- 1Institute of Global Health and Human Ecology, The American University in Cairo, New Cairo, Egypt
- 2The Social Research Center, The American University in Cairo, New Cairo, Egypt
- 3Department of Statistics, Faculty of Economics and Political Sciences, Cairo University, Giza, Egypt
Introduction: Inequitable access to COVID-19 vaccines among countries is a pressing global health issue. Factors such as economic power, political power, political stability, and health system strength contribute to disparities in vaccine distribution. This study aims to assess the inequality in vaccine distribution among countries based on these factors and identify their relationship with COVID-19 vaccine distribution.
Methods: A Concentration Index (CI) analysis was conducted to evaluate inequalities in the distribution of COVID-19 vaccines among countries based on four separate variables: GDP per capita, political stability (PS), World Power Index (WPI), and Universal Health Coverage (UHC). Additionally, Multiple Linear Regression (MLR) analysis was employed to explore the relationship between vaccine distribution and these independent variables. Two vaccine distribution variables were utilized for result reliability.
Results: The analysis revealed significant inequalities in COVID-19 vaccine distribution according to the countries’ GDP/capita, PS, WPI, and UHC. However, the multiple linear regression analysis showed that there is no significant relationship between COVID-19 vaccine distribution and the countries’ GDP/capita and that UHC is the most influential factor impacting COVID-19 vaccine distribution and accessibility.
Discussion: The findings underscore the complex interplay between economic, political, and health system factors in shaping vaccine distribution patterns. To improve the accessibility to vaccines in future pandemics, Global Health Governance (GHG) and countries should consider working on three areas; enhance political stabilities in countries, separate the political power from decision-making at the global level and most importantly support countries to achieve UHC.
1 Introduction
During the COVID-19 pandemic, health equity proves to be an issue of concern at both the national and international levels. At the national level, researchers have been concerned with disparities in the level of infection, consequences, and vaccination among different social groups within their countries (1–14). One of the major health equity concerns at the global level was the inequitable access to the COVID-19 vaccine, especially in the period following the start of COVID-19 vaccine production and before it became abundant. Global health governance (GHG) is responsible for the coordination of COVID-19 vaccine distribution equitably; however, this was not the case (15, 16). According to the Our World in Data website on 7 April 2022, the share of fully vaccinated people in high-income countries (HICs) and upper-middle-income countries (UMICs) reached 74.1% and 76.68%, respectively. In contrast, the share of fully vaccinated people in lower-middle-income countries (LMICs) and low-income countries (LICs) reached 50.51% and 11.51%, respectively. As for the share of partially vaccinated people, it was estimated to be 5.05%, 4.77%, 9.17%, and 3.26% in HICs, UMICs, LMICs, and LICs, respectively (17). These numbers indicate the presence of discrepancies in securing the vaccine across these country groups.
Several published studies discuss the reasons underlying inequities in COVID-19 vaccine distribution. Some studies discussed the influence of economic power in securing the vaccine as well as in controlling its distribution. Countries with high economic power can produce, trade, and control the value chain of COVID-19 vaccines (18). Their financing capacity enables the production as well as the purchase of needed vaccines. Countries’ purchasing power appeared to be determinative in the accessibility to the vaccine (19). Many HICs rushed to purchase the COVID-19 vaccine for their population even before its final approval (20). This action has affected the availability of the vaccine in other countries.
Other studies raised the issue of political power imbalance among actors and its role in vaccine accessibility. Political power has a dual role in COVID-19 vaccine accessibility, and it acts as a determinant as well as a consequence. Power has been detrimental to COVID-19 vaccine accessibility (21). Powerful countries compete to settle their ideological perspectives in the global health arena and use their power to influence less powerful countries’ accessibility to vaccines (22). Countries’ responses to the pandemic were influenced by their power resulting in vaccine nationalism (23). Western countries intentionally hoarded the vaccine for themselves and their allies ignoring other countries’ needs (24). On the other hand, countries aimed to gain power through higher accessibility to the vaccine. Fiddler stated that COVID-19-related decisions are influenced by geopolitical calculations. COVID-19 vaccine access is considered a source of political power (25). Countries with higher vaccine coverage are expected to have better chances for rapid economic recovery (26, 27). Furthermore, countries’ ability to manufacture the vaccine and decide on its distribution projects soft power and demonstrates ambition for geopolitical opportunities (28, 29).
On another front, several published studies discuss the reasons underlying inequalities in COVID-19 vaccine distribution related to countries’ health systems. These studies highlighted the limited countries’ capacities, poor infrastructure, inadequate supply chain capability, and limited technical expertise as main barriers to the manufacturing, storage, and administration of the COVID-19 vaccine in these countries, which in turn limited their access to the vaccine doses (30–34).
This research addresses two existing gaps in the literature. First, it provides quantitative measuring of the inequality in COVID-19 vaccine distribution by economic status, political stability (PS), political power, and health system strength. Second, it sheds light on the interplay between these factors with the aim of providing valuable insight into the root causes of these inequalities. Thus, the first objective of this study is to estimate the inequality in the distribution of COVID-19 vaccines among countries by their economic status, PS, political power, and health system strength. The second objective is to determine which of these factors are significantly related to the distribution of COVID-19 vaccines among countries.
2 Materials and methods
Given the objectives of the study, two types of analysis were used: concentration index (CI) analysis and multiple linear regression (MLR) analysis. CI analysis is used to determine inequalities in the distribution of the COVID-19 vaccines among countries by four separate variables. It is a recognized technique for evaluating disparities in the distribution of health-related outcomes. It is consistent with the study’s primary goal of evaluating the disparity in vaccine distribution among nations. Using CI analysis for four separate variables (political power, PS, economic status, and the strength of the health system) breaks down the analysis by these factors and helps identify specific dimensions of inequality, providing valuable insights into these factors’ contribution to the inequitable vaccine distribution.
MLR is a known method used to examine the relationship between a dependent variable and multiple independent variables. It allows this while controlling for other independent variables, enabling the identification of the significant factors influencing vaccine distribution. In this study, MLR helps in achieving the second objective by identifying the key drivers of vaccine distribution disparities among countries.
Together, CI analysis and MLR provide a comprehensive understanding of the inequities in COVID-19 vaccine distribution among countries and the underlying factors relating to this distribution.
2.1 Concentration index analysis
Different measures are used to assess inequality in health (35, 36). The most commonly used are the CI (37, 38), the Gini coefficient (39, 40), the index of dissimilarity (41), the range (42) and the slope and relative indices of inequality (37). The current research uses the CI approach to examine inequalities in COVID-19 vaccine distribution among countries using STATA 15.
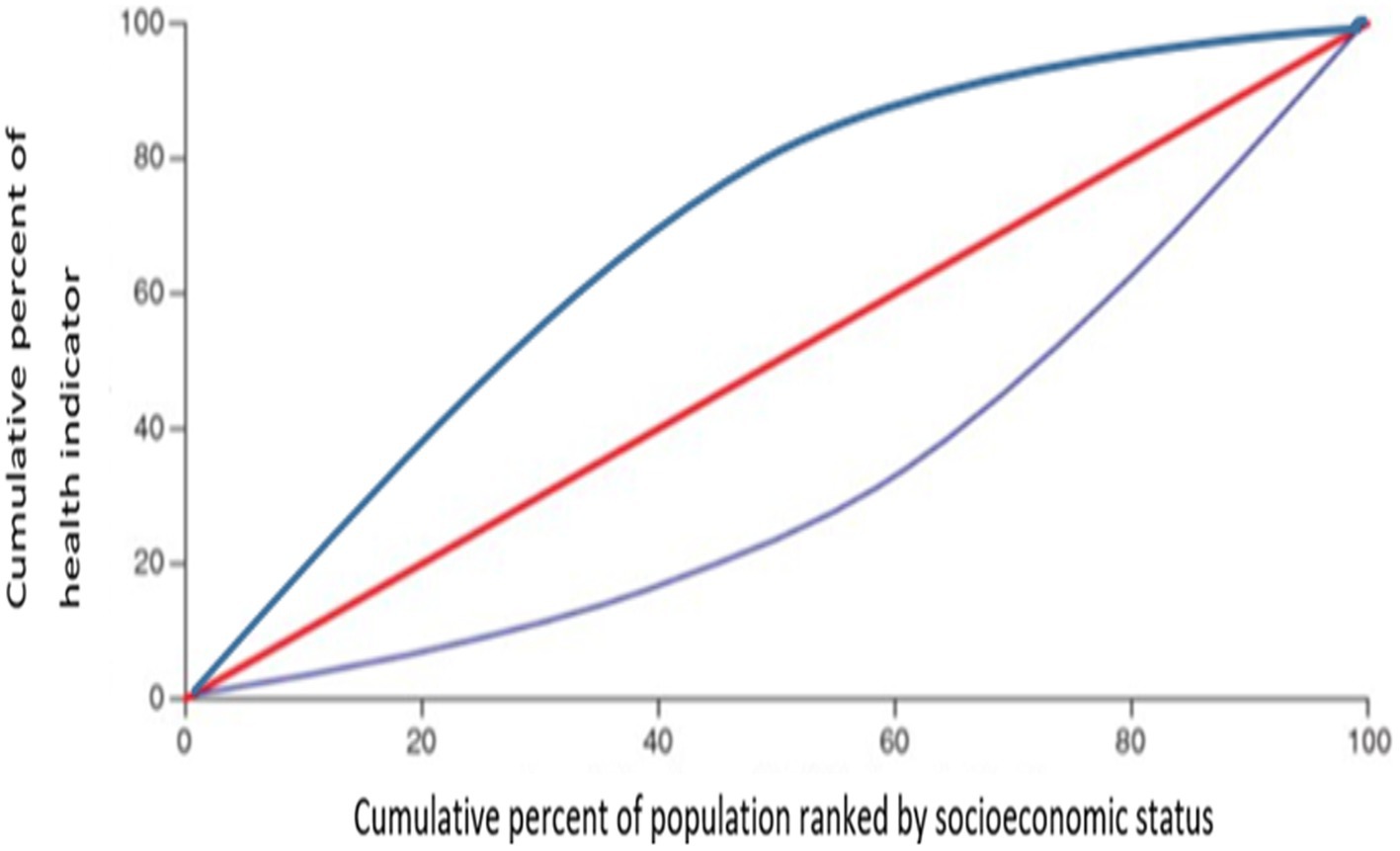
CI is an index used to measure inequalities in health that are associated systemically with socioeconomic status. It is calculated from the concentration curve. The concentration curve is plotted as follows: On the X-axis is the cumulative proportion of countries ranked according to their socioeconomic status (i.e., GDP/capita, for this study), starting from the least advantaged to the most advantaged. On the Y-axis is the cumulative proportion of health (i.e., vaccine distribution among countries, for this study). The CI is twice the area between the concentration curve and the diagonal (line of equality; Figure 1). Inequality is observed when the concentration curve is not aligned with the line of equality. The more convex the concentration curve, the higher the inequality (37, 43). The CI is calculated as follows:
N = the number of categories of the social grouping
hi = the health variable (vaccine distribution)
μ = the mean of the health variable
ri = is the fractional rank of country i in the social grouping, with i = 1 for the lowest social grouping and i = N for the highest
2.2 Multiple linear regression analysis
MLR is a statistical technique that estimates the relationship between one dependent variable and two or more independent variables and how the dependent variable will change when independent variables change (44).
Assuming that the used health indicator (y), which in this case is COVID-19 vaccine distribution (i.e., TVH and VPP), is related to a number of factors, the relationship between the health indicator and these factors can be written using a linear regression model:
= the predicted value of the dependent variable
= y-intercept, value of y when all other parameters are set to 0
= the regression coefficient ( ) of the first independent variable ()
= the regression coefficient of the last independent variable
= model error
MLR has three assumptions: there is no multicollinearity, which means that the independent variables are not highly correlated with each other. Homoscedasticity requires that the variance of the errors should be constant across all levels of the independent variables. Furthermore, autocorrelation requires that the residuals (errors) should be independent of each other.
To ensure the reliability of the MLR analysis results of this study, three tests were performed: a variance inflation factor (VIF) analysis was conducted to examine multicollinearity among independent variables. The results showed that all VIP scores were less than 5, meaning that multicollinearity is very law (45). A Breusch–Pagan test was performed to measure homoscedasticity. The result shows a high p-value (p = 0.980) suggesting that the all-independent data ensure homoscedasticity (46). The Durbin–Watson test was performed to detect autocorrelation in the residuals. The value of the Durbin–Watson test was 2.042, indicating no significant autocorrelation (47). The three aforementioned analyses along with the MLR, were performed using SPSS 26.
2.3 Data sources and study variables
For the COVID-19 vaccine distribution, two variables were used: first, total vaccinations per 100 people within a given population (TVH). TVH is the number of vaccine doses administered per 100 people within a given population, including booster doses. All doses are counted individually (17). Data for this indicator were extracted on 17 May 2022. Second, vaccine courses delivered as a proportion of the country’s population (VPP). VPP is the number of vaccine doses—in a full course for a given vaccine—as a proportion of the country’s population (48). Data for this indicator were extracted on 25 February 2022. These two indicators were chosen due to the credibility of their sources (the World in Data website and the UNICEF COVID-19 Vaccine Market Dashboard). The two different COVID-19 vaccine distribution indicators (TVH and VPP) were used separately as indicators for vaccine distribution among countries. This was performed to ascertain the credibility of the results, regardless of the indicator used.
Apart from VPP and TVH, four other variables were used in this study. These four variables served as stratifiers in the CI analysis and as independent variables in the MLR analysis. The first variable is GDP/capita (49). The second variable is the World Power Index (WPI), which is a composite index. It is composed of three subindexes that reflect the multi-dimensionality of the concept of state power. The three subindexes are the material capacities index (MCI), semi-material capacities index (SMCI), and immaterial capacities index (IMCI) (50). The third variable is the Political stability and absence of violence/terrorism, is one of the six world governance indicators created by the World Bank. PS measures the likelihood of violence and terrorism that can lead to government destabilization or being overthrown (51). The fourth variable is the Universal Health Coverage (UHC) service coverage index (52). A detailed description of the data and its sources is provided in Supplementary material. The selection of these four variables for analysis in this study is grounded in the existing literature, where scholars have identified these factors as crucial determinants of disparities in the distribution of COVID-19 vaccines among countries (18, 19, 21, 22, 26–32, 34).
Originally, 217 countries were included in the study. However, each of the previously mentioned variables had missing data points. Thus, the analysis in this study is limited to countries that had data for each variable, resulting in a final number of 163 countries being included. Given that complete data for all variables necessitated a reduction in sample size from 217 to 163 nations, the possible implications for the study’s findings and generalizability should be carefully considered. The refined sample adds a trade-off in terms of external validity, but it guarantees a more uniform dataset about the variables being studied.
3 Results
The analysis for TVH and VPP revealed significant disparities in COVID-19 vaccine distribution among countries. The CI analyses demonstrated inequalities in both TVH and VPP based on the four indicators. The MLR proved the presence of a significant relationship between COVID-19 vaccine distribution and PS, WPI, and UHC, but not GDP/capita. The breakdown of the results is detailed below.
3.1 TVH
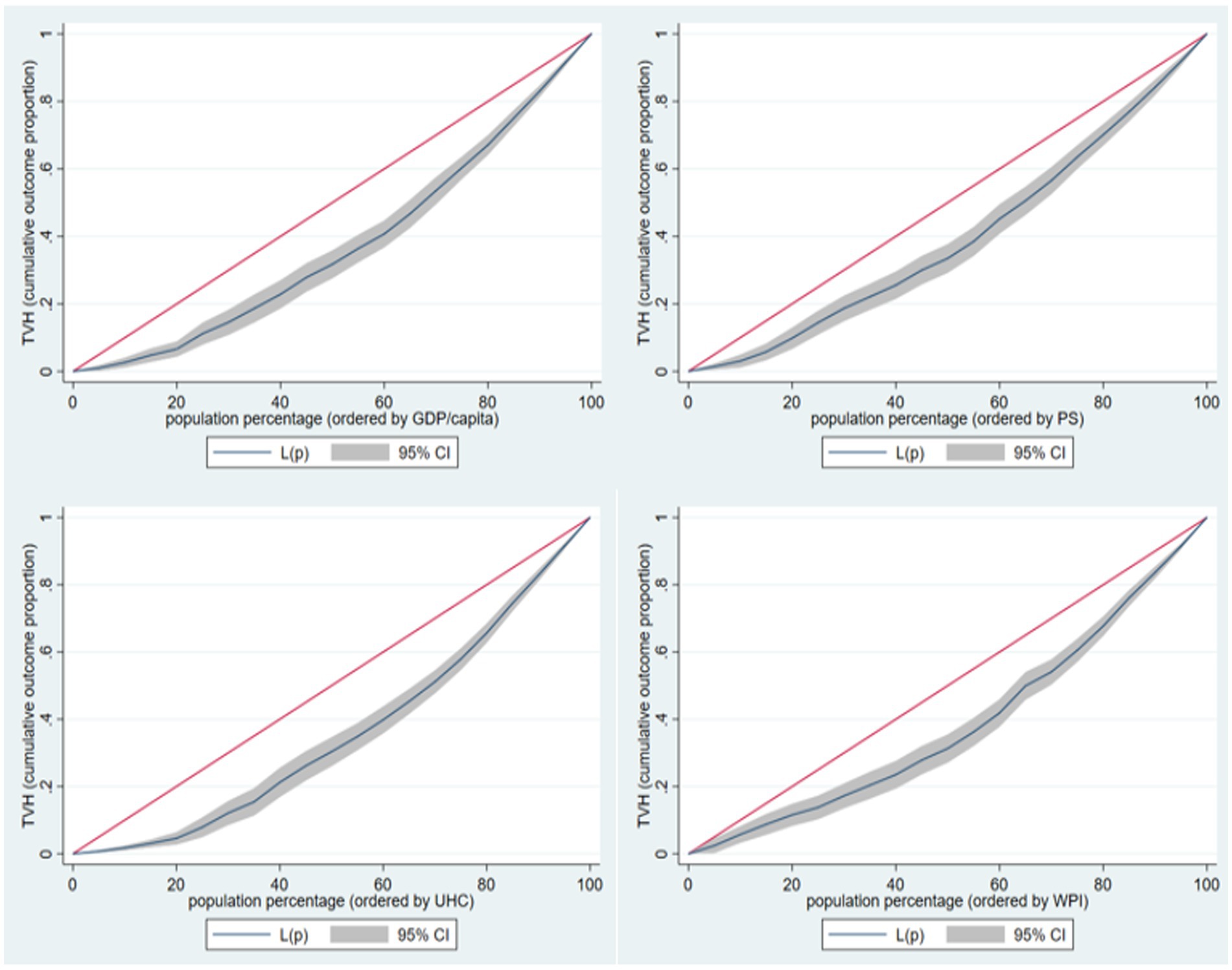
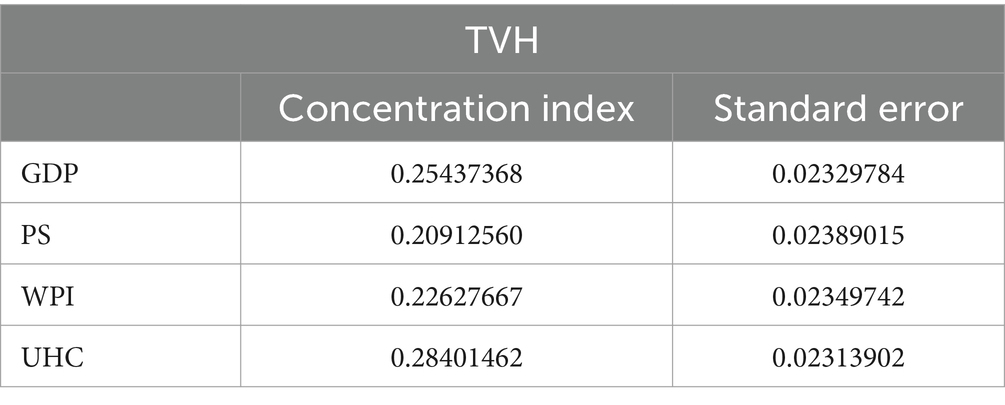
The CI analysis for TVH against the four indicators used as stratifiers (Figure 2) indicates the presence of inequality in TVH according to these countries’ GDP/capita, PS, WPI, and UHC.
The CI values for GDP/capita PS, WPI, and UHC range between 0.209 and 0.284, with the UHC having the higher CI value and PS having the lowest CI value (Table 1).
The MLR model for TVH against GDP/capita, PS, WPI, and UHC turned out to be statistically significant, with an F-value of 69.33 and a p-value of less than 0.001. The model explained 68% of the variability in TVH. Among the four variables: GDP/Capita was statistically insignificant, while PS, WPI, and UHC were statistically significant, indicating that these three are the ones related to TVH and can be used to explain the variation in its values (Table 2).
3.2 VPP
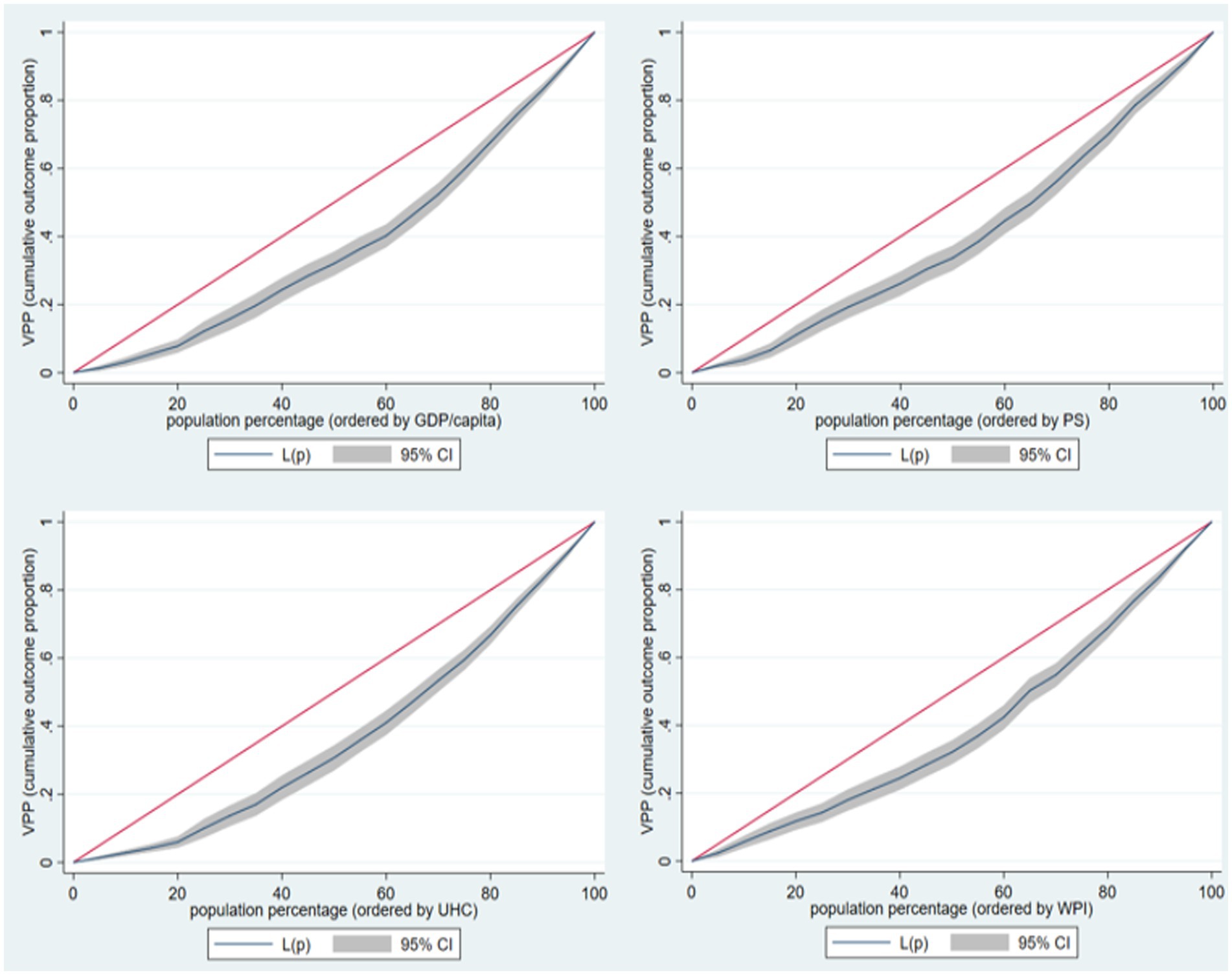
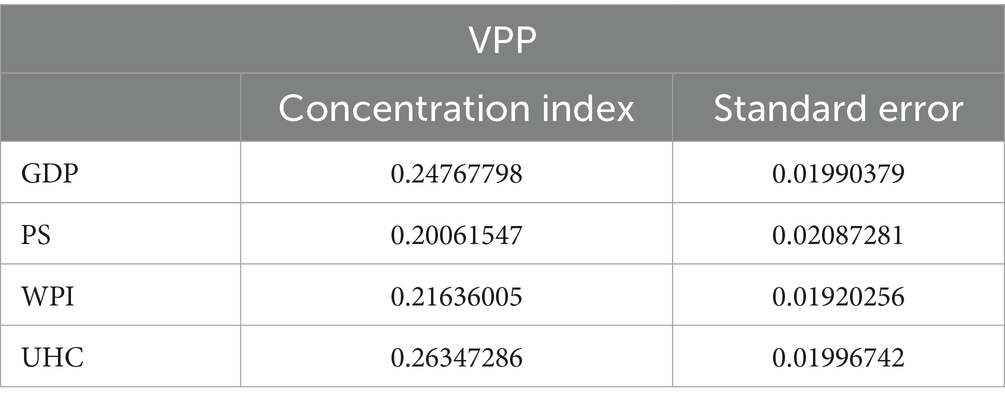
Similarly, to TVH, the CI analysis results for VPP against the four indicators used as stratifiers (Figure 3) indicate the presence of inequality in VPP according to these countries’ GDP/capita, PS, WPI, and UHC.
The CI values for PS, WPI, GDP/capita, and UHC range between 0.201 and 0.263, with the UHC having the higher CI value and PS having the lowest CI value (Table 3).
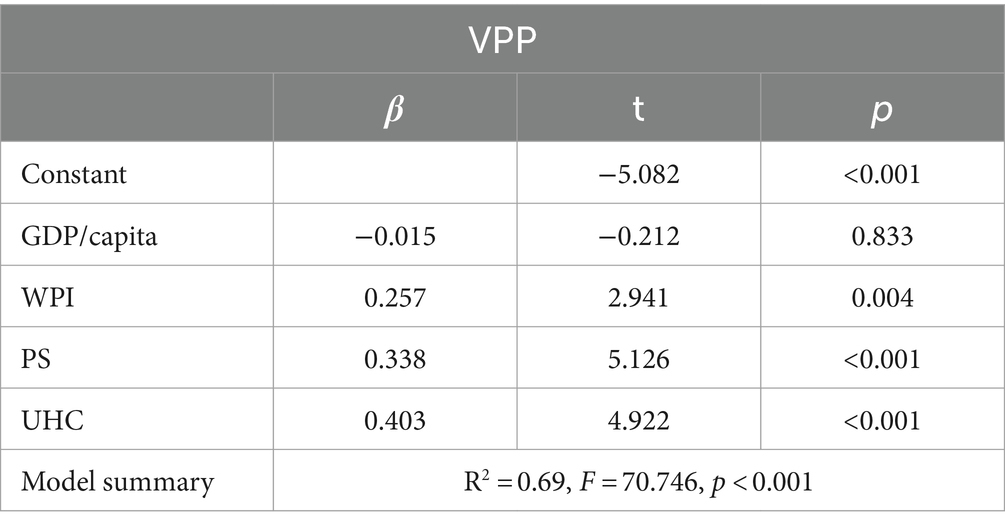
The MLR model for VPP against GDP/capita PS, WPI, and UHC turned out to be statistically significant, with an F-value of 70.746 and a p-value of less than 0.001. The model explained 69% of the variability in VPP. Among the four variables: GDP/Capita was statistically insignificant, while PS, WPI, and UHC were statistically significant, indicating that these three are the ones related to VPP and can be used to explain the variation in its values (Table 4).
4 Discussion
The literature on the COVID-19 vaccine and its distribution among different countries has strongly highlighted the unequal access to the vaccine. Some relate this inequity to factors that pertain to the country itself, namely its human and technological capacities, while others discuss external factors such as power imbalances in the global health arena, global solidarity, and health security. Almost all of these studies are of qualitative nature or descriptive at the very least. To the best of our knowledge, there is limited or no existing research that specifically utilizes the combination of our chosen methods, namely CI analysis and MLR, in the context of global-level COVID-19 distribution analysis. This research measures the inequality in COVID-19 vaccine distribution according to countries’ economic status, political power, PS, and health system strength, followed by investigating the relation between the intercountry COVID-19 vaccine distribution and the four variables (i.e., economic status, political stability, political power, and health system strength) with the aim of determining which of these factors is most important to address in order to enhance the accessibility to vaccines in future pandemics, which will indirectly lead to better equality in distribution.
The CI analysis results for both VPP and TVH proved the presence of inequity in the distribution of COVID-19 vaccines among countries according to the countries’ GDP/capita, PS, WPI, and UHC. The sign and the magnitude of the concentration indices for both indicators indicate that countries with high GDP/capita, PS, WPI, and UHC had higher accessibility to vaccines. This finding is concerning since it implies that countries with lower GDP/capita, PS, WPI, and UHC are facing greater challenges in accessing and administering COVID-19 vaccines, which exacerbate global health inequities and prolong the pandemic by allowing the COVID-19 virus to circulate in countries with lower vaccination rates, leading to potential outbreaks and the emergence of new variants. GHG policies ought to pay significant attention to countries with lower GDP/capita, PS, WPI, and UHC. GHG ought to secure and satisfy the need of these less fortunate countries for vaccines through international collaborations. Efforts should focus on bridging the gap between high- and low-income countries by facilitating vaccine access, increasing production capacities, and providing financial and technical support to countries in need in order to achieve global health equity and global health security.
Although the CI analysis indicated the presence of inequality in COVID-19 vaccine distribution according to their GDP/capita, PS, WPI, and UHC, unexpectedly, the regression analysis showed that there is no significant relationship between COVID-19 vaccine distribution and the countries’ GDP/capita. This interesting result means that although economic-based inequalities are present, the economic status of countries is not a main factor in affecting COVID-19 vaccine distribution but other factors. GDP/capita can enable the country to purchase the vaccine; however, it is not the determinant of COVID-19 vaccine distribution among and within countries. Other external and internal factors are involved. The regression analysis proved that both TVH and VPP are significantly related to the three other factors: WPI, PS, and UHC.
UHC had the highest significant positive coefficient, suggesting that in countries with higher levels of UHC, the quantity of COVID-19 vaccine doses delivered was higher. UHC is an indicator used as a proxy for the strength of the health system in a country. A country providing a decent level of UHC needs to have a relatively strong health system that can provide services and cover the population. A strong health system would facilitate the management of the COVID-19 vaccines, from procurement to distribution and finally administration. A strong health system means having the financial and human resources to accomplish adequate COVID-19 vaccine coverage for their population. This justifies the strong relationship between UHC and both TVH and VPP.
The second most significant predictor variable is the PS in a country. PS reflects the country’s context in terms of its ability to prioritize COVID-19 as a primary concern, its ability to import or manufacture vaccines, raise people’s awareness enough to accept vaccines, and the ability of the health system to function efficiently to administer vaccines. These governments or responsible parties do not have the required financial resources to acquire vaccines, and health may not be their top priority due to the political and sovereignty issues they need to concentrate on. COVID-19 has exacerbated the existing health inequities in these countries as well as added new ones, such as the inequity in accessibility to the COVID-19 vaccine. The inequity in the intercountry distribution of COVID-19 vaccines is not solely determined by socioeconomic factors within these countries. It extends to the global level, where entire nations are discriminated against by the global community in terms of vaccine allocation, particularly in the absence of strong global solidarity.
The third predictor variable related to COVID-19 vaccine distribution is WPI. The power of a state can stem from several attributes: economy, politics, military, culture, technology, etc. These attributes enable the state to make decisions and execute measures that it deems necessary to preserve its sovereignty. The COVID-19 pandemic threatens states at multiple levels: population health, economy, PS, and even their sovereignty. In the presence of a power imbalance among states and the absence of a GHG structure with the power to lead all states to a unified response against the pandemic, these powerful states prioritized their populations and interests regardless of the consequences of their decisions on other nations. Powerful states were capable of securing COVID-19 vaccines for their populations. Some of these powerful states secured more than double their needs, while weak nations struggled to secure the minimum amount of vaccine to cover the most vulnerable segment of their populations.
Acting on the above-mentioned factors (UHC, PS, and WPI) can enhance accessibility to the COVID-19 vaccine in countries and ultimately enhance equity in COVID-19 vaccine distribution. According to the results of the MLR, UHC has the highest coefficient meaning that working on enhancing countries’ UHC achievement will have the highest return on improving the accessibility of vaccines in future pandemics. UHC is based on the notion of equity. The aim of UHC is to ensure everyone’s accessibility to essential health services, including vaccines, without facing financial hardship. UHC requires strong health systems with enhanced capacity to store, distribute, and administer vaccines effectively, as well as ensure that vulnerable populations and marginalized communities have equal access to COVID-19 vaccines. Strengthening health systems and progressing in the attainment of UHC should be a priority on local as well as global health agendas to enhance vaccine accessibility and equity.
Regarding PS, PS creates an environment conducive to long-term planning and investment in healthcare infrastructure. Governments can allocate resources to strengthen healthcare systems, including vaccination facilities, cold chain storage, transportation networks, and healthcare workforce training. A stable political environment encourages sustained investments in these critical areas, ensuring efficient vaccine distribution and accessibility. Moreover, PS ensures effective policy implementation and attracts international aid.
Finally, countries’ economic and social powers. During the COVID-19 pandemic, countries’ powers were exploited in ways that favored nationalistic gains instead of global gains. Equity and solidarity, and hence accessibility to COVID-19 vaccines, were not top priorities for countries. Nevertheless, countries’ power can be leveraged to increase accessibility to vaccines. Political power can be directed to influence global health policies, such as policies to reduce trade barriers and intellectual property restrictions that might hinder the production and distribution of vaccines. Economic power can be directed to finance vaccines, support their manufacturing, and increase production and supply. Finally, countries with knowledge power need to collaborate with other nations and share their scientific knowledge and expertise to accelerate vaccine development.
The findings of this study can have significant implications for both the global response to the COVID-19 pandemic and the existing literature on vaccine distribution disparities. The disparities in access to COVID-19 vaccines that have been identified and their underlying causes highlight the interconnected nature of global power structures, healthcare systems, and political dynamics. This addition will enhance the current discussion on vaccines and global health equity.
4.1 Study limitations
Although the study offers insightful information regarding COVID-19 vaccine distribution inequality among countries and the factors associated with this distribution, it has its limitations. The analysis focused on COVID-19 vaccine distribution inequality among countries based on specific factors such as economic status, PS, political power, and health system strength. While these factors are important, they are not the only ones affecting COVID-19 vaccine distribution. Nevertheless, these factors are supported by the literature and other peer-reviewed studies.
Another limitation is that the study used COVID-19 vaccine distribution data from a specific point in time (at the beginning of the vaccine distribution), which entails that the results of the study are valid for this period and might have changed in the period that came after. This does not reduce the importance of the results, as they demonstrate that in the period when vaccines were not produced in enough quantities, equality in distribution was ignored.
5 Conclusion
Inequalities according to countries’ GDP/capita, PS, WPI, and UHC are present. However, it appears that COVID-19 vaccine distribution is significantly related to PS, WPI, and UHC and not to GDP/capita. To improve the accessibility of vaccines in future pandemics, GHG and countries should consider working on three areas: enhancing PS in countries, separating political power from decision-making at the global level, and most importantly, supporting countries to achieve UHC. Regarding future research, more in-depth research is needed to identify the specific mechanisms through which PS, world power dynamics, and health coverage impact vaccine accessibility.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
WA: Methodology, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. ZK: Formal analysis, Methodology, Writing – review & editing, Conceptualization, Validation. HE: Conceptualization, Validation, Supervision, Writing – review & editing. SC: Conceptualization, Supervision, Validation, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1348088/full#supplementary-material
References
2. Baena-Díez, JM, Barroso, M, Cordeiro-Coelho, SI, Díaz, JL, and Grau, M. Impact of COVID-19 outbreak by income: hitting hardest the most deprived. J Public Health. (2020) 42:698–703. doi: 10.1093/pubmed/fdaa136
3. Elgar, FJ, Stefaniak, A, and Wohl, MJ. The trouble with trust: time-series analysis of social capital, income inequality, and COVID-19 deaths in 84 countries. Soc Sci Med. (2020) 263:113365. doi: 10.1016/j.socscimed.2020.113365
4. Winskill, P, Whittaker, C, Walker, PG, Watson, O, and Laydon, D. Report 22: Equity in response to the COVID-19 pandemic: An assessment of the direct and indirect impacts on disadvantaged and vulnerable populations in low-and lower middle-income countries. Imperial College London; (2020).
5. Williamson, E, Walker, AJ, Bhaskaran, K, Bacon, S, Bates, C, Morton, CE, et al. Open SAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. medRxiv [Preprint]. (2020).
6. Public Health England. Disparities in the risk and outcomes of COVID-19. PHE publications: Public Health England (2020).
7. Tadiri, CP, Gisinger, T, Kautzy-Willer, A, Kublickiene, K, Herrero, MT, Raparelli, V, et al. The influence of sex and gender domains on COVID-19 cases and mortality. CMAJ. (2020) 192:E1041–5. doi: 10.1503/cmaj.200971
8. Power, K. The COVID-19 pandemic has increased the care burden of women and families. Sustain Sci Pract Policy. (2020) 16:67–73. doi: 10.1080/15487733.2020.1776561
9. Johnson, K, Green, L, Volpellier, M, Kidenda, S, McHale, T, Naimer, K, et al. The impact of COVID-19 on services for people affected by sexual and gender-based violence. Int J Gynecol Obstet. (2020) 150:285–7. doi: 10.1002/ijgo.13285
10. Bettinger-Lopez, C, and Bro, A. A double pandemic: domestic violence in the age of COVID-19. Counc Foreign Relat. (2020) 13.
11. Landivar, LC, Ruppanner, L, Scarborough, WJ, and Collins, C. Early signs indicate that COVID-19 is exacerbating gender inequality in the labor force. Socius. (2020) 6:237802312094799. doi: 10.1177/2378023120947997
12. Khunti, K, Singh, AK, Pareek, M, and Hanif, W. Is ethnicity linked to incidence or outcomes of covid-19? BMJ. (2020) 369:m1548. doi: 10.1136/bmj.m1548
13. Williams, DR, and Cooper, LA. COVID-19 and health equity—a new kind of “herd immunity”. JAMA. (2020) 323:2478–80. doi: 10.1001/jama.2020.8051
14. Burström, B, and Tao, W. Social determinants of health and inequalities in COVID-19. Eur J Pub Health. (2020) 30:617–8. doi: 10.1093/eurpub/ckaa095
15. Jones, L, and Hameiri, S. Explaining the failure of global health governance during COVID-19. Int Aff. (2022) 98:2057–76. doi: 10.1093/ia/iiac231
16. Abu El Kheir-Mataria, W, El-Fawal, H, and Chun, S. Global health governance performance during Covid-19, what needs to be changed? A delphi survey study. Glob Health. (2023) 19:1–13. doi: 10.1186/s12992-023-00921-0
17. Ritchie, H, Mathieu, E, Rodés-Guirao, L, Appel, C, Giattino, C, Ortiz-Ospina, E, et al. Our world in data. Coronavirus pandemic (COVID-19). (2020). Available at: https://ourworldindata.org/covid-vaccinations (Accessed 7 April 2022).
18. Sell, SK. What COVID-19 reveals about twenty-first century capitalism: adversity and opportunity. Development. (2020) 63:150–6. doi: 10.1057/s41301-020-00263-z
19. Zhou, YR. Vaccine nationalism: contested relationships between COVID-19 and globalization. Globalizations. (2022) 19:450–65. doi: 10.1080/14747731.2021.1963202
20. Launch & Scale Speedometer. Tracking Covid-19 vaccine purchases across the globe. (2022). Available at: https://public.tableau.com/views/Purchasesanddealsnew/Story1?:embed=y&:showVizHome=no&:host_url=https%3A%2F%2Fpublic.tableau.com%2F&:embed_code_version=3&:tabs=no&:toolbar=yes&:animate_transition=yes&:display_static_image=no&:display_spinner=no&:display_overlay=yes&:display_count=yes&:language=en&publish=yes&:loadOrderID=0 (Accessed 12 April 2022).
21. Rutschman, AS. Is there a cure for vaccine nationalism? Curr Hist. (2021) 120:9–14. doi: 10.1525/curh.2021.120.822.9
22. Fidler, DP. The Covid-19 pandemic, geopolitics, and international law. J Int Humanit Leg Stud. (2020) 11:237–48. doi: 10.1163/18781527-bja10010
24. Suzuki, M, and Yang, S. Political economy of vaccine diplomacy: explaining varying strategies of China, India, and Russia’s COVID-19 vaccine diplomacy. Rev Int Polit Econ. (2022) 30:865–90. doi: 10.1080/09692290.2022.2074514
25. Fidler, DP. Vaccine nationalism’s politics. Science. (2020) 369:749–9. doi: 10.1126/science.abe2275
26. Bollyky, TJ, Murray, CJL, and Reiner, RC. Epidemiology, not geopolitics, should guide COVID-19 vaccine donations. Lancet. (2021) 398:97–9. doi: 10.1016/S0140-6736(21)01323-4
27. Limaye, RJ, Sauer, M, and Truelove, SA. Politicizing public health: the powder keg of rushing COVID-19 vaccines. Hum Vaccin Immunother. (2021) 17:1662–3. doi: 10.1080/21645515.2020.1846400
28. Lee, ST. Vaccine diplomacy: nation branding and China’s COVID-19 soft power play. Place Brand Public Dipl. (2021) 19:64–78. doi: 10.1057/s41254-021-00224-4
29. Tevdovski, D, Jolakoski, P, and Stojkoski, V. The impact of state capacity on the cross-country variations in COVID-19 vaccination rates. Int J Health Econ Manag. (2022) 22:237–55. doi: 10.1007/s10754-021-09319-0
30. Eccleston-Turner, M, and Upton, H. International collaboration to ensure equitable access to vaccines for COVID-19: the ACT-accelerator and the COVAX facility. Milbank Q. (2021) 99:426–49. doi: 10.1111/1468-0009.12503
31. Wouters, OJ, Shadlen, KC, Salcher-Konrad, M, Pollard, AJ, Larson, HJ, Teerawattananon, Y, et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. (2021) 397:1023–34. doi: 10.1016/S0140-6736(21)00306-8
32. Price, WN, Rai, AK, and Minssen, T. Knowledge transfer for large-scale vaccine manufacturing. Science. (2020) 369:912–4. doi: 10.1126/science.abc9588
33. Diseases, TLI. COVID-19 vaccine equity and booster doses. Lancet Infect Dis. (2021) 21:1193. doi: 10.1016/S1473-3099(21)00486-2
34. Peacocke, EF, Heupink, LF, Frønsdal, K, Dahl, EH, and Chola, L. Global access to COVID-19 vaccines: a scoping review of factors that may influence equitable access for low and middle-income countries. BMJ Open. (2021) 11:e049505. doi: 10.1136/bmjopen-2021-049505
35. Regidor, E. Measures of health inequalities: part 1. J Epidemiol Community Health. (2004) 58:858–61. doi: 10.1136/jech.2003.015347
36. Schneider, MC, Castillo-Salgado, C, Bacallao, J, Loyola, E, Mujica, OJ, Vidaurre, M, et al. Methods for measuring inequalities in health. Rev Panam Salud Publica Pan Am J Public Health. (2002) 12:398–414. doi: 10.1590/S1020-49892002001200006
37. Wagstaff, A, Paci, P, and Van Doorslaer, E. On the measurement of inequalities in health. Soc Sci Med. (1991) 33:545–57. doi: 10.1016/0277-9536(91)90212-U
38. Wagstaff, A, and Van Doorslaer, E. Measuring and testing for inequity in the delivery of health care. J Hum Resour. (2000) 35:716. doi: 10.2307/146369
39. Le Grand, J. Inequalities in health: some international comparisons. Eur Econ Rev. (1987) 31:182–91. doi: 10.1016/0014-2921(87)90030-4
40. Illsley, R, and Grand, JL. The measurement of inequality in health In: Health and Economics: Proceedings of Section F (Economics) of the British Association for the Advancement of Science, Bristol. London: Palgrave Macmillan UK (1986). 12–36.
41. Jutz, R. The role of income inequality and social policies on income-related health inequalities in Europe. Int J Equity Health. (2015) 14:117. doi: 10.1186/s12939-015-0247-y
42. Townsend, P, and Davidson, N. Inequalities in health: The black report penguin. Harmondsworth: United Kingdom Department of Health and Social Security (1982).
43. Khadr, Z. Monitoring socioeconomic inequity in maternal health indicators in Egypt: 1995-2005. Int J Equity Health. (2009) 8:38. doi: 10.1186/1475-9276-8-38
44. Eberly, LE. Multiple linear regression. Methods Mol Biol. (2007) 404:165–87. doi: 10.1007/978-1-59745-530-5_9
45. Johnson, RA, and Wichern, DW. Applied multivariate statistical analysis. (2002). Available at: https://www.worldpowerindex.com/wpi-database/ (Accessed 10 January 2024).
46. Montgomery, DC, Peck, EA, and Vining, GG. Introduction to linear regression analysis. John Wiley & Sons (2021).
47. Neter, J, Kutner, MH, and Nachtsheim, CJ, Wasserman W. Applied linear statistical models. (1996) Available at: https://mubert.marshall.edu/bert/syllabi/310720160114404301635160.pdf (Accessed 11 January 2024).
48. UNICEF. UNICEF supply division. COVID-19 Vaccine Market Dashboard. (2021) Available at: https://www.unicef.org/supply/covid-19-vaccine-market-dashboard (Accessed 6 June 2022).
49. World Bank. Available at: https://databank.worldbank.org/metadataglossary/sustainable-development-goals-%28sdgs%29/series/NY.GDP.PCAP.KD (n.d.) (Accessed 6 June 2022).
50. Morales Ruvalcaba, D. World Power index. DatabaseWPI. (2023) Available at: https://www.worldpowerindex.com/data-wpi/ (Accessed 6 June 2022).
51. WorldBank. WorldBank governance indicators. WGI 2021 interactive data access. (2021) Available at: http://info.worldbank.org/governance/wgi/Home/Reports (Accessed 6 June 2022).
Keywords: COVID-19, vaccine distribution, equity, global health governance, concentration index, universal health coverage, health system strength, political power and economic power
Citation: Abu El Kheir-Mataria W, Khadr Z, El Fawal H and Chun S (2024) COVID-19 vaccine intercountry distribution inequality and its underlying factors: a combined concentration index analysis and multiple linear regression analysis. Front. Public Health. 12:1348088. doi: 10.3389/fpubh.2024.1348088
Edited by:
Maria Rosario O. Martins, New University of Lisbon, PortugalReviewed by:
Ana María Díaz Riofrío, University of the Americas, EcuadorLuzia Goncalves, New University of Lisbon, Portugal
Copyright © 2024 Abu El Kheir-Mataria, Khadr, El Fawal and Chun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sungsoo Chun, c3VuZ3Nvby5jaHVuQGF1Y2VneXB0LmVkdQ==
 Wafa Abu El Kheir-Mataria
Wafa Abu El Kheir-Mataria Zeinab Khadr2,3
Zeinab Khadr2,3 Hassan El Fawal
Hassan El Fawal Sungsoo Chun
Sungsoo Chun