- 1Department of Rehabilitation Medicine, The Second Hospital of Jilin University, Chang Chun, China
- 2School of Nursing, Jilin University, Chang Chun, China
Background: Home-based exercise (HBE) represents an alternative to increase the accessibility of rehabilitation programs and relieve the burden on the health care system for people with knee osteoarthritis.
Objectives: To summarize for the first time the effectiveness of HBE as compared to center-based exercise (CBE), both with and without HBE, on patient-reported and performance-based outcomes in people with KOA.
Methods: Searches were conducted on PubMed, Cochrane, Embase, Web of Science, and Scopus until March 10, 2023, without date or language restrictions. Randomized controlled trials investigating HBE versus CBE or HBE combined with CBE for people with KOA were eligible. The primary outcomes were patient-reported: pain, physical disability, and quality of life. The secondary outcomes were performance-based: walking ability, lower limb muscle strength, and balance function. Risk of bias was assessed with the Cochrane Risk of Bias tool and quality of evidence according to the GRADE.
Results: Eleven trials involving 956 participants were included. There was no difference in short-term pain (SMD, 0.22 [95% CI, −0.04 to 0.47], p = 0.09; I2 = 0%), physical disability (SMD, 0.17 [95% CI, −0.19 to 0.54], p = 0.35; I2 = 0%), walking ability (SMD, −0.21 [95% CI, −0.64 to 0.22], p = 0.33; I2 = 35%) and lower limb muscle strength (SMD, −0.24 [95% CI, −0.88 to 0.41], p = 0.47; I2 = 69%) between HBE and CBE. HBE combined with CBE has better benefits compared with HBE alone in short-term pain (SMD, 0.89 [95% CI, 0.60 to 1.17], p < 0.001; I2 = 11%) and physical disability (SMD, 0.25 [95% CI, 0.00 to 0.50], p = 0.05; I2 = 0%).
Conclusion: Based on limited evidence, HBE is as effective as CBE on short-term pain, physical disability, walking ability, and lower limb muscle strength in people with knee osteoarthritis. Furthermore, combining HBE with CBE may enhance the overall efficacy of the intervention.
Systematic review registration: PROSPERO, CRD42023416548.
1 Introduction
Knee osteoarthritis (KOA) is a chronic degenerative condition that involves the entire joint, including bone, synovium, and capsule, with an estimated 240 million persons suffering symptomatic and activity-limiting OA worldwide (1). Nearly 30% of individuals over 45 years old have radiographic evidence of KOA, with about half suffering knee symptoms (2, 3). To minimize the rising social and personal costs of KOA, interventions that alleviate symptoms and reduce prevalence through primary and secondary prevention programs are essential.
In recent years, a shift from pharmacologic therapy to nonpharmacologic therapy has occurred due to the limited efficacy of the former and mounting evidence indicating that nonpharmacologic modalities have superior long-term symptom relief and can delay or prevent functional decline for KOA. Among nonpharmacologic therapy, both center-based exercise (CBE) and home-based exercise (HBE) have been found to reduce pain and improve function in people with KOA compared to no intervention or usual care (4–8). HBE refers to exercise that takes place in an informal and flexible setting, generally in patients’ homes (9, 10), which offers a sense of familiarity within one’s surroundings, providing comfort and accessibility while also reducing costs, environmental challenges, and travel time to a healthcare center (11–14). Therefore, HBE represents an alternative to increase the accessibility of exercise programs and relieve the burden on the health care system (12–15). Nevertheless, the comparative effectiveness between HBE and CBE for KOA is debated.
A succession of systematic reviews has demonstrated that HBE is almost as effective as CBE for multiple conditions, such as cardiovascular diseases (16–20), Parkinson’s disease (21), and old healthy people (11, 22, 23). A previous review (24) attempted to investigate the effects of mixed home-based rehabilitation in people with KOA, not the effects of HBE, and the results were inconclusive. In addition, several clinical trials have been designed to determine whether supplementing HBE with CBE enhances its efficacy, but the results have been mixed (25–27). Despite these findings, there is yet been no evidence-based clinical practice guideline promoting the use of home-based exercise for KOA, therefore a rigorous systematic review with meta-analysis of the current high-quality evidence is warranted.
This study aimed to summarize for the first time the evidence on the effectiveness of HBE compared with CBE and HBE combined with CBE on patient-reported and performance-based outcomes in people with knee osteoarthritis.
2 Methods
2.1 Data sources and searches
The review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) statement (28), and followed the methods described in the Cochrane Handbook for Systematic Reviews of Interventions, Version 6.3 (29). The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO): CRD42023416548.
We searched PubMed, Cochrane, Embase, Web of Science, and Scopus until March 10, 2023, without date or language restrictions. The search string was built as follows: knee osteoarthritis, exercise, and home (see Supplementary Appendix S1 for the full search strategy). The electronic database search was supplemented by a manual search to identify potentially eligible records.
2.2 Study selection
Study selection was conducted by 2 authors using predetermined criteria independently. Disagreements were resolved by consensus after discussion with a third author. If the full manuscript could not be obtained, we contacted the author via email. Randomized controlled trials (RCTs) investigating HBE versus CBE or HBE combined with CBE for people with KOA were eligible. Participants were given an established diagnosis of KOA according to accepted criteria, regardless of age, gender, ethnicity, demography, and geography (30). The experimental intervention was HBE with all the exercise sessions being conducted at home. The control intervention was a supervised CBE with or without home-based exercise sessions, delivered in a hospital, outpatient department, private clinic, medical center, or community center. All interventions in the experimental and control groups were prescribed by a physical therapist or health professional. Excluding studies conducted on humans with non-KOA or conducted on animals. We determined and classified primary and secondary outcome measures in this review based on the international consensus on core outcome measures for phase III clinical trials of OA (31). The primary outcomes were self-reported measures, including pain, physical disability, and quality of life. The secondary outcomes were performance-based measures, including walking ability, lower limb muscle strength, and balance function.
2.3 Data extraction and quality assessment
Data from the included studies were independently extracted by 2 authors guided by Cochrane handbook (29). Any disagreement was resolved by discussion and a third author as required. The following descriptive data were extracted: Author, country of study, published year, participant characteristics (sample size, age, gender), intervention characteristics, and outcome measures at different follow-up times. The outcome measures were classified as patient-reported measures (1) pain (2), physical disability, and (3) quality of life; performance-based measures (4) walking ability (5) lower limb muscle strength, and (6) balance function. Where studies included more than one measurement scale, we extracted data from a scale that is highest on a suggested hierarchy (32, 33) (Supplementary Appendix S2). The short-term effect was defined as follow-up up to 3 months after baseline, and the long-term effect was defined as follow-up beyond 3 months after baseline. When multiple time points were available within the same follow-up period, the one closer to the endpoint of the intervention was used. The corresponding author of the relevant study was contacted to obtain missing data.
An assessment of the methodological quality of the primary articles was carried out by two reviewers independently, using the Cochrane risk of bias tool (version 2, ROB2) (34). This tool rates 7 potential sources of bias across 5 domains (randomization process, intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result). Each trial was assessed against 5 bias domains to produce a summary risk-of-bias assessment score for each domain and overall (low risk, some concerns, or high risk of bias). Disagreements were resolved by discussion or adjudication. Results from these questions were graphed and assessed using an Excel RoB2 tool.
2.4 Data synthesis and analysis
The post-intervention was used to obtain the pooled estimate of the effect of the intervention, using a random effects model due to the expected heterogeneity between the studies. We calculated standardized mean differences (SMDs) and 95% confidence intervals (CIs) for continuous variables with the inverse variance method. When necessary, SDs were calculated using available data (eg, 95% CI or p value) following the Cochrane guidelines. The effect size was interpreted as small (0.2), moderate (0.5), or large (0.8). Statistical heterogeneity was assessed using the I2, with classification as low (I2 < 25%), moderate (I2 = 25–50%), substantial (I2 = 50–75%), and considerable (I2 > 75%) (29). A funnel plot would be used to evaluate publication bias if ≥10 studies were available for a given meta-analysis (35), but the number found did not reach this. Sensitivity analyzes were conducted for each outcome by excluding one study in each round. We used Review Manager (version 5.4.1) to perform all statistical analyzes. Data unamenable to meta-analysis were reported narratively.
The overall quality of evidence for each outcome was rated according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) guidelines (36). Considering only RCTs were included, each outcome received a high certainty at the outset. Two reviewers assessed the quality of the evidence using the GRADE system, with potential disagreements resolved by discussion with a third reviewer. The GRADE downgrade details were presented in the Supplementary Appendix S3.
3 Results
3.1 Compliance with the registered protocol
To ensure a consistent comparison of primary studies and a robust conclusion, we categorized questions into two groups. The first group compared the efficacy between HBE and CBE in the control group, while the second group explored the efficacy between HBE and HBE combined with CBE. There were no other inconsistencies with the pre-registration protocol.
3.2 Study identification
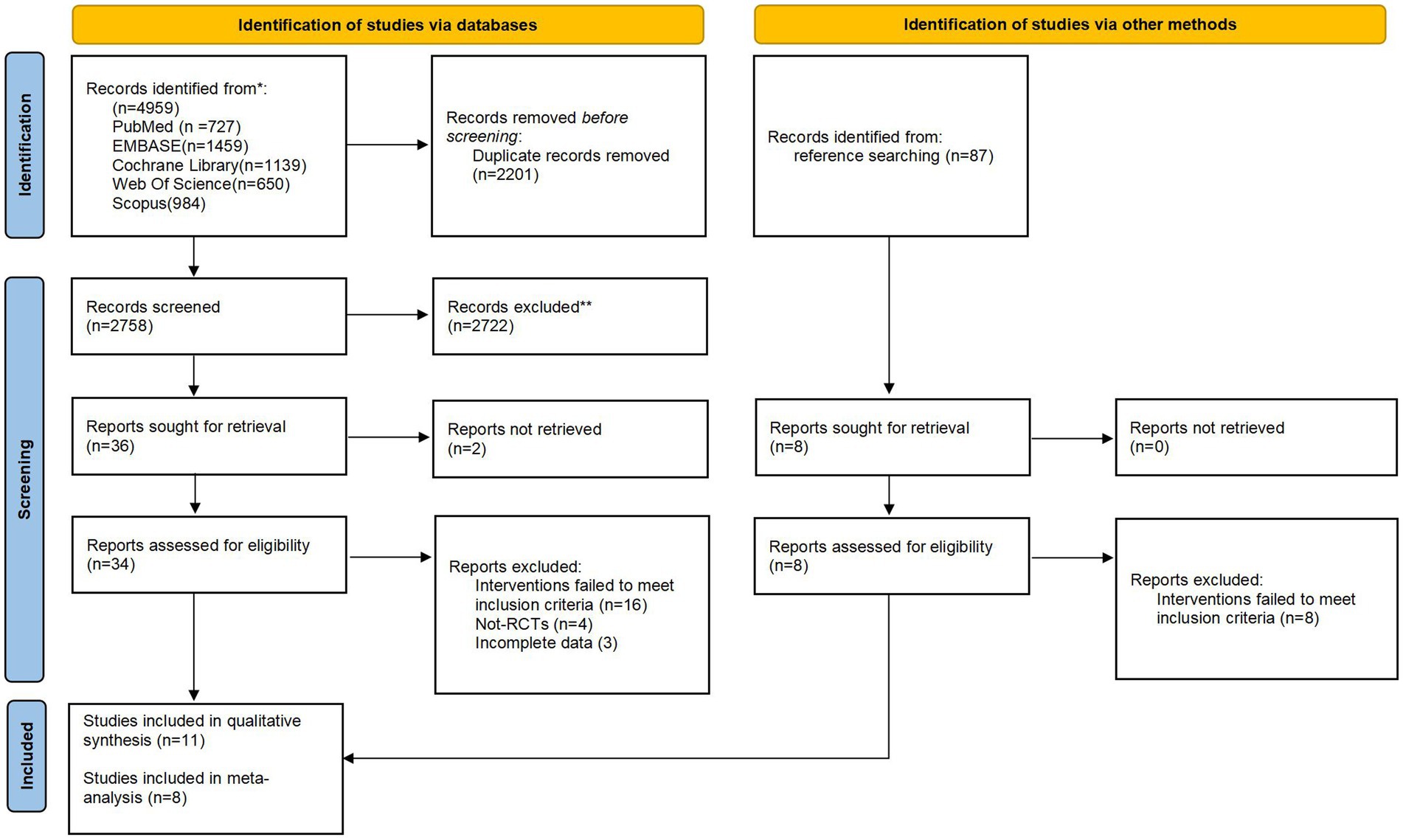
The initial database searches identified 4,959 citations (Figure 1). After the removal of duplicates, 2,758 records remained. Based on the title and abstract, we excluded 2,722 records that did not meet the eligibility criteria. The remaining 34 full texts were identified and 24 were excluded. Of these excluded studies, 16 for wrong intervention, 4 for wrong study design, and 3 for incomplete data (Supplementary Appendix S4). No additional articles were identified through manual searching.
3.3 Study characteristics
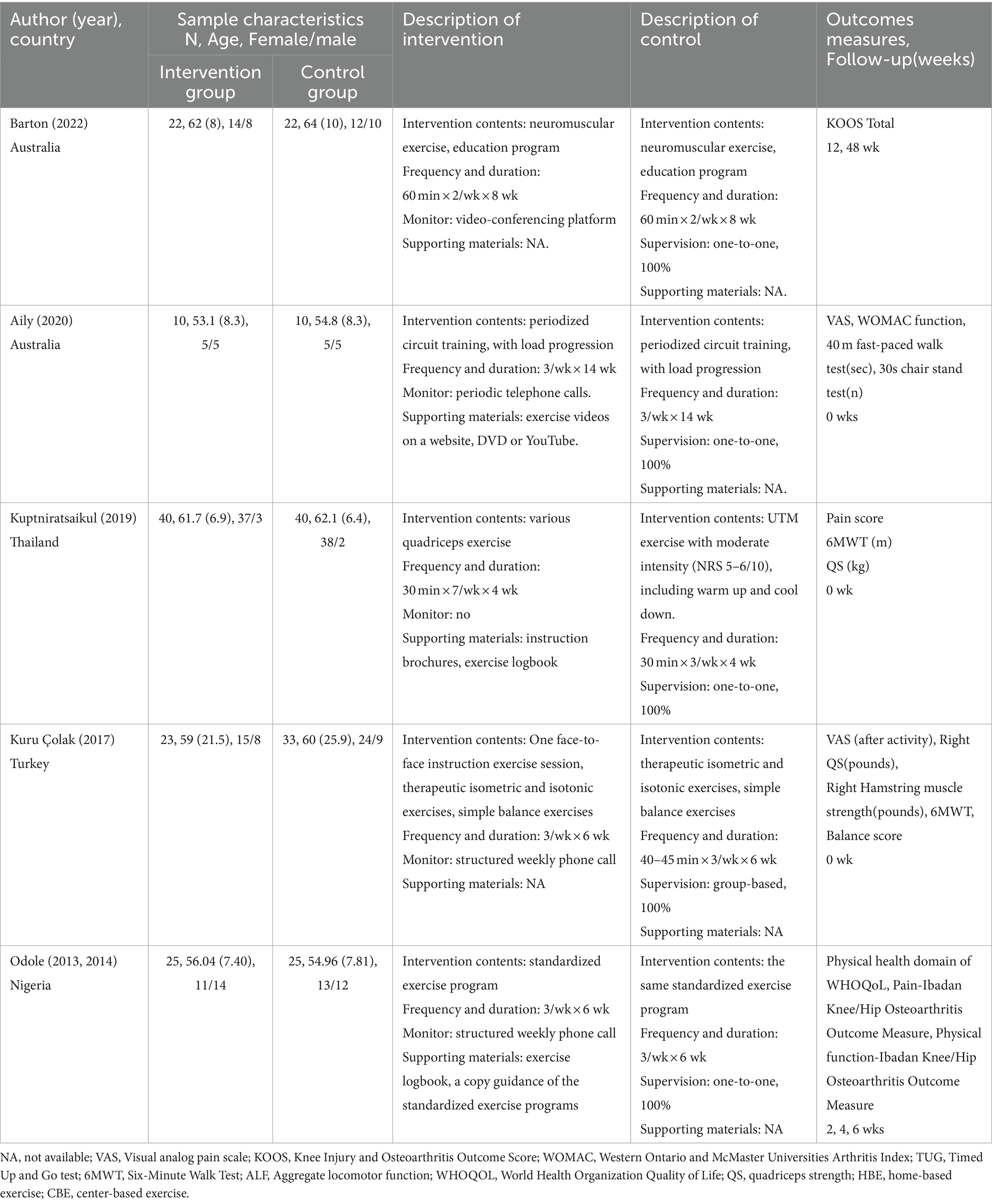
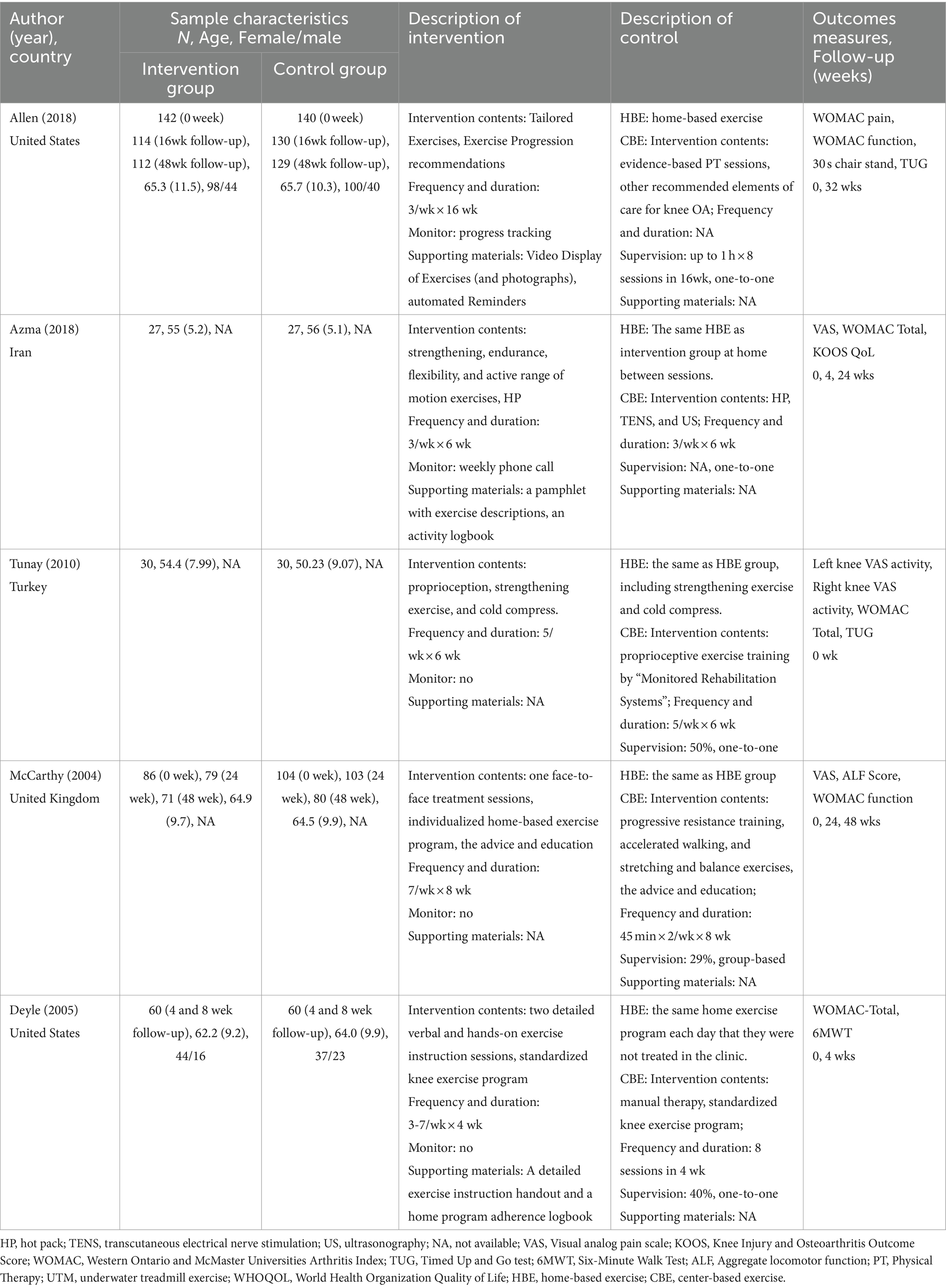
Descriptive characteristics of the 11 included studies are detailed in Tables 1, 2. HBE was compared with CBE in 6 studies (37–42), and with HBE combined with CBE in 5 studies (25–27, 43, 44). Studies were published from 2004 to 2022, with two studies conducted in Turkey (26, 39), two in Australia (37, 38), two in United States (25, 44), two in Nigeria (40, 41), with the remainder in Iran (43), Thailand (42), and United Kingdom (27). HBE had periodic remote monitoring by telephone (38–41, 43, 44) or videoconference (37), whereas four trials with no monitoring (25–27, 42). Support materials included exercise video (43, 44), exercise instruction manual (25, 40, 41, 43), exercise logbook (25, 40–43), and automated reminders (44). Two trials in the CBE were group-based exercise (27, 39) and the remaining trials were one-to-one exercises. Interventions for HBE combined with CBE additionally consisted of manual therapy (25), device-supported exercise therapy (26), and multiple physical factors (43). The intervention during for the included trials ranged from 4 to 24 weeks (2-7/wk), and participants were followed up for 0 to 48 weeks.
3.4 Risk of bias
Risk of bias assessment is provided in Supplementary Appendices S5, S6. The assessment resulted in some concerns of risk of bias in most trials (25, 27, 37–41, 43), high risk of bias in 1 trial (26), and low risk of bias in 2 trials (42, 44). Due to insufficient information, most trials were scored unclear or high risk in the randomization process or/and deviations from the intended interventions. Two-fives of the trials (26, 27, 37, 38) were unclear or at high risk of outcome measurement, mainly because of the lack of assessor blinding. Except for two trials (42, 44), most of the other trials lacked a pre-registered protocol, which might result in selective reporting bias risk.
3.5 Effect of HBE compared with CBE
Six studies involving 240 participants contributed data on the effectiveness of HBE versus CBE. The follow-up periods ranged from 0 to 12 months. The GRADE evidence profile comparing the efficacy of HBE and CBE for primary outcomes and secondary outcomes is reported in Supplementary Appendices S7, S8.
3.5.1 Primary outcomes
Meta-analysis of 5 studies showed the decrease of short-term pain in CBE was more than that in HBE (SMD, 0.22 [95% CI, −0.04 to 0.47], p = 0.09; I2 = 0%, GRADE moderate) (Figure 2A). However, the confidence intervals for the SMD were also consistent with the possibility that the difference is close to zero. Meta-analysis of 3 studies showed no between-groups difference for physical disability at short-term (SMD, 0.17 [95% CI, −0.19 to 0.54], p = 0.35; I2 = 0%, GRADE moderate) (Figure 2B). Only one study (40) with 50 participants reported patient-reported quality of life at short-term, and no difference was found. One study (37) reported 12-month follow-up of KOOS4 and showed no between-group statistical difference.
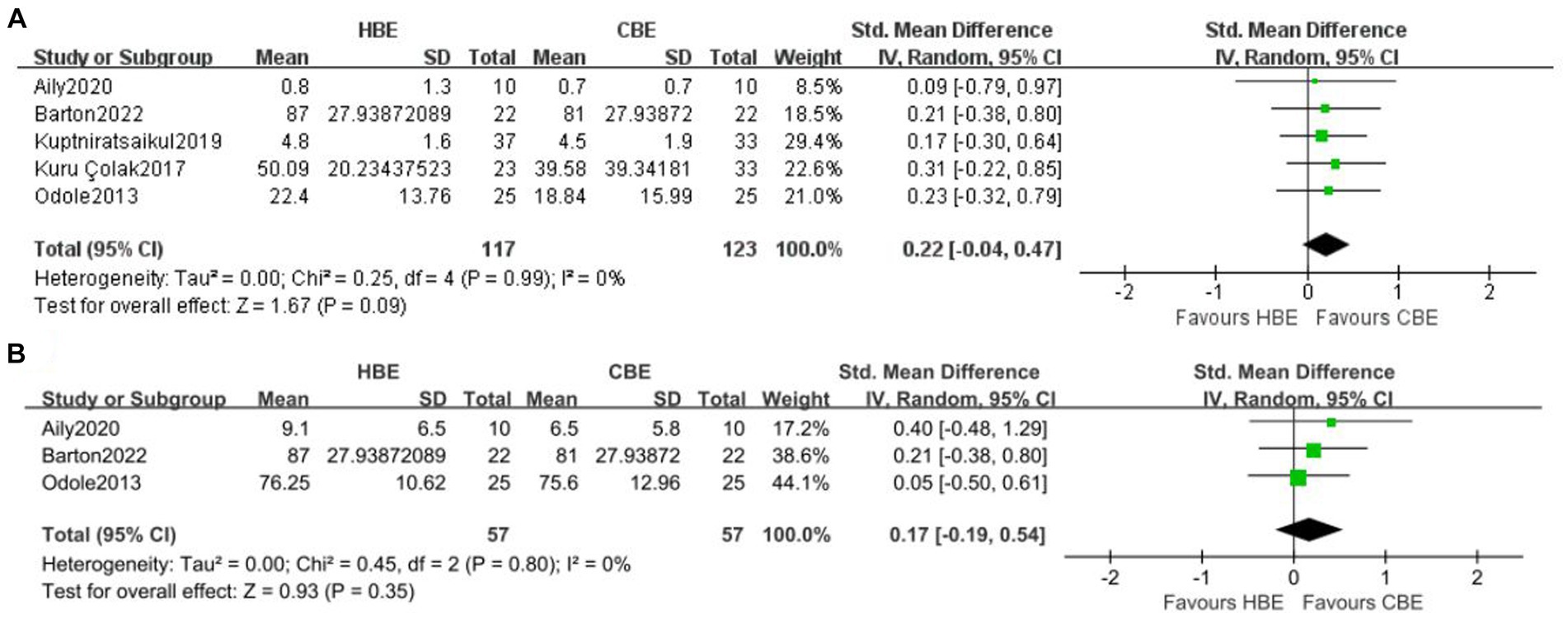
Figure 2. Meta-analysis of short-term effects of HBE versus CBE on (A) pain and (B) physical disability.
3.5.2 Secondary outcomes
Meta-analysis of 3 studies showed no between-groups difference for walking ability at short-term (SMD, −0.21 [95% CI, −0.64 to 0.22], p = 0.33; I2 = 35%, GRADE moderate) (Figure 3A). Meta-analysis of 3 studies showed no difference for lower limb muscle strength at short-term between HBE and CBE (SMD, −0.24 [95% CI, −0.88 to 0.41], p = 0.47; I2 = 69%, GRADE low) (Figure 3B). Only one study (39) reported the balance function at short-term, displaying no difference between HBE (n = 23) and CBE (n = 33). No studies reported long-term performance-based outcome measures comparing HBE and CBE.
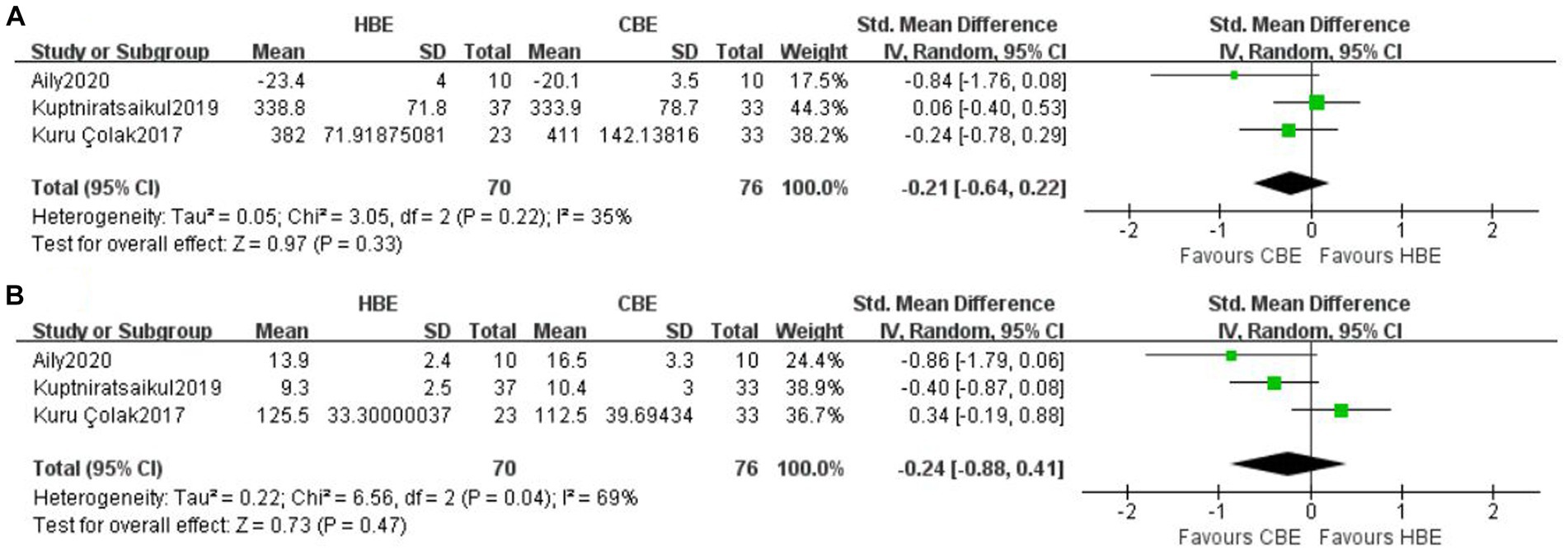
Figure 3. Meta-analysis of short-term effects of HBE versus CBE on (A) walking ability and (B) lower limb muscle strength.
3.6 Effect of HBE compared with HBE combined with CBE
Five studies investigated the effectiveness of HBE versus HBE combined with CBE, with two studies (26, 27) (250 participants) included in meta-analyzes. Three other studies (25, 43, 44) failed to include meta-analysis due to inconsistent interventions, which contained additional center-based interventions besides supervised in-person exercise in their CBEs, potentially confounding the effects of exercise therapy. The follow-up periods ranged from 0 to 12 months. The GRADE evidence profile comparing the efficacy of HBE and HBE combined with CBE for primary outcomes is reported in Supplementary Appendix S9.
3.6.1 Primary outcomes
Meta-analysis of 2 studies showed HBE was inferior to HBE combined with CBE for pain at short-term (SMD, 0.89 [95% CI, 0.60 to 1.17], p = 0.001; I2 = 11%, GRADE moderate) (Figure 4A). Meta-analysis of 2 studies showed HBE was inferior to HBE combined with CBE for physical disability at short-term (SMD, 0.25 [95% CI, 0.00 to 0.50], p = 0.05; I2 = 0%, GRADE moderate) (Figure 4B); however, the estimate also included the possibility of no between-group difference. No studies have reported quality of life between HBE and HBE combined with CBE. Only one study (27) reported the patient-reported pain and physical disability at long-term, and reduction in pain in HBE combined with CBE (n = 103) was noted to be statistically significant compared with HBE alone (n = 79).
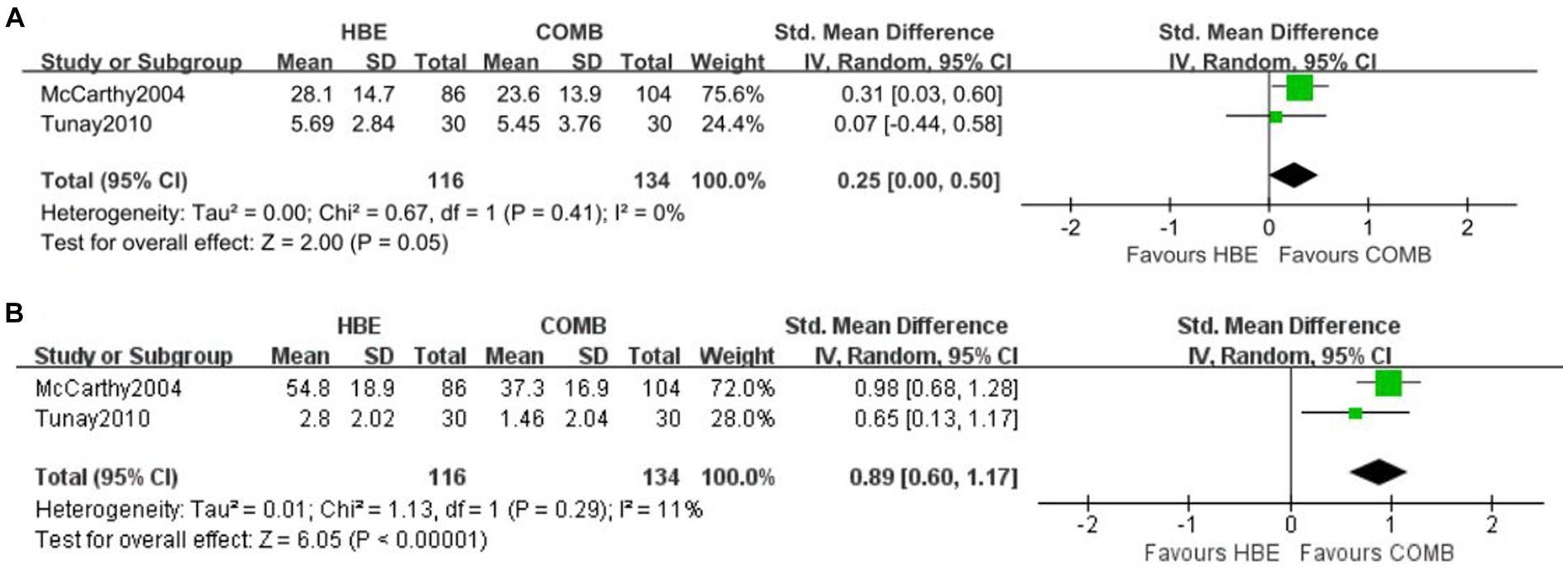
Figure 4. Meta-analysis of short-term effects of HBE versus HBE combined with CBE on (A) pain and (B) physical disability.
Three studies (25, 43, 44) were not included in the meta-analysis due to inconsistent interventions. Two studies showed no difference in short-term pain and physical disability (43, 44) and long-term pain and physical disability (44) in HBE compared with HBE combined with CBE. One study (25) showed poorer benefits for HBE than HBE combined with CBE in short-term pain and physical disability. Regular monitoring has been shown to augment the efficacy of HBE (45). The first 2 studies had regular remote monitoring in HBE (43, 44), whereas the latter one (25) had no monitoring, which may account for the inconsistent findings.
3.6.2 Secondary outcomes
Only One study (26) reported no between-groups difference for balance function at short-term. No studies reported long-term performance-based outcome measures comparing HBE and HBE combined with CBE.
3.7 Additional analyzes
Subgroup analyzes were not performed owing to the limited number of studies for each outcome. Sensitivity analyzes were conducted to evaluate the robustness of our meta-analysis findings when more than two studies were included. These sensitivity analyzes did not alter any of the meta-analysis results, which suggests this finding is robust.
3.8 Role of the funding source
The funders played no role in the design, conduct, or reporting of this study.
4 Discussion
This systematic review provides moderate-quality evidence that HBE was as effective as CBE for pain, physical disability, and walking ability in the short term. Based on low-quality evidence, there were also similar effects between HBE and CBE for lower limb muscle strength in the short term. When comparing HBE and HBE combined with CBE, there was moderate-quality evidence showing that HBE was inferior to HBE combined with CBE in short-term pain and physical disability. However, these findings need to be interpreted with caution as the number of included studies and participants is low. Insufficient data prevented the determination of differences beyond the intervention period. These findings imply that incorporating home-based exercise could serve as a complementary approach to center-based exercise, or that there is a need for future enhancements in the clinical effectiveness of center-based exercise for knee osteoarthritis.
This is the first systematic review and meta-analysis to specifically investigate the effects between HBE and CBE for people with KOA, resulting in a challenge to compare with previous reviews. A systematic review (24) published in 2016 reported that HBE and other treatments had similar effects, but the conclusion is conflicting because of inconsistent comparisons. Through six RCTs with consistent comparisons, this review enhances the findings that HBE yields benefits similar to CBE for pain, physical disability, walking ability, and lower limb muscle strength in the short term. As only studies with identical exercise interventions in both the intervention and control groups were included in the meta-analyzes, this approach effectively eliminates any confounding effects resulting from differences in intervention location and contents. GRADE provides very low-to moderate-quality evidence that HBE is as effective as CBE. The main reason for the lower quality of evidence is the restricted number of studies and participants included. In comparing HBE to CBE, it was observed that nearly all HBE programs incorporated regular telephone monitoring or supervision, although the frequency of such monitoring was only minimal weekly. These findings suggest that minimal supervised HBE has significant potential as a viable alternative to CBE in future clinical practice.
The second aim of this review was to determine the efficacy of HBE alone compared with HBE combined with CBE for people with KOA. Meta-analyzes of 2 RCTs suggest that additional sessions of supervised CBE may enhance the efficacy of HBE in short-term pain and physical disability. This finding is consistent with a previous study (46) demonstrating greater effectiveness in pain and physical disability with more supervised sessions when compared to a non-exercise control. Nevertheless, insufficient evidence from two RCTs precludes the definitive conclusion that HBE combined with CBE is superior to HBE alone in this review. Additionally, all HBE programs were without any telephone monitoring or supervision, which probably underestimated the effectiveness of HBE (47). Further, high-quality RCTs are necessary to establish conclusive evidence regarding the comparative efficacy of HBE alone versus HBE combined with CBE.
Exercise is one of the treatments that clinicians can deliver using telerehabilitation, and remote information technology can greatly enhance the effectiveness of home-based exercise. However, HBE has typically been used as an active control group in previous studies when compared with CBE in people with KOA, few studies have utilized it as the primary intervention. When home-based exercise versus home-based exercise supplemented center-based rehabilitation, several studies (43, 44) showed that additional center-based sessions probably showed a little increased effect. This is congruent with the findings of two reviews (48, 49) in orthopedic rehabilitation, where they found that additional outpatient interventions were not superior to home-based rehabilitation.
HBE tends to be more effective when it is supported by information technology, such as regular telephone monitoring (38–41, 43, 44), and CBE seems to be more effective when it is group-based (39). Future studies should maximize the efficacy of home rehabilitation by information technology or behavior promotion techniques, and then compare it with evidence-based clinic-based rehabilitation. The KOA’s latest clinical practice guidelines, while with an emphasis on home-based exercise (6, 7, 50), fail to recommend an optimal supervision frequency. Hence, there is a need to explore whether the combination of home-based rehabilitation and clinic-based rehabilitation would be superior to either intervention alone, and investigate the dose–response relationship of supervision. We have identified several ongoing randomized trials attempting to address these questions (51–54).
4.1 Limitations
There are several limitations to this systematic review with meta-analysis worth noting. Fewer trials and a small sample size limited the precision of the findings and undermined the capacity to assess publication bias graphically or statistically. Additionally, although data were extracted and pooled based on the priority of outcome indicators as recommended (5, 33), the pooled effect was calculated using the SMD, which is less clinically meaningful than a mean difference. When comparing HBE and HBE combined with CBE, no definitive conclusions were reached due to the limited number of studies. Future studies need to ascertain the amount of CBE supplementation for HBE that will have optimal cost-effectiveness, providing essential guidance for future clinical practice regarding people with KOA. On the other hand, individual adherence is the core component of HBE (55, 56), yet less reported in studies of HBR for KOA patients. Only one trial (27) reported adherence included in this review, showing no statistical difference between HBE and CBE. Lastly, fewer studies reported quality of life, performance-based outcomes, and long-term outcomes, leading to controversial results. Nevertheless, as the first systematic review to examine the effectiveness of HBE versus CBE, we can still have an impact on current clinical practice and future clinical research. More high-quality studies comparing the efficacy of HBE and CBE (with or without HBE) are needed in the future to strengthen the findings of this review.
4.2 Clinical implication
Home-based exercise presents comparable benefits to center-based exercise in terms of patient-reported and performance-based outcomes among people with knee osteoarthritis. This highlights the importance of prioritizing the incorporation of home exercise regimens into clinical guidelines for this population. Home-based exercise can effectively mitigate pain and functional deterioration in people with knee osteoarthritis with less medical supervision, hence decreasing the national healthcare burden. Furthermore, concurrent application of home-based and center-based rehabilitation may lead to superior outcomes. However, given the limited number of studies on the matter, it remains uncertain what the optimal number of supervised outpatient rehabilitation sessions would represent the most cost-effective strategy for the management of knee osteoarthritis. Further clinical research is warranted to address this issue. Finally, future studies should also include health economic analyzes and larger sample sizes. This could allow more robust subgroup analyzes and explore which specific subgroups might benefit most from home-based exercise.
5 Conclusion
In conclusion, this review provides evidence that HBE is as effective as CBE for KOA on pain, physical disability, walking ability, and lower limb muscle strength in short-term follow-up. Furthermore, with limited evidence, the efficacy of HBE maybe be enhanced by combined with CBE in short-term pain and physical disability. This review comprehensively synthesizes the differential efficacy of HBE compared with CBE for KOA, and the findings indicate that HBE could potentially serve as a favorable substitute for CBE in clinical settings characterized by limited healthcare resources or geographical constraints.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
Z-YZ: Conceptualization, Methodology, Writing – original draft. LH: Conceptualization, Methodology, Writing – original draft. LT: Data curation, Formal analysis, Methodology, Writing – original draft. JY: Conceptualization, Writing – review & editing. MG: Data curation, Methodology, Writing – original draft. X-QW: Data curation, Investigation, Writing – original draft. J-JJ: Conceptualization, Supervision, Writing – review & editing. Z-LL: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1360824/full#supplementary-material
References
1. Sharma, L . Osteoarthritis of the knee. N Engl J Med. (2021) 384:51–9. doi: 10.1056/NEJMcp1903768
2. Felson, DT, Naimark, A, Anderson, J, Kazis, L, Castelli, W, and Meenan, RF. The prevalence of knee osteoarthritis in the elderly. The framingham osteoarthritis study. Arthritis Rheum. (1987) 30:914–8. doi: 10.1002/art.1780300811
3. Jordan, JM, Helmick, CG, Renner, JB, Luta, G, Dragomir, AD, Woodard, J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County osteoarthritis project. J Rheumatol. (2007) 34:172–80.
4. Fan, I, Govil, D, and Semciw, A. The effectiveness of exercise based digital health interventions (requiring INTERNET) in management of hip and knee osteoarthritis: a systematic review and META-analysis. Osteoarthr Cartil. (2022) 30:S402. doi: 10.1016/j.joca.2022.02.540
5. Fransen, M, McConnell, S, Harmer, AR, Van der Esch, M, Simic, M, and Bennell, KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. (2015) 2015:CD004376. doi: 10.1002/14651858.CD004376.pub3
6. Kolasinski, SL, Neogi, T, Hochberg, MC, Oatis, C, Guyatt, G, Block, J, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the Management of Osteoarthritis of the hand, hip, and knee. Arthrit Care Res. (2020) 72:149–62. doi: 10.1002/acr.24131
7. Bannuru, RR, Osani, MC, Vaysbrot, EE, Arden, NK, Bennell, K, Bierma-Zeinstra, SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr Cartil. (2019) 27:1578–89. doi: 10.1016/j.joca.2019.06.011
8. Wang, J, Xie, D, Cai, Z, Luo, M, Chen, B, Sun, Y, et al. Does a home-based exercise program play any role in the treatment of knee osteoarthritis? A meta-analysis. Adv Clin Exp Med. (2022) 31:1187–96. doi: 10.17219/acem/151753
9. Hageman, D, Fokkenrood, HJ, Gommans, LN, van den Houten, MM, and Teijink, JA. Supervised exercise therapy versus home-based exercise therapy versus walking advice for intermittent claudication. Cochrane Database Syst Rev. (2018) 2018:CD005263. doi: 10.1002/14651858.CD005263.pub4
10. Shafizadeh, M, Parvinpour, S, and Ali, K. Effect of home-based exercise on falls in community-dwelling older adults: an umbrella review. Sport Sci Health. (2022) 19:743–56. doi: 10.1007/s11332-022-00993-2
11. Mañas, A, Gómez-Redondo, P, Valenzuela, PL, Morales, JS, Lucía, A, and Ara, I. Unsupervised home-based resistance training for community-dwelling older adults: a systematic review and meta-analysis of randomized controlled trials. Ageing Res Rev. (2021) 69:101368. doi: 10.1016/j.arr.2021.101368
12. Uzzaman, MN, Agarwal, D, Chan, SC, Patrick Engkasan, J, Habib, GMM, Hanafi, NS, et al. Effectiveness of home-based pulmonary rehabilitation: systematic review and meta-analysis. Eur Respir Rev. (2022) 31:220076. doi: 10.1183/16000617.0076-2022
13. Brown, RC, Coombes, JS, Jungbluth Rodriguez, K, Hickman, IJ, and Keating, SE. Effectiveness of exercise via telehealth for chronic disease: a systematic review and meta-analysis of exercise interventions delivered via videoconferencing. Br J Sports Med. (2022). doi: 10.1136/bjsports-2021-105118
14. Solis-Navarro, L, Gismero, A, Fernández-Jané, C, Torres-Castro, R, Solá-Madurell, M, Bergé, C, et al. Effectiveness of home-based exercise delivered by digital health in older adults: a systematic review and meta-analysis. Age Ageing.. (2022) 51:afac243.
15. Lacroix, A, Hortobágyi, T, Beurskens, R, and Granacher, U. Effects of supervised vs. unsupervised training programs on balance and muscle strength in older adults: A systematic review and Meta-analysis. Sports Med. (2017) 47:2341–61. doi: 10.1007/s40279-017-0747-6
16. Anderson, L, Sharp, GA, Norton, RJ, Dalal, H, Dean, SG, Jolly, K, et al. Home-based versus Center-based cardiac rehabilitation. Cochrane Database Syst Rev. (2017) 6:Cd007130. doi: 10.1002/14651858.CD007130.pub4
17. Nascimento, LR, Rocha, RJ, Boening, A, Ferreira, GP, and Perovano, MC. Home-based exercises are as effective as equivalent doses of Center-based exercises for improving walking speed and balance after stroke: a systematic review. J Physiother. (2022) 68:174–81. doi: 10.1016/j.jphys.2022.05.018
18. Imran, HM, Baig, M, Erqou, S, Taveira, TH, Shah, NR, Morrison, A, et al. Home-based cardiac rehabilitation alone and hybrid with center-based cardiac rehabilitation in heart failure: a systematic review and Meta-analysis. J Am Heart Assoc. (2019) 8:1–11. doi: 10.1161/JAHA.119.012779
19. Claes, J, Buys, R, Budts, W, Smart, N, and Cornelissen, VA. Longer-term effects of home-based exercise interventions on exercise capacity and physical activity in coronary artery disease patients: a systematic review and meta-analysis. Eur J Prev Cardiol. (2017) 24:244–56. doi: 10.1177/2047487316675823
20. Nascimento, LR, Gaviorno, LF, de Souza, BM, Gonçalves, JV, and Arêas, FZDS. Home-based is as effective as Center-based rehabilitation for improving upper limb motor recovery and activity limitations after stroke: a systematic review with meta-analysis. Clin Rehabil. (2022) 36:1565–77. doi: 10.1177/02692155221121015
21. Flynn, A, Allen, NE, Dennis, S, Canning, CG, and Preston, E. Home-based prescribed exercise improves balance-related activities in people with Parkinson’s disease and has benefits similar to Center-based exercise: a systematic review. J Physiother. (2019) 65:189–99. doi: 10.1016/j.jphys.2019.08.003
22. Chaabene, H, Prieske, O, Herz, M, Moran, J, Höhne, J, Kliegl, R, et al. Home-based exercise programmes improve physical fitness of healthy older adults: a PRISMA-compliant systematic review and meta-analysis with relevance for COVID-19. Ageing Res Rev. (2021) 67:101265. doi: 10.1016/j.arr.2021.101265
23. Mahjur, M, and Norasteh, AA. The effect of unsupervised home-based exercise training on physical functioning outcomes in older adults: a systematic review and Meta-analysis of randomized controlled trials. Biol Res Nurs. (2021) 23:504–12. doi: 10.1177/1099800421989439
24. Anwer, S, Alghadir, A, and Brismee, J-M. Effect of home exercise program in patients with knee osteoarthritis: a systematic review and Meta-analysis. J Geriatr Phys Ther. (2016) 39:38–48. doi: 10.1519/JPT.0000000000000045
25. Deyle, GD, Allison, SC, Matekel, RL, Ryder, MG, Stang, JM, Gohdes, DD, et al. Physical therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Phys Ther. (2005) 85:1301–17. doi: 10.1093/ptj/85.12.1301
26. Tunay, VB, Baltaci, G, and Atay, AÖ. Hospital-based versus home-based proprioceptive and strengthening exercise programs in knee osteoarthritis. Acta Orthop Traumato. (2010) 44:270–7. doi: 10.3944/AOTT.2010.2306
27. McCarthy, CJ, Mills, PM, Pullen, R, Roberts, C, Silman, A, and Oldham, JA. Supplementing a home exercise programme with a class-based exercise programme is more effective than home exercise alone in the treatment of knee osteoarthritis. Rheumatology (Oxford). (2004) 43:880–6. doi: 10.1093/rheumatology/keh188
28. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
29. Higgins, J, Thomas, J, Chandler, J, Cumpston, M, Li, T, Page, M, et al. (2022). Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Cochrane. Available at: www.training.cochrane.org/handbook
30. Katz, JN, Arant, KR, and Loeser, RF. Diagnosis and treatment of hip and knee osteoarthritis: a review. JAMA. (2021) 325:568–78. doi: 10.1001/jama.2020.22171
31. Bellamy, N, Kirwan, J, Boers, M, Brooks, P, Strand, V, Tugwell, P, et al. Recommendations for a core set of outcome measures for future phase III clinical trials in knee, hip, and hand osteoarthritis. Consensus development at OMERACT III. J Rheumatol. (1997) 24:799–802.
32. Jüni, P, Reichenbach, S, and Dieppe, P. Osteoarthritis: rational approach to treating the individual. Best Pract Res Clin Rheumatol. (2006) 20:721–40. doi: 10.1016/j.berh.2006.05.002
33. van Tuyl, LHD, and Boers, M. Patient-reported outcomes in core domain sets for rheumatic diseases. Nat Rev Rheumatol. (2015) 11:705–12. doi: 10.1038/nrrheum.2015.116
34. Sterne, JAC, Savović, J, Page, MJ, Elbers, RG, Blencowe, NS, Boutron, I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
35. Sterne, JAC, and Egger, M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. (2001) 54:1046–55. doi: 10.1016/S0895-4356(01)00377-8
36. Balshem, H, Helfand, M, Schünemann, HJ, Oxman, AD, Kunz, R, Brozek, J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. (2011) 64:401–6. doi: 10.1016/j.jclinepi.2010.07.015
37. Barton, C, Pazzinatto, M, Perraton, Z, Crossley, K, Dundules, K, Russell, T, et al. Telehealth-delivered group-based education and exercise-therapy for knee osteoarthritis: a randomised clinical trial interrupted by the COVID-19 pandemic. J Sci Med Sport. (2022) 25:S67–8. doi: 10.1016/j.jsams.2022.09.081
38. Aily, J, Almeida, A, Ribeiro, G, De Noronha, M, and Mattiello, S. Is a periodized circuit training delivered by telerehabilitation effective for patients with knee osteoarthritis? A phase i randomized controlled trial. Osteoarthr Cartil. (2020) 28:S468–9. doi: 10.1016/j.joca.2020.02.734
39. Kuru Çolak, T, Kavlak, B, Aydoğdu, O, Şahin, E, Acar, G, Demirbüken, İ, et al. The effects of therapeutic exercises on pain, muscle strength, functional capacity, balance and hemodynamic parameters in knee osteoarthritis patients: a randomized controlled study of supervised versus home exercises. Rheumatol Int. (2017) 37:399–407. doi: 10.1007/s00296-016-3646-5
40. Odole, AC, and Ojo, OD. Is telephysiotherapy an option for improved quality of life in patients with osteoarthritis of the knee? Int J Telemed Appl. (2014) 2014:e903816. doi: 10.1155/2014/903816
41. Odole, AC, and Ojo, OD. A telephone-based physiotherapy intervention for patients with osteoarthritis of the knee. Int J Telerehabilita. (2013) 5:11–20. doi: 10.5195/ijt.2013.6125
42. Kuptniratsaikul, V, Kittichaikarn, C, Suntornpiyapan, P, Kovintaset, K, and Inthibal, S. Is four-week underwater treadmill exercise regimen compared to home exercise efficacious for pain relief and functional improvement in obese patients with knee osteoarthritis? A randomized controlled trial. Clin Rehabil. (2019) 33:85–93. doi: 10.1177/0269215518792041
43. Azma, K, RezaSoltani, Z, Rezaeimoghaddam, F, Dadarkhah, A, and Mohsenolhosseini, S. Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: a randomized clinical trial. J Telemed Telecare. (2018) 24:560–5. doi: 10.1177/1357633X17723368
44. Allen, KD, Arbeeva, L, Callahan, LF, Golightly, YM, Goode, AP, Heiderscheit, BC, et al. Physical therapy vs. Internet-based exercise training for patients with knee osteoarthritis: results of a randomized controlled trial. Osteoarthr Cartil. (2018) 26:383–96. doi: 10.1016/j.joca.2017.12.008
45. Vetrovsky, T, Borowiec, A, Juřík, R, Wahlich, C, Śmigielski, W, Steffl, M, et al. Do physical activity interventions combining self-monitoring with other components provide an additional benefit compared with self-monitoring alone? A systematic review and meta-analysis. Brit J Sport Med. (2022) 56:1366–74. doi: 10.1136/bjsports-2021-105198
46. Juhl, C, Christensen, R, Roos, EM, Zhang, W, and Lund, H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis & rheumatology (Hoboken, NJ). (2014) 66:622–36. doi: 10.1002/art.38290
47. Yilmaz, M, Sahin, M, and Algun, C. Effectiveness of home based exercise program taught by physiotherapist on pain and function in knee osteoarthritis. Osteoporos Int. (2018) 29:149–565. doi: 10.1007/s00198-018-4465-1
48. Nutarelli, S, Delahunt, E, Cuzzolin, M, Delcogliano, M, Candrian, C, and Filardo, G. Home-based vs supervised inpatient and/or outpatient rehabilitation following knee meniscectomy a systematic review and Meta-analysis. JAMA Netw Open. (2021) 4:e2111582. doi: 10.1001/jamanetworkopen.2021.11582
49. Buhagiar, MA, Naylor, JM, Harris, IA, Xuan, W, Adie, S, and Lewin, A. Assessment of outcomes of inpatient or clinic-based vs home-based rehabilitation after Total knee arthroplasty: a systematic review and Meta-analysis. JAMA Netw Open. (2019) 2:e192810. doi: 10.1001/jamanetworkopen.2019.2810
50. Holden, MA, Metcalf, B, Lawford, BJ, Hinman, RS, Boyd, M, Button, K, et al. Recommendations for the delivery of therapeutic exercise for people with knee and/or hip osteoarthritis. An international consensus study from the OARSI rehabilitation discussion group. Osteoarthr Cartilage. (2023) 31:386–96. doi: 10.1016/j.joca.2022.10.009
51. Safran-Norton, CE, Sullivan, JK, Irrgang, JJ, Kerman, HM, Bennell, KL, Calabrese, G, et al. A consensus-based process identifying physical therapy and exercise treatments for patients with degenerative meniscal tears and knee OA: the TeMPO physical therapy interventions and home exercise program. Bmc Musculoskel Dis. (2019) 20:514. doi: 10.1186/s12891-019-2872-x
52. Hinman, RS, Kimp, AJ, Campbell, PK, Russell, T, Foster, NE, Kasza, J, et al. Technology versus tradition: a non-inferiority trial comparing video to face-to-face consultations with a physiotherapist for people with knee osteoarthritis. Protocol for the PEAK randomised controlled trial. Bmc Musculoskel Dis. (2020) 21:522. doi: 10.1186/s12891-020-03523-8
53. Saccol, MF (2022). Comparison between supervised group exercise and home exercise program for knee osteoarthritis. Available at: https://clinicaltrials.gov/ct2/show/NCT03356431 (accessed May 25, 2023)
54. Ojoawo, AO (2023). Effect of clinic-based and tele-monitored home-based intervention on pain intensity, function and quality of life in patients with knee osteoarthritis. Available at: https://clinicaltrials.gov/ct2/show/NCT05832866 (accessed May 25, 2023)
55. Argent, R, Daly, A, and Caulfield, B. Patient involvement with home-based exercise programs: can connected health interventions influence adherence? JMIR Mhealth Uhealth. (2018) 6:e47. doi: 10.2196/mhealth.8518
56. Duong, V, Daniel, MS, Ferreira, ML, Fritsch, CG, Hunter, DJ, Wang, X, et al. Measuring adherence to unsupervised, conservative treatment for knee osteoarthritis: a systematic review. Osteoarthr Cartil Open. (2021) 3:100171. doi: 10.1016/j.ocarto.2021.100171
Keywords: knee osteoarthritis, home based, exercise, systematic review, patient reported outcome measures
Citation: Zhang Z-Y, Huang L, Tian L, Yi J, Gao M, Wang X-Q, Jiang J-J and Liu Z-L (2024) Home-based vs center-based exercise on patient-reported and performance-based outcomes for knee osteoarthritis: a systematic review with meta-analysis. Front. Public Health. 12:1360824. doi: 10.3389/fpubh.2024.1360824
Edited by:
Hassane Zouhal, University of Rennes 2 – Upper Brittany, FranceReviewed by:
Adewale Adebajo, The University of Sheffield, United KingdomBeatriz Fernandes, Escola Superior de Tecnologia da Saúde de Lisboa (ESTeSL), Portugal
Copyright © 2024 Zhang, Huang, Tian, Yi, Gao, Wang, Jiang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun-Jie Jiang, ampqNTIwNTEyQDE2My5jb20=; Zhong-Liang Liu, emhvbmdsaWFuZ0BqbHUuZWR1LmNu
†These authors have contributed equally to this work
‡These authors have contributed equally to this work and share first authorship
 Zhi-Yuan Zhang1‡
Zhi-Yuan Zhang1‡ Lv Tian
Lv Tian Zhong-Liang Liu
Zhong-Liang Liu