Abstract
Objectives:
This article studied the single-factor causal relationships between the social environment, health cognition, and health behavior of the individuals with non-fixed employment and their adverse health outcomes, as well as the complex causal relationships of multiple factors on these outcomes.
Methods:
Partial Least Squares Structural Equation Modeling (PLS-SEM) and Fuzzy-Set Qualitative Comparative Analysis (fsQCA) are employed. Data is collected from the results of an open questionnaire Psychology and Behavior Investigation of Chinese Residents 2021.
Results:
PLS-SEM analysis reveals that health risk behaviors and cognition play a mediating role in impact of the social environment on adverse health outcomes, indicating that individuals with non-fixed employment susceptible to adverse health outcomes. fsQCA analysis identifies that weak social support is a core condition leading to outcomes of depression and anxiety. There are shared configurations and causal pathways between the outcomes of physical health and depression.
Conclusion:
The study supports the social determinants theory of health and suggests that the fundamental reason for people being trapped in adverse health outcomes is the health inequality caused by social stratification, and the external shock of uncertainty in the era of VUCA (Volatility, Uncertainty, Complexity, and Ambiguity).
Introduction
In a VUCA world, the population without fixed employment has been on the rise. The abbreviation “VUCA” stands for Volatility, Uncertainty, Complexity, and Ambiguity. This term originated in the military context of the United States in the 1990s, addressing the characteristics of the post-Cold War era, particularly in dealing with actions against terrorist organizations, which were perceived as more complex and uncertain than ever before. After the outbreak of the COVID-19 pandemic in 2020, instances of complexity and uncertainty have become more frequent, making the VUCA era a new normal (1). It is often expressed as “The only certainty is uncertainty in the external environment” and “Change is the only constant.” VUCA (Volatility, Uncertainty, Complexity, and Ambiguity) era has gained increased attention following the outbreak of the COVID-19 pandemic (2–4). Uncertainty is one of the defining characteristics of the VUCA era, prominently exemplified by measures of curbing the COVID-19 pandemic leading to rising unemployment rates (5) and potential long-term “scarring effects” on the labor market. As relief policies have been gradually phased out, more individuals face the looming threat of joblessness (6). In April 2022, survey data from 31 major cities in China indicated an urban unemployment rate of 6.7%, surpassing the highest point during the first wave of the pandemic in 2020 (5.9% in May 2020) (7). However, the unemployed population represents just the tip of the iceberg in terms of the labor market shocks in the VUCA era, with a more profound impact on those without fixed employment. The term “non-fixed employment” refers to the working-age population that have no stable jobs, including the jobless, unemployed, and underemployed (excluding students) (8). This group falls at the tenth stratum of contemporary Chinese society (9), characterized by a lack of organizational, economic, and cultural capital (10). Unemployment has become a common phenomenon and source of stress during economic crises. The status of having no fixed occupation not only affects individuals’ physical health (11) but also contributes to negative health behaviors such as smoking, heavy drinking (12), and poor mental health (13). Consequently, individuals without fixed employment often experience adverse health outcomes, exhibiting worse health conditions compared to the general population (14).
On 5 May 2023, the World Health Organization declared the “Public Health Emergency of International Concern” caused by the COVID-19 pandemic to be over (15). However, the VUCA era persists, and the population without fixed employment continues to grow, with adverse health outcomes remaining prevalent. Therefore, our study aims to investigate the influencing factors and underlying mechanisms of adverse health outcomes among individuals without fixed employment. This research endeavors to provide guidance and recommendations for proactively addressing health risks in the VUCA era.
Literature review and hypotheses
Literature review
Unemployment can have a profound impact on an individual’s physical health, mental health and other aspects of life. Firstly, there is a widespread agreement among academics that unemployment negatively affects an individual’s physical health. Compared to those in regular employment, unemployed people are at a higher risk of developing arthritis (16), committing suicide, and dying from other diseases (all illnesses excluding cancer and cardiovascular diseases) (17). Secondly, it is a common view among scholars that depression is a prevalent consequence of the mental health impact of unemployment (18). The longer the period of unemployment, the higher the chance of suffering from major depressive disorder (19). Lastly, numerous scholars also suggest that unemployment can lead to poor dietary habits (20) and increased alcohol consumption (21). Moreover, individuals with mental and physical health issues are at a higher risk of unemployment (22, 23). It is evident that unemployment can comprehensively affect an individual’s health status and can easily create a vicious cycle of mutual influence.
With the advancement of research, scholars have increasingly concentrated on the impact of unemployment on health. To this end, the academic community has primarily developed three representative viewpoints. The first is the perspective of lacking social support, which means that unemployment leads to reduced levels of social support and a decline in mental health (24). The second is the perspective of social exclusion, suggesting that unemployment often leads to social exclusion (25) and consequently a worsened psychosocial environment and health status (26). The third is the perspective of lack of health opportunities, arguing that unemployment results in fewer opportunities for medical care (27) and social resources (28), thereby impacting health levels. In essence, unemployment leads to a decrease in an individual’s socioeconomic status of an individual, which is then accompanied by a reduction in social support, health opportunities, and a lack of various resources, ultimately affecting the health of unemployed people.
How to mitigate the negative impact of unemployment on health. From a macro perspective, governments can issue unemployment allowances (29), social security, and welfare policies (30). However, some scholars have pointed out that the amount of unemployment relief is too low to significantly reduce men’s economic stress (31). And at the same time, differences in economic level and social resources can also lead to differences in health outcomes for unemployed people after receiving unemployment allowances (32). From a meso perspective, family and social support are very important for maintaining mental health during unemployment (33). Information, economic level or emotional support (34), strong social capital (the number of close friends) (35) helps to mitigate the negative impact of unemployment on health. In addition, there are also a few studies from a micro perspective that believe individual emotional intelligence (36) and leisure activities (37) can mitigate the negative impact of stress related to unemployment on mental health.
Based on the literature review, we believe that there are three research gaps. First, scientifically comprehensive measurement was conducted on adverse health outcomes as the dependent variable. Previous research has mainly focused on single dimensions of physiological health or mental health, lacking comprehensive measurement and explanation. This study integrated commonly used measures in the academic field, including the Chinese version of the European Quality of Life-5 Dimensions-5 Levels (EQ-5D-5 L), the Patient Health Questionnaire-9 (PHQ-9) for depression screening, and the Generalized Anxiety Disorder-7 (GAD-7) scale, to comprehensively measure physiological and mental health indicators, providing a scientific and comprehensive assessment of adverse health outcomes among individuals with non-fixed employment. Second, this study comprehensively considered both individual traits and external environment of individuals with non-fixed employment. Previous studies mainly focused on individual traits while neglecting the influence of the external environment. Given the externality of health outcomes, exploring their influencing factors requires consideration not only of individual traits but also of the external environment, including family environment and social environment. Third, this study utilized the advantages of quantitative research methods and qualitative comparative analysis. Previous studies primarily utilized quantitative methods to explore the influencing factors. They also explored linear relationships between influencing factors and adverse health outcomes among individuals with non-fixed employment. However, they failed to reveal the multiple causal relationships among numerous influencing factors and adverse health outcomes. This study integrates PLS-SEM and fsQCA, which not only explains the interactions between various influencing factors of individuals with non-fixed employment and adverse health outcomes but also reveals the multiple causal relationships among numerous influencing factors and adverse health outcomes.
Hypotheses
Adverse health outcomes are primarily influenced by social support and family health. Social support may have indirect effects on health through enhanced mental health, or by reducing the impact of stress (38). Individuals with no social ties or very few social ties exhibit the most pronounced risk of poor health (39). Repeated experience of unemployment results in fewer social support for workers, thereby posing stress on their health (40). Additionally, social network is one of the key determinants of heath and deteriorating social networks constitute a major adverse consequence of unemployment (41). Furthermore, family plays a crucial role in affecting health directly, while intimate friends and family members can promote individual’s well-being (42). To this end, we propose the following hypotheses:
Hypothesis 1: Social environment has a negative impact on adverse health outcomes.
Hypothesis 1-1: Social support has a negative impact on adverse health outcomes.
Hypothesis 1-2: Family health has a negative impact on adverse health outcomes.
Individuals without fixed employment often possess lower health literacy (43). Due to their disadvantaged social environment, individuals with non-fixed employment struggle to obtain and understand accurate, high-quality health information (44). Therefore, we propose the following hypotheses:
Hypothesis 2: The social environment has a positive impact on health cognition.
Hypothesis 2-1: Social support has a positive impact on health cognition.
Hypothesis 2-2: Family health has a positive impact on health cognition.
Social support has been shown to be associated with various health behaviors and outcomes. Socioeconomic resources shape health outcomes by influencing health risk behaviors, access to healthcare, and exposure to stressful life events (45, 46). Unstable employment status is often accompanied by poorer self-rated health, health behaviors, and mental health (47). Meanwhile, social connections can influence health behavior habits, and emotional support provided by social relationships can enhance psychological well-being, thereby reducing unhealthy behaviors and health risks (38). Additionally, family members within the same family system exhibit similar lifestyle habits and norms, which can mutually influence each other (48). Therefore, we propose the following hypotheses:
Hypothesis 3: Social environment has a negative impact on health risk behaviors.
Hypothesis 3-1: Social support has a negative impact on health risk behaviors.
Hypothesis 3-2: Family health has a negative impact on health risk behaviors.
There exists a close association between the level of health literacy and health outcomes. Health literacy is a key determinant of health (49), and it has been suggested that persons with low health literacy suffer from poorer overall health (50). Moreover, one of the population groups with a particularly high risk for low health literacy is unemployed persons (51). According to Bandura’s Social Cognitive Theory, a lack of social support may exacerbate adverse health behaviors and conditions among individuals with low health literacy (52), and higher health literacy is conducive to improving adverse health outcomes (53). Therefore, we propose the following hypothesis:
Hypothesis 4: Health cognition has a negative impact on adverse health outcomes.
Adverse health outcomes are largely related to health risk behaviors. Smoking, heavy alcohol drinking, unhealthy diet, and lack of physical exercise are the main causes of adverse health outcomes (15). Individuals with low socioeconomic status, in relative deprivation, are more susceptible to unemployment (54). Unemployment, as a stress-inducing life event, exerts serious negative effects on an individual’s health and health behaviors (55). Smoking, excessive alcohol consumption, and binge eating are coping mechanisms against stress (56), contributing to the poor health status of long-term unemployed individuals (57). Therefore, we propose the following hypothesis:
Hypothesis 5: Health risk behaviors have a positive impact on adverse health outcomes.
Health literacy has a widespread influence on individual health outcomes. An individual’s health literacy directly determines oneself health behaviors (58). Individuals with lower health literacy may experience a higher the risk of medical errors due to misunderstandings of medical information (59). Since employment status directly affects personal income, healthcare accessibility, and social status, low health literacy among individuals with non-fixed employment can have a negative impact on their health (60). Therefore, we propose the following hypothesis:
Hypothesis 6: Health cognition mediates the impact of the social environment on adverse health outcomes.
Hypothesis 6-1: Health cognition mediates the impact of social support on adverse health outcomes.
Hypothesis 6-2: Health cognition mediates the impact of family health on adverse health outcomes.
Hypothesis 7: Health risk behaviors mediate the impact of the social environment on adverse health outcomes.
Hypothesis 7-1: Health risk behaviors mediate the impact of social support on adverse health outcomes.
Hypothesis 7-2: Health risk behaviors mediate the impact of family health on adverse health outcomes.
Based on this, we construct a model for the formation mechanism of adverse health outcomes among the non-fixed employment population, as shown in Figure 1.
Figure 1
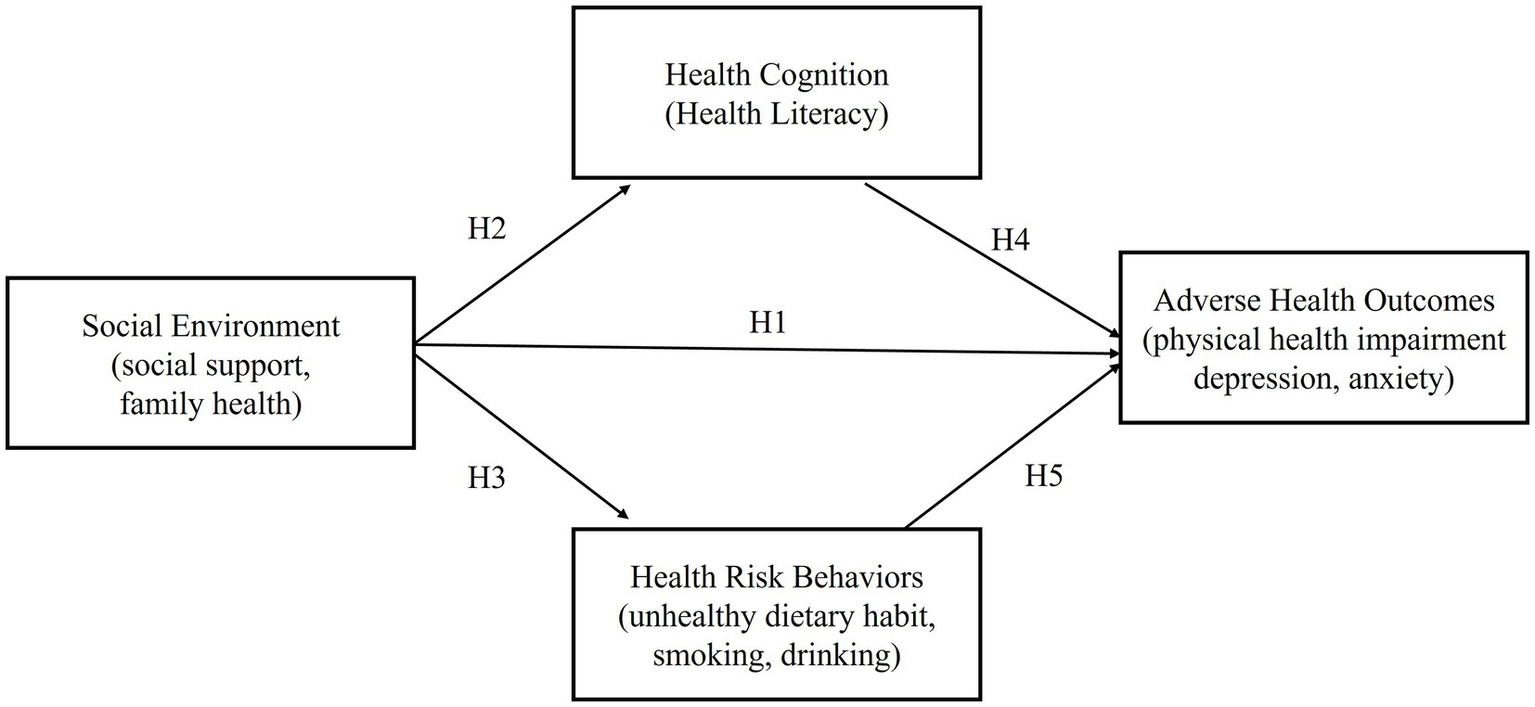
Research model.
Materials and methods
Research design
Based on the results from the open questionnaire Psychology and Behavior Investigation of Chinese Residents 2021 (PBICR-2021), the formation mechanisms of adverse health outcomes among individuals with Non-Fixed Employment were explored using PLS-SEM and fsQCA methods.
Data source
The research data is derived from the PBICR-2021, which includes all provinces, autonomous regions, and municipalities directly under the central government. A total of 120 cities were selected using random number tables from non-provincial capital cities in each province and autonomous region. The population of each city was stratified by gender, age, and urban–rural distribution. Sample sizes for each stratum were determined based on the population characteristics from the results of the 2021 Seventh National Population Census. Surveyors conducted convenient sampling while meeting quota requirements (61), and obtained approval from the Biomedical Ethics Committee of Peking University (JNUKY-2021-018). The sample number of individuals with non-fixed employment is 2,195, including 953 males (43.4%) and 1,242 females (56.6%). The age distribution is as follows: 10 individuals aged 18 and below (0.5%), 302 individuals aged 19–30 (13.8%), 404 individuals aged 31–40 (18.4%), 732 individuals aged 41–50 (33.3%), and 747 individuals aged 51 and above (34.0%). In terms of education, 1,937 individuals had an associate degree or below (88.2%), 223 had a bachelor’s degree (10.2%), 20 had a master’s degree (0.9%), and 15 had a doctorate or higher (0.7%). Regarding monthly income, 455 individuals earned 1,500 yuan or less (20.7%), 1,089 earned between 1,501 and 4,500 yuan (49.6%), 399 earned between 4,501 and 7,500 yuan (18.2%), 156 earned between 7,501 and 10,500 yuan (7.1%), and 95 earned 10,501 yuan or more (4.4%). The urban population consists of 1,094 individuals (49.8%), while the rural population consists of 1,101 individuals (50.2%).
Variable measurement
Dependent variables and its measurement
Adverse health outcomes
This section covers three dimensions: physical health impairment, depression, and anxiety. Physical health impairment is assessed using the Chinese version of EQ-5D-5L developed by Luo et al. (62). This scale measures an individual’s health-related quality of life and consists of 5 items. Each item is rated on a Likert five-point scale, ranging from “no problems” (1 point) to “extreme problems” (5 points). Scores are then converted using a utility value scoring system specifically designed for the Chinese population. Depression is measured using the Patient Health Questionnaire-9 (PHQ-9) developed by Kroenke et al. (63). This self-report tool is designed to screen for and assess the severity of depression symptoms based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria published by the American Psychiatric Association. It consists of 9 items, each rated on a Likert four-point scale, with responses such as “not at all “, “several days,” “more than half the days,” and “nearly every day,” corresponding to scores of 0, 1, 2, and 3, respectively. A representative statement is that “Feeling down, depressed, or hopeless about everything?” Anxiety is assessed using the Generalized Anxiety Disorder-7 (GAD-7) scale developed by Spitzer et al. (64). This scale is suitable for screening generalized anxiety disorder and assessing symptom severity. It consists of 7 items, each rated on a Likert four-point scale, with responses similar to the PHQ-9. Scores range from 0 for “not at all” to 3 for “nearly every day.” A typical statement is “Feeling nervous, anxious, or on edge?”
Independent variables and its measurement
Social environment
It includes two dimensions: social support and family health. Social support is measured using the Perceived Social Support Scale (PSSS) introduced by Blumenthal (65) and developed by Zimet and the Chinese version translated by Jiang Qianjin is adopted in this research (66). The scale measures the extent of an individual’s social support, which includes three dimensions: family support, friend support, and other support, with a total of 12 items. Each item uses a Likert seven-point rating scale, ranging from “strongly disagree” (1 point) to “strongly agree” (7 points). An example statement is that “I can get emotional help and support from my family when I need it.” Family health is measured using the Family Health Scale-Short Form (FHS-SF) developed by Crandall et al. (67). The scale measures family health function with a total of 10 items. Each item uses a Likert five-point rating scale, ranging from “strongly disagree” (1 point) to “strongly agree” (5 points). An example statement is that “In my family, we support each other.”
Health cognition
This involves a single dimension, health literacy, and is measured using the Health Literacy Scale-Short Form12 (HLS-SF12) developed by Van Duong et al. (68). The scale measures an individual’s level of health literacy, including three dimensions: medical health, disease prevention, and health promotion. Each dimension involves four items related to mastery, understanding, judgment, and application, resulting in a total of 12 items. Each item uses a Likert four-point rating scale, ranging from “very difficult” (1 point) to “very easy” (4 points). Standardization is performed using the formula index score = (mean − 1) × (50/3). A representative statement is that “Find treatment information for your diseases.”
Health risk behaviors
This includes three dimensions: unhealthy dietary habits, smoking, and drinking. Unhealthy dietary habits are measured using the Eating Behavior Scale (EB) developed by Tayama et al. (69). The scale assesses an individual’s eating behavior with a total of 7 items. Each item uses a Likert four-point rating scale, ranging from “strongly disagree” (1 point) to “strongly agree” (4 points), with higher scores indicating worse eating behavior. A representative statement is that “I have no regular eating time.” Smoking and drinking are single-item measures, with scoring based on the number of cigarettes smoked and the frequency of drinking set by Xia Delong et al. (70). Smoking is scored as follows: never smoking = 1, 1–5 cigarettes = 2, 6–10 cigarettes = 3, 11–20 cigarettes = 4, more than 20 cigarettes = 5. A higher score indicates more smoking. Drinking frequency is scored as follows: 0 times = 1, an average of 1–2 times per week = 2, an average of 3–4 times per week = 3, almost every day = 4. A higher score indicates higher drinking frequency. Self-rated health is one of the most common measurements of global health in social science and public health research and has been demonstrated to have high validity (71).
Control variables
The study selects gender, age, education level, per capita monthly income, and place of residence as control variables.
Research method selection
Partial least squares structural equation modeling
Hair et al. (72) argued that partial least squares structural equation modeling (PLS-SEM) is more suitable for complex models due to its stronger predictive capabilities compared to covariance-based SEM. It is also suitable for exploring or extending theoretical models. Therefore, SPSS 26.0 and SmartPLS 4 were used for statistical analysis of the data. This involved four steps. First, the Harman’s one-factor test was used to check for common method bias (73). Second, following Hair et al.’s (72) rules-of-thumb for reflective measurement models assessment, the internal consistency reliability (Cronbach’s alpha, Composite Reliability), convergent validity (Outer Loadings, AVE), and discriminant validity (cross-loadings, HTMT, Fornell-Larcker criterion) of the measurement model were assessed. Third, based on Hair’s rules-of-thumb (72) for evaluating structural models, assessments were made regarding multicollinearity among predictor variables, the significance of path coefficients using bootstrap method, the determination coefficient R2 of endogenous latent variables, the relative contribution of exogenous constructs to the determination coefficient of endogenous latent variables (effect size f2), predictive relevance (Stone-Geisser Q2), and model fit indices (SRMR). Fourth, Baron and Kenny (74)‘s four-step approach was referred to test the significance of mediating effect, and further, the Bootstrapping method using SmartPLS software was conducted to generate 5,000 iterations to estimate confidence intervals of mediating effect.
Fuzzy-set qualitative comparative analysis
PLS-SEM has limitations in explaining complex interaction effects, especially those involving three or more influencing factors (75). Qualitative Comparative Analysis (QCA) offers a suitable means to accommodate complex complementarity and nonlinear relationships among variables (75, 76). QCA takes research cases as configurations of conditions or attributes (77). Fuzzy-set qualitative comparative analysis (fsQCA) allows for a more detailed exploration of the possible configurations that lead to specific outcomes and is advantageous for in-depth discovery of conditions that contribute to the occurrence of results (78). This method involves four steps. First, data calibration. Second, construction of truth table. Third, necessity analysis. Fourth, configuration analysis. Therefore, social support, family health, health literacy, unhealthy eating behavior, smoking, and drinking are selected as antecedent conditions of adverse health outcomes among individuals without fixed employment, so as to further elucidate the mechanism behind adverse health outcomes in this population group.
PLS-SEM results
Common method bias
To test for common method bias, the Harman one-factor test was employed. All items from the measurement scales used in this study were subjected to factor analysis. Through principal component analysis, the variance contribution rate of first unrotated factor was found to be 28.875%, which is less than 50% (79). This indicates the absence of significant common method bias.
Measurement model assessment
Measurement model consists of reflective measurement model and formative measurement model, and the one employed in the study is reflective measurement model. The internal consistency of the models is presented in Table 1. The Cronbach’s alpha coefficients for all measurement variables are greater than 0.7, and all the Composite Reliability (CR) values are higher than 0.7 (with a minimum value of 0.794), indicating strong internal consistency of the measurement model. Convergent validity is shown in Table 1, the outer loadings of each measurement model were greater than 0.7, and the Average Variance Extracted (AVE) values were all above 0.5 (with a minimum value of 0.564), indicating good convergent validity of the measurement models.
Table 1
| Cronbach’s alpha | CR | AVE | |
|---|---|---|---|
| Family support | 0.952 | 0.950 | 0.658 |
| Social support | 0.938 | 0.958 | 0.656 |
| Social environment | 0.953 | 0.873 | 0.774 |
| Health cognition | 0.930 | 0.940 | 0.568 |
| Health risk behaviors | 0.854 | 0.794 | 0.564 |
| Adverse health outcomes | 0.944 | 0.852 | 0.658 |
Reliability and validity.
Discriminant validity (cross loadings, HTMT, Fornell-Larcker criterion) was also evaluated. First, the evaluation standard for cross loadings of factors of each measurement model is that an indicator’s external loading on its own construct should be higher than its cross loadings with all the other constructs. In this study, all indicators effectively distinguished their respective constructs. Second, as shown in Table 2, the criterion for Heterotrait-Monotrait Ratio (HTMT) states that the HTMT values between constructs should not exceed 0.85, and the confidence intervals for HTMT statistics should not include 1. Finally, as indicated in Table 3, discriminant validity was tested using the Fornell-Larcker criterion (80). Upon comparison, the square root of AVE values for each variable are higher than the correlation coefficients between variables. The results demonstrated good discriminant validity among the variables in this study.
Table 2
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Adverse health outcomes | |||||
| 2. Health cognition | 0.470 | ||||
| 3. Health risk behaviors | 0.563 | 0.642 | |||
| 4. Family health | 0.428 | 0.313 | 0.269 | ||
| 5. Social support | 0.487 | 0.368 | 0.364 | 0.582 |
HTMT-based discriminant validity evaluation.
Table 3
| Mean | Std. Deviation | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. Social support | 57.983 | 12.570 | 0.811 | |||||
| 2. Family health | 36.862 | 8.150 | 0.550** | 0.810 | ||||
| 3. Social environment | 94.845 | 18.363 | - | - | 0.880 | |||
| 4. Health cognition | 34.579 | 6.154 | 0.345** | 0.291** | 0.365** | 0.753 | ||
| 5. Health Risk behaviors | 1.697 | 0.538 | −0.277** | −0.200** | −0.278** | −0.493** | 0.751 | |
| 6. Adverse health outcomes | 17.277 | 10.434 | −0.414** | −0.363** | −0.445** | −0.376** | 0.341** | 0.811 |
Relevant analysis and Fornell-Larcker criterion.
**The square root of AVE value is higher than the correlation coefficients between variables.
Structural model evaluation
Based on the research hypotheses, two mediation models were constructed. Model 1 employed social environment as the independent variable, with health cognition and health risk behavior as the mediating variables, and adverse health outcomes as the dependent variable, creating a dual-path mediation model (as depicted in Figure 2). To separately investigate the effects of social support, the subdimensions of social environment, and family health on adverse health outcomes, Model 2 was constructed. In this model, social support and family health served as independent variables, while health cognition and health risk behavior acted as mediating variables, and adverse health outcomes remained the dependent variable, creating a dual-path mediation model (as shown in Figure 3). The results of the model tests are presented in Table 4.
Figure 2
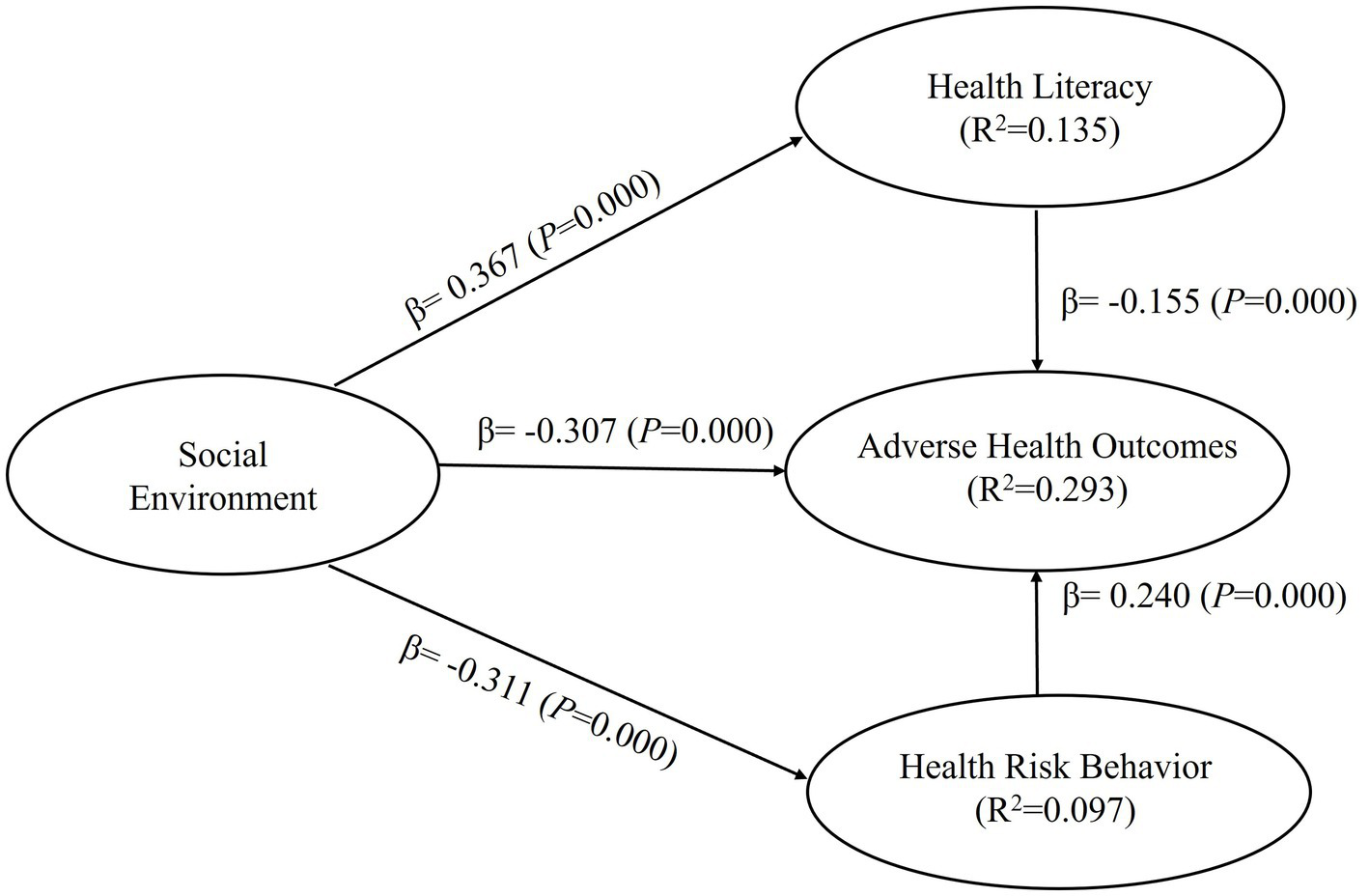
Results of structural model 1.
Figure 3
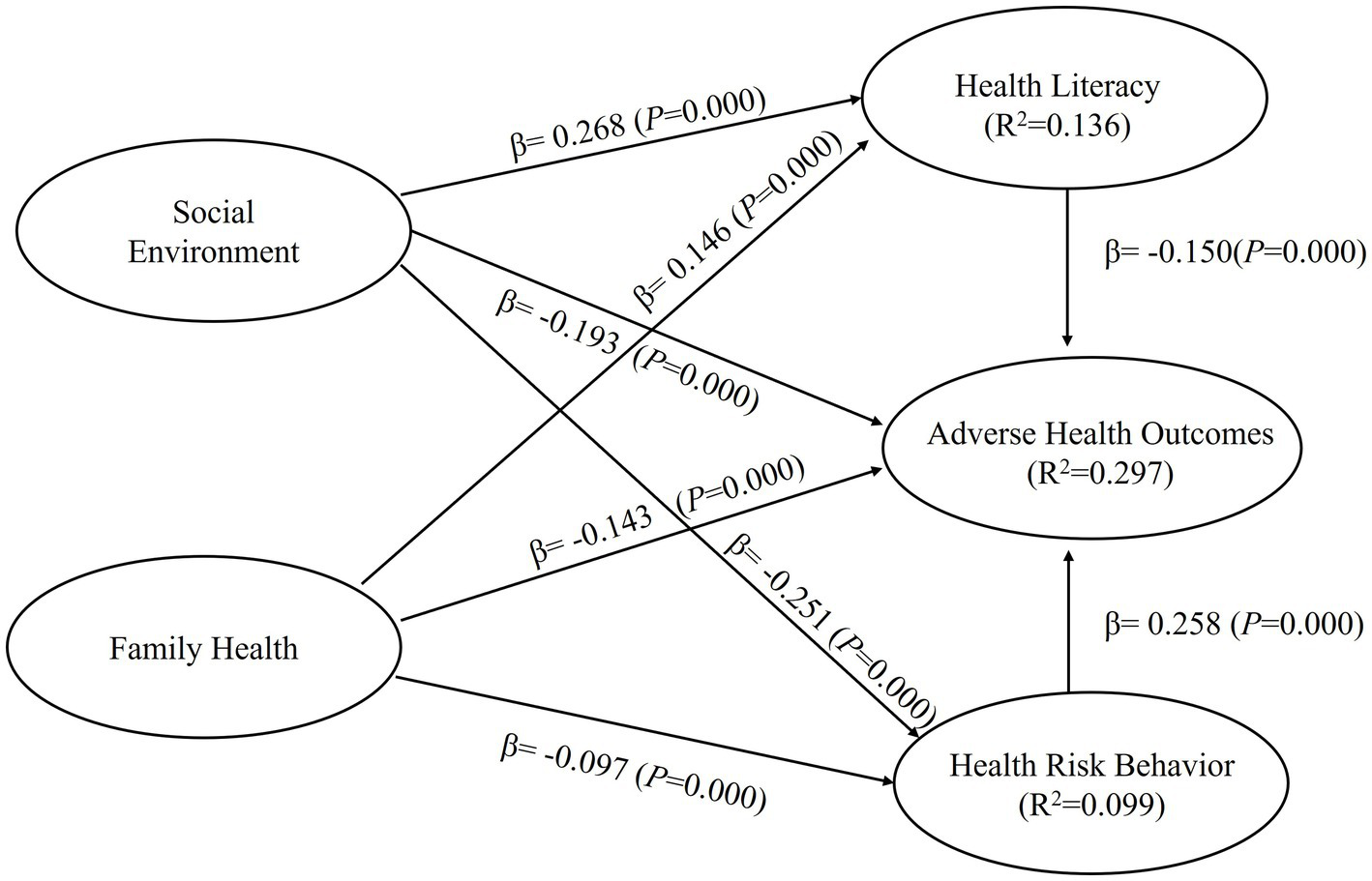
Results of structural model 2.
Table 4
| Hypotheses | Std. estimate | S.E. | t | P | f2 | VIF | Decision | |
|---|---|---|---|---|---|---|---|---|
| Mediation Model 1 | ||||||||
| H1 | Social environment → Adverse health outcomes | −0.307 | 0.029 | 10.586 | 0.000 | 0.112 | 1.184 | Support |
| H2 | Social environment → Health cognition | 0.367 | 0.024 | 15.017 | 0.000 | 0.156 | 1.000 | Support |
| H3 | Social environment → Health risk behaviors | −0.311 | 0.020 | 15.557 | 0.000 | 0.107 | 1.000 | Support |
| H4 | Health cognition → Adverse health outcomes | −0.155 | 0.028 | 5.549 | 0.000 | 0.024 | 1.440 | Support |
| H5 | Health risk behaviors → Adverse health outcomes | 0.240 | 0.027 | 8.810 | 0.000 | 0.059 | 1.379 | Support |
| Mediation Model 2 | ||||||||
| H1-1 | Social support → Adverse health outcomes | −0.193 | 0.030 | 6.539 | 0.000 | 0.034 | 1.545 | Support |
| H1-2 | Family health → Adverse health outcomes | −0.143 | 0.026 | 5.602 | 0.000 | 0.020 | 1.465 | Support |
| H2-1 | Social support → Health cognition | 0.268 | 0.026 | 10.297 | 0.000 | 0.058 | 1.438 | Support |
| H2-2 | Family health → Health cognition | 0.146 | 0.025 | 5.837 | 0.000 | 0.017 | 1.465 | Support |
| H3-1 | Social support → Health risk behaviors | −0.251 | 0.025 | 10.142 | 0.000 | 0.049 | 1.438 | Support |
| H3-2 | Family health → Health risk behaviors | −0.097 | 0.026 | 3.655 | 0.000 | 0.007 | 1.438 | Support |
Results of model tests.
First, in Model 1, the maximum Variance Inflation Factor (VIF) value for all predictor variables was 1.440. In Model 2, the maximum VIF value for all predictor variables was 1.545. Both values were less than 5, indicating no significant multicollinearity among the constructs.
Second, after applying the Bootstrapping method and performing 5,000 resamples to the mediation models, the analysis results of Model 1 showed that social environment had a significant negative effect on adverse health outcomes (β = −0.307, 95% CI = [−0.361, −0.248]), supporting Hypothesis H1. Social environment also had a significant positive effect on health cognition (β = 0.367, 95% CI = [0.317, 0.414]) and a significant negative effect on health risk behavior (β = −0.311, 95% CI = [−0.350, −0.271]), supporting Hypotheses H2 and H3, respectively. Health cognition had a significant negative effect on adverse health outcomes (β = −0.155, 95% CI = [−0.208, −0.097]), supporting Hypothesis H4, and health risk behavior had a significant positive effect on adverse health outcomes (β = 0.240, 95% CI = [0.187, 0.294]), supporting Hypothesis H5. In Model 2, the analysis results showed that social support had a significant negative effect on adverse health outcomes (β = −0.193, 95% CI = [−0.248, −0.132]), supporting Hypothesis H1-1. Family health also had a significant negative effect on adverse health outcomes (β = −0.143, 95% CI = [−0.193, −0.091]), supporting Hypothesis H1-2. Social support had a significant positive effect on health cognition (β = 0.268, 95% CI = [0.215, 0.316]), supporting Hypothesis H2-1, and family health had a significant positive effect on health cognition (β = 0.146, 95% CI = [0.098, 0.196]), supporting Hypothesis H2-2. Social support had a significant negative effect on health risk behavior (β = −0.251, 95% CI = [−0.297, −0.199]), supporting Hypothesis H3-1, and family health had a significant negative effect on health risk behavior (β = −0.097, 95% CI = [−0.149, −0.045]), supporting Hypothesis H3-2. Health cognition had a significant negative effect on adverse health outcomes, and health risk behavior had a significant positive effect on adverse health outcomes, confirming Hypotheses H4 and H5, respectively.
Third, the coefficient of determination (R2) is a measure of the model’s predictive ability. It is calculated by squaring the correlation between the actual values and predicted values of specific endogenous structures, indicating the overall impact of exogenous latent variables on endogenous latent variables. In Model 1, the R2 values for health cognition, health risk behavior, and adverse health outcomes of the endogenous latent variables were 0.135, 0.097, and 0.293, respectively. In Model 2, the R2 values for health cognition, health risk behavior, and adverse health outcomes of the endogenous latent variables were 0.136, 0.099, and 0.297, respectively. According to rules of thumb, R2 values of 0.75, 0.50, or 0.25 of the endogenous latent variables represent strong, moderate, or weak effects, respectively.
Fourth, the effect size ƒ2 measures the change in R2 when specific exogenous constructs are omitted from the model, providing an assessment of whether the omitted exogenous constructs have a substantial impact on the endogenous constructs. In Model 1, the ƒ2 for each path ranged from 0.024 to 0.156, while in Model 2, the ƒ2 for each path ranged from 0.007 to 0.058. The guidelines for evaluating ƒ2 suggest that values of 0.02, 0.15, and 0.35 represent small, medium, and large effects of exogenous latent variables, respectively, with values less than 0.02 indicating no effect.
Fifth, the Stone-Geisser Q2 for predictive relevance is obtained by using the blindfolding procedure on a specified omission distance D. Blindfolding is a sample re-use technique, which omits every D-th data point in the indicators of endogenous constructs, and estimates parameters by using the remaining data points. The omitted data represent missing values and are treated accordingly (e.g., by pairwise deletion or mean value replacement). The results then are used to predict the omitted data points. The difference between the omitted data points and the predicted ones is used to calculate the Q2 value. In Model 1, the Stone-Geisser Q2 values for social environment, health cognition, health risk behavior, and adverse health outcomes were 0.302, 0.487, 0.167, and 0.317, respectively. In Model 2, the Stone-Geisser Q2 values for social support, family health, health cognition, health risk behavior, and adverse health outcomes were 0.567, 0.584, 0.485, 0.154, and 0.243, respectively. A Q2 value larger than zero for a certain endogenous latent variable indicates the model has predictive relevance for the construct, while values at or below 0 indicate a lack of predictive relevance.
Sixth, PLS-SEM is based on the variance-based structural equation modeling (VB-SEM) principles. As a variance-based algorithm, it aims to maximize the explanatory power of endogenous variables. It differs from covariance-based SEM (CB-SEM), which is based on the covariance matrix and seeks to make the covariance matrix of samples as close as possible to the expected covariance matrix of the model, minimizing the residuals (squared differences). Consequently, global fit indices used in CB-SEM are not suitable for PLS-SEM. Henseler et al. (81) have suggested the SRMR (Standardized Root Mean Square Residual) as fit indices, with standards of less than 0.08 (ideal) or 0.12 (acceptable). In Model 1, the SRMR was 0.110, while in Model 2, the SRMR was 0.066.
Mediation effects assessment
For the mediation effects of health cognition and health risk behavior in the relationships between the social environment and its dimensions (family health and social support) and adverse health outcomes, the Bootstrapping method was conducted (5,000 resamples), and the results are presented in Table 5.
Table 5
| Hypothesis | Std. estimate | S.E. | Percentile Bootstrap | Decision | ||
|---|---|---|---|---|---|---|
| 95%LCI | 95%UCI | |||||
| Mediation Model 1 (Social environment → Adverse health outcomes) | ||||||
| Total effect | −0.438 | 0.026 | −0.486 | −0.384 | ||
| Direct effect | −0.307 | 0.029 | −0.361 | −0.248 | ||
| Total indirect effect | −0.131 | 0.011 | −0.154 | −0.111 | ||
| H6 | Social environment → Health cognition → Adverse health outcomes | −0.057 | 0.011 | 0.011 | −0.036 | Support |
| H7 | Social environment →Health risk behaviors→ Adverse health outcomes | −0.074 | 0.009 | 0.009 | −0.058 | Support |
| Mediation Model 2 (Social Support/Family health→ Adverse health outcomes) | ||||||
| Social support→ adverse health outcomes | ||||||
| Total effect | −0.298 | 0.026 | −0.353 | −0.251 | ||
| Direct effect | −0.193 | 0.027 | −0.254 | −0.148 | ||
| Total indirect effect | −0.105 | 0.011 | −0.124 | −0.081 | ||
| H6-1 | Social support → Health cognition → Adverse health outcomes | −0.040 | 0.009 | −0.058 | −0.024 | Support |
| H7-1 | Social support → Health risk behaviors → Adverse health outcomes | −0.065 | 0.010 | −0.087 | −0.047 | Support |
| Family health→ Adverse health outcomes | ||||||
| Total effect | −0.190 | 0.026 | −0.243 | −0.142 | ||
| Direct effect | −0.143 | 0.024 | −0.193 | −0.099 | ||
| Total indirect effect | −0.047 | 0.009 | −0.064 | −0.029 | ||
| H6-2 | Family health →Health cognition → Adverse health outcomes | −0.022 | 0.006 | −0.033 | −0.012 | Support |
| H7-2 | Family health → Health risk behavior s → Adverse health outcomes | −0.025 | 0.007 | −0.041 | −0.012 | Support |
Mediation effects assessment.
Regarding the mediating effect of health cognition on the relationship between the social environment and adverse health outcomes, the 95% confidence interval was [−0.079, −0.036] with the Bootstrapping method. Since this confidence interval does not include zero, it indicates a significant mediating effect of health cognition between the social environment and adverse health outcomes. The standardized effect size was −0.057, supporting the hypothesis H6. Similarly, for the mediating effect of health risk behavior on the relationship between the social environment and adverse health outcomes, the Bootstrapping method yielded a 95% confidence interval of [−0.093, −0.058], with a β value of −0.074, supporting hypothesis H7.
Concerning the mediating effects of health cognition and health risk behavior on the relationships between social support, family health, and adverse health outcomes, the results are as follows. Health cognition mediates the relationship between social support and adverse health outcomes, with a 95% confidence interval of [−0.058, −0.024] and a β value of −0.040, supporting hypothesis H6-1. Health cognition also mediates the relationship between family health and adverse health outcomes, with a 95% confidence interval of [−0.033, −0.012] and a β value of −0.022, supporting hypothesis H6-2. Health risk behavior mediates the relationship between social support and adverse health outcomes, with a 95% confidence interval of [−0.087, −0.047] and a β value of −0.065, supporting hypothesis H7-1. Health risk behavior mediates the relationship between family health and adverse health outcomes, with a 95% confidence interval of [−0.041, −0.012] and a β value of −0.025, supporting hypothesis H7-2.
fsQCA results
Data calibration
The variables involved in the study were calibrated. Based on the scoring rules, the degrees of related antecedent conditions are defined as follows. No depression (0–4 points) was assigned a value of 1; mild depression (5–9 points) was assigned a value of 2; moderate depression (10–14 points) was assigned a value of 3; moderately severe depression (15–19 points) was assigned a value of 4; severe depression (20 points and above) was assigned a value of 5. No anxiety (0–4 points) was assigned a value of 1; mild anxiety (5–9 points) was assigned a value of 2; moderate anxiety (10–14 points) was assigned a value of 3; severe anxiety (15 points and above) was assigned a value of 4. Low social support status (12–36 points) was assigned a value of 1; moderate social support status (37–60 points) was assigned a value of 2; high social support status (61–84 points) was assigned a value of 3. Poor family health condition (<6 points) was assigned a value of 1; moderate family health condition (6–8 points) was assigned a value of 2; good family health condition (9 or 10 points) was assigned a value of 3. Additionally, the degree of physical health impairment, health literacy level, and unhealthy eating behavior were calibrated based on Ragin’s criteria of 5% (Fully Out), 95% (Fully In), and the crossover point of 50% (82). Furthermore, smoking and drinking were assigned as binary variables (0 for non-smoking and non-drinking, 1 for smoking and drinking). Specific details are provided in the tables.
Construction of truth table and necessity analysis
Following Ragin’s approach, the algorithm function of truth table in the fsQCA software was used to compute the truth table with a result variable of 1 and no contradictory configurations. Necessity analysis was performed for individual antecedent conditions. Consistency and coverage are indicators of confirmed causal relationships in QCA analysis. Table 6 shows that the consistency and coverage of the antecedent conditions did not reach 0.9 or higher, which suggests that the occurrence of adverse health outcomes (physical health impairment, depression, anxiety) cannot be determined and explained by individual antecedent conditions alone. It is necessary to conduct configuration analysis of antecedent conditions.
Table 6
| Conditions | Physical health impairment | Conditions | Depression | Conditions | Anxiety | |||
|---|---|---|---|---|---|---|---|---|
| Consistency | Coverage | Consistency | Coverage | Consistency | Coverage | |||
| PS | 0.768 | 0.852 | PS | 0.851 | 0.285 | PS | 0.829 | 0.396 |
| FH | 0.561 | 0.854 | FH | 0.528 | 0.243 | FH | 0.485 | 0.318 |
| HL | 0.698 | 0.894 | HL | 0.728 | 0.282 | HL | 0.704 | 0.389 |
| EB | 0.510 | 0.766 | EB | 0.843 | 0.383 | EB | 0.803 | 0.520 |
| SM | 0.135 | 0.563 | SM | 0.216 | 0.273 | SM | 0.213 | 0.384 |
| DW | 0.280 | 0.602 | DW | 0.427 | 0.278 | DW | 0.421 | 0.390 |
| ~PS | 0.384 | 0.829 | ~PS | 0.729 | 0.475 | ~PS | 0.708 | 0.658 |
| ~FH | 0.535 | 0.755 | ~FH | 0.800 | 0.341 | ~FH | 0.798 | 0.485 |
| ~HL | 0.457 | 0.781 | ~HL | 0.829 | 0.429 | ~HL | 0.740 | 0.545 |
| ~EB | 0.628 | 0.897 | ~EB | 0.664 | 0.287 | ~EB | 0.600 | 0.370 |
| ~SM | 0.865 | 0.768 | ~SM | 0.784 | 0.210 | ~SM | 0.787 | 0.301 |
| ~DW | 0.720 | 0.799 | ~DW | 0.573 | 0.192 | ~DW | 0.579 | 0.277 |
Results of necessity analysis of adverse health outcomes.
The above information is compiled by the authors based on the calculation results of fsQCA software. PS, Social Support; FH, Family Health; HL, Family Literacy; EB, Unhealthy Eating Behaviors; SM, Smoking; DW, Drinking.
Configuration analysis
In the configuration analysis, three types of solutions are reported: complex solutions, intermediate solutions, and parsimonious solutions (83). Many studies tend to favor intermediate solutions because they are closer to theoretical reality without becoming overly complex (84). Therefore, we will analyze the intermediate solutions for each of the adverse health outcomes: physical health impairment, depression, and anxiety.
Configuration and causal explanatory pathways for physical health impairment outcome
The configuration analysis results for individuals without a fixed occupation experiencing physical health impairment include 10 configurations of intermediate solution, as shown in Table 7. Social support, health literacy, unhealthy eating behavior, drinking, and smoking simultaneously appear in both parsimonious and intermediate solutions, representing core conditions for physical health impairment. The remaining conditions only appear in intermediate solutions but not in parsimonious solutions, indicating that they are peripheral conditions for physical health impairment. Through Boolean minimization, the pathway can be expressed as PS*~FH*~HL*~EB*~SM*~DW*. This pathway indicates that even if individuals have strong social support, infrequent unhealthy eating behavior, do not smoke or drink, they will still experience physical health impairment if their family health level is low, and they have low health literacy, and no fixed occupation.
Table 7
| Antecedent conditions | Configurations | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| EQ1 | EQ2 | EQ3 | EQ4 | EQ5 | EQ6 | EQ7 | EQ8 | EQ9 | EQ10 | |
| Social support PS |

|
— | — | — |

|

|

|
— | — | — |
| Family health FH | — | — | ⊗ | ⊗ | — |

|

|
— | ⊗ | ⊗ |
| Family literacy HL | — |

|
— | — | ⊗ | — | — | ⊗ | — | ⊗ |
| Unhealthy eating behaviors EB | — | — | ⊗ | ⊗ | ⊗ | — | ⊗ |

|
— | — |
| Smoking SM | ⊗ | ⊗ | — | ⊗ | — | — | — |

|
⊗ | — |
| Drinking DW | — | — | ⊗ | — | — | ⊗ | — | ⊗ | ⊗ | ⊗ |
| Original coverage | 0.672 | 0.624 | 0.250 | 0.300 | 0.326 | 0.374 | 0.394 | 0.018 | 0.342 | 0.196 |
| Only coverage | 0.037 | 0.042 | 0.002 | 0.004 | 0.011 | 0.001 | 0.002 | 0.001 | 0.034 | 0.000 |
| Consistency | 0.880 | 0.910 | 0.919 | 0.910 | 0.925 | 0.927 | 0.938 | 0.748 | 0.832 | 0.871 |
| Overall consistency | 0.862 | |||||||||
| Overall coverage | 0.840 | |||||||||
Configurations of antecedent conditions for physical health impairment.
a.  or
or  represents the presence of this condition in the configuration, ⊗ or ⊗ represents the absence of this condition, —Indicates that this condition is optional; b.
represents the presence of this condition in the configuration, ⊗ or ⊗ represents the absence of this condition, —Indicates that this condition is optional; b.  or ⊗ represents core conditions,
or ⊗ represents core conditions,  or ⊗ represents auxiliary conditions. EQ, EuroQol Five Dimensions Questionnaire.
or ⊗ represents auxiliary conditions. EQ, EuroQol Five Dimensions Questionnaire.
Configuration and causal explanatory pathways for depression outcome
The configuration analysis results for individuals without a fixed occupation experiencing depression include 10 intermediate solution configurations, as shown in Table 8. The configuration analysis results for depression are consistent with those for physical health impairment, suggesting the possibility of shared causal pathways for both physical and mental adverse health outcomes in individuals with non-fixed employment. However, in the configuration for depression, the condition of social support appears in both parsimonious and intermediate solutions, indicating that it is a core condition for depression. The other conditions only appear in intermediate solutions but not in parsimonious solutions, suggesting that they are peripheral conditions for depression. After Boolean minimization, the pathway can be expressed as PS*~FH*~HL*~EB*~SM*~DW*. This pathway indicates that even if individuals have strong social support, infrequent unhealthy eating behavior, do not smoke or drink, they will still experience depression if their family health level is low, and they have low health literacy, and no fixed occupation. This causal pathway is consistent with that of physical health impairment.
Table 8
| Antecedent conditions | Configurations | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PH1 | PH2 | PH3 | PH4 | PH5 | PH6 | PH7 | PH 8 | PH 9 | PH 10 | |
| Social support PS |

|
— | — | — |

|

|

|
— | — | — |
| Family health FH | — | — | ⊗ | ⊗ | — |

|

|
— | ⊗ | ⊗ |
| Family literacy HL | — |

|
— | — | ⊗ | — | — | ⊗ | — | ⊗ |
| Unhealthy eating behaviors EB | — | — | ⊗ | ⊗ | ⊗ | — | ⊗ |

|
— | — |
| Smoking SM | ⊗ | ⊗ | — | ⊗ | — | — | — |

|
⊗ | — |
| Drinking DW | — | — | ⊗ | — | — | ⊗ | — | ⊗ | ⊗ | ⊗ |
| Original coverage | 0.676 | 0.614 | 0.339 | 0.451 | 0.567 | 0.312 | 0.415 | 0.039 | 0.419 | 0.377 |
| Only coverage | 0.035 | 0.010 | 0.000 | 0.006 | 0.025 | 0.001 | 0.001 | 0.001 | 0.014 | 0.000 |
| Consistency | 0.268 | 0.271 | 0.377 | 0.414 | 0.487 | 0.235 | 0.299 | 0.499 | 0.308 | 0.508 |
| Overall consistency | 0.865 | |||||||||
| Overall coverage | 0.255 | |||||||||
Configurations of antecedent conditions for depression.
a.  or
or  represents the presence of this condition in the configuration, ⊗ or ⊗ represents the absence of this condition, —Indicates that this condition is optional; b.
represents the presence of this condition in the configuration, ⊗ or ⊗ represents the absence of this condition, —Indicates that this condition is optional; b.  or ⊗ represents core conditions,
or ⊗ represents core conditions,  or ⊗ represents auxiliary conditions. PH, Patient Health Questionnaire.
or ⊗ represents auxiliary conditions. PH, Patient Health Questionnaire.
Configuration and causal explanatory pathways for anxiety outcome
The configuration analysis results for individuals without a fixed occupation experiencing anxiety include two intermediate solution configurations, as shown in Table 9. Social support, family health, and health literacy simultaneously appear in both parsimonious and intermediate solutions, representing core conditions for anxiety. The remaining conditions only appear in intermediate solutions but not in parsimonious solutions, indicating that they are peripheral conditions for anxiety. After Boolean minimization, the pathway can be expressed as ~PS*~HL*EB. This pathway suggests that weak social support, low health literacy, and high-frequency unhealthy eating behavior will lead to anxiety outcomes in individuals without a fixed occupation.
Table 9
| Antecedent conditions | Configurations | |
|---|---|---|
| GA1 | GA2 | |
| Social support PS | ⊗ | ⊗ |
| Family health FH | ⊗ |

|
| Family literacy HL | ⊗ | ⊗ |
| Unhealthy eating behaviors EB | — |

|
| Smoking SM | ⊗ |

|
| Drinking DW |

|
⊗ |
| Original coverage | 0.132 | 0.014 |
| Only coverage | 0.132 | 0.014 |
| Consistency | 0.796 | 0.831 |
| Overall consistency | 0.799 | |
| Overall coverage | 0.146 | |
Configurations of antecedent conditions for anxiety.
a.  or
or  represents the presence of this condition in the configuration, ⊗ or ⊗ represents the absence of this condition, —Indicates that this condition is optional; b.
represents the presence of this condition in the configuration, ⊗ or ⊗ represents the absence of this condition, —Indicates that this condition is optional; b.  or ⊗ represents core conditions,
or ⊗ represents core conditions,  or ⊗ represents auxiliary conditions. GA, Generalized anxiety.
or ⊗ represents auxiliary conditions. GA, Generalized anxiety.
Discussion
Challenges for individuals with non-fixed employment in escaping external environmental control
Social factors play a crucial role in determining health outcomes, and an individual’s health status is closely linked to their social environment. Our study has demonstrated that the social environment has a significant negative impact, to the extent of 0.307%, on adverse health outcomes, with social support contributing negatively by 0.193% and family health by 0.143%. Furthermore, weak social support (~PS) has been identified as a core factor leading to depression and anxiety, as evidenced in configurations GA1 and GA2. This finding provides new evidence that aligns, to some extent, with Amartya Sen’s Capability Approach. The health outcomes of individuals with unstable employment depend on external social and family environment, while the external social and family environment also have considerable influence on their health outcomes. This aligns with the viewpoint put forth by Amartya Sen (85), who believes that health is a critical human “capability” that is often shaped by the social networks and social capital one possesses. Michael Marmot (86) has also asserted that the root cause of health inequalities lies in social inequality, with social determinants being the “causes of the causes” of health inequalities. When viewed from a family perspective, family not only significantly influences an individual’s health status over their entire lifespan but also impacts the health of multiple generations within the family (87). Therefore, individuals with non-fixed employment find it challenging to break free from external environmental control, and improving both the social and family environments is crucial for avoiding adverse health outcomes.
Challenges for individuals with non-fixed employment in enhancing personal health cognition
Health cognition plays a pivotal role in influencing health outcomes, as an individual’s level of health literacy may determine their health outcomes. Our research has revealed that health cognition has a negative impact, to the extent of 0.155%, on adverse health outcomes. Meanwhile, low level of health literacy (~HL) has been identified as a core factor leading to anxiety, as confirmed in configurations GA1 and GA2. Moreover, low level of health literacy (~HL) also appears in the causal pathways of physical health impairment and depression, as reflected in configurations PH5, PH8, PH10, EQ5, EQ8, and EQ10. This finding, to a certain extent, supports the health communication theory. Health literacy is a direct manifestation of health cognition and can positively alter adverse health outcomes. However, individuals with unstable employment often face challenges in obtaining health education due to unfavorable living environments and limited access to social networks, resulting in lower health literacy (88). Therefore, it is crucial to focus on and improve the health literacy of individuals with unstable employment, provide health education, and disseminate health information to help them avoid adverse health outcomes.
Challenges for individuals with non-fixed employment in changing health behaviors
Health behaviors have a significant impact on health outcomes, as the choices individuals make regarding their health behaviors can directly influence their health outcomes. Our research has confirmed that health risk behaviors have a substantial positive impact, amounting to 0.240%, on adverse health outcomes. Additionally, poor eating habits have been identified in the causal pathways leading to anxiety. Furthermore, unhealthy dietary habits, smoking, and alcohol consumption appear in configurations EQ8, PH8, GA1, and GA 2, respectively. This finding provides new evidence that aligns with health behavior theory. Health behavior theory mainly explores the health-related consequences of health behaviors and influencing factors. It also holds that differences in health status among individuals are mainly attributed to variations in health behaviors (89). Smoking, drinking, and other unhealthy behaviors not only lead to adverse health outcomes but also significantly increase mortality rates (90). Moreover, the link between health behaviors and health outcomes is influenced by behavioral motivation (91), and behavioral motivation, along with health behaviors themselves, exhibits stability over time (92). Therefore, individuals with unstable employment face challenges in changing their health behaviors within a short period. It is crucial to focus on the health behaviors of individuals with non-fixed employment and improve their lifestyle habits to help them avoid adverse health outcomes.
Challenge for individuals with non-fixed employment in escaping the trap of adverse health outcomes
Individuals with non-fixed employment often find themselves in unfavorable social environment, leading to lower levels of health cognition, ultimately resulting in adverse health outcomes. Our research has confirmed that health cognition plays a mediating role of −0.057% in the influence of the social environment on adverse health outcomes. Specifically, health cognition has a mediating effect of −0.040% of social support on adverse health outcomes and −0.022% of family health on adverse health outcomes. As the shared configurations and causal pathways for both physical health impairment and depression outcomes shown in the fsQCA analysis, adverse physical and mental health outcomes among unstable employment populations result from the combined effects of multiple antecedent conditions, and these adverse health outcomes may have relations with each other. This, to a certain extent, provides new evidence for social cognitive theory. We have extended and refined this theory by focusing on adverse health outcomes as a more realistic and theoretically valuable dependent variable.
Individuals with non-fixed employment, due to their exposure to harsher social environment, tend to engage in health risk behaviors, further resulting in adverse health outcomes. Our research has confirmed that health risk behaviors play a mediating role of −0.074% in the impact of the social environment on adverse health outcomes. Specifically, health risk behaviors mediate −0.065% of the effect of the social environment on adverse health outcomes and −0.025% of the effect of family health on adverse health outcomes. From the perspective of social determinants theory, an individual’s social structure determines their life opportunities and socialization experiences, which, in turn, influence their life choices. Life opportunities and choices develop into habits through interactions, ultimately manifesting as behaviors related to healthy lifestyles (93). Therefore, it can be argued that social class or socioeconomic status is the fundamental determinant of health disparities, including health behaviors.
Going deeper, similar to the concept of the health-poverty trap, unstable employment populations may become ensnared in an adverse health outcome-social environment trap, potentially linked to the solidification of social stratification. The mechanisms of adverse health outcome-social environment trap are prominently characterized by a positive feedback loop: exposure to increasingly adverse social environments heightens the likelihood of adverse health outcomes, which, in turn, increase the probability of further exposure to even more adverse social environments. With the diminishing occurrence of “rags to riches” narratives (93), Chinese social structures have gradually solidified and social mobility has been decreased (94), resulting in a formidable “class divide” (95). Scholars like Stephens et al. (96) contend that social class is an ideal standard, behavioral norm, and social system shaped by society and history. Individual characteristics and social environmental characteristics can influence health behaviors and health outcomes by activating the cultural systems within social class. Therefore, individuals within the lowest strata of Chinese society face formidable challenges in breaking free from the adverse health outcome trap, much akin to their struggle to escape poverty traps or traverse social class boundaries.
Conclusion
In the backdrop of the VUCA era, individuals with non-fixed employment in China face various uncertainties that make it challenging to avoid adverse health outcomes. However, this challenge is not a particular case in China but rather a critical research topic globally. Utilizing data from the Psychology and Behavior Investigation of Chinese Residents 2021 (PBICR-2021) and employing the PLS-SEM and fsQCA methods, we have explored the mediating mechanisms and complex configurations of the social environment, health cognition, and health behavior concerning adverse health outcomes among the unstable employment populations in China. Based on the PLS-SEM analysis, we made the following key findings. Social environment negatively influences adverse health outcomes, indicating that individuals in unstable employment have difficulty escaping external environmental control. Social environment has a positive impact on health cognition, making it difficult for the group improving health cognition. Social environment negatively affects health risk behaviors, and individuals in unstable employment struggle to change their behavioral habits. Furthermore, health risk behaviors and health cognition mediate the influence of the social environment on adverse health outcomes, underscoring the difficulty for unstable employment populations in breaking free from the adverse health outcome trap. In the fsQCA analysis, we found that adverse health outcomes among unstable employment populations result from multiple antecedent conditions in complex configurations. No single variable is sufficient to adequately explain their causal relationships. Weak social support emerges as a core condition leading to depression and anxiety outcomes, which are also attributed to multiple factors. Additionally, there are shared configurations and causal pathways between physical health impairment and depression outcomes, suggesting potential interconnections among multiple adverse health outcomes. Overall, our research aligns with the tenets of the social determinants of health theory, emphasizing that the fundamental cause of the entrenched adverse health outcomes among China’s unstable employment populations is health inequality stemming from class stratification as well as the uncertainties shock of external factors in the era of VUCA.
Theoretically, our research enriches and expands the viewpoints of the health social determinants theory, demonstrating the mechanism of adverse health outcomes among the individuals with Non-Fixed Employment, and constructs a theoretical model that is fully explanatory both in terms of linear relationships and multiple concurrent causal relationships. Practically, this study can provide a reference for the government to formulate policies to improve the adverse health outcomes of the individuals with Non-Fixed Employment better safeguard the health of the public. At the same time, it can also provide a basis for the individuals with non-fixed employment to maintain their own health levels to a certain extent.
Limitations and future directions
However, this study has its limitations. We did not define the duration of unstable employment status, nor did we measure the health status of unstable employment populations before their transition to unstable employment, making it challenging to infer whether their poor health status contributed to their unstable employment status. Moreover, our study employed cross-sectional data, which cannot reveal the dynamic causal relationships between the variables under investigation. Given that the primary objective of our research was to explore the influencing factors and mechanisms of adverse health outcomes, and we have successfully drawn corresponding conclusions, addressing these limitations will be a focus of our future research efforts.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was obtained from the Ethics Committee at the Shaanxi University of Commerce and Business, Health Care Culture Research Center, Shaanxi (College) Philosophy and Social Science Key Research Base.
Author contributions
HW: Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Validation, Writing – original draft, Writing – review & editing. QW: Formal analysis, Investigation, Project administration, Software, Validation, Visualization, Writing – review & editing, Writing – original draft. JC: Data curation, Formal analysis, Methodology, Software, Writing – review & editing. ZL: Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. YW: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – review & editing. HL: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The article process charge of this paper is supported by Guangxi University of Chinese Medicine (H-2023-09/H-2023-10/H-2023-11) and Fangchenggang International Medical Open Experimental Zone Expenses.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
VUCA, Volatile, Uncertain, Complex, Ambiguous; HTMT, Heterotrait-Monotrait Ratio; AVE, Average Variance Extracted; CR, Composite Reliability; fsQCA, Fuzzy-set Qualitative Comparative Analysis; QCA, Qualitative Comparative Analysis; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders; PHQ, Patient Health Questionnaire; HLS-SF, Health Literacy Scale-Short Form; FHS-SF, Family Health Scale-Short Form; PS, Social Support; FH, Family Health; HL, Family Literacy; EB, Unhealthy Eating Behaviors; SM, Smoking; DW, Drinking; EQ, EuroQol Five Dimensions Questionnaire; PH, Patient Health Questionnaire; GA, Generalized anxiety.
References
1.
U.S. Army Hetitage and Education Center . Who first originated the term VUCA volatility, uncertainty, complexity and ambiguity? US Army. (2022). Available online at: https://usawc.libanswers.com/faq/84869 (Accessed 5 September 2023)
2.
Cao H Liang S . Reconstructing the National Security System in the era of VUCA: trajectory of transformation, logical compliance, and path selection. Zhejiang Acad J. (2023) 2:13–21. doi: 10.16235/j.cnki.33-1005/c.2023.02.018
3.
Gajić T Blešić I Petrović MD Radovanović MM Đoković F Demirović Bajrami D et al . Stereotypes and prejudices as (non) attractors for willingness to revisit tourist-spatial hotspots in Serbia. Sustain For. (2023) 15:5130. doi: 10.3390/su15065130
4.
Gajić T Petrović MD Blešić I Vukolić D Milovanović I Radovanović M et al . COVID-19 certificate as a cutting-edge issue in changing the perception of restaurants’ visitors illustrations from Serbian urban centers. Front Psychol. (2022) 13:914484. doi: 10.3389/fpsyg.2022.914484
5.
Rosén M Stenbeck M . Interventions to suppress the coronavirus pandemic will increase unemployment and lead to many premature deaths. Scand J Public Health. (2021) 49:64–8. doi: 10.1177/1403494820947974
6.
Yu J . Analysis and comparison of the tax reform trend in the post-epidemic era. Int For Rev. (2021) 12:51–6. doi: 10.19376/j.cnki.cn10-1142/f.2021.12.008
7.
Macroeconomic Forecasting Research Group of Institute for Chinese Economic Practice and Thinking of Tsinghua University Li D Chen D Li K Wu S . Comprehensive measures to stabilize the economy: analysis of China’s macroeconomic situation and future prospects in the first half of 2022. Reformation. (2022) 6:20–37.
8.
Li C . The economic differentiation of contemporary social classes in China. Jiangsu Soc Sci. (2002) 4:64–73.
9.
Zheng H . China’s sociology in new century China. Beijing: Renmin University of China Press (2006).
10.
Lu X . Research report on contemporary social class in China. Beijing: Social Sciences Literature Press (2002).
11.
Eisenberg P Lazarsfeld PF . The psychological effects of unemployment. Psychol Bull. (1938) 35:358–90. doi: 10.1037/h0063426
12.
Montgomery SM Cook DG Bartley MJ Wadsworth ME . Unemployment, cigarette smoking, alcohol consumption and body weight in young British men. Eur J Pub Health. (1998) 8:21–7. doi: 10.1093/eurpub/8.1.21
13.
Gathergood J . An instrumental variable approach to unemployment, psychological health and social norm effects: unemployment and psychological health. Health Econ. (2013) 22:643–54. doi: 10.1002/hec.2831
14.
Zou X Qiang Q Yin Z Zhang R Liu J Ding H . The reflection on the wave of violence against medical personnel. J Med Philos. (2016) 37:77–9.
15.
World Health Organization . Statement on the fifteenth meeting of the IHR (2005) emergency committee on the COVID-19 pandemic. World Health Organization (2023) Available online at: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic (Accessed May 24, 2024).
16.
Ahn J Kim NS Lee BK Park J Kim Y . Comparison of the physical and mental health problems of unemployed with employees in South Korea. Arch Environ Occup Health. (2020) 76:163–72. doi: 10.1080/19338244.2020.1783503
17.
Gerdtham UG . Johannesson M.A note on the effect of unemployment on mortality. J Health Econ. (2003) 22:505–18. doi: 10.1016/S0167-6296(03)00004-3
18.
Vancea M Utzet M . How unemployment and precarious employment affect the health of young people: a scoping study on social determinants. Scand J Public Health. (2017) 45:73–84. doi: 10.1177/1403494816679555
19.
Nurmela K Mattila A Heikkinen V Uitti J Ylinen A Virtanen P . Identification of major depressive disorder among the long-term unemployed. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:45–52. doi: 10.1007/s00127-017-1457-y
20.
Davison J Share M Hennessy M Bunting B Markovina J Stewart-Knox B . Correlates of food choice in unemployed young people: the role of demographic factors, self-efficacy, food involvement, food poverty and physical activity. Food Qual. (2015) 46:40–7. doi: 10.1016/j.foodqual.2015.06.014
21.
Reine I Novo M Hammarström A . Unemployment and ill health – a gender analysis: results from a 14-year follow-up of the northern Swedish cohort. Public Health. (2013) 127:214–22. doi: 10.1016/j.puhe.2012.12.005
22.
Kaspersen SL Pape K Vie GÅ Ose SO Krokstad S Gunnell D et al . Health and unemployment: 14 years of follow-up on job loss in the Norwegian HUNT study. Eur J Pub Health. (2016) 26:312–7. doi: 10.1093/eurpub/ckv224
23.
Salm M . Does job loss cause ill health?Health Econ. (2009) 18:1075–89. doi: 10.1002/hec.1537
24.
Neubert M Süssenbach P Rief W Euteneuer F . Unemployment and mental health in the German population: the role of subjective social status. Psychol Res Behav Manag. (2019) 12:557–64. doi: 10.2147/PRBM.S207971
25.
Wigand EM Oexle N Waldmann T Staiger T Becker T Rüsch N . Predictors of help-seeking in unemployed people with mental health problems. Int J Soc Psychiatry. (2019) 65:543–7. doi: 10.1177/0020764019868262
26.
Sage D . Do active labour market policies promote the well-being, health and social Capital of the Unemployed? Evidence from the UK. Soc Indic Res. (2015) 124:319–37. doi: 10.1007/s11205-014-0788-2
27.
Madureira-Lima J Reeves A Clair A Stuckler D . The great recession and inequalities in access to health care: a study of unemployment and unmet medical need in Europe in the economic crisis. Int J Epidemiol. (2018) 47:58–68. doi: 10.1093/ije/dyx193
28.
Huegaerts K Puig-Barrachina V Vanroelen C . The mental health of unemployed Brussels youth: the role of social and material resources. Arch Public Health. (2017) 75:19. doi: 10.1186/s13690-017-0187-7
29.
Jeong S Fox AM . Enhanced unemployment benefits, mental health, and substance use among low-income households during the COVID-19 pandemic. Soc Sci Med. (2023) 328:115973. doi: 10.1016/j.socscimed.2023.115973
30.
Vahid Shahidi F Siddiqi A Muntaner C . Does social policy moderate the impact of unemployment on health? A multilevel analysis of 23 welfare states. Eur J Pub Health. (2016) 26:1017–22. doi: 10.1093/eurpub/ckw050
31.
Huijts T Reeves A McKee M Stuckler D . The impacts of job loss and job recovery on self-rated health: testing the mediating role of financial strain and income. Eur J Pub Health. (2015) 25:801–6. doi: 10.1093/eurpub/ckv108
32.
Zuelke AE Luck T Schroeter ML Witte AV Hinz A Engel C et al . The association between unemployment and depression–results from the population-based LIFE-adult-study. J Affect Disord. (2018) 235:399–406. doi: 10.1016/j.jad.2018.04.073
33.
Mayer D Hollederer A . What helps the unemployed to stay healthy? A qualitative study of coping with the negative effects of job loss. Am J Public Health Res. (2021) 11:2492. doi: 10.4081/jphr.2021.2492
34.
Krug G Prechsl S . The role of social integration in the adverse effect of unemployment on mental health – testing the causal pathway and buffering hypotheses using panel data. Soc Sci Res. (2020) 86:102379. doi: 10.1016/j.ssresearch.2019.102379
35.
Krug G Eberl A . What explains the negative effect of unemployment on health? An analysis accounting for reverse causality. Res Soc Stratif Mobil. (2018) 55:25–39. doi: 10.1016/j.rssm.2018.03.001
36.
Peláez-Fernández MA Rey L Extremera N . Pathways from emotional intelligence to well-being and health outcomes among unemployed: mediation by health-promoting behaviours. J Health Psychol. (2022) 27:879–89. doi: 10.1177/1359105320974431
37.
Goodman WK Geiger AM Wolf JM . Leisure activities are linked to mental health benefits by providing time structure: comparing employed, unemployed and homemakers J Epidemiol. Community Health. (2017) 71:4–11. doi: 10.1136/jech-2016-207260
38.
Thoits PA . Stress, coping, and social support processes: where are we? What next?J Health Soc Behav. (1995) 35:53–79. doi: 10.2307/2626957
39.
Seeman TE Singer BH Ryff CD Love GD Levy-Storms L . Social relationships, gender, and allostatic load across two age cohorts. Psychosom Med. (2002) 64:395–406. doi: 10.1097/00006842-200205000-00004
40.
Dooley D Prause J Ham-Rowbottom KA . Underemployment and depression: longitudinal relationships. J Health Soc Behav. (2000) 41:421–36. doi: 10.2307/2676295
41.
Jones L . Unemployment and social integration: a review. J Sociol Soc Welf. (1988) 15:161.
42.
Landale NS Oropesa RS . Migration, social support and perinatal health: an origin-destination analysis of Puerto Rican women. J Health Soc Behav. (2001) 42:166–83. doi: 10.2307/3090176
43.
Tong L Hu J Hou P . Health quality and health competence. Chin J Health Educ. (2006) 4:293–5.
44.
Dai L Tian D Luo J Liu X Chen Y Yang X . Analysis on the degree of concern and access to health information of residents in Xiamen. Chin J Health Educ. (2013) 29:348–51. doi: 10.16168/j.cnki.issn.1002-9982.2013.04.009
45.
Mirowsky J Hu PN . Physical impairment and the diminishing effects of income. Soc Forces. (1996) 74:1073–96. doi: 10.2307/2580393
46.
Willson AE Shuey KM Elder GH Jr . Cumulative advantage processes as mechanisms of inequality in life course health. Am J Sociol. (2007) 112:1886–924. doi: 10.1086/512712
47.
Ferrie JE Shipley MJ Marmot MG Stansfeld SA Smith GD . An uncertain future: the health effects of threats to employment security in white-collar men and women. Am J Public Health. (1998) 88:1030–6. doi: 10.2105/AJPH.88.7.1030
48.
Li C Yang Z Xue C . Analysis of health intergenerational transmission and mechanisms. Chin J Popul Health. (2021) 6:127–8.
49.
Nutbeam D . Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. (2000) 15:259–67. doi: 10.1093/heapro/15.3.259
50.
Svendsen MT Bak CK Sørensen K Pelikan J Riddersholm SJ Skals RK et al . Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large national population-based survey among Danish adults. BMC Public Health. (2020) 20:565. doi: 10.1186/s12889-020-08498-8
51.
Samkange-Zeeb F Singh H Lakeberg M Kolschen J Schüz B Christianson L et al . Health literacy needs among unemployed persons: collating evidence through triangulation of interview and scoping review data. Front Public Health. (2022) 10:798797. doi: 10.3389/fpubh.2022.798797
52.
Zhu Z Bi X Peng W Li D . Effect of social support on Oral health care behavior of pregnant women in a top three Hospital in Chengdu. Med Soc. (2023) 36:56–61. doi: 10.13723/j.yxysh.2023.05.010
53.
Cho YI Lee S-YD Arozullah AM Crittenden KS . Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med. (2008) 66:1809–16. doi: 10.1016/j.socscimed.2008.01.003
54.
Pearlin LI Menaghan EG Lieberman MA Mullan JT . The stress process. J Health Soc Behav. (1981) 22:337–56. doi: 10.2307/2136676
55.
Pearlin LI . The sociological study of stress. J Health Soc Behav. (1989) 30:241–56. doi: 10.2307/2136956
56.
Gilbert PA Zemore SE . Discrimination and drinking: a systematic review of the evidence. Soc Sci Med. (2016) 161:178–94. doi: 10.1016/j.socscimed.2016.06.009
57.
Degni F Vaherkylä M Hurme S . Health behavior and self-assessed health among some long-term unemployed living in Turku, Finland. Open Public Health J. (2017) 10:232–43. doi: 10.2174/1874944501710010232
58.
Zeng Q Chang C Jiang Y . The relationship between health competence and hypertension health management. J Pecking Univ. (2014) 46:492–7.
59.
Shrank WH Avorn J . Educating patients about their medications: the potential and limitations of written drug information. Health Aff. (2007) 26:731–40. doi: 10.1377/hlthaff.26.3.731
60.
Chen Q Hu Y Fu H . The Short-term and Long-term Impacts of Mass Unemployment on Health: Evidence from the Wave of Layoffs in China in the late 1990s (2017) 5:51–61.
61.
Min H Sun X . The relationship between family health functioning, five personality traits, and smoking among the population aged 18 and above in China. J Pecking Univ. (2022) 54:483–9. doi: 10.19723/j.issn.1671-167X.2022.03.013
62.
Luo N Liu G Li M Guan H Jin X Rand-Hendriksen K . Estimating an EQ-5D-5L value set for China. Value Health. (2017) 20:662–9. doi: 10.1016/j.jval.2016.11.016
63.
Kroenke K Spitzer RL Williams JBW . The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
64.
Spitzer RL Kroenke K Williams JB Löwe B . A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
65.
Blumenthal JA Burg MM Barefoot J Williams RB Haney T Zimet G . Social support, type a behavior, and coronary artery disease. Psychosom Med. (1987) 49:331–40. doi: 10.1097/00006842-198707000-00002
66.
Jiang Q . Perceived social support scale (PSSS). Chin Ment Health J. (1999):131–3.
67.
Crandall A Weiss-Laxer NS Broadbent E Holmes EK Magnusson BM Okano L et al . The family health scale: reliability and validity of a short-and long-form. Front Public Health. (2020) 8:587125. doi: 10.3389/fpubh.2020.587125
68.
Van Duong T Chang PW Yang S-H Chen M-C Chao W-T Chen T et al . A new comprehensive short-form health literacy survey tool for patients in general. Asian Nurs Res. (2017) 11:30–5. doi: 10.1016/j.anr.2017.02.001
69.
Tayama J Ogawa S Takeoka A Kobayashi M Shirabe S . Item response theory-based validation of a short form of the eating behavior scale for Japanese adults. Medicine. (2017) 96:e8334. doi: 10.1097/MD.0000000000008334
70.
Xia D Zhu B . Can socioeconomic status affect health through lifestyle--a comparative analysis based on urban and rural laborers. Hubei Soc Sci. (2021) 2:50–8. doi: 10.13660/j.cnki.42-1112/c.015561
71.
Singh-Manoux A Martikainen P Ferrie J Zins M Marmot M Goldberg M . What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies. J Epidemiol Community Health. (2006) 60:364–72. doi: 10.1136/jech.2005.039883
72.
Hair JF Hult GTM Ringle CM Sarstedt M . A primer on partial least squares structural equation modeling (PLS-SEM). 2nd ed. California: Sage (2017).
73.
Podsakoff PM MacKenzie SB Lee J-Y Podsakoff NP . Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. doi: 10.1037/0021-9010.88.5.879
74.
Baron RM Kenny DA . The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173
75.
Ganter A Hecker A . Configurational paths to organizational innovation: qualitative comparative analyses of antecedents and contingencies. J Bus Res. (2014) 67:1285–92. doi: 10.1016/j.jbusres.2013.03.004
76.
Woodside AG . Moving beyond multiple regression analysis to algorithms: calling for adoption of a paradigm shift from symmetric to asymmetric thinking in data analysis and crafting theory. J Bus Res. (2013) 66:463–72. doi: 10.1016/j.jbusres.2012.12.021
77.
Ragin CC . Fuzzy-set social science. Chicago: University of Chicago Press (2000).
78.
He J . Fuzzy set methods in comparative political analysis. Soc Sci. (2013) 5:30–8.
79.
Tang D Wen Z . Statistical approaches for testing common method Bias: problems and suggestions. J Psychol Sci. (2020) 43:216. doi: 10.16719/j.cnki.1671-6981.20200130
80.
Fornell C Larcker DF . Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. (1981) 18:39–346. doi: 10.2307/3151312
81.
Henseler J Dijkstra TK Sarstedt M Ringle CM Diamantopoulos A Straub DW . Common beliefs and reality about partial least squares: Comments on Rönkkö & Evermann. Organ Res Methods. (2013) 17:182–209. doi: 10.1177/1094428114526928
82.
Rihoux B Ragin CC . Configurational comparative methods: Qualitative comparative analysis (QCA) and related techniques. ThousandOaks: Sage (2009).
83.
Du Y Jia L . Configurational perspective and qualitative comparative analysis (QCA): a new pathway for management studies research. J Manage World. (2013) 5:155–67. doi: 10.19744/j.cnki.11-1235/f.2017.06.012
84.
Crilly D Zollo M Hansen MT . Faking it or muddling through? Understanding decoupling in response to stakeholder pressures. AMJ. (2012) 55:1429–48. doi: 10.5465/amj.2010.0697
85.
Sen A . Development as Freedom. Beijing: China Renmin University Press (2013).
86.
Marmot M . The health gap: The challenge of an unequal world. Beijing: People’s Daily Press (2019).
87.
Haskins R Garfinkel I Mclanahan S . Introduction: Two-generation mechanisms of child development. Futur Child. (2014) 24:3–12. doi: 10.1353/foc.2014.0001
88.
Cockham W . Medical Sociology. Beijing: China Renmin University Press (2012).
89.
Mokdad AH Marks JS Stroup DF Gerberding JL . Actual causes of death in the United States, 2000. JAMA. (2004) 291:1238–45. doi: 10.1001/jama.291.10.1238
90.
Conner M Norman P . Predicting health behavior: Research and practice with social cognition models. Maindenhead: Open University Press (1996).
91.
Hall PA Fong GT . The effects of a brief time perspective intervention for increasing physical activity among young adults. Psychol Health. (2003) 18:685–706. doi: 10.1080/0887044031000110447
92.
Conner M Norman P Bell R . The theory of planned behavior and healthy eating. Health Psychol. (2002) 21:194–201. doi: 10.1037/0278-6133.21.2.194
93.
Cockerham WC . Health lifestyle theory and the convergence of agency and structure. J Health Soc Behav. (2005) 46:51–67. doi: 10.1177/002214650504600105
94.
Li Q . New trends in the changes of social stratification structure in contemporary China. Jiangsu Soc Sci. (2004) 6:93–9.
95.
Wen J Li S . The class differences in the intergenerational transmission of cultural capital and their impacts: a comparative study based on middle-class and working-class families in Shanghai. J East China Normal Univ. (2018) 5:101–13. doi: 10.16382/j.cnki.1000-5579.2018.04.011
96.
Stephens NM Markus HR Fryberg SA . Social class disparities in health and education: reducing inequality by applying a sociocultural self model of behavior. Psychol Rev. (2012) 119:723–44. doi: 10.1037/a0029028
Summary
Keywords
social environment, health cognition, health behavior, non-fixed employment, adverse health outcomes, mediating mechanism, configurational analysis
Citation
Wei H, Wang Q, Chen J, Liang Z, Wu Y and Luo H (2024) Social environment, health cognition, and health behavior: how individuals with non-fixed employment end up with adverse health outcomes in China under the era of VUCA?—findings from PLS-SEM and fsQCA. Front. Public Health 12:1341213. doi: 10.3389/fpubh.2024.1341213
Received
20 November 2023
Accepted
01 August 2024
Published
20 August 2024
Volume
12 - 2024
Edited by
Zhiqiang Feng, University of Edinburgh, United Kingdom
Reviewed by
Tamara Gajić, Serbian Academy of Sciences and Arts, Serbia
Li Liu, China Medical University, China
Updates
Copyright
© 2024 Wei, Wang, Chen, Liang, Wu and Luo.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongye Luo, hongye283@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.