
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Public Health , 27 February 2024
Sec. Life-Course Epidemiology and Social Inequalities in Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1346293
This article is part of the Research Topic Examining Upstream to Understand Downstream: Use of Telehealth and Other Health Equity Measures for Addressing Health Disparities View all 8 articles
Background: The objective of this study was to examine differences in availability and use of telehealth services among Medicare enrollees according to Alzheimer’s disease and related dementias (ADRD) status and enrollment in Medicare Advantage (MA) versus Traditional Medicare (TM) during the period surrounding the COVID-19 pandemic.
Methods: This was a retrospective cross-sectional analysis of data from community-dwelling MA and TM enrollees with and without ADRD from the Medicare Current Beneficiary Survey (MCBS) Fall 2020 and Winter 2021 COVID-19 Supplement Public Use Files. We examined self-reported availability of telehealth service before and during the COVID-19 pandemic and use of telehealth services during COVID-19. We analyzed marginal effects under multivariable logistic regression.
Results: There were 13,700 beneficiaries with full-year enrollment in MA (6,046) or TM (7,724), 518 with ADRD and 13,252 without ADRD. Telehealth availability during COVID-19 was positively associated with having a higher income (2.81 pp. [percentage points]; 95% CI: 0.57, 5.06), having internet access (7.81 pp.; 95% CI: 4.96, 10.66), and owning telehealth-related technology (3.86; 95% CI: 1.36, 6.37); it was negatively associated with being of Black Non-Hispanic ethnicity (−8.51 pp.; 95% CI: −12.31, −4.71) and living in a non-metro area (−8.94 pp.; 95% CI: −13.29, −4.59). Telehealth availability before COVID-19 was positively associated with being of Black Non-Hispanic ethnicity (9.34 pp.; 95% CI: 3.74, 14.94) and with enrollment in MA (4.72 pp.; 95% CI: 1.63, 7.82); it was negatively associated having dual-eligibility (−5.59 pp.; 95% CI: −9.91, −1.26). Telehealth use was positively associated with being of Black Non-Hispanic ethnicity (6.47 pp.; 95% CI: 2.92, 10.01); it was negatively associated with falling into the age group of 75+ years (−4.98 pp.; 95% CI: −7.27, −2.69) and with being female (−4.98 pp.; 95% CI: −7.27, −2.69).
Conclusion: Telehealth services were available to and used by Medicare enrollees with ADRD to a similar extent compared to their non-ADRD counterparts. Telehealth services were available to MA enrollees to a greater extent before COVID-19 but not during COVID-19, and this group did not use telehealth services more than TM enrollees during COVID-19.
Alzheimer’s disease and related dementias (ADRD) are brain diseases that result from progressive neuron damage; they affect cognitive function, language skills, and memory, with no currently known cure (1). The number of adults with ADRD in the United States is expected to increase from 6.7 million in 2023 to 13.8 million by 2060 (1). Patients with ADRD use health services at a high rate, with an average of 6.82 to 10.18 physician office visits per year (2). When the COVID-19 pandemic arrived in the United States in 2020, patients with ADRD faced greater disruptions in their routine healthcare than their non-ADRD counterparts (3).
Telehealth became a major form of healthcare provision during the COVID-19 pandemic due to the risk of contracting COVID-19 if meeting in person, with the CDC reporting a 154% increase in telehealth use in the last week of March 2020 compared to the same week in 2019 (4). While telehealth use increased for the general population during the COVID-19 pandemic, there may be barriers to telehealth access and use among vulnerable populations, such as older adults living at home and those with ADRD (5).
Medicare is the health insurance program that is provided to adults above the age of 65 years or those with debilitating disabilities in the United States. Medicare enrollees have two options to choose from: a fee-for-service option, also known as Traditional Medicare (TM), or a managed care option known as Medicare Advantage (MA). MA may be more efficient in containing health expenditure and covering additional services such as internet access (6–9). The Creating High-Quality Results and Outcomes Necessary to Improve Chronic (CHRONIC) Care Act of 2017 provided a provision for MA plans to cover social determinants of health, such as internet costs, starting in 2020, which coincidentally aligned with the beginning of the COVID-19 pandemic in the US (10, 11).
Before the COVID-19 pandemic, TM covered telehealth only for rural areas, and patients could not use telehealth at home but rather had to go to an approved facility to receive telehealth services, while MA plans had more flexibility to offer telehealth coverage without restrictions (12). On 6 March 2020, the Centers for Medicare & Medicaid Services (CMS) released a 1,135 Waiver by authority of the Coronavirus Preparedness and Response Supplemental Appropriations Act, which expanded telehealth access for TM enrollees (13). Recent research has found that, during the COVID-19 pandemic, TM and MA enrollees had similar rates of telehealth use (44 and 45%, respectively) (12).
A previous study found no significant differences in care satisfaction or health status between TM and MA enrollees with ADRD in 2010–2016, despite MA enrollees using fewer health services (14). However, evidence comparing MA and TM enrollees with ADRD is limited, and no study has examined differences in telehealth access and use among patients with ADRD during the COVID-19 pandemic.
Guided by Penchansky and Thomas’s seminal work on the “five A’s” of access to care (availability, accessibility, accommodation, affordability, and acceptability) (15), this study examined the differences in the availability of telehealth services to Medicare enrollees before and during COVID-19 and their use of telehealth during COVID-19. We hypothesized that Medicare enrollees with ADRD would be found to use telehealth to a lesser extent than non-ADRD enrollees due to barriers to the usage of telehealth technology. We also hypothesized that MA enrollees with ADRD used telehealth services during the COVID-19 pandemic to a greater extent than TM enrollees due to the flexibility of MA plans in providing additional coverage of services such as internet access.
This study uses the Medicare Current Beneficiary Survey (MCBS) COVID-19 Supplements for Fall 2020 and Winter 2021 (16, 17). The MCBS is an annual nationally representative survey of community-dwelling Medicare beneficiaries who are above the age of 50 years, with information on demographics, health status, and care status. The survey is conducted three times per year (in winter, covering January, February, March, and April; summer, covering May, June, July, and August; and fall, covering September, October, November, and December). The MCBS produced a series of COVID-19 Supplements providing information regarding health status and healthcare access during the COVID-19 pandemic. Data for the first COVID-19 Supplement were collected in the summer of 2020; however, we did not use this dataset, as it does not contain certain variables of interest, such as telehealth use. Informed consent was obtained at the time of the survey enrollment and was not required for this secondary data analysis.
The sample for this study consisted of respondents with self-reported ADRD status, with full-year TM or MA enrollment, who knew whether their primary care provider (PCP) offered telehealth appointments. Across the combined MCBS COVID-19 Supplements for Fall 2020 and Winter 2021, data were collected from 13,770 full-year TM and MA enrollees, from a survey-weighted population of 75,141,661.
Three dependent variables were examined in this study, selected using Penchansky and Thomas’s access to care model: (15) telehealth availability before COVID-19, telehealth availability during COVID-19, and telehealth use during COVID-19. Telehealth availability before COVID-19 was defined based on whether the respondent’s PCP offered telehealth services before COVID-19. Telehealth availability during COVID-19 was defined based on whether the respondent’s PCP offered telehealth appointments at the time of the survey. Telehealth use was defined based on whether the respondent had received any telehealth visits since the previous survey wave, a period of approximately 3 months (since July 1, 2020 in the Fall 2020 survey and since November 1, 2020 in the Winter 2021 survey).
The independent variables of interest were the enrollee’s ADRD status and MA vs. TM enrollment; the interaction between ADRD status and MA enrollment was also a key effect of interest. ADRD status was defined according to whether the respondent self-reported ever having been diagnosed with ADRD. MA/TM enrollment status was determined according to whether the enrollee had either full-year MA or full-year TM enrollment; respondents with partial-year enrollment were excluded based on administrative data sources.
Other covariates were selected based on the Andersen Behavioral Model of Health Services Use (18), their availability in the MCBS data, and recent literature on telehealth use during the COVID-19 pandemic. The Andersen model examines enrollee characteristics that are classified as relating to predisposing factors (age, sex, race and ethnicity, metro area residence, region, survey wave time period, and COVID-19 preventive behaviors), enabling resources (insurance payer, dual-eligibility status, income, speaking a language other than English at home, internet access, and telehealth-related technology access), and need characteristics (ADRD status and comorbidities).
Respondents were categorized by age as 50–64, 65–74, or 75+ years old. Sex was given as male or female. Race and ethnicity were provided under the categories White Non-Hispanic, Black Non-Hispanic, Hispanic, and Other/Unknown. Income was dichotomized as <$25,000 or ≥ $25,000 per year. Respondents’ metro residence status was defined based on the core-based statistical area (CBSA) as living in a metro or non-metro area. Region was categorized as Northeast, Midwest, South, or West. Dual-eligibility status was determined according to whether the respondent was eligible for Medicaid benefits. Speaking a language other than English at home was defined according to whether the respondent person stated that a language other than English was spoken at home. Comorbidity status are defined according to whether the respondent had ever had a heart condition, hypertension/high blood pressure, stroke, high cholesterol, cancer, osteoporosis/broken hip, emphysema/asthma/COPD (chronic obstructive pulmonary disease), diabetes/high blood sugar, depression, or a weak immune system. Survey wave was defined as Fall 2020 or Winter 2021.
We also controlled for other covariates that may predict the use of telehealth services based on Penchansky and Thomas’s model, as they related to the availability, affordability, and acceptability of digital technology. Internet access was defined according to whether the respondent had access to the internet. Having previously used video or voice calls was defined according to whether the respondent had previously used video or voice calls (for any reason) (19, 20). Telehealth-related technology access was defined according to whether the respondent owned a computer, smartphone, or tablet.
The survey also presented a set of 15 preventive behaviors and respondents were asked whether they had engaged in these behaviors due to COVID-19 (washed hands, used sanitizer, avoided touching their face, coughed/sneezed into tissue and/or sleeve, wore a facemask, cleaned common areas, avoided contact with sick people, kept 6 feet distance, avoided large groups, sheltered in place, bought extra food, bought extra cleaning supplies, bought extra medicines, consulted with their medical provider, avoided other people). The median number of preventive behaviors engaged in was 12; we created a binary index in which ≥12 was categorized as an above-median number of preventive behaviors and < 12 as a below-median number of preventive behaviors. These variables are components of accessibility and acceptability according to Penchansky and Thomas’s model; previous research has found no differences between TM and MA enrollees in the amount of preventive behavior (21).
Logistic regression models with marginal effects were used in this study to model the outcomes while controlling for all the covariates. This was a cross-sectional analysis that used the complex survey design of the MCBS. To account for serial and inter-cluster correlation in the MCBS, balanced repeated replication (BRR) using Fay’s adjustment of 0.3 was used to estimate the variances for the standard errors. Person weights and replicate weights were pooled to account for the use of multiple waves of data. Chi-squared tests were used for categorical variables and are reported with a two-sided significance level of 0.05. All analyses were performed using Stata 15/MP and were approved by the University of Maryland Institutional Review Board.
Figure 1 shows the three outcome variables by ADRD status and TM/MA enrollment. MA enrollees were offered telehealth services at higher rates than TM enrollees before the COVID-19 pandemic (30.76% vs. 25.85%), with no significant differences between enrollees with ADRD and without ADRD. During the COVID-19 pandemic, the group with the smallest percentage of members offered telehealth services compared to all other enrollees was TM enrollees with ADRD (76.28%). A larger percentage of Medicare enrollees with ADRD used telehealth services during the COVID-19 pandemic than enrollees without ADRD (48.76% vs. 44.71%), with no significant differences between TM and MA enrollees.
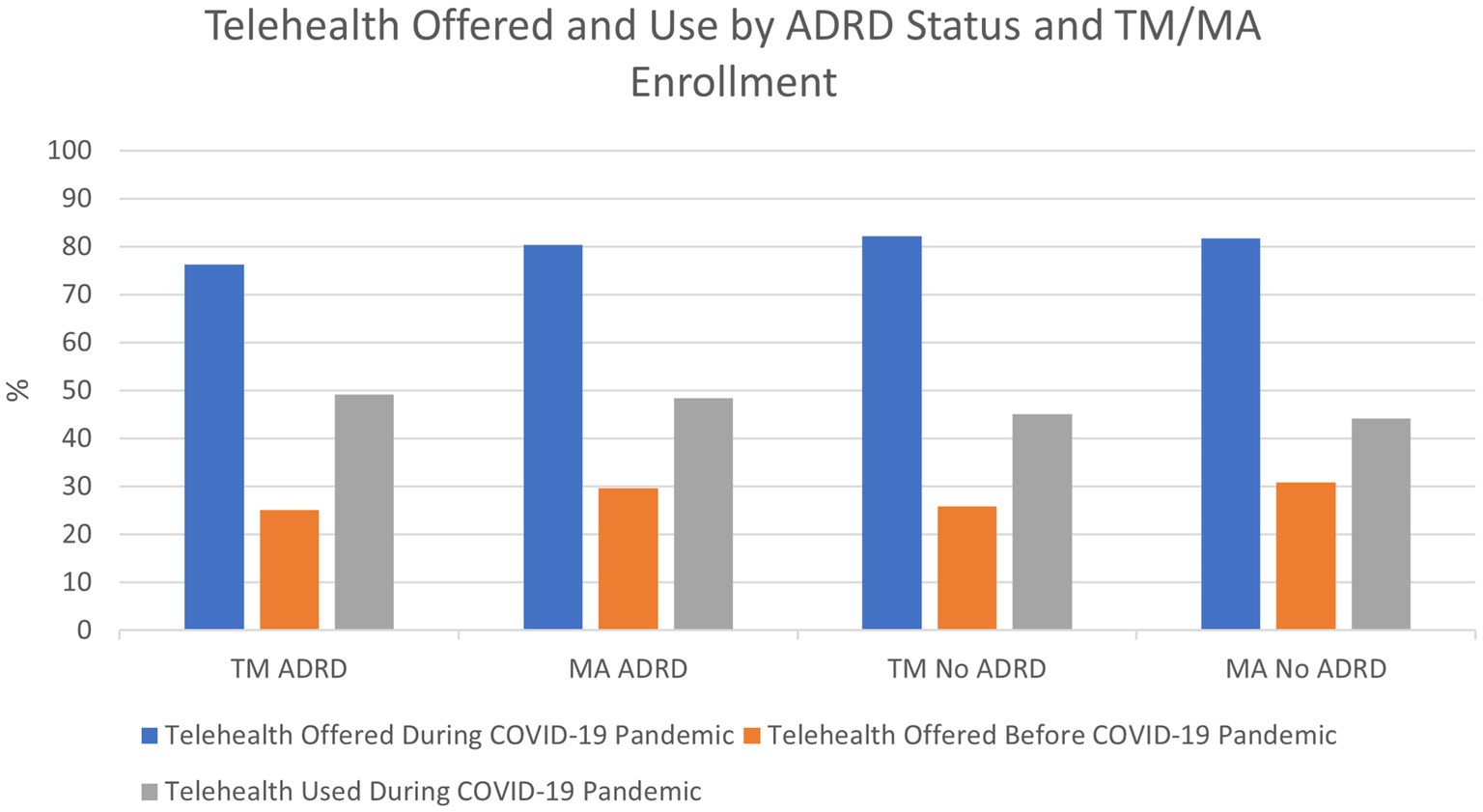
Figure 1. Source: 2020 Fall and 2021 Winter Medicare Current Beneficiary Survey COVID-19 Supplements. ADRD: Alzheimer’s Disease and Related Dementias, TM: Traditional Medicare, MA: Medicare Advantage.
Table 1 presents and compares the sample characteristics of Medicare enrollees with ADRD and those without ADRD. Enrollees with ADRD were more likely to be older (75+), to be non-White, to have an income below $25,000, to be enrolled in Medicare Advantage (46.40% vs. 39.44%), to be dual-eligible (26.30% vs. 13.84%), and to speak a language other than English at home; they were also less likely to access the internet (62.95% vs. 86.68%), to use video or voice calls (33.60% vs. 50.62%), to own telehealth-related technology (52.04% vs. 86.91%), or to engage in an above-median number of COVID-19 preventive behaviors. Enrollees with ADRD were also more likely to have ever had depression, a heart condition, hypertension, diabetes, osteoporosis/broken hip, asthma/COPD, or stroke.
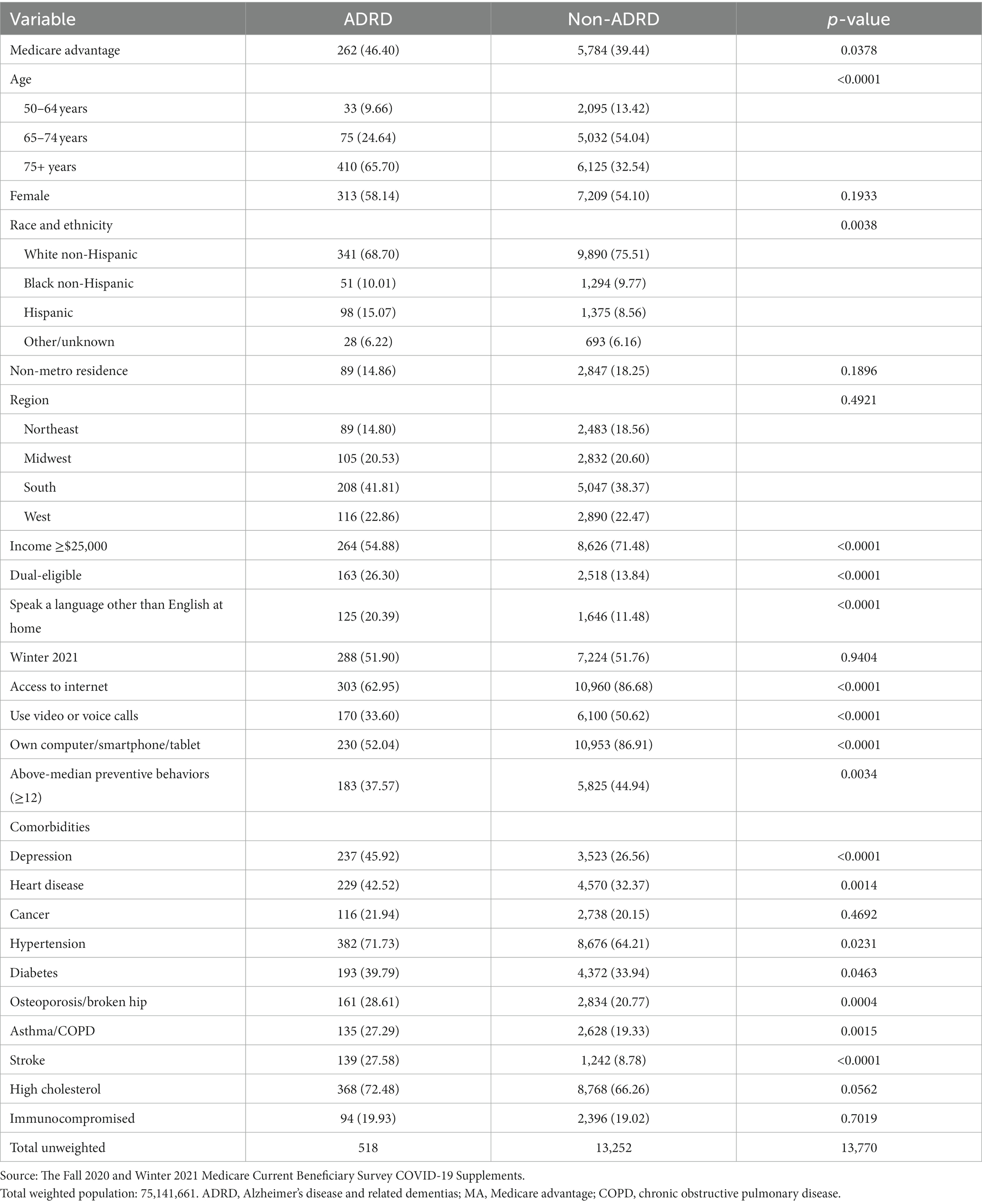
Table 1. Sample characteristics: Medicare enrollees by Alzheimer’s disease and related dementias status.
Table 2 presents and compares the sample characteristics by MA vs. TM enrollment status. MA enrollees were more likely to have ADRD (3.16% vs. 2.40%), to be more than 75 years old, to be non-White, to have an income below $25,000, to live in a metro area, to be dual-eligible (18.66% vs. 11.23%), to speak a language other than English at home, and to be represented in the Winter 2021 survey; they were also less likely to access the internet (82.80% vs. 88.17%), to use video or voice calls, or to own telehealth-related technology (82.93% vs. 87.95%). MA enrollees were more likely to have hypertension, diabetes, or high cholesterol, but less likely to have a weak immune system.
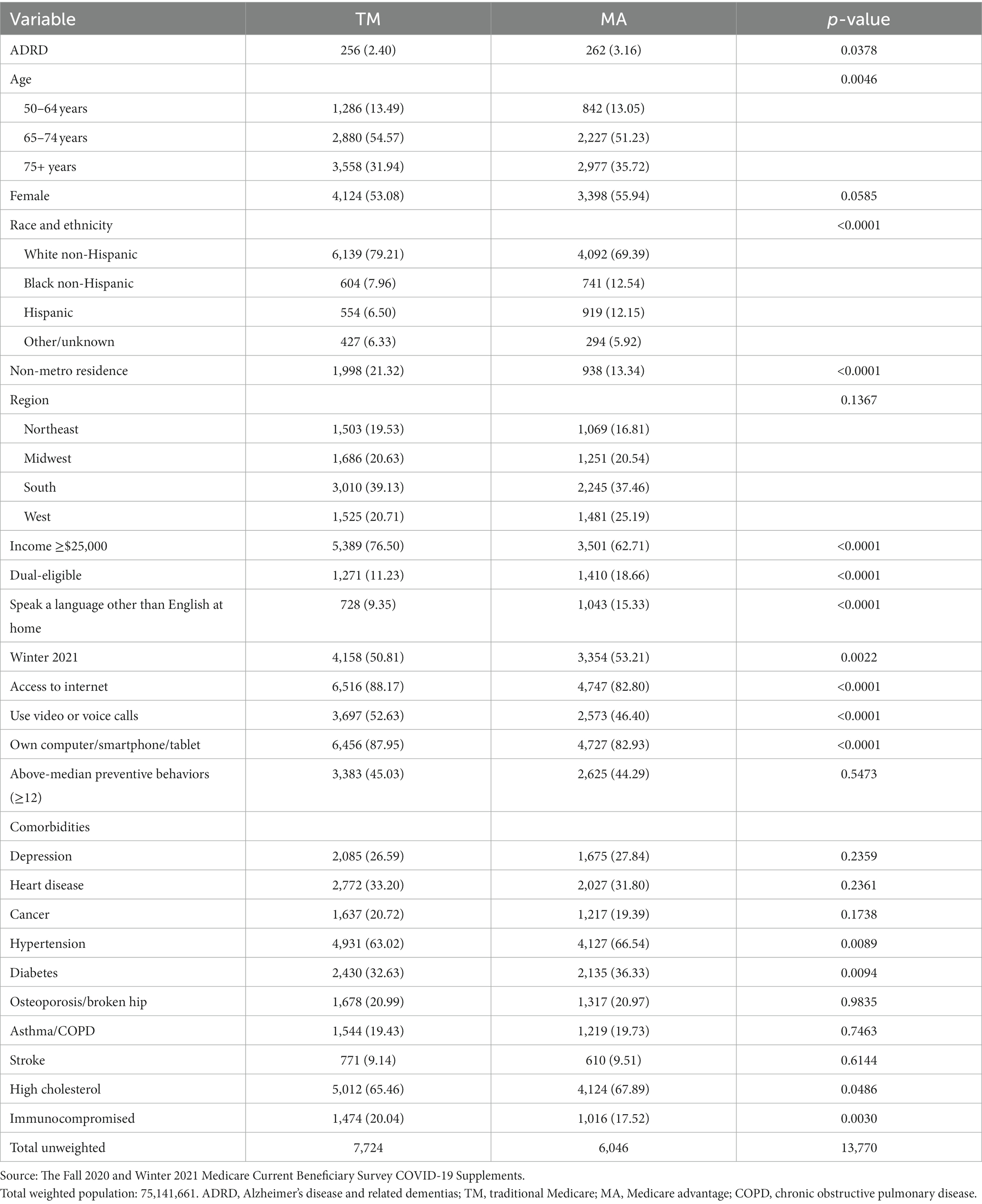
Table 2. Sample characteristics by full-year enrollment in traditional Medicare vs. Medicare advantage.
Table 3 shows the regression for telehealth availability during and before the COVID-19 pandemic and telehealth use during the COVID-19 pandemic. The availability of telehealth services during the COVID-19 pandemic was positively associated with having an income ≥$25,000 (2.81 pp. [percentage points]; 95% CI: 0.57, 5.06), having internet access (7.81 pp.; 95% CI: 4.96, 10.66), using video or voice calls (6.28 pp.; 95% CI: 4.56, 8.00), owning a computer/smartphone/tablet (3.86 pp.; 95% CI: 1.36, 6.37), engaging in an above-median number of preventive behaviors (3.46 pp.; 95% CI: 1.77, 5.15), and being immunocompromised (2.53 pp.; 95% CI: 0.21, 4.84); it was negatively associated with being of Black Non-Hispanic ethnicity (−8.51 pp., 95% CI: −12.31, −4.71), being of “other” race and ethnicity (−5.35 pp.; 95% CI: −9.63, −1.07), living in a non-metro area (−8.94 pp.; 95% CI: −13.29, −4.59), and participating in the Winter 2021 survey (−2.77 pp.; 95% CI: −4.37, −1.16).
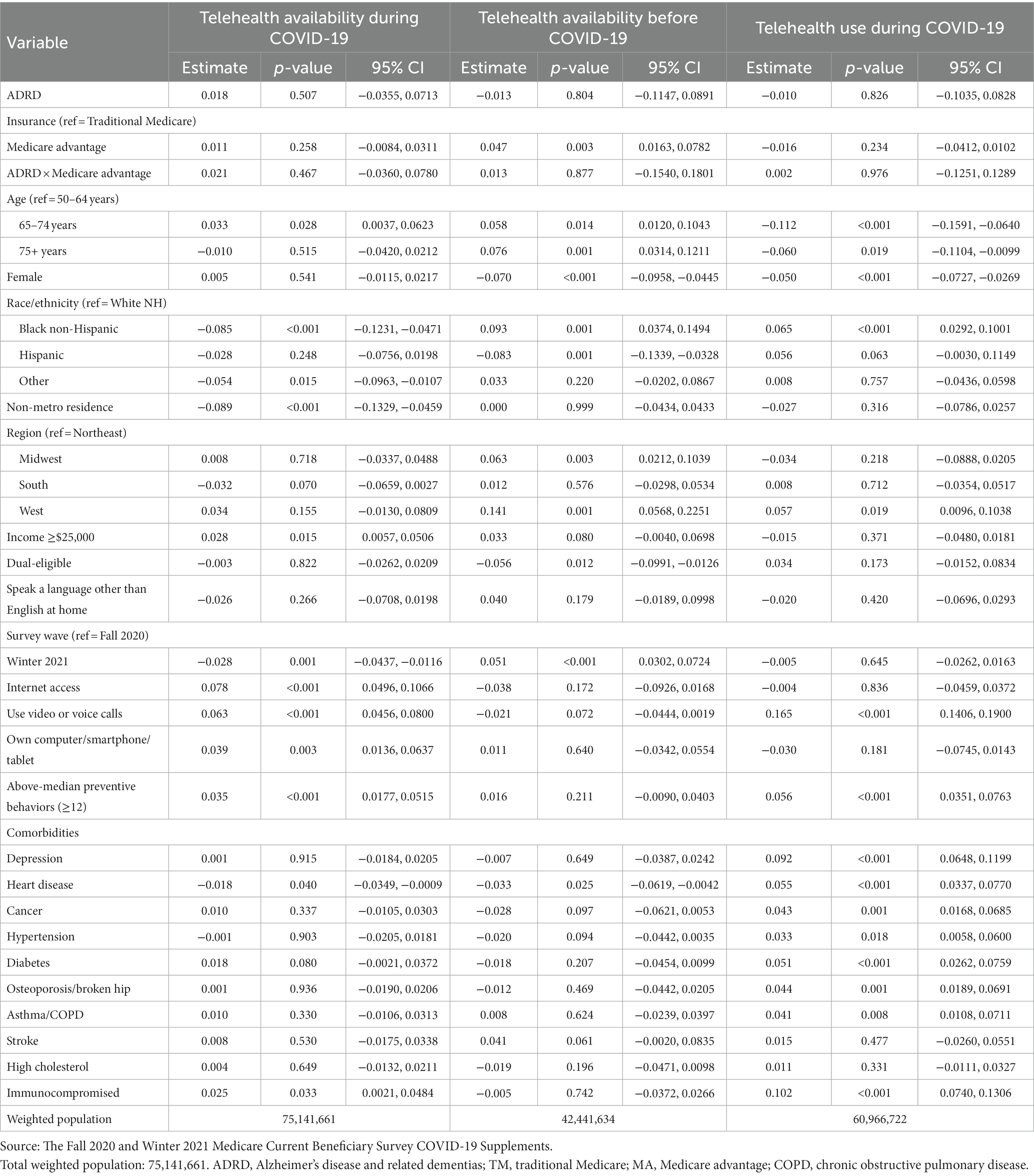
Table 3. Logistic regression: marginal effects on availability and use of telehealth services before and during COVID-19.
Telehealth availability before the COVID-19 pandemic was positively associated with being of Black Non-Hispanic ethnicity (9.34 pp.; 95% CI: 3.74, 14.94), being enrolled in Medicare Advantage (4.72 pp.; 95% CI: 1.63, 7.82), falling into the age category of 65–74 years (5.82 pp.; 95% CI: 1.20, 10.43) or 75+ years (7.62 pp.; 95%CI: 3.14, 12.11), being from the Midwest (6.26 pp.; 95% CI: 2.02, 8.67) or the West (14.09 pp.; 95% CI: 5.68, 22.51), participating in the Winter 2021 survey wave (5.13 pp.; 95% CI: 3.02, 7.24); it was negatively associated with being of Hispanic ethnicity (−8.34 pp.; 95% CI: −13.39, −3.28), being female (−7.01 pp.; 95% CI: −9.58, −4.45), being dual-eligible (−5.59 pp.; 95%CI:-9.91, −1.26), and having a history of heart disease (−3.31 pp.; 95% CI:-6.19, −0.42).
Telehealth use during the COVID-19 pandemic was positively associated with being of Black Non-Hispanic ethnicity (6.47 pp.; 95% CI: 2.92, 10.01), living in the West region (5.67 pp.; 95% CI: 0.96, 10.38), using video or voice calls (16.53 pp.; 95% CI: 14.06, 19.00), engaging in an above-median number of preventive behaviors (5.57 pp.; 95% CI: 3.51, 7.63), having a history of depression (9.23 pp.; 95% CI: 6.48, 11.99), heart disease (5.53 pp.; 95% CI: 3.37, 7.70), cancer (4.26 pp.; 95% CI: 1.68, 6.85), hypertension (3.29 pp.; 95% CI: 0.58, 6.00), diabetes (5.11 pp., 95% CI: 2.62, 7.59), osteoporosis/broken hip (4.40 pp.; 95% CI: 1.89, 6.91), asthma/COPD (4.10 pp.; 95% CI: 1.08, 7.11), or being immunocompromised (10.23 pp.; 95% CI: 7.40, 13.06); it was negatively associated with falling into the age category of 65–74 years (−11.15 pp.; 95% CI: −15.91, −6.40) or 75+ years (−6.02 pp.; 95% CI: −11.04, −0.99) and with being female (−4.98 pp.; 95% CI: −7.27, −2.69).
Supplementary analysis was conducted for each of the three outcome variables while removing the use of video or voice calls and engagement in preventive behaviors as covariates; and the results of these analyses are presented in Supplementary Tables S1, S2. All variables in the model retained significance.
This study examined the availability of telehealth services before and during the COVID-19 pandemic and telehealth use during the COVID-19 pandemic, with a focus on Medicare enrollees with respect to ADRD status and Medicare Advantage enrollment; the findings did not indicate significant differences between ADRD and non-ADRD Medicare enrollees in terms of the availability of telehealth services to these groups or their use of telehealth services. This study also showed that MA enrollees were likely to be offered telehealth services by their primary care provider before the COVID-19 pandemic, but there was no difference in availability or use of telehealth services between this group and TM enrollees during the COVID-19 pandemic.
These results suggest that policy reforms such as the CMS 1135 waivers to increase telehealth coverage for TM enrollees may have effectively addressed the TM/MA disparity in telehealth availability that was present before the COVID-19 pandemic. This notion is also supported by evidence of a sharp increase in telehealth visits among TM enrollees, from 13,000 beneficiaries receiving telehealth visits during a week before COVID-19 to 1.7 million during the last week of April 2020 (22). Another finding was that MA enrollees reported lower rates of internet access and ownership of telehealth-related technology, despite reforms such as the CHRONIC Care Act. Further analysis can examine whether reforms such as the CHRONIC Care Act are functioning to achieve their desired outcomes of improving social determinants of health for MA enrollees and whether there were challenges in implementing the CHRONIC Care Act during the COVID-19 pandemic.
While ADRD was not a significant factor in telehealth use, other comorbidities such as depression and diabetes were significantly associated with greater use of telehealth services. These comorbidities have higher prevalence in the ADRD population as compared to the non-ADRD population, which means that many patients with ADRD have co-existing conditions that need to be treated alongside ADRD to ensure good health outcomes and quality of life. In particular, depression was present in almost half of the ADRD sample and has been identified as a modifiable risk factor for ADRD (23); therefore, it is crucial to ensure that medical services such as telehealth services are available to treat both conditions. The COVID-19 pandemic may have exacerbated both ADRD and depression symptoms due to social distancing and isolation, while provision of telehealth can help improve the management of both conditions by providing virtual health services and patient monitoring when in-person services are difficult to access (24). As a result of accessing telehealth services, patients with ADRD may be less stressed about the risk of contracting COVID-19 by seeing an in-person provider and the burden of transportation for patients and their caregivers is reduced (25).
Race and ethnicity was a significant factor for all three outcomes, with Black Non-Hispanic Medicare enrollees being less likely to be offered telehealth services during the COVID-19 pandemic, more likely to be offered telehealth services before the COVID-19 pandemic, and more likely to use telehealth services during COVID-19 compared to White Non-Hispanic enrollees. These results may seem contradictory; however, they support previous research that shows that telehealth services were available to Black Non-Hispanic Medicare enrollees at higher rates than to White Non-Hispanic enrollees before COVID-19, but that during the COVID-19 pandemic, telehealth coverage subsequently increased the most for White Non-Hispanic enrollees and increased the least for Black Non-Hispanic enrollees, leading to a disparity in telehealth coverage (26). Previous research also shows that, despite telehealth services being less available to them during COVID-19, Black Medicare enrollees were more likely to use telehealth services during COVID-19 than White enrollees (12), while other research shows that Black patients were more likely to use audio-only telehealth services compared to video visits during COVID-19 (27). Further research could examine satisfaction with telehealth services and types of telehealth services used according to race and ethnicity to further examine disparities in telehealth access and quality.
Previous findings have shown that the individuals enrolled in MA are more likely to be dually enrolled in Medicaid and also more likely to be Black compared to individuals enrolled in TM (28), which we also observed in our sample. Despite differences in population characteristics, a systematic review of the literature on MA vs. TM enrollees indicated that MA enrollees had better quality of health, better health outcomes, and lower cost of care compared to TM enrollees (29).
Our study has several limitations. First, the study only included data on community-dwelling Medicare enrollees and excluded institutionalized enrollees. Previous research shows that 65% of older adults with ADRD live in the community compared to 98% of their non-ADRD counterparts (1); however, this exclusion could be regarded as a strength, as it allowed us to focus on a specific and comparable group. In addition, telehealth services were not differentiated according to whether they were provided through voice or video calls. Another limitation of this study is that we did not track switching of Medicare plans between TM and MA. Previous research as part of the 2006–2012 MCBS has shown that newly diagnosed patients with ADRD switched from TM to MA at high rates and switched away from MA plans at low rates (30), while more recent data have shown that MA enrollees with ADRD are more likely to unenroll into TM than MA enrollees without ADRD, which may indicate that MA is not meeting the medical needs of all patients with ADRD (31). This study used the MCBS COVID-19 Supplement PUFs, which were limited in the scope of available study variables compared to the MCBS Limited Data Set (LDS) (32). Further analysis of the MCBS COVID-19 Supplements linked with the MCBS LDS files could enable examination of geographic variables, such as county-level MA enrollment, as a measure of possible advantageous selection in MA (14). Finally, there is also a possibility of undercounting ADRD in survey data, as previous research has shown that improvements in the identification of neuropsychiatric disorders can be achieved by combining survey data with claims data (33).
Telehealth emerged as a crucial form of healthcare during the COVID-19 pandemic, but it is one that may not benefit all groups equally, potentially disadvantaging those such as patients with ADRD. This study shows that Medicare beneficiaries with ADRD did not encounter significant differences in the availability of telehealth services or make use of these services to a different extent compared to their non-ADRD counterparts. Further analysis could show changes over time in how Medicare enrollees with ADRD fared during the COVID-19 pandemic.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
NW: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing, Software, Visualization. MS: Supervision, Validation, Writing – review & editing. JC: Funding acquisition, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the National Institutes of Health and National Institute on Aging Grants R01AG062315 (JC, PI) and 1RF1AG083175 (JC, PI).
The authors thank the Office of Enterprise Data and Analytics (OEDA) of the Centers for Medicare & Medicaid Services (CMS) for conducting the Medicare Current Beneficiary Survey (MCBS) that was used in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1346293/full#supplementary-material
1. Alzheimer’s Association. 2023 Alzheimer’s disease facts and figures. Alzheimers Dement. (2023) 19:1598–695. doi: 10.1002/alz.13016
2. Weber, SR, Pirraglia, PA, and Kunik, ME. Use of services by community-dwelling patients with dementia: a systematic review. Am J Alzheimers Dis Other Dement. (2011) 26:195–204. doi: 10.1177/1533317510392564
3. Tannous, J, Pan, A, Bako, A, Potter, T, Jones, SL, Janjan, N, et al. COVID-19 associated disruptions in routine health care of people with mild cognitive impairment or dementia. Alzheimers Dement (Amst). (2022) 14:e12323. doi: 10.1002/dad2.12323
4. Koonin, LM, Hoots, B, Tsang, CA, Leroy, Z, Farris, K, Jolly, T, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic – United States, January-march 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1595–9. doi: 10.15585/mmwr.mm6943a3
5. Kalicki, AV, Moody, KA, Franzosa, E, Gliatto, PM, and Ornstein, KA. Barriers to telehealth access among homebound older adults. J Am Geriatr Soc. (2021) 69:2404–11. doi: 10.1111/jgs.17163
6. Langwell, KM, and Hadley, JP. Capitation and the Medicare program: history, issues, and evidence. Health Care Financ Rev. (1986) 1986:9–20.
7. Newhouse, JP, and McGuire, TG. How successful is Medicare advantage? Milbank Q. (2014) 92:351–94. doi: 10.1111/1468-0009.12061
8. Anderson, KE, Darden, M, and Jain, A. Improving prior authorization in Medicare advantage. JAMA. (2022) 328:1497–8. doi: 10.1001/jama.2022.17732
9. Jacobson, G, Cicchiello, A, Sutton, JP, and Shah, A. Medicare advantage vs. traditional Medicare: how do beneficiaries’ characteristics and experiences differ? Commonwealth Fund (2021) Available at: https://www.commonwealthfund.org/publications/issue-briefs/2021/oct/medicare-advantage-vs-traditional-medicare-beneficiaries-differ (Accessed March 8, 2023)
10. Sorbero, ME, and Kranz, AM. Perspectives on opportunities and challenges for Medicare advantage plans to address social determinants of health via the CHRONIC care act. Inquiry. (2019) 56:46958019862120.
11. Brown, B. Medicare advantage plans can now pay for internet. Health Tech Insider (2022). Available at: https://healthtechinsider.com/2022/02/21/medicare-advantage-plans-can-now-pay-for-internet/
12. Koma, W, Cubanski, J, and Neuman, T. Medicare and telehealth: coverage and use during the COVID-19 pandemic and options for the future. KFF (2021) Available at: https://www.kff.org/medicare/issue-brief/medicare-and-telehealth-coverage-and-use-during-the-covid-19-pandemic-and-options-for-the-future/
13. CMS. Medicare telemedicine health care provider fact sheet | CMS (2020) Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
14. Park, S, White, L, Fishman, P, Larson, EB, and Coe, NB. Health care utilization, care satisfaction, and health status for Medicare advantage and traditional Medicare beneficiaries with and without Alzheimer disease and related dementias. JAMA Netw Open. (2020) 3:e201809. doi: 10.1001/jamanetworkopen.2020.1809
15. Penchansky, R, and Thomas, JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. (1981) 19:127–40. doi: 10.1097/00005650-198102000-00001
16. Centers for Medicare & Medicaid Services. 2020 Medicare current beneficiary survey COVID-19 fall supplement public use file [data files and code books] (2020) Available at: https://www.cms.gov/research-statistics-data-and-systems/downloadable-public-use-files/mcbs-public-use-file
17. Centers for Medicare & Medicaid Services. 2021 Medicare current beneficiary survey COVID-19 winter supplement public use file [data files and code books] (2021) Available at: https://www.cms.gov/research-statistics-data-and-systems/downloadable-public-use-files/mcbs-public-use-file
18. Andersen, RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. (1995) 36:1–10. doi: 10.2307/2137284
19. Davis-Ajami, ML, Lu, ZK, and Wu, J. Telemedicine use in 2020 during the COVID-19 pandemic among community dwelling U.S. Medicare beneficiaries. JHA. (2021) 10:32. doi: 10.5430/jha.v10n4p32
20. Benjenk, I, Franzini, L, Roby, D, and Chen, J. Disparities in audio-only telemedicine use among Medicare beneficiaries during the coronavirus disease 2019 pandemic. Med Care. (2021) 59:1014–22. doi: 10.1097/MLR.0000000000001631
21. Park, S, Jung, J, and Larson, EB. Preventable health behaviors, COVID-19 severity perceptions, and vaccine uptake in traditional Medicare and Medicare advantage: a survey-based study. J Gen Intern Med. (2021) 36:1837–40. doi: 10.1007/s11606-021-06801-w
22. Verma, S. Early impact of CMS expansion of Medicare telehealth during COVID-19 | health affairs. Health Affairs Forefront (2020); Available at: https://www.healthaffairs.org/do/10.1377/forefront.20200715.454789/full/
23. Livingston, G, Huntley, J, Sommerlad, A, Ames, D, Ballard, C, Banerjee, S, et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet. (2020) 396:413–46. doi: 10.1016/S0140-6736(20)30367-6
24. Soares, WB, Silvestre, IT, Lima De, AMO, and De Almondes, KM. The influence of telemedicine care on the Management of Behavioral and Psychological Symptoms in dementia (BPSD) risk factors induced or exacerbated during the COVID-19 pandemic. Front Psychiatry. (2020) 11:577629. doi: 10.3389/fpsyt.2020.577629
25. Yi, JS, Pittman, CA, Price, CL, Nieman, CL, and Oh, ES. Telemedicine and dementia care: a systematic review of barriers and facilitators. J Am Med Dir Assoc. (2021) 22:1396–1402.e18. doi: 10.1016/j.jamda.2021.03.015
26. Jacobs, M, and Ellis, C. Telemedicine disparities during COVID-19: provider offering and individual technology availability. J Am Geriatr Soc. (2021) 69:2432–4. doi: 10.1111/jgs.17280
27. Chen, J, Li, KY, Andino, J, Hill, CE, Ng, S, Steppe, E, et al. Predictors of audio-only versus video telehealth visits during the COVID-19 pandemic. J Gen Intern Med. (2022) 37:1138–44. doi: 10.1007/s11606-021-07172-y
28. Weeks, WB, Cao, SY, Smith, J, Wang, H, and Weinstein, JN. Trends in characteristics of adults enrolled in traditional fee-for-service Medicare and Medicare advantage, 2011-2019. Med Care. (2022) 60:227–31. doi: 10.1097/MLR.0000000000001680
29. DuGoff, E, Tabak, R, Diduch, T, and Garth, V. Quality, health, and spending in Medicare advantage and traditional Medicare. Am J Manag Care. (2021) 27:395–400. doi: 10.37765/ajmc.2021.88641
30. Park, S, Fishman, P, White, L, Larson, EB, and Coe, NB. Disease-specific plan switching between traditional Medicare and Medicare advantage. Perm J. (2020) 24:19.059. doi: 10.7812/TPP/19.059
31. Meyers, DJ, Rahman, M, Rivera-Hernandez, M, Trivedi, AN, and Mor, V. Plan switching among Medicare advantage beneficiaries with Alzheimer’s disease and other dementias. Alzheimers Dement (NY). (2021) 7:e12150. doi: 10.1002/trc2.12150
32. CMS. (2022). Limited Data Sets. Medicare Current Beneficiary Survey (MCBS). Available at: https://www.cms.gov/research-statistics-data-and-systems/files-for-order/limiteddatasets/mcbs
Keywords: telehealth, Alzheimer’s disease and related dementias, Medicare advantage, COVID-19, racial disparities
Citation: Wang N, Seale M and Chen J (2024) Availability and use of telehealth services among patients with ADRD enrolled in traditional Medicare vs. Medicare advantage during the COVID-19 pandemic. Front. Public Health. 12:1346293. doi: 10.3389/fpubh.2024.1346293
Received: 09 December 2023; Accepted: 02 February 2024;
Published: 27 February 2024.
Edited by:
Gulzar H. Shah, Georgia Southern University, United StatesReviewed by:
Jose Antonio Pagan, New York University, United StatesCopyright © 2024 Wang, Seale and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nianyang Wang, bndhbmcxMjNAdW1kLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.