- 1School of Public Health, Wuhan University, Wuhan, China
- 2Jiangxi Provincial People's Hospital, The First Affiliated Hospital of Nanchang Medical College, Nanchang, China
Background: One of the biggest challenges facing older adults is cognitive decline and social participation has always been considered a protective factor. However, it is not clear whether social participation predicts cognitive function in this population, rather than depressive symptoms, self-reported health, and activities of daily life, with sufficient capacity to detect unique effects.
Methods: This study included adults aged 45 and above in China (N = 5,258) who participated in a large national older adult health survey and provided data from 2011, 2013, 2015, and 2018. The unique associations between the predictors of social participation and cognitive function over time and context were evaluated in the Latent Growth Model (LGM).
Results: Among the 5,258 participants in our study, an overall cognitive decline was observed. Social participation predicts two dimensions of cognitive function, with a degree of impact comparable to depressive symptoms, self-reported health, and activities of daily life. Among them, social participation exhibits a noteworthy prognostic impact on episodic memory during the same period. The regression coefficient is approximately 0.1 (p < 0.05) after controlling other mixed variables (depressive symptoms, self-reported health, and activities of daily life). In contrast, social participation is also a significant predictor of mental intactness in the same period, with a regression coefficient of 0.06 (p < 0.05), even if all mixed variables are controlled.
Conclusion: Over time, the correlation strength of social participation is comparable to other recognized cognitive function prediction indicators, indicating that promoting social participation among middle-aged and older Chinese adults is a meaningful way to improve cognitive function degradation, which has important policy and practical significance.
1 Introduction
In 2020, the population of China aged 65 and above exceeded 190.6 million, accounting for 13.5% of the total population (1). According to official forecast data, the olde adult population aged 65 and above in China will reach approximately 330 million by 2050 (1, 2). With the deepening of population aging, the scale of cognitive dysfunction in older adults is also increasing, with a prevalence rate of 15.5% (3). Cognitive function refers to the advanced function of the cerebral cortex in processing and understanding received information, determined by various neural, psychological, and emotional factors, and is crucial for memory storage, emotional control, and decision-making (4, 5). In the process of aging, once cognitive impairment becomes severe, it can develop into neurodegenerative diseases such as Alzheimer’s disease, seriously reducing the quality of life of older adults. Furthermore, the demand for treatment and rehabilitation will also increase significantly, and the intervention of family and social resources is urgently needed (6).
Social participation refers to the provision of accompanying activities for individuals to interact with others in society (7, 8). It is an important contributor to the health and well-being outcomes of older adults and one of the three pillars of the World Health Organization’s (WHO) policy to promote active aging societies. Due to its popularity, low cost, and expected benefits for mental health, it has attracted much attention (9). Previous studies have shown that the social participation rate of older adults in China ranges from 45.90 to 53.32% (10–14). There are two main theories about the relationship between social participation and cognitive function: the use and disuse theory suggests that a decrease in social participation leads to cognitive decline of the brain, while a stimulated mind can improve cognitive function (15). Therefore, cognitive decline can be prevented in old age through participation in a variety of mental and physical activities. Especially when cognitive abilities begin to decline, external stimulation is more important for older adults. Social identity theory holds that social participation can enable individuals to acquire the identity of a being member of a certain group (16, 17). This identity influences the individual’s values, emotions, and health-related behaviors and provides the individual with social resources and support that can help improve the individual’s cognitive function.
Some empirical studies provide support for the above theory. The findings of James et al. suggest that social activities are related to cognition throughout life, especially among older adults (18). For example, traditional Chinese social participation activities such as Tai Chi and Qing Kung can help maintain cognitive function among older adults in China (19–21). Moreover, a population-based longitudinal study conducted by Glei showed that participating in volunteer activities and socializing with friends can help maintain the cognitive function of older adults (22). In addition, there have been a few observational studies and studies based on pathophysiological mechanisms, indicating a possible reverse association between social participation and cognitive function. For example, a pathologically controlled study suggests that individuals in the preclinical stages of long-term dementia might be more likely to avoid participating in cognitive activities than their healthy peers (23). An Israeli study of adults also found a similar bidirectional association result (24). However, the current academic mainstream studies still regard the decrease in social activity participation as the cause rather than the result of cognitive decline (25), especially given the low proportion and single form of social participation of older adults in China, the inadequate construction of the community for older adults, and the increasing proportion of older adults living alone year by year (26, 27). Therefore, it is necessary to identify the impact of social participation over time on the cognitive function of middle-aged and older Chinese adults.
In previous studies, many factors have been associated with cognitive decline in older adults (28). Although most existing studies focus on the genetic and biological determinants, these findings create more space for the role of social factors in the decline of cognitive function in older adults. Existing research has reached a consensus on alleviating cognitive decline, indicating that physical health, depressive symptoms, and activities of daily life (ADL) are important cognitive resources in the lives of older adults (29–31). Social participation, depressive symptoms, self-rated health, and ADL may not be the only predictors of cognitive function. On the contrary, they have a common path. For example, a decline in health may lead to an increase in depressive symptoms, which in turn affects cognitive function (14). Social participation can also play a role alongside other predictors. For example, people with poor health may be unable to participate in social activities, and people with more severe depressive symptoms may reduce going out to socialize. However, participating in social activities also provides older adults with a unique opportunity to engage in cognitive tasks beyond the influence of health, depressive symptoms, and ADL to maintain cognitive function (32, 33).
The social structure background in China is different from that in developed countries. In family life, older adults may need to play both the roles of children and grandparents, which means that most of them need to take on the responsibility of taking care of their older adults parents and young grandchildren at the same time. Their focus has shifted from work and family to personal life and family. In terms of time allocation, older adults may face a choice between personal life and family care and may even sacrifice a more autonomous lifestyle due to the responsibility of family care, so the opportunities for Chinese older adults to participate in social activities are very limited (34). Therefore, our paper has two main purposes. Firstly, we use the sample data of middle-aged and older Chinese adults to assess the strength of the correlation between social participation and cognitive function over time. Secondly, we attempt to determine whether social participation is independently correlated with cognitive function. This study hypothesizes that after controlling for three recognized predictors of cognitive decline, i.e., depressive symptoms, self-reported health, and ADL, social participation would uniquely predict cognitive function. Finally, we explore whether the correlation between social participation and cognitive function differs from other predictors.
2 Methods
2.1 Sample
This sample was derived from the China Health and Retirement Longitudinal Study (CHARLS), which surveyed people aged 45 and above in 150 county-level units and 450 communities in 28 provinces of China in 2011, 2013, 2015, and 2018. After excluding all missing indicators included in the baseline periods of 2011, 2013, 2015, and 2018, 5,258 participants aged 45 and above were included in this study. The longitudinal data analysis of the cognitive function of middle-aged and older Chinese adults in relation to their social participation was conducted using four waves of data in 2011 (T1), 2013 (T2), 2015 (T3), and 2018 (T4).
2.2 Measurements
2.2.1 Dependent variable – cognitive function
The calculation of cognitive function can be divided into episodic memory and mental intactness (35, 36). The calculation of episodic memory scores is based on the word recall test, which is divided into immediate recall and delayed recall. Immediate recall refers to the examiner randomly reading out 10 words and then asking participants to immediately recall as many words as possible, scoring the correct number of words recalled (21). Delayed recall refers to 10 min later when participants are asked to recall the same word list (36). The score of episodic memory refers to the average number of words in both immediate and delayed recall, ranging from 0 to 10 (37). Mental intactness aims to capture the mental intactness or state of individuals. In CHARLS, mental intactness problems include 7 consecutive subtractions from 100 (up to 5 times), date (month, day, year), day of the week, season, and cross pentagon replication tests. The answers to these questions are summarized into a mental intactness score of 0 ~ 11 (36).
2.2.2 Independent variables – social participation
In CHARLS, we evaluated 10 social activities of older adults over the past month, including communicating with friends, stock investment, and using the Internet. The frequency of each activity was categorized as never, irregular, almost weekly, or almost daily, with a score of 0 ~ 3. These were used to calculate a comprehensive social participation score ( ). Overall, the total score of social participation ranged from 0 to 24. The higher the score, the higher the level of social participation (36, 38, 39).
2.2.3 Covariates
2.2.3.1 Depressive symptoms
The Center for Epidemiological Studies Depression Scale (CES-D) was adopted, which was composed of 10 items (40). The answer options were never, sometimes or rarely, often, and always, with a score of 0 ~ 3. The total score of depressive symptoms ranged from 0 to 30. The higher the score, the more severe the depressive symptoms.
2.2.3.2 Self-reported health
The respondents were asked “How would you rate your health?,” and the response options ranged from “very good” to “poor.” While the response options for this question in 2018 were slightly different from the data of the previous three phases, it was treated as a continuous variable, on a scale of 1 to 5. The higher the score, the worse the self-reported health.
2.2.3.3 Activities of daily life
Respondents were asked if they had difficulties in six lifestyle habits (dressing, bathing, eating, getting up, going to the bathroom, and doing things themselves) or five instrumental activities (doing housework, cooking, shopping, managing finances, and taking medicine). The answer scale included four options: (1) No, I have no difficulty; (2) I have difficulties but I can still do it; (3) Yes, I have difficulties and need help; (4) I cannot do it (41). The subjects of this study were middle-aged and older adults, and most of them could independently complete the above behaviors. Therefore, this variable was considered a binary variable. If they reported having difficulty completing any item, it was defined as limited activities of daily life (ADL). Each ADL or instrumental activity of daily living (IADL) item had a score of 0 or 1, with a total score of up to 11 points. The higher the total score of ADL, the poorer the functional health (31, 42, 43).
2.2.3.4 Other covariates
Other covariates include demographic variables in the baseline period, including age, gender, and education level.
2.3 Statistical analysis
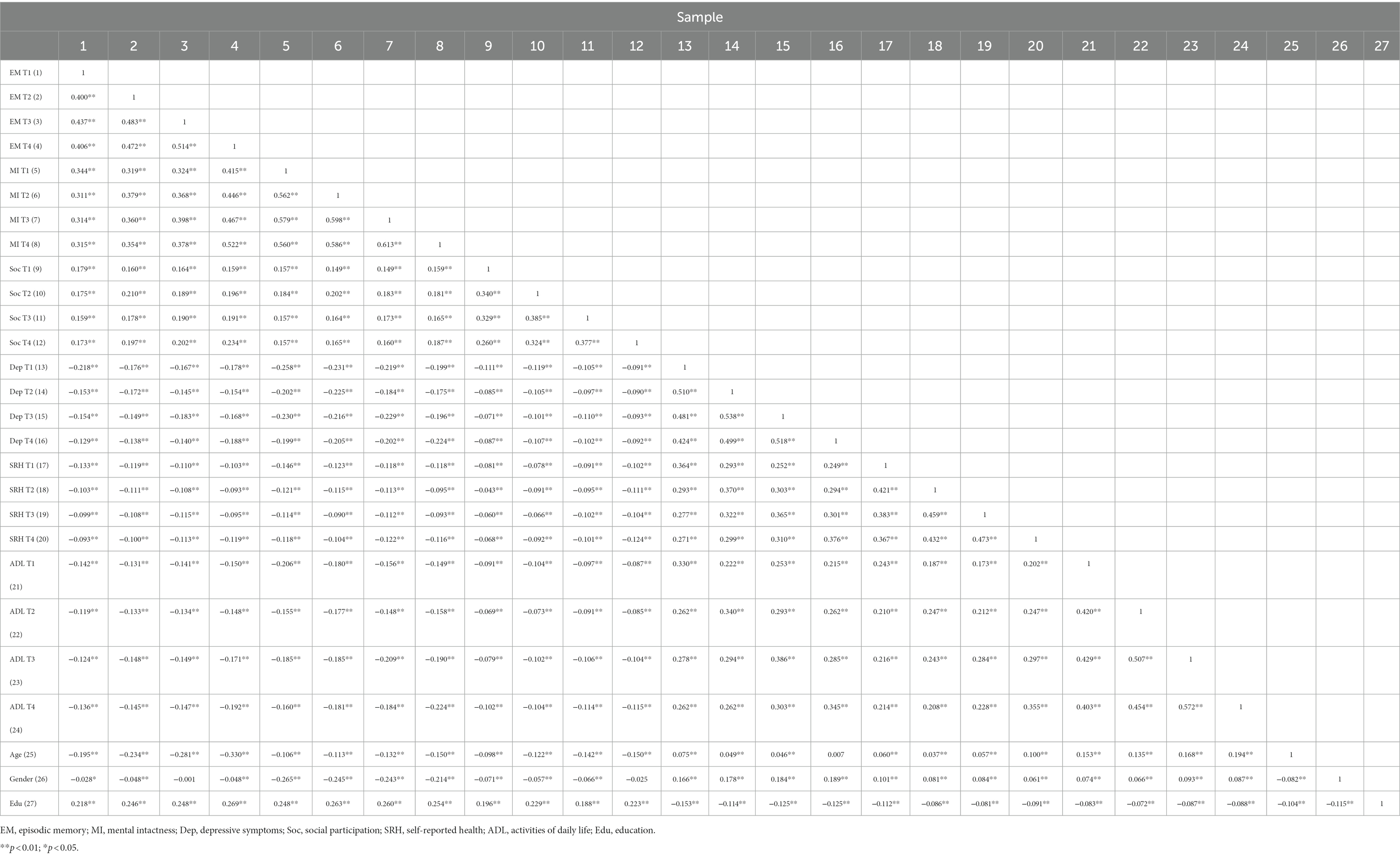
In this study, we first conducted descriptive statistics of each variable and calculated the correlation coefficient between them, examining the stability of interrelationships of other variables such as cognitive function and social participation in middle-aged and older Chinese adults.
Then, we constructed an unconditional LGM to examine the trajectory of cognitive function changes among middle-aged and older Chinese adults and whether there were significant individual differences in the initial level and development rate of cognitive function. On this basis, we ultimately constructed a conditional LGM and added the age, gender, and education level in the baseline period, which are three constant factors that do not change with time, to investigate whether there were demographic differences in cognitive function. The four time-varying factors of social participation, depressive symptoms, self-reported health, and ADL were added to investigate whether the cognitive function was affected over time by social participation, depressive symptoms, self-reported health, and ADL. Statistical analysis was conducted using Mplus 8.0 software, with a significance level of 0.05. The conceptual analysis model is shown in Figures 1, 2.
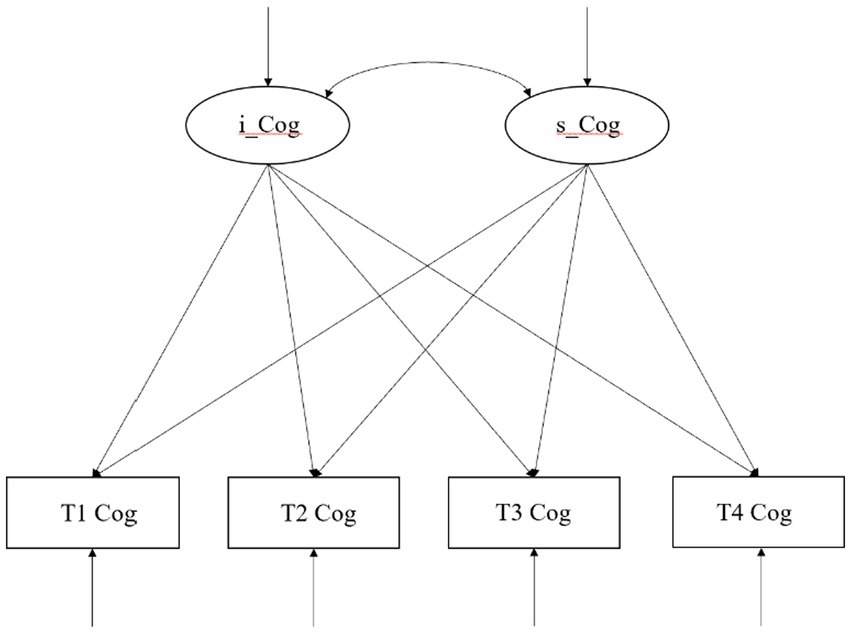
Figure 1. A linear unconditional latent growth model of cognitive function of middle-aged and older adults in China.
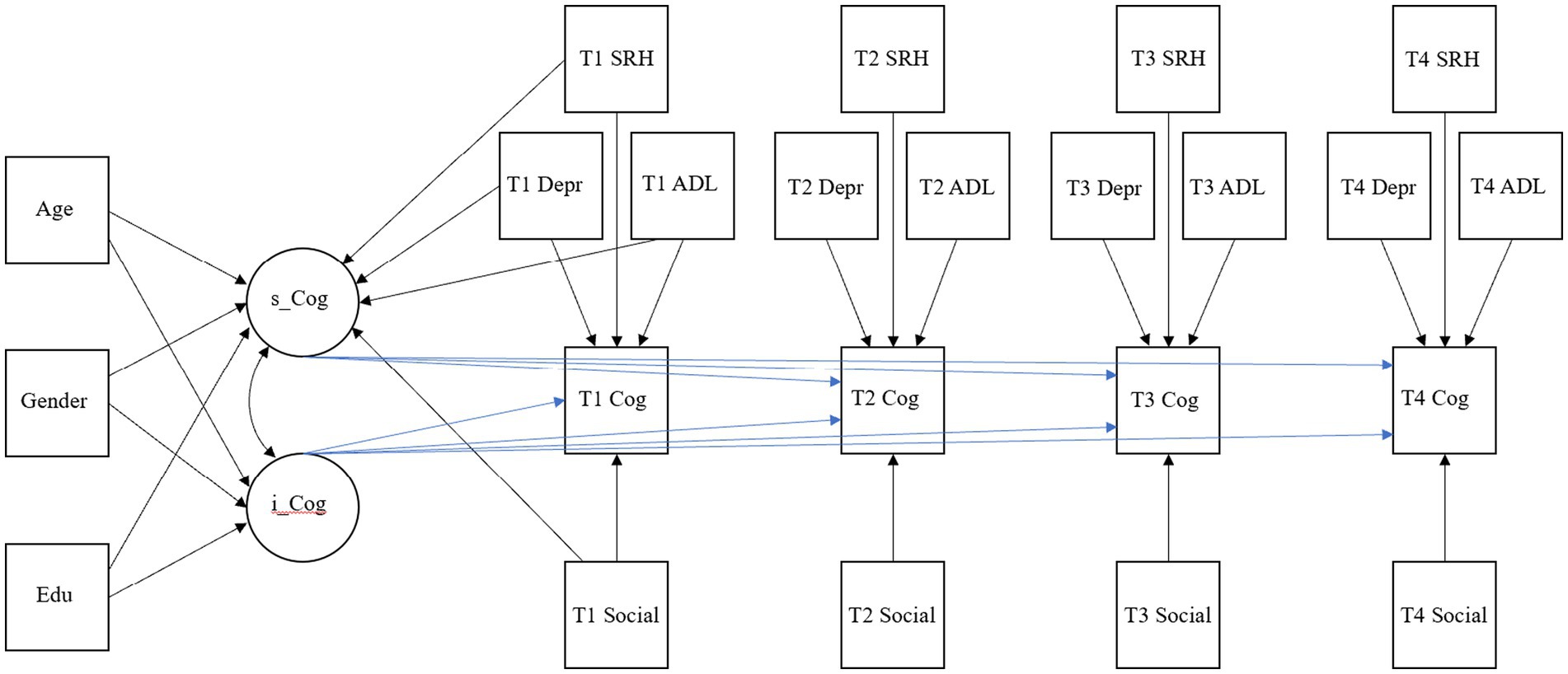
Figure 2. A conceptual model for predicting cognitive function in middle-aged and older adults through social participation. The model was suitable for episodic memory and mental intactness, including time-varying and invariant covariates. It regressed the explicit variables and latent parameters of cognitive function, respectively, to provide a comparative analysis of their impact on cognitive function. For T1, T2, T3, and T4, the parameter estimates for calculating the slope of cognitive function were constrained to 1, 2, 3, and 4, respectively. The residuals of endogenous variables are not specified but were included in the final model. All paths represent standardized model values. Cog, cognitive function; dep, depressive symptoms; Social, social participation; SRH, self-reported health; ADL, activities of daily life; Edu, education; s_ and i_, the slope and intercept of the described structure.
3 Results
3.1 Study characteristics
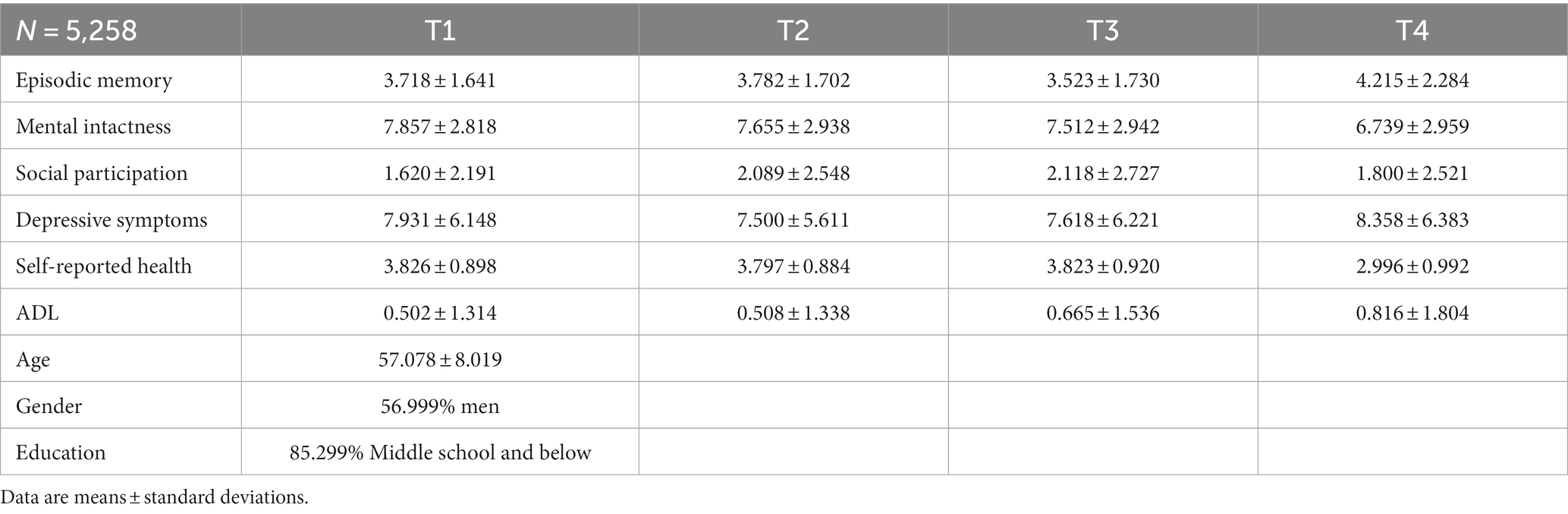
The average age of the participants in T1 was 57.078 years (SD = 8.019). Most of them were men, accounting for 56.999%. The education level of the cohort was mainly junior high school or below, accounting for 85.299%. The mean social participation scores at T1, T2, and T3 increased from 1.620 to 2.118, with a slight decline in T4. From T1 to T4, the mental intactness of cognitive function showed a declining trend, with an average of 7.857 to 6.739. In addition, the ADL showed an increasing trend, from 0.502 to 0.816 (see Table 1). The Pearson’s test obtained the correlation matrix for all study variables (see Table 2). There was a significant positive correlation between social participation and cognitive function among middle-aged and older adults at different times. Depressive symptoms, self-rated health, and ADL showed a negative correlation.
3.2 Unconditional LGM
To test whether the developmental trajectory of cognitive function in middle-aged and older adults is linear or nonlinear, we built linear and nonlinear unconditional LGM, respectively. From the fitting index, it can be seen that the linear unconditional LGM has a better fitting effect on the data than the nonlinear unconditional LGM, indicating that the development of cognitive function (episodic memory and mental intactness) in middle-aged and older adults showed a linear trend from T1 to T4.
Therefore, first, we built the unconditional linear LGM of episodic memory. According to the common evaluation standard of fitting index, the model fitted well. The model fitting indexes were: χ2 = 543.373, df = 5, p < 0.001, TLI = 0.894, CFI =0.873, SRMR = 0.052. Next, we built the unconditional linear LGM of mental intactness. The model fitting result of mental intactness was good, χ2 = 172.590, df = 5, p < 0.001, TLI = 0.976, CFI =0.980, SRMR = 0.024. After establishing the basic LGM, we introduced relevant time-varying variables (social participation, depressive symptom, self-reported health, and ADL) that predicted the cognitive variables in T1, T2, T3, and T4, and non-time-varying covariates (baseline age, gender, and education level) to predict the slope and intercept of episodic memory and mental intactness in the two models. Finally, we included direct correlations between social participation, depressive symptoms, self-reported health, and ADL at T1 to predict the slope of cognitive measurement.
3.3 LGM included covariates
3.3.1 Episodic memory
The model results of the final episodic memory fitted well, χ2 (35, N = 5,258) =226.847, p < 0.001, CFI = 0.975, RMSEA = 0.024. Firstly, age, as a covariate that does not change with time, had a significant predictive effect on the intercept and slope of episodic memory [B = -0.250, (−0.293, −0.206), B = -0.519, (−0.651, −0.386)]. Education level also predicted the intercept [B = 0.288, (0.244, 0.332)] and slope [B = 0.213, (0.121, 0.305)] of episodic memory. Gender had no predictive effect on the intercept and slope of episodic memory, and the p-values were not significant and not statistically significant.
Next, we investigated the strength of the time-varying covariates that predict episodic memory over time: social participation, depressive symptoms, self-reported health, and ADL. Both social participation and depressive symptoms significantly predicted episodic memory at all time points, T1, T2, T3, and T4. However, self-reported health and ADL could not significantly predict episodic memory at T1 and T3, respectively, with p > 0.05, which was not statistically significant. In addition, social participation, depressive symptoms, and ADL independently predicted the slope of episodic memory. For example, lower social participation and ADL and more severe depressive symptoms uniquely predicted the sharp decline of episodic memory function (44). See Table 3 below for the complete standardized model results. The comparison of the standardized strength of social participation and depressive symptoms’ association with episodic memory revealed that competing predictors were relatively comparable, in terms of context and predicting the slope of episodic memory (44).
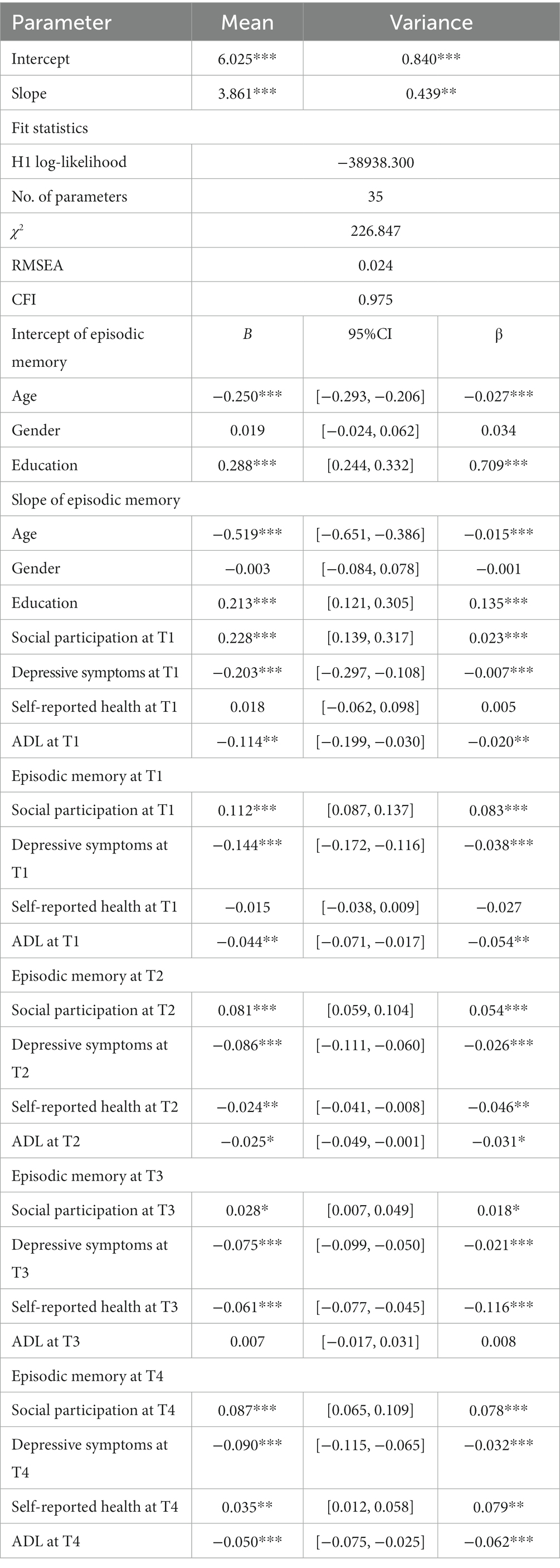
Table 3. Parameter estimates for LGM parameters, model fit, and regression coefficients predicting episodic memory.
3.3.2 Mental intactness
The final model results of mental intactness fitted well, χ2 (35, N = 5,258) =243.244, p < 0.001, CFI = 0.982, RMSEA = 0.026. First, age, a covariate that does not change over time, had a significant predictive effect on the intercept and slope of mental intactness, B = -0.107, [−0.140, 0.075], B = -0.155, [−0.267, −0.042]. Gender also predicted intercept [B = -0.315, (−0.346, −0.283)] and slope [B = 0.154, (0.042, 0.266)] of mental intactness. In contrast, the intercept of education level in predicting mental intactness [B = 0.262, (0.230, 0.295)] cannot predict the slope of mental intactness, and the value of p is not significant, which is not statistically significant.
Next, we examine the strength of time-varying covariates; social participation, depressive symptoms, self-reported health, and ADL predicted mental intactness over time. Social participation, depressive symptoms, and ADL significantly predicted mental intactness at four time points. In addition, social participation and depressive symptoms can independently predict the slope of mental intactness. For example, lower social participation and higher depressive symptoms can independently predict the sharp decline of mental intactness. See Table 4 for the complete standardized model results. Comparisons of the standardized strength of social participation, depressive symptoms, and ADL’s association with mental intactness reveal that competing predictors were relatively comparable in terms of context and predicting the slope of mental intactness.
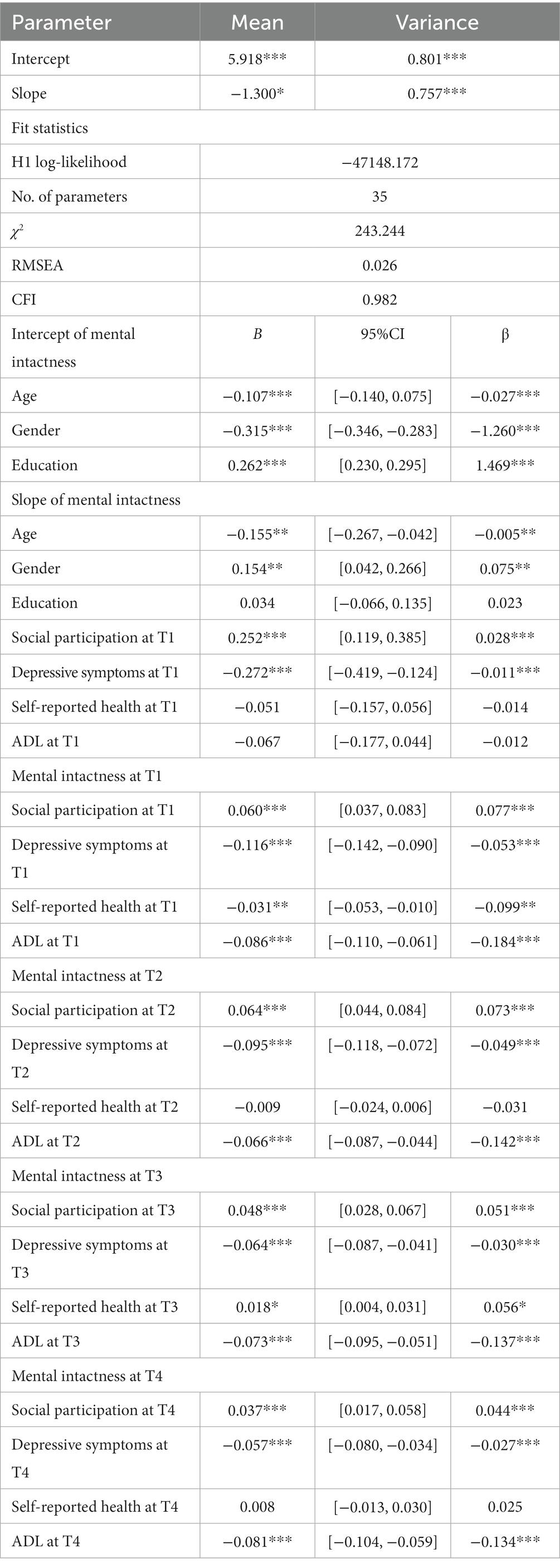
Table 4. Parameter estimates for LGM parameters, model fit, and regression coefficients predicting mental intactness.
4 Discussion
This study analyzed the relationship between social participation and cognitive function using four-wave longitudinal data of 5,258 middle-aged and older Chinese adults (45). After controlling for depressive symptoms, self-reported health, and ADL, we examined the different intensities of frequency and duration of social participation and cognitive function of this population (episodic memory and mental intactness). The results showed that the higher the level of social participation, the higher the score of cognitive function. Consistent with previous studies, social participation can reduce the risk of cognitive decline (18, 46, 47). In addition, this study also found that social participation during the baseline period can predict changes in cognitive function over time (48). At the same level, factors such as social participation, depressive symptoms, self-reported health, and ADL also affect the cognitive function of middle-aged and older Chinese adults.
Consistent with previous research results, social participation and cognitive function (episodic memory and mental intactness) showed a significant positive correlation over time, which also confirms the first hypothesis of this study. According to the theory of “cognitive reserve,” the participation of older adults in intellectual, social, and physical activities can optimize the memory-related brain regions or brain networks, resulting in less impact on memory function in middle-aged and older Chinese adults, thus preventing the occurrence of dementia (49). The stress theory suggests that the body needs attention to break down stress, which can compete for cognitive resources (50). In addition, stress may be related to the dysregulation of cortisol and inflammatory cytokines, which can lead to a series of negative health outcomes, such as cognitive decline, when stress levels are elevated (51–53). Furthermore, social participation has a protective effect on cognitive function by regulating stress to eliminate the negative effects of stressful events (54). The vascular theory suggests that active social participation reduces the risk of vascular diseases and their risk factors (55), and vascular diseases or vascular risk factors are closely related to the progression of cognitive disorders such as Alzheimer’s disease; therefore, social participation can affect the occurrence of cognitive decline by affecting vascular diseases (56).
Inconsistent with previous studies on the single impact of social participation on cognitive function, this study suggests that low social participation, high depressive symptoms, and ADL at T1 can uniquely predict cognitive decline in middle-aged and older Chinese adults, further supporting the cognitive enrichment hypothesis (44). First of all, the results of this study found that those who rated themselves as healthier had better cognitive function. Consistent with previous research results, individual health not only affects cognitive function over time, but also, the higher the degree of self-perceived health, the better their cognitive abilities (57, 58). These findings support the Strength and Vulnerability Integration (SAVI) model, which suggests that, due to the increased physical vulnerability of middle-aged and older adults, they may be more vulnerable to stress and suffer more severe cognitive and emotional consequences than younger adults (59). Compared with middle-aged and older adults with good health, people with poor health are more likely to suffer from stress, resulting in impaired cognitive function (60). In addition, other studies have found that cognitive performance and health may have a common cause; if the effects of this common cause become increasingly pronounced with age, it could explain the current findings. For example, the aforementioned vascular theory suggests that vascular risk factors (such as hypertension, coronary heart disease, and dyslipidemia) become more common with age, and they are related to cognitive impairment disorders such as Alzheimer’s disease (61, 62).
Second, numerous studies have emphasized the possibility of multiple mechanisms that explain the decline in cognitive ability caused by depressive symptoms (63, 64). The results of this study enrich existing research, showing that depressive symptoms in middle-aged and older Chinese adults predict cognitive decline (episodic memory and mental intactness) over time (63, 65). The occurrence factors of depressive symptoms in middle-aged and older Chinese adults are complex and are influenced by heredity, physical diseases, and environment. Persistent stress events are one of the important factors leading to depression, and they also have the potential to damage cognitive function in older adults. The impairment of episodic memory and mental intactness is the most common manifestation, but the molecular mechanism involved is still unclear. Based on previous literature, one possible mechanism is that depressive symptoms may be a psychological response to a decline in self-awareness, a decline in interest in anything, and a reluctance to communicate with the outside world. People with depressive symptoms also have greater impairments in attention and language function, interfering with daily activities and resulting in an inability to exert greater effort when carrying out tasks (66). In terms of physiological mechanism, hippocampal volume has been linked to language and spatial memory function (66). Depressive symptoms may lead to dysregulation of the hypothalamic pituitary adrenal axis, leading to prolonged hypercortisolemia, hippocampal atrophy, and impaired language and spatial memory functions (66, 67). In addition, previous studies on the genetic susceptibility of depressive symptoms have shown that patients with depressive symptoms cannot bear the excessive and severe living demands, leading to chronic stress and potentially interfering with cognitive functions such as attention, memory, and information processing (68, 69).
Third, the measurement of cognitive function in older adults through episodic memory mainly focuses on memory ability, while mental intactness involves other mental abilities such as reading and computing. Previous studies have shown that the daily activities of middle-aged and older Chinese adults are associated with a slowdown in brain atrophy, which may support the decline of the executive control processes and memory function of older adults (70–72). Juan Wang et al. also found that daily activities are associated with cognitive function in older adults, which is also consistent with our research (31). The reason may be that limited daily behavior ability can cause older adults to be unable to take care of themselves completely, resulting in a reduced range of activities, decreased interaction with the outside world, and less information obtained. Due to the lack of sufficient information stimulation, the brain cannot always be active, which leads to the deterioration of brain function and increases the risk of cognitive function damage (73).
Therefore, when formulating social health interventions targeting middle-aged and older Chinese adults, we should pay attention to their physical and emotional aspects. Firstly, families, communities, governments, and other social organizations should consider how to take targeted measures to reduce the negative emotions of this population, enhance their openness and enthusiasm toward life, and prevent “dementia” caused by “depression.” Secondly, according to the enrichment hypothesis, communities, governments, and other social organizations should formulate corresponding activity plans to make social activities attractive, stimulating, and enjoyable, creating more fun for retired older adults (74). Middle-aged and older Chinese adults should be encouraged to actively participate in social interactions and increase their channels of social participation. The establishment of community mutual aid organizations, the promotion of the “Time Bank” project, and the protection of the cognitive function of older adults should also be encouraged.
This study also has some limitations. First, due to the bias of the self-report method, the prevalence of sensitive issues such as cognitive function and depressive symptoms in China may be underestimated, and there is a certain recall bias. Our research results show that the self-report method may also be considered an advantage and may be a necessary preliminary method to lay the foundation for subsequent perceptual intervention trials to examine these mechanisms through objective mechanisms. Second, this study found that higher social participation was associated with better cognitive function. However, reverse causation is also possible. Similar to previous studies, there is still insufficient evidence for reverse causal relationships between social participation and cognitive function in this study (18, 36, 74). Third, the current study is limited to general indicators of social activities. The existing data do not include specific physiological and psychological information about social activities. In the future, we can use data such as the specific psychological benefits derived from participating in social activities to elaborate more on the potential mechanisms.
5 Conclusion
This study provides evidence for the mechanisms of the influence of social participation on cognitive function among middle-aged and older Chinese adults. Over time, social participation predicts episodic memory and mental intactness in middle-aged and older Chinese adults, independent of the effects of depressive symptoms, self-reported health, and ADL, and to the same extent as these competing predictors and cognitive ability. Therefore, interventions that target cognition by participating in social activities are promising and may be as effective or more effective than treatments that target other predictors of cognitive decline, such as depressive symptoms, self-reported health, and ADL.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number (s) can be found below: the original databases of this study are available from the online site: https://charls.charlsdata.com/index/zh-cn.html.
Ethics statement
The studies involving humans were approved by the Approval for the original CHARLS was obtained from the Biomedical Ethics Review Committee of Peking University (IRB00001052-11015), and all participants signed informed consent at the time of participation. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XL: Conceptualization, Data curation, Methodology, Software, Writing – original draft, Writing – review & editing. WX: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors are grateful to the National School of Development of Peking University for providing the data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang, W, Shi, HY, and Li, Q. Pension gap between the Chinese public and nonpublic sectors: evidence in the context of the integration of dual-track pension schemes. International Review of Economics & Finance. (2023) 85:664–88. doi: 10.1016/j.iref.2023.01.023
2. Report, WM. World Population Prospects: The 2017 Revision. (2017). Available at: https://esa.un.org/unpd/wpp/Download/Standard/Population/ (Accessed August 12, 2020).
3. Jia, LF, Quan, MN, Fu, Y, Zhao, T, Li, Y, Wei, CB, et al. Dementia in China: epidemiology, clinical management, and research advances. Lancet Neurol. (2020) 19:81–92. doi: 10.1016/S1474-4422(19)30290-X
4. Semkovska, M, Quinlivan, L, O'Grady, T, Johnson, R, Collins, A, O'Connor, J, et al. Cognitive function following a major depressive episode: a systematic review and meta-analysis. Lancet Psychiatry. (2019) 6:851–61. doi: 10.1016/S2215-0366(19)30291-3
5. Ye, X, Zhu, DW, and He, P. Direct and indirect associations between childhood socioeconomic status and cognitive function in the middle-aged and older adults in China. Aging Ment Health. (2022) 26:1730–7. doi: 10.1080/13607863.2021.1935459
6. Darko, EM, Kleib, M, and Olson, J. Social media use for research participant recruitment: integrative literature review. J Med Internet Res. (2022) 24:e38015. doi: 10.2196/38015
7. Guo, QJ, Bai, X, and Feng, N. Social participation and depressive symptoms among Chinese older adults: a study on rural-urban differences. J Affect Disord. (2018) 239:124–30. doi: 10.1016/j.jad.2018.06.036
8. Hajek, A, Brettschneider, C, Mallon, T, Ernst, A, Mamone, S, Wiese, B, et al. The impact of social engagement on health-related quality of life and depressive symptoms in old age - evidence from a multicenter prospective cohort study in Germany. Health Qual Life Outcomes. (2017) 15:140. doi: 10.1186/s12955-017-0715-8
9. Li, FZ. Physical activity and health in the presence of China's economic growth: meeting the public health challenges of the aging population. J Sport Health Sci. (2016) 5:258–69. doi: 10.1016/j.jshs.2016.06.004
10. Ning, HT, Zhang, H, Xie, ZH, Jiang, WH, and Xie, SB. Relationship of hearing impairment, social participation and depressive symptoms to the incidence of frailty in a community cohort. J Am Geriatr Soc. (2023) 71:1167–76. doi: 10.1111/jgs.18164
11. Feng, ZY, Cramm, JM, Jin, CL, Twisk, J, and Nieboer, AP. The longitudinal relationship between income and social participation among Chinese older people. SSM-Population Health. (2020) 11:100636. doi: 10.1016/j.ssmph.2020.100636
12. Sun, J, Kong, XY, Li, HM, Chen, JY, Yao, Q, Li, HX, et al. Does social participation decrease the risk of frailty? Impacts of diversity in frequency and types of social participation on frailty in middle-aged and older populations. BMC Geriatr. (2022) 22:553. doi: 10.1186/s12877-022-03219-9
13. Zhou, YJ, Chen, Z, Shaw, I, Wu, X, Liao, SM, Qi, L, et al. Association between social participation and cognitive function among middle- and old-aged Chinese: a fixed-effects analysis. J. Glob. Health. (2020) 8:1–11. doi: 10.7189/jogh.10.020801
14. Dan-dan, SUN, Duo-duo, SUN, Jingdong, SUO, Qing, Z, and Chong-xiang, H. The mediating role of depression in the relationship between social engagement and cognitive function in older persons. Chin J Dis Control Prevent. (2022) 2:212–3. doi: 10.16462/j.cnki.zhjbkz.2022.02.015
15. Light, LL. Theoretical perspectives on cognitive aging – Salthouse, TA. Am J Psychol. (1993) 106:601–8. doi: 10.2307/1422973
16. Haslam, SA, Jetten, J, Postmes, T, and Haslam, C. Social identity, health and well-being: an emerging agenda for applied psychology. Appl Psychol. (2009) 58:1–23. doi: 10.1111/j.1464-0597.2008.00379.x
17. Jetten, J, Haslam, C, Haslam, SA, Dingle, G, and Jones, JM. How groups affect our health and well-being: the path from theory to policy. Soc Issues Policy Rev. (2014) 8:103–30. doi: 10.1111/sipr.12003
18. James, BD, Wilson, RS, Barnes, LL, and Bennett, DA. Late-life social activity and cognitive decline in old age. Am J Epidemiol. (2011) 173:S74–S. doi: 10.1017/S1355617711000531
19. Guo, YC, Shi, HY, Yu, DH, and Qiu, PX. Health benefits of traditional Chinese sports and physical activity for older adults: a systematic review of evidence. J Sport Health Sci. (2016) 5:270–80. doi: 10.1016/j.jshs.2016.07.002
20. Ding, D, Fu, H, and Bauman, AE. Step it up: advancing physical activity research to promote healthy aging in China. J Sport Health Sci. (2016) 5:255–7. doi: 10.1016/j.jshs.2016.06.003
21. Fu, C, Li, Z, and Mao, ZF. Association between social activities and cognitive function among the elderly in China: a cross-sectional study. Int J Environ Res Public Health. (2018) 15:231. doi: 10.3390/ijerph15020231
22. Glei, DA, Landau, DA, Goldman, N, Chuang, YL, Rodriguez, G, and Weinstein, M. Participating in social activities helps preserve cognitive function: an analysis of a longitudinal, population-based study of the elderly. Int J Epidemiol. (2005) 34:864–71. doi: 10.1093/ije/dyi049
23. Wilson, RS, Scherr, PA, Schneider, JA, Tang, Y, and Bennett, DA. Relation of cognitive activity to risk of developing Alzheimer disease. Neurology. (2007) 69:1911–20. doi: 10.1212/01.wnl.0000271087.67782.cb
24. Lifshitz-Vahav, H, Shrira, A, and Bodner, E. The reciprocal relationship between participation in leisure activities and cognitive functioning: the moderating effect of self-rated literacy level. Aging Ment Health. (2017) 21:524–31. doi: 10.1080/13607863.2015.1124838
25. Li, XC, Zhang, JJ, Hou, R, Zheng, MQ, Singh, M, Li, HB, et al. Bidirectional associations of intellectual and social activities with cognitive function among middle-aged and elderly adults in China. J Affect Disord. (2022) 319:83–9. doi: 10.1016/j.jad.2022.09.031
26. Li, Y, and Lu, JH. Social participation of the elderly in China: connotation, present situation and challenge. Popul Family Plan. (2018) 11:14–7. doi: CNKI:SUN:RKSY.0.2018-11-006
27. Wang, L. Characteristics and trends of older adults living alone in China. Sci Res Aging. (2023) 11:47–64.
28. Dufouil, C, and Glymour, MM. Prediction to prevention in Alzheimer's disease and dementia. Lancet Neurol. (2018) 17:388–9. doi: 10.1016/S1474-4422(18)30123-6
29. Sharifian, N, Kraal, AZ, Zaheed, AB, Sol, K, and Zahodne, LB. Longitudinal associations between contact frequency with friends and with family, activity engagement, and cognitive functioning. J Int Neuropsychol Soc. (2020) 26:815–24. doi: 10.1017/S1355617720000259
30. Sundstrom, A, Ronnlund, M, and Josefsson, M. A nationwide Swedish study of age at retirement and dementia risk. Int J Geriatr Psychiatry. (2020) 35:1243–9. doi: 10.1002/gps.5363
31. Wang, J, Zhu, WH, Li, YF, and Zhu, WW. Temporal precedence of cognitive function and functional abilities: a latent difference score model of the Chinese community-dwelling elders. Int J Geriatr Psychiatry. (2019) 34:1892–9. doi: 10.1002/gps.5206
32. Kim, D, Arai, H, and Kim, S. Social activities are associated with cognitive decline in older Koreans. Geriatr Gerontol Int. (2017) 17:1191–6. doi: 10.1111/ggi.12861
33. Fratiglioni, L, Paillard-Borg, S, and Winblad, B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. (2004) 3:343–53. doi: 10.1016/S1474-4422(04)00767-7
34. He, WJ, Zhang, X, and Liu, LZ. Social participation patterns and their impact on the mental health of the elderly-a personal-family balance perspective. Gov Stud. (2022) 38:12–24. doi: 10.15944/j.cnki.33-1010/d.2022.05.006
35. Lei, XY, Hu, YQ, McArdle, JJ, Smith, JP, and Zhao, YH. Gender differences in cognition among older adults in China. J Hum Resour. (2012) 47:951–71. doi: 10.1353/jhr.2012.0033
36. Li, HB, Li, CW, Wang, AX, Qi, YL, Feng, W, Hou, CB, et al. Associations between social and intellectual activities with cognitive trajectories in Chinese middle-aged and older adults: a nationally representative cohort study. Alzheimers Res Ther. (2020) 12:1–12. doi: 10.1186/s13195-020-00691-6
37. Li, BY, Bi, JF, Wei, C, and Sha, F. Specific activities and the trajectories of cognitive decline among middle-aged and older adults: a five-year longitudinal cohort study. J Alzheimers Dis. (2021) 80:1039–50. doi: 10.3233/JAD-201268
38. Huang, YF, Guo, XY, Du, J, and Liu, YL. Associations between intellectual and social activities with frailty among community-dwelling older adults in China: a prospective cohort study. Front Med. (2021) 8:693818. doi: 10.3389/fmed.2021.693818
39. Su, Q, Wang, H, and Fan, LJ. The impact of home and community care services pilot program on healthy aging: a difference-in-difference with propensity score matching analysis from China. Arch Gerontol Geriatr. (2023) 110:020801:104970. doi: 10.1016/j.archger.2023.104970
40. Jian-kang, LIU, Li, S, Jing, LIN, Fu-sheng, XU, Yuan, ZHANG, Li, SUN, et al. The comorbid relationship between activities of daily living and symptoms of depression and anxiety in the elderly. Chin J Prevent Control Chronic Dis. (2022) 30:251–5. doi: 10.16386/j.cjpccd.issn.1004-6194.2022.04.003
41. Li, MM, Yang, YH, Pang, L, Wu, MC, Wang, ZQ, Fu, YA, et al. Gender-specific associations between activities of daily living disability and depressive symptoms among older adults in China: evidence from the China health and retirement longitudinal study. Arch Psychiatr Nurs. (2019) 33:160–6. doi: 10.1016/j.apnu.2019.08.010
42. Li, JX, Cacchione, PZ, Hodgson, N, Riegel, B, Keenan, BT, Scharf, MT, et al. Afternoon napping and cognition in Chinese older adults: findings from the China health and retirement longitudinal study baseline assessment. J Am Geriatr Soc. (2017) 65:373–80. doi: 10.1111/jgs.14368
43. Sha, TT, Cheng, WW, and Yan, Y. Prospective associations between pulse pressure and cognitive performance in Chinese middle-aged and older population across a 5-year study period. Alzheimers Res Ther. (2018):10. doi: 10.1186/s13195-018-0355-1
44. Bourassa, KJ, Memel, M, Woolverton, C, and Sbarra, DA. Social participation predicts cognitive functioning in aging adults over time: comparisons with physical health, depression, and physical activity. Aging Ment Health. (2017) 21:133–46. doi: 10.1080/13607863.2015.1081152
45. Hwang, J, Kim, S, and Kim, S. Gender differences in the impact of depression on cognitive decline among Korean older adults. Asia Pac J Public Health. (2021) 33:67–75. doi: 10.1177/1010539520961715
46. Verghese, J, LeValley, A, Derby, C, Kuslansky, G, Katz, M, Hall, C, et al. Leisure activities and the risk of amnestic mild cognitive impairment in the elderly. Neurology. (2006) 66:821–7. doi: 10.1212/01.wnl.0000202520.68987.48
47. Su, XF, Huang, XB, Jin, Y, Wan, SW, and Han, ZL. The relationship of individual social activity and cognitive function of community Chinese elderly: a cross-sectional study. Neuropsychiatr Dis Treat. (2018) 14:2149–57. doi: 10.2147/NDT.S160036
48. Anaturk, M, Suri, S, Zsoldos, E, Filippini, N, Mahmood, A, Singh-Manoux, A, et al. Associations between longitudinal trajectories of cognitive and social activities and brain health in old age. JAMA Netw Open. (2020) 3:e2013793. doi: 10.1001/jamanetworkopen.2020.13793
49. Barulli, D, and Stern, Y. Efficiency, capacity, compensation, maintenance, plasticity: emerging concepts in cognitive reserve. Trends Cogn Sci. (2013) 17:502–9. doi: 10.1016/j.tics.2013.08.012
50. Hyun, J, Sliwinski, MJ, and Smyth, JM. Waking up on the wrong side of the bed: the effects of stress anticipation on working memory in daily life. J Gerontol Ser B-Psychol Sci Soci Sci. (2019) 74:38–46. doi: 10.1093/geronb/gby042
51. Panayiotou, G, Panteli, M, and Vlemincx, E. Adaptive and maladaptive emotion processing and regulation, and the case of alexithymia. Cognit Emot. (2021) 35:488–99. doi: 10.1080/02699931.2019.1671322
52. Lupien, SJ, Schwartz, G, Ng, YK, Fiocco, A, Wan, N, Pruessner, JC, et al. The Douglas Hospital longitudinal study of Normal and pathological aging: summary of findings. J Psychiatry Neurosci. (2005) 30:328–34. doi: 10.1016/j.jpsychires.2004.11.005
53. Marsland, AL, Petersen, KL, Sathanoori, R, Muldoon, MF, Neumann, SA, Ryan, C, et al. Interleukin-6 covaries inversely with cognitive performance among middle-aged community volunteers. Psychosom Med. (2006) 68:895–903. doi: 10.1097/01.psy.0000238451.22174.92
54. Zuelsdorff, ML, Engelman, CD, Friedman, EM, Koscik, RL, Jonaitis, EM, La Rue, A, et al. Stressful events, social support, and cognitive function in middle-aged adults with a family history of Alzheimer's disease. J Aging Health. (2013) 25:944–59. doi: 10.1177/0898264313498416
55. Sans, S. Mediterranean diet, active lifestyle and cardiovascular disease: a recipe for immortality? Eur J Prev Cardiol. (2018) 25:1182–5. doi: 10.1177/2047487318785745
56. Peloso, GM, Beiser, AS, Satizabal, CL, Xanthakis, V, Vasan, RS, Pase, MP, et al. Cardiovascular health, genetic risk, and risk of dementia in the Framingham heart study. Neurology. (2020) 95:E1341–e1350. doi: 10.1212/WNL.0000000000010306
57. Rosano, C, Simonsick, EM, Harris, TB, Kritchevsky, SB, Brach, J, Visser, M, et al. Association between physical and cognitive function in healthy elderly: the health, aging and body composition study. Neuroepidemiology. (2005) 24:8–14. doi: 10.1159/000081043
58. Dostalova, R, Stillman, C, Erickson, KI, Slepicka, P, and Mudrak, J. The relationship between physical activity, self-perceived health, and cognitive function in older adults. Brain Sci. (2021) 11:492. doi: 10.3390/brainsci11040492
59. Charles, ST. Strength and vulnerability integration: a model of emotional well-being across adulthood. Psychol Bull. (2010) 136:1068–91. doi: 10.1037/a0021232
60. Chen, YW, Wang, JX, Liang, Y, Sun, F, and Dong, XQ. Perceived stress and cognitive functions among Chinese older adults: the moderating role of health status. Gerontol Geriatric Med. (2018) 4:233372141877839. doi: 10.1177/2333721418778390
61. Loprinzi, PD. Multimorbidity, cognitive function, and physical activity. Age. (2016) 38:8. doi: 10.1007/s11357-016-9874-5
62. Jokela, M, Singh-Manoux, A, Ferrie, JE, Gimeno, D, Akbaraly, TN, Shipley, MJ, et al. The association of cognitive performance with mental health and physical functioning strengthens with age: the Whitehall II cohort study. Psychol Med. (2010) 40:837–45. doi: 10.1017/S0033291709991024
63. Saenz, JL, Garcia, MA, and Downer, B. Late life depressive symptoms and cognitive function among older Mexican adults: the past and the present. Aging Ment Health. (2020) 24:413–22. doi: 10.1080/13607863.2018.1544214
64. Erten-Lyons, D, and Silbert, L. Depressive symptoms are associated with late life cognitive decline independent of common age-related pathologies. Evid Based Ment Health. (2015) 18:50. doi: 10.1136/eb-2014-101980
65. Mourao, RJ, Mansur, G, Malloy-Diniz, LF, Costa, EC, and Diniz, BS. Depressive symptoms increase the risk of progression to dementia in subjects with mild cognitive impairment: systematic review and meta-analysis. Int J Geriatr Psychiatry. (2016) 31:905–11. doi: 10.1002/gps.4406
66. Wu, CR, Chen, PY, Hsieh, SH, Huang, HC, Chen, YT, Chen, TJ, et al. Sleep mediates the relationship between depression and cognitive impairment in older men. Am J Mens Health. (2019) 13:1557988319825765. doi: 10.1177/1557988319825765
67. Saito, S, Kimura, S, Adachi, N, Numakawa, T, Ogura, A, and Tominaga-Yoshino, K. An in vitro reproduction of stress-induced memory defects: effects of corticoids on dendritic spine dynamics. Sci Rep. (2016) 6:19287. doi: 10.1038/srep19287
68. Bae, SM. Autoregressive cross-lagged modelling of the relationship between social activity, depressive symptoms, and cognitive function in Korean elderly. Psychogeriatrics. (2021) 21:350–8. doi: 10.1111/psyg.12674
69. Rodrigues, R, Petersen, RB, and Perry, G. Parallels between major depressive disorder and Alzheimer's disease: role of oxidative stress and genetic vulnerability. Cell Mol Neurobiol. (2014) 34:925–49. doi: 10.1007/s10571-014-0074-5
70. Kesavayuth, D, Liang, Y, and Zikos, V. An active lifestyle and cognitive function: evidence from China. J Econom Ageing. (2018) 12:183–91. doi: 10.1016/j.jeoa.2018.05.001
71. Colcombe, SJ, Erickson, KI, Scalf, PE, Kim, JS, Prakash, R, McAuley, E, et al. Aerobic exercise training increases brain volume in aging humans. J Gerontol Series A-Biol Sci Med Sci. (2006) 61:1166–70. doi: 10.1093/gerona/61.11.1166
72. Bai, AY, Tao, LY, Huang, J, Tao, J, and Liu, J. Effects of physical activity on cognitive function among patients with diabetes in China: a nationally longitudinal study. BMC Public Health. (2021) 21:481–90. doi: 10.1186/s12889-021-10537-x
73. Li, MM, Fu, YN, Wu, MC, Wang, ZQ, and Li, K. Correlation between activities of daily living and cognitive function of the elderly. Nurs Res China. (2018) 32:1749–52. doi: 10.12102/j.issn.1009-6493.2018.11.023
Keywords: cognitive function, social participation, longitudinal study, aging, China
Citation: Li X and Xu W (2024) A change in social participation affects cognitive function in middle-aged and older Chinese adults: analysis of a Chinese longitudinal study on aging (2011–2018). Front. Public Health. 12:1295433. doi: 10.3389/fpubh.2024.1295433
Edited by:
Ljiljana T. Majnaric, Josip Juraj Strossmayer University of Osijek, CroatiaReviewed by:
Wenbin Liu, Fujian Medical University, ChinaYaqing Xue, Southern Medical University, China
Copyright © 2024 Li and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenyan Xu, d2VueWFueHUxOTk0QDEyNi5jb20=
 Xuyang Li
Xuyang Li Wenyan Xu
Wenyan Xu