- 1Indian Institute of Public Health-Delhi, Public Health Foundation of India, Gurgaon, India
- 2Academy of Scientific and Innovative Research (AcSIR), Ghaziabad, India
- 3Division of Reproductive, Child Health and Nutrition, Indian Council of Medical Research, Department of Health Research, Ministry of Health and Family Welfare, Government of India, New Delhi, India
- 4Institute of Genomics and Integrative Biology, Council of Scientific and Industrial Research (CSIR), New Delhi, India
- 5Department of Cardiology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India
- 6Department of Neurology, Institute of Human Behaviour and Allied Sciences, University of Delhi, New Delhi, India
- 7Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
The coronavirus pandemic that began in December 2019, has had an unprecedented impact on the global economy, health systems and infrastructure, in addition to being responsible for significant mortality and morbidity worldwide. The “new normal” has brought along, unforeseen challenges for the scientific community, owing to obstructions in conducting field-based research in lieu of minimizing exposure through in-person contact. This has had greater ramifications for the LMICs, adding to the already existing concerns. As a response to COVID-19 related movement restrictions, public health researchers across countries had to switch to remote data collections methods. However, impediments like lack of awareness and skepticism among participants, dependence on paper-based prescriptions, dearth of digitized patient records, gaps in connectivity, reliance on smart phones, concerns with participant privacy at home and greater loss to follow-up act as hurdles to carrying out a research study virtually, especially in resource-limited settings. Promoting health literacy through science communication, ensuring digitization of health records in hospitals, and employing measures to encourage research participation among the general public are some steps to tackle barriers to remote research in the long term. COVID-19 may not be a health emergency anymore, but we are not immune to future pandemics. A more holistic approach to research by turning obstacles into opportunities will not just ensure a more comprehensive public health response in the coming time, but also bolster the existing infrastructure for a stronger healthcare system for countries.
Introduction
In December 2019, the city of Wuhan in China reported the first human case of the novel coronavirus infection caused by the SARS-CoV2, a disease that we now know as COVID-19. The outbreak spread globally soon after, with the World Health Organization (WHO) declaring COVID-19 a global pandemic on March 11, 2020 (1). Three years on, the total number of confirmed COVID-19 cases (as of March 10, 2023) worldwide are more than 676 million, while the total number of confirmed deaths stand close to 6.9 million (2). The pandemic has resulted in huge economic losses, a breakdown of the fragile health infrastructure especially in the lower- and middle-income countries, and a significant increase in poverty and unemployment, above and beyond the high mortality and morbidity rates in the affected populations (3–7). The effects of COVID-19 have thus been far-reaching, and we continue to grapple with multiple concerns encountered in this “new normal”.
One of the greatest unrivaled challenges faced by the medical and scientific communities has been the disruption of non-coronavirus related clinical and public health research activities with trials and field studies getting delayed or prematurely concluded (8–11). Protocols like maintaining physical distancing, restricting travel and avoiding gatherings and meetings to lower the risk of transmission of this highly infectious viral disease, as well as redirection of existing funds for pandemic research, have made field-based research work involving human participants in healthcare settings like hospitals and clinics as well as in the community rather challenging (10, 11). Although non-COVID research took a hit across countries, low-middle-income countries (LMICs) have suffered a greater impact due to amplification of existing difficulties (12). As a response to this, researchers across the globe have shifted to virtual or remote methods of collecting study data during the pandemic (13, 14). This involves telephonic and tele-conference methods, as well as web-based applications to communicate with the participants, while ensuring the wellbeing of everyone involved in such studies. Digital approaches and the use of technology have thus gathered immense momentum in the last 2 years since they allow people to participate without worrying about exposing themselves to the infection. Such methods make it easier for the researchers to continue their work safely, while adhering to COVID-19 appropriate mandates. Various remote methods have been in use in high-income countries, such as interactive voice response (IVR), computer-assisted telephone interviews (CATI), short message service (SMS) and video conferencing (via zoom/skype), for both qualitative and quantitative purposes (13, 15). Due to lower levels of education and internet access and availability issues in spite of extensive use of mobile phones in low and middle income countries (LMICs), telephonic methods are more common and preferred over online internet-based methods (16). However, such approaches come with their own set of complications, especially in developing nations. Such challenges have been further augmented by COVID-19 (17).
Our paper aims to document the significant impediments to epidemiological research amidst the pandemic, in a resource-limited setting, based on our experience of conducting a hospital-based observational study in North India, substantiating them with existing evidence in this regard. We also propose ways to address some of these setbacks and suggest feasible solutions. Our research study is an ongoing prospective cohort involving in-person recruitment of patients on statins from the cardiology outpatient department of a tertiary care hospital in Delhi, and subsequent remote data collection telephonically, for a 2 year follow-up period with data obtained at baseline, and at the end of the first and second years.
Barriers to conducting field-based research during the COVID-19 pandemic
Economic constraints, lack of awareness and skepticism
The health system in the LMICs comprises of both private and public health care facilities and a significant proportion of the population opts for private health centers (18, 19). According to a few published reports, the private sector accounts for a considerable share of healthcare services in developing economies and caters to the lower income groups as well (40%, 57% and 62% in the African, South-East Asian, and Western Mediterranean regions) (20–22). The population groups that cannot afford private healthcare services are thus dependent on large public tertiary care centers offering medical care at a highly subsidized cost (18, 19, 23). Thus, in developing nations, a significant proportion of the patients at tertiary care centers belong to the lowest socio-economic strata.
The literacy levels in patients are also rather low, with studies reporting a 30%−45% prevalence of low to no education across LMICs (24–28). This in turn leads to a sub-optimal level of health literacy, i.e., their understanding and knowledge of their disease condition and medications. Limited awareness of clinical research and its relevance have also been reported as deterrents to research interest and participation in a few studies (29–34).
The pandemic has exacerbated this challenge. Remote interactions are now more feasible and safer as compared to in-person interactions, and it is difficult to explain things telephonically and convey the point across as effectively as one would, in a face-to-face setting (35). Gaps in communication act as hindrances to data collection. Also, building trust without an in-person interaction requires both patience and time, since a phone call doesn't offer the same personal touch (13, 36).
Unavailability of digital records and the use of paper-based prescriptions
Large government/public hospitals have a high burden of patients, a heavy footfall in their Out Patient Departments (OPD) and limited resources (37, 38). The existing infrastructure makes it difficult to establish and maintain digital records or online databases for admitted patients and OPD patients in most such facilities. Unlike the west, the implementation and use of electronic medical record (EMR) systems in the LMICs remains rather minimal, and is limited to a handful of private tertiary care centers, while an overwhelming majority in the private and public sector still work with paper-based records (39–44). Additionally, the paper-based prescriptions are usually available only with the patient (45). Prescriptions and other documents like test reports and discharge summaries tend to get lost, torn or misplaced, and unavailability of records makes it impossible to track patients or obtain their history remotely (46).
Ensuring correctness of contact information
Since remote modes of data collection are largely dependent on establishing contact through a mobile phone in resource limited settings, the contact information provided to the researcher is of prime importance. However, the numbers provided for the call may turn out to be erroneous or out of service, leaving the investigators with no choice but to drop the participant. At times the contact number may stop functioning due to inability of patients/caregivers to recharge/top up the talk time given the financial constraints exacerbated by the pandemic. This also gives rise to the need for multiple contact points within the participant's family, so that if the primary phone number turns out to be incorrect or non-functional, contact can still be established through alternate numbers. This is a time-intensive activity since the respondents' family/friends need to be contacted first, in order to be able to communicate with the participant (36).
Dependence on smart phones and instant messengers
Remote data collection methods involve the use of a smartphone with an internet connection and instant messaging apps like WhatsApp. This can be used to obtain drug prescriptions, biochemical test reports, scans and other such source documents from the patient. According to a 2023 report, more than half of the world's current population, now owns a smartphone, with 4.3 billion users (47). WhatsApp messenger is also gaining momentum for use in population-based surveys and provides new opportunities for enhanced communication and engagement during fieldwork (48). However, its use is currently limited in LMICs and both its potential and concerns with respect to data collection in health research need further exploration (49). Also, roughly 3 billion people, about 38% of the world population, despite living in mobile broadband network areas, do not use the Internet (47). Therefore, participants with limited means, especially those in the older age groups, may not possess a smart phone/WhatsApp, or may not be well versed with its functioning and correct usage (50, 51). In such cases, gathering data becomes an arduous task (36, 52).
Connectivity and network issues in rural areas
The economy has taken a massive hit as a result of the pandemic. This has led to a significant increase in unemployment, which in turn has pushed the working class into poverty. Consequently, a large number of people belonging to the lower socio-economic strata had to migrate back to their ancestral homes often in remote rural locations (53–55). This has inevitably affected data collection procedures adversely. Network and connectivity play a major role in carrying out remote research work. City outskirts, suburban and rural areas may not have adequate network coverage which results in weak signals, call drops and patchy internet connectivity (13, 16). Each interview with a participant residing in such a location takes longer and usually involves more than one call making it a time-intensive endeavor. These disturbances and interruptions also hamper the overall quality of the data collected during remote telephone-based interviews (36). Virtual modes of collecting research data have compounded the already existing digital divide, putting the economically weaker participants at a disadvantage in many aspects (14, 56).
Decreased patient footfall in the hospitals
There is often a dearth of tertiary care health services in low-and middle income countries (LMICs). Tertiary care hospitals even when available, are present only in the major cities (57, 58). Hence, they cater to patients not just from the same city, but also from various neighboring cities and regions across the country. In the wake of COVID-19, health related travel went down, unless there was a medical emergency or a health condition that required immediate attention. This could be to avert the risk of infection and to avoid spending money on inter-city travel at a time when finances are rather limited. As a consequence, the total number of patients visiting these health facilities was much lesser than it used to be pre-pandemic (59–62).
Lesser footfall means a smaller sampling frame to choose from. This leads to longer periods of recruitment and contributes to delays in study conduct. Progress of studies requiring in person follow ups can be expected to be hampered similarly. Transport and distance related concerns have always been barriers to participating in field based research that have been further compounded during the pandemic times (32).
Issues with privacy
Unlike in-person interviews, where the investigator can choose an appropriate setting for the patient to be in, interviews conducted remotely do not offer the same flexibility in terms of the surrounding environment of the participant (63). Often, participants when called, are at home, sitting with their family members. Space constraints and overcrowding with several people living together makes it almost impossible to talk to the participant privately. Sometimes participants find a place outside their homes where they may be joined by a neighbor or a friend (13, 14). In face-to-face settings, the researcher has significant control on the environment and can ensure privacy at all times. However, this onus is placed on the participants in remote research (13). Such situations act as obstacles to data collection which ideally requires a silent area. It thus becomes difficult to ensure confidentiality and accuracy of responses which affects validity of the data and continued participation (34).
Ethical challenges
Conducting research during a pandemic is essential as well as necessary, but the appropriateness of the same may be debatable. Subjecting the participant to an extensive interview or survey during unprecedented times when people are struggling with a deadly virus, monetary losses and other peculiar disruptions in the wake of a global pandemic could pose a moral dilemma. Additionally, obtaining verbal consent in remote research work comes with its own set of challenges, in terms of maintaining a record of the consent obtained, while being mindful of privacy and mitigating the risk for coercion, in order to maintain the voluntary participation requirement. This becomes an even more important consideration when dealing with vulnerable groups or studies involving sensitive topics (17). Remote data collection may also put a greater responsibility on the participants, in terms of getting their phones recharged, figuring out the use of WhatsApp or other remote data collection apps, and finding an appropriate space at home to respond to the investigator's calls. On the contrary, such methods relieve the participants of the burden associated with spending time and the opportunity cost to travel to the study setting/hospital, and in many cases, missing out on their daily wages. Such issues often find themselves at the center of debate and discussion. The pros and cons of this conundrum need to be weighed for every research study, following which it should be dealt with in a manner that is sensitive, does no harm to participants while also ensuring that science and biomedical research are not unduly hampered by the pandemic (13).
Increased frequency of non-response and higher attrition rates
Conducting research using remote methods like mobile phones can lead to a higher non-response rate in the study population (64, 65). Response rates ranging from 40 to 55% for telephonic surveys and interviews have been previously reported in literature (66–70). Higher non-response has been correlated to older, less affluent and less educated individuals, and is found to be affected by connectivity and low internet bandwidth issues too (65–68, 71). This becomes even more relevant when it comes to living in small crowded spaces, joint phone ownership in the family and limited availability of resources to maintain digital connectivity, along with mistrust in unknown numbers and misconstruing calls as being phishing/spam (13, 16). Also, the older adults are sometimes uncomfortable speaking over the phone and prefer a face-to-face discussion which could be a reason for their refusal to participate. At times, this translates to women and the aged being under-represented owing to lack of autonomy and independence in the household (13). In some patriarchal settings, the male spouse may choose to respond on behalf of the female which affects the accuracy of the answers (13, 72). Moreover, since mobile phones are the predominant mode of communication, tracking participants down for follow-up investigations and interviews is an uphill task too. Once they are aware of how the telephonic survey would go, some of them stop taking follow-up calls saying they don't have time for another round of interview, or that they don't understand the reason for a second call (13, 16). Also, a majority of mobile phone users subscribe to prepaid connections (73, 74), which are more likely to get discontinued, and thus could immediately cut the participant off from the researcher. Thus, remote surveys might run the risk of a higher dropout rates and greater loss to follow-up, as compared to in-person studies (75). It is possible that such studies have a slight overrepresentation of people belonging to the higher socio-economic groups, those with access to individual smartphones and ability to use the internet, those with higher literacy and those living in relatively less crowded homes (13, 76).
Maintaining respondent engagement and interest
Ensuring the interest and attention of the respondents over a phone call is rather demanding. Additional efforts need to be made to keep participants engaged since this can affect the overall quality and accuracy of the collected data (64). This pertains to very young and very old individuals, who may get bored or lose interest and hang up in the middle of the interview, leaving responses incomplete. Longer interactions/questionnaires may further fatigue or distract the participants, leading to the information captured being unreliable and/ or invalid (16, 36).
Possible solutions for conducting field based research in a pandemic scenario
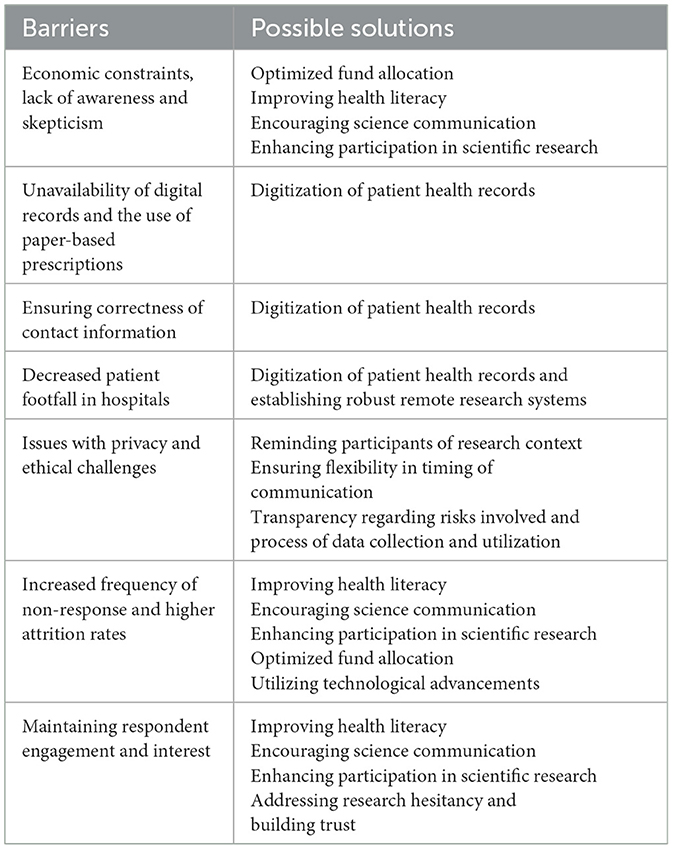
Clinical research is vital to reducing disease burden, enhancing health, and increasing the overall quality of life in populations. It also provides insights into disease pathology and epidemiology that can help scientists and researchers tackle new diseases and improve patient outcomes (77, 78). Thus, research becomes even more essential during a public health crisis. Even as the COVID-19 pandemic subsides, the challenges of conducting research, especially remotely, continue to exist. We have provided insights based on our experience with quantitative research. However, the restrictions that come with a pandemic have equally affected qualitative research as well (79–81). In fact, there are several overlapping issues affecting both the approaches to health research conduct, while some remain unique to each methodology (82). The following section describes possible solutions to address some of the barriers highlighted above (Table 1).
Improving health literacy
The World Health Organization defines health literacy as ‘the achievement of a level of knowledge, personal skills, and confidence to take action to improve personal and community health by changing personal lifestyles, and living conditions' (83). In other words, it is the ability of a person to make sense of health related information so as to implement the same in their routine activities, and augment their quality of life (84). Health literacy rates in the developing countries are significantly low, owing to inadequate education, economic constraints, and other socio-cultural barriers (84, 85).
Improving health literacy among populations can enable people to play a more active role in their treatment and overall health. Targeted health interventions focused on populations with limited or no health literacy can improve their understanding of their health, reduce skepticism toward scientific research, enhance treatment compliance and strengthen doctor-patient relationships (86). This would ultimately augment interest in research participation and support remote research activities in the long term. Better knowledge of their own health, clinical care and the relevance and need for research could improve response rates and encourage willingness of the participants to contribute both in-person and virtually.
This would require improvements in the existing health infrastructure to support access to relevant health information, more manpower for engagement with medical professionals as well as the general public, and encouraging the practice of science communication in healthcare for communicating information to the patients in a language and manner they understand. Easy to read infographics, posters and pamphlets prepared in local languages, training health educators for interacting with communities, integrating health literacy in the educational curriculum in schools, and sensitizing researchers, scientists and medical professionals about this issue have been shown to be effective in this regard (84, 87). However, it is important to note that health literacy is a complex issue which is a function of various systemic factors like linguistic, social and cultural barriers, poverty and lower standards of living, gender disparities, as well as shortcomings of the current education system, which in turn result in lack of basic education and sub-optimal literacy levels overall (88–92). Addressing these fundamental concerns through policy level changes and national reforms, with various stakeholders working synergistically, is a starting point that would eventually contribute to improved health literacy levels as well.
Encouraging science communication
Science communication (SciComm) has gathered a lot of momentum over the years, as a result of growing interest of educators, scientists and communication experts in this field. It is based on the broad concept that distinguishes information availability and accessibility. Readily available medical information in research papers, textbooks, newspapers, may not be accessible to the layperson. Also, accessibility itself does not ensure usability. Technical jargon, unfamiliar vocabulary and complex texts can act as major hindrances to uptake of information by the general population. Science communication aims to bridge this knowledge gap, by making important information available and accessible to the public, through simpler narratives translated in multiple languages, for easier consumption (93–96). A good example of SciComm is clinicians communicating information about a disease condition to a patient (explanation of their illness, the treatment regimen, adverse-effects if any, and precautions to be taken) in a simplified manner and in the vernacular language specific to that region. It is an ecosystem that encompasses numerous stakeholders, each with a designated role, and involves multiple communication pathways -digital, verbal, visual amongst others (93, 97).
Changes at the individual as well as the policy level can contribute to improved health literacy through SciComm. There is a dearth of literature on the effect of various interventions on health literacy rates in resource limited settings, warranting the need for extensive research to understand economic implications of low literacy rates and the cost-effectiveness of various interventions- traditional/learning based (booklets, pamphlets), art based (storytelling), interaction based (peer-support programs) and technology based (digital devices and websites) (88, 98, 99). However, evidence from the developed world settings does suggest that higher literacy could prove to be cost-effective since lower health literacy levels are associated with higher medical costs (100, 101).
Digitization of patient health records
An electronic health record (EHR) is a collection of medical records of a person that are created during a clinical event and get accumulated over their lifetime. Maintaining an electronic database helps keep a record of important medical information and history of the patient, avoid repeat investigations and improve the overall therapeutic experience for both care providers and receivers. The public sector IT system needs improvements in terms of internet speed and connectivity issues. Apart from data protection concerns, setting up infrastructure for digital systems is resource intensive and requires personnel (102). Other challenges that hamper the broader implementation of digital record systems in healthcare include limited financial backing, lack of processes for data integration, inadequate training and capacity building, low education levels, legislation and policy gaps, and concerns with cyber security laws, ethics and regulatory bottlenecks (103–106). Filling these lacunae is a herculean task and would require concerted efforts over time but can have a substantial positive impact on public health research and contribute to more robust evidence synthesis. Digital records become even more essential in remote research where participants might be required to furnish information through mobile phones. Availability of medical documents and other records in an online format could enable easy access for participants as well as easy sharing with the study investigators, ensuring completeness of the medical data obtained from each participant.
As part of the above, shifting to e-prescriptions can make doctor-patient consultations a much more seamless experience. Paper based prescriptions are prone to errors, can have handwriting issues, and run the risk of getting lost or misplaced, leading to permanent loss of crucial patient information and disease history (107–109). Some physicians have also suggested incorporating printed terms for “Morning,” “Afternoon,” and “Evening” in different local languages on the prescription sheet to overcome the language barrier (110). Keeping a scanned copy of the patient prescription with the consulting doctor/hospital is also believed to be a useful way of ensuring that a record of the patient history exists with the hospital in case the patient loses or forgets to carry it with them (110). Additionally, there is literature evidence to show that hospitals with electronic patient health records incur lower costs due to fewer errors and a more streamlined management system (111).
However, one needs to remember that the transition from paper based records to electronic records can only happen in phases, with establishments gradually shifting to a hybrid mode before operating in a paperless fashion. Even then, the paper based approach has its own advantages that cannot be overlooked or rendered redundant and while digital technology is the future, offline documentation can always serve as a backup repository for data storage.
Enhancing participation in scientific research
People's willingness to participate in a study, whether hospital-based, field-based or remote, is one of the most pivotal aspects of clinical research. Acknowledging systemic and individual level hurdles in this regard is the first step toward enhanced participation rates at the start of the study and reduced attrition while it is ongoing. Systematic reviews conducted in the past have suggested a few factors that could effectively favor participation in research (34, 95, 96, 112).
Providing clarity regarding short-term or long term benefits for the participant
Patients are found to be more likely to participate in research studies if they are convinced that the output will benefit their health. It is essential to be transparent as well as realistic with participants in terms of what they can expect from their involvement (34, 95, 96, 112). Additionally, efforts should be made to make them understand that research is not the same as medical care and immediate treatment benefit may not be a possibility (95).
Instilling a sense of altruism
The feeling of being able to contribute to collective good has been found to influence patients' decision to participate in research in some cases. Making them aware of the larger goal of improved therapeutic experience and enhanced clinical care for future patients could serve as an impetus for participation (113, 114).
Sharing details of any risks involved
Adequately informing participants of any major or minor risks involved can ensure greater trust in the research process, which in turn could positively impact participation rates. This requires detailed patient information sheets and availability of the study team/personnel for answering questions and addressing apprehensions (34, 96).
Maintaining transparency in data collection and utilization processes
Various approaches to garner greater confidence in the research and its findings have been suggested in literature, including sharing of study data where applicable, dissemination of results among the participants, and keeping them updated about the study progress along with other stakeholders (34, 95, 96, 112). The language and terminology used for communicating such information plays a crucial role in communication (34, 95, 96, 112).
Facilitating access to the healthcare provider
In tertiary care public health facilities, the doctor-patient ratio is highly skewed, resulting in heavy patient loads in most outpatient as well as inpatient departments. Making efforts to provide participants better access to therapeutic care, especially where the clinician researcher is leading the study, could also serve as a significant impetus to continued participation and retention in the study (34, 95, 96, 112).
Addressing research hesitancy
Tackling skepticism about research among the patients is paramount. Alleviating their concerns with empathy and establishing the importance of their participation through regular engagement and communication can help avoid feelings of distrust and apprehension toward research (34, 95, 96, 112).
Building patients' trust in the researchers
Rapport building is an essential component of any clinical research study. Being available for the patients, providing them with a contact number they could use and setting aside some time to address any queries they may have, related to the ongoing research or the clinical care, could be a source of validation for them, lowering their reluctance to engage with the investigators over the course of the study (34, 95, 96, 112).
Further, remote data collection brings along some peculiar issues pertaining to privacy, the participant's overall understanding of the setting (since they are usually in their homes), establishment of initial contact, and internet and connectivity hassles. The following ways could ensure greater willingness to participate in such studies and lower the risk of attrition (14, 115).
Reminding them of research context
Remote research involves participants attending interviews from their homes, instead of being present in a formal setting. This can lead to them forgetting the purpose or context of the investigator's call. In such cases, reminding them of the purpose of the study can improve data quality while allowing participants to speak comfortably (14, 115).
Offering alternative times for communication
Participation in research while being at home means less stringent schedules for investigators to operate within. Additionally, pandemic related disruptions can further interrupt people's daily routines and data collection may not always happen as planned. Sending a reminder beforehand, as well as providing a different time slot based on the participant's convenience saves the researchers' time and the flexibility keeps the participant interested (14, 115).
Working closely with their friends/family
Establishing more than one level of contact could help minimize drop outs and loss to follow ups. Efforts to obtain contact information of a family member, or friend who is either a caregiver, accompanies the patient for their hospital visits or is involved in any other aspect of their treatment becomes important if access to the patient is getting difficult (14, 115). Communication with a family member could also ensure greater trust from their end.
Optimizing fund allocation
Since remote research involves much lesser travel to the hospital/clinical setting, provisions could be made to divert that component of the study grant toward providing call and internet services to the participants (14, 115). Enhanced access to technology through resource optimization can streamline the process of study data collection considerably and ensure continued participant engagement (14, 115).
Utilizing technological advancements
A remote research setting may not always allow immediate communication with the participant. Technological features like voice notes in WhatsApp can come in very handy in situations when a voice call is not feasible. Besides, text reminders for upcoming or missed follow-up calls can be helpful in ensuring participant availability at scheduled times (14, 115). This could foster continuity in research and can help keep the participants engaged during follow-ups.
Conclusion
The pandemic has significantly altered the world we live in, bringing in a multitude of changes in various aspects of our routine lives. This has inevitably affected the way we conduct field-based research activities as well. Some of the challenges are unfamiliar, while others have just resurfaced or been magnified. However, the myriad of issues associated with carrying out primary research also bring opportunities to work differently and perhaps improve and strengthen the existing systems in place.
Remote research comes with its own set of concerns, but can also be highly effective in organizing routine surveillance measures for timely capture of health-related data. Addressing the barriers highlighted above through leveraging technology, investing in health infrastructure, and facilitating greater awareness can modify our overall approach to research.
The worst of the COVID-19 pandemic has come to an end, but we are not immune to threats of future epidemics (116–120). Further, the lessons learned during this period can elevate existing research processes as a whole, fostering greater opportunities for scientific advancements in the coming time. Even when traditional methods of face-to-face research are possible, remote methods can help save time and money that could be employed elsewhere to improve the efficiency of field-based research. This transition may not be straightforward and would require being more receptive to incorporating newer ideas into our usual ways of conducting health research. However, the outcomes would be rather rewarding and worth the effort in the long run.
Author contributions
RM: Conceptualization, Investigation, Methodology, Resources, Writing—original draft. TL: Methodology, Project administration, Supervision, Writing—review & editing. SG: Methodology, Project administration, Supervision, Writing—review & editing. HI: Methodology, Supervision, Writing—review & editing. RD: Methodology, Supervision, Writing—review & editing. AK: Conceptualization, Methodology, Resources, Supervision, Writing—review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. RM was supported by a fellowship grant from Council of Scientific and Industrial Research (CSIR), India.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19-−11 March 2020. (2020). Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-−11-march-2020 (accessed March 11, 2022).
2. COVID-19 Map. Johns Hopkins Coronavirus Resource Center. Available online at: https://coronavirus.jhu.edu/map.html (accessed November 10, 2022).
3. Kaye AD, Okeagu CN, Pham AD, Silva RA, Hurley JJ, Arron BL, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: international perspectives. Best Pract Res Clin Anaesthesiol. (2021) 35:293–306. doi: 10.1016/j.bpa.2020.11.009
4. Khan MA, Naqvi HA, Hakeem MM, Din GM, Iqbal N. Economic and financial impact of the COVID-19 pandemic in South Asia. Environ Sci Pollut Res. (2022) 29:15703–15712. doi: 10.1007/s11356-021-16894-9
5. Khetan AK, Yusuf S, Lopez-Jaramillo P, Szuba A, Orlandini A, Mat-Nasir N, et al. Variations in the financial impact of the COVID-19 pandemic across 5 continents: a cross-sectional, individual level analysis. eClinicalMedicine. (2022) 44:101284. doi: 10.1016/j.eclinm.2022.101284
6. Khetrapal S, Bhatia R. Impact of COVID-19 pandemic on health system and Sustainable Development Goal 3. Indian J Med Res. (2020) 151:395–9. doi: 10.4103/ijmr.IJMR_1920_20
7. Pak A, Adegboye OA, Adekunle AI, Rahman KM, McBryde ES, Eisen DP. Economic consequences of the COVID-19 outbreak: the need for epidemic preparedness. Front Public Health. (2020) 8:241. doi: 10.3389/fpubh.2020.00241
8. Eke OF, Morone CC, Liteplo AS, Shokoohi H. Non–COVID-19 clinical research in the era of pandemic. Am J Emerg Med. (2021) 39:231–2. doi: 10.1016/j.ajem.2020.05.013
9. Hillman A. COVID-19 two years on: persistent symptoms of clinical trial disruption trouble certain therapy areas. Clinical Trials Arena. (2022). Available online at: https://www.clinicaltrialsarena.com/features/covid-19-two-years-on-clinical-trial-disruption/ (accessed April 11, 2023).
10. Ledford H. The COVID pandemic's lingering impact on clinical trials. Nature. (2021) 595:341–2. doi: 10.1038/d41586-021-01569-9
11. Sathian B, Asim M, Banerjee I, Pizarro AB, Roy B, van Teijlingen ER, et al. Impact of COVID-19 on clinical trials and clinical research: a systematic review. Nepal J Epidemiol. (2020) 10:878–87. doi: 10.3126/nje.v10i3.31622
12. Hermes CD. COVID challenges for trials in low-to-middle-income countries. Appl Clin Trials. (2020) 29.
13. Hensen B, Mackworth-Young CRS, Simwinga M, Abdelmagid N, Banda J, Mavodza C, et al. Remote data collection for public health research in a COVID-19 era: ethical implications, challenges and opportunities. Health Policy Plan. (2021). doi: 10.1093/heapol/czaa158
14. Walker L, Bailey D, Churchill R, Peckham E. Remote data collection during COVID-19 restrictions: an example from a refugee and asylum-seeker participant group in the UK. Trials. (2021) 22:117. doi: 10.1186/s13063-021-05058-2
15. Lobe B, Morgan D, Hoffman KA. Qualitative data collection in an era of social distancing. Int J Qual Methods. (2020) 19:1609406920937875. doi: 10.1177/1609406920937875
16. Chaudhuri T. Collecting data during COVID-19. Medium. (2020). Available online at: https://trishachaudhuri.medium.com/collecting-data-during-covid-19-477de14bdd2 (accessed March 16, 2022).
17. Khalil K, Das P, Kammowanee R, Saluja D, Mitra P, Das S, et al. Ethical considerations of phone-based interviews from three studies of COVID-19 impact in Bihar, India. BMJ Glob Health. (2021) 6:e005981. doi: 10.1136/bmjgh-2021-005981
18. Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. Lancet. (2011) 377:505–15. doi: 10.1016/S0140-6736(10)61894-6
19. Malhotra C, Do YK. Socio-economic disparities in health system responsiveness in India. Health Policy Plan. (2013) 28:197–205. doi: 10.1093/heapol/czs051
20. Health Services Utilization and Out-of-Pocket Expenditure at Public and Private Facilities in Low-Income Countries- World Health Report 2010. Available online at: https://cdn.who.int/media/docs/default-source/financial-protection/world-health-report-2010.pdf?sfvrsn=c6d4c10a_8anddownload=true (accessed June 1, 2023).
21. Montagu D, Chakraborty N. Standard survey data: insights into private sector utilization. Front. Med. (2021) 8:624285. doi: 10.3389/fmed.2021.624285
22. Tung E, Bennett S. Private sector, for-profit health providers in low and middle income countries: can they reach the poor at scale? Glob Health. (2014) 10:52. doi: 10.1186/1744-8603-10-52
23. Zwi AB, Brugha R, Smith E. Private health care in developing countries: if it is to work, it must start from what users need. BMJ. (2001) 323:463–4. doi: 10.1136/bmj.323.7311.463
24. Clarke-Deelder E, Afriyie DO, Nseluke M, Masiye F, Fink G. Health care seeking in modern urban LMIC settings: evidence from Lusaka, Zambia. BMC Public Health. (2022) 22:1205. doi: 10.1186/s12889-022-13549-3
25. Singh K, Kondal D, Shivashankar R, Ali MK, Pradeepa R, Ajay VS, et al. Health-related quality of life variations by sociodemographic factors and chronic conditions in three metropolitan cities of South Asia: the CARRS study. BMJ Open. (2017) 7:e018424. doi: 10.1136/bmjopen-2017-018424
26. Pati S, Swain S, Knottnerus JA, Metsemakers JFM, van den Akker M. Magnitude and determinants of multimorbidity and health care utilization among patients attending public versus private primary care: a cross-sectional study from Odisha, India. Int J Equity Health. (2020) 19:57. doi: 10.1186/s12939-020-01170-y
27. Naheed A, Hakim M, Islam MS, Islam MB, Tang EYH, Prodhan AA, et al. Prevalence of dementia among older age people and variation across different sociodemographic characteristics: a cross-sectional study in Bangladesh. Lancet Reg Health - Southeast Asia. (2023) 17:100257. doi: 10.1016/j.lansea.2023.100257
28. Mwaka AD, Garimoi CO, Were EM, Roland M, Wabinga H, Lyratzopoulos G. Social, demographic and healthcare factors associated with stage at diagnosis of cervical cancer: cross-sectional study in a tertiary hospital in Northern Uganda. BMJ Open. (2016) 6:e007690. doi: 10.1136/bmjopen-2015-007690
29. Anderson A, Borfitz D, Getz K. Global public attitudes about clinical research and patient experiences with clinical trials. JAMA Network Open. (2018) 1:e182969. doi: 10.1001/jamanetworkopen.2018.2969
30. Fogel DB. Factors associated with clinical trials that fail and opportunities for improving the likelihood of success: a review. Contemp Clin Trials Commun. (2018) 11:156–64. doi: 10.1016/j.conctc.2018.08.001
31. Hamel LM, Penner LA, Albrecht TL, Heath E, Gwede CK, Eggly S. Barriers to clinical trial enrollment in racial and ethnic minority patients with cancer. Cancer Control. (2016) 23:327–37. doi: 10.1177/107327481602300404
32. Neumann S, Bamford A, Lithander FE, Tenison E, Henderson EJ. Public attitudes to the use of remote data collection in clinical research. Contemp Clin Trials. (2021) 111:106595. doi: 10.1016/j.cct.2021.106595
33. Occa A, Leip A, Merritt AS, Stapleton JL. Prevalence and correlates of invitation to participate in clinical trials among US adults. Prev Med Rep. (2022) 26:101742. doi: 10.1016/j.pmedr.2022.101742
34. Shah JY, Phadtare A, Rajgor D, Vaghasia M, Pradhan S, Zelko H, et al. What leads indians to participate in clinical trials? A meta-analysis of qualitative studies. PLoS ONE. (2010) 5:e10730. doi: 10.1371/journal.pone.0010730
35. McDermott MM, Newman AB. Remote research and clinical trial integrity during and after the coronavirus pandemic. JAMA. (2021) 325:1935–6. doi: 10.1001/jama.2021.4609
36. Ali Z, Azlor del Valle L, Fletcher EK, Josephat J, Salisbury T. (2020). Challenges of remote surveying during COVID-19. Results for Development. Available online at: https://r4d.org/blog/remote-surveying-during-covid-19-challenges/ (accessed March 16, 2022).
37. Bajpai V. The challenges confronting public hospitals in india, their origins, and possible solutions. Adv Public Health. (2014) 2014:e898502. doi: 10.1155/2014/898502
38. Kasthuri A. Challenges to healthcare in India—the Five A's. Indian J Community Med. (2018) 43:141–3. doi: 10.4103/ijcm.IJCM_194_18
39. Akhlaq A, McKinstry B, Muhammad KB, Sheikh A. Barriers and facilitators to health information exchange in low- and middle-income country settings: a systematic review. Health Policy Plan. (2016) 31:1310–25. doi: 10.1093/heapol/czw056
40. Ferry AM, Davis MJ, Rumprecht E, Nigro AL, Desai P, Hollier LH. Medical documentation in low- and middle-income countries: lessons learned from implementing specialized charting software. Plast Reconstr Surg Glob Open. (2021) 9:e3651. doi: 10.1097/GOX.0000000000003651
41. Ngugi P, Babic A, Kariuki J, Santas X, Naanyu V, Were MC. Development of standard indicators to assess use of electronic health record systems implemented in low-and medium-income countries. PLoS ONE. (2021) 16:e0244917. doi: 10.1371/journal.pone.0244917
42. Oluoch T, de Keizer NF. Evaluation of health IT in low-income countries. Stud Health Technol Inform. (2016) 222:324–35. doi: 10.3233/978-1-61499-635-4-324
43. Shapiro LM, Kamal RN. Implementation of electronic health records during global outreach: a necessary next step in measuring and improving quality of care. J Hand Surg Am. (2022) 47:279–83. doi: 10.1016/j.jhsa.2021.09.016
44. Srivastava SK. Adoption of electronic health records: a roadmap for India. Healthc Inform Res. (2016) 22:261–9. doi: 10.4258/hir.2016.22.4.261
45. Mishra. A Study to Assess the Degree of Adherence of Prescription to WHO and MCI Guidelines at a Tertiary Health Care Teaching Hospital in North India. Available online at: https://www.jpsiconline.com/article.asp?issn=2214-207X;year=2019;volume=7;issue=2;spage=48;epage=52;aulast=Mishra doi: 10.4103/jpsic.jpsic_12_19 (accessed November 19, 2022).
46. Electronic Prescriptions: Opportunities and Challenges for the Patient | AHCT. Available online at: https://www.dovepress.com/electronic-prescriptions-opportunities-and-challenges-for-the-patient–peer-reviewed-fulltext-article-AHCT (accessed November 18, 2022).
47. GSMA Press Office. Smartphone Owners Are Now the Global Majority, New GSMA Report Reveals. Newsroom (2023). Available online at: https://www.gsma.com/newsroom/press-release/smartphone-owners-are-now-the-global-majority-new-gsma-report-reveals/
48. Jailobaev T, Jailobaeva K, Baialieva M, Baialieva G, Asilbekova G. WhatsApp groups in social research: new opportunities for fieldwork communication and management. Bull Sociol Methodol. (2021) 149:60–82. doi: 10.1177/0759106320978337
49. Manji K, Hanefeld J, Vearey J, Walls H, de Gruchy T. Using WhatsApp messenger for health systems research: a scoping review of available literature. Health Policy Plan. (2021) 36:774–89. doi: 10.1093/heapol/czab024
50. Singh A. Smartphone Ownership In India Depends Upon Income Level And Age: [Report]. (2013). Available online at: https://dazeinfo.com/2013/02/07/smartphone-ownership-in-india-depends-income/
51. Stalin P, Abraham SB, Kanimozhy K, Prasad RV, Singh Z, Purty AJ. Mobile phone usage and its health effects among adults in a semi-urban area of Southern India. J Clin Diagn Res. (2016) 10:LC14–6. doi: 10.7860/JCDR/2016/16576.7074
52. Mahmood S, Hasan K, Carras MC, Labrique A. Global preparedness against COVID-19: we must leverage the power of digital health. JMIR Public Health Surveill. (2020) 6:e18980. doi: 10.2196/preprints.18980
53. Jesline J, Romate J, Rajkumar E, George AJ. The plight of migrants during COVID-19 and the impact of circular migration in India: a systematic review. Humanit Soc Sci Commun. (2021) 8:1. doi: 10.1057/s41599-021-00915-6
54. Sahoo PK, Biswal S, Kumar H, Powell M. Urban to rural COVID-19 progression in India: the role of massive migration and the challenge to India's traditional labour force policies. Int J Health Plann Manage. (2022) 37:528–35. doi: 10.1002/hpm.3327
55. Iyengar KP, Jain VK. COVID-19 and the plight of migrants in India. Postgrad Med J. (2021) 97:471–2. doi: 10.1136/postgradmedj-2020-138454
56. Loucks TL, Tyson C, Dorr D, Garovic VD, Hill J, McSwain SD, et al. Clinical research during the COVID-19 pandemic: the role of virtual visits and digital approaches. J Clin Transl Sci. (2021) 5:e102. doi: 10.1017/cts.2021.19
57. Hamid H, Abid Z, Amir A, Rehman TU, Akram W, Mehboob T. Current burden on healthcare systems in low- and middle-income countries: recommendations for emergency care of COVID-19. Drugs Ther Perspect. (2020) 36:466–8. doi: 10.1007/s40267-020-00766-2
58. Olayemi E, Asare EV, Benneh-Akwasi Kuma AA. Guidelines in lower-middle income countries. Br J Haematol. (2017) 177:846–54. doi: 10.1111/bjh.14583
59. Dutt A. OPD footfall dipped by 57%, surgeries by 43% at one of Delhi's biggest hospitals. Hindustan Times. (2021). Available online at: https://www.hindustantimes.com/cities/delhi-news/opd-footfall-dropped-by-57-surgeries-by-43-at-one-of-delhi-s-biggest-hospitals-101625899593686.html (accessed November 18, 2022).
60. Healthcare Facilities in India Witness 80% Fall in Demand Following COVID-19 Finds Nathealth Survey. (2020). http://www.pharmabiz.com/NewsDetails.aspx?aid=126455andsid=2 (accessed November 18, 2022).
61. Mehrotra A, Chernew ME, Linetsky D, Hatch H, Cutler DM. The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges. (2020). doi: 10.26099/ds9e-jm36
62. Sinha M. Patient footfall decreases by 80% at district hospital. The Times of India. (2020). Available online at: https://timesofindia.indiatimes.com/city/noida/patient-footfall-decreases-by-80-at-district-hospital/articleshow/77187718.cms (accessed March 16, 2022).
63. Al Masri A, Masannat M. Data Collection in COVID-19 Restrictions. (2020). Available online at: https://www.gage.odi.org/multimedia/data-collection-in-covid-19-restrictions/
64. APHRC Report- Data Collection Methods To Use During The Covid-19 Pandemic And Beyond. APHRC. (2021). Available online at: https://aphrc.org/blogarticle/data-collection-methods-to-use-during-the-covid-19-pandemic-and-beyond/ (accessed March 16, 2022).
65. Gourlay S, Kilic T, Martuscelli A, Wollburg P, Zezza A. Viewpoint: high-frequency phone surveys on COVID-19: good practices, open questions. Food Policy. (2021) 105:102153. doi: 10.1016/j.foodpol.2021.102153
66. Amaral S, Dinarte L, Dominguez-Rivera P, Perez-Vincent SM, Romero S. Talk or Text? Evaluating Response Rates by Remote Survey Method during COVID-19 (SSRN Scholarly Paper 4006505). (2022). doi: 10.2139/ssrn.4006505
67. Ballivian A, Azevedo JP, Durbin W. Using Mobile Phones for High-Frequency Data Collection. London: Ubiquity Press (2015).
68. Gibson DG, Wosu AC, Pariyo GW, Ahmed S, Ali J, Labrique AB, et al. Effect of airtime incentives on response and cooperation rates in non-communicable disease interactive voice response surveys: randomised controlled trials in Bangladesh and Uganda. BMJ Glob Health. (2019) 4:e001604. doi: 10.1136/bmjgh-2019-001604
69. Matías-Guiu J, Serrano-Castro PJ, Mauri-Llerda JÁ, Hernández-Ramos FJ, Sánchez-Alvarez JC, Sanz M. Analysis of factors influencing telephone call response rate in an epidemiological study. Sci World J. (2014) 2014:179375. doi: 10.1155/2014/179375
70. O'Toole J, Sinclair M, Leder K. Maximising response rates in household telephone surveys. BMC Med Res Methodol. (2008) 8:71. doi: 10.1186/1471-2288-8-71
71. Dabalen A, Etang A, Hoogeveen J, Mushi E, Schipper Y, von Engelhardt J. Mobile Phone Panel Surveys in Developing Countries: A Practical Guide for Microdata Collection. Washington, DC: World Bank (2016). Available online at: http://hdl.handle.net/10986/24595
72. Hersh S, Nair D, Komaragiri PB, Adlakha RK. Patchy signals: capturing women's voices in mobile phone surveys of rural India. BMJ Glob Health. (2021) 6:e005411. doi: 10.1136/bmjgh-2021-005411
73. India: Prepaid Mobile Subscribers by Telecom Circles 2022. Statista. (n.d.). Available online at: https://www.statista.com/statistics/639922/prepaid-mobile-subscribers-by-telecom-circles-india/ (accessed June 1, 2023).
74. Telecom Billing—Pre-Paid vs Post-Paid. (n.d.). Available online at: https://www.tutorialspoint.com/telecom-billing/prepaid-vs-postpaid.htm (accessed June 1, 2023).
75. Pratap A, Neto EC, Snyder P, Stepnowsky C, Elhadad N, Grant D, et al. Indicators of retention in remote digital health studies: a cross-study evaluation of 100,000 participants. Npj Digit Med. (2020) 3:1. doi: 10.1038/s41746-020-0224-8
76. Elliott R, Berman A, October 2020, S. L. // 12. Opinion: How to adapt to remote research methods in rapidly changing circumstances. Devex. (2020). Available online at: https://www.devex.com/news/sponsored/opinion-how-to-adapt-to-remote-research-methods-in-rapidly-changing-circumstances-98241 (accessed March 16, 2022).
77. Nass SJ Levit LA Gostin LO Institute Institute of Medicine (US) Committee on Health Research and the Privacy of Health Information: The HIPAA Privacy Rule. The Value, Importance, and Oversight of Health Research. In Beyond the HIPAA Privacy Rule: Enhancing Privacy, Improving Health Through Research. Washington, DC: National Academies Press (2009). doi: 10.17226/12458
78. The Need for Awareness of Clinical Research. National Institutes of Health (NIH). (2015). Available online at: https://www.nih.gov/health-information/nih-clinical-research-trials-you/need-awareness-clinical-research (accessed February 20, 2023).
79. Cornejo M, Bustamante J, Del Río M, De Toro X, Latorre MS. Researching with qualitative methodologies in the time of coronavirus: clues and challenges. Int J Qual Methods. (2023) 22:16094069221150110. doi: 10.1177/16094069221150110
80. Gailloux C, Furness WW, Myles CC, Wiley DS, Collins K. Fieldwork without the field: navigating qualitative research in pandemic times. Front Sustain Food Syst. (2022) 6:750409. doi: 10.3389/fsufs.2022.750409
81. Suslow A, Giehl C, Hergesell J, Vollmar HC, Otte IC. Conducting qualitative research under pandemic restrictions - considerations, challenges, and benefits: a methodological field report. Gesundheitswesen. (2023) 85(S 03):S189–96. doi: 10.1055/a-2129-6311
82. Uleanya C, Yu K. Data collection in times of pandemic: a self-study and revisit of research practices during a crisis. Sage Open. (2023) 13:21582440231160698. doi: 10.1177/21582440231160698
83. Improving health literacy. (n.d.). Available online at: https://www.who.int/activities/improving-health-literacy (accessed November 18, 2022).
84. Saiesha. Low Health Literacy in Developing Countries. The Borgen Project. (2021). Available online at: https://borgenproject.org/low-health-literacy/ (accessed November 18, 2022).
85. Cuthino FL, Sheilini M, Chandrababu R. The comparison of health literacy between health science and non-health science members-a cross sectional study of multifaceted public health affair. Clin Epidemiol Glob Health. (2021) 12:100893. doi: 10.1016/j.cegh.2021.100893
86. Benjamin RM. Improving health by improving health literacy. Public Health Rep. (2010) 125:784–5. doi: 10.1177/003335491012500602
87. Murthy P. Health Literacy and Sustainable Development. United Nations UN Chronicle; United Nations (n.d.). Available online at: https://www.un.org/en/chronicle/article/health-literacy-and-sustainable-development (accessed November 18, 2022).
88. Health Literacy around the World: Policy Approaches to Wellbeing through Knowledge and Empowerment. (n.d.). Available online at: https://impact.economist.com/perspectives/sites/default/files/lon__es__health_literacy_paper_v8_0.pdf (accessed November 19, 2022).
89. Levin-Zamir D, Leung AYM, Dodson S, Rowlands G. Health literacy in selected populations: individuals, families, and communities from the international and cultural perspective. Inf Serv Use. (2017) 37:131–51. doi: 10.3233/ISU-170834
90. Lynch MA-M, Franklin GV, Lynch MA-M, Franklin GV. Health literacy: an intervention to improve health outcomes. In:Mullings J, Thoms-Rodriguez C-A, McCaw-Binns AM, Paul T, , editors. Strategies to Reduce Hospital Mortality in Lower and Middle Income Countries (LMICs) and Resource-Limited Settings. London: IntechOpen (2019).
91. Mathias EG, Dhyani VS, Krishnan JB, Rani U, Gudi N, Pattanshetty S. Community based health literacy interventions in India: a scoping review. Clin Epidemiol Glob Health. (2023) 22:101310. doi: 10.1016/j.cegh.2023.101310
92. Singleton K, Krause E. Understanding cultural and linguistic barriers to health literacy. Online J Issues Nurs. (2009) 14. doi: 10.3912/OJIN.Vol14No03Man04
93. Fontaine G, Maheu-Cadotte M-A, Lavallée A, Mailhot T, Rouleau G, Bouix-Picasso J, et al. Communicating science in the digital and social media ecosystem: scoping review and typology of strategies used by health scientists. JMIR Public Health Surveill. (2019) 5:e14447. doi: 10.2196/14447
94. Rudd RE. A call for more rigor in science and health communication. Int J Environ Res Public Health. (2022) 19:1825. doi: 10.3390/ijerph19031825
95. Sacristán JA, Aguarón A, Avendaño-Solá C, Garrido P, Carrión J, Gutiérrez A, et al. Patient involvement in clinical research: why, when, and how. Patient Prefer Adherence. (2016) 10:631–40. doi: 10.2147/PPA.S104259
96. Townsend A, Cox SM. Accessing health services through the back door: a qualitative interview study investigating reasons why people participate in health research in Canada. BMC Med Ethics. (2013) 14:40. doi: 10.1186/1472-6939-14-40
97. Matta G. Science communication as a preventative tool in the COVID19 pandemic. Humanit Soci Sci Commun. (2020) 7:1. doi: 10.1057/s41599-020-00645-1
98. Meherali S, Punjani NS, Mevawala A. Health literacy interventions to improve health outcomes in low- and middle-income countries. Health Lit Res Pract. (2020) 4:e251–66. doi: 10.3928/24748307-20201118-01
99. Malik M. Health literacy as a global public health concern: a systematic review. J Pharmacol Clin Res. (2017) 4. doi: 10.19080/JPCR.2017.04.555632
100. Kickbusch I, Pelikan JM, Apfel F, Tsouros AD. Health Literacy: The Solid Facts. World Health Organization. Regional Office for Europe. (2013). Available online at: https://apps.who.int/iris/handle/10665/326432 (accessed Jun 1, 2023).
101. Rasu RS, Bawa WA, Suminski R, Snella K, Warady B. Health literacy impact on national healthcare utilization and expenditure. Int J Health Policy Manag. (2015) 4:747–55. doi: 10.15171/ijhpm.2015.151
102. Jain E. India's Digital Health Mission: The Growing Need to Introduce Electronic Health Records. (2021). Available online at: https://www.orfonline.org/expert-speak/indias-digital-health-mission/ (accessed November 19, 2022).
103. Al Meslamani AZ. Technical and regulatory challenges of digital health implementation in developing countries. J Med Econ. (2023) 26:1057–60. doi: 10.1080/13696998.2023.2249757
104. Harahap NC, Handayani PW, Hidayanto AN. Barriers and facilitators of personal health record adoption in Indonesia: health facilities' perspectives. Int J Med Inform. (2022) 162:104750. doi: 10.1016/j.ijmedinf.2022.104750
105. Kaboré SS, Ngangue P, Soubeiga D, Barro A, Pilabré AH, Bationo N, et al. Barriers and facilitators for the sustainability of digital health interventions in low and middle-income countries: a systematic review. Front Digit Health. (2022) 4:1014375. doi: 10.3389/fdgth.2022.1014375
106. Whitelaw S, Pellegrini DM, Mamas MA, Cowie M, Van Spall HGC. Barriers and facilitators of the uptake of digital health technology in cardiovascular care: a systematic scoping review. Eur Heart J Digit Health. (2021) 2:62–74. doi: 10.1093/ehjdh/ztab005
107. Electronic Prescribing Systems. (2022). Available online at: https://ww2.health.wa.gov.au/Articles/A_E/Electronic-Prescribing-Systems (accessed November 19, 2022).
108. Lanham AE, Cochran GL, Klepser DG. Electronic prescriptions: opportunities and challenges for the patient and pharmacist. Adv Health Care Technol. (2016) 2:1–11. doi: 10.2147/AHCT.S64477
109. Singh A, Yadav M, Sharma A, Mishra A, Prakash A, Medhi B, et al. E-Prescription (CPOE) in Indian Hospitals: A Strategy To Prevent Prescription Errors. (2020).
110. Shanker KS. Govt. Hospital prescriptions a puzzle for many patients—The Hindu. (2022). Available online at: https://www.thehindu.com/news/national/telangana/govt-hospital-prescriptions-a-puzzle-for-many-patients/article65476444.ece (accessed November 19, 2022).
111. Wang SJ, Middleton B, Prosser LA, Bardon CG, Spurr CD, Carchidi PJ, et al. A cost-benefit analysis of electronic medical records in primary care. Am J Med. (2003) 114:397–403. doi: 10.1016/S0002-9343(03)00057-3
112. MacDermod C, Pettie MA, Carrino EA, Garcia SC, Padalecki S, Finch JE, et al. Recommendations to encourage participation of individuals from diverse backgrounds in psychiatric genetic studies. Am J Med Genet B Neuropsychiatr Genet. (2022) 189:163–73. doi: 10.1002/ajmg.b.32906
113. Limkakeng AT, Oliveira LLHde, Moreira T, Phadtare A, Rodrigues CG, Hocker MB, et al. Systematic review and metasummary of attitudes toward research in emergency medical conditions. J Med Ethics. (2014) 40:401–8. doi: 10.1136/medethics-2012-101147
114. Warburton J, Dyer M. Older volunteers participating in a university research registry: helping others my age. Educ Gerontol. (2004) 30:367–81. doi: 10.1080/03601270490433567
115. Davies, N. How to Overcome the Challenges of Doing Research during COVID-19. Institute of Development Studies. (2021). Available online at: https://www.ids.ac.uk/opinions/how-to-overcome-the-challenges-of-doing-research-during-covid19/ (accessed November 19, 2022).
116. Ebola-WHO Update. (2022). Available online at: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON425 (accessed April 11, 2023).
117. Influenza-WHO Update. (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) (accessed April 11, 2023).
118. Monkeypox-WHO Update. (2022). Available online at: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON396 (accessed April 11, 2023).
119. Nipah-WHO Update. (2023). Available online at: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON442 (accessed April 11, 2023).
120. Zika-WHO Update. (2021). Available online at: https://www.who.int/emergencies/disease-outbreak-news/item/zika-virus-disease-india (accessed April 11, 2023).
Keywords: COVID-19, field research, remote research, telephonic survey, digital health, LMICs
Citation: Mulchandani R, Lyngdoh T, Gandotra S, Isser HS, Dhamija RK and Kakkar AK (2024) Field based research in the era of the pandemic in resource limited settings: challenges and lessons for the future. Front. Public Health 12:1309089. doi: 10.3389/fpubh.2024.1309089
Received: 07 October 2023; Accepted: 30 January 2024;
Published: 29 February 2024.
Edited by:
Adam Wilcox, Washington University in St. Louis, United StatesReviewed by:
Erwin Calgua, Universidad de San Carlos de Guatemala, GuatemalaKylie McCullough, Edith Cowan University, Australia
Copyright © 2024 Mulchandani, Lyngdoh, Gandotra, Isser, Dhamija and Kakkar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ashish Kumar Kakkar, ZHJhc2hpc2hrYWtrYXJAZ21haWwuY29t
 Rubina Mulchandani
Rubina Mulchandani Tanica Lyngdoh3
Tanica Lyngdoh3 Sheetal Gandotra
Sheetal Gandotra Rajinder K. Dhamija
Rajinder K. Dhamija Ashish Kumar Kakkar
Ashish Kumar Kakkar