- 1Association for Socially Applicable Research (ASAR), Pune, Maharashtra, India
- 2Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY, United States
- 3GEMINI Research Center, Duke University School of Medicine, Durham, NC, United States
- 4Dr. D.Y. Patil Medical College, Hospital, and Research Centre, Pune, Maharashtra, India
- 5Global Alliance for Surgery, Obstetric, Trauma and Anaesthesia Care, Chicago, IL, United States
- 6Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India
- 7Department of Health and Human Sciences, Baylor University, Waco, TX, United States
- 8Department of Biology and Statistics, George Washington University, Washington, DC, United States
- 9India Hub, NIHR Health Research Unit On Global Surgery, Christian Medical College, Ludhiana, Punjab, India
- 10Indraprastha Apollo Hospital, New Delhi, India
- 11Department of Anesthesiology, Dalhousie University, Halifax, NS, Canada
- 12Apollo Hospital, Hyderguda, Hyderabad, Telangana, India
- 13Department of Surgery, Vardhman Mahavir Medical College Safdarjung Hospital, New Delhi, India
- 14Department of Surgery, NSCB Government Medical College, Jabalpur, India
- 15Karunya Rural Community Hospital Karunya Nagar, Coimbatore, Tamil Nadu, India
- 16Association of Rural Surgeons of India, Wardha, India
- 17International Federation of Rural Surgeons, Ujjain, India
- 18Rural Surgery Innovations Private Limited, Dimapur, Nagaland, India
- 19IRD Pakistan and the Global Surgery Foundation, Karachi, Sindh, Pakistan
- 20University of Central Florida College of Medicine, Orlando, FL, United States
- 21Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- 22Department of Surgery, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India
- 23WHO Collaborating Centre for Research in Surgical Care Delivery in LMIC, Mumbai, Maharashtra, India
- 24Department of Surgery, Aga Khan University, Karachi, Sindh, Pakistan
- 25Department of Pediatric Surgery, Mugda Medical College, Dhaka, Bangladesh
- 26American College of Surgeons: Bangladesh Chapter, Dhaka, Bangladesh
- 27Bangladesh Health Economist Forum, Dhaka, Bangladesh
- 28Association of Pediatric Surgeons of Bangladesh (APSB), DMCH, Dhaka, Bangladesh
- 29Narmada Fertility Centre, Hyderabad, Telangana, India
- 30International Trauma Anesthesia and Critical Care Society, Stavander, Stavanger, Norway
- 31Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India
- 32College of Anaesthesiologists and Intensivists of Sri Lanka, Rajagiriya, Sri Lanka
- 33Department of Anaesthesia, Perioperative Medicine and Critical Care, AIG Hospitals, Hyderabad, Telangana, India
- 34Department of Neurosurgery, Northwest School of Medicine, Peshawar, Khyber Pakhtunkhwa, Pakistan
- 35Army Medical Services, Military Hospital, Thimphu, Bhutan
- 36Jigme Dorji Wangchuck National Referral Hospital, Thimphu, Bhutan
- 37Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan
- 38LV Prasad Eye Institute, Hyderabad, Telangana, India
South Asia is a demographically crucial, economically aspiring, and socio-culturally diverse region in the world. The region contributes to a large burden of surgically-treatable disease conditions. A large number of people in South Asia cannot access safe and affordable surgical, obstetric, trauma, and anesthesia (SOTA) care when in need. Yet, attention to the region in Global Surgery and Global Health is limited. Here, we assess the status of SOTA care in South Asia. We summarize the evidence on SOTA care indicators and planning. Region-wide, as well as country-specific challenges are highlighted. We also discuss potential directions—initiatives and innovations—toward addressing these challenges. Local partnerships, sustained research and advocacy efforts, and politics can be aligned with evidence-based policymaking and health planning to achieve equitable SOTA care access in the South Asian region under the South Asian Association for Regional Cooperation (SAARC).
1 Background
Universal health coverage (UHC) is not possible without equitable access to surgical, obstetric, trauma, and anesthesia (SOTA) care for all. The year 2015 can be considered Annus Mirabilis for global SOTA care with the resolution on emergency and essential SOTA care from the World Health Organization (WHO) (1), evidence on disease burden, cost-beneficiality, and cost-effectiveness of essential SOTA care from the Disease Control Priorities Network (DCPN) (2), and evidence on lack of access to SOTA care and developmental gains from scale-up of services from the Lancet Commission on Global Surgery (LCoGS) (3). Since then there has been a global movement for underscoring SOTA care in international and national policy agendas. Assessing systemic and epidemiological indicators related to SOTA care for monitoring and evaluation purposes and introduction and implementation of national SOTA plans are two critical initiatives that multiple countries have invested in. Countries such as Brazil (4), Colombia (5, 6), Mexico and Peru in Latin America (7), Somaliland (8), Madagascar (9), and Uganda (10) in Africa, and Mongolia (11) in East Asia among others around the world have conducted comprehensive high-resolution subnational mapping of indicators for informing policies, while Rwanda, Tanzania, Nigeria, and Zambia among others have committed to national SOTA care plans (12). Despite the global movement, focus on SOTA care in South Asia—one of the world’s most densely populated, culturally diverse, and economically aspirational regions—remains limited.
Here, South Asia refers to the countries in the South Asian Association for Regional Cooperation (SAARC). SAARC includes eight countries: Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka. The South Asian countries together contribute to 24.1% of the global population (13), 4.2% of the global gross domestic product (GDP) (14), and 25.1% of the global disease burden (15). As of 2023, all other countries except Maldives (upper-middle-income) and Afghanistan (low-income) are lower-middle-income countries (LMICs). The eight countries have several differences across their demographic, socioeconomic, and health-related indicators (16, 17). There are also notable differences in the health systems of these countries (18). All South Asian countries have mixed models for health service delivery engaging public and private sectors at different healthcare levels. The financing is heterogeneous with large portions paid out-of-pocket by patients. However, countries have implemented public financing schemes with varying levels of success (19). Regardless of their differences, these countries share the general trend toward progress on health indicators in the last two decades, limited healthcare financing, and the pervasive issue of within-country inequalities in healthcare provision. Further, different crises have currently impacted healthcare and previous health gains in some South Asian countries (20–24).
This review aims to assess the state of SOTA care in South Asia and provide recommendations for universalizing care in the region. The article proceeds into five main sections that focus on discussing (1) the disease burden and economic burden of surgically avertable conditions, (2) literature on SOTA care indicators for the region and the individual countries, (3) SOTA care relevant policy-making and planning progress, (4) region-wide and country-specific challenges, and (5) potential solutions addressing the challenges.
2 Disease and economic burden of surgically avertable diseases
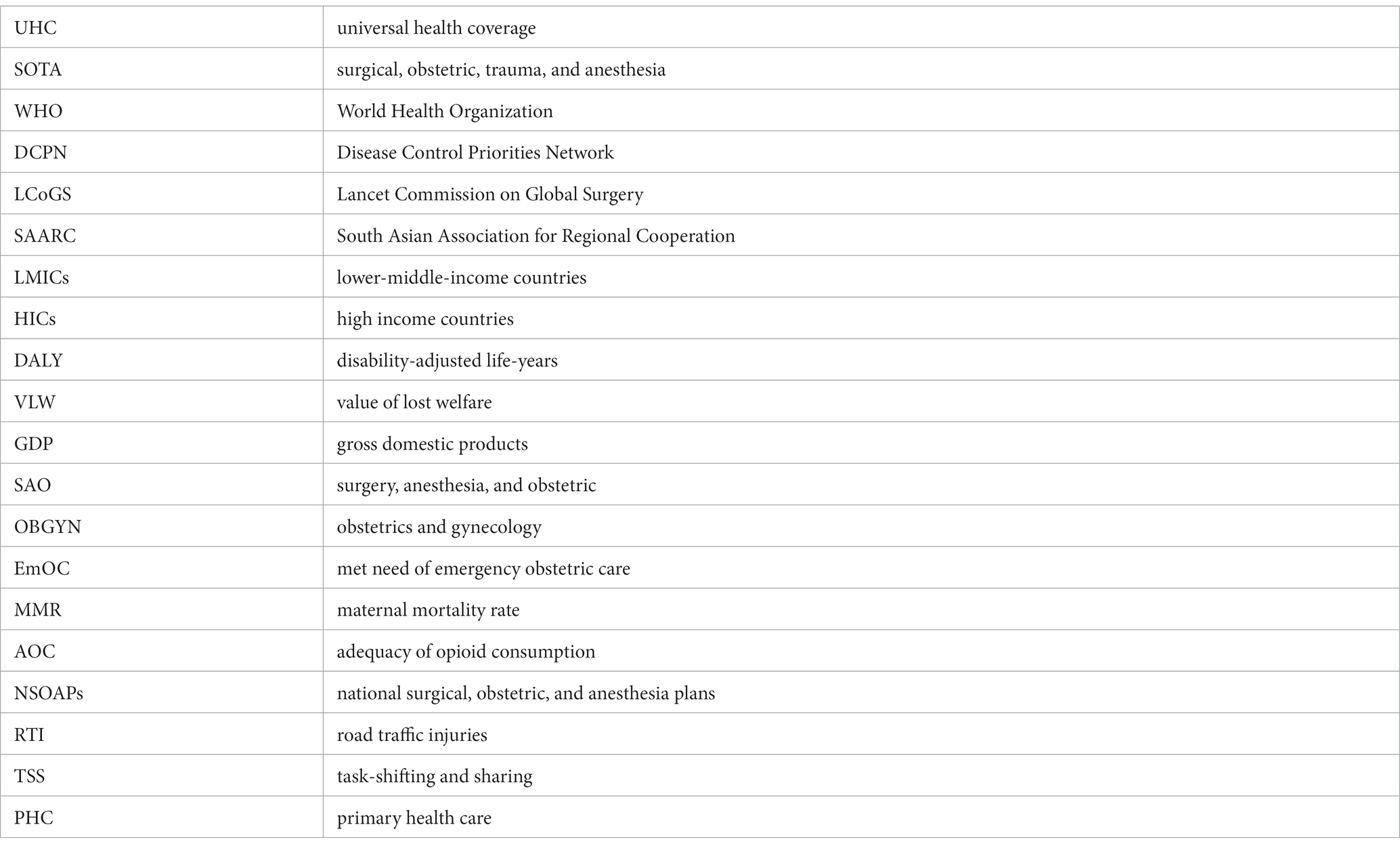
One of the most critical elements for achieving universal and equitable SOTA care is the monitoring and evaluation of relevant health systems and population health outcomes. An overarching population-level outcome is disease burden measured using disability-adjusted life-years (DALYs) that account for mortality and morbidity. In 2015, DCPN provided a comprehensive assessment of the mortality and morbidity burden due to surgically avertable conditions in low- and middle-income countries (LMICs) (25). Surgically avertable conditions were considered to be the ones that can be provided at first-level hospitals and can potentially improve health outcomes. These included multiple conditions such as obstructed labor, injuries, intra-abdominal emergencies, correctable congenital anomalies, such as clubfoot and cleft lip or palate, symptomatic hernias, cataracts, osteomyelitis, otitis media, etc. The DCPN and subsequent research from Higashi and colleagues noted that South Asian countries contribute to a significant proportion of the burden of surgically treatable diseases among LMICs (25–29). For instance, South Asia contributed 50.46, 32.49, 26.67, and 33.35% of the surgically avertable burden of neonatal and maternal diseases, congenital anomalies, digestive conditions, and injuries. Generally, South Asia had higher avertable disease burden rates, i.e., DALYs per 100,000 population than the overall LMIC rates (Figure 1).
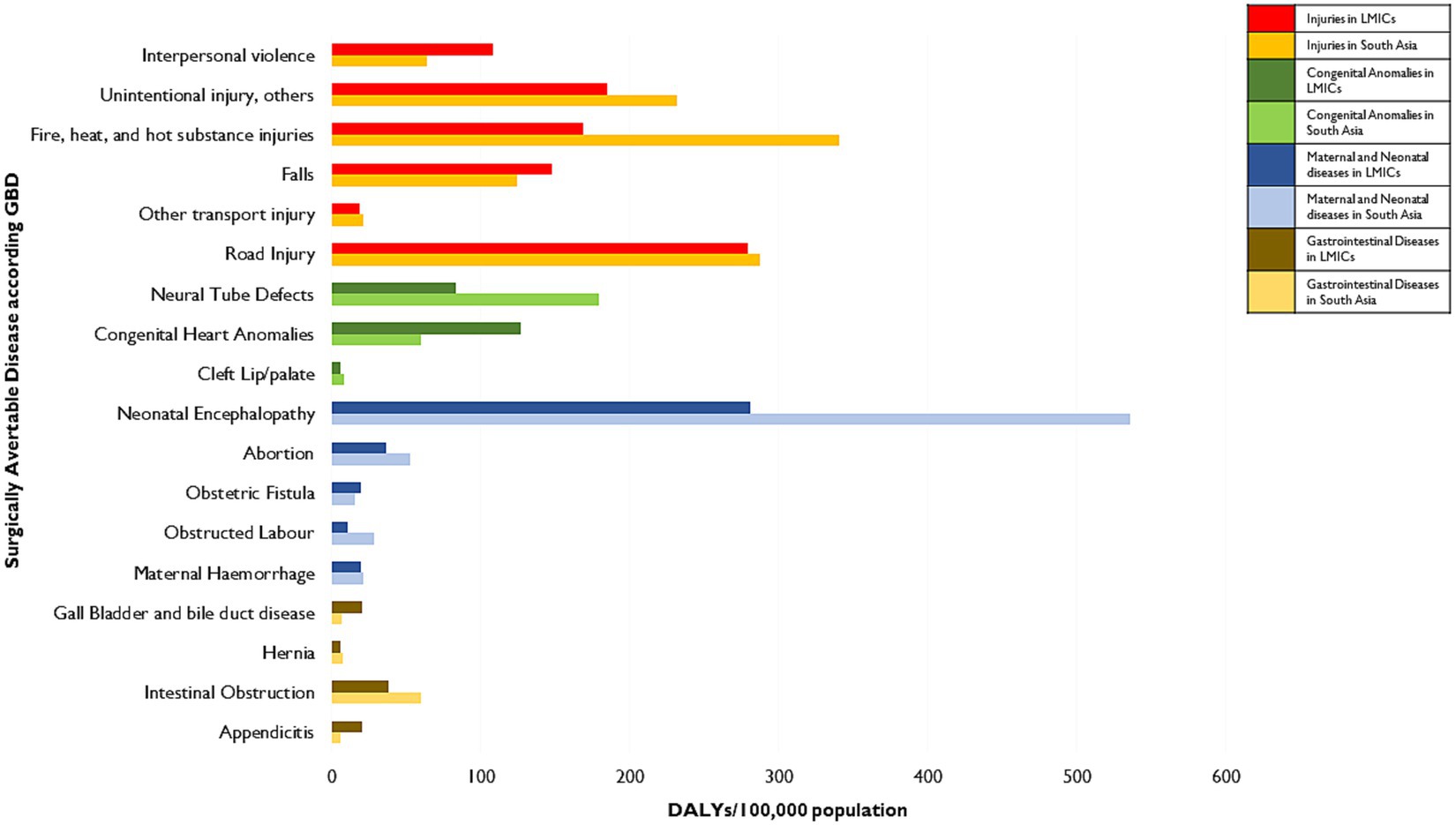
Figure 1. Burden of surgically-avertable diseases in South Asia compared to LMICs. Data has been obtained from studies conducted by Higashi et al. (26–29). Burden is measured in disability-adjusted life-years (DALYs). Unintentional injuries include exposure to mechanical forces, adverse effects of medical treatment, animal contact (venomous/nonvenomous), and unintentional injuries not classified elsewhere in the GBD 2010 Study. Poisoning, drowning, self-harm, and intentional injury, others (including exposure to forces of nature, collective violence, and legal intervention) are not included here.
The high avertable disease burden can be partially attributed to limited access to SOTA care. LCoGS defined access to emergency and essential SOTA care as a composite of timeliness, systemic capacity, safety, and affordability. The associated modeling exercise revealed that 5.3 billion people globally lack access to emergency and essential SOTA care (30). Of these, over 1.6 billion or 30.2% of the total people lacking access live in South Asia. This translates to over 98% of the South Asian population lacking access to safe and affordable SOTA care. However, it should be noted that these are modeled approximations that do not represent the differences in access across rural and urban areas, health sectors, population groups, etc. For instance, access in urban areas can be better than that in rural areas partly due to the presence of private SOTA care providers (31).
Furthermore, premature mortality and morbidity burden adversely impact the gross domestic product of an economy. This was captured using the value of lost welfare (VLW) in an LCoGS-associated study (32). The VLW approach relies on the value of statistical life-years that capture the long-term losses going beyond accounting for lost workforce productivity, forgone leisure, non-health consumption, etc. The study noted that in the single year—2010, the value of lost welfare for South Asia was about USD 986 billion (2010 PPP), forming 6.8% of the global losses. This value varied across countries from USD 808.49 billion (2010 PPP) for India to USD 0.25 billion (2010 PPP) for Maldives (Figure 2A). The losses also ranged from 21.33% for Afghanistan to 7.41% for the Maldives, expressed as proportions of countries’ gross domestic products (GDPs) (Figure 2B). These losses correspond to only select surgically avertable conditions and the magnitude of losses will only be greater for a more comprehensive enumeration of conditions.
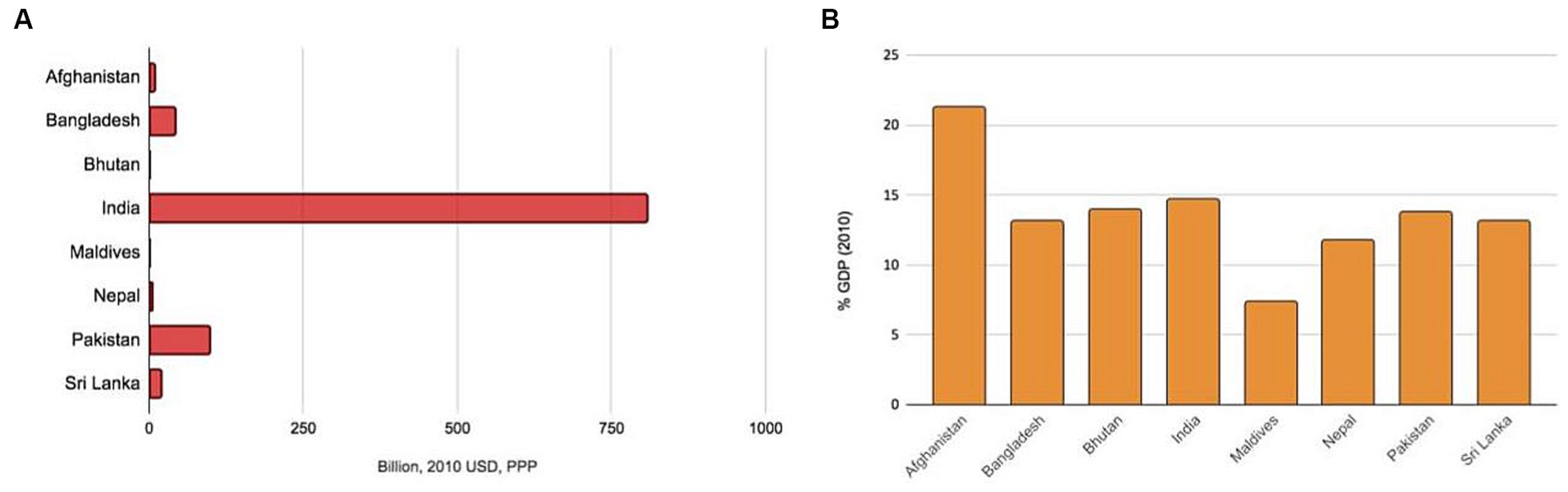
Figure 2. Value of lost economic welfare due to surgically-avertable disease burden in 2010 for South Asian countries as expressed in (A) absolute amount in billion 2010 USD PPP and (B) % GDP in 2010. Data has been obtained from a previous modeling study by Alkire and colleagues associated with the Lancet Commission on Global Surgery (32). USD, United States dollar; PPP, Purchasing Power Parity; GDP, Gross Domestic Product.
3 SOTA care indicators in South Asia
LCoGS suggested six indicators to track surgical care preparedness (timely access and workforce), delivery (volumes and perioperative mortality rates), and impact (catastrophic and impoverishing expenditures) (3). There have also been suggestions for contextualizing LCoGS indicators and adding others that are relevant for trauma and perioperative anesthesia care (33, 34). Collecting data on indicators is critical for monitoring and evaluation which, in turn, is important for evidence-based policymaking and planning. For South Asian countries, research on SOTA care indicators is limited. Data for some of the relevant indicators from international comparisons and those associated with LCoGS are compiled for South Asian countries in Table 1.
Table 1. SOTA care indicators for South Asian countries with target achievements marked by green cells.
There is limited national-level data on timely access to surgical care (51). The available data for Sri Lanka and Bangladesh suggests that they have crossed the LCoGS target of 80% population within 2 h of travel time from a facility providing bellwether procedures (52). For the SAO workforce, recent comparable data are not readily available but that collected and imputed during LCoGS suggests that all South Asian countries fall short of the target of 20 surgery, anesthesia, and obstetric (SAO) specialists per 100,000 population (36). Modeled estimates for population-level surgical volumes depict deficits in all countries compared to the target of 5,000 surgeries per 100,000 people per year (37). Further, models also suggest that at the current rate of scale-up, no country in South Asia would achieve the target rate before 2035 (53). While a systematic review provides a compilation of POMR studies in LMICs (54), data on South Asian countries are scattered. More importantly, there are no standard national perioperative mortality rate registries across the eight countries. Estimates for catastrophic and expenditures based on cesarean section rates depict that risk protection against catastrophic and impoverishing expenses due to seeking surgery when needed is limited and does not meet the aspirational target of 100% protection coverage set by LCoGS (Table 1) (38, 55). There have been some recent preliminary efforts for subnational data collection and/or estimation of LCoGS indicators for India (31, 56–59) and Pakistan (60, 61), but high-resolution subnational data remain largely missing for other countries.
Going beyond LCoGS, the GlobalSurg and COVIDSurg Collaboratives introduced and validated a hospital-level elective surgery assessment named surgical preparedness index (SPI) which is a composite of 23 variables capturing facilities and consumables, staffing, prioritization, and systems (39). Bangladesh, India, and Nepal had SPI scores above the global average of 84.5. Bhutan and Maldives did not have data. For obstetric indicators, we used cesarean section rates, obstetrics and gynecology (OBGYN) specialist density, met need of emergency obstetric care (EmOC), and maternal mortality rate (MMR). The WHO recommends that cesarean sections should form 10–15% of deliveries for a country to lower its MMR (48). Across South Asia, countries face the dual challenge of inadequate cesarean section rates in some places and excess cesarean section in others. For instance, only Bhutan has a rate that falls within the WHO recommended range. Afghanistan and Nepal fall below the threshold while other countries exceed the recommended cesarean section rates (41). Excess cesarean sections are a well-documented public health problem in South Asia (62). OBGYN density is poor in all South Asian countries (36). Except for the Maldives and Sri Lanka, all other countries also fall behind in achieving the target of reducing MMR to 70 per 100,000 live births by 2030 (49). Except for Sri Lanka, all the other countries have less than 50% of EmOC met need (40).
National data on the trauma care workforce and national registries on trauma surgical volumes and mortality are severely limited, though there have been recent studies conducted in parts of India and Sri Lanka (63–65). Adequate and safe supply of blood for transfusions is an important component of trauma care for which some data is available. LCoGS noted that 15 units per 1,000 persons per year is an adequate standard for a voluntary blood donation rate (3). A cross-country comparison of blood banking conducted by WHO reveals that among the South Asian countries, only Sri Lanka satisfies this threshold (44). On the positive side, except Maldives, all other South Asian countries have national standards in place for ensuring safe blood transfusions. For anesthesia care, anesthetist density is limited across all countries (36). Another important indicator is an adequate supply of analgesics for perioperative pain management which can be captured using the scaled index called adequacy of opioid consumption (AOC) (50). Estimation of the AOC index reveals that the values for all South Asian countries are below one compared to the target of 100 (43).
4 SOTA care planning in South Asia
The World Health Assembly Resolution 68.15, which noted the importance of emergency and essential SOTA care for UHC, was signed by all South Asian countries (1). However, greater policy attention and political will for specific investments directed toward SOTA care are needed. African countries such as Rwanda, Tanzania, Zambia, etc. have formulated National Surgical, Obstetric, and Anesthesia Plans (NSOAPs) that provide pathways toward improving surgical care by strengthening surgical systems in alignment with the countries’ national health policies and plans (12).
In South Asia, there has been some development concerning SOTA care planning. The Ministry of National Health Services, Regulation and Coordination in Pakistan has drafted a National Surgical Care Vision 2025 with the involvement of local and national partners including health service delivery organizations, individual practitioners (specialist surgeons, OBGYNs, anesthetists, and pediatric surgeons) and health planners and support from international organizations such as WHO (66). In terms of policy framing, it is in line with Pakistan’s National Health Vision 2016–2025. The National Surgical Care Vision 2025 accounts for the federal-provincial health system structure in Pakistan and has proposed the development of detailed Provincial Surgical, Obstetric, and Anesthesia Plans to cater to local needs and demands. With support from the United Nations Institute for Training and Research and several other global partners, the Ministry of Health and Population in Nepal has also initiated its NSOAP development process by conducting high-level stakeholder orientation meetings (67).
In the case of India, after LCoGS, the National Surgical Forum was conducted in 2016 where important stakeholders discussed priorities and potential implementation opportunities for improving SOTA care in India (68). The Karad Consensus Statement drafted by the Association of Rural Surgeons of India was signed by multiple partners (69). Additionally, under the implementing-LCoGS-India initiative centers for excellence were started (70). All these efforts have identified the poor and unsafe blood supply infrastructure in the country, low rural SOTA workforce availability marred by limited training and unsustained partnerships, as well as lack of needs assessment, relevant targets, and surgical innovations scaleup for rural India as significant gaps. Importantly, India has a National Programme for Prevention & Management of Trauma & Burn Injuries aimed at capacity building (infrastructure, human resources, equipment, etc.) in public hospitals for quality trauma care provision (71). However, the scheme was valid only till March 2020. A dedicated SOTA care plan is still lacking for India and its states (72). Further, there is also some evidence that SOTA care has had limited prioritization in national policies and programs across the last seven decades (73). Of note, it is also crucial that decision-making in health-related matters is driven by evidence and not just political priority.
Sri Lanka has a “National Policy and Strategic Framework on Injury Prevention and Management” that includes pre-hospital and emergency trauma care under secondary prevention and more recently a “Multi-sectoral Strategic Action Plan on Injury Prevention and Management 2021–2025” that envisions developing clinical management guidelines for trauma care at all levels of care, establishing a trauma cluster care system, ensuring adequate capacity and training of staff for trauma patients, and collecting appropriate data for assessment (74, 75). To our knowledge, there has not been any development toward national SOTA care planning in other South Asian countries. Urgent attention, committed investments, and sustained efforts are necessary for equitable and universal SOTA care. This can be achieved through local collaborations within the region and shared learning under SAARC.
5 Current challenges
5.1 Suboptimal distribution, utilization, and quality of services
Suboptimal distribution and utilization of services especially at the primary and secondary levels of care enhance access disparities. On the supply side, resource allocation, including staffing, based on one-size-fits-all standards leads to wastage of resources at some SOTA care facilities while shortage at others. On the utilization side, secondary-level care facilities remain under-utilized while tertiary hospitals are over-burdened by patients who bypass the referral system in search of assurance for better SOTA care. While the limited geographical access to SOTA care facilities might be high in some South Asian countries as noted before (see Table 1), quality of care needs improvement on several fronts. The lapses in quality can be attributed to inadequate human resources and limited financing for the development and maintenance of SOTA care facilities (3, 76).
5.2 Inequitable obstetric care—cesarean section disparities
Access to safe and affordable obstetric care, including cesarean sections, is highly inequitable. While the national aggregate numbers show excess cesarean section rates compared to the WHO threshold for multiple South Asian countries, it is noteworthy that several factors lead to large within-country differences in cesarean section rates (77–79). Cesarean sections are frequent in urban private facilities among older, educated, and financially independent women (77). However, access to cesarean sections in rural regions is limited. For instance, using the rate values (as % institutional deliveries), when we calculate rural-to-urban ratios for cesarean sections, they come out to be 0.87, 0.54, 0.82, and 0.53 for Bangladesh, India, Maldives, and Nepal, respectively (78). Cesarean section rates are also known to be different across public and private health sectors. When we calculate private-to-public ratios using the values for the cesarean section rates (as % institutional deliveries) for Bangladesh, India, and rural Nepal, we get 2.52, 1.00, and 2.14, respectively (80). Seeking healthcare in private healthcare facilities is often beyond the reach of women from the lower socioeconomic strata, which in turn points to disparities in access to cesarean sections. More broadly, for a large section of women in South Asia safe, affordable, and rights-based obstetric care remains beyond reach (81, 82).
5.3 Limited SOTA care in rural areas
SOTA care delivery in rural and remote areas is a challenge faced throughout the region. Lack of infrastructure and limited workforce availability are major impediments to service delivery (31, 69, 83–85). Infrastructural challenges can be wide-ranging from poor road conditions limiting access to the hospitals, frequent power outages, limited maintenance of operating rooms, inadequate surgical equipment, insufficient and irregular supply of blood products and drugs, lack of lodging facilities for patients and their caregivers during the perioperative period, etc. Innovations by rural SOTA care experts can mitigate several issues. For instance, the last decade has seen massive progress in the development of minimally invasive surgical equipment, including gasless laparoscopic systems tailored specifically to the needs and contingencies of rural South Asia (86–88). Similarly, innovative alternatives for surgical techniques have been tested that can ensure safe SOTA care delivery at reduced costs to rural patients (89–91). However, a consistent investment in SOTA care innovations is missing and additional pathways for scale-up and integration of such innovations are required.
While the South Asian region has low SAO workforce densities (see Table 1), however, these numbers drop further for rural areas. Among the workforce personnel, there are fewer anesthetists than surgeons, even at district-level hospitals, which limits the delivery of emergency and essential surgeries (85). Further, those working in rural and remote might require additional training and competency building to adequately deal with uncertain and challenging conditions (e.g., frequent power outages, working without appropriate equipment, etc.). However, specialty programs providing such training are limited (92–94). Additionally, rural and remote areas are severely underrepresented in research which necessitates data collection that can be used to assess the efficacy and safety of interventions and innovations being undertaken at rural hospitals.
5.4 Workforce migration
Multiple South Asian countries suffer from the “brain drain” due to the emigration of SAO specialists, which leads to the weakening of the SOTA care systems (95). The proportion of surgical specialists trained in South Asia who practice abroad ranges from 3.9% for Nepal to 61.1% for Sri Lanka (96). There are multiple reasons for emigration with opportunities for better quality training, prospects for employment, and improvement in socioeconomic status being some of the main ones (97). These emigration rates are comparable to those among general physicians and other specialists. Hence, data on physician emigration can be a useful proxy. In the United Kingdom alone, physicians trained in India, Pakistan, and Sri Lanka contribute to 24.5% of the total physicians (98). Overall, the physician brain drain costs South Asian countries about 5.2 billion USD annually (99).
Beyond specialists and physicians, the brain drain is also prevalent among nurses who play a critical role in delivering SOTA care services. For instance, the countries accounting for the largest shortages (in absolute terms) in 2018 included Bangladesh, India, and Pakistan. From April to September 2021, more than 10,000 new international nurses were registered in the UK, of these over 4,500 were from India (100).
5.5 Burden of road traffic injuries and limited trauma care
Rapid growth in the past years, high urban population density, and limited planning in countries such as India and Sri Lanka have presented them with a growing burden of road traffic injuries (RTI) (17, 101). India and Sri Lanka together contribute to 36% of global RTI incidence and 18% of mortality (102). Further, the RTI burden is also associated with a greater financial burden captured by higher out-of-pocket spending and catastrophic health expenses in households with RTIs compared to those without an RTI event (103). This points to a clear need to invest in upscaling trauma care systems including the blood transfusion capabilities. Delays in access due to communication gaps in prehospital care, limited training for basic clinical care within hospitals, and lack of trauma data systems as well as necessary administrative support are major systemic barriers to trauma care for RTI patients in India (104). Recently, there have been more efforts to set up hospital-based trauma registries in India and Sri Lanka (63–65). However, ensuring continued functioning and high quality of such registries is a challenge due to limited policy attention to SOTA care and funding constraints.
India has seen progress in the last few decades for emergency and trauma care with public-private service delivery models such as “108 emergency ambulances” operated by the EMRI Green Health Services formerly known as the GVK EMRI (105) and neurotrauma management including the comprehensive guidelines from the Neurotrauma Society of India for integrated prehospital, hospital, and rehabilitative care of traumatic brain injury (106). Similarly, Sri Lanka has witnessed calls for establishing a National Trauma System that can optimize patient referrals and reduce injury-related mortality (107). India and Sri Lanka have policies and programs directed toward trauma care but a comprehensive assessment of their implementation remains to be seen.
5.6 Poor access to anesthesia and pain management
India and Sri Lanka also share some challenges related to anesthesia care. First, most anesthetists work as consultants working between the public and private healthcare sectors (108, 109). This means that their availability at a given health facility cannot be assured which impacts public SOTA care systems (85). Second, there is limited access to perioperative pain management (see AOC values in Table 1). The limited number of anesthesiologists who can prescribe such medication, high costs for patients, and the complex regulatory framework that intends to avoid opioid misuse but simultaneously limit access to prescription pain medication, are some of the factors that make pain management challenging. The economic crisis in Sri Lanka is further expected to exacerbate these challenges. Over 65% of the anesthetists trained in Sri Lanka typically emigrate to HICs (110). This emigration can rise further as consultant anesthetists try to look for stable work opportunities and better professional lives. Access to pain medications can go down due to supply chain disruptions (111). Both these threats can reduce the quality of care in the country despite organized efforts of Sri Lankan anesthetists to make ends meet in a strained health system (112). Most importantly, such challenges, while prevalent, are not given the deserved attention in the broader global SOTA care discourse.
5.7 Neglect toward pediatric care
South Asian countries constitute some of the largest pediatric (under 18) populations globally with a high burden of amenable pediatric mortality (113), yet pediatric SOTA care capacity is limited (114, 115). The critical threshold for needed pediatric surgical workforce density per 100,000 children under the age of 15 years is found to be 0.37 (116). While Maldives has a density above this threshold, Bangladesh, India, and Pakistan do not (116, 117). Data on other South Asian countries is limited. A shortage of pediatric SOTA care workforce is associated with greater neonatal, infant, and under-5 child mortality (115). Moreover, data from India depicts that pediatric surgery contributes to only 0.7% of the total subspecialty training spots (118). This depicts a lack of training capacity that can contribute to the continuation of workforce shortages in the future. Similarly, data from Pakistan depicts an unmet need for pediatric surgery due to a lack of trained workforce due to limited capacity and low quality of training (119, 120). Nepal noted limited services, lack of money and time, and lack of acceptability toward surgical care providers as reasons for unmet pediatric surgery needs (121).
5.8 Limited attention to allied professionals in SOTA care
The role of nurses and midwives in improving access to quality services, especially among the hard-to-reach populations, often goes unappreciated in global SOTA care discourse. South Asia faces a large burden of maternal mortality due to hemorrhage, eclampsia, obstructed labor, sepsis, and unsafe abortions among other reasons that can be prevented through timely access to cost-effective interventions (122). Scaling up well-trained nurses and midwives to ensure complete skilled birth attendance coverage is important. In rural and remote areas lacking access to trained specialists and physicians and equipment and technologies, experienced nurses and midwives handle complications during deliveries. While South Asian countries have observed progress toward achieving international nursing and midwifery standards, there is a long road ahead (123).
5.9 Impact of COVID on SOTA care
Similar to other parts of the world, SOTA care in South Asia suffered from disruptions due to the COVID-19 pandemic. The disease spread and the movement restrictions aimed to curb it, stalled service delivery and adversely impacted training. For instance, early on in the pandemic, volumes of emergency surgery were reduced to lockdowns, elective surgeries, and outpatient appointments were canceled followed by delays (124). At the Phuentsholing General Hospital in Bhutan, cesarean section deliveries dropped by 6.6% and gynecological surgeries dropped to 13.9% of the total gynecological services from 20.6% during the pandemic years (2020–21) compared to 2019 (125). Across cancer, cardiovascular, respiratory, and other conditions, surgical treatments during COVID-19 (2020–21) were reduced by 4 to 97% across different studies for India compared to 2019 and previous years (126). In Nepal, all neurosurgery centers postponed elective surgeries and shut down outpatient care early on in the pandemic (127). Major reductions in training hours and capacity were recorded for obstetrics and gynecology residency training programs in India and general surgical residency in Pakistan among others (128, 129). These point to the need for including SOTA care in public health emergency response. Further, there is also a need to expand the notion of emergencies beyond epidemics or pandemics to include mass casualties and climate emergencies (130, 131).
5.10 Lack of need-based policy-making
Policymaking related to SOTA care needs to be determined based on patient needs. For instance, pain management significantly burdens surgical patients. About 20–25% of the global population experiences chronic pain but management in South Asia is faced with barriers due to cultural beliefs, physician education, infrequent use of standardized pain management tools, and healthcare infrastructure (132). The rest of the above-mentioned challenges also call for tailored advocacy. Hence, any policy and planning efforts should include this and other such issues based on the lived experiences of the patients and suggestions of the providers.
5.11 Some country-specific challenges
Given the diversity in the region, beyond those noted above, some challenges are more pronounced in some places than others. For instance, political instability and the COVID-19 pandemic have contributed to the extant challenge of high maternal mortality in Afghanistan. This can be, in part, attributed to the limited availability of obstetric surgeons, nurses, and other healthcare workers (133). Bhutan has been hiring surgeons and anesthetists from other countries. Currently, training programs for physicians and surgical specialists are limited (134), which forces the country to recruit and fund medical students in other countries who are willing to commit to serving in Bhutan post-training. In Nepal, accessibility, affordability, and acceptability (lack of trust in providers or fear of healthcare seeking) are major barriers to SOTA care (135, 136). National projections suggest that 2.4 million residents in Nepal may not get care when they need it (137). Further, differences in capacity and quality of care, as well as training of surgical specialists, play an important role in within-country variations in SOTA care provision (138).
6 Potential directions
Achieving equitable SOTA care in South Asia is dependent on local partnerships that enable the free exchange of knowledge, resource mobilization, and priority-setting. Achieving equitable SOTA care requires collaborative and sustainable efforts in various directions. Though not exhaustive, we list some important directions here.
6.1 Enhancing SOTA care research efforts
Research efforts for data on SOTA care indicators are needed for all countries. Such a research program should ensure the following:
(a) Identification of disparities. Emphasis should be on high-resolution subnational estimates instead of aggregate national numbers. Further, disaggregated data for rural and urban regions, and types of healthcare sectors (public, nonprofit/trust/faith-based, and for-profit private) are essential for the equitable distribution of resources.
(b) Focus on under-resourced settings. It is crucial to orient research efforts and resources toward rural and remote areas as well as underserved populations to quantify the needs and test effective interventions.
(c) Ownership by and opportunities for local research investigators. The research has to be locally owned and governed and not too reliant on limited-term external funding.
(d) Ensuring equity within the investigators in terms of gender, institutional portfolio, regions, etc. is further important to ensure the decentralization of research efforts.
(e) Priority setting by local interested/affected parties. While the work can be facilitated through international collaborations including high-income country academic institutions and funders, the research agenda should be set by those working for and affected by SOTA care issues including caregivers, patients, advocates, and policymakers. Diversity in decision-making over priorities might be challenging to manage but it can help better align limited resources toward feasible and actionable goals.
(f) Setting contextually relevant targets. While LCoGS, WHO, and other international and intergovernmental efforts have provided targets for various SOTA care indicators, it is critical to rethink and revise them according to the regional/local context. Participatory research for deciding contextually relevant targets should consider the trade-off between aspirational and implementable targets.
(g) Evidence for targeted interventions. The research needs to go beyond the measurement of problems and should be oriented toward potential solutions. Testing of efficacy and safety, effectiveness, cost-effectiveness, and implementation feasibility of different interventions is central. Further, evidence synthesis for new interventions and tailoring existing interventions for specific populations, geographies, etc. is critical for success given the within and between-country diversity in South Asia.
(h) Leveraging existing data systems. Research should focus on auditing, collating, and utilizing extant data sources and systems for SOTA care indicators before initiating primary data collection given that the latter is resource-intensive (72). Resources can thus be optimally allocated to epidemiological and interventional research.
(i) Working toward absorptive capacity for integration of SOTA care indicators. Rather than introducing new systems for parallel data collection dedicated to SOTA care, these indicators should be integrated into current health management and information systems and demographic surveys for sustained monitoring and evaluation (139).
6.2 Training and retaining high-quality SOTA care workforce
High-quality training of surgeons, obstetricians, anesthetists, nurses, and allied professionals as well as timely scale-up of the SOTA care workforce needs to consider the following:
(a) Investing in increasing residency and fellowship level training spots for the next generation of SAO specialists is the key. The scale-up should happen at an adequate rate/level in a target-oriented manner. For instance, to achieve the target density of 20 SAO specialists per 100,000 population by 2030, Bangladesh, India, and Pakistan would need 40,288, 291,824, and 47,710 more SAO specialists compared to 2015 (140). Additionally, the training spots should be equitably distributed (141).
(b) Retaining existing SAO specialists and ensuring their distribution across different parts of the country should be prioritized. However, there has to be a major policy change in the context of curbing the “brain drain.” Punitive policies need to be replaced with those that focus on strengthening health systems to ensure better working environments and behavioral modifications as well as incentives for SAO specialists to serve in their countries of origin (85, 142). Opportunities for professional growth and better environment and security for families of SAO specialists can help in retention. It is also important to integrate and retain the nursing and midwifery workforce into SOTA care as they contribute to health system strengthening.
(c) Changes in training to ensure high-quality service delivery and good patient outcomes are necessary. Rural surgery residency, fellowship, and short-term programs that cut across subspecialties to equip trainees with skills to operate under resource constraints should be expanded. For instance, promoted by the Association of Rural Surgeons of India, the National Board Examination offers a 3-year DNB in Rural Surgery (postgraduate diploma program) (143). The COVID-19 pandemic brought out some innovative and resilient methods of training that need to be integrated into the system. For instance, telementoring, hybrid models of learning, and a greater focus on the well-being of trainees as observed in Pakistan could be tested in other countries for potential scale-up (129, 144).
(d) Participating in shared training opportunities including exchange programs and rotations is critical for South Asian countries to ensure good quality SAO workforce. Effective implementation of such multi-country or exchange programs would require competency-based training, standardization of curricula, independent quality assessments, and uniform accreditation standards. Such efforts can particularly benefit countries with limited programs including Bhutan and Nepal. In the long run, they can promote pathways for multi-country clinical licenses and intra-regional SAO specialist need-based movement to improve equitable distribution.
(e) Providing opportunities for research and advocacy skills learning for those who are inclined toward these is also necessary as these skills are different yet can be equally important as clinical training for revolutionizing SOTA care access. While integrating cursory introduction to these in routine training is important, such opportunities should be more trainee-led. For instance, trainee-led collaborations (e.g., PakSurg) and peer-led student research interest groups or networks that are aligned with the country’s research needs have seen some initial success in Pakistan (145, 146). There have been proposals for advocacy fellowships that would train residents in policy-brief and op-ed writing, public speaking, traditional and social media advocacy, activism, story-telling, etc. (147)
(f) Training of allied (non-specialist) professionals who are currently or can be potentially involved in delivering SOTA care services should be urgently considered. There is accumulating evidence on the need and practice of task- shifting and sharing (TSS) in global SOTA care (148). Training of allied professionals for specific surgical or anesthesia management skills has been gaining momentum in some South Asian countries with trials in Afghanistan, Bhutan, India, and Nepal (149). TSS initiatives can be classified into those where some tasks performed by specialists are shifted to/shared by adequately trained non-specialist physicians and those where the tasks performed by specialist or non-specialist physicians are shifted to/shared by other health professionals including nurses, midwives, technicians, etc.
It is important to note that beyond evidence on effectiveness, for successful introduction and implementation of TSS initiatives at programmatic scales, understanding acceptability from involved parties (e.g., SAO specialists) is crucial. There has been greater acceptance of task-sharing than task-shifting (150). Additionally, the specialist to non-specialist TSS has faced less resistance from SAO specialists (149). Hence, interventions establishing the effectiveness of TSS should be accompanied by interventions that improve their acceptability among the existing SAO workforce. Regulatory barriers also need to be navigated for successful implementation as several South Asian countries currently allow only SAO specialists to independently perform several procedures. Perhaps, for South Asia, there needs to be some rethinking around the traditional approaches used in TSS. Ultimately, the broader idea of team building and optimization needs to be focused on in this discourse.
6.3 Harnessing technical innovations in SOTA care
South Asian countries can leverage technical innovations—equipment, technologies, and procedures—to mitigate the challenges associated with resource constraints and access disparities. Over the last three decades, there have been several instances of low-cost surgical equipment designed with a human-centered approach and safe alternative procedures/techniques born out of the need that have enhanced access to SOTA care in rural and remote areas. For instance, gasless laparoscopy as a part of the broader suite of minimally invasive surgery has improved access to care, reduced costs, and ensured patient safety for basic procedures such as cholecystectomy, appendectomy, etc. (86, 151). Growing uptake of telemedicine and digital health in South Asia also has a role in improving SOTA care access. Telemedicine including phone calls, video chat, and WhatsApp-like services is increasingly used for perioperative patient consultations, postoperative follow-up, and provider-to-provider communications. Digital tools are also being used for learning at a distance, improving access to education and training (152). Systemic propagation of such innovations needs: (a) dedicated funding mechanisms for early-on development, (b) fast-tracked pathways for testing and establishing efficacy and safety, (c) well-structured regulatory environments for mainstream integration, and (d) implementation grants specifically targeted toward their uptake in low-resource settings that can benefit the most. It is critical to note that for achieving health equity, cost-effective technical innovations (e.g., gasless laparoscopy) that can potentially cater to common problems of large populations needing emergency and essential SOTA care and must be prioritized over costly innovations (e.g., robot-assisted surgeries) (153) that can be housed only in urban multispecialty tertiary centers that can be accessed by a select few.
6.4 Promoting healthcare tourism across South Asia
Promoting healthcare tourism in the context of SOTA care across South Asian countries can benefit patients while building regional cooperation and solidarity in the long run. Healthcare tourism is popular in the region with India as a major hub for receiving patients from other South Asian countries. For instance, 53.3% of medical tourists coming to India are from South Asian countries while these countries contribute to only 17.2% of general tourists, depicting a clear priority for health seeking (154). A large chunk of healthcare tourists visit private sector hospitals in India for SOTA care treatments related to orthopedic and trauma surgery, surgical eye care, plastic surgeries, cancer care, etc. (155). While variations exist across sender South Asian countries the overall trend in healthcare tourism has been increasing over years thereby establishing the need for expanding the capacity to serve such patients. Regional tourism makes SOTA care accessible but seeking care in the private sector can put a financial burden on patients, especially those arriving from lower socioeconomic strata of low-income countries. Additionally, logistic and legal hurdles involved in migration can deter those in need of care.
There are multiple ways to improve SOTA care access for South Asian healthcare tourists: (a) Ensuring that SOTA care tourism is not limited to those who can afford it but includes everyone in need is most important. The SAARC member nations can initiate a shared financing mechanism for supporting SOTA care tourists across countries. Such financing can learn from and add to the current efforts toward universal healthcare coverage in South Asian countries. For instance, India recently expanded its government-funded healthcare insurance to cover the bottom 40% of the country’s population under the Pradhan Mantri Jan Arogya Yojana (PMJAY). While ambitious in its vision and implementation, there have been notable limitations in the equitable uptake of the scheme that need to be rectified for target coverage achievement (156). (b) Accreditation of SOTA care facilities and standardization can ensure high-quality service delivery (157). (c) Resources for healthcare tourism should be based on demand patterns that depict investments in building SOTA care capacity. (d) Continuing to cut down red tape and easing up visa processes for healthcare tourists can further improve access (158).
6.5 Scaling up model (exemplary) SOTA care systems
Learning from and adapting exemplary or model SOTA care delivery systems and initiatives for scale-up can have large gains with some assurance about implementation feasibility. In 2015, LCoGS initiated cataloging such models including Jan Swasthya Sahyog in India and Indus Hospital in Pakistan among others (159, 160). Cataloging more such models operational across South Asia is essential. Beyond compiling high-level evidence, the catalog can act as an important resource to demonstrate to decision-makers reliability and local stewardship regarding universal and equitable SOTA care. Examples of models include a collaborative trauma care initiative for managing road traffic injuries in Nepal (138), quality improvement model solving infrastructural challenges in the maternity ward of the national referral hospital in Bhutan (161), and a sustainable and efficient model for low-cost cataract surgery in India among others (162). The catalog can be further expanded to models beyond South Asia to include countries and settings that can promote Global South–South learning.
6.6 Boosting advocacy efforts
Globally, effective advocacy has played a major role in reducing the neglect of SOTA care and ensuring its inclusion in intergovernmental resolutions and policy agenda. However, only local advocacy efforts can make a true difference. Advocacy for attending to and investing in SOTA care is based on multiple complementary arguments. Ensuring SOTA care for all is embedded in countries’ commitment to human rights (163). Hence, by working on SOTA care access, policymakers and political leaders can affirm their commitment to the rights of their citizens. Expanding SOTA care has a major role in countries achieving universal health coverage (164). Further, SOTA care access is also tied to multiple SDGs beyond health (165). Essential and emergency SOTA care interventions are as cost-effective as immunization and other common healthcare interventions (166). Not investing in SOTA care will lead to health losses for South Asian countries’ populations (see avertable burden in Figure 1) (25–29) and financial losses for the aspiring economies (see welfare losses in Figure 2) (32).
SOTA care advocates have opportunities to learn from the advocacy movements for universal health coverage (UHC) and primary health care (PHC). For instance, understanding the political prerequisites and governance nuances has been critical for UHC advocacy (167). While aligning with demographic transitions, integrating technological innovations, formulating regional strategies, focusing on inequalities, exploring alternative financing models, involving community-level workers, etc. have been important for the prioritization of the PHC movement in Southeast Asia (168).
For success, advocates for SOTA care in South Asia should be aware of and act on the following:
(a) Speaking the language of policymakers. Health policymaking is complex with no set model and can differ across countries and contexts. Advocates must align SOTA care with the priorities of policymakers and present evidence in ways that are acceptable or appreciable to those involved in the decision-making process. For example, this involves assimilating academic studies into simpler policy briefs.
(b) Understanding local power sharing. Stakeholder mapping is a crucial tool for understanding the roles held by different players and how they influence each other in a formal or informal capacity. Further, in several South Asian countries, relying on personal and informal connections beyond formal professional collaborations can help further the cause. Hence, local SOTA care advocates from grassroots service delivery organizations, tertiary care centers, academic institutes, think tanks, etc. who have established connections have a major role to play.
(c) Advocates should focus on specific asks supported by evidence and consensus. In the case of South Asia, these can include monitoring and evaluation of SOTA care indicators, integration of these indicators in national targets and policies, advocating at the intergovernmental level for integration of SOTA care among international targets, development and implementation of national and/or subnational SOTA plans, inclusion of SOTA care issues horizontally across other health, environment, economic welfare, and social development policies and programs, and sustained financing for SOTA care scale-up.
(d) The SOTA care advocacy community should be more inclusive and expand beyond SAO specialists. Successful advocacy is dependent on involving various interested and affected parties such as non-specialist SOTA care professionals (nurses, midwives, etc.), non-SOTA health workers (community health workers, pharmacists, etc.), researchers, health-technology entrepreneurs, journalists, funders, and most importantly patients. These parties bring diverse views and skills and can increase the size of the audience and enhance engagement. Bringing out patient voices that share lived experiences about lack of timely geographical access, facing low-quality care, and suffering from financial distress can add to the appeal for political leadership beyond the evidence.
6.7 Involving SAARC Secretariat
Bringing SOTA care to the SAARC Secretariat’s initiatives is critical. Previously, SAARC had recognized bodies relevant to SOTA care including the SAARC Surgical Care Society headquartered in Colombo, Sri Lanka, which had a valid recognition till 2017, the Federation of Association of Pediatric Surgeons of SAARC Countries headquartered in Chittagong, Bangladesh, valid till 2019, and SAARC Academy of Ophthalmology headquartered in New Delhi, India, valid till 2017 (169).
The Secretariat should establish and sustain a dedicated SAARC Center for SOTA Care to lead future initiatives and collaborations in all domains of SOTA care. This can be done in multiple ways that have positive implications for SAARC Areas of Cooperation as detailed in Table 2. The Center can learn from the successful functioning and follow the governance structure of the SAARC TB and HIV/AIDS Centre (171). Ultimately, SAARC countries must demonstrate explicit commitment to SOTA care by including it under “Health” in any future SAARC Summit Declarations.
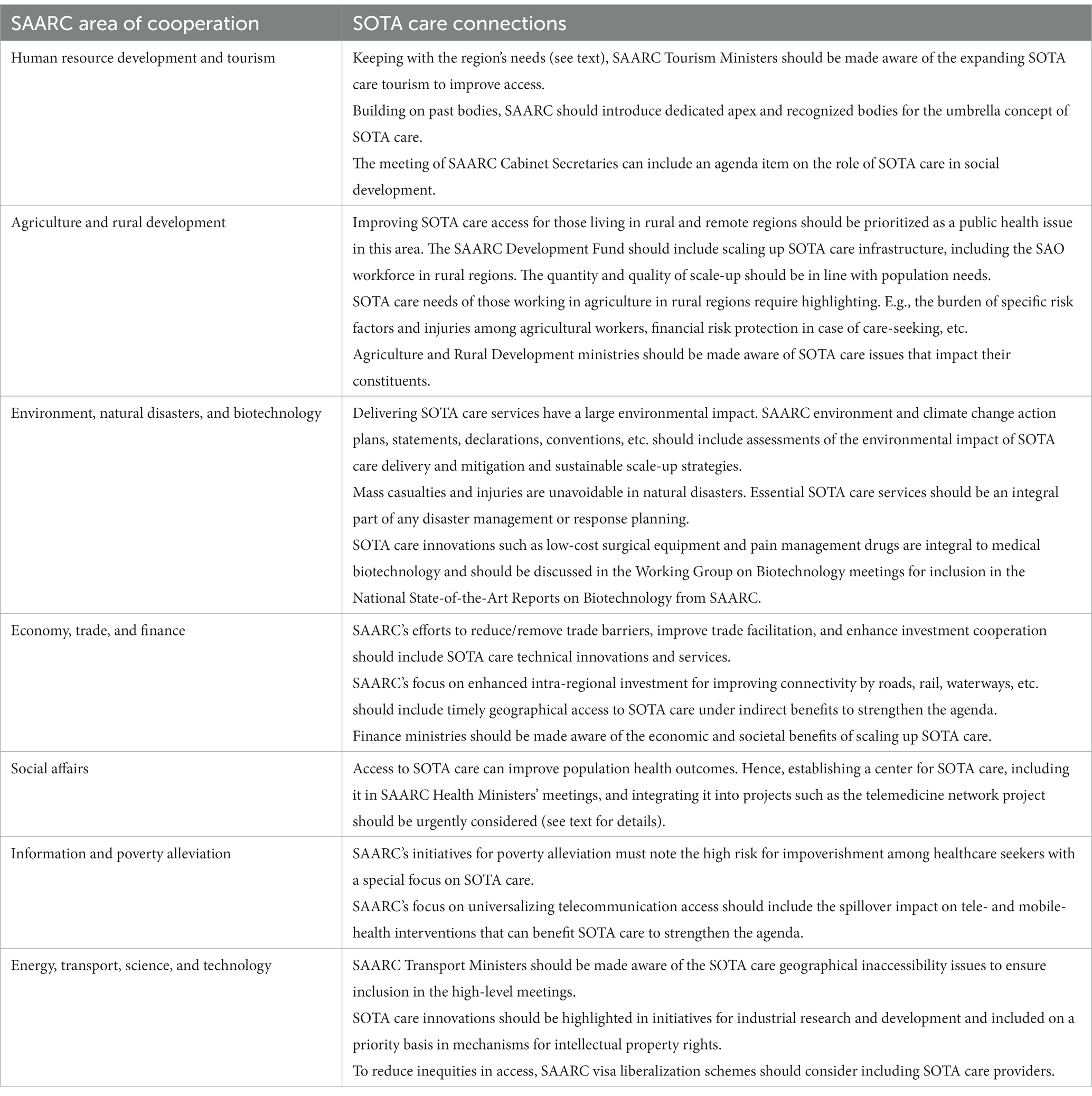
Table 2. Implications of SOTA care access across multiple SAARC areas of cooperation (170).
7 Conclusion
South Asia’s path toward universal health coverage necessitates prioritization of and investments in SOTA care. Currently, South Asian countries face several shared and country-specific challenges with limited subnational data on SOTA care indicators and the need for national planning. Case studies of exemplary SOTA care delivery systems, research initiatives, and policy processes are vital for shared learning of countries to be able to tailor the approach toward SOTA care planning. Sustainable and strategic local partnerships under SAARC are of key importance. Evidence-based policymaking, political will, and patients’ participation would ensure SOTA care for all in the region.
Author contributions
SZ: Conceptualization, Formal analysis, Project administration, Supervision, Resources, Writing – original draft, Writing – review & editing. SR: Methodology, Formal Analysis, Data Curation, Visualization, Validation, Writing – original draft, Writing – review & editing. IG: Data curation, Formal analysis, Methodology, Project administration, Validation, Writing - original draft, Writing – review & editing. NS: Writing – review & editing. CP: Writing – review & editing. AN: Writing – review & editing. HI: Writing – review & editing. AK: Writing – review & editing. AP: Writing – review & editing. GAF: Writing – review & editing. CRKP: Writing – review & editing. C: Writing – review & editing. DS: Writing – review & editing. DG: Writing – review & editing. GJ: Writing – review & editing. IF: Writing – review & editing. JP: Writing – review & editing. JK: Writing – review & editing. LB: Writing – review & editing. MS: Writing – review & editing. MA: Writing – review & editing. NH: Writing – review & editing. NM: Writing – review & editing. NW: Writing – review & editing. PS: Writing – review & editing. SK: Writing – review & editing. SP: Writing – review & editing. TK: Writing – review & editing. TT: Writing – review & editing. VH: Writing – review & editing. DP: Project administration, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The funds for covering APCs were provided by the generous support from the Hydrocephalus and Neuroscience Institute, Orlando FL USA, the Association for Socially Applicable Research (ASAR), Pune, Maharashtra, India, and individual contributions from authors.
Conflict of interest
SZ represents the Association for Socially Applicable Research (ASAR) on the drafting committee of the Maharashtra State Mental Health Policy. He has previously received honoraria from Think Global Health, Harvard Public Health Magazine, and The Hindu. He is on the advisory board of ASAR and Nivarana. JP has received consulting fees from Integra Neurosciences and Johnson & Johnson in the past. GJ was employed by the Rural Surgery Innovations Private Limited.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Price, R, Makasa, E, and Hollands, M. World health assembly resolution WHA68.15: “strengthening emergency and essential surgical care and anesthesia as a component of universal health coverage”—addressing the public health gaps arising from lack of safe, affordable and accessible surgical and anesthetic services. World J Surg. (2015) 39:2115–25. doi: 10.1007/s00268-015-3153-y
2. Debas, HT, Donkor, P, Gawande, A, Jamison, DT, Kruk, ME, and Mock, CN eds. Essential surgery: disease control priorities. 3rd ed. Washington, DC: The International Bank for Reconstruction and Development/The World Bank (2015).
3. Meara, JG, Leather, AJM, Hagander, L, Alkire, BC, Alonso, N, Ameh, EA, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. (2015) 386:569–624. doi: 10.1016/S0140-6736(15)60160-X
4. Massenburg, BB, Saluja, S, Jenny, HE, Raykar, NP, Ng-Kamstra, J, Guilloux, AGA, et al. Assessing the Brazilian surgical system with six surgical indicators: a descriptive and modelling study. BMJ Glob Health. (2017) 2:e000226. doi: 10.1136/bmjgh-2016-000226
5. Hanna, JS, Herrera-Almario, GE, Pinilla-Roncancio, M, Tulloch, D, Valencia, SA, Sabatino, ME, et al. Use of the six core surgical indicators from the lancet commission on global surgery in Colombia: a situational analysis. Lancet Glob Health. (2020) 8:e699–710. doi: 10.1016/S2214-109X(20)30090-5
6. Samper, AFG, Herrera-Almario, GE, Tulloch, D, Blanco, D, Cardoso, LL, Rocha, REN, et al. A granular analysis of service delivery for surgical system strengthening: application of the lancet indicators for policy development in Colombia. Lancet Reg Health Am. (2022) 10:100217. doi: 10.1016/j.lana.2022.100217
7. Pérez-Soto, RH, Trolle-Silva, AM, Valdés, GAB-R, Sánchez-Morales, GE, Velázquez-Fernández, D, Medina, ARD, et al. Timely access to essential surgery, surgical workforce, and surgical volume: global surgery indicators in mexico. Glob Health Sci Pract. (2023) 11:e2100745. doi: 10.9745/GHSP-D-21-00745
8. Dahir, S, Cotache-Condor, CF, Concepcion, T, Mohamed, M, Poenaru, D, Adan Ismail, E, et al. Global initiative for Children’s surgery. Interpreting the lancet surgical indicators in Somaliland: a cross-sectional study. BMJ Open. (2020) 10:e042968. doi: 10.1136/bmjopen-2020-042968
9. Bruno, E, White, MC, Baxter, LS, Ravelojaona, VA, Rakotoarison, HN, Andriamanjato, HH, et al. An evaluation of preparedness, delivery and impact of surgical and anesthesia care in Madagascar: a framework for a national surgical plan. World J Surg. (2017) 41:1218–24. doi: 10.1007/s00268-016-3847-9
10. Albutt, K, Punchak, M, Kayima, P, Namanya, DB, Anderson, GA, and Shrime, MG. Access to safe, timely, and affordable surgical care in Uganda: a stratified randomized evaluation of nationwide public sector surgical capacity and core surgical indicators. World J Surg. (2018) 42:2303–13. doi: 10.1007/s00268-018-4485-1
11. Nunez, JM, Nellermoe, J, Davis, A, Ruhnke, S, Gonchigjav, B, Bat-Erdene, N, et al. Establishing a baseline for surgical care in Mongolia: a situational analysis using the six indicators from the lancet commission on global surgery. BMJ Open. (2022) 12:e051838. doi: 10.1136/bmjopen-2021-051838
12. Peters, AW, Roa, L, Rwamasirabo, E, Ameh, E, Ulisubisya, MM, Samad, L, et al. National surgical, obstetric, and anesthesia plans supporting the vision of universal health coverage. Glob Health Sci Pract. (2020) 8:1–9. doi: 10.9745/GHSP-D-19-00314
13. United Nations Population Fund. World population dashboard. (2022) Available at: https://www.unfpa.org/data/world-population-dashboard (Accessed May 20, 2023).
14. The World Bank. GDP (current US$) data. (2021). Available at: https://data.worldbank.org/indicator/NY.GDP.MKTP.CD (Accessed May 20, 2023).
15. Institute for Health Metrics and Evaluation. GBD 2019 results - VizHub. GBD 2019 results tool (2020) Available at: https://vizhub.healthdata.org/gbd-results/?params=gbd-api-2019-permalink/91f6967efb4e64a836428f2f312d5134 (Accessed May 19, 2023).
16. Rahman, MM, Karan, A, Rahman, MS, Parsons, A, Abe, SK, Bilano, V, et al. Progress toward universal health coverage: a comparative analysis in 5 south asian countries. JAMA Intern Med. (2017) 177:1297–305. doi: 10.1001/jamainternmed.2017.3133
17. Das, S, and Paul, R. Urbanization trend of south, east, and southeast asian countries: influence of economic growth and changing trends in employment sectors. CUS. (2021) 9:694–719. doi: 10.4236/cus.2021.94041
18. Khatun, F, Ahmed, MG, Chaturvedi, S, Sharma, P, Sapkota, C, Ahmed, A, et al. Liberalising health services under SAARC agreement on trade in services (SATIS): Implications for south Asian countries. Nepal: South Asia Centre for Policy Studies (SACEPS) (2011).
19. Zaidi, S, Saligram, P, Ahmed, S, Sonderp, E, and Sheikh, K. Expanding access to healthcare in South Asia. BMJ. (2017) 357:j1645. doi: 10.1136/bmj.j1645
20. Izquierdo, G, Trelles, M, and Khan, N. Reducing maternal mortality in conflict areas: surgical-anesthetic experience in boost hospital – Afghanistan. Colomb J Anesthesiol. (2016) 44:13–6. doi: 10.1016/j.rcae.2015.11.001
21. Sarkar, S. Pakistan floods pose serious health challenges. BMJ. (2022):o2141. doi: 10.1136/bmj.o2141
22. Jamil, H, Liaqat, A, Lareeb, I, Tariq, W, Jaykumar, V, Kumar, L, et al. Monsoon and cholera outbreaks in Pakistan: a public health concern during a climate catastrophe. Int J Surg. (2023) 6:e105–5. doi: 10.1097/GH9.0000000000000105
23. Sarkar, S. The devastating health consequences of Sri Lanka’s economic collapse. BMJ. (2022) 377:o1543. doi: 10.1136/bmj.o1543
24. Matthias, AT, and Jayasinghe, S. Worsening economic crisis in Sri Lanka: impacts on health. Lancet Glob Health. (2022) 10:e959. doi: 10.1016/S2214-109X(22)00234-0
25. Bickler, SN, Weiser, TG, Kassebaum, N, Higashi, H, Chang, DC, Barendregt, JJ, et al. Global burden of surgical conditions In: HT Debas, P Donkor, A Gawande, DT Jamison, ME Kruk, and CN Mock, editors. Essential surgery: disease control priorities. 3rd ed. Washington, DC: The International Bank for Reconstruction and Development/The World Bank (2015)
26. Higashi, H, Barendregt, JJ, Kassebaum, NJ, Weiser, TG, Bickler, SW, and Vos, T. Burden of injuries avertable by a basic surgical package in low- and middle-income regions: a systematic analysis from the global burden of disease 2010 study. World J Surg. (2015) 39:1–9. doi: 10.1007/s00268-014-2685-x
27. Higashi, H, Barendregt, JJ, Kassebaum, NJ, Weiser, TG, Bickler, SW, and Vos, T. Surgically avertable burden of obstetric conditions in low- and middle-income regions: a modelled analysis. BJOG. (2015) 122:228–36. doi: 10.1111/1471-0528.13198
28. Higashi, H, Barendregt, JJ, Kassebaum, NJ, Weiser, TG, Bickler, SW, and Vos, T. The burden of selected congenital anomalies amenable to surgery in low and middle-income regions: cleft lip and palate, congenital heart anomalies and neural tube defects. Arch Dis Child. (2015) 100:233–8. doi: 10.1136/archdischild-2014-306175
29. Higashi, H, Barendregt, JJ, Kassebaum, NJ, Weiser, TG, Bickler, SW, and Vos, T. Surgically avertable burden of digestive diseases at first-level hospitals in low and middle-income regions. Surgery. (2015) 157:411–9. discussion: 420. doi: 10.1016/j.surg.2014.07.009
30. Alkire, BC, Raykar, NP, Shrime, MG, Weiser, TG, Bickler, SW, Rose, JA, et al. Global access to surgical care: a modelling study. Lancet Glob Health. (2015) 3:e316–23. doi: 10.1016/S2214-109X(15)70115-4
31. Zadey, S. Measuring access to surgical care in rural India: synthesis of data and novel index. (2021). Available at: https://hdl.handle.net/10161/23143 (Accessed August 28, 2021).
32. Alkire, BC, Shrime, MG, Dare, AJ, Vincent, JR, and Meara, JG. Global economic consequences of selected surgical diseases: a modelling study. Lancet Glob Health. (2015) 3:S21–7. doi: 10.1016/S2214-109X(15)70088-4
33. Peck, G, Saluja, S, Blitzer, DN, Sarma, D, Anderson, GA, Rodas, E, et al. Using global surgical indicators to improve trauma care in Latin America. Bull Am Coll Surg. (2017) 102:11–6.
34. Santhirapala, V, Peden, CJ, Meara, JG, Biccard, BM, Gelb, AW, Johnson, WD, et al. Towards high-quality peri-operative care: a global perspective. Anaesthesia. (2020) 75:e18–27. doi: 10.1111/anae.14921
35. The Lancet Commission on Global Surgery. Data for the sustainable development of surgical systems: a global collaboration. The Lancet Commission on Global Surgery (2015).
36. Holmer, H, Lantz, A, Kunjumen, T, Finlayson, S, Hoyler, M, Siyam, A, et al. Global distribution of surgeons, anaesthesiologists, and obstetricians. Lancet glob. Health. (2015) 3:S9–S11. doi: 10.1016/S2214-109X(14)70349-3
37. Weiser, TG, Haynes, AB, Molina, G, Lipsitz, SR, Esquivel, MM, Uribe-Leitz, T, et al. Size and distribution of the global volume of surgery in 2012. Bull World Health Organ. (2016) 94:201–209F. doi: 10.2471/BLT.15.159293
38. Shrime, MG, Dare, A, Alkire, BC, and Meara, JG. A global country-level comparison of the financial burden of surgery. Br J Surg. (2016) 103:1453–61. doi: 10.1002/bjs.10249
39. NIHR Global Health Unit on Global Surgery, COVIDSurg Collaborative. Elective surgery system strengthening: development, measurement, and validation of the surgical preparedness index across 1632 hospitals in 119 countries. Lancet. (2022) 400:1607–17. doi: 10.1016/S0140-6736(22)01846-3
40. Holmer, H, Oyerinde, K, Meara, JG, Gillies, R, Liljestrand, J, and Hagander, L. The global met need for emergency obstetric care: a systematic review. BJOG. (2015) 122:183–9. doi: 10.1111/1471-0528.13230
41. Betran, AP, Ye, J, Moller, A-B, Souza, JP, and Zhang, J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health. (2021) 6:e005671. doi: 10.1136/bmjgh-2021-005671
42. World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations population division. Geneva: World Health Organization (2019).
43. Rao, SR, and Zadey, S. Global analysis of adequacy of prescription opioid consumption across 214 countries and territories. medRxiv. (2023). doi: 10.1101/2023.05.30.23290676
44. World Health Organization. Global status report on blood safety and availability 2021. Geneva: World Health Organization (2022). Available at: https://www.who.int/publications/i/item/9789240051683 (Accessed May 1, 2023).
45. Holmer, H, Shrime, MG, Riesel, JN, Meara, JG, and Hagander, L. Towards closing the gap of the global surgeon, anaesthesiologist, and obstetrician workforce: thresholds and projections towards 2030. Lancet. (2015) 385:S40. doi: 10.1016/S0140-6736(15)60835-2
46. Rose, J, Weiser, TG, Hider, P, Wilson, L, Gruen, RL, and Bickler, SW. Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health estimate. Lancet Glob Health. (2015) 3:S13–20. doi: 10.1016/S2214-109X(15)70087-2
47. Paxton, A, Bailey, P, and Lobis, S. The United Nations process indicators for emergency obstetric care: reflections based on a decade of experience. Int J Gynaecol Obstet. (2006) 95:192–208. doi: 10.1016/j.ijgo.2006.08.009
48. Department of Reproductive Health and Research, World Health Organization. WHO statement on caesarean section rates. World Health Organization. (2015). Available at: https://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf (Accessed February 8, 2023).
49. World Health Organization. Trends in maternal mortality 2000 to2020: Estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/population division. Geneva, Switzerland: World Health Organization (2023). Available at: https://www.who.int/publications/i/item/9789240068759 (Accessed May 29, 2023).
50. Scholten, WK, Christensen, A-E, Olesen, AE, and Drewes, AM. Quantifying the adequacy of opioid analgesic consumption globally: an updated method and early findings. Am J Public Health. (2019) 109:52–7. doi: 10.2105/AJPH.2018.304753
51. Holmer, H, Bekele, A, Hagander, L, Harrison, EM, Kamali, P, Ng-Kamstra, JS, et al. Evaluating the collection, comparability and findings of six global surgery indicators. Br J Surg. (2019) 106:e138–50. doi: 10.1002/bjs.11061
52. Knowlton, LM, Banguti, P, Chackungal, S, Chanthasiri, T, Chao, TE, Dahn, B, et al. A geospatial evaluation of timely access to surgical care in seven countries. Bull World Health Organ. (2017) 95:437–44. doi: 10.2471/BLT.16.175885
53. Verguet, S, Alkire, BC, Bickler, SW, Lauer, JA, Uribe-Leitz, T, Molina, G, et al. Timing and cost of scaling up surgical services in low-income and middle-income countries from 2012 to 2030: a modelling study. Lancet Glob Health. (2015) 3:S28–37. doi: 10.1016/S2214-109X(15)70086-0
54. Ng-Kamstra, JS, Arya, S, Greenberg, SLM, Kotagal, M, Arsenault, C, Ljungman, D, et al. Perioperative mortality rates in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Glob Health. (2018) 3:e000810. doi: 10.1136/bmjgh-2018-000810
55. Shrime, MG, Dare, AJ, Alkire, BC, O’Neill, K, and Meara, JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health. (2015) 3:S38–44. doi: 10.1016/S2214-109X(15)70085-9
56. Zadey, S, and Nickenig Vissoci, JR. Analyzing surgical volumes, rates, and need in rural India. medRxiv. (2021). doi: 10.1101/2021.11.03.21265903
57. Zadey, S, Iyer, H, Nayan, A, Shetty, R, Sonal, S, Smith, ER, et al. Evaluating the status of the lancet commission on global surgery indicators for India. Lancet Reg Health. (2023) 13:100178. doi: 10.1016/j.lansea.2023.100178
58. Jadhav, T, Vissoci, JRN, and Zadey, S. Measuring timely geographical access to surgical care in India: a geospatial modelling study. Lancet Glob Health. (2022) 10:S29. doi: 10.1016/S2214-109X(22)00158-9
59. Zadey, S, Smith, ER, Staton, CA, Fitzgerald, TN, and Vissoci, JRN. Population-level surgical rates and unmet need in India: a retrospective analysis of districts and states from 2011 to 2019. Int J Surg. (2024). doi: 10.1097/JS9.0000000000001024
60. Ashraf, M, Vervoort, D, Rizvi, S, Fatima, I, Shoman, H, Meara, JG, et al. Access to safe, timely and affordable surgical, anaesthesia and obstetric care in Pakistan: a 16-year scoping review. East Mediterr Health J. (2022) 28:302–13. doi: 10.26719/emhj.22.009
61. Fatima, I, Shoman, H, Peters, A, Vervoort, D, Samad, L, and Meara, JG. Assessment of pakistan’s surgical system by tracking the lancet global surgery indicators toward a national surgical, obstetric, and anaesthesia plan. J Am Coll Surg. (2019) 229:S125. doi: 10.1016/j.jamcollsurg.2019.08.278
62. Betrán, AP, Ye, J, Moller, A-B, Zhang, J, Gülmezoglu, AM, and Torloni, MR. The increasing trend in caesarean section rates: global, regional and National Estimates: 1990-2014. PLoS One. (2016) 11:e0148343. doi: 10.1371/journal.pone.0148343
63. Roy, N, Gerdin, M, Ghosh, S, Gupta, A, Kumar, V, Khajanchi, M, et al. 30-day in-hospital trauma mortality in four Urban University hospitals using an Indian trauma registry. World J Surg. (2016) 40:1299–307. doi: 10.1007/s00268-016-3452-y
64. Shivasabesan, G, O’Reilly, GM, Mathew, J, Fitzgerald, MC, Gupta, A, Roy, N, et al. Establishing a multicentre trauma registry in India: an evaluation of data completeness. World J Surg. (2019) 43:2426–37. doi: 10.1007/s00268-019-05039-2
65. Gobyshanger, T, Bales, AM, Hardman, C, and McCarthy, M. Establishment of a road traffic trauma registry for northern Sri Lanka. BMJ Glob Health. (2020) 5:e001818. doi: 10.1136/bmjgh-2019-001818
66. Fatima, I, Shoman, H, Peters, AW, Samad, L, and Nishtar, S. Pakistan’s National Surgical, obstetric, and anesthesia plan: an adapted model for a devolved federal-provincial health system. Can J Anaesth. (2020) 67:1212–6. doi: 10.1007/s12630-020-01708-2
67. Ministry of Health and Population Vision for Surgical Care Strengthening Nepal 2030: concept note. Nepal: Ministry of Health and Population (2021). Available at: http://www.nsi.edu.np/uploaded/Notices/NSOAP%20Orientation%20Concept%20Note.pdf (Accessed August 10, 2022).
68. Lancet Commission on Global Surgery. India National Surgical Forum, lancet commission on global surgery. (2016) Available at: https://www.lancetglobalsurgery.org/india-national-surgical-forum (Accessed February 10, 2021).
69. Association Of Rural Surgeons Of India-Lancet Commission On Global Surgery Consensus Committee Arsi-LCoGS Consensus Committee. The lancet commission on global surgery - Association of Rural Surgeons of India Karad consensus statement on surgical system strengthening in rural India. Healthc. (2019) 7:7–9. doi: 10.1016/j.hjdsi.2018.10.003
70. Raykar, N, Mukhopadhyay, S, Saluja, S, Amte, S, David, S, Gnanaraj, J, et al. Implementation of the lancet commission on global surgery in India. Healthc. (2019) 7:4–6. doi: 10.1016/j.hjdsi.2018.11.001
71. Directorate General of Health Services, Ministry of Health and Family Welfare. National programme for prevention and management of trauma and burn injuries. Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India (2013). Available at: https://dghs.gov.in/content/1528_3_NationalProgrammeforPreventionandManagement.aspx (Accessed August 1, 2022).
72. Zadey, S, Sonal, S, Iyer, H, Baxy, H, Smith, ER, Staton, CA, et al. Roadblocks and solutions to planning surgical care for a billion Indians. BMJ Glob Health. (2022) 7:e010292. doi: 10.1136/bmjgh-2022-010292
73. Shetty, R, Zadey, S, Jindal, A, Iyer, H, Dubey, S, Jesudian, G, et al. Prioritization of surgical, obstetric, trauma, and anesthesia care in India over seven decades: a systematic analysis of policy documents. PLoS Glob Public Health. (2023) 3:e0002084. doi: 10.1371/journal.pgph.0002084
74. Injury Prevention Division, Non Communicable Diseases Unit, Ministry of Health. National policy and strategic framework on injury prevention and management in Sri Lanka. Sri Lanka: Ministry of Health - Sri Lanka (2016).
75. Directorate of Non communicable Diseases, Ministry of Health. Multi-sectoral strategic action plan on injury prevention and management - Sri Lanka (2021-2025). Colombo: Ministry of Health - Sri Lanka (2022).
76. Mazingi, D, Navarro, S, Bobel, MC, Dube, A, Mbanje, C, and Lavy, C. Exploring the impact of COVID-19 on Progress towards achieving global surgery goals. World J Surg. (2020) 44:2451–7. doi: 10.1007/s00268-020-05627-7
77. Dhakal-Rai, S, van Teijlingen, E, Regmi, PR, Wood, J, Dangal, G, and Dhakal, KB. Factors contributing to rising cesarean section rates in south Asian countries: a systematic review. Asian J Med Sci. (2022) 13:143–74. doi: 10.3126/ajms.v13i2.40904
78. Verma, V, Vishwakarma, RK, Nath, DC, Khan, HTA, Prakash, R, and Abid, O. Prevalence and determinants of caesarean section in south and south-east Asian women. PLoS One. (2020) 15:e0229906. doi: 10.1371/journal.pone.0229906
79. Ronsmans, C, Holtz, S, and Stanton, C. Socioeconomic differentials in caesarean rates in developing countries: a retrospective analysis. Lancet. (2006) 368:1516–23. doi: 10.1016/S0140-6736(06)69639-6
80. Neuman, M, Alcock, G, Azad, K, Kuddus, A, Osrin, D, More, NS, et al. Prevalence and determinants of caesarean section in private and public health facilities in underserved south Asian communities: cross-sectional analysis of data from Bangladesh, India and Nepal. BMJ Open. (2014) 4:e005982. doi: 10.1136/bmjopen-2014-005982
81. Panda, BK, Nayak, I, and Mishra, US. Determinant of inequality in cesarean delivery in India: a decomposition analysis. Health Care Women Int. (2020) 41:817–32. doi: 10.1080/07399332.2020.1711757
82. Mumtaz, S, Bahk, J, and Khang, Y-H. Rising trends and inequalities in cesarean section rates in Pakistan: evidence from Pakistan demographic and health surveys, 1990-2013. PLoS One. (2017) 12:e0186563. doi: 10.1371/journal.pone.0186563
83. Siddiqi, S, Khan, MS, Rizvi, N, Naeem, I, Rozi, S, Enam, A, et al. Are rural hospitals in Pakistan responding to the global surgery movement? An analysis of the gaps, challenges and opportunities. World J Surg. (2020) 44:1045–52. doi: 10.1007/s00268-019-05327-x
84. Alvi, R. Experience of developing rural surgical care in a remote mountainous region of Pakistan: challenges and opportunities. Ann Trop Med Public Health. (2011) 4:57. doi: 10.4103/1755-6783.80541
85. Zadey, S. Why India’s surgical care crisis is less jigsaw, More Tetris – in Three Charts. The Wire (2019) Available at: https://thewire.in/health/why-indias-surgical-care-crisis-is-less-jigsaw-more-tetris-in-three-charts (Accessed August 28, 2021).
86. Mishra, A, Bains, L, Jesudin, G, Aruparayil, N, Singh, R, and Shashi,. Evaluation of gasless laparoscopy as a tool for minimal access surgery in low-to middle-income countries: a phase II noninferiority randomized controlled study. J Am Coll Surg. (2020) 231:511–9. doi: 10.1016/j.jamcollsurg.2020.07.783
87. Aruparayil, N, Gnanaraj, J, Maiti, S, Chauhan, M, Quyn, A, Mishra, A, et al. Training programme in gasless laparoscopy for rural surgeons of India (TARGET study) - observational feasibility study. Int J Surg Open. (2021) 35:100399. doi: 10.1016/j.ijso.2021.100399
88. Tshering, S, Dorji, T, Dorji, N, Monger, R, Choden, K, and Lhamo, K. Setting up minimal invasive surgery services in gynecology in a resource-limited setting: an experience from Bhutan. BMC Res Notes. (2022) 15:59. doi: 10.1186/s13104-022-05953-0
89. Bajaj, J, Yadav, YR, Pateriya, A, Parihar, V, Ratre, S, and Dubey, A. Indigenous inexpensive practice models for skill development in neuroendoscopy. J Neurosci Rural Pract. (2017) 8:170–3. doi: 10.4103/jnrp.jnrp_495_16
90. Sharma, D, Agrawal, S, and Saxena, A. Dissection with a metal dissector: a useful adjunct to transhiatal oesophagectomy. Asian J Surg. (2005) 28:100–3. doi: 10.1016/S1015-9584(09)60271-2
91. Sharma, D, Agrawal, S, Saxena, A, and Raina, VK. A modified technique of devascularization for surgical management of portal hypertension in children. Trop Dr. (2001) 31:93–5. doi: 10.1177/004947550103100213
92. Banu, T, Chowdhury, TK, Kabir, M, Talukder, R, and Lakhoo, K. Bringing surgery to rural children: Chittagong, Bangladesh experience. World J Surg. (2013) 37:730–6. doi: 10.1007/s00268-013-1916-x
93. Talati, JJ, and Syed, NA. Surgical training programs in Pakistan. World J Surg. (2008) 32:2156–61. doi: 10.1007/s00268-008-9639-0
94. Evans, CL, Maine, D, McCloskey, L, Feeley, FG, and Sanghvi, H. Where there is no obstetrician--increasing capacity for emergency obstetric care in rural India: an evaluation of a pilot program to train general doctors. Int J Gynaecol Obstet. (2009) 107:277–82. doi: 10.1016/j.ijgo.2009.09.006
95. Nagral, S, Hussain, M, Nayeem, SA, Dias, R, Enam, SA, and Nundy, S. Unmet need for surgery in South Asia. BMJ. (2017) 357:j1423. doi: 10.1136/bmj.j1423
96. Lantz, A, Holmer, H, Finlayson, SRG, Ricketts, TC, Watters, DA, Gruen, RL, et al. Measuring the migration of surgical specialists. Surgery. (2020) 168:550–7. doi: 10.1016/j.surg.2020.04.014
97. Hagander, LE, Hughes, CD, Nash, K, Ganjawalla, K, Linden, A, Martins, Y, et al. Surgeon migration between developing countries and the United States: train, retain, and gain from brain drain. World J Surg. (2013) 37:14–23. doi: 10.1007/s00268-012-1795-6
98. Brennan, N, Langdon, N, Bryce, M, Gale, T, Knapton, A, Burns, L, et al. Drivers of international migration of doctors to and from the United Kingdom. United Kingdom: CAMERA, Peninsula Medical School, University of Plymouth (2021). Available at: https://www.gmc-uk.org/-/media/documents/drivers-of-international-migration-research-final-report_pdf-88769526.pdf (Accessed May 19, 2023).
99. Saluja, S, Rudolfson, N, Massenburg, BB, Meara, JG, and Shrime, MG. The impact of physician migration on mortality in low and middle-income countries: an economic modelling study. BMJ Glob Health. (2020) 5:e001535. doi: 10.1136/bmjgh-2019-001535
100. Buchan, J, Catton, H, and Shaffer, FA. Sustain and retain in 2022 and beyond: the global nursing workforce and the COVID-19 pandemic. Philadelphia, PA: International Centre on Nurse Migration (2022). Available at: https://www.icn.ch/system/files/2022-01/Sustain%20and%20Retain%20in%202022%20and%20Beyond-%20The%20global%20nursing%20workforce%20and%20the%20COVID-19%20pandemic.pdf (Accessed June 29, 2023).
101. Vinish, V, Chakrabarty, J, Vijayan, S, Nayak, BS, Shashidhara, YN, Kulkarni, M, et al. Prevalence of road traffic injuries in south east and south Asian region - a systematic review. J Neurosci Rural Pract. (2023) 14:214–23. doi: 10.25259/JNRP_25_2022
102. Global Burden of Disease Collaborative Network. Global burden of disease study 2019 (GBD 2019) results. Institute for Health Metrics and Evaluation (IHME), Seattle. (2020). Available at: https://vizhub.healthdata.org/gbd-results/ (Accessed May 25, 2023).
103. Alam, K, and Mahal, A. The economic burden of road traffic injuries on households in South Asia. PLoS One. (2016) 11:e0164362. doi: 10.1371/journal.pone.0164362
104. Wesson, HKH, and Kwong, M. Trauma care in India: a review of the literature. Surgery. (2017) 162:S85–S106. doi: 10.1016/j.surg.2017.01.027
105. Sriram, VM, Gururaj, G, and Hyder, AA. Public-private implementation of integrated emergency response services: case study of GVK emergency management and research Institute in Karnataka, India. Surgery. (2017) 162:S63–76. doi: 10.1016/j.surg.2017.01.026
106. Neurotrauma Society of India. National guidelines for the management of traumatic brain injury, eds. M. Joseph, S. Sinha, D. Shukla, and V. D. Sinha Uttar Pradesh: Thieme (2022). Available at: https://neurosocietyindia.com/wp-content/uploads/2022/03/NTBI_merged_seventh-proof.pdf (Accessed June 29, 2023).
107. Fitzgerald, MC, O’Reilly, GM, Seneviratne, R, Ellawala, R, and Cameron, PA. Towards a Sri Lankan national trauma system. J Cey Coll Phys. (2017) 48:24. doi: 10.4038/jccp.v48i1.7808
108. Shidhaye, RV, Divekar, DS, Goel, G, and Shidhaye, R. Influence of working conditions on job satisfaction in Indian anesthesiologists: a cross-sectional survey. Anaesthesia, Pain & Intensive Care (2011). Available at: https://www.apicareonline.com/index.php/APIC/article/view/972 (Accessed May 24, 2023).
109. Bindu, B, Bindra, A, Kumar, S, Kulkarni, S, Rath, G, Prabhakar, H, et al. Survey of work practices among anesthesiologists in India. Indian Anaesth Forum. (2019) 20:1. doi: 10.4103/TheIAForum.TheIAForum_9_19
110. Lantz, A, Holmer, H, Finlayson, S, Ricketts, TC, Watters, D, Gruen, R, et al. International migration of surgeons, anaesthesiologists, and obstetricians. Lancet Glob Health. (2015) 3:S11–2. doi: 10.1016/S2214-109X(15)70084-7
111. Devi, S. Sri Lankan health system facing lengthy shortages. Lancet. (2022) 399:1682. doi: 10.1016/S0140-6736(22)00774-7
112. Wijesuriya, N. Anaesthetists seeing through the economic crisis of Sri Lanka. Sri Lankan J Anaesthesiol. (2022) 30:149–50. doi: 10.4038/slja.v30i2.9105
113. Alhattab, S, and Mahat, P. Three children or youth died every minute in South Asia in 2021 – UN report. UNICEF (2023). Available at: https://www.unicef.org/rosa/press-releases/three-children-or-youth-died-every-minute-south-asia-2021-un-report#:~:text=1%2C287%2C000%20children%20in%20South%20Asia%20died%20before%20their%205th%20birthday%20in%202021 (Accessed May 22, 2023).
114. Stokes, SC, and Farmer, DL. Paediatric surgery for congenital anomalies: the next frontier for global health. Lancet. (2021) 398:280–1. doi: 10.1016/S0140-6736(21)01547-6
115. Truche, P, Botelho, F, Bowder, AN, Levis, AW, Greenberg, SLM, Smith, E, et al. Potentially avertable child mortality associated with surgical workforce scale-up in low- and middle-income countries: a global study. World J Surg. (2021) 45:2643–52. doi: 10.1007/s00268-021-06181-6
116. Bouchard, ME, Tian, Y, Justiniano, J, Linton, S, DeBoer, C, Abdullah, F, et al. A critical threshold for global pediatric surgical workforce density. Pediatr Surg Int. (2021) 37:1303–9. doi: 10.1007/s00383-021-04939-6
117. Lalchandani, P, and Dunn, JCY. Global comparison of pediatric surgery workforce and training. J Pediatr Surg. (2015) 50:1180–3. doi: 10.1016/j.jpedsurg.2014.11.032
118. Rao, S, and Zadey, S. Surgical, anesthesia and obstetrics (SAO) workforce production capacity in India: a retrospective analysis of postgraduate and sub-specialty training spots. medRxiv. (2023). doi: 10.1101/2023.01.12.23284480
119. Qazi, SH, Meerza, SSA, Groen, RS, Dogar, SA, Mirani, M, Jamali, MK, et al. Assessment of pediatric surgical needs, health-seeking behaviors, and health systems in a rural district of Pakistan. PLoS Glob Public Health. (2022) 2:e0000810. doi: 10.1371/journal.pgph.0000810
120. Sohail, AH, Maan, MHA, Sachal, M, and Soban, M. Challenges of training and delivery of pediatric surgical services in developing economies: a perspective from Pakistan. BMC Pediatr. (2019) 19:152. doi: 10.1186/s12887-019-1512-9
121. Nagarajan, N, Gupta, S, Shresthra, S, Varadaraj, V, Devkota, S, Ranjit, A, et al. Unmet surgical needs in children: a household survey in Nepal. Pediatr Surg Int. (2015) 31:389–95. doi: 10.1007/s00383-015-3684-1
122. Kunaviktikul, W, Turale, S, Petrini, MA, Tungpunkom, P, and Avant, KC. Experiences from Southeast Asia on nursing education, practice, mobility and influencing policy. Int Nurs Rev. (2019) 66:474–81. doi: 10.1111/inr.12556
123. Bogren, MU, Wiseman, A, and Berg, M. Midwifery education, regulation and association in six south Asian countries--a descriptive report. Sex Reprod Healthc. (2012) 3:67–72. doi: 10.1016/j.srhc.2012.03.004
124. Huang, WN, Xin, X, Rao, V, Wong, TH, Chow, P, and Tan, HK. Battling against the great disruption to surgical care in a pandemic: experiences of 11 south and southeast Asian countries. BMJ Open. (2023) 13:e060770. doi: 10.1136/bmjopen-2022-060770
125. Dorjey, Y, Tshomo, Y, Wangchuk, D, Bhandari, P, Dorji, C, Pradhan, D, et al. Impact of COVID-19 pandemic on reproductive, maternal, newborn, and child health care services in Phuentsholing general hospital: a retrospective descriptive study. Health Sci Rep. (2022) 5:e946. doi: 10.1002/hsr2.946
126. Gadsden, T, Downey, LE, Vilas, VDR, Peiris, D, and Jan, S. The impact of COVID-19 on essential health service provision for noncommunicable diseases in the South-East Asia region: a systematic review. Lancet Reg Health Southeast Asia. (2022) 1:100010. doi: 10.1016/j.lansea.2022.04.006
127. Thapa, A. COVID-19 and the role of neurosurgeons in Nepal. World Neurosurg. (2020) 139:629–31. doi: 10.1016/j.wneu.2020.05.093
128. Gothwal, M, Singh, P, Sharma, C, Yadav, G, and Gupta, MK. Impact of COVID-19 pandemic on obstetrics and gynecology residency training program in India: a national online survey. J Obstet Gynaecol Res. (2022) 48:1955–60. doi: 10.1111/jog.15291
129. Osama, M, Zaheer, F, Saeed, H, Anees, K, Jawed, Q, Syed, SH, et al. Impact of COVID-19 on surgical residency programs in Pakistan; a residents’ perspective. Do programs need formal restructuring to adjust with the “new normal”? A cross-sectional survey study. Int J Surg. (2020) 79:252–6. doi: 10.1016/j.ijsu.2020.06.004
130. Ehsan, AN, Park, KB, and Pigeolet, M. An open letter to the executive board of WHO from the surgical and anaesthesia community. Lancet. (2022) 399:1380–1. doi: 10.1016/S0140-6736(22)00521-9
131. Kundu, S, Sana, H, Dutta, R, Gerk, A, Pigeolet, M, and Raykar, NP. Call for standardised emergency preparedness and response. Lancet. (2023) 401:1924–5. doi: 10.1016/S0140-6736(23)01070-X
132. Sindhu, J, and Singh, G. Analysis of chronic pain Management in Canada and South Asia. GHAR (2021) 1. Available at: https://journals.mcmaster.ca/ghar/article/view/2695/1936 (Accessed May 21, 2023).
133. Tharwani, ZH, Kumar, P, Shaeen, SK, Islam, Z, Essar, MY, and Ahmad, S. Maternal mortality in Afghanistan: challenges, efforts, and recommendations. Clin Epidemiol Glob Health. (2022) 15:101038. doi: 10.1016/j.cegh.2022.101038
134. Dargay, S, Tenzin, T, and Tenzin, K. Postgraduate surgical education in Bhutan. Indian J Surg. (2021) 84:313–7. doi: 10.1007/s12262-021-03163-9
135. van Loenhout, JAF, Delbiso, TD, Gupta, S, Amatya, K, Kushner, AL, Gil Cuesta, J, et al. Barriers to surgical care in Nepal. BMC Health Serv Res. (2017) 17:72. doi: 10.1186/s12913-017-2024-7
136. Knulst, AJ, Gupta, S, Groen, RS, Maharjan, D, Kapendra, AS, Dankelman, J, et al. Directions for surgical capacity developments in Nepal: a population-based assessment. Trop Med Int Health. (2019) 24:1128–37. doi: 10.1111/tmi.13292
137. Boeck, MA, Nagarajan, N, Gupta, S, Varadaraj, V, Groen, RS, Shrestha, S, et al. Assessing access to surgical care in Nepal via a cross-sectional, countrywide survey. Surgery. (2016) 160:501–8. doi: 10.1016/j.surg.2016.03.012
138. Shah, RK, Markus, AF, and Shah, NK. Tackling the challenges of providing surgical services in low resource LMICs: shortcomings in surgical healthcare in Nepal. J Oral Biol Craniofac Res. (2022) 12:63–7. doi: 10.1016/j.jobcr.2021.09.019
139. Juran, S, Moren, S, Santhirapala, V, Roa, L, Makasa, E, Davies, J, et al. The development and inclusion of questions on surgery in the 2018 Zambia demographic and health survey. Glob Health Sci Pract. (2021) 9:905–14. doi: 10.9745/GHSP-D-20-00619
140. Daniels, KM, Riesel, JN, Verguet, S, Meara, JG, and Shrime, MG. The scale-up of the global surgical workforce: can estimates be achieved by 2030? World J Surg. (2020) 44:1053–61. doi: 10.1007/s00268-019-05329-9
141. Rao, S, and Zadey, S. Surgical, anesthesia and obstetrics (SAO) workforce production capacity in India: a retrospective analysis of postgraduate and subspecialty training spots. Global Surg Educ. (2023) 2:77. doi: 10.1007/s44186-023-00154-0
142. Zadey, S, and Dubey, S. Helping doctors reach rural India. Global Health NOW (2021). Available at: https://www.globalhealthnow.org/2021-02/helping-doctors-reach-rural-india (Accessed August 22, 2021).
143. National Board of Examinations. Guidelines for competency-based training Programme in DNB - rural surgery. Available at: https://nbe.edu.in/mainpdf/curriculum/rural-surgery.pdf (Accessed June 10, 2023).
144. Mubarik, F, Shahzad, H, Abidi, SS, Zeeshan, S, Vohra, L, Khan, S, et al. Telementoring for breast surgeons practicing in remote areas. J Pak Med Assoc. (2021) 71:S120–3.
145. Waqar, U, Ahmed, S, Ukrani, RD, Mansoor, M, Khan, S, and Enam, SA. PakSurg: the first trainee-lead model for multicenter surgical research collaboration in Pakistan. J Pak Med Assoc. (2022) 72:S130–3. doi: 10.47391/JPMA.AKU-27
146. Ali, M, Babar Chauha, SS, Noor, A, Khan, S, and Enam, SA. Peer-led surgery education: a model for a surgery interest group. J Pak Med Assoc. (2021) 71:S112–6.
147. Jumbam, DT, Bustamante, A, Alayande, BT, Ayala, R, Kouam, JC, Dzirasa, I, et al. To advance global surgery and anaesthesia, train more advocates. BMJ Glob Health. (2023) 8:e012848. doi: 10.1136/bmjgh-2023-012848
148. Falk, R, Taylor, R, Kornelsen, J, and Virk, R. Surgical task-sharing to non-specialist physicians in low-resource settings globally: a systematic review of the literature. World J Surg. (2020) 44:1368–86. doi: 10.1007/s00268-019-05363-7
149. Ashengo, T, Skeels, A, Hurwitz, EJH, Thuo, E, and Sanghvi, H. Bridging the human resource gap in surgical and anesthesia care in low-resource countries: a review of the task sharing literature. Hum Resour Health. (2017) 15:77. doi: 10.1186/s12960-017-0248-6
150. Robertson, FC, Esene, IN, Kolias, AG, Khan, T, Rosseau, G, Gormley, WB, et al. Global perspectives on task shifting and task sharing in neurosurgery. World Neurosurg. (2020) 6:100060. doi: 10.1016/j.wnsx.2019.100060
151. Aruparayil, N, Bolton, W, Mishra, A, Bains, L, Gnanaraj, J, King, R, et al. Clinical effectiveness of gasless laparoscopic surgery for abdominal conditions: systematic review and meta-analysis. Surg Endosc. (2021) 35:6427–37. doi: 10.1007/s00464-021-08677-7
152. Owolabi, EO, Mac Quene, T, Louw, J, Davies, JI, and Chu, KM. Telemedicine in surgical care in low- and middle-income countries: a scoping review. World J Surg. (2022) 46:1855–69. doi: 10.1007/s00268-022-06549-2
153. Ho, C, Tsakonas, E, Tran, K, Cimon, K, Severn, M, Mierzwinski-Urban, M, et al. Robot-assisted surgery compared with open surgery and laparoscopic surgery: clinical effectiveness and economic analyses. Ottawa: Canadian Agency for Drugs and Technologies in Health (2011). Available at: https://www.ncbi.nlm.nih.gov/books/NBK168933/ (Accessed June 6, 2023).
154. Ravi, S. SAARC and India’s healthcare opportunities. Brookings India Briefing Book (2014) Available at: https://www.brookings.edu/research/saarc-and-indias-healthcare-opportunities/ (Accessed June 7, 2023).
155. Rai, A, Chakraborty, P, and Sarkar, A. India as a medical tourism hub in SAARC – a geographical analysis. Indian J Spat Sci. (2014) 5:12–20.
156. Dubey, S, Deshpande, S, Krishna, L, and Zadey, S. Evolution of government-funded health insurance for universal health coverage in India. Lancet Reg Health. (2023) 13:100180. doi: 10.1016/j.lansea.2023.100180
157. Jadhav, S, Yeravdekar, R, and Kulkarni, M. Cross-border healthcare access in south Asian countries: learnings for sustainable healthcare tourism in India. Procedia Soc Behav Sci. (2014) 157:109–17. doi: 10.1016/j.sbspro.2014.11.014
158. PTI. Quick visa for SAARC patients to boost India’s medical tourism. The Economic Times (2014) Available at: https://economictimes.indiatimes.com/nri/visa-and-immigration/quick-visa-for-saarc-patients-to-boost-indias-medical-tourism/articleshow/45307855.cms?from=mdr (Accessed June 7, 2023).
159. Sethuraman, K, Tirupati, D, Raykar, N, and Awasthy, PJan Swasthya Sahyog Referral Centre. Surgical care for low-income, rural populations: an alternative delivery model from Jan Swasthya Sahyog, India. The Lancet Commission on Global Surgery (2015). Available at: https://www.lancetglobalsurgery.org/_files/ugd/346076_0042c02da6be4bb1b4e66933efdb0d6a.pdf (Accessed June 7, 2023).
160. Arnquist, S, Rosenberg, J, and Weintraub, R. The Indus Hospital: building surgical capacity in Pakistan. The Lancet Commission on Global Surgery (2015). Available at: https://www.globalhealthdelivery.org/files/ghd/files/ghd-023s_indus_hospital-_building_surgical_capacity_condensed_version.pdf (Accessed August 15, 2022).
161. Tshering, S, Dorj, N, Monger, R, Sonam, S, and Koirala, N. Quality improvement initiative to address bed shortage in the maternity ward at the National Referral Hospital. Health Sci Rep. (2022) 5:e721. doi: 10.1002/hsr2.721
162. Le, H-G, Ehrlich, JR, Venkatesh, R, Srinivasan, A, Kolli, A, Haripriya, A, et al. A sustainable model for delivering high-quality, efficient cataract surgery in southern India. Health Aff. (2016) 35:1783–90. doi: 10.1377/hlthaff.2016.0562
163. Ma, X, Marinos, J, De Jesus, J, Lin, N, Sung, C-Y, and Vervoort, D. Human rights-based approach to global surgery: a scoping review. Int J Surg. (2020) 82:16–23. doi: 10.1016/j.ijsu.2020.08.004
164. Ghandour, H, and Truche, P. UHC surgery and anesthesia as essential components of universal health coverage (WHA 68.15) In: J Kpodonu, editor. Global cardiac surgery capacity development in low and middle income countries sustainable development goals series. Cham: Springer International Publishing (2022). 29–37.
165. Roa, L, Jumbam, DT, Makasa, E, and Meara, JG. Global surgery and the sustainable development goals. Br J Surg. (2019) 106:e44–52. doi: 10.1002/bjs.11044
166. Chao, TE, Sharma, K, Mandigo, M, Hagander, L, Resch, SC, Weiser, TG, et al. Cost-effectiveness of surgery and its policy implications for global health: a systematic review and analysis. Lancet Glob Health. (2014) 2:e334–45. doi: 10.1016/S2214-109X(14)70213-X
167. Greer, SL, and Méndez, CA. Universal health coverage: a political struggle and governance challenge. Am J Public Health. (2015) 105:S637–9. doi: 10.2105/AJPH.2015.302733
168. Khetrapal Singh, P, Cassels, A, and Travis, P. Primary healthcare at forty: reflections from South-East Asia. New Delhi: World Health Organization, Regional Office for South-East Asia (2018). Available at: https://www.who.int/docs/default-source/primary-health-care-conference/phc-regional-report-south-east-asia.pdf?sfvrsn=1c2a8e85 (Accessed June 29, 2023).
169. SAARC. SAARC recognized bodies. (2020). Available at: https://www.saarc-sec.org/index.php/about-saarc/saarc-recognized-bodies (Accessed June 7, 2023).
170. SAARC Secretariat. SAARC Secretariat - areas of cooperation. SAARC Secretariat (2023). Available at: https://www.saarc-sec.org/ (Accessed June 12, 2023).
171. STAC. About - SAARC TB and HIV/AIDS Centre. (2023). Available at: https://www.saarctb.org/saarc-tb-and-hivaids-centre/ (Accessed June 7, 2023).
Glossary
Keywords: global surgery, SOTA care, South Asia, priorities, health planning, LMICs
Citation: Zadey S, Rao S, Gondi I, Sheneman N, Patil C, Nayan A, Iyer H, Kumar AR, Prasad A, Finley GA, Prasad CRK,, Sharma D, Ghosh D, Jesudian G, Fatima I, Pattisapu J, Ko JS, Bains L, Shah M, Alam MS, Hadigal N, Malhotra N, Wijesuriya N, Shukla P, Khan S, Pandya S, Khan T, Tenzin T, Hadiga VR and Peterson D (2024) Achieving Surgical, Obstetric, Trauma, and Anesthesia (SOTA) care for all in South Asia. Front. Public Health. 12:1325922. doi: 10.3389/fpubh.2024.1325922
Edited by:
Soham Bandyopadhyay, University of Oxford, United KingdomReviewed by:
Gitismita Naik, All India Institute of Medical Sciences, Kalyani (AIIMS Kalyani), IndiaLanfranco Iodice, Ministry of Health (Italy), Italy
Copyright © 2024 Zadey, Rao, Gondi, Sheneman, Patil, Nayan, Iyer, Kumar, Prasad, Finley, Prasad, Chintamani, Sharma, Ghosh, Jesudian, Fatima, Pattisapu, Ko, Bains, Shah, Alam, Hadigal, Malhotra, Wijesuriya, Shukla, Khan, Pandya, Khan, Tenzin, Hadiga and Peterson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Siddhesh Zadey, c2lkemFkZXlAYXNhcmZvcmluZGlhLm9yZw==
 Siddhesh Zadey
Siddhesh Zadey Shirish Rao1,5,6
Shirish Rao1,5,6