
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 21 March 2024
Sec. Public Health and Nutrition
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1368069
This article is part of the Research Topic Diet and Training Strategies to Optimize Health Parameters View all 12 articles
Introduction: Lifestyle factors, including inadequate eating patterns, emerge as a critical determinant of chronic disease. Apart from caring for patients, nurses should also take an active role in monitoring and managing their own health. Understanding the intricate relationship between nurses’ eating behavior and managing their own health is crucial for fostering a holistic approach to healthcare, therefore our study aimed to evaluate eating behavior and demographic factors influencing chronic disease prevalence in a sample of community nurses from Romania.
Methods: Between October–November 2023, 1920 community nurses were invited to answer an online survey, using an advertisement in their professional network. Of them, 788 responded. In the survey, which included a semi-quantitative food frequency questionnaire with 53 food items, the Intuitive Eating Survey 2 (IES-2), and demographic items were used.
Results: A multivariate model was built for the prediction of the association between eating behavior and other factors associated with chronic diseases. The majority of participants were females (95.1%), with the largest age group falling between 40 and 49.9 years (48.2%). Regarding the EFSA criteria for adequate carbohydrate and fat intake, 20.2% of the group have a high intake of carbohydrates, respectively, 43.4% of the group have a high intake of fat. Analysis of chronic diseases indicated that 24.9% of individuals reported at least one diagnosis by a physician. The presence of chronic disease was associated with a low level of perceived health status, with an OR = 3.388, 95%CI (1.684–6.814), compared to those reporting excellent or very good perceived health status. High stress had an OR = 1.483, 95%CI (1.033–2.129). BMI had an OR = 1.069, 95%CI (1.032–1.108), while low carbohydrate diet score had an OR = 0.956, 95%CI (0.920–0.992). Gender and IES-2 did not significantly contribute to the model, but their effect was controlled.
Discussion: By unraveling the intricate interplay between nutrition, lifestyle, and health outcomes in this healthcare cohort, our findings contribute valuable insights for the development of targeted interventions and support programs tailored to enhance the well-being of community nurses and, by extension, the patients they support.
Lifestyle factors, notably inadequate eating patterns, emerge as pivotal determinants influencing the onset and progression of chronic diseases (1). Inadequate dietary patterns have emerged as significant contributors to the development of obesity and various diseases of civilization, presenting a pressing public health concern globally. These dietary patterns, characterized by excessive intake of energy-dense foods high in sugars, unhealthy fats, and processed ingredients, coupled with insufficient consumption of nutrient-rich whole foods, have been closely linked to the rising prevalence of obesity and overweight populations. Furthermore, such dietary habits are implicated in the onset and progression of chronic diseases such as type 2 diabetes, cardiovascular diseases, hypertension, and certain cancers (2–4).
Nurses play a vital role in chronic disease management, serving as frontline healthcare providers. Their responsibilities encompass patient education, monitoring, and coordination of care to enhance patient outcomes. Nurses often facilitate lifestyle interventions, medication adherence, and provide emotional support to individuals with chronic conditions. Their holistic approach addresses not only the physical aspects of the disease but also the psychological and social components, promoting a patient-centered care model. The collaborative efforts of nurses contribute significantly to the overall well-being and quality of life of individuals living with chronic diseases (5, 6).
Beyond their dedicated roles in patient care, nurses should actively participate in monitoring and managing their own health. Nurses must maintain adequate eating behavior for several reasons. Firstly, nurses play a pivotal role in promoting health, and their own well-being sets an example for others. Secondly, proper nutrition contributes to sustained energy levels, enhancing nurses’ ability to meet the physical and mental demands of their profession. Additionally, adequate eating behavior is linked to overall health, reducing the risk of chronic diseases that could affect job performance. Lastly, nurses with healthy eating habits are better equipped to educate and guide patients on lifestyle choices, creating a positive impact on public health (1, 7, 8).
Recognizing the intricate relationship between nurses’ eating behavior and their overall well-being is paramount for fostering a comprehensive and proactive approach to healthcare (9). In light of this, our study delves into the evaluation of eating behavior and demographic factors influencing chronic disease diagnosis, focusing specifically on a sample of community nurses from Romania. This research aims to unravel the nuanced connections between nurses’ lifestyles, eating habits, and their susceptibility to chronic conditions, offering valuable insights for promoting individual health and advancing healthcare practices.
In Romania, community nurses play a crucial role in providing medical and nursing care to patients outside of traditional hospital settings. Their main objective is to enhance access to quality medico-social services for the population, particularly for vulnerable groups. This involves offering preventive, curative, and recovery medical services and managing complex cases of chronic or rare diseases. Between October–November 2023, out of the 1920 community nurses (90% females) employed in Romania, 788 participants willingly took part in this study, resulting in a response rate of 41.1%.
The recruitment of participants for our research project took place in October–November 2023 through an advertisement on a professional network and a national work platform targeting community nurses in Romania. We used the Google Forms platform to embed the questionnaire link in the advertisement. The introductory page of the questionnaire provided details about the study’s purpose, estimated completion time, instruments used, and anticipated outcomes. Participants were required to answer all questions, and their explicit agreement was necessary to gain access to survey. Only those who completed the entire questionnaire were permitted to submit the form. A flow-diagram depicting important aspects of the procedure is presented in Figure 1.
Our study protocol received approval from the Research Ethics Committee of Victor Babes University of Medicine and Pharmacy (Approval No. 30/31.03.2022). Participants voluntarily consented to participate, adhering to the principles outlined in the Helsinki Declaration throughout the study.
Our nutritional assessment involved using a validated FFQ (10, 11), which included 53 different food items. This questionnaire was designed to gather information about food intake over the course of last 30 days. For each item, we investigated the frequency and usual amount of consumption. Additional questions regarding specific items were asked to estimate the quantity of fat or added sugar. The Romanian version of the FFQ is available as a supplementary material (Supplementary material 1). We converted the intakes to grams using household scale guidelines (12) and calculated energy and macronutrient intakes for each individual using a specialized computer program. Finally, we transformed macronutrient intakes into a percentage of contribution to the total energy consumed.
To determine adherence to a low carbohydrate diet, a score called the low carbohydrate diet (LCD) score was calculated, using deciles of the percentage of macronutrients (13, 14). The score for carbohydrates ranged from one to ten, with the lowest decile receiving the highest score of 10, and the highest decile receiving the lowest score of one. For fat and protein, the lowest decile received a score of one, and the highest decile received a score of 10. The individual scores for each macronutrient were then added to get the LCD score, which can range from 3 to 30, with higher scores indicating better adherence to a low carbohydrate diet. European Food and Safety Authority (EFSA) recommendations (15) for adequate intake, were used to create two variables for individual meeting or not the recommended intake for carbohydrates and fat, using the contributing percentage of each of the macronutrients to total energy intake.
The Intuitive Eating Scale-2 (IES-2) is the most widely used measure to assess intuitive eating (16) and was recently validated in Romanian (17). It consists of 23 items. Items 4, 5, 6, 11–23 are scored Strongly Disagree = 1, Disagree = 2, Neutral = 3, Agree = 4, Strongly Agree = 5 and for items 1, 2, 3, 7, 8, 9, and 10 the scoring is reversed. The IES-2 score is obtained by adding all the individual item scores and then by division to the number of items (23 items). Higher scores on the IES-2 indicate a greater ability to eat intuitively. The Romanian version of the IES-2 is available as a supplementary material (Supplementary material 2).
In addition to the aforementioned instruments, the study also included questions regarding gender, age, relationship status (5 categories), education level, using International Standard Classification of Education (ISCED) (18), self-perceived health status (5 levels), years of experience as a community nurse, and self-perceived stress levels. Stress levels were rated on a 10-point scale, with higher values indicating higher levels of stress. Moreover, community nurses were requested to assess their height and weight through measurement, as well as to indicate the existence of chronic diseases and provide diagnoses of such diseases, which were set by physicians. Participants were presented with a dropdown list of seven chronic diseases that have a significant impact on public health and are heavily influenced by lifestyle choices (1). These diseases included hypertension, heart failure, ischemic heart disease, type 2 diabetes, obesity, asthma, and chronic obstructive pulmonary disease. Additionally, participants were given the option to provide an open response and list any other chronic diseases that have been diagnosed by their physicians. For those who reported one or more diagnoses, a follow-up question was asked regarding their treatment of the chronic disease (s).
Data transformations and statistical analyses were performed using IBM SPSS version 21. All submitted participant responses were included in the analysis. Height and weight were self-reported, but nurses were asked to report a measurement not older than 3 months. Height and weight were further used for the calculation of body mass index (BMI; BMI = weight (kg)/height (m)2). The nutritional status of the participants was determined using the following BMI thresholds: underweight (BMI below 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (over 30 kg/m2). Other variables were categorized as such: age was split into 3 groups: <=40 years, 40–49.9 years and > =50 years; relationship status was dichotomized: in a relationship versus alone; education was divided into 2 levels, equivalent to ISCED 4 or less, ISCED 5 or above; self-perceived health status was categorized into 2 levels: excellent or very good health status vs. lower levels of perception; years of experience as a community nurse were split into 3 groups: <5 years, 5–9.9 years and > =10 years; self-perceived stress levels were split into tertiles and highest tertile was used to define the variable high levels of stress.
Normal distribution was tested using the Kolmogorov-Smirnoff test. Mean and standard deviation (SD) were used to present continuous variables. Absolute and relative frequencies were used for categorical variables. Statistical significance was determined by a p-value < 0.05. To compare means, ANOVA with Sidak correction was utilized. To compare proportions, the Mann–Whitney test was used for the comparison of 2 factors, and the Kruskal–Wallis test was used for the comparison of 3 factors. Bonferroni correction was used to assess the statistical significance when multiple Mann–Whitney tests were applied. Demographic and nutritional intake quality data, including LCD score and intuitive eating score, were used in a regression analysis model to determine the association with the presence of at least a chronic disease diagnosis established by a physician.
Out of the sample, the majority were females, making 95.1% (749). The largest age group in the sample was 40–49.9 years old, consisting of 380 individuals (48.2%). A significant proportion of the nurses, 36.5% had worked as community nurses for more than 10 years, while 32.7% had worked between 5–9.9 years. The mean age of the whole group was 43.4 years with a standard deviation of 7.8 years, ranging from 22 to 65 years old. On average, the group had worked as community nurses for 8 years, ranging from 0 to 22 years (Table 1).
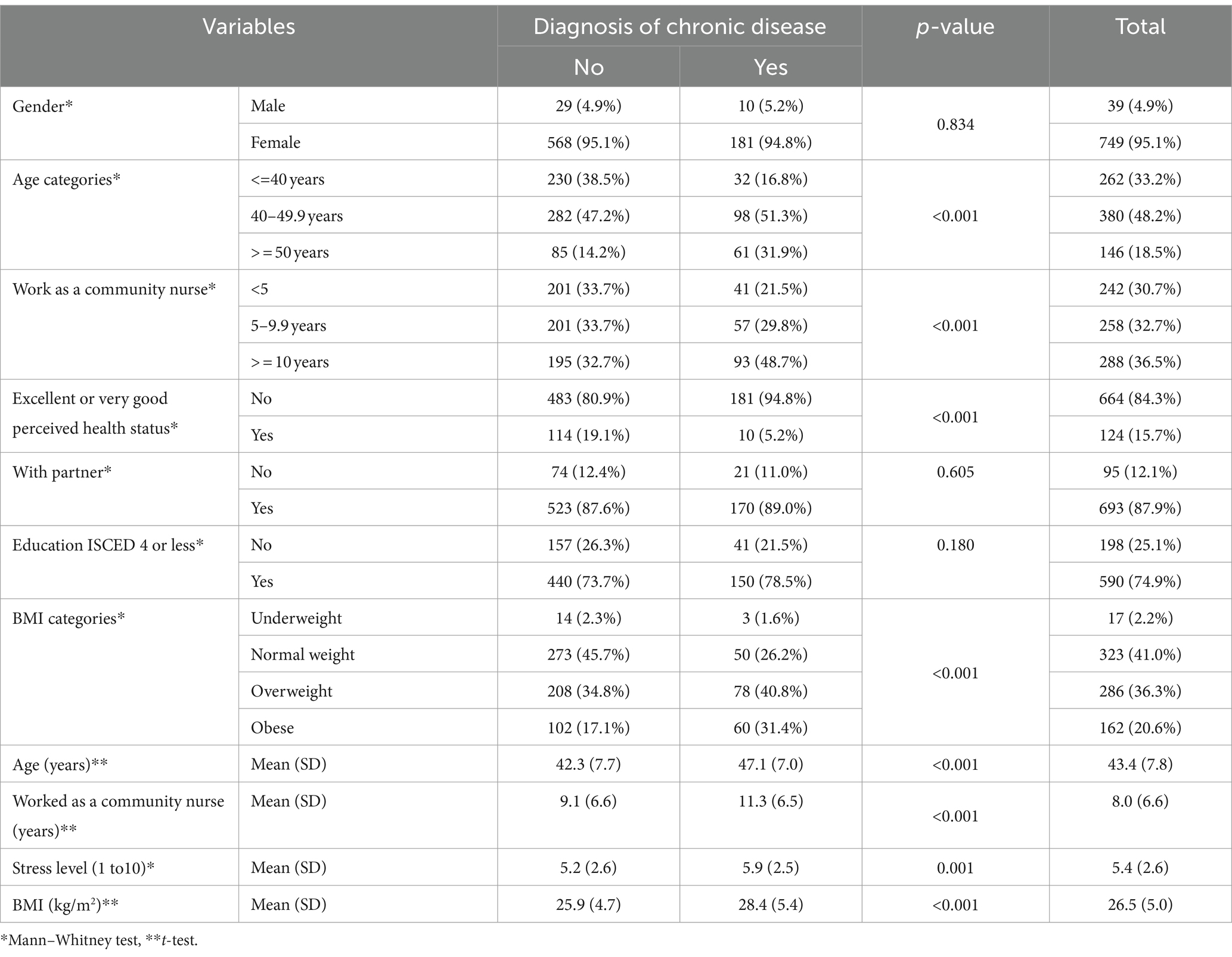
Table 1. Descriptive statistics of the sample of community nurses per presence of a diagnosis of chronic disease and total (N = 788).
Regarding personal status and education, most of the nurses were in a relationship, comprising 87.9% or 693 individuals, and 74.9% had obtained at most an ISCED 4 diploma. Only 15.7% or 124 individuals reported an excellent or very good perceived health status. The mean BMI of the group was 26.5 kg/m2. Among the participants, 36.3% were overweight, 20.6% were classified as obese, 2.2% were underweight and 41.0% had a normal weight (Table 1). Using the presence/absence of chronic disease as a factor, no significant differences were found between the different categories in the following variables: gender (p = 0.834), social status (p = 0.605), and education level (p = 0.180). However, the group with the chronic disease did exhibit higher age [47.1 (7.0) vs. 42.3 (7.7)] and experience as community nurses [11.3 (6.5) vs. 9.1 (6.6)], than those without chronic disease. Additionally, the group with chronic diseases reported greater stress levels and perceived their health status to be lower. In terms of nutrition status, those with chronic disease had a higher reported BMI of 28.4 (5.4) kg/m2, than those without chronic disease which had a mean of 25.9 (4.7) kg/m2, the difference being significant (Table 1).
In terms of chronic diseases, 24.9% or 191 individuals reported having at least one diagnosed by a physician. Among all community nurses, 16.5% had one chronic disease, 4.6% had two, and 3.2% had three or more. The community nurses reported several diagnoses of chronic diseases, with hypertension being the most prevalent at 9.8% (77 cases). This was followed by obesity at 4.4% (35 cases), thyroid diseases at 3.8% (30 cases), and dyslipidemia at 3.7% (29 cases). Type II diabetes had a prevalence of 2.2% with 17 cases, while heart failure and ischemic heart disease recorded 1.9% (15 cases) and 1.6% (13 cases) point prevalence, respectively. Asthma had a point prevalence of 1.4% (11 cases), while other diseases had significantly lower point prevalence (data not shown).
In regards to chronic disease treatment, it is noteworthy that only 22 out of 191 individuals (11.5%) who reported a chronic condition did not adhere to their prescribed treatment plan. Interestingly, all of these non-adherers reported only a single chronic condition. Additionally, it is worth mentioning that for both heart failure and ischemic heart disease, all patients followed their prescribed treatment plan.
The mean (SD) LCD score was 16.5 (6.8) with a range from a minimum of 3 and a maximum of 29 points. The mean (SD) IES-2 score, on the other hand, was 3.3 (0.3), ranging from a minimum of 1.91 to a maximum of 4.13 points. Energy intake ranged from a minimum of 808.0 kcal to a maximum of 3772.2 kcal, with a mean and a standard deviation of 1917.9 (612.6) kcal. In terms of EFSA’s recommended intake, 481 individuals, or 61%, meet the suggested proportion of carbohydrate intake, while 56.6% of the overall group meet the recommended proportion of fat intake. However, it’s worth noting that 18.8% of the group, or 148 individuals, have a low intake of carbohydrates, while 20.2% of the group, or 159 individuals, have a high intake of carbohydrates. Additionally, 43.4% of the group have a high intake of fat.
Based on the LCD score tertiles, the medium carbohydrate intake group shows a significantly higher IES-2 score (p < 0.001), but only when compared to the high carbohydrate group. Additionally, the medium carbohydrate group features the highest proportions of EFSA recommended carbohydrate intake, while the high carbohydrate group has the highest proportion of recommended fat intake (p < 0.001). Those in the high carbohydrate intake group have a higher prevalence of chronic diseases (p = 0.001), while those in the low carbohydrate intake group have a higher prevalence of excellent or very good perceived health status (p = 0.002). It’s worth noting that education level (p = 0.649), high-stress level (p = 0.127), total energy intake (p = 0.960), age (p = 0.227), experience as a community nurse (p = 0.568), and BMI (p = 0.983) are not influenced by the tertiles of LCD score (Table 2).
When dividing participants into tertiles based on their IES-2 scores, we found that the recommended carbohydrate intake proportions were similar across all groups (p = 0.331). However, those who achieved the recommended fat intake were more prevalent in the top tertile of intuitive eating (p = 0.045). Furthermore, individuals in the highest tertile tended to perceive their health status as excellent or very good (p < 0.001), had greater experience as a community nurse (p = 0.003), were older (p = 0.002), had a lower BMI (p < 0.001) and had lower energy intake (p < 0.001) than those in the lower tertiles. The presence of chronic disease, level of education, and high-stress levels remained consistent across all IES-2 tertiles (Table 3).
We used a prediction model to analyze the connection between demographic variables, IES-2, and LCD score concerning the diagnosis of at least one chronic disease, set by a physician. Table 4 displays the OR and 95% confidence intervals of each predictor fitted in the model. Our findings indicate that a low level of perceived health status has the strongest association with the presence of diagnosis of chronic diseases, with an OR of 3.388, 95%CI 1.684–6.814, compared to those reporting excellent or very good perceived health status. High stress has an OR of 1.483, 95%CI 1.033–2.129. BMI had an OR of 1.069, 95%CI 1.032–1.108, while LCD score had an OR of 0.956, 95%CI 0.920–0.992. While other social demographic factors did not significantly contribute to the model, they were still taken into account (Table 4).
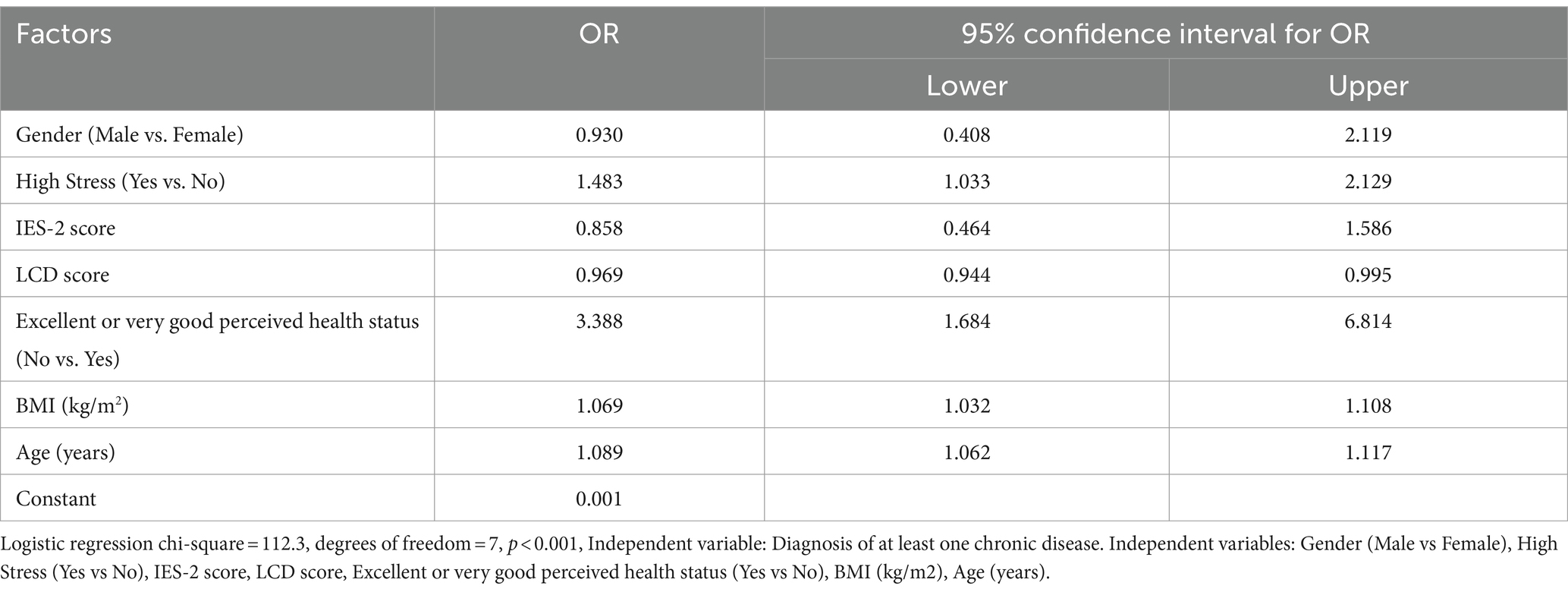
Table 4. Prediction model for the association of demographic and eating habits to the presence of a diagnosis of chronic disease (N = 788).
To the best of our knowledge, this is the first study to shed light on the eating habits concerning chronic diseases in community nurses from Romania. This assessment is important for future programs targeting improvement in eating habits in community nurses, with personal benefits, but also for their patients’ benefits, because being able to provide nutrition screening and appropriate nutrition advice is essential to improve healthy eating and subsequent health outcomes of their patients.
The trend of chronic diseases in Europe is marked by a significant rise in prevalence, posing substantial challenges to healthcare systems. Lifestyle factors, including sedentary behavior and poor dietary habits, contribute to the increasing burden of diseases such as diabetes, cardiovascular conditions, and obesity. Aging populations further amplify this trend, as chronic diseases are often more prevalent in older demographics (19, 20). In our analysis, we found that among individuals with an age range from 22 to 65 years, the point prevalence of any chronic disease was 24.2%, and for those with more than two chronic diseases, it was 7.8%.
This increase in multimorbidity among adults under the age of 65 challenges the traditional perception that chronic conditions primarily affect older populations. Overall, the prevalence of multimorbidity across Europe is estimated to be 39.2% with a 95% confidence interval of 33.2–45.2%, with higher prevalences in Europe in women 43.4% (24.8–50.0), compared to men 37.4% (31.7–55.1) (21). The burden of multimorbidity not only impacts individual well-being but also poses significant challenges to healthcare systems in terms of management and resource allocation (21, 22).
According to our study, the predictive model for the association between demographics and eating habits with chronic disease diagnosis found that individuals diagnosed with chronic disease tend to experience higher levels of stress, perceive their health status as poor, have an older age and higher BMI, and consume more carbohydrates compared to those without a diagnosis.
Individuals diagnosed with chronic conditions often report a lower perceived health status, reflecting the multifaceted impact of these conditions on well-being. The psychological and emotional burden associated with chronic diseases can contribute to a negative perception of overall health (23). Conversely, those with a positive perception of health may exhibit better coping mechanisms and adherence to healthcare recommendations. Understanding the interplay between chronic diseases and subjective health assessments is crucial for comprehensive health management and targeted interventions (24).
While age is not a modifiable factor, factors such as high levels of stress, high BMI, and low food intake quality can be improved. Incorporating mindfulness practices, like meditation and deep breathing exercises, can effectively reduce stress levels, promoting mental well-being (25, 26). The management of BMI can include practicing a regular exercise routine, including both aerobic and strength-training exercises, which are a key strategy for promoting weight loss and improving overall physical health (27). Interventions providing education plus personalized advice and feedback empower individuals to make healthier food choices, emphasizing a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to enhance overall food quality (28). Behavioral interventions, such as goal-setting and self-monitoring, can foster sustainable lifestyle changes, aiding in stress reduction, BMI management, and the adoption of healthier eating habits (1). Systemic interventions to improve walkability, access to healthy food and sport facilities are equally important (29).
Our investigation of the eating habits of community nurses analyzed both the quality of their food intake using the Low Carbohydrate Diet (LCD) score, which is a score based on deciles of macronutrients, as well as their intuitive eating habits with the Intuitive Eating Score 2 (IES-2) index. Our findings revealed that community nurses with a high carbohydrate intake had a much higher prevalence of chronic disease (45.0%) compared to those in the middle (27.7%) and low carbohydrate diet tertiles (27.2%), but no effect was found between LCD score and BMI.
Low-carbohydrate diets have gained popularity due to their effectiveness in achieving short-term weight loss, which is further enhanced when coupled with high-protein diets (30, 31). However, recent studies have yielded inconsistent findings regarding their long-term impact on diabetes (32, 33). Though useful and popular for short-term weight loss and short-term reduction in cardiovascular risk factors (34), diets low in carbohydrates and high in fat, especially saturated fat put a supplementary risk for all-cause mortality (33–35). On the other hand, increased consumption of dietary carbohydrate intake is associated with an increased risk of cardiovascular disease, the risk increasing by 1.02 times for every 5% rise in dietary carbohydrate consumption (36). The ARIC cohort showed a U-shaped all-cause mortality, with the lowest risk of mortality in diets with 50–55% energy from carbohydrates (37). The source of fat and protein further modulated the increased mortality in high and low percentages of energy from carbohydrates, with plant sources having a protective effect and animal-derived fat or protein having a detrimental effect on all-cause mortality (37).
Intuitive eating is a holistic approach to nutrition that prioritizes one’s body cues over external diet rules. By listening to and trusting internal signals, such as hunger and fullness, one can develop a mindful and non-restrictive relationship with food that promotes overall well-being and a healthier relationship with eating. Recent meta-analyses have found that those who practice intuitive eating tend to have a lower BMI (38) and a higher quality diet (39). In our study, higher levels of intuitive eating were linked to lower BMI levels and lower energy intake and higher percentage of adequate intake of fat. We discovered that nurses in the highest tertile of intuitive eating had significantly lower BMI values of 25.26 (4.37), compared to those in the lowest tertile of intuitive eating, who had BMI values of 27.40 (5.26). Additionally, energy intake was found to be associated with tertiles of intuitive eating score, with the highest tertile of intuitive eating being linked to lower energy intake with a mean of 1773.0 (566.4) kcal when compared to other tertiles 2008.1 (623.7) kcal, respective 1959.8 (620.3) kcal.
Our research has shown that community nurses with more age and experience tend to have higher intuitive scores. This may be attributed to the fact that as individuals age, they develop a greater understanding of their body and personal preferences, leading to a more refined and knowledgeable approach to intuitive eating. The principles of intuitive eating are in line with mindfulness techniques, which encourage individuals to be fully present and aware of their eating habits (40). Our investigation did not uncover any previous studies utilizing the Intuitive Eating Scale 2 (IES-2) specifically among nurses.
Nurses often experience high levels of occupational stress due to demanding workloads, long hours, and the emotionally charged nature of their profession, impacting their mental well-being and work performance (41, 42). Chronic stress triggers physiological responses that can contribute to the development and exacerbation of chronic diseases, including cardiovascular conditions and metabolic disorders (43, 44). Stress often influences unhealthy coping behaviors, such as poor dietary choices and lack of exercise, which are linked to the development of chronic conditions like obesity and diabetes (43, 45). The interplay between chronic stress and chronic diseases forms a complex cycle, where stress exacerbates the conditions, and the presence of chronic diseases can, in turn, amplify stress levels, highlighting the importance of holistic approaches to health management (44).
The Body Mass Index (BMI) analysis in Europe reveals an increasing prevalence of overweight and obesity across diverse populations (46, 47). Elevated BMI is closely linked to the rising incidence of chronic diseases, including diabetes, cardiovascular conditions, and certain cancers. The NCD Risk Factor Collaboration reports a mean BMI of 27.3 (26.3–27.7) kg/m2 for Romania, which is comparable to our sample’s BMI of 26.5 (5.0) kg/m2. The prevalence of obesity in the community nurse cohort, measured by weight and height, is 20.6% and the prevalence of combined overweight and obesity is 56.9%, consistent with other estimates (48). There is a significant difference in the prevalence of the diagnosis of obesity reported by nurses in the chronic diseases section of just 4.4% and the prevalence obtained from measurements of 20.6%. The missed diagnosis of obesity remains a prevalent concern in healthcare, as it often goes unrecognized due to societal misconceptions and biases. Healthcare providers may not consistently assess or address obesity during routine examinations, leading to underdiagnosis in both adult and child populations (49–51). The consequences of missed obesity diagnoses include delayed intervention and increased risk for associated health conditions such as diabetes, cardiovascular diseases, and mental health issues (52, 53).
According to our study, hypertension exhibited the highest point prevalence (9.8%) among chronic reported diseases. The prevalence of hypertension (in males and females) has doubled worldwide between 1990 and 2019 (54). According to the same review (54), in Romania, the prevalence of hypertension is 43.9% (with 95% CI 35.1–52.8) with a detection awareness of 74.6% (with 95%CI 61.8–85.4). The alarming increase in hypertension diagnosis highlights an unsettling trend in multimorbidity. Hypertension frequently acts, along with heart diseases, and diabetes, as a primary contributor in later multimorbidity (55).
Treatment non-adherence in our group was 11.5% of all patients with a chronic disease. Non-adherence to treatment poses a significant risk to multimorbidity, as individuals with chronic conditions may experience worsening health outcomes when failing to follow prescribed medical plans. The complex interplay of multiple chronic diseases can exacerbate if treatments are not consistently adhered to, leading to increased morbidity and complications (56, 57). Poor adherence to medication regimens, lifestyle modifications, and regular health check-ups may contribute to the progression and development of additional chronic conditions. Addressing non-adherence is crucial in preventing the cascade of health issues associated with multimorbidity, highlighting the importance of patient education, support systems, and healthcare interventions to promote treatment compliance (1, 55).
Our study has certain limitations, such as self-reporting bias and selection bias. The self-reported bias pertains not only to the nutrition evaluation, but also to the reported diagnosis of chronic disease. It is important to note that the design of this study was cross sectional, which means that no causality can be established between eating patterns and the presence of chronic diseases. Instead, the findings can only be interpreted as associations. Although the response rate of our study was good, it is common knowledge that individuals who participate in nutrition studies are typically more interested in nutrition and healthy living than those who do not participate. There is a predominantly female cohort, however this is concordant with the prevalence of female community nurses in Romania.
The present study on the eating habits and health profiles of community nurses in Romania provides comprehensive insights, which may serve as a foundation for future research endeavors. Given the findings of this study, several key areas warrant further attention. Longitudinal studies could clarify on the dynamic nature of dietary patterns, stress levels, and chronic disease diagnoses among nurses over time, thereby facilitating a deeper understanding of their interchange. Moreover, comparative research across diverse healthcare settings and regions could provide valuable insights into the factors influencing these outcomes.
Additionally, intervention studies targeting modifiable factors identified in this research, such as stress reduction techniques, healthy weight management strategies, and nutritional education programs, could be explored to assess their effectiveness in promoting overall well-being among healthcare professionals. Such research would not only benefit the healthcare professionals but also the patients they serve. It is widely acknowledged that the health of healthcare professionals is directly linked to the quality of care that patients receive, and therefore, interventions that improve the health and well-being of healthcare professionals can have a positive impact on patient outcomes (58, 59).
Lastly, collaborative efforts between healthcare institutions, policymakers, and researchers are essential to develop and implement tailored programs that prioritize the health and resilience of nurses, thereby contributing to the mitigation of the burden of chronic diseases within healthcare systems. The implementation of such programs would require a concerted effort and the development of strategies that are feasible, sustainable, and evidence-based. Overall, these research endeavors can contribute significantly to the advancement of knowledge in this field and ultimately lead to positive health outcomes for healthcare professionals and patients alike.
This study provides a comprehensive insight into the eating habits and health profiles of community nurses in Romania, uncovering noteworthy associations between dietary patterns, stress levels, and chronic disease diagnoses. The prevalence of chronic diseases among this population, particularly hypertension, underscores the importance of targeted interventions for healthcare professionals. Notably, the study identifies modifiable factors, including stress, BMI, and dietary habits based on high carbohydrate diets, offering potential avenues for personalized health interventions. The findings emphasize the need for holistic strategies, encompassing stress reduction, healthy weight management, and nutritional education to enhance overall well-being. As healthcare systems struggle with the increasing burden of chronic diseases, these insights contribute to the development of tailored programs that prioritize the health and resilience of healthcare providers.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Research Ethics Committee of Victor Babes University of Medicine and Pharmacy. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
L-MO: Conceptualization, Investigation, Writing – original draft, Methodology. MP: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. AC-E: Conceptualization, Data curation, Methodology, Writing – review & editing. CS: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors want to thank the community nurses who provided an answer to the survey for their invaluable contribution and commitment to advancing healthcare knowledge.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Guerreiro, MP, Brito Félix, I, and Moreira Marques, M. A practical guide on behaviour change support for self-managing chronic disease. Cham: Springer International Publishing (2023).
2. Jayedi, A, Soltani, S, Abdolshahi, A, and Shab-Bidar, S. Healthy and unhealthy dietary patterns and the risk of chronic disease: an umbrella review of meta-analyses of prospective cohort studies. Br J Nutr. (2020) 124:1133–44. doi: 10.1017/S0007114520002330
3. Pan, B, Wu, Y, Yang, Q, Ge, L, Gao, C, Xun, Y, et al. The impact of major dietary patterns on glycemic control, cardiovascular risk factors, and weight loss in patients with type 2 diabetes: a network meta-analysis. J Evid-Based Med. (2019) 12:29–39. doi: 10.1111/jebm.12312
4. English, LK, Ard, JD, Bailey, RL, Bates, M, Bazzano, LA, Boushey, CJ, et al. Evaluation of dietary patterns and all-cause mortality: A systematic review. JAMA Netw Open. (2021) 4:e2122277. doi: 10.1001/jamanetworkopen.2021.22277
5. Stephen, C, McInnes, S, and Halcomb, E. The feasibility and acceptability of nurse-led chronic disease management interventions in primary care: an integrative review. J Adv Nurs. (2018) 74:279–88. doi: 10.1111/jan.13450
6. Wagner, EH . The role of patient care teams in chronic disease management. BMJ. (2000) 320:569–72. doi: 10.1136/bmj.320.7234.569
7. Swanson, M, Wong, ST, Martin-Misener, R, and Browne, AJ. The role of registered nurses in primary care and public health collaboration: a scoping review. Nurs Open. (2020) 7:1197–07. doi: 10.1002/nop2.496
8. Iriarte-Roteta, A, Lopez-Dicastillo, O, Mujika, A, Ruiz-Zaldibar, C, Hernantes, N, Bermejo-Martins, E, et al. Nurses’ role in health promotion and prevention: a critical interpretive synthesis. J Clin Nurs. (2020) 29:3937–49. doi: 10.1111/jocn.15441
9. Marko, S, Wylie, S, and Utter, J. Enablers and barriers to healthy eating among hospital nurses: a systematic review. Int J Nurs Stud. (2023) 138:104412. doi: 10.1016/j.ijnurstu.2022.104412
10. Haftenberger, M, Heuer, T, Heidemann, C, Kube, F, Krems, C, and Mensink, GB. Relative validation of a food frequency questionnaire for national health and nutrition monitoring. Nutr J. (2010) 9:36. doi: 10.1186/1475-2891-9-36
11. Serban, CL, Banu, AM, Putnoky, S, Butica, SI, Niculescu, MD, and Putnoky, S. Relative validation of a four weeks retrospective food frequency questionnaire versus 7-day paper-based food Records in Estimating the intake of energy and nutrients in adults. Nutr Diet Suppl [Internet]. (2021). doi: 10.2147/NDS.S310260
12. Nutrition C for FS and A . Guidance for industry: guidelines for determining metric equivalents of household measures. FDA (2023) Available at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-guidelines-determining-metric-equivalents-household-measures
13. de Koning, L, Fung, TT, Liao, X, Chiuve, SE, Rimm, EB, Willett, WC, et al. Low-carbohydrate diet scores and risk of type 2 diabetes in men 123. Am J Clin Nutr. (2011) 93:844–50. doi: 10.3945/ajcn.110.004333
14. Halton, TL, Willett, WC, Liu, S, Manson, JE, Albert, CM, Rexrode, K, et al. Low-carbohydrate-diet score and the risk of coronary heart disease in women. N Engl J Med. (2006) 355:1991–02. doi: 10.1056/NEJMoa055317
15. EFSA (European Food Safety Authority) . Dietary reference values for nutrients: summary report. EFSA Supp Publ. (2017) 14:92, e15121. doi: 10.2903/sp.efsa.2017.e15121
16. Tylka, TL, and Kroon Van Diest, AM. The intuitive eating Scale-2: item refinement and psychometric evaluation with college women and men. J Couns Psychol. (2013) 60:137–53. doi: 10.1037/a0030893
17. Vintilă, M, Todd, J, Goian, C, Tudorel, O, Barbat, CA, and Swami, V. The Romanian version of the intuitive eating Scale-2: assessment of its psychometric properties and gender invariance in Romanian adults. Body Image. (2020) 35:225–36. doi: 10.1016/j.bodyim.2020.09.009
18. International Standard Classification of Education (ISCED) Available at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=International_Standard_Classification_of_Education_(ISCED) (Accessed December 30, 2023).
19. Brennan, P, Perola, M, van Ommen, GJ, and Riboli, E. Chronic disease research in Europe and the need for integrated population cohorts. Eur J Epidemiol. (2017) 32:741–9. doi: 10.1007/s10654-017-0315-2
20. Hajat, C, and Stein, E. The global burden of multiple chronic conditions: a narrative review. Prev Med Rep. (2018) 12:284–93. doi: 10.1016/j.pmedr.2018.10.008
21. Chowdhury, SR, Das, DC, Sunna, TC, Beyene, J, and Hossain, A. Global and regional prevalence of multimorbidity in the adult population in community settings: a systematic review and meta-analysis. eClinicalMed. (2023) 57:101860. doi: 10.1016/j.eclinm.2023.101860
22. Marengoni, A, Angleman, S, Melis, R, Mangialasche, F, Karp, A, Garmen, A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. (2011) 10:430–9. doi: 10.1016/j.arr.2011.03.003
23. Axon, DR, Jang, A, Son, L, and Pham, T. Determining the association of perceived health status among United States older adults with self-reported pain. Aging Health Res. (2022) 2:100051. doi: 10.1016/j.ahr.2021.100051
24. Cheng, C, Inder, K, and Chan, SWC. Coping with multiple chronic conditions: an integrative review. Nurs Health Sci. (2020) 22:486–97. doi: 10.1111/nhs.12695
25. Geiger, C, Cramer, H, Dobos, G, and Kohl-Heckl, WK. A systematic review and meta-analysis of mindfulness-based stress reduction for arterial hypertension. J Hum Hypertens. (2023) 37:161–9. doi: 10.1038/s41371-022-00764-z
26. David Creswell, J, Lindsay, EK, Villalba, DK, and Chin, B. Mindfulness training and physical health: mechanisms and outcomes. Psychosom Med. (2019) 81:224–32. doi: 10.1097/PSY.0000000000000675
27. LeBlanc, ES, Patnode, CD, Webber, EM, Redmond, N, Rushkin, M, and O’Connor, EA. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: updated evidence report and systematic review for the US preventive services task force. JAMA. (2018) 320:1172–91. doi: 10.1001/jama.2018.7777
28. Whatnall, MC, Patterson, AJ, Ashton, LM, and Hutchesson, MJ. Effectiveness of brief nutrition interventions on dietary behaviours in adults: a systematic review. Appetite. (2018) 120:335–47. doi: 10.1016/j.appet.2017.09.017
29. Jiang, Q, Forseth, B, Fitzpatrick, L, Laroche, HH, Hampl, S, Davis, AM, et al. Prospective associations of neighborhood healthy food access and walkability with weight status in a regional pediatric health system. Int J Behav Nutr Phys Act. (2023) 20:113. doi: 10.1186/s12966-023-01514-1
30. Maula, A, Kai, J, Woolley, AK, Weng, S, Dhalwani, N, Griffiths, FE, et al. Educational weight loss interventions in obese and overweight adults with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabet Med. (2020) 37:623–35. doi: 10.1111/dme.14193
31. Clifton, PM, Condo, D, and Keogh, JB. Long term weight maintenance after advice to consume low carbohydrate, higher protein diets – A systematic review and meta analysis. Nutr Metab Cardiovasc Dis. (2014) 24:224–35. doi: 10.1016/j.numecd.2013.11.006
32. Huntriss, R, Campbell, M, and Bedwell, C. The interpretation and effect of a low-carbohydrate diet in the management of type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr. (2018) 72:311–25. doi: 10.1038/s41430-017-0019-4
33. Churuangsuk, C, Lean, MEJ, and Combet, E. Low and reduced carbohydrate diets: challenges and opportunities for type 2 diabetes management and prevention. Proc Nutr Soc. (2020) 79:498–13. doi: 10.1017/S0029665120000105
34. Qin, P, Suo, X, Chen, S, Huang, C, Wen, W, Lin, X, et al. Low-carbohydrate diet and risk of cardiovascular disease, cardiovascular and all-cause mortality: a systematic review and meta-analysis of cohort studies. Food Funct. (2023) 14:8678–91. doi: 10.1039/D3FO01374J
35. Noto, H, Goto, A, Tsujimoto, T, and Noda, M. Low-carbohydrate diets and all-cause mortality: a systematic review and Meta-analysis of observational studies. PLoS One. (2013) 8:e55030. doi: 10.1371/journal.pone.0055030
36. Qin, P, Huang, C, Jiang, B, Wang, X, Yang, Y, Ma, J, et al. Dietary carbohydrate quantity and quality and risk of cardiovascular disease, all-cause, cardiovascular and cancer mortality: a systematic review and meta-analysis. Clin Nutr. (2023) 42:148–65. doi: 10.1016/j.clnu.2022.12.010
37. Seidelmann, SB, Claggett, B, Cheng, S, Henglin, M, Shah, A, Steffen, LM, et al. Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. Lancet Public Health. (2018) 3:e419–28. doi: 10.1016/S2468-2667(18)30135-X
38. Van Dyke, N, and Drinkwater, EJ. Review article relationships between intuitive eating and health indicators: literature review. Public Health Nutr. (2014) 17:1757–66. doi: 10.1017/S1368980013002139
39. Hensley-Hackett, K, Bosker, J, Keefe, A, Reidlinger, D, Warner, M, D’Arcy, A, et al. Intuitive eating intervention and diet quality in adults: a systematic literature review. J Nutr Educ Behav. (2022) 54:1099–15. doi: 10.1016/j.jneb.2022.08.008
40. Serban, DM, Serban, CL, Ursoniu, S, Putnoky, S, Moleriu, RD, and Putnoky, S. Mindful eating questionnaire: validation and reliability in Romanian adults. Int J Environ Res Public Health. (2022) 19:10517. doi: 10.3390/ijerph191710517
41. Khamisa, N, Peltzer, K, Ilic, D, and Oldenburg, B. Work related stress, burnout, job satisfaction and general health of nurses: a follow-up study. Int J Nurs Pract. (2016) 22:538–45. doi: 10.1111/ijn.12455
42. Sarafis, P, Rousaki, E, Tsounis, A, Malliarou, M, Lahana, L, Bamidis, P, et al. The impact of occupational stress on nurses’ caring behaviors and their health related quality of life. BMC Nurs. (2016) 15:56. doi: 10.1186/s12912-016-0178-y
43. Agorastos, A, and Chrousos, GP. The neuroendocrinology of stress: the stress-related continuum of chronic disease development. Mol Psychiatry. (2022) 27:502–13. doi: 10.1038/s41380-021-01224-9
44. Kivimäki, M, and Steptoe, A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol. (2018) 15:215–29. doi: 10.1038/nrcardio.2017.189
45. Hill, D, Conner, M, Clancy, F, Moss, R, Wilding, S, Bristow, M, et al. Stress and eating behaviours in healthy adults: a systematic review and meta-analysis. Health Psychol Rev. (2022) 16:280–04. doi: 10.1080/17437199.2021.1923406
46. Stival, C, Lugo, A, Odone, A, van den Brandt, PA, Fernandez, E, Tigova, O, et al. Prevalence and correlates of overweight and obesity in 12 European countries in 2017–2018. Obes Facts. (2022) 15:655–65. doi: 10.1159/000525792
47. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. (2016) 387:1377–96. doi: 10.1016/S0140-6736(16)30054-X
48. Overweight and obesity BMI statistics. Available at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Overweight_and_obesity_-_BMI_statistics (Accessed December 30, 2023).
49. Kim, EG, and Kaelber, DC. Phenotypic prevalence of obesity and metabolic syndrome among an underdiagnosed and underscreened population of over 50 million children and adults. Front Genet. (2022) 13:961116. doi: 10.3389/fgene.2022.961116
50. Kapoor, A, Kim, J, Zeng, X, Harris, ST, and Anderson, A. Weighing the odds: assessing underdiagnosis of adult obesity via electronic medical record problem list omissions. Digit Health. (2020) 6:91871. doi: 10.1177/2055207620918715
51. Lydecker, JA, and Grilo, CM. The missed diagnosis and Mis-diagnosis of pediatric obesity. Psychother Psychosom. (2017) 86:173–4. doi: 10.1159/000452501
52. Valenzuela, PL, Carrera-Bastos, P, Castillo-García, A, Lieberman, DE, Santos-Lozano, A, and Lucia, A. Obesity and the risk of cardiometabolic diseases. Nat Rev Cardiol. (2023) 20:475–94. doi: 10.1038/s41569-023-00847-5
53. Safaei, M, Sundararajan, EA, Driss, M, Boulila, W, and Shapi’i, A. A systematic literature review on obesity: understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput Biol Med. (2021) 136:104754. doi: 10.1016/j.compbiomed.2021.104754
54. Zhou, B, Carrillo-Larco, RM, Danaei, G, Riley, LM, Paciorek, CJ, Stevens, GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. (2021) 398:957–80. doi: 10.1016/S0140-6736(21)01330-1
55. Kudesia, P, Salimarouny, B, Stanley, M, Fortin, M, Stewart, M, Terry, A, et al. The incidence of multimorbidity and patterns in accumulation of chronic conditions: a systematic review. J Multimorb Comorbidity. (2021) 11:10328. doi: 10.1177/26335565211032880
56. Tazzeo, C, Zucchelli, A, Vetrano, DL, Demurtas, J, Smith, L, Schoene, D, et al. Risk factors for multimorbidity in adulthood: a systematic review. Ageing Res Rev. (2023) 91:102039. doi: 10.1016/j.arr.2023.102039
57. Foley, L, Larkin, J, Lombard-Vance, R, Murphy, AW, Hynes, L, Galvin, E, et al. Prevalence and predictors of medication non-adherence among people living with multimorbidity: a systematic review and meta-analysis. BMJ Open. (2021) 11:e044987. doi: 10.1136/bmjopen-2020-044987
58. Oberg, E, and Frank, E. Physicians’ health practices strongly influence patient health practices. J R Coll Physicians Edinb. (2009) 39:290–1. doi: 10.4997/JRCPE.2009.422
Keywords: chronic diseases, non-communicable diseases, community nurses, eating behavior, high carbohydrate diet, low carbohydrate diet score, intuitive eating
Citation: Onofrei L-M, Puiu M, Chirita-Emandi A and Serban CL (2024) A comprehensive analysis concerning eating behavior associated with chronic diseases among Romanian community nurses. Front. Public Health. 12:1368069. doi: 10.3389/fpubh.2024.1368069
Received: 09 January 2024; Accepted: 11 March 2024;
Published: 21 March 2024.
Edited by:
Alejandro Galán-Mercant, University of Cádiz, SpainReviewed by:
Aureliusz Kosendiak, Wroclaw Medical University, PolandCopyright © 2024 Onofrei, Puiu, Chirita-Emandi and Serban. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Puiu, bWFyaWFfcHVpdUB1bWZ0LnJv
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.