
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Public Health , 31 January 2024
Sec. Aging and Public Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1369827
This article is part of the Research Topic Innovations in Older Adult Care and Health Service Management: A Focus on the Asia-Pacific Region View all 15 articles
Editorial on the Research Topic
Innovations in older adult care and health service management: a focus on the Asia-Pacific region
Population aging in the Asia-Pacific Region is a significant challenge for the 21st century. With countries in the Asia-Pacific aging faster than any region in the world, demographic transition and challenges associated with it have grown to utmost social, political, healthcare, and economic significance. Nearly 60 percent of the world's population over 60 years of age reside in the Asia-Pacific region, which amounts to 630 million people (1). This population is projected to reach 1.3 billion by 2050 (1). In general, older adults exhibit higher prevalence of chronic conditions, comorbidities, and hospital admissions, which in turn elevate health care costs. Women comprise of over 60% of the older adult population in the Asia Pacific (2). Gender imbalance has implications for social support and health care systems, given that women typically have greater life expectancy and can face more years of potential disability. Given the traditional role of women as family caregivers in many societies in the region, older women could face greater pressure potentially impacting their health and wellbeing. Traditional models of health workforce development and service delivery are less likely to be effective in addressing the growing concerns if the focus remains centered on specialized and tertiary care. It is essential to strengthen primary and community-based models of care that caters to the growing needs of and are sensitive to cultural contexts, local challenges, and specific requirements of older adults.
Based on the United Nations Economic and Social Commission of Asia and the Pacific, the region is divided into five divisions (1): (i) East and Northeast Asia, (ii) South-East Asia, (iii) South and South-West Asia, (iv) North and Central Asia, and (v) Pacific (see Figure 1). The 56 countries in this region come with varying levels of social and economic progress. The World Bank identifies two of these countries as low-income economies, 26 as lower middle-income economies, 17 as upper middle-income economies and 11 as high-income economies (see Supplementary Table 1). Over the last two decades, China, India, Indonesia, Philippines, Thailand, and Vietnam consistently outperformed other emerging markets in the world economically. In addition to the fast-paced economic growth in the region, Asia-Pacific countries share a rich and diverse cultural history. In many cultures, particularly those in the Indian subcontinent, China and Southeast Asia, there is a deeply ingrained tradition of venerating older adults, with the care for aged parents being viewed as a sacred duty bestowed by the divine. Nevertheless, these societies are facing increasing pressure of globalization and westernization of care, reshaping conventional approaches to older adult care.
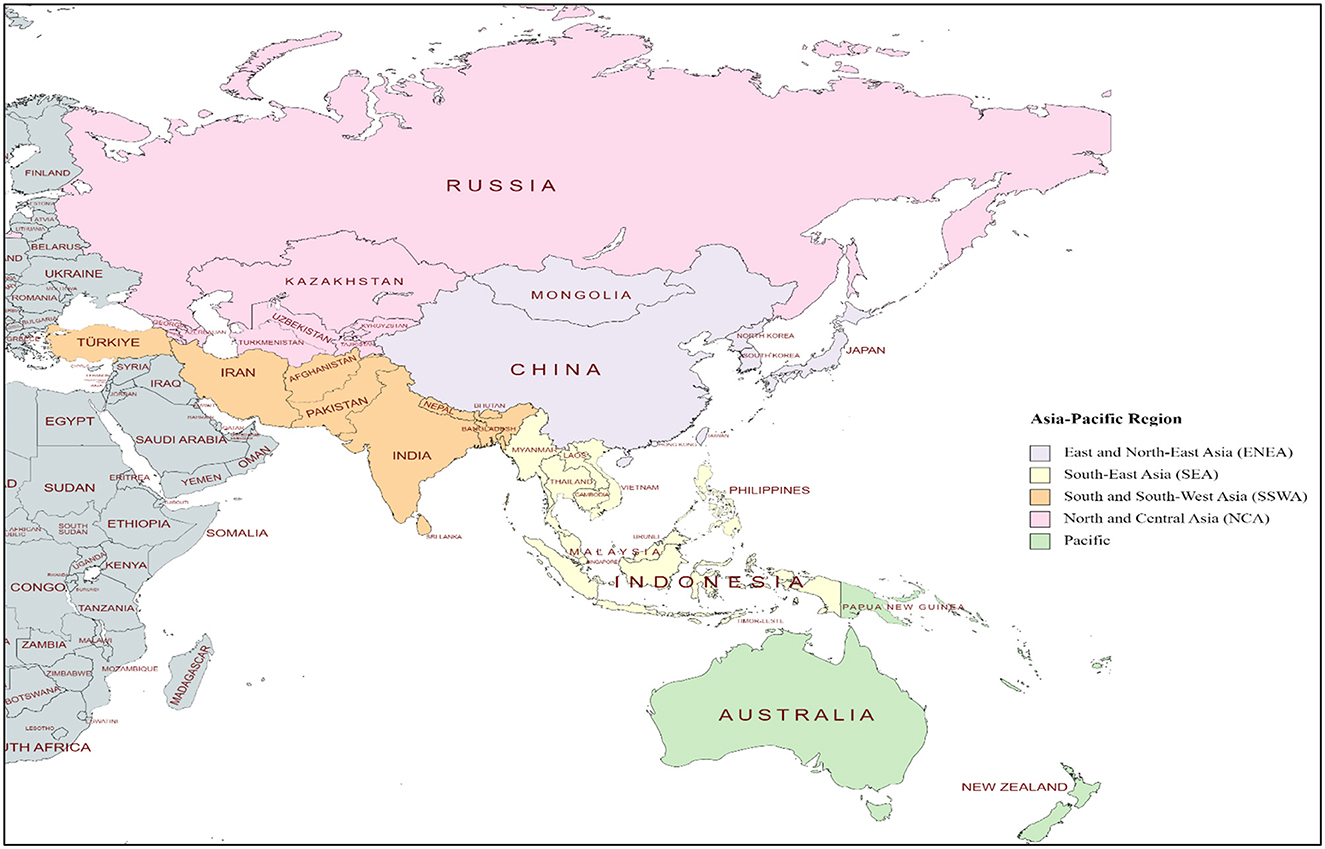
Figure 1. The Asia-Pacific Region. Asia-Pacific subregions and country classification is based on the United Nations Economic and Social Commission for Asia and the Pacific categorization. This map has been generated utilizing mapping tools available at mapchart.net, licensed under CC BY-SA 4.0.
To steer the global response to aging, the WHO released the first World report on aging and health reviewing knowledge gaps and instigating a public health framework that identified four key areas: integrated care provision, long term care, age friendly environments and improved measurement and monitoring (3). Healthy aging was built on the notion of functional ability, seen as a combination of intrinsic capacity of individual, environmental characteristics, and interactions between individual and the environment. For the first time, a population aging metric reflecting both on longevity and health status was developed by the global burden of disease study conducted by Chang et al. (4). By incorporating 92 age related diseases, they extended our thinking beyond chronological age to account for both health status and disease severity, allowing cross country comparisons to inform policy decisions. Utilizing this metric, the top five countries globally with the highest aged-standardized disease burden rates are all in the Asia-Pacific region (Papua New Guinea, Marshall Islands, Vanuatu, Afghanistan, and Solomon Islands). Meanwhile Singapore, South Korea and Japan have some of the lowest age standardized disease burden. Comparing across countries, the equivalent age for the reference population (65 years) varied widely ranging from 76.1 years in Japan to 45.6 years in Papua New Guinea; meaning that a 76-year-old in Japan has the same age-related disease burden as a 65-year-old globally (4). The onus falls on the countries, and as mentioned in the WHO Global Strategy and Action Plan on Aging and Health (5), to accelerate action to ensure older adults can live a long and healthy life.
Our Research Topic was one of the first attempts to explore innovations in aged care and health service management across Asia and the Pacific, especially with a country- or region-specific approach. We adopted a co-design process of by working collaboratively with key country-level experts well-positioned to reach out to policymakers, academics, and researchers working in aged care and aged care management in different healthcare contexts in the region. The country co-leads or experts were well positioned to promote and disseminate findings to academic and policy networks. The issue and articles were widely marketed in the Asia-Pacific Region through networks, organizations, and media channels.
Since the launch of the Research Topic in July 2022, the issue has garnered significant interest among academics, researchers, and community, amassing close to 15,000 views. The published articles included in the issue have been viewed 12,663 times and downloaded 3,850 times. The level of engagement is also underscored by the 2,250 views on the topic itself. Moreover, the year 2023 has seen a continued upward trend in both views and downloads, indicating a rising interest on the subject matter and the research published therein (see Supplementary Figures 1, 2).
The Research Topic offers a rich and diverse collection of scholarly work on innovations in aged care and health service management across the Asia-Pacific region. We include a total of 14 articles, comprising 12 original research articles, one research report, and one perspective article. The research presented comes from nine countries, including Australia, Bangladesh, China, India, Japan, the Republic of Korea, Singapore, Thailand, and Vietnam. Table 1 presents a summary of studies included in the Research Topic, which are further described below.
Dix et al. present a case study on infection prevention and control (IPC) and the use of personal protective equipment (PPE) training for Australia's aged care workforce, set against the backdrop of the COVID-19 pandemic and involving residential aged care facilities (RACF) in the state of Victoria. Utilizing mixed methods techniques, the authors argue that the government, working in partnership with Monash University, an academic institution, had improved the design, development, and implementation of the program. This initiative is argued to be the largest state-funded program delivered to residential aged care workers and addresses the urgent need for rapid training of RACH staff in IPC and PPE. Over 4,200 RACF staff, including 1,207 facility champions, completed this program. This research sheds light on how collaborative efforts that integrate academic expertise can lead to swift and well-founded implementation, a strategy that was especially effective in the initial phase of the COVID-19 crisis in Australia.
A study from Bangladesh by Mistry et al. explored the COVID-19 related stigma among older adults in Bangladesh. Utilizing a cross-sectional design, over 1,000 older adults were surveyed through telephone interviews. The study identified that the prevalence of stigma related to COVID-19 was high among older adults, providing several implications to policymakers and public health personnel, and toward the design of mass media campaigns to inform and educate people on the stigma associated with COVID19. The authors also indicate that failure to understand the role of stigma might result in suboptimal reach of public health programs aimed at COVID19 prevention and management. Reflecting on this fascinating study, one could see similar pivots across the Asia-Pacific region, and relevance to many rural, remote, and disadvantaged communities.
Studies from China focused on community-based services, the role of informal carers, and long-term functional outcomes. Through a study utilizing China Health and Retirement Longitudinal Survey, Yi et al. conclude that the use of home- and community-based services can both reduce hospital utilization and expenditures among disabled older adults that contribute to their physical and psychological health. Hu et al. looked at informal care and examined the association between caring load and family caregivers' burden. The paper concludes that there is a significant positive association between caring load and caregiver burden and recommends more guidance services and support for family caregivers. Nhu et al. used a dynamic ensemble selection modeling approach in the prediction of posttraumatic functional recovery in middle-aged and older patients. They conclude that preexisting conditions can predict long-term functional outcomes, and thereby influence prognosis and clinical decision-making for older adult care.
Sastry et al. provided insights into the rich cultural heritage of India, and how the country is adapting the UN Health Aging Framework to the country's unique historical context and traditions. The paper highlights some interesting innovations by the Indian government such as “Savera Yojana” where older people can utilize digital technologies to reach friendly cops for personal security issues. Newer models of care such as 'adopting a granny' by school children, when a nursing home and school for orphans are cohabitated, are emerging in India, and seen as an avenue to improve intergenerational bonding. In another article by Reddy et al. the study examined the prevalence, associated factors and health expenditures of non-communicable disease multimorbidity from a health district in India. They identified that a significant proportion of the people had NCDs and argued that those with multimorbidity spent almost four times higher out of pocket expenditure than those without NCDs. The study suggests that national programs (such as Ayushman Bharat Scheme) can improve access to care and address the financial burden for care among older adults.
Japan, a pioneer in aged care solutions, presents valuable opportunities for international learning in this sector. The study by Katayama et al. examined the relationship between vision and hearing conditions among older adults. The study, which employs a mix of audiovisual, olfactory, and medical assessments, explores the connection between tinnitus and olfactory dysfunction. It determines that understanding the interplay between different sensory organs is crucial in assessing how sensory impairments affect cognitive function. The study provides some insights into the interconnectedness of sensory diseases and offers arguments into how and why integrated service provision needs to emerge in primary care.
A strong research environment is the backbone for evidence-informed policy and practice decision-making. In a cross-country study, Kotani et al. examined the critical care research environment in three Asian countries: Japan, South Korea, and Singapore. The study identified that having secured time for research activities, practicing at a university-affiliated hospital, and having clinical experience of 10 years or longer for whom? Were significantly associated with higher research productivity. The authors also argue the importance of building a collaborative environment between academia and non-academia (clinicians, public health professionals, community personnel etc.) as it contributes to the development of an evidence-based culture for care provision.
Boo and Oh, in their research on the use of Artificial Intelligence for a health care pilot project in South Korea, examined the perception of registered nurses on implementing smart technologies for older adults in primary care. The authors confirmed the need for future healthcare policies and strategies for the implementation of digital health technologies, particularly in the context of home visiting technologies. Also from South Korea, Lim et al. examined the risk of hospitalization and emergency department visits due to potentially inappropriate medication use among older adults. The study recommended the development of deprescribing strategies to control potentially inappropriate medication (PIM) and polypharmacy collectively.
A study conducted in Thailand by Pengpid et al. examined the bidirectional association between functional disability and multimorbidity among middle-aged and older adults. Using longitudinal data from the Thailand Health, Aging and Retirement Survey, the study identified that baseline multimorbidity increased the risk of functional disability, and further baseline functional disability increased the risk of incident multimorbidity. The authors argued that health services in Thailand should be reoriented to tailor the intervention to individuals with multimorbidity to prefer future functional disabilities.
The final two included studies from Vietnam by Pardoel et al. and Mackenzie et al. looked at the implementation of the intergenerational self-help clubs (ISHCs) and fall prevention tools respectively. Pardoel et al. conducted assessed the benefits of 97 ISHCs in nine provinces in Vietnam. The authors reported a high reach and uptake of services by ISHC, and a satisfaction rate of almost 75% among participants using them. Mackenzie et al. evaluated the validity and reliability of a home falls and accidents screening tool. Considering the relevance of home and informal care in Vietnam, the use of early screening and prevention tools cannot be underestimated.
A highly cited article published in Frontiers in Medicine by Franceschi et al. (6) argue that aging and age-related diseases share similar molecular and cellular mechanisms, and thus the primary focus of medicine should be on combating aging. The authors also venture to discuss on aging and rejuvenation (or feasible age extension) research and call for the importance of identifying biomarkers able to distinguish individuals with higher risk of developing age related diseases. From a public health perspective, this approach might seem unorthodox, but despite the progress achieved, it calls for wider engagement with a multidisciplinary audience. Our Research Topic, mainly from a public health and health management standpoint, shed light on a number of innovations on aged care in the Asia Pacific region. Although we don't argue that the challenges brought forth in this issue as comprehensive or even methodically organized, we recognize the importance to combat aging through innovative strategies that demand creative and unconventional thinking.
Our issue mainly makes the case for three arguments. First, aging is widely affecting the Asia-Pacific region, and countries are adopting innovative approaches and strategies to deal with aging. Second, Asia-Pacific countries bring rich cultural history and connotations to aged care, and its vital that traditional learnings and practices are nurtured to develop culturally sensitive and locally responsive models for aged care. Finally, the disease disparity and aged care practices across the region, provides an opportunity for cross-cultural and cross-country learnings, which can benefit both the developed and developing economics in the region and beyond.
This Research Topic has featured original research articles (n = 12), short reports (n = 1) and perspectives (n = 1) from nine countries in the region (Australia, Bangladesh, China, India, Japan, Republic of Korea, Singapore, Thailand, and Vietnam). Commissioned in July 2022, we began with a unique process of involving country leads across the region in the promotion of the Research Topic and aimed at improving social impact through the rapid dissemination of research findings. Over the last 18 months, the Research Topic has generated 14,913 views and 3,850 article downloads. We included research on innovative models such as the intergenerational self-help clubs (Vietnam), artificial intelligence based smart care (Republic of Korea) and infection control training programs during COVID19 (Australia). The Research Topic also included studies that examined role of stigma toward older adults with COVID-19 (Bangladesh), cost benefits of home-based models (China) and the role of United Nations Healthy Aging agenda (India). The dominant themes emerging from the Research Topic mainly included: (i) service redesign, (ii) training for providers, (iii) shift to community/home-based care, and (iv) adapting successful global frameworks/instruments. Overall, it was particularly noteworthy to observe that several countries are thoughtfully assessing and evolving their unique and culturally rich traditional systems of older adult care to addressing contemporary needs and expectations.
MB: Conceptualization, Writing – original draft, Writing – review & editing. AS: Conceptualization, Writing – review & editing. ZL: Conceptualization, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. MB acknowledges NHMRC Sidney Sax Fellowship Grant (GNT1121576) and Flinders University CBGL Establishment Fund that assisted in various phases of conceptualization and development of this issue.
We thank Prof. Marcia G. Ory, Specialty Chief Editor of Frontiers in Public Health (Aging and Public Health), for commissioning this Research Topic. We acknowledge the support from Ms. Bethany Gallagher and other members of the Frontiers Editorial and Publishing team for their constant support and guidance over the last 2 years. We also thank all country level leads and authors for their contributions.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1369827/full#supplementary-material
1. United Nations Economic and Social Commission for Asia and the Pacific (ESCAP). Asia-Pacific Report on Population Ageing 2022 Trends, Policies and Good Practices Regarding Older Persons and Population Ageing. Bangkok: United Nations Publishing (2022).
2. United Nations Populations Fund. Perspectives on Population Ageing in the Asia-Pacific Region - Where Do Selected Countries Stand 15 Years After the Adoption of the Madrid International Plan of Action on Ageing? Bangkok: United Nations Publishing (2017).
3. Beard JR, Officer A, De Carvalho IA, Sadana R, Pot AM, Michel J-P, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. (2016) 387:2145–54. doi: 10.1016/S0140-6736(15)00516-4
4. Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health. (2019) 4:e159–67. doi: 10.1016/S2468-2667(19)30019-2
5. World Health Organization. Global Strategy and Action Plan on Ageing and Health. Geneva: WHO. (2017). Available online at: http://apps.who.int/bookorders (accessed December 30, 2023).
Keywords: older adults, aged care, Asia-Pacific, health workforce, models of care, health systems
Citation: Balasubramanian M, Shafei AA and Liang Z (2024) Editorial: Innovations in older adult care and health service management: a focus on the Asia-Pacific region. Front. Public Health 12:1369827. doi: 10.3389/fpubh.2024.1369827
Received: 13 January 2024; Accepted: 18 January 2024;
Published: 31 January 2024.
Edited and reviewed by: Marcia G. Ory, Texas A&M University, United States
Copyright © 2024 Balasubramanian, Shafei and Liang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Madhan Balasubramanian, bWFkaGFuLmJhbGFzdWJyYW1hbmlhbkBmbGluZGVycy5lZHUuYXU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.