- 1Department of Environmental Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
- 2Department of Public Health, College of Health Science, Salale University, Fitche, Ethiopia
Introduction: The public health concern of tobacco smoking is more prevalent in low- and middle-income countries including Ethiopia. Various studies have investigated tobacco smoking in various parts of Ethiopia. However, the findings have been inconsistent and characterized by significant variability. Besides, there is no nationally representative data on the subject, which could deter the design of effective intervention strategies to reduce tobacco-related problems. Therefore, this study aimed to estimate the pooled prevalence of tobacco smoking and associated factors among adults in Ethiopia.
Methods: The study was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols Guideline. A detailed search was conducted from international databases including PubMed, Cochrane Library, Science Direct, CINAHL, African Journals Online, HINARI, Global Health, and Google Scholar. The extracted data was analyzed using STATA 14 software. A random-effects model was used to estimate the effect size. The Egger regression test and I2 statistics were used to determine potential publication bias and heterogeneity among the reviewed articles, respectively.
Results: A total of 32 studies with 69,897 study participants were included in this systematic review and meta-analysis. The pooled prevalence of lifetime tobacco smoking among adults in Ethiopia was 16.0% (95% confidence Interval (CI): 13.6–18.39) and there was significant heterogeneity among the included studies (I2 = 99.1%, p < 0.001). Male adults were three times more likely to smoke tobacco as compared with females [OR = 3.22 (95% CI: 2.06–5.03)]. Being an alcohol user [OR = 3.78 (95%CI: 1.27–11.24)] and having tobacco-smoking friends [OR = 7.21 (95%CI: 5.56–9.35)] are potential determinant factors for tobacco smoking.
Conclusion: The pooled prevalence of lifetime and current tobacco smoking among adults in Ethiopia was high, which calls for urgent intervention. Therefore, prioritization of tobacco control strategies, such as creating awareness about the public health importance of tobacco smoking, can help prevent and mitigate the effects of tobacco smoking. Alcohol control law enforcement should also be strengthened.
Introduction
Tobacco smoking is one of the causes of mortality and morbidity worldwide (1). It is the second significant cause of death globally. Every 6.5 s, one tobacco user dies as a result of a tobacco-related disease (2). According to the World Health Organization (WHO), annually, 8 million deaths are reported worldwide as a result of tobacco smoking (3); 6 million are direct smokers (4, 5). It has been confirmed that tobacco smoking can cause various types of cancers (6), chronic obstructive pulmonary disease, and lung disease. For instance, 90% of all lung cancer deaths in the United States were due to tobacco smoking (7). This is associated with the fact that tobacco contains up to 7,000 health-threatening chemicals (8). Beyond mortality and morbidity, the use of tobacco adds a burden to the national economy by increasing global health expenditures by about 6% and other indirect costs (9). According to the WHO report, the cost of smoking alone is estimated to be US$ 1.4 trillion, or 1.8% of the global GDP (10).
Over 80% of the global 1.3 billion smokers are found in low- and middle-income countries, where the burden of tobacco-related illness and death is significant (1). For instance, the prevalence of tobacco smoking was 60.2% in Bangladesh (11), 30.1% in Cameron (12), 20.2% in India (13), 14.7% in Malaysia (14), 13.7% in Nigeria (15), 12.4% in Yemen (16), and 10.7% in Pakistan (17). In Ethiopia, around 2.9 million adults are cigarette smokers. Of these, one-third of adults are exposed to secondhand smoke in public places (14), which is a significant cause of premature morbidity and mortality.
Numerous studies have been conducted to assess the prevalence of tobacco smoking and associated factors in Ethiopia (18–49). However, the study reports are inconsistent and characterized by significant variability [e.g., 2.4% (33) to 45.3% (28)], which could negatively influence the design of effective intervention strategies. Moreover, although a systematic review and meta-analysis is conducted among specific groups of the population (e.g., students) (14), there is no nationwide study assessing the pooled prevalence of tobacco smoking among the general adult population in Ethiopia. Therefore, this systematic review and meta-analysis aimed to estimate the pooled prevalence of tobacco smoking and identify factors contributing to tobacco smoking among adults in Ethiopia. The findings from this meta-analysis would generate evidence that will be important inputs for tobacco smoking prevention and control program planners, policymakers, and health service providers to design and implement evidence-based interventions to reduce the burden of tobacco-related mortality and morbidity in the country and other similar settings.
Methods and materials
Protocol registration
The protocol for this systematic review has been registered in the International Prospective Registry of Systematic Review (PROSPERO) with a specific registration number CRD42023415610.
Searching strategies
This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline (50). Studies were searched through PubMed/Medline, Cochrane Library, Science Direct, CINAHL, African Journals Online, HINARI, Global Health, and Google Scholar. In addition, digital libraries were searched to identify grey literature.
Endnote software was used to collect, organize, and remove the duplications of search outcomes. The search was made using the search terms: “prevalence,” “proportion,” “magnitude,” “incidence,” “tobacco smoking,” “cigarette smoking,” “smoking,” “tobacco,” “cigarette” “substance use” “factors,” “determinants,” “predictors,” “factors associated,” “associated factors,” “risk factors,” “adult,” and “Ethiopia.” All key terms were searched by a combination of Boolean operators “AND” or “OR” as appropriate, and the search was carried out from April 1 to May 15, 2023, by three authors independently (CD, AA, and BD).
Inclusion and exclusion criteria
Population: this systematic review and meta-analysis includes studies conducted among tobacco-smoking adults in Ethiopia. Exposure: an individual adult who experienced tobacco smoking whereas an individual adult who did not tobacco smoking was considered as a comparison. Outcome: studies assessed tobacco smoking as a primary outcome. All studies conducted with observational studies design (cohort, cross-sectional, and case–control) and institutional and community-based studies were also included in systematic review and meta-analysis. Besides, studies published from 2000 to 15 May 2023 in the English language were also included in the meta-analysis. However, qualitative studies, unretrievable studies, editorial letters, studies with poor methodological quality, and studies that did not report the outcome of interest were excluded from the meta-analysis.
Outcome measurement
The primary outcome of the study was the pooled prevalence of tobacco smoking among adults in Ethiopia, calculated by dividing the number of smokers by the total sample size and multiplying by 100. Additionally, the study aimed to identify the factors linked to tobacco smoking in the form of a log odds ratio.
Data extraction
After searching for relevant studies from the aforementioned electronic databases, they were exported to Endnote X20 (51) and any duplicates were removed. Three authors (CD, BD, and MG) independently extracted all the required data from the included studies by using a standardized data extraction template. The data extraction template consisted of various study details, such as the author’s name, region, publication year, study area/region, study population, study setting, study design, sample size, response rate, and tobacco smoking prevalence (current and lifetime prevalence). In the case of any disagreements during data extraction, other authors (AA, MD, and SAD) resolved them.
Quality assessment
After duplicate files were removed, four reviewers (CD, MG, BD, and SAD) screened the relevant studies for inclusion. The Joana Brigg Institute (JBI) critical appraisal checklist for prevalence studies was employed to evaluate the quality of each article (52) and those studies scored more than 50% were included for analysis (53, 54). Each study’s quality was assessed independently out of 100% by four authors (CD, BD, MG, and SAD). If any discrepancies arose during the quality assessment, the mean score was calculated from the results of all reviewers to resolve the differences.
Statistical analysis
The extracted data was exported into STATA/ SE version-14 statistical software for analysis (55). The level of heterogeneity among the included studies was statistically evaluated using the Higgs I2 test, with values greater than 75% considered high heterogeneity (56). DerSimonian and Liard’s method of random-effects model at a p-value less than 0.05 with a 95% CI was used to estimate the pooled prevalence of tobacco smoking using a forest plot. A p-value of less than 0.05 was considered indicative of the presence of heterogeneity (57).
Subgroup analysis was also conducted by characteristics of the study, such as region (Oromia, Amhara, Tigray, SNNPR (Southern Nation, Nationality, and People Region), all regions, or others), study setting (institutional or community), sample size (large—≥ 600 or small—<600), study population (students or community), and year of publication (before 2015 or 2015 and after). The different factors associated with tobacco smoking were presented using odds ratios (ORs) with 95% CI. Moreover, univariate meta-regression was carried out to identify the source of variations among studies that exhibited high heterogeneity.
Additionally, publication bias was assessed using a funnel plot and Egger’s test method with a significance level of p < 0.05 (58). Likewise, Duval and Tweedie’s ‘trim and fill’ analysis was also conducted to adjust the effect of publication bias among the studies included. A sensitivity analysis was also performed to assess the influence of a single study on the pooled prevalence estimates.
Results
Study selection
After conducting the electronic database search, a total of 1,063 studies were identified. Out of these, 802 articles were excluded based on their titles and abstracts. Besides, 20 articles were also excluded due to poor quality and did not report the outcome of the interest. Finally, 32 full-text articles were found eligible for this systematic review (Figure 1).
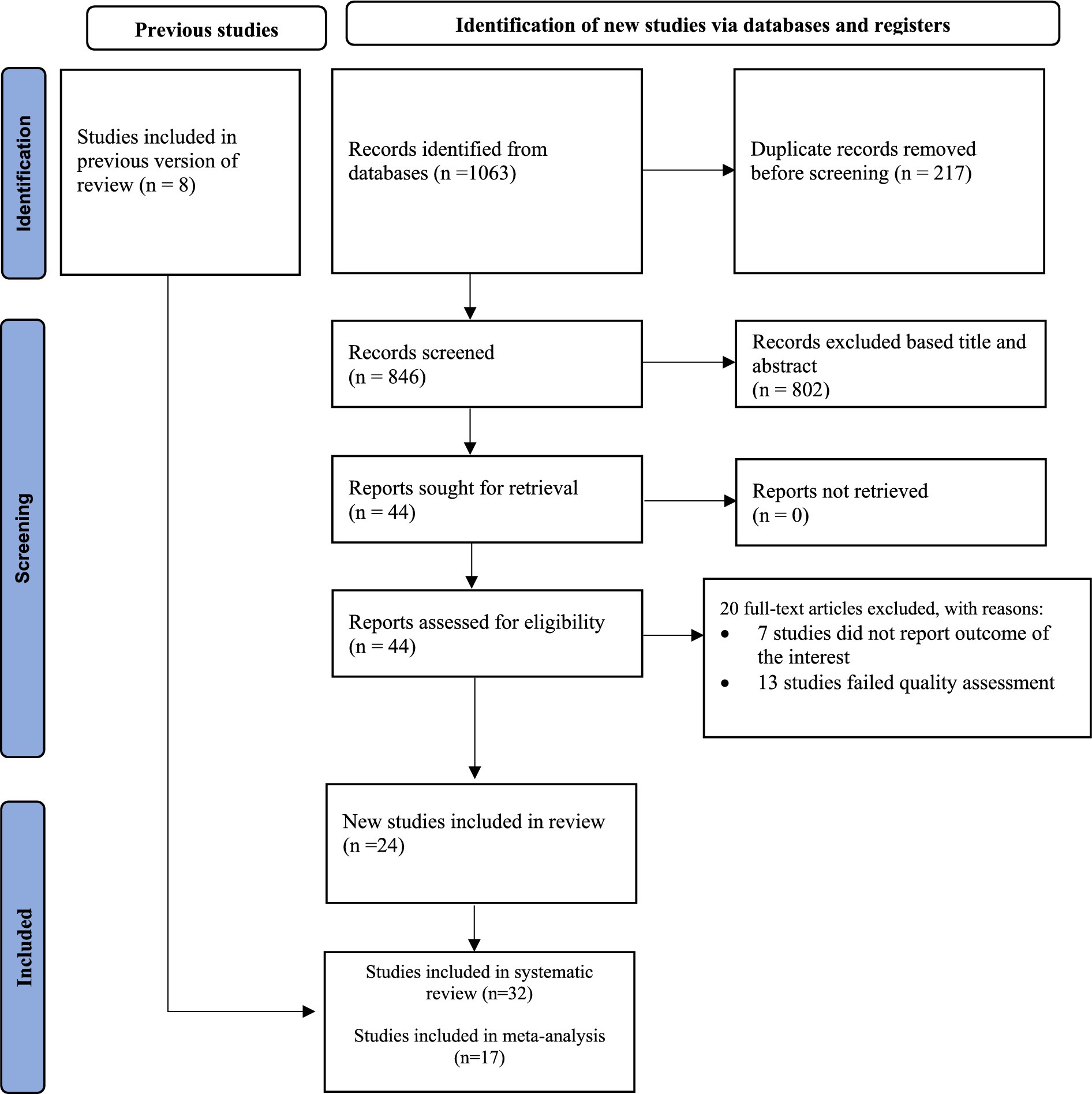
Figure 1. PRISMA flow diagram of the included studies for the systematic review and meta-analysis of the prevalence of tobacco smoking and associated factors among adults in Ethiopia, 2023.
Characteristics of the included studies
A total of 32 articles were reviewed to estimate the pooled prevalence of tobacco smoking among adults in Ethiopia. The highest prevalence of tobacco smoking was reported in a study conducted in the Oromia region (45.3%) (28) while the lowest (2.4%) was reported in a study conducted among all regions of Ethiopia (33). The total number of study participants included in the systematic review and meta-analysis was 69,897. In this meta-analysis, eight studies were conducted in the SNNPR (20, 26, 31, 34, 38–40, 46), seven in the Oromia region (19, 22, 24, 25, 28, 42, 49), three in Amhara region (18, 35, 48), three in Tigray region (27, 29, 32), three in all regions of Ethiopia (33, 37, 41), three in Addis Ababa (23, 45, 47), two in Somalia region (21, 44), and one each in Harari region (43), Benishangul Gumiz (30) and Dire-Dawa city administration (36). Although attempts were made to search cohort, case–control, and cross-sectional studies, we found only cross-sectional studies (Table 1).
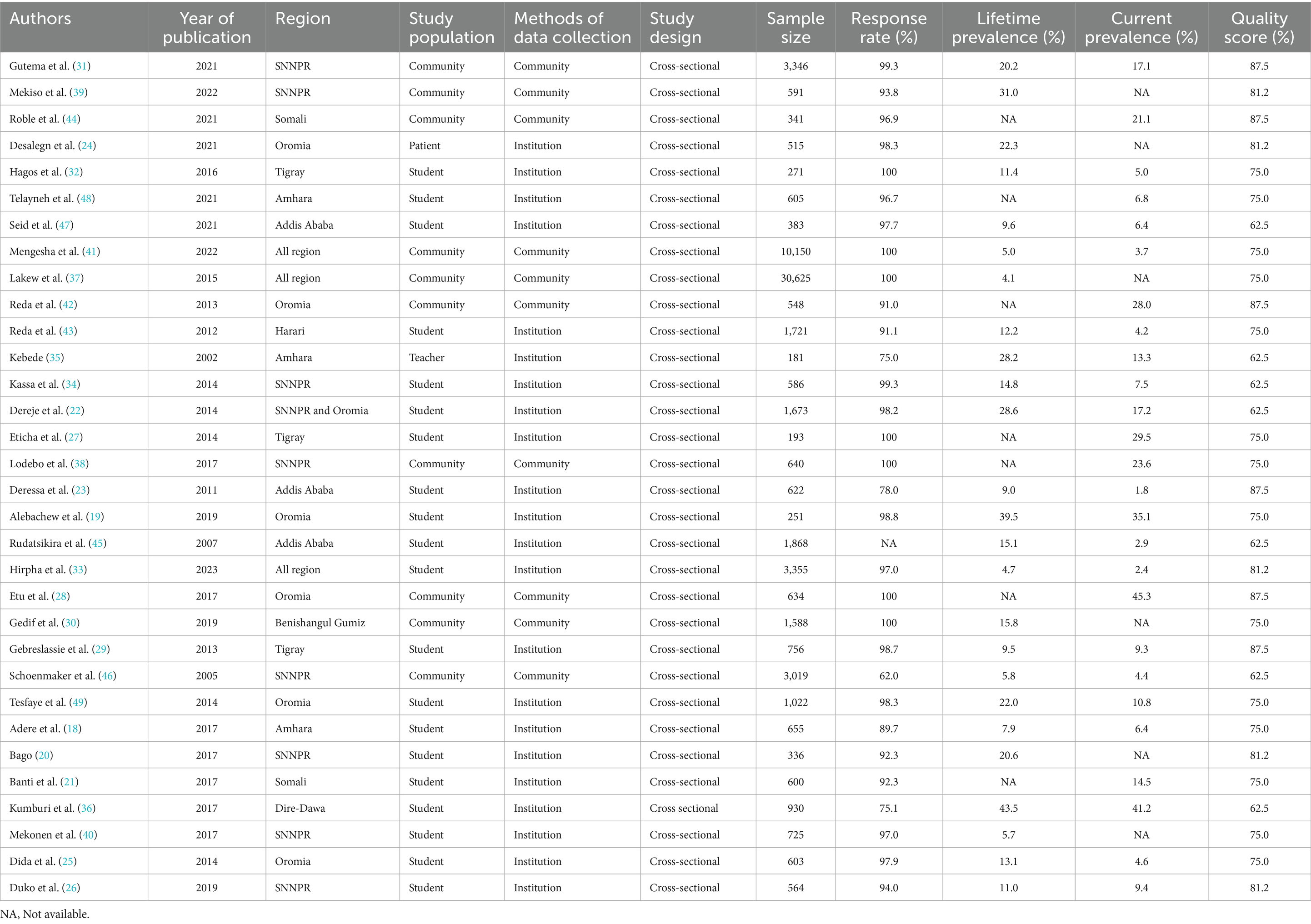
Table 1. A descriptive summary of 32 studies included estimating the pooled prevalence of tobacco smoking and associated factors among adults in Ethiopia, 2023.
Prevalence of tobacco smoking
In this meta-analysis, 25 and 26 studies were included to estimate the pooled prevalence of lifetime and current tobacco smoking, respectively. The pooled prevalence of lifetime tobacco smoking among adults was 16.0% (95% CI: 13.6–18.39). A random-effects model revealed that the included articles have high heterogeneity (I2 = 99.1%; p < 0.001) (Figure 2). Similarly, the pooled prevalence of current tobacco smoking was 13.7% (95% CI: 11.40–16.10), with significant heterogeneity (I2 = 98.9%; p < 0.001) (Figure 3).
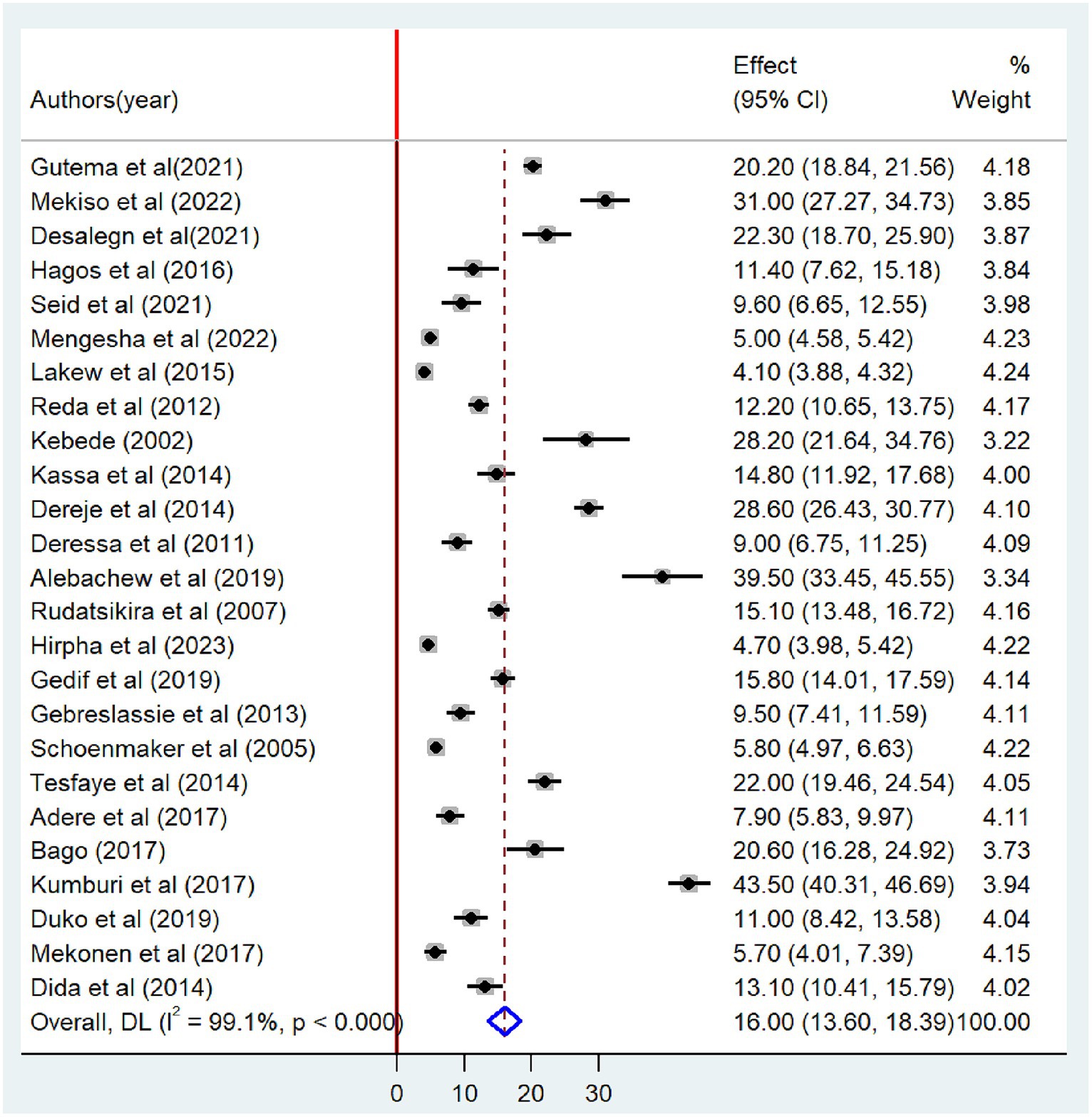
Figure 2. Forest plot showing the pooled prevalence of lifetime tobacco smoking among adults in Ethiopia, 2023.
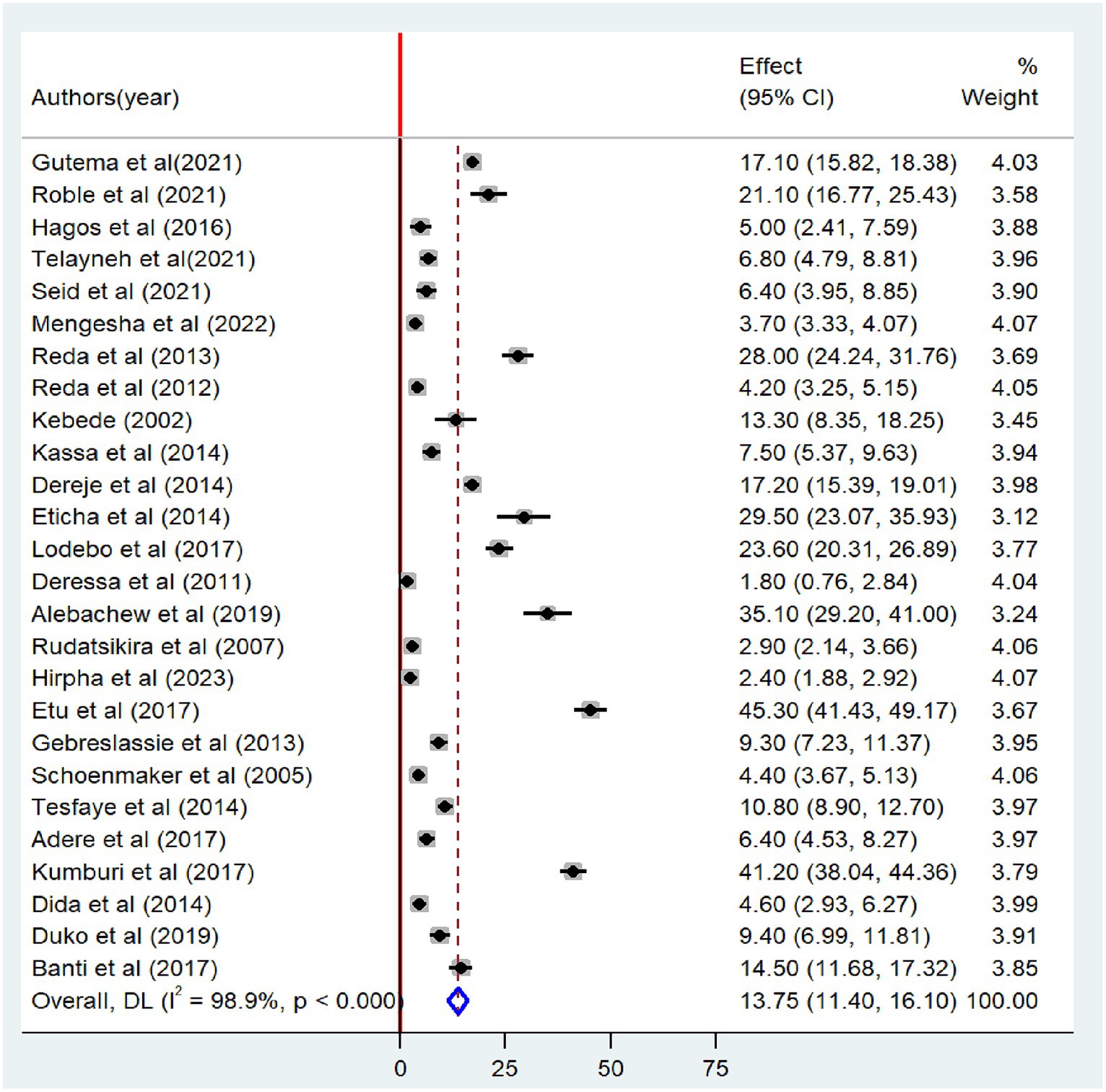
Figure 3. Forest plot of the pooled prevalence of current tobacco smoking among adults in Ethiopia, 2023.
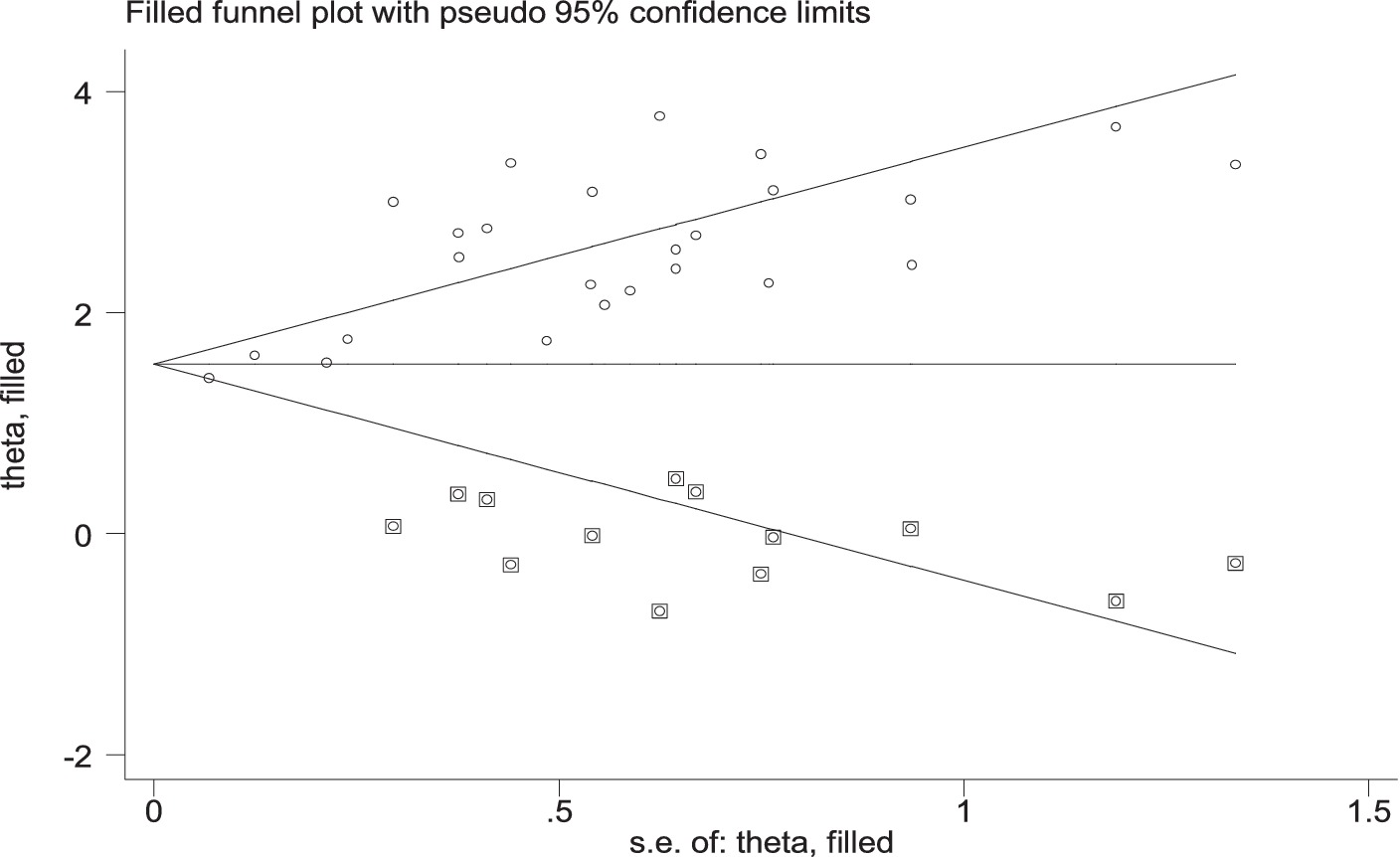
Publication bias
Publication bias was subjectively evaluated by using a funnel plot. The finding indicated that there is asymmetrical distribution of the studies, which suggests the presence of publication bias (Figure 4). The Egger test statistics also revealed the presence of statistically significant publication bias (p < 0.001). Duval and Tweedie’s “trim and fill” analysis indicates significant variation in the newly estimated pooled odds ratio (the adjusted point estimate) [OR = 1.68, (95% CI: 1.36–1.99)] as compared to the initial or observed point estimate [OR = 2.42, (95% CI: 2.11–2.73)] (Figure 5).
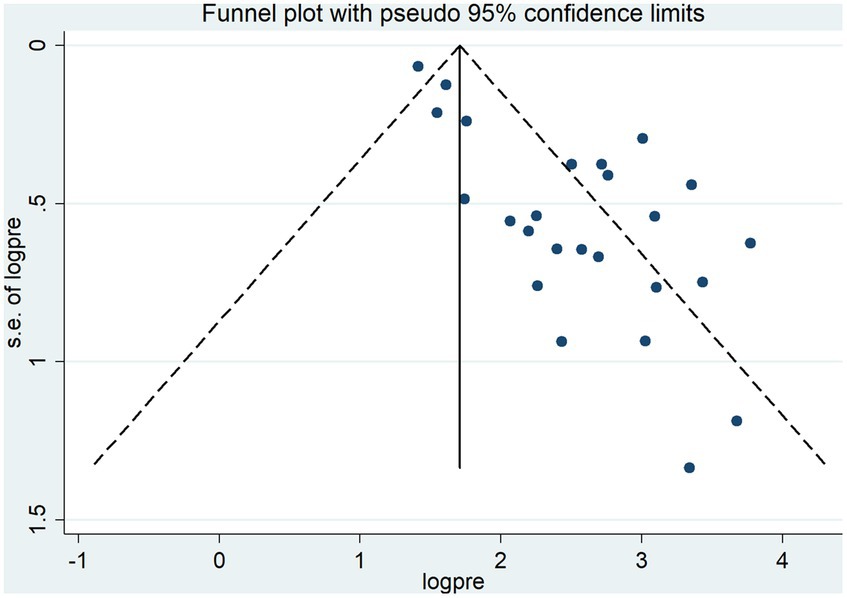
Figure 4. Funnel plot of the pooled lifetime prevalence of tobacco smoking among adults in Ethiopia, 2023.
Sensitivity analysis
The findings of sensitivity analysis suggest no evidence of a single study’s effect on the overall pooled prevalence (Figure 6).
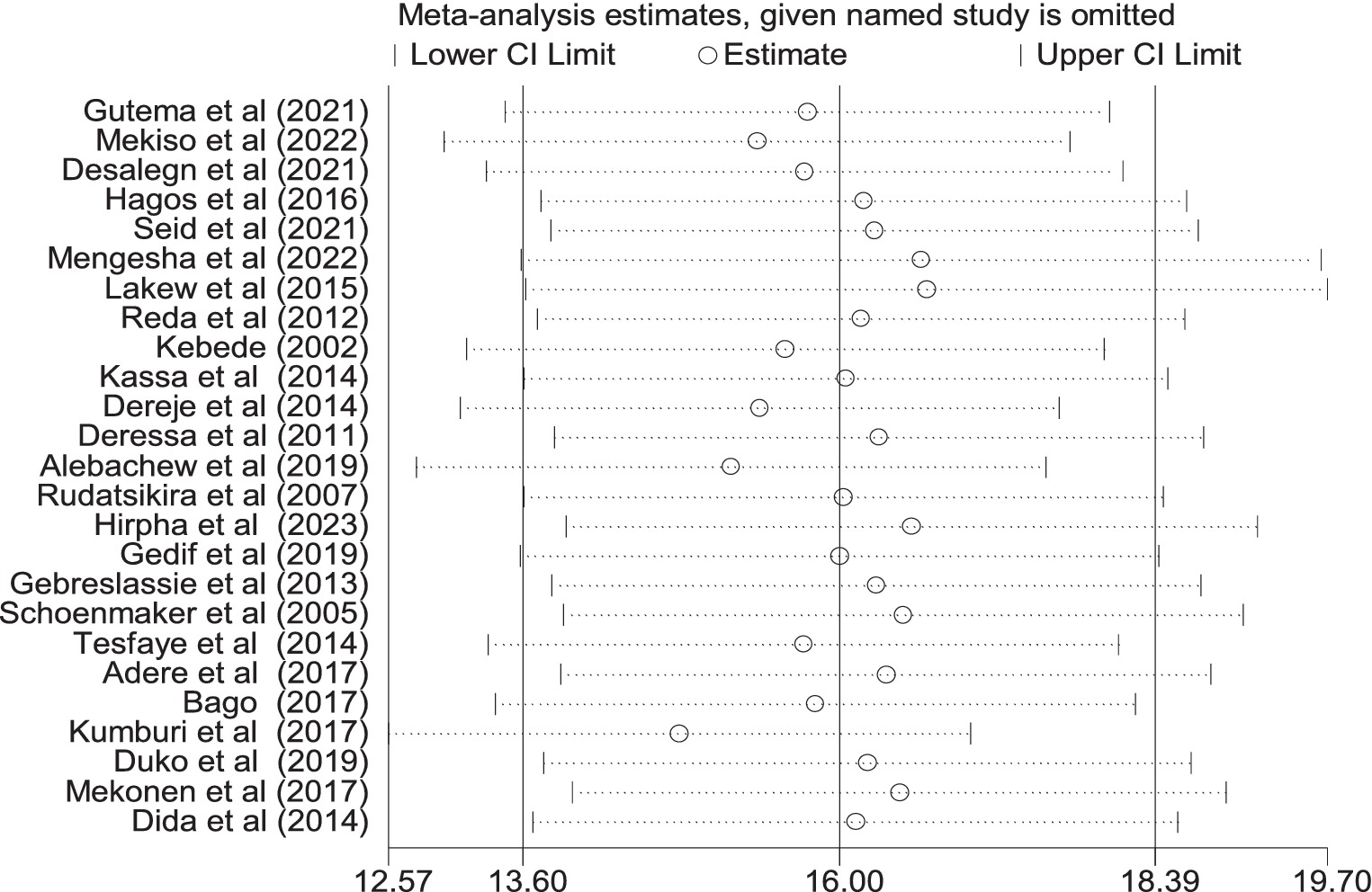
Figure 6. Sensitivity analysis of the pooled prevalence of lifetime cigarette smoking among adults in Ethiopia, 2023.
Subgroup analysis
To identify the source of heterogeneity among the included research articles, sub-group analysis was carried out based on the region where the studies were conducted, study population, year of publication, study setting, and sample size. Even though heterogeneity was not resolved among the included articles, the pooled prevalence of lifetime tobacco smoking was relatively higher among students than the general population [16.2 (95% CI: 11.94–20.45)]. In addition, a high prevalence of tobacco smoking was observed in the studies done in the Oromia region as compared to other regions [24.7 (95%CI: 17.87–31.71)], with significant heterogeneity (I2 = 96.3; p < 0.001). Similarly, the prevalence of tobacco smoking was high among institutional-based studies [15.9 (95%CI: 13.59–18.39)] as compared with community-based studies [13.1 (95%CI: 9.64–16.60)], with statistically significant heterogeneity (I2 = 99.4; p < 0.001) (Table 2). In addition, a univariate meta-regression was conducted using the study population, sample size, and study year as factors. However, neither of them was found to be a statistically significant source of heterogeneity (Table 3).
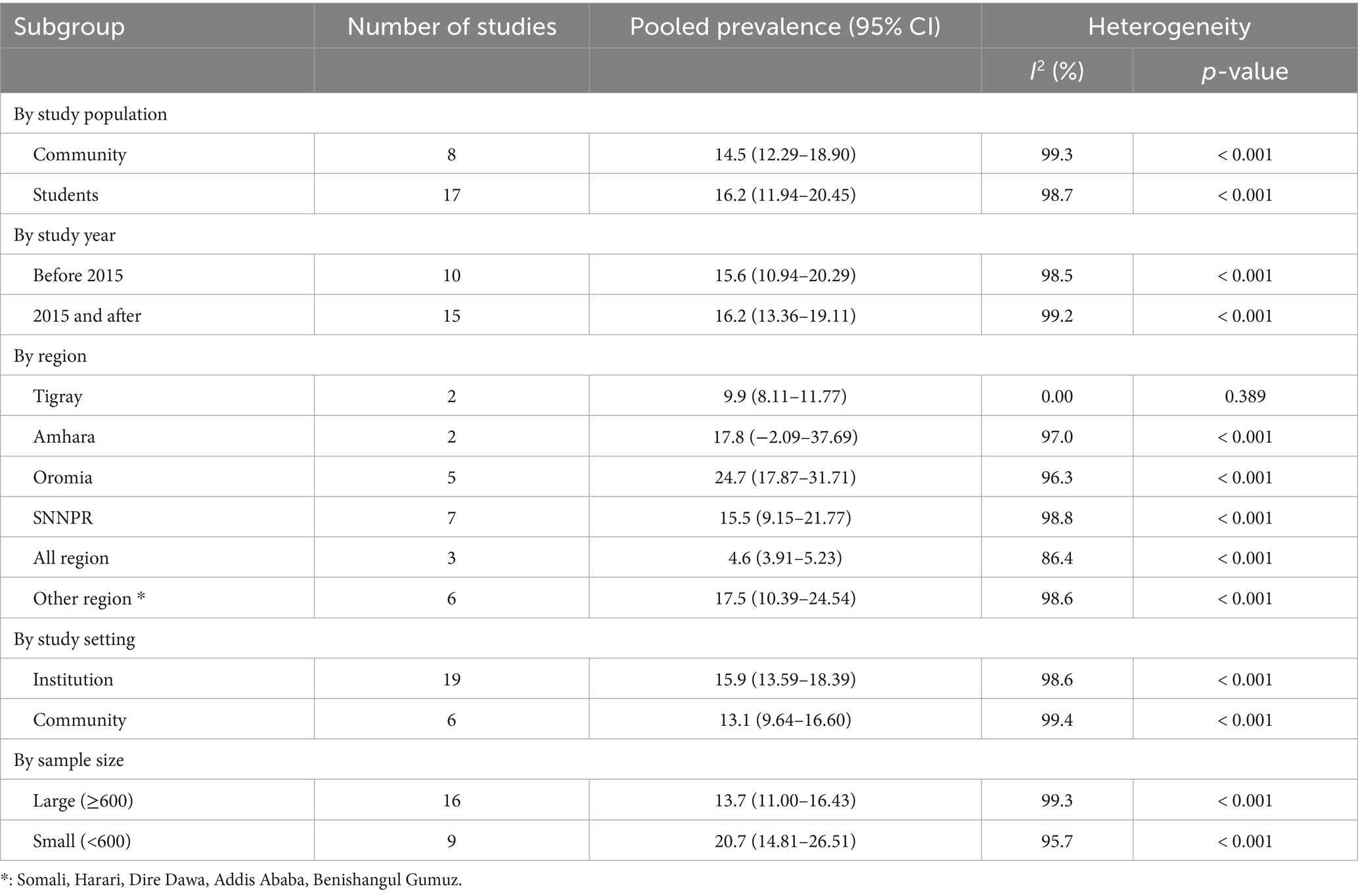
Table 2. Subgroup analysis of the pooled prevalence of tobacco smoking among adults in Ethiopia, 2023.
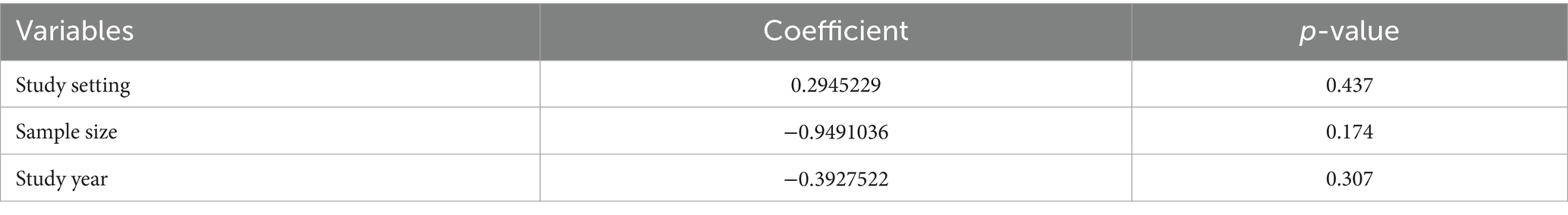
Table 3. Univariate meta-regression analysis to identify factors associated with the heterogeneity of the prevalence of tobacco smoking in Ethiopia, 2023.
Factors associated with tobacco smoking
A total of 17 studies were used to identify factors associated with tobacco smoking (18–24, 26, 27, 29, 30, 34–36, 38, 39, 44). The results from the random-effects model showed that the odds of tobacco smoking were three times higher among males compared with females (OR = 3.22, 95% CI: 2.06–5.03). Significant heterogeneity was observed among the included articles (I2 = 93.1%, p < 0.001) (Figure 7). The association between alcohol consumption factors and tobacco smoking was examined based on the results of ten studies (18, 20–23, 26, 29, 31, 34, 39). Eight of the included studies had a positive association (18, 20–22, 26, 29, 31, 34) while a negative association was noted in the other two studies (23, 39). The odds of tobacco smoking were 3.78 times higher among alcohol users than non-alcohol users (OR = 3.78, 95%CI: 1.27–11.24) (Figure 8).
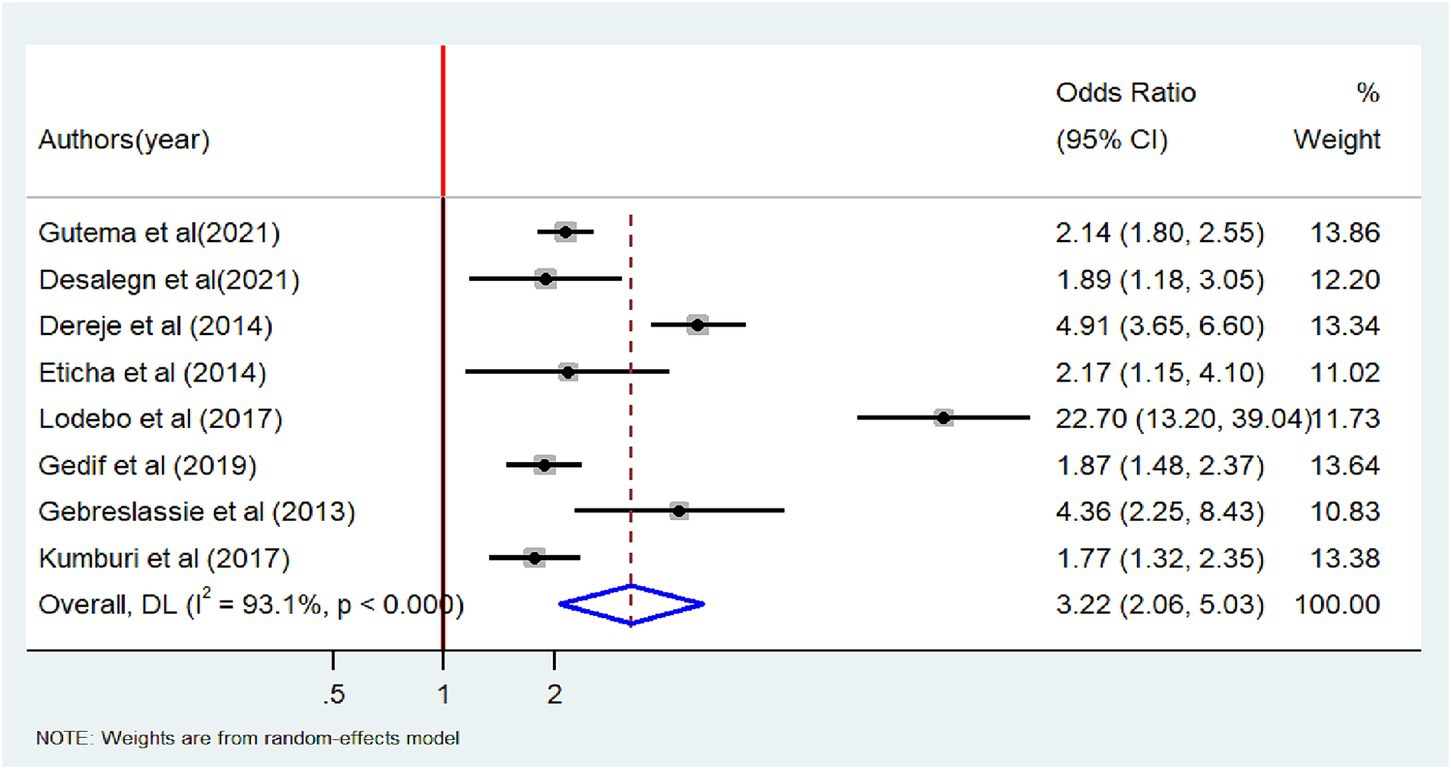
Figure 7. Forest plot of odds ratio for the association between male and tobacco smoking among adults in Ethiopia, 2023.
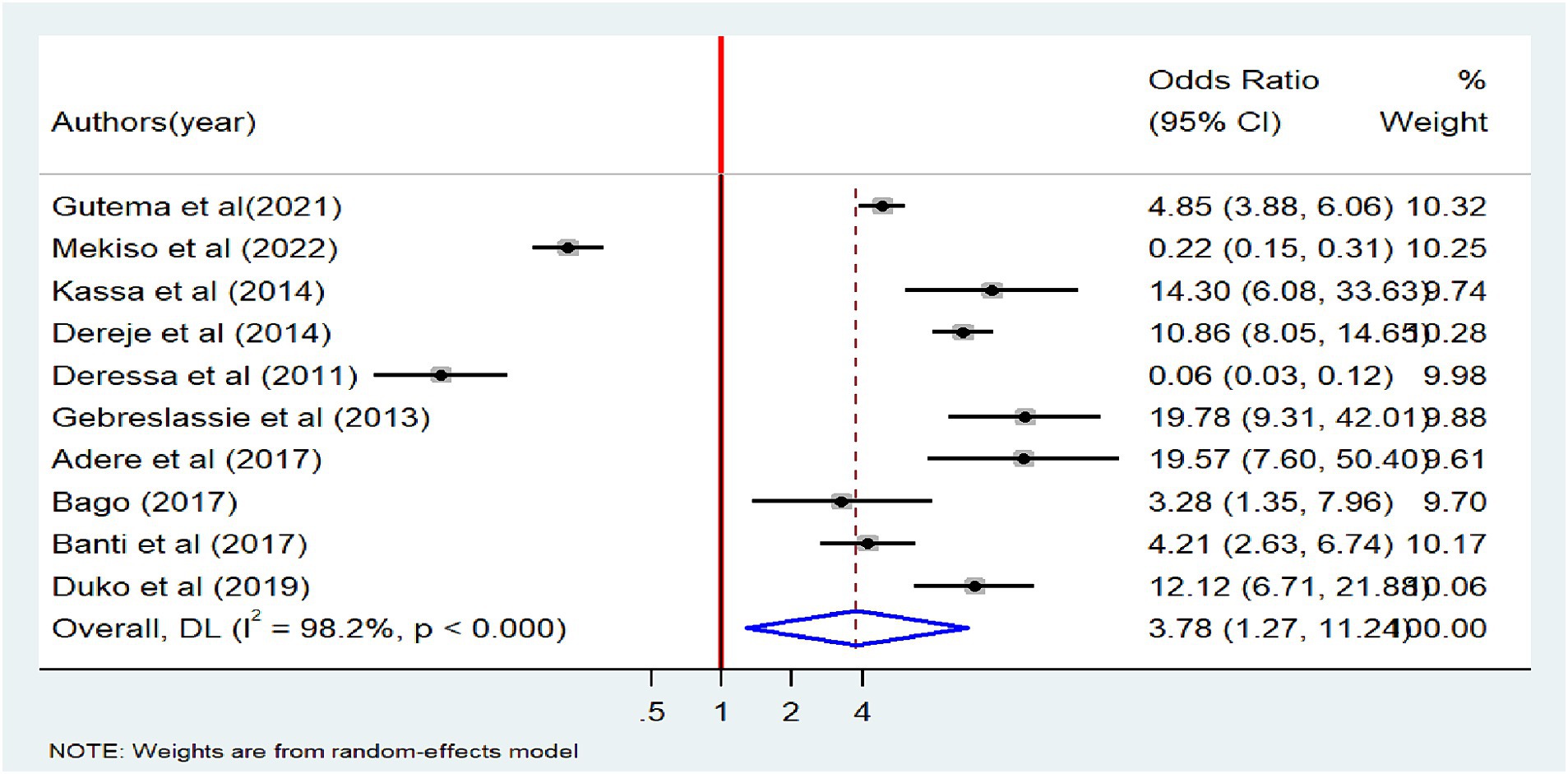
Figure 8. Forest plot of odds ratio for the association between alcohol use and tobacco smoking among adults in Ethiopia, 2023.
A total of 12 studies were included to identify the association between chewing khat and tobacco smoking (18, 20, 21, 23, 26, 27, 29, 31, 34, 36, 38, 44). Ten of the included studies had a positive association (18, 21, 26, 27, 29, 31, 34, 36, 38, 44) while a negative association was noted in the other two studies (20, 23). The result of the random-effects meta-analysis showed that non-significant association between tobacco smoking and chewing khat (OR = 3.96, 95%CI: 0.96–16.29) (Table 4).

Table 4. The pooled effect size of factors associated with lifetime tobacco smoking among adults in Ethiopia, 2023.
Five studies (22, 26, 29, 36, 44) were included to assess if having tobacco-smoking friends is associated with tobacco smoking. All of the included studies had a positive association. The meta-analysis also showed that the odds of tobacco smoking were seven times higher among adults who have tobacco-smoking friends compared to those who did not have smoking friends [OR = 7.21 (95%CI: 5.56–9.35)], with extreme heterogeneity (I2 = 40.1%, p = 0.154) (Figure 9).
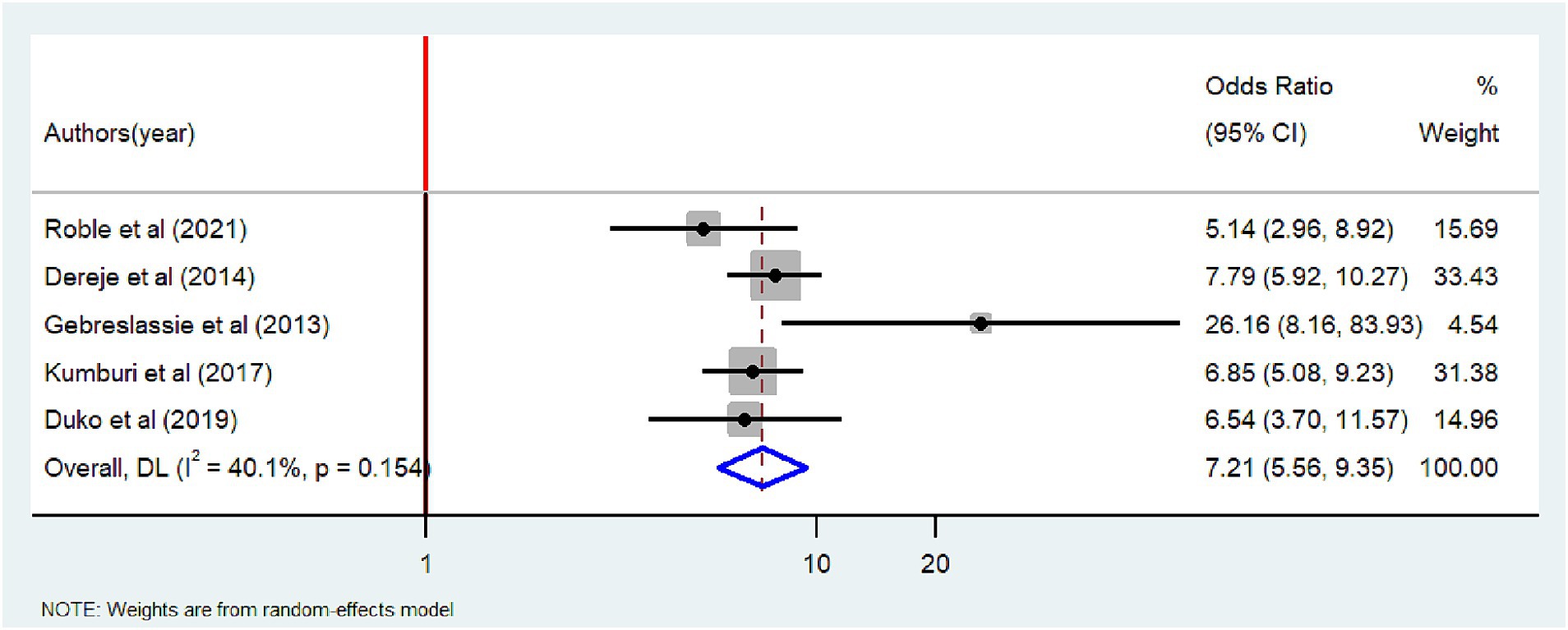
Figure 9. Forest plot of odds ratio describing having tobacco smoking friends and tobacco smoking among adults in Ethiopia, 2023.
A total of 4 studies (22, 35, 39, 44) were included to assess if having a tobacco-smoking parent is associated with tobacco smoking. Three of the included studies had a positive association (22, 35, 44) while a negative association in one study (39). Meta-analysis also showed that there was a non-significant association between parental smoking habits and adult tobacco smoking [OR = 2.16 (95%CI: 0.28–16.83)] (Table 4).
Discussion
Tobacco smoking continues to be a global public health problem and its burden increases over time, particularly in low- and middle-income countries. This systematic review and meta-analysis was conducted to estimate the pooled prevalence of tobacco smoking among adults in Ethiopia. The lifetime and current pooled prevalence of tobacco smoking among adults were 16.0 and 13.7%, respectively, with high heterogeneity. The figures in our report are greater than the findings from a meta-analysis conducted in Mainland China (10.8%) (59) and East Africa (9.0%) (60), which could be due to the lack of full enforcement and implementation of tobacco smoking in Ethiopia. It is documented that the lack of effective implementations of cigarette sale prevention policies contributes to the high proportion of tobacco smokers (61).
On the other hand, the prevalence in our study is lower than that reported in Saudi Arabia (28.1%) (62), Kenya (42.8%) (63), Poland (30.8%) (64), China (31.8%) (65), Madagascar (28.5%) (66), and Bangladesh (23.2%) (67). This difference could be due to variations in the study population and setting. For instance, most of the aforementioned studies were conducted among students, who were likely to be exposed to smoking as a result of their age and peer pressure. Evidence from our subgroup analysis also showed that the pooled prevalence of tobacco smoking was significantly higher among students than studies conducted among the general population, which is in agreement with previous reports from systematic review and meta-analyses (68).
Gender was a significant predictor of tobacco smoking. The odds of tobacco smoking were two times higher among males than females. This finding was in line with a report from systematic reviews done in Iran (69), Sub-Saharan Africa (70), Saudi Arabia (62), and a meta-analysis conducted among students in Ethiopia (68). This might be associated with better social acceptance of substance use, such as khat, tobacco, and alcohol, among males than females. On the other hand, family relationships including care and family-related activities may protect females from being involved in tobacco use (71).
The odds of tobacco smoking were three times higher among alcohol users than non-users. Our finding was in agreement with a previous report from the Nigerian community (72). This might be due to the fact that alcohol use often takes place in social settings where smoking is prevalent, especially in public places. Another possible reason for this finding might be due to peer influence and social norms that can enhance tobacco smoking behavior. Other studies also indicated that adults who drink alcohol are highly likely to smoke tobacco (73, 74). This implies that addiction invites further addictions.
The meta-analysis showed that the odds of tobacco smoking were seven times higher among adults who have smoking friends compared to those who did not have smoking friends. This finding was consistent with studies conducted in Nepal (75), Madagascar (76), Cameroon (77), and Jordan (78). This implies the need for continuous social influence programs that can help create social norms that discourage young people from starting to smoke.
Strengths and limitations of the study
This review included most regions of the country and a diverse target population (students and other community members including healthcare workers and patients). The study followed preferred reporting items for systematic review and meta-analysis guideline. However, studies included in this systematic review and meta-analysis were cross-sectional, which limits the causality of predictors on tobacco smoking. Besides, this study included articles published in the English language only, which could induce publication bias.
Conclusion
The pooled prevalence of tobacco smoking was high in Ethiopia. We found that one in six adults was engaged in tobacco smoking, which calls for urgent intervention. Being male and alcohol users, and having tobacco-smoking parents and friends were found to be factors positively associated with tobacco smoking. Therefore, urgent comprehensive public health intervention should be taken to reduce the burden of the problem. Moreover, the federal Ministry of Health, community leaders, and other concerned bodies should take strong action to protect the health of adults. In addition, alcohol control law enforcement should be strengthened.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CD: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AA: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. SD: Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing. MD: Data curation, Funding acquisition, Investigation, Resources, Supervision, Validation, Writing – review & editing. BD: Conceptualization, Investigation, Methodology, Resources, Supervision, Validation, Writing – review & editing. MG: Data curation, Investigation, Resources, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization . Tobacco fact sheet. Available at: https://www.who.int/news-room/fact-sheets/detail/tobacco (2022).
2. Guidon, G, and Boisclair, D. Current and future trends in tobacco use. World Bank human development network. Health Nutr Popul Discuss Pap. (2007) 4:1–62.
3. WHO . Global status report on noncommunicable diseases. Available at: http://www.who.int/substance_abuse (2010).
4. NF, M . Epidemiology of tobacco use and dependence in sub-Saharan Africa: a systematic review. J Pulmonol Clin Res. (2018) 2:9–15.
5. World Health Organization . WHO global report on trends in prevalence of tobacco use 2000–2025. Geneva: World Health Organization (2019).
6. Schuller, HM . The impact of smoking and the influence of other factors on lung cancer. Expert Rev Respir Med. (2019) 13:761–9. doi: 10.1080/17476348.2019.1645010
7. U.S. Department of Health and Human Services . The health consequences of smoking: 50 years of progress. a report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health (2014).
8. Eriksen, M, Mackay, J, Schluger, N, Gomeshtapeh, F, and Drope, J. The tobacco atlas. Atlanta, GA: American Cancer Society, Word Lung (2015).
9. Goodchild, M, Nargis, N, and Tursan, d'E E. Correction: global economic cost of smoking-attributable diseases. Tob Control. (2018) 27:58–64. doi: 10.1136/tobaccocontrol-2016-053305
10. WHO Regional Office for South-East Asia . Tobacco control for sustainable development. Available at: https://apps.who.int/iris/handle/10665/255509 (2017)
11. Hossain, S, Hossain, S, Ahmed, F, Islam, R, Sikder, T, and Rahman, A. Prevalence of tobacco smoking and factors associated with the initiation of smoking among university students in Dhaka, Bangladesh. Cent Asian J Glob Health. (2017) 6. doi: 10.5195/cajgh.2017.244
12. Mbatchou Ngahane, B, Luma, H, Mapoure, Y, Fotso, Z, and Afane, ZE. Correlates of cigarette smoking among university students in Cameroon. Int J Tuberc Lung Dis. (2013) 17:270–4. doi: 10.5588/ijtld.12.0377
13. Pankaj, JP, Rathore, MS, Saini, P, and Mangal, A. Prevalence and associated factors of tobacco smoking among undergraduate medical and dental students in Rajasthan. Int J Sci Study. (2015) 3:63–7. doi: 10.17354/ijss/2015/307
14. Saravanan, C, and Heidhy, I. Psychological problems and psychosocial predictors of cigarette smoking behavior among undergraduate students in Malaysia. Asian Pac J Cancer Prev. (2014) 15:7629–34. doi: 10.7314/APJCP.2014.15.18.7629
15. Elegbede, O, Babatunde, O, Ayodele, L, Atoyebi, O, Ibirongbe, D, and Adeagbo, A. Cigarette smoking practices and its determinants among university students in southwest, Nigeria. Asian J Sci Res. (2012) 2:1–10.
16. Nasser, AM, Salah, BA, Regassa, LT, Alhakimy, AA, and Zhang, X. Smoking prevalence, attitudes and associated factors among students in health-related departments of community college in rural Yemen. Tob Induc Dis. (2018) 16:31. doi: 10.18332/tid/92547
17. Khubaib, MU, Shahid, ZY, Lodhi, SK, Malik, H, and Jan, MM. Prevalence and associated factors of smoking among final year medical students: a multicentric survey from Pakistan. Cureus. (2016) 8:e701. doi: 10.7759/cureus.701
18. Adere, A, Yimer, NB, Kumsa, H, and Liben, ML. Determinants of psychoactive substances use among Woldia University students in northeastern Ethiopia. BMC Res Notes. (2017) 10:1–7. doi: 10.1186/s13104-017-2763-x
19. Alebachew, W, Semahegn, A, Ali, T, and Mekonnen, H. Prevalence, associated factors and consequences of substance use among health and medical science students of Haramaya University, eastern Ethiopia, 2018: a cross-sectional study. BMC Psychiatry. (2019) 19:1–9. doi: 10.1186/s12888-019-2340-z
20. Bago, BJ . Prevalence of cigarette smoking and its associated risk factors among students of Hawassa University, College of Medicine and Health Sciences, 2016. J Addict Res Ther. (2017) 08:2. doi: 10.4172/2155-6105.1000331
21. Banti, TK, Mengesha, DS, and Mamade, GF. Prevalence of cigarette smoking and factors associated with it among undergraduate students of Jigjiga University. Int J Psychol Brain Sci. (2017) 2:87–91. doi: 10.11648/j.ijpbs.20170203.13
22. Dereje, N, Abazinab, S, and Girma, A. Prevalence and predictors of cigarette smoking among adolescents of Ethiopia: School based cross sectional survey. J. Child. Adolesc. Behav. (2014) 3: 182. doi: 10.4172/2375-4494.1000182
23. Deressa, W, and Azazh, A. Substance use and its predictors among undergraduate medical students of Addis Ababa University in Ethiopia. BMC Public Health. (2011) 11:1–11. doi: 10.1186/1471-2458-11-660
24. Desalegn, D, Abdu, Z, and Hajure, M. Prevalence of tobacco dependence and associated factors among patients with schizophrenia attending their treatments at Southwest Ethiopia; hospital-based cross-sectional study. PLoS One. (2021) 16:e0261154. doi: 10.1371/journal.pone.0261154
25. Dida, N, Kassa, Y, Sirak, T, Zerga, E, and Dessalegn, T. Substance use and associated factors among preparatory school students in bale zone, Oromia regional state. Southeast Ethiop Harm Reduct J. (2014) 11:21–6. doi: 10.1186/1477-7517-11-21
26. Duko, B, Melese, Y, and Ebrahim, J. Determinants of cigarette smoking among adolescents in Ethiopia: a cross-sectional study. Tob Induc Dis. (2019) 17:17. doi: 10.18332/tid/110800
27. Eticha, T, and Kidane, F. The prevalence of and factors associated with current smoking among College of Health Sciences students, Mekelle University in northern Ethiopia. PLoS One. (2014) 9:e111033. doi: 10.1371/journal.pone.0111033
28. Etu, ES, Gemeda, DH, and Hussen, MA. Prevalence and factors that influence smokeless tobacco use among adults in pastoralist communities of Borena zone, Ethiopia: mixed method study. Tob Induc Dis. (2017) 15:1–11. doi: 10.1186/s12971-016-0106-7
29. Gebreslassie, M, Feleke, A, and Melese, T. Psychoactive substances use and associated factors among Axum University students, Axum town, North Ethiopia. BMC Public Health. (2013) 13:1–9. doi: 10.1186/1471-2458-13-693
30. Gedif, T, Azale, T, and Nigusie, A. Substance use and associated factors among Gumuz people in Benishangul-Gumuz regional state, Mandura woreda, Northwest Ethiopia. Subst Abuse Treat Prev Policy. (2019) 14:1–9. doi: 10.1186/s13011-019-0225-2
31. Gutema, BT, Chuka, A, Ayele, G, Estifaons, W, Melketsedik, ZA, Tariku, EZ, et al. Tobacco use and associated factors among adults reside in Arba Minch health and demographic surveillance site, southern Ethiopia: a cross-sectional study. BMC Public Health. (2021) 21:1–10. doi: 10.1186/s12889-021-10479-4
32. Hagos, EG, Asfeha, GG, and Berihu, BA. Prevalence of substance abuse among regular degree health science students in Sheba University College in Mekelle Town, Tigray-Ethiopia. J Neurosci Rural Pract. (2016) 7:200–5. doi: 10.4103/0976-3147.178670
33. Hirpa, S, Fogarty, AW, Addissie, A, Bauld, L, Frese, T, Unverzagt, S, et al. Prevalence and risk factors for tobacco, khat and alcohol consumption among high school students in Ethiopia. BMC Public Health. (2023) 23:226. doi: 10.1186/s12889-023-15088-x
34. Kassa, A, and Deyno, S. Prevalence and determinants of active and passive cigarette smoking among undergraduate students at Hawassa University, Hawassa, Ethiopia. J Trop Dis. (2014) 2:2. doi: 10.4172/2329-891X.1000145
35. Kebede, Y . Cigarette smoking and khat chewing among university instructors in Ethiopia. East Afr Med J. (2002) 79:274–8. doi: 10.4314/eamj.v79i5.8869
36. Kumburi, GT, Gelgile, AK, Hatehu, BT, and Gemechu, DT. Psycho-active substances use and determining factors among regular undergraduate students of Dire-Dawa University, eastern Ethiopia. Sci J Public Health. (2017) 5:68–76. doi: 10.11648/j.sjph.20170502.13
37. Lakew, Y, and Haile, D. Tobacco use and associated factors among adults in Ethiopia: further analysis of the 2011 Ethiopian demographic and health survey. BMC Public Health. (2015) 15:1–8. doi: 10.1186/s12889-015-1820-4
38. Lodebo, T, Hajito, K, Gebrehiwot, T, and Achicha, T. Prevalence of cigarette smoking and its associated factors among parents at Misrak Bedawacho District, southern Ethiopia. J Addict Prev. (2017) 5:9.
39. Mekiso, AB, Fonkamo, TT, Wontamo, TE, Liben, FE, Turuse, EA, Watumo, AM, et al. Prevalence of cigarette smoking and associated factors among residents of Hossana town, southern Ethiopia. Biomed Res Int. (2022) 2022:1–7. doi: 10.1155/2022/2272281
40. Mekonen, T, Fekadu, W, Mekonnen, TC, and Workie, SB. Substance use as a strong predictor of poor academic achievement among university students. Psychiatry J. (2017) 2017:1–9. doi: 10.1155/2017/7517450
41. Mengesha, SD, Teklu, KT, Weldetinsae, A, Serte, MG, Kenea, MA, Dinssa, DA, et al. Tobacco use prevalence and its determinate factor in Ethiopia-finding of the 2016 Ethiopian GATS. BMC Public Health. (2022) 22:1–13. doi: 10.1186/s12889-022-12893-8
42. Reda, AA, Kotz, D, and Biadgilign, S. Adult tobacco use practice and its correlates in eastern Ethiopia: a cross-sectional study. Harm Reduct J. (2013) 10:28–6. doi: 10.1186/1477-7517-10-28
43. Reda, AA, Moges, A, Yazew, B, and Biadgilign, S. Determinants of cigarette smoking among school adolescents in eastern Ethiopia: a cross-sectional study. Harm Reduct J. (2012) 9:39–6. doi: 10.1186/1477-7517-9-39
44. Roble, AK, Osman, MO, Lathwal, OP, and Aden, AA. Prevalence of cigarette smoking and associated factors among adolescents in eastern Ethiopia. Subst Abus Rehabil. (2020) 12:73–80. doi: 10.2147/SAR.S331349
45. Rudatsikira, E, Abdo, A, and Muula, AS. Prevalence and determinants of adolescent tobacco smoking in Addis Ababa, Ethiopia. BMC Public Health. (2007) 7:1–6. doi: 10.1186/1471-2458-7-176
46. Schoenmaker, N, Hermanides, J, and Davey, G. Prevalence and predictors of smoking in Butajira town, Ethiopia. Ethiop J Health Dev. (2005) 19:182–7.
47. Seid, L, Gintamo, B, Mekuria, ZN, Hassen, HS, and Gizaw, Z. Substance use and associated factors among preparatory school students in Kolfe-Keranyo sub-city of Addis Ababa, Ethiopia. Environ Health Prev Med. (2021) 26:1–12. doi: 10.1186/s12199-021-01032-1
48. Telayneh, AT, Gedefaw, M, Haile, D, Habtegiorgis, SD, Getahun, DS, Tafere, Y, et al. Cigarette smoking prevalence and associated factors among college students, Amhara, Ethiopia. Pan Afr Med J. (2021) 40. doi: 10.11604/pamj.2021.40.170.24413
49. Tesfaye, G, Derese, A, and Hambisa, MT. Substance use and associated factors among university students in Ethiopia: a cross-sectional study. J Addict. (2014) 2014:1–8. doi: 10.1155/2014/969837
50. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906.
52. Peters, MD, Godfrey, CM, McInerney, P, Soares, CB, Khalil, H, and Parker, D. The Joanna Briggs institute reviewers' manual 2015: Methodology for JBI scoping reviews Adelaide, SA Australia: The Joanna Briggs Institute.(2015) 24.
53. Tufanaru, C, Munn, Z, Aromataris, E, Campbell, J, and Hopp, L. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. (2017).
54. Munn, Z, Moola, S, Lisy, K, Riitano, D, and Tufanaru, C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. JBI Evidence Implementation. (2015) 13:147–53. doi: 10.1097/XEB.0000000000000054
56. Higgins, JP, and Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
57. DerSimonian, R, and Laird, N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. (2015) 45:139–45. doi: 10.1016/j.cct.2015.09.002
58. Egger, M SG, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ (1997); 315:629–634. doi: 10.1136/bmj.315.7109.629
59. Niu, L, Liu, Y, Luo, D, and Xiao, S. Current smoking behavior among medical students in mainland China: a systematic review and meta-analysis. Asia Pac J Public Health. (2018) 30:610–23. doi: 10.1177/1010539518800339
60. Tezera, N, and Endalamaw, A. Current cigarette smoking and its predictors among school-going adolescents in East Africa: a systematic review and meta-analysis. Int J Pediatr. (2019) 2019:1–9. doi: 10.1155/2019/4769820
61. Habebo, TT, and Takian, A. Retrospective policy analysis of tobacco prevention and control in Ethiopia. Ethiop J Health Sci. (2020) 30. doi: 10.4314/ejhs.v30i3.14
62. Al Mohamed, H, and Amin, T. Pattern and prevalence of smoking among students at king faisal university, Al Hassa, Saudi Arabia. East Mediterr Health J. (2010) 16:56–64. doi: 10.26719/2010.16.1.56
63. Atwoli, L, Mungla, PA, Ndung'u, MN, Kinoti, KC, and Ogot, EM. Prevalence of substance use among college students in Eldoret, western Kenya. BMC Psychiatry. (2011) 11:1–9. doi: 10.1186/1471-244X-11-34
64. Kanicka, M, Szpak, A, Drygas, W, Rzeźnicki, A, and Kowalska, A. The prevalence of tobacco smoking among public health students at medical University of Białystok. Adv Med Sci. (2007) 52:60–3.
65. Li, Z, Yao, Y, Han, W, Yu, Y, Liu, Y, Tao, Y, et al. Smoking prevalence and associated factors as well as attitudes and perceptions towards tobacco control in Northeast China. Int J Environ Res Public Health. (2015) 12:8606–18. doi: 10.3390/ijerph120708606
66. Pampel, F . Tobacco use in sub-Sahara Africa: estimates from the demographic health surveys. Soc Sci Med. (2008) 66:1772–83. doi: 10.1016/j.socscimed.2007.12.003
67. Sultana, P, Akter, S, Rahman, M, and Alam, M. Prevalence and predictors of current tobacco smoking in Bangladesh. J Biostat Biometric App. (2015) 1:102. doi: 10.15744/2455-765X.1.102
68. Deressa Guracho, Y, Addis, GS, Tafere, SM, Hurisa, K, Bifftu, BB, Goedert, MH, et al. Prevalence and factors associated with current cigarette smoking among Ethiopian university students: a systematic review and meta-analysis. J Addict. (2020) 2020:1–10. doi: 10.1155/2020/9483164
69. Haghdoost, AA, and Moosazadeh, M. The prevalence of cigarette smoking among students of Iran's universities: a systematic review and meta-analysis. J Res Med Sci. (2013) 18:717–25.
70. Brathwaite, R, Addo, J, Smeeth, L, and Lock, K. A systematic review of tobacco smoking prevalence and description of tobacco control strategies in sub-Saharan African countries; 2007 to 2014. PLoS One. (2015) 10:e0132401. doi: 10.1371/journal.pone.0132401
71. Van Den Bree, MB, Whitmer, MD, and Pickworth, WB. Predictors of smoking development in a population-based sample of adolescents: a prospective study. J Adolesc Health. (2004) 35:172–81. doi: 10.1016/j.jadohealth.2003.09.021
72. Eniojukan Joshua, F, and Owonaro, PA. Prevalence and contexts of smoking among the people of Kaiama community in Bayelsa state, Nigeria. UK J Pharm Biosci. (2016) 4:52–62. doi: 10.20510/ukjpb/4/i1/87846
73. De Leon, J, Rendon, DM, Baca-Garcia, E, Aizpuru, F, Gonzalez-Pinto, A, Anitua, C, et al. Association between smoking and alcohol use in the general population: stable and unstable odds ratios across two years in two different countries. Alcohol Alcohol. (2007) 42:252–7. doi: 10.1093/alcalc/agm029
74. Falk, DE, Yi, H-y, and Hiller-Sturmhöfel, S. An epidemiologic analysis of co-occurring alcohol and tobacco use and disorders: findings from the National Epidemiologic Survey on alcohol and related conditions. Alcohol Res Health. (2006) 29:162.
75. Bhaskar, RK, Sah, MN, Gaurav, K, Bhaskar, SC, Singh, R, Yadav, MK, et al. Prevalence and correlates of tobacco use among adolescents in the schools of Kalaiya, Nepal: a cross-sectional questionnaire based study. Tob Induc Dis. (2016) 14:1–7. doi: 10.1186/s12971-016-0075-x
76. Veeranki, SP, Mamudu, HM, John, RM, and Ouma, AE. Prevalence and correlates of tobacco use among school-going adolescents in Madagascar. J Epidemiol Glob Health. (2015) 5:239–47. doi: 10.1016/j.jegh.2014.12.005
77. Mbatchou Ngahane, BH, Atangana Ekobo, H, and Kuaban, C. Prevalence and determinants of cigarette smoking among college students: a cross-sectional study in Douala, Cameroon. Arch Public Health. (2015) 73:1–7. doi: 10.1186/s13690-015-0100-1
Keywords: tobacco smoking, addiction, adult population, meta-analysis, Ethiopia
Citation: Daba C, Atamo A, Debela SA, Dagne M, Desye B and Gebrehiwot M (2024) Prevalence of tobacco smoking and associated factors among adults in Ethiopia: a systematic review and meta-analysis. Front. Public Health. 12:1353033. doi: 10.3389/fpubh.2024.1353033
Edited by:
Lei Wei, Shanghai University of Traditional Chinese Medicine, ChinaReviewed by:
Mamunur Rashid, University of Gävle, SwedenGiuseppa Minutolo, Provincial Health Authority of Palermo, Italy
Copyright © 2024 Daba, Atamo, Debela, Dagne, Desye and Gebrehiwot. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chala Daba, Y2hhbGFkYWJhMjkzQGdtYWlsLmNvbQ==
 Chala Daba
Chala Daba Amanuel Atamo
Amanuel Atamo Sisay Abebe Debela
Sisay Abebe Debela Mengesha Dagne1
Mengesha Dagne1 Belay Desye
Belay Desye Mesfin Gebrehiwot
Mesfin Gebrehiwot