- 1Shaanxi University of Chinese Medicine, Xianyang, China
- 2The Second Affiliated Hospital of Shaanxi University of Chinese Medicine, Xianyang, China
Objective: With increasing rates of anxiety and depression during COVID-19, exercise treatment has drawn attention for its effects on COVID-19 patients with anxiety and depression. This study set out to assess the impact of exercise therapy on COVID-19 patients’ anxiety and depression.
Methods: PubMed, EMBASE, Web of Science and Cochrane Library were used to search articles about exercise therapy as a means of treating anxiety and depression in COVID-19 patients from inception to April 30, 2023. The risk of bias was assessed by the Cochrane Collaboration bias risk tool. Data were pooled with the random effects model. RevMan version 5.4 was used for the statistical analyses. This work was registered in the PROSPERO database (registration number: CRD42023406439).
Selection criteria: Randomized clinical trials (RCTs) of COVID-19 patients with anxiety and depression were included to assess the impact of physical exercise on COVID-19 patients with anxiety and depression.
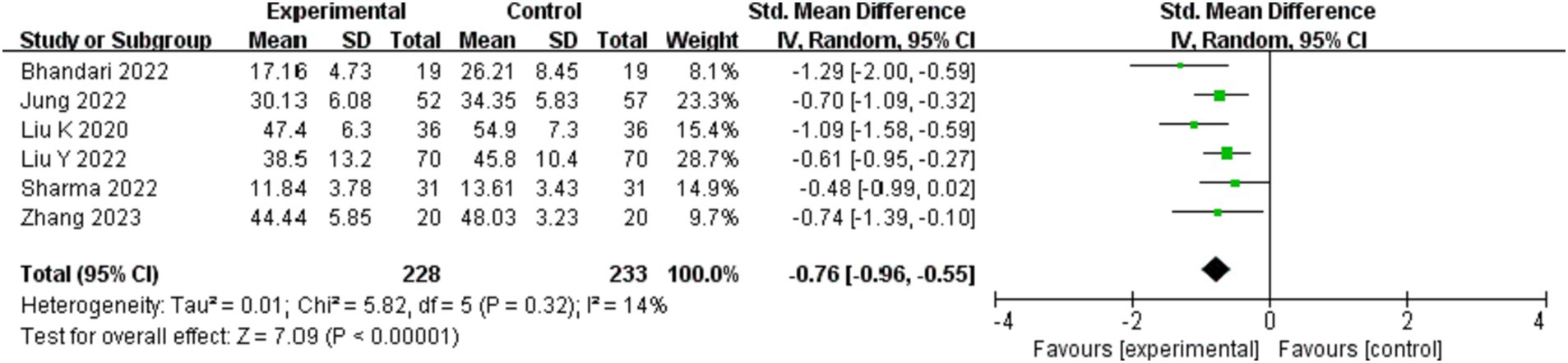
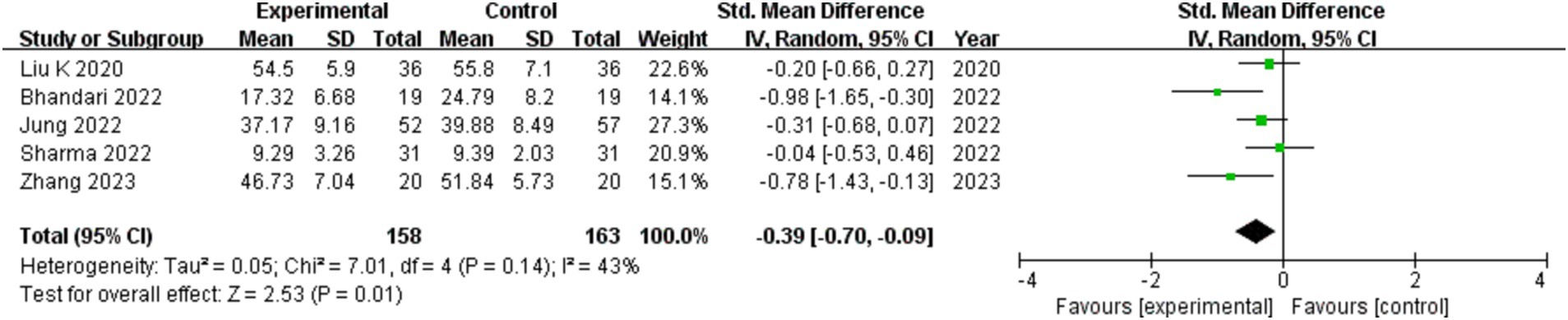
Results: 6 studies including a total of 461 COVID-19 patients were analyzed in this meta-analysis. Overall, the meta-analysis showed that compared with the control group, exercise could significantly improve anxiety (SMD = −0.76; 95%CI: −0.96, −0.55; p < 0.00001), depression level (SMD = −0.39; 95%CI: −0.70, −0.09; p = 0.01), the PHQ-9 score (MD = −1.82; 95%CI: −2.93, −0.71; p = 0.001) and the sleep quality (SMD = −0.73; 95%CI: −1.32, −0.14; p = 0.01) in COVID-19 patients.
Conclusion: The research provided evidence that exercise therapy is able to help COVID-19 patients experience less anxiety and depression and have better-quality sleep.
Systematic review registration: CRD42023406439.
Introduction
The novel coronavirus SARS-CoV-2 caused a febrile respiratory sickness outbreak, which swiftly led to a global outbreak known as coronavirus disease 2019 (COVID-19) (1, 2). The WHO estimates that there are currently over 760 million infected COVID-19 and over 6 million fatalities worldwide (3). To date, there is no specific therapy established to treat COVID-19 and only symptomatic treatment can alleviate the symptoms, but it is unable to keep up with the rate of mutation (4). In particular, the appearance of the Omicron variant BA.1 has presented a rigorous challenge in the fight against COVID-19 (5). COVID-19 in addition to seriously jeopardizing the physical and mental health of COVID-19 patients, it caused severe morbidity, mortality, and financial stress for families and society (6).
Both depression and anxiety are severe neurological illnesses that may lead to suicidal thoughts and self-inflicted injury, as well as impairing memory and sleep. Globally, the COVID-19 epidemic has a profound psychological impact. Studies have shown that patients with COVID-19 had a markedly elevated chance of acquiring mental health issues, especially anxiety and depression. The total prevalence of anxiety and the total prevalence of depression were over 40% (7–9). Despite the fact that there are currently effective medications for depression or anxiety, many individuals do not benefit from them, find them intolerable, or get withdrawal symptoms when the medication is stopped (10). In recent years, many people who suffer from depression or anxiety turn to unconventional and non-pharmacological therapies (11). A randomized controlled trial showed that young people hospitalized to mental hospitals for anxiety and depression benefit both physically and psychologically from physical exercise (12). Exercise may offer individuals with COVID-19 and anxiety and depression a flexible, easy-to-use, and promising therapeutic option. The clinical evidence hierarchy is headed by a systematic review and meta-analysis (13). For the purpose of providing a reference for treating health crises brought on by post-COVID-19 anxiety and depression, this study will carry out a meta-analysis and systematic review to look into the impacts of exercise therapy in treating anxiety and depression produced by COVID-19.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) criteria were followed in the conduct of this meta-analysis (14). And the PRISMA-Checklist is added in the Supplement.
Search strategy
This study searched articles about RCTs that the impacts of exercise therapy on COVID-19 patients with anxiety and depression in the online databases of PubMed, EMBASE, Web of Science and Cochrane Library from inception to April 30, 2023. We devised search techniques that blended free-text phrases containing people with COVID-19, depression, anxiety, exercise treatment, and randomized clinical trials (RCTs) with medical subject categories. The search strategy used in each database is shown in Supplementary File S1.
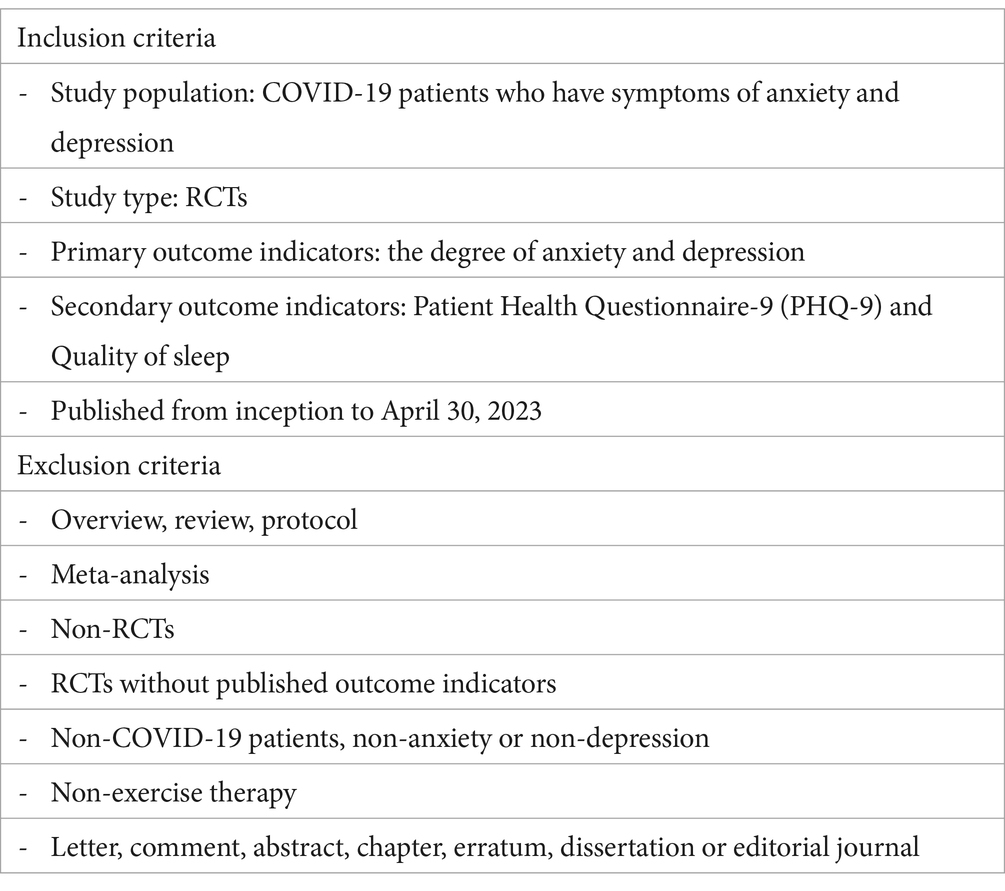
Inclusion criteria and exclusion criteria
Interventions
Patients in the experimental group were treated by exercise therapy. The comparison groups involve other treatments except exercise therapy.
Outcome
The main results were the degree of anxiety and depression, with scores changing during treatment. Anxiety was assessed by the Self-Rating Anxiety Scale (SAS), the Hamilton Anxiety Rating Scale (HAM-A), State Anxiety Inventory (SAI), Generalized Anxiety Disorder Scale-7 Item (GAD-7), Hospital Anxiety and Depression Scale (HADS). Depression was assessed by the HADS, Self-Rating Depression Scale (SDS), Beck Depression Inventory (BDI). Secondary outcomes were Patient Health Questionnaire-9 (PHQ-9) and Quality of sleep.
Study selection
The studies are independently reviewed and screened by two reviewers (JT and HZ) in accordance with the review’s inclusion and exclusion criteria. To exclude duplicate articles, the reviewers used EndNote X9 software. They then study the article titles and abstracts to weed out any plainly irrelevant material. They next read the complete contents of the remaining publications, filter them, and justify the exclusion of the researches that were not qualified. Disputes were resolved through discussing with the third reviewer (L-LC).
Data collection and analysis
Independently, after reading the literature, two reviewers (PW and L-LC) took the data out of the studies that were included. Each study’s details, such as the publication year, first author, sample size, participant age, intervention, control, treatment plan, and primary outcome, were among the data that were gathered. In cases where there was a disagreement between the two reviewers throughout the screening process, the judgment was ultimately made after consulting a third reviewer (FM).
Risk of bias analysis of included studies
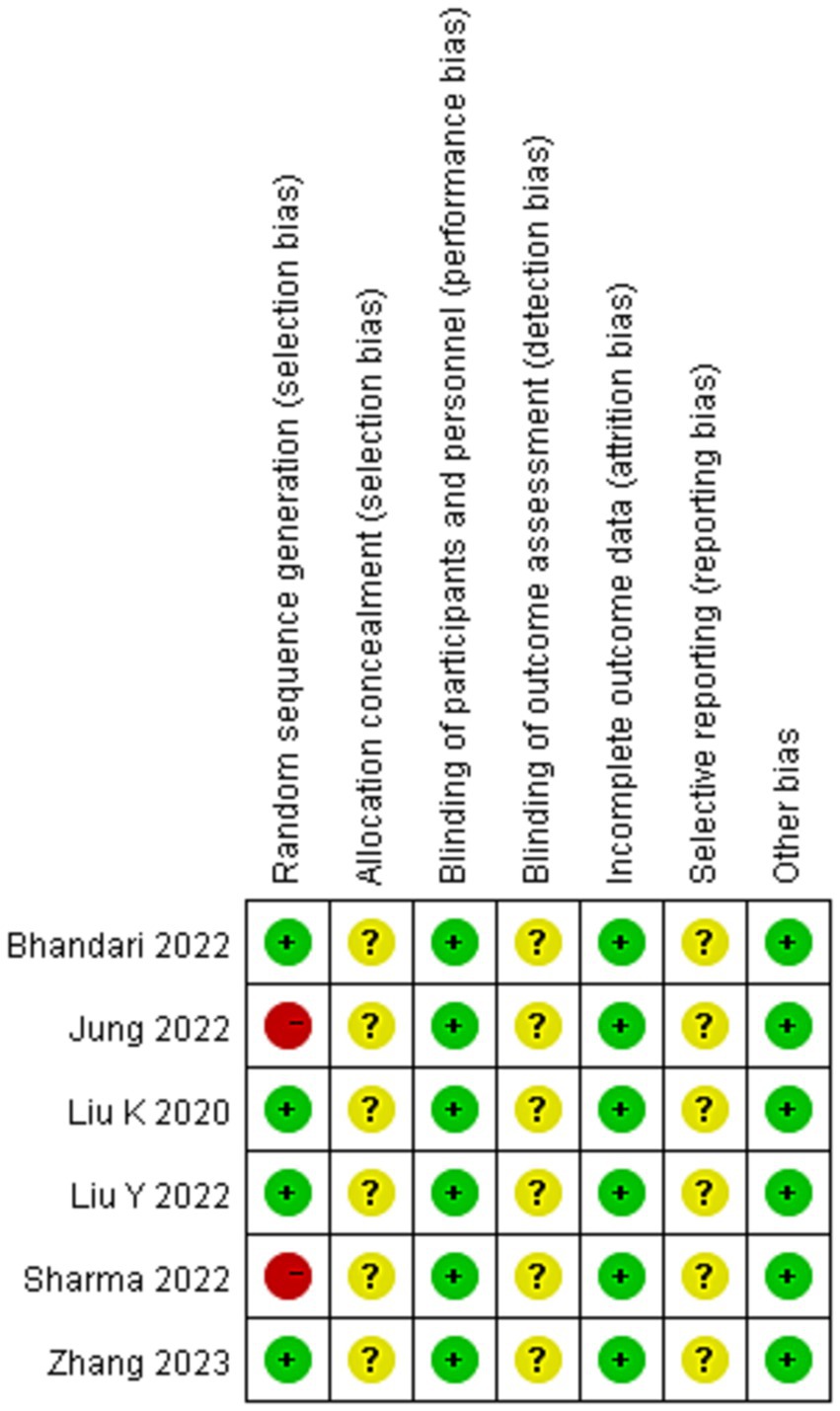
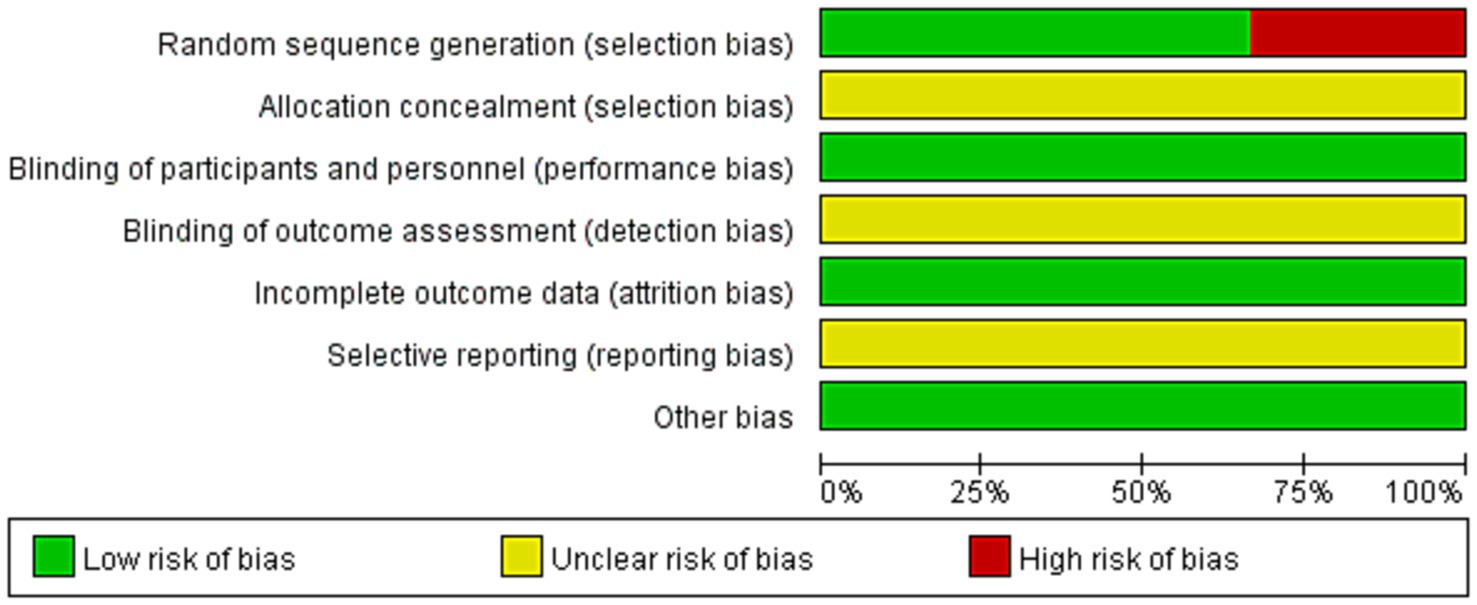
Two researchers (PW and L-LC) used the seven-item Cochrane Collaboration Risk of Bias assessment to independently assess the methodological quality of the literature (15). Each component’s bias risk was evaluated, and the findings were divided into three risk categories: low risk of bias, unclear risk of bias and high risk of bias and then the risk of bias assessment was plotted by Review Manager 5.4 software.
Data analysis
RevMan version 5.4 was used to analyze the statistical. Continuous outcomes were analyzed using MD or SMD with a 95% CI, and the SMD statistic was selected when the outcome was assessed using different scales. Data were pooled with the random effects model. The assessment of study heterogeneity was conducted using I2 statistic measurements. If I2 < 25%, will be considered as no significant heterogeneity. I2 is between 25 and 50%, will be considered as moderate heterogeneity. I2 > 50% will be considered as significant heterogeneity. When I2 ≥ 25%, subgroup analysis was performed to identify the source of any clinical heterogeneity seen in the pooled findings.
Results
Study selection and basic characteristics
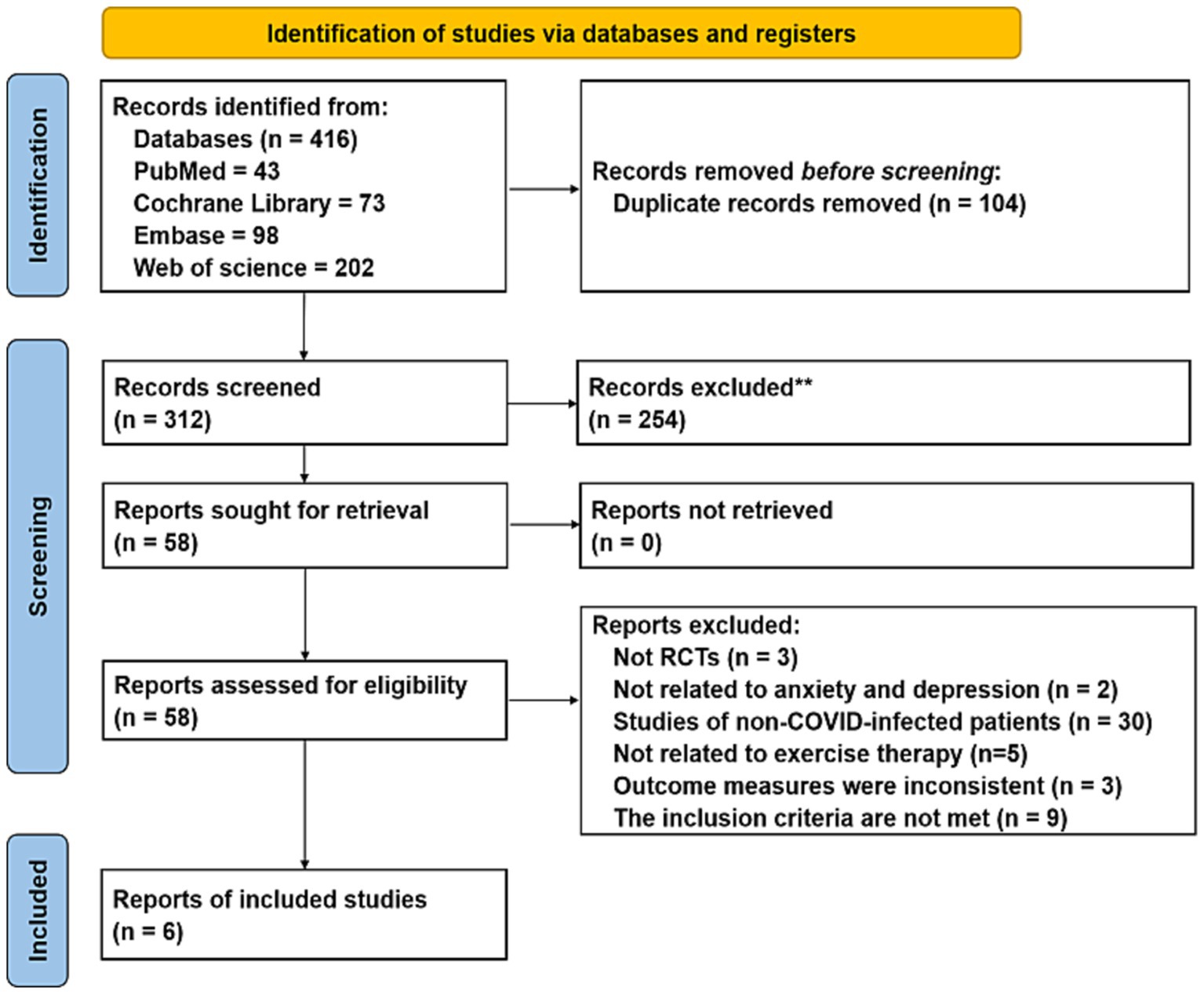
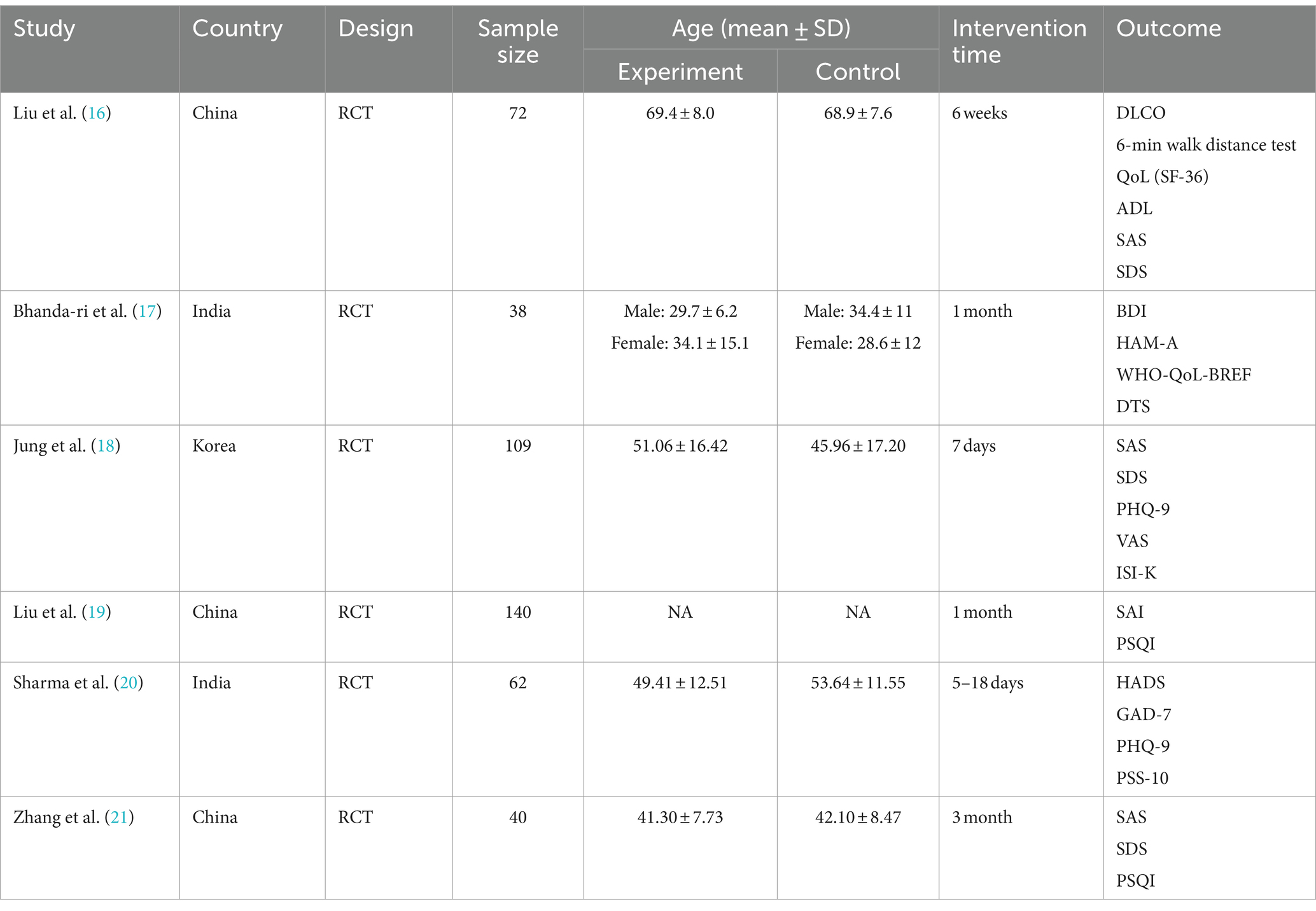
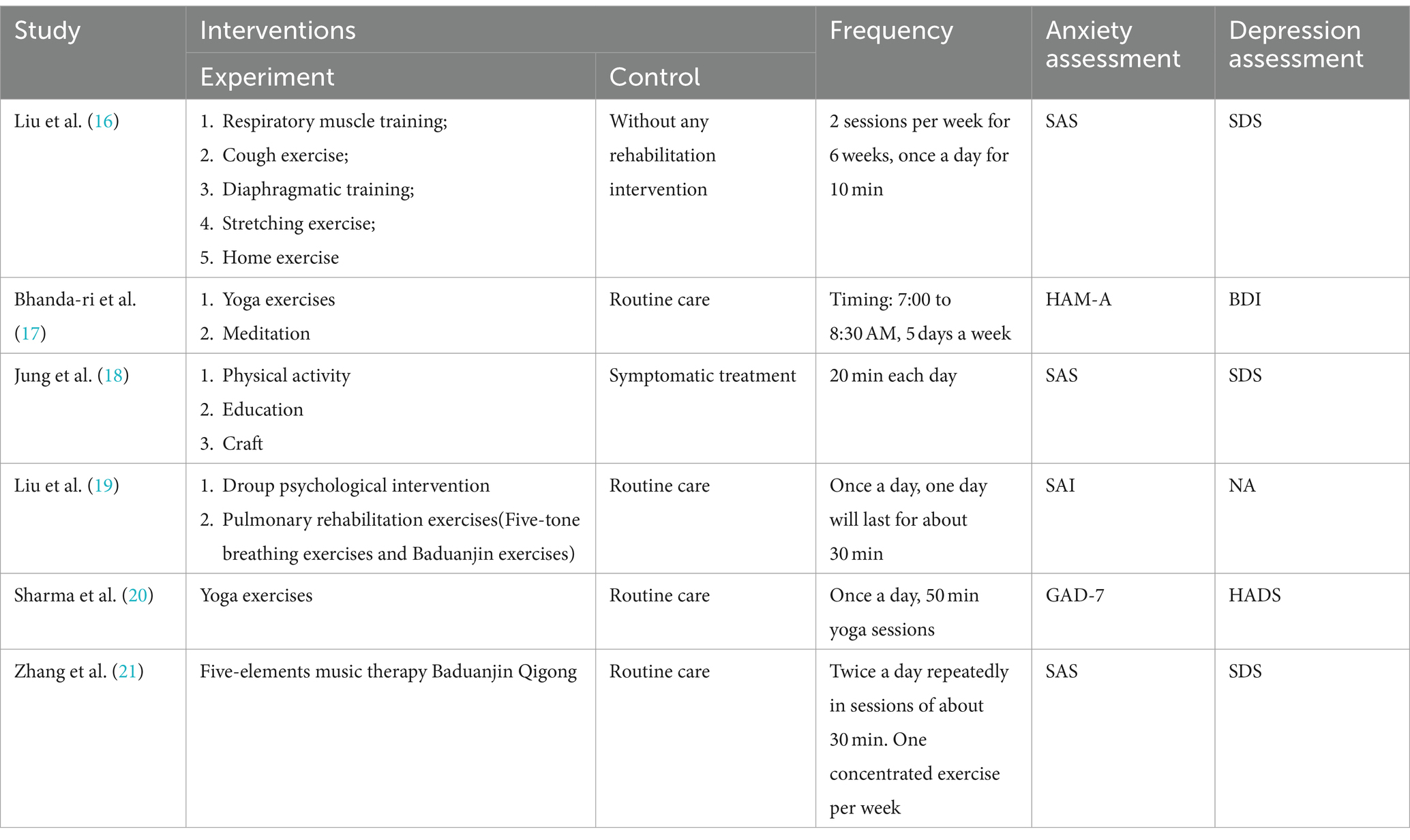
4 electronic databases were searched, yielding a total of 416 documents. 104 duplicate articles were eliminated. The titles and abstracts of these papers led to the exclusion of 294 citations. 12 researches were eliminated due to their failure to meet the qualifying requirements, leaving 18 papers that passed the full-text examination. Figure 1 illustrates how the remaining 6 RCTs, which had 461 individuals, fulfilled the eligibility requirements. Table 1 provides a summary of the baseline characteristics of the six trials.
Risk of bias assessment
All studies (16–21) mentioned randomly divided, due to Jung et al. (18) divided groups according to their bed number and Sharma’s study was a quasi-randomized study were assessed high risk of bias. None of the studies had sufficient information to judge whether to perform allocation scheme concealment and blinding of outcome evaluators were unclear risk of bias. Included studies were treated for exercise therapy, and for RCTs, the outcome indicators were not affected by allocation concealment, so all studies were low risk of bias. The outcome data for all study were complete were low risk. None of all studies had sufficient information to assess the risk of selective reporting were unclear risk of bias. No other potential sources of bias in all studies were low risk of bias (show in Figures 2, 3).
Primary outcomes
Anxiety level
Six studies (16–21) involving 461 participants examined how exercise therapy affected COVID-19 patients’ anxiety. Anxiety was measured using the SAS, HAM-A, SAI, HADS, and GAD-7. Due to the wide range of dimensions, the study employed SMD to aggregate the data on anxiety symptoms. The meta-analysis shows that, in comparison to the control group, the intervention group significantly improved the anxiety levels of COVID-19 patients overall (SMD = −0.76; 95%CI: −0.96, −0.55; p < 0.00001), the difference was statistically significant (show in Figure 4).
Depression level
321 participants in five studies (16–18, 20, 21) assessed how exercise therapy affected COVID-19 patients’ depression. The investigation employed SMD to compile the data on depression symptoms using assessment techniques such as SDS, BDI, and HADS. The comprehensive data showed that, overall, the treatment group outperformed the control group in improving COVID-19 patient depression symptoms (SMD = −0.39; 95%CI: −0.70, −0.09; p = 0.01), the difference was statistically significant (show in Figure 5).
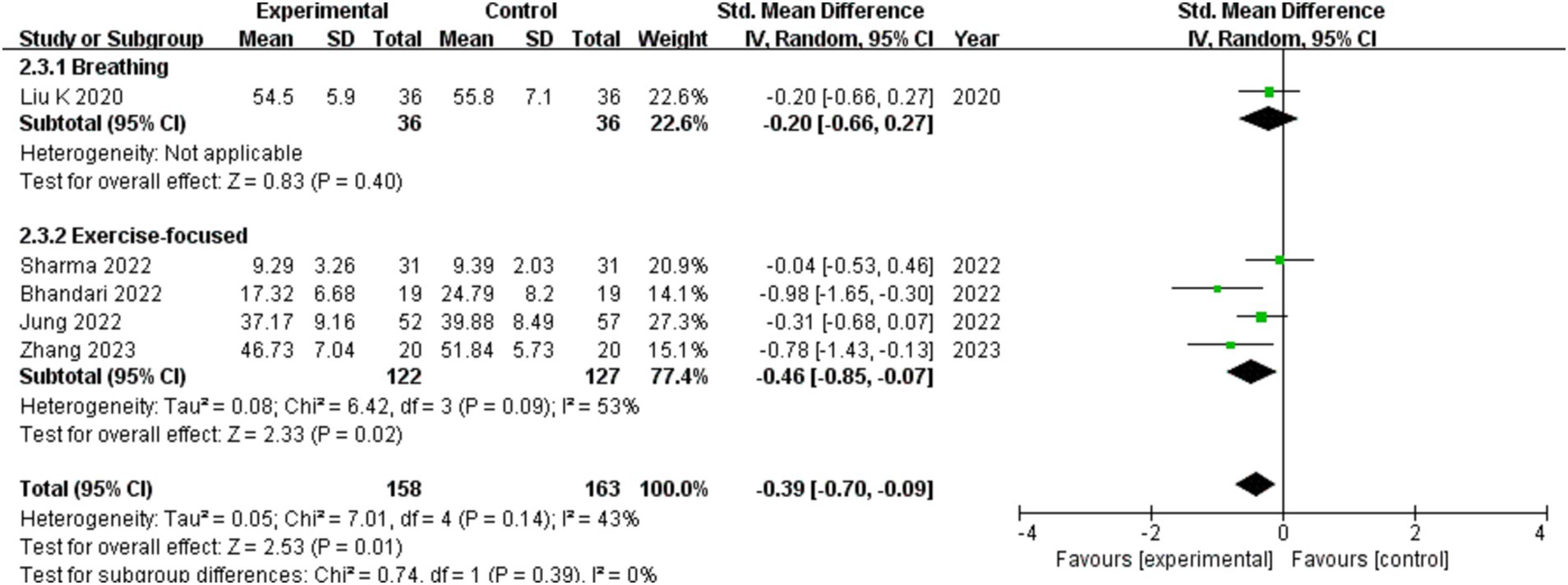
Subgroup analysis
The treatment time is split into two categories: less than 1 month and more than 1 month, depending on how long the intervention is. The treatment group and the control group differ from one another, as seen by the results from different intervention durations. Subgroup distinctions exist, and in contrast to the control group, individuals with COVID-19 can experience improved depression with more than a month of exercise therapy (show in Figure 6).
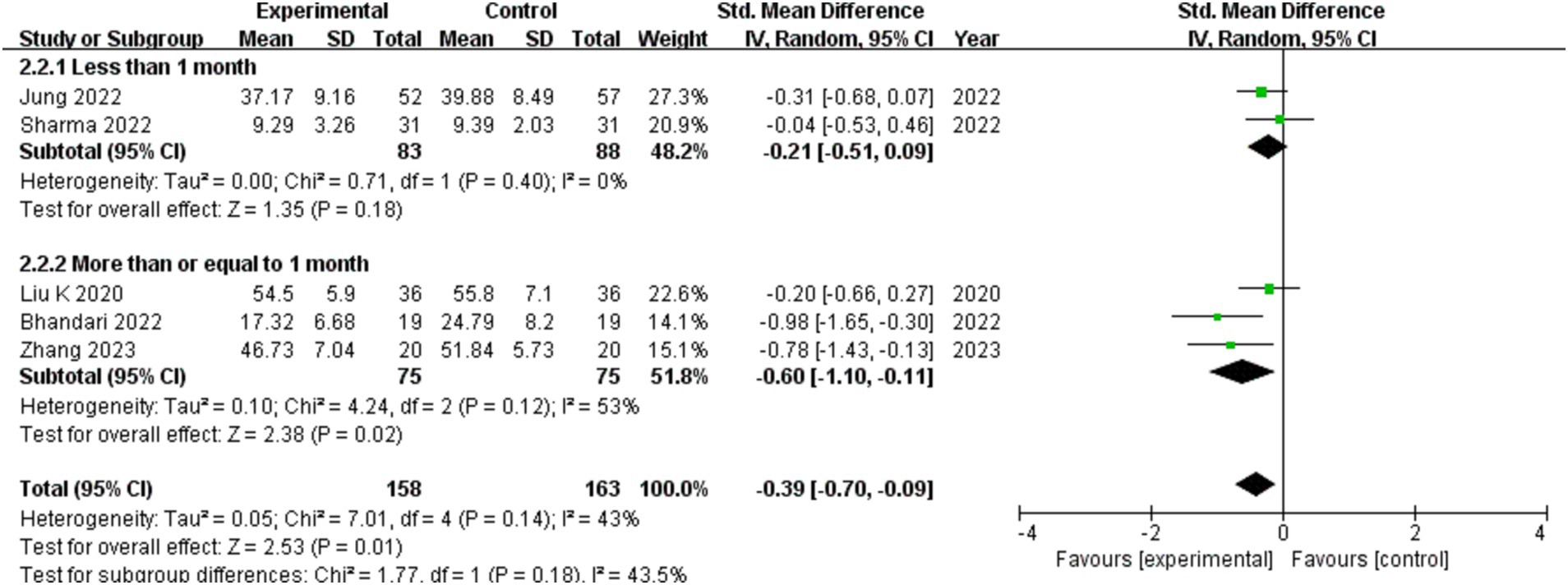
Figure 6. The effect of different of the length of intervention on depression in patients with COVID-19.
One on respiratory motion study reached no conclusions. Four exercise-focused studies suggesting that there are subgroup differences, and exercise-focused exercise therapy can help COVID-19 patients who are depressed compared with the control group. Comprehensive outcomes of various intervention types demonstrate that the experimental group and the control group differ from one another (show in Figure 7).
Secondary outcomes
PHQ-9
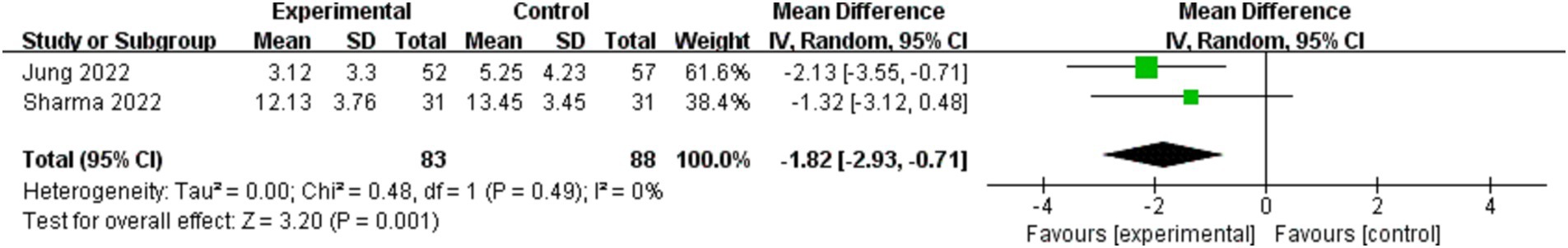
According to DSM-IV criteria, the PHQ-9 is a standard screening tool used to identify depression. It is an accurate and reliable indicator of the severity of depression (22). The intended outcome, PHQ-9, was reported in two studies (18, 20). The intervention group significantly outperformed the control group in terms of improving PHQ-9 score (MD = −1.82; 95%CI: −2.93, −0.71; p = 0.001), a statistically significant difference was present (show in Figure 8).
Quality of sleep
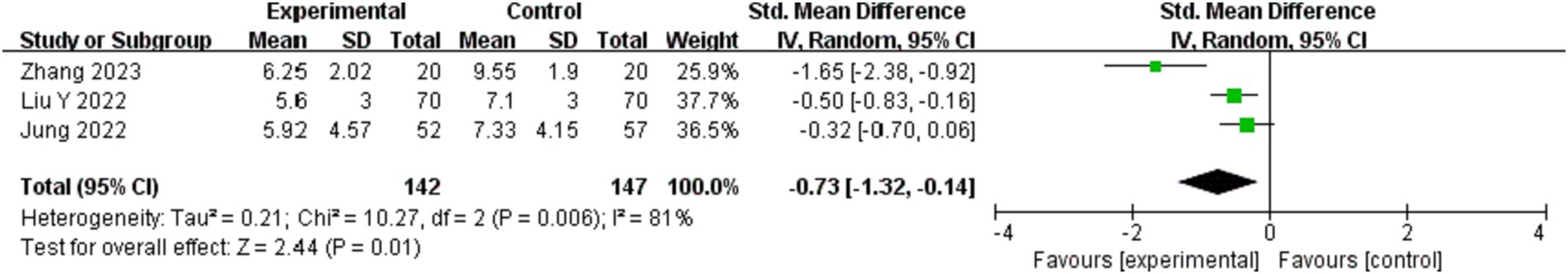
There were 4 studies that reported on the patients’ sleep quality, and since the data from 1 study was insufficient, 3 studies (18, 19, 21) were included. Quality of sleep was assessed by the PSQI and ISI-K. The data on depressive symptoms were combined by the study using SMD. The findings indicate a noteworthy distinction in the improvement of sleep quality between the intervention group and the control group (SMD = −0.73; 95%CI: −1.32, −0.14; p = 0.01), the difference was statistically significant (show in Figure 9).
Conclusion
For this study, the effects of exercise therapy on depression and anxiety were evaluated in six trials with a total of 461 COVID-19 participants. When compared to the control group, the intervention group significantly improved COVID-19 patients’ anxiety overall. When compared to the control group, the intervention group showed improvements in the depressed symptoms of COVID-19 patients. This study conducted subgroup analysis because the total results were quite statistically diverse. The findings indicated that depression could be improved with more than a month of exercise therapy, and that depression could be improved with activity-focused exercise therapy when compared to the control group in COVID-19 patients. Patients with COVID-19 may have improvements in their PHQ-9 and sleep quality with exercise therapy. In conclusion, our study discovered evidence to suggest that exercise therapy significantly improves anxiety and depression in COVID-19 patients.
The form of exercise in this study had an impact on exercise therapy to treat depression in patients, and Table 2 lists the various strategies used in each study. The impact of breathing-based exercise on depression in COVID-19 patients did not differ statistically; all other exercise modalities effectively reduced depressive symptoms in these individuals. Among other things, the genre of literature and the sample size of the included literature may have an impact on this finding. Second, the set of changes achieved was not necessarily entirely due to exercise because five of the six included trials were multimodal therapies with an emphasis on exercise therapy. In certain research, secondary outcome indicators for anxiety and depression may have affected the results.
Discussion
Currently, there are no existing licensed anti-viral therapies, so non-pharmaceutical therapies continue to be essential for COVID-19 management (23). Increased rates of mental illness, depression, anxiety, self-harm, and suicide have been linked to the COVID-19 pandemic (24, 25). Depression and anxiety are serious public health problems. It is estimated that around 20–40% of patients who experience depressive episodes do not respond clinically to the antidepressant treatments now being used, furthermore, around half of the patients who get symptom amelioration still have persistent symptoms that impair their functioning and raise the risk of relapse (26). Furthermore, 76–85% of those suffering from mental illnesses get no therapy at all, which has a detrimental effect on the individuals, their families, and society (27). Studies have shown that mental illnesses make about 2% of all diseases worldwide. Study show that from 2010 to 2030, the estimated $2.5 trillion in treatment costs are predicted to have increased to $6 trillion (28). The prevalence of anxiety and depression has increased significantly, and new treatments are urgently needed because there is still a high failure rate in the treatment of these conditions, which poses a serious threat to people’s mental health, particularly in the context of the long-term COVID-19 (29, 30). Research on anxiety and depression in COVID-19 patients has gained international attention since these conditions have a serious negative impact on patients’ and their families’ physical and emotional well-being throughout the pandemic. Furthermore, studies have shown that the COVID-19 pandemic may promote depression, anxiety symptoms, including children and adolescents (31, 32). And all types of physical activity among children and adolescents had a precipitous decline during the COVID-19 pandemic (33).
According to this study, exercise therapy could reduce anxiety and depressive symptoms in patients with COVID-19. It is well known that physical activity is good for both physical and mental health (34). When compared to psychotherapy and medicine, exercise therapy offers numerous advantages in terms of cost, side effects, and additional health benefits. It may produce results that are similar to those of psychotherapy and pharmacology (35). A study demonstrates that engaging in sport-based activities, whether solo or in a group setting, can reduce anxiety. Moreover, a higher frequency of physical activity is linked to reduced levels of melancholy and anxiety (36).
Exercise can reduce the symptoms of anxiety and depression through a variety of mechanisms. Increased oxidative stress and inflammation have been associated with depression and anxiety disorders (37–39), glucocorticoid release, overload of immune, anabolic and cardiovascular functions and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, (40, 41) imbalance of intestinal flora (42) and so on in several studies and meta-analyses. Beheshti et al. found that Lipopolysaccharide (LPS)-induced depression- and anxiety-like behaviors were linked to the oxidative damage and neuroinflammation status of braintissues and the anti-LPS effects of amino guanidine included a decrease in inflammatory cytokines, a decrease in oxidative stress and a rise in anti-inflammatory mediators (43). Angulo et al. mentioned that exercise lowers oxidative damage and chronic inflammation, boosts autophagy, and enhances mitochondrial function (44). Wang et al. study found that aerobic exercise could decrease malondialdehyde (MDA), myeloperoxidase (MPO) levels and levels of IL-1β, TNF-α, and TGF-β in mice, supported that aerobic exercise was more effective in reducing cell apoptosis, oxidative stress damage, and the inflammatory response (45). Research indicates that exercise treatment can impact the HPA axis, which is crucial for mood and cognition, and can lower levels of inflammatory cytokines (46). According to Ghannoum et al., an imbalance in the gut flora had a number of detrimental outcomes, such as imbalance of neurotransmitter levels and neuronal circuits, excessive production of proinflammatory cytokines in the immunological system, disruption of the intestinal barrier, and hyper activation of the HPA axis (47). Exercise has been demonstrated by Xia et al. to modify gut microbiota and improve malfunctioning gut-brain axis (48). Exercise increases the diversity of intestinal microorganisms, enriches good bacteria, and increases the number of butyrate-producing intestinal microbes, according to research by Du et al. These benefits are linked to improved health status (49). Overall, the effects of exercise on microbiota have been reported, mostly to improve colon health by increasing microbiota diversity and balancing the populations of harmful and helpful bacteria.
Exercise therapy can be effectively implemented in clinical practice because, according to this study, it can reduce the symptoms of anxiety and depression following COVID-19. It is also more acceptable than oral medication and aids patients’ recovery with better compliance. In addition to the COVID-19, there are many epidemics such as HIV, tuberculosis (TB) and so on, which can also promote depression, anxiety symptoms (50–52). Exercise therapy can be used in future pandemics which promote depression and anxiety symptoms.
Limitations of the study
The limited number of publications included in this analysis is the first of its many shortcomings. Second, SMD was used in the analysis of the results due to the large number of various anxiety-depression-related rating scales that were used in the collected literature. The age in the third included study was primarily concentrated over 40 years, which may restrict the generalizability of the findings. Extensive high-quality randomized controlled trials are necessary to ascertain whether exercise therapy is beneficial in treating anxiety and depression in COVID-19 patients, especially those with varying age ranges. There is not enough information to determine how exercise treatment alone affects anxiety and depression in COVID-19 patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
JT: Writing – original draft. L-LC: Writing – review & editing. HZ: Writing – review & editing. PW: Writing – review & editing. FM: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by Shaanxi Provincial Administration of Chinese Medicine “Double Chain Integration” Middle-aged and Young Research Innovation Team Project (No. 2022-SLRH-YQ-008), Shaanxi University of Chinese Medicine Clinical Medicine Excellence Discipline Team Building Project (No. 104-1720201024), Shaanxi University of Chinese Medicine Innovative Team Project for Research on the Theory of Medicinal Properties of Chinese Medicine under Grant (No. 2020XKTD-A04), Science and Technology Research and Development Program of Xianyang Municipality (No. 2021ZDYF-SF-0044).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1330521/full#supplementary-material
Abbreviations
RCTs, Randomized controlled trials; SMD, Standard mean difference; MD, Mean difference; COVID-19, Coronavirus disease 2019; SAS, Self-Rating Anxiety Scale; HAM-A, Hamilton Anxiety Rating Scale; SAI, State Anxiety Inventory; GAD-7, Generalized Anxiety Disorder Scale-7 Item; HADS, Hospital Anxiety and Depression Scale; SDS, Self-Rating Depression Scale; BDI, Beck Depression Inventory; PHQ-9, Patient Health Questionnaire-9; LPS, Lipopolysaccharide.
References
1. Hui, DS, I Azhar, E, Madani, TA, Ntoumi, F, Kock, R, Dar, O, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health – The latest 2019 Novel coronavirus outbreak in Wuhan, China. Int J Infect Diseases. (2019) 91:264–6. doi: 10.1016/j.ijid.2020.01.009
2. Wu, JT, Leung, K, and Leung, GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. (2020) 395:689–97. doi: 10.1016/S0140-6736(20)30260-9
3. WHO. WHO Coronavirus (COVID-19) Dashboard. Accessed June 21, 2023. Available at: https://covid19.who.int/
4. Han, F, Liu, Y, Mo, M, Chen, J, Wang, C, Yang, Y, et al. Current treatment strategies for COVID-19 (review). Mol Med Rep. (2021) 24:858. doi: 10.3892/mmr.2021.12498
5. Araf, Y, Akter, F, Tang, YD, Fatemi, R, Parvez, MSA, Zheng, C, et al. Omicron variant of SARS-CoV-2: genomics, transmissibility, and responses to current COVID-19 vaccines. J Med Virol. (2022) 94:1825–32. doi: 10.1002/jmv.27588
6. George, TK, Sharma, P, Joy, M, Seelan, G, Sekar, A, Gunasekaran, K, et al. The economic impact of a COVID-19 illness from the perspective of families seeking care in a private hospital in India. Dialog Health. (2023) 2:100139. doi: 10.1016/j.dialog.2023.100139
7. Schou, TM, Joca, S, Wegener, G, and Bay-Richter, C. Psychiatric and neuropsychiatric sequelae of COVID-19 – a systematic review. Brain Behav Immun. (2021) 97:328–48. doi: 10.1016/j.bbi.2021.07.018
8. Pérez-Cano, HJ, Moreno-Murguía, MB, Morales-López, O, Crow-Buchanan, O, English, JA, Lozano-Alcázar, J, et al. Anxiety, depression, and stress in response to the coronavirus disease-19 pandemic. Cir Cir. (2020) 88:562–8. doi: 10.24875/CIRU.20000561
9. Deng, J, Zhou, F, Hou, W, Silver, Z, Wong, CY, Chang, O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
10. Goodwin, GM, and Stein, DJ. Generalised anxiety disorder and depression: contemporary treatment approaches. Adv Ther. (2021) 38:45–51. doi: 10.1007/s12325-021-01859-8
11. Saeed, SA, Cunningham, K, and Bloch, RM. Depression and anxiety disorders: benefits of exercise, yoga, and meditation. Am Fam Physician. (2019) 99:620–7.
12. Philippot, A, Dubois, V, Lambrechts, K, Grogna, D, Robert, A, Jonckheer, U, et al. Impact of physical exercise on depression and anxiety in adolescent inpatients: a randomized controlled trial. J Affect Disord. (2022) 301:145–53. doi: 10.1016/j.jad.2022.01.011
13. Izzo, AA, Hoon-Kim, S, Radhakrishnan, R, and Williamson, EM. A critical approach to evaluating clinical efficacy, adverse events and drug interactions of herbal remedies. Phytother Res. (2016) 30:691–700. doi: 10.1002/ptr.5591
14. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10:89. doi: 10.1186/s13643-021-01626-4
15. Sterne, JAC, Savović, J, Page, MJ, Elbers, RG, Blencowe, NS, Boutron, I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
16. Liu, K, Zhang, W, Yang, Y, Zhang, J, Li, Y, and Chen, Y. Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract. (2020) 39:101166. doi: 10.1016/j.ctcp.2020.101166
17. Bhandari, R. Online yoga and Ayurveda intervention as tertiary prevention of psychological comorbidities in COVID-19 survivors: a randomized controlled trial. Ann Neurosci. (2022) 29:233–44. doi: 10.1177/09727531221117623
18. Jung, JH, Won, JJ, and Ko, JY. Psychological rehabilitation for isolated patients with COVID-19 infection: a randomized controlled study. PLoS One. (2022) 17:e0278475. doi: 10.1371/journal.pone.0278475
19. Liu, Y, Yang, YQ, Liu, Y, Pei, SL, Yang, HH, Wu, JJ, et al. Effects of group psychological intervention combined with pulmonary rehabilitation exercises on anxiety and sleep disorders in patients with mild coronavirus disease 2019 (COVID-19) infections in a Fangcang hospital. Psychol Health Med. (2022) 27:333–42. doi: 10.1080/13548506.2021.1916956
20. Sharma, N, Sahni, PS, Sharma, US, Kumar, J, and Garg, R. Effect of yoga on the stress, anxiety, and depression of COVID-19-positive patients: a quasi-randomized controlled study. Int J Yoga Ther. (2022) 32:e13. doi: 10.17761/2022-D-22-00013
21. Zhang, H, Yin, L, Peng, Y, Zhang, G, Chen, Q, Liang, J, et al. Effect of five-elements music therapy combined with Baduanjin qigong on patients with mild COVID-19. Hong Kong J Occup Ther. (2023) 36:31–8. doi: 10.1177/15691861231167536
22. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
23. Heymann, DL, and Shindo, N. COVID-19: what is next for public health? Lancet. (2020) 395:542–5. doi: 10.1016/S0140-6736(20)30374-3
24. Zhu, J, Yalamanchi, N, Jin, R, Kenne, DR, and Phan, N. Investigating COVID-19’s impact on mental health: trend and thematic analysis of Reddit Users’ discourse. J Med Internet Res. (2023) 25:e46867. doi: 10.2196/46867
25. Penninx, B, Benros, ME, Klein, RS, and Vinkers, CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. (2022) 28:2027–37. doi: 10.1038/s41591-022-02028-2
26. Touloumis, C. The burden and the challenge of treatment-resistant depression. Psychiatrike. (2021) 32:11–4. doi: 10.22365/jpsych.2021.046
27. Wolf, S, Seiffer, B, Zeibig, JM, Welkerling, J, Brokmeier, L, Atrott, B, et al. Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? A rapid systematic review. Sports Med. (2021) 51:1771–83. doi: 10.1007/s40279-021-01468-z
28. Marquez, PV, and Saxena, S. Making mental health a global priority. Cerebrum Dana Forum Brain Sci. (2016) 2016:e10-16.
29. Sikorska, M, Antosik-Wójcińska, AZ, and Dominiak, M. Probiotics as a tool for regulating molecular mechanisms in depression: a systematic review and meta-analysis of randomized clinical trials. Int J Mol Sci. (2023) 24:3081. doi: 10.3390/ijms24043081
30. Mazza, MG, Palladini, M, Poletti, S, and Benedetti, F. Post-COVID-19 depressive symptoms: epidemiology, pathophysiology, and pharmacological treatment. CNS Drugs. (2022) 36:681–702. doi: 10.1007/s40263-022-00931-3
31. Ludwig-Walz, H, Dannheim, I, Pfadenhauer, LM, Fegert, JM, and Bujard, M. Anxiety increased among children and adolescents during pandemic-related school closures in Europe: a systematic review and meta-analysis. Child Adolesc Psychiatry Ment Health. (2023) 17:74. doi: 10.1186/s13034-023-00612-z
32. Ludwig-Walz, H, Dannheim, I, Pfadenhauer, LM, Fegert, JM, and Bujard, M. Increase of depression among children and adolescents after the onset of the COVID-19 pandemic in Europe: a systematic review and meta-analysis. Child Adolesc Psychiatry Ment Health. (2022) 16:109. doi: 10.1186/s13034-022-00546-y
33. Ludwig-Walz, H, Siemens, W, Heinisch, S, Dannheim, I, Loss, J, and Bujard, M. How the COVID-19 pandemic and related school closures reduce physical activity among children and adolescents in the WHO European region: a systematic review and meta-analysis. Int J Behav Nutr Phys Activity. (2023) 20:149. doi: 10.1186/s12966-023-01542-x
34. Salman, D, Vishnubala, D, Le Feuvre, P, Beaney, T, Korgaonkar, J, Majeed, A, et al. Returning to physical activity after covid-19. BMJ. (2021) 372:m4721. doi: 10.1136/bmj.m4721
35. Singh, B, Olds, T, Curtis, R, Dumuid, D, Virgara, R, Watson, A, et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Br J Sports Med. (2023) 57:1203–9. doi: 10.1136/bjsports-2022-106195
36. McMahon, EM, Corcoran, P, O’Regan, G, Keeley, H, Cannon, M, Carli, V, et al. Physical activity in European adolescents and associations with anxiety, depression and well-being. Eur Child Adolesc Psychiatry. (2017) 26:111–22. doi: 10.1007/s00787-016-0875-9
37. Black, CN, Bot, M, Scheffer, PG, Cuijpers, P, and Penninx, BW. Is depression associated with increased oxidative stress? A systematic review and meta-analysis. Psychoneuroendocrinology. (2015) 51:164–75. doi: 10.1016/j.psyneuen.2014.09.025
38. Ren, Y, Sun-Waterhouse, D, Ouyang, F, Tan, X, Li, D, Xu, L, et al. Apple phenolic extracts ameliorate lead-induced cognitive impairment and depression- and anxiety-like behavior in mice by abating oxidative stress, inflammation and apoptosis via the miR-22-3p/SIRT1 axis. Food Funct. (2022) 13:2647–61. doi: 10.1039/D1FO03750A
39. Patki, G, Solanki, N, Atrooz, F, Allam, F, and Salim, S. Depression, anxiety-like behavior and memory impairment are associated with increased oxidative stress and inflammation in a rat model of social stress. Brain Res. (2013) 1539:73–86. doi: 10.1016/j.brainres.2013.09.033
40. Stetler, C, and Miller, GE. Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom Med. (2011) 73:114–26. doi: 10.1097/PSY.0b013e31820ad12b
41. Westfall, S, Caracci, F, Zhao, D, Wu, QL, Frolinger, T, Simon, J, et al. Microbiota metabolites modulate the T helper 17 to regulatory T cell (Th17/Treg) imbalance promoting resilience to stress-induced anxiety- and depressive-like behaviors. Brain Behav Immun. (2021) 91:350–68. doi: 10.1016/j.bbi.2020.10.013
42. Simpson, CA, Diaz-Arteche, C, Eliby, D, Schwartz, OS, Simmons, JG, and Cowan, CSM. The gut microbiota in anxiety and depression—a systematic review. Clin Psychol Rev. (2021) 83:101943. doi: 10.1016/j.cpr.2020.101943
43. Beheshti, F, Hashemzehi, M, Hosseini, M, Marefati, N, and Memarpour, S. Inducible nitric oxide synthase plays a role in depression- and anxiety-like behaviors chronically induced by lipopolysaccharide in rats: evidence from inflammation and oxidative stress. Behav Brain Res. (2020) 392:112720. doi: 10.1016/j.bbr.2020.112720
44. Angulo, J, El Assar, M, Álvarez-Bustos, A, and Rodríguez-Mañas, L. Physical activity and exercise: strategies to manage frailty. Redox Biol. (2020) 35:101513. doi: 10.1016/j.redox.2020.101513
45. Wang, X, Wang, Z, and Tang, D. Aerobic exercise alleviates inflammation, oxidative stress, and apoptosis in mice with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. (2021) 16:1369–79. doi: 10.2147/COPD.S309041
46. Dionysopoulou, S, Charmandari, E, Bargiota, A, Vlahos, N, Mastorakos, G, and Valsamakis, G. The role of hypothalamic inflammation in diet-induced obesity and its association with cognitive and mood disorders. Nutrients. (2021) 13:498. doi: 10.3390/nu13020498
47. Ghannoum, MA, Ford, M, Bonomo, RA, Gamal, A, and McCormick, TS. A microbiome-driven approach to combating depression during the COVID-19 pandemic. Front Nutr. (2021) 8:672390. doi: 10.3389/fnut.2021.672390
48. Xia, WJ, Xu, ML, Yu, XJ, Du, MM, Li, XH, Yang, T, et al. Antihypertensive effects of exercise involve reshaping of gut microbiota and improvement of gut-brain axis in spontaneously hypertensive rat. Gut Microbes. (2021) 13:1–24. doi: 10.1080/19490976.2020.1854642
49. Du, Y, Gao, Y, Zeng, B, Fan, X, Yang, D, and Yang, M. Effects of anti-aging interventions on intestinal microbiota. Gut Microbes. (2021) 13:1994835. doi: 10.1080/19490976.2021.1994835
50. Fabrazzo, M, Cipolla, S, Pisaturo, M, Camerlengo, A, Bucci, P, Pezzella, P, et al. Bidirectional relationship between HIV/HBV infection and comorbid depression and/or anxiety: a systematic review on shared biological mechanisms. J Personalized Med. (2023) 13:1689. doi: 10.3390/jpm13121689
51. Assefa, S, Boru, B, Gebeyehu, DA, and Terefe, B. Depression, anxiety and their associated factors among patients with tuberculosis attending in Gondar city health facilities, north West Ethiopia. BMC Psychiatry. (2023) 23:91. doi: 10.1186/s12888-023-04573-7
Keywords: exercise therapy, COVID-19, anxiety, depression, meta-analysis
Citation: Tang J, Chen L-L, Zhang H, Wei P and Miao F (2024) Effects of exercise therapy on anxiety and depression in patients with COVID-19: a systematic review and meta-analysis. Front. Public Health. 12:1330521. doi: 10.3389/fpubh.2024.1330521
Edited by:
Steffen Schulz, Charité University Medicine Berlin, GermanyReviewed by:
Helena Ludwig-Walz, Bundesinstitut für Bevölkerungsforschung, GermanyFarzin Bagheri Sheykhangafshe, Tarbiat Modares University, Iran
Copyright © 2024 Tang, Chen, Zhang, Wei and Miao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peifeng Wei, d2VpcGVpZmVuZ0AxNjMuY29t; Feng Miao, bWlhb2ZlbmcyMzA0QDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Ju Tang
Ju Tang Liang-Liang Chen2†
Liang-Liang Chen2†