
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Public Health, 24 September 2024
Sec. Public Health Policy
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1370500
 Marwa Rashad Salem1*
Marwa Rashad Salem1* Nelly Hegazy2
Nelly Hegazy2 Sherif Eldeeb3
Sherif Eldeeb3 Jerome A. Shaguy4
Jerome A. Shaguy4 Ramesh Mohammad Nassery4
Ramesh Mohammad Nassery4 Abdullah Khawari4
Abdullah Khawari4 Jamshed Tanoli4
Jamshed Tanoli4 Alaa Abouzeid1,4
Alaa Abouzeid1,4Background: In Afghanistan, providing universal health coverage (UHC) in accordance with the principles of the UHC declaration is challenging on two fronts: the geographic topography of the country and the prevailing gender dynamics within the local culture.
Methods: We conducted a desk review of underserved areas in the context of health services by gathering and analyzing existing literature, reports, and data using a combination of keywords and phrases such as: “underserved areas,” “healthcare disparities,” “access to healthcare,” and “health services.” The primary data were derived from an analysis of underserved populations conducted by the World Health Organization (WHO) Afghanistan's Emergency Program, supplemented by information from in-country partners. In addition to other reports, this review focused on analyzing the geographical availability of primary healthcare (PHC) services by employing the guidelines set forth in the SPHERE framework. It also took into account the social dynamics within the Afghan population that may create barriers to equity in terms of demand and access to PHC services.
Results: Although there are a significant number of primary healthcare facilities in operation (4,242), they are unevenly distributed across different regions of Afghanistan, resulting in almost 25% of the population being underserved. The underserved population is nearly equally distributed between genders, with the majority residing in rural communities. Women of childbearing age represent 28% of the underserved population. Children under the age of five represent 16–18% of the underserved population in all regions, except in the western region, where they represent between 12 and 13%. Individuals over 60 years of age represent 1–3% of the underserved population across all regions. More than 50% of the population in the Central Highlands of Afghanistan is underserved, followed by the western and southern regions. Ghor province in the western region has the highest proportion of underserved populations, followed by Zabul province in the southern region.
Conclusion: Afghanistan is currently experiencing a protracted humanitarian crisis, with millions of people living in poverty and lacking access to healthcare. This situation exposes them to serious risks such as disease epidemics, starvation, and maternal and child mortality. It is crucial to implement alternative strategies to reach the most affected populations and to increase funding for the delivery of healthcare services in Afghanistan.
In Afghanistan, health services are provided mainly through primary healthcare (PHC) facilities (4,242), with different categories distributed in 401 districts of 34 provinces, through two key programs: the Basic Package of Health Services (BPHS) and the Essential Package of Hospital Services (EPHS) (1). In early 2021, the Integrated Package of Essential Health Services (IPEHS) was endorsed by the previous republican government to expand the coverage and scope of health services and to help move the country toward universal health coverage (UHC) (2). However, the latter was not implemented due to a lack of commitment, a lack of resources, and the country's health strategy (3).
The World Health Organization (WHO) recently completed a geospatial analysis of underserved areas in Afghanistan in September 2022; the country's health system has made significant strides in recent years, which has also improved the population's health (4). Despite these improvements, Afghanistan's health indicators are near the bottom of international indices (5) and are lower than any other country in the region. With one of the highest rates of acute malnutrition and stunting in children under the age of five worldwide, health is still of utmost importance in this nation (6). According to the United Nations Children's Fund (UNICEF), 1 million children are expected to suffer from acute severe malnutrition, while 7.4 million children in Afghanistan need humanitarian aid to survive. The mortality rate for children under the age of five is 55.7 deaths per 1,000 live births (7). Afghanistan's mountainous landscape, vulnerability to natural disasters, history of numerous conflicts over the years, and its designation as the most impoverished nation in the Asia–Pacific region in terms of the average per capita income have collectively made achieving universal access to primary healthcare extremely challenging (8, 9).
Despite the distribution of 4,242 primary healthcare facilities throughout the country, 9.5 million people still lack access to primary healthcare (underserved) (10). This finding is alarming as equitable access to primary healthcare (PHC) is a key policy concern and also a fundamental human right. The accessibility and equitable distribution of PHC are fundamental to achieving the Sustainable Development Goals (SDGs) and universal health coverage (10). The highest possible level of health and wellbeing for people can be achieved through PHC. Defined by the World Health Organization and UNICEF, PHC is a comprehensive approach that focuses on people's needs, promoting health, preventing diseases, and providing access to treatment, rehabilitation, and palliative care (11).
According to the World Health Organization, universal health coverage “means that all people have access to the full range of quality health services they need, when and where they need them, without financial hardship.” It covers the full continuum of essential health services, from health promotion to prevention, treatment, rehabilitation, and palliative care across the life course (12).
In Afghanistan, providing universal health coverage in accordance with the principles of UHC declaration is challenging on two fronts: the geographic topography of the country and the prevailing gender dynamics within the local culture. Nonetheless, a quantum of resources and a high level of effort have been expended in implementing universal health coverage. This study aimed to review the level of primary healthcare penetration into the most vulnerable and hard-to-reach populations in Afghanistan. This review article focused on analyzing the geographical availability of PHC services by employing the guidelines set forth in the SPHERE framework. It also took into account the social dynamics within the Afghan population that may create barriers to equity in terms of demand and access to PHC services.
We conducted a desk review on underserved areas in the context of health services by gathering and analyzing existing literature, reports, and data to provide a comprehensive overview of the issue. The collected data were analyzed using a descriptive approach. This approach aimed to provide a detailed and itemized description of the social conditions of vulnerable populations in Afghanistan and to identify how these conditions intersect with the ability to either demand or access the health services provided. The gathered data—all of it secondary—were screened by the research team using a systematic approach. This approach involved data display and line-by-line and keyword associations to identify themes. This approach was considered the most rigorous, providing the level of granularity and contextual grounding necessary for examining socioeconomic issues.
There were two stages in the review process:
1) Initial literature search: The systematic search process helped formulate the inclusion criteria, which included the following: the date of publication, the location of the study, and peer-reviewed papers and data. The following search keywords and phrases related to the current research question were used: “underserved areas,” “healthcare disparities,” “access to healthcare,” “health services,” and other relevant terms. The primary data were derived from an analysis of underserved populations conducted by the WHO Afghanistan's Emergency Program, supplemented by information from in-country partners. In addition to a total of 20 publications, the following were included: the underserved population analysis, which is a geographic illustration published in 2022, the Humanitarian Development Report (23), the WHO Emergency Operational Plan (24), addressing the health needs of Afghanistan crisis-affected populations, and key Afghanistan demographic indicators (based on UNICEF's 2023 data). These data were collated, carefully reviewed, and subsequently analyzed for quality in the next stage.
2) Paper review and analysis: The research team leader divided the documents among seven team members. Each member reviewed the documents that best aligned with their core training and backgrounds. Then, the team members organized and presented the data using simple Excel spreadsheets. This display process enabled investigators to identify themes and patterns, which corresponded to the study's goal of understanding the factors that affect vulnerable populations and the level of choice and agency these populations have in accessing primary healthcare. The analytical approach in this study was thematic, involving scheming and reading through data sources to reveal common areas that showed a convergence of issues. This process, in turn, validated them and, by extension, demonstrated rigor and robustness.
By reviewing, cross-validating, and analyzing the data and reports, this review determined the underlying dynamics in terms of social determinants and how they affect universal health coverage. It focuses on population access and the ways to improve healthcare and outcomes. The collected data and information were analyzed in iterative and interconnected steps (as shown in Figure 1).
The total population of Afghanistan is ~38.2 million (10). However, 9.4 million people are deprived of primary healthcare services (Figure 2). The underserved population is nearly equally distributed between genders, with the majority of them residing in rural communities (Table 1).
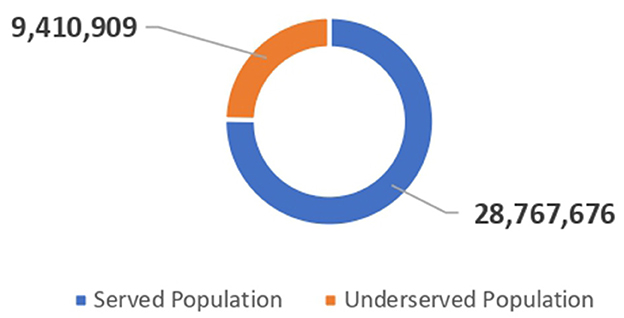
Figure 2. The pie chart represents the total served population vs. the total underserved population in Afghanistan.
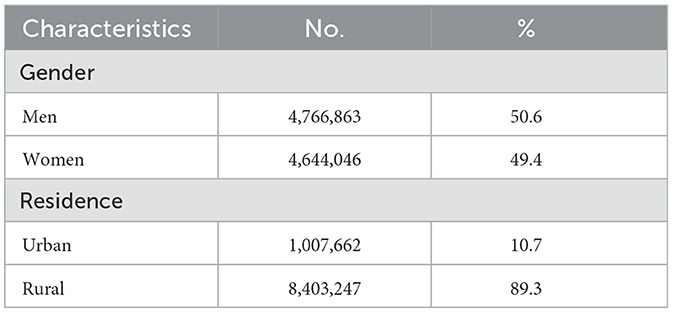
Table 1. Distribution of the studied underserved population by gender and residence (n = 9,410,909).
As shown in Table 2, the available health services are predominantly provided through primary healthcare facilities (4,242), among which the sub-health center and the basic health center are the most prevalent. The Health Emergency Response (HER) Project, which is funded by the World Bank, supports more than half (55%) of the health facilities in Afghanistan.
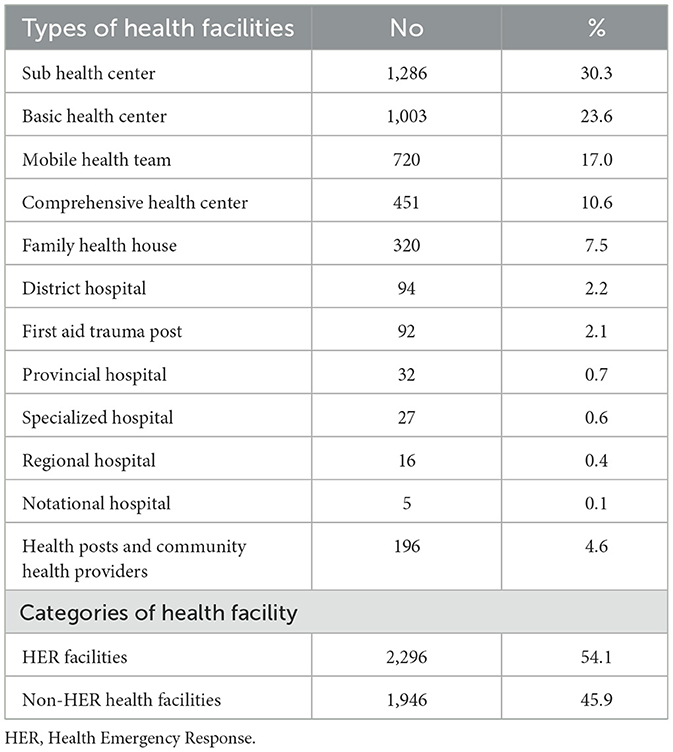
Table 2. Percentage distribution of health facilities by type and category in Afghanistan (n = 4,242).
Tables 3–5 show the percentage distribution of the underserved populations in 34 provinces of Afghanistan. Although there are a significant number of health services in operation (4,242), they are unevenly distributed across different regions of Afghanistan, resulting in 25% of the population being underserved. Women of childbearing age (15–49 years) represent 28% of the underserved population in the whole of Afghanistan. Children under the age of five represent 16–18% of the underserved population in all regions, except in the western region, where they represent between 12 and 13%. Individuals over 60 years of age represent 1–3% of the underserved population across all regions.
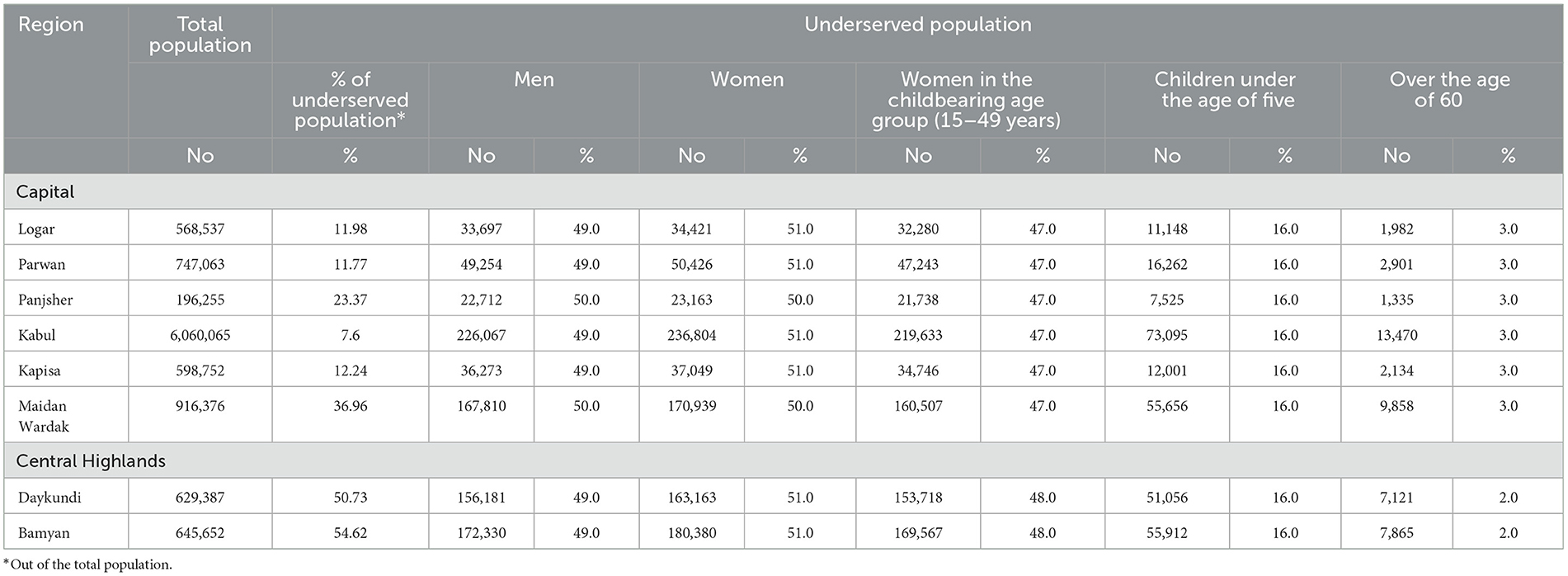
Table 3. Percentage distribution of the underserved population in the capital and Central Highlands of Afghanistan by gender and vulnerable age groups (n = 10,362,087).
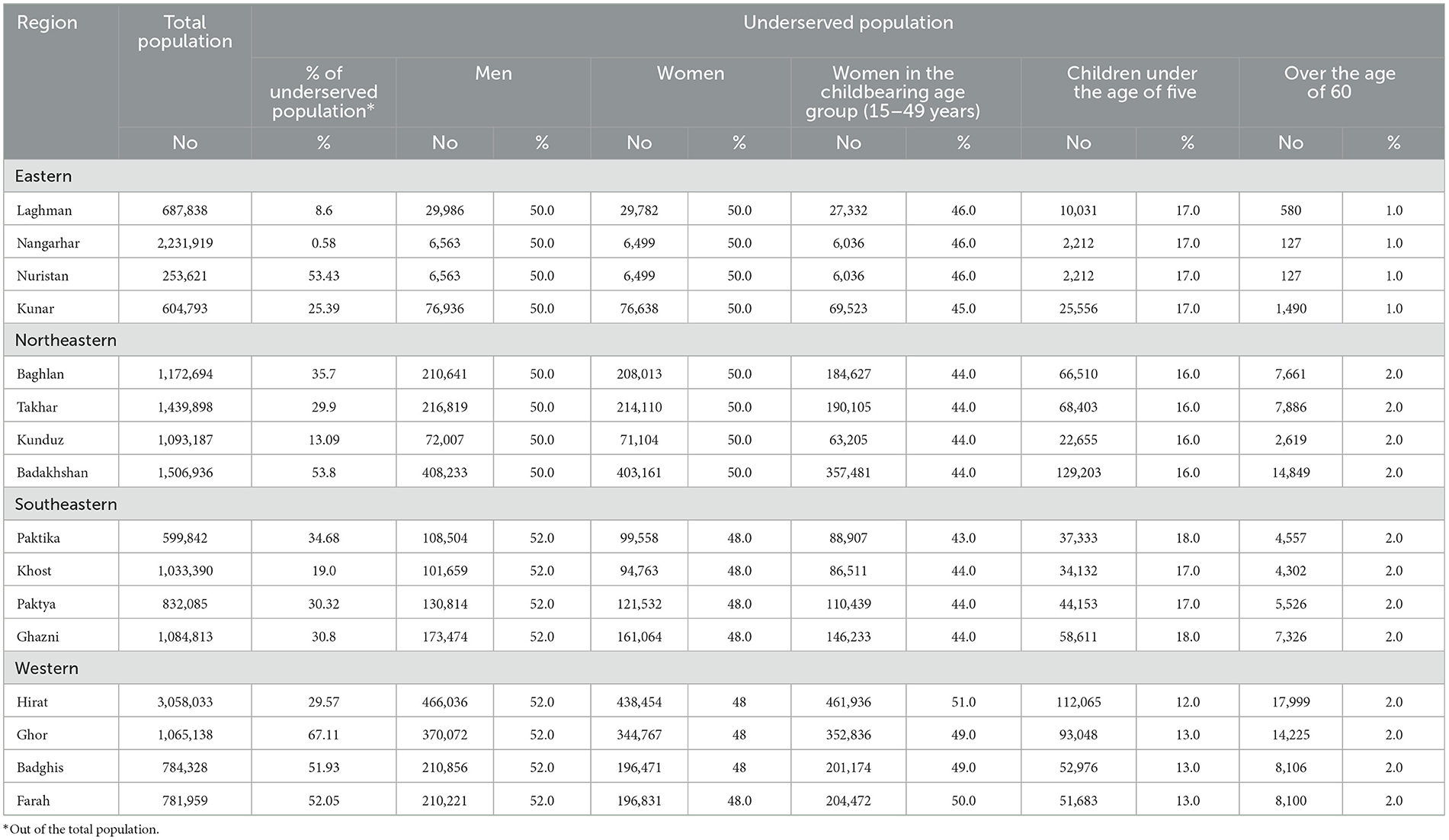
Table 4. Percentage distribution of the underserved population in eastern, northeastern, southeastern, and western regions of Afghanistan by gender and vulnerable age groups (n = 18,230,474).
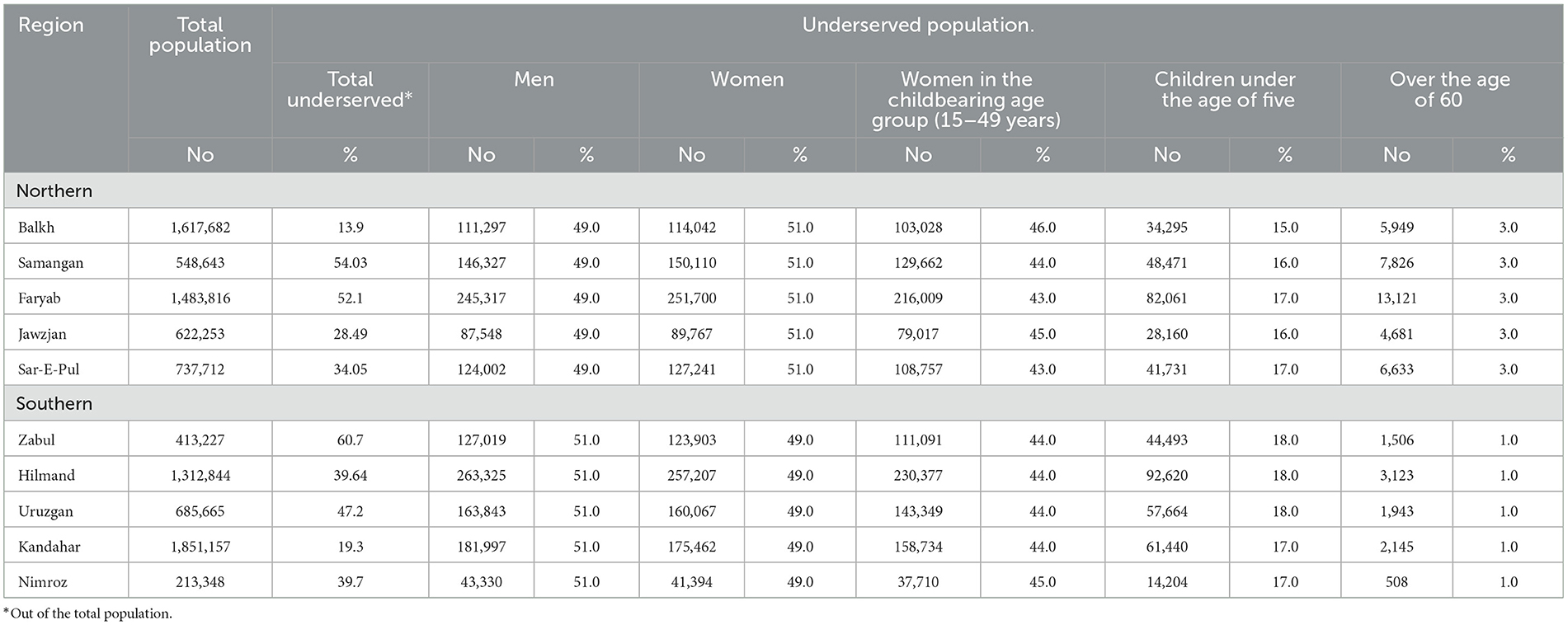
Table 5. Percentage distribution of the underserved population in northern and southern regions in Afghanistan by gender and vulnerable age groups (n = 9,486,347).
Figure 3 shows that more than 50% of the population of the Central Highlands of Afghanistan is underserved, followed by the western region at 42.1% and the southern region at 35.5%. This finding is in contrast with the capital region, which demonstrates the lowest percentage in White areas (1.7%), and the Eastern region (9.5%).
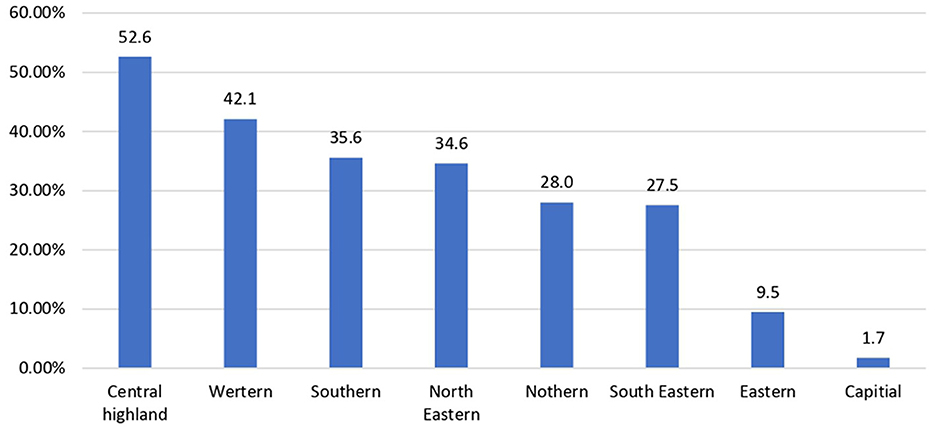
Figure 3. The bar chart represents the percentage distribution of the underserved areas by region in Afghanistan.
Ghor province in the western region has the highest percentage of underserved populations (67.1%), followed by Zabul province in the southern region (60.7%) and Bamyan province in the Central Highlands (54.6%). Almost the entire population in Nangarhar province in the eastern region is provided with primary healthcare services, while only 7.6% of the population of Kabul province is underserved (Figure 4).
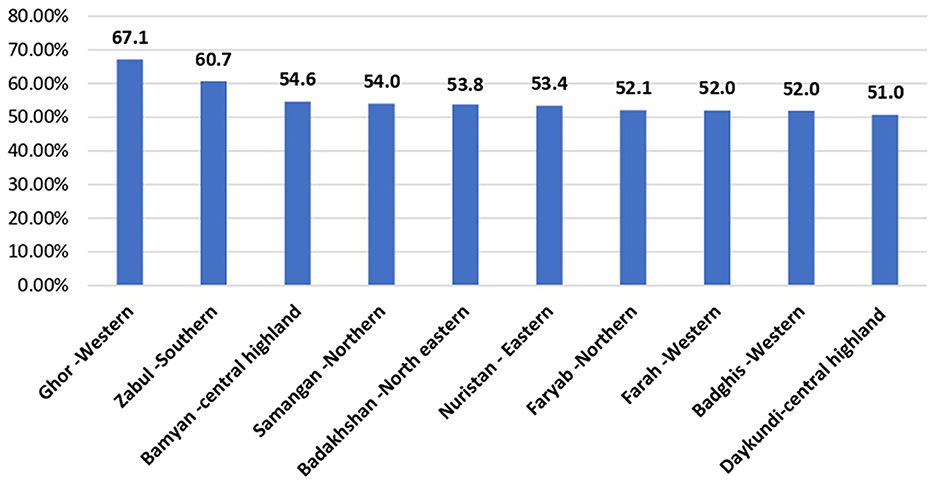
Figure 4. The bar chart represents the top 10 provinces demonstrating the high percentage of underserved populations in Afghanistan.
The present study aimed to highlight the current situation of underserved areas in Afghanistan (as a percentage of the total population, highly ranked regions, and provinces) and demonstrate the characteristics of the highly affected groups in the underserved areas by disaggregating the data of the underserved areas, based on genders and vulnerable age groups to identify the most vulnerable groups in these areas.
Approximately one-quarter of the population living in Afghanistan is deprived of any primary healthcare services. In our study, among those deprived, almost no differences were observed based on gender, and the majority (~90%) were found to reside in rural areas. The latter finding may raise major concerns and may have consequences for the health of the population, especially in a developing country with instability. The high percentage of the underserved population could be attributed to the fewer number of healthcare workers (HCWs) in rural areas compared to urban areas (13), where it is estimated that, for every 10,000 individuals, there are 17 HCWs in rural areas compared to 36 in urban areas (1). Furthermore, the gender of HCWs aggravates this problem as it is not culturally acceptable for a female patient to be examined by a male HCW (14). This is crucial considering that the United Nations Development Program has reported the rate of development to have taken slow progress, which exposes the country to insecurities and unstable conditions that affect the health status of the citizens (15).
Approximately half of the proportion of the services is delivered through either basic or sub-health centers. Providing basic health services is crucial for maintaining the health status of individuals, yet it should be also noted that only 2.2% of the services are delivered through a specialist or at least a secondary level of care (district hospital) with < 1% providing specialized care. Moreover, emergency or first aid trauma services are delivered by 2% of the health facilities. The latter two figures are of extreme value in areas of conflict. Afghanistan is characterized by having more than 80% of the land as mountainous. This aspect forces the population to be distributed or scattered over multiple small terrains (9), with a high proportion of them being mobile population (16). This is why the presence of mobile health teams or clinics delivering services is also of high value, which accounts for 17% in the present study. It should also be noted that over half of the services delivered through HER facilities rely mainly on funds from the World Bank, which can expose the country to major health consequences in case of new epidemics or catastrophes necessitating shifting of the fund.
The most affected region in the country is the Central Highlands, characterized by rugged and mountainous terrain that makes travel challenging and hinders the construction of reliable transportation infrastructure, thereby limiting access to health facilities. Even though the two provinces of this region—Daykundi and Bamyan—are not highly affected, the absence of variation could indicate that the entire region is affected in the same way. Furthermore, there are minor differences between the population of men, women, and women of childbearing age (~50%). This is different from the provinces of the western region, which fall in the second place among the overall underserved regions. It is the highest in Ghor (67%), whereas it is the lowest in Hirat, which was below 30%. The latter figure indicates that the variations within provinces require different approaches to adjust and apply. In the southern region—the third most affected one—the variation is much greater, being highest in Zabul and lowest in Kandahar.
The capital region has the lowest percentage of the underserved population, with Kabul having the lowest and Maidan Wardak province the highest, showing nearly a 30% variation in the percentage. Nangarhar province, in the eastern region, has the lowest underserved population (< 1%). However, as in most regions, there are wide variations between provinces in the eastern region. These disparities between different regions and provinces could be attributed to many factors, such as poverty, transportation, roads, and areas of previous conflicts (16). A high percentage of out-of-pocket health expenditures alongside poverty presents a major challenge to the access to health services, which results in the population being underserved (17). Moreover, in early 2000, approximately half of the respondents in a survey reported not seeking treatment for health problems (18). The presence of transportation and well-constructed roads were the key factors leading to contrasting figures. In Kabul, the capital, more than 50% of the population had access to transport for emergency obstetric facilities; however, this figure decreased to < 20% in Badakhshan province in the far northeast (13). Furthermore, harsh weather conditions, including snowfall and flooding, can augment the problem of internally displaced people, disrupt transportation, and make it difficult for individuals to reach health facilities, especially during the winter months in some parts of the country (19). In addition, unstable conditions, such as war or conflicts, are also responsible for the inability to provide citizens with health services. In areas of conflict, such as Helmand, the health facilities have dropped by more than 35% owing to unstable conditions during the years 2004–2006 (20). Furthermore, challenges related to the presence of landmines and unexploded ordnance, particularly in previous conflict-affected areas, can pose a threat to individuals seeking healthcare and limit the development of infrastructure (21).
Minimal overall differences between men and women were also present within each region and province. This finding could indicate that the lack of access to primary or any health service is not primarily based on gender discrimination. Moreover, women of childbearing age show similar patterns, yet this group is highly vulnerable. The latter group represents a major challenge in recruiting female HCWs because the problem of unmet needs exists despite multiple efforts (22).
The region with the highest underserved older adult population is the northern region, with the same percentage (3%) in all provinces of this region. However, it does not have the highest percentage of underserved populations of children under the age of five. On the other hand, southern and southeastern regions have the highest percentages of underserved populations of children under the age of five. This could require different approaches to provide these age groups with suitable services. The group comprising children under the age of five is a vulnerable one, especially with an estimated mortality rate of 55.7 deaths per 1,000 live births and with approximately one million children experiencing symptoms associated with malnutrition [(7) in the background].
This study employed robust methodologies, gathering the most reliable and recent data on the social and economic situation in Afghanistan. Additionally, the data on the presence of primary healthcare services were also collated. However, this study was conducted within the constraints of the available population data. Primary data on Afghanistan are generally hard to find, and most comprehensive surveys are too old and outdated to be considered credible. Furthermore, data sources relating to Afghanistan are often not open-source, i.e., they are not accessible. These limitations are acknowledged in relation to the findings of the study.
Afghanistan is currently experiencing a protracted humanitarian crisis, which is impacting millions of people living in poverty or lacking access to healthcare. Approximately 9.4 million Afghans lack access to primary healthcare services, with the majority residing in rural communities. The Central Highlands, western region, and southern region exhibit the highest rates of underserved populations. Notably, Ghor province in the western region and Zabul province in the southern region stand out as having the most significant number of individuals without access to primary healthcare. Furthermore, the analysis highlights the vulnerabilities of women of childbearing age, as well as children under the age of five, who comprise a considerable portion of the underserved population. This situation elevates the risk of disease outbreaks, famine, and heightened mortality, particularly among the vulnerable populations. The status is further exacerbated by ongoing conflicts, extreme weather events, and the legacy of decades of instability, which have significantly weakened the healthcare system. Addressing this crisis requires a multi-pronged approach that prioritizes increasing funding for healthcare services, implementing alternative strategies to reach the most vulnerable populations, and ensuring equitable access to healthcare across the nation, particularly in under-resourced and marginalized communities.
MS: Writing – original draft. NH: Writing – original draft. SE: Writing – original draft. JS: Conceptualization, Writing – review & editing. RN: Formal analysis, Writing – review & editing. AK: Formal analysis, Writing – review & editing. JT: Validation, Writing – original draft. AA: Conceptualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ministry of Public Health. A Basic Package of Health Services for Afghanistan 2010/1389. Berlin: Islamic Republic of Afghanistan (2010).
2. Safi N, Anwari P, Safi H. Afghanistan's health system under the Taliban: key challenges. Lancet. (2022) 400:1179–80. doi: 10.1016/S0140-6736(22)01806-2
3. Safi N, Singh LS, Naseri S, Anwari P. An alternative model for health service delivery in Afghanistan. Lancet. (2021) 398:1481–2. doi: 10.1016/S0140-6736(21)02187-5
4. Mohammed RN, Khawari A, Shaguy JA, Abouzied A. A GIS-based approach to identifying communities underserved by primary health care services—An Afghanistan case study. Front Public Health. (2023) 11:1209986. doi: 10.3389/fpubh.2023.1209986
5. World Health Organization. WHO Afghanistan Emergency Plan: Meeting the Health Needs of Afghanistan's Crisis-Affected Populations. WHO (2021). Available at: https://www.who.int/publications/m/item/who-afghanistan-emergency-plan-meeting-the-health-needs-of-afghanistan-s-crisis-affected-populations (accessed November 12, 2023).
6. The World Bank. 2020 Policy Notes: Priorities for Inclusive Development in Afghanistan. (2021). Available at: https://thedocs.worldbank.org/en/doc/8033eefca38ca8af7b653869a3469087-0310012021/original/Policy-Notes-report-Jan-12-2021-Final-version-2.pdf (accessed October 26, 2023).
7. UNICEF. Afghanistan: Key Demographic Indicators. (2023). Available at: https://data.unicef.org/country/afg/?_gl=1*1v6ofi2*_ga*MTU3MzExMDY2OS4xNjc2NzE2MDcw*_ga_ZEPV2PX419*MTcwMDc1Mzc3OS4xLjEuMTcwMDc1MzgwNC4zNS4wLjA (accessed November 1, 2023).
8. UNDP. Human Development Report. (2020). Available at: https://hdrundporg/content/human-development-report-2020 (accessed November 26, 2023).
9. Country Reports. Afghanistan Geography. (2023). Available at: https://www.countryreports.org/country/Afghanistan/geography.htm#:~:text=Afghanistan's%20geography%20consists%20of%20irrigated,peaks%20rising%20about%2024%2C000%20feet (accessed October 6, 2023).
10. World Health Organization. Underserved areas-WHO Afghanistan Health Information Hub. WHO (2023). Available at: https://dashboard.whe-him.org/index.php/maps-3/ (accessed December 14, 2023).
11. World Health Organization. Primary Health Care: Key Facts. WHO (2023). Available at: https://www.who.int/news-room/fact-sheets/detail/primary-health-care
12. World Health Organization. Universal Health Coverage (UHC): Key Facts. WHO (2023). Available at: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc) (accessed November 12, 2023).
13. Carvalho N, Salehi AS, Goldie SJ. National and sub-national analysis of the health benefits and cost-effectiveness of strategies to reduce maternal mortality in Afghanistan. Health Policy Plan. (2013) 28:62–74. doi: 10.1093/heapol/czs026
14. Ahmadi Q, Danesh H, Makharashvili V, Mishkin K, Mupfukura L, Teed H, et al. SWOT analysis of program design and implementation: a case study on the reduction of maternal mortality in Afghanistan. Int J Health Plann Manage. (2016) 31:247–59. doi: 10.1002/hpm.2288
15. UNDP Afghanistan. Economic Instability and Uncertainty in Afghanistan after August 15: A Rapid Appraisal 2021. (2023). Available at: https://www.undp.org/publications/economic-instability-and-uncertainty-afghanistan-after-august-15 (accessed Decmber 20, 2023).
16. International organization for Migration. Afghanistan: Displacement Tracking Matrix: International organization for Migration. (2022). Available at: https://dtm.iom.int/afghanistan
17. Sabri B, Siddiqi S, Ahmed A, Kakar F, Perrot J. Towards sustainable delivery of health services in Afghanistan: options for the future. Bull World Health Organ. (2007) 85:712–8. doi: 10.2471/BLT.06.036939
18. Steinhardt LC, Waters H, Rao KD, Naeem AJ, Hansen P, Peters DH. The effect of wealth status on care seeking and health expenditures in Afghanistan. Health Policy Plan. (2009) 24:1–17. doi: 10.1093/heapol/czn043
19. Sayed N, Sadat S. Climate Change Compounds Longstanding Displacement in Afghanistan. Berlin: Migration Policy Institute (2022).
20. Belay TA. Building on Early Gains in Afghanistan's Health, Nutrition, and Population Sector: Challenges and Options. Kabul: World Bank (2010).
21. Kadir A, Shenoda S, Goldhagen J. Effects of armed conflict on child health and development: a systematic review. PLoS ONE. (2019) 14:e0210071. doi: 10.1371/journal.pone.0210071
22. Mansoor GF, Hill PS, Barss P. Midwifery training in post-conflict Afghanistan: tensions between educational standards and rural community needs. Health Policy Plan. (2012) 27:60–8. doi: 10.1093/heapol/czr005
23. Humanitarian Development Report (2020). Available at: https://afghanistan.un.org/en/89938-afghanistan-human-development-report-2020
24. WHO Emergency Operational Plan. Available at: https://worldhealthorg.sharepoint.com/sites/AFGWHEHIM/_layouts/15/viewer.aspx?
Keywords: Afghanistan, underserved areas, provinces, equity, vulnerable groups, health services
Citation: Salem MR, Hegazy N, Eldeeb S, Shaguy JA, Nassery RM, Khawari A, Tanoli J and Abouzeid A (2024) The current situation of health equity in underserved areas of Afghanistan. Front. Public Health 12:1370500. doi: 10.3389/fpubh.2024.1370500
Received: 14 January 2024; Accepted: 15 August 2024;
Published: 24 September 2024.
Edited by:
Nicolai Savaskan, District Office Neukölln of Berlin Neukölln, GermanyReviewed by:
Roberto Carlos Hincapie, Pontifical Bolivarian University, ColombiaCopyright © 2024 Salem, Hegazy, Eldeeb, Shaguy, Nassery, Khawari, Tanoli and Abouzeid. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marwa Rashad Salem, bXI4MDAwMjAwMEBrYXNyYWxhaW55LmVkdS5lZw==; bXI4MDAwMjAwMEBjdS5lZHUuZWc=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.