1 Introduction
Malnutrition is defined as the excesses, imbalances, or deficiencies in a person's dietary intake. In all its forms, malnutrition comprises two large groups: undernutrition (wasting, stunting, underweight, and micronutrient deficiencies) and the second group, which covers overweight, obesity, and their resulting diet-related non-communicable diseases (1). Malnutrition happens in urban and rural areas alike since urbanization, poverty, economic development, and lifestyle behaviors are the most common causes of malnutrition across high- and low-income countries (2). Food insecurity (FI), one of the most important leading causes of malnutrition, is defined as “a situation that exists when people lack regular access to adequate amount of safe and nutritious food for normal growth and development and an active and healthy life” (3). During the past decade, there was a significant global rise in the level of moderate-to-severe food insecure people, which accounts for almost 30% of the world's population, with more than 50% of them hailing from Asia, and 33% from Africa (4).
2 The global burden of malnutrition
According to the WHO, the double burden of malnutrition is the coexistence of undernutrition along with overweight/obesity or diet-related non-communicable diseases (5). Worldwide, in 2020, 1.9 billion were overweight, with body mass index (BMI) between 25 and 29.9, or obese (BMI > 30), while 462 million adults were underweight (BMI < 18.5). For children under five, 149 million, 45 million, and 38.9 million were estimated to be stunted, wasted, and overweight, respectively. Moreover, in low- and middle-income countries, undernutrition resulted in ~45% of deaths among children under five, along with an increase in the rates of overweight and obesity in these countries (1). In fact, in the Arab region, the double burden of malnutrition at the individual level, such as stunting coexisting with overweight in children, is twice as high as in other countries worldwide and has exceeded expectations (6). Therefore, the Arab region countries are facing an overlap of overnutrition and undernutrition, mainly in Palestinian and Syrian refugee populations in Lebanon (7, 8).
2.1 The health burden of malnutrition in Lebanon
Lebanon is one of the countries in the Arab region that has shown rapid urbanization, changes in its food system, and accelerated transition in nutrition norms despite political challenges and conflicts. However, in 2019, the Lebanese economic crisis affected the official currency as the Lebanese pound collapsed and lost more than 90% of its value (1), diminishing the population's accessibility to basic needs such as food, water, education, and healthcare services. Accordingly, the prices of food increased by 550% between 2020 and 2021 (9). The United Nations (UN) declared that in 2021, ~78% of the Lebanese population lived in poverty, which was three times higher than the estimated number in 2020 (10). On the other hand, the World Bank declared in its latest reports on food security worldwide that Lebanon achieved the highest nominal food price inflation rate in the world during the February 2022–February 2023 period. The country registered a 261% annual change in the food Consumer Price Index (CPI), followed by Zimbabwe (128%) (11). Living below the national poverty line will increase food insecurity, as well as hidden hunger, within the Lebanese population, raising the risk of developing the problem of malnutrition in the coming years.
2.2 National nutrition and food insecurity
Since 2019, the socioeconomic situation in Lebanon has worsened further due to the COVID-19 pandemic and the measures implemented to control it. The worsening of the economic status of the Lebanese population led to a reduction in the monthly income and a shortage in food availability and affordability. Therefore, food insecurity increased during these difficult times with the country facing many financial, political, economic, and health crises. Lebanon urgently needs policies to ensure food security and alleviate the burden of the current situation on its population, especially Lebanese children who are at a higher risk of malnutrition (12). Therefore, the majority of the Lebanese population has been plunged into poverty, with 22% of Lebanese being food-insecure due to considerable inequities in access to healthy foods across the population (13). In 2021, Lebanon's Ministry of Public Health conducted a survey supported by the United Nations International Children's Emergency Fund (UNICEF) and Action Against Hunger (AAH); the survey revealed that ~200,000 children under 5 are suffering from at least one form of malnutrition, including wasting, stunting, and micronutrients deficiencies (13). A recent study in Lebanon showed that ~37.6% and 37.4% had moderate and severe food insecurities. In addition, participants who reported a bad overall health status of their children declared that they were severely food insecure. Moreover, those with severe food insecurity stated that their children's daily snacking habit between meals had decreased, with a decreased quantity of meals and intake of vegetables/fruits. Moreover, severe food insecurity was significantly associated with higher mean financial burdens than the other groups (12).
In Lebanon, the prevalence of wasting and underweight is found to be 1.1 and 3.71%, respectively (14), where wasting drivers include inadequate diet and services, poor practices, and disease. Furthermore, more than 70% of children are not receiving breastfeeding, only 6% were consuming minimum acceptable diets, and 54% of survey participants tend to reduce portions of meals when they do not have enough food, rendering 1.8 and 5% of children and pregnant and lactating women malnourished. According to the survey, stunting was recorded at 7%, with a prevalence slightly higher in the capital city than in the other governorates with levels similar to the national stunting prevalence (13).
On the other hand, adequate dietary intake during childhood is a key component for promoting health and development as well as for disease prevention throughout a lifetime (15). In Lebanon, the last few years have shown an alarming rise in the rates of overweight (21.2%) and obesity (10.9%) among school-age children, higher than the global estimate of 6.7% (16); such an increase could be explained by the rapid transition in lifestyle behavior (less physical activities, more addiction to video games) and due to the switch from the Lebanese Mediterranean Diet rich in fruits, vegetables, grains, olive oil, and protein to a Westernized dietary pattern with high fat, sugar, and salt contents. Several studies have shown that this transition in dietary patterns is correlated with an increase in the rate of overweight and obesity, as well as the increase in the risk of early development of non-communicable diseases among children (17–19). Accordingly, a recent study has estimated that by 2030, only 14%−20% of adolescents in Lebanon will remain adherent to the Mediterranean Diet pattern as a projection from the norm of food consumption trend of Lebanese children between 1995 and 2009 (20) (Figure 1). Several studies provide considerable evidence for the importance of the Mediterranean diet in protection against non-communicable diseases, mainly diabetes, hypertension, cancer, and cardiometabolic risk factors (18). On the other hand, based on the national survey conducted among Lebanese preschoolers, ~9% of Lebanese children under five are classified as overweight or obese (14); this study revealed that overweight and obesity in this age group was significantly associated with the presence of a household maid, which affected the children's adherence to the traditional pattern, in addition to the high intake of sweets and beverages with added sugar.
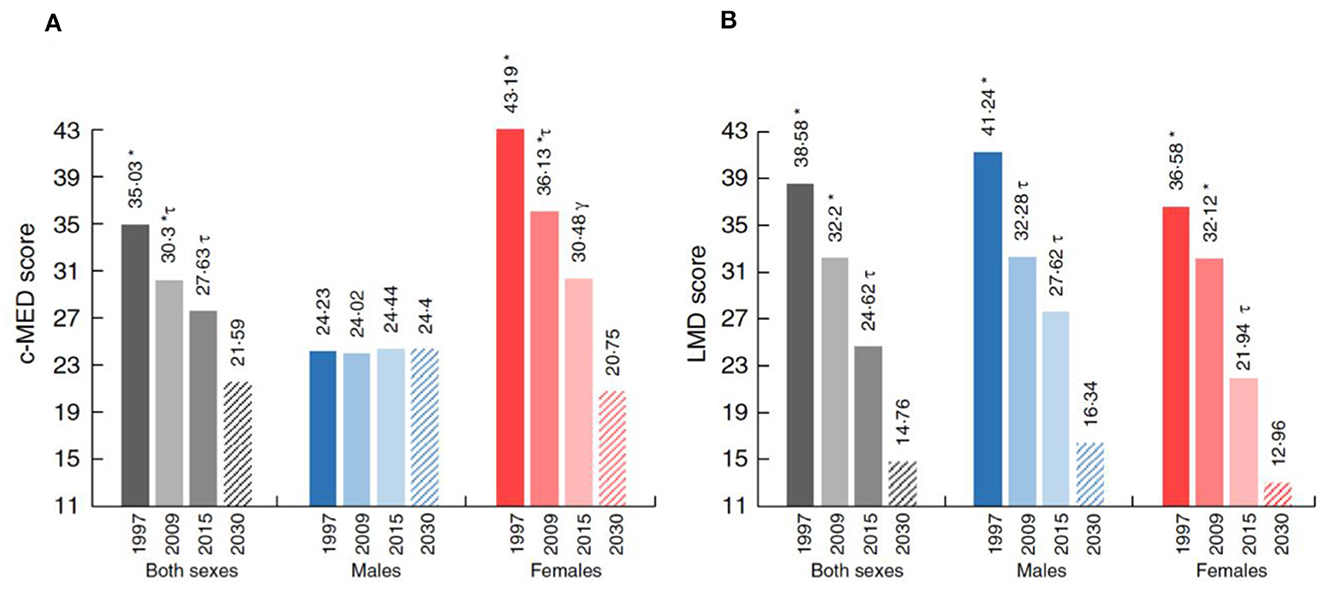
Figure 1. (A, B) Proportion of the study population's level of adherence to the Mediterranean diet scores by sex and survey year and projection to 2030. c-MED, composite Mediterranean diet; LMD, Lebanese Mediterranean diet. Projections are presented by the dashed rectangles. *, τ, γDifferent symbols indicate significant difference between the corresponding groups.
2.3 Double burden of malnutrition
Lebanon is classified as a low-income country in early nutrition transition. Studies revealed that Lebanon is one of the countries in the Arab region manifesting an increasing trend in the prevalence of obesity in school-age children along with an anemia prevalence of 28.3% (Figures 2, 3). Moreover, iron, vitamin D, and iodine deficiencies reached 11%, 21%, and 56%, respectively, in 1998 (21, 22, 31). Therefore, if obesity is attributed to bad lifestyle behavior, such as lack of physical activities and consumption of unhealthy foods with high sugar and fat contents, micronutrient deficiency or hidden hunger is another form of malnutrition correlated with poor adherence to the average daily intake level of nutrients. Accordingly, several studies reported an inadequate micronutrient intake among this age group, where 35%, 84%, 85%, and 95% did not meet two-thirds of the Recommended Daily Allowance (RDA) for iron, calcium, copper, and vitamin D, respectively (21, 32). As mentioned previously, Lebanese school-age children showed a high prevalence of obesity coexisting with micronutrient deficiencies, which highlights the double burden of malnutrition in Lebanon. On the other hand, when the prevalence of stunting in Lebanon was compared with the World Health Assembly recommendation for a reduction in the number of children under 5 years who are stunted and wasted by 40% and 5%, respectively, as targets for 2025 (33), Lebanon seems to be on the right track. However, in light of the economic crisis, the rates of malnutrition are expected to rise even more in the upcoming years (13). Therefore, actions should be taken to reduce the double burden of malnutrition in Lebanon, especially the risks of non-communicable diseases, which accounted for 71% of all deaths in 2018 (34). One of the implemented actions is the school feeding programs (SFP) in collaboration with the World Food Program, where fruits, vegetables, nuts, and milk are introduced instead of high-energy snacks to control the double burden of malnutrition among this age group in Lebanon (Figure 4) (8).
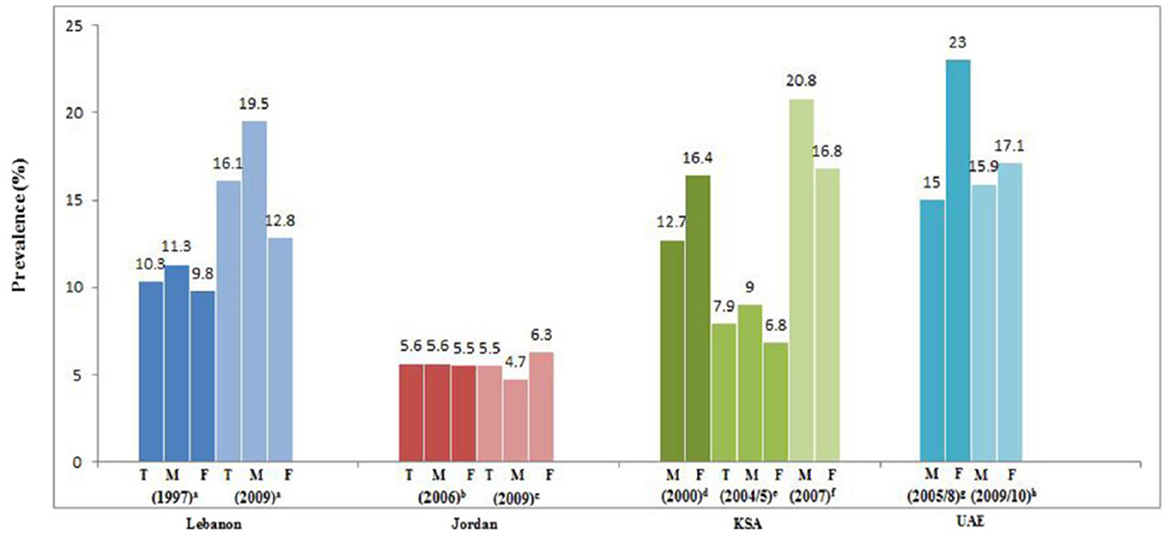
Figure 2. Prevalence (%) and trends of obesity in school-aged children in the eastern Mediterranean region. T, total; M, Males; F, Females (Lebanon: left/blue). Source: Nasreddine et al. (21). a: FAO (22); b: Food and Agriculture Organization (FAO) (23); c: Assaf and Bradley (24); d: Hossain et al. (25); e: Miller et al. (26); f: Ministry of Health (MOH) (27); g: Khatib and Elmadfa (28); h: Ministry of Health (MOH) (29).
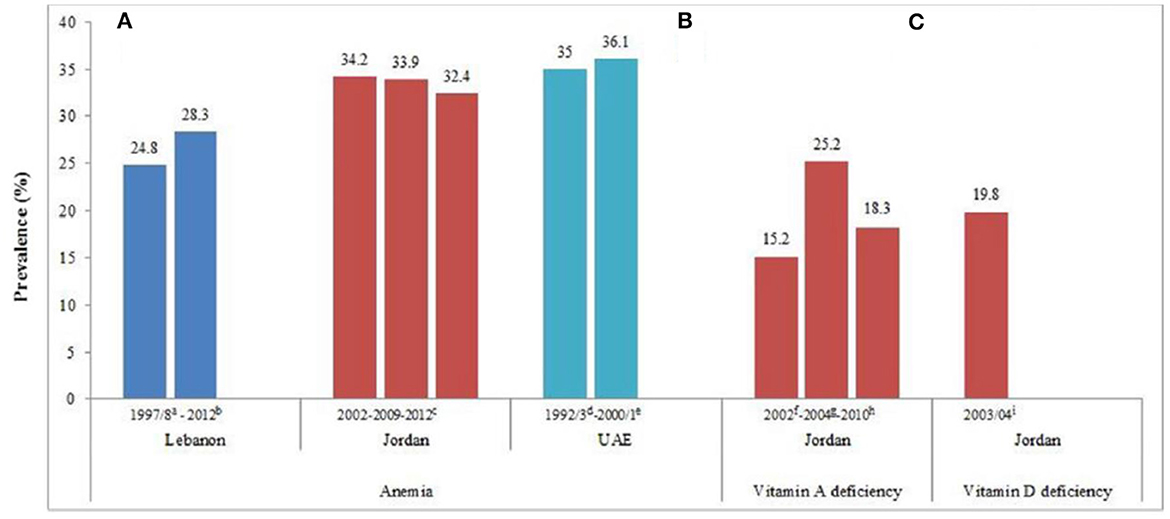
Figure 3. (A–C) Prevalence (%) of anemia, vitamin A deficiency, and vitamin D deficiency in preschool children in the Eastern Mediterranean Region. Abbreviation: UAE, United Arab Emirates. a: FAO (22); b: Food and Agriculture Organization (FAO) (23); c: Assaf and Bradley (24); d: Hossain et al. (25); e: Miller et al. (26); f: Ministry of Health (MOH) (27); g: Khatib and Elmadfa (28); h: Ministry of Health (MOH) (29); i: Ministry of Health (MOH) (30).
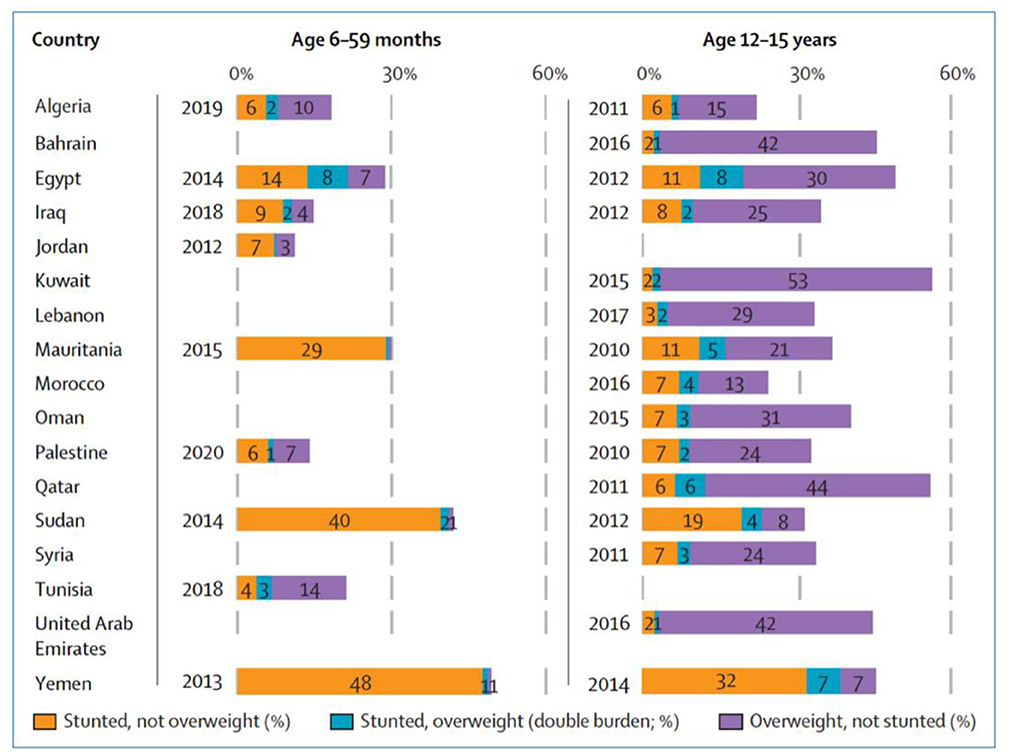
Figure 4. Prevalence of stunting, overweight, and individual-level double burden in adolescents aged 12–15 years in Lebanon (2017), no data available for children aged 6–59 months. Source: Ghattas et al. (8).
2.4 Determinants and consequences of malnutrition
Malnutrition is attributed to individual lifestyle behavior, socio-demographic characteristics, and economic, physiological, and pathological factors (35). In Lebanon, Mitri et al. (36) reported that among older adults aged 65 years and above, women were significantly more at risk for malnutrition than men. The risk of poor nutrition increased with low level of education and the absence of health insurance and fixed income. Moreover, the population with comorbidities and taking several medications was significantly at higher risk for malnutrition than those with good health and practicing daily physical activities. Surprisingly, oral health in adults, mainly older individuals, can affect their nutrition and may put them at risk of poor nutrition when dentures cannot cover their nutritional needs (36). Furthermore, depression and BMI are among the socio-demographic variables that are significantly associated with a greater risk of malnutrition among Lebanese older adults (35). For school-age children, malnutrition was mainly associated with age, time spent on electronic devices, skipping meals, and inadequate intake of nutrients (37). Among micronutrient deficiencies that affect the physical growth, psychological development, and academic performance of children, Vitamin A, Vitamin D, and pediatric anemia represent a great challenge in Lebanon. Moreover, studies have shown that the increase in overweight and obesity prevalence in Lebanon among school-age children raises the risk for type 2 diabetes mellitus, hypertension, and cardiovascular diseases among this age group and worsens the burden of non-communicable diseases in the country in the long term (16).
3 Data reliability
Amid the political challenges and socioeconomic crisis faced by Lebanon in recent years, the country has hosted a large number of refugees, with an estimated 1.5 million and 14,815 refugees of Syrian and other nationalities, respectively (38). The majority of Syrian refugees do not hold legal residency in Lebanon; thus, they suffer from a lack of healthcare services and have no access to basic daily needs such as healthy food and water. Moreover, the attention of humanitarian organizations was transferred to this population living in extreme poverty. Moreover, most surveys, studies, data collections, and analyses focused on the living conditions of Syrian and Palestinian refugees in their camps and ignored the national sector. Therefore, we have encountered difficulties in describing and analyzing the burden of malnutrition in Lebanon, especially among older Lebanese adults aged 65 years and older. This age group is expected to account for 10.2% of the total population in 2025, according to projections (39). Moreover, Choueiry et al. (35) reported that since 2008, there has been no update on the nutritional status of hospitalized Lebanese patients; the nutritional survey of rural older adults was recently targeted in 2013 (36), and not enough data for vitamin A deficiency among Lebanese population has been published (21).
4 Mitigating the burden of malnutrition through health system approach
Vertical and horizontal approaches are used in health systems planning to address health problems (40). Tackling malnutrition across the population suffering from the double burden of malnutrition should include two main levels: First, the implementation of interventions at the individual level through a vertical approach; and second, multi-level actions by collaborating with different governmental sectors through a horizontal approach for policy development and enactment. In addressing undernutrition, schools can help significantly in the prevention and management of micronutrient deficiencies among this age group by providing effective nutrition education. Therefore, the organization of nutrition campaigns in schools is the best way to increase children's knowledge of healthy food choices and to improve their adherence to the recommended dietary intake guidelines. The outcomes of the vertical approach are time-limited, with rapid interactions and responses to the implemented interventions. The effectiveness of the previously mentioned approach is justified by one of the most important implemented nutrition interventions in Lebanon under the title “Your health is on your plate” where Said et al. (41) have demonstrated the great outcomes of implemented action in increasing knowledge and adherence to dietary guidelines in Lebanese adolescents. However, policies that fight overnutrition across the population through a horizontal approach need the engagement of several sectors, such as stakeholders, health, justice, environment, agriculture, and education. These sectors interact together for policy development and enactment to control the availability of energy-dense food and sweetened drinks at local stores, enhance physical activities at schools by limiting screen time access, enhance breastfeeding, and raise parental awareness toward a healthy lifestyle. Serious strategies and effective interventions should be implemented to avoid further inflation and ensure food security for the Lebanese population, such as encouraging internal agriculture, decreasing food prices, food-wasting, and unemployment, and improving infrastructural programs, trade policies, and diversification.
The success of implemented approaches could be evaluated through the Health Economic Evaluation and Health Impact Assessment (HIA), which assesses the health and equity impact of the implemented policies. This allows us to not only evaluate the success of interventions but also enables early detection of problem to find solutions. Several studies have shown the significant association between parent's socio-demographic characteristics, education level, maternal BMI, and child feeding practices (19). Therefore, response strategies are mandatory to avoid further hunger and the impact of food insecurity on human physical and mental health.
5 Conclusion
Currently, the burden of malnutrition is considered to be one of the most important public health challenges. Malnutrition in all its forms has short- and long-term complications that affect the psychological and physical wellbeing of children and adults. Therefore, a multi-sectoral collaboration between stakeholders, non-governmental organizations, social protection, and welfare and funding agencies is highly needed to address the root causes of malnutrition and decrease the attributed risk factors earlier in life (42).
Author contributions
AA: Conceptualization, Writing—original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. Malnutrition. (2022). Available online at: https://www.who.int/health-topics/malnutrition (accessed November 12, 2022).
2. Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. (2020) 395:75–88. doi: 10.1016/S0140-6736(19)32472-9
3. FAO. The State of Food Security and Nutrition in the World 2023. Repurposing Food and Agricultural Policies to Make Healthy Diets More Affordable. (2023). Available online at: https://www.fao.org/documents/card/en?details=cc3017en (accessed January 24, 2024).
4. Yasmin SMT, Yasmin SMT, Sultan S, Hong SA. Prevalence of adolescent-reported food insecurity and the determinants including coping strategies living in urban slum communities of Bangladesh during the era of COVID-19: a cross-sectional study. BMC Public Health. (2023) 23:2046. doi: 10.1186/s12889-023-16984-y
5. WHO. Double Burden of Malnutrition. (2017). Available online at: http://www.who.int/nutrition/double-burden-malnutrition/en/ (accessed November 9, 2022).
6. Ghattas H, Acharya Y, Jamaluddine Z, Assi M, El Asmar K, Jones AD, et al. Child-level double burden of malnutrition in the MENA and LAC regions: prevalence and social determinants. Mat Child Nutr. (2020) 16:e12923. doi: 10.1111/mcn.12923
7. Abou-Rizk J, Jeremias T, Nasreddine L, Jomaa L, Hwalla N, Tamim H, et al. Anemia and nutritional status of Syrian refugee mothers and their children under five years in Greater Beirut, Lebanon. Int J Environ Res Public Health. (2021) 18:6894. doi: 10.3390/ijerph18136894
8. Ghattas H, Jamaluddine Z, Akik C. Double burden of malnutrition in children and adolescents in the Arab region. The Lancet Child Adoles Health. (2021) 5:462–4. doi: 10.1016/S2352-4642(21)00162-0
9. HRW. Lebanon Event of 2021. (2021). Available online at: https://www.hrw.org/world-report/2022/country-chapters/lebanon (accessed November 10, 2022).
10. UN. Lebanon: Almost Three-Quarters of the Population Living in Poverty. (2021). Available online at: https://news.un.org/en/story/2021/09/1099102 (accessed November 15, 2022).
11. World Bank. Food Security Update Report. Lebanon Tops World's Food Price Inflation Rate. (2023). Available online at: https://thedocs.worldbank.org/en/doc/40ebbf38f5a6b68bfc11e5273e1405d4-0090012022/related/Food-Security-Update-XC-July-27-2023.pdf (accessed January 24, 2024).
12. Gedeon R, Hallit S, Wakim LH. Food insecurity and eating habits of Lebanese children aged 5–11 years during the COVID-19 pandemic and the socioeconomic crisis: a national study. BMC Pub Health. (2022) 22:1–11. doi: 10.1186/s12889-022-14387-z
13. UNICEF. UNICEF Initiative Tackles Rising Malnutrition in Lebanon. (2021). Available online at: https://www.unicef.org/lebanon/stories/unicef-initiative-tackles-rising-malnutrition-lebanon (accessed November 12, 2022).
14. Nasreddine L, Hwalla N, Saliba A, Akl C, Naja F. Prevalence and correlates of preschool overweight and obesity amidst the nutrition transition: findings from a national cross-sectional study in Lebanon. Nutrients. (2017) 9:266. doi: 10.3390/nu9030266
15. CDC. Childhood Nutrition Facts. (2021). Available online at: https://www.cdc.gov/healthyschools/nutrition/facts.htm (accessed November 14, 2022).
16. Nasreddine L, Hwalla N, Al Zahraa Chokor F, Naja F, O'Neill L, Jomaa L, et al. Food and nutrient intake of school-aged children in Lebanon and their adherence to dietary guidelines and recommendations. BMC Public Health. (2022) 22:1–18. doi: 10.1186/s12889-022-13186-w
17. Nasreddine L, Naja F, Chamieh MC, Adra N, Sibai AM, Hwalla N, et al. Trends in overweight and obesity in Lebanon: evidence from two national cross-sectional surveys (1997 and 2009). BMC Public Health. (2012) 12:1–11. doi: 10.1186/1471-2458-12-798
18. Naja F, Hwalla N, Itani L, Karam S, Sibai AM, Nasreddine L, et al. A Western dietary pattern is associated with overweight and obesity in a national sample of Lebanese adolescents (13–19 years): a cross-sectional study. Br J Nutr. (2015) 114:1909–19. doi: 10.1017/S0007114515003657
19. Nasreddine L, Shatila H, Itani L, Hwalla N, Jomaa L, Naja F, et al. A traditional dietary pattern is associated with lower odds of overweight and obesity among preschool children in Lebanon: a cross-sectional study. Eur J Nutr. (2019) 58:91–102. doi: 10.1007/s00394-017-1574-0
20. Naja F, Hwalla N, Hachem F, Abbas N, Chokor FAZ, Kharroubi S, et al. Erosion of the Mediterranean diet among adolescents: evidence from an Eastern Mediterranean Country. Br J Nutr. (2021) 125:346–56. doi: 10.1017/S0007114520002731
21. Nasreddine LM, Kassis AN, Ayoub JJ, Naja FA, Hwalla NC. Nutritional status and dietary intakes of children amid the nutrition transition: the case of the Eastern Mediterranean Region. Nutr Res. (2018) 57:12–27. doi: 10.1016/j.nutres.2018.04.016
22. FAO. Nutrition Country Profile Lebanese Republic. (2007). Available online at: http://www.fao.org/docrep/017/aq041e/aq041e.pdf (accessed November 20, 2022).
23. Food and Agriculture Organization (FAO). Notes for the Annex Table (2012). Available online at: http://www.fao.org/docrep/018/i3300e/i3300e07.pdf (accessed January 28, 2015).
24. Assaf S, Bradley SE. Trends in Demographic and Health Indicators in Jordan: Data from the 1990–2012 Jordan Population and Family Health Surveys (2014).
25. Hossain MM, Bakir M, Pugh RNH, Sheekh-Hussen M, Ishaq SB, Berg DB, et al. The prevalence and correlates of anaemia among young children and women of childbearing age in Al Ain, United Arab Emirates. Ann Trop Paediatr. (1995) 15:227–35.
26. Miller CJ, Dunn EV, Abdouni SF, Shaheen HM, Ullah MS. Factors associated with iron depletion and iron deficiency anemia among Arabic preschool children of the United Arab Emirates. Saudi Med J. (2004) 25:843–7.
27. Ministry of Health (MOH). National Micronutrient Survey, Jordan 2010 (2011). Available online at: http://www.gainhealth.org/sites/www.gainhealth.org/files/2010%20Jordan%20survey%20report.pdf (accessed February 8, 2016).
28. Khatib IM, Elmadfa I. Poor nutritional health of Bedouin preschool children in Jordan: the irony of urbanization. Ann Nutr Metab. (2009) 54:301–9.
29. Ministry of Health (MOH). National Micronutrient Survey, Jordan 2010, Vitamin A Deficiency (2011). Available online at: http://www.gainhealth.org/sites/www.gainhealth.org/files/2010%20Jordan%20survey%20report.pdf (accessed February 8, 2016).
30. Ministry of Health (MOH). National Micronutrient Survey, Jordan 2010. Vitamin D Deficiency (2011). Available online at: http://www.gainhealth.org/sites/www.gainhealth.org/files/2010%20Jordan%20survey%20report.pdf (accessed February 8, 2016).
31. Ghattas H, Francis S, El Mallah C, Shatila D, Merhi K, Hlais S, et al. Lebanese children are iodine deficient and urinary sodium and fluoride excretion are weak positive predictors of urinary iodine. Eur J Nutr. (2017) 56:749–55. doi: 10.1007/s00394-015-1120-x
32. Salamoun MM, Kizirian AS, Tannous RI, Nabulsi MM, Choucair MK, Deeb ME, et al. Low calcium and vitamin D intake in healthy children and adolescents and their correlates. Eur J Clin Nutr. (2005) 59:177–84. doi: 10.1038/sj.ejcn.1602056
33. WHO. Indicator Progress. (2016). Available online at: http://www.who.int/nutrition/indicator_progress.pdf (accessed November 12, 2022).
34. WHO. Noncommunicable Diseases Country Profiles 2018, 2018. (2018). Available online at: https://www.who.int/nmh/publications/ncd-profiles-2018/en/ (accessed November 9, 2022).
35. Choueiry G, Fattouh N, Hallit R, Kazour F, Hallit S. Nutritional status of lebanese hospitalized patients with chronic disease: a cross-sectional study. Hosp Pharm. (2021) 56:102–8. doi: 10.1177/0018578719867664
36. Mitri R, Boulos C, Adib SM. Determinants of the nutritional status of older adults in urban Lebanon. Geriatrics Gerontol Int. (2017) 17:424–32. doi: 10.1111/ggi.12732
37. El-Kassas G, Ziade F. The dual burden of malnutrition and associated dietary and lifestyle habits among lebanese school age children living in orphanages in North Lebanon. J Nutr Metab. (2017) 2017:4863431. doi: 10.1155/2017/4863431
38. UNHCR. UNHCR Lebanon: Fact Sheet. (2021). Available online at: https://reliefweb.int/report/lebanon/unhcr-lebanon-fact-sheet-september-2021 (accessed November 15, 2022).
39. Sibai AM, Sen K, Baydoun M. Population ageing in Lebanon: current status, future prospects and implications for policy. Bull World Health Organ. (2004) 82:219–25. doi: 10.1590/S0042-96862004000300012
40. Mercer T, Chang AC, Fischer L, Gardner A, Kerubo I, Tran DN, et al. Mitigating the burden of diabetes in Sub-Saharan Africa through an integrated diagonal health systems approach. Diab Metab Syndr Obes Targets Ther. (2019) 12:2261. doi: 10.2147/DMSO.S207427
41. Said L, Gubbels JS, Kremers SP. Effect evaluation of Sahtak Bi Sahnak, a Lebanese secondary school-based nutrition intervention: a cluster randomised trial. Front Nutr. (2022) 428:824020. doi: 10.3389/fnut.2022.824020
Keywords: COVID-19, food insecurity, double burden, malnutrition, Lebanon
Citation: Al Khatib A (2024) COVID-19, economic crisis, and food insecurity worsen the double burden of malnutrition in Lebanon. Front. Public Health 12:1333565. doi: 10.3389/fpubh.2024.1333565
Received: 21 December 2023; Accepted: 12 February 2024;
Published: 05 March 2024.
Edited by:
Carlo Pedrolli, Azienda Provinciale per i Servizi Sanitari (APSS), ItalyReviewed by:
Olutosin Ademola Otekunrin, Federal University of Agriculture, Abeokuta, NigeriaCopyright © 2024 Al Khatib. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alissar Al Khatib, YS5raGF0aWJAYWxtb29zYWNvbGxlZ2UuZWR1LnNh
 Alissar Al Khatib
Alissar Al Khatib