- 1Department of Traditional Chinese Medicine, School of Graduate Students, Liaoning University of Traditional Chinese Medicine, Shenyang, China
- 2China National Health Development Research Center, Beijing, China
- 3Department of Public Management, School of Economics and Management, Liaoning University of Traditional Chinese Medicine, Shenyang, China
Introduction: Anxiety disorders are the most common mental disorder, experienced by more than a quarter of the population. This study examines total outpatient curative care expenditures (CCE) for anxiety disorders and changes in their composition based on the System of Health Accounts 2011 (SHA 2011).
Methods: This study used multi-stage stratified random from a total of 9,318,513 outpatient sample data by 920 healthcare organizations, a total of 109,703 cases of anxiety disorders from 53 sample organizations (5.76%) from 2015 to 2020. Univariate analysis, multifactor analysis and structural equation modeling (SEM) were used to explore the influential factors affecting outpatient CCE for anxiety disorders.
Results: Anxiety disorder outpatient CCE from 2015 to 2020 continued to increase from CNY 99.39million in 2015 to CNY 233.84 million in 2020, mainly concentrated in western medicine costs, 15–64 years, general hospital, generalized anxiety disorder and public financing. The results of univariate analysis showed statistically significant differences in all subgroups, and the results of multivariate analysis and SEM showed that the choice to purchase western drugs, purchase prepared Chinese drugs, choice to have a checkup, urban employees’ basic medical insurance, and 0–14 years old were associated with high anxiety disorder outpatient CCE.
Conclusion: Initiatives to improve the essential drug system, reduce the out-of-pocket (OOP) ratio, and strengthen primary health care to effectively reduce the medical burden on patients.
Introduction
Anxiety disorders are among the most common mental disorders worldwide (1), are a leading cause of disability and premature death (2), and are ranked by the World Health Organization as the sixth contributor to disability [3.4% of disability-adjusted life-years (DALYs) in 2015] (3). More than a quarter of the total population experiences anxiety disorders at some point in their lives (4), and the duration of the illness averages 23.4 months (5), the lifetime prevalence of anxiety disorders is 34.0%, with a lifetime prevalence of 13.0% for social anxiety disorder, 6.2% for generalized anxiety disorder, 5.2% for panic disorder, and 2.6% for agoraphobia (6). Due to their intense, persistent and recurrent fear, anxiety, and restlessness, often accompanied by a range of physical symptoms such as palpitations, chest tightness, dizziness, vertigo, and syncope (1), and may precipitate or exacerbate cardiovascular disease, gastrointestinal disorders, lung diseases, cancer, chronic pain, and migraine (7). Both the mental torment caused by anxiety disorders themselves and the utilization of outpatient and specialized health care services (1, 8), as well as their leading to reduced educational programs, impaired interpersonal relationships (9), unemployment, impaired personal functioning, and even suicide in patients, place a heavy burden on individuals, families, and society. Information on the direct medical financial burden of the disease is essential for healthcare policy makers attempting to reduce the financial burden of anxiety disorders, so it is important to estimate the direct financial burden of anxiety disorders (10).
Countries around the world have a large number of people with anxiety disorders. As of 2019, there were 301.39 million people with anxiety disorders worldwide, accounting for 31.07% of people with mental illnesses, with a prevalence of 4.05, 1.13% of DALYs for all disorders, and 3.34% of years lived with disability (YLDs) for all disorders (11). Anxiety disorders impose a significant economic burden on all countries. The direct cost of anxiety disorders is 2.08% of health care costs (12) and 0.25–0.78% of GDP (2). All other costs are projected to reach £14.2 billion by 2026, with healthcare costs reaching £2 billion (13).
Previous studies in China have focused on epidemiology (14, 15), examining the prevalence of anxiety disorders in different dimensions and in different provinces, and have not addressed anxiety disorder cost accounting and measured province-specific costs (16–23). Others focused on cost analyses of specific treatments [including cognitive-behavioral therapy (24–26), digital intervention therapies (27), and reception and commitment therapy (28)], randomized controlled trials (29), specific types of anxiety disorders [generalized anxiety disorder (30, 31)], treatment with medications (32, 33), and co-morbidities (2, 34, 35) were analyzed for costs. Although these studies help to promote the development of anxiety disorder cost analysis, there is currently no larger system representative sample or systematic accounting framework to account for anxiety disorder costs in a region, and having a systematic accounting framework to account for anxiety disorder costs can improve the accuracy of measurement and comparability between different countries.
For “Whether to purchase western drugs,” the grouping method was that the answer to the question of “Whether to purchase western drugs” was “Yes” for those who had western drug costs in the cost breakdown of outpatient visits for anxiety patients, and the answer to the question of “Whether to purchase western drugs” was “NO” for those who did not have western drug costs in the cost breakdown of outpatient visits for anxiety patients. The answer to the question “Whether to purchase western drugs” is “Yes” for those who do not have western drugs in the cost breakdown of anxiety disorder outpatient visits, and the answer to the question “No” for those who do not have western drugs in the cost breakdown of anxiety disorder outpatient visits. For Whether to purchase prepared Chinese drugs, the grouping method was that the answer to Whether to purchase prepared Chinese drugs was “Yes” for prepared prescription (Chinese medicine) and herbal medicines that existed in the cost breakdown of the outpatient clinics for anxiety patients, and the answer to “Whether to purchase prepared Chinese drugs” was “No” for prepared prescription (Chinese medicine) and herbal medicines that did not exist in the cost breakdown of the outpatient clinics for anxiety patients. For “Whether to purchase prepared Chinese drugs,” the answer is “NO”; for “Whether to select to have a checkup,” the grouping method is that if there is a checkup fee in the cost breakdown of the outpatient consultation fee for patients with anxiety disorders, the answer is “NO.” For “Whether to select to have a checkup,” the grouping method was that for those who had a checkup fee in the cost breakdown of outpatient visits for patients with anxiety disorders, the answer to “Whether to select to have a checkup” was “Yes”; for those who did not have a checkup fee in the cost breakdown of outpatient visits for patients with anxiety disorders, the answer to “Whether to select to have a checkup” was “NO”; sex is divided into female and male; age is divided into 0–44 years old, 45–59 years old, and 60 years old and above according to the overall trend of rising and then falling in the cost distribution line graph (36); insurance status is divided into urban employees’, urban employees’, urban employees’, and urban employees’ according to the major insurance payment methods in China; insurance status is categorized into urban employees’ basic medical insurance, urban residents’ basic medical insurance, new rural cooperative medical care, self-funded; the type of patient insurance is categorized as medical care, self-funded; hospital level is mainly based on the existing comprehensive rating of the Chinese health care system for the hospital as tertiary hospital, secondary hospital, first-class hospital, unclassified institutions; institution level is mainly based on the existing comprehensive rating of the Chinese health care system for the hospital as tertiary hospital, secondary hospital, first-class hospital, unclassified institutions; and institutions; institution level is mainly based on the geographical location of the current medical and health institutions and the service ability of the strong and weak in China to determine the division into provincial level, municipal level, district level, country level; institution type of medical institutions in accordance with the “Medical Institutions, Health Care, Self-funded”; institution type is divided into general hospital, traditional Chinese medicine hospital, specialized hospital, primary medical institutions according to the Medical Institution Practice License and disease diagnosis and treatment activities.
The most widely used system for accounting for health costs is the System of Health Accounts 2011 (SHA2011), which is the second version of the health cost accounting system jointly revised by several authoritative international organizations in 2011 (37). SHA2011 can be better used to respond to the complex and changing forms and channels of health financing globally, the massive innovation in medical technology and medical knowledge, the increase in data sophistication of health information systems, and policy changes in key populations and diseases. Therefore, this study selects a sample of patients from health care institutions in Liaoning Province from 2015 to 2020, and analyzes different dimensions of costs for outpatients with anxiety disorders from 2015 to 2020 as a way to propose more targeted and informative policy recommendations for anxiety disorders, as well as to promote the progress of research on anxiety disorders in cost analysis.
Materials and methods
Data resources
The data and information of this study are obtained from two parts, one part is from the Liaoning Provincial Health and Family Planning Statistical Yearbook, Liaoning Provincial Statistical Yearbook, Liaoning Provincial Financial Annual Report, Liaoning Provincial Government Health Input Monitoring Data, and Liaoning Provincial Social Insurance Fund Accounts from 2015 to 2020, as the total data of Liaoning Province costs, etc.; the other part is from the sample data of the selected medical institutions filled in the consultation information of patients attending the clinic.
Sampling method
The sampling method adopted in this study was multi-stage stratified random sampling, district sampling based on factors such as the level of economic development and availability of health services in the district. In the first stage, five cities, Dalian, Panjin, Tieling, Fushun and Jinzhou, were selected based on a combination of regional economic development and health resource allocation; in the second stage, one district and two counties were selected in each city, for a total of 15 districts and counties as sample sites; in the third stage, medical institutions were selected in the 15 districts and counties, and the selected medical institutions filled in the consultation information of patients attending the clinic according to the National Center for Health Development Research’s outpatient data template, but a code system was adopted for patients’ personal information, thus discarding obtaining patients’ consent.
Sample situation
The study discarded the analysis of hospitalization costs due to the small number of hospitalization data entries screened for anxiety disorders, which accounted for less than 1%. From a total of 9,318,513 sample data from 920 healthcare organizations, a total of 109,703 cases of anxiety disorders from 53 sample organizations (5.76%) were screened according to the International Classification of Basic Classification, Tenth Edition (ICD-10) F40-F41 (38), including F40 for phobias (including square phobia: F40.0, social phobia: F40.1, specific phobia: F40.2), F41 for other anxiety disorders (including panic disorder: F41.0, generalized anxiety disorder. F41.1, Mixed anxiety disorder: F41.2-F41.3, Anxiety: F41.8-F41.9) (39). Mental disorders were defined according to a review of the literature according to ICD-10 as F00-F99 (40). The software used for data accounting was STATA 15.0 (Stata Corp, College Station, State of Texas, USA). The cost dates for this study are from January 1, 2015 to December 31, 2020, and since the costs involved in this study are denominated in CNY, there is no unit conversion problem as this study involves costs in Liaoning Province, China. The age range of the study population for anxiety disorders was greater than or equal to 0 years. Gender was categorized as male and female. Information on the characteristics of the study population’s disease included name, ICD-10. And information on costs included total disease outpatient costs, exams, office visits, lab tests, medications, other costs, type of insurance payment, amount paid by insurance, amount paid by the individual in cash. Unclassified institutions for in accordance with the hospital level division standards, is China according to the hospital size, scientific research direction, human resources and technical strength, medical hardware and equipment, etc. on the hospital qualification assessment indicators, in accordance with the “Hospital Classification and Management Standards,” the national unity, regardless of the background of the hospital, all the nature of hospitals, etc., hospitals after the review, determined as unclassified institutions, first-class hospital, secondary hospital, tertiary hospital (41).
Calculation of CCE
The overall idea of the SHA2011 methodology for accounting for anxiety outpatient costs in Liaoning Province is to use the sample to estimate the whole. This was done by first determining the total health costs in Liaoning Province as the sum of the total costs of public healthcare organizations as determined by the Liaoning Health Financial Yearbook and the total costs of non-public healthcare organizations as determined by the Liaoning Health Statistics Yearbook. Then, based on multi-stage stratified random sampling to obtain the outpatient data of the sample healthcare institutions, and then screening the outpatient data of anxiety disorders of the sample institutions through ICD-10, using the proportion of the outpatient costs of anxiety disorders of the sample institutions to the total outpatient costs of the sample institutions and then multiplying it by the total outpatient costs of Liaoning Province to obtain the total outpatient costs of anxiety disorders in Liaoning Province (42–44). The calculation formula is as follows:
SOCCE is the cost of the anxiety outpatient clinic, SnINC is the cost of the anxiety outpatient treatment, SnALL is the anxiety outpatient basic expense benefit, and the anxiety outpatient cost is the sum of the anxiety outpatient treatment cost and the anxiety outpatient basic expense benefit.
SINC is the cost of outpatient treatment per person with an anxiety disorder, STINC is the total cost of outpatient treatment for anxiety disorders, ɑp is the cost of total preventive services for outpatient treatment for anxiety disorders, and ɑ is the total treatment revenue for anxiety disorders.
ɑi is the cost of outpatient treatment services per anxiety disorder patient, and SnINC is formed by summing the anxiety disorder outpatient treatment costs through each anxiety disorder outpatient.
STALL is the anxiety outpatient total basic expenditure grant, SPALL is the anxiety outpatient prevention basic expenditure grant, and SALL is the anxiety outpatient total treatment basic expenditure grant.
SnALL is the sum of the basic expenditure benefit per anxiety outpatient.
Analysis of factors influencing CCE in outpatient anxiety disorders
Descriptive statistics were analyzed for anxiety disorder outpatient CCE based on different longitudinal groupings (including sex, age, insurance type, etc.), and then one-way analysis was used to determine whether the differences within groups were significant. Since anxiety disorder outpatient costs are skewed data, a logarithmic transformation of outpatient costs to make them normally distributed was performed for multifactor and SEM analysis of factors associated with high anxiety disorder outpatient CCE. Descriptive statistics, univariate analysis, and multifactor analysis were analyzed using IBM SPSS Statistics V.25.0 (IBM Corp), and SEM was constructed and analyzed using AMOS Graphics, V24.0 (SPSS).
Results
Summary of anxiety disorder results
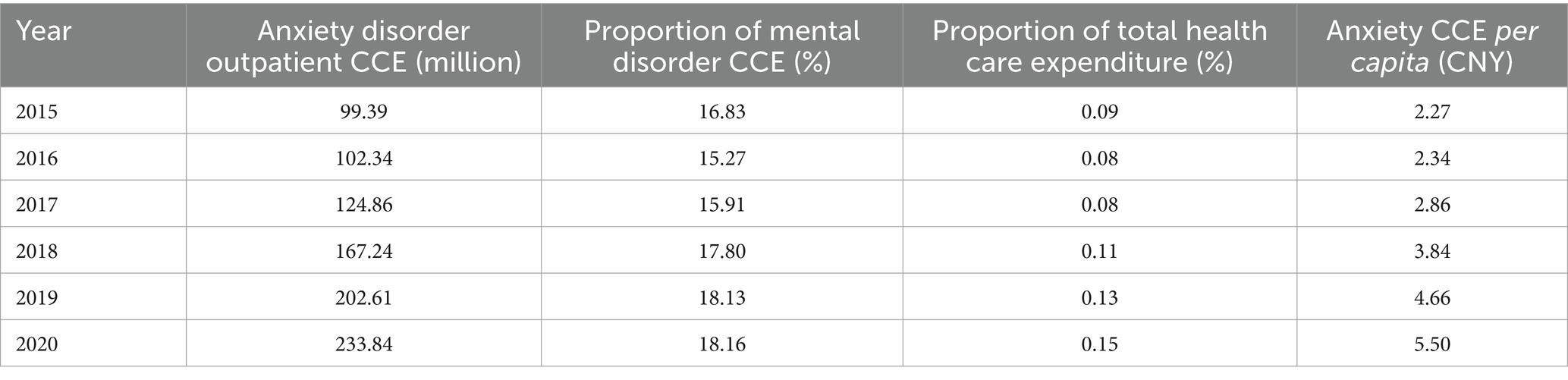
More than 90% of anxiety disorder costs occur in outpatient settings, so we only measured CCE for outpatient anxiety disorders. Overall, CCE for anxiety disorders continued to grow from 2015 to 2020 studied, from CNY 99.39 million in 2015 to CNY 233.84 million in 2020. However, CCE for anxiety disorders accounted for more than 15% of CCE for mental disorders of more than 15%, with the lowest percentage of 15.27% in 2015 and the highest percentage in recent years with a value of 18.16% in 2020. The proportion of total health care expenditure (THE) showed a slightly fluctuating trend, leveling off from 2015 to 2017 and gradually increasing from 2018 to 2020. The per capita anxiety CCE increases from CNY 2.27 in 2015 to CNY 5.50 in 2020 (Table 1).
Different classifications and costs of anxiety disorders
The anxiety disorders in this study were mainly divided into phobias and other anxiety disorders, and since other anxiety disorders accounted for about 99% of the total, the study was launched on the subdivision of other anxiety disorders, which were mainly divided into panic disorder, generalized anxiety, mixed anxiety disorder, and anxiety, of which the highest outpatient CCE combined in 2015–2020 was generalized anxiety. According to the overall results in Table 1, the outpatient CCE was mainly concentrated in choosing to purchase western drugs, choosing to purchase prepared Chinese drugs, choosing to have a checkup, female, 0–44 years old, self-funded, tertiary hospital, provincial level, general hospital, and 2020. The cost of different types of anxiety disorders varied widely under different subgroups, with a higher proportion of mixed anxiety disorders in choosing to purchase western drugs, choosing to purchase prepared Chinese drugs, tertiary hospitals, provincial level, and 2020; a higher proportion of anxiety in choosing to have a checkup, female, and general hospitals; the highest proportion of phobias in 0–44 years old; and the highest proportion of generalized anxiety disorders in self-funded (Table 2).
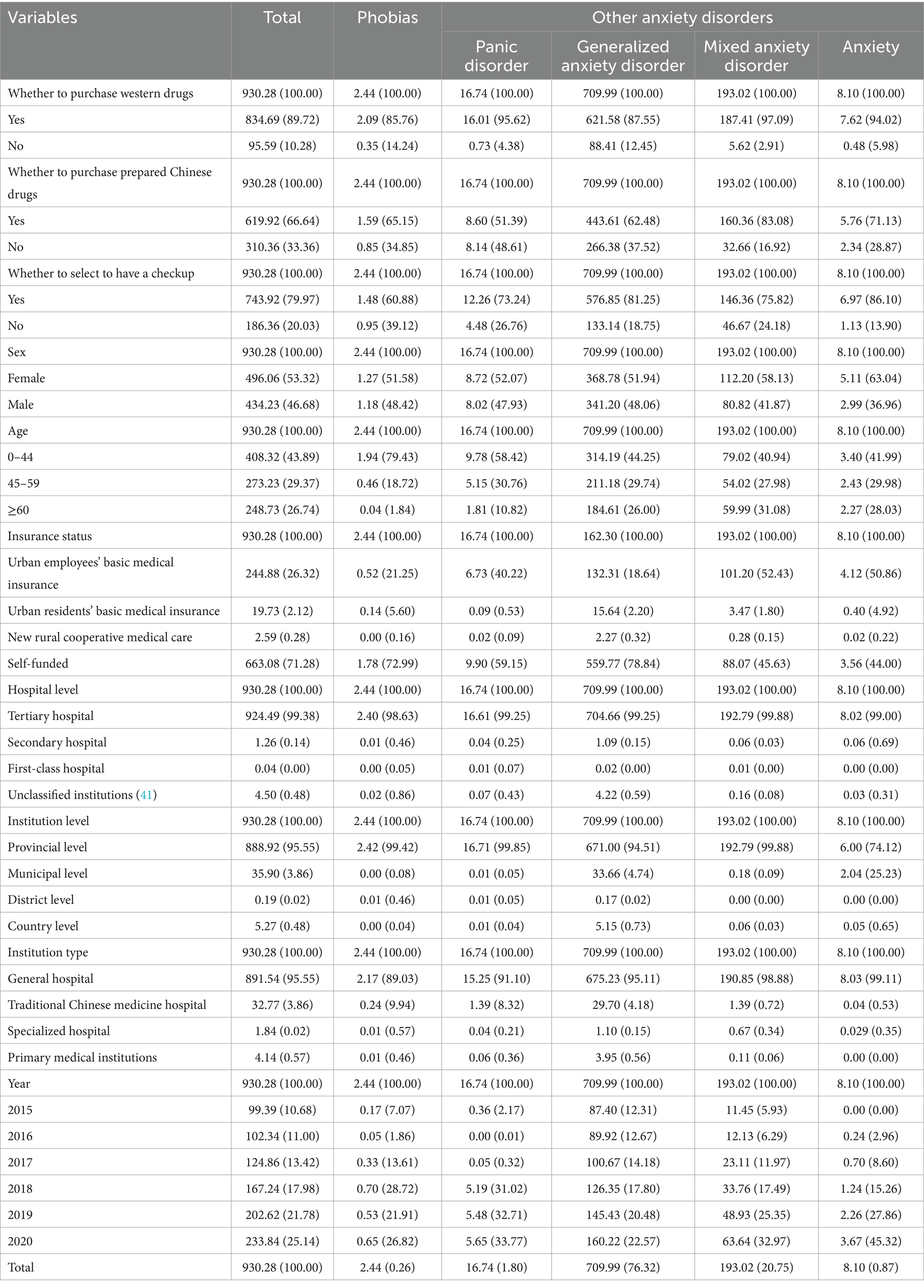
Table 2. Composition of outpatient CCE for different types of anxiety disorders and different subgroups under them [CNY million (%)].
Health financing schemes
The main source of financing for anxiety disorders among the three financing methods is public financing (50–60%). In this study, the percentage of public financing shows a trend of increasing and then decreasing, increasing to 62.47% in 2015–2019 and decreasing to 60.97% in 2020, with a continuous increase in costs to CNY 142.57 million in 2015-2020. Public Funding is mainly composed of social health insurance, in line with the overall trend of public funding, with the highest percentage of 58.64% in 2019 and the highest funding value of CNY 131.51 million in 2020. Funding sources are followed by out-of-pocket payments (30–40%). The overall funding value continues to grow to CNY 78.53 million in 2020, in contrast to the trend of public funding share, which gradually decreases to a minimum value of 30.36% in 2015–2019 and rises by 3 percentage points in 2020 (Table 3). From the Sankey diagram (Figure 1), the three types of financing flows to different institutions, the main source of financing for general hospitals comes from public financing (57.96%), followed by out-of-pocket payments (38.23%), and the main source of financing for primary care institutions (including community health service centers, community health service stations, township health centers, outpatient clinics, clinics, and village health offices) Voluntary financing scheme mainly goes to general hospitals (96.08%), but it is also the least source of financing for general hospitals (3.81%).
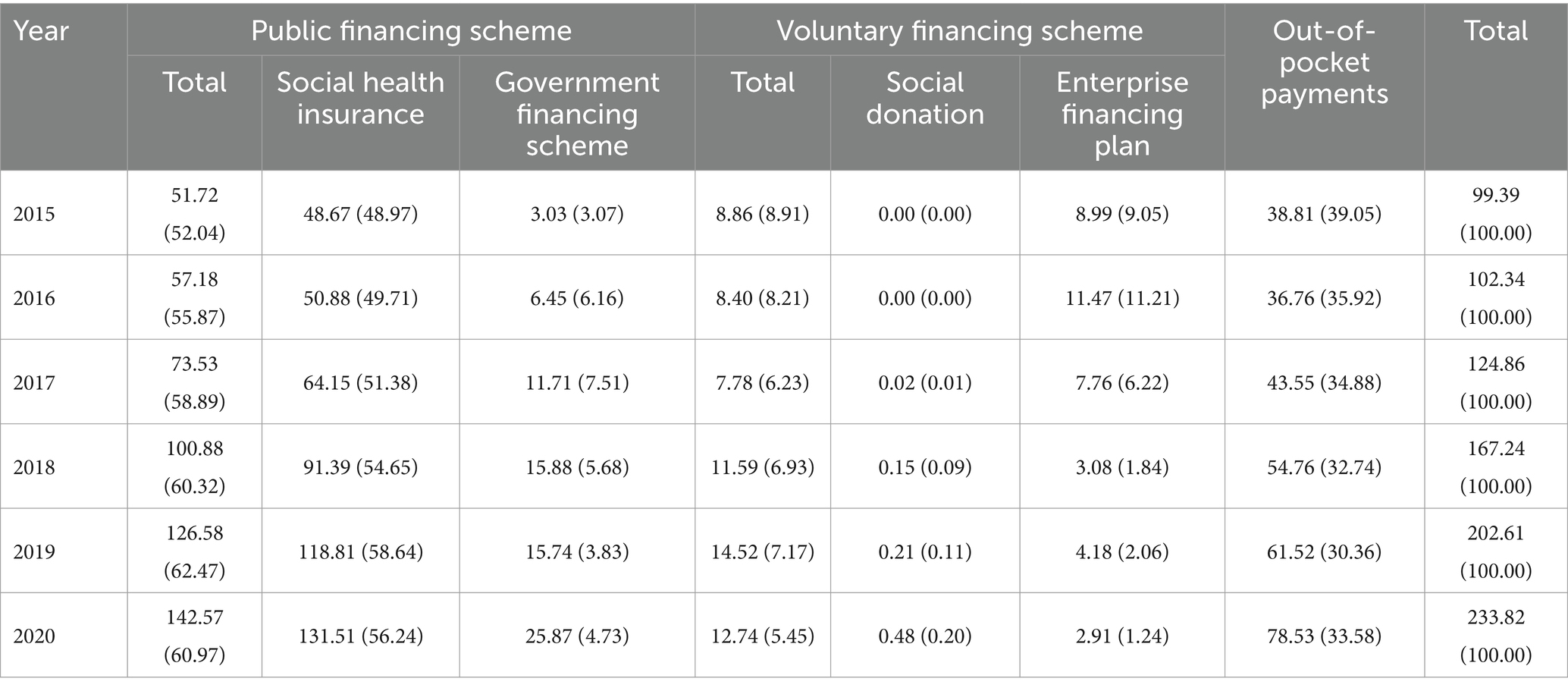
Table 3. Distribution of anxiety outpatient financing costs in Liaoning Province, 2015–2020 [million (%)].
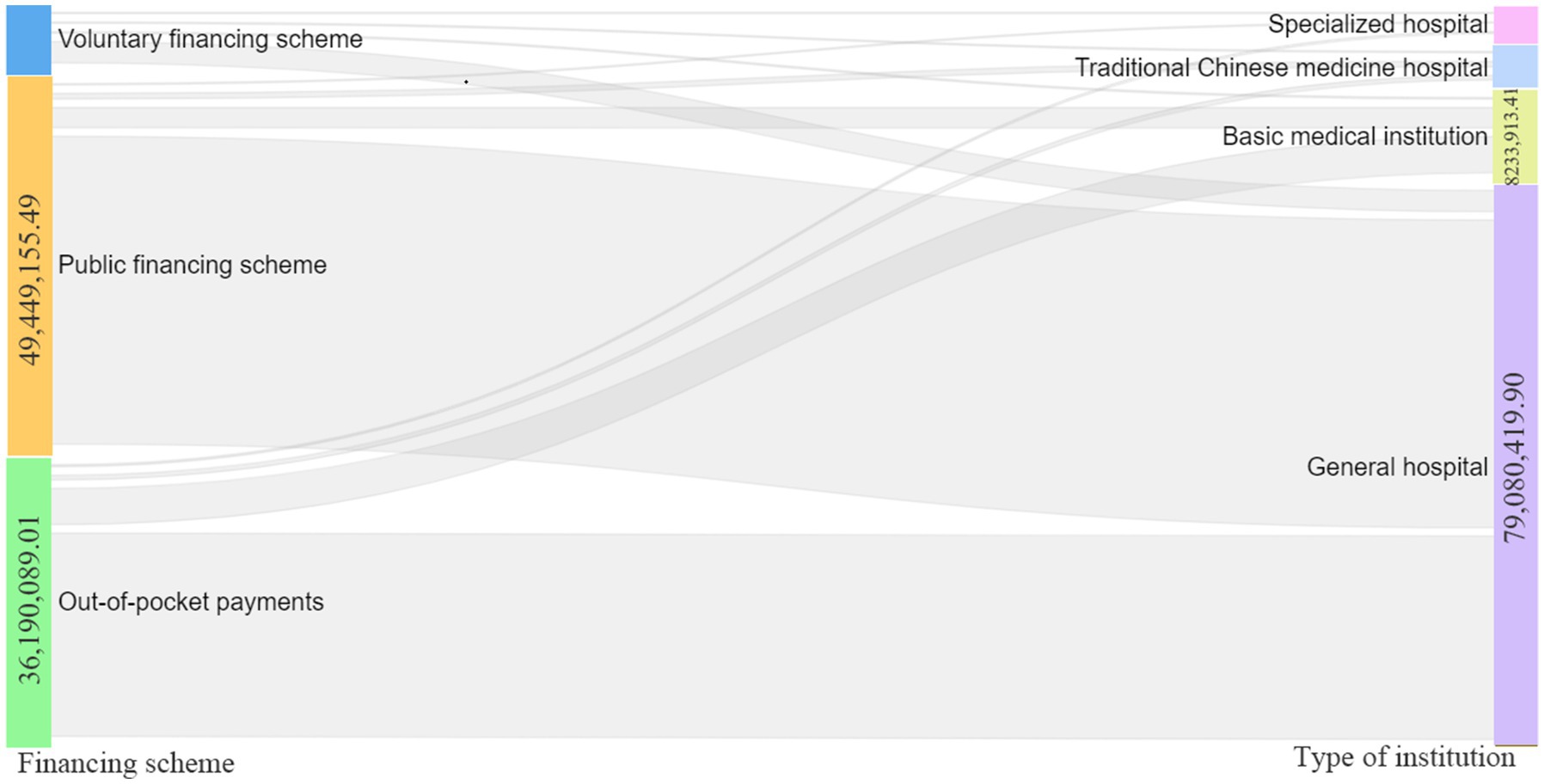
Figure 1. Sankey diagram CCE with 2015–2020 anxiety disorders according to funding structure flow to different institutions average. CCE, current care expenditures.
Factors affecting the cost of anxiety disorders
According to the results of the one-way analysis of factors (including Mann–Whitney U test and Kruskal-Wallis H test) in Table 4, the p-values are all less than or equal to 0.05, so there is a significant difference in the results of the different subgroups; further two-by-two comparisons of the results and the median comparison show that purchase western drugs, purchase prepared Chinese drugs, have a checkup, male, 45–59 years old, tertiary hospital, provincial level, general hospital, the year of 2017 with two-by-two comparisons within the group p-value are less than or equal to 0.05, and outpatient costs for anxiety disorders had the largest median value, indicating that purchase western drugs, purchase prepared Chinese drugs, have a checkup, male, 45–59 years old, tertiary hospital, provincial level, general hospital, the year of 2017 was associated with high outpatient costs for anxiety disorders.
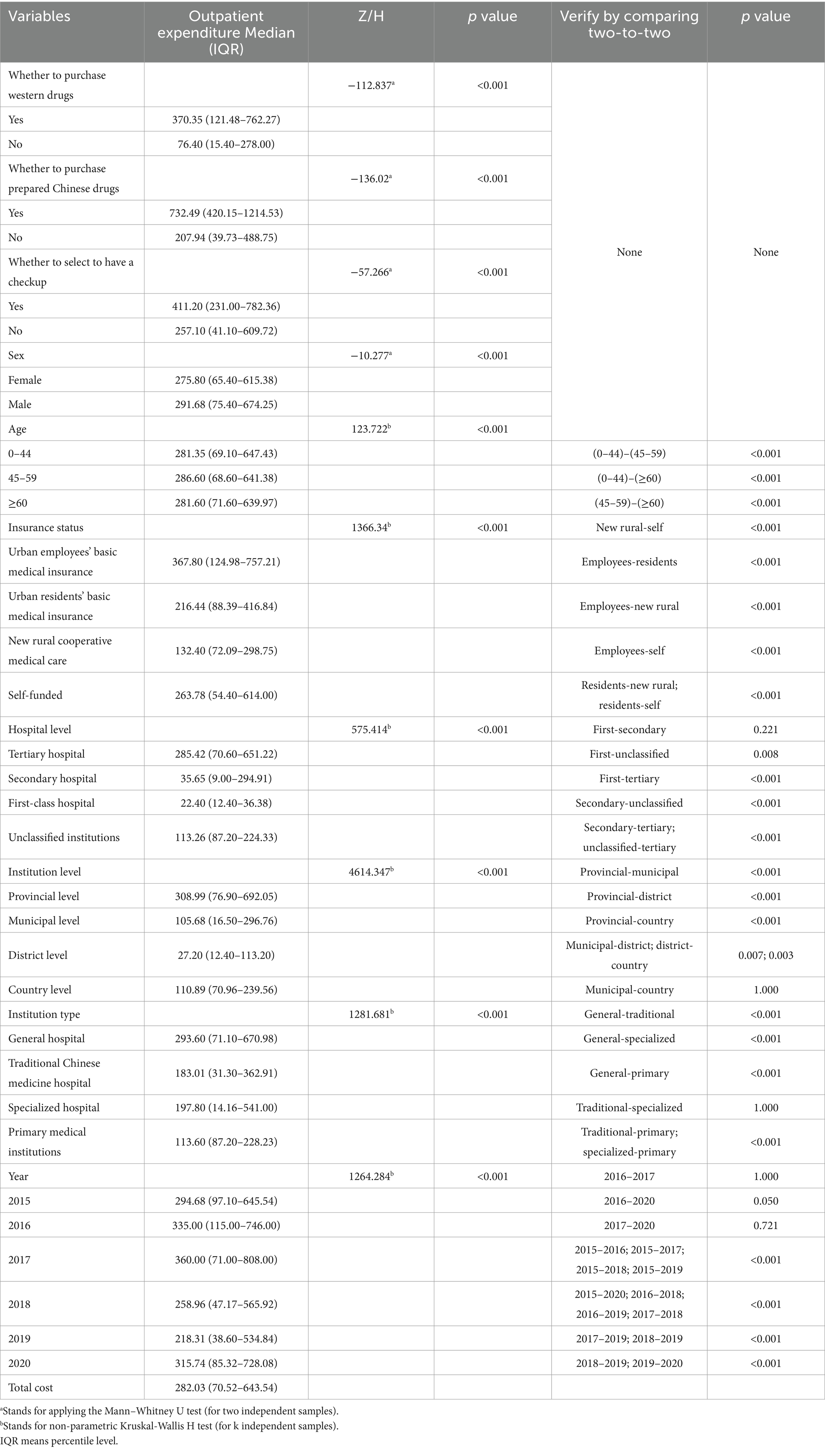
Table 4. Composition of different subgroups and differences in outpatient costs for anxiety disorders in the sample.
This study had a high linear correlation between the independent variables, the independent variables were not covariate with the dependent variable, and the multivariate analysis model explained 34.8% of the variation in outpatient costs for anxiety disorders in Liaoning Province. According to the standardized coefficient results of the multiple linear regression analysis in Table 5, the high positive effects on high outpatient costs for anxiety disorders were, in order, provincial level, purchase of western drugs, purchase of prepared Chinese drugs, choice of having a checkup, urban employees’ basic medical insurance, 0–44 years old, and the negative effects were, in order, tertiary hospitals, and time of visit for 2018, Traditional Chinese medicine hospital, female, and district level.
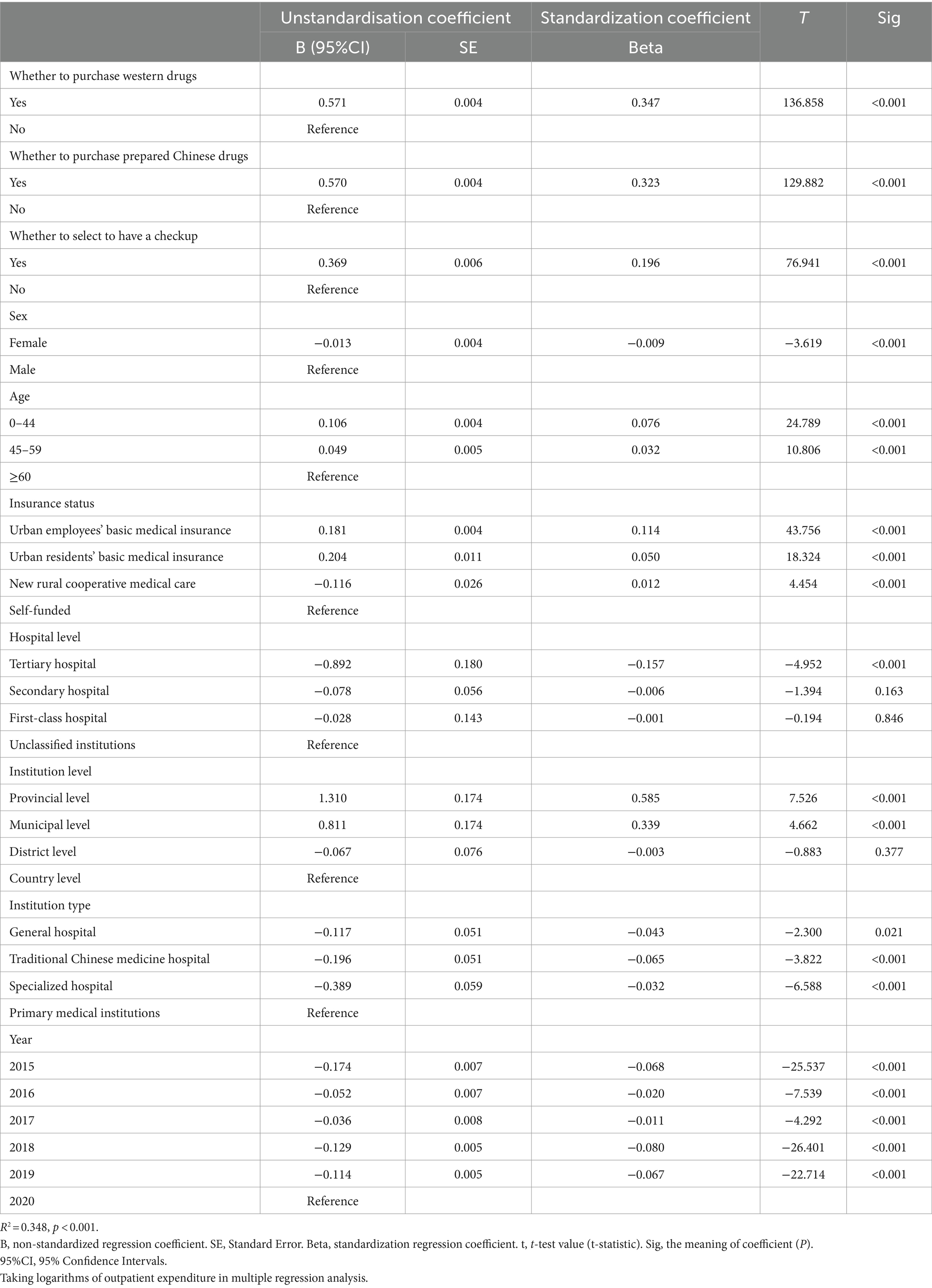
Table 5. Results of multiple linear regression analysis of outpatient costs for anxiety disorders by different groups.
Model construction to explore the influencing factors
After constant adjustment and correction the SEM shown in Figure 2 was constructed to explore the factors influencing the outpatient expenditure for anxiety disorders. According to the constant fitting to exclude some variables, the variables included in the model are insurance status, institution type, year, age, and lg (outpatient expenditure), and combined with the reference range of the goodness-of-fit index, it was judged that this model fits well, that is, χ2 = 0.980, df = 1, χ2/df = 0.980, CFI = 1.000, NFI = 1.000, RFI = 0.999, IFI = 1.000, TLI = 1.000, RMSEA = 0.000. Insurance status can be determined by institution type (β = −0.06, p < 0.001), age (β = −0.13, p < 0.001) and purchase western drugs (drug_w) (β = −0.07, p < 0.001) negatively and indirectly affect anxiety disorder outpatient expenditure, can positively and indirectly affect anxiety disorder outpatient expenditure through year (β = −0.11, p < 0.001). Institution type can negatively and indirectly affect anxiety disorder outpatient expenditure through year (β = −0.05, p < 0.001), and drug_w can indirectly and positively affect anxiety disorder outpatient expenditure through age (β = 0.16, p < 0.001). Insurance status (β = −0.10, p < 0.001), and institution type (β = −0.07, p < 0.001), and age (β = −0.11, p < 0.001) negatively, year (β = 0.03, p < 0.001) and drug_w (β = 0.35, p < 0.001) positively, all directly influenced anxiety disorder outpatient expenditure. This model explained 32.20% of the variation in anxiety disorder outpatient costs.
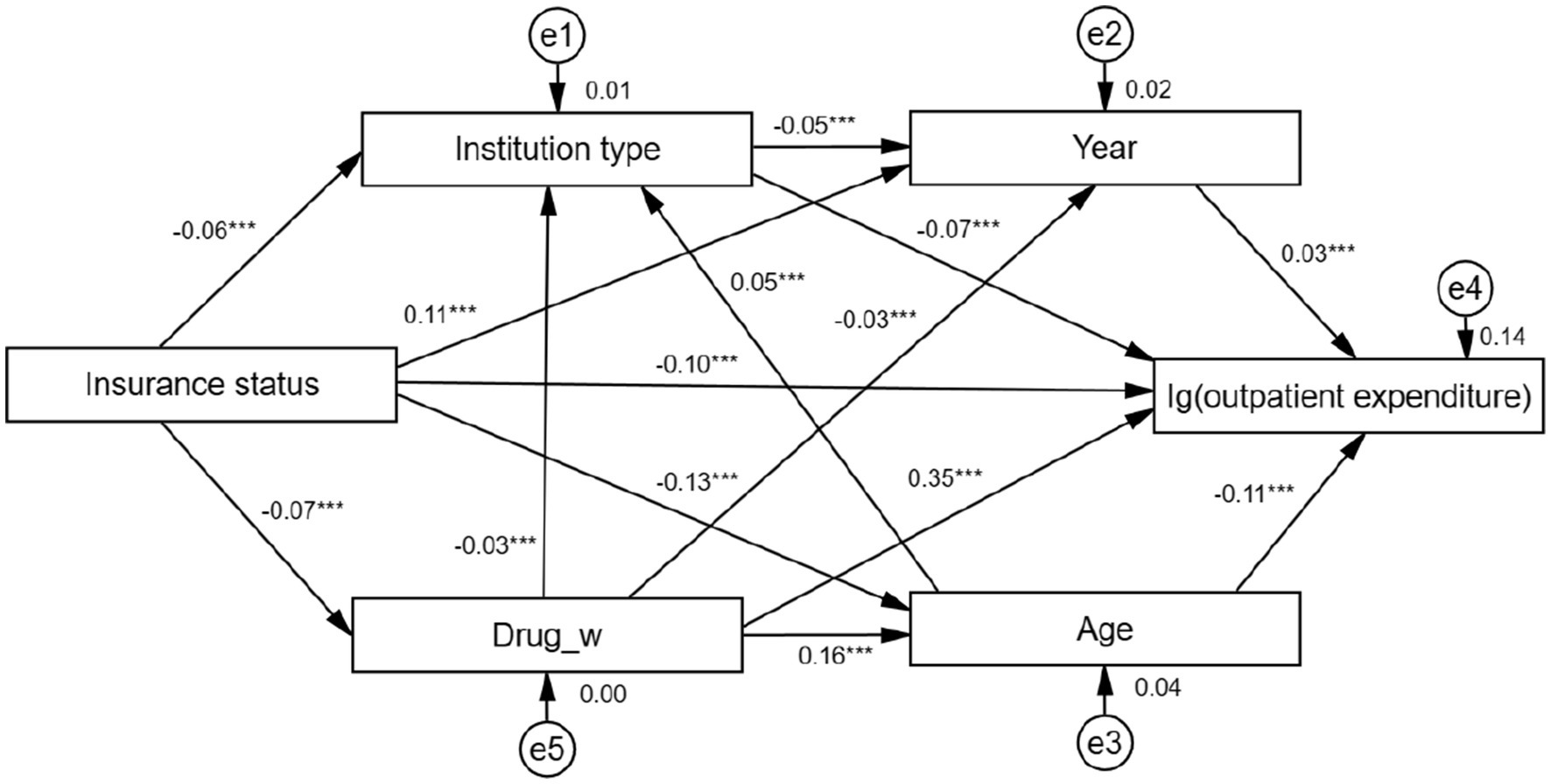
Figure 2. Structural equation modeling of factors influencing anxiety disorder outpatient expenditure. ***Coefficients of the structural equation modeling are of significant meaning.
Insurance status (in order of actual reimbursement ratio): Basic medical insurance for urban workers [actual reimbursement ratio = 75.60% (45)] = 1, urban residents’ basic medical insurance [59.70% (45)] = 2, new rural cooperative medical care [35.00% (46)] = 3, self-funded (0.00%) = 4. Institution type include general hospitals = 1, Chinese hospitals = 2, specialty hospitals = 3, primary health care institutions = 4. Drug_w includes if no western drugs are purchased = 0, purchase of western drugs = 1. Year contain 2015, 2016, 2017, 2018, 2019, 2020. Age: 0–44 = 1.45–59 = 2≥60 = 3.
Taking logarithms of outpatient expenditure in the structural equation model.
Discussion
This is the first study to measure and analyze the outpatient costs of anxiety disorders in Liaoning Province, China based on SHA2011. Our study provides a certain methodological and theoretical basis for domestic and foreign scholars to assess the economic burden of anxiety disorders, and fills the gap of studying the costs of anxiety disorders based on SHA2011, an international accounting system.
Our study found that funding for the treatment of anxiety disorders comes primarily from public funding programs and out-of-pocket payments, with higher levels in general hospitals, followed by primary care. Out-of-pocket costs are an important correlate of catastrophic healthcare expenditures (47), and if they could be reduced to less than 15%, the likelihood of catastrophic healthcare expenditures for families could be greatly reduced (48). With an out-of-pocket percentage of 35% in this study, families are likely to incur catastrophic medical expenditures and fall into poverty as a result of treating anxiety disorders. And when patients are unable to afford treatment, they are less likely to seek treatment and take medication as prescribed (49), leading to disability and loss of life (50). Therefore, efforts and policies should be focused on reducing OOP costs and their rates (51).
From the point of view of the flow of funds, general hospitals accounted for a large proportion, and primary care organizations accounted for a small proportion. The reasons for this are, firstly, the lack of institutional constraints on patients’ first-visit institutions leads to overuse of excellent health resources and increases the burden of disease (52); and secondly, as patients with anxiety disorders are often accompanied by a variety of physical illnesses, patients are more willing to choose large hospitals with complex laboratory and examination equipment (53). However, anxiety disorders are common in primary care (54–56), only 13% of patients were treated in primary care (57) and 31–41% receive appropriate care for anxiety disorders (58, 59). The main reasons for this are that 84.0 and 86.1% of primary healthcare workers generally have low educational qualifications, resulting in relatively poor service capacity and quality; poor salary and benefits, and more serious brain drain; only basic medicines are allowed to be equipped, with fewer types of medicines, and distribution distances are farther away and inconvenient for transportation, resulting in patients’ medication needs not being met (53); primary care general physicians have limited training in anxiety assessment, evidence-based behavioral and cognitive interventions (58, 60–62).
This study found that among anxiety disorders, generalized anxiety disorder had the highest cost burden, which is consistent with Marciniak’s findings (63). The cost per patient for generalized anxiety disorder was $2,165–3,607 in Europe (64, 65), $6,472 in the United States (66), £1,313 in the United Kingdom (67) and €6,152 in Spain (68). The next most common disorder is mixed anxiety disorder, with 58–59% of patients suffering from both anxiety and depression (69–71), which is the most disabling disorder in the world (72). With an investment of $147 billion in 36 countries to expand coverage of this disorder in 2016–2030 (73). The total cost of mixed anxiety disorders in Spain is about €60 million and the indirect cost is about 40.2 million euros (72); the annual direct medical cost per patient in Singapore is S$1050 (2); the per capita social cost of care in the Netherlands is €1,035 (74); the health system, patient, and social costs for Canadian patients to receive minimal appropriate treatment are $5,752, $536, and $6,266, respectively (35); the average annual medical cost of this disorder in the United States cost is $20,963, and the health insurance system pays $9,132 more than without any illness (75). In summary, the burden of treating anxiety disorders is very large.
We explored the factors influencing the cost of outpatient anxiety disorders by univariate analysis, multifactor analysis, and constructing structural equation models. The results of the univariate analysis showed significant differences within each subgroup (p < 0.001). Multiple linear regression analysis was used for the multifactor analysis, and the standardized coefficient B for the purchase of western and prepared Chinese drugs was 0.347 and 0.323 higher than that for the absence of western and prepared Chinese drugs, and the SEM results showed the highest path coefficient of 0.35 for the cost of western drugs and log anxiety disorder outpatient costs, indicating that the purchase of drugs was the factor most associated with high anxiety disorder outpatient costs. Some studies have shown that drugs are an effective and more cost-effective first-line treatment option (6) because of its higher dispersion of resources and better patient accessibility (76). Drugs are fundamental to ensuring healing from anxiety disorders (77, 78),with about half of patients with anxiety disorders choosing drugs (approximately $16,855 million) (10, 13) and drugs using increased over time to 63.8% (79), the criterion for adequacy of anxiety disorder treatment is at least 2 months of drugs (80), thus providing evidence that drugs affect a significant factor in high costs. The study found a higher standardized coefficient of 0.196 for selecting to have a checkup than not selecting to have a checkup, suggesting that the choice to have a checkup is associated with high anxiety disorder outpatient costs, which is consistent with the findings of a study in Turkey, which noted that the highest expenditures were for having a checkup (81). A similar finding was found in a study in Sri Lanka, where 14% of the costs in the study were spent on having a checkup (82). The study also found that the standardized coefficient B results from multiple regression analysis showed that urban employees’ basic medical insurance were 0.114 higher than self-funded and the path coefficient between SEM insurance type and log outpatient costs was −0.10, both indicating that urban employees’ basic medical insurance were associated with higher outpatient costs for anxiety disorders, which may be due to the fact that the uninsured consume fewer health care resources and make less use of health care resources, while those with insurance utilize more health resources and therefore have higher health care costs, which is consistent with existing research (83). The standardized coefficient B for age 0–44 years is 0.076 higher than age 60 years, indicating that the young are associated with high anxiety disorder outpatient costs, adolescents are an important part of youth, and some studies have shown that anxiety disorders are the most common psychiatric disorders in adolescence (84), with initial symptoms appearing before school age, with typical anxiety symptoms appearing around age 7 (84), and then a gradual increase in prevalence through adolescence (85), with an average onset age at 13 years (86) and affecting 2.9% of children and 4.6% of adolescents (87). Some studies have shown that the annual per capita cost of treating anxiety disorders in adolescents is $6,405, the average cost of using mental health services is $8,615, and the average cost of primary health care is $1,591 (88). Thus the individual and family cost burden of anxiety disorders in adolescence is enormous, and screening, early prevention, and early intervention treatment must focus on this age group in adolescents.
In terms of health care financing and insurance, it is recommended to increase financial investment, raise the proportion of anxiety health investment in government health expenditure, and increase the outpatient reimbursement ratio for anxiety disorders, which can reduce the burden of anxiety treatment for insured people and low-income people; it can also learn from Australia, the United Kingdom, and the Philippines to raise the tax on tobacco to be used for health care financing (52); and learn from the French special tax of 1% on pharmaceutical companies and advertising companies for social security fundraising. At present, the coverage rate of the three basic medical care for urban workers, urban residents and new rural cooperative medical care in China has reached 95%, but there are still many phenomena of poverty due to illness and a large burden of medical care due to illness, which prompts us to establish an integrated medical care policy with consistent rights and responsibilities to realize the integration of the three basic medical care (52). In the choice of institutions, the establishment of grass-roots first diagnosis, hierarchical diagnosis and treatment, two-way referral system of medical care, the first treatment at the grass-roots level, patients who meet the referral conditions are referred to higher-level institutions, and the medical insurance of patients who go beyond the level of treatment will not be reimbursed (52). For primary care institutions, the first step is to improve the psychiatric expertise, medication protocols, and basic cognitive-behavioral therapy knowledge of general practitioners; second, to discuss individualized treatment plans with the patient’s family members (89) and to provide routine psychoeducational and cognitive-behavioral interventions (53); furthermore, and then, to actively integrate video consultations with mental health specialists (90) to reduce the cost of patients’ medical care and the costs outside of the health insurance; Finally, increase primary diagnosis and care by primary care general practitioners; due to the strong emotional confusion and somatic symptoms of anxiety disorders, it is recommended to increase the proportion of primary care facilities less than 1 km away from the population, so as to provide patients with better access to general practitioners (52). Improve the basic drug system and increase the reimbursement ratio of anxiety disorder medication and psychological counseling, because anxiety disorder is a chronic disease that lasts for a long time, so that patients have the ability to afford the cost of anxiety disorder treatment on a continuous basis, which can improve the adherence of patients. Strengthening mental health education for anxiety disorders and other mental health disorders; a large percentage of stigmatized mental illnesses exist in China, carrying stigmatized labels for medical care and treatment (91).
For anxiety disorders, it is best to diagnose and treat them early, so that the prognosis will be better. First of all, in order to enable residents to detect the disease early and receive professional treatment in hospitals at the first time, to reduce the public’s sense of shame from all angles, to guide patients to standardize their medical treatment, and to reduce the medical burden brought by deterioration of the disease, community general practitioners should strengthen the training of knowledge and skills of anxiety disorders and improve the attitude toward patients with anxiety disorders, and strengthen the preventive work, and psychiatrists should also give a certain degree of knowledge of anxiety disorders in the consultation, so that patients can rationally view anxiety disorders and seek medical treatment and prevention earlier. Psychiatrists should also provide some knowledge about anxiety disorders during consultation, so that patients can rationally view anxiety disorders and seek medical treatment and prevention at an earlier stage (90).
This study has some limitations. First, this study only examined direct health care costs regarding anxiety disorders and did not account for economic losses involving other aspects such as lost production, lost work, and lost manpower; second, this study only considered the cost of the first anxiety visit and did not consider the cost of other comorbidities (91). Therefore the above limitations may have contributed to the underestimation of the cost of anxiety disorders in this study. Secondly, as anxiety disorders first develop mostly during adolescence and have associated social and economic costs throughout life (92, 93), schools are one of the key places to provide preventive interventions for anxiety disorders, while being less likely to pose a social risk, are more cost-effective, and, if implemented early, have the potential to prevent the emergence of mental health problems by building resilience and coping strategies in young people (94). Furthermore, exercise can help prevent anxiety symptoms and significantly reduce the risk of anxiety. Exercise can help the body to improve stress capacity and relieve anxiety, and aerobic exercise is more effective in combating anxiety. From early intervention to early prevention, early exercise to reduce psychological stress can prevent people from developing depression and anxiety, thus reducing the incidence of depression and anxiety disorders (95). Finally, residents are more exposed to green spaces, forests or the outdoors, or to blue spaces such as rivers, streams, ponds, lakes and the coast, and for those who live in cities, urban parks can offer similar benefits to forests, and spending time in nature can intervene and reduce the symptoms of anxiety as well as emotional recurrence (96–98).
Conclusion
This study analyzed the total anxiety disorder outpatient CCE, subtype anxiety disorder costs, funding structure, and specific costs for different subgroups in Liaoning Province from 2015 to 2020 based on SHA2011. Univariate analysis, multi-factor analysis, and construction of SEM on anxiety disorder outpatient costs were used to explore the factors influencing high anxiety disorder outpatient CCE. Finally, actionable recommendations were made in order to reduce the burden of anxiety disorder outpatients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Patients’ personal information is digitally coded, and the numbers inside are desensitized, so there is no personal privacy involved.
Author contributions
XS: Conceptualization, Data curation, Investigation, Software, Visualization, Writing – original draft. YZ: Data curation, Investigation, Software, Writing – original draft. QW: Investigation, Methodology, Project administration, Writing – review & editing. PC: Conceptualization, Data curation, Investigation, Software, Supervision, Validation, Writing – review & editing. YM: Funding acquisition, Project administration, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was funded by China National Health Development Research Center Project of Humanities and Social Sciences Grant No. 2022000000430.
Acknowledgments
We thank all the participants and China National Health Development Research Center for help with SHA 2011 analysis. We thank to the support of Health Economics Association of Liaoning Province in providing data. We are grateful for the support of Health Commission of Liaoning Province in providing data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1329596/full#supplementary-material
References
1. Kessler, RC, Aguilar-Gaxiola, S, Alonso, J, Chatterji, S, Lee, S, Ormel, J, et al. The global burden of mental disorders: an update from the WHO world mental health (WMH) surveys. Epidemiol Psichiatr Soc. (2009) 18:23–33. doi: 10.1017/s1121189x00001421
2. Chodavadia, P, Teo, I, Poremski, D, Fung, DSS, and Finkelstein, EA. Prevalence and economic burden of depression and anxiety symptoms among Singaporean adults: results from a 2022 web panel. BMC Psychiatry. (2023) 23:104. doi: 10.1186/s12888-023-04581-7
3. World Health Organization. Depression and other common mental disorders: global health estimates. Geneva: World Health Organization (2017).
4. Patel, S, Boutry, C, Patel, P, Craven, MP, Guo, B, Zafar, A, et al. A randomised controlled trial investigating the clinical and cost-effectiveness of alpha-stim AID cranial electrotherapy stimulation (CES) in patients seeking treatment for moderate severity depression in primary care (alpha-stim-D trial). Trials. (2022) 23:250. doi: 10.1186/s13063-022-06192-1
5. Préville, M, Boyer, R, Vasiliadis, H-M, Grenier, S, Streiner, D, Cairney, J, et al. Persistence and remission of psychiatric disorders in the Quebec older adult population. Can J Psychiatr. (2010) 55:514–22. doi: 10.1177/070674371005500806
6. Szuhany, KL, and Simon, NM. Anxiety disorders: a review. JAMA. (2022) 328:2431–45. doi: 10.1001/jama.2022.22744
7. Nyuthe, CK, and Stein, DJ. Anxiety and related disorders and physical illness. Basel, Switzerland: Key Issues in Mental Health: Comorbidity of Mental and Physical Disorders (2015).
8. Lépine, J-P. The epidemiology of anxiety disorders: prevalence and societal costs. J Clin Psychiatry. (2002) 63:4–6. doi: 10.4088/JCP.v63n0101
9. Lochner, C, Mogotsi, M, Toit, PLD, Kaminer, D, Niehaus, DJ, Stein, DJ, et al. Quality of life in anxiety disorders: a comparison of obsessive-compulsive disorder, social anxiety disorder, and panic disorder. Psychopathology. (2003) 36:255–62. doi: 10.1159/000073451
10. Shirneshan, E, Bailey, J, Relyea, G, Franklin, BE, Solomon, DK, and Brown, LM. Incremental direct medical expenditures associated with anxiety disorders for the U.S. adult population: evidence from the medical expenditure panel survey. J Anxiety Disord. (2013) 27:720–7. doi: 10.1016/j.janxdis.2013.09.009
11. Evaluation IfHMa. Explore results from the 2019 global burden of disease (GBD) study. (2019). Available at: https://vizhub.healthdata.org/gbd-results/ (Acceseed March 25th, 2023).
12. Konnopka, A, and König, H. Economic burden of anxiety disorders: a systematic review and meta-analysis. PharmacoEconomics. (2020) 38:25–37. doi: 10.1007/s40273-019-00849-7
13. Mccrone, P, Dhanasiri, S, Patel, A, et al. Paying the price: the cost of mental health care in England to 2026. London: Kings Fund (2008).
14. Guo, X, Meng, Z, Huang, G, Fan, J, Zhou, W, Ling, W, et al. Meta-analysis of the prevalence of anxiety disorders in mainland China from 2000 to 2015. Sci Rep. (2016) 6:28033. doi: 10.1038/srep28033
15. Phillips, MR, Zhang, J, Shi, Q, Song, Z, Ding, Z, Pang, S, et al. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey. Lancet. (2009) 373:2041–53. doi: 10.1016/S0140-6736(09)60660-7
16. Guo, K, Cui, Z, Cui, L, et al. Epidemiological survey of mental illness in people aged 18 years and above in Hebei Province. Papers of the seventh annual National Academic Conference of the Chinese Medical Association psychiatry branch; 2006; Beijing. Beijing, China: Hebei Sixth People's Hospital (2006). p. 21–22.
17. Li, N, Jiang, C, Liu, H, et al. Epidemiological survey of anxiety disorders in urban and rural residents of Liaoning Province. China J Preven Control Chronic Non-commun Dis. (2008) 16:179–81. doi: 10.3969/j.issn.1004-6194.2008.02.023
18. Chen, X. Epidemiological survey of mental health in community population in Xi’an, China. Xi'an,China: Fourth Military Medical University (2012).
19. Li, T. The investigation of mental disorders and their impact factors in rural areas adults of Ningxia. Ningxia: Ningxia Medical University (2013).
20. Lu, D, Zheng, H, Xiao, Y, et al. Epidemiologic survey of anxiety disorders in community population aged 15 and older in Yunfu City. J Clin Psychiatry. (2015) 25:107–8.
21. Zhang, X. Study on prevalence of anxiety disorders and correlation factors. Dalian: Dalian Medical University (2010).
22. Wei, B, Chen, Q, Feng, Q, et al. Epidemiological survey on mental illness in urban and rural residents of Guangxi Zhuang autonomous region. J Guangxi Med Univ. (2010) 27:951–6.
23. Chen, H, Guo, H, Pan, H, et al. Qinhuangdao epidemiological survey of 18 years age and people over mental illness. Shanxi Med J. (2012) 41:1191–4.
24. Chapdelaine, A, Vasiliadis, H-M, Provencher, MD, Norton, PJ, and Roberge, P. Cost-effectiveness of transdiagnostic group cognitive behavioural therapy for anxiety disorders v. treatment as usual: economic evaluation of a pragmatic randomized controlled trial over an 8-month time horizon using self-reported data. Psychol Med. (2023) 53:6570–82. doi: 10.1017/S0033291722003920
25. Kaczkurkin, AN, and Foa, EB. Cognitive-behavioral therapy for anxiety disorders: an update on the empirical evidence. Dialogues Clin Neurosci. (2015) 17:337–46. doi: 10.31887/DCNS.2015.17.3/akaczkurkin
26. Witlox, M, Kraaij, V, Garnefski, N, Bohlmeijer, E, Smit, F, and Spinhoven, P. Cost-effectiveness and cost-utility of an acceptance and commitment therapy intervention vs. a cognitive behavioral therapy intervention for older adults with anxiety symptoms: a randomized controlled trial. PLoS One. (2022) 17:e0262220. doi: 10.1371/journal.pone.0262220
27. Jankovic, D, Saramago Goncalves, P, Gega, L, Marshall, D, Wright, K, Hafidh, M, et al. Cost effectiveness of digital interventions for generalised anxiety disorder: a model-based analysis. PharmacoEconomics. (2022) 6:377–88. doi: 10.1007/s41669-021-00318-y
28. Risør, BW, Frydendal, DH, Villemoes, MK, Nielsen, CP, Rask, CU, and Frostholm, L. Cost effectiveness of internet-delivered acceptance and commitment therapy for patients with severe health anxiety: a randomised controlled trial. Pharmacoecon Open. (2022) 6:179–92. doi: 10.1007/s41669-021-00319-x
29. Jones, BG, Reardon, T, Creswell, C, Dodd, HF, Hill, C, Jasper, B, et al. Minimising young Children's anxiety through schools (MY-CATS): statistical analysis plan for a cluster randomised controlled trial to evaluate the effectiveness and cost-effectiveness of an online parent-led intervention compared with usual school practice for young children identified as at risk for anxiety disorders. Trials. (2022) 23:1054. doi: 10.1186/s13063-022-06899-1
30. Zhou, Y, Cao, Z, Yang, M, Xi, X, Guo, Y, Fang, M, et al. Comorbid generalized anxiety disorder and its association with quality of life in patients with major depressive disorder. Sci Rep. (2017) 7:40511. doi: 10.1038/srep40511
31. Ma, X, Xiang, Y, Cai, Z, Lu, JY, Li, SR, Xiang, YQ, et al. Generalized anxiety disorder in China: prevalence, sociodemographic correlates, comorbidity, and suicide attempts. Perspect Psychiatr Care. (2009) 45:119–27. doi: 10.1111/j.1744-6163.2009.00212.x
32. Puspitasari, IM, Sinuraya, RK, Rahayu, C, Witriani, W, Zannah, U, Hafifah, A, et al. Medication profile and treatment cost estimation among outpatients with schizophrenia, bipolar disorder, depression, and anxiety disorders in Indonesia. Neuropsychiatr Dis Treat. (2020) 16:815–28. doi: 10.2147/NDT.S240058
33. Sicras-Mainar, A, Rejas-Gutiérrez, J, Pérez-Paramo, M, Sánchez-Alvarez, L, Navarro-Artieda, R, and Darbà, J. Consequences on economic outcomes of generic versus brand-name drugs used in routine clinical practice: the case of treating peripheral neuropathic pain or generalized anxiety disorder with pregabalin. Expert Rev Pharmacoecon Outcomes Res. (2019) 19:45–57. doi: 10.1080/14737167.2019.1519399
34. Torres-Granados, GI, Santana-Miranda, R, Barrera-Medina, A, Cruz-Cruz, C, Jiménez-Correa, U, Rosenthal, L, et al. The economic costs of insomnia comorbid with depression and anxiety disorders: an observational study at a sleep clinic in Mexico. Sleep Biol Rhythms. (2023) 21:23–31. doi: 10.1007/s41105-022-00412-6
35. Lamoureux-Lamarche, C, Berbiche, D, and Vasiliadis, HM. Health care system and patient costs associated with receipt of minimally adequate treatment for depression and anxiety disorders in older adults. BMC Psychiatry. (2022) 22:175. doi: 10.1186/s12888-022-03759-9
36. Aizhan, S. The World Health Organization classifies a few to a few years of age as youth, and how about middle-age. (2022). Available at: https://edu.iask.sina.com.cn/jy/hlxbyCzxti.html (Acceseed April 19, 2024).
37. Zhai, T, Zhang, Y, Wan, Q, et al. New system of health accounts introduction of system of health accounts 2011. Chinese Health Econ. (2013) 32:13–5. doi: 10.7664/CHE20130103
38. Alwhaibi, M, Meraya, AM, and AlRuthia, Y. Healthcare expenditures associated with comorbid anxiety and depression among adults with migraine. Front Neurol. (2021) 12:658697. doi: 10.3389/fneur.2021.658697
39. World Health Organization. ICD-10 classification of mental behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization (1993).
40. Plana-Ripoll, O, Momen, NC, McGrath, JJ, Wimberley, T, Brikell, I, Schendel, D, et al. Temporal changes in sex- and age-specific incidence profiles of mental disorders-a nationwide study from 1970 to 2016. Acta Psychiatr Scand. (2022) 145:604–14. doi: 10.1111/acps.13410
41. Fei Zhong, ZC, and Long, H. Primary care entrepreneurship tutorial for college students. Tianjing, China: Tianjin Science and Technology Press (2012).
42. He, J, Yin, Z, Duan, W, Wang, Y, and Wang, X. Factors of hospitalization expenditure of the genitourinary system diseases in the aged based on "system of health account 2011" and neural network model. J Glob Health. (2018) 8:020504. doi: 10.7189/jogh.08.020504
43. Zhu, Y, Liu, C, Zhang, L, Fang, Q, Zang, S, and Wang, X. How to control the economic burden of treating cardio-cerebrovascular diseases in China? Assessment based on system of health accounts 2011. J Glob Health. (2020) 10:010802. doi: 10.7189/jogh.10.010802
44. Li, M, Zheng, A, Duan, W, Mu, X, Liu, C, Yang, Y, et al. How to apply SHA 2011 at a subnational level in China's practical situation: take children health expenditure as an example. J Glob Health. (2018) 8:010801. doi: 10.7189/jogh.08.010801
45. Administration NHS. Statistical bulletin on the development of the national health care insurance business in 2019. (2020). Available at: http://www.nhsa.gov.cn/art/2020/6/24/art_7_3268.html (Acceseed April 13, 2023).
46. Ma, W, and Li, H. From new rural cooperative medical care to basic medical insurance for urban and rural residents: an analysis of the policy effects of urban and rural medical insurance coordination. China Econ Stud. (2021) 4:146–57. doi: 10.19365/j.issn1000-4181.2021.04.11
47. Tong, W, and Ning, X. Analysis and implications of health care financing in Russia from the perspective of universal health coverage. Comp Econ Soc Syst. (2019):160–74.
48. Xu, K, Evans, DB, Kawabata, K, Zeramdini, R, Klavus, J, and Murray, CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. (2003) 362:111–7. doi: 10.1016/s0140-6736(03)13861-5
49. Iuga, AO, and McGuire, MJ. Adherence and health care costs. Risk Manag Healthc Policy. (2014) 7:35–44. doi: 10.2147/RMHP.S19801
50. Tamblyn, R, Laprise, R, Hanley, JA, Abrahamowicz, M, Scott, S, Mayo, N, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. (2001) 285:421–9. doi: 10.1001/jama.285.4.421
51. World Health Organization. Universal health coverage. (2022). Available at: https://www.who.int/zh/news-room/fact-sheets/detail/universal-health-coverage-(uhc) (Acceseed April 13, 2023).
52. Wang, Y, Wang, X, Jia, X, et al. Suggestions for strategies to achieve the goal of universal health coverage in China. J Nanjing Med Univ. (2015) 15:176–81. doi: 10.7655/NYDXBSS20150303
53. Roy-Byrne, PP, and Wagner, A. Primary care perspectives on generalized anxiety disorder. J Clin Psychiatry. (2004) 18:841–58. doi: 10.1016/j.janxdis.2003.10.005
54. Nisenson, LG, Pepper, CM, Schwenk, TL, and Coyne, JC. The nature and prevalence of anxiety disorders in primary care. Gen Hosp Psychiatry. (1998) 20:21–8. doi: 10.1016/s0163-8343(97)00096-0
55. Serrano-Blanco, A, Palao, DJ, Luciano, JV, Pinto-Meza, A, Luján, L, Fernández, A, et al. Prevalence of mental disorders in primary care: results from the diagnosis and treatment of mental disorders in primary care study (DASMAP). Soc Psychiatry Psychiatr Epidemiol. (2010) 45:201–10. doi: 10.1007/s00127-009-0056-y
56. Harris, EC, and Barraclough, B. Excess mortality of mental disorder. Br J Psychiatry. (1998) 173:11–53. doi: 10.1192/bjp.173.1.11
57. Wang, PS, Lane, M, Olfson, M, Pincus, HA, Wells, KB, and Kessler, RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. (2005) 62:629–40. doi: 10.1001/archpsyc.62.6.629
58. Stein, MB, Roy-Byrne, PP, Craske, MG, Campbell-Sills, L, Lang, AJ, Golinelli, D, et al. Quality of and patient satisfaction with primary health care for anxiety disorders. J Clin Psychiatry. (2011) 72:970–6. doi: 10.4088/JCP.09m05626blu
59. Stein, MB, Sherbourne, CD, Craske, MG, Means-Christensen, A, Bystritsky, A, Katon, W, et al. Quality of care for primary care patients with anxiety disorders. Am J Psychiatry. (2004) 161:2230–7. doi: 10.1176/appi.ajp.161.12.2230
60. Prevention CfDCa Annual number and percent distribution of ambulatory care visits by setting type according to diagnosis group, United States 2009–2010. (2014). Available at: https://www.cdc.gov/nchs/data/ahcd/combined_tables/2009-2010_combined_web_table01.pdf (Acceseed April 13, 2023).
61. Fernández, A, Mendive, JM, Salvador-Carulla, L, Rubio-Valera, M, Luciano, JV, Pinto-Meza, A, et al. Adjustment disorders in primary care: prevalence, recognition and use of services. Br J Psychiatry. (2012) 201:137–42. doi: 10.1192/bjp.bp.111.096305
62. Mitchell, AJ, Rao, S, and Vaze, A. Do primary care physicians have particular difficulty identifying late-life depression? A meta-analysis stratified by age. Psychother Psychosom. (2010) 79:285–94. doi: 10.1159/000318295
63. Marciniak, MD, Lage, MJ, Dunayevich, E, Russell, JM, Bowman, L, Landbloom, RP, et al. The cost of treating anxiety: the medical and demographic correlates that impact total medical costs. Depress Anxiety. (2005) 21:178–84. doi: 10.1002/da.20074
64. Andlin-Sobocki, P, and Wittchen, H-U. Cost of anxiety disorders in Europe. Eur J Neurol. (2005) 12:39–44. doi: 10.1111/j.1468-1331.2005.01196.x
65. Souĕtre, E, Lozet, H, Cimarosti, I, Martin, P, Chignon, JM, Adés, J, et al. Cost of anxiety disorders: impact of comorbidity. J Psychosom Res. (1994) 38:151–60. doi: 10.1016/0022-3999(94)90145-7
66. François, C, Despiégel, N, Maman, K, Saragoussi, D, and Auquier, P. Anxiety disorders, major depressive disorder and the dynamic relationship between these conditions: treatment patterns and cost analysis. J Med Econ. (2010) 13:99–109. doi: 10.3111/13696991003591321
67. Chollet, J, Saragoussi, D, Clay, E, and François, C. A clinical research practice datalink analysis of antidepressant treatment patterns and health care costs in generalized anxiety disorder. Value Health. (2013) 16:1133–9. doi: 10.1016/j.jval.2013.09.001
68. Rovira, J, Albarracin, G, Salvador, L, Rejas, J, Sánchez-Iriso, E, and Cabasés, JM. The cost of generalized anxiety disorder in primary care settings: results of the ANCORA study. Commun Ment Health J. (2012) 48:372–83. doi: 10.1007/s10597-012-9503-4
69. Kessler, RC, Berglund, P, Demler, O, Jin, R, Koretz, D, Merikangas, KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. (2003) 289:3095–105. doi: 10.1001/jama.289.23.3095
70. Kessler, RC, Gruber, M, Hettema, JM, Hwang, I, Sampson, N, and Yonkers, KA. Co-morbid major depression and generalized anxiety disorders in the National Comorbidity Survey follow-up. Psychol Med. (2008) 38:365–74. doi: 10.1017/S0033291707002012
71. Mittal, D, Fortney, JC, Pyne, JM, Edlund, MJ M.D., and Wetherell, JL Ph.D. Impact of comorbid anxiety disorders on health-related quality of life among patients with major depressive disorder. Psychiatr Serv. (2006) 57:1731–7. doi: 10.1176/ps.2006.57.12.1731
72. Fernandez-Piciochi, C, Martín-Saborido, C, Bimbela-Pedrola, JL, and Sarria-Santamera, A. The economic burden of anxiety and depression on the working age population with diabetes in Spain. Int J Health Plann Manag. (2022) 37:715–24. doi: 10.1002/hpm.3367
73. Chisholm, D, Sweeny, K, Sheehan, P, Rasmussen, B, Smit, F, Cuijpers, P, et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry. (2016) 3:415–24. doi: 10.1016/S2215-0366(16)30024-4
74. Prins, M, Bosmans, J, Verhaak, P, van der Meer, K, van Tulder, M, van Marwijk, H, et al. The costs of guideline-concordant care and of care according to patients’ needs in anxiety and depression. J Eval Clin Pract. (2011) 17:537–46. doi: 10.1111/j.1365-2753.2010.01490.x
75. Wallace, K, Zhao, X, Misra, R, and Sambamoorthi, U. The humanistic and economic burden associated with anxiety and depression among adults with comorbid dabetes and hypertension. J Diabetes Res. (2018) 2018:4842520. doi: 10.1155/2018/4842520
76. Slee, A, Nazareth, I, Bondaronek, P, Liu, Y, Cheng, Z, and Freemantle, N. Pharmacological treatments for generalised anxiety disorder: a systematic review and network meta-analysis. Lancet. (2019) 393:768–77. doi: 10.1016/S0140-6736(18)31793-8
77. Dworkin, RH, O’Connor, AB, Kent, J, Mackey, SC, Raja, SN, Stacey, BR, et al. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain. (2013) 154:2249–61. doi: 10.1016/j.pain.2013.06.004
78. Locke, AB, Kirst, N, and Shultz, CG. Diagnosis and management of generalized anxiety disorder and panic disorder in adults. Am Fam Physician. (2015) 91:617–24.
79. Wu, CH, Wang, C-C, Katz, AJ, and Farley, J. National trends of psychotropic medication use among patients diagnosed with anxiety disorders: results from medical expenditure panel survey 2004-2009. J Anxiety Disord. (2013) 27:163–70. doi: 10.1016/j.janxdis.2012.11.004
80. Roberge, P, Fournier, L, Duhoux, A, Nguyen, CT, and Smolders, M. Mental health service use and treatment adequacy for anxiety disorders in Canada. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:321–30. doi: 10.1007/s00127-010-0186-2
81. Islek, D, Kilic, B, and Akdede, BB. Out-of-pocket health expenditures in patients with bipolar disorder, anxiety, schizophrenia and other psychotic disorders: findings from a study in a psychiatry outpatient clinic in Turkey. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:151–60. doi: 10.1007/s00127-017-1465-y
82. Silva, J, Hanwella, R, and Silva, V. Direct and indirect cost of schizophrenia in outpatients treated in a tertiary care psychiatry unit. Ceylon Med J. (2012) 57:14–8. doi: 10.4038/cmj.v57i1.4195
83. Tuckera, K, Darkb, T, and Harmanb, JS. Variation in out of pocket health care costs for individuals with anxiety disorders by type of insurance coverage. J Anxiety Disord. (2018) 58:18–22. doi: 10.1016/j.janxdis.2018.06.003
84. Bennett, S, Walkup, JT, Brent, D, et al. Anxiety disorders in children and adolescents: epidemiology, pathogenesis, clinical manifestations, and course. (2018). Available at: https://www.uptodate.com/contents/anxiety-disorders-in-children-and-adolescents-epidemiology-pathogenesis-clinical-manifestations-and-course (Acceseed April 13, 2023).
85. Bandelow, B, and Michaelis, S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. (2015) 17:327–35. doi: 10.31887/DCNS.2015.17.3/bbandelow
87. Stein, DJ, Lim, CCW, Roest, AM, et al. The cross-national epidemiology of social anxiety disorder: data from the world mental health survey initiative. BMC Med. (2017) 15:143. doi: 10.1186/s12916-017-0889-2
88. Pella, JE, Slade, EP, Pikulski, PJ, and Ginsburg, GS. Pediatric anxiety disorders: a cost of illness analysis. J Abnorm Child Psychol. (2020) 48:551–9. doi: 10.1007/s10802-020-00626-7
89. Zhang, X. Analysis of substance abuse and its treatment countermeasures among elderly patients with anxiety/depression at the primary level. J Pract Cardiopulmonary Vasc Dis. (2014) 22:73–5.
90. Haun, MW, Oeljeklaus, L, Hoffmann, M, Tönnies, J, Wensing, M, Szecsenyi, J, et al. Primary care patients' experiences of video consultations for depression and anxiety: a qualitative interview study embedded in a randomized feasibility trial. BMC Health Serv Res. (2023) 23:9. doi: 10.1186/s12913-022-09012-z
91. Ying, DG-C, Jiang, S, Yang, H, and Zhu, S. Frequency of generalized anxiety disorder in Chinese primary care. Postgrad Med. (2010) 122:32–8. doi: 10.3810/pgm.2010.07.2173
92. Hu, T-w. Perspectives: an international review of the national cost estimates of mental illness, 1990-2003. J Ment Health Policy Econ. (2006) 9:3–13.
93. Patton, GC, Coffey, C, Romaniuk, H, Mackinnon, A, Carlin, JB, Degenhardt, L, et al. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. Lancet. (2014) 383:1404–11. doi: 10.1016/S0140-6736(13)62116-9
94. Jack, L, Andrews, LB, Chapman, C, Teesson, M, Newton, N, Allsop, S, et al. Evaluating the effectiveness of a universal eHealth school-based prevention programme for depression and anxiety, and the moderating role of friendship network characteristics. Psychol Med. (2023) 53:5042–51. doi: 10.1017/S0033291722002033
95. Ni, X. The effects of two different exercise modalities, aerobic exercise and high-intensity interval training, on anxiety and depression in medical students. Hebei: Hebei University (2022).
96. Victoria Houlden, SW, de Albuquerque, JP, Jarvis, S, and Rees, K. The relationship between greenspace and the mental wellbeing of adults: a systematic review. PLoS One. (2018) 13:e0203000. doi: 10.1371/journal.pone.0203000
97. Sus Sola Corazon, US, Poulsen, DV, Gramkow, MC, and Stigsdotter, UK. Psycho-physiological stress recovery in outdoor nature-based interventions: a systematic review of the past eight years of research. Int J Environ Res Public Health. (2019) 16:1711. doi: 10.3390/ijerph16101711
98. Isabelle Bray, RR, Sinnett, D, Martin, F, and Hayward, R. Exploring the role of exposure to green and blue spaces in preventing anxiety and depression among young people aged 14-24 years living in urban settings: a systematic review and conceptual framework. Environ Res. (2022) 214:114081. doi: 10.1016/j.envres.2022.114081
Keywords: anxiety disorder, outpatient expenditure, CCE, SHA2011, burden
Citation: Shi X, Zhao Y, Wan Q, Chai P and Ma Y (2024) Curative care expenditure of outpatient anxiety disorder in Liaoning Province, 2015-2020-based on “System of Health Accounts 2011”. Front. Public Health. 12:1329596. doi: 10.3389/fpubh.2024.1329596
Edited by:
Hai Fang, Peking University, ChinaReviewed by:
Liming Liu, Capital Medical University, ChinaMustafa Kursat Sahin, Ondokuz Mayıs University, Türkiye
Copyright © 2024 Shi, Zhao, Wan, Chai and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuedan Ma, bXlkcG9ueUAxNjMuY29t
 Xiaoxia Shi1
Xiaoxia Shi1