- 1Menelik II Medical and Health Science College, Addis Ababa, Ethiopia
- 2The Three Aid Foundation, Barneveld, Netherlands
Introduction: The satisfaction of the public with the healthcare system of Ethiopia is a crucial but unanswered question. This is an essential issue since recent trends indicate that the demographic and epidemiological makeup of the population is changing. Therefore, the aim of this study was to assess the overall satisfaction of the public with the Ethiopian healthcare system in Addis Ababa, Ethiopia, in 2022.
Methods: A community-based convergent parallel mixed methods study was conducted. Bivariable and multivariable logistic regression analyses were used to determine the factors associated with public satisfaction. A 95% confidence interval along with a p < 0.05 was deemed sufficient to declare a significant association. For the qualitative component, we used thematic analysis.
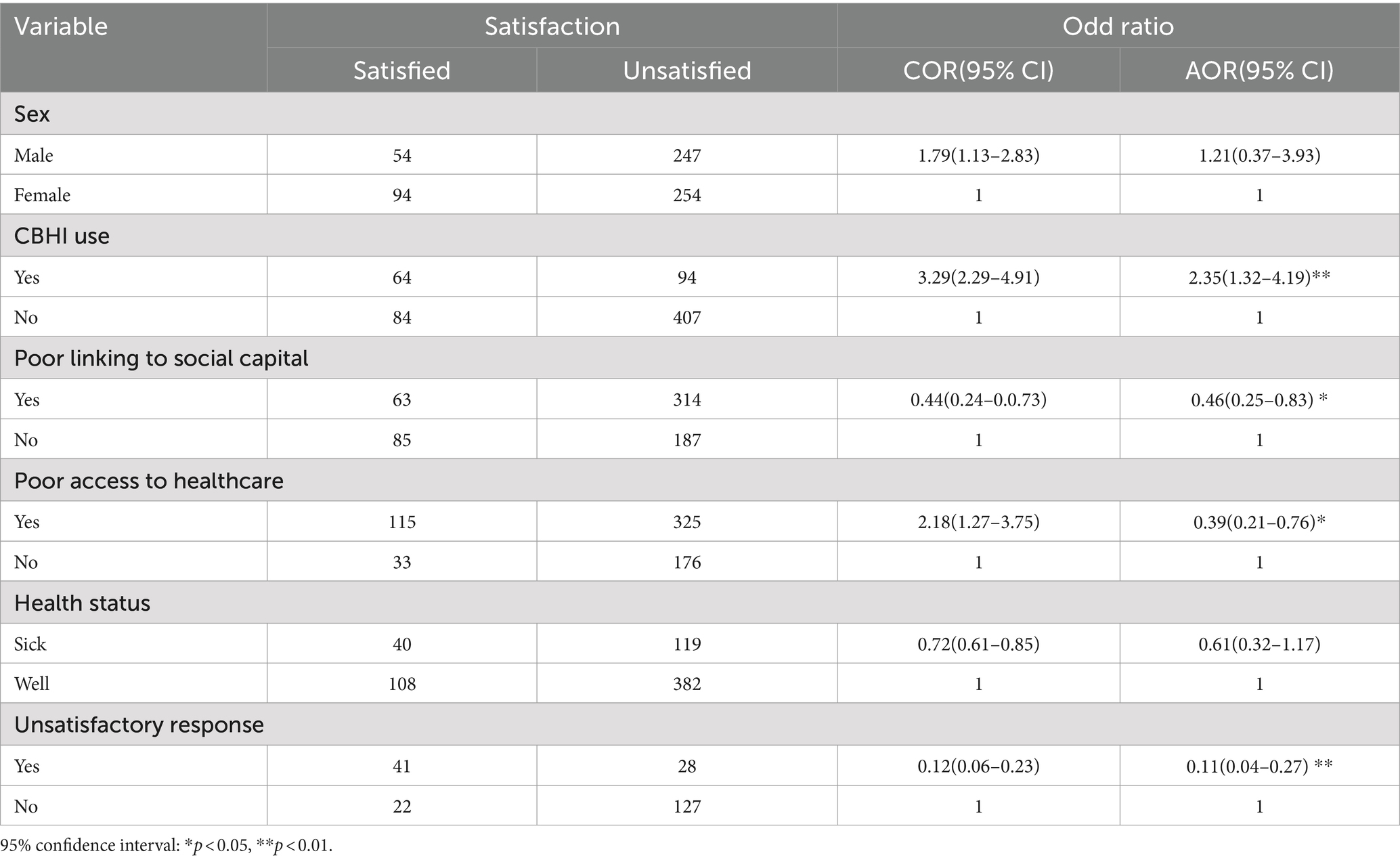
Results: The vast majority, 77.2% (95% CI: 76.18–78.22%), of respondents were dissatisfied with the existing healthcare system. Moreover, Community-Based Health Insurance (CBHI) enrollment (2.35; 95% CI: 1.32–4.19), poor linkage to social capital (0.46; 95% CI: 0.25–0.83), poor access to healthcare services (0.39; 95% CI: 0.21–0.76), and absence of satisfactory responses to complaints (0.11; 95% CI: 0.04–0.27) were significantly associated with public dissatisfaction.
Conclusion: Public satisfaction with the Ethiopian healthcare system is notably low and is affected by various factors, including enrollment in the CBHI, linkage to social capital, accessibility to healthcare, and satisfactory response to issues. Therefore, the Ethiopian government should focus on expanding CBHI coverage, improving access to healthcare services, and developing an immediate compliant solution strategy.
1 Introduction
Public satisfaction is a fundamental indicator of healthcare service quality and serves as a means of assessing healthcare performance (1). Globally, healthcare service strategies are becoming more reliant on public satisfaction, which is considered a basic criterion for evaluating clinical efficiency and performance improvement (2). Accreditation and regulatory requirements from organizations such as the National Committee on Quality Assurance (NCQA) and the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) prove the need for quantifiable public satisfaction data as a crucial component of performance improvement programs (3, 4).
Public satisfaction is a comprehensive element that reflects consumers’ perceptions and attitudes toward their overall experience with healthcare services (5). The WHO uses public satisfaction with the healthcare system as one of the metrics to evaluate the quality of healthcare services (6–8). It is well recognized that patient satisfaction significantly influences their likelihood of seeking additional medical advice, adhering to their treatment plan, and maintaining an ongoing and friendly relationship with their healthcare practitioner (9, 10). In addition, public satisfaction might vary depending on the tool used to measure it, making it difficult to determine a precise level of satisfaction (11, 12). A study carried out in 30 different countries found that, despite some variations within each of those countries, people in the developed world generally agree that public acceptance is fairly high (8).
While accessibility, quality, financial burden, and healthcare equity have all been individually measured and assessed in the past, in countries such as Ethiopia, public opinion can only be inferred from other studies in which patient and/or healthcare professional satisfaction has been fairly explored (13, 14). The evaluation of public perception and satisfaction might aid in the decision-making process to improve the responsiveness of the healthcare system (15–17).
The Ethiopian healthcare system is vulnerable to many criticisms and opinions (18). Issues related to poor healthcare delivery, minimal healthcare coverage, and low adherence to community-based insurance are just a few of the numerous factors that could be taken into consideration (19, 20).
The assessment of public opinion and satisfaction can help for a better understanding of the public’s needs and improve quality health services by identifying their determinant factors through a continuous quality improvement process (21, 22). Ignorance of public opinion, on the other hand, may be a roadblock to reaching milestones by combining public perception and understanding with available resources to achieve universal healthcare (17, 23). In addition, in the context of Ethiopia’s current health sector reform, healthcare facilities are working to improve the effectiveness, efficiency, and quality of the services they provide (24). Moreover, this study was conducted to explore the current context and the determinants of healthy individuals’ satisfaction with the health services provided after the reform. Therefore, this study aimed to assess the overall satisfaction of healthy individuals with the Ethiopian healthcare system in Addis Ababa, Ethiopia, in 2022.
2 Methods
2.1 Study area and period
This study was conducted in Addis Ababa, Ethiopia. Addis Ababa is the capital city of Ethiopia, which is a metropolitan city in the highlands of Ethiopia with an area of 527 km2, an elevation of 2,355 m2, and a population of approximately 5 million people (25). Addis Ababa is the most densely populated and urbanized city in Ethiopia, with a high concentration of both public and private health institutions and an easily accessible target group. There are 11 sub-cities and 116 districts. The data were collected between February and April 2022.
2.2 Study design and population
We used a community-based convergent parallel mixed methods study (interpretative paradigm; a social science approach that asserts that understanding the beliefs, motivations, and reasoning of individuals in a social situation is critical to decoding the meaning of data gathered around a phenomenon). All households in selected sub-cities of Addis Ababa, Ethiopia, were considered the study population.
2.3 Eligibility criteria
All selected individuals over the age of 18 years were included in the study. However, individuals who lived in the selected areas for <6 months or who were unable to communicate for any reason were excluded from the study.
2.4 Sample size determination and sampling procedure
For the quantitative study, the sample size was calculated using a single population proportion formula considering an assumption of a 50% prevalence to have a relatively larger sample size, a 5% precision at the 95% confidence level, and a 15% non-response rate.
Since multistage sampling was used, considering a 1.5 design effect and a 15% non-response rate provided a required sample size of 663. For the qualitative study, a theoretical maximum saturation technique was applied.
Multistage sampling was used, starting with the 11 sub-cities of Addis Ababa. Simple random sampling (lottery method) was used to select three sub-cities (Kolfe Keranio, Yeka, and Lideta). From each sub-city, three districts (woreda) were chosen using the lottery method, and using proportional allocation, the number of households was determined.
A convenience sampling method was used for the key informant interviews. New volunteers were gathered for the interview until data saturation was achieved (no new ideas were emerging). Subsequently, nine participants were included in this study. The goal of the qualitative components was to explain the barriers and facilitators of public satisfaction.
2.5 Study variables and operational definition
Public satisfaction was considered an outcome variable, and the independent variables were categorized as intra-personal, interpersonal, community, and organizational-related factors.
Intra-personal factors were as follows: age, sex, educational status, employment status, income, health status, and wellbeing.
Interpersonal factors were as follows: social capital (bonding, bridging, and linking), marital status, and family size.
Organizational and public policy included political affiliation, enrollment in a health insurance scheme, and attitude toward the healthcare system.
Satisfaction factors included fulfillment of one’s objectives, expectations, or requirements in relation to one’s healthcare experience.
Healthcare system included institutions, people, and resources involved in providing public healthcare.
2.6 Data collection procedure
The data were collected using a pretested questionnaire, which was developed after reviewing previous similar studies (9, 11, 14). For the quantitative part, data were collected through an interviewer-administered questionnaire that was developed in English first and translated into the local language Amharic and then returned to English to ensure consistency and maintain conceptual equivalence. The data were collected through house-to-house visits. The data collection was begun with the permission and consent of the study participants. The respondents were quizzed on socio-demographic, interpersonal or relationship, organizational, and policy-related questions. The validity of the questionnaire was evaluated by subject-matter experts and senior researchers. Moreover, the reliability of the tool was checked using Cronbach’s alpha coefficient, and the result was 0.71, indicating that the rule was not violated. Data quality was assured through pretesting the questionnaire and careful supervision during data collection. Pre-testing was conducted at Arada Sub-City with 34 study participants prior to the actual data collection to estimate the time required for each data collection and testing the tool. Following that, we made modifications to some components of the questionnaire.
The qualitative data, on the other hand, were collected through an in-depth discussion guided by an interview guide. The interview guide asked questions about the importance of friends, family, and society in making decisions about healthcare, the quality and expense of healthcare services, the attitudes, behaviors, and communication styles of healthcare providers, the accessibility of medical supplies and resources through community-based health insurance programs, and the respondents’ satisfaction with the overall services received.
All of the interviewees provided their consent for their voices to be recorded and interviewed. The interview lasted between 30 and 45 min. The key informants that were approached for this study had no prior relationship with the interviewer, which helped to minimize the possibility of bias.
2.7 Data quality management and analysis
Before analysis, the data were cleansed and double-checked for completeness and consistency. The quantitative data were collected, categorized, coded, and entered into EPI Info version 7.2.1 before being exported to SPSS for further analysis. A binary and multivariable logistic regression analysis was performed to assess the statistical significance and strength of the association between independent variables and public satisfaction. A p < 0.05 in the final multivariable logistic regression analysis model was considered significantly associated. Based on the data acquired, the findings of the study were provided in the form of tables, figures, and text. The results of the study were presented using tables, figures, and texts.
For the qualitative component, we used an inductive technique to investigate the intricacies of the public’s perspective of the healthcare system, as well as the reasons for their contentment or displeasure with it. Data were collected only from adults since they were more likely to interact with the healthcare system on their own. The interviews were transcribed for analysis by the principal investigators, and the remaining two co-authors, who are skilled in collecting qualitative data, translated the transcripts into English. Then, we looked for recurring themes and variances in the transcripts and field notes. After that, the coder read over each transcript to make sense. Using the preliminary code guide, all transcripts were coded individually. The final version of the code guide was developed by following these procedures. Then, the transcript was converted to open-code 4.03 format. Finally, the investigators looked into the relationships between the codes that had been generated previously and categorized them into groups.
2.8 Ethical consideration
Ethical clearance was obtained from Kotebe Metropolitan University, Menelik II Medical and Health Science College Ethical Committee. A permission letter was secured from the Addis Ababa City Administration Health Bureau Public Health Record and Emergency Management Directorate. Formal letters of cooperation were given to each district, and written consent was obtained from individual participants by explaining the aim of the research.
3 Results
3.1 Socio-demographic characteristics of the study participants
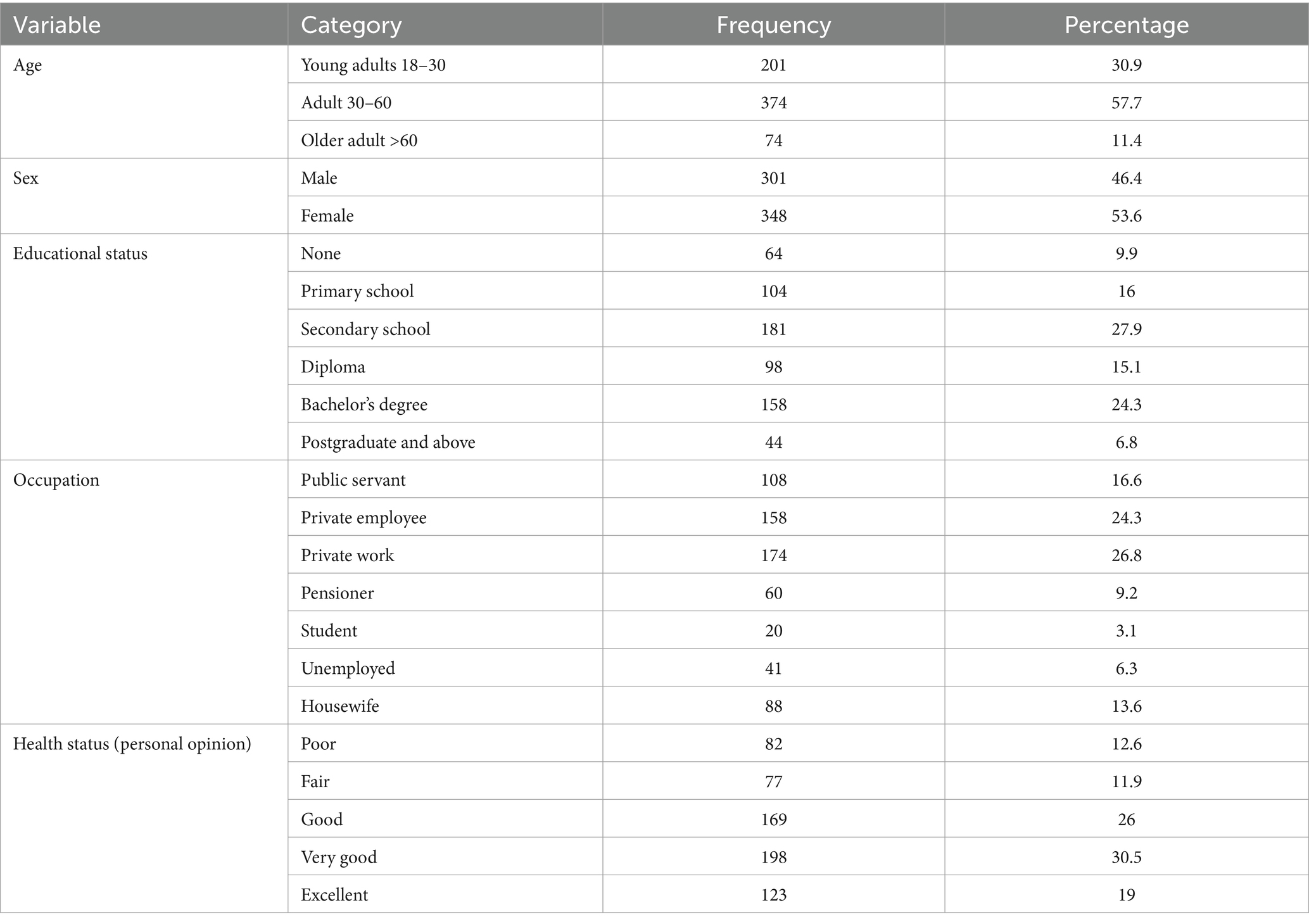
From a total of 663 study participants, a complete set of information was obtained from 649 respondents, giving a response rate of 97.9%. The mean and standard deviation of the age of respondents were 41.3 (±15.8) years, with a range of 18–86 years. The majority of the study participants were private workers and employees, comprising 26.8 and 24.3%, respectively. More than half (53.6%) of the respondents were women (Table 1).
3.2 Interpersonal (relationship)-related characteristics
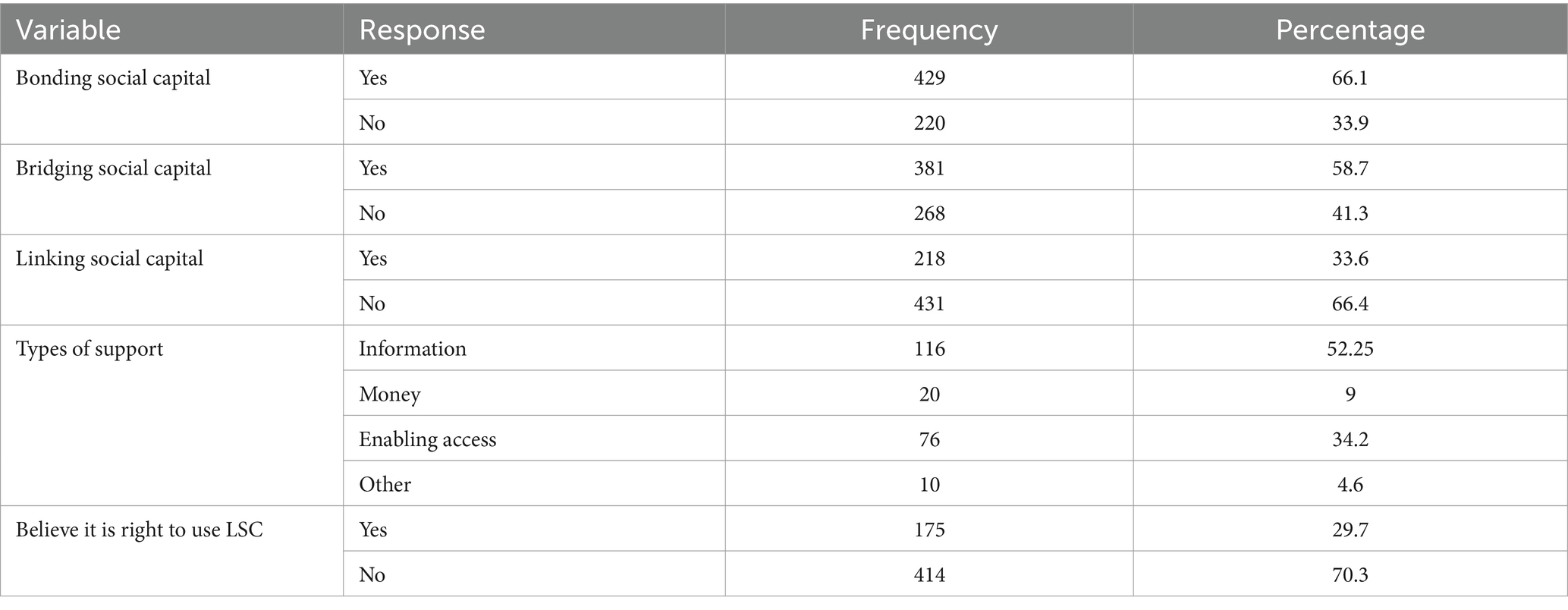
According to the data obtained from this study, the majority (66.4%) of the study participants reported that they had a strong linking social capital followed by 66.1% bonding social capital as a relationship-related domain (Table 2).
3.3 Organizational and public policy-related domains
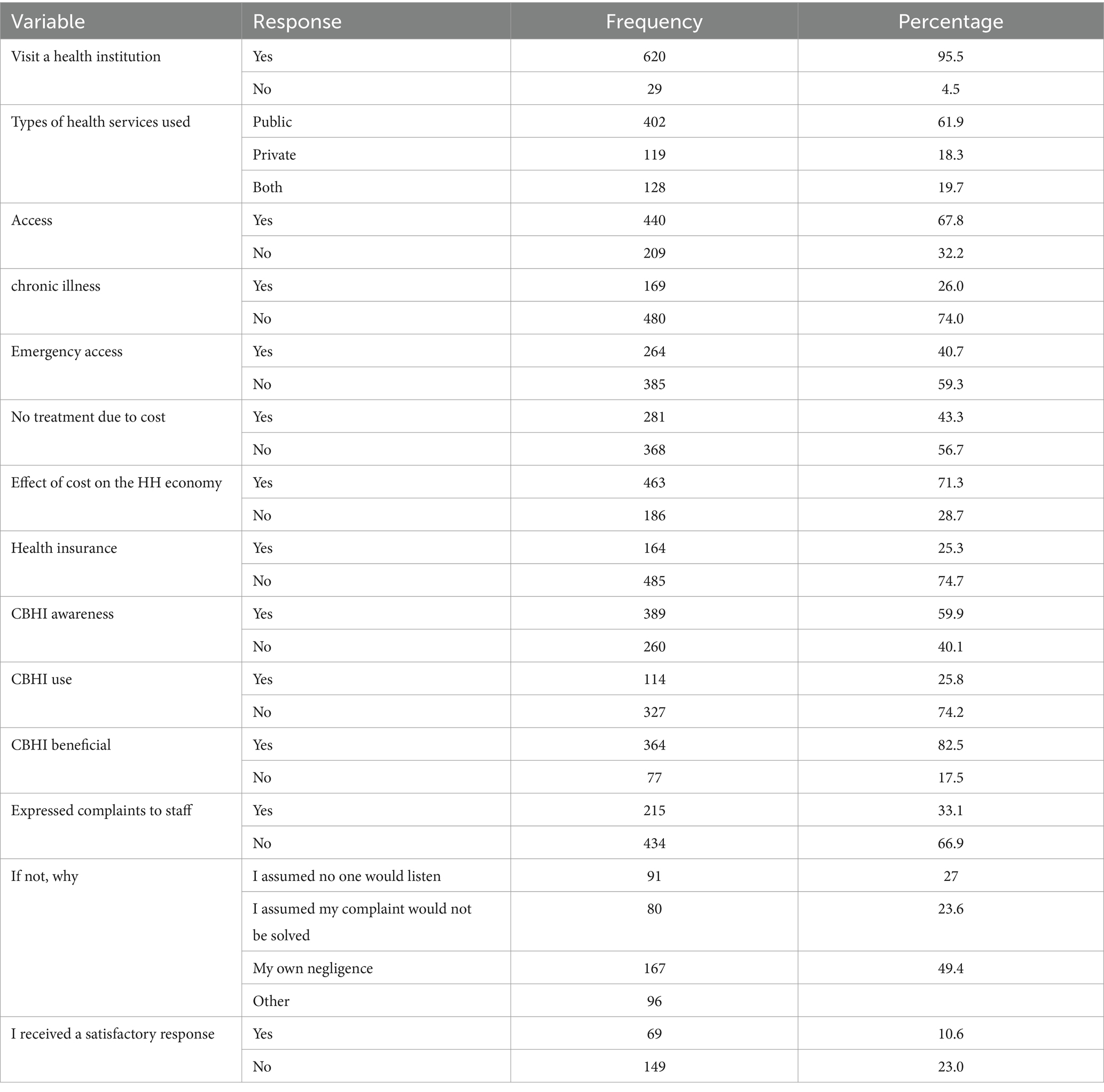
Almost all (95.5%) respondents reported having visited health institutions, with public health organizations being the most common. In addition, only 40.7% of the respondents believed that they had emergency access to health services. Moreover, 25.8 and 10.7% of the total individuals interviewed were CBHI users and satisfied with the responses provided by healthcare providers, respectively (Table 3).
3.4 Level of public satisfaction with the Ethiopian healthcare system
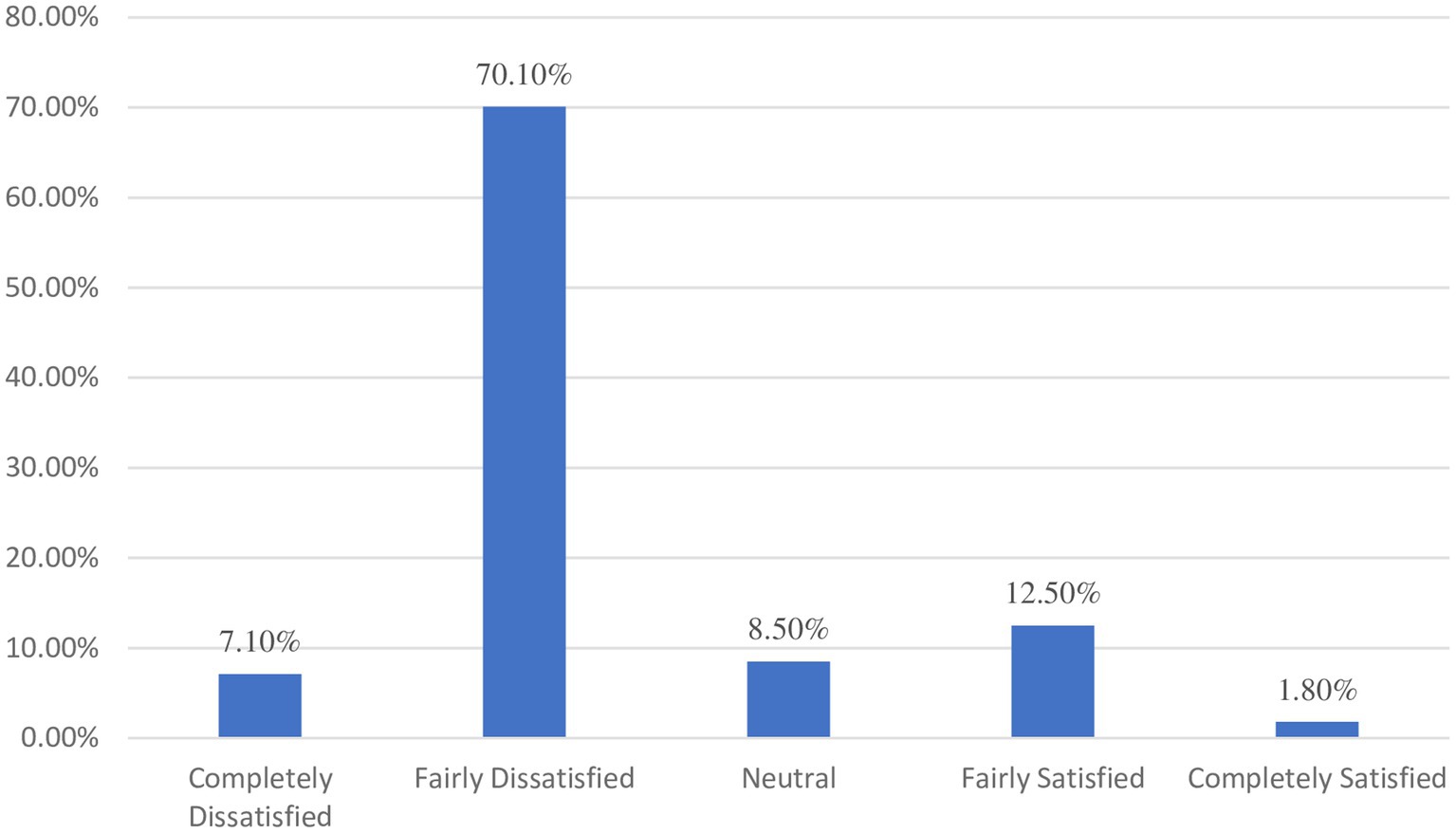
The majority of respondents, 77.2% (95% CI: 76.18–78.22), were dissatisfied with the existing healthcare system, with 7.1% being completely dissatisfied. On the other hand, 12.5% reported being fairly satisfied, and 1.8% responded that they were completely satisfied (Figure 1).
3.5 Factors associated with respondents satisfaction level
In multivariable logistic regression analysis, variables with a p < 0.25 from the bivariable analysis were identified. As a result, CBHI enrollment, linking with social capital, access to healthcare services, and satisfactory responses to client complaints were significantly associated with the satisfaction level at a p < 0.05.
Respondents enrolled in CBHI had more than two times (2.35, 95% CI: 1.32–4.19) more odds of being satisfied with the Ethiopian healthcare system than their counterparts who were not enrolled. On the other hand, study participants who had poor linkage to social capital had (0.46; 95% CI: 0.25–0.83) 54% higher odds of being dissatisfied with the Ethiopian healthcare system than their counterparts. Furthermore, study participants who had unsatisfactory responses to their complaints had 0.11 (95% CI: 0.04–0.27) or 89% more odds of having poor satisfaction than their counterparts. Study participants who had poor access to health care services had a 61% higher odds of dissatisfaction 0.39 (95% CI: 0.21-0.76) compared with their counterparts (Table 4).
3.6 Qualitative results
The respondents’ opinions can be categorized into three clusters or themes that cross over one another. The key finding is that respondents to varying degrees were dissatisfied.
3.6.1 Theme 1: cost of healthcare
One of the main causes of respondents’ discontent with the healthcare system was mentioned as the expense of healthcare or financial obstacles. A 45-year-old government-employed male study participant explained the issue as follows:
“In contrast to affordability and access, the primary concern of private health service providers is money. The cost makes it challenging to receive treatments on a regular basis. As I noticed it throughout the time of my surgery.”
Other respondents agreed that CBHI plays a critical role and expressed hope that it would help ease some of the financial challenges that public healthcare facilities, particularly in the public sector, are currently experiencing. Two women, aged 51 and 39 years, expressed their opinions as follows:
“I’ve heard about CBHI, and it sounds like a wonderful idea. Although I do not use CBHI, it would be beneficial for those with chronic illnesses like mine to have more affordable access to care and medication.”
“I am confident that CBHI offers treatment and aftercare services at a reasonable cost since I have seen it in action.”
3.6.2 Theme 2: attitudes and behaviors of health personnel
One major source of participant unhappiness was the attitude of the medical staff. People who have social connections with healthcare professionals tend to get better care, which is largely related to the interpersonal level of social capital linkage.
“People who have social relationships with healthcare experts have better access to care, prescriptions, and other facilities in both the private and public health sectors. However, if you do not have someone, you will inevitably experience all the drawbacks, especially if you aren’t paired with a trustworthy or familiar person.”
In addition, a widespread criticism among participants was the administrative staff’s and professionals’ failure to listen to and address issues. Moreover, a 35-year-old man reported his experience as follows:
“Based on my experience, understanding patient concern is critically important to enhance health services, but doing so is impossible due to the unwillingness of administrative and medical staff to take complaints seriously or find solutions.”
Another thing to note is that respondents have extremely strong ideas about how unqualified health service providers treat people, and several said they would stress adequate training for health workers if they could.
“According to my observations, one of the major issues in the nation is the carelessness of professionals, which is a result of their inadequate training and education as well as their unethical treatment of patients. Because of the carelessness of specialists, I have lost relatives.”
3.6.3 Theme 3: public opinion on the adequateness of medical facilities and their services
According to previous findings, the public is dissatisfied with the healthcare system and the health services provided in both private and public settings for a variety of reasons. The majority of respondents cited the inadequacy of medical facilities and their services as one of the main causes of this dissatisfaction.
“Despite the high cost, private health institutions provided relatively better satisfaction despite having insufficient access to both public and private healthcare facilities. My personal experience with the medical care I have received and witnessed being provided to others has left me very unsatisfied.”
Some respondents stated that the major reasons they feel the need to attend private institutions are the difficulties they encounter and the general inadequacy of public institutions.
“I avoid going to public health facilities because it’s difficult to find professionals there, and even when medications have been ordered, it can be challenging to obtain them. I’ve also seen people travel far and wide in search of medications that are out of their price range. For these reasons, I usually go to private health facilities. Going to a public health facility is usually inconvenient, which is why I select a private facility.”
4 Discussion
This study used a mixed methods approach to provide an assessment of public opinions and satisfaction with the healthcare system in Ethiopia. The degree of satisfaction with the given healthcare services significantly influences a person’s decision to seek medical advice, adherence to treatment, and keeping a positive connection with healthcare providers. According to this report, dissatisfaction (77.2%; 95% CI: 76.18–78.22) with the healthcare system is far greater than satisfaction. It is higher than previous study findings from different parts of Ethiopia, including 53.8% in Addis Ababa (26), 38.1% in Southwest Ethiopia (27), 36.3% from a systematic review and meta-analysis in Ethiopia (28), and 33% in Nairobi, Kenya (29). The possible reason behind this might be due to the difference in study period and measurement tools used to quantify the satisfaction. In addition, the variations in the dedication of healthcare administrators and healthcare professionals may be the difference.
Several significant factors were observed in this study, with four standing out: CBHI enrollment, social capital linkage, access to healthcare services, and a satisfactory response from health professionals regarding their complaints were statistically associated with public satisfaction.
As established in the quantitative portion and supported by the qualitative interviews, participants who used and believed in their linking social capital with health professionals were more likely to be satisfied with the healthcare system. As a result, participants with poor linking social capital had 54% (95% CI: AOR = 0.46, 0.25–0.83) higher odds of dissatisfaction than their counterparts. This result was in line with a study finding from Ghana (14). According to the findings, people are more likely to receive better care when they have a social relationship with medical experts. This will consequently change their perception of the efficacy and caliber of the care they receive. On the other hand, people without a strong social network might feel that it is inappropriate to use and are considerably less likely to be happy with the medical care they receive. The qualitative findings also reveal that there is some animosity toward individuals who have social capital links and toward professionals who are believed to treat people with whom they have a social relationship more favorably (30, 31).
When compared to non-users, those who were enrolled through CBHI were substantially more likely to report feeling satisfied with the current state of healthcare. As a result, those research participants who used CBHI had more than two times (95% CI: AOR = 2.35, 1.32–4.19) higher odds of being satisfied than their counterparts. Studies previously carried out in Bangladesh and Ethiopia reported similar findings (32, 33). This could be due to the fact that people’s happiness with the health system is greatly influenced by the absence or reduced burden of health-related costs as these charges are more likely to have an impact on their household budgets (32). Even though the majority of the respondents in the qualitative component were not CBHI beneficiaries, it is noted that some respondents favor and think it should be made more freely available.
Moreover, the findings of this study showed that those study participants who have had their complaints satisfactorily resolved have a much higher likelihood of being pleased with their health treatment. The result was consistent with previous study results conducted in different countries (34–36). According to the in-depth interview findings, respondents’ major complaints were about appropriate and satisfactory responses from healthcare providers. It is important to emphasize that, in spite of every complaint that respondents have voiced, how the public perceives the healthcare system is mostly dependent on the competence of administrators, personnel, or healthcare professionals to appropriately resolve issues.
Poor access to healthcare services was also identified as a significant factor for public dissatisfaction. Those respondents who perceived poor access to healthcare services had 89% higher odds of dissatisfaction with the healthcare system than their counterparts. It was consistent with a study finding from earlier research (37, 38). The fact that healthcare services are becoming a more competitive market justifies the negative correlation between poor access to healthcare services and satisfaction with the care received.
5 Limitations of the study
The study was conducted from the viewpoint of the general public, as opposed to patients who had more recent experiences. As a result, this study may have some recall bias. Furthermore, because the study concentrated on the general population and broad socio-ecological issues, it was challenging to dig deeply into the specifics. Therefore, this could be a subject for future research including a larger and more diverse sample size.
6 Conclusion
According to the current study findings, the majority of respondents (77.2%) were dissatisfied with the Ethiopian healthcare system. Furthermore, the benefit of CBHI, access to healthcare services, and satisfactory resolutions of complaints were the most important elements for public satisfaction. As a result, managers of healthcare facilities should develop a strategy for improving access to healthcare services and CBHI enrollment to improve the satisfaction of the public with the Ethiopian healthcare system.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Kotebe Metropolitan University, Menelik II Medical and Health Science College Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
GG: Conceptualization, Formal analysis, Writing – review & editing. BD: Conceptualization, Data curation, Supervision, Writing – original draft. SB: Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the study participants and data collectors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Salmani, N, Abbaszadeh, A, Rasouli, M, and Hasanvand, S. The process of satisfaction with nursing care in parents of hospitalized children: a grounded theory study. Int J Pediatr. (2015):3, 1021–1103.
2. Prakash, B . Patient satisfaction. J Cutan Aesthet Surg. (2010) 3:151–5. doi: 10.4103/0974-2077.74491
3. Hahn, KA, Gonzalez, MM, Etz, RS, and Crabtree, BF. National Committee for quality assurance (NCQA) patient-centered medical home (PCMH) recognition is suboptimal even among innovative primary care practices. J Am Board Family Med. (2014) 27:312–3. doi: 10.3122/jabfm.2014.03.130267
5. Al-Abri, R, and Al-Balushi, A. Patient satisfaction survey as a tool towards quality improvement. Oman Med J. (2014) 29:3–7. doi: 10.5001/omj.2014.02
6. Footman, K, Roberts, B, Mills, A, Richardson, E, and McKee, M. Public satisfaction as a measure of health system performance: a study of nine countries in the former Soviet Union. Health Policy. (2013) 112:62–9. doi: 10.1016/j.healthpol.2013.03.004
7. Amoah, PA . Social participation, health literacy, and health and well-being: a cross-sectional study in Ghana. SSM-Population Health. (2018) 4:263–70. doi: 10.1016/j.ssmph.2018.02.005
8. Yuan, Y . Public satisfaction with health care system in 30 countries: the effects of individual characteristics and social contexts. Health Policy. (2021) 125:1359–66. doi: 10.1016/j.healthpol.2021.08.005
9. Wagner, D, and Bear, M. Patient satisfaction with nursing care: a concept analysis within a nursing framework. J Adv Nurs. (2009) 65:692–701. doi: 10.1111/j.1365-2648.2008.04866.x
10. Abolfotouh, MA, Al-Assiri, MH, Alshahrani, RT, Almutairi, ZM, Hijazi, RA, and Alaskar, AS. Predictors of patient satisfaction in an emergency care Centre in Central Saudi Arabia: a prospective study. Emerg Med J. (2017) 34:27–33. doi: 10.1136/emermed-2015-204954
11. Shirley, E, Josephson, G, and Sanders, J. Fundamentals of patient satisfaction measurement. Phys Leadership J. (2016) 3:12
12. Larson, E, Sharma, J, Bohren, MA, and Tunçalp, Ö. When the patient is the expert: measuring patient experience and satisfaction with care. Bull World Health Organ. (2019) 97:563–9. doi: 10.2471/BLT.18.225201
13. Wamai, RG . Reviewing Ethiopia’s health system development. Japan Med Assoc J. (2009) 52:279–86.
14. Eriksson, M . Social capital and health – implications for health promotion. Glob Health Action. (2011) 4:5611. doi: 10.3402/gha.v4i0.5611
15. Darby, C, Valentine, N, De Silva, A, and Murray, CJ. Strategy On Measuring Responsiveness. Geneva: World Health Organization (WHO) (2003).
16. Amoah, PA, Nyamekye, KA, and Addo, EO. A multidimensional study of public satisfaction with the healthcare system: a mixed-method inquiry in Ghana. BMC Health Serv Res. (2021) 21:1–17. doi: 10.1186/s12913-021-07288-1
17. Zimmerman, E, and Woolf, SH. Understanding the relationship between education and health. NAM Perspect. (2014) 4:347–84. doi: 10.31478/201406a
18. Almomani, R, Al-Ghdabi, R, and Banyhamdan, K. Patients’ satisfaction of health service quality in public hospitals: a PubHosQual analysis. Management Sci Lett. (2020) 10:1803–12. doi: 10.5267/j.msl.2019.12.038
19. Mirach, TH, Demissie, GD, and Biks, GA. Determinants of community-based health insurance implementation in west Gojjam zone, Northwest Ethiopia: a community based cross sectional study design. BMC Health Serv Res. (2019) 19:1–8. doi: 10.1186/s12913-019-4363-z
20. Xesfingi, S, and Vozikis, A. Patient satisfaction with the healthcare system: assessing the impact of socio-economic and healthcare provision factors. BMC Health Serv Res. (2016) 16:1–7. doi: 10.1186/s12913-016-1327-4
21. Akale, SY, Getahun, GK, Akalu, SY, and Alaminie, FA. Assessment of urban health extension package utilization and healthcare seeking behavior among model and non-model households in Addis Ababa, Ethiopia: a comparative community based study. Nutr Res. (2024) 251:911658149. doi: 10.32388/H3F4OU.2
22. Park, K, Park, J, Kwon, YD, Kang, Y, and Noh, JW. Public satisfaction with the healthcare system performance in South Korea: universal healthcare system. Health Policy. (2016) 120:621–9. doi: 10.1016/j.healthpol.2016.01.017
23. Wallin, E, Lundgren, PO, Ulander, K, and Von Holstein, CS. Does age, gender or educational background effect patient satisfaction with short stay surgery? Ambul Surg. (2000) 8:79–88. doi: 10.1016/S0966-6532(99)00039-6
24. Yip, W, and Hafez, RWorld Health Organization. Improving health system efficiency: Reforms for improving the efficiency of health systems: Lessons from 10 country cases. Geneva: World Health Organization (2015).
25. CSA . 2007 population and housing census of Ethiopia: administrative report. Addis Ababa: CSA (2012).
26. Asamrew, N, Endris, AA, and Tadesse, M. Level of patient satisfaction with inpatient services and its determinants: a study of a specialized hospital in Ethiopia. J Environ Public Health. (2020) 2020:1–12. doi: 10.1155/2020/2473469
27. Woldeyohanes, TR, Woldehaimanot, TE, Kerie, MW, Mengistie, MA, and Yesuf, EA. Perceived patient satisfaction with in-patient services at Jimma University specialized hospital, Southwest Ethiopia. BMC Res Notes. (2015) 8:1–8. doi: 10.1186/s13104-015-1179-8
28. Biresaw, H, Mulugeta, H, Endalamaw, A, Yesuf, NN, and Alemu, Y. Patient satisfaction towards health care services provided in Ethiopian health institutions: a systematic review and meta-analysis. Health Serv Insights. (2021) 14:117863292110406. doi: 10.1177/11786329211040689
29. Ndambuki, J . The level of patients’ satisfaction and perception on quality of nursing services in the renal unit, Kenyatta National Hospital Nairobi, Kenya. Open J Nurs. (2013) 3:186–94. doi: 10.4236/ojn.2013.32025
30. Nieminen, T, Prättälä, R, Martelin, T, Härkänen, T, Hyyppä, MT, Alanen, E, et al. Social capital, health behaviours and health: a population-based associational study. BMC Public Health. (2013) 13:1–11. doi: 10.1186/1471-2458-13-613
31. Tariq, M . Social capital as a determinant of population health outcomes: a global perspective Pakistan. Econstor. (2018) 12:52–77. Available at: https://hdl.handle.net/10419/188335
32. Sarker, AR, Sultana, M, Ahmed, S, Mahumud, RA, Morton, A, and Khan, JA. Clients’ experience and satisfaction of utilizing healthcare services in a community based health insurance program in Bangladesh. Int J Environ Res Public Health. (2018) 15:1637. doi: 10.3390/ijerph15081637
33. Getahun, GK, Kinfe, K, and Minwuyelet, Z. The role of community-based health insurance on healthcare seeking behavior of households in Addis Ababa, Ethiopia. Prev Med Rep. (2023) 34:102234. doi: 10.1016/j.pmedr.2023.102234
34. Bjertnaes, OA, Sjetne, IS, and Iversen, HH. Overall patient satisfaction with hospitals: effects of patient-reported experiences and fulfilment of expectations. BMJ Quality Safety. (2012) 21:39–46. doi: 10.1136/bmjqs-2011-000137
35. Bidmon, S, Elshiewy, O, Terlutter, R, and Boztug, Y. What patients value in physicians: analyzing drivers of patient satisfaction using physician-rating website data. J Med Internet Res. (2020) 22:e13830. doi: 10.2196/13830
36. Manzoor, F, Wei, L, Hussain, A, Asif, M, and Shah, SI. Patient satisfaction with health care services; an application of physician’s behavior as a moderator. Int J Environ Res Public Health. (2019) 16:3318. doi: 10.3390/ijerph16183318
37. Shi, L, Lebrun-Harris, LA, Daly, CA, Sharma, R, Sripipatana, A, Hayashi, AS, et al. Reducing disparities in access to primary care and patient satisfaction with care: the role of health centers. J Health Care Poor Underserved. (2013) 24:56–66. doi: 10.1353/hpu.2013.0022
38. Stepurko, T, Pavlova, M, and Groot, W. Overall satisfaction of health care users with the quality of and access to health care services: a cross-sectional study in six central and eastern European countries. BMC Health Serv Res. (2016) 16:1–3. doi: 10.1186/s12913-016-1585-1
Keywords: public satisfaction, social ecological model, healthcare system, Ethiopia, mixed method study
Citation: Getahun GK, Demissie BD and Baraki SG (2024) Public satisfaction with the Ethiopian healthcare system: a mixed methods approach. Front. Public Health. 12:1275233. doi: 10.3389/fpubh.2024.1275233
Edited by:
Meghna Ranganathan, University of London, United KingdomReviewed by:
Faiza Manzoor, Zhejiang University, ChinaSurapaneni Krishna Mohan, Panimalar Medical College Hospital and Research Institute, India
Copyright © 2024 Getahun, Demissie and Baraki. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Genanew Kassie Getahun, Z2VuYW5hdzIxa2Fzc2F5ZUBnbWFpbC5jb20=
‡ORCID: Genanew Kassie Getahun, https://orcid.org/0000-0002-0796-5433
 Genanew Kassie Getahun
Genanew Kassie Getahun Bemnet Dires Demissie
Bemnet Dires Demissie Semere Gebremariam Baraki
Semere Gebremariam Baraki