
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 22 July 2024
Sec. Public Health Policy
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1329787
This article is part of the Research Topic The Epidemiology of Missed and Delayed Medical Diagnosis: Implications for Health Equity and Public Health View all 10 articles
Background: Postnatal care (PNC) is a crucial component of continuous healthcare and can be influenced by sociodemographic factors. This study aimed to examine the sociodemographic disparities in PNC coverage in Hamedan City.
Methods: In this cross-sectional study, we utilized existing data recorded in the Health Integrated System of Hamedan City, located in Iran, from 2020 to 2021. The study population consisted of 853 women who were over 15 years old and had given birth within the past 42 days. The Health Equity Assessment Toolkit (HEAT) software was used to evaluate the socioeconomic inequalities in PNC coverage.
Results: Overall, 531 (62.3%) of the women received three postnatal visits. The absolute concentration index (ACI) indicates that women aged 20–35 years, illiterate women, housewives, insured individuals, and urban residents experience a higher magnitude of inequality in PNC coverage. The negative values of the ACI suggest that the health index is concentrated among disadvantaged groups, with educational level inequalities being more pronounced than those related to age.
Conclusion: Postnatal care coverage among mothers was relatively adequate; however, sociodemographic inequalities existed in the utilization of PNC services. It is recommended that policymakers make efforts to increase access to PNC services for mothers from low socio-economic groups.
Most maternal deaths occur during the postnatal period, and an estimated 2.8 million babies die within the first month of life (1). Postnatal care (PNC) services are crucial for improving outcomes for mothers and infants in low- and middle-income countries (2). Inadequate PNC can expose mothers to risks such as postpartum bleeding, eclampsia, puerperal infection, thromboembolic disease, breastfeeding problems, and psychological issues such as depression (3). In some countries, PNC coverage is relatively poorer compared to other maternal and child care services (4). The World Health Organization (WHO) recommends that mothers and their newborns receive postnatal care within 24 h of birth, on the third day, during the second week, and at 6 weeks postpartum (5).
In Iran, postpartum care is typically provided at governmental and nongovernmental facilities, with all services delivered outside the home. Governmental postnatal care services are provided free of charge and include the prevention, early detection, and treatment of complications and diseases, as well as counseling on breastfeeding, birth spacing, immunization, and maternal nutrition (6). Improving social conditions and facilitating access to health services and education can play a valuable role in ensuring the health of mothers and children, who are among the most vulnerable groups.
Considering the necessity of PNC as an essential strategy to save the lives of mothers and newborns, it is crucial to identify the factors that prevent mothers and infants from benefiting from postnatal care (6). Health inequality, defined as the disproportionate concentration of people with specific health behaviors in certain demographic subgroups, remains a significant challenge for health systems, especially in low-income countries (7). For instance, mothers with lower levels of education and income are much less likely to initiate and continue breastfeeding than those from higher socioeconomic classes (8).
Global research has identified various factors influencing the use of PNC services, with varied outcomes, including maternal age, education level, occupation, place and method of delivery, number of pregnancies, and awareness of PNC services (9, 10). Economic and social determinants can affect the receipt of these essential services or lead to adverse health consequences during the postnatal period. Individuals with lower socioeconomic status are less likely to receive routine healthcare or preventive health advice and have a higher incidence of adverse health outcomes (11, 12).
The results of the FiNaL Study showed that women belonging to low socioeconomic levels face significant deprivations in terms of access to formal and informal breastfeeding support and even access to information (13). A study conducted in Nigeria classified the determinants of PNC services into family and community levels, which include education level, financial status, urban or rural residence, religion, source of information, mother’s age, and previous experience with health services (14). Another study on determinants affecting maternal health outcomes in Ghana revealed that rural residents are less likely than urban residents to undergo PNC (15).
It is important to note that the variables affecting PNC service use differ based on socio-cultural factors within a particular community. These differences may be attributed to factors such as access to health facilities, intentional government interventions, geographic location, and cultural practices. Identifying sociodemographic factors associated with PNC utilization can help health planners design and implement evidence-based interventions to strengthen the health system and improve access to and use of PNC services. This study aimed to investigate the social and economic inequalities in postnatal care coverage among mothers in Hamedan City.
In this cross-sectional study, existing data from the Health Integrated System of Hamedan City, located in Iran, for the years 2020–2021 were analyzed to assess socioeconomic inequalities in postnatal care (PNC) coverage. In Hamedan city, comprehensive health coverage is provided to all residents, both urban and rural, through health centers. All healthcare information, including PNC, is electronically recorded in the integrated health system. According to national guidelines, postpartum care includes three visits on days 1–3, 10–15, and 42–60 after delivery.
The study population comprised women over 15 years old who had given birth within the past 42 days. A total of 853 women met these criteria and their data were included in the analysis.
In Hamedan City, there are 17 comprehensive urban and 13 comprehensive rural health centers. For this study, a simple random sampling method was used to select 8 out of the 17 comprehensive urban health centers and 5 out of the 13 comprehensive rural health centers. Subsequently, all eligible participants within the selected centers were enrolled using the census sampling method.
The checklist included the following variables: age, occupation, education level, place of residence, insurance status, delivery method, experience of preterm delivery, and exclusive breastfeeding.
The primary outcome of the present study is the number of postnatal visits within 42 days after delivery, which ranges from 0 to 3 visits according to national guidelines.
Data analysis was performed using SPSS software version 16. Descriptive statistics were used to summarize the data. The relationship between qualitative variables was assessed using the Chi-square test, and a logistic regression model was employed to identify predictive variables associated with receiving postnatal care (PNC) at a 95% confidence level.
To assess inequalities in PNC coverage across socio-economic subgroups, the Health Equity Assessment Toolkit (HEAT) software version 4.0 (Beta) was utilized. Inequality was evaluated using the ACI (absolute concentration index) and R indices. The R ratio is a simple measure indicating relative inequality between two subgroups, with values greater than 1 indicating higher inequality (16). The ACI is a weighted measure that assesses inequality based on a natural ordering scale, where positive values indicate concentration among advantaged groups and negative values indicate concentration among disadvantaged groups. A higher absolute ACI indicates greater inequality (17).
The results of data analysis indicated that the highest frequency distribution was observed among individuals aged 20–35 years (74.7%), unemployed individuals (91.3%), those who were illiterate (43.3%), urban residents (82.2%), and those with insurance coverage (95.3%).
Analysis of postnatal care (PNC) coverage based on demographic characteristics revealed that the highest frequency distribution of receiving at least one or more PNC visits was among individuals aged 20–35 years (74.4%), unemployed individuals (91.9%), those who were illiterate (44%), urban residents (82.1%), and those with insurance coverage (95.2%).
Furthermore, comparing PNC coverage according to employment status showed statistically significant differences (p = 0.014) (Table 1).
More than 62% (531) of mothers received all three postnatal care visits. However, less than 5% (42) of women did not receive any postnatal care. The rate of exclusive breastfeeding up to 42 days after childbirth was 94.4% (805) (Table 2).
The prevalence of cesarean section was 53.2% (454), preterm labor was 7.6% (65), and unwanted pregnancy was 19.1% (690). Cesarean section was significantly associated with the number of postnatal care (PNC) visits, with a higher percentage of individuals not receiving any PNC at all following cesarean section compared to normal vaginal delivery (Table 3).
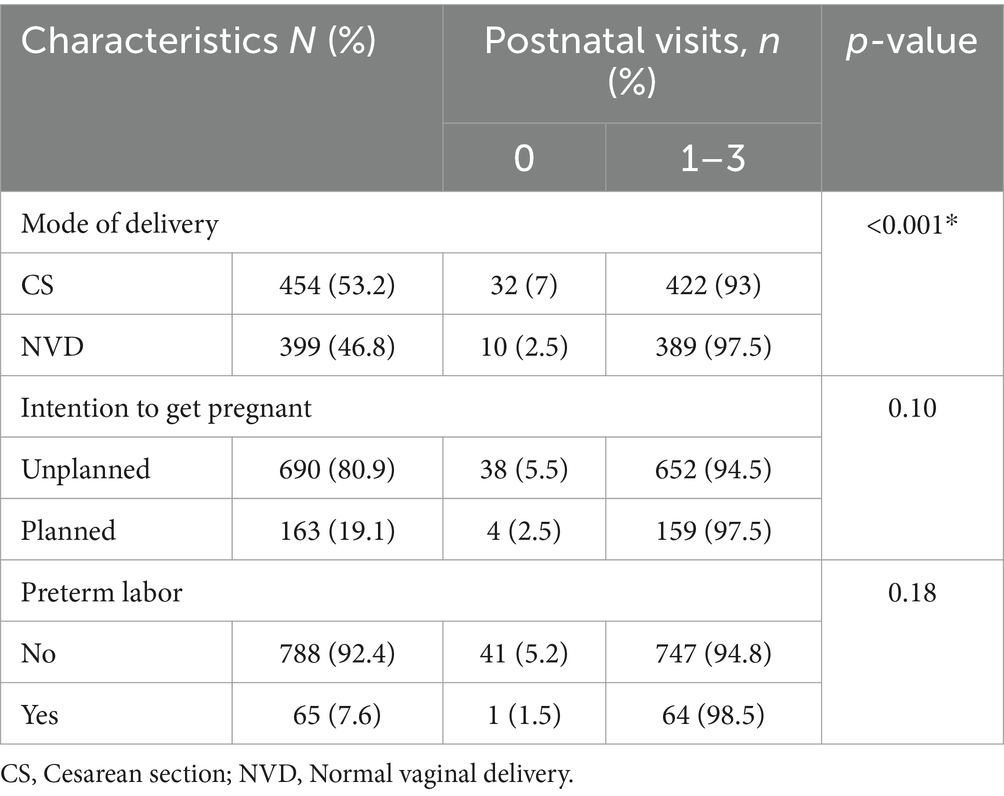
Table 3. The relationship between postnatal visits with obstetric characteristics of women (N = 853).
A logistic regression model was employed to identify predictive variables associated with postnatal care (PNC). The results indicated that, after controlling for variables such as age, education, insurance, and residence of mothers, occupation showed a significant relationship with the frequency of PNC visits. Specifically, the odds of receiving care were 5.5 times higher among non-employed mothers compared to employed mothers (p = 0.018) (Table 4).
The results from Table 5 indicate that the coverage of at least one postnatal care visit was 95%. The absolute concentration index (ACI) highlights that the age group 20–35 years exhibits a higher magnitude of inequality in postnatal care (PNC) coverage compared to other age groups. Specifically, PNC coverage was more equitable in the age groups under 20 and over 35 years old.
Regarding other demographic characteristics, inequalities in PNC coverage were more pronounced among the illiterate, housewives, insured individuals, and urban residents compared to other subgroups.
Furthermore, the R indices (R) revealed that the level of inequality was greater for the “insurance” variable (R > 1) and lower for variables such as age, education, occupation, and place of residence (R < 1). This suggests that inequality in PNC coverage is more pronounced based on insurance status compared to other demographic factors.
Negative values of the ACI indicate that the concentration of the health index is among disadvantaged populations, with educational inequalities being more prominent than age-related disparities (Table 5).
The results of the present study revealed that postnatal care (PNC) coverage in Hamedan, a city in Iran, was moderately high, with more than 62% of postpartum mothers receiving PNC, aligning with World Health Organization recommendations. Evidence suggests that widespread PNC availability could prevent between 10 and 27% of infant deaths (18). In this study, 37.7% of mothers received care 1–2 times, while approximately 5% did not receive any PNC at all. Limited PNC coverage is evident, particularly among economically disadvantaged families. For instance, in the Democratic Republic of the Congo, only 35% of women receive PNC (19), while in Nepal, PNC utilization stands at around 22% (20). In contrast, a study in Sri Lanka reported 76.9% coverage of recommended PNC visits (21).
In Iran, studies on PNC coverage are scarce, with data typically managed by the Ministry of Health. However, a longitudinal study in Tehran found high rates of prenatal care utilization (95%) and recommended visits (99%) among pregnant women (22).
Notably, a significant proportion of deliveries in the present study were by cesarean section (53.2%), and these mothers were less likely to receive PNC compared to those with vaginal deliveries. Similar findings on socio-economic inequality in PNC utilization after cesarean sections were reported in other studies (23), although some research in Ethiopia suggests cesarean delivery may increase PNC utilization due to perceived higher risks (24).
Iran has one of the highest cesarean section rates globally (25). Most cesarean sections in this study were likely emergency procedures, underscoring the critical need for post-cesarean care and follow-up due to higher complication risks compared to vaginal deliveries (26). Financial and cultural barriers may hinder cesarean-section mothers from accessing PNC, as seen in studies from Pakistan highlighting transportation and healthcare costs as deterrents (27).
Regarding demographics, PNC coverage was better among women under 20 and over 35 years old compared to those aged 20–35 years. In Iran, younger mothers (<20 years) receive heightened attention due to perceived higher pregnancy risks, while older mothers (>35 years) benefit from greater healthcare awareness and support. Similar findings on increased PNC utilization with advancing maternal age have been reported elsewhere (28, 29).
Education also significantly influenced PNC coverage, with lower rates among illiterate or minimally educated women compared to others (24–29). Education enhances health awareness and promotes health-seeking behavior, influencing service utilization (30).
Non-employed mothers in the study were 5.5 times more likely to receive PNC compared to employed counterparts, contrary to some expectations about economic independence and service access (29, 31). Rural residents also showed higher PNC coverage than urban counterparts, differing from findings in some studies (32, 33), but consistent with others (20, 34). Urban areas may offer better access to private healthcare facilities and health promotion programs, influencing PNC utilization (21).
Interestingly, while 95.3% of mothers in this study had health insurance, uninsured individuals had better PNC coverage in comprehensive health centers. The availability of health insurance allows mothers to choose private facilities or gynecologists’ offices, potentially reducing visits to public health centers. Efforts to improve PNC service quality in public centers could enhance overall access and utilization, regardless of socio-economic status.
The study benefits significantly from using data from the Health Integrated System, which likely offers a large sample size. This enables a comprehensive analysis of postnatal care (PNC) utilization and inequalities. The data within this system are objective and reliable, systematically collected as part of the healthcare system. This enhances the credibility of the study findings and reduces biases associated with self-reported data or survey responses. As a result, the study provides more accurate and representative insights into disparities in postnatal care. These findings can have profound implications for healthcare policies and interventions aimed at reducing inequality in PNC, thereby contributing to improved maternal and child health outcomes.
This study has several limitations that should be considered. Firstly, it is unable to examine disparities in postnatal care (PNC) provided at private facilities, focusing solely on public health centers. Secondly, as a cross-sectional analysis, it can establish associations between variables but cannot determine causation. Additionally, using secondary data introduces limitations such as potential exclusion of important factors like family support, proximity to healthcare facilities, and availability of healthcare providers. Maternal factors like residence patterns can also impact PNC access; for example, many Iranian mothers, particularly first-time mothers, often return to their parents’ homes postpartum, seeking care from family members, especially their mothers.
Furthermore, the study’s scope is limited to Hamedan City, a specific geographic area in Iran, which may restrict the generalizability of findings to other regions. To gain a comprehensive understanding of maternal and child health disparities, ongoing monitoring and evaluation of health indicators and related inequities are crucial. Future research that considers geographical and socio-economic factors could provide valuable insights into variations in postnatal care across diverse social and cultural contexts.
Our analysis revealed significant disparities in postnatal care (PNC) utilization, particularly among specific demographic groups such as women aged 20–35, those with low education levels, housewives, insured individuals, and urban residents. By elucidating the intricate relationship between socioeconomic status and PNC coverage, our study offers valuable insights into global health inequalities. The negative values of the absolute concentration index (ACI) underscore the concentration of inadequate PNC coverage among marginalized individuals, emphasizing the urgent need for targeted interventions at a systemic level.
As we strive for universal health coverage and work toward achieving the Sustainable Development Goals, the findings of this research hold relevance Hamedan City, extending to regions worldwide grappling with similar challenges in ensuring equitable maternal healthcare. Addressing socioeconomic disparities in PNC coverage demands collective responsibility and coordinated action from policymakers, healthcare providers, and communities globally.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the ethics committee of Hamadan University of Medical Sciences approved this study with the code of IR.UMSHA.REC.1401.265. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
AM: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. FS: Conceptualization, Writing – original draft, Writing – review & editing. MA: Data curation, Methodology, Writing – original draft, Writing – review & editing. RB: Investigation, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Vice-Chancellor for Research and Technology, Hamedan University of Medical Sciences of Iran [Grant number 140104072342].
We would like to thank the Clinical Research Development Unit of Ayatollah Mousavi Hospital, Zanjan University of Medical Sciences for their collaboration.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
PNC, Postnatal care; HEAT, Health Equity Assessment Toolkit; R, Ratio; ACI, Absolute Concentration Index; DHS, Department of Homeland Security; WHO, World Health Organization.
1. WHO . Newborns: improving survival and well-being. (2020). Available at:https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality
2. Michel-Schuldt, M, McFadden, A, Renfrew, M, and Homer, C. The provision of midwife-led care in low-and middle-income countries: an integrative review. Midwifery. (2020) 84:102659. doi: 10.1016/j.midw.2020.102659
3. Konje, ET, Msuya, IE, Matovelo, D, Basinda, N, and Dewey, D. Provision of inadequate information on postnatal care and services during antenatal visits in Busega, Northwest Tanzania: a simulated client study. BMC Health Serv Res. (2022) 22:700. doi: 10.1186/s12913-022-08071-6
4. Chaka, EE, Abdurahman, AA, Nedjat, S, and Majdzadeh, R. Utilization and determinants of postnatal care services in Ethiopia: a systematic review and meta-analysis. Ethiop J Health Sci. (2019) 29:935–44. doi: 10.4314/ejhs.v29i1.16
5. Organization, W.H . WHO recommendations on postnatal care of the mother and newborn World Health Organization. Geneva, Switzerland: World Health Organization (2014). 1–72.
6. Iranian National Program on Safe Motherhood . Integrated care on Mother's health, outside hospital services guide. 3rd ed. Tehran: Iranian Ministry of Health and Medical Education (2010).
7. Ilinca, S, di Giorgio, L, Salari, P, and Chuma, J. Socio-economic inequality and inequity in use of health care services in Kenya: evidence from the fourth Kenya household health expenditure and utilization survey. Int J Equity Health. (2019) 18:1–13. doi: 10.1186/s12939-019-1106-z
8. McMaughan, DJ, Oloruntoba, O, and Smith, ML. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Front Public Health. (2020) 8:231. doi: 10.3389/fpubh.2020.00231
9. Appiah, F, Salihu, T, Fenteng, JOD, Darteh, AO, Kannor, P, Ayerakwah, PA, et al. Postnatal care utilisation among women in rural Ghana: analysis of 2014 Ghana demographic and health survey. BMC Pregnancy Childbirth. (2021) 21:1–9. doi: 10.1186/s12884-020-03497-4
10. Sakeah, E, Aborigo, R, Sakeah, JK, Dalaba, M, Kanyomse, E, Azongo, D, et al. The role of community-based health services in influencing postnatal care visits in the Builsa and the west Mamprusi districts in rural Ghana. BMC Pregnancy Childbirth. (2018) 18:1–9. doi: 10.1186/s12884-018-1926-7
11. Kim, MK, Lee, SM, Bae, SH, Kim, HJ, Lim, NG, Yoon, SJ, et al. Socioeconomic status can affect pregnancy outcomes and complications, even with a universal healthcare system. Int J Equity Health. (2018) 17:1–8. doi: 10.1186/s12939-017-0715-7
12. Lindquist, A, Kurinczuk, JJ, Redshaw, M, and Knight, M. Experiences, utilisation and outcomes of maternity care in England among women from different socio-economic groups: findings from the 2010 National Maternity Survey. BJOG Int J Obstet Gynaecol. (2015) 122:1610–7. doi: 10.1111/1471-0528.13059
13. Temple Newhook, J, Newhook, LA, Midodzi, WK, Murphy Goodridge, J, Burrage, L, Gill, N, et al. Poverty and breastfeeding: comparing determinants of early breastfeeding cessation incidence in socioeconomically marginalized and privileged populations in the FiNaL study. Health Equity. (2017) 1:96–102. doi: 10.1089/heq.2016.0028
14. Iyanda, H. I. Determinants of utilization of postnatal care services in Nigeria. Amsterdam, Master degree thesis, The Netherlands: KIT (Royal Tropical Institute) Health Unit. (2017). Available at: https://bibalex.org/baifa/Attachment/Documents/BGct4B5LmS_20180404151219943.pdf
15. Adu, J, Tenkorang, E, Banchani, E, Allison, J, and Mulay, S. The effects of individual and community-level factors on maternal health outcomes in Ghana. PLoS One. (2018) 13:e0207942. doi: 10.1371/journal.pone.0207942
16. Schlotheuber, A, and Hosseinpoor, AR. Summary measures of health inequality: a review of existing measures and their application. Int J Environ Res Public Health. (2022) 19:3697. doi: 10.3390/ijerph19063697
17. Moore, S, Stewart, S, and Teixeira, A. Decomposing social capital inequalities in health. J Epidemiol Community Health. (2014) 68:233–8. doi: 10.1136/jech-2013-202996
18. Darmstadt, GL, Bhutta, ZA, Cousens, S, Adam, T, Walker, N, de Bernis, L, et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. (2005) 365:977–88. doi: 10.1016/S0140-6736(05)71088-6
19. Abel Ntambue, ML, Françoise Malonga, K, Dramaix-Wilmet, M, and Donnen, P. Determinants of maternal health services utilization in urban settings of the Democratic Republic of Congo–a case study of Lubumbashi City. BMC Pregnancy Childbirth. (2012) 12:66. doi: 10.1186/1471-2393-12-66
20. Aryal, KK, Sharma, SK, Khanal, MN, Bista, B, Sharma, SL, Kafle, S, et al. Maternal health care in Nepal: trends and determinants, vol. 118. Rockville, Maryland, USA: ICF International Publisher (2019) 1–61. Available at: https://dhsprogram.com/pubs/pdf/FA118/FA118.pdf.
21. Perera, UAP, Assefa, Y, and Amilani, U. Postnatal care coverage and its determinants in Sri Lanka: analysis of the 2016 demographic and health survey. BMC Pregnancy Childbirth. (2021) 21:1–13. doi: 10.1186/s12884-021-03770-0
22. Kolahi, AA, Abbasi-Kangevari, M, Abdollahi, M, Ehdaeivand, F, and Arshi, S. Pattern of prenatal care utilization in Tehran: a population based longitudinal study. Women Birth. (2018) 31:e147–51. doi: 10.1016/j.wombi.2017.09.013
23. Abegunde, D, Hutchinson, P, Anaba, U, Oyedokun-Adebagbo, F, Johansson, EW, Feyisetan, B, et al. Socioeconomic inequality in exclusive breastfeeding behavior and ideation factors for social behavioral change in three north-western Nigerian states: a cross-sectional study. Int J Equity Health. (2021) 20:1–14. doi: 10.1186/s12939-021-01504-4
24. Akibu, M, Tsegaye, W, Megersa, T, and Nurgi, S. Prevalence and determinants of complete postnatal care service utilization in northern Shoa, Ethiopia. J Pregnancy. (2018) 2018:1–7. doi: 10.1155/2018/8625437
25. Shirzad, M, Shakibazadeh, E, Hajimiri, K, Betran, AP, Jahanfar, S, Bohren, MA, et al. Prevalence of and reasons for women’s, family members’, and health professionals’ preferences for cesarean section in Iran: a mixed-methods systematic review. Reprod Health. (2021) 18:3. doi: 10.1186/s12978-020-01047-x
26. Yang, X-J, and Sun, S-S. Comparison of maternal and fetal complications in elective and emergency cesarean section: a systematic review and meta-analysis. Arch Gynecol Obstet. (2017) 296:503–12. doi: 10.1007/s00404-017-4445-2
27. Misu, F, and Alam, K. Comparison of inequality in utilization of maternal healthcare services between Bangladesh and Pakistan: evidence from the demographic health survey 2017–2018. Reprod Health. (2023) 20:43. doi: 10.1186/s12978-023-01595-y
28. Appiah, F, Salihu, T, Fenteng, JOD, Darteh, AO, Djan, ET, Takyi, M, et al. Factors influencing early postnatal care utilisation among women: evidence from the 2014 Ghana demographic and health survey. PLoS One. (2021) 16:e0249480. doi: 10.1371/journal.pone.0249480
29. Khaki, JJ, and Sithole, L. Factors associated with the utilization of postnatal care services among Malawian women. Malawi Med J. (2019) 31:2–11. doi: 10.4314/mmj.v31i1.2
30. Beyene, T, Melka, AS, and Yadecha, B. Determinants of postnatal care service utilization among married women in rural areas in western Ethiopia. J Health Popul Nutr. (2022) 41:38–7. doi: 10.1186/s41043-022-00320-y
31. Maitanmi, BT, Adelaja, AA, Okunola, DR, Maitanmi, JO, Tola, YO, and Akingbade, O. Association between socioeconomic status and the utilization of maternal health Services in Nigeria. Iran J Nurs Midwifery Res. (2023) 28:514–9. doi: 10.4103/ijnmr.ijnmr_61_22
32. Khankhell, RM, Ghotbi, N, and Hemat, S. Editors’ choice factors influencing utilization of postnatal care visits in Afghanistan. Nagoya J. Med. Sci. (2020) 82:711. doi: 10.18999/nagjms.82.4.711
33. Berhe, A, Bayray, A, Berhe, Y, Teklu, A, Desta, A, Araya, T, et al. Determinants of postnatal care utilization in Tigray, northern Ethiopia: a community based cross-sectional study. PLoS One. (2019) 14:e0221161. doi: 10.1371/journal.pone.0221161
Keywords: postnatal care coverage, midwifery services, women health, Iran, disparities - definition and paradigm
Citation: Maleki A, Soltani F, Abasalizadeh M and Bakht R (2024) Sociodemographic disparities in postnatal care coverage at comprehensive health centers in Hamedan City. Front. Public Health. 12:1329787. doi: 10.3389/fpubh.2024.1329787
Received: 29 October 2023; Accepted: 28 June 2024;
Published: 22 July 2024.
Edited by:
Ronald Wyatt, Society to Improve Diagnosis in Medicine, United StatesReviewed by:
John Parrish-Sprowl, Indiana University, Purdue University Indianapolis, United StatesCopyright © 2024 Maleki, Soltani, Abasalizadeh and Bakht. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Farzaneh Soltani, ZmFyemFuZWhzb2x0YW5pMjAwOEB5YWhvby5jb20=
†ORCID: Azam Maleki, orcid.org/0000-0001-7888-1985
Farzaneh Soltani, orcid.org/0000-0002-5407-6858
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.