
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 09 February 2024
Sec. Life-Course Epidemiology and Social Inequalities in Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1264230
Background: There is a scarcity of research on discriminatory experiences and their association with health outcomes among Syrian Refugees in Norway. Thus, this study aims to examine the relationship between perceived discrimination, self-rated health (SRH), chronic pain, poor mental health, and healthcare utilization among Syrian refugees resettled in Norway.
Methods: Cross-sectional data from the Integration for Health project were analyzed, including 154 Syrian refugees who resettled in Norway in 2018–19. Perceived discrimination, SRH, chronic pain, psychological distress, post-traumatic stress symptoms, and healthcare visits were assessed. Statistical analyses, including Poisson regression and multinomial logistic regression, were conducted. The significant statistical level was set at 0.05.
Results: Approximately 30% of participants reported experiencing discrimination, with no significant associations between sociodemographic factors and perceived discrimination. Perceived discrimination was significantly associated with psychological distress (adjusted PR: 2.07, 95%CI: 1.21–3.55), post-traumatic stress symptoms (adjusted PR: 11.54, 95%CI: 1.25–106.16), and 4 or more psychologist visits (adjusted OR: 12.60, 95%CI: 1.72–92.16). However, no significant associations were found between perceived discrimination and SRH; pain symptoms, or general healthcare utilization.
Conclusion: Experienced discrimination is highly prevalent and seems to be associated with mental health outcomes, but not clearly with SRH, pain, or general healthcare visits among Syrian refugees living in Norway. Efforts should focus on reducing discrimination, promoting social inclusion, and improving access to mental health services for refugees. Public awareness campaigns, anti-discrimination policies, and cultural training for healthcare professionals are recommended to address these issues and improve the well-being of Syrian refugees in Norway.
The appropriate integration of refugees in their new home countries is a global humanitarian concern, with millions of individuals forced to leave their home countries due to conflicts and persecution. Among these displaced populations, Syrian refugees constitute one of the largest groups worldwide (1). The Syrian refugee crisis has led to the displacement of millions of individuals who have fled their homes due to violence, persecution, and war. Since the start of the conflict in 2011, more than six million Syrians have been internally displaced, and around five million have sought asylum in other countries or have been placed in refugee camps worldwide (2). As of 2021, UNHCR reported that more than a million Syrian asylum-seekers and refugees ended up in the European Union (EU), with Germany and Sweden being the main host countries (3). In Norway, the Syrian immigrant population increased substantially between 2011 and 2018 (4). Since September 2015, more than half of the asylum seekers to Norway have been from Syria, with a total of 30,110 asylum seekers arriving in Norway in that year (5). The latest data from 2023 indicates 42,397 Syrian refugees are currently living in Norway (6).
Discrimination is defined as the unequal treatment of individuals or groups based on their race, ethnicity, nationality, religion, or immigration status. It can be experienced in various forms, including verbal abuse, physical violence, and social exclusion (7). Although Norway is known for its commitment to human rights and social justice, Syrian refugees living in Norway may still face discrimination, which can have negative impacts on their health and access to healthcare (8, 9). In examining the report from Norway in 2018, the United Nations Committee on the Elimination of Racial Discrimination highlighted concerns about the lack of equal treatment in recruitment processes and the disproportionately high unemployment rate among immigrants in Norway (10). Additionally, a survey in 2020 by the Norwegian Institute for Social Research revealed that the number of Norwegians who believe discrimination occurs “to a large degree” has tripled in the last 6 years, indicating an increasing acknowledgment of discrimination against immigrants in Norway (11). In a study on perceived discrimination among migrants in Norway in 2016, approximately 27% of participants reported perceived discrimination, ranging from 12.8% among Sri Lankans to 38.7% among Iranian Immigrants (12). However, the absence of Syrian refugees in the sample necessitates further investigation to delineate their specific experiences of discrimination.
Discrimination, both perceived and experienced, is recognized as a significant stressor that can negatively impact the mental and physical health of immigrants (12, 13). Discrimination based on race, ethnicity, nationality, religion, or immigration status is consistently associated with poor mental health outcomes in refugees and asylum seekers in general (14). Regular discrimination in daily life has been linked to individuals’ overall poor self-assessment of health and a higher likelihood of experiencing one or more chronic diseases (15). A study in 2016 among migrant groups in Norway observed poorer mental health among migrant groups with discriminatory experiences, however, the Syrian refugees were not represented in this study (12). There might be differences among refugee groups that have to be better understood, as failing to recognize or acknowledge discrimination can have negative health consequences for some individuals from specific groups (16). Despite Syrians being the fourth-largest migrant group in Norway (6), there remains limited research addressing their specific needs. Studies have been conducted on the health-related quality of life and mental distress of Syrian refugee youth resettled in Norway (7), the use of healthcare services among Syrian refugees migrating to Norway (8), and mental health in adult refugees from Syria resettled in Norway (9). However, there is no specific information on the unique discriminatory experiences and consequent psychological outcomes among Syrian refugees in Norway.
Chronic pain is a common health problem that can significantly affect an individual’s function and quality of life. Different forms of pain have been linked to stress through the concept of allostatic load, which is defined as the cumulative wear and tear on the body due to adapting to adverse physical or psychosocial situations such as those caused by perceived discrimination in migrants (17, 18). Recent evidence has indicated that immigrants and refugees may face unique challenges in managing pain conditions, which could be exacerbated by the experience of discrimination (19–21); however, no research has specifically focused on the association between perceived discrimination and chronic pain among Syrian migrants in Norway. Understanding the association between perceived discrimination and these specific pain conditions is crucial for developing targeted interventions and improving the health outcomes of this migrant group.
Discrimination can also limit refugees’ access to regular healthcare, exacerbating physical and mental health problems and creating barriers to recovery and well-being (22, 23). Experiences with discrimination can lead to decreased trust, avoidance of healthcare services, and disparities in health outcomes and could be associated with delays in seeking medical care and poor adherence to medical care recommendations (24, 25). Additionally, refugees and asylum seekers face several barriers to accessing healthcare (26) and evidence shows unmet healthcare needs among specific groups (27), especially when it comes to mental and dental health in the EU member states (28, 29). However, there is limited knowledge of the unique experiences of different migrant groups, particularly Syrian refugees, in accessing healthcare services and the extent to which discrimination affects their health outcomes in Norway (30). Lack of appropriate health care can in turn lead to adverse outcomes like increased diabetes comorbidities (31), and low adherence among hypertensive patients (32). In the latest report on the National strategy to equalize social health differences by the Norwegian Ministry of Health and Care Services, discrimination in access to healthcare among migrants and minorities has been acknowledged repeatedly (33); however, the report failed to specifically address this issue which makes it necessary to explore more the underlying causes and produce clear evidence for the Norwegian context. Additionally, we need granularity of evidence for specific migrant groups to account for both differences in religious and cultural backgrounds of refugees this case Syrian refugees well as sociopolitical contexts of host country, in this case Norway.
Against this background, the purpose of this paper is to examine the relationship of perceived discrimination with self-rated health, pain conditions, poor mental health, and utilization of health services among Syrian refugees resettled in Norway in 2018–19 using the latest data from the Integration for Health project (I4H). In this study, we explored the discrimination experiences of Syrian refugees in Norway and provided valuable knowledge for the association of such experiences with the health challenges they face and their utilization of health services in Norway.
We used cross-sectional data from the I4H project, which followed up on the Changing Health and Health Care Needs Along the Syrian Refugees’ Trajectories to Norway (CHART) project (34, 35). In the first wave of CHART, all adults (16 + years) Syrian refugees in Lebanon, who were deemed to move to Norway according to the UNHCR quota at two specific missions facilitated by the International Organizartion of Migrants (IOM), were invited, recruited, and interviewed (2016–17) (N = 506, 98% of invited). The same cohort was followed up in wave 2 of the CHART project a year after settlement in Norway (2017–18) of which 464 could be tracked and invited for an interview and 350 completed the interview. In I4H, the same cohort (n = 464) was approached and invited for an interview approximately 4 years after living in Norway (2021–22) and 154 completed the interview. The interview was conducted on the phone by bilingual interviewers (Arabic, Norwegian) using a researcher-developed questionnaire on the SurveyXact platform. The main reason for attrition (154/464) in the I4H project was the inability to reach out to the participants due to changes in their contact information or not responding after three phone contact attempts. In addition, two deaths and one deaf participant were excluded. The interviews were conducted from September 2022 to February 2023. The questionnaire was developed by the Int4Health team including bilingual members (Arabic, Norwegian), and was based on the previous CHART questionnaires. The questionnaire collected data on the participants’ scoiodemograhy, physical health, mental health, perceived discrimination, and integration using validated questions from relevant standard scales. The questionnaire was translated into the Arabic language by a professional entity and the accuracy and comprehensibility of the questionnaires were assessed through a pilot study recruiting 11 Syrian refugees during which attempts were made to replicate the real interview scenario by two bilingual interviewers (Arabic, Norwegian) supervised by a bilingual advisor (Arabic, Norwegian). The questionnaire was revised minorly after the pilot study to enhance the comprehensibility of the questionnaire.
Sociodemographic variables included age, sex, marital status, education level, annual income, having children, and number of children. Perceived discrimination was assessed by asking about the frequency of experiencing discrimination by authorities, at work/school, by nationality, and by race using a 5-point Likert scale (never, seldom, sometimes, often, very often), using four validated questions from the refugee post-migration stress scale (RPMS) which is proved to be a valid instrument among Syrian refugees (36). A composite variable for perceived discrimination was further created by combining the four types of discrimination with two alternative responses (0 “never/seldom,” 1 “sometimes/often/very often”).
Self-rated health (SRH) was measured by asking “How do you consider your health at the moment?” on a 5-point Likert scale (1 “very bad,” 2 “bad,” 3 “fair,” 4 “good,” and 5 “very good”), a validated question from the European Social Survey 2010 (37), this variable further recoded as 1″ poor,” 2″ fair,” and 3 “good” (38). Chronic pain (lasted >6 months) was assessed by asking “Do you have physical pain now that has lasted more than 6 months?,” a single, validated question from the Trøndelag Health Study (HUNT) study (39). Psychological distress was assessed by the Hopkins Symptom Checklist (HSCL-10), which required participants to reflect on their experiences over the past week and quantify the severity of various anxiety and depression symptoms using a 4-point Likert scale. A mean HSCL-10 score of 1.85 (range 1–4) was used as a cut-off indicating clinically relevant psychological distress (40). Post-traumatic stress symptoms (scores>2.5 on the HTQ scale) were assessed by the Harvard Trauma Questionnaire (HTQ) on a 4-point Likert scale with a mean HTQ score of 2.5 (range 1–4) as a threshold, indicating the possibility of clinically significant symptoms relevant to post-traumatic stress disorder (PTSD) (41). GP/specialist/psychologist visits were measured by asking “During the last 12 months, have you visited any of the following?” with three alternative responses (No, 1–3 times, 4 or more times), a question from the HUNT study (39).
Descriptive statistics were used to present the distribution of sample characteristics and prevalence of perceived discrimination by type, as well as the prevalence of outcomes of interest including SRH, chronic pain, psychological distress, post-traumatic stress symptoms, and GP/specialist/psychologist visits in the past 12 months. Principal Component Analysis (PCA) was employed to facilitate the construction of a composite variable for perceived discrimination, intended for subsequent utilization in multivariate analysis. Combining the four questions related to discrimination was instigated by the low number of positive responses for each question which hindered reliable and powerful individual multivariate analyses. This approach was supported by the results produced in PCA analysis in which we realized that all four questions reflect the same construct (perceived discrimination). This was evidenced by the emergence of a single factor with an eigenvalue of more than 1 with all questions loaded on this factor. Thus, we used four questions related to discrimination to create a composite variable of perceived discrimination with two alternative responses (never/rarely, sometimes/often). The chi-square test was used to examine the relationship between perceived discrimination and sociodemographic factors. Poisson regression with robust variance error (vce) for binary outcomes (42) (chronic pain, psychological distress, and PTSD) and multinomial logistic regression for multinomial outcomes (Self-rated health, GP/specialist visits) were used to assess the relationship between perceived discrimination and each outcome of interest in separate models before and after adjustment for potential confounders based on the previous literature, namely, age, sex, education, and income (43–45). To account for non-response and attrition biases, we calculated outcome-specific sampling weights based on participants’ characteristics from the baseline survey in Lebanon (CHART wave 1) that predicted the attrition in the H4I project (age, sex) and applied them in bivariate and multivariate analyses. Results were reported as frequency (%), mean ± standard deviation (year), prevalence ratio (PR), and odds ratio (OR), with a value of p set at 0.05. All the analyses were carried out in STATA version 17.
Out of 464 participants at the baseline of the CHART study in Lebanon, 154 (33.19%) with a median age of 41 (IQR = 33.5–46) consented and completed the interview 3–4 years after their resettlement in Norway. In the sample, 54% were female,75% were married and 62% had lower secondary or less education (Table 1). Of 154 respondents, 130 had children with a median number of 4 (IQR = 3–5).
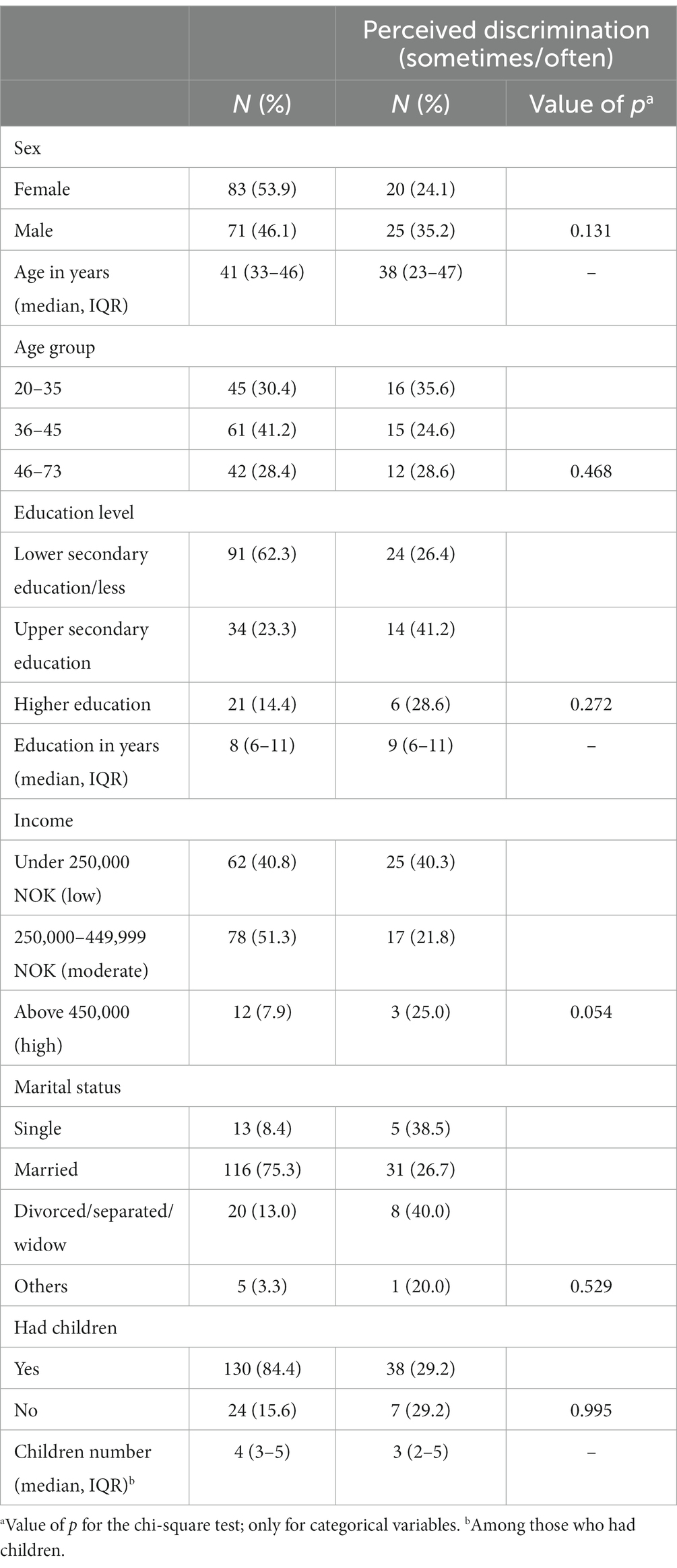
Table 1. Distribution of respondents’ sociodemographic characteristics (n = 154), by perceived discrimination.
An estimated 12.3% (7.6–18.6), 14.9% (9.7–21.6), 14.3% (9.2–20.8), 13.0% (8.1–19.3), and 29.2% (22.2–38.1) of the participants sometimes or often experienced discrimination by authorities, by colleagues at wo1rk/school, by nationality, by race, or any type of discrimination, respectively (Figure 1). Although the prevalence of the perceived discrimination appeared to be higher among males (35.2%), the youngest (35.6%), those with upper secondary education (41.2%), those with a lowest annual income (40.3%), and in the divorced/separated/widow group (40.0%); no statistically significant association was observed between these sociodemographic factors and perceived discrimination (Table 1).
Almost half of respondents reported good SRH and approximately a fifth rated their health as poor. As shown in Table 2, the weighted prevalence of the different symptoms varied from 50% for chronic pain to 5% reporting PTSD symptoms. An estimated 87.2% of participants had at least one GP visit in the past 12 months, while 28.7 and 8.6% of participants visited specialists and psychologists at least once during the same period. In both adjusted and unadjusted models, perceived discrimination was only associated with psychological distress (adjusted PR = 2.07, 95%CI: 1.21–3.55), PTSD (adjusted PR = 11.54, 95%CI: 1.25–106.16), and visiting psychologist 4 times or more (adjusted OR = 12.60, 95%CI: 1.72–92.16).
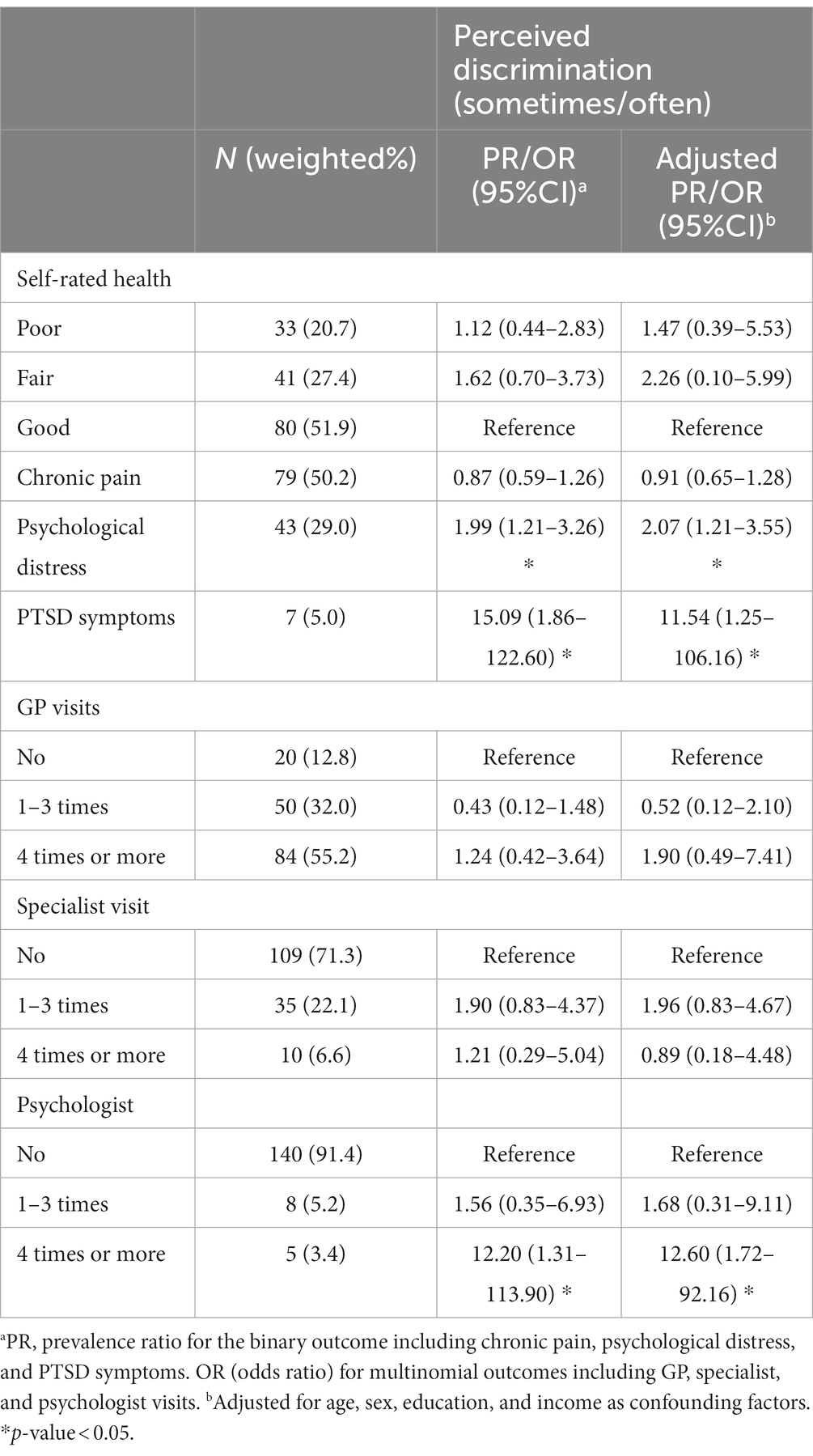
Table 2. Prevalence of physical symptoms, mental health complaints, and utilization of healthcare and their association with perceived discrimination (n = 154).
To the best of our knowledge, this is one of the first studies exploring the prevalence of perceived discrimination and its association with physical and mental well-being, and utilization of health services among Syrian refugees in Norway. The findings indicated relatively high perceived discrimination among the study population and almost 30% of respondents reported sometimes or often experienced one type of discrimination. Despite the small sample size in our study, the prevalence of perceived discrimination among Syrian refugees in this study approximates the one from a recent survey in Norway. This survey involved 4,294 migrants aged 16–66 years from 12 countries including Poland, Turkey, Bosnia-Herzegovina, Kosovo, Eritrea, Somalia, Afghanistan, Sri-Lanka, Iraq, Iran, Pakistan, and Vietnam, the reported prevalence of perceived discrimination was 27% (12). Although Syrian refugees were not represented in this survey, our finding suggested similar rate of perceived discrimination as other migrant groups in Norway. However, it was slightly lower than a German study in which the prevalence of perceived discrimination was 36% among a smaller sample of 116 Syrian refugees (46). Previous studies consistently reported a high prevalence of perceived discrimination in other migrant groups from different countries of origin and destination (45, 47–49). However, the discrepancies in reported prevalence could be due to several reasons such as the sample size, and methodological differences, and also highlight the influence of cultural and sociopolitical differences in the discriminatory experiences of various migrant groups.
In our study, the prevalence of perceived discrimination appeared to be higher among specific groups such as men, individuals who were divorced/separated/widowed, those with upper secondary education, and individuals with low annual income; however, these associations were not statistically significant. This could be due to the sample size which was not large enough to detect subtle differences or that there was considerable variability within the demographic groups examined, which could have masked significant associations. With regard to the sociodemographic background of refugees and its relation to perceived discrimination, the results from previous studies are also inconsistent (12, 46, 48). For instance, a study in Spain found higher perceived discrimination among migrant men from Ecuador, Morocco, Romania, and Colombia as compared to women (50), while another study in Canada found a higher prevalence among a sample of migrant women from Ethiopia, Korea, Iran, Vietnam, and Ireland (51). Gender-responsive data on migration has been suggested as a potential solution to promote greater equality and offer insights into the specific vulnerabilities and experiences of women and men in migration processes (52). There is also no clear consensus on whether wealth and education could influence the experiences of discrimination among migrants and refugees. For example, research in Sweden found that many asylum seekers, including those with higher education, experience discrimination in the labor market (53), while another study from the United States did not find any association between these two and perceived discrimination (54) which is in line with our findings. These discrepancies, however, could be attributed to the specific context and characteristics of the study population, sample size, differences in instruments and scales, and discrepancies in methodological approaches across studies that can influence the observed relationships between perceived discrimination and demographic factors (13).
The present study found no relationship between perceived discrimination and SRH and chronic pain. In contrast, previous research has reported significant associations between perceived discrimination and various physical symptoms such as headaches, generalized musculoskeletal pain, and low back pain (13, 55). It is important to consider the complex and multifaceted nature of physical symptoms and the potential influence of various mediators and moderators (13). Perceived discrimination may interact with other psychosocial factors, such as stress, coping mechanisms, social support, and cultural factors, which can collectively contribute to the development and expression of physical symptoms (13, 56, 57). Some cultures may view physical symptoms as a sign of weakness or a lack of willpower, while others may view them as a natural part of life (56). Similarly, the coping mechanism can mediate the effect that stress and anxiety, caused by discrimination, on associated physical symptoms (57). Therefore, the absence of a significant association in our study does not necessarily negate the potential impact of perceived discrimination on physical symptoms included in this study but highlights the need for further investigation into potential mediators and moderators including specific cultural factors and coping mechanisms that might influence the relationship between perceived discrimination and physical symptoms among Syrian refugees in Norway.
The present study revealed a significant association between perceived discrimination and adverse mental health outcomes among Syrian refugees in Norway. Previous research among diverse migrant populations also documented the detrimental effects of discrimination on mental well-being, however at different degrees (13, 45, 58). Research has shown that individuals who perceive discrimination in different domains of their lives, such as employment, education, and healthcare, often experience elevated psychological distress (13, 46). This can sabotage a person’s sense of identity, self-worth, and social support systems and lead to chronic stress, which, in turn, contributes to the development of anxiety and depressive symptoms (13), particularly salient among marginalized populations, including refugees and other immigrants, who may already face multiple stressors associated with their displacement and acculturation processes (45). However, the strength of this association could vary and depend on factors such as a sense of belonging to the host country and cultural integration of migrants (12). This study, for the first time, documented the association of experienced discrimination with poor mental health among Syrian refugees with unique cultural disparities and integration processes in the socio-political climates of Norway. Additionally, long-term discrimination exposure may increase vigilance to the point of hypervigilance, which exacerbates stress-related mental health problems (13) such as PSTD symptoms observed in this study.
Refugees have unique healthcare needs that are shaped by their experiences in their country of origin, their migration journey, their host country’s entry and integration policies, and living and working conditions (59). These experiences can increase the vulnerability of refugees to chronic and infectious diseases, making access to healthcare services critical for their well-being (60). On the other hand, perceived discrimination may discourage individuals from seeking and utilizing available health services, exacerbating their health disparities and limiting their access to necessary care (61, 62). Discrimination in healthcare and the utilization of healthcare services among refugees and migrants in Norway is a critical topic that warrants more attention (63, 64). Despite Norway’s comprehensive welfare state with health care provision for all migrants staying legally in the country and emphasis on culturally sensitive care, there are various barriers that some migrants may encounter when accessing and consuming healthcare services (64). These barriers, including discrimination, can contribute to disparities in healthcare utilization and health outcomes among different migrant groups. However, in this study, there was no significant relationship between perceived discrimination and GP and specialist visits. Although one of the limitations of this study was not asking specifically about discrimination experienced in encountering the health system, the absence of a notable association may suggest that primary care in Norway is equitable and accessible to all residents, irrespective of their migrant status.
Despite the lack of association between perceived discrimination and utilization of specialist and GP services, the significant association between perceived discrimination and increased utilization of psychologist visits in our study highlights the unique impact of discrimination on mental health service use. Discrimination experienced by refugees may contribute to psychological distress and mental health concerns, leading individuals to seek specialized mental health support, such as psychologist visits. This is in line with previous studies showing that perceived discrimination is associated with higher rates of mental health service utilization among marginalized populations (65–67). However, in contrast to our finding, a cross-sectional survey among Syrian refugees in Turkey found no significant association between perceived discrimination and mental health service use, despite the high prevalence of mental health symptoms and the gap in treatment was mainly attributed to factors beyond perceived discrimination such as structural (e.g., limited knowledge and difficulties in navigation), linguistic, and cultural obstacles (68). Nonetheless, the complex interplay between perceived discrimination and healthcare-seeking behaviors within the migrant populations in Norway underscores the need for a more thorough investigation. Addtionally, further studies with larger sample size are recommended to specify the use of mental health services and characterize the underlying obstacles, if any, among migrants in need living in Norway.
In summary, a multi-faceted approach is necessary to address discrimination as a public health concern and implement interventions to reduce its prevalence and mitigate its negative consequences among migrant and refugee populations. Efforts should focus on promoting inclusivity, cultural sensitivity, and equal opportunities for all individuals, regardless of their backgrounds (29). Systemic and structural forms of discrimination should be removed by scrutinizing and reforming policies, laws, and institutions, ensuring equal access to resources and opportunities across all sectors, including education, employment, and housing (69). Education and awareness campaigns targeting both the general population, the migrants, and healthcare providers can help foster understanding and combat discriminatory attitudes and behaviors and foster cultural competency among health staff and health literacy among migrants themselves (70).
Although this study contributes to the existing literature by providing a better understanding of the potential impact that discrimination could have on Syrian refugees’ health and their utilization of healthcare in Norway, it is important to acknowledge that the study’s findings should not be interpreted as definitive, as there may still be other sources of bias or unmeasured confounding variables that could affect the results. The cross-sectional design of the study did not allow for any causal inferences. Given the self-reported measures of discrimination, there might be social desirability bias or recall bias and may understimate or overestimate the prevalence of perceived discrimantion and distort its association with study outcomes. Furthermore, it should be noted that the small sample size in the study resulted in low statistical power, which means that the study might not have been able to detect small yet meaningful effects accurately. The high attrition rate might cause a selection bias; for example, if Syrian refugees with lower self-rated health or lower access to the health system had refused to participate in H4I. It is worth noting, however, that such challenges are not uncommon in longitudinal research (71) as the I4H project, even though cross-sectional in design, was the longitudinal follow-up of the CHART project collecting data on the same cohort of Syrian refugees after 4 years settling in Norway. Thus, there is a possibility that there are underlying effects related to perceived discrimination that were not identified due to the limited sample size. However, applying outcome-specific sampling weights in analyses could compensate for such bias to some extent and enhace the validity of our findings. Additionally, it is important to consider that certain factors, such as personality traits, skills, and coping mechanisms, were not assessed in the study. For instance, the study did not investigate how personality traits like resilience or openness might influence individuals’ perceptions of discrimination. Examining these factors could provide a more comprehensive understanding of the complex dynamics involved in perceived discrimination among the studied population. In addition, the frequency of physical symptoms was not explored in this study which may overestimate the rate of physical symptoms if the chronicity is overlooked.
Syrian refugees in Norway report high rates of discrimination, and those who have experienced discrimination are more likely to suffer from mental health symptoms and have a higher frequency of visits to psychologists. The results can contribute to increasing awareness among policy makers and practitioners and development of targeted interventions and policies aimed at improving the well-being, particulary mental health, and the appropriate integration of Syrian refugees in Norway. Future policies and interventions should aim at promoting social inclusion and reducing discrimination through the implementation of anti-discrimination policies in employment, housing, and education. Additionally, it is important to address the root causes of discrimination, such as negative attitudes towards refugees, stereotyping, and lack of knowledge about refugee issues. Public awareness campaigns and education programs could help to combat these negative attitudes and promote greater understanding and acceptance of refugees.
The datasets presented in this article are not readily available because all data and material produced in the present study are stored on the UiB SAFE server and considwred Uib Property and could only be available through a reasonable request upon the approval of the REK and UiB adminstrive entities. Requests to access the datasets should be directed to ZXNwZXJhbnphLmRpYXpAdWliLm5v.
The studies involving humans were approved by the regional committees for medical and health research ethics (REK), Oslo, Norway. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
OD: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. ED: Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Validation, Writing – review & editing, Investigation.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The I4H project was funded by the Research Council of Norway and received support from the University of Bergen.
We would like to thank Elisabeth Marie Strømme and Wegdan Hamed Nasser Hasha for their valuable efforts and contributions to the design of the questionnaire and data collection. We also appreciate the advice that we have received from Lars T. Fadnes for data analysis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
OD declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Nissen, A, Cauley, P, Saboonchi, F, Andersen, AJ, and Solberg, Ø. Mental health in adult refugees from Syria resettled in Norway between 2015 and 2017: a nationwide, questionnaire-based, cross-sectional prevalence study. Eur J Psychotraumatol. (2021) 12. doi: 10.1080/20008198.2021.1994218
2. UNHCR. Syria refugee crisis explained (2023). Available at: https://www.unrefugees.org/news/syria-refugee-crisis-explained/#:~:text=As%20of%20March%202023%2C%20the,in%20urgent%20need%20of%20shelter
3. UNHCR. Syria refugee crisis – globally, in Europe and in Cyprus (2021). Available at: https://www.unhcr.org/cy/2021/03/18/syria-refugee-crisis-globally-in-europe-and-in-cyprus-meet-some-syrian-refugees-in-cyprus/
4. Tønnessen, M, Aradhya, S, and Mussino, E. How Assad changed population growth in Sweden and Norway: Syrian refugees’ impact on Nordic national and municipal demography. PLoS One. (2021) 16:e0244670. doi: 10.1371/journal.pone.0244670
5. Statistics Norway. Refugees in Norway. Norway: Statistics Norway. (2023). Available at: https://www.ssb.no/en/befolkning/innvandrere/statistikk/personer-med-flyktningbakgrunn
6. KommuneProfilen. Antall innvandrere etter land i valgt region. (2023). Available at: https://www.kommuneprofilen.no/Profil/Befolkning/DinRegion/bef_innvandrere_land_region.aspx.
7. Fibbi, R, Midtbøen, AH, Simon, P, Fibbi, R, Midtbøen, AH, and Simon, P. Concepts of discrimination. Mig Discrim. (2021):13–20. doi: 10.1007/978-3-030-67281-2_2
8. Thorud, EImmigration and integration 2017–2018. Report for Norway to the OECD 2019. Norway: Norwegian Ministries. (2020). Available at: https://www.regjeringen.no/contentassets/6a652e6b53594e42ba9aeedacc73a68f/immigration-and-integration-2018-2019-report-for-norway.pdf
9. UNHCR. Syria emergency. (2023). Available at: https://www.unhcr.org/emergencies/syria-emergency
10. United Nations Committee on the elimination of racial discrimination examines report of Norway United Nations human office of the high rights Commissioner 2018. Available at: https://www.ohchr.org/en/press-releases/2018/12/committee-elimination-racial-discrimination-examines-report-norway
11. Brekke, J, Fladmoe, A, and Wollebæk, D. Holdninger til innvandring, integrering og mangfold i Norge. Norway: Institutt for samfunnsforskning. (2020). Available at: https://samfunnsforskning.brage.unit.no/samfunnsforskning-xmlui/handle/11250/2657621
12. Straiton, ML, Aambø, AK, and Johansen, R. Perceived discrimination, health and mental health among immigrants in Norway: the role of moderating factors. BMC Public Health. (2019) 19:325. doi: 10.1186/s12889-019-6649-9
13. Pascoe, EA, and Smart, RL. Perceived discrimination and health: a meta-analytic review. Psychol Bull. (2009) 135:531–54. doi: 10.1037/a0016059
14. Fazel, M, Wheeler, J, and Danesh, J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. (2005) 365:1309–14. doi: 10.1016/S0140-6736(05)61027-6
15. Earnshaw, VA, Rosenthal, L, Carroll-Scott, A, Santilli, A, Gilstad-Hayden, K, and Ickovics, JR. Everyday discrimination and physical health: exploring mental health processes. J Health Psychol. (2016) 21:2218–28. doi: 10.1177/1359105315572456
16. Huebner, DM, and Davis, MC. Perceived antigay discrimination and physical health outcomes. Health Psychol. (2007) 26:627–34. doi: 10.1037/0278-6133.26.5.627
17. Offidani, E, and Ruini, C. Psychobiological correlates of allostatic overload in a healthy population. Brain Behav Immun. (2012) 26:284–91. doi: 10.1016/j.bbi.2011.09.009
18. Morina, N, Kuenburg, A, Schnyder, U, Bryant, RA, Nickerson, A, and Schick, M. The association of post-traumatic and postmigration stress with pain and other somatic symptoms: an explorative analysis in traumatized refugees and asylum seekers. Pain Med. (2018) 19:50–9. doi: 10.1093/pm/pnx0005
19. Altun, A, Soh, S-E, Brown, H, and Russell, G. The association between chronic pain and pre-and-post migration experiences in resettled humanitarian refugee women residing in Australia. BMC Public Health. (2022) 22:911. doi: 10.1186/s12889-022-13226-5
20. Dragioti, E, Tsamakis, K, Larsson, B, and Gerdle, B. Predictive association between immigration status and chronic pain in the general population: results from the SwePain cohort. BMC Public Health. (2020) 20:1462. doi: 10.1186/s12889-020-09546-z
21. Altun, A, Brown, H, Sturgiss, L, and Russell, G. Evaluating chronic pain interventions in recent refugees and immigrant populations: A systematic review. Patient Educ Couns. (2022) 105:1152–69. doi: 10.1016/j.pec.2021.08.021
22. Keygnaert, I, Guieu, A, Ooms, G, Vettenburg, N, Temmerman, M, and Roelens, K. Sexual and reproductive health of migrants: does the EU care? Health Policy. (2014) 114:215–25. doi: 10.1016/j.healthpol.2013.10.007
23. Li, SS, Liddell, BJ, and Nickerson, A. The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Curr Psychiatry Rep. (2016) 18:82. doi: 10.1007/s11920-016-0723-0
24. Casagrande, SS, Gary, TL, LaVeist, TA, Gaskin, DJ, and Cooper, LA. Perceived discrimination and adherence to medical Care in a Racially Integrated Community. J Gen Intern Med. (2007) 22:389–95. doi: 10.1007/s11606-006-0057-4
25. Rivenbark, JG, and Ichou, M. Discrimination in healthcare as a barrier to care: experiences of socially disadvantaged populations in France from a nationally representative survey. BMC Public Health. (2020) 20:31. doi: 10.1186/s12889-019-8124-z
26. Murray, SB, and Skull, SA. Hurdles to health: immigrant and refugee health care in Australia. Aust Health Rev. (2005) 29:25–9. doi: 10.1071/AH050025
27. Diaz, E, Mbanya, VN, Gele, AA, and Kumar, BN. Differences in primary health care use among sub-Saharan African immigrants in Norway: a register-based study. BMC Health Serv Res. (2017) 17:509. doi: 10.1186/s12913-017-2404-z
28. Lebano, A, Hamed, S, Bradby, H, Gil-Salmerón, A, Durá-Ferrandis, E, Garcés-Ferrer, J, et al. Migrants’ and refugees’ health status and healthcare in Europe: a scoping literature review. BMC Public Health. (2020) 20:1039. doi: 10.1186/s12889-020-08749-8
29. Galanis, P, Spyros, K, Siskou, O, Konstantakopoulou, O, Angelopoulos, G, and Kaitelidou, D. Healthcare services access, use, and barriers among migrants in Europe: a systematic review. medRxiv. (2022). doi: 10.1101/2022.02.24.22271449
30. Pattillo, M, Stieglitz, S, Angoumis, K, and Gottlieb, N. Racism against racialized migrants in healthcare in Europe: a scoping review. Int J Equity Health. (2023) 22:201. doi: 10.1186/s12939-023-02014-1
31. Peek, ME, Wagner, J, Tang, H, Baker, DC, and Chin, MH. Self-reported racial/ethnic discrimination in healthcare and diabetes outcomes. Med Care. (2011) 49:618–25. doi: 10.1097/MLR.0b013e318215d925
32. Cuffee, YL, Hargraves, JL, Rosal, M, Briesacher, BA, Schoenthaler, A, Person, S, et al. Reported racial discrimination, trust in physicians, and medication adherence among inner-city African Americans with hypertension. Am J Public Health. (2013) 103:e55–62. doi: 10.2105/AJPH.2013.301554
34. Haj-Younes, J, Strømme, EM, Igland, J, Kumar, B, Abildsnes, E, Hasha, W, et al. Changes in self-rated health and quality of life among Syrian refugees migrating to Norway: a prospective longitudinal study. Int J Equity Health. (2020) 19:188. doi: 10.1186/s12939-020-01300-6
35. Strømme, EM, Haj-Younes, J, Hasha, W, Fadnes, LT, Kumar, B, Igland, J, et al. Changes in health among Syrian refugees along their migration trajectories from Lebanon to Norway: a prospective cohort study. Public Health. (2020) 186:240–5. doi: 10.1016/j.puhe.2020.07.016
36. Malm, A, Tinghög, P, Narusyte, J, and Saboonchi, F. The refugee post-migration stress scale (RPMS) - development and validation among refugees from Syria recently resettled in Sweden. Confl Heal. (2020) 14:2. doi: 10.1186/s13031-019-0246-5
38. Bridley, ALWDJ. Fundamentals of psychological disorders. 3rd ed. Washington: Washigton State University (2022).
39. Landmark, T, Romundstad, P, Dale, O, Borchgrevink, PC, and Kaasa, S. Estimating the prevalence of chronic pain: validation of recall against longitudinal reporting (the HUNT pain study). Pain. (2012) 153:1368–73. doi: 10.1016/j.pain.2012.02.004
40. Strand, BH, Dalgard, OS, Tambs, K, and Rognerud, M. Measuring the mental health status of the Norwegian population: a comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36). Nord J Psychiatry. (2003) 57:113–8. doi: 10.1080/08039480310000932
41. Mollica, RF, Caspi-Yavin, Y, Bollini, P, Truong, T, Tor, S, and Lavelle, J. The Harvard trauma questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis. (1992) 180:111–6. doi: 10.1097/00005053-199202000-00008
42. Barros, AJD, and Hirakata, VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. (2003) 3:21. doi: 10.1186/1471-2288-3-21
43. Mougenot, B, Amaya, E, Mezones-Holguin, E, Rodriguez-Morales, AJ, and Cabieses, B. Immigration, perceived discrimination and mental health: evidence from Venezuelan population living in Peru. Glob Health. (2021) 17:1–9. doi: 10.1186/s12992-020-00655-3
44. Oyarte, M, Cabieses, B, Espinoza, M, Valenzuela, MT, and Delgado, I. Perception of discrimination against immigrants compared to Chilean-born and its relationship with access to services and health outcomes. Rev Saude Publica. (2023) 56:121. doi: 10.11606/s1518-8787.2022056004125
45. Szaflarski, M, and Bauldry, S. The effects of perceived discrimination on immigrant and refugee physical and mental health. Adv Med Sociol. (2019) 19:173–204. doi: 10.1108/S1057-629020190000019009
46. Viazminsky, A, Borho, A, Morawa, E, Schmitt, GM, and Erim, Y. Perceived discrimination among Syrian refugees in Germany and its associations with mental health. Glob Public Health. (2022) 17:2854–67. doi: 10.1080/17441692.2022.2026449
47. Hadley, C, and Patil, C. Perceived discrimination among three groups of refugees resettled in the USA: associations with language, time in the USA, and continent of origin. J Immigr Minor Health. (2009) 11:505–12. doi: 10.1007/s10903-009-9227-x
48. Te Lindert, A, Korzilius, H, Van de Vijver, FJR, Kroon, S, and Arends-Tóth, J. Perceived discrimination and acculturation among Iranian refugees in the Netherlands. Int J Intercult Relat. (2008) 32:578–88. doi: 10.1016/j.ijintrel.2008.09.003
49. Jasinskaja-Lahti, I, Liebkind, K, Jaakkola, M, and Reuter, A. Perceived discrimination, social support networks, and psychological well-being among three immigrant groups. J Cross-Cult Psychol. (2006) 37:293–311. doi: 10.1177/0022022106286925
50. Agudelo-Suárez, AA, Ronda-Pérez, E, Gil-González, D, Vives-Cases, C, García, AM, Ruiz-Frutos, C, et al. The effect of perceived discrimination on the health of immigrant workers in Spain. BMC Public Health. (2011) 11:1–9. doi: 10.1186/1471-2458-11-652
51. Kim, I-H, and Noh, S. Ethnic and gender differences in the association between discrimination and depressive symptoms among five immigrant groups. J Immigr Minor Health. (2014) 16:1167–75. doi: 10.1007/s10903-013-9969-3
52. Migration Portal Data. Gender and migration. (2023). Available at: https://www.migrationdataportal.org/themes/gender-and-migration.
53. Reumert, AS. Refugees and migrants arrive in the same boat, but are treated differently. The century foundation. (2016). Available at: https://tcf.org/content/commentary/refugees-migrants-arrive-boat-treated-differently/.
54. Inocencio-Gray, J, and Stone, DL. The relations between race, differences in cultural values, and experienced discrimination of immigrants in the US. (2013). Working Papers 0224mgt, University of Texas at San Antonio: College of Business. Available at: https://ideas.repec.org/p/tsa/wpaper/0224mgt.html
55. Edwards, RR. The association of perceived discrimination with low back pain. J Behav Med. (2008) 31:379–89. doi: 10.1007/s10865-008-9160-9
56. Yu, NX, Ni, MY, and Stewart, SM. A moderated mediation analysis on the association between perceived discrimination and physical symptoms among immigrant women from mainland China into Hong Kong: evidence from the FAMILY cohort. J Immigr Minor Health. (2021) 23:597–605. doi: 10.1007/s10903-020-01042-1
57. Cénat, JM, Kouamou, LN, Farahi, SMMM, Darius, WP, Dalexis, RD, Charles, M, et al. Perceived racial discrimination, psychosomatic symptoms, and resilience among black individuals in Canada: A moderated mediation model. J Psychosom Res. (2022) 163:111053. doi: 10.1016/j.jpsychores.2022.111053
58. Montgomery, E, and Foldspang, A. Discrimination, mental problems and social adaptation in young refugees. Eur J Pub Health. (2007) 18:156–61. doi: 10.1093/eurpub/ckm073
59. WHO. World report on the health of refugees and migrants. World health Organization; (2022). Available at: https://www.who.int/publications/i/item/9789240054462
60. UNHCR. Access to healthcare. (2022). Available at: https://www.unhcr.org/what-we-do/protect-human-rights/public-health/access-healthcare
61. Gil-Salmerón, A, Katsas, K, Riza, E, Karnaki, P, and Linos, A. Access to healthcare for migrant patients in Europe: healthcare discrimination and translation services. Int J Environ Res Public Health. (2021) 18:7901. doi: 10.3390/ijerph18157901
62. Dang, R. Perceived discrimination when using health-care services, health outcomes, and health-care utilisation among Romani people in Europe: evidence from the second European Union minorities and discrimination survey. Lancet Glob Health. (2022) 10:S11. doi: 10.1016/S2214-109X(22)00140-1
63. Laue, J, and Risør, T. Refugees and healthcare services. Tidsskr Nor Laegeforen. (2018) 137. doi: 10.4045/tidsskr.17.0628
64. Debesay, J, Arora, S, and Bergland, A. 4. Migrants’ consumption of healthcare Services in Norway: Inclusionary and exclusionary structures and practices. Inclusive consumption. Norway: Books: Universitetsforlaget. p. 63–78.
65. Pager, D, and Shepherd, H. The sociology of discrimination: racial discrimination in employment, housing, credit, and consumer markets. Annu Rev Sociol. (2008) 34:181–209. doi: 10.1146/annurev.soc.33.040406.131740
66. Skosireva, A, O’Campo, P, Zerger, S, Chambers, C, Gapka, S, and Stergiopoulos, V. Different faces of discrimination: perceived discrimination among homeless adults with mental illness in healthcare settings. BMC Health Serv Res. (2014) 14:376. doi: 10.1186/1472-6963-14-376
67. Burgess, DJ, Ding, Y, Hargreaves, M, Van Ryn, M, and Phelan, S. The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. J Health Care Poor Underserved. (2008) 19:894–911. doi: 10.1353/hpu.0.0063
68. Fuhr, D, Acarturk, C, McGrath, M, Ilkkursun, Z, Sondorp, E, Sijbrandij, M, et al. Treatment gap and mental health service use among Syrian refugees in Sultanbeyli, Istanbul: a cross-sectional survey. Epidemiol Psychiatr Sci. (2020) 29:e70. doi: 10.1017/S2045796019000660
69. Bailliet, CM. Protection of refugees, returnees, migrants, and internally displaced persons against racism, xenophobia, and discriminatory practices. Returnees, migrants, and internally displaced persons against racism, xenophobia, and discriminatory practices (2018).
70. Burgess, D, van Ryn, M, Dovidio, J, and Saha, S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. (2007) 22:882–7. doi: 10.1007/s11606-007-0160-1
Keywords: Syrian refugees, perceived discrimination, self-rated health, pain symptoms, mental health, healthcare utilization
Citation: Dadras O and Diaz E (2024) Perceived discrimination and its association with self-rated health, chronic pain, mental health, and utilization of health services among Syrian refugees in Norway: a cross-sectional study. Front. Public Health. 12:1264230. doi: 10.3389/fpubh.2024.1264230
Received: 20 July 2023; Accepted: 22 January 2024;
Published: 09 February 2024.
Edited by:
Cyrille Delpierre, INSERM Public Health, FranceReviewed by:
Sousan Hamwi, New University of Lisbon, PortugalCopyright © 2024 Dadras and Diaz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Omid Dadras, b21pZC5kYWRyYXNAdWliLm5v
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.