- 1Non-communicable Diseases Research Center, Alborz University of Medical Sciences, Karaj, Iran
- 2Department of Epidemiology, School of Public Health, Iran University of Medical Sciences, Tehran, Iran
- 3Research Unit of General Practice, Department of Public Health, University of Southern Denmark, Odense, Denmark
- 4Obesity and Eating Habits Research Center, Endocrinology and Metabolism Clinical Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
- 5Endocrinology and Metabolism Research Center, Endocrinology and Metabolism Clinical Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
- 6Department of Epidemiology and Biostatistics, Tehran University of Medical Sciences, Tehran, Iran
- 7Deputy of Research & Technology, Ministry of Health & Medical Education, Tehran, Iran
- 8School of Public Health and Preventive Medicine, Monash University, Melbourne, VIC, Australia
- 9Baker Heart and Diabetes Institute, Melbourne, VIC, Australia
- 10Chronic Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
Background: With the rapid increase in the prevalence of DM, studies on the awareness, treatment, and control of this condition are essential. Therefore, this study aimed to review the literature and pool the awareness, treatment, and control of diabetes at the global, regional, and national levels.
Methods: In this systematic review and meta-analysis, several databases, including MEDLINE/PubMed, Institute of Scientific Information (ISI), Scopus, and Google Scholar, were searched using appropriate keywords up to June 2022. Observational studies investigating the awareness, treatment, and control of glucose levels among diabetic individuals were included. Awareness, treatment, and control were defined as the proportion of participants who were aware of their diabetes condition, treated pharmacologically, and achieved adequate glucose control, respectively. Two investigators independently conducted the study selection, data extraction, and quality assessment. Heterogeneity among studies was calculated using Chi-square, and a random-effect meta-analysis was used to pool the rates.
Results: A total of 233 studies published between 1985 and 2022 met the inclusion criteria. The included studies had a combined population of 12,537,968. The pooled awareness of DM was 60% (95%CI: 56–63) and ranged from 41% (25–57) in low-income countries to 68% (64–72) in high-income countries, with no significant trend observed over the assessed periods at the global level. The pooled treatment of DM globally was 45% (42–48) and varied from 37% (31–43) in lower-middle-income countries to 53% (47–59) in high-income countries, showing variation over the examined time period. Before 2000, the proportion of adequate DM control was 16% (12–20), which significantly improved and reached 22% (19–25) after 2010. The pooled awareness, treatment, and control of DM were higher in females, high-income countries, and urban areas compared to males, upper and lower-middle-income countries, and rural areas, respectively. The older adults population had higher awareness and treatment rates than the adult population, but their DM control did not differ significantly.
Conclusion: Despite the high level of awareness and treatment among the diabetic population, treatment success (control) is considerably low, particularly in low-income countries and rural areas. It is crucial to improve awareness, treatment, and control by strengthening the primary care system in all countries.
Introduction
Type 2 diabetes mellitus (DM) is a metabolic disorder and a major risk factor for many other diseases, resulting in both long-term and short-term complications. Diabetes, along with its associated complications, can lead to mortality and severe morbidity (1). In 1980, the number of people aged 18–99 years with diabetes was 108 million, which increased to 451 million in 2017. Unfortunately, these numbers are projected to increase to 693 million by 2045. The prevalence of diabetes has been rapidly increasing, especially in low- and middle-income countries. Additionally, the burden, treatment, and costs of DM and its complications are increasing at a fast pace (2).
Education on the early signs of diabetes, along with effective screening programs, is crucial in identifying DM in its early stages. This results in increased awareness, timely treatment, and a significant reduction in diabetes complications (3). The treatment options for diabetes vary based on several factors, including the severity and duration of DM, individual circumstances, and the level of social disadvantage. These options range from inexpensive dietary and lifestyle changes in the early stages to the use of expensive multiple glucose-lowering medications and insulin treatment in the later stages of the disorder (4–6). Therefore, if managed appropriately, diabetes could lead to significantly fewer complications, premature deaths, and less burden on the government and healthcare system (7).
With the rapid increase in the prevalence of DM, studies on the awareness, treatment, and control of this condition are essential to illuminate a path for governments and public health officials worldwide to manage this illness more effectively. There have been no systematic reviews and meta-analyses based on individual patient data (IPD) or aggregated data on a global scale over the past few years. Thus, this study aimed to examine the long-term awareness, treatment, and control of DM in the general population at the national, regional, and global levels.
Material and methods
This systematic review and meta-analysis was conducted following the guidelines outlined in the Cochrane Handbook for Systematic Reviews of Interventions (8). Furthermore, the study’s findings were reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement (9).
Search strategy
Several international databases, including MEDLINE/PubMed, the Institute of Scientific Information (ISI), Scopus, and Google Scholar, were searched up until June 2022. The search strategy was developed based on the outcomes (awareness, treatment, and control of diabetes). The databases were searched using keywords such as “diabetes,” “awareness,” “treatment,” and “control,” along with related keywords based on each database’s search strategy. The search strategy in the selected databases is presented in Supplementary Appendix Table 1. Additionally, the reference lists of the included articles were manually searched. The search results from all databases were imported into EndNote software, and duplicate studies were removed. The search was conducted by one researcher and approved by a second researcher, following the search strategy.
Eligibility criteria
All cross-sectional studies that investigated the awareness, treatment, and control of glucose levels among individuals with diabetes were included. Studies with the following characteristics were excluded: (1) participants below 18 years old, (2) type 1 diabetes, (3) non-English studies, and 4) case reports, case series, and letters to the editor studies. If a study did not specify the type of study, it was still included.
Definition of outcomes
DM was defined as having fasting blood sugar (FBS) above the cutoff level specified by the studies, a self-reported previous diagnosis of DM by a healthcare professional, or being on pharmacological treatment for DM. Awareness was defined as the proportion of participants who were aware of their condition with DM. Treatment was defined as the proportion of participants who were treated with medication due to having DM (adherence to treatment). Control was defined as the proportion of participants whose DM was adequately controlled. Control was calculated using two types of denominators: control among all diabetic individuals or DM control among treated diabetic individuals.
Data extraction
Two researchers independently extracted the data using an electronic data extraction form. The following characteristics and outcomes of the included studies were extracted: first author, year of publication, country, study design, living area (urban or rural), sample size, gender, age (mean ± standard deviation (SD) or range), definition of diabetes, awareness, treatment, and DM control, along with their 95% confidence interval (CI). Any disagreements between the two researchers were resolved through discussion or with the involvement of a third researcher.
Quality assessment (Q.A)
The Newcastle–Ottawa scale for cross-sectional studies was used to assess the quality of the included studies. This scale evaluates eight items in three main domains: selection, comparability, and outcome. The Q.A score, which is the sum of the scores of each item, ranges from 0 to 10. Higher scores indicate a lower risk of bias. On this scale, low-quality studies with a high risk of bias were assigned scores ranging from 0 to 3, middle-quality studies with a medium risk of bias were assigned scores from 4 to 6, and high-quality studies with a low risk of bias were assigned scores from 7 to 10. Any disagreements between the two researchers regarding the Q.A score were resolved through discussion or with the involvement of a third researcher.
Statistical analysis
The estimates were pooled using the “Metaprop” command in Stata. Heterogeneity among the studies was assessed using chi-square-based Q-tests. If heterogeneity was statistically significant, a random-effects model was used; otherwise, a fixed-effects model was used. Subgroup analyses were conducted based on gender, study population (adult/older adults), country income (classified according to the World Bank’s Classification) (10), living area (urban or rural), and Q.A score. All analyses were stratified by time periods (before 2000, 2001–2010, and after 2010). Meta-regression was performed to identify the source of heterogeneity among studies. Stata 17 (Copyright Stata Corp., LP, United States) was used for the meta-analysis. All figures were generated using R version 4.1.3 statistical software.
Role of the funding source
The funding body had no involvement in the preparation, investigation, design, interpretation of the findings, or drafting of the study.
Results
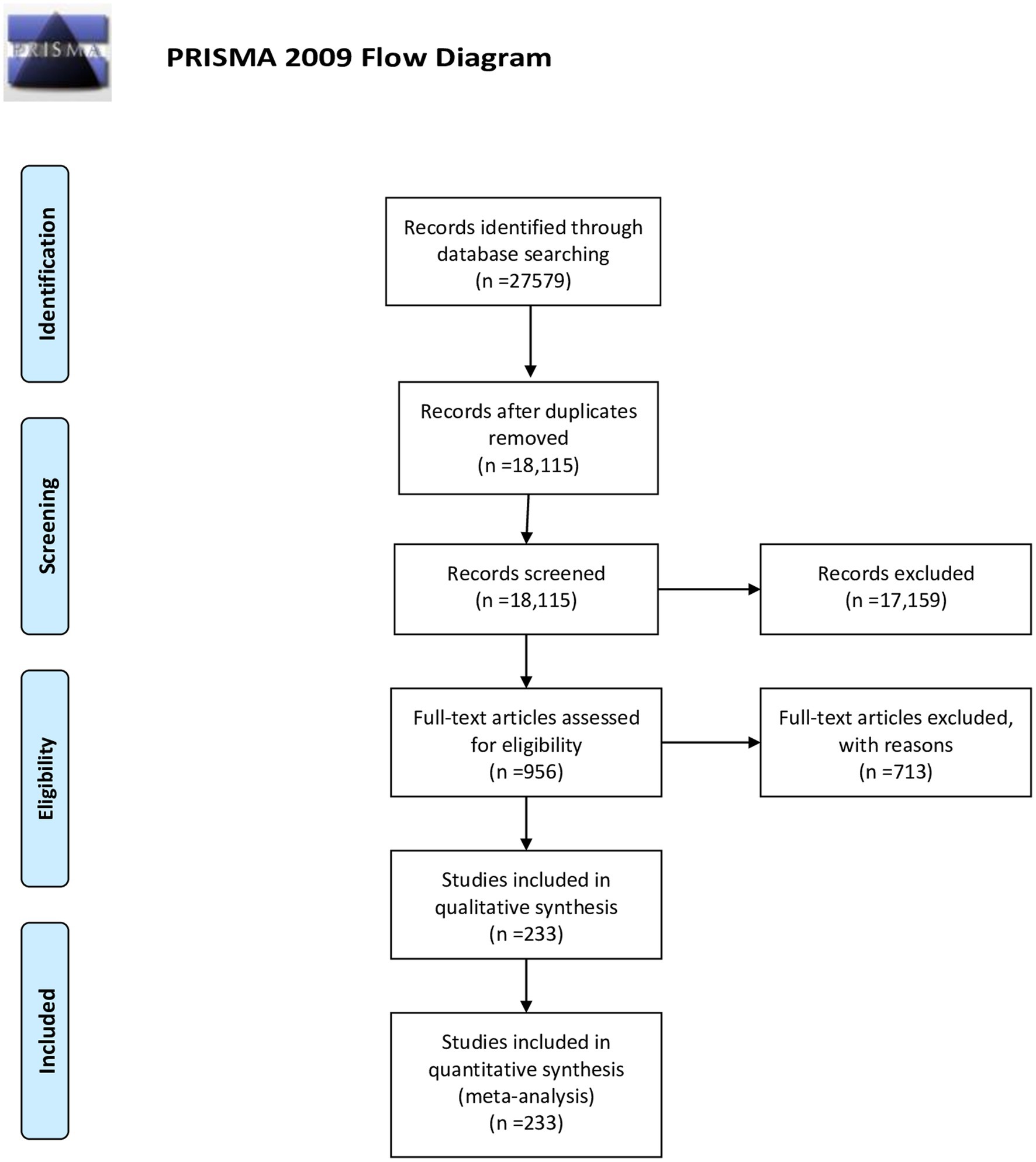
A total of 27,579 documents were retrieved from the search across all databases. After removing duplicate and irrelevant studies based on titles, abstracts, and full texts, 953 studies were reviewed for eligibility criteria. Finally, 233 studies met the inclusion criteria for qualitative and quantitative analyses (11–242). The study selection process is illustrated in Figure 1.
Qualitative synthesis
The characteristics of the included studies and the reported awareness, treatment, and control of DM are presented in Supplementary Appendix Table 2. These studies were published between 1985 and 2022 and encompassed 84 countries and 2 regions (the Southern Cone of Latin America and South Asia). The majority of studies were conducted in China (34 studies), the United States (20 studies), Iran (15 studies), and India (13 studies). The combined total population of all included studies was 12,537,968, with a mean age of 48.7 (SD 10) among the participants. The highest reported levels of awareness, treatment, and control were observed in China (92%), the United States of America (87%), and China (76%), respectively.
Quantitative synthesis
Heterogeneity
A significant level of heterogeneity was observed among the included studies regarding awareness, treatment, and control of DM (p-value <0.001). Therefore, the random-effects model was used to pool the proportions.
Global level awareness, treatment, and control of DM
Figures 2–5 present the pooled awareness, treatment, and control rates stratified by gender, study population, living area, and country’s income. The pooled awareness and treatment rates at the global level were 60% (95% CI: 56–63) and 45% (95% CI: 42–48), respectively. The proportion of DM control among all diabetic individuals was 20% (95% CI: 18–22), while among those receiving treatment, it was 42% (95% CI: 39–44).
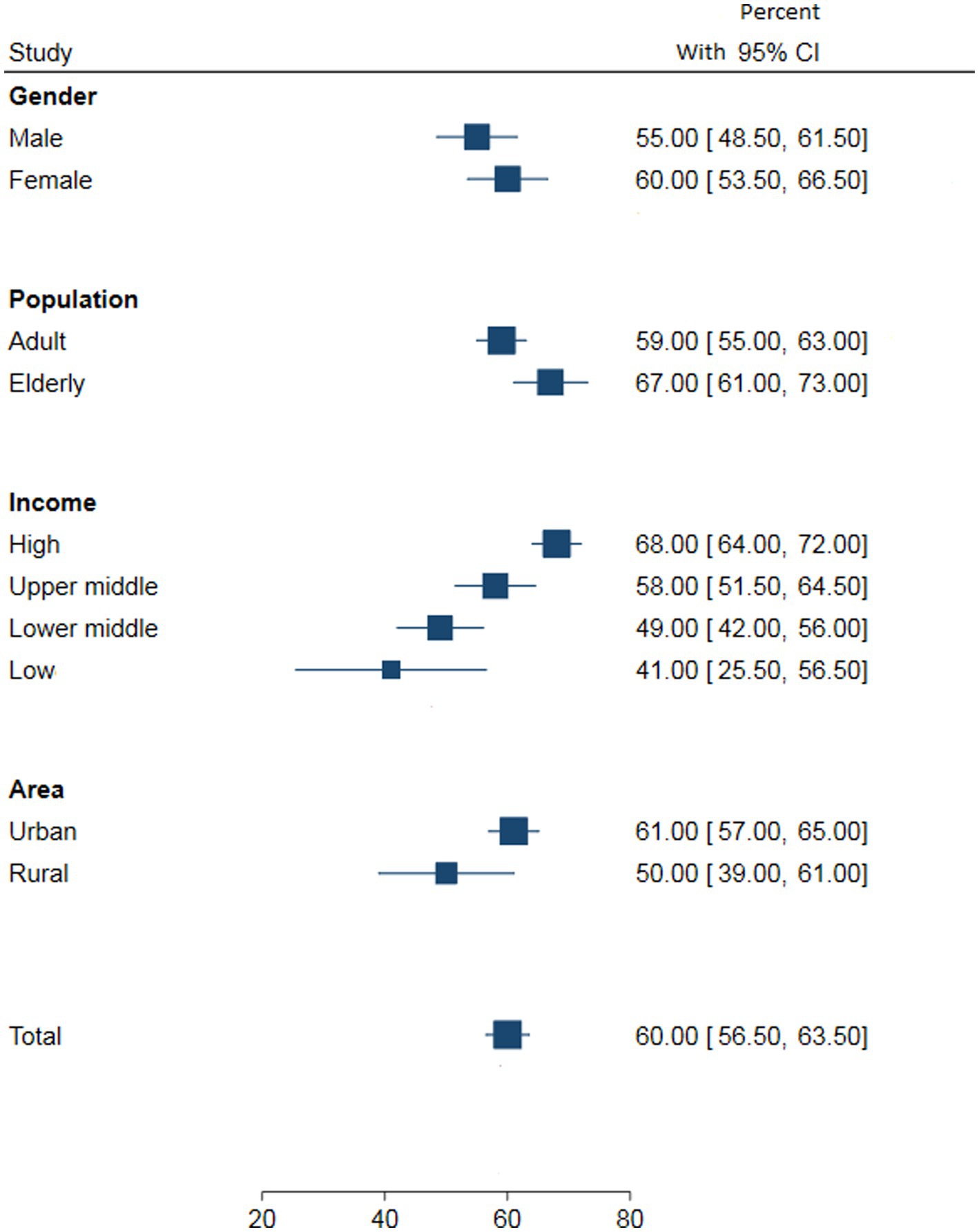
Figure 2. The pooled DM awareness by gender, study population, country’s income and living area at the global level.
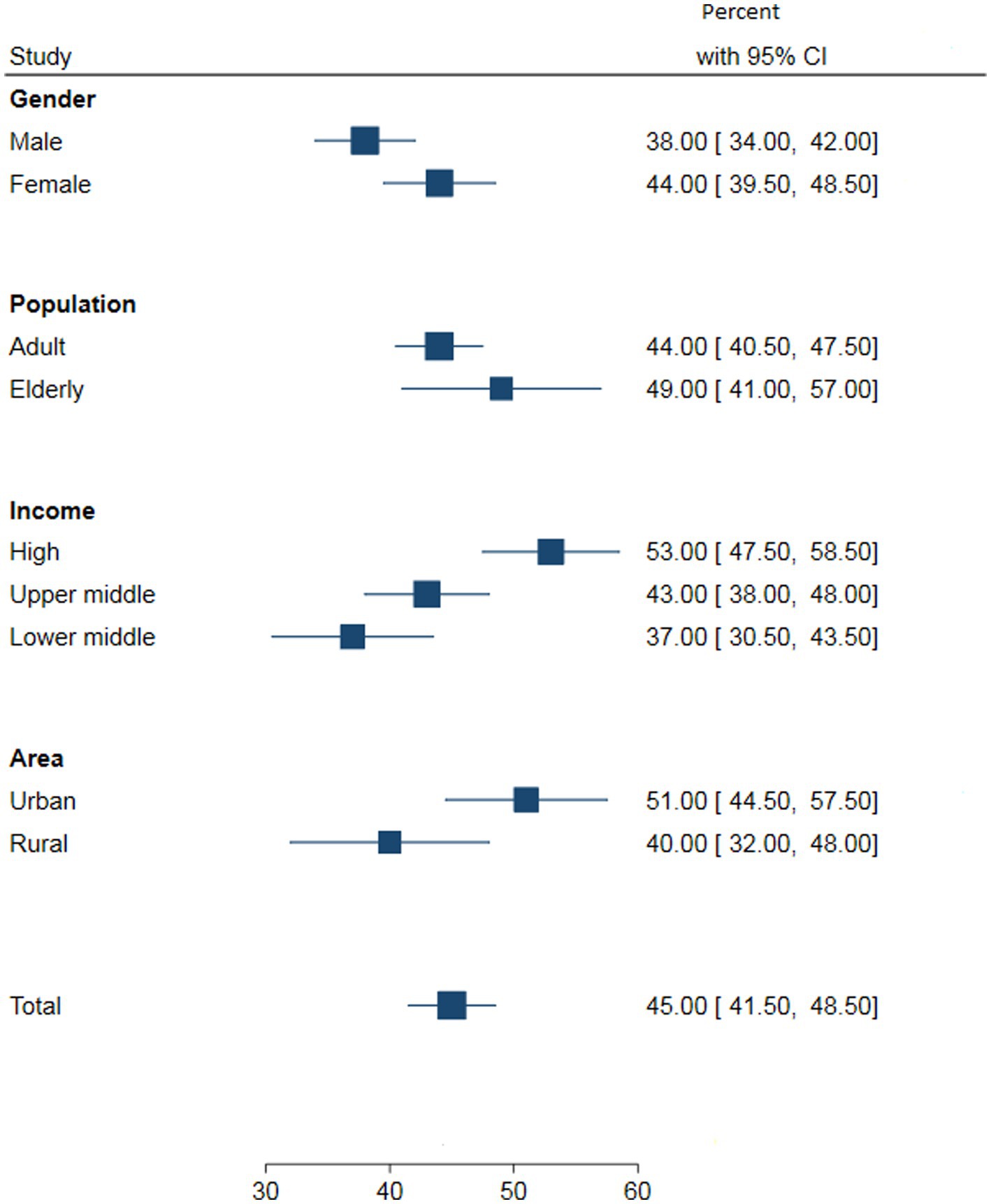
Figure 3. The pooled DM treatment by gender, study population, country’s income and living area at the global level.
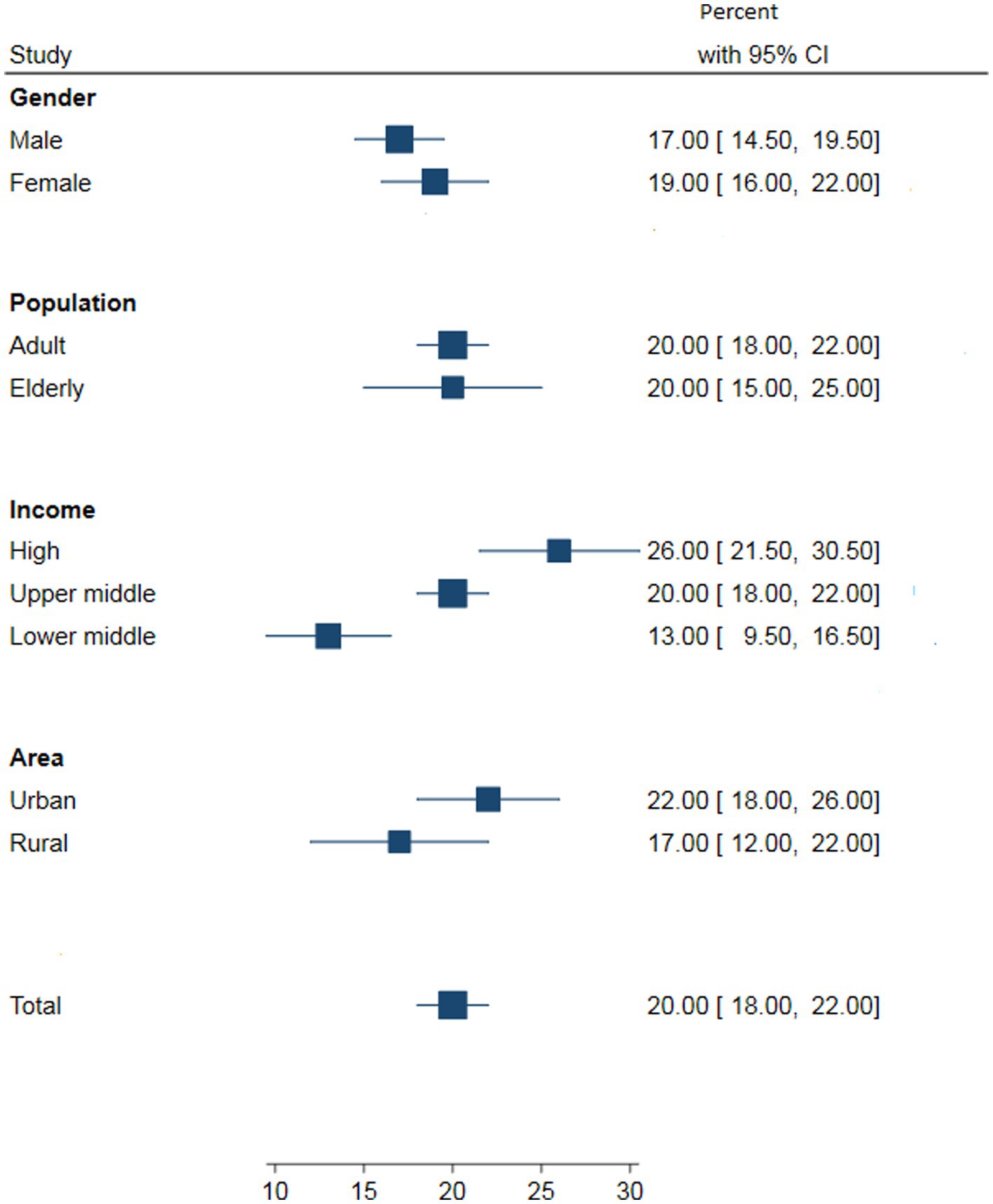
Figure 4. The pooled DM control by gender, study population, country’s income and living area among all the diabetic individuals at the global level.
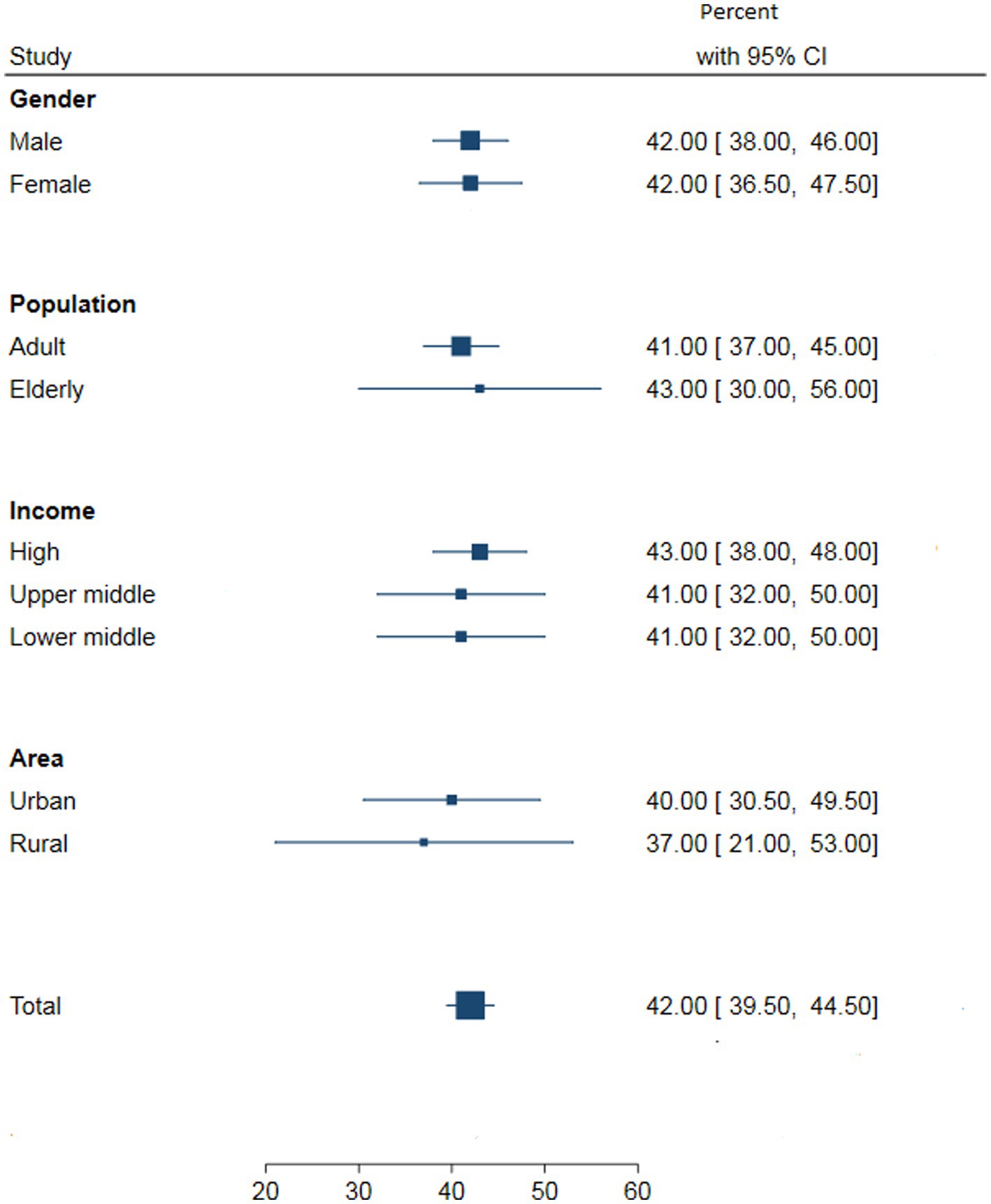
Figure 5. The pooled DM control by gender, study population, country’s income and living area among those receiving treatment at the global level.
Awareness, treatment, and control of DM by the time period
Table 1 displays the meta-analysis results for the pooled estimates of awareness, treatment, and control of DM according to three study periods. Although the awareness of diabetes showed a decreasing trend across the three study periods, it was not statistically significant (before 2000: 61% (95% CI: 56, 66); 2000 to 2010: 60% (95% CI: 53, 66); after 2010: 59% (95% CI: 54, 64)). In all three periods, female subjects had higher awareness compared to male subjects. Awareness also increased with income level and was higher in urban and older adults populations compared to rural and adult populations, respectively.
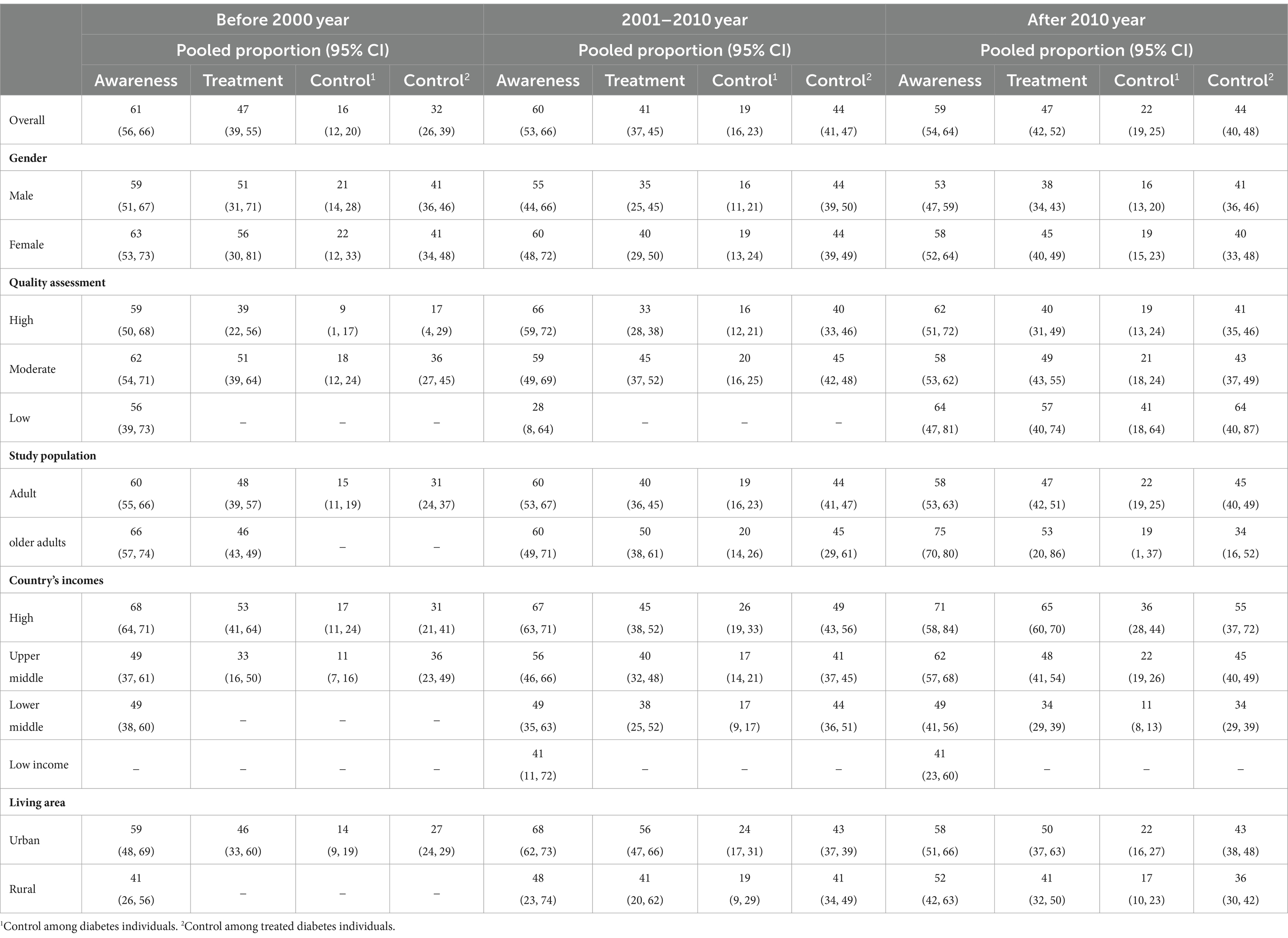
Table 1. The proportion of awareness, treatment and control of diabetes according to gender, quality assessment, population, country incomes and study area.
Regarding treatment, the pooled proportions were equal in the first and third study periods (47%). However, treatment rates increased from the second to the third period (41 to 47%). More women received treatment for diabetes than men in all three periods. Treatment rates were higher in high-income countries compared to upper- and lower-middle-income countries based on the country’s income. Additionally, treatment rates were higher in urban and older adults populations compared to rural and adult populations, respectively.
Among all diabetic individuals, the proportion of people with adequate DM control increased across the three periods (before 2000: 16%; 2000 to 2010: 19%; after 2010: 22%). The proportion of women with adequate DM control was higher than that of men. Based on the country’s income, high-income countries had significantly higher proportions of adequate DM control compared to upper- and lower-middle-income countries in all three periods. In terms of living area, urban populations had higher proportions of adequate DM control compared to rural populations. The reported proportions of adequate DM control were somewhat higher in the adult population compared to the older adults population in the third period, but almost the same in the second period.
The proportion of adequate DM control among treated diabetic individuals increased across the three periods (before 2000: 32%; 2000 to 2010: 44%; after 2010: 44%). There were no significant differences in diabetes management between men and women who were treated. The proportion of adequate DM control among those receiving treatment was significantly higher in high-income countries compared to upper- and lower-middle-income countries in the second and third periods. However, in the first period, this proportion was higher in upper-middle-income countries compared to high- and lower-middle-income countries. Urban populations had higher proportions of adequate DM control among treated individuals compared to rural populations. The reported proportion of adequate DM control among treated individuals was somewhat higher in the adult population compared to the older adults population in the third period, but almost the same in the second period.
The awareness, treatment, and control of DM at the regional level (Figure 6) illustrates the regional-level awareness, treatment, and control of DM according to sex and time period. The highest awareness rates in male and female subjects were observed in the North American region, with proportions of 83 and 73% in the first and second studied periods, respectively. From 2001 to 2010, the highest awareness in male subjects was reported in Europe (66%), while in female subjects, it was estimated in North America (70%). After 2010, the highest awareness rates in male and female subjects were observed in Europe, with 71 and 78%, respectively.
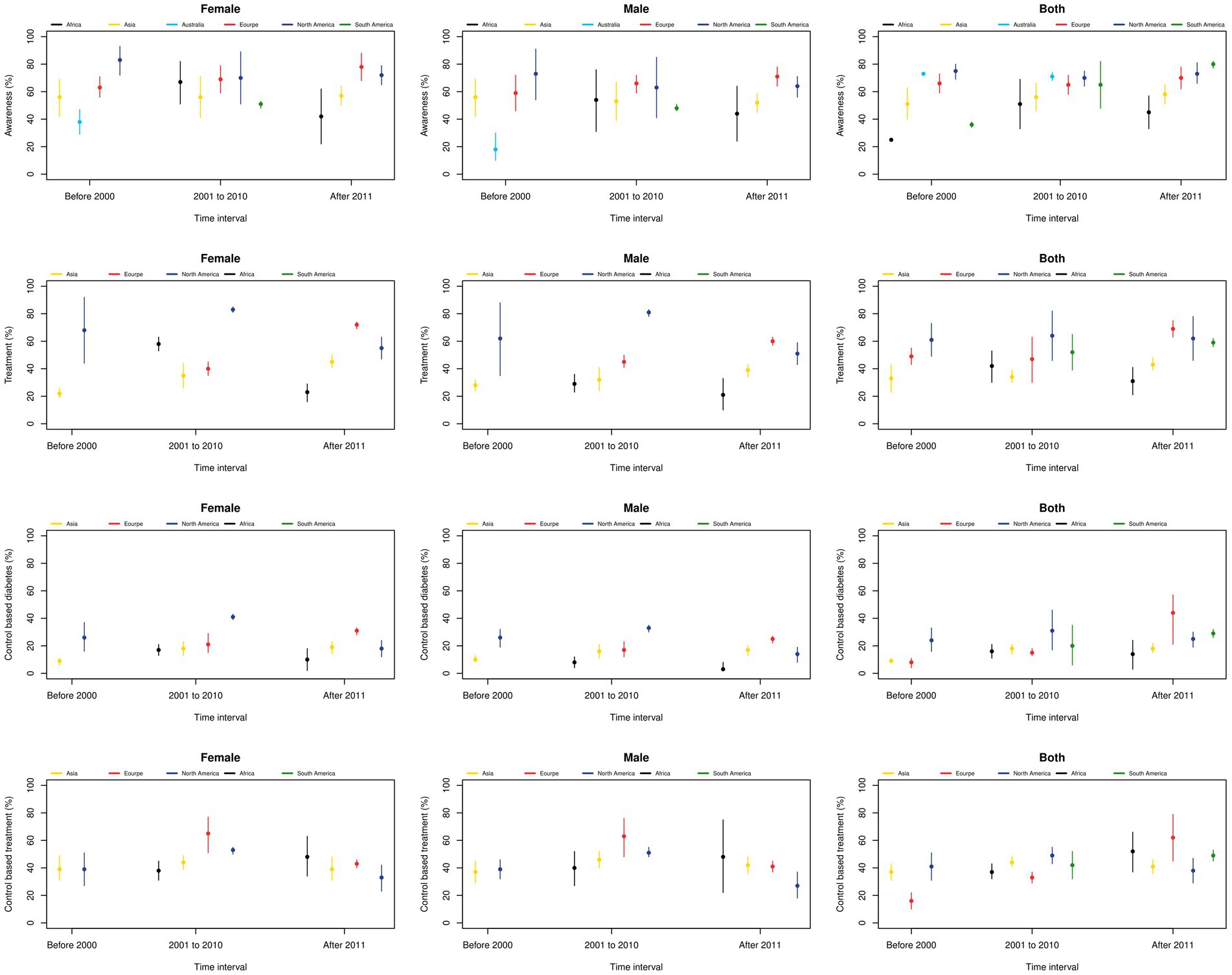
Figure 6. DM awareness, treatment, and control according to gender and time period at the regional level.
Regarding treatment, the highest rates in both genders in the first and second studied periods were observed in North America (61 and 64%, respectively) and in Europe (69%) after 2010. By sex, the highest treatment rates in women were seen in North America (68, 83, and 55% in the three time periods, respectively), and in men in North America (62, 81%) in the first and second periods, and in Europe (60%) in the third period.
The highest proportion of adequate DM control among all diabetic individuals in the first and second periods was seen in North America, with proportions of 24 and 31%, respectively, and in Europe, with 44% in the third period. Moreover, the sex-stratified meta-analysis shows that the highest proportion of adequate DM control among women was seen in North America in the first (26%) and second (41%) periods, and in Europe (31%) in the third period. Among those using glucose-lowering treatments, both genders showed that North America had the highest control rates in the first and second studied periods, with proportions of 41 and 49%, respectively. However, after 2010, Europe had the highest proportion of adequate DM control (62%). The highest proportion of adequate DM control among women treated for diabetes was seen in Asia, followed by Europe and Africa during the three studied periods, respectively. For men, the highest proportion of adequate DM control was observed in North America, followed by Europe and then Africa in the third studied period.
The awareness, treatment, and control of DM at the national level
The highest awareness rates among women were seen in the United States (83%), followed by Turkey (91%), and Mauritania (87%) during the three studied periods (Supplementary Appendix Figure 1). The highest awareness rates in men were observed in England (78%), South Africa (84%), and Mauritania (91%), during the three studied periods (Supplementary Appendix Figure 2).
The highest treatment rates in women were observed in the United States in the first and second periods, with proportions of 68 and 83%, respectively, and in France with a proportion of 82% in the third period (Supplementary Appendix Figure 3). In men, the highest treatment rates were seen in the United States in the first and second studied periods, with proportions of 62 and 81%, respectively, and in Nepal with a proportion of 65% in the third period (Supplementary Appendix Figure 4).
The highest proportion of adequate DM control among all diabetic women was seen in the United States, with proportions of 26 and 41% in the first two studied periods, respectively, and in Iran with a 31% proportion in the third decade (Supplementary Appendix Figure 5). In men, the highest proportion of adequate DM control was reported in the United States in the first and second studied periods (26 and 33%, respectively), and in Iran in the last period (25%) (Supplementary Appendix Figure 6).
The highest proportion of adequate DM control among treated women was seen in Guinea (43%), Italy (65%), and Angola (83%) during the three studied periods (Supplementary Appendix Figure 7). For men, the highest proportion was observed in the United States (39%), Italy (63%), and Cameroon (67%) during the three studied periods (Supplementary Appendix Figure 8).
Discussion
To the best of our knowledge, this systematic review and meta-analysis is the first comprehensive study to estimate the global proportion of people with DM who are aware of their condition, receiving treatment, and achieving adequate control of their glucose levels. The pooled proportion of people with diabetes who are aware of their disease was 60%, varying from 41% in low-income countries to 68% in high-income countries. The proportion of people with diabetes who were on treatment was 45%, ranging from 37 to 53% in different countries. Besides, we observed that diabetes management was adequate only in 16% of patients before 2000 and 22% after 2010. It should be noted that we observed a high variation in the reported proportions among different countries (85, 145, 196). This variation could be attributed to methodological differences, as well as the variety of age, characteristics, lifestyle, and economic status of the participants, and the screening practices of the healthcare systems.
Despite the progress in the accuracy of diagnostic methods, the trend in the proportion of people who were aware of their diabetes was surprisingly low, even in developed countries. Assessing diabetes awareness in the Latin America region showed that only 50% of patients were aware of their diseases. Considering that the prevalence of diabetes continues to increase across these countries, more comprehensive diabetes assessments in national surveys have been suggested (243). Moreover, a meta-analysis regarding diabetes trends in China from 1979 to 2012 showed that there was no obvious improvement in awareness of diabetes despite an increase observed in diabetes prevalence (244) This highlights that extra efforts should be made to increase screening for diabetes in communities. This finding was concordant with previous studies, which show a trend in awareness of other NCDs such as hypertension over the past three decades (245, 246).
Regarding the trend in treatment proportions, the pooled proportions illustrating the ratio of diabetic individuals under treatment did not differ significantly from the first studied period to the last. It should be noted that during these years, the diagnostic thresholds for diabetes diagnosis changed, leading to a decrease in the proportion of people with diabetes who were treated. Additionally, improved screening methods and public education efforts resulted in a larger proportion of previously undiagnosed individuals being recognized. Despite this increase in the number of individuals with diabetes, treatment proportions did not differ significantly, suggesting that treatment rates have improved across these three periods.
The difference between diabetes awareness and treatment emphasizes that converting knowledge to change in behavior and performance is difficult and time-consuming. According to the transtheoretical model, changing a behavior is a process with five stages: precontemplation, contemplation, preparation, action, and maintenance. Applying this model could be effective in the prevention and control of chronic diseases (247). Moreover, it should be noted that the motivation for treatment adherence can be influenced by factors such as the absence of adverse symptoms, family support, cost of medication, lack of resources, polypharmacy and complexity of medications, poor health literacy, and other social and financial barriers that should be investigated in different countries (248).
Moreover, over the three study periods, the pooled proportion of individuals with adequate DM control improved from 16 to 22%. These improvements in adequate DM control could be attributed to the utilization of the public health system, better access to physicians and healthcare facilities, and advancements in anti-diabetic agents.
Approximately 40% of all individuals with diabetes were undiagnosed, and only one-fifth of these individuals managed to achieve adequate blood glucose control. Early screening for diabetes is crucial, as it can lead to easier management and a reduction in subsequent chronic complications and related economic losses. Therefore, the healthcare infrastructure for diabetes screening and easy access to health services are of paramount importance (26). Additionally, there is a need to improve perceptions regarding medication adherence, as studies have shown that health insurance positively affects adherence to pharmacological treatment (243). Policy-making in this regard should be prioritized. In this regard, a systematic review examined the health system-level factors affecting diabetes awareness, treatment, adherence, and control and showed that financial constraints on patients and limited access to health services and medication were the main barriers. Task-sharing with pharmacists in care delivery and improvement of education programs led by healthcare professionals were two proposed solutions in this systematic review (249).
Overall, in the current study, awareness, treatment, and control of DM were found to be higher in women, the older adults, urban areas, and high-income countries. Consistent with previous studies, our findings indicate that women are more likely to be aware of their diabetes, receive treatment, and achieve better glycemic control than men, possibly due to their higher level of health concern compared to men (250). However, it is important to note that sociocultural factors may also influence these disparities (15). Furthermore, the older adults population tends to have higher awareness and treatment rates compared to other age groups, which may be attributed to their increased health consciousness (24). On the other hand, living in rural areas was associated with lower awareness, treatment, and adequate control of DM, likely due to limited access to healthcare services and a lack of knowledge (251). This aligns with a population-based study conducted in Chinese rural areas, which also reported increasing trends of awareness, treatment, and control with age (31). Additionally, populations in high-income countries demonstrate better awareness and management of diabetes, potentially due to higher education levels, better socioeconomic status, and improved access to treatment (252, 253). Evidence suggests that diabetes awareness increases significantly with education and academic level (15).
The low proportion of adequate DM control and the gap between diagnosis and treatment can be attributed to various factors, such as low adherence to therapeutic regimes due to multiple medications, inadequate access to healthcare services, and insufficient health insurance coverage for medications (254, 255). These factors should be considered in international and national health policy-making.
Considering the large burden of diabetes, it is of critical importance to understand diabetes management status, and this comprehensive systematic review and meta-analysis plays an important role in this regard. Moreover, assessing the changing trend of these proportions during the past decades is essential.
Limitations and strength
This study has some limitations. First, although the term ‘treatment of diabetes’ encompasses broad concepts from lifestyle modification to medication treatment, in most of the included studies and our study, “adherence to medication” was considered diabetes treatment, which may affect treatment and control rates. Second, the included studies used different diagnostic tools, measurements, and definitions for diabetes, which may have resulted in misclassification. Additionally, the uneven distribution of studies across different countries and time periods, as well as the varying quality of some studies, may have influenced the results to some extent. Moreover, methodological variations, including sampling weight considerations, different survey analysis methods, and sampling techniques, are important limitations. To obtain more robust findings, it is suggested to use individual participant data (IPD) meta-analysis. Nevertheless, this study gathered data on diabetes awareness, treatment, and control on a worldwide scale, including a large number of studies in the analysis. Furthermore, we conducted stratified analyses to assess these proportions and their trends in various subgroups over the past 40 years.
Conclusion
Based on the results of this systematic review and meta-analysis, despite the high level of awareness and treatment among the diabetic population, the success of treatment (control) is considerably low, particularly in low-income countries and rural areas. It is crucial to improve awareness, treatment, and control by strengthening the primary care system in all countries. The global state of diabetes management highlights the urgent need for a comprehensive intervention strategy, especially for diabetes control. Implementation of appropriate community-oriented public health policies, promotion of health education, development of simplified clinical guidelines, and regular screening and physician consultation can contribute to better diabetes management.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ESh: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. NM: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. ESe: Investigation, Writing – review & editing. FB: Conceptualization, Writing – review & editing. H-SE: Conceptualization, Writing – review & editing. AS: Data curation, Formal analysis, Writing – review & editing. SD: Investigation, Writing – review & editing. DM: Writing – review & editing. MQ: Conceptualization, Formal analysis, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Alborz University of Medical Sciences funded this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1305304/full#supplementary-material
References
1. Tripathi, BK, and Srivastava, AK. Diabetes mellitus: complications and therapeutics. Med Sci Monit. (2006) 12:RA130–RA47.
2. Herman, WH . The global burden of diabetes: an overview In: Diabetes mellitus in developing countries and underserved communities. Cham: Springer (2017). 1–5. doi: 10.1007/978-3-319-41559-8_1
3. Contreras, F, Sanchez, M, Martinez, M, Castillo, MC, Mindiola, A, Bermudez, V, et al. Management and education in patients with diabetes mellitus. Med Clin Rev. (2017) 3:7. doi: 10.21767/2471-299X.1000049
4. Blonde, L . Current antihyperglycemic treatment guidelines and algorithms for patients with type 2 diabetes mellitus. Am J Med. (2010) 123:S12–8. doi: 10.1016/j.amjmed.2009.12.005
5. Salim, B. Diabetes mellitus and its treatment. Journal of diabetes & metabolism. (2005) 13:11–134.
6. Mishra, V, Nayak, P, Sharma, M, Albutti, A, Alwashmi, ASS, Aljasir, MA, et al. Emerging treatment strategies for diabetes mellitus and associated complications: an update. Pharmaceutics. (2021) 13:1568. doi: 10.3390/pharmaceutics13101568
7. Skyler, JS, Bakris, GL, Bonifacio, E, Darsow, T, Eckel, RH, Groop, L, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. (2017) 66:241–55. doi: 10.2337/db16-0806
8. Higgins, J, Thomas, J, Chandler, J, Cumpston, M, and Li, T. (editors) MPWV Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). (2023). Available at: https://training.cochrane.org/handbook
9. Page, MJ, McKenzie, J, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
10. World Bank . World Bank's Classification. (2019–2020). (2021). Available at: https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2021-2022#:~:text=The%20World%20Bank%20assigns%20the,i.e.%202020%20in20this20case
11. Mou, C, Xu, M, and Lyu, J. Predictors of undiagnosed diabetes among middle-aged and seniors in China: application of Andersen’s behavioral model. Int J Environ Res Public Health. (2021) 18:8396. doi: 10.3390/ijerph18168396
12. Bai, A, Tao, J, Tao, L, and Liu, J. Prevalence and risk factors of diabetes among adults aged 45 years or older in China: a national cross-sectional study. Endocrinol Diabet Metabol. (2021) 4:e00265-e. doi: 10.1002/edm2.265
13. Liu, C, Li, X, Lin, M, Zheng, L, and Chen, X. A cross-sectional study on diabetes epidemiology among people aged 40 years and above in Shenyang, China. Sci Rep. (2020) 10:17742. doi: 10.1038/s41598-020-74889-x
14. Zhang, H, Qi, D, Gu, H, Wang, T, Wu, Y, Li, J, et al. Trends in the prevalence, awareness, treatment and control of diabetes in rural areas of northern China from 1992 to 2011. J Diabetes Investig. (2020) 11:241–9. doi: 10.1111/jdi.13095
15. Li, J, Ni, J, Wu, Y, Zhang, H, Liu, J, Tu, J, et al. Sex differences in the prevalence, awareness, treatment, and control of diabetes mellitus among adults aged 45 years and older in rural areas of northern China: a cross-sectional, population-based study. Front Endocrinol. (2019) 10:147. doi: 10.3389/fendo.2019.00147
16. Li, C, and Lumey, LH. Impact of disease screening on awareness and management of hypertension and diabetes between 2011 and 2015: results from the China health and retirement longitudinal study. BMC Public Health. (2019) 19:421. doi: 10.1186/s12889-019-6753-x
17. Cai, L, Li, X, Cui, W, You, D, and Golden, AR. Trends in diabetes and pre-diabetes prevalence and diabetes awareness, treatment and control across socioeconomic gradients in rural Southwest China. J Public Health. (2018) 40:375–80. doi: 10.1093/pubmed/fdx097
18. Zhang, FL, Xing, YQ, Guo, ZN, Wu, YH, Liu, HY, and Yang, Y. Prevalence and risk factors for diabetes and impaired fasting glucose in Northeast China: results from the 2016 China National Stroke Screening Survey. Diabetes Res Clin Pract. (2018) 144:302–13. doi: 10.1016/j.diabres.2018.09.005
19. Wang, Q, Zhang, X, Fang, L, Guan, Q, Guan, L, and Li, Q. Prevalence, awareness, treatment and control of diabetes mellitus among middle-aged and elderly people in a rural Chinese population: a cross-sectional study. PLoS One. (2018) 13:e0198343. doi: 10.1371/journal.pone.0199935
20. Yan, X, Xia, H, Li, H, Deng, X, Yang, L, Zhao, S, et al. Diabetes in Shenzhen, China: epidemiological investigation and health care challenges. J Glob Health. (2017) 7:011102. doi: 10.7189/jogh.07.011102
21. Wang, L, Gao, P, Zhang, M, Huang, Z, Zhang, D, Deng, Q, et al. Prevalence and ethnic pattern of diabetes and Prediabetes in China in 2013. JAMA. (2017) 317:2515–23. doi: 10.1001/jama.2017.7596
22. Liu, X, Wang, L, Wang, P, Liu, R, Yang, K, Qian, X, et al. The dynamics of type 2 diabetes mellitus prevalence and management rates among rural population in Henan Province. Exp Diabetes Res. (2017) 2017:9092759. doi: 10.1155/2017/9092759
23. Hu, M, Wan, Y, Yu, L, Yuan, J, Ma, Y, Hou, B, et al. Prevalence, awareness and associated risk factors of diabetes among adults in Xi'an, China. Sci Rep. (2017) 7:10472. doi: 10.1038/s41598-017-10797-x
24. Feng, B-Y, Huang, C, Cao, J, Dong, Z, Liu, FC, Ji, LN, et al. Diabetes awareness, treatment, control rates and associated risk factors among Beijing residents in 2011: a cross-sectional survey. Chronic Diseases Transl Med. (2016) 2:147–58. doi: 10.1016/j.cdtm.2016.11.011
25. Qin, Y, Wang, R, Ma, X, Zhao, Y, Lu, J, Wu, C, et al. Prevalence, awareness, treatment and control of diabetes mellitus-a population based study in Shanghai, China. Int J Environ Res Public Health. (2016) 13. doi: 10.3390/ijerph13050512
26. Liu, M, Wang, J, He, Y, Jiang, B, Wu, L, Wang, Y, et al. Awareness, treatment and control of type 2 diabetes among Chinese elderly and its changing trend for past decade. BMC Public Health. (2016) 16:278. doi: 10.1186/s12889-016-2874-7
27. Yue, J, Mao, X, Xu, K, Lü, L, Liu, S, Chen, F, et al. Prevalence, awareness, treatment and control of diabetes mellitus in a Chinese population. PLoS One. (2016) 11:e0153791. doi: 10.1371/journal.pone.0153791
28. Su, R, Cai, L, Cui, W, He, J, You, D, and Golden, A. Multilevel analysis of socioeconomic determinants on diabetes prevalence, awareness, treatment and self-Management in Ethnic Minorities of Yunnan Province, China. Int J Environ Res Public Health. (2016) 13. doi: 10.3390/ijerph13080751
29. Wang, R, Zhang, P, Lv, X, Jiang, L, Gao, C, Song, Y, et al. Situation of diabetes and related disease surveillance in rural areas of Jilin Province, Northeast China. Int J Environ Res Public Health. (2016) 13:538. doi: 10.3390/ijerph13060538
30. Yang, F, Qian, D, Chen, J, Hu, D, Hou, M, Chen, S, et al. Prevalence, awareness, treatment and control of diabetes mellitus in rural China: results from Shandong Province. Diabet Med. (2016) 33:454–8. doi: 10.1111/dme.12842
31. Liu, X, Li, Y, Li, L, Zhang, L, Ren, Y, Zhou, H, et al. Prevalence, awareness, treatment, control of type 2 diabetes mellitus and risk factors in Chinese rural population: the RuralDiab study. Sci Rep. (2016) 6:31426. doi: 10.1038/srep31426
32. Yin, M, Augustin, B, Shu, C, Qin, T, and Yin, P. Probit models to investigate prevalence of Total diagnosed and undiagnosed diabetes among aged 45 years or older adults in China. PLoS One. (2016) 11:e0164481. doi: 10.1371/journal.pone.0164481
33. Zhou, X, Guan, H, Zheng, L, Li, Z, Guo, X, Yang, H, et al. Prevalence and awareness of diabetes mellitus among a rural population in China: results from Liaoning Province. Diabet Med. (2015) 32:332–42. doi: 10.1111/dme.12599
34. Wang, C, Yu, Y, Zhang, X, Li, Y, Kou, C, Li, B, et al. Awareness, treatment, control of diabetes mellitus and the risk factors: survey results from Northeast China. PLoS One. (2014) 9:e103594. doi: 10.1371/journal.pone.0103594
35. Zhang, H, Xu, W, Dahl, AK, Xu, Z, Wang, H-X, and Qi, X. Relation of socio-economic status to impaired fasting glucose and type 2 diabetes: findings based on a large population-based cross-sectional study in Tianjin, China. Innovative Care. (2013) 30:e157–62. doi: 10.1111/dme.12156
36. Xu, S, Ming, J, Xing, Y, Gao, B, Yang, C, Ji, Q, et al. Regional differences in diabetes prevalence and awareness between coastal and interior provinces in China: a population-based cross-sectional study. BMC Public Health. (2013) 13:299. doi: 10.1186/1471-2458-13-299
37. Xu, Y, Wang, L, He, J, Bi, Y, Li, M, Wang, T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. (2013) 310:948–59. doi: 10.1001/jama.2013.168118
38. Zhang, YH, Ma, WJ, Thomas, GN, Xu, YJ, Lao, XQ, Xu, XJ, et al. Diabetes and pre-diabetes as determined by glycated haemoglobin A1c and glucose levels in a developing southern Chinese population. PLoS One. (2012) 7:e37260. doi: 10.1371/journal.pone.0037260
39. Yang, YN, Xie, X, Ma, YT, Li, XM, Fu, ZY, Ma, X, et al. Type 2 diabetes in Xinjiang Uygur autonomous region, China. PLoS One. (2012) 7:e35270. doi: 10.1371/journal.pone.0035270
40. Xu, W, Xu, Z, Jia, J, Xie, Y, Wang, H-X, and Qi, X. Detection of Prediabetes and undiagnosed type 2 diabetes: a large population-based study. Can J Diabetes. (2012) 36:108–13. doi: 10.1016/j.jcjd.2012.04.014
41. Le, C, Jun, D, Zhankun, S, Yichun, L, and Jie, T. Socioeconomic differences in diabetes prevalence, awareness, and treatment in rural Southwest China. Trop Med Int Health. (2011) 16:1070–6. doi: 10.1111/j.1365-3156.2011.02805.x
42. Yang, W, Lu, J, Weng, J, Jia, W, Ji, L, Xiao, J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. (2010) 362:1090–101. doi: 10.1056/NEJMoa0908292
43. Hu, D, Fu, P, Xie, J, Chen, CS, Yu, D, Whelton, PK, et al. Increasing prevalence and low awareness, treatment and control of diabetes mellitus among Chinese adults: the InterASIA study. Diabetes Res Clin Pract. (2008) 81:250–7. doi: 10.1016/j.diabres.2008.04.008
44. Tian, H, Song, G, Xie, H, Zhang, H, Tuomilehto, J, and Hu, G. Prevalence of diabetes and impaired fasting glucose among 769792 rural Chinese adults. Diabetes Res Clin Pract. (2009) 84:273–8. doi: 10.1016/j.diabres.2009.03.015
45. Katulanda, P, Constantine, GR, Mahesh, JG, Sheriff, R, Seneviratne, RDA, Wijeratne, S, et al. Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka—Sri Lanka diabetes, cardiovascular study (SLDCS). Diabet Med. (2008) 25:1062–9. doi: 10.1111/j.1464-5491.2008.02523.x
46. Gupta, S, Kumar, R, Kalaivani, M, Nongkynrih, B, Kant, S, and Gupta, SK. Prevalence, awareness, treatment, and control of diabetes and hypertension among elderly persons in a rural area of Ballabgarh, Haryana. J Family Med Prim Care. (2020) 9:777–82. doi: 10.4103/jfmpc.jfmpc_1057_19
47. Rajbhandari, SM, Kumar, KV, Selvarajan, R, and Murali, T. High prevalence of diabetes in young people in Bangalore, India. Br J Diabetes. (2020) 20:104–6. doi: 10.15277/bjd.2020.259
48. Prenissl, J, Jaacks, LM, Mohan, V, Manne-Goehler, J, Davies, JI, Awasthi, A, et al. Variation in health system performance for managing diabetes among states in India: a cross-sectional study of individuals aged 15 to 49 years. BMC Med. (2019) 17:92. doi: 10.1186/s12916-019-1325-6
49. Kandasamy, K, Rajagopal, SS, Ramalingam, K, and Krishnan, K. Prevalence of diagnosed and undiagnosed diabetes in a rural community: a home-based screening. AJPCR. (2018) 11:454. doi: 10.22159/ajpcr.2018.v11i5.24906
50. Anusuya, GS, Ravi, R, Gopalakrishnan, S, Abiselvi, A, and Stephen, T. Prevalence of undiagnosed and uncontrolled diabetes mellitus among adults in South Chennai. Int J Community Med Public Health. (2018) 5:5200–4. doi: 10.18203/2394-6040.ijcmph20184790
51. Tripathy, JP, Thakur, JS, Jeet, G, Chawla, S, Jain, S, Pal, A, et al. Prevalence and risk factors of diabetes in a large community-based study in North India: results from a STEPS survey in Punjab, India. Diabetol Metab Syndr. (2017) 9:8. doi: 10.1186/s13098-017-0207-3
52. Negi, PC, Chauhan, R, Rana, V, and Vidyasagar, LK. Epidemiological study of non-communicable diseases (NCD) risk factors in tribal district of Kinnaur, HP: a cross-sectional study. Indian Heart J. (2016) 68:655–62. doi: 10.1016/j.ihj.2016.03.002
53. Gupta, R, Sharma, KK, Gupta, BK, Gupta, A, Gupta, RR, and Deedwania, PC. Educational status-related disparities in awareness, treatment and control of cardiovascular risk factors in India. Heart Asia. (2015) 7:1–6. doi: 10.1136/heartasia-2014-010551
54. Singh, AK, Mani, K, Krishnan, A, Aggarwal, P, and Gupta, SK. Prevalence, awareness, treatment and control of diabetes among elderly persons in an urban slum of Delhi. Indian J Commun Med. (2012) 37:236–9. doi: 10.4103/0970-0218.103472
55. Joshi, SR, Saboo, B, Vadivale, M, Dani, SI, Mithal, A, Kaul, U, et al. Prevalence of diagnosed and undiagnosed diabetes and hypertension in India--results from the screening India's twin epidemic (SITE) study. Diabetes Technol Ther. (2012) 14:8–15. doi: 10.1089/dia.2011.0243
56. Bansal, M, Shrivastava, S, Mehrotra, R, Agrawal, V, and Kasliwal, RR. Time-trends in prevalence and awareness of cardiovascular risk factors in an asymptomatic north Indian urban population. J Assoc Physicians India. (2009) 57:568–73.
57. Zargar, AH, Wani, AA, Laway, BA, Masoodi, SR, Wani, AI, Bashir, MI, et al. Prevalence of diabetes mellitus and other abnormalities of glucose tolerance in young adults aged 20–40 years in North India (Kashmir Valley). Diabetes Res Clin Pract. (2008) 82:276–81. doi: 10.1016/j.diabres.2008.08.006
58. Menon, VU, Kumar, KV, Gilchrist, A, Sugathan, TN, Sundaram, KR, Nair, V, et al. Prevalence of known and undetected diabetes and associated risk factors in Central Kerala — ADEPS. Diabetes Res Clin Pract. (2006) 74:289–94. doi: 10.1016/j.diabres.2006.03.025
59. Khodakarami, R, Abdi, Z, Ahmadnezhad, E, Sheidaei, A, and Asadi-Lari, M. Prevalence, awareness, treatment and control of diabetes among Iranian population: results of four national cross-sectional STEPwise approach to surveillance surveys. BMC Public Health. (2022) 22:1216. doi: 10.1186/s12889-022-13627-6
60. Khamseh, ME, Sepanlou, SG, Hashemi-Madani, N, Joukar, F, Mehrparvar, AH, Faramarzi, E, et al. Nationwide prevalence of diabetes and Prediabetes and associated risk factors among Iranian adults: analysis of data from PERSIAN cohort study. Diabetes Ther. (2021) 12:2921–38. doi: 10.1007/s13300-021-01152-5
61. Mirzaei, M, Rahmaninan, M, Mirzaei, M, and Nadjarzadeh, A. Epidemiology of diabetes mellitus, pre-diabetes, undiagnosed and uncontrolled diabetes in Central Iran: results from Yazd health study. BMC Public Health. (2020) 20:1–9. doi: 10.1186/s12889-020-8267-y
62. Shamshirgaran, SM, Ghorbani, Z, Najafipour, F, Sarbakhsh, P, and Aminisani, N. Prevalence of diabetes, prediabetes, awareness, treatment and control among people 35 years and up. Research Square (2020). doi: 10.21203/rs.3.rs-22638/v1
63. Safari-Faramani, R, Rajati, F, Tavakol, K, Hamzeh, B, Pasdar, Y, Moradinazar, M, et al. Prevalence, awareness, treatment, control, and the associated factors of diabetes in an Iranian Kurdish population. J Diabetes Res. (2019) 2019:1–9. doi: 10.1155/2019/5869206
64. Mahtab, N, Farzad, H, Mohsen, B, and Nakisa, D. The 10-year trend of adult diabetes, prediabetes and associated risk factors in Tehran: phases 1 and 4 of Tehran lipid and glucose study. Diabetes Metab Syndr Clin Res Rev. (2017) 11:183–7. doi: 10.1016/j.dsx.2016.08.028
65. Yazdanpanah, L, Shahbazian, HB, Moravej Aleali, A, Jahanshahi, A, Ghanbari, S, and Latifi, SM. Prevalence, awareness and risk factors of diabetes in Ahvaz (south west of Iran). Diabetes Metab Syndr. (2016) 10:S114–8. doi: 10.1016/j.dsx.2016.03.007
66. Mohtasham-Amiri, Z, Barzigar, A, Kolamroudi, HR, Hoseini, S, Rezvani, SM, Shakib, RJ, et al. Prevalence, awareness and control of diabetes in urban area of north of Iran, 2009. Int J Diabetes Dev Ctries. (2015) 35:346–50. doi: 10.1007/s13410-015-0305-4
67. Khalilzadeh, S, Afkhami-Ardekani, M, and Afrand, M. High prevalence of type 2 diabetes and pre-diabetes in adult Zoroastrians in Yazd, Iran: a cross-sectional study. Electron Physician. (2015) 7:998. doi: 10.14661/2015.998-1004
68. Katibeh, M, Hosseini, S, Soleimanizad, R, Manaviat, MR, Kheiri, B, Khabazkhoob, M, et al. Prevalence and risk factors of diabetes mellitus in a central district in Islamic Republic of Iran: a population-based study on adults aged 40-80 years. East Mediterr Health J. (2015) 21:412–9. doi: 10.26719/2015.21.412
69. Lotfi, MH, Saadati, H, and Afzali, M. Prevalence of diabetes in people aged≥ 30 years: the results of screen-ing program of Yazd Province, Iran, in 2012. J Res Health Sci. (2013) 14:88–92.
70. Veghari, G, Sedaghat, M, Joshaghani, H, Hoseini, SA, Niknezad, F, Angizeh, A, et al. Association between socio-demographic factors and diabetes mellitus in the north of Iran: a population-based study. Int J Diabetes Mellitus. (2010) 2:154–7. doi: 10.1016/j.ijdm.2010.09.001
71. Shirani, S, Kelishadi, R, Sarrafzadegan, N, Khosravi, A, Sadri, G, Amani, A, et al. Awareness, treatment and control of hypertension, dyslipidaemia and diabetes mellitus in an Iranian population: the IHHP study. East Mediterr Health J. (2009) 15:1455–63.
72. Hadaegh, F, Bozorgmanesh, MR, Ghasemi, A, Harati, H, Saadat, N, and Azizi, F. High prevalence of undiagnosed diabetes and abnormal glucose tolerance in the Iranian urban population: Tehran lipid and glucose study. BMC Public Health. (2008) 8:1–7. doi: 10.1186/1471-2458-8-176
73. Sajjadi, F, Mohammadifard, N, Kelishadi, R, Ghaderian, N, Alikhasi, H, and Maghrun, M. Clustering of coronary artery disease risk factors in patients with type 2 diabetes and impaired glucose tolerance. EMHJ. (2008) 14:1080–9.
74. Sadeghi, M, Roohafza, H, Shirani, S, Poormoghadas, M, Kelishadi, R, Baghaii, A, et al. Diabetes and associated cardiovascular risk factors in Iran: the Isfahan healthy heart Programme. Ann Acad Med Singap. (2007) 36:175–80. doi: 10.47102/annals-acadmedsg.V36N3p175
75. Khan, MN, Oldroyd, JC, Hossain, MB, and Islam, RM. Awareness, treatment, and control of diabetes in Bangladesh: evidence from the Bangladesh demographic and health survey 2017/18. medRxiv. (2021) 2022:8349160. doi: 10.1155/2022/8349160
76. Chowdhury, MA, Uddin, MJ, Khan, HM, and Haque, MR. Type 2 diabetes and its correlates among adults in Bangladesh: a population based study. BMC Public Health. (2015) 15:1070. doi: 10.1186/s12889-015-2413-y
77. Rahman, M, Nakamura, K, and Kizuki, M. Socioeconomic differences in the prevalence, awareness, and control of diabetes in Bangladesh. J Diabetes Complicat. (2015) 29:788–93. doi: 10.1016/j.jdiacomp.2015.04.011
78. Rahman, MS, Akter, S, Abe, SK, Islam, MR, Mondal, MNI, Rahman, JAMS, et al. Awareness, treatment, and control of diabetes in Bangladesh: a nationwide population-based study. PLoS One. (2015) 10:e0118365. doi: 10.1371/journal.pone.0118365
79. Akter, S, Rahman, MM, Abe, SK, and Sultana, P. Prevalence of diabetes and prediabetes and their risk factors among Bangladeshi adults: a nationwide survey. Bull World Health Organ. (2014) 92:204–13. doi: 10.2471/BLT.13.128371
80. Mahar, P, Awan, MZ, Manzar, N, and Memon, MS. Prevalence of type-II diabetes mellitus and diabetic retinopathy: the Gaddap study. J Coll Physicians Surg Pak. (2010) 20:528–32.
81. Afghani, T, Qureshi, N, and Chaudhry, KSA. Screening for diabetic retinopathy: a comparative study between hospital and community based screening and between paying and non-paying patients. J Ayub Medical College Abbottabad. (2007) 19:16–22.
82. Shera, A, Rafique, G, Khwaja, I, Ara, J, Baqai, S, and King, H. Pakistan national diabetes survey: prevalence of glucose intolerance and associated factors in Shikarpur, Sindh Province. Diabetic Med. (1995) 12:1116–21. doi: 10.1111/j.1464-5491.1995.tb00430.x
83. Adedokun, AO, Ter Goon, D, Owolabi, EO, Adeniyi, OV, and Ajayi, AI. Prevalence, awareness, and determinants of type 2 diabetes mellitus among commercial taxi drivers in buffalo city metropolitan municipality South Africa: a cross-sectional survey. Medicine (Baltimore). (2019) 98:e14652. doi: 10.1097/MD.0000000000014652
84. Bailey, SL, Ayles, H, Beyers, N, Godfrey-Faussett, P, Muyoyeta, M, du Toit, E, et al. Diabetes mellitus in Zambia and the Western cape province of South Africa: prevalence, risk factors, diagnosis and management. Diabetes Res Clin Pract. (2016) 118:1–11. doi: 10.1016/j.diabres.2016.05.001
85. Shen, J, Kondal, D, Rubinstein, A, Irazola, V, Gutierrez, L, Miranda, JJ, et al. A multiethnic study of pre-diabetes and diabetes in LMIC. Glob Heart. (2016) 11:61–70. doi: 10.1016/j.gheart.2015.12.015
86. Erasmus, RT, Soita, DJ, Hassan, MS, Blanco-Blanco, E, Vergotine, Z, Kengne, AP, et al. High prevalence of diabetes mellitus and metabolic syndrome in a south African coloured population: baseline data of a study in Bellville, Cape Town, South African. J Obstetrics Gynaecol. (2012) 102:841–4. doi: 10.7196/SAMJ.5670
87. Dajani, R, Khader, YS, Fatahallah, R, El-Khateeb, M, Shiyab, AH, and Hakooz, N. Diabetes mellitus in genetically isolated populations in Jordan: prevalence, awareness, glycemic control, and associated factors. J Diabetes Complicat. (2012) 26:175–80. doi: 10.1016/j.jdiacomp.2012.03.009
88. Ajlouni, K, Khader, YS, Batieha, A, Ajlouni, H, and El-Khateeb, M. An increase in prevalence of diabetes mellitus in Jordan over 10 years. J Diabetes Complicat. (2008) 22:317–24. doi: 10.1016/j.jdiacomp.2007.01.004
89. Fahs, I, Khalife, Z, Malaeb, D, Iskandarani, M, and Salameh, P. The prevalence and awareness of cardiovascular diseases risk factors among the Lebanese population: a prospective study comparing urban to rural populations. Cardiol Res Pract. (2017) 2017:1–10. doi: 10.1155/2017/3530902
90. Dankner, R, Geulayov, G, Olmer, L, and Kaplan, G. Undetected type 2 diabetes in older adults. Age Ageing. (2008) 38:56–62. doi: 10.1093/ageing/afn218
91. Ben Ali, RA, Hannoun, Z, Harraqui, K, Zeghari, L, Aboussaleh, Y, Mohamed, S, et al. Profile of diabetes and cardiovascular risk factors in adults Anjouan Island (Comoros). Pan Afr Med J. (2019) 33:140. doi: 10.11604/pamj.2019.33.140.19016
92. Alkerwi, A, Pagny, S, Lair, ML, Delagardelle, C, and Beissel, J. Level of unawareness and management of diabetes, hypertension, and dyslipidemia among adults in Luxembourg: findings from ORISCAV-LUX study. PLoS One. (2013) 8:e57920. doi: 10.1371/journal.pone.0057920
93. Aung, WP, Bjertness, E, Htet, AS, Stigum, H, and Kjollesdal, MKR. Trends in diabetes prevalence, awareness, treatment and control in Yangon Region, Myanmar, between 2004 and 2014, two cross-sectional studies. Int J Environ Res Public Health. (2019) 16. doi: 10.3390/ijerph16183461
94. Bijlholt, M, Meeks, KAC, Beune, E, Addo, J, Smeeth, L, Schulze, MB, et al. Type 2 diabetes mellitus management among Ghanaian migrants resident in three European countries and their compatriots in rural and urban Ghana - the RODAM study. Diabetes Res Clin Pract. (2018) 136:32–8. doi: 10.1016/j.diabres.2017.11.032
95. Balde, NM, Camara, A, Diallo, AA, Kake, A, Diallo, AM, Diakite, M, et al. Prevalence and awareness of diabetes in Guinea: findings from a WHO STEPS. J Endocrinol Metab Diabetes S Afr. (2017) 22:36–42. doi: 10.1080/16089677.2017.1366091
96. Sagna, Y, Tieno, H, Guira, O, Yanogo, D, Benon, L, Zida, S, et al. Prevalence and associated risk factors of diabetes and impaired fasting glucose in urban population; a study from Burkina Faso. J Diabetol. (2014) 2:4.
97. Snijder, MB, Agyemang, C, Peters, RJ, Stronks, K, Ujcic-Voortman, JK, and van Valkengoed, IG. Case finding and medical treatment of type 2 diabetes among different ethnic minority groups: the HELIUS study. J Diabetes Res. (2017) 2017:9896849. doi: 10.1155/2017/9896849
98. Heidemann, C, Du, Y, Paprott, R, Haftenberger, M, Rathmann, W, and Scheidt-Nave, C. Temporal changes in the prevalence of diagnosed diabetes, undiagnosed diabetes and prediabetes: findings from the German health interview and examination surveys in 1997–1999 and 2008–2011. Diabet Med. (2016) 33:1406–14. doi: 10.1111/dme.13008
99. Icks, A, Claessen, H, Strassburger, K, Tepel, M, Waldeyer, R, Chernyak, N, et al. Drug costs in Prediabetes and undetected diabetes compared with diagnosed diabetes and Normal glucose tolerance: results from the population-based KORA survey in Germany. Diabetes Care. (2013) 36:e53–4. doi: 10.2337/dc12-0997
100. Meisinger, C, Strassburger, K, Heier, M, Thorand, B, Baumeister, SE, Giani, G, et al. Prevalence of undiagnosed diabetes and impaired glucose regulation in 35–59-year-old individuals in southern Germany: the KORA F4 study. Diabet Med. (2010) 27:360–2. doi: 10.1111/j.1464-5491.2009.02905.x
101. Hauner, H, Hanisch, J, Bramlage, P, Steinhagen-Thiessen, E, Schunkert, H, Jöckel, KH, et al. Prevalence of undiagnosed Type-2-diabetes mellitus and impaired fasting glucose in German primary care: data from the German metabolic and cardiovascular risk project (GEMCAS). Exp Clin Endocrinol Diabetes. (2008) 116:18–25. doi: 10.1055/s-2007-985359
102. Rathmann, W, Haastert, B, Icks, A, Löwel, H, Meisinger, C, Holle, R, et al. High prevalence of undiagnosed diabetes mellitus in southern Germany: target populations for efficient screening. The KORA survey 2000. Diabetologia. (2003) 46:182–9. doi: 10.1007/s00125-002-1025-0
103. Huang, Y-T, Steptoe, A, and Zaninotto, P. Prevalence of undiagnosed diabetes in 2004 and 2012: evidence from the English longitudinal study of aging. J Gerontol. (2020) 76:922–8. doi: 10.1093/gerona/glaa179
104. Dos Santos, ESM, de Oliveira, MR, de Andrade, FB, de Oliveira, C, Lima-Costa, MF, and da Silva, AT. Differences in the prevalence of prediabetes, undiagnosed diabetes and diagnosed diabetes and associated factors in cohorts of Brazilian and English older adults. Public Health Nutr. (2021) 24:4187–94. doi: 10.1017/S1368980020003201
105. Moody, A, Cowley, G, Ng Fat, L, and Mindell, JS. Social inequalities in prevalence of diagnosed and undiagnosed diabetes and impaired glucose regulation in participants in the health surveys for England series. BMJ Open. (2016) 6:e010155. doi: 10.1136/bmjopen-2015-010155
106. Thomas, MC, Walker, MK, Emberson, JR, Thomson, AG, Lawlor, DA, Ebrahim, S, et al. Prevalence of undiagnosed type 2 diabetes and impaired fasting glucose in older B ritish men and women. Diabet Med. (2005) 22:789–93. doi: 10.1111/j.1464-5491.2005.01516.x
107. Riste, L, Khan, F, and Cruickshank, K. High prevalence of type 2 diabetes in all ethnic groups, including Europeans, in a British inner city: relative poverty, history, inactivity, or 21st century Europe? Diabetes Care. (2001) 24:1377–83. doi: 10.2337/diacare.24.8.1377
108. Simmons, D, Williams, D, and Powell, M. The Coventry diabetes study: prevalence of diabetes and impaired glucose tolerance in Europids and Asians. QJM. (1991) 81:1021–30. doi: 10.1093/qjmed/81.3.1021
109. Simmons, D, Williams, DR, and Powell, MJ. Prevalence of diabetes in a predominantly Asian community: preliminary findings of the Coventry diabetes study. Br Med J. (1989) 298:18–21.
110. Lailler, G, Piffaretti, C, Fuentes, S, Nabe, HD, Oleko, A, Cosson, E, et al. Prevalence of prediabetes and undiagnosed type 2 diabetes in France: results from the national survey ESTEBAN, 2014–2016. Diabetes Res Clin Pract. (2020) 165:108252. doi: 10.1016/j.diabres.2020.108252
111. Carrère, P, Fagour, C, Sportouch, D, Gane-Troplent, F, Hélène-Pelage, J, Lang, T, et al. Diabetes mellitus and obesity in the French Caribbean: a special vulnerability for women? Women Health. (2018) 58:145–59. doi: 10.1080/03630242.2017.1282396
112. Fuentes, S, Fosse-Edorh, S, Regnault, N, Goldberg, M, and Cosson, E. Prevalence of Prediabetes and undiagnosed diabetes among adults aged 18 to 70 years in France—the CONSTANCES cohort. Diabetes. (2018) 67:1657-P. doi: 10.2337/db18-1657-P
113. Bonaldi, C, Vernay, M, Roudier, C, Salanave, B, Oleko, A, Malon, A, et al. A first national prevalence estimate of diagnosed and undiagnosed diabetes in France in 18-to 74-year-old individuals: the French nutrition and health survey 2006/2007. Diabet Med. (2011) 28:583–9. doi: 10.1111/j.1464-5491.2011.03250.x
114. Omboni, S, Carabelli, G, Ghirardi, E, and Carugo, S. Awareness, treatment, and control of major cardiovascular risk factors in a small-scale Italian community: results of a screening campaign. Vasc Health Risk Manag. (2013) 9:177–85. doi: 10.2147/VHRM.S40925
115. Scuteri, A, Najjar, SS, Orru', M, Albai, G, Strait, J, Tarasov, KV, et al. Age- and gender-specific awareness, treatment, and control of cardiovascular risk factors and subclinical vascular lesions in a founder population: the SardiNIA study. Nutr Metab Cardiovasc Dis. (2009) 19:532–41. doi: 10.1016/j.numecd.2008.11.004
116. Muntoni, S, Atzori, L, Mereu, R, Manca, A, Satta, G, Gentilini, A, et al. Prevalence of diagnosed and undiagnosed diabetes mellitus and impaired fasting glucose in Sardinia. Acta Diabetol. (2009) 46:227–31. doi: 10.1007/s00592-008-0081-4
117. Gnasso, A, Calindro, MC, Carallo, C, de Novara, G, Ferraro, M, Gorgone, G, et al. Awareness, treatment and control of hyperlipidaemia, hypertension and diabetes mellitus in a selected population of southern Italy. Eur J Epidemiol. (1997) 13:421–8. doi: 10.1023/A:1007369203648
118. Kaiser, A, Vollenweider, P, Waeber, G, and Marques-Vidal, P. Prevalence, awareness and treatment of type 2 diabetes mellitus in Switzerland: the CoLaus study. Diabet Med. (2012) 29:190–7. doi: 10.1111/j.1464-5491.2011.03422.x
119. Bennet, L, Johansson, S-E, Agardh, C-D, Groop, L, Sundquist, J, Råstam, L, et al. High prevalence of type 2 diabetes in Iraqi and Swedish residents in a deprived Swedish neighbourhood-a population based study. BMC Public Health. (2011) 11:1–10. doi: 10.1186/1471-2458-11-303
120. Ylihärsilä, H, Lindström, J, Eriksson, JG, Jousilahti, P, Valle, TT, Sundvall, J, et al. Prevalence of diabetes and impaired glucose regulation in 45- to 64-year-old individuals in three areas of Finland. Diabet Med. (2005) 22:88–91. doi: 10.1111/j.1464-5491.2005.01420.x
121. Hiltunen, L, Luukinen, H, Koski, K, and Kivelä, S-L. Prevalence of diabetes mellitus in an elderly Finnish population. Diabet Med. (1994) 11:241–9. doi: 10.1111/j.1464-5491.1994.tb00266.x
123. Midthjell, K, Bjørndal, A, Holmen, J, Krüger, Ø, and Bjartveit, K. Prevalence of known and previously unknown diabetes mellitus and impaired glucose tolerance in an adult Norwegian population. Indications of an increasing diabetes prevalence. The Nord-Trøndelag diabetes study. Scand J Prim Health Care. (1995) 13:229–35.
124. O Connor, JM, Millar, SR, Buckley, CM, Kearney, PM, and Perry, IJ. The prevalence and determinants of undiagnosed and diagnosed type 2 diabetes in middle-aged Irish adults. PLoS One. (2013) 8:e80504. doi: 10.1371/journal.pone.0080504
125. Moustgaard, H, Bjerregaard, P, Borch-Johnsen, K, and Jørgensen, MEStudy TGP. Diabetes among Inuit migrants in Denmark. Int J Circumpolar Health. (2005) 64:354–64. doi: 10.3402/ijch.v64i4.18013
126. Puzianowska-Kuźnicka, M, Januszkiewicz-Caulier, J, Kurylowicz, A, Mossakowska, M, Zdrojewski, T, Szybalska, A, et al. Prevalence and socioeconomic predictors of diagnosed and undiagnosed diabetes in oldest-old and younger Caucasian seniors: results from the PolSenior study. Endokrynol Pol. (2021) 72:249–55. doi: 10.5603/EP.a2021.0029
127. Jørgensen, ME, Bjeregaard, P, Borch-Johnsen, K, Backer, V, Becker, U, Jørgensen, T, et al. Diabetes and impaired glucose tolerance among the Inuit population of Greenland. Diabetes Care. (2002) 25:1766–71. doi: 10.2337/diacare.25.10.1766
128. Papazoglou, N, Manes, C, Chatzimitrofanous, P, Papadeli, E, Tzounas, K, Scaragas, G, et al. Epidemiology of diabetes mellitus in the elderly in northern Greece: a population study. Diabet Med. (1995) 12:397–400. doi: 10.1111/j.1464-5491.1995.tb00502.x
129. Aguayo, A, Urrutia, I, González-Frutos, T, Martínez, R, Martínez-Indart, L, Castaño, L, et al. Prevalence of diabetes mellitus and impaired glucose metabolism in the adult population of the Basque Country. Innovative Care. (2017) 34:662–6. doi: 10.1111/dme.13181
130. Redondo, A, Benach, J, Subirana, I, Martinez, JM, Muñoz, MA, Masiá, R, et al. Trends in the prevalence, awareness, treatment, and control of cardiovascular risk factors across educational level in the 1995-2005 period. Ann Epidemiol. (2011) 21:555–63. doi: 10.1016/j.annepidem.2011.02.008
131. Tsuchiya, K, and Demmer, RT. Citizenship status and prevalence of diagnosed and undiagnosed hypertension and diabetes among adults in the U.S., 2011–2016. Diabetes Care. (2021) 44:e38–9. doi: 10.2337/dc20-2453
132. Kalra, R, Parcha, V, Patel, N, Bhargava, A, Booker, KS, Arora, G, et al. Increased awareness, inadequate treatment, and poor control of cardiovascular risk factors in American young adults: 2005-2016. Eur J Prev Cardiol. (2021) 28:304–12. doi: 10.1177/2047487320905190
133. Lee, J, Kim, KH, Ahn, JC, Kim, JA, Lee, G, Son, JS, et al. Prevalence, awareness, treatment, and control of diabetes mellitus by depressive symptom severity: a cross-sectional analysis of NHANES 2011-2016. BMJ Open Diabetes Res Care. (2021) 9:e002268. doi: 10.1136/bmjdrc-2021-002268
134. He, S, Ryan, KA, Streeten, EA, McArdle, PF, Daue, M, Trubiano, D, et al. Prevalence, control, and treatment of diabetes, hypertension, and high cholesterol in the Amish. BMJ Open Diabetes Res Care. (2020) 8:e000912. doi: 10.1136/bmjdrc-2019-000912
135. Cheng, YJ, Kanaya, AM, Araneta, MRG, Saydah, SH, Kahn, HS, Gregg, EW, et al. Prevalence of diabetes by race and ethnicity in the United States, 2011-2016. JAMA. (2019) 322:2389–98. doi: 10.1001/jama.2019.19365
136. Bucholz, EM, Gooding, HC, and de Ferranti, SD. Awareness of cardiovascular risk factors in U.S. young adults aged 18-39 years. Am J Prev Med. (2018) 54:e67–77. doi: 10.1016/j.amepre.2018.01.022
137. Fisher-Hoch, SP, Vatcheva, KP, Rahbar, MH, and McCormick, JB. Undiagnosed diabetes and pre-diabetes in health disparities. PLoS One. (2015) 10:e0133135. doi: 10.1371/journal.pone.0133135
138. Parton, JM . Association between awareness, treatment, and control of diabetes and rural/urban access to care. Association between stroke risk factors and access to care. (2011) 47.
139. Cowie, CC, Rust, KF, Byrd-Holt, DD, Gregg, EW, Ford, ES, Geiss, LS, et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988–2006. Diabetes Care. (2010) 33:562–8. doi: 10.2337/dc09-1524
140. Cowie, CC, Rust, KF, Ford, ES, Eberhardt, MS, Byrd-Holt, DD, Li, C, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988–1994 and 2005–2006. Diabetes Care. (2009) 32:287–94. doi: 10.2337/dc08-1296
141. Thorpe, LE, Upadhyay, UD, Chamany, S, Garg, R, Mandel-Ricci, J, Kellerman, S, et al. Prevalence and control of diabetes and impaired fasting glucose in New York City. Diabetes Care. (2009) 32:57–62. doi: 10.2337/dc08-0727
142. Hertz, RP, Unger, AN, and Ferrario, CM. Diabetes, hypertension, and dyslipidemia in Mexican Americans and non-Hispanic whites. Am J Prev Med. (2006) 30:103–10. doi: 10.1016/j.amepre.2005.10.015
143. Menke, A, Casagrande, S, Geiss, L, and Cowie, CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. (2015) 314:1021–9. doi: 10.1001/jama.2015.10029
144. Schneiderman, N, Llabre, M, Cowie, CC, Barnhart, J, Carnethon, M, Gallo, LC, et al. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic community health study/study of Latinos (HCHS/SOL). Diabetes Care. (2014) 37:2233–9. doi: 10.2337/dc13-2939
145. Sims, M, Diez Roux, AV, Boykin, S, Sarpong, D, Gebreab, SY, Wyatt, SB, et al. The socioeconomic gradient of diabetes prevalence, awareness, treatment, and control among African Americans in the Jackson heart study. Ann Epidemiol. (2011) 21:892–8. doi: 10.1016/j.annepidem.2011.05.006
146. McDonald, M, Hertz, RP, Unger, AN, and Lustik, MB. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A Biol Sci Med Sci. (2009) 64:256–63. doi: 10.1093/gerona/gln016
147. Jaber, LA, Brown, MB, Hammad, A, Nowak, SN, Zhu, Q, Ghafoor, A, et al. Epidemiology of diabetes among Arab Americans. Diabetes Care. (2003) 26:308–13. doi: 10.2337/diacare.26.2.308
148. Hosseini, Z, Whiting, SJ, and Vatanparast, H. Type 2 diabetes prevalence among Canadian adults—dietary habits and sociodemographic risk factors. Appl Physiol Nutr Metab. (2019) 44:1099–104. doi: 10.1139/apnm-2018-0567
149. Rosella, LC, Lebenbaum, M, Fitzpatrick, T, Zuk, A, and Booth, GL. Prevalence of prediabetes and undiagnosed diabetes in Canada (2007–2011) according to fasting plasma glucose and HbA1c screening criteria. Diabetes Care. (2015) 38:1299–305. doi: 10.2337/dc14-2474
150. Leiter, LA, Barr, A, Bélanger, A, Lubin, S, Ross, SA, Tildesley, HD, et al. Diabetes screening in Canada (DIASCAN) study: prevalence of undiagnosed diabetes and glucose intolerance in family physician offices. Diabetes Care. (2001) 24:1038–43. doi: 10.2337/diacare.24.6.1038
151. Young, TK . Undiagnosed diabetes burden and significance in the Canadian population. Diabetes and Cardiovascular Disease. Springer; (2001): 7–10.
152. Leong, A, Dasgupta, K, Chiasson, J-L, and Rahme, E. Estimating the population prevalence of diagnosed and undiagnosed diabetes using health administrative data. Can J Diabetes. (2013) 37:S76–7. doi: 10.1016/j.jcjd.2013.08.234
153. Vonglokham, M, Kounnavong, S, Sychareun, V, Pengpid, S, and Peltzer, K. Prevalence and social and health determinants of pre-diabetes and diabetes among adults in Laos: a cross-sectional national population-based survey, 2013. Trop Med Int Health. (2019) 24:65–72. doi: 10.1111/tmi.13164
154. Stanifer, JW, Cleland, CR, Makuka, GJ, Egger, JR, Maro, V, Maro, H, et al. Prevalence, risk factors, and complications of diabetes in the Kilimanjaro region: a population-based study from Tanzania. PLoS One. (2016) 11:e0164428. doi: 10.1371/journal.pone.0164428
155. Ruhembe, CC, Mosha, TC, and Nyaruhucha, CN. Prevalence and awareness of type 2 diabetes mellitus among adult population in Mwanza city, Tanzania. Tanzan Health Res Bull. (2014) 16:89–97. doi: 10.4314/thrb.v16i2.4
156. Silva-Matos, C, Gomes, A, Azevedo, A, Damasceno, A, Prista, A, and Lunet, N. Diabetes in Mozambique: prevalence, management and healthcare challenges. Diabetes Metab. (2011) 37:237–44. doi: 10.1016/j.diabet.2010.10.006
157. Islam Saeed, KM . Diabetes mellitus among adults in Herat, Afghanistan: a cross-sectional study. Cent Asian J Glob Health. (2017) 6:271. doi: 10.5195/cajgh.2017.271
158. Selcuk, KT, Sozmen, MK, and Togrul, BU. Diabetes prevalence and awareness in adults in the Balcova district in Turkey. Turk J Med Sci. (2015) 45:1220–7. doi: 10.3906/sag-1312-62
159. Satman, I, Yilmaz, T, Sengül, A, Salman, S, Salman, F, Uygur, S, et al. Population-based study of diabetes and risk characteristics in Turkey: results of the Turkish diabetes epidemiology study (TURDEP). Diabetes Care. (2002) 25:1551–6. doi: 10.2337/diacare.25.9.1551
160. Albache, N, Al Ali, R, Rastam, S, Fouad, FM, Mzayek, F, and Maziak, W. Epidemiology of type 2 diabetes mellitus in Aleppo. Syria J Diabetes. (2010) 2:85–91. doi: 10.1111/j.1753-0407.2009.00063.x
161. Bahijri, SM, Jambi, HA, Al Raddadi, RM, Ferns, G, and Tuomilehto, J. The prevalence of diabetes and Prediabetes in the adult population of Jeddah, Saudi Arabia--a community-based survey. PLoS One. (2016) 11:e0152559. doi: 10.1371/journal.pone.0152559
162. al-Rubeaan, K, al-Manaa, HA, Khoja, TA, Ahmad, NA, al-Sharqawi, AH, Siddiqui, K, et al. Epidemiology of abnormal glucose metabolism in a country facing its epidemic: SAUDI-DM study. J Diabetes. (2015) 7:622–32. doi: 10.1111/1753-0407.12224
163. al-Rubeaan, K, al-Manaa, H, Khoja, T, Ahmad, N, al-Sharqawi, A, Siddiqui, K, et al. The Saudi abnormal glucose metabolism and diabetes impact study (SAUDI-DM). Ann Saudi Med. (2014) 34:465–75. doi: 10.5144/0256-4947.2014.465
164. el Bcheraoui, C, Basulaiman, M, Tuffaha, M, Daoud, F, Robinson, M, Jaber, S, et al. Status of the diabetes epidemic in the Kingdom of Saudi Arabia, 2013. Int J Public Health. (2014) 59:1011–21. doi: 10.1007/s00038-014-0612-4
165. Al-Baghli, NA, Al-Ghamdi, AJ, Al-Turki, KA, Al Elq, AH, El-Zubaier, AG, and Bahnassy, A. Prevalence of diabetes mellitus and impaired fasting glucose levels in the Eastern Province of Saudi Arabia: results of a screening campaign. Singapore Med J. (2010) 51:923–30.
166. al-Nozha, MM, al-Maatouq, MA, al-Mazrou, YY, al-Harthi, SS, Arafah, MR, Khalil, MZ, et al. Diabetes mellitus in Saudi Arabia. Saudi Med J. (2004) 25:1603–10.
167. Al-Lawati, J, Al Riyami, A, Mohammed, A, and Jousilahti, P. Increasing prevalence of diabetes mellitus in Oman. Diabet Med. (2002) 19:954–7. doi: 10.1046/j.1464-5491.2002.00818.x
168. Al Riyami, A, Elaty, A, Attia, M, and Morsi, M. Oman world health survey: part 1 methodology, sociodemographic profile and epidemiology of non-communicable diseases in Oman. Oman Med J. (2012) 100:1–19.
169. Ismail, H, Omar, MA, Saminathan, TA, Muhammad Yusof, MF, Mohd Zaki, NA, Lim, KK, et al. Prevalence of undiagnosed type 2 diabetes mellitus and its associated factors among the Malaysian population: the 2015 National Health and morbidity survey, Malaysia. Global J Health Sci. (2018) 10:153. doi: 10.5539/gjhs.v10n8p153
170. Yen, ST, Tan, AKG, and Mustapha, FI. Awareness of diabetes, hypertension, and hypercholesterolemia in Malaysia. J Diabetes. (2017) 9:874–83. doi: 10.1111/1753-0407.12502
171. Ho, BK, Jasvindar, K, Gurpreet, K, Ambigga, D, Suthahar, A, Cheong, SM, et al. Prevalence, awareness, treatment and control of diabetes mellitus among the elderly: the 2011 National Health and morbidity survey, Malaysia. Malaysian Family Physician. (2014) 9:12–9.
172. Rampal, S, Rampal, L, Rahmat, R, Azhar Md Zain,, Yee Guan Yap,, Mohamed, M, et al. Variation in the prevalence, awareness, and control of diabetes in a multiethnic population: a nationwide population study in Malaysia. Asia Pac J Public Health. (2010) 22:194–202. doi: 10.1177/1010539509334816
173. Pramono, LA, Setiati, S, Soewondo, P, Subekti, I, Adisasmita, A, Kodim, N, et al. Prevalence and predictors of undiagnosed diabetes mellitus in Indonesia. Age. (2010) 46:100.
174. Barreto, M, Kislaya, I, Gaio, V, Rodrigues, AP, Santos, AJ, Namorado, S, et al. Prevalence, awareness, treatment and control of diabetes in Portugal: results from the first National Health examination survey (INSEF 2015). Diabetes Res Clin Pract. (2018) 140:271–8. doi: 10.1016/j.diabres.2018.03.052
175. Gardete-Correia, L, Boavida, JM, Raposo, JF, Mesquita, AC, Fona, C, Carvalho, R, et al. First diabetes prevalence study in Portugal: PREVADIAB study. Diabet Med. (2010) 27:879–81. doi: 10.1111/j.1464-5491.2010.03017.x
176. Bikbov, MM, Fayzrakhmanov, RR, Kazakbaeva, GM, Zainullin, RM, Arslangareeva, II, Gilmanshin, TR, et al. Prevalence, awareness and control of diabetes in Russia: the Ural eye and medical study on adults aged 40+ years. PLoS One. (2019) 14:e0215636. doi: 10.1371/journal.pone.0215636
177. Dedov, I, Shestakova, M, Benedetti, MM, Simon, D, Pakhomov, I, and Galstyan, G. Prevalence of type 2 diabetes mellitus (T2DM) in the adult Russian population (NATION study). Diabetes Res Clin Pract. (2016) 115:90–5. doi: 10.1016/j.diabres.2016.02.010
178. Cunningham-Myrie, C, Younger-Coleman, N, Tulloch-Reid, M, McFarlane, S, Francis, D, Ferguson, T, et al. Diabetes mellitus in Jamaica: sex differences in burden, risk factors, awareness, treatment and control in a developing country. Trop Med Int Health. (2013) 18:1365–78. doi: 10.1111/tmi.12190
179. Faeh, D, William, J, Tappy, L, Ravussin, E, and Bovet, P. Prevalence, awareness and control of diabetes in the Seychelles and relationship with excess body weight. BMC Public Health. (2007) 7:163.
180. Gyawali, B, Hansen, MRH, Povlsen, MB, Neupane, D, Andersen, PK, McLachlan, CS, et al. Awareness, prevalence, treatment, and control of type 2 diabetes in a semi-urban area of Nepal: findings from a cross-sectional study conducted as a part of COBIN-D trial. PLoS One. (2018) 13:e0206491. doi: 10.1371/journal.pone.0206491
181. Chhetri, MR, and Chapman, RS. Prevalence and determinants of diabetes among the elderly population in the Kathmandu Valley of Nepal. Nepal Med Coll J. (2009) 11:34–8.
182. Aekplakorn, W, Chariyalertsak, S, Kessomboon, P, Sangthong, R, Inthawong, R, Putwatana, P, et al. Prevalence and Management of Diabetes and Metabolic Risk Factors in Thai adults: the Thai National Health Examination Survey IV, 2009. Diabetes Care. (2011) 34:1980–5. doi: 10.2337/dc11-0099
183. Porapakkham, Y, Pattaraarchachai, J, and Aekplakorn, W. Prevalence, awareness, treatment and control of hypertension and diabetes mellitus among the elderly: the 2004 National Health Examination Survey III, Thailand. Singapore Med J. (2008) 49:868–73.
184. Aekplakorn, W, Abbott-Klafter, J, Premgamone, A, Dhanamun, B, Chaikittiporn, C, Chongsuvivatwong, V, et al. Prevalence and Management of Diabetes and Associated Risk Factors by regions of Thailand: third National Health Examination Survey 2004. Diabetes Care. (2007) 30:2007–12. doi: 10.2337/dc06-2319
185. Aekplakorn, W, Stolk, RP, Neal, B, Suriyawongpaisal, P, Chongsuvivatwong, V, Cheepudomwit, S, et al. The prevalence and Management of Diabetes in Thai adults: the international collaborative study of cardiovascular disease in Asia. Diabetes Care. (2003) 26:2758–63. doi: 10.2337/diacare.26.10.2758
186. Pan, WH, Yeh, WT, Chang, HY, Hwu, CM, and Ho, LT. Prevalence and awareness of diabetes and mean fasting glucose by age, sex, and region: results from the nutrition and health survey in Taiwan, 1993-1996. Diabet Med. (2003) 20:182–5. doi: 10.1046/j.1464-5491.2003.00772.x
187. Supiyev, A, Kossumov, A, Kassenova, A, Nurgozhin, T, Zhumadilov, Z, Peasey, A, et al. Diabetes prevalence, awareness and treatment and their correlates in older persons in urban and rural population in the Astana region, Kazakhstan. Diabetes Res Clin Pract Suppl. (2016) 112:6–12. doi: 10.1016/j.diabres.2015.11.011
188. Makusidi, MA, Liman, HM, Yakubu, A, Isah, MD, Jega, RM, Adamu, H, et al. Prevalence of non-communicable diseases and its awareness among inhabitants of Sokoto metropolis: outcome of a screening program for hypertension, obesity, diabetes mellitus and overt proteinuria. Arab J Nephrol Transplant. (2013) 6:189–91.
189. Ben Romdhane, H, Ali, SB, Aissi, W, Traissac, P, Aounallah-Skhiri, H, Bougatef, S, et al. Prevalence of diabetes in northern African countries: the case of Tunisia. BMC Public Health. (2014) 14:86. doi: 10.1186/1471-2458-14-86
190. Bouguerra, R, Alberti, H, Salem, LB, Rayana, CB, Atti, JE, Gaigi, S, et al. The global diabetes pandemic: the Tunisian experience. Eur J Clin Nutr. (2007) 61:160–5. doi: 10.1038/sj.ejcn.1602478
191. Colagiuri, S, Colagiuri, R, Na’ati, S, Muimuiheata, S, Hussain, Z, and Palu, T. The prevalence of diabetes in the Kingdom of Tonga. Diabetes Care. (2002) 25:1378–83. doi: 10.2337/diacare.25.8.1378
192. Mohamed, SF, Mwangi, M, Mutua, MK, Kibachio, J, Hussein, A, Ndegwa, Z, et al. Prevalence and factors associated with pre-diabetes and diabetes mellitus in Kenya: results from a national survey. BMC Public Health. (2018) 18:1215. doi: 10.1186/s12889-018-6053-x
193. Oti, SO, van de Vijver, SJ, Agyemang, C, and Kyobutungi, C. The magnitude of diabetes and its association with obesity in the slums of Nairobi, Kenya: results from a cross-sectional survey. Trop Med Int Health. (2013) 18:1520–30. doi: 10.1111/tmi.12200
194. Huang, OS, Tay, WT, Tai, ES, Wang, JJ, Seang-Mei, SM, Jeganathan, VSE, et al. Lack of awareness amongst community patients with diabetes and diabetic retinopathy: the Singapore Malay eye study. Ann Acad Med Singap. (2009) 38:1048–55. doi: 10.47102/annals-acadmedsg.V38N12p1048
195. Man, REK, Gan, AHW, Fenwick, EK, Gan, ATL, Gupta, P, Sabanayagam, C, et al. Prevalence, determinants and association of unawareness of diabetes, hypertension and hypercholesterolemia with poor disease control in a multi-ethnic Asian population without cardiovascular disease. Popul Health Metrics. (2019) 17:17. doi: 10.1186/s12963-019-0197-5
196. Pedro, JM, Brito, M, and Barros, H. Prevalence, awareness, treatment and control of hypertension, diabetes and hypercholesterolaemia among adults in Dande municipality, Angola. Cardiovasc J Afr. (2018) 29:73–81.
197. Katte, JC, Dzudie, A, Sobngwi, E, Mbong, EN, Fetse, GT, Kouam, CK, et al. Coincidence of diabetes mellitus and hypertension in a semi-urban Cameroonian population: a cross-sectional study. BMC Public Health. (2014) 14:696. doi: 10.1186/1471-2458-14-696
198. Eltom, MA, Babiker Mohamed, AH, Elrayah-Eliadarous, H, Yassin, K, Noor, SK, Elmadhoun, WM, et al. Increasing prevalence of type 2 diabetes mellitus and impact of ethnicity in North Sudan. Diabetes Res Clin Pract. (2018) 136:93–9. doi: 10.1016/j.diabres.2017.11.034
199. Elmadhoun, WM, Noor, SK, Ibrahim, AAA, Bushara, SO, and Ahmed, MH. Prevalence of diabetes mellitus and its risk factors in urban communities of North Sudan: population-based study: 北苏丹城市人群中的糖尿病患病率及其危险因素: 基于人群的研究. J Diabetes. (2016) 8:839–46. doi: 10.1111/1753-0407.12364
200. Djrolo, F, Adoukonou, T, Houehanou, C, Houinato, JD, and Houinato, D. Diabetes in Borgou Department in Benin: prevalence and associated factors. Journal of Diabetes Mellitus. (2015) 5:90.
201. Bahendeka, S, Wesonga, R, Mutungi, G, Muwonge, J, Neema, S, and Guwatudde, D. Prevalence and correlates of diabetes mellitus in Uganda: a population-based national survey. Trop Med Int Health. (2016) 21:405–16. doi: 10.1111/tmi.12663
202. Otgontuya, D, Oum, S, Palam, E, Rani, M, and Buckley, BS. Individual-based primary prevention of cardiovascular disease in Cambodia and Mongolia: early identification and management of hypertension and diabetes mellitus. BMC Public Health. (2012) 12:254.
203. Dereje, N, Earsido, A, Temam, L, and Abebe, A. Prevalence and associated factors of diabetes mellitus in hosanna town, southern Ethiopia. Ann Glob Health. (2020) 86:18. doi: 10.5334/aogh.2663
204. Endris, T, Worede, A, and Asmelash, D. Prevalence of diabetes mellitus, prediabetes and its associated factors in Dessie town, Northeast Ethiopia: a community-based study. Diabetes Metabolic Syndrome Obesity. (2019) 12:2799. doi: 10.2147/DMSO.S225854
205. Bantie, GM, Wondaye, AA, Arike, EB, Melaku, MT, Ejigu, ST, Lule, A, et al. Prevalence of undiagnosed diabetes mellitus and associated factors among adult residents of Bahir Dar city, Northwest Ethiopia: a community-based cross-sectional study. BMJ Open. (2019) 9:e030158. doi: 10.1136/bmjopen-2019-030158
206. Aynalem, SB, and Zeleke, AJ. Prevalence of diabetes mellitus and its risk factors among individuals aged 15 years and above in Mizan-Aman town, Southwest Ethiopia, 2016: a cross sectional study. Int J Endocrinol. (2018) 2018:9317987. doi: 10.1155/2018/9317987
207. Animaw, W, and Seyoum, Y. Increasing prevalence of diabetes mellitus in a developing country and its related factors. PLoS One. (2017) 12:e0187670. doi: 10.1371/journal.pone.0187670
208. Seifu, W, Woldemichael, K, and Tsehaineh, B. Prevalence and risk factors for diabetes mellitus and impaired fasting glucose among adults aged 15–64 years in Gilgel gibe field research center, Southwest Ethiopia, 2013: through a WHO step wise approach. MOJ Public Health. (2015) 2:00035.
209. Abebe, SM, Berhane, Y, Worku, A, and Assefa, A. Diabetes mellitus in north West Ethiopia: a community based study. BMC Public Health. (2014) 14:1–8. doi: 10.1186/1471-2458-14-97
210. Irazola, V, Rubinstein, A, Bazzano, L, Calandrelli, M, Chung-Shiuan, C, Elorriaga, N, et al. Prevalence, awareness, treatment and control of diabetes and impaired fasting glucose in the southern cone of Latin America. PLoS One. (2017) 12:e0183953. doi: 10.1371/journal.pone.0183953
211. Matthys, B, Steinmann, P, Karimova, G, Tagoev, T, Abdurahmonov, A, Costa, J, et al. Prevalence of impaired glucose metabolism and potential predictors: a rapid appraisal among >/= 45 years old residents of southern Tajikistan. J Diabetes. (2015) 7:540–7. doi: 10.1111/1753-0407.12214
212. Lerner, AG, Bernabe-Ortiz, A, Gilman, RH, Smeeth, L, and Miranda, JJ. The "rule of halves" does not apply in Peru: awareness, treatment, and control of hypertension and diabetes in rural, urban, and rural-to-urban migrants. Crit Pathw Cardiol. (2013) 12:53–8.
213. Seclen, SN, Rosas, ME, Arias, AJ, Huayta, E, and Medina, CA. Prevalence of diabetes and impaired fasting glucose in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diab Res Care. (2015) 3:e000110. doi: 10.1136/bmjdrc-2015-000110
214. Mc Donald P, AJ, Montenegro G, JA, Cruz G, CE, Moreno de Rivera, AL, and Cumbrera O, A. Prevalence, sociodemographic distribution, treatment and control of diabetes mellitus in Panama. Diabetol Metab Syndr. (2013) 5:69. doi: 10.1186/1758-5996-5-69
215. Basto-Abreu, A, López-Olmedo, N, Rojas-Martínez, R, Aguilar-Salinas, CA, de la Cruz-Góngora, VV, Rivera-Dommarco, J, et al. Prevalence of diabetes and glycemic control in Mexico: national results from 2018 and 2020. Salud Publica Mex. (2021) 63:725–33. doi: 10.21149/12842
216. Aguilar-Ramirez, D, Alegre-Díaz, J, Gnatiuc, L, Ramirez-Reyes, R, Wade, R, Hill, M, et al. Changes in the diagnosis and Management of Diabetes in Mexico City between 1998–2004 and 2015–2019. Diabetes Care. (2021) 44:944–51. doi: 10.2337/dc20-2276
217. Barquera, S, Hernández-Alcaraz, C, Jáuregui, A, Medina, C, Mendoza-Herrera, K, Pedroza-Tobias, A, et al. Diabetes awareness, treatment, and control among Mexico City residents. Diabetology. (2021) 2:16–30. doi: 10.3390/diabetology2010002
218. Villalpando, S, de la Cruz, V, Rojas, R, Shamah-Levy, T, Ávila, MA, Gaona, B, et al. Prevalence and distribution of type 2 diabetes mellitus in Mexican adult population: a probabilistic survey. Salud Publica Mex. (2010) 52:S19–26. doi: 10.1590/S0036-36342010000700005
219. Vecino-Ortiz, AI, Trujillo, AJ, and Ruiz, F. Undetected diabetes in Colombia. Int J Public Policy. (2012) 8:362–73.
220. Alkandari, A, Longenecker, JC, Barengo, NC, Alkhatib, A, Weiderpass, E, al-Wotayan, R, et al. The prevalence of pre-diabetes and diabetes in the Kuwaiti adult population in 2014. Diabetes Res Clin Pract. (2018) 144:213–23. doi: 10.1016/j.diabres.2018.08.016
221. Bener, A, Zirie, M, Janahi, IM, Al-Hamaq, AOAA, Musallam, M, and Wareham, NJ. Prevalence of diagnosed and undiagnosed diabetes mellitus and its risk factors in a population-based study of Qatar. Diabetes Res Clin Pract. (2009) 84:99–106. doi: 10.1016/j.diabres.2009.02.003
222. Leahy, S, O’ Halloran, AM, O’ Leary, N, Healy, M, McCormack, M, Kenny, RA, et al. Prevalence and correlates of diagnosed and undiagnosed type 2 diabetes mellitus and pre-diabetes in older adults: findings from the Irish longitudinal study on ageing (TILDA). Diabetes Res Clin Pract. (2015) 110:241–9. doi: 10.1016/j.diabres.2015.10.015
223. Schmidt, MI, Hoffmann, JF, de Fátima Sander Diniz, M, Lotufo, PA, Griep, RH, Bensenor, IM, et al. High prevalence of diabetes and intermediate hyperglycemia – the Brazilian longitudinal study of adult health (ELSA-Brasil). Diabetol Metab Syndr. (2014) 6:123. doi: 10.1186/1758-5996-6-123
224. Malerbi, DA, and Franco, LJBrazilian Cooperative Group on the Study of Diabetes Prevalence. Multicenter study of the prevalence of diabetes mellitus and impaired glucose tolerance in the urban Brazilian population aged 30–69 yr. Diabetes Care. (1992) 15:1509–16. doi: 10.2337/diacare.15.11.1509
225. Mansour, AA, Al-Maliky, AA, Kasem, B, Jabar, A, and Mosbeh, KA. Prevalence of diagnosed and undiagnosed diabetes mellitus in adults aged 19 years and older in Basrah, Iraq. Diabetes Metabolic Syndrome Obesity. (2014) 7:139. doi: 10.2147/DMSO.S59652
226. Mansour, AA, Wanoose, HL, Hani, I, Abed-Alzahrea, A, and Wanoose, HL. Diabetes screening in Basrah, Iraq: a population-based cross-sectional study. Diabetes Res Clin Pract. (2008) 79:147–50.
227. Abdul-Rahim, HF, Husseini, A, Giacaman, R, Jervell, J, and Bjertness, E. Diabetes mellitus in an urban Palestinian population: prevalence and associated factors. East Mediterr Health J. (2001) 7:67–78. doi: 10.26719/2001.7.1-2.67
228. Husseini, A . Prevalence of diabetes mellitus and impaired glucose tolerance in a rural Palestinian population. EMHJ-Eastern Mediterranean Health J. (2000) 6:1039–45. doi: 10.26719/2000.6.5-6.1039
229. Saadi, H, Nagelkerke, N, Al-Kaabi, J, Afandi, B, Al-Maskari, F, and Kazam, E. Screening strategy for type 2 diabetes in the United Arab Emirates. Asia Pac J Public Health. (2010) 22:54s–9s. doi: 10.1177/1010539510373036
230. Malik, M, Bakir, A, Abi Saab, B, Roglic, G, and King, H. Glucose intolerance and associated factors in the multi-ethnic population of the United Arab Emirates: results of a national survey. Diabetes Res Clin Pract. (2005) 69:188–95. doi: 10.1016/j.diabres.2004.12.005
231. Meiloud, G, Arfa, I, Kefi, R, Abdelhamid, I, Veten, F, Lasram, K, et al. Type 2 diabetes in Mauritania: prevalence of the undiagnosed diabetes, influence of family history and maternal effect. Prim Care Diabetes. (2013) 7:19–24. doi: 10.1016/j.pcd.2012.12.002
232. Metelko, Ž, Pavlić-Renar, I, Poljičanin, T, Szirovitza, L, and Turek, S. Prevalence of diabetes mellitus in Croatia. Diabetes Res Clin Pract. (2008) 81:263–7. doi: 10.1016/j.diabres.2008.04.016
233. Coppell, KJ, Mann, JI, Williams, SM, Jo, E, Drury, PL, Miller, JC, et al. Prevalence of diagnosed and undiagnosed diabetes and prediabetes in New Zealand: findings from the 2008/09 adult nutrition survey. NZ Med J. (2013) 126:23–42.
234. Sundborn, G, Metcalf, P, Scragg, R, Schaaf, D, Dyall, L, Gentles, D, et al. Ethnic differences in the prevalence of new and known diabetes mellitus, impaired glucose tolerance and impaired fasting glucose. Diabetes heart and health survey (DHAH) 2002-2003, Auckland New Zealand. New Zealand Med J. (2007) 120:U2607.
235. Glatthaar, C, Welborn, TA, Stenhouse, NS, and Garcia-Webb, P. Diabetes and impaired glucose tolerance: a prevalence estimate based on the Busselton 1981 survey. Med J Aust. (1985) 143:436–40. doi: 10.5694/j.1326-5377.1985.tb123131.x
236. Goto, M, Goto, A, Ikeda, N, Noda, H, Shibuya, K, and Noda, M. Factors associated with untreated diabetes: analysis of data from 20,496 participants in the Japanese National Health and nutrition survey. PLoS One. (2015) 10:e0118749. doi: 10.1371/journal.pone.0118749
237. Sekikawa, A, Tominaga, M, Takahashi, K, Eguchi, H, Igarashi, M, Ohnuma, H, et al. Prevalence of diabetes and impaired glucose tolerance in Funagata area, Japan. Diabetes Rev. (1993) 16:570–4. doi: 10.2337/diacare.16.4.570
238. Boo, S, Yoon, YJ, and Oh, H. Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database: a cross-sectional analysis. Medicine. (2018) 97:e13713
239. Kim, HJ, Kim, Y, Cho, Y, Jun, B, and Oh, KW. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and nutrition examination survey, 1998-2012. Int J Cardiol. (2014) 174:64–72. doi: 10.1016/j.ijcard.2014.03.163
240. Cho, EH, Shin, D, Cho, KH, and Hur, J. Prevalences and Management of Diabetes and pre-diabetes among Korean teenagers and young adults: results from the Korea National Health and nutrition examination survey 2005-2014. J Korean Med Sci. (2017) 32:1984–90. doi: 10.3346/jkms.2017.32.12.1984
241. Lee, J-w, Kang, H-T, Lim, H-J, and Park, B. Trends in diabetes prevalence among Korean adults based on Korean National Health and nutrition examination surveys III–VI. Diabetes Res Clin Pract. (2018) 138:57–65. doi: 10.1016/j.diabres.2018.01.013
242. Kim, SM, Lee, JS, Lee, J, Na, JK, Han, JH, Yoon, DK, et al. Prevalence of diabetes and impaired fasting glucose in Korea: Korean National Health and nutrition survey 2001. Diabetes Care. (2006) 29:226–31. doi: 10.2337/diacare.29.02.06.dc05-0481
243. Avilés-Santa, ML, Monroig-Rivera, A, Soto-Soto, A, and Lindberg, NM. Current state of diabetes mellitus prevalence, awareness, treatment, and control in Latin America: challenges and innovative solutions to improve health outcomes across the continent. Curr Diab Rep. (2020) 20:62.
244. Li, MZ, Su, L, Liang, BY, Tan, JJ, Chen, Q, Long, JX, et al. Trends in prevalence, awareness, treatment, and control of diabetes mellitus in mainland China from 1979 to 2012. Int J Endocrinol. (2013) 2013:753150. doi: 10.1155/2013/753150
245. Mohammadian Khonsari, N, Shahrestanaki, E, Ejtahed, HS, Djalalinia, S, Sheidaei, A, Hakak-Zargar, B, et al. Long-term trends in hypertension prevalence, awareness, treatment, and control rate in the Middle East and North Africa: a systematic review and meta-analysis of 178 population-based studies. Curr Hypertens Rep. (2021) 23:41. doi: 10.1007/s11906-021-01159-0
246. Long-term and recent trends in hypertension awareness . Treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. (2019) 394:639–51. doi: 10.1016/S0140-6736(19)31145-6
247. Hashemzadeh, M, Rahimi, A, Zare-Farashbandi, F, Alavi-Naeini, AM, and Daei, A. Transtheoretical model of health behavioral change: a systematic review. Iran J Nurs Midwifery Res. (2019) 24:83–90. doi: 10.4103/ijnmr.IJNMR_94_17
248. Kvarnström, K, Westerholm, A, Airaksinen, M, and Liira, H. Factors contributing to medication adherence in patients with a chronic condition: A Scoping Review of Qualitative Research. Pharmaceutics. (2021) 13:1100. doi: 10.3390/pharmaceutics13071100
249. Ong, SE, Koh, JJK, Toh, SES, Chia, KS, Balabanova, D, McKee, M, et al. Assessing the influence of health systems on type 2 diabetes mellitus awareness, treatment, adherence, and control: a systematic review. PLoS One. (2018) 13:e0195086. doi: 10.1371/journal.pone.0195086
250. Yin, J, Yeung, R, Luk, A, Tutino, G, Zhang, Y, Kong, A, et al. Gender, diabetes education, and psychosocial factors are associated with persistent poor glycemic control in patients with type 2 diabetes in theJointAsiaDiabetesEvaluation (JADE) program. J Diabetes. (2016) 8:109–19. doi: 10.1111/1753-0407.12262
251. Khattab, M, Khader, YS, Al-Khawaldeh, A, and Ajlouni, K. Factors associated with poor glycemic control among patients with type 2 diabetes. J Diabetes Complicat. (2010) 24:84–9. doi: 10.1016/j.jdiacomp.2008.12.008
252. Dupre, ME, Silberberg, M, Willis, JM, and Feinglos, MN. Education, glucose control, and mortality risks among US older adults with diabetes. Diabetes Res Clin Pract. (2015) 107:392–9. doi: 10.1016/j.diabres.2014.12.013
253. Talfournier, J, Bitu, J, Paquet, C, Gobron, C, Guillausseau, PJ, Hugon, J, et al. Relationship between blood pressure, cognitive function and education level in elderly patients with diabetes: a preliminary study. Diabetes Metab. (2013) 39:418–23. doi: 10.1016/j.diabet.2013.02.008
254. Houghton, N, Bascolo, E, and Riego, A. Socioeconomic inequalities in access barriers to seeking health services in four Latin American countries. Rev Panam Salud Publica. (2020) 44:e11. doi: 10.26633/RPSP.2020.11
255. Lopez Stewart, G, Tambascia, M, Rosas Guzmán, J, Etchegoyen, F, Ortega Carrión, J, and Artemenko, S. Control of type 2 diabetes mellitus among general practitioners in private practice in nine countries of Latin America. Rev Panam Salud Publica. (2007) 22:12–20. doi: 10.1590/s1020-49892007000600002
Keywords: diabetes, awareness, treatment, control, systematic review, meta-analysis
Citation: Shahrestanaki E, Mohammadian Khonsari N, Seif E, Baygi F, Ejtahed H-S, Sheidaei A, Djalalinia S, Magliano DJ and Qorbani M (2024) The worldwide trend in diabetes awareness, treatment, and control from 1985 to 2022: a systematic review and meta-analysis of 233 population-representative studies. Front. Public Health. 12:1305304. doi: 10.3389/fpubh.2024.1305304
Edited by:
Khalid Siddiqui, King Saud University, Saudi ArabiaReviewed by:
Daniela Lopes Gomes, Federal University of Pará, BrazilKhalid Hattaf, Centre Régional des Métiers de l’Education et de la Formation (CRMEF), Morocco
Copyright © 2024 Shahrestanaki, Mohammadian Khonsari, Seif, Baygi, Ejtahed, Sheidaei, Djalalinia, Magliano and Qorbani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mostafa Qorbani, TXFvcmJhbmkxMzc5QHlhaG9vLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Ehsan Shahrestanaki
Ehsan Shahrestanaki Nami Mohammadian Khonsari
Nami Mohammadian Khonsari Ehsan Seif
Ehsan Seif Fereshteh Baygi
Fereshteh Baygi Hanieh-Sadat Ejtahed
Hanieh-Sadat Ejtahed Ali Sheidaei
Ali Sheidaei Shirin Djalalinia
Shirin Djalalinia Dianna J. Magliano8,9
Dianna J. Magliano8,9 Mostafa Qorbani
Mostafa Qorbani