- 1Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Public Health Emergency Management Directorate, Benishangul Gumuz Regional Health Bureau, Assosa, Ethiopia
- 3Department of Clinical Midwifery, School of Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Tuberculosis is a major global public health problem and a leading cause of morbidity and mortality in Ethiopia. TB prevention and control in low-income countries, such as Ethiopia, face significant challenges, including late detection and treatment initiation. A delay in the initiation of tuberculosis treatment increases the morbidity and mortality of patients and community transmission. Therefore, this study aimed to assess patient delay and associated factors among pulmonary tuberculosis patients attending public health facilities in the Metekel Zone, Benishangul Gumuz Region, Western Ethiopia.
Methods: An institution-based cross-sectional study was conducted from March to August 2020 among newly diagnosed pulmonary tuberculosis patients. All pulmonary tuberculosis patients (416) who came to all public health facilities of the Metekel zone for treatment during the period were included. Data were collected through face-to-face interviews using a structured and pretested questionnaire. A multivariable logistic regression was fitted to identify independent factors for delay in seeking treatment among PTB patients. Adjusted odds ratios with 95% CIs were determined, and variables with p values <0.05 were considered statistically significant.
Results: Nearly three-fourths 302 (72.6, 95% CI: 68.5, 76.7) of the patients were delayed in seeking medical advice, with a median patient delay of 27 days (IQR: 21–31). Age of the patients [above 54 years (AOR = 2.65, 95% CI: 1.30, 5.40), 36–54 years (AOR = 1.86, 95% CI: 1.14,3.02)], family size of 5 members and above (AOR = 1.62, 95% CI: 1.10–3.14), travel time above 60 min (AOR = 3.65, 95% CI: 1.55, 8.60), history of visits to informal care providers (AOR = 1.74, 95% CI: 1.11, 3.14), and poor knowledge about PTB (AOR = 1.64, 95% CI: 1.04–2.44) were statistically significant factors associated with delays in seeking treatment among PTB patients.
Conclusion: Most pulmonary tuberculosis patients delay seeking medical advice for their illnesses. Delays in seeking treatment were associated with older age, large household size, longer travel time to reach the nearby health facility, visiting informal care providers, and poor knowledge about pulmonary tuberculosis. Hence, it is crucial to consider community screening programs, enhance public awareness, and ensure the accessibility of TB diagnostic and treatment services.
Background
Tuberculosis (TB) is an infectious bacterial disease caused by the bacillus Mycobacterium tuberculosis. It primarily affects the lungs (pulmonary TB), accounting for 85% of all TB cases, but it can also affect other parts of the body (1). It is a major cause of morbidity, ranking among the top 10 causes of death worldwide and being the leading cause of death from a single infectious agent (2).
TB is a significant public health problem, with an estimated one-quarter of the global population being infected with tubercle bacilli and therefore at risk of developing active disease (3). According to the 2019 WHO report, approximately 10.0 million people globally (132 cases per 100,000 population) fell ill with TB in 2018. In Africa, the estimated total incidence and HIV-negative TB mortality were 231 and 37 per 100,000 population, respectively. Ethiopia is one of the top 20 high-burden countries for TB, TB/HIV, and MDR-TB, with an estimated annual incidence of TB and HIV-negative TB mortality of 151 and 22 per 100,000 populations, respectively (4).
Achieving the goal of eradicating the TB epidemic by 2030 is one of the health targets outlined in the United Nations Sustainable Development Goals (SDGs) (5). The End TB Strategy focuses on actions needed to accelerate progress in providing access to TB diagnosis and treatment in each country. It emphasizes integrated patient-centered care and prevention, along with early diagnosis and prompt treatment within 2 weeks of the onset of signs and symptoms (6). Ethiopia has officially supported the global “END TB strategy” and aligned the National TB Strategic Plan with the National Health Sector Transformation Plan. The National End TB Strategy aims to reduce TB-related mortality by 95% and new TB cases by 90% between 2015 and 2035. The program is dedicated to enhancing accessibility and fairness in TB services for vulnerable and marginalized populations, as these groups often face socioeconomic and legal obstacles that result in delays in receiving appropriate care (7).
Ensuring early detection and timely initiation of treatment is crucial for an effective tuberculosis control program. Delays in diagnosis and treatment remain a challenge in TB prevention and control programs. Delays in the initiation of tuberculosis treatment pose various risks, including unfavorable treatment outcomes, adverse social and economic consequences, increased transmission of TB, and reduced productivity and social stability (7, 8).
Studies in different regions of Ethiopia indicate that late patient health-seeking behavior is the major contributor to treatment delay in tuberculosis treatment (8–10). The magnitude of patient delay among pulmonary tuberculosis patients ranges from 30 to 90%, with a median delay of 17 days to 45 days (9–15). Patient delay can be associated with various factors that either promote or impede health-seeking behavior. Previous studies in different areas of Ethiopia have identified factors such as older age (9, 16), lower educational status (10, 17), rural residence (10, 18), low monthly income (15, 18), large family size (9), long distance from the health institution (10, 11), lack of knowledge about tuberculosis (12, 15), self-medication practice (9, 14), prior visit to informal providers (14, 15, 18), and low perceived severity of the illness (10, 15).
The TB case detection rate in the Metekel zone of Benishangul Gumuz Regional State, West Ethiopia, was 36% in 2015, which is significantly lower than the minimum national target of 70% (19). The low case detection rate could be attributed to patients’ delay in seeking health care for their TB symptoms. Therefore, it is crucial to conduct a study on patients’ delay in seeking treatment and the associated factors among pulmonary TB patients.
Methods and materials
Study design and period
A multicenter institution-based cross-sectional study was conducted from March 10 to August 10, 2020.
Study setting
The study was conducted in the Metekel Zone, Benishangul Gumuz Regional State public health facilities. The Benishangul Gumuz region is located in the western part of the country and is bordered by the Amhara region in the northeast, the Oromia region in the southeast, and Sudan in the west. The Mekel zone is one of the three administrative zones in the region. It comprised seven districts and a one-city administration. The zonal capital, Gilgel Belese town, is situated 446 km west of Addis Ababa. The total population of the zone, as based on the 2007 census projection in 2020, is approximately 468,353, of which 49% were male and 95% were living in rural areas. Agriculture and grazing are the main sources of livelihood in the zone. In the zone, there are 3 public hospitals and 16 public health centers that provide tuberculosis laboratory diagnosis and DOT services to the community. A total of 1,100 health care professionals were working in these institutions, and a total of 825 PTB patients were reported in the zone in 2019.
Population and sample
All adult clients diagnosed with PTB at the DOTs unit of public health facilities of the Metekel zone during the study period were the study population. The sample size of the study was calculated using a single population proportion formula [n = (Zα/2)2 × p(1 − p)/d2] with the following assumptions: the proportion of PTB patients who were delayed in seeking health care from the previous study (53.4%) (16), the probability of type 1 error or alpha 0.05, and the 95% confidence level. The calculated sample size was 382, and the final sample size used in this study was 420 considering a 10% nonresponse rate.
From 16 health centers and 3 hospitals that provide tuberculosis diagnosis and DOT services in the Metekel Zone, 3 health centers were not included in this study due to insecurity in the areas at the time of data collection. All newly diagnosed PTB patients from each DOT center of the 16 public health facilities (3 hospitals and 13 health centers) of the Metekel Zone during the study period were included in the study. Accordingly, the following samples were included from each DOTs center: Mankush HC (34), Dibati HC (30), Gublak HC (18), Manbuk HC (30), Gilgel Beles HC (34), Mender 14 HC (15), F/Selam HC (30), Berber HC (22), Galesa HC (24), Bullen HC (30), Dobi HC (16), Gesgesa HC (15), Debre Zeit HC (32), Pawe Hospital (40), Bullen Hospital (22), and Wombera Hospital (24).
Variables of the study
Dependent variable: Delay in seeking treatment (Delayed or Not Delayed).
Independent variables:
Sociodemographic variables: Age, sex, marital status, residence, educational status, household size, occupation, family income, and time to reach the nearest health facility.
Clinical and behavioral variables: Status of a patient at the first visit, comorbidity, contact history to TB patient, history of a visit to informal care providers, types of treatment center, history of smoking, alcohol drinking status, and knowledge about TB.
Operational definition
Delay in seeking treatment
This is the time interval between the onset of patient-recognized PTB symptom(s) and consultation with a healthcare provider. TB patients who consulted a formal health care provider longer than 21 days (2 weeks entry point for presumptive TB case and 1 week period to seek health care) after the onset of initial constitutional signs and symptoms of TB were considered delayed (11, 20, 21).
Knowledge of TB
Six item questions about knowledge of TB (causes, symptoms, mechanism of transmission, curability, the existence of vaccine) were used, and variables measuring knowledge were recorded on a 3-point Likert scale (0–worst and 2-best). We assessed the reliability of items used to measure knowledge about TB, and we found a Cronbach alpha of 0.73. Patients who scored more than average were considered to have good knowledge, and those who scored less than average (50%) were considered to have poor knowledge (11, 22).
Informal healthcare providers are drug shops/vendors, traditional injectors/healers, religious institutions, etc. (23).
Smear-positive PTB
A person who has at least one positive result on AFB microscopy or a person whose Xpert MTB/RIF test result detected mycobacteria with susceptibility to rifampicin (24).
Smear-negative PTB
Patient with symptoms suggestive of TB, with at least two sputum specimens that were negative for AFB by microscopy and in whom Xpert MTB/RIF test results detect no mycobacterium; the decision to empirically treat with a full course of Anti-TB regimen is made with the help of evidence from supporting tests and with aid of sound clinical decision (24).
Data collection tools and procedure
An interviewer-administered structured questionnaire adapted from previous studies (8, 25) was used to collect sociodemographic, clinical, behavioral, and other variables related to TB treatment delay. The self-reported date of onset for the illness was taken as the date of onset of signs and symptoms for tuberculosis. Cough was taken as the main symptom, followed by nonspecific systemic symptoms such as chest pain, fever, night sweats, shortness of breath, and loss of weight taken as the onset of illness, whichever came first used to count the date of patient care seeking.
At each study site, we recruited a nurse with a degree in nursing and fluent in Amharic, and local languages such as Gumuz and Shinashigna, as data collector Data collectors and supervisors were trained for 1 day on the objective of the study and the basics of interviewing before the actual data collection. The questionnaire was first prepared in English and then translated into Amharic and back to English by language experts to check consistency and conceptual similarity, and it was also pretested at Assossa Health Center. The data collection process was closely monitored by the principal investigator and the supervisors throughout the data collection period. Filled questionnaires were checked regularly for completeness of information, and any problems were immediately discussed with the data collectors.
Data processing and analysis
Data were entered into Epi info version 7 and exported to SPSS version 20 software for analysis. Frequency distribution tables and summary measures such as percentages and medians were used to describe the data. A binary logistic regression model was fitted to identify factors associated with delays in seeking treatment among pulmonary tuberculosis patients. Bivariable analysis was carried out for all independent variables with an outcome variable, and variables with a p value ≤0.2 were entered into a multivariable logistic regression model to identify the independently associated factors of delay in seeking treatment for PTB. The adjusted odds ratio with 95% CI was determined, and variables with a p value ≤0.05 were considered statistically significant.
Results
Sociodemographic characteristics of the study participants
A total of 416 newly diagnosed pulmonary tuberculosis patients were included in the study, with a response rate of 99.5%. The mean age of the study participants was 40 years (SD ± 14 years), and more than half 232 (55.8%) of the patients were males. Nearly two-thirds (268, 64.4%) of the study subjects resided in rural areas. Approximately 161 (38.7%) were farmers by occupation, and 94 (22.6%) patients were not able to read and write. More than half (241, 57.9%) of the participants traveled on foot to the nearest health facility, and 165 (39.7%) reported that it took more than half an hour to reach the nearest health facility (Table 1).
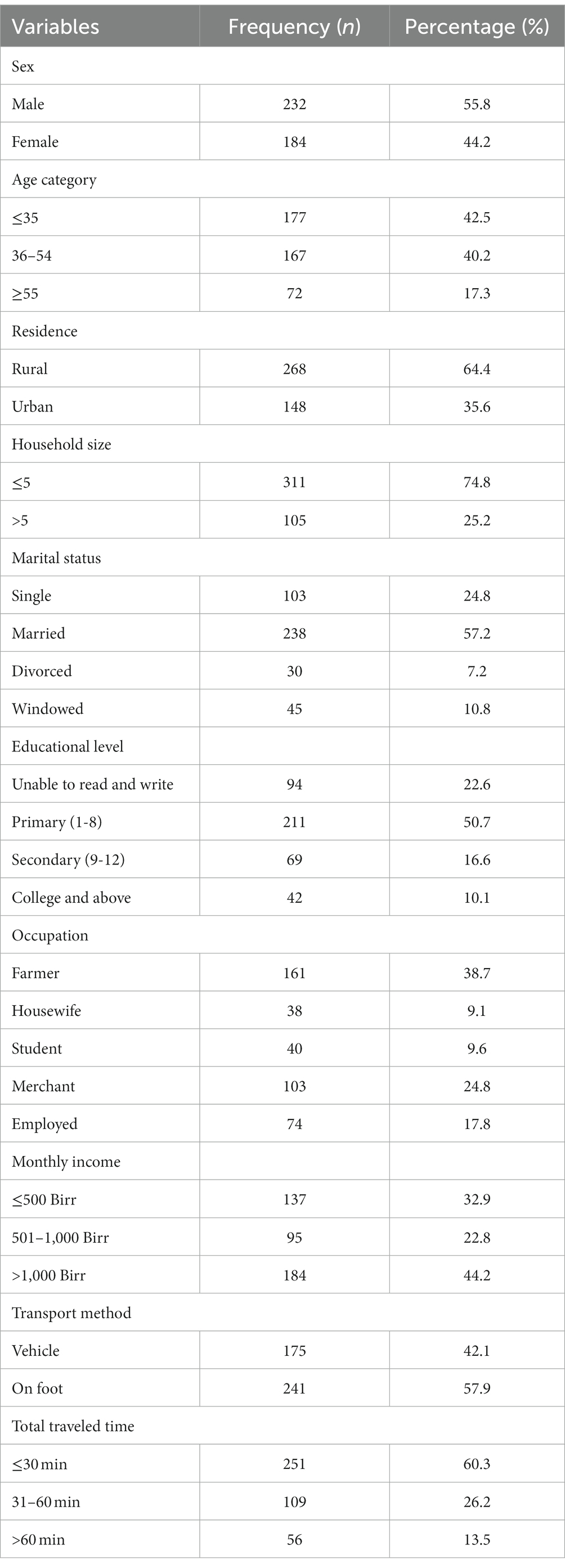
Table 1. Sociodemographic characteristics of PTB patients attending public health facilities in the Metekel Zone, West Ethiopia, 2020 (n = 416).
Clinical and behavioral characteristics of respondents
Of the total participants, 309 (74.3%) were smear-positive, and the majority (407, 97.8%) of patients presented with persistent cough followed by shortness of breath (84, 20.2%). One-third (133, 32%) of the respondents had a history of contact with previous TB patients. Approximately 121 (27%) had comorbidities, of which HIV/AIDS accounted for 49 (40.4%), diabetes accounted for 36 (29.8%), and hypertension accounted for 36 (29.8%). More than two-thirds 283 (68%) of the respondents had poor knowledge of TB. Although most of the study participants (347, 83.4%) had heard about TB before, approximately 330 (79.3%) of the respondents did not know microbes as the cause of TB disease. Nearly half (202, 48.6%) of the participants heard information about TB from their friends or relatives. The majority of respondents did not know about the symptoms (238, 57.2%) and contagiousness (267, 64.2%) of TB. Of the total participants, 18 (4.3%) were smokers, and 83 (20%) were current alcohol drinkers (Table 2).
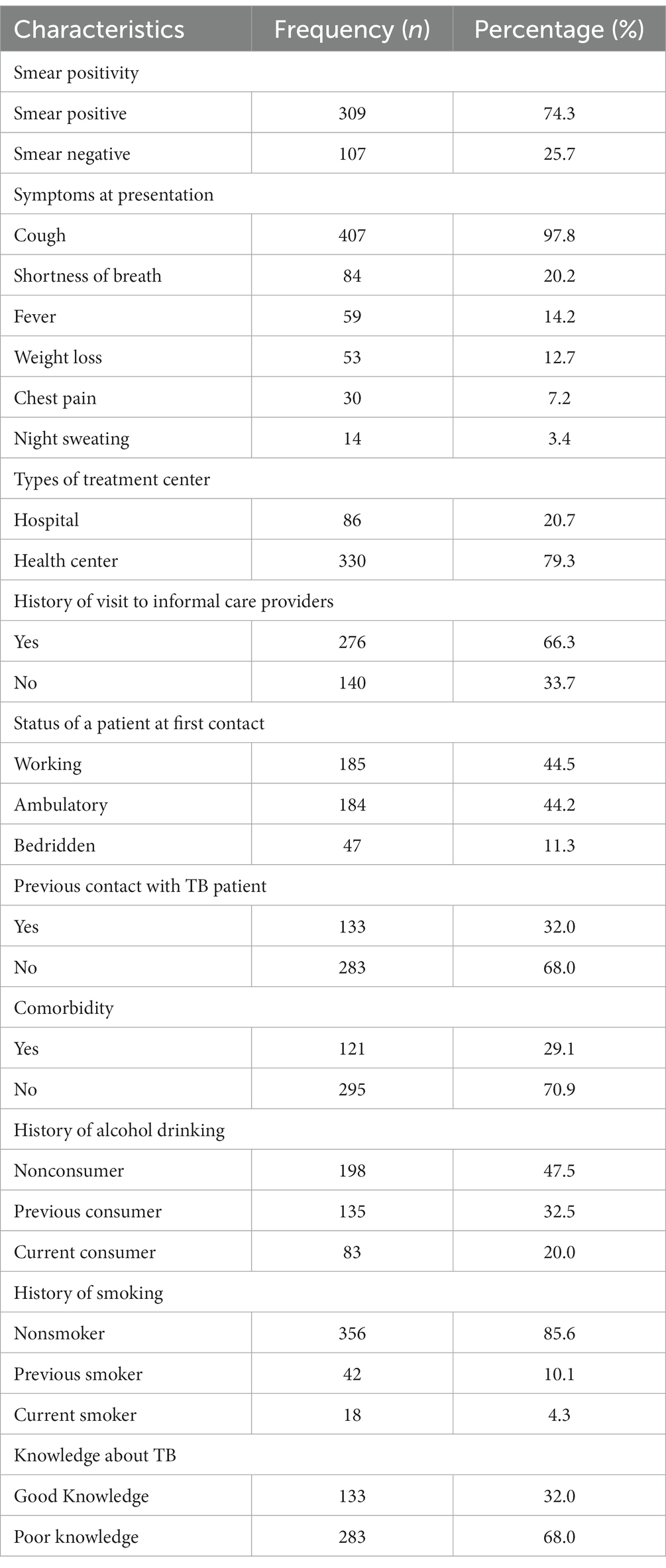
Table 2. Clinical and behavioral characteristics of PTB patients attending public health facilities in the Metekel Zone, West Ethiopia, 2020 (n = 416).
Proportion of pulmonary tuberculosis patients who delayed seeking treatment
Nearly three-fourths 302 (72.6, 95% CI: 68.5, 76.7) of the patients were delayed in seeking medical advice, which means they visited health institutions 21 days after the onset of their illness. Two-thirds 276 (66.3%) of the participants had a history of visits to informal health care providers for the current symptoms before they came to the current health facilities from which 90 (21.6%) visited drug vendors. The median patient delay was 27 days (IQR: 21–31), with minimum and maximum delays of 10 and 120 days, respectively.
Factors associated with delay in seeking treatment among pulmonary tuberculosis patients
In this study, age, family size, time to reach the nearest health facility, and knowledge about PTB were significantly associated with delays in seeking treatment among PTB patients.
The odds of delay in seeking treatment for PTB were 2.65 times higher (AOR = 2.65, 95% CI: 1.30, 5.40) among patients aged above 54 years and 1.86 times higher (AOR = 1.86, 95% CI: 1.14,3.02) among patients aged 36–54 years than among patients aged less than 35 years. Tuberculosis patients with family sizes of 5 and above were 1.62 times more likely (AOR = 1.62, 95% CI: 1.10–3.14) to delay seeking treatment than those with a family size of fewer than 5 members. The odds of delay in seeking treatment among PTB patients who traveled above 60 min to reach a nearby health facility were 3.65 times higher (AOR = 3.65, 95% CI: 1.55, 8.60) than those who traveled less than 30 min. Patients who had a history of visits to informal care providers were 1.74 times more likely (AOR = 1.74, 95% CI: 1.11, 3.14) to delay seeking treatment from formal care providers than their counterparts. Tuberculosis patients who had poor knowledge about PTB were 1.64 times more likely (AOR = 1.64, 95% CI: 1.04–2.44) to delay seeking treatment than patients with good knowledge (Table 3).
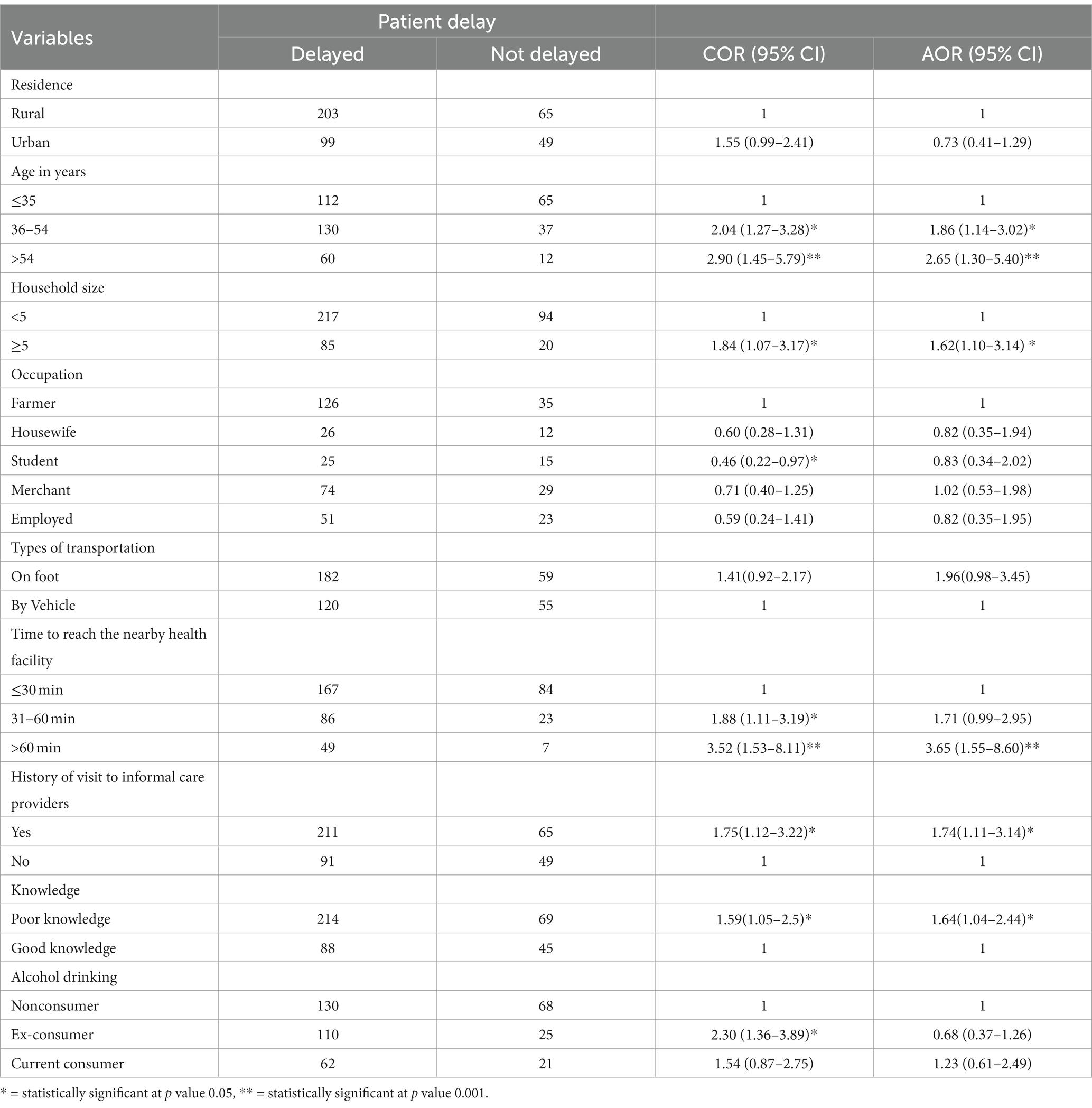
Table 3. Factors associated with patients’ delay in PTB treatment in public health facilities in the Metekel Zone, West Ethiopia, 2020 (n = 416).
Discussion
In the current study, the majority (72.6%) of patients were delayed in seeking medical advice beyond the WHO-recommended time, which is 21 days since they first experienced symptoms of tuberculosis (25). This finding is consistent with a nationwide study conducted in Ethiopia 72.3% (26), Northwest Ethiopia (68.7%) (27), India (73.7) (28), and Tanzania (71%) (29). However, it is higher than studies conducted in other parts of the country, such as Bahirdar (62%) (30), Hadiya (58.2%) (30), North Shewa (59.9%) (12), and Addis Ababa (42.1%) (11), as well as studies in Zimbabwe (48%) (31), Kenya (65.4%) (32), Nigeria (42%) (33), and Ghana (60.3%) (34). This implies that a large proportion of TB patients continued to serve as reservoirs of infection and would have continued to transmit the disease in the community.
In our study, the median patient delay was 27 days. This finding is consistent with studies conducted in other parts of Ethiopia (13, 20, 30, 35), Zimbabwe (31), Kenya (36), and Uganda (37), which revealed a median patient delay of 25–30 days. However, the median patient delay in our study was higher than that in studies in different areas of Ethiopia (17–21 days) (11, 14, 26, 28) and Nigeria (8 days) (39). This difference may be due to sociocultural differences between study participants since our study was conducted in one of the developing regional states of the country, Benishangul Gumuz. In our study, two-thirds of the study participants visited informal health care providers such as religious institutions, self-treatment from drug vendors and traditional healers before seeking care at public health institutions, which contributed to a higher median patient delay. This finding highlights the need to improve patients’ health-seeking behavior by raising community awareness about the importance of the early recognition of PTB symptoms.
Furthermore, patients older than 54 years and patients aged 36–54 years were more likely to experience prolonged delays in seeking treatment compared to patients under 35 years. This finding is consistent with studies conducted in Ethiopia (9, 16, 30, 38), Nigeria (39), Portugal (40), and Tanzania (29). This may be related to the fact that older people may depend on others, making it difficult for them to visit health facilities at their preferred time. Patients between the ages of 36 and 54 are productive and independent but are also more likely to have larger family sizes than patients under the age of 35, which can burden them with other family matters and delay their visits to healthcare facilities for their symptoms.
The time taken to reach a health facility was a significant factor associated with delays in seeking treatment among PTB patients. Patients who traveled more than an hour to reach a nearby health facility had a threefold increased delay in seeking treatment compared to those who traveled less than 30 min. This finding is supported by studies from different parts of Ethiopia (11, 41), China (42), Italy (43), Nigeria (39), and Nepal (44). This might be due to the difficulties in accessing health facilities, and it is crucial to utilize health extension workers to improve the detection of presumed tuberculosis cases at the community level.
Tuberculosis patients with a family size of five members or more were more likely to delay seeking treatment compared to those with smaller families. This finding is consistent with studies conducted in the Eastern and Southern parts of Ethiopia (9, 13). A larger family size may lead to increased responsibilities and financial constraints, which can hinder timely visits to healthcare facilities for their illnesses.
Patients who had a history of visits to informal care providers were nearly twice as likely to delay seeking treatment from formal care providers as their counterparts. This finding is consistent with previous studies in Ethiopia (14–16, 38, 41), Mozambique (45), and Zimbabwe (31). In our study, two-thirds of the patients initially sought care from informal providers before coming to health institutions. This indicates a higher preference for informal treatments among TB patients, which may increase the risk of community transmission and the severity of the illness. Therefore, increasing awareness about the disease and utilizing the aid of informal health care providers, such as traditional or religious healers and drug vendors, in the referral process can help in the early identification of suspected TB cases and prompt linkage to DOT centers.
Knowledge about tuberculosis was also found to be an important factor associated with delays in seeking treatment. Patients with poor knowledge about PTB were 1.64 times more likely to delay seeking treatment than patients with good knowledge. This finding is similar to studies conducted in other parts of Ethiopia (15, 16, 20, 38), Nigeria (33), and Mozambique (45). This demonstrates how patients with limited understanding of the signs and natural course of the disease thought that their symptoms would eventually go away or that they would seek out alternative therapies from informal providers such as traditional or religious healers or engage in self-medication with over-the-counter medications, leading to delays in seeking medical advice.
In light of our findings, it is imperative to consider strategic interventions aimed at reducing delays in seeking treatment among pulmonary TB patients. Implementing targeted public health campaigns could play a pivotal role in enhancing public awareness regarding the importance of early TB detection and timely treatment (46). Community engagement, especially involving community leaders, is instrumental in reshaping healthcare-seeking behaviors (47). Establishing collaborative efforts with community leaders can facilitate the dissemination of accurate information about TB, dispelling myths, and encouraging individuals to seek formal medical care promptly (48). The introduction of community screening programs is another key strategy to address delays in seeking treatment (49). By bringing TB testing and treatment closer to communities, these programs can overcome barriers related to geographical distance and contribute to early case detection.
Limitation of study
One potential limitation of this study is the possibility of recall bias, as patients may not accurately estimate or remember the exact date of onset of their illness. Additionally, this study may not be generalizable to all pulmonary tuberculosis patients since it did not include participants from private health facilities.
Conclusion
The majority of pulmonary tuberculosis patients delay seeking medical advice for their illnesses. Factors associated with these delays included older age, large household size, longer travel time to reach the nearby health facility, visits to informal care providers, and poor knowledge about pulmonary tuberculosis. Therefore, it is important to strengthen community awareness activities, introduce community screening programs, and ensure the accessibility of TB diagnostic and treatment services.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Review Board (IRB) of the Institute of Public Health, University of Gondar, Ethiopia. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because since the study was an observational study based on interviews it doesn't have any risk, But we obtained informed verbal consent.
Author contributions
YA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. AG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Writing – review & editing. SN: Formal analysis, Investigation, Methodology, Software, Supervision, Writing – review & editing. SA: Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank Benshangul Gumuz Regional Health Bureau and Metekel Zone Health Office for technical support. We would also like to extend our gratitude to the supervisors, data collectors, and study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AFB, Acid Fast Baccili; AIDS, Acquired Immuno Deficiency Syndrome; AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; DOTS, Directly Observed Treatments; HC, Health Center; HIV, Human Immune Deficiency Virus; IQR, Inter Quartile Range; km, Kilo Meter; MDR-TB, Multidrug Resistant Tuberculosis; MTB/RIF, Mycobacterium Tuberculosis Rifampicillin Resistant; PTB, Pulmonary Tuberculosis; SD, Standard Deviation; SDGs, Sustainable Development Goals; SPSS, Statistical Package for Social Science; TB, Tuberculosis; WHO, World Health Organization.
References
2. World Health Organization. First WHO global ministerial conference: Ending TB in the sustainable development era: A multisectoral response: 16–17 November 2017. Moscow: Russian Federation, World Health Organization (2017).
3. World Health Organization. Tuberculosis key facts 2019. (2019). Available at: https://www.who.int/news-room/fact-sheets/detail/tuberculosis.
4. World Health Organization. Global tuberculosis report 2019 Geneva (2019). Available at: https://www.who.int/publications/i/item/9789241565714.
5. United Nations. Sustainable Development Goals. (2023). Available at: https://www.un.org/sustainabledevelopment/health/.
6. World Health Organization. Implementing the end TB strategy: the essentials. Geneva: World Health Organization (2015).
7. Federal Democratic Republic of Ethiopia Ministry of Health. Guidelines for clinical and programmatic management of TB, TB/HIV and leprosy. 6th ed. Addis Ababa, Ethiopia: Federal Democratic Republic of Ethiopia Ministry of Health (2016).
8. Getnet, F, Demissie, M, Assefa, N, Mengistie, B, and Worku, A. Delay in diagnosis of pulmonary tuberculosis in low-and middle-income settings: systematic review and meta-analysis. BMC Pulm Med. (2017) 17:1–15. doi: 10.1186/s12890-017-0551-y
9. Seid, A, and Metaferia, Y. Factors associated with treatment delay among newly diagnosed tuberculosis patients in Dessie city and surroundings, northern Central Ethiopia: a cross-sectional study. BMC Public Health. (2018) 18:931. doi: 10.1186/s12889-018-5823-9
10. Hussen, A, Biadgilign, S, Tessema, F, Mohammed, S, Deribe, K, and Deribew, A. Treatment delay among pulmonary tuberculosis patients in pastoralist communities in bale zone, Southeast Ethiopia. BMC Res Notes. (2012) 5:320. doi: 10.1186/1756-0500-5-320
11. Adenager, GS, Alemseged, F, Asefa, H, and Gebremedhin, AT. Factors associated with treatment delay among pulmonary tuberculosis patients in public and private health facilities in Addis Ababa, Ethiopia. Tuberc Res Treat. (2017) 2017:5120841. doi: 10.1155/2017/5120841
12. Shiferaw, MB, and Zegeye, AM. Delay in tuberculosis diagnosis and treatment in Amhara state, Ethiopia. BMC Health Serv Res. (2019) 19:232. doi: 10.1186/s12913-019-4056-7
13. Asefa, ATW. Total delay in treatment among smear positive pulmonary tuberculosis patients in five primary health centers, southern Ethiopia: a cross sectional study. PLoS One. (2014) 9:e102884. doi: 10.1371/journal.pone.0102884
14. Belay, M, Bjune, G, Ameni, G, and Abebe, F. Diagnostic and treatment delay among tuberculosis patients in Afar region, Ethiopia: a cross-sectional study. BMC Public Health. (2012) 12:369. doi: 10.1186/1471-2458-12-369
15. Alema, HB, Hailemariam, SA, Misgina, KH, Weldu, MG, Gebregergis, YS, Mekonen, GK, et al. Health care seeking delay among pulmonary tuberculosis patients in north west zone of Tigrai region, North Ethiopia. BMC Infect Dis. (2019) 19:309. doi: 10.1186/s12879-019-3893-7
16. Asres, M, Gedefaw, M, Kahsay, A, and Weldu, Y. Patients' delay in seeking health Care for Tuberculosis Diagnosis in east Gojjam zone, Northwest Ethiopia. Am J Trop Med Hyg. (2017) 96:1071–5. doi: 10.4269/ajtmh.16-0892
17. Gebeyehu, E, Azage, M, and Abeje, G. Factors associated with patient's delay in tuberculosis treatment in Bahir Dar City administration, Northwest Ethiopia. Biomed Res Int. (2014) 2014:701429:1–6. doi: 10.1155/2014/701429
18. Bogale, S, Diro, E, Shiferaw, AM, and Yenit, MK. Factors associated with the length of delay with tuberculosis diagnosis and treatment among adult tuberculosis patients attending at public health facilities in Gondar town, northwest, Ethiopia. BMC Infect Dis. (2017) 17:145. doi: 10.1186/s12879-017-2240-0
19. Federal Ministry of Health Ethiopia. Health and health related indicators. Addis Ababa, Ethiopia: Federal Ministry of Health Ethiopia (2015).
20. Osei, E, Akweongo, P, and Binka, F. Factors associated with DELAY in diagnosis among tuberculosis patients in Hohoe municipality, Ghana. BMC Public Health. (2015) 15:721. doi: 10.1186/s12889-015-1922-z
21. Fuge, TG, Bawore, SG, Solomon, DW, and Hegana, TY. Patient delay in seeking tuberculosis diagnosis and associated factors in Hadiya zone, southern Ethiopia. BMC Res Notes. (2018) 11:115. doi: 10.1186/s13104-018-3215-y
22. Bassili, A, Seita, A, Baghdadi, S, AlAbsi, A, Abdilai, I, Agboatwalla, M, et al. Diagnostic and treatment delay in tuberculosis in 7 countries of the eastern Mediterranean region. Infect Dis Clin Pract. (2008) 16:23–35. doi: 10.1097/IPC.0b013c31815d8d61
23. Federal Democratic Republic of Ethiopia Ministry of Health. National guidelines for TB, DR-TB and leprosy in Ethiopia. Addis Ababa: MoH (2017).
24. Nyatichi, FO, Amimo, FA, Nabie, B, and Ondimu, TO. Factors contributing to delay in seeking treatment among pulmonary tuberculosis patients in Suneka Sub-County, Kenya. J Health Educ Res Dev. (2016) 4:170. doi: 10.4172/2380-5439.1000170
25. Santos, JA, Leite, A, Soares, P, Duarte, R, and Nunes, C. Delayed diagnosis of active pulmonary tuberculosis - potential risk factors for patient and healthcare delays in Portugal. BMC Public Health. (2021) 21:2178. doi: 10.1186/s12889-021-12245-y
26. Wondawek, TM, and Ali, MM. Delay in treatment seeking and associated factors among suspected pulmonary tuberculosis patients in public health facilities of Adama town, eastern Ethiopia. BMC Public Health. (2019) 19:1527. doi: 10.1186/s12889-019-7886-7
27. Federal Ministry of Health. Guidelines for clinical and programmatic management of TB, TB/HIV and leprosy in Ethiopia. Addis Ababa: Federal Ministry of Health of Ethiopia (2013).
28. Das, S, Basu, M, Mandal, A, Roy, N, Chatterjee, S, and Dasgupta, A. Prevalence and determinants of delay in diagnosis of pulmonary tuberculosis in Darjeeling district of West Bengal. J Family Med Prim Care. (2017) 6:627–35. doi: 10.4103/2249-4863.214432
29. World Health Organization. Early detection of tuberculosis: An overview of approaches, guidelines and tools. Geneva: World Health Organization (2011).
30. Datiko, DG, Jerene, D, and Suarez, P. Patient and health system delay among TB patients in Ethiopia: Nationwide mixed method cross-sectional study. BMC Public Health. (2020) 20:1–10. doi: 10.1186/s12889-020-08967-0
31. Yimer, SA, Bjune, GA, and Holm-Hansen, C. Time to first consultation, diagnosis and treatment of TB among patients attending a referral hospital in northwest, Ethiopia. BMC Infect Dis. (2014) 14:19. doi: 10.1186/1471-2334-14-19
32. Van Ness, SE, Chandra, A, Sarkar, S, Pleskunas, J, Ellner, JJ, Roy, G, et al. Predictors of delayed care seeking for tuberculosis in southern India: an observational study. BMC Infect Dis. (2017) 17:1–9. doi: 10.1186/s12879-017-2629-9
33. Tarimo, GB. Delay in seeking care among tuberculosis patients attending tuberculosis clinics in Rungwe district. Tanzania: Muhimbili University of Health and Allied Sciences (2012).
34. Takarinda, KC, Harries, AD, Nyathi, B, Ngwenya, M, Mutasa-Apollo, T, and Sandy, C. Tuberculosis treatment delays and associated factors within the Zimbabwe national tuberculosis programme. BMC Public Health. (2015) 15:29. doi: 10.1186/s12889-015-1437-7
35. Biya, O, Gidado, S, Abraham, A, Waziri, N, Nguku, P, Nsubuga, P, et al. Knowledge, care-seeking behavior, and factors associated with patient delay among newly-diagnosed pulmonary tuberculosis patients, Federal Capital Territory, Nigeria, 2010. Pan Afr Med J. (2014) 18:6. doi: 10.11694/pamj.supp.2014.18.1.4166
36. Asres, A, Jerene, D, and Deressa, W. Delays to anti-tuberculosis treatment intiation among cases on directly observed treatment short course in districts of southwestern Ethiopia: a cross sectional study. BMC Infect Dis. (2019) 19:481. doi: 10.1186/s12879-019-4089-x
37. Kunjok, DM, Mwangi, JG, Mambo, S, and Wanyoike, S. Assessment of delayed tuberculosis diagnosis preceding diagnostic confirmation among tuberculosis patients attending Isiolo County level four hospital, Kenya. Pan Afr Med J. (2021) 38:51. doi: 10.11604/pamj.2021.38.51.21508
38. Buregyeya, E, Criel, B, Nuwaha, F, and Colebunders, R. Delays in diagnosis and treatment of pulmonary tuberculosis in Wakiso and Mukono districts, Uganda. BMC Public Health. (2014) 14:586. doi: 10.1186/1471-2458-14-586
39. Gebreegziabher, SB, Bjune, GA, and Yimer, SA. Patients’ and health system’s delays in the diagnosis and treatment of new pulmonary tuberculosis patients in west Gojjam zone, Northwest Ethiopia: a cross-sectional study. BMC Infect Dis. (2016) 16:673. doi: 10.1186/s12879-016-1995-z
40. Ukwaja, KN, Alobu, I, Nweke, CO, and Onyenwe, EC. Healthcare-seeking behavior, treatment delays and its determinants among pulmonary tuberculosis patients in rural Nigeria: a cross-sectional study. BMC Health Serv Res. (2013) 13:1–9. doi: 10.1186/1472-6963-13-25
41. Getnet, F, Demissie, M, Worku, A, Gobena, T, Seyoum, B, Tschopp, R, et al. Determinants of patient delay in diagnosis of pulmonary tuberculosis in Somali pastoralist setting of Ethiopia: a matched case-control study. Int J Environ Res Public Health. (2019) 16:3391. doi: 10.3390/ijerph16183391
42. Tong, Y, Guan, X, Hou, S, Cai, L, Huang, Y, Wang, L, et al. Determinants of health care-seeking delay among tuberculosis patients in rural area of Central China. Int J Environ Res Public Health. (2018) 15:1998. doi: 10.3390/ijerph15091998
43. Quattrocchi, A, Barchitta, M, Nobile, C, Prato, R, Sotgiu, G, Alessandra Casuccio, A, et al. TB network. Determinants of patient and health system delay among Italian and foreignborn patients with PULMONARY TB: a multicentre cross-sectional study. BMJ Open. (2013) 8:e019673. doi: 10.1136/bmjopen-2017-019673
44. Laohasiriwong, W, Mahato, RK, Koju, R, and Vaeteewootacharn, K. Delay for first consultation and its associated factors among new pulmonary tuberculosis patients of Central Nepal. Tuberc Res Treat. (2016) 2016:1–8. doi: 10.1155/2016/4583871
45. Saifodine, A, Gudo, PS, Sidat, M, and Black, J. Patient and health system delay among patients with pulmonary tuberculosis in Beira city, Mozambique. BMC Public Health. (2013) 13:559. doi: 10.1186/1471-2458-13-559
46. Samal, J, and Dehury, RK. Impact of a structured tuberculosis awareness strategy on the knowledge and behaviour of the families in a slum area in Chhattisgarh, India. J Clin Diagn Res. (2017) 11:Lc11–5. doi: 10.7860/JCDR/2017/24107.9489
47. Querri, A, Ohkado, A, Yoshimatsu, S, Coprada, L, Lopez, E, Medina, A, et al. Enhancing tuberculosis patient detection and care through community volunteers in the urban poor, the Philippines. Public Health Action. (2017) 7:268–74. doi: 10.5588/pha.17.0036
48. Hadley, M, and Maher, D. Community involvement in tuberculosis control: lessons from other health care programmes. Int J Tuberc Lung Dis. (2000) 4:401–8.
49. Feasey, HR, Burke, RM, Nliwasa, M, Chaisson, LH, Golub, JE, Naufal, F, et al. Do community-based active case-finding interventions have indirect impacts on wider TB case detection and determinants of subsequent TB testing behaviour? A systematic review. PLoS Glob Public Health. (2021) 1:e0000088. doi: 10.1371/journal.pgph.0000088
Keywords: patient delay, pulmonary tuberculosis, treatment, Western Ethiopia, associated factors
Citation: Animut Y, Godno AB, Nigatu SG and Abiy SA (2024) Delay in seeking treatment and associated factors among pulmonary tuberculosis patients attending public health facilities in the Metekel zone, Benishangul Gumuz region, Western Ethiopia. Front. Public Health. 12:1356770. doi: 10.3389/fpubh.2024.1356770
Edited by:
Faris Lami, University of Baghdad, IraqReviewed by:
Layth Al-Salihi, National Tuberculosis Institute, IraqMudher Al-Khairalla, NHS Tayside, United Kingdom
Copyright © 2024 Animut, Godno, Nigatu and Abiy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yaregal Animut, eWFyZWdhbGFlQGdtYWlsLmNvbQ==
 Yaregal Animut
Yaregal Animut Abera Birhanu Godno2
Abera Birhanu Godno2 Solomon Gedlu Nigatu
Solomon Gedlu Nigatu Saron Abeje Abiy
Saron Abeje Abiy