- 1Department of Human Physiology, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Department of Human Physiology, College of Medicine and Health Sciences, Ambo University, Ambo, Ethiopia
- 3Department of Neonatal Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Department of Internal Medicine, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 5Department of Environmental and Occupational Health and Safety, College of Medicine and Health Sciences, Institute of Public Health, University of Gondar, Gondar, Ethiopia
- 6Department of General Midwifery, School of Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Introduction: Effective communication between adolescents and their parents is crucial for reducing sexual health problems. This open dialogue can help address misconceptions, provide accurate information, and foster a supportive environment where adolescents feel comfortable seeking guidance and discussing sensitive issues related to their sexual health. In Ethiopia, with its diverse ethnic and cultural background, effective communication between parents and adolescents about sexual and reproductive health (SRH) is crucial in reducing the likelihood of adolescents engaging in risky sexual behaviors. Despite the importance of such communications, there were no data showing the level of parent–adolescent communication (PAC) in secondary public schools in Gondar town. Therefore, this study aimed to determine the level of parent–adolescent communication on sexual and reproductive health issues along with its influencing factors, among secondary students in Gondar town, northwest Ethiopia.
Methods: We employed an institution-based cross-sectional study design. A total of 424 students were recruited using a systematic random sampling technique, with a 100% response rate. We developed a structured questionnaire from the related literature to collect data from the participants of the study. The data were entered using EpiData version 4.6, and analyzed using SPSS version 25. A binary logistic regression model was fitted to identify associated factors.
Results: The proportion of adolescents who had communicated with their parents was 37.7% (95% CI: 34.65–44.76). In a multivariable analysis at a 95% confidence interval (CI), variables such as being female (adjusted odds ratio (AOR) = 2.23; 95% CI: 1.09–7.45), belonging to grades 11–12 (AOR = 1.25; 95% CI: 1.19–6.98), living with parents/caregivers (AOR = 1.26; 95% CI: 1.07–5.66), having a positive attitude toward sexual health (AOR = 2.4; 95% CI: 1.34–7.82), having poor knowledge about SRH issues (AOR = 1.23; 95% CI: 1.04–7.81), and having good knowledge about the puberty period (AOR=1.23; 95% CI:1.04–7.89) were statistically associated with parent–adolescent communication.
Conclusion and recommendations: This study found a low level of communication between parents and adolescents regarding sexual and reproductive health (SRH) issues. To address this challenge, it is crucial to implement evidence-based education on SRH topics, such as consent, healthy relationships, communication skills, STDs, contraception, and interpersonal dynamics. Enhancing parent–adolescent dialogue on SRH can be achieved by implementing peer education among senior students and training teachers in effective communication techniques. The study also recommended conducting qualitative research to explore the specific barriers affecting parent–adolescent communication.
Introduction
Poor communication skills between parents and adolescents regarding sexual and reproductive health (SRH) can lead to misinformation, misunderstandings, and a reluctance to seek help (1–3). The level of parent–adolescent communication on sexual and reproductive health issues varies across different countries in developed regions. For instance, it was reported to be highest in the United States of America at 70.6% and in Mexico at 83.1%. Conversely, lower levels of parent–adolescent communication were observed in Myanmar at 6.8% and in India at 13% (4–7). Similarly, the prevalence of parent–adolescent communication was reported to be lower in African countries. For instance, in Nigeria, it was reported as 37.4% (8), while in Lesotho, the prevalence was 20 % (9). In Ethiopia, the prevalence was reported to be within the range of 25.3% and 36.9% (10). Parent–adolescent communication regarding sexuality is critical in informing young people about risks and protective behaviors, which, in turn, decreases the likelihood of involvement in risky sexual behaviors (11, 12).
Factors that affect parent–adolescent communication concerning sexual and reproductive health (SRH) issues include cultural taboos, embarrassment in discussing sexual matters, lack of communication skills, beliefs about sexuality, and knowledge gaps (13, 14).
Adolescents are often underserved by current health services, which highlights the importance of prioritizing their needs in universal health coverage initiatives after 2015 (15). Many adolescents die prematurely due to preventable or treatable causes, including accidents, suicide, violence, pregnancy complications, and reproductive illnesses (16, 17). According to the WHO reports, 1.3 million young people die each year from preventable causes (18). In sub-Saharan Africa, 82% of the 2.1 million adolescents are affected with HIV, with 58% being female individuals. Comprehensive knowledge about HIV, condom use, testing, and treatment remains low in the poorest countries (16, 18, 19). In addition, approximately 16 million women aged 15–19 years give birth annually, with 95% of these births occurring in low- and middle-income countries (17, 18). Parents who openly discuss sexuality with their young children foster better communication, helping to reduce risky behaviors, such as early sexual initiation, unwanted pregnancies, and other reproductive health problems (13, 15). Effective parent–adolescent communication is important to reduce adolescents' engagement in risky sexual behaviors (13, 14). Discussions between parents and adolescents about sexual and reproductive health enhance awareness, reduce risky behaviors, and promote positive SRH outcomes (20–25). Various studies have indicated that factors such as parents' reluctance to discuss, feelings of shame, cultural taboos, lack of communication skills, limited awareness, and the belief that discussions might encourage sexual activity are key elements that affect parent–adolescent conversations on SRH topics (26–28). In sub-Saharan African countries, including Ethiopia, evidence shows that a lack of parental interest in discussions, feelings of shame, and cultural taboos around discussing sexual matters are factors affecting parent–adolescent communication (29, 30).
In the Ethiopian context of ethnic and cultural diversity, effective parent–adolescent communication is crucial to reduce adolescents' engagement in risky sexual behaviors (10, 31). However, there is limited information on parent–adolescent communication among adolescents attending secondary schools. Hence, the primary objective of this study was to assess the level of parent–adolescent communication and identify associated factors. The research sought to provide valuable insights that could inform strategies to enhance SRH communication, thereby contributing to better health outcomes for adolescents in Gondar town.
Methods and materials
Study design
An institution-based cross-sectional study design was employed.
Study area and period
The study was conducted in secondary public schools located in Gondar town, spanning from 18 August 2023 to 20 September 2023. Gondar town is located approximately 728 km away from Addis Ababa, the nation's capital. In addition, it is situated approximately 180 km away from Bahir Dar, which serves as the capital of the Amhara regional state. Moreover, Gondar town has 22 kebeles and 14 high schools, including 9 government schools and 5 private schools (32).
Source population
The source population comprised all regular students aged 10–19 years who were attending high schools and preparatory schools in Gondar town during 2023. The study population included students who met the specified inclusion criteria.
Inclusion criteria
All regular students aged 10–19 years who were attending secondary schools in Gondar town at the time of data collection were included.
Exclusion criteria
Adolescents who were critically ill or had mental disabilities were excluded from the study.
Sample size determination
The sample size was calculated using a single population proportion formula. This calculation was based on the assumption that the proportion of parent–adolescent communication on sexual and reproductive health issues is 50% (i.e., p = 0.5), with a 95% confidence level and a 5% margin of error.
Finally, a 10% non-response rate = 39 + 385 = 424 was considered.
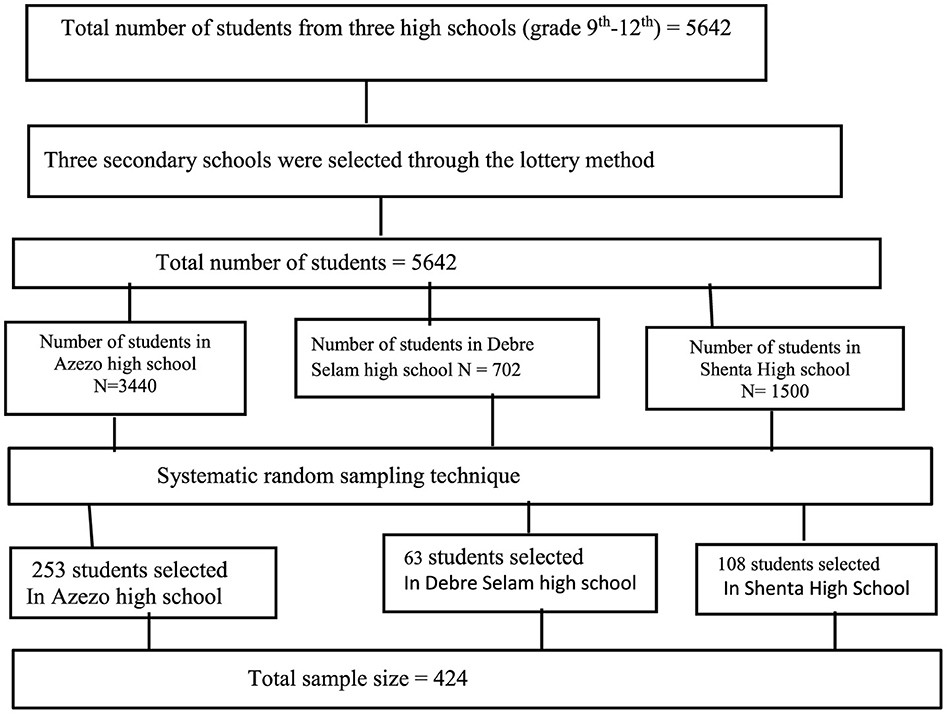
Sampling technique and procedure
This study included three public secondary schools (Arezo, Debre Selam, and Shinta). These schools were chosen using a lottery method, and proportional allocation was then applied to each school. To select students for the study, a sampling interval (k) was determined and used for sampling. This interval was calculated by dividing the total number of students in the selected schools (5,642) by the desired sample size (424), which resulted in an interval of 14. Using this sampling interval, we systematically selected every 14th student from the roster books (refer to Figure 1).
Data collection tool and quality procedures
The data were collected using a pretested, structured, interviewer-administered questionnaire. The questionnaire was initially prepared in English, then translated into the local language (Amharic), and subsequently back-translated into English by language experts to ensure consistency in word meanings. It covered sociodemographic characteristics and sexual reproductive health issues. Data collectors received 2 days of training on the study's objectives, sampling procedures, questionnaire administration, and ensuring questionnaire completeness. Confidentiality was maintained by omitting participants' names from the questionnaire.
Study variables
Dependent variables
Parent–adolescent communication (Yes/No).
The study assessed parent–adolescent communication (PAC) regarding sexual and reproductive health (SRH) issues by assessing the following components: condom use, STIs/HIV/AIDS, sexual intercourse, menstruation, unwanted pregnancy, contraception, and physical and psychological changes during puberty. If the students discussed at least two of the SRH topics with their parents/caregivers in the past 12 months, the communication was marked as “yes”. If not, it was marked as “no”. This approach has been utilized in similar studies (33, 34).
Independent variables
The independent variables included the students' grade level, number of children, attitudes and knowledge about sexual and reproductive health issues, and students' religion.
Operational definitions of the dependent and independent variables
Adolescents
All individuals in the 10–19 year age group were defined as adolescents (35).
Parents
Parents were defined as individuals who play a significant role in an adolescent's life and provide unpaid care for their work, including biological parents (mother and father), grandparents, older relatives, and other caregivers (36).
Knowledgeable about SRH
Students who scored above the mean score on the knowledge questions regarding sexual and reproductive health (SRH) were categorized as knowledgeable, while those who scored below or equal to the mean score were categorized as not knowledgeable (37, 38).
Perception of students regarding SRH
We assessed the students' perceptions of discussions on sexual and reproductive health using open-ended questions rated on a Likert scale. The perception index was established, ranging from 0 to 11, with a median score of 9. High perception was defined as scores at or above the median score, while low perception was defined as scores below the median score (39, 40).
Data processing and statistical analysis
The collected data were coded and entered into EpiData version. Subsequently, the data were analyzed using IBM SPSS Statistics version 25.0 software. Summary statistics, such as proportions and frequencies, were used to represent the results. Bivariable and multivariable logistic regressions were conducted to identify factors associated with the outcome variable. In the bivariable logistic regression, variables with a p ≤ 0.2 were included in the multivariable logistic regression model. In this model, variables significantly associated with parent–adolescent communication were identified at a p ≤ 0.05. The normality of continuous data was assessed using the Shapiro–Wilk test, and the model's fitness was evaluated using the Hosmer–Lemeshow goodness-of-fit test. The validity of the assessment tool was verified using Cronbach's alpha, which yielded a reliability coefficient of 0.75.
Ethical consideration
The study received ethical approval from the Institutional Review Board of the University of Gondar (IRB 416/2023). After the approval of the proposal, an official letter was written to the Gondar town administration to request permission and support. In addition, permission was secured from the school administration and the school parent–teacher committee. Before participation, each individual provided informed verbal consent or assent after receiving a detailed explanation of the study's purpose. The confidentiality of the information was strictly maintained.
Background profile of the study participants
In this study, 424 adolescents were included, with a 100% response rate. The mean age of the adolescents was 16 (±1.73) years. A significant portion, comprising 68.4%, were enrolled in grades 9–10. Out of the total adolescents surveyed, nearly half (48.1%) of them identified as orthodox religious followers. Furthermore, the majority (55.7%) of adolescents reported that they live with their parents or other family members (Table 1).
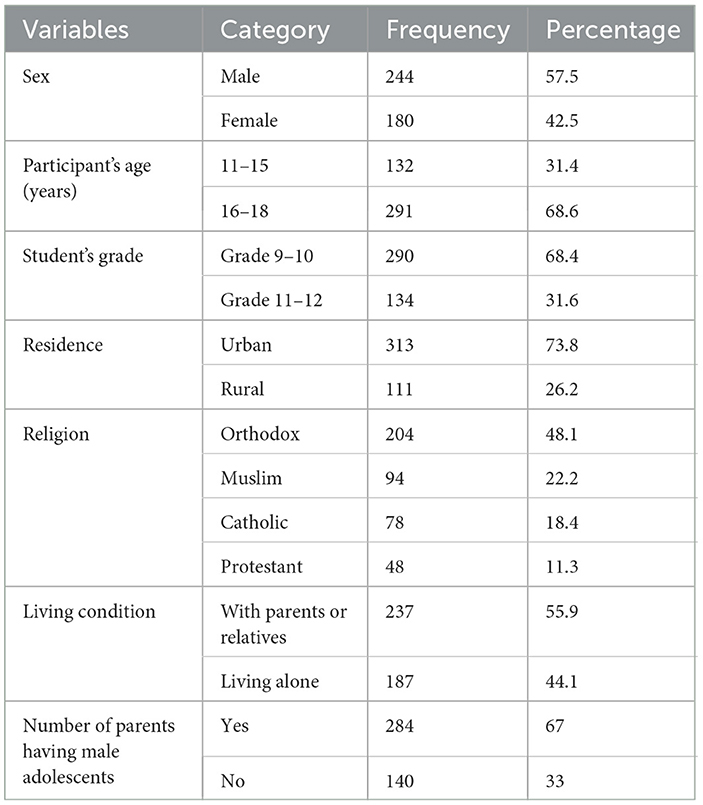
Table 1. Sociodemographic Characteristics of the study's participants in Gondar town public secondary schools, northwest Ethiopia, 2023.
Knowledge of the adolescents on sexual and reproductive health issues
Nearly 73% of the study participants correctly identified the typical onset of puberty. Among the female respondents, an impressive 89.4% accurately recognized the onset of the puberty period. More than half of the adults responded correctly regarding the development of secondary sex organs during puberty. The majority of the female respondents, 72%, responded correctly regarding the growth of sexual organs during the puberty period. Approximately two-thirds, i.e., 66%, of the adult study participants correctly acknowledged that experiencing attraction toward the opposite sex during puberty is considered normal. Among the respondents who responded correctly regarding this aspect, approximately 64% were categorized as adult adolescents. Out of all the adolescents surveyed, a significant majority of 72% was aware of the average age at which girls typically begin menstruating. It was astonishing how well-informed the majority of the female respondents were on this issue. Over two-thirds of the adults were knowledgeable about the typical duration of menstrual bleeding. Impressively, approximately 95% of the female respondents were informed about this aspect. Nearly 73% of the students were knowledgeable about contemporary contraception methods, while over 95% of the female respondents were well-informed on the subject.
The majority of the student participants (75%) were acquainted with information about safe abortion practices. Moreover, over 80% of the female respondents demonstrated familiarity with the topic of safe abortion (Table 2).
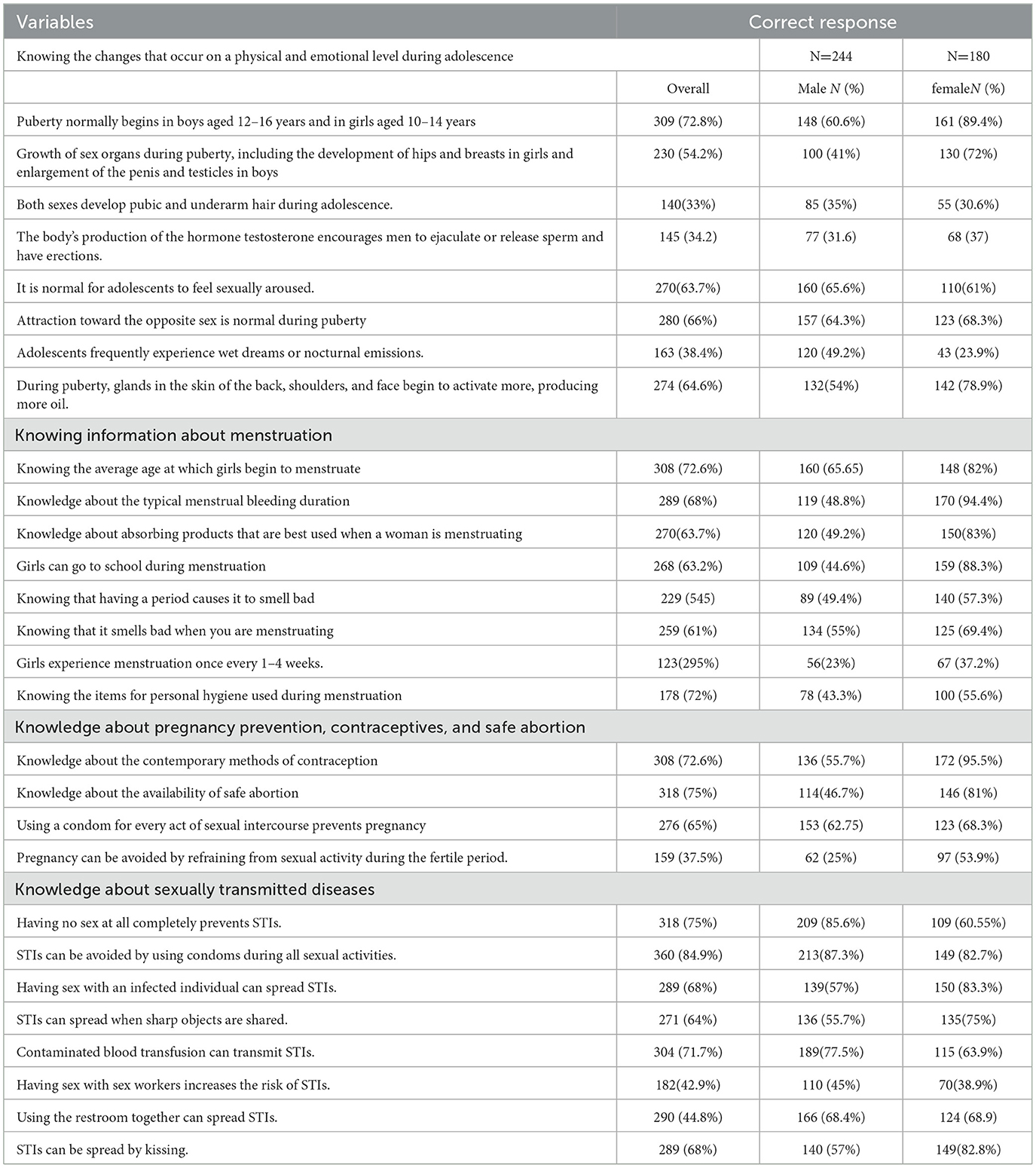
Table 2. Knowledge about sexual and reproductive health issues among the adolescent students in Gondar town government secondary schools, northwest Ethiopia, 2023.
Frequently perceived barriers by adolescents in communicating about sexual reproductive health with their parents
A significant hindrance to initiating conversations about sexual health with adolescents stems from feelings of shame or embarrassment among parents, as reported by 52.8% of them. Furthermore, adolescents face several challenges when trying to communicate with their parents about sexual and reproductive health (SRH). These obstacles include concerns about social stigma or fear of social rejection (41%), doubts regarding the accuracy of SRH information or a perceived lack of knowledge (44.6%), apprehension that openly discussing SRH issues may encourage sexual activity (46.2%), and the perception of cultural barriers (30.4%) (Table 3).
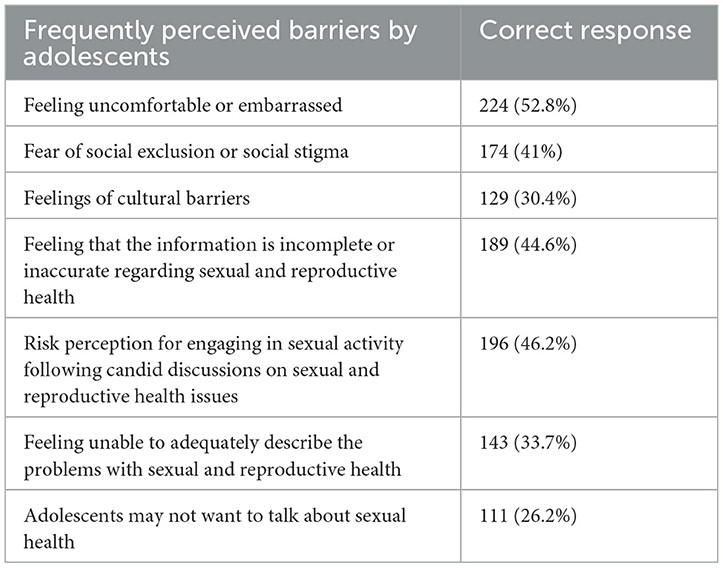
Table 3. Frequently perceived barriers by adolescents in communicating about sexual reproductive health with their parents in Gondar town government secondary schools, northwest Ethiopia, 2023.
Factors associated with parental communication regarding sexual and reproductive health with adolescents
These factors included sex, religion, student grade level, number of adolescent children, living arrangements for adolescents, students' knowledge about puberty, students' knowledge about sexual and reproductive health (SRH) issues, attitudes toward SRH, and knowledge about SRH services at health facilities. However, in the multivariable logistic regression analysis, several factors were significantly associated with parent–adolescent communication on SRH issues, with a p ≤ 0.05. These factors included sex, student grade level, living arrangements, students' knowledge about puberty, students' knowledge about SRH communication, and students' attitudes toward sexual and reproductive health (SRH). The odds of parent–adolescent communication were higher among the female adolescents compared to male adolescents (adjusted odds ratio (AOR) = 1.23; 95% confidence interval (CI): 1.09, 7.45). The students in grades 11–12 had higher odds of engaging in parent–adolescent communication on SRH compared to those in grades 9–10 (AOR = 1.25; 95% CI: 1.19–6.98).
The students who lived with their parents or caregivers had higher odds of having parent–adolescent communication compared to those who lived alone (AOR = 1.26; 95% CI: 1.07, 5.66). The students with good knowledge about puberty had higher odds of engaging in parent–adolescent communication compared to those with poor knowledge (AOR = 1.23; 95% CI: 1.04, 7.89). The students who had positive attitudes toward sexual reproductive health issues were more likely to have good parent–adolescent communication compared to those with negative attitudes (AOR = 2.4; 95% CI: 1.34–7.82). Furthermore, students with poor knowledge about sexual reproductive health issues were less likely to engage in parent–adolescent communication compared to those with good knowledge about these issues (AOR = 0.21; 95% CI: 0.13, 0.45) (Table 4).
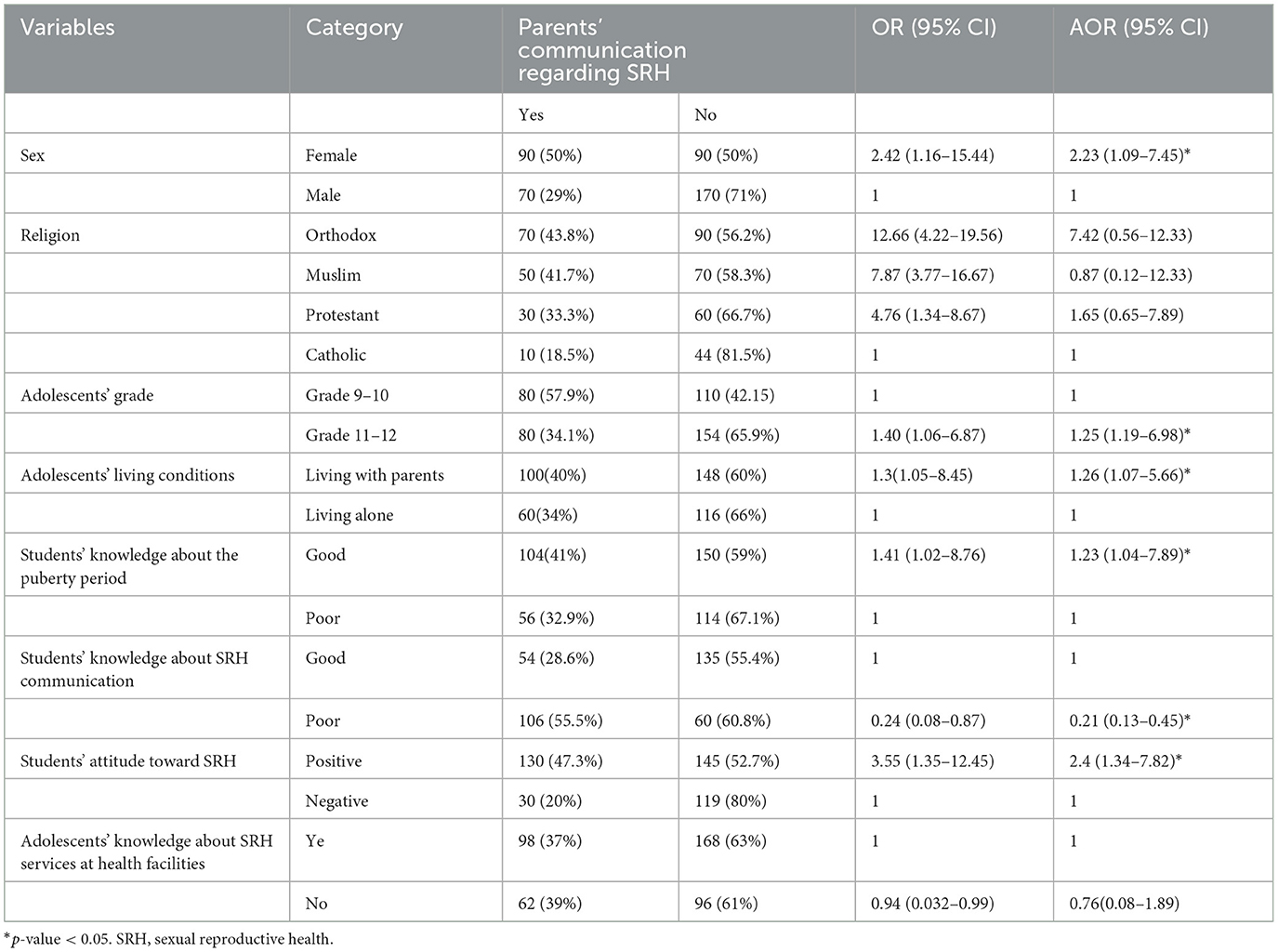
Table 4. Factors associated with parent–adolescent communication regarding SRH among secondary school students in Gondar town, northwest Ethiopia, 2023.
Discussion
Adolescents who engage in risky sexual behaviors have a risk of contracting STIs, unintended pregnancies, and delayed health care. Parent–adolescent communication on sexual and reproductive health helps mitigate these risks. This study assessed communication levels between adolescents and parents on these topics and identified associated factors among secondary school students in Gondar town, northwest Ethiopia.
This study found that 37.7% of the adolescents communicated with their parents or caregivers about sexual and reproductive health issues in the past 12 months (95% CI: 34.65–44.76) (Figure 2). This result is consistent with the results from similar investigations carried out in Debre Markos, Northwest Ethiopia (36.9%) (41), Amhara region of Ethiopia (37.5%) (42), and Nepal (40.9%) (43). However, this study's result is lower than the 56.9% reported in Central Ethiopia and Woldia Town (46), and the 56.3% in Dabat Town (46), but higher than the 21.3% found in Assela, Oromia (45). The differences in results stem from socioeconomic factors, cultural norms, and access to sexual and reproductive health (SRH) information. Socioeconomic status affects resources, such as education and healthcare, impacting parental involvement in adolescent health discussions. Cultural beliefs influence attitudes toward discussing SRH, with variations in openness across different cultures. Access to SRH information also varies by region, influencing adolescents' knowledge and comfort level in discussing these topics with parents. Regions with better SRH education tend to have more parent–adolescent communication on these issues (47, 48).
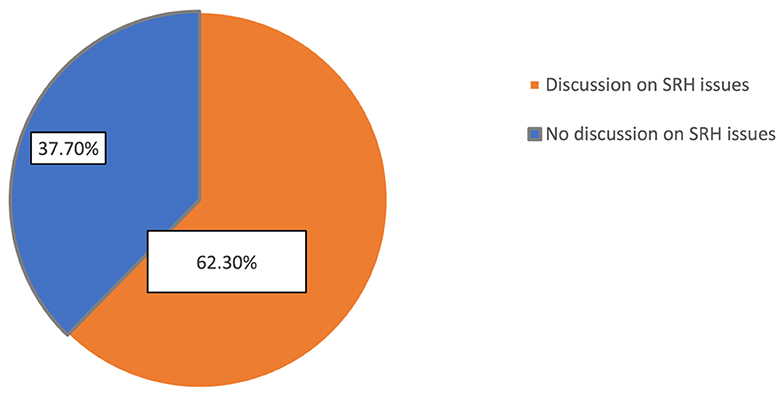
Figure 2. Distribution of parent–adolescent communication on SRH issues in Gondar town, northwest Ethiopia, 2023 (n = 424).
In this study, parent–adolescent communication was significantly associated with several factors: sex, student grade level, living arrangements, students' knowledge about puberty, their understanding of SRH communication, and their attitudes toward sexual and reproductive health (SRH). Female students tended to have higher levels of communication with their parents about SRH compared to male students, which is consistent with the findings from other studies (47, 49, 50). This might be attributed to factors such as female adolescents being generally more open to discussing sensitive topics with their parents and feeling more comfortable seeking guidance and information from their parents regarding SRH concerns (25, 50–53). Moreover, female adolescents often have more opportunities to spend time at home, which could facilitate discussions with their parents on these matters. In addition, parents or caregivers may feel more compelled to communicate with or provide guidance to their daughters regarding SRH topics as a means of preventing premarital sexual activity, unintended pregnancies, and induced abortions among female adolescents. Ultimately, effective and open parent–adolescent communication about SRH issues are equally crucial for both sexes (20, 54, 55).
It was found that the students in grades 11–12 were more likely to discuss sexual and reproductive health (SRH) issues with their parents or caregivers compared to the students in grades 9–10. This finding aligns with the results of a similar study conducted in Woreta, Ethiopia (30). This might be due to the fact that older students are generally more mature and understand the complexities of SRH issues better, which enables them to approach these topics with greater confidence. By grades 11 and 12, they typically receive a more comprehensive education on SRH, which equips them to ask informed questions and seek guidance. Furthermore, as they age, they become more open and less embarrassed about discussing personal matters, making it easier to talk about SRH (25, 42, 47, 56).
The students who lived with their parents or caregivers were more likely to engage in parent–adolescent communication compared to those who lived alone. This finding aligns with the findings from studies conducted in Debre Markos (42, 57). Living with parents or caregivers provides immediate access to familial support and guidance, which fosters regular interactions and conversations about various topics, including sexual and reproductive health (SRH). This closeness builds stronger bonds and encourages open communication, making adolescents feel more comfortable while discussing sensitive topics such as SRH. Parents or caregivers, feeling a greater sense of responsibility for their children's wellbeing, actively engage in SRH discussions to provide accurate information and guidance. Furthermore, living together allows for greater supervision and monitoring of adolescents' activities, which leads to spontaneous conversations about SRH as parents become aware of their children's concerns. Overall, the presence of parents or caregivers creates a supportive environment conducive to effective parent–adolescent communication about SRH, which promotes better-informed decision-making and healthier behaviors among adolescents (42, 57–59).
The students who had a poor understanding of sexual and reproductive health (SRH) topics were less likely to have parent–adolescent communication on these issues compared to the students with good knowledge. This finding is consistent with the findings of research conducted in Myanmar (60) and Eastern Ethiopia (34). This is because students with good knowledge about SRH topics recognize the importance of seeking guidance on potential risks and consequences associated with sexual behaviors. Their confidence in initiating conversations, coupled with parents' receptiveness to their inquiries, fosters productive dialogue within the family. Furthermore, adolescents with good SRH knowledge actively seek opportunities to discuss these topics with their parents, highlighting the value of parental guidance in making informed decisions about their sexual health. Overall, this emphasizes the critical role of education and open communication in promoting healthy behaviors among young people (43, 61, 62).
The students who had positive attitudes toward sexual reproductive health issues were significantly more likely to have good parent–adolescent communication compared to those with negative attitudes. This finding is similar to the finding of a study conducted in Asella, Ethiopia (44). This could be attributed to the willingness of adolescents to engage in open and honest discussions about sensitive topics related to sexual health. Positive attitudes may indicate a level of comfort and acceptance regarding discussing these issues, which, in turn, fosters effective communication between parents and adolescents. Furthermore, adolescents with positive attitudes may actively seek out information and support from their parents, leading to more frequent and meaningful conversations about sexual reproductive health (44, 63, 64).
Limitations of the study
The limitations of this study include recall bias and the inability to establish cause-and-effect relationships due to its cross-sectional design. Self-reporting may have been influenced by social desirability bias, especially given the sensitivity of the topic. It is also important to note that not all discussions assumed positive outcomes, as negative and harmful conversations could occur. Furthermore, the study primarily interviewed adults, overlooking valuable perspectives of adolescents that could align or diverge with parental views.
Conclusion and recommendations
This study revealed a low level of communication between parents and adolescents regarding sexual and reproductive health (SRH). Evidence-based education focusing on SRH topics, such as consent, healthy relationships, communication skills, STDs, contraception, and interpersonal dynamics, is crucial for addressing the low level of communication between parents and adolescents. Implementing peer education among senior students and training teachers in effective communication techniques can enhance parent–adolescent dialogue on SRH. Qualitative research on SRH topics and communication barriers can provide valuable insights for developing interventions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethical Review Board of University of Gondar (ref. no. 416/2023). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MM: Writing – original draft, Conceptualization. DE: Conceptualization, Investigation, Writing – original draft. TS: Writing – review & editing. YW: Conceptualization, Methodology, Writing – original draft. JA: Validation, Conceptualization, Writing – original draft. BM: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank all study participants and data collectors for their contributions to the success of this study. The authors would also like to thank the University of Gondar for providing ethical approval.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; OR, odds ratio; HIV, human immunodeficiency virus; WHO, World Health Organization; RH, reproductive health; SPSS, statistical package for social science; STIs, sexually transmitted infections; SRH, sexual and reproductive health.
References
1. Ndugga P, Kwagala B, Wandera SO, Kisaakye P, Mbonye MK, Ngabirano F. “If your mother does not teach you, the world will…”: a qualitative study of parent-adolescent communication on sexual and reproductive health issues in Border districts of eastern Uganda. BMC Public Health. (2023) 23:678. doi: 10.1186/s12889-023-15562-6
2. Maina BW, Ushie BA, Kabiru CW. Parent-child sexual and reproductive health communication among very young adolescents in Korogocho informal settlement in Nairobi, Kenya. Reprod Health. (2020) 17:1–14. doi: 10.1186/s12978-020-00938-3
3. Agbeve AS. Sexual and Reproductive Health Education among Rural Families in Ghana: A Study in Adaklu, Volta Region. Cape Coast: University of Cape Coast; 2020.
4. Jejeebhoy SJ, Zavier A, Santhya K, Singh SK, Acharya R, Gogoi A, et al. Promoting parent-Child Interaction and Communication for Healthy Development of Adolescents: Lessons from a Pilot Project in Rural Bihar. (2014).
5. Miller KS, Levin ML, Whitaker DJ, Xu X. Patterns of condom use among adolescents: the impact of mother-adolescent communication. Am J Public Health. (1998) 88:1542–4. doi: 10.2105/AJPH.88.10.1542
6. Oo YTN, Zaw KK, Than KK, Mar KK. Do parents and adolescents talk about reproductive health? Myanmar adolescents' perspective. South East Asia J Public Health. (2013) 1:40–5. doi: 10.3329/seajph.v1i1.13219
7. Robin L, Dittus P, Whitaker D, Crosby R, Ethier K, Mezoff J, et al. Behavioral interventions to reduce incidence of HIV, STD, and pregnancy among adolescents: a decade in review. J Adolesc Health. (2004) 34:3–26. doi: 10.1016/S1054-139X(03)00244-1
8. Ojebuyi BR, Fagbamigbe AF, Akinola OO. Prevalence of and factors influencing parent–child communication about HIV/AIDS, and sexual and reproductive health issues in Nigeria. Sage Open. (2019) 9:2158244019833880. doi: 10.1177/2158244019833880
9. Randall NM. Influence of HIV Attitude towards Abstinence on Peer-Led Sex Education among Adolescents in Mafeteng District, Lesotho. (2021).
10. Mekie M, Addisu D, Melkie A, Taklual W. Parent-adolescent communication on sexual and reproductive health issues and its associated factors in Ethiopia: a systematic review and meta-analysis. Ital J Pediatr. (2020) 46:1–13. doi: 10.1186/s13052-020-00921-5
11. Cottrell L, Yu S, Liu H, Deveaux L, Lunn S, Bain RM, et al. Gender-based model comparisons of maternal values, monitoring, communication, and early adolescent risk behavior. J Adolesc Health. (2007) 41:371–9. doi: 10.1016/j.jadohealth.2007.05.006
12. Terzian MA, Andrews KM, Moore KA. Preventing multiple risky behaviors among adolescents: seven strategies. Child Trends. (2011) 24:1–12.
13. Mekie M, Taklual W, Melkie A, Addisu D. Parental communication on sexual and reproductive health issues and its associated factors among preparatory school students in Debre Tabor, Northcentral Ethiopia: institution based cross-sectional study. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4644-y
14. Ayalew M, Mengistie B, Semahegn A. Adolescent-parent communication on sexual and reproductive health issues among high school students in Dire Dawa, Eastern Ethiopia: a cross sectional study. Reprod Health. (2014) 11:1–8. doi: 10.1186/1742-4755-11-77
15. World Health Organization. Health for the World's Adolescents: A Second Chance in the Second Decade. (2014). Available at: http://appswhoint/adolescent/second-decade/files/1612_MNCAH_HWA_Executive_Summarypdf (accessed September 09, 2015).
16. Moghaddam HT, Bahreini A, Abbasi MA, Fazli F, Saeidi M. Adolescence Health: the needs, problems and attention. Int J Pediatr. (2016) 4:1423–38.
17. Morris JL, Rushwan H. Adolescent sexual and reproductive health: the global challenges. Int J Gynecol Obstet. (2015) 131:S40–S2. doi: 10.1016/j.ijgo.2015.02.006
18. Dick B, Ferguson BJ. Health for the world's adolescents: a second chance in the second decade. J Adolesc Health. (2015) 56:3–6. doi: 10.1016/j.jadohealth.2014.10.260
19. Tessema GA, Laurence CO, Melaku YA, Misganaw A, Woldie SA, Hiruye A, et al. Trends and causes of maternal mortality in Ethiopia during 1990–2013: findings from the Global Burden of Diseases study 2013. BMC Public Health. (2017) 17:1–8. doi: 10.1186/s12889-017-4071-8
20. Malango NT, Hegena TY, Assefa NA. Parent–adolescent discussion on sexual and reproductive health issues and its associated factors among parents in Sawla town, Gofa zone, Ethiopia. Reprod Health. (2022) 19:108. doi: 10.1186/s12978-022-01414-w
21. World Health Organization. Regional Strategic Framework for accelerating universal access to sexual and reproductive health in the WHO South-East Asia Region 2020–2024: World Health Organization. New Delhi: Regional Office for South-East Asia. (2020).
22. Denno DM, Hoopes AJ, Chandra-Mouli V. Effective strategies to provide adolescent sexual and reproductive health services and to increase demand and community support. J Adolesc Health. (2015) 56:S22–41. doi: 10.1016/j.jadohealth.2014.09.012
23. Bishaw A, Tesfa M, Tiruneh Y, Addis A. Sexual and Reproductive Health Services Utilization and Associated Factors Among Preparatory School Students in Mecha District, Northwest Ethiopia: Cross Sectional Study. (2018).
24. Liang M, Simelane S, Fillo GF, Chalasani S, Weny K, Canelos PS, et al. The state of adolescent sexual and reproductive health. J Adolesc Health. (2019) 65:S3–S15. doi: 10.1016/j.jadohealth.2019.09.015
25. Sahay S. Coming of Age with HIV: a need for disclosure of HIV diagnosis among children. Adolesc J HIV AIDS Infect Dis. (2013) 1:1–7. doi: 10.17303/jaid.2013.103
26. Wellings K, Collumbien M, Slaymaker E, Singh S, Hodges Z, Patel D, et al. Sexual behaviour in context: a global perspective. Lancet. (2006) 368:1706–28. doi: 10.1016/S0140-6736(06)69479-8
27. Widman L, Choukas-Bradley S, Noar SM, Nesi J, Garrett K. Parent-adolescent sexual communication and adolescent safer sex behavior: a meta-analysis. JAMA Pediatr. (2016) 170:52–61. doi: 10.1001/jamapediatrics.2015.2731
28. World Health Organization. Promoting Adolescent Sexual and Reproductive Health Through Schools in Low Income Countries: An Information Brief. Geneva: World Health Organization. (2009).
29. Bankole A, Biddlecom A, Singh S, Guiella G, Zulu E. Sexual behavior, knowledge and information sources of very young adolescents in four sub-Saharan African countries. Afr J Reprod Health. (2007) 11:28–43. doi: 10.2307/25549730
30. Wudineh KG, Chekole FA, Tesfu AA. Adolescent-parent communication on sexual and reproductive health issues and associated factors among secondary school students in Woreta town, Northwest Ethiopia: an institutional based cross sectional study. Heliyon. (2021) 7:e06528. doi: 10.1016/j.heliyon.2021.e06528
31. Abdissa D, Sileshi W. Parent-young communication on sexual and reproductive health issues and its associated factors: experience of students in Agaro Town, Ethiopia. Reprod Health. (2023) 20:11. doi: 10.1186/s12978-022-01553-0
32. Belete GT, Anbesse DH, Tsegaye AT, Hussen MS. Prevalence and associated factors of myopia among high school students in Gondar town, northwest Ethiopia. Clini Optomet. (2016) 2016:11–8. doi: 10.2147/OPTO.S120485
33. Mekonen MT, Dagnew HA, Yimam TA, Yimam HN, Reta MA. Adolescent-parent communication on sexual and reproductive health issues and associated factors among high school students in Woldia town, Northeastern Ethiopia. Pan African Med J. (2018) 31:1.
34. Dagnachew Adam N, Demissie GD, Gelagay AA. Parent-adolescent communication on sexual and reproductive health issues and associated factors among preparatory and secondary school students of Dabat Town, Northwest Ethiopia. J Environm Public Health. (2020) 2020:4708091. doi: 10.1155/2020/4708091
35. World Health Organization. Regional Atlas on Adolescent and Youth 2017: Monitor the Health Status and Trend of Adolescent and Youth in Africa. (2018).
36. World Health Organization. Helping Parents in Developing Countries Improve Adolescents' Health. (2007).
37. Habte NM, Melku AT, Alemayehu MT. Parent-adolescent communication on sexual and reproductive health matters and associated factors among secondary and preparatory school students in robe town, bale zone, Southeast Ethiopia, 2017. J Public Health Int. (2019) 1:1–15. doi: 10.14302/issn.2641-4538.jphi-19-2860
38. Yadeta TA, Bedane HK, Tura AK. Factors affecting parent-adolescent discussion on reproductive health issues in Harar, Eastern Ethiopia: a cross-sectional study. J Environm Public Health. (2014) 2014:102579. doi: 10.1155/2014/102579
39. Mohan SBVR, Dhanapal S, Govindasamy V, Pillay P. Psychological impact of parent-adolescent communication: a critical analysis. Int J Public Health. (2022) 11:1210–22. doi: 10.11591/ijphs.v11i4.21461
40. Iqbal S, Zakar R, Zakar MZ, Fischer F. Perceptions of adolescents' sexual and reproductive health and rights: a cross-sectional study in Lahore District, Pakistan. BMC Int Health Hum Rights. (2017) 17:1–13. doi: 10.1186/s12914-017-0113-7
41. Kusheta S, Bancha B, Habtu Y, Helamo D, Yohannes S. Adolescent-parent communication on sexual and reproductive health issues and its factors among secondary and preparatory school students in Hadiya Zone, Southern Ethiopia: institution based cross sectional study. BMC Pediatr. (2019) 19:1–11. doi: 10.1186/s12887-018-1388-0
42. Mihretie GN, Muche Liyeh T, Ayalew Goshu Y, Gebrehana Belay H, Abe Tasew H, Belay Ayalew A. Young-parent communication on sexual and reproductive health issues among young female night students in Amhara region, Ethiopia: Community-based cross-sectional study. PLoS ONE. (2021) 16:e0253271. doi: 10.1371/journal.pone.0253271
43. Singh DR, Shrestha S, Karki K, Sunuwar DR, Khadka DB, Maharjan D, et al. Parental knowledge and communication with their adolescent on sexual and reproductive health issues in Nepal. PLoS ONE. (2023) 18:e0289116. doi: 10.1371/journal.pone.0289116
44. Bekele D, Deksisa A, Abera W, Megersa G. Parental communication on sexual and reproductive health issues to their adolescents and affecting factors at Asella town, Ethiopia: a community-based, cross-sectional study. Reprod Health. (2022) 19:114. doi: 10.1186/s12978-022-01408-8
45. Masresha SA, Alen GD, Aberra IA, Dender DK, Mamo ZA, Girma AD, et al. Parent-Adolescent Communication about Sexual and Reproductive Health and Its Association with Gender and Pre-Marital Sex Among Secondary and Preparatory School Students in Woldia Town, North East Ethiopia, 2019. (2019).
46. Aliyu TK, Aransiola JO. Parent-adolescent communication about reproductive health issues in Nigeria. SAGE Open. (2023) 13:21582440231166607. doi: 10.1177/21582440231166607
47. Wamoyi J, Fenwick A, Urassa M, Zaba B, Stones W. Parent-child communication about sexual and reproductive health in rural Tanzania: implications for young people's sexual health interventions. Reprod Health. (2010) 7:1–18. doi: 10.1186/1742-4755-7-6
48. Wakjira DB, Habedi D. Barriers to access and utilisation of sexual and reproductive health services among adolescents in Ethiopia: a sequential mixed-methods study. BMJ Open. (2022) 12:e063294. doi: 10.1136/bmjopen-2022-063294
49. Ayehu A, Kassaw T, Hailu G. Young people's parental discussion about sexual and reproductive health issues and its associated factors in Awabel woreda, Northwest Ethiopia. Reprod Health. (2016) 13:1–8. doi: 10.1186/s12978-016-0143-y
50. Fanta M, Lemma S, Sagaro GG, Meskele M. Factors associated with adolescent–parent communication of reproductive health issues among high school and preparatory students in Boditi town, Southern Ethiopia: a cross-sectional study. Patient Intell. (2016) 8:57–70. doi: 10.2147/PI.S97838
51. Thin Zaw PP, Liabsuetrakul T, McNeil E, Htay TT. Gender differences in exposure to SRH information and risky sexual debut among poor Myanmar youths. BMC Public Health. (2013) 13:1–9. doi: 10.1186/1471-2458-13-1122
52. Ouahid H, Mansouri A, Sebbani M, Nouari N, Khachay FE, Cherkaoui M, et al. Gender norms and access to sexual and reproductive health services among women in the Marrakech-Safi region of Morocco: a qualitative study. BMC Pregn Childbirth. (2023) 23:407. doi: 10.1186/s12884-023-05724-0
53. Bikila TS, Dida N, Bulto GA, Debelo BT, Temesgen K. Adolescents' communication on sexual and reproductive health matters with their parents and associated factors among secondary and preparatory school students in Ambo town, Oromia, Ethiopia. Int J Reprod Med. (2021) 2021:6697837. doi: 10.1155/2021/6697837
54. McNaughton J, Niedzwiecki C. Gender differences in parent child communication patterns. J Undergrad Res. (2000) 3:25–32.
55. Noller P, Bagi S. Parent—adolescent communication. J Adolesc. (1985) 8:125–44. doi: 10.1016/S0140-1971(85)80042-7
56. Fantahun M. Assessing Communication on Sexual and Reproductive Health Issues among High School Students with their Parents, Bullen Woreda Benishangul Gumuz Region North West Ethiopia. Addis Ababa: Addis Ababa University. (2016).
57. Shiferaw K, Getahun F, Asres G. Assessment of adolescents' communication on sexual and reproductive health matters with parents and associated factors among secondary and preparatory schools' students in Debremarkos town, North West Ethiopia. Reprod Health. (2014) 11:1–10. doi: 10.1186/1742-4755-11-2
58. Sleshi S, Alemu AA, Dagnew Z, Aynalem BY. Parent-adolescent discussion about reproductive health issues and associated factors among parents in Debre Markos town, Northwest, Ethiopia: a cross-sectional study. Pan African Med J. (2022) 41:32447. doi: 10.11604/pamj.2022.41.266.32447
59. Feyissa M, Nigussie T, Mamo Y, Aferu T. Adolescent girl–mother communication on sexual and reproductive health issues among students in Fiche Town, Oromia, Central Ethiopia. J Prim Care Community Health. (2020) 11:2150132720940511. doi: 10.1177/2150132720940511
60. Noe MTN, Saw YM, Soe PP, Khaing M, Saw TN, Hamajima N, et al. Barriers between mothers and their adolescent daughters with regards to sexual and reproductive health communication in Taunggyi Township, Myanmar: what factors play important roles? PLoS ONE. (2018) 13:e0208849. doi: 10.1371/journal.pone.0208849
61. Bhatta BR, Kiriya J, Shibanuma A, Jimba M. Parent–adolescent communication on sexual and reproductive health and the utilization of adolescent-friendly health services in Kailali, Nepal. PLoS ONE. (2021) 16:e0246917. doi: 10.1371/journal.pone.0246917
62. Muhwezi WW, Katahoire AR, Banura C, Mugooda H, Kwesiga D, Bastien S, et al. Perceptions and experiences of adolescents, parents and school administrators regarding adolescent-parent communication on sexual and reproductive health issues in urban and rural Uganda. Reprod Health. (2015) 12:1–16. doi: 10.1186/s12978-015-0099-3
63. Eshete A, Shewasinad S. Adolescent-parent communication on sexual and reproductive health issues in Ethiopia: a systematic review and meta-analysis. Ethiop J Health Sci. (2020) 30:817–28. doi: 10.4314/ejhs.v30i5.22
64. Mihretie GN, Goshu YA, Belay HG, Tassew HA, Ayalew AB, Beshah MH, et al. Sexual and reproductive health issues and associated factors among female night school students in Amhara Region, Ethiopia: an institution-based cross-sectional study. BMJ Open. (2023) 13:e066244. doi: 10.1136/bmjopen-2022-066244
Keywords: parent–adolescent communication, sexual and reproductive health issues, students, secondary schools, Ethiopia
Citation: Melese M, Esubalew D, Siyoum TM, Worku YB, Azanaw J and Mengistie BA (2024) Parent–adolescent communication on sexual and reproductive health issues and associated factors among secondary public-school students in Gondar town, northwest Ethiopia: an institution based cross-sectional study. Front. Public Health 12:1342027. doi: 10.3389/fpubh.2024.1342027
Received: 25 November 2023; Accepted: 31 July 2024;
Published: 19 August 2024.
Edited by:
Sultan Hussen Hebo, Arba Minch University, EthiopiaReviewed by:
Niguss Cherie, Wollo University, EthiopiaSemere Gebremariam, Kotebe University of Education, Ethiopia
Copyright © 2024 Melese, Esubalew, Siyoum, Worku, Azanaw and Mengistie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mihret Melese, bWloaHJldDg2QGdtYWlsLmNvbQ==
 Mihret Melese
Mihret Melese Dereje Esubalew
Dereje Esubalew Tsehayu Melak Siyoum
Tsehayu Melak Siyoum Yilkal Belete Worku
Yilkal Belete Worku Jember Azanaw
Jember Azanaw Berihun Agegn Mengistie
Berihun Agegn Mengistie