
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Public Health, 27 February 2024
Sec. Substance Use Disorders and Behavioral Addictions
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1331190
This article is part of the Research TopicExploring the Interaction between Health-promoting and Health Risk Behaviours in HealthView all 16 articles
 Harpreet Jaswal1,2,3
Harpreet Jaswal1,2,3 Ivneet Sohi1
Ivneet Sohi1 Jürgen Rehm1,2,3
Jürgen Rehm1,2,3 Samuel Churchill4
Samuel Churchill4 Adam Sherk4
Adam Sherk4 Tim Stockwell4
Tim Stockwell4 Christine Levesque5
Christine Levesque5 Nitika Sanger5
Nitika Sanger5 Hanie Edalati5
Hanie Edalati5 Peter R. Butt5
Peter R. Butt5 Catherine Paradis6
Catherine Paradis6 Kevin D. Shield1,2,3*
Kevin D. Shield1,2,3*Objective: To quantify and communicate risk equivalencies for alcohol-and tobacco-attributable mortality by comparing per standard drinks consumed to per number of cigarettes smoked in Canada.
Methods: Alcohol-and tobacco-attributable premature deaths (≤75 years of age) and years of life lost (YLL) were estimated using a lifetime risk modeling approach. Alcohol-attributable death statistics were obtained from the 2023 Canadian Guidance on Alcohol and Health data source. Tobacco-attributable death statistics were derived from the Mortality Population Risk Tool (MPoRT) model.
Results: The risk of alcohol use on premature death and YLL increased non-linearly with the number of drinks consumed, while the risk for tobacco use on these two measures increased linearly with the number of cigarettes smoked. Males who consumed 5 drinks/day—a standard drink contains 13.45 grams of alcohol in Canada—had an equivalent risk as smoking 4.9 cigarettes/day (when modeling for premature death) and 5.1 cigarettes/day (when modeling for YLL). Females who consumed 5 drinks/day experienced an equivalent risk as smoking 4.2 cigarettes/day for premature deaths and YLL. At all levels of alcohol consumption females and males who consumed <5 drinks/day have less risks from consuming a standard drink than from smoking a cigarette. For males who consumed 5 drinks/day, the increased risks of death from per drink consumed and per cigarette smoked were equal.
Conclusion: Risk equivalencies comparing alcohol use to tobacco use could help people who drink improve their knowledge and understanding of the mortality risks associated with increased number of drinks consumed per day.
Alcohol use is a causal risk factor for over 230 disease conditions based on the three-digit International Classification of Diseases, Revision 10 (ICD-10) codes (1). These health risks, however, are not always well understood by the public for a multitude of reasons. Studies have shown that people generally have difficulties understanding, evaluating, and communicating mortality risk associated with alcohol use (2). Although the general public tends to be aware of the protective effects of alcohol use on ischemic heart disease, ischemic stroke, and diabetes, especially for people who drink and who drink low amounts or do not engage in heavy episodic drinking (1), they, for the most part, are unaware of the many of the diseases that excessive alcohol consumption can cause (3, 4). For example, alcohol use is a leading cause of many forms of cancer and associated medical complications (1). Gaps in this knowledge is a major reason for why people often underestimate the risks of excessive drinking, and the catastrophic drinking patterns that often result. Providing information on the risk of alcohol use has been found to improve health literacy, decrease peoples’ intention to drink, and decrease the harms associated with alcohol consumption (5). Unfortunately, communicating this information about risks has not always been conducted effectively. As a prevention strategy, it is often underutilized by health and public health professionals.
People’s understanding of health risks related to alcohol use can be improved by communicating risk equivalencies. A ‘risk equivalency’ refers to a comparative assessment whereby different risks of health behaviors or related conditions are compared or evaluated so they can be expressed in terms of a common unit or metric — for an example, please see reference 6. Providing risk equivalency information can aid people in improving their understanding of the risks or health impacts they may experience acutely or over time from excessive alcohol use. Such information can also help individuals assess their situation(s) and prioritize their responses to alcohol availability. In contrast to alcohol use, the risk of tobacco use are well known to the general public (7–9). Various studies from different countries have shown that people are generally knowledgeable about diseases related to tobacco use and second-hand smoke exposure (10, 11). Because of this greater awareness about tobacco’s risks for harm, risk equivalencies can add value when communicating about risks associated with alcohol use — i.e., equating health loss or harm from standard drinks to health loss or harm from the number of cigarettes smoked. The present study uses Canadian data to address this gap in public health communication, by quantifying the risk equivalencies for alcohol and tobacco use. Premature death and years life lost (YLL) are the two main measures used to generate these equivalencies.
The lifetime risks of an alcohol- or tobacco-attributable death were operationalized using the risk of a premature death (i.e., a death which occurred among people 75 years of age and younger) and YLL. YLL were estimated based on the age of death and sex-specific lifetables for 2019, as obtained from Statistics Canada (12). This data source contained lifetables of probabilities on life expectancy and mortality for Canadians by age and sex.
Exposures to alcohol and tobacco were operationalized using different dimensions. For the present study alcohol use was operationalized as standard drinks consumed per week (in the analyses, this was converted to per day). In Canada, a standard drink comprises 13.45 grams of ethanol (13). Exposure to tobacco was operationalized as the average number of cigarettes smoked per day. To estimate alcohol-and tobacco-attributable deaths, and YLL a theoretical minimum risk exposure level (TMREL) for lifetime abstention was applied. No assumptions were made about the level of exposure for alcohol use that would result in the lowest risk of overall health loss or harm.
The lifetime risk estimates of an alcohol-attributable death and YLL were extracted using statistics from the 2023 Canadian Guidance on Alcohol and Health (see (14)). These 2023 statistics were used to generate alcohol use risks for people who consumed 0 to 5 drinks per day using a lifetime risk approach containing multiple steps and data sources (14, 15).
The first step in this approach was to estimate the number of cause-, sex- and age-specific alcohol-attributable deaths in Canada for 2019; this was carried out using a Levin-based population-attributable fraction method that combined data on alcohol exposure, relative risk estimates and mortality estimates (16, 17). The data on alcohol exposure were obtained from the Canadian Alcohol and Drug Use Monitoring Survey (CADUMS); the Canadian Tobacco, Alcohol and Drugs (CTADS) Survey; and Canada’s national statistical office, Statistics Canada (18). The data on the relative risk estimates were obtained from meta-analyses found in the literature (14). And the data on mortality estimates were obtained from the Statistics Canada Canadian Vital Statistics database (CVSD) (19).
The second step in the approach was to estimate the number of non-alcohol-attributable deaths in Canada (i.e., the deaths that would occur if no one person consumed alcohol); this was done by subtracting the number of alcohol-attributable deaths (estimated in the first step) from the total number of deaths. The number of non-alcohol-attributable deaths in Canada was subsequently divided by the population of Canada [via Statistics Canada (20)], yielding the risk measure for non-alcohol-attributable deaths - i.e., the risk of death among lifetime abstainers.
The third and final step in the approach was to estimate the lifetime risk of an alcohol-attributable death. To do this, the age- and sex-specific risks of an alcohol-attributable death (estimated in the second step) were summed across the life course (from age 15 years and onward). The age at which an alcohol-attributable death occurred was then used to estimate the alcohol-attributable YLL.
Because the lifetime risk of an alcohol-attributable death was characterized as a measure of public health impact, principally to provide guidance on alcohol use that is considered low risk, the modeling for the lifetime risk approach did not incorporate health loss or harm from causes such as alcohol poisoning, alcohol use disorders, or alcohol cardiomyopathy (14, 15). The latter condition, for instance, disproportionately affects people with alcohol use disorders and/or those who engage in heavy chronic drinking (21, 22). For additional information about how lifetime risks of premature death and the YLL attributable to alcohol were modeled, please see the Supplementary Material.
The lifetime risk of a tobacco-attributable death and YLL in Canada were modeled using data from the Mortality Population Risk Tool (MPoRT) (23). The MPoRT was developed and validated using 2001 to 2008 exposure data from the Canadian Community Health Surveys and mortality data from the Canadian Registered Persons Database (23). The MPoRT estimates the risk of death based on a person’s age, sex, neighborhood deprivation, education, immigration status, smoking, alcohol use, physical activity, body mass index, and presence of heart disease, stroke, cancer and/or diabetes. The age- and sex-specific risks of a tobacco-attributable death were estimated by comparing the risk of death for smokers and non-smokers. The age- and sex-specific risks of a tobacco-attributable death (estimated in step 2 of the approach) were summed across the life course to estimate the lifetime risk of this measure. The age at which a tobacco-attributable death occurred was used to estimate the tobacco-attributable YLL. To properly scale the lifetime risk of a tobacco-attributable death and the associated YLL per cigarette smoked, age-specific risks for tobacco use were divided by the average number of cigarettes smoked by Canadians. The average number of cigarettes smoked by Canadians per day among smokers, by sex, was obtained from the 2017 Canadian Tobacco, Alcohol and Drugs Survey (24). This estimate relied on the assumption that the relative risk of death based on the number of cigarettes smoked per day is linear, and that this assumption is consistent with the observations from large cohort studies in the literature (25, 26). Details about the MPoRT model can be found in the Supplementary Material.
The exposure equivalency ratio for each alcohol use category was determined by dividing the tobacco equivalency, which is the ratio of the number of cigarettes smoked to produce a similar health loss or harm for a person’s alcohol use, by that person’s number of drinks/day.
The 95% uncertainty intervals were based on a set of 1,000 simulations of all lowest level parameters (i.e., parameters sampled from their respective error distributions). These parameters were then utilized to estimate 1,000 simulated estimates. In these simulations, the 2.5th and 97.5th percentiles were the boundaries for the 95% uncertainty intervals (UIs).
As alcohol consumption increased, the equivalency ratio decreased for both males and females (Table 1; Figures 1, 2). For individuals who consumed 1 drink per day, each drink was equivalent to 0.4 cigarette smoked. For a male who consumes 5 drinks per day, the risk was equivalent to smoking 4.9 cigarettes per day. In other words, each drink was equivalent to one cigarette smoked. Similarly, for a female who consumes 5 drinks per day, the risk was equivalent to smoking 4.2 cigarettes per day (i.e., each drink was equivalent to 0.8 cigarette smoked). In all cases, evaluation of the risks were based on health loss or harm related to the two key study measures: premature death and YLL.
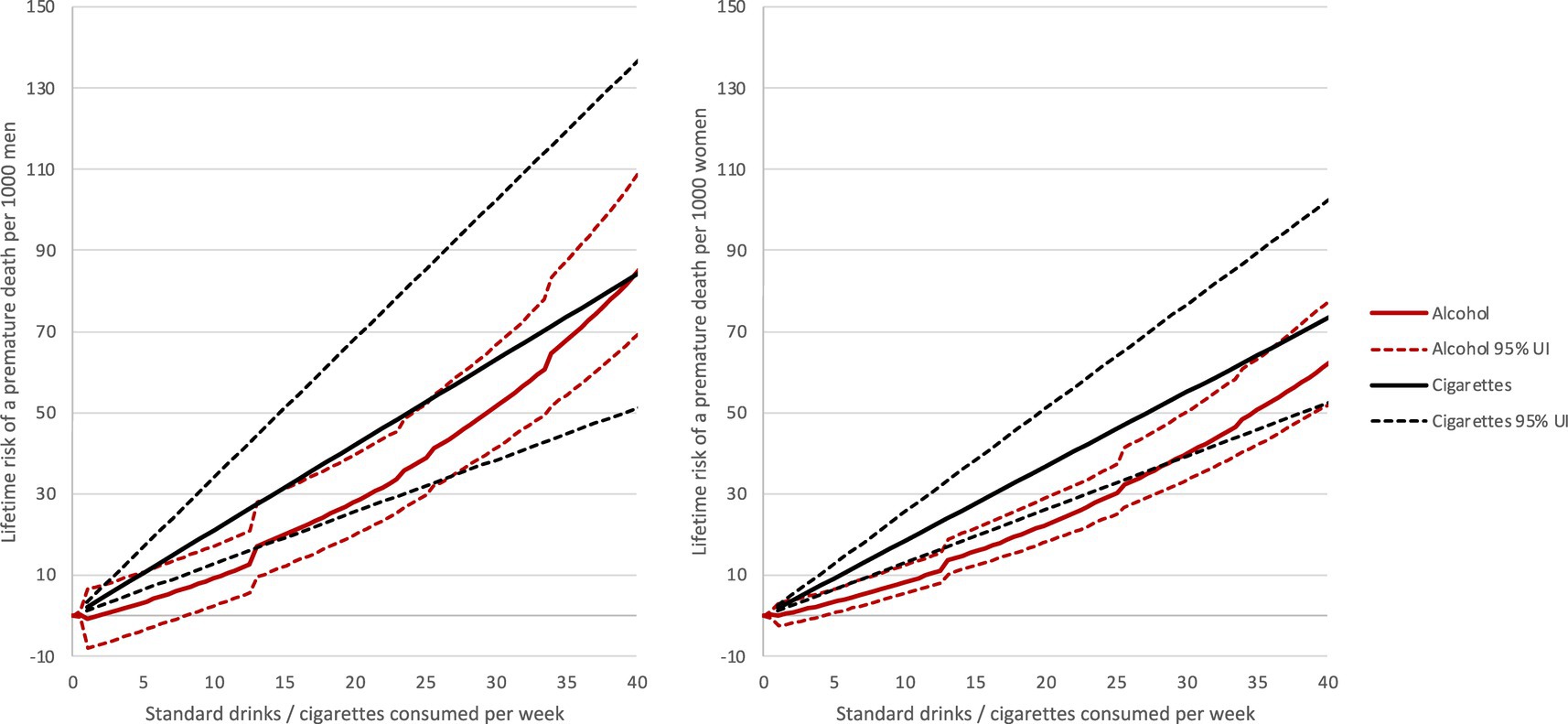
Figure 1. Lifetime deaths per 1,000 males and 1,000 females attributable to alcohol and tobacco use.
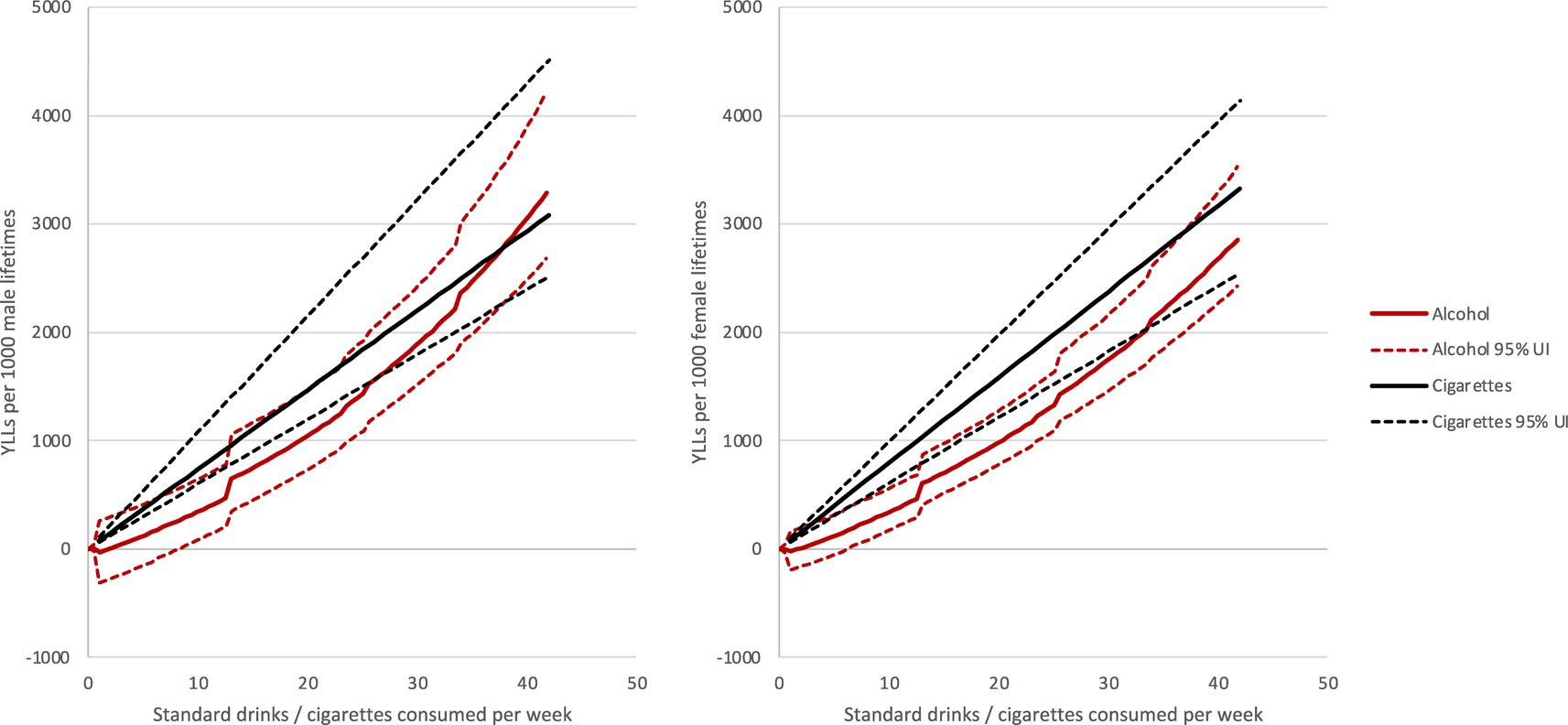
Figure 2. Years of life lost per 1,000 male and 1,000 female lifetimes attributable to alcohol and tobacco use.
The equivalency ratio for alcohol use and tobacco use varied by sex. For females, consuming a standard drink did not result in as much of a negative impact on health (e.g., loss or harm) as smoking a cigarette; this was true for all alcohol use categories examined. For males who consume fewer than 5 drinks per day, drinking a standard drink also did not result in as much of a negative impact on health as smoking a cigarette. For males who consume 5 drinks per day, the risk associated with alcohol use was equal to that of tobacco use.
Risk equivalencies were explored to characterize the risks associated with alcohol use among Canadians as compared to risks associated with tobacco use, expressed in terms of the number of cigarettes smoked. For both males and females, a negative association was observed between alcohol use and equivalency ratios, such that as the number of standard drinks increased, equivalency ratios decreased. This result implies that for males who consume less than 5 drinks per day, consuming alcohol was less of a risk for health loss than smoking cigarettes, whereas for females, in all alcohol use categories examined, the risks associated with consuming alcohol were lower than the risks associated with smoking cigarettes. The fluctuation in these exposure equivalency ratios is likely related to the daily amount of alcohol consumed, as this amount is directly correlated with the risk of health loss or harm per unit of alcohol used (27). In contrast, the number of cigarettes smoked daily does not necessarily alter this relationship to the risk of health loss or harm per cigarettes smoked (25, 26). In other words, the number of standard drinks consumed per day carries a dose-dependent effect that the number of cigarettes smoked daily do not.
Given the magnitude of risks associated with alcohol use, and the generally poor communication of these risks to the target populations alcohol-related health outcomes (they are generally poor) when expressed as a measure of the number of cigarettes smoked, could resonate substantively better with the public than just straight statistics about alcohol consumption’s harm. Currently, the general public is not as aware of what constitutes a standard drink, let alone having adequate knowledge about the guidance on what is daily or weekly low-risk drinking; suffice to say, misconceptions about alcohol use are plenty (5, 28, 29). By contrast, tobacco-related risks are very well known to the general public, due in part to the heavy stigma associated with them and the decades of public health counter-advertising levied against the tobacco industry and their sales of tobacco products (30). As such awareness about risks associated with alcohol use could be enhanced if the public health or medical community uses similar public health messaging tactics and/or field tested strategies proven to work when communicating these risks. In a previous study, researchers showed that consumers of alcohol would decrease their drinking if they were informed about alcohol-attributable risks or harms — e.g., the link between excessive drinking and cancer (5). These consumers would take action (decrease drinking) if they were incentivized and understood alcohol-attributable consequences in more familiar terms. Since tobacco use is associated with several diseases that are also related to alcohol consumption (e.g., cancer, cardiovascular diseases, liver disease), it has become an example to emulate for communications purposes (31). However, a one-to-one translation of tobacco control strategies to reducing alcohol use may not be entirely possible since tobacco is highly addictive, the mechanisms of addiction may be different from alcohol, and most mainstream tobacco control interventions typically advocate for complete cessation (32). The approach to alcohol use, on the other hand, often relies on a harm reduction perspective, especially for those with problem drinking but not in full dependency. Furthermore, alcohol and tobacco use often occur concurrently. Thus, when conveying risk equivalencies to alcohol users it may be necessary to exercise caution in how risks are presented so as to avoid normalizing or downplaying the health consequences of tobacco use.
Risk perceptions about alcohol and tobacco use can also be influenced by the following factors: perceived benefit, immediacy of effect, knowledge about the risk to the exposed person, certainty of the scientific information regarding the risk, control over risk, newness of the risk, the severity of the consequences, and the extent to which each of these behaviors are normalized in society (33). These, factors are particularly important to consider when communicating risks about these two different behaviors. For example, the risk perception about alcohol use frequently is complicated by the fact that drinking alcohol has both protective and detrimental effects on health. Previous studies have noted that at low levels of consumption, alcohol use has a protective effect on ischemic heart disease, ischemic stroke, and diabetes; however, at the same level of consumption, there could also be a detrimental effect on other diseases, such as cancer (1). Thus, to tease out these more nuanced health impacts of alcohol use — i.e., protective versus detrimental — more objective measures of burden could be used to communicate accurate facts about alcohol’s effects, as has been done in this present study, which used premature death and YLL as primary measures to quantify potential health loss or harm (risks) associated with alcohol use.
Finally, it is also important to take into consideration the levels of alcohol versus tobacco use when communicating public health information. There is a notable difference in the number of people who consume alcohol versus those who use tobacco products. For example, in 2019, 76% of Canadian adults consumed alcohol while only 12% of adults smoked cigarettes in the past year (34, 35). This difference in prevalence between the two behaviors suggests a normalization of alcohol use versus tobacco use, likely the result of alcohol’s historical significance, coupled with its role in religious rituals, social gatherings, and cultural traditions. These various factors may have perpetuated the use of alcohol in spite of its known risks or harms, and inhibited public health’s progress to reform this behavior (36). In contrast, decades of public health policies and campaigns have rendered tobacco use more unacceptable and represent factors that have lowered smoking prevalence in Canada and elsewhere around the world (37).
The risk equivalency estimates reported here have numerous limitations that should be considered. First, the presented risk equivalencies do not take into account the following factors which may interact with alcohol and tobacco: harms to others, disability, non-health harms, and differences in an person’s risk factors For example, both alcohol and tobacco carry risks for second-hand harms through non-user exposure—i.e., increased risk of alcohol-related injuries (e.g., motor vehicle accidents) or secondhand exposure due to drifting tobacco smoke (1, 38). Second-hand harms from alcohol and tobacco are both prevalent and difficult to avoid. They are dependent upon whether the exposure is acute or chronic. For instance second-hand harms from alcohol use are generally due to the intoxicating effects of the use (i.e., acute alcohol use) (1). Whereas second-hand harms through non-user exposure to tobacco smoke are generally not as acute, imparting a more cumulative effect over time (39). When communicating risks of these two substances, these indirect, second-hand harms, should be explained carefully, in conjunction with the more immediate, direct effects of their use.
Second, alcohol and tobacco have been noted to interact and share risk factors—e.g., and further interactions through co-use have been shown to exponentially increase the risk of head and neck cancers (1). Alcohol and tobacco use also tend to cluster with other chronic disease risks, such as high body mass index (BMI) (40). This clustering to other risks may be important to consider when formulating individualized treatment plans for patients with alcohol use disorders and tobacco dependence together. While some treatment programs may provide cigarettes as an incentive or reward in drug use treatment (41), this may be counterproductive (42). A systematic review found that in 16 out of 31 studies that examined pharmacological and psychotherapeutic alcohol use disorder treatments, being a non-smoker or having decreased tobacco consumption was significantly associated with reduced alcohol use (42). In stop-smoking studies, however, reduced smoking had no observable effect on drinking behaviors (42). In short, based on these results, treatment of alcohol use disorders may be more effective if tobacco addiction is also being treated concurrently.
Third and lastly, the data analysis and modeling employed in this study have several limitations. For example, the main analysis did not account for heavy drinking or patterns of drinking. Such indirect risks should be publicly communicated in addition to the direct harms experienced by users. Alcohol and tobacco use also contribute greatly to the risk of disability (43). Accordingly, the alcohol lifetime risk estimates are reflective of the patterns of drinking of the participants from the cohort and case–control studies that were used in the meta-analyses which reported cause-specific relative risk functions. There is evidence that drinking patterns affect the risk of infectious diseases (44), the risk of breast cancer (45), the risk of ischemic heart disease and ischemic stroke (46), the risk of diabetes (47), the risk of epilepsy (48), and the risk of injuries (49). Thus, if a person has a higher tendency to engage in heavy episodic drinking than the cohort and case–control participants, they would experience more health loss or harm than reported in the risk curves. If a person has a lower tendency to engage in heavy episodic drinking than the cohort and case–control participants, they will experience less health loss or harm than reported in the risk curves. The tendency to engage in heavy episodic drinking in the underlying cohort and case–control participants was not examined or reported in the meta-analyses.
As previously noted, the lifetime risk curves for alcohol were modeled for people who consume 0 to 5 standard drinks, these health loss or harms related to alcohol use would surpass those associated with tobacco use. It would be pertinent to explore this estimate, as it expands the utility of risk equivalency estimates in knowledge translation products—especially for people who are heavy chronic drinkers and people with alcohol use disorders.
The lifetime risk estimates for alcohol and tobacco use are derived using two different models, thereby limiting their comparability. Ideally, the risks of alcohol and tobacco use would be estimated using identical methods and data sources. The MPoRT model produces risk estimates for alcohol. These risk estimates are based on the reference group of non-drinkers and do not consider “sick quitters,” and therefore these risk estimates are biased and should not be used (17).
The data presented in this study are also based on population statistics for Canada. Therefore, the risks presented here apply to Canadians in general, but do not reflect the risks for specific Canadians. For example, for a person who consumes low amounts of alcohol, the risk of developing liver disease and dying from liver cirrhosis is highly dependent upon that person’s other risk factors, such as obesity and hepatitis infection (50). Canadians who are obese and/or have a hepatitis infection are at risk for death due to alcohol-attributable liver cirrhosis (i.e., a death that would not occur if the person abstained from alcohol); however, people without these co-occurring risk factors would not be at risk for death due to liver cirrhosis if they consumed small amounts of alcohol. Thus, it is important to note that the risk curves presented are for public health guidance, and are not meant to present health advice that is specific to a person.
The risk curves in this study only apply to people living in Canada. Risk curves for alcohol use were constructed using data from Canada, and are dependent upon the mortality risks of Canadians. Risk curves for tobacco use were based on the MPoRT model which is based on Canadian cohort data (23). Construction of risk curves for alcohol use is feasible for other countries around the world if there are data on alcohol use and mortality [(see 14, 15)]. Similarly, tobacco risk curves could be constructed if there is country-specific cohort data or region-specific cohort data. Both of these endeavors may be arduous for low- and middle-income countries where such data are sparse (51, 52).
The impacts of health risks from alcohol and tobacco use can be directly compared using standardized measurements of lifetime risk for premature death and YLL. While the equivalency estimates for alcohol and tobacco do not incorporate social harms, comparisons of alcohol to tobacco in standard units (number of drinks versus number of cigarettes) could provide alcohol users with a better understanding, in comparative terms, of the risks they partake when they drink.
Publicly available datasets were analyzed in this study. This data can be found at: 2022 Canadian Guidance on Alcohol and Health: https://www.ccsa.ca/sites/default/files/2022-08/CCSA-LRDG-Update-of-Canada%27s-LRDG-Final-report-for-public-consultation-en.pdf. MPoRT Model data: https://pubmed.ncbi.nlm.nih.gov/27529741/.
HJ: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. IS: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. JR: Conceptualization, Investigation, Writing – review & editing. SC: Formal analysis, Methodology, Writing – review & editing. AS: Formal analysis, Investigation, Methodology, Writing – review & editing. TS: Conceptualization, Investigation, Methodology, Writing – review & editing. CL: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. NS: Data curation, Investigation, Methodology, Writing – review & editing. HE: Data curation, Investigation, Methodology, Writing – review & editing. PB: Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. CP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KS: Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Funding for this study was provided to KS by the Canadian Centre on Substance Use and Addiction.
We extend our gratitude to Rachel Visontay for their contributions in meticulously editing the journal article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1331190/full#supplementary-material
1. Rehm, J, Gmel, GE Sr, Gmel, G, Hasan, OS, Imtiaz, S, Popova, S, et al. The relationship between different dimensions of alcohol use and the burden of disease—an update. Addiction. (2017) 112:968–1001. doi: 10.1111/add.13757
2. Galesic, M, and Garcia-Retamero, R. Statistical numeracy for health: a cross-cultural comparison with probabilistic national samples. Arch Intern Med. (2010) 170:462–8. doi: 10.1001/archinternmed.2009.481
3. Lin, W. Knowledge of the health consequences of heavy alcohol consumption among individuals with different substance use statuses: a cross-sectional analysis of 2019 HINT survey. Chronic Illn. (2023). doi: 10.1177/17423953231213853
4. Buykx, P, Li, J, Gavens, L, Hooper, L, Lovatt, M, Gomes de Matos, E, et al. Public awareness of the link between alcohol and cancer in England in 2015: a population-based survey. BMC Public Health. (2016) 16:1–12. doi: 10.1186/s12889-016-3855-6
5. Vallance, K, Stockwell, T, Zhao, J, Shokar, S, Schoueri-Mychasiw, N, Hammond, D, et al. Baseline assessment of alcohol-related knowledge of and support for alcohol warning labels among alcohol consumers in northern Canada and associations with key sociodemographic characteristics. J Stud Alcohol Drugs. (2020) 81:238–48. doi: 10.15288/jsad.2020.81.238
6. Chen, J. Canadian lung cancer relative risk from radon exposure for short periods in childhood compared to a lifetime. Int J Environ Res Public Health. (2013) 10:1916–26. doi: 10.3390/ijerph10051916
7. Evans, AT, Peters, E, Strasser, AA, Emery, LF, Sheerin, KM, and Romer, D. Graphic warning labels elicit affective and thoughtful responses from smokers: results of a randomized clinical trial. PLoS One. (2015) 10:e0142879. doi: 10.1371/journal.pone.0142879
8. Rutten, LJF, Augustson, EM, Moser, RP, Beckjord, EB, and Hesse, BW. Smoking knowledge and behavior in the United States: sociodemographic, smoking status, and geographic patterns. Nicotine Tob Res. (2008) 10:1559–70. doi: 10.1080/14622200802325873
9. Roberts, B, Stickley, A, Gilmore, AB, Danishevski, K, Kizilova, K, Bryden, A, et al. Knowledge of the health impacts of smoking and public attitudes towards tobacco control in the former Soviet Union. Tob Control. (2013) 22:e12-e. doi: 10.1136/tobaccocontrol-2011-050249
10. Minh An, DT, Van Minh, H, Huong, LT, Bao Giang, K, Thanh Xuan, LT, Thi Hai, P, et al. Knowledge of the health consequences of tobacco smoking: a cross-sectional survey of Vietnamese adults. Glob Health Action. (2013) 6:18707–9. doi: 10.3402/gha.v6i0.18707
11. Petersen, AB, Thompson, LM, Dadi, GB, Tolcha, A, and Cataldo, JK. An exploratory study of knowledge, attitudes, and beliefs related to tobacco use and secondhand smoke among women in Aleta Wondo. Ethiopia BMC Women Health. (2018) 18:1–10. doi: 10.1186/s12905-018-0640-y
12. Statistics Canada. Life tables, Canada, provinces and territories, catalogue no. 84-537-X. Ottawa, Canada: Statistics Canada (2021).
13. Schoueri-Mychasiw, N, Weerasinghe, A, Stockwell, T, Vallance, K, Hammond, D, Greenfield, TK, et al. Use as directed: do standard drink labels on alcohol containers help consumers drink (ir) responsibly? Real-world evidence from a quasi-experimental study in Yukon. Canada Drug Alcohol Rev. (2021) 40:247–57. doi: 10.1111/dar.13165
14. Shield, K, Churchill, S, Sherk, A, Stockwell, T, Lévesque, C, Sanger, N, et al. Lifetime risk of alcohol-attributable death and disability. Ottawa, Canada: Canadian Centre on Substance Use and Addiction (2023).
15. Shield, KD, Gmel, G, Gmel, G, Mäkelä, P, Probst, C, Room, R, et al. Life-time risk of mortality due to different levels of alcohol consumption in seven European countries: implications for low-risk drinking guidelines. Addiction. (2017) 112:1535–44. doi: 10.1111/add.13827
17. Rehm, J, Irving, H, Ye, Y, Kerr, WC, Bond, J, and Greenfield, TK. Are lifetime abstainers the best control group in alcohol epidemiology? On the stability and validity of reported lifetime abstention. Am J Epidemiol. (2008) 168:866–71. doi: 10.1093/aje/kwn093
18. Statistics Canada. Table 10-10-0010-01 Sales of alcoholic beverages types by liquor authorities and other retail outlets, by value, volume, and absolute volume. Ottawa, Canada: Statistics Canada (2021).
19. Statistics Canada. Canadian vital statistics-death database. Ottawa, Canada: Statistics Canada (2021).
20. Statistics Canada. Table 17-10-0005-01; population estimates on July 1st, by age and sex. Ottawa, Canada: Statistics Canada (2021).
21. Peterson, K. Biomarkers for alcohol use and abuse: a summary. Alcohol Res Health. (2004) 28:30–7.
22. Lazarević, AM, Nakatani, S, Nešković, AN, Marinković, J, Yasumura, Y, Stojičić, D, et al. Early changes in left ventricular function in chronic asymptomatic alcoholics: relation to the duration of heavy drinking. J Am Coll Cardiol. (2000) 35:1599–606. doi: 10.1016/S0735-1097(00)00565-9
23. Manuel, DG, Perez, R, Sanmartin, C, Taljaard, M, Hennessy, D, Wilson, K, et al. Measuring burden of unhealthy behaviours using a multivariable predictive approach: life expectancy lost in Canada attributable to smoking, alcohol, physical inactivity, and diet. PLoS Med. (2016) 13:e1002082. doi: 10.1371/journal.pmed.1002082
24. Statistics Canada. Canadian tobacco, alcohol and drugs survey (CTADS) 2018. Ottawa, Ontario: Statistics Canada (2018).
25. Thun, MJ, Carter, BD, Feskanich, D, Freedman, ND, Prentice, R, Lopez, AD, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. (2013) 368:351–64. doi: 10.1056/NEJMsa1211127
26. Pirie, K, Peto, R, Reeves, GK, Green, J, Beral, V, and Collaborators, MWS. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet. (2013) 381:133–41. doi: 10.1016/S0140-6736(12)61720-6
27. Rehm, J, Rovira, P, Llamosas-Falcón, L, and Shield, KD. Baseline assessment of alcohol-related knowledge of and support for alcohol warning labels among alcohol consumers in northern Canada and associations with key sociodemographic characteristics. Nutrients. (2021) 13:2652. doi: 10.3390/nu13082652
28. Buykx, P, Gilligan, C, Ward, B, Kippen, R, and Chapman, K. Public support for alcohol policies associated with knowledge of cancer risk. Int J Drug Policy. (2015) 26:371–9. doi: 10.1016/j.drugpo.2014.08.006
29. Canadian Centre on Substance Use and Addiction. Update of Canada’s low-risk alcohol drinking guidelines: Summary of findings from public consultation. Ottawa, Canada: Canadian Centre on Substance Use and Addiction (2021).
30. Hammett, P, Fu, SS, Nelson, D, Clothier, B, Saul, JE, Widome, R, et al. A proactive smoking cessation intervention for socioeconomically disadvantaged smokers: the role of smoking-related stigma. Nicotine Tobacco Res. (2018) 20:286–94. doi: 10.1093/ntr/ntx085
31. Larsson, SC, and Burgess, S. Appraising the causal role of smoking in multiple diseases: a systematic review and meta-analysis of Mendelian randomization studies. EBioMedicine. (2022) 82:104154. doi: 10.1016/j.ebiom.2022.104154
32. Rodu, B, and Godshall, WT. Tobacco harm reduction: an alternative cessation strategy for inveterate smokers. Harm Reduct J. (2006) 3:37–23. doi: 10.1186/1477-7517-3-37
33. Fischhoff, B, Slovic, P, Lichtenstein, S, Read, S, and Combs, B. How safe is safe enough? A psychometric study of attitudes towards technological risks and benefits. Policy Sci. (1978) 9:127–52. doi: 10.1007/BF00143739
34. Statistics Canada. Canadian tobacco, alcohol and drugs survey (CTADS) 2019. Ottawa, Ontario: Statistics Canada (2019).
35. Statistics Canada. Canadian tobacco and nicotine survey 2019. Ottawa, Canada: Statistics Canada (2019).
36. Sudhinaraset, M, Wigglesworth, C, and Takeuchi, DT. Social and cultural contexts of alcohol use: influences in a social–ecological framework. Alcohol Res. (2016) 38:35–45.
37. Kelly, BC, Vuolo, M, Frizzell, LC, and Hernandez, EM. Denormalization, smoke-free air policy, and tobacco use among young adults. Soc Sci Med. (2018) 211:70–7. doi: 10.1016/j.socscimed.2018.05.051
38. Naeem, Z. Second-hand smoke–ignored implications. Int J Health Sci. (2015) 9:V–vi. doi: 10.12816/0024103
39. Asomaning, K, Miller, DP, Liu, G, Wain, JC, Lynch, TJ, Su, L, et al. Second hand smoke, age of exposure and lung cancer risk. Lung Cancer. (2008) 61:13–20. doi: 10.1016/j.lungcan.2007.11.013
40. Alamian, A, and Paradis, G. Clustering of chronic disease behavioral risk factors in Canadian children and adolescents. Prev Med. (2009) 48:493–9. doi: 10.1016/j.ypmed.2009.02.015
41. Centers for Disease Control and Prevention. People with behavioral health conditions encounter barriers to quitting successfully. Atlanta, United States of America: Centers for Disease Control and Prevention (2023).
42. van Amsterdam, J, and van den Brink, W. Smoking as an outcome moderator in the treatment of alcohol use disorders. Alcohol Alcohol. (2022) 57:664–73. doi: 10.1093/alcalc/agac027
43. Institute of Health Metrics and Evaluation. GBD Results Tool. Seattle, USA: Institute of Health Metrics and Evaluation (2021).
44. Romeo, J, Wärnberg, J, and Marcos, A. Drinking pattern and socio-cultural aspects on immune response: an overview. Proc Nutr Soc. (2010) 69:341–6. doi: 10.1017/S0029665110001904
45. Shield, KD, Soerjomataram, I, and Rehm, J. Alcohol use and breast cancer: a critical review. Alcohol Clin Exp Res. (2016) 40:1166–81. doi: 10.1111/acer.13071
46. Roerecke, M, and Rehm, J. Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Med. (2014) 12:182. doi: 10.1186/s12916-014-0182-6
47. Holst, C, Becker, U, Jørgensen, ME, Grønbæk, M, and Tolstrup, JS. Alcohol drinking patterns and risk of diabetes: a cohort study of 70, 551 men and women from the general Danish population. Diabetologia. (2017) 60:1941–50. doi: 10.1007/s00125-017-4359-3
48. Alldredge, BK, and Lowenstein, DH. Status epilepticus related to alcohol abuse. Epilepsia. (1993) 34:1033–7. doi: 10.1111/j.1528-1157.1993.tb02130.x
49. Cherpitel, CJ, Witbrodt, J, Ye, Y, and Korcha, R. A multi-level analysis of emergency department data on drinking patterns, alcohol policy and cause of injury in 28 countries. Drug Alcohol Depend. (2018) 192:172–8. doi: 10.1016/j.drugalcdep.2018.07.033
50. Roerecke, M, Vafaei, A, Hasan, OSM, Chrystoja, BR, Cruz, M, Lee, R, et al. Alcohol consumption and risk of liver cirrhosis: a systematic review and meta-analysis. Am J Gastroenterol. (2019) 114:1574–86. doi: 10.14309/ajg.0000000000000340
51. Williams, J, Allen, L, Wickramasinghe, K, Mikkelsen, B, Roberts, N, and Townsend, N. A systematic review of associations between non-communicable diseases and socioeconomic status within low-and lower-middle-income countries. J Glob Health. (2018) 8:409. doi: 10.7189/jogh.08.020409
Keywords: alcohol use, tobacco use, Canada, mortality metrics, guidance on alcohol and health
Citation: Jaswal H, Sohi I, Rehm J, Churchill S, Sherk A, Stockwell T, Levesque C, Sanger N, Edalati H, Butt PR, Paradis C and Shield KD (2024) A drink equals how many cigarettes? Equating mortality risks from alcohol and tobacco use in Canada. Front. Public Health. 12:1331190. doi: 10.3389/fpubh.2024.1331190
Received: 01 November 2023; Accepted: 22 January 2024;
Published: 27 February 2024.
Edited by:
Huixuan Zhou, Beijing Sport University, ChinaReviewed by:
Tony Kuo, University of California, Los Angeles, United StatesCopyright © 2024 Jaswal, Sohi, Rehm, Churchill, Sherk, Stockwell, Levesque, Sanger, Edalati, Butt, Paradis and Shield. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kevin D. Shield, S2V2aW4uU2hpZWxkQGNhbWguY2E=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.