
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 23 July 2024
Sec. Life-Course Epidemiology and Social Inequalities in Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1356430
This article is part of the Research Topic Reviews in Social Determinants in Epidemiology and Disease Prevention View all 7 articles
Background: It has been recognized that HIV-related stigma hinders efforts in testing, treatment, and prevention. In this systematic review, we aimed to summarize available findings on the association between HIV-related stigma and age, social support, educational status, depression, employment status, wealth index, gender, residence, knowledge about HIV, marital status, duration since diagnosis, and disclosure status using a large number of studies.
Methods: Electronic databases including Scopus, Medline/PubMed, Web of Sciences (WOS), Cochrane Library, Google Scholar, and Open Research Dataset Challenge were systematically searched until 15 April 2023. We included all kinds of HIV-stigma studies, regardless of language, publishing date, or geographic location. The inclusion criteria were met by 40 studies, with a total of 171,627 patients. A mixed-effect model was used to pool estimates and evaluate publication bias, as well as to conduct sensitivity analysis.
Results: Factors such as older age, social support, greater education, higher socioeconomic status, good knowledge of HIV, and longer years of living with HIV significantly lowered the likelihood of HIV-related stigma. Contrarily, factors such as depression, residing in rural areas, female respondents, and non-disclosure of HIV status were significantly associated with a high risk of HIV-related stigma.
Conclusion: To combat systemic HIV-associated stigma, it is crucial to develop wholesome and comprehensive social methods by raising community-level HIV awareness. In addition to activism, local economic development is also crucial for creating thriving communities with a strong social fabric.
HIV-related stigma and discrimination pose significant obstacles to HIV responses. Progress has thus far been stalled by fragmented efforts to fight HIV-related stigma and prejudice (1). It is important to analyze the various existing measures to derive lessons that can guide future interventions and strengthen the evidence base on HIV-related stigma.
HIV-related stigma is defined by stigmatizing actions such as treating people differently, verbally abusing them, undervaluing them, and rejecting them in social settings (2, 3). According to the Joint United Nations Programme on HIV/AIDS (UNAIDS), HIV-related stigma is defined as negative attitudes, feelings, and beliefs toward people living with HIV, groups associated with people living with HIV (PLWH), and other important populations at a higher risk of contracting HIV (1). There are three wars through which people who live with HIV may feel stigmatized: Internalized stigma, anticipated stigma, and enacted stigma (4). Internalized stigma is the acceptance of unfavorable thoughts, opinions, and sentiments about oneself in relation to one's HIV-positive status (5). Anticipated stigma is the awareness of unfavorable social attitudes regarding HIV and the expectation that an HIV-positive individual would eventually face prejudice and discrimination (6). Enacted stigma describes the prejudice that HIV-positive individuals encounter, and it may take the form of violence and marginalization (7).
Experiences of stigmatization have been linked to poorer quality of life, poorer mental health and wellbeing, and reduced access to care for people with HIV (8). Numerous studies have emphasized the detrimental effects of HIV-related stigma on those who are living with the virus. For instance, in recent research on HIV-related stigma, stigma was found to be associated with poorer mental health outcomes, including anxiety (6, 9), depression (10, 11), emotional distress (12), and life satisfaction (13, 14). Research conducted by Turan et al. (15) demonstrated that HIV-related stigma within communities can lead individuals living with HIV to internalize stigma and expect stigmatizing encounters, which can subsequently lead to negative health and psychosocial consequences. Furthermore, a meta-analysis by Rueda et al. (6) found high levels of stigma to be linked to risky sexual behavior, depression, lower medication adherence, reduced use of health and social services, anxiety, negative self-image, poorer quality of life, mental distress, and reduced social support from friends, family, and health services. These findings imply that stigma associated with HIV can have a negative effect on people living with HIV in terms of a variety of health-related outcomes.
Although several studies (8, 16–21) have been carried out to identify potential risk factors of HIV-related stigma, there remains a scarcity of research demonstrating the common causes of HIV-related stigma. Numerous studies have investigated various factors associated with HIV-related stigma; however, they have often been confined to specific geographic areas, cases, or characteristics. Therefore, the objective of this study was to evaluate a wide range of HIV-related stigma risk factors by summarizing findings from over 40 scientific research articles.
To investigate the relationship between high levels of HIV-related stigma and age, social support, educational status, depression, employment status, wealth index, gender, residence, knowledge about HIV, marital status, duration since diagnosis, and disclosure status, we followed PRISMA criteria (22) to perform a meta-analysis of articles identified through our reviews.
A comprehensive search was conducted until 15 April 2023, across the following electronic databases: EMBASE, Scopus, Medline/PubMed, Web of Sciences (WOS), Google Scholar, Cochrane Library, and Open Research Dataset. The search terms used in the strategy were “HIV-related stigma” and/or “internalized stigma,” “anticipated stigma,” and “enacted stigma.” In addition, the search was limited to studies that considered sociodemographic traits, risk factors, and clinical aspects as possible indicators of high levels of stigma associated with HIV. No restrictions were applied regarding the timing and language of the publications. We downloaded the literature results into EndNote X9 to speed up the screening process and save time.
The initial search results were evaluated for relevancy using titles and abstracts after removing duplicates. The eligibility requirements were examined in all the studies (Figure 1). The analysis did not include studies without a full text and/or abstract, expert opinion pieces, novels, theses, editorials, or review articles. It also did not include correspondence letters. In addition, we only utilized studies from the eligible literature if they provided odds ratios (ORs) or estimated coefficients (β) together with 95% confidence intervals (CI) for the correlation between risk factors, epidemiological factors, or demographic variables and HIV-related stigma.
Both authors separately evaluated the downloaded EndNoteX9 search outputs' suitability for inclusion. Any disagreements between the authors were resolved through dialogue and consensus. Both extracted information about the sample size, outcome, publication year, author's name, countries, study design, variables (e.g., age, social support, educational status, depression, employment status, wealth index, gender, residence, knowledge about HIV, marital status, duration since diagnosis, and disclosure status), and odds ratios (ORs) or estimated coefficients (β). The authors independently assessed the quality of the methodological approaches of the studies by using the Newcastle–Ottawa method (23). In this method, the comparability of study groups, the evaluation of results, and patient selection were used as three key components to gauge the quality of the studies. Each of the seven domains in the Newcastle–Ottawa method was given a score between 3 and 0 (from low to high bias), and the average score was then calculated.
The eligible studies used various measures to assess HV/AIDS stigma, and the most common were the Berger HIV Stigma Scale (24), the HIV Stigma Measure (25, 26), and the Internalized HIV Stigma instrument (27). When studies reported multiple forms of HIV-related stigma, such as internalized stigma, personalized stigma, self-stigma, enacted stigma, and/or aggregated stigma, the finding that was most strongly associated with the outcome was chosen. The tools in the Berger HIV Stigma Scale consist of four subscales: (1) negative self-image, (2) disclosure concerns, (3) public attitudes, and (4) personalized stigma. Each question can be rated based on a 4-point Likert scale (strongly disagree, disagree, agree, and strongly agree). The overall stigma score is dichotomized as “high level of stigma” if the participants' score is greater than or equal to the mean score scales, or otherwise “low level of stigma (24).” Moreover, the adapted 10-item HIV Stigma Scale by Wright et al. (26) gauges anticipated stigma, personalized stigma, and negative self-image while also generating an overall stigma assessment. Each item employs a 5-point Likert scale, spanning from 1 (“strongly disagree”) to 5 (“strongly agree”). An overall stigma score from 0 to 100 is computed by adjusting each item's values. Based on the mean, both an overall stigma measure and sub-dimensional measures are categorized, which results in a binary assessment of higher or lower stigma levels.
The effect size statistic was defined as the association between HIV-related stigma and covariates. We examined the link between HIV-related stigma and risk factors from peer-reviewed published research using odds ratios (ORs) or estimated coefficients (β) (with 95%CI). We calculated a mixed-effect model, taking into account the anticipated between-study heterogeneity. We calculated Cochran's Q test and the I2 statistic measure to evaluate the heterogeneity. The Cochran's Q test was employed to ascertain whether there was heterogeneity in effect sizes; a significant Q value indicated heterogeneity as opposed to homogeneity. The I2 statistic was employed to determine the percentage of the total variance that could be attributable to study heterogeneity (28). In addition, mild, moderate, and severe conditions were assigned to I2 levels between 0% and 39%, 40% and 59%, and 60% and 90%, respectively (28). Funnel plots using Egger's weighted regression test were employed to assess publication bias (29). A p-value of 0.05 was considered statistically significant. For each analysis, STATA version 17 and R-4.3.0 statistical tools were used to calculate the pooled estimate and analyze publication bias.
Electronic databases [such as Scopus database, Medline/PubMed, EMBASE, Web of Sciences (WOS), Cochrane Library, and Google Scholar] were used to retrieve a total of 498 titles and abstracts. Duplicate records were eliminated, leaving 182 records that might be relevant. After additional screening, 94 full-text articles were used for the eligibility assessment. These were evaluated under the exclusion criteria, and 87 studies were selected for inclusion. From these 87 studies, 18 qualitative studies and 14 studies with missing data were excluded. A total of 15 studies did not include ORs or β and were thus excluded. Consequently, we only included 40 studies that met all the eligibility requirements (see Figure 1).
A thorough description of all the chosen studies (3–8, 10, 12, 14, 16, 30–45) is provided in Table 1. Most of the studies were released between 2018 and 2022. All the included studies reported a total number of 171,627 patients. Five of them were carried out in the United States, seven in China, four in South Africa, nine in Ethiopia, four in Uganda, two each in Canada and Thailand, one each in India, Kenya, Morocco, Sub-Saharan Africa, Cameroon, and Tanzania, and one in a mixed region. Between 123 and 56,367 patients were included in the sample. In the studies, the participants' age ranged from 42.8 to 68 years (Table 1).
The results from the mixed effect meta-analysis model are shown in Figure 2. We deduced from this plot that, among the studies considered, the prevalence of HIV stigma ranged from a minimum level of 19% (95%CI: 18.9%−20.1%) (31) to a maximum level of 88% (95%CI: 85%−91%) (37). Approximately 171,627 patients were enrolled in the study, of which 69, 978 patients reported high stigma levels, yielding a weighted pooled overall high stigma level of 44% (95% CI, 37%−51%) (Figure 2).
The meta-analysis of 12 studies (16, 32, 36, 38, 40, 42–44, 46, 54, 57, 65) that examined the association between HIV-related stigma and social support among people living with HIV is presented in Figure 3A and Table 2. From the results, we observed that social support reduced the impacts of poor care retention and HIV-related stigma [pooled β: −0.34(95%CI: −0.52, −0.16)]. In Figure 3B, the association between HIV-related stigma and depression is shown to be positive. Depression showed an increased level of stigma, and the pooled estimate was 0.49(95%CI: 0.20, 059). The combined 18 effect sizes from 18 studies (16, 19, 31, 33–35, 39, 40, 42, 47, 48, 51) revealed that the level of HIV-related stigma significantly decreased with an increasing level of education (pooled β: −0.71(95%CI: −1.08, −0.34) (Table 2 and Figure 4A). Furthermore, from socioeconomic factors, it was observed that the level of HIV-related stigma significantly decreased among patients who were richer [pooled β: −0.43(95%CI: −0.64, −0.22)] (Figure 5A) and employed (pooled β: −0.57(95%CI: −1.52, −0.37) (Figure 4B), as compared to patients who were poorer and unemployed.
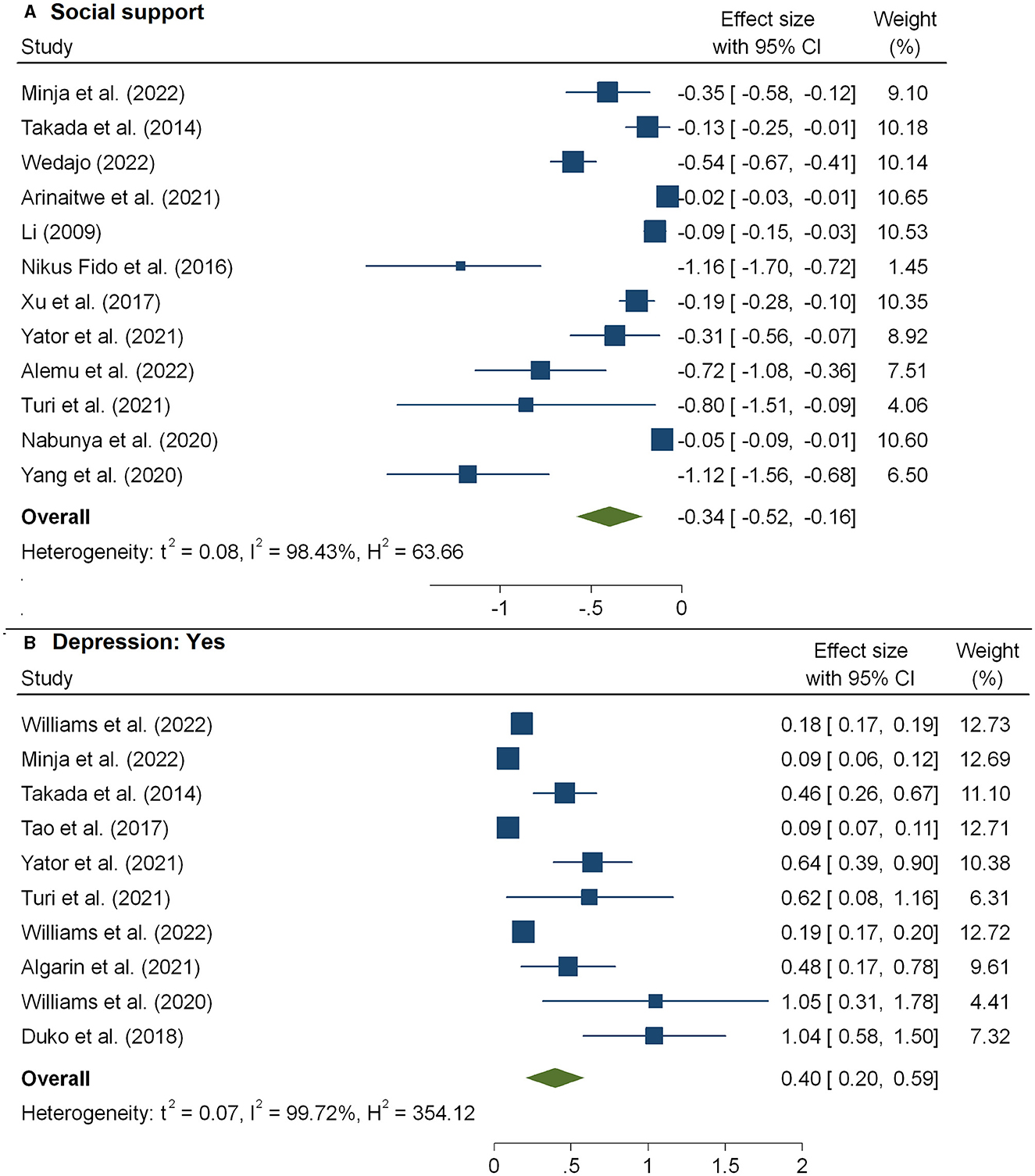
Figure 3. The pooled effect size showing the association between HIV-related stigma and social support (A) and depression (B).
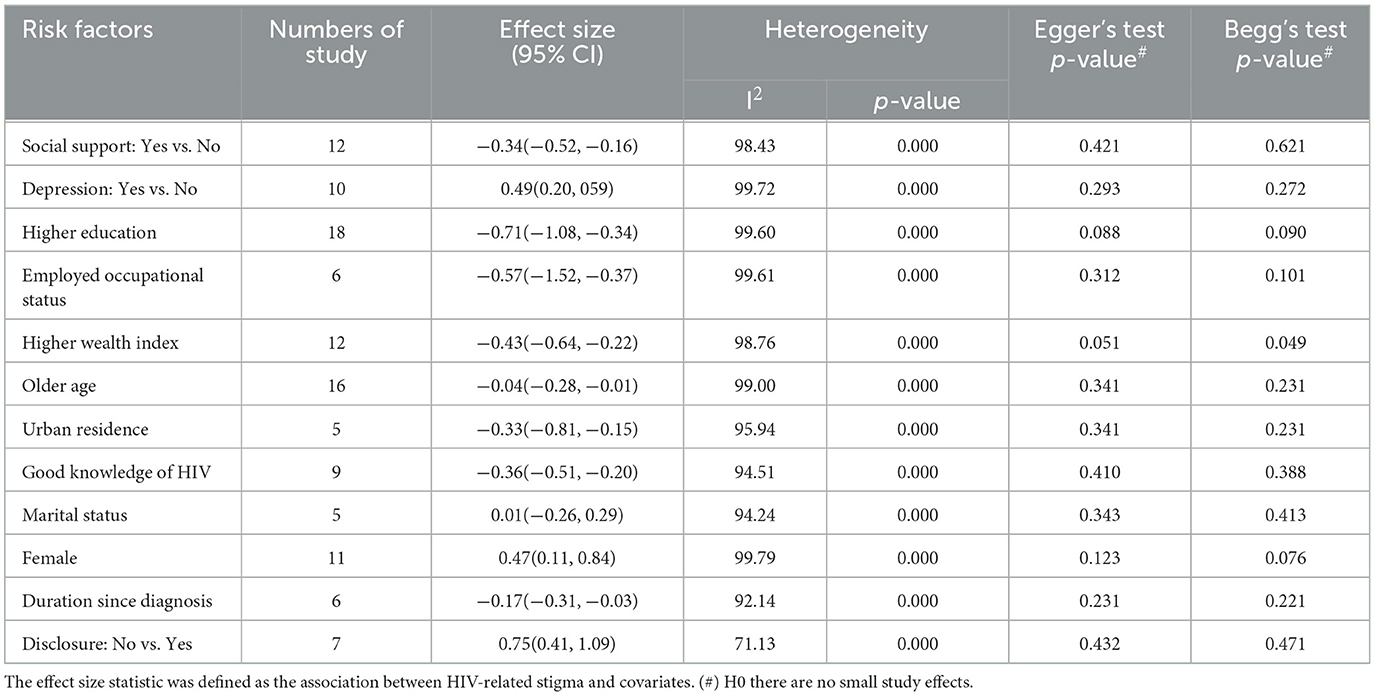
Table 2. Results of the subgroup analysis based on clinical and demographic variables associated with high stigma levels.
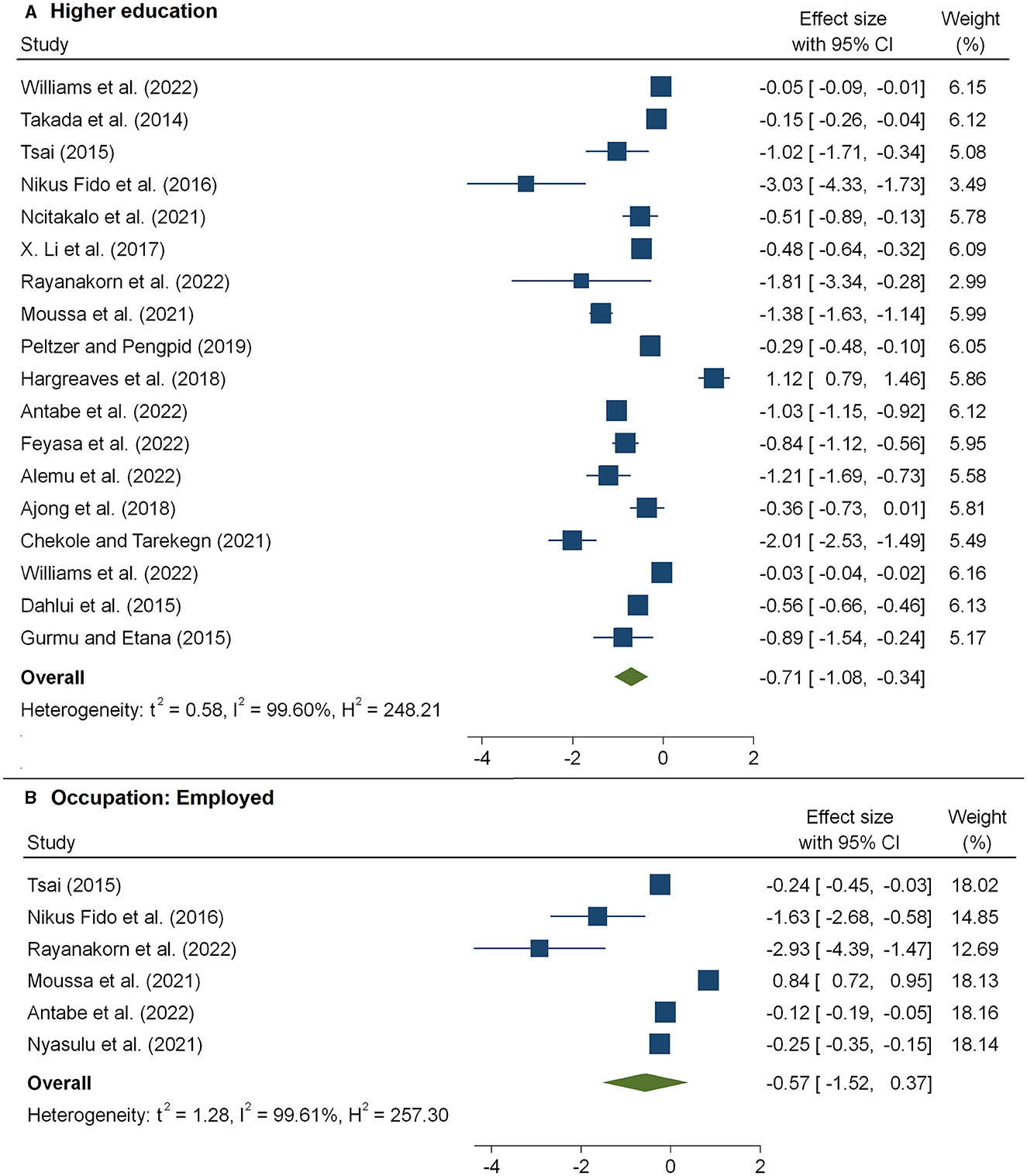
Figure 4. The pooled effect size showing the association between HIV-related stigma and educational level (A) and occupational status (B).
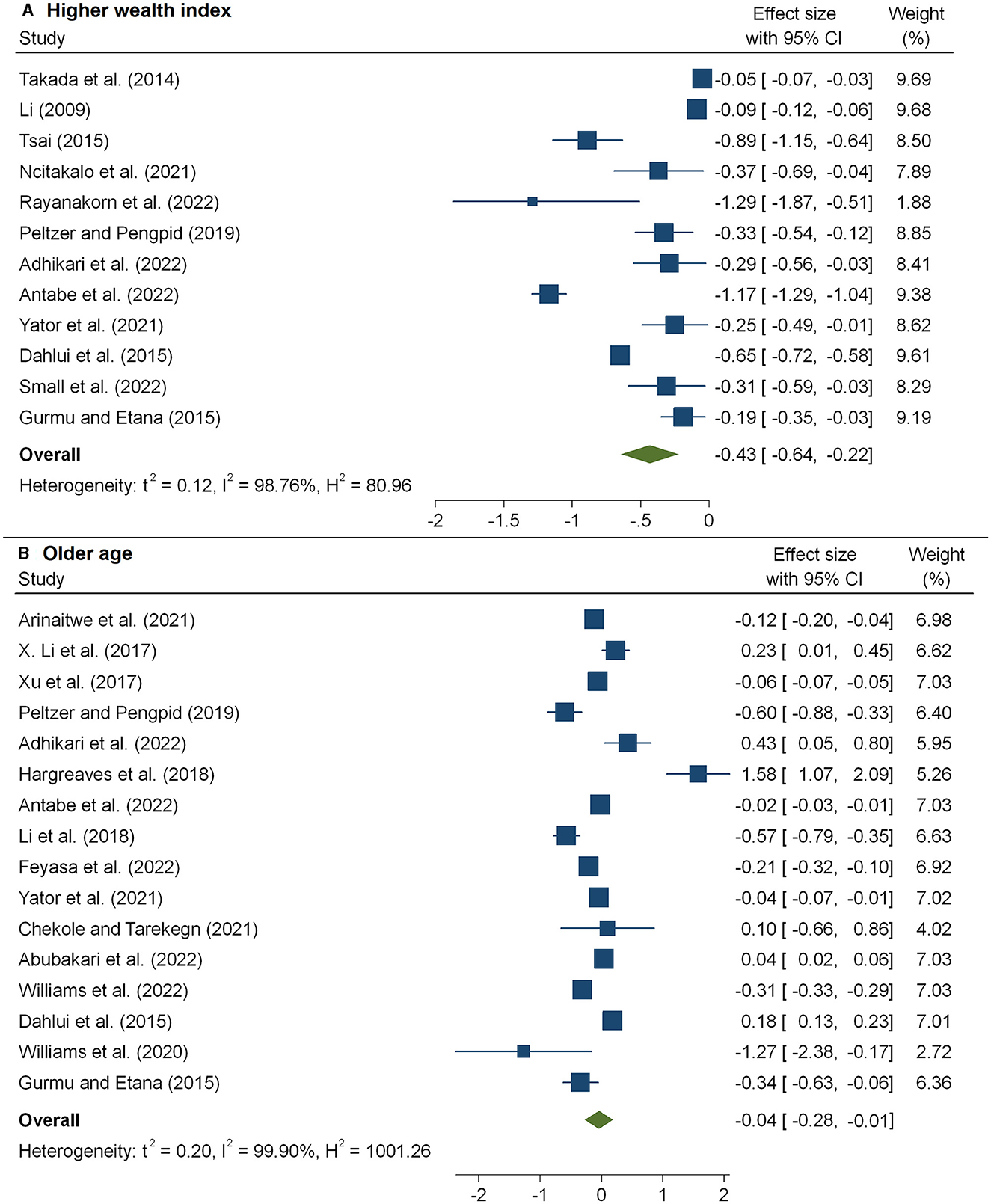
Figure 5. The pooled effect size showing the association between HIV-related stigma and wealth index (A) and age (B).
The meta-analysis of 16 studies (30–35, 37, 44, 51, 54) that examined the association between the level of HIV-related stigma and age is presented in Figure 5B and Table 2. From the results, we observed that older age was associated with a decreased level of stigma, and the pooled estimate was −0.04 (95%CI: −0.28, −0.01). According to five studies (17, 20, 31, 34, 48), patients living in urban areas faced a considerably decreased level of stigma, and the pooled estimate was −0.33(95%CI: −0.81, −0.15) (Figure 6A and Table 2).
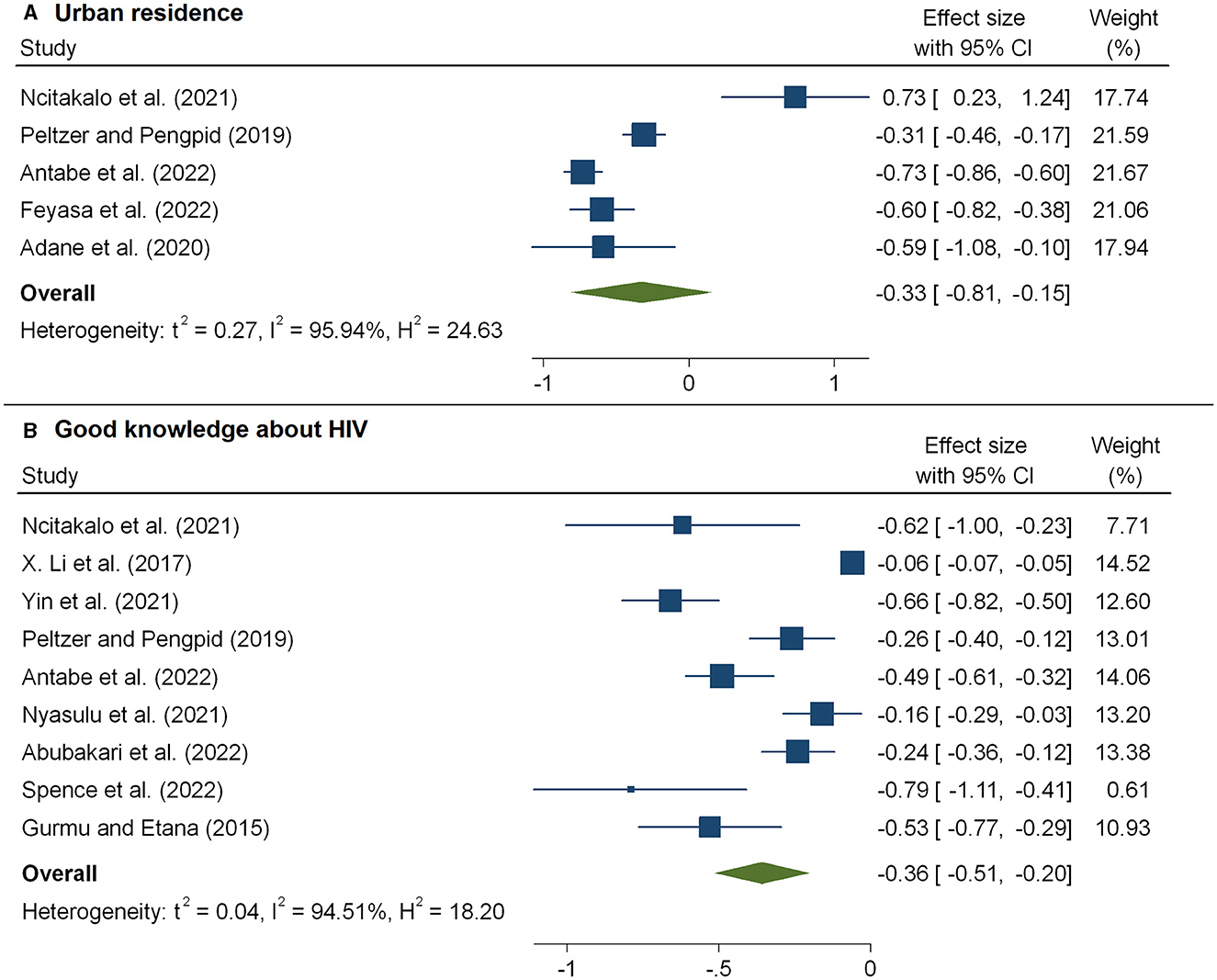
Figure 6. The pooled effect size showing the association between HIV-related stigma and residence (A) and knowledge about HIV (B).
The HIV/AIDS knowledge score significantly predicted the level of HIV-related stigma. As shown in Figure 6B, we observed that the level of stigma significantly decreased with an increasing HIV/AIDS knowledge score, and the pooled estimate was −0.36(95%CI: −0.51, −0.20). The combined 11 effect sizes from 11 studies (17, 20, 21, 33, 41, 43, 51) revealed that women were more likely to face a high level of stigma, and the pooled estimate was 0.47(95%CI: 0.11, 0.84) (Figure 7B). However, the association of marital status with HIV-related stigma was not found to be significant (pooled β: 0.01; 95% CI: −0.26, 0.29; Figure 7A and Table 3). The association between the level of HIV-related stigma and disclosure status is presented in Figure 8B. We observed that not disclosing their HIV status was positively associated with HIV-related stigma (pooled β: 0.75(95%CI: 0.41, 1.09). Furthermore, the level of HIV-related stigma significantly decreased with increasing years of living with HIV, and the pooled estimate was −0.17 (95%CI: −0.31, −0.03) (Figure 8A and Table 2). However, marital status association with HIV-related stigma was not found to be significant (pooled β: 0.01; 95% CI: −0.26, 0.29; Figure 7A and Table 3).
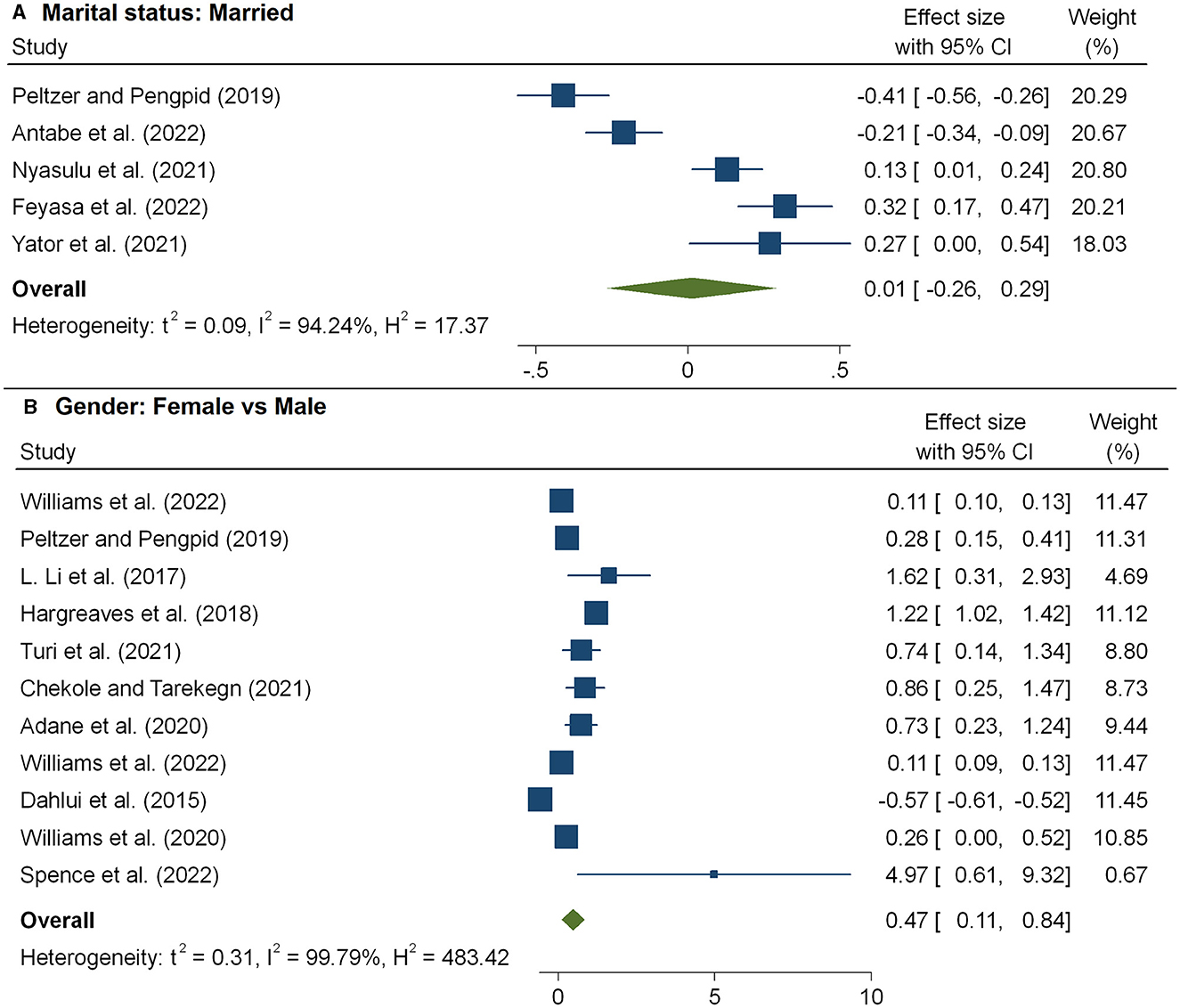
Figure 7. The pooled effect size showing the association between HIV-related stigma and marital status (A) and gender (B).
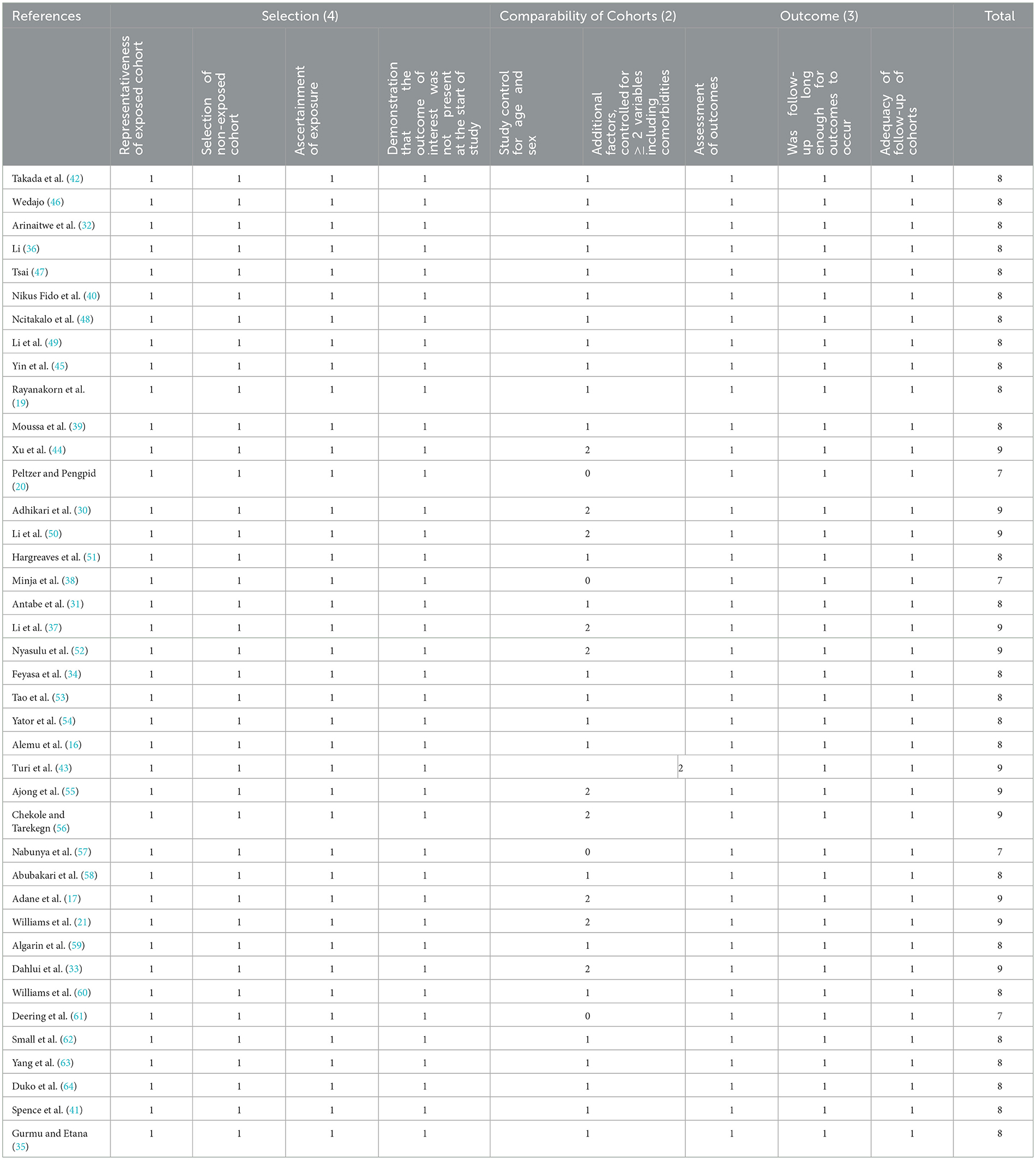
Table 3. Risk of bias assessment of 40 studies included in the meta-analysis using the Newcastle–Ottawa Scale.
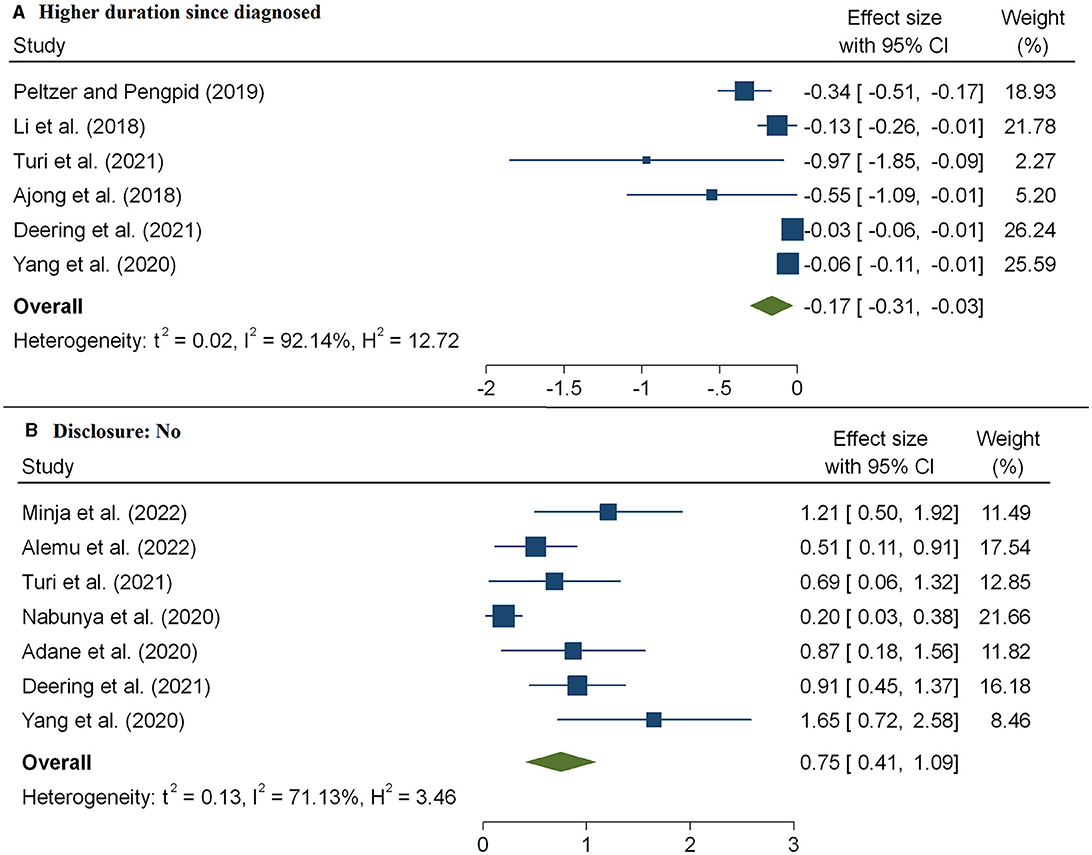
Figure 8. The pooled effect size showing the association between HIV-related stigma and duration since diagnosis (A) and disclosure status (B).
The selected studies had a Newcastle–Ottawa score of 7–9, and the studies' quality was considered to be high (Table 3).
The I2 values for age, social support, educational status, depression, employment status, wealth index, gender, residence, knowledge about HIV, marital status, duration since diagnosis, and disclosure status demonstrated heterogeneity among the studies under consideration. According to the results of the sensitivity analysis, the estimates for the overall effects of age, social support, educational status, depression, employment status, wealth index, gender, residence, knowledge about HIV, marital status, duration since diagnosis, and disclosure status on the level of HIV-related stigma did not depend on any particular study. According to the funnel plots of the studies included in the meta-analysis, no discernible bias was observed (Figure 9). In addition, neither Egger's regression nor Begg's correlation rank revealed any discernible publication bias (see Table 2).
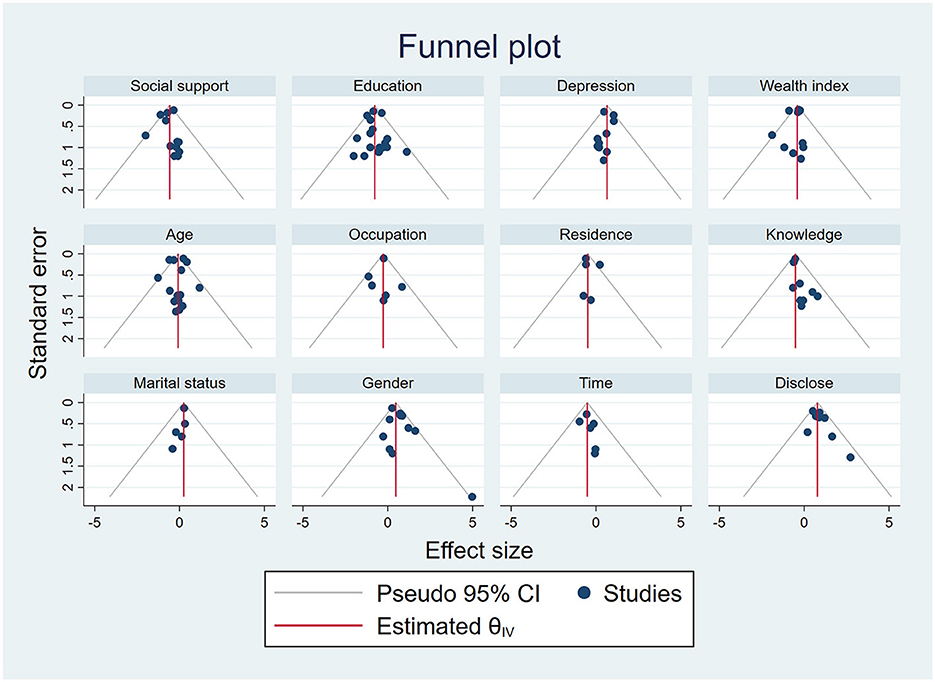
Figure 9. Funnel plots for the publication bias of the effect of age, social support, educational status, depression, employment status, wealth index, gender, residence, knowledge about HIV, marital status, duration since diagnosis, and disclosure status on HIV-related stigma.
This review used a series of meta-analyses and data gathered from 40 published studies involving people living with HIV to explore the relationship between a number of health, risk, and sociodemographic factors and HIV-related stigma. In terms of the scale and breadth of risk, health, and sociodemographic factors, our study is by far the largest meta-analysis on the level of HIV-related stigma.
According to our findings, which were consistent with those of earlier research (6, 66), social support significantly reduced the level of HIV-related stigma. According to self-report data from prior studies (67, 68), PLWH with little social support had a higher likelihood of engaging in suicidal behaviors. Social support accessibility provides guidance and relevant information on HIV treatment to people living with HIV (69). Previous reports have suggested that HIV-related stigma could be reduced by improving positive social support, including self-reported social support (70). Thus, social support is crucial for the psychological adjustment of PLWH. Both policymakers and healthcare professionals should look toward enhancing family counseling and support services, such as care for PLWH, and increasing HIV screening among high-risk populations.
In our study, depression was significantly associated with higher levels of HIV-related stigma. This finding was consistent with those of earlier research that found a robust correlation between high levels of HIV-related stigma and high levels of depression (54, 71, 72). It is plausible that stigmatizing beliefs and reactions associated with HIV could evoke feelings of self-blame, guilt, or rejection in people living with HIV (54). Other previous studies (73, 74) on PLWH have discovered that stigma related to HIV is associated with mental health problems, including depression. Thus, to guide future interventions, more research is required to determine how depression affects HIV-related stigma.
Older age at diagnosis was associated with a lower level of HIV-related stigma. Previous studies conducted in different countries also reported similar findings (34, 37, 75). This could be attributed to increased awareness of the disease among older HIV/AIDS patients due to advancement in the education level, exposure to different media, and utilization of the Internet, which promotes HIV-related knowledge. We also observed that women were more likely to face a high level of stigma. This finding was in accordance with those of previous studies (18, 56, 76, 77) that observed that being a woman was significantly associated with a high level of stigma. Existing biases against women may make them more susceptible to HIV-related stigma (40).
We also observed that socioeconomic factors were positively associated with HIV-related stigma. A higher level of education was found to be associated with a lower level of HIV-related stigma in patients. This finding was in accordance with those of previous studies (40, 78) that observed that a lower level of education was significantly associated with a higher level of HIV-related stigma. It has also been demonstrated that an increased level of education reduces HIV-related stigma (48, 79). Moreover, lower household wealth was significantly associated with a high level of HIV-related stigma. This finding was consistent with the findings of previous research that suggested that a higher socioeconomic status helps combat HIV-related stigma (31).
In addition, our data implied that stigmatizing PLWH was associated with psychological issues. For instance, among patients, a lower risk of HIV-related stigma was associated with having high clinical knowledge about HIV and longer years of living with HIV. These findings were consistent with those of previous research (31) that suggested the usefulness of HIV knowledge in rejecting HIV misconceptions and being receptive to PLWH. Therefore, biomedical and clinical knowledge absolve PLWH from being social outcasts who require stigmatization.
Despite providing pooled estimates from 40 studies across various geographic regions, our analysis has a few limitations. First, some of the included studies had very small sample sizes, which made it difficult to identify any potential influences on high HIV-related stigma. Second, high heterogeneity was observed, which may be due to the wide range of study approaches and sample sizes (ranging from 123 to 56,367 patients).
Our study indicated a consistent and statistically significant effect of socioeconomic, demographic, psychosocial, and risk variables, including older age, social support, higher educational level, higher socioeconomic status, good knowledge about HIV, disclosure of HIV status, and longer years of living with HIV, which significantly reduced the level of HIV-related stigma. It is crucial to develop complete and comprehensive social strategies through community-level awareness about HIV to tackle systemic HIV-associated stigma.
Moreover, our systematic review results also confirmed that depression, residing in rural areas, female respondents, and poor economic status were significantly associated with a high risk of HIV-related stigma. In addition to advocacy, community economic development or local economic development is essential to build healthy and socially cohesive communities. It would be especially important for policies and programs to effectively integrate agendas across psychosocial, demographic, and socioeconomic interventions to fulfill the UNAIDS 95-95-95 objective by 2030.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
ZD: Conceptualization, Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. TZ: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Bahir Dar University and the University of KwaZulu-Natal did not have any role in the study design and collection, analysis, and interpretation of data and in writing the manuscript.
We would like to thank Bahir Dar University and the University of KwaZulu-Natal for providing their guidance and support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. HIV/AIDS JUNPo. Reduction of HIV-related Stigma and Discrimination: Guidance Note. Geneva: UNAIDS (2014).
2. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. (2001) 27:363–85. doi: 10.1146/annurev.soc.27.1.363
3. Friedland BA, Gottert A, Hows J, Baral SD, Sprague L, Nyblade L, et al. The people living with HIV Stigma Index 20: generating critical evidence for change worldwide. AIDS. (2020) 34:S5–18. doi: 10.1097/QAD.0000000000002602
4. Thomas BE, Rehman F, Suryanarayanan D, Josephine K, Dilip M, Dorairaj V, et al. How stigmatizing is stigma in the life of people living with HIV: a study on HIV positive individuals from Chennai, South India. AIDS Care. (2005) 17:795–801. doi: 10.1080/09540120500099936
5. Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: an empirical assessment. Am Sociol Rev. (1989) 54:400–23. doi: 10.2307/2095613
6. Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. (2016) 6:e011453. doi: 10.1136/bmjopen-2016-011453
7. Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV Stigma Scale. AIDS Educ Prevent. (2007) 19:198–208. doi: 10.1521/aeap.2007.19.3.198
8. Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health. (2017) 107:863–9. doi: 10.2105/AJPH.2017.303744
9. Ivanova EL, Hart TA, Wagner AC, Aljassem K, Loutfy MR. Correlates of anxiety in women living with HIV of reproductive age. AIDS Behav. (2012) 16:2181–91. doi: 10.1007/s10461-011-0133-6
10. Lambert CC, Westfall A, Modi R, Amico RK, Golin C, Keruly J, et al. HIV-related stigma, depression, and social support are associated with health-related quality of life among patients newly entering HIV care. AIDS Care. (2020) 32:681–8. doi: 10.1080/09540121.2019.1622635
11. Felker-Kantor EA, Wallace ME, Madkour AS, Duncan DT, Andrinopoulos K, Theall K, et al. stigma, mental health, and alcohol use disorders among people living with HIV/AIDS in New Orleans. J Urban Health. (2019) 96:878–88. doi: 10.1007/s11524-019-00390-0
12. Siegel K, Lekas H-M, Schrimshaw EW. Serostatus disclosure to sexual partners by HIV-infected women before and after the advent of HAART. Women Health. (2005) 41:63–85. doi: 10.1300/J013v41n04_04
13. Hsieh E, Polo R, Qian H-Z, Fuster-RuizdeApodaca MJ, Del Amo J. Intersectionality of stigmas and health-related quality of life in people ageing with HIV in China, Europe, and Latin America. Lancet Healthy Longevity. (2022). doi: 10.1016/S2666-7568(22)00003-4
14. Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India–a community based cross sectional study. BMC Public Health. (2012) 12:1–11. doi: 10.1186/1471-2458-12-463
15. Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. (2017) 21:283–91. doi: 10.1007/s10461-016-1451-5
16. Alemu A, Meskele M, Darebo TD, Beyene Handiso T, Abebe A, Paulos K. Perceived HIV stigma and associated factors among adult ART patients in Wolaita Zone, Southern Ethiopia. HIV AIDS. (2022) 14:487–501. doi: 10.2147/HIV.S372738
17. Adane B, Yalew M, Damtie Y, Kefale B. Perceived stigma and associated factors among people living with HIV attending ART clinics in public health facilities of Dessie City, Ethiopia. HIV AIDS. (2020) 12:551–7. doi: 10.2147/HIV.S274019
18. Bagchi AD, Holzemer W, Peavy D. Predictors of enacted, internal, and anticipated stigma among PLHIV in New Jersey. AIDS Care. (2019) 31:827–35. doi: 10.1080/09540121.2018.1554242
19. Rayanakorn A, Ong-Artborirak P, Ademi Z, Chariyalertsak S. Predictors of stigma and health-related quality of life among people living with HIV in Northern Thailand. AIDS Patient Care STDS. (2022) 36:186–93. doi: 10.1089/apc.2022.0035
20. Peltzer K, Pengpid S. Prevalence and associated factors of enacted, internalized and anticipated stigma among people living with HIV in South Africa: results of the first national survey. HIV AIDS. (2019) 11:275–85. doi: 10.2147/HIV.S229285
21. Williams R, Brumback B, Cook R, Cook C, Ezenwa M, Lucero R. Prevalence of HIV-related stigma in adults living with HIV & disability in Florida, 2015–2016. AIDS Care. (2022) 34:47–54. doi: 10.1080/09540121.2021.1929812
22. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
23. Wells G. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. (2004). Available online at: http://www.ohrica/programs/clinical_epidemiologyoxfordhtm (accessed March 14, 2023).
24. Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. (2003) 121:31–49. doi: 10.1016/j.psychres.2003.08.008
25. Sowell RL, Lowenstein A, Moneyham L, Demi A, Mizuno Y, Seals BF. Resources, stigma, and patterns of disclosure in rural women with HIV infection. Public Health Nurs. (1997) 14:302–12. doi: 10.1111/j.1525-1446.1997.tb00379.x
26. Wright K, Naar-King S, Lam P, Templin T, Frey M. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV+ youth. J adolescent health. (2007) 40:96–8. doi: 10.1016/j.jadohealth.2006.08.001
27. Sayles JN, Hays RD, Sarkisian CA, Mahajan AP, Spritzer KL, Cunningham WE. Development and psychometric assessment of a multidimensional measure of internalized HIV stigma in a sample of HIV-positive adults. AIDS Behav. (2008) 12:748–58. doi: 10.1007/s10461-008-9375-3
28. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
29. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. (2006) 295:676–80. doi: 10.1001/jama.295.6.676
30. Adhikari K, Dutt D, Pal D, Hazra S. Stigma and its associated factors among people living with HIV/AIDS (PLHA) attending ART Centre in a Tertiary Care Institute in Kolkata. MAMC J Med Sci. (2022) 8:62. doi: 10.4103/mamcjms.mamcjms_87_21
31. Antabe R, Sano Y, Atuoye KN, Baada JN. Determinants of HIV-related stigma and discrimination in Malawi: evidence from the demographic and health survey. Afr Geogr Rev. (2022) 42:594–606. doi: 10.1080/19376812.2022.2086591
32. Arinaitwe I, Amutuhaire H, Atwongyeire D, Tusingwire E, Kawungezi PC, Rukundo GZ, et al. Social support, food insecurity, and HIV stigma among men living with HIV in rural Southwestern Uganda: a cross-sectional analysis. HIV AIDS. (2021) 13:657–66. doi: 10.2147/HIV.S316174
33. Dahlui M, Azahar N, Bulgiba A, Zaki R, Oche OM, Adekunjo FO, et al. HIV/AIDS related stigma and discrimination against PLWHA in Nigerian population. PLoS ONE. (2015) 10:e0143749. doi: 10.1371/journal.pone.0143749
34. Feyasa MB, Gebre MN, Dadi TK. Levels of HIV/AIDS stigma and associated factors among sexually active Ethiopians: analysis of 2016 Ethiopian Demographic and Health Survey Data. BMC Public Health. (2022) 22:1080. doi: 10.1186/s12889-022-13505-1
35. Gurmu E, Etana D. HIV/AIDS knowledge and stigma among women of reproductive age in Ethiopia. African J AIDS Res. (2015) 14:191–9. doi: 10.2989/16085906.2015.1051066
36. Li L, Lee SJ, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care. (2009) 21:1013. doi: 10.1080/09540120802614358
37. Li Z, Morano JP, Khoshnood K, Hsieh E, Sheng Y. HIV-related stigma among people living with HIV/AIDS in rural Central China. BMC Health Serv Res. (2018) 18:1–7. doi: 10.1186/s12913-018-3245-0
38. Minja AA, Larson E, Aloyce Z, Araya R, Kaale A, Kaaya SF, et al. Burden of HIV-related stigma and associated factors among women living with depression accessing PMTCT services in Dar es Salaam, Tanzania. AIDS Care. (2022) 34:1572–9. doi: 10.1080/09540121.2022.2050174
39. Moussa AB, Delabre RM, Villes V, Elkhammas M, Bennani A, Ouarsas L, et al. Determinants and effects or consequences of internal HIV-related stigma among people living with HIV in Morocco. BMC Public Health. (2021) 21:1–11. doi: 10.1186/s12889-021-10204-1
40. Nikus Fido N, Aman M, Brihnu Z. HIV stigma and associated factors among antiretroviral treatment clients in Jimma town, Southwest Ethiopia. HIV AIDS. (2016) 8:183–93. doi: 10.2147/HIV.S114177
41. Spence AB, Wang C, Michel K, Ocampo JM, Kharfen M, Merenstein D, et al. A related stigma among healthcare providers: opportunities for education and training. J Int Assoc Provid AIDS Care. (2022) 21:23259582221114797. doi: 10.1177/23259582221114797
42. Takada S, Weiser SD, Kumbakumba E, Muzoora C, Martin JN, Hunt PW, et al. The dynamic relationship between social support and HIV-related stigma in rural Uganda. Ann Behav Med. (2014) 48:26–37. doi: 10.1007/s12160-013-9576-5
43. Turi E, Simegnew D, Fekadu G, Tolossa T, Desalegn M, Bayisa L, et al. High perceived stigma among people living with HIV/AIDS in a resource limited setting in Western Ethiopia: the effect of depression and low social support. HIV AIDS. (2021) 13:389–97. doi: 10.2147/HIV.S295110
44. Xu X, Sheng Y, Khoshnood K, Clark K. Factors predicting internalized stigma among men who have sex with men living with HIV in Beijing, China. J Assoc Nurses AIDS Care. (2017) 28:142–53. doi: 10.1016/j.jana.2016.08.004
45. Yin Y, Chen AC-C, Wan S, Chen H. Factors associated with HIV-related stigma toward people living with HIV among nurses in Liangshan Yi Autonomous Prefecture, China: a cross-sectional study. Front Psychiatry. (2021) 12:714597. doi: 10.3389/fpsyt.2021.714597
46. Wedajo S, Degu G, Deribew A, Ambaw F. Social support, perceived stigma, and depression among PLHIV on second-line antiretroviral therapy using structural equation modeling in a multicenter study in Northeast Ethiopia. Int J Ment Health Syst. (2022) 16:27. doi: 10.1186/s13033-022-00536-9
47. Tsai AC. Socioeconomic gradients in internalized stigma among 4,314 persons with HIV in sub-Saharan Africa. AIDS Behav. (2015) 19:270–82. doi: 10.1007/s10461-014-0993-7
48. Ncitakalo N, Mabaso M, Joska J, Simbayi L. Factors associated with external HIV-related stigma and psychological distress among people living with HIV in South Africa. SSM-Popul Health. (2021) 14:100809. doi: 10.1016/j.ssmph.2021.100809
49. Li X, Yuan L, Li X, Shi J, Jiang L, Zhang C, et al. Factors associated with stigma attitude towards people living with HIV among general individuals in Heilongjiang, Northeast China. BMC Infect Dis. (2017) 17:1–6. doi: 10.1186/s12879-017-2216-0
50. Li L, Lin C, Ji G. Gendered aspects of perceived and internalized HIV-related stigma in China. Women Health. (2017) 57:1031–43. doi: 10.1080/03630242.2016.1235075
51. Hargreaves JR, Krishnaratne S, Mathema H, Lilleston PS, Sievwright K, Mandla N, et al. Individual and community-level risk factors for HIV stigma in 21 Zambian and South African communities: analysis of data from the HPTN071 (PopART) study. AIDS. (2018) 32:783. doi: 10.1097/QAD.0000000000001757
52. Nyasulu PS, Tshuma N, Sigwadhi LN, Nyasulu J, Ogunrombi M, Chimoyi L. Factors associated with high HIV-related stigma among commuter populations in Johannesburg, South Africa. SAHARA-J. (2021) 18:149–55. doi: 10.1080/17290376.2021.1989022
53. Tao J, Wang L, Kipp AM, Qian H-Z, Yin L, Ruan Y, et al. Relationship of stigma and depression among newly HIV-diagnosed Chinese men who have sex with men. AIDS Behav. (2017) 21:292–9. doi: 10.1007/s10461-016-1477-8
54. Yator O, Mathai M, Albert T, Kumar M. Burden of HIV-related stigma and post-partum depression: a cross-sectional study of patients attending prevention of mother-to-child transmission clinic at Kenyatta National Hospital in Nairobi. Front Psychiatry. (2021) 11:532557. doi: 10.3389/fpsyt.2020.532557
55. Ajong AB, Njotang PN, Nghoniji NE, Essi MJ, Yakum MN, Agbor VN, et al. Quantification and factors associated with HIV-related stigma among persons living with HIV/AIDS on antiretroviral therapy at the HIV-day care unit of the Bamenda Regional Hospital, North West Region of Cameroon. Global Health. (2018) 14:1–7. doi: 10.1186/s12992-018-0374-5
56. Chekole YA, Tarekegn D. HIV-related perceived stigma and associated factors among patients with HIV, Dilla, Ethiopia: a cross-sectional study. Ann Med Surg. (2021) 71:102921. doi: 10.1016/j.amsu.2021.102921
57. Nabunya P, Byansi W, Sensoy Bahar O, McKay M, Ssewamala FM, Damulira C. Factors associated with HIV disclosure and HIV-related stigma among adolescents living with HIV in Southwestern Uganda. Front Psychiatry. (2020) 11:772. doi: 10.3389/fpsyt.2020.00772
58. Abubakari GMR, Smith MD, Boyd DT, Ramos SR, Johnson C, Benavides JL, et al. Assessing different types of HIV communication and sociocultural factors on perceived HIV stigma and testing among a national sample of youth and young adults. Int J Environ Res Public Health. (2022) 19:1003. doi: 10.3390/ijerph19021003
59. Algarin AB, Sheehan DM, Varas-Diaz N, Fennie K, Zhou Z, Spencer EC, et al. Enacted HIV-related stigma's association with anxiety & depression among people living with HIV (PLWH) in Florida. AIDS Behav. (2021) 25:93–103. doi: 10.1007/s10461-020-02948-5
60. Williams R, Cook R, Brumback B, Cook C, Ezenwa M, Spencer E, et al. The relationship between individual characteristics and HIV-related stigma in adults living with HIV: medical monitoring project, Florida, 2015–2016. BMC Public Health. (2020) 20:1–10. doi: 10.1186/s12889-020-08891-3
61. Deering KN, Logie C, Krüsi A, Ranville F, Braschel M, Duff P, et al. Prevalence and correlates of HIV stigma among women living with HIV in metro Vancouver, Canada. AIDS Behav. (2021) 25:1688–98. doi: 10.1007/s10461-020-03084-w
62. Small E, Nikolova SP, Zhou Y, Okumu M. Exploring factors associated with HIV secondary stigma among adolescents and young adults in Uganda: a cross-sectional study. Glob Public Health. (2022) 17:526–37. doi: 10.1080/17441692.2020.1869286
63. Yang H, Xie X, Nie A, Yin Y, Wang H, Chen H. HIV-related stigma among people living with HIV in Liangshan Yi Autonomous Prefecture, China. J Assoc Nurses AIDS Care. (2020) 31:199–207. doi: 10.1097/JNC.0000000000000119
64. Duko B, Geja E, Zewude M, Mekonen S. Prevalence and associated factors of depression among patients with HIV/AIDS in Hawassa, Ethiopia, cross-sectional study. Ann Gen Psychiatry. (2018) 17:1–6. doi: 10.1186/s12991-018-0215-1
65. Yang SX, Hewitt SM Yu J. Locoregional tumor burden and risk of mortality in metastatic breast cancer. NPJ Prec Oncol. (2022) 6:1–7. doi: 10.1038/s41698-022-00265-9
66. Armoon B, Fleury M-J, Bayat A-H, Fakhri Y, Higgs P, Moghaddam LF, et al. related stigma associated with social support, alcohol use disorders, depression, anxiety, and suicidal ideation among people living with HIV: a systematic review and meta-analysis. Int J Ment Health Syst. (2022) 16:1–17. doi: 10.1186/s13033-022-00527-w
67. Kim BJ, Kihl T. Suicidal ideation associated with depression and social support: a survey-based analysis of older adults in South Korea. BMC Psychiatry. (2021) 21:1–9. doi: 10.1186/s12888-021-03423-8
68. Scardera S, Perret LC, Ouellet-Morin I, Gariépy G, Juster R-P, Boivin M, et al. Association of social support during adolescence with depression, anxiety, and suicidal ideation in young adults. JAMA Netw Open. (2020) 3:e2027491–e2027491. doi: 10.1001/jamanetworkopen.2020.27491
69. Maman S, Van Rooyen H, Groves AK, HIV. status disclosure to families for social support in South Africa (NIMH Project Accept/HPTN 043). AIDS Care. (2014) 26:226–32. doi: 10.1080/09540121.2013.819400
70. Yadav S. Perceived social support, hope, and quality of life of persons living with HIV/AIDS: a case study from Nepal. Quality Life Res. (2010) 19:157–66. doi: 10.1007/s11136-009-9574-z
71. Logie C, James L, Tharao W, Loutfy M. Associations between HIV-related stigma, racial discrimination, gender discrimination, and depression among HIV-positive African, Caribbean, and Black women in Ontario, Canada. AIDS Patient Care STDS. (2013) 27:114–22. doi: 10.1089/apc.2012.0296
72. Lowther K, Selman L, Harding R, Higginson IJ. Experience of persistent psychological symptoms and perceived stigma among people with HIV on antiretroviral therapy (ART): a systematic review. Int J Nurs Stud. (2014) 51:1171–89. doi: 10.1016/j.ijnurstu.2014.01.015
73. Levi-Minzi MA, Surratt HL, HIV. stigma among substance abusing people living with HIV/AIDS: implications for HIV treatment. AIDS Patient Care STDS. (2014) 28:442–51. doi: 10.1089/apc.2014.0076
74. Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the internalized AIDS-related stigma scale. AIDS Care. (2009) 21:87–93. doi: 10.1080/09540120802032627
75. Srithanaviboonchai K, Chariyalertsak S, Nontarak J, Assanangkornchai S, Kessomboon P, Putwatana P, et al. Stigmatizing attitudes toward people living with HIV among general adult Thai population: results from the 5th Thai National Health Examination Survey (NHES). PLoS ONE. (2017) 12:e0187231. doi: 10.1371/journal.pone.0187231
76. Blessed NO, Ogbalu AI. Experience of HIV-related stigma by people living with HIV/AIDS (PLWHA), based on gender: a case of PLWHA attending clinic in the federal medical center, Owerri, IMO states, Nigeria. J Public Health Epidemiol. (2013) 5:435–9. doi: 10.5897/JPHE2013.0496
77. Colombini M, Mutemwa R, Kivunaga J, Stackpool Moore L, Mayhew SH. Experiences of stigma among women living with HIV attending sexual and reproductive health services in Kenya: a qualitative study. BMC Health Serv Res. (2014) 14:1–9. doi: 10.1186/1472-6963-14-412
78. Tzemis D, Forrest JI, Puskas CM, Zhang W, Orchard TR, Palmer AK, et al. Identifying self-perceived HIV-related stigma in a population accessing antiretroviral therapy. AIDS Care. (2013) 25:95–102. doi: 10.1080/09540121.2012.687809
Keywords: Begg's test, effect size, Egger's test, heterogeneity, funnel plot, publication bias, sensitivity analysis
Citation: Dessie ZG and Zewotir T (2024) HIV-related stigma and associated factors: a systematic review and meta-analysis. Front. Public Health 12:1356430. doi: 10.3389/fpubh.2024.1356430
Received: 15 December 2023; Accepted: 14 June 2024;
Published: 23 July 2024.
Edited by:
Cyrille Delpierre, INSERM Public Health, FranceReviewed by:
Cyrus Mugo Wachira, Kenyatta National Hospital, KenyaCopyright © 2024 Dessie and Zewotir. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zelalem G. Dessie, WmVsYWxlbV9nZXRhaHVuZUB5YWhvby5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.