- National Institute of Public Health, Ljubljana, Slovenia
Background: Public health interventions aim to reduce the burden of chronic non-communicable diseases. Implementing evidence-based interventions that are proven to be successful and effective is widely recognized as the best approach to addressing public health challenges. To avoid the development and implementation of less effective or successful or even harmful practices, clear criteria for the assessment of practices, that consider different dimensions of the interventions in public health, are needed. The main aim of the research was to test our Criteria and assessment procedure for recognizing good practices in the field of public health by estimating the consistency between the evaluators and thereby gaining insight into the adequacy and reliability of the criteria as well as to check how the evaluators understand the criteria and methodology and if it is properly used in assessing the interventions.
Methods: The assessment of the interventions took place from 2021 to 2022. The individual evaluator’s scores on the scale from 1 to 5 for each specific sub-criterion were collected, which was followed by a panel discussion to reach a final score for each sub-criterion. The inter-rater agreement was measured using percent overall agreement and Fleiss’ kappa coefficient.
Results: We found moderate inter-rater agreement on the level of the assessment criteria group. The lowest agreement was observed for the effectiveness and efficiency sub-criteria group, which also received the lowest scores from the evaluators. Challenges identified with the scoring process were due to the descriptive 1 to 5 scale and the varying specificity of the criteria.
Conclusion: The results showed that studying consistency between evaluators can highlight areas for improvement or adjustment in the assessment criteria and enhance the quality of the assessment instrument. Therefore, such analysis would be useful part of both newly and well-established health promotion and prevention program registries.
1 Background
Public health interventions aim to reduce the burden of chronic non-communicable diseases by addressing risk factors such as tobacco smoking, alcohol consumption, unhealthy diet, physical inactivity, and overweight (1). Implementing evidence-based interventions that are proven to be successful and effective in improving individual, community, and population health is widely recognized as the best approach to addressing public health challenges (2, 3). While randomized controlled trials held as gold standard for the quality of evidence that supports causality between the intervention and outcomes, there is growing awareness of the importance of demonstrating effectiveness in actual program settings for public health interventions (4–6). Practice-based evidence, including theories and approaches such as community-based participatory research, PRECEDE-PROCEDE, and RE-AIM framework, has been proposed as a more relevant source of evidence for public health decision-making due to the focus on populations, consideration of contextual factors, and complexity of multi-disciplinary interventions (4, 7, 8). Therefore, evaluation of existing public health interventions and selection of best practices are a valuable source of practice-based evidence (4, 9, 10). To avoid the development and implementation of less effective or successful or even harmful practices, clear criteria for the assessment of practices, that are considering different dimensions of the interventions in public health, are needed (11). Health promotion and prevention program registries (HPPRs) serve as valuable “portals for the exchange of good practices” as long as appropriate evaluation and assessment criteria are utilized when selecting the presented practices. These registers increase transparency and highlight effective and successful interventions, aiding decision-makers in selecting and implementing the most appropriate interventions. They serve as entry points and practice repositories, providing easy access to evidence-based practices (12, 13). There is a number of practice portals within the health domain in the EU, such as EU Best Practice portal, The European Monitoring Center for Drugs and Drug Addiction (EMCDDA) portal, Healthy Workplaces Campaigns of good practice, and several national best practice portals. This is a welcome development as it means that more institutions have recognized the need and added value of this approach. The exchange of best practices has a potential to improve health by demonstrating what interventions worked well in similar settings and populations, and it avoids “re-inventing the wheel” in designing and piloting similar interventions, building upon ones’ expertise and more efficient use of resources (14).
Nevertheless, the challenge of choosing the “right” approach and criteria in assessing the health promotion and disease prevention interventions still remains (15, 16). This was recognized as one of the important challenges at the EuroHealthNet Thematic Working Group on health promotion and disease prevention program registries (17). The development of the system for the assessment of health promotion and disease prevention interventions consists of several steps, from defining the criteria, development of evaluation methodology, selection of evaluators, piloting the assessment procedure, and, finally, regular use of the entire system/portal. An often-overlooked but important step is how the evaluators understand the criteria and methodology if it is properly used in assessing the interventions (18).
The main aim of our research was to test our criteria and assessment procedure for recognizing good practices in the field of public health by estimating the consistency between the evaluators, thereby gaining insight into the adequacy and reliability of the criteria as a measuring instrument for the assessment of the interventions and to check how the evaluators understand the criteria and methodology if it is properly used in assessing the interventions.
2 Methods
2.1 Assessment criteria for evidence-based public health interventions
The Slovenian “criteria for assessing public health interventions for the purpose of identifying and selecting good practices” were developed based on the European Commission’s Criteria to select best practices in health promotion and disease prevention and management in Europe (14, 19). The major difference between these criteria is that European Commission’s Criteria are focusing on selecting “best” practices while the Slovenian Criteria are intended to acquire also those practices that are recognized as examples of “good” practices and have a potential to further develop and improve.
The aim of the Slovenian criteria is to establish a system for recognizing examples of good practices and promote the use of these approaches in the field of public health. The objectives of the Slovenian HPPRs are (1): to raise the standards of public health interventions and improve their quality (2); to provide an overview on quality and effectiveness of public health interventions; and (3) to support knowledge exchange and the use of effective approaches by providing a pool of reviewed interventions.
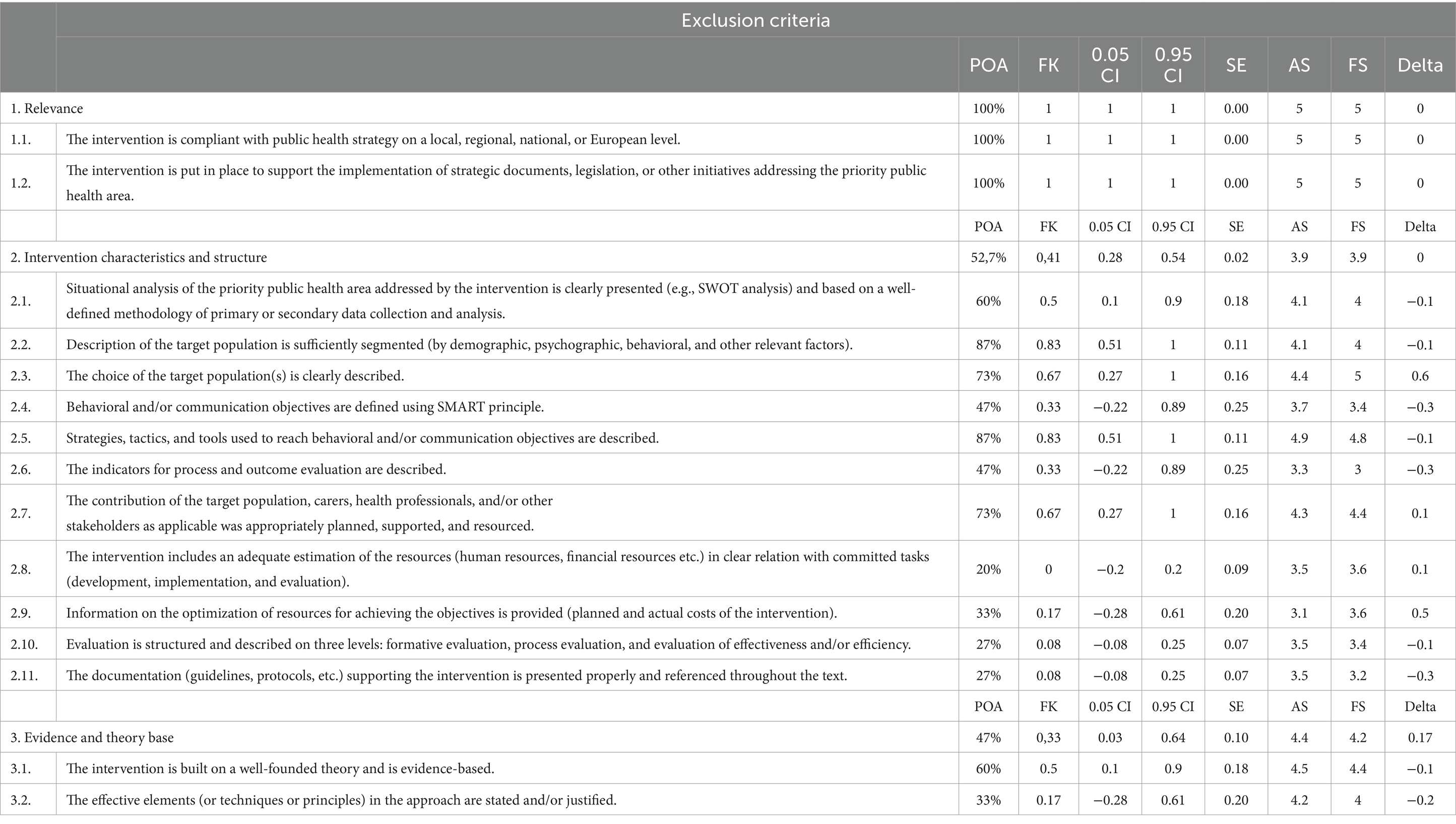
The criteria are organized in three levels, namely, exclusion, core, and additional criteria (Figure 1), and each group of criteria is used in successive manner to assess submitted interventions. The exclusion criteria assess the adequacy and completeness of the information provided and whether the intervention meets the basic conditions for further assessment. It is the first sieve, where it is assessed whether the intervention has a political and strategic relevance, is supporting current public health needs, furthermore these criteria are assessing if the intervention has a potential to produce beneficial results for the population in need in a scientifically sound manner, is free from any commercial benefits and have key elements for being successful or there is a risk that it could be harmful, unjust or ineffective. An intervention that passes the first inclusion threshold is further evaluated according to the core criteria that include its effectiveness and efficacy, as well as its contribution to reducing health inequalities. At the third level, the potential to transfer the intervention to other areas, another geographical environment, and another population is assessed. Therefore, additional criteria include an assessment of whether the interventions contain elements that enable the adaptation, upgrade, or transfer of the intervention to other settings. As recommended by many scholars, the Slovenian Criteria included the key elements for the assessment of public health interventions such as importance of assessing the implementation process and short-term and long-term outcomes, influence of contextual factors, importance of setting the objectives, theoretical underpinnings, and scope of interventions, and issues of sustainability, relevance, and stakeholder collaboration (4, 16, 20–26).
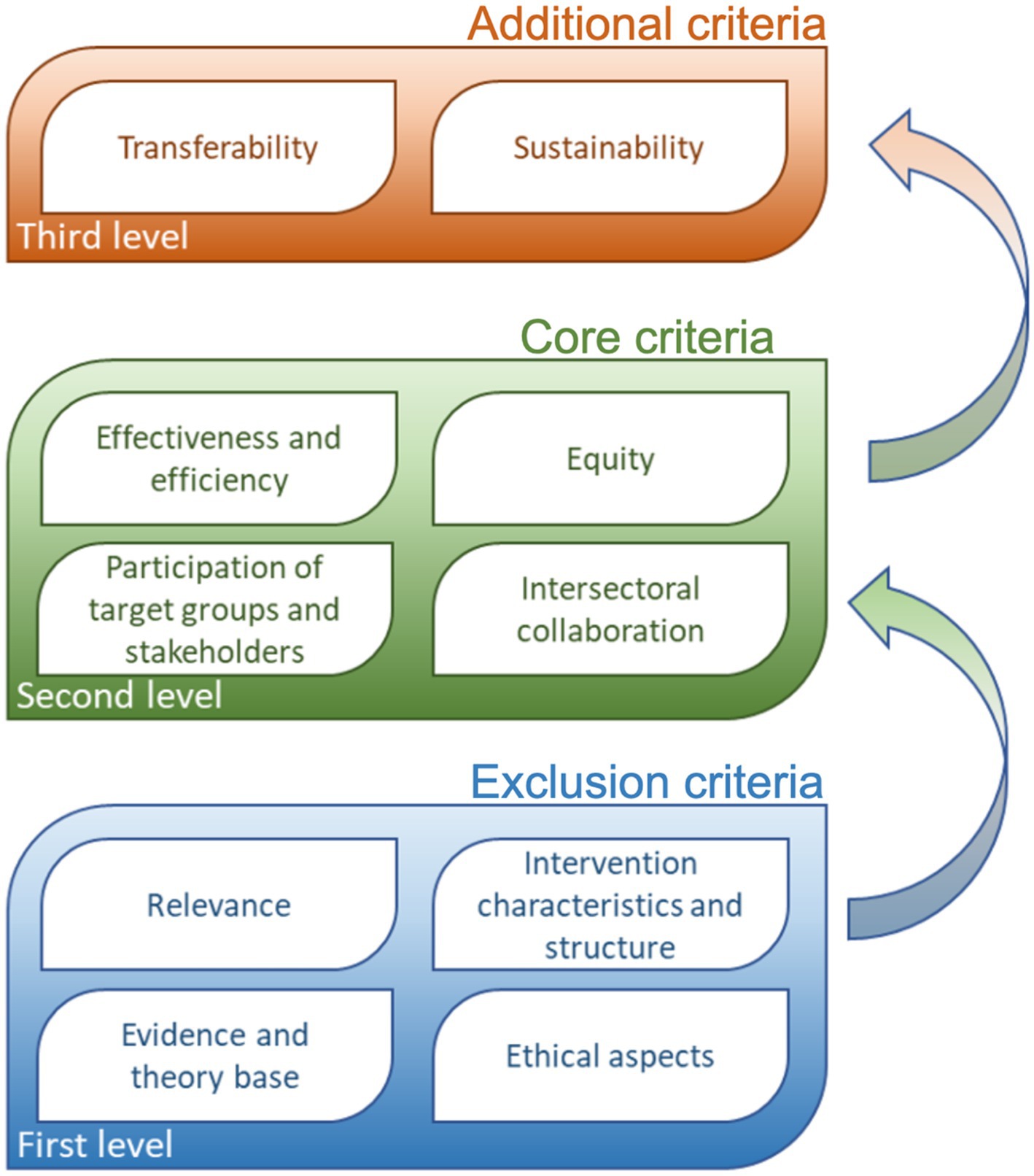
Figure 1. Criteria for assessing public health interventions for the purpose of identifying and selecting good practices.
For the purpose of assessment, each sub-criterion is assigned one of the numerical values (from 1–the intervention does not meet the requirements or does not take into account the criterion being studied or cannot be assessed due to missing or incomplete information to 5–the intervention successfully addresses all important aspects of the assessment criteria.), with the exception of the group of criteria used to evaluate the ethics of the intervention, where only yes or no answers were possible.
2.2 Data and processes
At least three public health professionals independently evaluated five interventions using the assessment criteria for evidence-based public health interventions (two interventions were evaluated by four evaluators and three interventions were evaluated by three evaluators). One evaluator was a medical doctor and an expert in the priority public health area that the interventions were addressing alcohol use. Second and third evaluators were medical doctors and experts in public mental health and epidemiology of non-communicable diseases. Fourth evaluator was a psychologist. The evaluators were familiar with each other, either due to working on the development of the Slovenian criteria or other public health research-related projects within the public health institute where they were all employed. The team of evaluators was selected on a personal invitation based on the leading expert of the team that developed Slovenian Criteria which also acted as one of the evaluators. Each intervention was evaluated by assigning a numerical value (from 1 to 5) to each criterion. The assessment took place from February 2021 to June 2022. Individual scores of the assessment criteria for each intervention were compiled, and a panel discussion was held to reach a consensus on the final score.
2.3 Statistical analysis
To determine the inter-rater agreement percent overall agreement (POA), Fleiss’ kappa (FK) coefficient with 95% confidence intervals and standard error were estimated (27). We assessed the inter-rater agreement on the level of the criteria for assessing public health interventions and the level of individual interventions that were included in the pilot assessment process. Values from 1.00 to 0.81 were described as high agreement, 0.80 to 0.61 were described as substantial agreement, 0.60 to 0.41 were described as moderate agreement, 0.40 to 0.21 were described as fair agreement, 0.20 to 0.00 were described as slight agreement, and values below 0.00 were described as poor agreement (28). Additionally, we provide average scores by individual evaluators (AS), final score (FS) reached, and the difference in scores between AS and FS (delta). To assess the correlation between average scores by individual evaluators and Fleiss’ kappa coefficient, Spearman’s Rho was calculated.
3 Results
Inter-rater agreement on the level of the assessment criteria group for evidence-based public health interventions was moderate (FK = 0.43 (0.36–0.49), SE = 0.0004) (54.1%) for overall agreement.
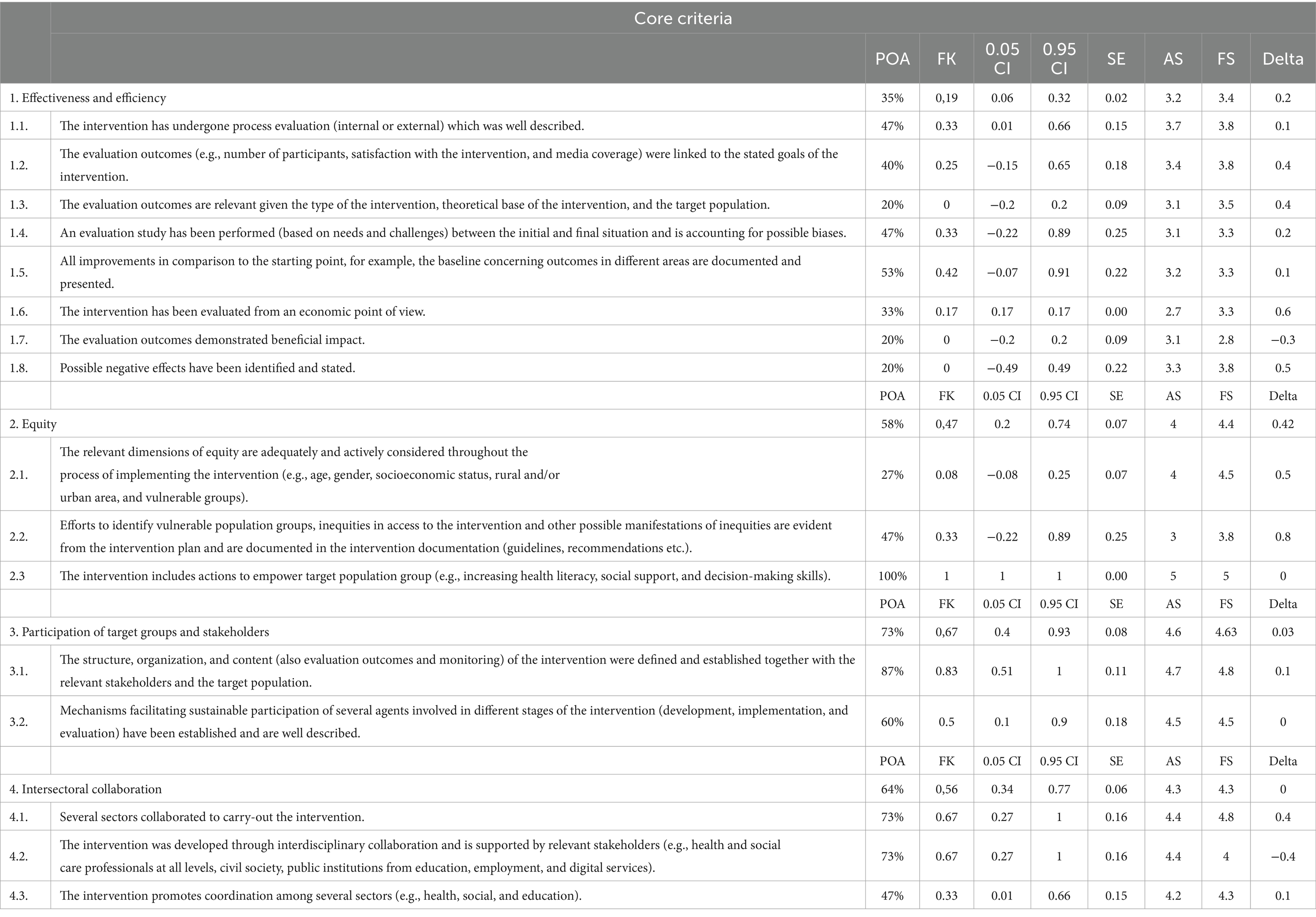
The highest inter-rater agreement on the level of exclusion criteria was achieved among the relevance sub-criteria group with all criteria rated 5 by all evaluators (Table 1). A moderate agreement was reached for the intervention characteristics and structure sub-criteria group, with slight agreement for criteria 2.8 to 2.11. The average FS and AS for this group was 3.9. Fair agreement was reached for the evidence and theory-based sub-criteria group, with an average FS of 4.2 and AS of 4.4.
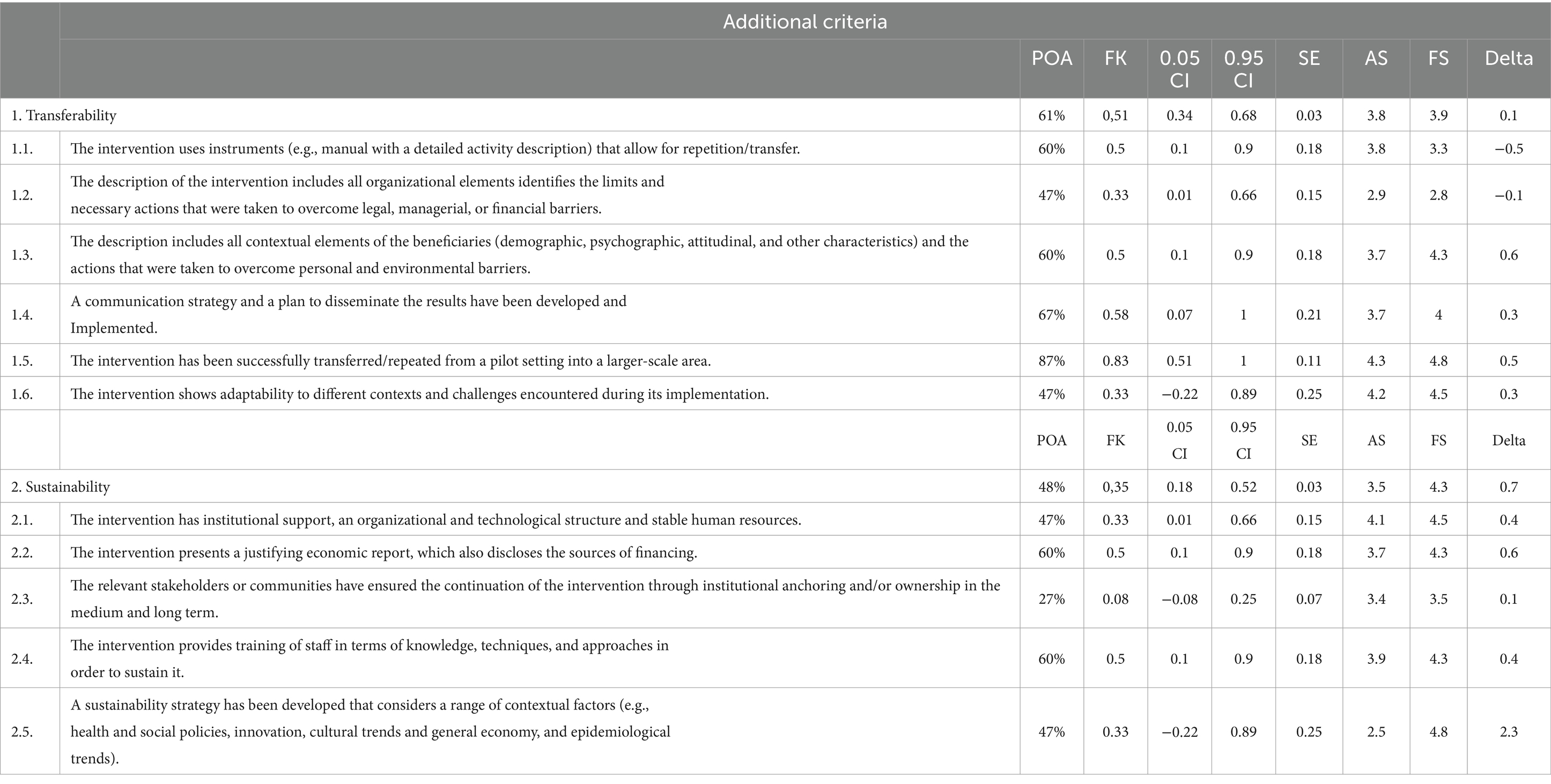
Among the core criteria group, the inter-rater agreement on the level of effectiveness and efficiency sub-criteria group was only slight (Table 2). Average FS in the sub-criteria group was 3.4 and the average AS was 3.2, which were the lowest scores of all sub-criteria groups. Inter-rater agreements of the equity, participation of target groups and stakeholders, and intersectoral collaboration sub-criteria groups were substantial or moderate with all reaching AS and FS of 4 or higher.
In the additional criteria group, the inter-rater agreement for the transferability sub-criteria group was moderate with an average FS of 3.9 and AS of 3.8 (Table 3). The agreement for the sustainability sub-criteria group was fair, with an average FS of 4.3 and AS of 3.5, which also had the largest difference between FS and AS among all sub-criteria groups.
A statistically significant correlation (rs = 0.73577, p < 0.0001) is present on the level of AS and FK with criteria with higher AS reaching higher inter-rater agreement and vice versa (Figure 2).
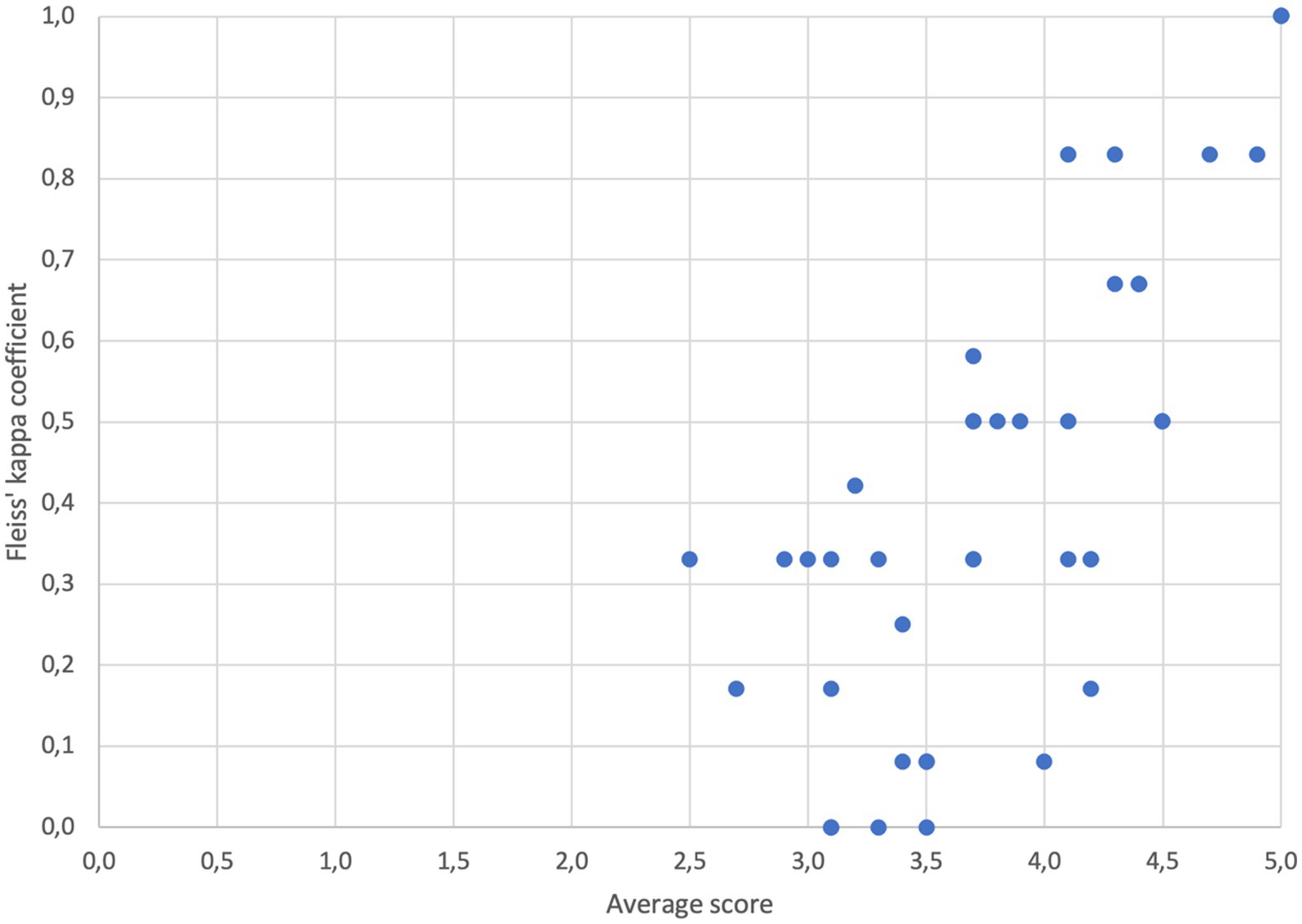
Figure 2. Association between average scores by individual evaluators and Fleiss’ kappa coefficient (rs = 0.73577, p < 0.0001).
4 Discussion
The primary purpose of an intervention assessment for recognizing the good practice in public health is to impact decision-making. The level of intricacy and accuracy required in the evaluation is contingent on the needs of the decision maker and the nature of decisions that will be made based on the results (29). The results presented in this article showed a moderately high degree of consistency in the assessment, demonstrating the validity of the Slovenian Criteria as a useful tool for identifying and promoting effective public health interventions. Despite being the first time that the criteria were used and the evaluators lacking prior experience, a moderate level of inter-rater agreement was achieved. As part of the comprehensive assessment, a concurrent review and updating of criteria was performed, resulting in the establishment and optimization of the assessment procedure.
The lowest agreement was observed for the effectiveness and efficiency of the sub-criteria group, which also received the lowest scores from the evaluators. A relationship between low scores and low inter-rater agreement was noted among the criteria. This could be attributed to the scoring method, where criteria were rated on a scale of 1 to 5 with descriptions for each grade. The grade 3 is described as “the intervention generally addresses this criterion well, with few shortcomings remaining.” The evaluators relied on these descriptions to score the interventions, but when interventions performed poorly, the evaluators had to determine the magnitude of shortcomings and score accordingly, leading to subjectivity. Additionally, criteria with varying specificity caused challenges in assigning scores, as the evaluator had to make subjective assessments of the contribution of individual processes or aspects to the final score. For example, criterion 1.3 in the core criteria group (“the evaluation outcomes are relevant given the type of the intervention, theoretical base of the intervention and the target population”) required the evaluator to provide a single score for three different but related aspects, which added complexity to the scoring process. The issue of subjectivity is probably common problem of health promotion and prevention program registries (HPPRs) since most European national HPPRs have developed assessment criteria divided into three to four main assessment sections and multiple sub-sections and are using scoring system that requires from the evaluator to determine how successful is the intervention in fulfilling the criteria and score accordingly (12, 18). In fact, some degree of subjective judgments is unavoidable in any evaluation, for instance, in weighing the importance of the various criteria used (30). In addition, Ng and De Colombani in their systematic literature review found out that the subjectivity at various stages of selection or evaluation is a universal feature across all reviewed sources (4).
The interventions were assessed using a questionnaire and supplementary intervention documentation such as guidelines and evaluation studies supplied by the owners of the interventions. The completeness and organization of the literature, however, varied greatly among the interventions, and some parts of the questionnaire were narrative and qualitative to accommodate the uniqueness of the practice, which could make it difficult for evaluators to extract the relevant information for scoring. To generate appropriate evidence for effective interventions, it is vital to adhere to the basic principles of evidence-based public health, which necessitate comprehensive intervention documentation (8, 31). Providing in-depth guidance on how to effectively present documentation before the assessments could greatly enhance the usability and effectiveness of the tool. This added level of detail can also help streamline the assessment process and make it simpler for users to understand and implement.
Similar methodological approaches are used in prevention programs that take place in a clinical setting confirming its usefulness in supporting decision-making process. For example, in breast cancer screening programs, radiologists perform a third independent reading in cases of disagreement between the first two independent readings, and the inter-rater agreement is then calculated (32, 33).
A limitation of our analysis is the choice of the inter-rater agreement measure we used (34). Since we did not use weighted Fleiss’ kappa coefficient or any other measure that consider the distance in the evaluation of inter-rater agreement, the magnitude of disagreement between raters is not reflected in the computed Fleiss’ kappa value. Additionally, evaluators did not receive training on the use of the criteria. It is expected that the agreement between evaluators would have been higher if they had received training in the use of the assessment tool before assessing the pilot interventions. The lack of training may have resulted in inconsistent application of the tool and a lower level of agreement among evaluators (35). However, the evaluators experienced public health professionals and sufficiently proficient in all theoretical and practical domains described by the criteria. Careful consideration of the composition of the panel of reviewers is recognized as an important element of the assessment procedure to avoid biases due to vested interests, and details of the composition should be made transparent (4).
5 Conclusion
The development and use of criteria for the assessment of practices that are considering different dimensions of the interventions in public health offers valuable insights for various stakeholders into the realm of public health. It caters to funders or clients by presenting a clear and informative categorization of practices into “best” and “good” categories. Additionally, it benefits researchers and practitioners who are involved in the development and implementation of interventions by offering specific feedback on each criterion that can assist in further refining the practice.
Despite confirmed usefulness and the importance of best practice assessment instruments, there is a relative lack of research on their performance (4). Furthermore, the literature on evaluator’s agreement in assessment of the specific intervention, as an important indicator of reliability of assessment procedure, is scarce. In this study we have shown that the inter-rater agreement differs across the sub-criteria groups depending on clarity of descriptions of specific criterion and scoring system, especially for the interventions that performed poorly or that were not successful in fulfilling the requirements of specific criterion or group of criteria. This discovery prompted us to investigate these criteria further and make necessary adjustments to increase the reliability of the assessment process. Studying the consistency between evaluators can provide valuable insights into the performance of the assessment instrument. This is not just of great importance for the institutions that are currently in the phase of developing or just have developed criteria for the assessment of interventions in the field of prevention and health promotion but also for well-established HPPRs. Such analysis can reveal areas of the assessment or specific criteria that perform inadequately and need improvement or adjustment. Through this process, researchers can gather valuable information that can be used to enhance the overall quality of the assessment instrument. Improving the assessment and selection process of good/best practices can then facilitate and promote the use of the practice-based evidence which can complement research findings in public health. Further research is needed to clarify the importance and usefulness of the inter-evaluator alignment and the best methodology for determining it.
To further improve best practice assessments, we suggest involving policymakers more extensively in the assessment process. This could include their participation in either the development or upgradation of the criteria and during the actual assessment process (36). While researchers may prefer to maintain independence from policymaking and implementation, public health research can have the most significant impact when researchers, practitioners, and decision-makers take responsibility for its production and application (37).
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The data is provided by the owners of the interventions included in the research. Requests to access these datasets should be directed to c3RhdGlzdGljbmEucGlzYXJuYUBuaWp6LnNp.
Author contributions
MV: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. TL: Conceptualization, Investigation, Methodology, Validation, Writing – review & editing. SR: Conceptualization, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to express their sincere gratitude to Gorazd Levičnik for his invaluable technical support throughout the course of this research. The authors would also like to thank Vida Peternelj for her support in evaluating best practices.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Budreviciute, A, Damiati, S, Sabir, DK, Onder, K, Schuller-Goetzburg, P, Plakys, G, et al. Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Front Public Health. (2020) 8:574111. doi: 10.3389/fpubh.2020.574111
2. Armstrong, R, Waters, E, Dobbins, M, Anderson, L, Moore, L, Petticrew, M, et al. Knowledge translation strategies to improve the use of evidence in public health decision making in local government: intervention design and implementation plan. Implement Sci. (2013) 8:121. doi: 10.1186/1748-5908-8-121
3. Faggiano, F, Allara, E, Giannotta, F, Molinar, R, Sumnall, H, Wiers, R, et al. Europe needs a central, transparent, and evidence-based approval process for Behavioural prevention interventions. PLoS Med. (2014) 11:e1001740. doi: 10.1371/journal.pmed.1001740
4. Ng, E, and De Colombani, P. Framework for selecting best practices in public health: a systematic literature review. J Public Health Res. (2015) 4:577. doi: 10.4081/jphr.2015.577
5. Glasgow, RE, Lichtenstein, E, and Marcus, AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. (2003) 93:1261–7. doi: 10.2105/AJPH.93.8.1261
6. Farris, RP, Haney, DM, and Dunet, DO. Expanding the evidence for health promotion: developing best practices for WISEWOMAN. J Women's Health. (2002) 13:634–43. doi: 10.1089/1540999041281098
7. Green, LW. Public health asks of systems science: to advance our evidence-based practice, can you help us get more practice-based evidence? Am J Public Health. (2006) 96:406–9. doi: 10.2105/AJPH.2005.066035
8. Ammerman, A, Smith, TW, and Calancie, L. Practice-based evidence in public health: improving reach, relevance, and results. Annu Rev Public Health. (2014) 35:47–63. doi: 10.1146/annurev-publhealth-032013-182458
9. Brownson, RC, Fielding, JE, and Maylahn, CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health. (2009) 30:175–201. doi: 10.1146/annurev.publhealth.031308.100134
10. Ng, E. A methodological approach to “best practices” In: E Øyen, editor. Best practices in poverty reduction: an analytical framework. London: Zed Books (2002).
11. Stratil, JM, Biallas, RL, Movsisyan, A, Oliver, K, and Rehfuess, EA. Anticipating and assessing adverse and other unintended consequences of public health interventions: the (CONSEQUENT) framework. SSRN Electron J. (2023) 2023:4347085. doi: 10.2139/ssrn.4347085
12. Rossmann, C, Krnel, SR, Kylänen, M, Lewtak, K, Tortone, C, Ragazzoni, P, et al. Health promotion and disease prevention registries in the EU: a cross country comparison. Arch Public Health. (2023) 81:85. doi: 10.1186/s13690-023-01097-0
13. Quinn, E, Huckel-Schneider, C, Campbell, D, Seale, H, and Milat, AJ. How can knowledge exchange portals assist in knowledge management for evidence-informed decision making in public health? BMC Public Health. (2014) 14:443. doi: 10.1186/1471-2458-14-443
14. Stepien, M, Keller, I, Takki, M, and Caldeira, S. European public health best practice portal - process and criteria for best practice assessment. Arch Public Health. (2022) 80:131. doi: 10.1186/s13690-022-00892-5
15. Jetha, N, Robinson, K, Wilkerson, T, Dubois, N, Turgeon, V, and Des, MM. Supporting knowledge into action: the Canadian best practices initiative for health promotion and chronic disease prevention. Can J Public Health. (2008) 99:I1–8. doi: 10.1007/BF03405258
16. Kahan, B, and Goodstadt, M. The interactive domain model of best practices in health promotion: developing and implementing a best practices approach to health promotion. Health Promot Pract. (2001) 2:43–67. doi: 10.1177/152483990100200110
17. Gilardi, L, and Maassen, A. Good practice portals: mapping and evaluating interventions for health promotion, disease prevention and equity across Europe. Euro Health Net Magazine (2020). Available at: https://eurohealthnet-magazine.eu/good-practice-portals-mapping-and-evaluating-interventions-for-health-promotion-disease-prevention-and-equity-across-europe/.
18. Fernandez, ME, Ruiter, RAC, Markham, CM, and Kok, G. Intervention mapping: theory-and evidence-based health promotion program planning: perspective and examples. Front Public Health. (2019) 7:209. doi: 10.3389/fpubh.2019.00209
19. Radoš Krnel, S, Kamin, T, Jandl, M, Gabrijelčič Blenkuš, M, Hočevar Grom, M, Lesnik, T, et al. Merila za vrednotenje intervencij na področju javnega zdravja za namen prepoznavanja in izbire primerov dobrih praks. Ljubljana: National Institute of Public Health of Slovenia (2020). Available at: https://www.nijz.si/sites/www.nijz.si/files/publikacije-datoteke/merila.pdf
20. Rootman, I. Evaluation in health promotion: Principles and perspectives. Geneva: WHO Regional Office Europe (2001).
21. Albert, D, Fortin, R, Lessio, A, Herrera, C, Riley, B, Hanning, R, et al. Strengthening chronic disease prevention programming: The toward evidence-informed practice (TEIP) program assessment tool. Prev Chronic Dis. (2013) 10:E88. doi: 10.5888/pcd10.120106
22. Thurston, WE, Vollman, AR, Wilson, DR, MacKean, G, Felix, R, and Wright, MF. Development and testing of a framework for assessing the effectiveness of health promotion. Soz Praventivmed. (2003) 48:301–16. doi: 10.1007/s00038-003-2057-z
23. Hercot, D, Meessen, B, Ridde, V, and Gilson, L. Removing user fees for health services in low-income countries: a multi-country review framework for assessing the process of policy change. Health Policy Plan. (2011) 26 Suppl 2:ii5-15. doi: 10.1093/heapol/czr063
24. World Health Organization. Health promotion evaluation: Recommendations to policy-makers: Report of the WHO European working group on health promotion evaluation. Copenhagen: WHO Regional Office for Europe (1998).
25. Bauer, G, Davies, JK, Pelikan, J, Noack, H, Broesskamp, U, Hill, C, et al. Advancing a theoretical model for public health and health promotion indicator development: proposal from the EUHPID consortium. Eur J Pub Health. (2003) 13:107–13. doi: 10.1093/eurpub/13.suppl_1.107
26. Bollars, C, Kok, H, Van den Broucke, S, and Mölleman, G. European quality instrument for health promotion. User man Verfügbar Unter Httpsubsites Nigz Nlsysteem 3site2index cfm. (2005).
27. Randolph, JJ. Free-marginal multirater kappa (multirater K[free]): an alternative to Fleiss’ fixed-marginal multirater kappa. Online Submission (2005). Available at: https://eric.ed.gov/?id=ED490661.
28. Landis, JR, and Koch, GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33:159–74. doi: 10.2307/2529310
29. Habicht, JP, Victora, CG, and Vaughan, JP. Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. Int J Epidemiol. (1999) 28:10–8. doi: 10.1093/ije/28.1.10
30. Glasgow, RE, Klesges, LM, Dzewaltowski, DA, Estabrooks, PA, and Vogt, TM. Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res. (2006) 21:688–94. doi: 10.1093/her/cyl081
31. Brownson, RC, Baker, EA, Deshpande, AD, and Gillespie, KN. Evidence-based public health. 3rd ed. Oxford, NY: Oxford University Press (2017). 368 p.
32. Guertin, MH, Théberge, I, Dufresne, MP, Zomahoun, HTV, Major, D, Tremblay, R, et al. Clinical image quality in daily practice of breast cancer mammography screening. Can Assoc Radiol J. (2014) 65:199–206. doi: 10.1016/j.carj.2014.02.001
33. Jarm, K, Kadivec, M, Šval, C, Hertl, K, Žakelj, MP, Dean, PB, et al. Quality assured implementation of the Slovenian breast cancer screening programme. PLoS One. (2021) 16:e0258343. doi: 10.1371/journal.pone.0258343
34. Gisev, N, Bell, JS, and Chen, TF. Interrater agreement and interrater reliability: key concepts, approaches, and applications. Res Soc Adm Pharm. (2013) 9:330–8. doi: 10.1016/j.sapharm.2012.04.004
35. Pufpaff, LA, Clarke, L, and Jones, RE. The effects of rater training on inter-rater agreement. Mid West Educ Res. (2015) 27:3.
36. Loncarevic, N, Andersen, PT, Leppin, A, and Bertram, M. Policymakers’ research capacities, engagement, and use of research in public health policymaking. Int J Environ Res Public Health. (2021) 18:11014. doi: 10.3390/ijerph182111014
Keywords: criteria, evidence-based interventions, public health practice, public health interventions, good practice portals
Citation: Vinko M, Lesnik T and Radoš Krnel S (2024) Evaluator’s alignment as an important indicator of adequacy of the criteria and assessment procedure for recognizing the good practice in public health. Front. Public Health. 12:1286509. doi: 10.3389/fpubh.2024.1286509
Edited by:
Nick Sevdalis, National University of Singapore, SingaporeReviewed by:
Christian T. K. -H. Stadtlander, Independent Researcher, Destin, FL, United StatesKeren Dopelt, Ashkelon Academic College, Israel
Copyright © 2024 Vinko, Lesnik and Radoš Krnel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matej Vinko, bWF0ZWoudmlua29Abmlqei5zaQ==
 Matej Vinko
Matej Vinko Tina Lesnik
Tina Lesnik Sandra Radoš Krnel
Sandra Radoš Krnel