approach (39). A coding framework was developed after multiple readings of the transcripts and notes (40). This framework was systematically applied to the dataset with attention to recurring codes and their clustering around specific contexts. The coded data were organized to facilitate thematic interpretation. Ongoing discussions among all authors informed this analytical process, with consensus achieved through iterative reviews of codes and themes. Emphasis was placed on discerning similarities and differences across participants’ data, aiming to construct an explanation of the findings. Notably, any deviant cases were scrutinized to enhance the trustworthiness and rigor of the qualitative analysis (41).
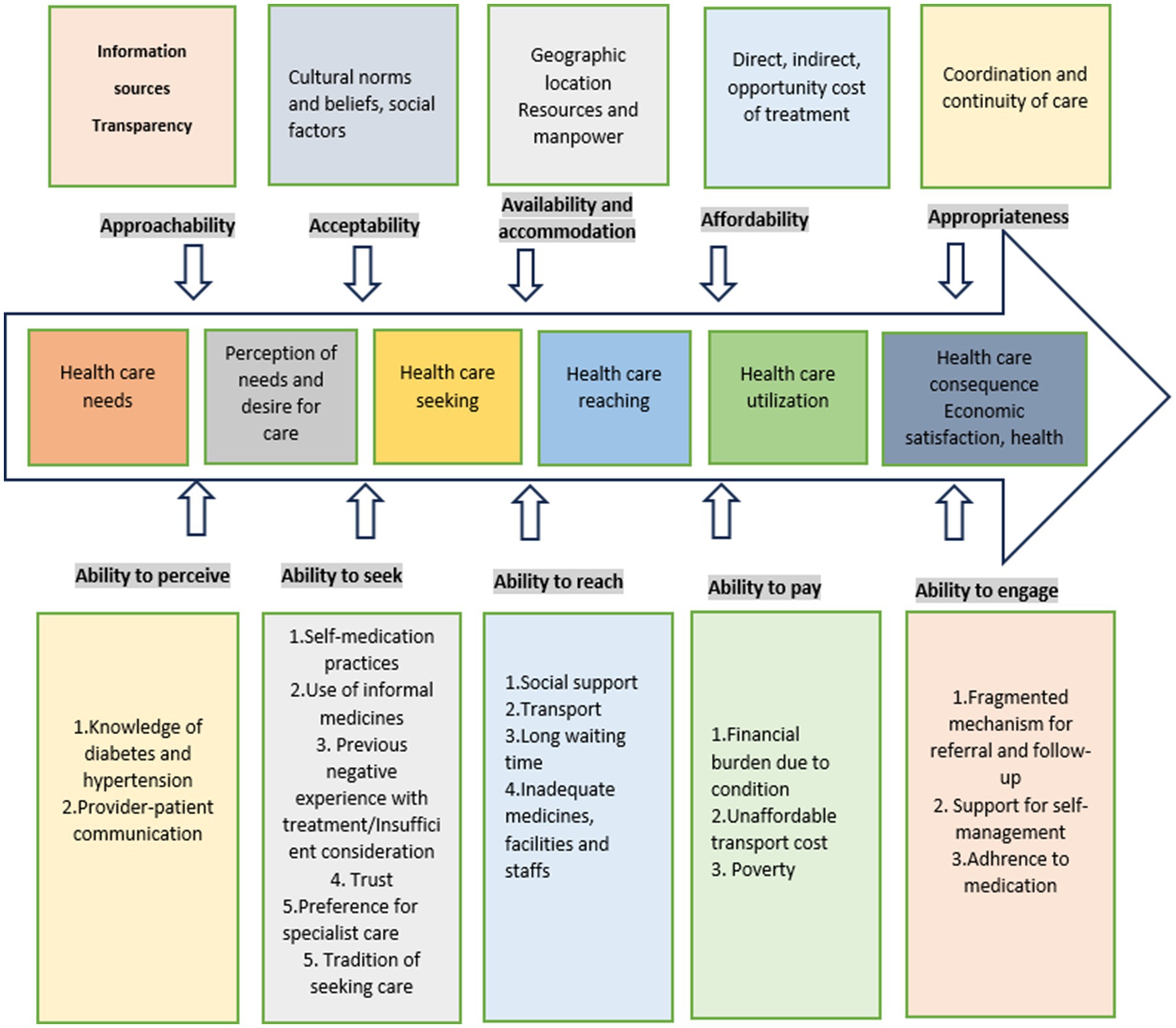
The thematic framework derived from this analytical process closely aligns with the conceptual framework proposed, which focuses on the patient’s ability to access healthcare services (42). However, it is important to note that this framework was not applied as an a priori model for the research; instead, it was introduced in a subsequent stage to inform further analysis of patients’ health-seeking pathways and to explore perceived barriers to care among these healthcare users. The Levesque framework encompasses different stages of healthcare-seeking pathways, providing a valuable lens for examining the narratives of the study participants.
The patient journey for NCDs can be structured into five stages: awareness, screening, diagnosis, treatment, and adherence (Figure 1) incorporating rehabilitation (43). The accessibility of services shapes the patient’s journey. Levesque et al.’s access-to-care model served as our conceptual framework to examine the factors influencing access to care at both the health system and population levels. The model examined healthcare access across five dimensions: approachability, acceptability, availability and accommodation, affordability, and appropriateness. The above-mentioned access dimensions are influenced by the patient’s ability to perceive, seek, reach, pay, and engage. Access results from the interplay between supply and demand dimensions within the continuum of care, spanning from individuals’ recognition of health needs to healthcare outcomes (42).
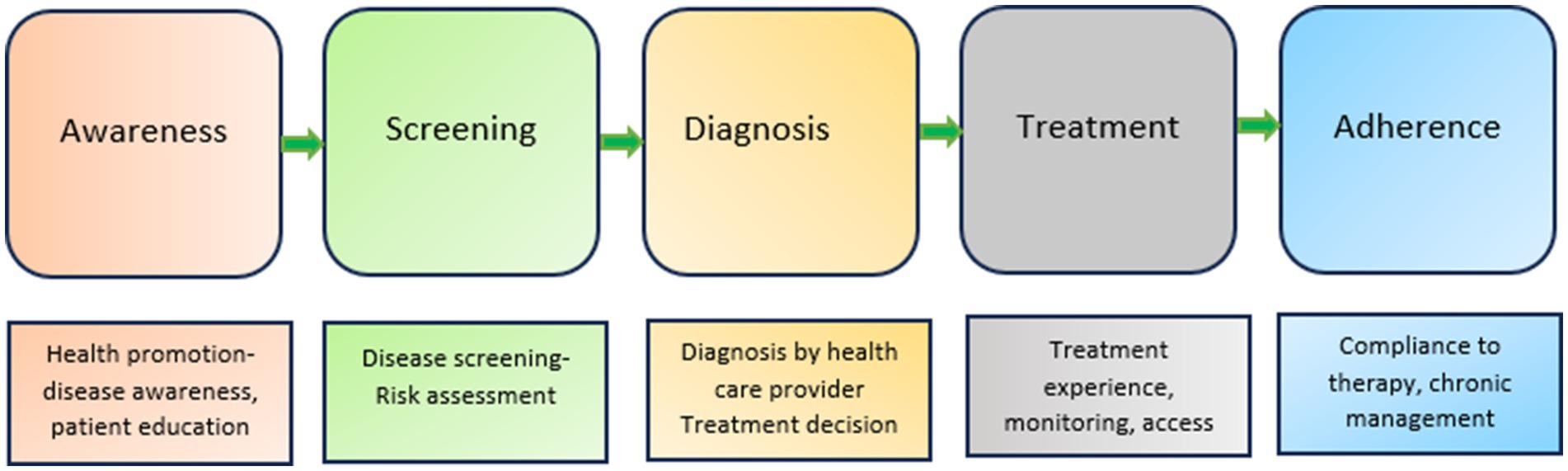
Figure 1. Patient journey for NCDs [Reprinted from Devi et al. (43)].
3 Results
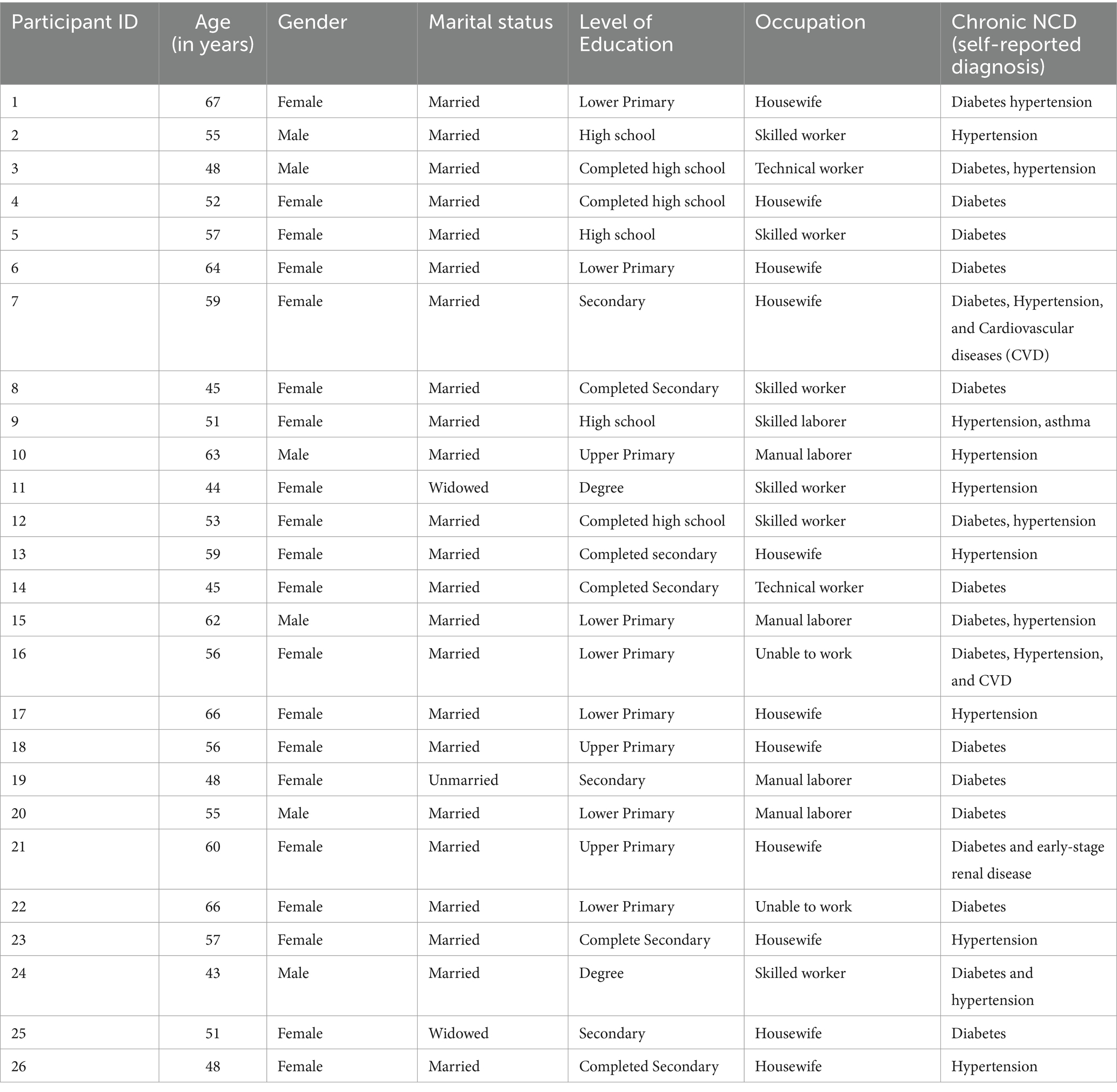
A total of 26 people living with diabetes/hypertension or both participated in the study. These participants varied in age, chronic conditions, control status, and background. The patients were aged between 43 and 67 years, with seven participants diagnosed only with diabetes, five with hypertension, and three with both diabetes and hypertension, while the remaining four participants suffered from other comorbidities associated with these conditions (Table 1). Most of them were unemployed (n = 14), and identified themselves as poor.
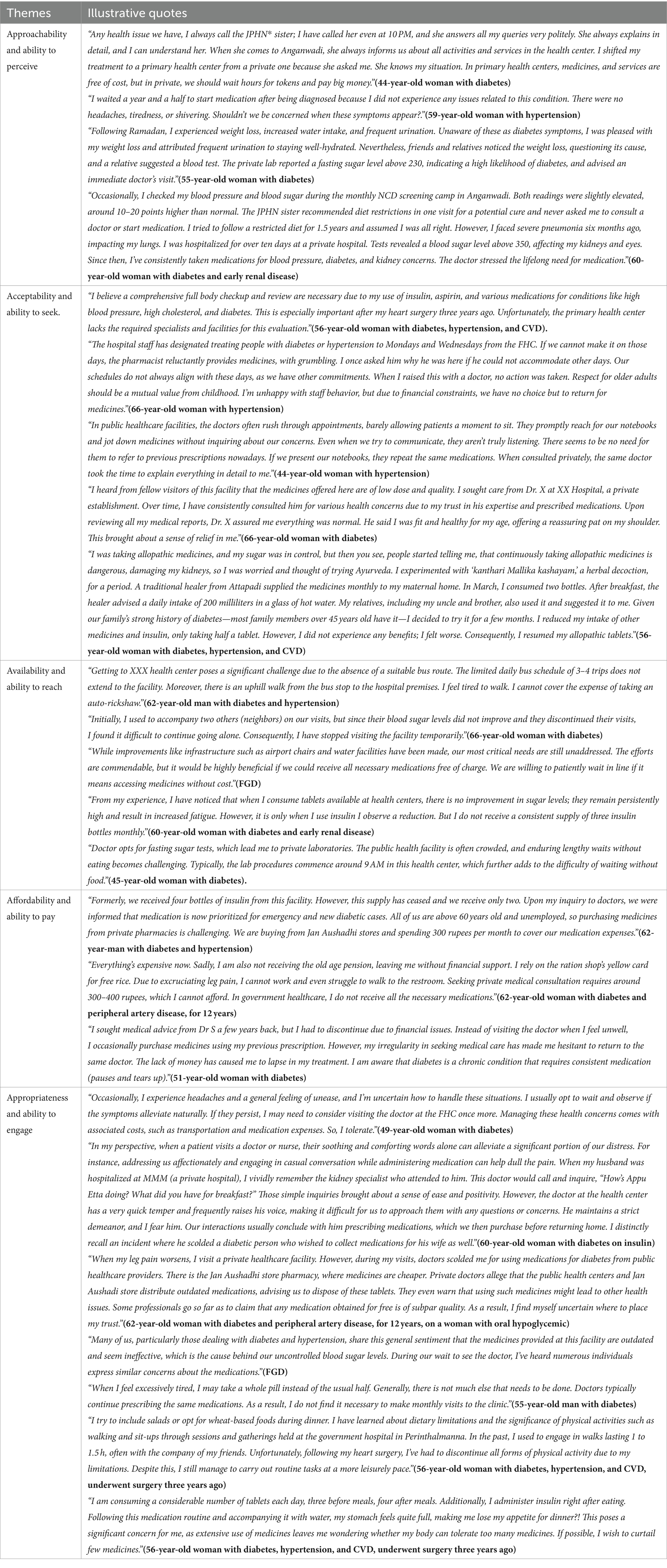
Our analysis demonstrated factors contributing to a complex health-seeking pathway for individuals with diabetes and hypertension. These factors align with the five domains outlined in the Levesque framework (42). The five identified themes correspond to the key access dimensions and associated abilities from the patient’s viewpoint, as depicted in Figure 2. The themes and the illustrative quotes are presented in Table 2. Additional quotes can be found in Supplementary Table S2.
3.1 Approachability and ability to perceive
Approachability refers to the “ability of individuals with healthcare needs to identify, to seek information on the existing forms of services and perceive their potential impact on their health” (42). Some participants said they were provided sufficient information on the services available in health facilities through community health staff like ASHAs and JPHNs. Few participants recalled outreach screening activities for diabetes and hypertension conducted in public spaces like Anganwadi’s in their area. However, many patients also reported several other sources of information available to them besides those provided by community health workers and doctors. For instance, patients gained prior knowledge through personal experience from family members, friends, and media. Patients reported these sources provided information on lifestyle changes, medication adherence, etc.
Participants’ ability to perceive the need for care was determined by factors such as patients’ knowledge about health conditions (perception of risk), age, education, and beliefs related to health and illness. Ensuring timely access to healthcare services and optimal adherence to long-term treatments relied on patients’ understanding of their chronic condition when symptoms arise. Most of the patients reported being aware of hypertension and diabetes before diagnosis. However, participants reported sub-optimal knowledge of preventive measures and treatment needs. Older women interviewed in the study were unaware that hypertension is usually asymptomatic, and there was limited knowledge of potential outcomes. When asked what causes hypertension, one patient interviewed reported that stress causes hypertension. Some of the participants failed to understand their symptoms were indicative of diabetes and hypertension and that addressing their condition might entail more than just making lifestyle changes; instead, it may require long-term treatment as well. Some participants also believed that chronic diseases like diabetes and hypertension only impact older adults.
Instances were reported when patients did not receive sufficient information and support from the healthcare field staff to develop an adequate understanding of their condition, even after being suspected of diabetes or hypertension, in screening camps. Inadequate knowledge about their conditions led these participants to wait until their conditions were no longer manageable, leading to delays in seeking care.
In general, when assessing the patients’ views in our study on diabetes and hypertension, the younger individuals minimized its importance. In contrast, mostly the older group of patients acknowledged the severity of the condition and sought treatment.
3.2 Acceptability and ability to seek
This theme addresses “the social and cultural factors that affect patient’s ability to receive and accept healthcare services” (42). Our conversations showed that study participants desired FHCs to function as health facilities catering to minor health concerns. There was a general acknowledgment among people that FHCs were not equipped to handle complex medical conditions. As a result, people did not anticipate that FHC staff would address all health issues. Moreover, patients did not expect to get integrated care for managing multiple chronic conditions from FHCs.
Despite the nature of the visit being routine follow-ups, some patients preferred specialist services if their budget allowed. However, the availability of free medications and services and proximity to the residence enticed them to seek care from the FHCs.
We found that private care with specialists was predominantly reserved for managing immediate medical issues or complications arising from their conditions. The participants also commonly believed that higher-level hospitals would offer superior healthcare due to enhanced diagnostic capabilities and skilled medical professionals. Most of the patients had consulted multiple providers since their initial diagnosis.
The participants’ social background and trust in the healthcare system affected their ability to access healthcare services. The degree of trust was influenced by their personal (or social network’s) prior encounters with services, the reputation of selected health facilities, and the belief that higher-level health facilities offered better service quality. Prescribers’ attitudes influenced trust in treatment. People had preconceived notions about the doctors and other staff. People often complained that doctors in FHCs failed to give them sufficient attention and respect. The perception of the government doctors’ indifferent attitude stemmed from the belief that they were not incentivized or paid extra at government facilities. Patients also believed that in private practice, doctors spent time and prescribed medications that were more effective in improving blood sugar levels and controlling blood pressure, enhancing the perception of better healthcare outcomes under private care. Thus, in addition to expertise in clinical skills, patients valued the doctor’s communication style. On the other hand, we observed a decline in trust in a physician due to an unfavorable experience, leading a participant to abstain from using health services provided by that doctor.
Many participants were accustomed to pursuing alternative therapies, such as traditional medicines, rooted in their cultural practices. Our interviews with some patients revealed that they discontinued the prescribed allopathic medications and adopted traditional medicines without any formal advice after achieving the control status. Some patients considered medicines as chemicals with potential side effects and resorted to alternate systems of medicines. While others developed a fear of becoming dependent on medications lifelong, leading them to explore alternative treatments to reduce reliance on medicines provided by the facility. Previous lack of improvement with allopathic treatment and success stories from people who have experienced positive results with alternate treatment prompted a few to consider these options.
3.3 Availability and ability to reach
This theme concerns “the extent to which people can avail healthcare services” (42). Few participants highlighted that the remote geographic location of the health center hindered their access to healthcare services. Private transportation to healthcare facilities was expensive and challenging for older patients, restricted by the distance they could travel.
The capability of the older participants to reach the facility was influenced by the presence of a family member or neighbor who could accompany them to the healthcare facilities.
Most respondents emphasized that in the past few years (due to the restructuring of primary care services under the Aardram mission), they have experienced improved healthcare services through upgrades in infrastructure, greater availability of doctors and laboratory facilities, and the introduction of evening out patients’ departments (OPDs). While expanded provision of the services was positively viewed to enhance accessibility, respondents noted the major deficiencies in service adequacy. A prevailing concern among most patients was the irregular availability of free medicines, leading to challenges in adhering to their prescribed treatment. Several patients reported that the shortage of drugs compelled them to personally bear the cost of purchasing them from local pharmacies. Furthermore, few patients expressed dissatisfaction with the facility’s restricted range of treatment options, often limited to just two or three medications for addressing their medical conditions.
Patients who had multiple NCDs described intensified symptoms associated with a lack of access to medicines. One patient talked about the challenges she faced in accessing a reliable supply of insulin.
In some cases, health services were available to patients, but this did not translate to services being accessible to patients. For instance, in health centers, laboratories and pharmacies were available at the same location. Still, these services were often unavailable due to a lack of supplies, medicines, or human resources. Most participants said the public health facility was usually crowded, with substantial waiting times and an inconvenience in managing fasting tests due to the overcrowding and the timing of lab procedures. Consequently, many patients resorted to visiting private clinics or laboratories to monitor their glucose levels, incurring additional time and expenses. Almost all the patients voiced their dissatisfaction with being asked to return to FHC every month to obtain medicines, finding it inconvenient and burdensome.
3.4 Affordability and ability to pay
This theme encompasses the economic capacity of people to afford healthcare expenses. Despite medications being free at public health facilities, the recurring scarcity of medicines and the need for frequent doctor visits were deemed financially challenging for many. This financial barrier had two aspects: the expense of regular medications and the cost of immediate prescriptions during symptom exacerbations, requiring hospitalizations, antibiotics, etc. Participants perceived that private health facilities offer superior service quality, leading many participants to choose out-of-pocket expenses for these hospitals despite the financial strain. Most respondents reported they lacked any form of health insurance.
The burden of out-of-pocket spending was highlighted as a core issue for older adults with chronic illnesses. Out-of-pocket expenses and financial constraints resulted in treatment gaps and often resulted in making choices about which medications to buy following a doctor’s prescription.
Participants emphasized that time spent on all-day travel hindered patients from working, earning an income, or attending to family responsibilities. Young male patients reported discontinuing monthly visits to public facility doctors due to the substantial time investment.
3.5 Appropriateness and ability to engage
Appropriateness refers to “how well services align with client requirements, including timely delivery, a thorough evaluation of health issues for accurate treatment determination, and the technical and interpersonal excellence of services” (42).
The long-term management of diabetes and hypertension demands consistent adherence to a treatment plan. Various factors affected the participants’ ability to follow their extended management plan. Long-term care involved regular hospital visits for obtaining medications and during worsening of symptoms. However, not all patients in our study could manage regular visits due to affordability issues, which interfered with adherence. The patient-provider relationship was an important factor related to adherence and patient satisfaction. Our interviews with patients revealed trust was is fostered when providers see patients as individuals, not merely cases. Additionally, displaying acceptance and respect contributed to nurturing this sense of confidence. Patients also expressed their frustration while reporting that they often left OPDs without getting the information they wanted, feeling overwhelmed and unable to understand the information provided. It was evident from patients’ accounts that they lacked preparedness to manage their health conditions when experiencing symptoms like pain and fatigue. These factors contributed to feelings of uncertainty about their future health. However, a few patients felt capable and confident in managing their conditions. They acquired skills through diverse experiences—some from their encounters and others from both within and outside the healthcare system. Patients with positive experiences in managing their conditions exhibited greater motivation to remain committed to long-term care.
People with multiple chronic conditions often required multiple healthcare providers, which were rarely coordinated with one another. Most of the interviewed patients with multimorbidity reported visiting different doctors and usually received conflicting advice. A patient in our study felt conflicted because private doctors criticized her for using medications from government healthcare providers. Private doctors claimed these medicines might be outdated or of poor quality. This created confusion and uncertainty for her when deciding whom to trust for her healthcare. Furthermore, some patients during discussions shared their belief that any medicines received for free could be of lower quality.
Most patients believed that their medical conditions were both progressive and permanent, with little influence from either themselves or their doctors on their future prognosis. This perspective made it difficult for them to grasp the concept of preventive care and how it could benefit them. Patients adhered to the advice they perceived as beneficial, pragmatic, and able to sustain them. Some patients mentioned that they were more inclined to follow medication prescriptions at the time of diagnosis. However, as they gained more experience and knowledge, they became discerning about the advice they followed and adjusted it to fit their situations. Interestingly, patients had received dietary advice from various sources outside the health center, with the most common sources being private doctors, community members, and social media.
Patients dealing with multiple health conditions in our study emphasized the influence of pill burden on their adherence to therapy. They found it challenging to cope with a substantial number of daily tablets. Moreover, the quantity of tablets also appeared to affect how patients subjectively viewed their health status.
4 Discussion
This study provides valuable insights into the healthcare processes of people living with diabetes and hypertension in public health facilities in Kerala, India. The access to Healthcare conceptual framework (42) enabled us to analyze the intricate process of access within the health systems and the context of the population. Our analysis identified various factors that influence the access to primary health services for the management of diabetes and hypertension, including participants’ limited knowledge of their condition, self-medication practices, physical distance to health facilities, availability of social support, high out-of-pocket expenditure, lack of trust, attitude of healthcare providers, medicine availability, and pill burden. Currently, primary healthcare services often do not sufficiently address the community’s needs. Provision of care to individuals with diabetes and hypertension was often fragmented, leading to multiple visits to advanced healthcare facilities (hospitals), consultations with specialists, and the simultaneous use of various medications. These findings are similar to a study in the Kolar district of Karnataka, which found that the fragmented “treatment-in-silos” hindered patients’ long-term adherence to treatment, especially as they age or face disabilities (19).
In our study, participant’s understanding of diabetes and hypertension varied and was often linked to their symptoms, presence of comorbidities, age, and education. The practice of self-medication emerged as a prevalent health behavior, where people sought advice from relatives or friends and obtained traditional remedies. Formal allopathic healthcare was mostly sought when self-medication did not improve their condition, potentially delaying timely treatment and sometimes even worsening the condition. Diagnosed patients also practiced self-medication when their symptoms were controlled. Previous studies reported using self-medication, including traditional herbal remedies, in Indian healthcare (44, 45). During the interviews, participants also spoke about the restricted variety of drugs at PHCs and frequently expressed doubts about the effectiveness of these drugs for their conditions.
Participants in our study who were predominantly from a low economic status reported limited access to hypertension and diabetes services. Previous evidence suggests clustering of NCDs in disadvantaged groups who have low education status and live in poor communities. These, together with inadequate access to health care, further exacerbate health inequalities in NCD (46). The Makkale Thedi Maruthuvam” scheme is an initiative by the Government of Tamil Nadu to enhance equitable access by screening people aged 30 years and above for diabetes and hypertension, delivering essential medicines, and reviewing treatment compliance at the doorsteps of eligible patients (47). Such initiatives may reduce the frequency of monthly visits for medication refills and improve follow-up care. Practical actions to reduce NCD inequities should encompass prioritizing the service delivery and follow-up for the most susceptible people with diabetes and hypertension based on risk assessment and disparities in access to care.
Access to care was facilitated through support from family and other social networks. This finding is consistent with earlier research, as systematic reviews have established that social support enhances treatment adherence among individuals with NCDs by offering consistent reminders for timely medication consumption (48–50). In high-income countries, well-designed randomized control trials have demonstrated that diabetic populations benefit from peer/CHWs support, improving clinical and behavioral outcomes, including better glycaemic control (51–53). Programs like the UK’s Expert Patient Program provide a cost-effective approach combining peer support and structured education to enhance chronic health support (54, 55). Similarly, the Kerala Diabetes Prevention Program (K-DPP) (56) is a community-based peer-support lifestyle intervention program adapted from evidence-based interventions developed initially in high-income countries and has successfully reduced cardiometabolic risk in high-risk adults over two years. Furthermore, K-DPP encouraged healthier behaviors in peer leaders, like increased physical activity, improved dietary habits, and reduced alcohol consumption (57).
Participants recognized hypertension and diabetes as a lifelong disease, but older individuals were more committed to medication adherence. However, their understanding of long-term prevention steps and self-management was limited due to inadequate communication and support from healthcare workers at all healthcare system levels. Many patients felt overwhelmed by the complexity of managing chronic disease, struggling to initiate and sustain health-promoting behaviors due to uncertainty about where to start. In previous studies most patients seeking care from public healthcare facilities reported minimal or no assistance for self-management (19, 58). This highlights the need to enable and empower patients to participate in managing their care along the continuum spanning from prevention to end of life. Self-care or self-management is one form of intervention that has been of particular interest to manage chronic conditions better and address the socioeconomic challenges LMICs face (59). Many experts have asserted that effective management of chronic diseases occurs when patients are empowered to participate in their care actively. Most chronic care models, including the chronic care model, support self-management skills as an essential component of chronic care (60). Self-management interventions, including SMS-based education, guideline-based teaching sessions, and telephonic counseling, have demonstrated the potential to improve patient health outcomes (61–63). Our findings indicate the need for further research on self-management strategies for CVD, focusing on long-term sustainability, to suit the Kerala context.
Participants’ access to healthcare services was strongly shaped by their trust in the health system and social environment. Trust was influenced by previous personal or network experiences, the reputation of healthcare facilities, and the belief that higher-level facilities offer better service quality and prescribers’ attitudes. While FHC doctors reported to address patients hastily, people expected extensive conversations and meticulous examinations. This finding aligns with previous research, emphasizing the significance of positive patient-health professional relationships on patients’ adherence to treatment (64), particularly when patients perceive healthcare providers as compassionate and caring.
Among our study participants, medication non-adherence stemmed from multifaceted factors, encompassing psychosocial elements (perceived lack of social support), structural challenges (clinic distance and medication expenses), therapy-related issues (multiple visits, polypharmacy, pill burden), and barriers within the healthcare system (e.g., insufficient counseling, erratic medicine supply from public health facilities, and patient-provider relationship). Additionally, patients trust in healthcare systems and beliefs regarding medications and their perceptions of their illness contribute to non-adherence. Evidence suggests that the use of single-pill combination (SPC) is safe and has the potential to improve patient adherence and blood pressure control, particularly in LMICs (65). In 2019, the World Health Organization (WHO) incorporated SPC into the Essential medicines list (66). We encourage the uptake and use of SPCs in primary care settings to improve blood pressure control and simplify treatment regimens.
Previous studies have proposed that an integrated approach to NCD care can streamline and save patient time and costs. For example, Peck et al. (67) have shown that integrating NCD and human immunodeficiency virus (HIV) treatment services reduces patient travel burden, allows personalized treatment approaches, and addresses the lack of support for patient follow-up and self-management in the current healthcare system. Frenk discusses integrating interventions and adopting a diagonal approach to health system improvements across multiple conditions while emphasizing the need for tangible improvements in health outcomes (68).
Our further observation pertains to the linear nature of Levesque et al.’s framework (42). While this framework has recognized factors influencing the healthcare-seeking pathways of individuals with NCDs, it does not fully explain why patients progress through these multidirectional pathways. Consistent with Nguyen et al.’s findings (69), we observed that patients frequently navigate the care pathway in a non-linear manner due to the challenges of diagnosis and the long-term management of chronic conditions. This process involves loops and cycles, with patients moving forward and backward in pursuit of healthcare across various facilities. Consequently, an alternative non-linear representation, incorporating broader healthcare system factors, would better depict the interconnected elements influencing access to healthcare services.
Consistent with prior research, our study reveals that individual “abilities” are primarily influenced by the “system” and its deficiencies, rather than solely being the responsibility of individuals. Thus, the central aspect of any intervention may involve a substantial investment in enhancing the accessibility of the system to empower an individual’s “ability” to interact with it effectively.
4.1 Strengths and limitations of the study
The study has several limitations. Firstly, in its emphasis on capturing patients’ viewpoints, the study did not incorporate the healthcare workers (supply side), which could have provided valuable insights. Secondly, although efforts were made to include equal representation of male and female participants, most respondents were women, reflecting the predominant population seeking healthcare in the state. Thirdly, the quality of care provided to the patients and the resulting health outcomes were beyond the scope of the study.
A key strength of our study is that we have considered the most prevalent NCDs, like diabetes and hypertension, to explore how patients seek care for chronic conditions in Malappuram. Although variations may exist among different illnesses, experiences are likely similar due to the current state of the healthcare system in Kerala and India. Primary care services are weak, and health systems lack capacity to address chronic illnesses. Secondly, our prolonged engagement within the study sites, as we regularly visited the facilities and stayed in the local community, enabled us to obtain data with rich insights into how people experience care. Thirdly, using Levesque’s access framework in the analysis enhances the potential for replication of this study in other contextually similar settings.
4.2 Implication for practice and research
Preventing the rising burden of NCDs is challenging as it necessitates addressing the underlying social determinants of health (70). Moreover, the organization of care for individuals with NCDs is intricate and resource-intensive, and multiple concurrent chronic conditions, known as multimorbidity, further complicate matters (71–74). It is important to recognize that the roots of NCDs are deeply entrenched in society’s social, political, and economic structures.
Unfortunately, it appears that those shaping current policies and resource allocation are either unaware of or choose to overlook the realities on the frontlines of healthcare. Physicians often find themselves bridging the gap between treating individual illnesses and meeting the needs of patients grappling with multimorbid NCDs. Reachable and reliable care and support must be ensured at the initial point of contact. Healthcare professionals must deliver attentive support tailored to individuals’ perceived needs, incorporate self-management support to influence patients’ behavior, and maximize the use and effectiveness of community service. Furthermore, we need a more comprehensive approach to healthcare policy that recognizes the interconnectedness of NCDs and the social determinants that affect their occurrence and management. Such a shift in policy and resource allocation is essential to effectively address our society’s growing burden of NCDs.
5 Conclusion
The patient journey in managing diabetes and hypertension is multifaceted, involving multiple entry and exit points within the healthcare system. This study underscores the complexity of healthcare access and how access was affected by various factors. Unfortunately, there is a lack of a patient-centred care process that delves into the self-management efforts required by patients and explores how healthcare providers can offer adequate support. Consequently, it is crucial to rethink the design and organization of care for individuals with chronic diseases. This involves reframing the patient journey, acknowledging it as one characterized by multiple touchpoints where patients may initiate their healthcare pathway at different stages but consistently require good quality, affordable care and support at various junctures.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Ethics Committee of Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCT/IEC/ 1908). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
RR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. PS: Conceptualization, Methodology, Supervision, Writing – review & editing. SS: Conceptualization, Methodology, Supervision, Writing – review & editing. KT: Conceptualization, Methodology, Supervision, Writing – review & editing. PJ: Conceptualization, Formal analysis, Funding acquisition, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study is partially funded through the Health Policy Analysis Fellowship program, supported by the Alliance for Health Policy and Systems Research, Switzerland, and managed through the University of Cape Town, South Africa. RR was awarded this fellowship.
Acknowledgments
The authors express their appreciation to the Alliance for Health Policy and Systems Research, Switzerland, for supporting this study. Gratitude is extended to individuals with diabetes and hypertension who generously shared their valuable insights during the study. Special acknowledgment is given to Linju Maria Joseph, Tijo George, Krishnendu C, and Arun Jose for their significant contributions to interpreting the study’s results.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1375227/full#supplementary-material
References
1. Lancet, T. GBD 2017: a fragile world. Lancet. (2018) 392:1683. doi: 10.1016/S0140-6736(18)32858-7
2. Niessen, LW, Mohan, D, Akuoku, JK, Mirelman, AJ, Ahmed, S, Koehlmoos, TP, et al. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the sustainable development agenda. Lancet Lond Engl. (2018) 391:2036–46. doi: 10.1016/S0140-6736(18)30482-3
3. WHO. (2023) Non communicable diseases. Available at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
4. Amarchand, R, Kulothungan, V, Krishnan, A, and Mathur, P. Hypertension treatment cascade in India: results from National Noncommunicable Disease Monitoring Survey. J Hum Hypertens. (2023) 37:394–404. doi: 10.1038/s41371-022-00692-y
5. Prenissl, J, Jaacks, LM, Mohan, V, Manne-Goehler, J, Davies, JI, Awasthi, A, et al. Variation in health system performance for managing diabetes among states in India: a cross-sectional study of individuals aged 15 to 49 years. BMC Med. (2019) 17:92. doi: 10.1186/s12916-019-1325-6
6. Sarma, PS, Sadanandan, R, Thulaseedharan, JV, Soman, B, Srinivasan, K, Varma, RP, et al. Prevalence of risk factors of non-communicable diseases in Kerala, India: results of a cross-sectional study. BMJ Open. (2019) 9:e027880. doi: 10.1136/bmjopen-2018-027880
7. WHO. (2023) WHO package of essential noncommunicable (PEN) disease interventions for primary health care. Available at: https://www.who.int/publications-detail-redirect/9789240009226
8. Demaio, AR, Nielsen, KK, Tersbøl, BP, Kallestrup, P, and Meyrowitsch, DW. Primary health care: a strategic framework for the prevention and control of chronic non-communicable disease. Glob Health Action. (2014) 7:24504. doi: 10.3402/gha.v7.24504
9. Haque, M, Islam, T, Rahman, NAA, McKimm, J, Abdullah, A, and Dhingra, S. Strengthening primary health-care services to help prevent and control long-term (chronic) non-communicable diseases in low- and middle-income countries. Risk Manag Healthc Policy. (2020) 13:409–26. doi: 10.2147/RMHP.S239074
10. Hansen, J, Groenewegen, PP, Boerma, WGW, and Kringos, DS. Living in A country with A strong primary care system is beneficial to people with chronic conditions. Health Aff (Millwood). (2015) 34:1531–7. doi: 10.1377/hlthaff.2015.0582
11. Bitton, A, Fifield, J, Ratcliffe, H, Karlage, A, Wang, H, Veillard, JH, et al. Primary healthcare system performance in low-income and middle-income countries: a scoping review of the evidence from 2010 to 2017. BMJ Glob Health. (2019) 4:e001551. doi: 10.1136/bmjgh-2019-001551
12. Varghese, C, Nongkynrih, B, Onakpoya, I, McCall, M, Barkley, S, and Collins, TE. Better health and wellbeing for billion more people: integrating non-communicable diseases in primary care. BMJ. (2019) 364:l327. doi: 10.1136/bmj.l327
13. Vlassoff, C, Tanner, M, Weiss, M, and Rao, S. Putting people first: A primary health care success in rural India. Indian J Community Med. (2010) 35:326–30. doi: 10.4103/0970-0218.66896
14. Samb, B, Desai, N, Nishtar, S, Mendis, S, Bekedam, H, Wright, A, et al. Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Lancet. (2010) 376:1785–97. doi: 10.1016/S0140-6736(10)61353-0
15. Gabert, R, Ng, M, Sogarwal, R, Bryant, M, Deepu, RV, McNellan, CR, et al. Identifying gaps in the continuum of care for hypertension and diabetes in two Indian communities. BMC Health Serv Res. (2017) 17:846. doi: 10.1186/s12913-017-2796-9
16. Ramani, S, and Sivakami, M. Community perspectives on primary health centers in rural Maharashtra: what can we learn for policy? J Fam Med Prim Care. (2019) 8:2837–44. doi: 10.4103/jfmpc.jfmpc_650_19
17. Sodani, P, and Sharma, K. Strengthening primary level health service delivery: lessons from a state in India. J Fam Med Prim Care. (2012) 1:127–31. doi: 10.4103/2249-4863.104983
18. Bhaumik, S. Health and beyond. Strategies for a better India: concept paper on primary health Care in India. J Fam Med Prim Care. (2014) 3:94–7. doi: 10.4103/2249-4863.137608
19. Lall, D, Engel, N, Devadasan, N, Horstman, K, and Criel, B. Challenges in primary care for diabetes and hypertension: an observational study of the Kolar district in rural India. BMC Health Serv Res. (2019) 19:44. doi: 10.1186/s12913-019-3876-9
20. Patel, V, Mazumdar-Shaw, K, Kang, G, Das, P, and Khanna, T. Reimagining India’s health system: a Lancet citizens’ commission. Lancet Lond Engl. (2021) 397:1427–30. doi: 10.1016/S0140-6736(20)32174-7
21. Angell, BJ, Prinja, S, Gupt, A, Jha, V, and Jan, S. The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana and the path to universal health coverage in India: overcoming the challenges of stewardship and governance. PLoS Med. (2019) 16:e1002759. doi: 10.1371/journal.pmed.1002759
22. Ministry of Health and Family Welfare, Governmnet of India. (2023) Operational guidelines on wellness interventions for Ayushman Bharat health and wellness Centres | National Health Systems Resource Centre. Available at: https://nhsrcindia.org/operational-guidelines-wellness-interventions-ayushman-bharat-health-and-wellness-centres
23. Government Of India. (2022) Ayushman Bharat – national health protection mission. Available at: https://www.india.gov.in/spotlight/ayushman-bharat-national-health-protection-mission. (Accessed on September, 2022).
24. Government Of India. (2022) Official website Ayushman Bharat. Available at: https://ab-hwc.nhp.gov.in/. (Accessed on January, 2022).
25. Arogyakeralam. (2022) National Health Mission Kerala-Aardram. Available at: https://arogyakeralam.gov.in/2020/04/01/aardram/. (Accessed on October, 2022).
26. Sadanandan, R, and Sivaprasad, S. Adding screening for “end organ damage” to the noncommunicable disease package in primary care. Indian J Ophthalmol. (2021) 69:3064–7. doi: 10.4103/ijo.IJO_1496_21
27. Sivaprasad, S, Netuveli, G, Wittenberg, R, Khobragade, R, Sadanandan, R, Gopal, B, et al. Complex interventions to implement a diabetic retinopathy care pathway in the public health system in Kerala: the Nayanamritham study protocol. BMJ Open. (2021) 11:e040577. doi: 10.1136/bmjopen-2020-040577
28. Oben, P. Understanding the patient experience: A conceptual framework. J Patient Exp. (2020) 7:906–10. doi: 10.1177/2374373520951672
29. Stebbins, RA. Exploratory research in the social sciences [internet]. Thousand Oaks, CA: SAGE Publications, Inc (2001).
30. Sandelowski, M. What’s in a name? Qualitative description revisited. Res Nurs Health. (2010) 33:77–84. doi: 10.1002/nur.20362
31. Population Census. (2022) Malappuram Municipality City population census 2011-2023 | Kerala. Available at: https://www.census2011.co.in/data/town/803269-malappuram-kerala.html. (Accessed on September, 2022).
32. Philip, RR, Philip, S, Tripathy, JP, Manima, A, and Venables, E. Twenty years of home-based palliative care in Malappuram, Kerala, India: a descriptive study of patients and their care-givers. BMC Palliat Care. (2018) 17:26. doi: 10.1186/s12904-018-0278-4
33. Ismail, S, Stanley, A, and Jeemon, P. Prevalence of multimorbidity and associated treatment burden in primary care settings in Kerala: a cross-sectional study in Malappuram District, Kerala, India. Wellcome Open Res. (2022) 7:67. doi: 10.12688/wellcomeopenres.17674.2
34. Joseph, L, Greenfield, S, Manaseki-Holland, S, Lekha, TR, Sujakumari, S, Panniyammakal, J, et al. Patients’, carers’ and healthcare providers’ views of patient-held health records in Kerala, India: A qualitative exploratory study. Health Expect. (2023) 26:1081–95. doi: 10.1111/hex.13721
35. Given, LM. The SAGE encyclopedia of qualitative research methods. Thousand Oaks, CA: SAGE Publications (2008). 1073 p.
36. Britten, N. Qualitative interviews in medical research. BMJ. (1995) 311:251–3. doi: 10.1136/bmj.311.6999.251
37. Caillaud, S, and Flick, U. Focus groups in triangulation contexts In: RS Barbour and DL Morgan, editors. A new era in focus group research: Challenges, innovation and practice. London: Palgrave Macmillan UK (2017). 155–77.
38. Hennink, MM, Kaiser, BN, and Marconi, VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. (2017) 27:591–608. doi: 10.1177/1049732316665344
39. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
40. Kiger, ME, and Varpio, L. Thematic analysis of qualitative data: AMEE guide no. 131. Med Teach. (2020) 42:846–54. doi: 10.1080/0142159X.2020.1755030
41. Pope, C, Ziebland, S, and Mays, N. Analysing qualitative data. BMJ. (2000) 320:114–6. doi: 10.1136/bmj.320.7227.114
42. Levesque, JF, Harris, MF, and Russell, G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. (2013) 12:18. doi: 10.1186/1475-9276-12-18
43. Devi, R, Kanitkar, K, Narendhar, R, Sehmi, K, and Subramaniam, K. A narrative review of the patient journey through the Lens of non-communicable diseases in low- and middle-income countries. Adv Ther. (2020) 37:4808–30. doi: 10.1007/s12325-020-01519-3
44. Vishnu, N, Mini, GK, and Thankappan, KR. Complementary and alternative medicine use by diabetes patients in Kerala, India. Glob Health Epidemiol Genomics. (2017) 2:e6. doi: 10.1017/gheg.2017.6
45. Greenhalgh, T. Drug prescription and self-medication in India: An exploratory survey. Soc Sci Med. (1987) 25:307–18. doi: 10.1016/0277-9536(87)90233-4
46. Cesare, MD, Khang, YH, Asaria, P, Blakely, T, Cowan, MJ, Farzadfar, F, et al. Inequalities in non-communicable diseases and effective responses. Lancet. (2013) 381:585–97. doi: 10.1016/S0140-6736(12)61851-0
47. Thiagesan, R, Soundari, H, Kalpana, B, and Gopichandran, V. “Makkalai Thedi Maruthuvam” scheme in Tamil Nadu: an intersectionality-based analysis of access to NCD care. Indian. J Med Ethics. (2023) VIII:203–9. doi: 10.20529/IJME.2023.015
48. Miller, TA, and DiMatteo, MR. Importance of family/social support and impact on adherence to diabetic therapy. Diabetes Metab Syndr Obes. (2013) 6:421–6. doi: 10.2147/DMSO.S36368
49. Walsh, JME, McDonald, KM, Shojania, KG, Sundaram, V, Nayak, S, Lewis, R, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. (2006) 44:646–57. doi: 10.1097/01.mlr.0000220260.30768.32
50. Glynn, LG, Murphy, AW, Smith, SM, Schroeder, K, and Fahey, T. Self-monitoring and other non-pharmacological interventions to improve the management of hypertension in primary care: a systematic review. Br J Gen Pract J R Coll Gen Pract. (2010) 60:e476–88. doi: 10.3399/bjgp10X544113
51. Knowler, WC, Barrett-Connor, E, Fowler, SE, Hamman, RF, Lachin, JM, Walker, EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. (2002) 346:393–403. doi: 10.1056/NEJMoa012512
52. Pan, XR, Li, GW, Hu, YH, Wang, JX, Yang, WY, An, ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and diabetes study. Diabetes Care. (1997) 20:537–44. doi: 10.2337/diacare.20.4.537
53. Tuomilehto, J, Lindström, J, Eriksson, JG, Valle, TT, Hämäläinen, H, Ilanne-Parikka, P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. (2001) 344:1343–50. doi: 10.1056/NEJM200105033441801
54. Donaldson, L. Expert patients usher in a new era of opportunity for the NHS: the expert patient programme will improve the length and quality of lives. BMJ. (2003) 326:1279–80. doi: 10.1136/bmj.326.7402.1279
55. Tattersall, R. The expert patient: a new approach to chronic disease management for the twenty-first century. Clin Med. (2002) 2:227–9. doi: 10.7861/clinmedicine.2-3-227
56. Thankappan, KR, Sathish, T, Tapp, RJ, Shaw, JE, Lotfaliany, M, Wolfe, R, et al. A peer-support lifestyle intervention for preventing type 2 diabetes in India: A cluster-randomized controlled trial of the Kerala diabetes prevention program. PLoS Med. (2018) 15:e1002575. doi: 10.1371/journal.pmed.1002575
57. Haregu, T, Aziz, Z, Cao, Y, Sathish, T, Thankappan, KR, Panniyammakal, J, et al. A peer support program results in greater health benefits for peer leaders than other participants: evidence from the Kerala diabetes prevention program. BMC Public Health. (2023) 23:1175. doi: 10.1186/s12889-023-16049-0
58. Humphries, C, Jaganathan, S, Panniyammakal, J, Singh, S, Goenka, S, Dorairaj, P, et al. Investigating clinical handover and healthcare communication for outpatients with chronic disease in India: A mixed-methods study. PLoS One. (2018) 13:e0207511. doi: 10.1371/journal.pone.0207511
59. Hearn, J, Ssinabulya, I, Schwartz, JI, Akiteng, AR, Ross, HJ, and Cafazzo, JA. Self-management of non-communicable diseases in low- and middle-income countries: A scoping review. PLoS One. (2019) 14:e0219141. doi: 10.1371/journal.pone.0219141
60. Bodenheimer, T, Wagner, EH, and Grumbach, K. Improving primary Care for Patients with Chronic IllnessThe chronic care model, part 2. JAMA. (2002) 288:1909–14. doi: 10.1001/jama.288.15.1909
61. Sherifali, D, Berard, LD, Gucciardi, E, MacDonald, B, and MacNeill, G. Self-management education and support. Can J Diabetes. (2018) 42:S36–41. doi: 10.1016/j.jcjd.2017.10.006
62. McManus, RJ, Mant, J, Bray, EP, Holder, R, Jones, MI, Greenfield, S, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. (2010) 376:163–72. doi: 10.1016/S0140-6736(10)60964-6
63. McLean, G, Band, R, Saunderson, K, Hanlon, P, Murray, E, Little, P, et al. Digital interventions to promote self-management in adults with hypertension systematic review and meta-analysis. J Hypertens. (2016) 34:600–12. doi: 10.1097/HJH.0000000000000859
64. Mechanic, D. Changing medical organization and the Erosion of trust. Milbank Q. (1996) 74:171–89. doi: 10.2307/3350245
65. Bruyn, E, Nguyen, L, Schutte, AE, Murphy, A, Perel, P, and Webster, R. Implementing single-pill combination therapy for hypertension: A scoping review of key health system requirements in 30 low- and middle-income countries. Glob Heart. (2022) 17:6. doi: 10.5334/gh.1087
66. WHO. (2023) WHO model lists of essential medicines. Available at: https://www.who.int/groups/expert-committee-on-selection-and-use-of-essential-medicines/essential-medicines-lists
67. Peck, R, Mghamba, J, Vanobberghen, F, Kavishe, B, Rugarabamu, V, Smeeth, L, et al. Preparedness of Tanzanian health facilities for outpatient primary care of hypertension and diabetes: a cross-sectional survey. Lancet Glob Health. (2014) 2:e285–92. doi: 10.1016/S2214-109X(14)70033-6
68. Frenk, J. Reinventing primary health care: the need for systems integration. Lancet. (2009) 374:170–3. doi: 10.1016/S0140-6736(09)60693-0
69. Nguyen, TA, Pham, YN, Doan, NP, Nguyen, TH, Do, TT, Van Vu, G, et al. Factors affecting healthcare pathways for chronic lung disease management in Vietnam: a qualitative study on patients’ perspectives. BMC Public Health. (2021) 21:1145. doi: 10.1186/s12889-021-11219-4
70. Sreekumar, S, and Ravindran, TKS. A critique of the policy discourse on primary health care under the Aardram mission of Kerala. Health Policy Plan. (2023) 38:949–59. doi: 10.1093/heapol/czad041
71. Pefoyo, AJK, Bronskill, SE, Gruneir, A, Calzavara, A, Thavorn, K, Petrosyan, Y, et al. The increasing burden and complexity of multimorbidity. BMC Public Health. (2015) 15:415. doi: 10.1186/s12889-015-1733-2
72. Mini, GK, and Thankappan, KR. Pattern, correlates and implications of non-communicable disease multimorbidity among older adults in selected Indian states: a cross-sectional study. BMJ Open. (2017) 7:e013529. doi: 10.1136/bmjopen-2016-013529
73. Oni, T, McGrath, N, BeLue, R, Roderick, P, Colagiuri, S, May, CR, et al. Chronic diseases and multi-morbidity--a conceptual modification to the WHO ICCC model for countries in health transition. BMC Public Health. (2014) 14:575. doi: 10.1186/1471-2458-14-575
Keywords: access, primary health, health needs, community, NCD, qualitative research, health care pathway
Citation: Ravindranath R, Sarma PS, Sivasankaran S, Thankappan KR and Jeemon P (2024) Voices of care: unveiling patient journeys in primary care for hypertension and diabetes management in Kerala, India. Front. Public Health. 12:1375227. doi: 10.3389/fpubh.2024.1375227
Edited by:
Yun Gao, Sichuan University, ChinaReviewed by:
Joao Soares Martins, National University of East Timor, Timor-LesteDaniel Edem Kpewou, University for Development Studies, Ghana
Copyright © 2024 Ravindranath, Sarma, Sivasankaran, Thankappan and Jeemon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Panniyammakal Jeemon, amVlbW9uQHNjdGltc3QuYWMuaW4=
 Ranjana Ravindranath
Ranjana Ravindranath P. Sankara Sarma1
P. Sankara Sarma1 Sivasubramonian Sivasankaran
Sivasubramonian Sivasankaran Kavumpurathu Raman Thankappan
Kavumpurathu Raman Thankappan Panniyammakal Jeemon
Panniyammakal Jeemon