- Pediatric Clinic, Pietro Barilla Children’s Hospital, Department of Medicine and Surgery, University Hospital of Parma, Parma, Italy
Adolescents face an increased risk of contracting sexually transmitted infections (STIs) with alarming data especially concerning HIV. Limited data exists for teenagers regarding the influence of their gender identity (GI) and sexual orientation on the risk of STIs. This narrative review aims to analyse the available data to provide a comprehensive overview of STIs incidence and risk factors among adolescents, taking into account the unique circumstances related to various sexual orientations and GIs. Transgender and gender minority (TGM) youth experience more challenges accessing health services compared to cisgender youth. This is often attributed to non-inclusive health environments, barriers to obtaining medical gender affirmation, and an underestimation of sexual risk perception. Literature analysis has revealed that the majority of adolescents, both cisgender and TGM, have limited awareness regarding the risks associated with their sexual behaviors, the most common sexually transmitted diseases, and strategies for prevention, such as PrEP and HPV vaccination. Moreover, a significant portion of pediatricians possess limited knowledge and comfort in addressing various aspects of sexual health, particularly when it involves discussing topics such as sexual orientation, gender identity, and sexual behaviors with sexually active adolescents. This underscores the pressing need for enhanced education for pediatricians, specifically focusing on STIs diagnosis, prevention, and screening.
1 Introduction
Sexually transmitted infections (STIs) refer to a wide spectrum of bacterial, fungal, viral and protozoal infections that share a common pattern of transmission through sexual contact (1). It has been largely observed that adolescents are at increased risk for acquiring STIs. The World Health Organization (WHO) estimates that more than 1 million STIs affect people between the ages of 15 and 49 every day, and that number is constantly rising (2). Recent data from United States reported that of about 20 million new STIs every year, 50% of cases occur among youth aged 15–24 y.o (3). Similar data have been collected in Australia, reporting 25% of chlamydia infections diagnosed among people younger than 20 y.o (4). In Ireland, Davoren et al. reported that the incidence of STIs among adolescents was 225/100,000 person-years (5). Moreover, as reported by Viottini et al. the incidence of STIs in Italy has particularly increased in the population aged 15–24 y.o. across the last 10 years (6, 7). The literature has demonstrated that various risk factors, both biological and neuro-behavioral, make adolescents more susceptible to contracting sexually transmitted infections; however, such data are almost always reported in the pediatric population without taking into account different sexual orientations and expressions of gender identity (GI) (8–13). This narrative review aims to analyse the available data to provide a comprehensive overview of STIs incidence and risk factors among adolescents, taking into account the unique circumstances related to various sexual orientations and GIs.
2 Methods
This is a narrative review of literature on STIs among cisgender and transgender minority youth in pediatrics. Systematic searches were performed in Pubmed and Google Scholar up to September 2023. Language was restricted to English. Search terms included “STIs” OR “sexually transmitted infection” AND “cisgender” OR “transgender” OR “gender nonconforming” OR “non-Binary” in combination with “adolescents” OR “youth.” Original research studies, review articles, letters to the editor, cohort studies published between 2012 and 2023 were included. Relevant papers were scrutinized for additional sources not identified by the electronic search, thereby enriching the research findings through a snowballing approach. We excluded papers that did not focus specifically on adolescent cisgender and TGD populations. Data from earlier studies were taken into account if relevant to the scope of this review. All relevant articles were then evaluated, and pertinent articles were included in this review.
3 Risk factors
Main risks for increased STIs rates among adolescents regardless their sexual orientation and GI are summarized in Table 1.
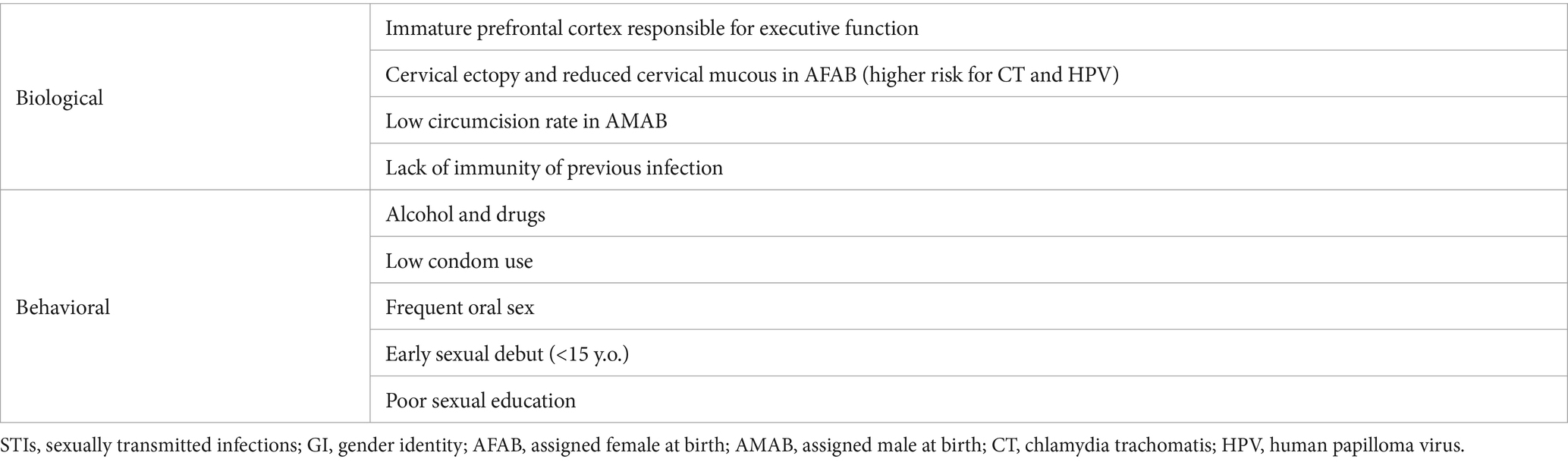
Table 1. Risk factors for increased STIs rates among adolescents regardless of sexual orientation and GI.
4 Epidemiology
Four treatable STIs, i.e., those due to Trichomonas vaginalis (42%), CT (34%), Neisseria gonorrhoeae (NG) (22%), and Treponema pallidum (2%), are mostly responsible for the 374 million new cases that have been reported globally in 2020 (2). According to additional WHO data, the Herpes Simplex Virus-2 (HSV-2) infection that causes genital herpes is currently affecting about 500 million adults, although the number of cases due to HSV-1 is now increasing (14). Additionally HPV, which is the main cause of anal cancer in males who have sex with men and cervical cancer in women, is present in more than 300 million women and 300 million men (6, 14). Moreover, there are resurgent STIs like lymphogranuloma venereum as well as new outbreaks of illnesses that can spread through sexual contact, including monkeypox, Shigella sonnei, Neisseria meningitidis, Ebola, and Zika (2). Recent data from USA enlightened the epidemiological context of STIs among the young population (12). Teenagers have been found to have the highest prevalence of CT and NG of any age group. In the population aged 15–19 years old, the CT rate infection has increased by 4.1% among girls and 15.3% among boys, while the NG rate infection has increased by 11.3%. In the same population and period, syphilis has increased by 24.5% (12).
There is lack of data regarding the HPV prevalence in the adolescent population (15). Markowitz et al. have estimated that 29% of adolescent girls aged 14–19 y.o. had HPV infection (16). Remarkably, the study has also highlighted the positive impact of the HPV vaccine against the infection rate in USA, reporting a 64% reduction in HPV 6, 11, 16 and 18 prevalence among adolescent girls. These findings fully agree with more recent studies. Ju et al. have reported a decrease of HPV 16 prevalence rate (35% in vs. 5%) in Swedish youth after HPV vaccine was offered to 10–12 years old girls through the school-based vaccination program (17). Similarly, in Spinner et al. findings HPV detection decreased from 35 to 6.7% among HPV vaccinated girls after 10 years from the vaccine introduction (18). Numbers may be different elsewhere according to HPV vaccination recommendations and coverage.
Sexually active youth also have a high risk of contracting human immunodeficiency virus (HIV) (8). As reported in data from USA, adolescents and young adults represented 4% of persons living with HIV infection in 2018, while teenagers made up 21% of all new HIV diagnoses (19, 20). According to Underwood et al. only 54% of sexually active high school adolescents reported condom use in their last sexual intercourse and this rate was even lower among homosexual adolescents (21). Those ones also reported a larger number of sexual partners in their lifetime compared to the heterosexual peers. Adolescents also have poorer viral suppression rates, which reduces their likelihood of maintaining good health and raises their risk of HIV transmission to others (22, 23).
5 Transgender and other gender minority youth
GI is the sense of being male, female, a combination of both, or neither (24). Individuals who identify as transgender (TGD) are those whose gender identification does not match the sex they were assigned at birth. Adolescence is a critical time for the development of GI, as young people navigate the completion of developmental tasks such as forming an identity, developing relationships, and exploring sexuality (8).
It has been observed that transgender and gender minority youth (TGMY) experience unique risks that can lead to increased rates of STIs and sexual risk behaviors (25). As described by Phillips et al. one of the factors that must be taken into account could be the role of minority stress, which is the excessive stress experienced by a marginalized community as a result of proximal (e.g., perceived stigma) and distal (e.g., systemic stigmatization) elements (26). Together with the gender affirmation framework, which relates to the way social affirmation/non-affirmation of one’s perceived gender may influence behavioral risk factors, this has been related to potentially dangerous experiences for TGMY (27). Adolescents who experience non-inclusive background at school as well as non-inclusive families might be more likely to incur into loss of health services, engagement in sex work, weak social support networks, all factors associated with HIV risk (28–32). Reisner et al. have reported that 31% of transgender youth had been engaged in any condomless receptive or insertive intercourse (vaginal and/or anal) within the last 6 months (25). Moreover, 33% had ever diagnosed with an STI in their lifetime and 55% of transgender girls had been diagnosed with syphilis (25).
Among STIs, HIV represents a critical situation. Data available from a recent USA surveillance report estimated that 21% of all new HIV diagnoses in 2019 and 45% of all undiagnosed HIV cases affect young people aged between 13 and 24 years old (19, 33). We still have lack of data among TGMY; however, it has been estimated an HIV prevalence of 9.2% for all TGD persons in USA. In view of this, we can expect that in the same way TGMY are at disproportionate risk of being infected (34). Fisher et al. have reported that 58% of TGMY aged 14–17 years had had at least one lifetime sexual partner and that the majority of adolescents believed extremely unlikely to be infected with HIV (35). Nevertheless, Reisner et al. have showed a high proportion of TGD boys that engaged into condomless receptive anal sex (41% against 2.4% among TGD girls), which is the most efficient HIV transmission risk behavior (25). Sevelius et al. highlighted that the 52.9% of TGMY had never tested for HIV and the 66% had never tested for any STDs (27). Compared to TGD peers, condom use at last sex was more likely among cisgender adolescents (36).
According to research, TGMY may encounter the same obstacles to HIV prevention programs catered to their needs as TGD adults. These obstacles include a lack of TGD-friendly and competent clinicians and uncomfortable talking about TGD-specific health issues with medical doctors (37–40). In according with these findings, in the Fisher et al. study population nearly half of the participants said their medical provider was ignorant of their GI and expressed worry that disclosure would lead to rejection; moreover, younger participants showed higher levels of gender-related stigma (35). Compared to cisgender peers, TGD adolescents seem to receive a pourer sex education. As observed by Bloom et al. sexual education provided among American schools focuses predominantly on pregnancy prevention and cis-heterosexual intercourses (41). Literature showed that medical gender affirmation may increase awareness of HIV and STIs prevention; after affirming their GI, young individuals may be more likely to engage in self-care or health-promoting actions (27).
Table 2 reports main risks for increased STIs rates among TGMY.
6 Prevention of HIV and HPV
To contain the continuous increase in STIs among adolescents, it is essential to instill awareness of the importance of prevention.
Concerning HIV, pre-exposure prophylaxis (PrEP) has been found to be effective in reducing the risk of HIV transmission by >90% (42, 43). Recent research has revealed that TGMY have poor PrEP awareness and very low uptake despite the medication’s well-known effectiveness (44). In accordance with this, Horvath et al. have reported that almost 44% of TGMY have never heard about PrEP and only 0.5% were currently using PrEP (45). The majority of individuals did not want to use PrEP because they believed their personal level of HIV risk to be low (45). Similar data were collected by other authors among TGD adults (27, 46–48).
As underlined by the American Academy of Pediatrics (AAP) in 2022, the majority of pediatricians still experiment lack of knowledge, personal discomfort discussing sexual issues with adolescents and insufficient training in how to treat and prevent STIs and HIV. However, pediatricians should play a key role in preventing and controlling HIV infection (49). Therefore, it has been recommended routine HIV screening for all youth 15 years or older at least once in health care setting; then those with increased risk (i.e., sexually active adolescents) should receive a screening every year and those with high risk (i.e., male youth who report same sex contact, substance abusers, TGMY, partners of HIV-infected ones or of drug users) should be rescreened every 3–6 months (49). As part of an all-encompassing preventative plan that also includes other prevention measures (such as safer sex behaviors and use of barrier protection) to lower the risk of STIs, the AAP highlighted that HIV PrEP should be made available to all youth at risk for HIV acquisition. For young people who may have been exposed to HIV during a period of high-risk sexual activity, unsafe needle use, or sexual assault, HIV post-exposure prophylaxis (PEP) along with antiretroviral medication should be taken into consideration (49).
With Resolution of the BoD No. 15 of April 26, 2023, the Italian Medicines Agency has admitted the reimbursability of the association Emtricitabine/Tenofovir Disoproxil for PrEP in order to reduce the risk of sexually transmitted HIV infection in adults and adolescents at high risk (50). As PrEP, it is recommended to administrate Emtricitabine/Tenofovir Disoproxil in adolescents aged 12 years and older (51).
HPV vaccine is recommended for preventing precancerous lesions, malignancies of the cervix, vulva, vagina, penis, and anus, as well as genital condyloma acuminata, which are caused by HPV subtypes (52). Given before the start of sexual activity, the HPV vaccination is most effective. According to data, 11% of girls and 16% of males had their first sexual experience by the age of 15 years, with the first sexual encounter occurring on average at 17 y.o (53). It is crucial to be immunized before the age of 13 years, as 2% of female and 5% of male adolescents are thought to have had their sexual debut before turning 13 (54). As summarized by Bednarczyk et al., evidence for prevention of high-grade pre-cancers and cervical cancer is strong, with several clinical trials documenting HPV vaccines efficacy against CIN2+ of 95 to 98 and 100% against high grade vaginal and vulvar lesions (55–57).
Along with promotion of the available vaccinations, it is crucial that pediatricians provide inclusive sex education, with an eye on both cisgender and TGMY, which can result in delayed sex debut, increased condom use and reduced sexual risk behaviors (58, 59).
7 Conclusion
STIs represent a common cause of disease among all adolescents. Literature analysis showed increasing rates of STIs overall in this population, with alarming data particularly related to HPV in those who did not receive the vaccine, and HIV. Our literature review has highlighted a significant lack of data regarding the sexual health of cisgender and, even more so, transgender adolescents in European and Italian studies; for this reason, many of the presented data come from American studies. However, it is important to emphasize how the specific situation of transgender and cisgender youth can vary significantly across countries, even among Western countries. Moreover, the majority of pediatricians have limited knowledge and comfort on many items regarding sexual health, especially when it comes to discuss sexual orientation, GI and sexual behaviors with sexually active adolescents. Compared with cisgender youth, TGMY experiment worse access to health services due to a non-inclusive health environment, difficult access to medical gender affirmation and underestimated sexual risk perception. Specific training should be provided to pediatricians related to TGMY care, including how to discuss about their sexual identity, how to share information about STIs screening, particularly about HIV testing and PrEP. Both cisgender and TGD youth still have poor PrEP awareness, which leads to lack of access to the medication even where it is available for free, and their HIV personal risk is perceived as low by the majority of them. In addition, a strong communication about the importance of some vaccines against STIs should be done with all adolescent patients. Finally, due to the limited data, further studies are urgently needed on the epidemiology of STIs among patients aged under 18 years with non-heterosexual orientation and non-cisgender identity.
Author contributions
PD: Conceptualization, Data curation, Investigation, Writing – original draft. SE: Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The publication of this manuscript was supported by the Laboratory for Clinical Pediatric Research, University of Parma, Parma, Italy (PED-2023-12).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Stary, A . The changing Spectrum of sexually transmitted infections in Europe. Acta Derm Venereol. (2020) 100:adv00114–247. doi: 10.2340/00015555-3470
2. WHO . Sexually transmitted infections (STIs). Available at: https://www.who.int/news-room/fact-sheets/detail/sexuallytransmitted-infections-(STIs) (Accessed September 23, 2023).
3. Shannon, CL , and Klausner, JD . The growing epidemic of sexually transmitted infections in adolescents: a neglected population. Curr Opin Pediatr. (2018) 30:137–43. doi: 10.1097/MOP.0000000000000578
4. National Notifiable Disease Surveillance System . Notifications of a selected disease by age group, sex and year 2012. Available at: http://www9.health.gov.au/cda/source/Rpt_5_sel.cfm (Accessed September 23, 2023).
5. Davoren, MP , Hayes, K , Horgan, M , and Shiely, F . Sexually transmitted infection incidence among adolescents in Ireland. J Fam Plann Reprod Health Care. (2014) 40:276–82. doi: 10.1136/jfprhc-2013-100596
6. Viottini, E , Albanesi, B , Casabona, E , Onorati, R , Campagna, S , and Borraccino, A . Ten-year trend in emergency department visits for sexually transmitted infections among adolescents: a retrospective cross-sectional study in Italy. Int J Environ Res Public Health. (2022) 19:14207. doi: 10.3390/ijerph192114207
7. Istituto Superiore di Sanità . Notiziario Dell’ISS (Volume 35, n. 6, 2022)—Le Infezioni Sessualmente Trasmesse: Aggiornamento Dei Dati Dei Due Sistemi Di Sorveglianza Sentinella Attivi in Italia al 31 Dicembre 2020. Available at: https://www.epicentro.iss.it/ist/NotiziarioIssCoa (Accessed September 23, 2023).
8. Diana, P , and Esposito, S . LGBTQ+ youth health: an unmet need in pediatrics. Children (Basel). (2022) 9:1027. doi: 10.3390/children9071027
9. Ayerdi Aguirrebengoa, O , Vera Garcia, M , Rueda Sanchez, M , D’Elia, G , Chavero Méndez, B , Alvargonzalez Arrancudiaga, M, et al. Risk factors associated with sexually transmitted infections and HIV among adolescents in a reference clinic in Madrid. PLoS One. (2020) 15:e0228998. doi: 10.1371/journal.pone.0228998
10. Agwu, A . Sexuality, sexual health, and sexually transmitted infections in adolescents and young adults. Top Antivir Med. (2020) 28:459–62.
11. Burchell, AN , Winer, RL , de Sanjosé, S , and Franco, EL . Epidemiology and transmission dynamics of genital HPV infection. Vaccine. (2006) 24:S52–61. doi: 10.1016/j.vaccine.2006.05.031
12. Sexually Transmitted Disease Surveillance , (2016). Division of STD prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Sep. 2017.
13. Zhang, C , and Vermund, SH . Voluntary medical male circumcision for HIV prevention: a global overview. Curr HIV/AIDS Rep. (2022) 19:474–83. doi: 10.1007/s11904-022-00632-y
14. WHO . Consolidated guidelines on HIV, viral hepatitis and STI prevention, diagnosis, treatment and care for key populations. Geneva, Switzerland: WHO (2022).
15. Tommasino, M . The human papillomavirus family and its role in carcinogenesis. Semin Cancer Biol. (2014) 26:13–21. doi: 10.1016/j.semcancer.2013.11.002
16. Markowitz, LE , Liu, G , Hariri, S , Steinau, M , Dunne, EF , and Unger, ER . Prevalence of HPV after introduction of the vaccination program in the United States. Pediatrics. (2016) 137:e20151968. doi: 10.1542/peds.2015-1968
17. Du, J , Ährlund-Richter, A , Näsman, A , and Dalianis, T . Human papilloma virus (HPV) prevalence upon HPV vaccination in Swedish youth: a review based on our findings 2008–2018, and perspectives on cancer prevention. Arch Gynecol Obstet. (2021) 303:329–35. doi: 10.1007/s00404-020-05879-7
18. Spinner, C , Ding, L , Bernstein, DI , Brown, DR , Franco, EL , Covert, C, et al. Human papillomavirus vaccine effectiveness and herd protection in young women. Pediatrics. (2019) 143:e20181902. doi: 10.1542/peds.2018-1902
19. Centers for Disease Control and Prevention . Estimated HIV incidence and prevalence in the United States, 2014–2018. HIV Surveillance Supplemental Report 2020; volume 25, No. 1. 2020. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillancesupplemental-report-vol-25-1.pdf (Accessed September 23, 2023).
20. HIV Surveillance Report . (2018) (Updated); vol. 31. 2020. Available at: https://www.cdc.gov/mmwr/volumes/68/wr/mm6811e1.htm (Accessed September 23, 2023).
21. Underwood, JM , Brener, N , Thornton, J , Harris, WA , Bryan, LN , Shanklin, SL, et al. Overview and methods for the youth risk behavior Surveillance — United States, 2019. MMWR Morb Mortal Wkly Rep. (2020) 69:1–10. doi: 10.15585/mmwr.su6901a1
22. Bradley, H , Hall, HI , Wolitski, RJ , Van Handel, MM , Stone, AE , LaFlam, M, et al. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV–United States, 2011. MMWR Morb Mortal Wkly Rep. (2014) 63:1113–7.
23. Zanoni, BC , and Mayer, KH . The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Patient Care STDs. (2014) 28:128–35. doi: 10.1089/apc.2013.0345
24. Diana, P , and Esposito, S . A gender-based point of view in pediatric neurology. J Pers Med. (2023) 13:483. doi: 10.3390/jpm13030483
25. Reisner, SL , Jadwin-Cakmak, L , Sava, L , Liu, S , and Harper, GW . Situated vulnerabilities, sexual risk, and sexually transmitted Infections' diagnoses in a sample of transgender youth in the United States. AIDS Patient Care STDs. (2019) 33:120–30. doi: 10.1089/apc.2018.0249
26. Meyer, IH . Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. (2003) 129:674–97. doi: 10.1037/0033-2909.129.5.674
27. Sevelius, JM . Gender affirmation: a framework for conceptualizing risk behavior among transgender women of color. Sex Roles. (2013) 68:675–89. doi: 10.1007/s11199-012-0216-5
28. Johns, MM , Zamantakis, A , Andrzejewski, J , Boyce, L , Rasberry, CL , and Jayne, PE . Minority stress, coping, and transgender youth in schools-results from the resilience and transgender youth study. J Sch Health. (2021) 91:883–93. doi: 10.1111/josh.13086
29. Reisner, SL , Sava, LM , Menino, DD , Perrotti, J , Barnes, TN , Humphrey, DL, et al. Addressing LGBTQ student bullying in Massachusetts schools: perspectives of LGBTQ students and school health professionals. Prev Sci. (2020) 21:408–21. doi: 10.1007/s11121-019-01084-4
30. Rew, L , Yeargain, O , Peretz, C , and Croce, E . "I'm losing everything all over again": responses from youth experiencing homelessness during the COVID-19 pandemic. Arch Psychiatr Nurs. (2021) 35:653–7. doi: 10.1016/j.apnu.2021.08.002
31. Shelton, J . Reframing risk for transgender and gender-expansive young people experiencing homelessness. J Gay Lesbian Soc Serv. (2016) 28:277–91.
32. Brennan, J , Kuhns, LM , Johnson, AK , Belzer, M , Wilson, EC , and Garofalo, R . Adolescent medicine trials network for HIV/AIDS interventions. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. (2012) 102:1751–7. doi: 10.2105/AJPH.2011.300433
33. Center for Disease Control and Prevention . (2021). HIV Infection, risk, prevention, and testing behaviors among transgender women – National HIV behavioral surveillance, 7 U.S.Cities, 2019–2020 (HIV surveillance special report 27, issue). Available at: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html (Accessed September 23, 2023).
34. Becasen, JS , Denard, CL , Mullins, MM , Higa, DH , and Sipe, TA . Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and Meta-analysis, 2006-2017. Am J Public Health. (2019) 109:e1–8. doi: 10.2105/AJPH.2018.304727
35. Fisher, CB , Fried, AL , Desmond, M , Macapagal, K , and Mustanski, B . Perceived barriers to HIV prevention services for transgender youth. LGBT Health. (2018) 5:350–8. doi: 10.1089/lgbt.2017.0098
36. Phillips, G 2nd, Davoudpour, S , Floresca, YB , Felt, D , Curry, CW , Wang, X, et al. Disparities in HIV testing, condom use, and HIV education between transgender and not transgender high school-aged youth: findings from the 2019 youth risk behavior survey. Health Educ Behav. (2023) 50:29–40. doi: 10.1177/10901981221142238
37. Macapagal, K , Bhatia, R , and Greene, GJ . Differences in healthcare access, use, and experiences within a community sample of racially diverse lesbian, gay, bisexual, transgender, and questioning emerging adults. LGBT Health. (2016) 3:434–42. doi: 10.1089/lgbt.2015.0124
38. Corliss, HL , Belzer, M , Forbes, C , and Wilson, EC . An evaluation of service utilization among male to female transgender youth: qualitative study of a clinic-based sample. J LGBT Health Res. (2007) 3:49–61. doi: 10.1300/J463v03n02_06
39. Poteat, T , German, D , and Kerrigan, D . Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc Sci Med. (2013) 84:22–9. doi: 10.1016/j.socscimed.2013.02.019
40. Snelgrove, JW , Jasudavisius, AM , Rowe, BW , Head, EM , and Bauer, GR . "completely out-at-sea" with "two-gender medicine": a qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Serv Res. (2012) 12:110. doi: 10.1186/1472-6963-12-110
41. Bloom, BE , Kieu, TK , Wagman, JA , Ulloa, EC , and Reed, E . Responsiveness of sex education to the needs of LGBTQ + undergraduate students and its influence on sexual violence and harassment experiences. Am J Sex Educ. (2022) 17:368–99. doi: 10.1080/15546128.2022.2033662
42. Grant, RM , Lama, JR , Anderson, PL , McMahan, V , Liu, AY , Vargas, L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. (2010) 363:2587–99. doi: 10.1056/NEJMoa1011205
43. Liu, AY , Vittinghoff, E , Sellmeyer, DE , Irvin, R , Mulligan, K , Mayer, K, et al. Bone mineral density in HIV-negative men participating in a tenofovir pre-exposure prophylaxis randomized clinical trial in San Francisco. PLoS One. (2011) 6:e23688. doi: 10.1371/journal.pone.0023688
44. Giguere, R , Frasca, T , Dolezal, C , Febo, I , Cranston, RD , Mayer, K, et al. Acceptability of three novel HIV prevention methods among young male and transgender female sex Workers in Puerto Rico. AIDS Behav. (2016) 20:2192–202. doi: 10.1007/s10461-016-1387-9
45. Horvath, KJ , Todd, K , Arayasirikul, S , Cotta, NW , and Stephenson, R . Underutilization of pre-exposure prophylaxis services among transgender and nonbinary youth: findings from project moxie and TechStep. Transgend Health. (2019) 4:217–21. doi: 10.1089/trgh.2019.0027
46. Dolezal, C , Frasca, T , Giguere, R , Ibitoye, M , Cranston, RD , Febo, I, et al. Awareness of post-exposure prophylaxis (PEP) and pre-exposure prophylaxis (PrEP) is low but interest is high among men engaging in Condomless anal sex with men in Boston, Pittsburgh, and San Juan. AIDS Educ Prev. (2015) 27:289–97. doi: 10.1521/aeap.2015.27.4.289
47. Misra, K , and Udeagu, CC . Disparities in awareness of HIV Postexposure and Preexposure prophylaxis among notified partners of HIV-positive individuals, new York City 2015–2017. J Acquir Immune Defic Syndr. (2017) 76:132–40. doi: 10.1097/QAI.0000000000001473
48. Finlayson, T , Cha, S , Xia, M , Trujillo, L , Denson, D , Prejean, J, et al. Changes in HIV Preexposure prophylaxis awareness and use among men who have sex with men – 20 urban areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep. (2019) 68:597–603. doi: 10.15585/mmwr.mm6827a1
49. Hsu, KK , and Rakhmanina, NY . Adolescents and young adults: the Pediatrician's role in HIV testing and pre- and Postexposure HIV prophylaxis. Pediatrics. (2022) 149:e2021055207. doi: 10.1542/peds.2021-055207
50. AIFA . AIFA approves reimbursability of drugs for pre-exposure prophylaxis to HIV-1 (PrEP). Available at: https://www.aifa.gov.it/documents/20142/1804917/Comunicato_AIFA_n.704_EN.pdf (Accessed September 23, 2023).
51. European Medicines Agency . Truvada. Available at: https://www.ema.europa.eu/en/documents/product-information/emtricitabine/tenofovir-disoproxil-zentiva-epar-product-information_it.pdf (Accessed September 23, 2023).
52. Barbieri, M , and Boccalini, S . Return on investment (ROI) of three vaccination Programmes in Italy: HPV at 12 years, herpes zoster in adults, and influenza in the elderly. Vaccines (Basel). (2023) 11:924. doi: 10.3390/vaccines11050924
53. Abma, JC , and Martinez, GM . Sexual activity and contraceptive use among teenagers in the United States, 2011–2015. Natl Health Stat Report. (2017) 104:1–23.
54. Kann, L , McManus, T , Harris, WA , Shanklin, SL , Flint, KH , Hawkins, J, et al. Youth risk behavior surveillance – United States, 2015. MMWR Surveill Summ. (2016) 65:1–174. doi: 10.15585/mmwr.ss6506a1
55. Bednarczyk, RA . Addressing HPV vaccine myths: practical information for healthcare providers. Hum Vaccin Immunother. (2019) 15:1628–38. doi: 10.1080/21645515.2019.1565267
56. Mennini, FS , Silenzi, A , Marcellusi, A , Conversano, M , Siddu, A , and Rezza, G . HPV vaccination during the COVID-19 pandemic in Italy: opportunity loss or incremental cost. Vaccines (Basel). (2022) 10:1133. doi: 10.3390/vaccines10071133
57. Ibrahim Khalil, A , Zhang, L , Muwonge, R , Sauvaget, C , and Basu, P . Efficacy and safety of therapeutic HPV vaccines to treat CIN 2/CIN 3 lesions: a systematic review and meta-analysis of phase II/III clinical trials. BMJ Open. (2023) 13:e069616. doi: 10.1136/bmjopen-2022-069616
58. Pelucchi, C , Esposito, S , Galeone, C , Semino, M , Sabatini, C , Picciolli, I, et al. Knowledge of human papillomavirus infection and its prevention among adolescents and parents in the greater Milan area, northern Italy. BMC Public Health. (2010) 10:378. doi: 10.1186/1471-2458-10-378
59. Chin, HB , Sipe, TA , Elder, R , Mercer, SL , Chattopadhyay, SK , Jacob, V, et al. The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections. Am J Prev Med. (2012) 42:272–94. doi: 10.1016/j.amepre.2011.11.006
Keywords: adolescents, behavioral risk factors, gender minority youth, sexually transmitted infections, transgender, cisgender
Citation: Diana P and Esposito S (2024) Epidemiology, risk factors, and prevention strategies of HIV, HPV, and other sexually transmitted infections among cisgender and transgender youth: a narrative review. Front. Public Health. 12:1342532. doi: 10.3389/fpubh.2024.1342532
Edited by:
Antoinette van der Kuyl, University of Amsterdam, NetherlandsReviewed by:
Eustachio Cuscianna, University of Bari Aldo Moro, ItalySnezana Miodraga Radovanovic, University of Kragujevac, Serbia
Copyright © 2024 Diana and Esposito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susanna Esposito, c3VzYW5uYW1hcmlhcm9iZXJ0YS5lc3Bvc2l0b0B1bmlwci5pdA==
 Pierluigi Diana
Pierluigi Diana Susanna Esposito
Susanna Esposito