- 1National Resource Center for Refugees, Immigrants, and Migrants, University of Minnesota, Minneapolis, MN, United States
- 2Refugee Women’s Network, Decatur, GA, United States
- 3School of Nursing, University of Minnesota, Minneapolis, MN, United States
- 4Centers for Disease Control and Prevention, Division of Global Migration and Quarantine, Immigrant, Refugee and Migrant Health Branch, Atlanta, GA, United States
- 5Department of Pediatrics, University of Washington, Seattle, WA, United States
This case study describes the design, implementation, and evaluation of an initiative to increase COVID-19 vaccine confidence and uptake among refugee and immigrant women in Clarkston, Georgia. Applying the principles and practices of human-centered design, Mothers x Mothers was co-created by Refugee Women’s Network and IDEO.org as a series of gatherings for refugee and immigrant mothers to discuss health issues, beginning with the COVID-19 vaccine. The gatherings included both vaccinated and unvaccinated mothers and used a peer support model, with facilitation focused on creating a trusting environment and supporting mothers to make their own health decisions. The facilitators for Mothers x Mothers gatherings were community health workers (CHWs) recruited and trained by Refugee Women’s Network. Notably, these CHWs were active in every phase of the initiative, from design to implementation to evaluation, and the CHWs’ professional development was specifically included among the initiative’s goals. These elements and others contributed to an effective public health intervention for community members who, for a variety of reasons, did not get sufficient or appropriate COVID-19 vaccine information through other channels. Over the course of 8 Mothers x Mothers gatherings with 7 distinct linguistic/ethnic groups, 75% of the unvaccinated participants decided to get the COVID-19 vaccine and secured a vaccine referral.
1 Introduction
Community health workers (CHW) facilitate connections between health systems and communities, providing vital outreach and education to underserved populations (1, 2). CHW programs, once primarily associated with low-resource settings in the Global South, have more recently attracted interest in higher-resource settings, where health disparities persist despite well-funded and well-developed health systems (3, 4). The COVID-19 pandemic accentuated these disparities globally and highlighted the importance of community-level health work, not only for the pandemic response but also for routine healthcare delivery (5, 6).
In the United States, CHWs’ roles and work settings are varied, but studies have shown that they create unprecedented levels of engagement in traditionally underserved communities (1, 4, 7). CHWs in the United States have facilitated innovative approaches to the primary, secondary, and tertiary prevention and management of common chronic diseases like diabetes, cardiovascular disease, HIV, and some cancers (4). During the COVID-19 pandemic, CHWs’ work in the United States included public health communication and education, health system navigation, occasional contact tracing and monitoring, and attending to the larger social, economic, and behavioral health needs of underserved communities (1, 7).
The CHW model of care figures prominently in a landmark 2020 paper by Holeman and Kane about the promise of human-centered design for global health equity (8). Human-centered design is an approach to systems-level problem-solving that prioritizes intended users’ perspectives and needs throughout an iterative design process (9). Holeman and Kane draw a parallel between the designer’s obligation to communities and the CHW’s responsibility to patients—“not only to deliver efficient biomedical services, but to accompany patients, to ease suffering and to offer their caring presence as an antidote to despair” (8). By imagining health-equity-oriented design as “accompanying a community,” Holeman and Kane emphasize the need to cultivate relationships with community members, understand their experiences and perspectives, and build interventions with them (8).
2 Background and rationale
CHWs have historically served as community health liaisons, but there was an additional need during the COVID-19 pandemic for CHWs to provide critical services to refugee and immigrant communities, like providing support for case investigation and contact tracing (CICT), facilitating access to vaccines, and conducting education and outreach (7, 10, 11). With regard to CICT and vaccine access, refugee and immigrant communities faced overlapping challenges due to different cultural practices around health and healthcare, difficulties accessing health information and services, community concerns about vaccines and, sometimes, distrust of government or health systems (12, 13). As for education and outreach, the COVID-19 pandemic challenged public health departments across the United States to develop clear messaging for diverse populations. Unfortunately, refugees and immigrants who navigate their social environments and media in languages other than English often missed out on crucial COVID-19 information due to messaging that was: (1) not adequately or completely translated, (2) not culturally or situationally concordant, or (3) not delivered through effective or accessible communication channels (14, 15).
Community-based organizations and CHWs, often working together, addressed some of these gaps and therefore served as crucial partners to public health departments in their efforts to connect refugees and immigrants to COVID-19 information and vaccines (7, 16). Community-based organizations adapted the COVID-19 public health response for local refugee and immigrant communities by providing culturally responsive education, services, and advocacy in ways that emphasized community strengths over mere compliance (11). Meanwhile, CHWs extended the reach of public health and health systems—as well as social service agencies—through culturally responsive communication and robust relationships built on trust, support, and advocacy (1, 17).
3 Context
Refugee Women’s Network (RWN) is a 501c3 non-profit in Northeastern Atlanta, Georgia, led by refugee and immigrant women since its founding 25 years ago. RWN serves refugee and immigrant families who have resettled in the state of Georgia, with a mission “to support women survivors of war, conflict, and displacement in overcoming cultural and systemic barriers to achieving healthy, self-sufficient, and fulfilling lives” (18). RWN’s work is largely based in Clarkston, a small city adjacent to the Atlanta metropolitan area that receives many of Georgia’s resettled refugees.
Of Clarkston’s 14,538 residents, 52.5% are foreign-born and 61.9% of those aged 5 or older speak a language other than English at home (19)–much higher than the corresponding national figures of 13.6 and 21.6%, respectively (20). These populations face challenges to getting relevant health information and services in their own languages from sources they trust (21).
In 2019 and 2020, Georgia State University Prevention Research Center conducted two multilingual surveys among Clarkston residents 18 and older who self-identified as refugees or asylees. Of those surveyed, 57% self-reported “marginal reading, writing and speaking skills in English” (21), significantly more than the 8.3% of U.S. residents who say they speak English less than “very well” (20). Some 31% of Clarkston survey respondents were living in high-density households (≥6 people) (21), while the average U.S. household has 2.54 people (20). Finally, among survey respondents, 66% reported high levels of daily stress, 82% had high levels of financial insecurity, and 70% “did not know where to get benefits like unemployment or financial assistance” (21) (Table 1).
4 Mothers x mothers: key programmatic elements
In November 2021, RWN launched an innovative community health initiative called Mothers x Mothers. This initiative was made possible by a grant from the National Association of City and County Health Officials (NACCHO), which funded local health departments and community-based organizations around the United States to promote COVID-19 mitigation and management strategies in refugee and immigrant communities (22). The Mothers x Mothers initiative was also supported by the National Resource Center for Refugees, Immigrants, and Migrants (NRC-RIM) (23).
The Mothers x Mothers initiative had three goals: (1) to increase vaccine confidence among refugee and immigrant mothers, (2) to empower these same mothers to make informed decisions about their own health more generally, and (3) to gain enough community trust to sustain future interventions. Mothers x Mothers was jointly designed by RWN and IDEO.org, an international 501c3 nonprofit specializing in human-centered design for health equity, community engagement, and humanitarian aid.
4.1 Community health gatherings
Mothers x Mothers was a series of gatherings designed for participants with shared identities, experiences, and interests. The gatherings used a peer support model and were structured around a template that included icebreaker questions, safe space agreements, and a Google Slides deck about selected health topics, starting with COVID-19 and the COVID-19 vaccine. Peer support has been used as an intervention model to address issues ranging from mental health (24) to perinatal maternal health (25) to breastfeeding (26) to vaccine hesitancy and misinformation (27). Peer support appears to be most effective when organizations co-design culturally concordant programs with communities rather than imposing ideas top-down (28).
Each group that gathered for Mothers x Mothers at RWN consisted of refugee and immigrant mothers who were living in Clarkston and shared a language or region of origin. There were seven groups in all: one each for Burmese-, Arabic-, Sango-, French-, Swahili-, Somali-, and Amharic- and Tigrinya-speaking mothers (the last two being combined into a single group). Each gathering was facilitated by a Community Health Promoter (RWN’s job title for a CHW). The first 1–2 gatherings for each group focused on the COVID-19 vaccine, and the slides for these meetings presented facts to counter misinformation about COVID-19 and the vaccine common to each community. Through deliberate recruitment, some of the participants in these gatherings were unvaccinated while others had already received the COVID-19 vaccine. As one Community Health Promoter explained,
“You’re more likely to believe someone who is in a similar life situation as you, and if a unvaccinated mother hears from a vaccinated mother who’s the exact same as her, has kids in the same age range, speaks the same language, they’re more likely to change their mind.”
After the first 1–2 gatherings focused on COVID-19, the Community Health Promoters asked group members to choose the future direction of the gatherings. The manager of the program stated:
“[We] honor them, saying, ‘Okay, we pushed COVID the first two meetings, but now it’s yours,’ like we want this to be a sustainable model so that these women are looking forward to coming back every month, and we want them to drive it.”
Examples of topics chosen by participants were nutrition and diet, high blood pressure, diabetes, and oral hygiene.
4.2 Human-centered design involving community representatives
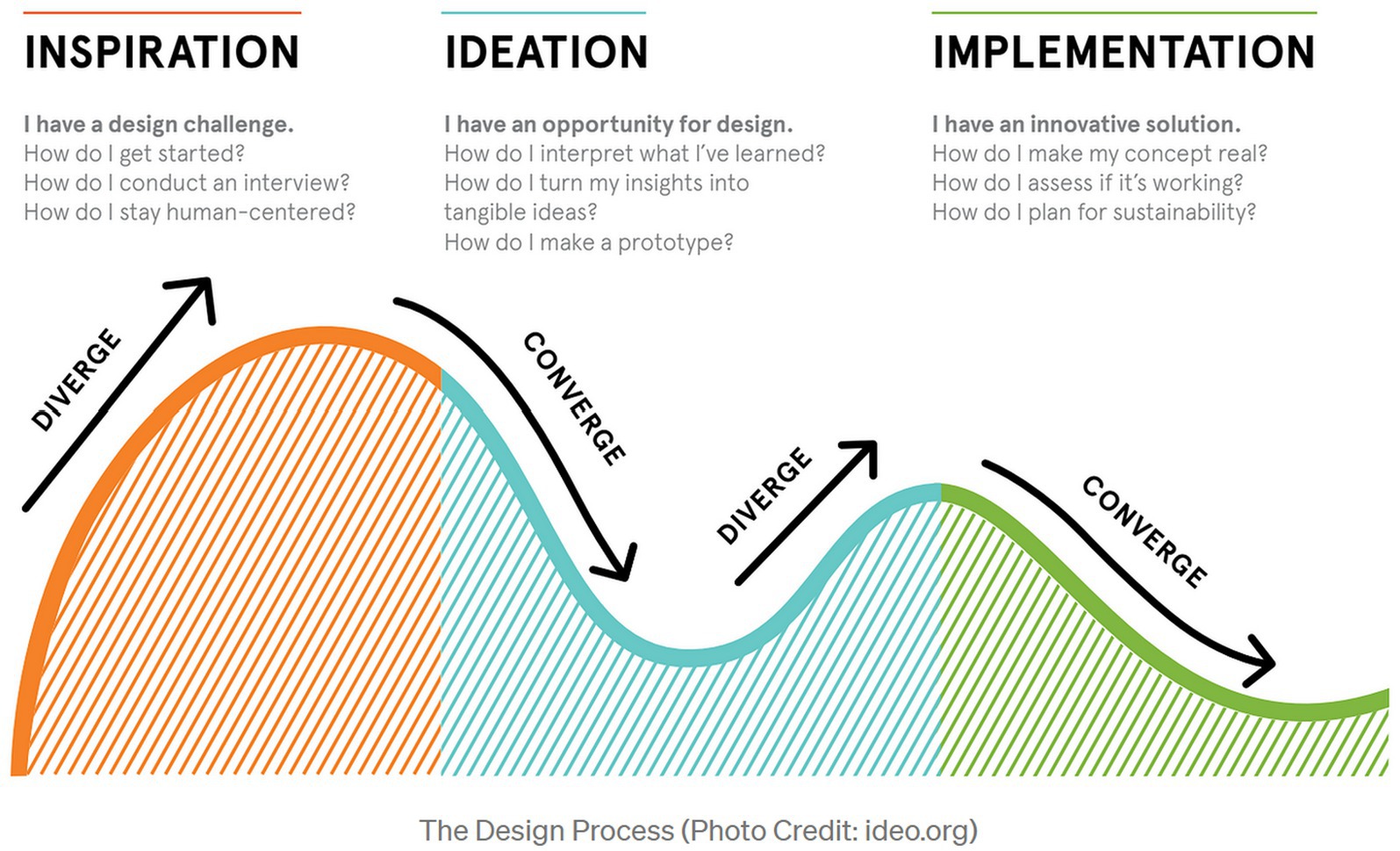
A particularly innovative aspect of Mothers x Mothers was the design process that paired IDEO.org designers with a group of women co-designers from the Somali, Eritrean, and Ethiopian communities, including RWN Community Health Promoters. Using a human-centered design process (Figure 1)—i.e., one that actively involved the intended users throughout the iterative design process—the diverse team worked to understand the specific challenges facing refugee and immigrant women during the COVID-19 pandemic (inspiration), creatively explored a range of possible culturally-concordant solutions (ideation), and developed prototypes to test the viability of specific interventions (implementation).
Early in this process, IDEO.org and RWN considered a wide range of ideas to address vaccine hesitancy, from relatively modest proposals (e.g., peer-to-peer conversations) to technologically sophisticated ones (e.g., automated messaging via WhatsApp). When IDEO.org designers found the idea of peer support gaining traction, they proceeded with the broad idea of gatherings of mothers using a peer support model. Why peer support? Co-designers from the community had noted that vaccination was not common in their countries of origin, making the support of like-minded peers crucial for mothers considering the COVID-19 vaccine (29). Additionally, during the inspiration phase, co-designers had shared anecdotes that demonstrated the impact of social endorsements–negative as well as positive–regarding the vaccine.
At this point, more options were weighed and discussed: in-person vs. virtual gatherings; gatherings primarily focused on COVID-19 vs. gatherings coupling COVID-19 with a low-stakes theme like food; gatherings pairing mothers with Community Health Promoters, religious leaders, friends, or their own children. Design team members were most enthusiastic about in-person gatherings for mothers, facilitated by a Community Health Promoter. One of the aims of these gatherings would be to create space for mothers to hear positive social endorsements of the COVID-19 vaccine.
The next step in the design process was to start holding in-person prototype gatherings, carefully observing and assessing how the sessions went, and making needed refinements to the concept and organization of gatherings. Two prototype gatherings were held, one with Somali mothers and another with Eritrean and Ethiopian mothers. In this phase, all 13 participating mothers were unvaccinated, and 4 decided to get the vaccine as a result of the prototype gatherings.
Later, as recruitment for pilot gatherings and regular Mothers x Mothers gatherings ramped up, RWN began to include vaccinated mothers alongside unvaccinated ones. At first, this was an accident of the recruitment process: RWN did not ask participants for their vaccination status before gatherings so that they would not feel singled out or discouraged from joining just because they did not hold a specific view about vaccination. However, the mix turned out to be fortuitous: in a mixed gathering, unvaccinated mothers could learn from vaccinated mothers about their views and experiences, while vaccinated mothers had an opportunity to share their experiences and also raise concerns about vaccinating their children. Realizing the potential for greater impact, RWN made a special effort to recruit both vaccinated and unvaccinated mothers from that point forward.
4.3 Roles
4.3.1 Community health promoters
Much of CHWs’ work falls under the rubric of health promotion, that is, encouraging health awareness and specific health practices through education and counseling (2). Starting in late 2019, RWN began recruiting and hiring CHWs, called Community Health Promoters, from the refugee and immigrant communities the organization serves. Twenty of these Community Health Promoters have been recruited, hired, and trained since then. Collectively, they speak 18 languages: Amharic, Arabic, Bengali, Burmese, Chin (Hakha), Dari, English, French, Hindi, Kurdish, Lingala, Pashto, Rohingya, Somali, Sango, Spanish, Swahili, and Tigrinya.
Each Community Health Promoter received 15+ hours of required standard training, in addition to ongoing monthly opportunities for further optional training on emerging topics of interest. The required training included modules on health communication, motivational interviewing, COVID-19 and COVID-19 vaccines, vaccine education, health insurance basics, and healthcare navigation for new refugees, in addition to basics about chronic disease, nutrition, and women’s health. The Community Health Promoters were trained to facilitate group conversations, refer community members to health services, help community members navigate vaccine clinics, and more.
In the design of Mothers x Mothers, the Community Health Promoters facilitated gatherings, created a trusting environment, and supported mothers to make health decisions that were in their own best interests. They were not expected to act as experts on COVID-19 or the COVID-19 vaccine; however, they knew where to refer mothers for COVID-19 information. The Community Health Promoters also worked to increase access to services by providing information about testing and vaccination locations, as well as guidelines for staying safe and keeping others safe. As one Community Health Promoter pointed out, the key to doing this work effectively was
“a lot of communication training, like how do you talk to people without bias, being neutral and third person… ways to back off in an argument that might be happening… because people do get angry and people will argue with you about COVID, so when is the right time to back off? When is the right time to respect someone’s boundary and just let the situation go?”
Thus it was especially important for the Community Health Promoters to build and refine group communication skills.
4.3.2 Mothers
The Mothers x Mothers initiative specifically focused on mothers, who RWN recognizes as “health broker[s] of the family and community” (18). In an early phase of design, IDEO.org had worked toward ways to increase vaccine uptake among refugee and immigrant adolescents, but found that “designing with and for their mothers was crucial as they are the advocates—and gatekeepers—of their children’s health” (29). This realization aligns with research showing that in the United States, it is mothers who make about 80% of healthcare decisions for their children (30). Moreover, while there are many cultural and situational factors in play, in many cases it is mothers, not fathers, whose level of vaccine confidence predicts whether children will be vaccinated (31, 32). In the United States, mothers have generally been more hesitant than fathers to accept the COVID-19 vaccine for their children (33, 34), making it vitally important to reach mothers and address their concerns.
4.3.3 Content experts
Content experts participated in the Mothers x Mothers program by contributing ideas for slides and sometimes sharing information in person, but their role was intentionally limited to give priority to peer support. As the manager of the program explained, “we try to make everyone feel on the same level, so a Health Promoter is there, but the Health Promoter, by nature, is on the same level.” At one point, one of the groups asked for a doctor to be present at their next gathering. RWN acknowledged the request and arranged for a culturally and linguistically concordant doctor to be present, but structured the meeting so that there was no expectation that the doctor would give a lecture or be positioned “above” the group of mothers in some other way.
Reflecting on how well peer support had worked to shift vaccine confidence in Mothers x Mothers groups, the program manager said,
“It wasn't because it was a… doctor, it was because there was a bunch of women from those communities that related to each other, and we created a safe atmosphere where they could share their concerns and they could have dialogue… especially because that social network was so damaged during COVID.”
4.4 Logistical coordination
RWN identified ways to expand opportunities for engagement, not only for mothers to get COVID-19 tests and vaccines, but also for them to participate in the kind of open peer-to-peer conversation about COVID-19 vaccines that Mothers x Mothers provided. They offered three kinds of help to Mothers x Mothers participants:
1. Transportation in the form of rides provided by volunteers, organized carpooling, or reimbursement for mileage;
2. Childcare provided on-site during gatherings so the mothers could take a break from caregiving, deeply engage in the activity, and connect with other women from their community; and,
3. Other incentives, such as gift cards, diapers, hygiene products, or food boxes, to compensate for the time and effort it took to come to the gatherings.
RWN’s Community Health Promoters recruited participants for Mothers x Mothers by distributing flyers and talking face-to-face with potential attendees. The Community Health Promoters emphasized that the gatherings would be welcoming, non-judgmental spaces, and mentioned the help and incentives described above.
5 Evaluation: process and outcomes
RWN’s leadership and Community Health Promoters placed equal emphasis on process and outcome evaluation. All case study interviewees spoke of wanting an initiative that prioritized trust, sustainability, and participant-led programming, with an accompanying benefit of increasing vaccine uptake. They conceptualized and operationalized Mothers x Mothers through three process-oriented goals: (1) building vaccine confidence, (2) building trust, and (3) building capacity.
5.1 Building vaccine confidence
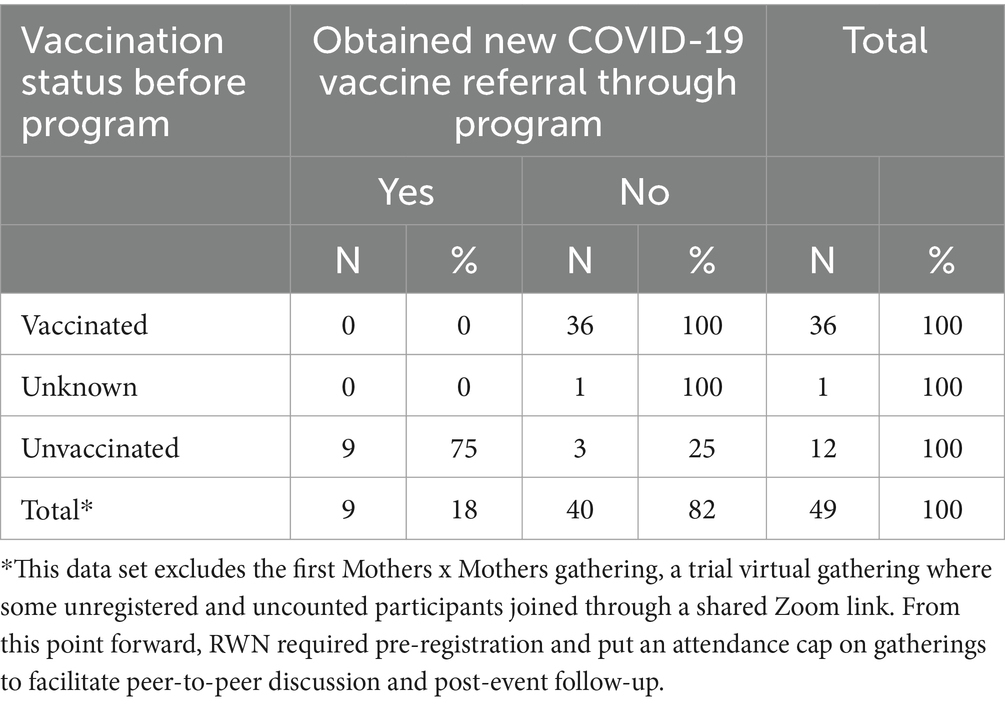
RWN built vaccine confidence by promoting honest, informed discussion about COVID-19 so that community members could consider vaccination and get vaccinated, especially in more vaccine-hesitant communities. Table 2 shows the shift in vaccination status among Mothers x Mothers participants. Over the course of 8 Mothers x Mothers gatherings with 7 distinct groups, there were 49 participants (36 vaccinated, 1 unknown, 12 unvaccinated). Of the 12 unvaccinated participants who were eligible to get a COVID-19 vaccine, 9 (75%) decided to get the vaccine and secured a vaccine referral through Mothers x Mothers. Most gatherings had 5–7 participants, and no single gathering yielded more than 2 new vaccine referrals.
5.2 Building trust
RWN prioritized building and maintaining community trust. Community Health Promoters therefore took a respectful, linguistically and culturally responsive approach to conversations about the COVID-19 vaccine. RWN’s long-term goal with Mothers x Mothers was to gain trust so that community members would come back to RWN in the future for COVID-19 boosters, flu shots, pediatric vaccines, and other health resources. As one Community Health Promoter explained, “Once you gain [the mothers’] trust, it’s easier for them to bring their family on board, it’s easier for them to bring their friends on board, their other relatives… it spreads like wildfire.” The topic of trust came up several times in every interview conducted for this case study.
At the conclusion of each gathering, RWN collected feedback from Mothers x Mothers participants, either in person or via a phone call; Community Health Promoters helped by interpreting. RWN decided to ask relatively few questions at first, recognizing that questioning itself can become a barrier to participation. RWN’s original questions were:
1. Did your mind get changed about the vaccine?
2. Did you learn anything new about the vaccine?
3. In the future, would you bring friends? / Do you feel comfortable enough to bring friends?
4. What do you specifically want to learn about at the next event?
As RWN got more feedback from mothers and built more rapport, the questions were adjusted and broadened, thereby gathering needed information while maintaining an emphasis on participants’ levels of comfort and trust. Later questions included:
1. Were you able to speak honestly and ask questions you had during the Mothers x Mothers gathering? Did anything make you uncomfortable or nervous to share?
2. Are you COVID-19 vaccinated, including the booster?
3. Are you/your children HPV vaccinated?
4. Do you need a Health Promoter to set you or your child up with an appointment for the COVID-19 booster, flu shot, or HPV vaccine?
5. What health-related topic would you like to learn about next?
RWN evaluated how effectively it built trust by weighing (1) feedback collected from mothers after gatherings and (2) Community Health Promoters’ observations of how the groups interacted during gatherings. Reflecting on Mothers x Mothers as a whole, one Community Health Promoter said:
“Everyone who attends has said how much they enjoy their time coming to the mothers’ program, how well it has been run and how comfortable they feel sharing their thoughts in a judgment-free space.”
Another reflected on a series of gatherings as follows:
“I feel like it's honestly working, because I have people who aren't vaccinated still show up to every event, every time, never miss an event, and I'm like, ‘Okay, you're here for a reason’… so I'm going to keep doing what I'm doing.”
Finally, a Community Health Promoter observed after a typical gathering: “We had such a positive reception [when] we held it… we successfully held a safe space and we gave them information that they trusted.” Comments like these speak to RWN’s emphasis on trust as an integral ingredient of Mothers x Mothers.
5.3 Building capacity
RWN encouraged the Community Health Promoters to develop as community leaders so that, whether or not they continued with RWN, they could attain a level of confidence, connection, and empowerment that would allow them to play key roles around health in their communities. To evaluate the professional development of the Community Health Promoters, RWN conducted pre- and post-practice quality improvement assessments. These assessments gauged levels of self-confidence, ability to speak about the vaccine, and capacity to connect with community members and community leaders. Overall, RWN found that the Community Health Promoters approached their training and work with great care and dedication and developed accordingly. One Community Health Promoter spoke positively of her own growth, saying:
“When I started to do it, I was very scared… but when I came here they said, ‘No problem, you can learn.’ For me it was a good opportunity, health promotion…. I feel good because I’m doing something good for my community.”
Another said,
“I plan on going to medical school next year but I'm just like, I don't want to leave this program. This program has made such an impact. And it reminds me of programs we had back in the day in Clarkston that actually sponsored my family and brought them here.”
6 Discussion
6.1 Elevating community health promoters
RWN’s Community Health Promoters were involved in the Mothers x Mothers initiative in several notable ways. First, the Community Health Promoters were recruited and trained by RWN, a local community-based organization. Their training covered topics that might be relevant to CHWs anywhere, but with a special emphasis on serving refugee and immigrant women from local communities. Second, Community Health Promoters were involved in every phase of the initiative, from design to implementation to evaluation. This not only led to an initiative that was well suited for Clarkston refugees and immigrants, it also increased the engagement and interest of the Community Health Promoters–which in turn increased the engagement and interest of participating mothers. Third, the Community Health Promoters’ professional development was specifically included among the initiative’s goals. As part of its mission to empower refugee and immigrant women, RWN deliberately hired and trained women from local refugee and immigrant communities, and supported their growth.
6.2 Applying human-centered design principles
RWN, in close collaboration with IDEO.org, applied core aspects of human-centered design to plan an intervention for building vaccine awareness, confidence, and uptake among local refugee and immigrant mothers. The Mothers x Mothers initiative included strategies to provide information aligned with community values, engagement of peers as trusted messengers, and a commitment to affirm participants’ choices. The key elements of the human-centered design process were facilitated listening, ideation (i.e., creatively imagining solutions), prototyping (i.e., experimenting with proposed solutions), and implementation of the initiative (see Figure 1). RWN’s work serves as a foundational case study for increasing the evidence base around human-centered design as a critical tool in planning public health interventions, and the Mothers x Mothers toolkit has now been piloted across a handful of select sites. For other organizations considering implementing Mothers x Mothers, the toolkit is free to use and customizable (23).
6.3 Investing in peer support as an intervention model
When designing and implementing Mothers x Mothers, RWN and IDEO.org made a special effort to acknowledge and support the agency and experience of participants, allowing enough time for relationships between RWN and community members to develop and flourish. This approach aligns with Harris et al.’s and Schleiff et al.’s reviews of community-based peer support programs, which suggest that these programs are most effective when organizations share governance, respect cultural perspectives, and devote sufficient time and effort to assessing community needs and developing relationships (28, 35). Similarly, RWN and IDEO.org’s choice to focus on mothers as part of a campaign to address COVID-19 vaccine hesitancy squares with Schleiff et al.’s observation that “participatory women’s groups have been particularly successful in changing complex sets of behaviors that are embedded in cultural belief systems” (35).
Though Mothers x Mothers was admittedly a small-scale intervention for a specific demographic segment, it is worth briefly considering its possible ripple effects. When we take into account the role of these mothers in health decisions for their households and recall the high proportion of high-density households in Clarkston, we realize the possible exponential impact of the mothers’ improved vaccine confidence on vaccine uptake in their homes and communities.
7 Methodological constraints and strengths
This intervention and community case study have constraints and strengths worth noting. First, the design and implementation of Mothers x Mothers were tailored specifically to refugee and immigrant communities, which affects transferability and generalizability. Rather than viewing this as a limitation, however, we prefer to highlight that this intervention met the needs of local women from traditionally underserved populations. Second, recruitment for Mothers x Mothers involved self-selection and therefore our evaluation may reflect positive deviance. Third, our case study considered in detail the perspectives of Mothers x Mothers designers and group facilitators, without an equally in-depth look at the first-hand perspectives of participants. This limits our ability to draw definitive conclusions about why participants went to gatherings and how they changed their minds about the COVID-19 vaccine. Nevertheless, we were able to provide a rich description of Mothers x Mothers’ program design and its key elements, which we hope will allow other community organizations to attempt similar approaches to planning and intervention.
8 Conclusion
In this case study we examine and describe features of the design, implementation, and evaluation of Mothers x Mothers that resulted in an increase in COVID-19 vaccine confidence and uptake among refugee and immigrant women in Clarkston, Georgia. When RWN launched the Mothers x Mothers initiative in late 2021, the participating mothers had been eligible for COVID-19 vaccination since March 2021 in the state of Georgia, yet many had not been vaccinated (36). Gatherings leveraged the influence and support of community peers, including CHWs, to shift attitudes and prompt action among unvaccinated participants—even in a climate of COVID misinformation and information fatigue.
Our goal in presenting this community case study is both to provide programmatic guidance and recommendations for other community organizations considering similar initiatives, and to increase the evidence base supporting small-scale community-led public health interventions. The Mothers x Mothers initiative succeeded in increasing vaccine acceptance, but the program was successful in two other respects that other organizations might seek to emulate as well. First, it empowered participating mothers to make informed health decisions. Mothers—described by RWN and IDEO.org as the “brokers,” “advocates,” and “gatekeepers” of their children’s and family’s health—play a significant role in community health decisions and behavior, so public health interventions that focus on mothers often have a broader impact. Second, the program built enough community trust to make future interventions possible, as evidenced by the continuing Mothers x Mothers gatherings that focus on health topics beyond COVID-19. Organizations designing similar programs might also seek to balance “success” here and now with the kind of long-term relationship-building that makes “success” more likely in the future.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
DA led the writing and analyses. TM and FA co-coordinated the interventions and assisted with the writing. SH, MK, and EM assisted with the writing and conceptualization of the study. ED-H was team lead and assisted with the writing. All authors contributed to the article and approved the submitted version.
Funding
This case study was performed under the National Resource Center for Refugees, Immigrants, and Migrants (NRC-RIM) which is funded by the US Centers for Disease Control and Prevention (CDC) and the International Organization for Migration (IOM; award number CK000495-03-00 / ES1874). Refugee Women’s Network’s Mothers x Mothers initiative work was made possible by a grant from the National Association of City and County Health Officials (NACCHO), which is also funded by the CDC (award number NU38OT000306).
Acknowledgments
We wish to thank Ridhi Arun and Claudia Sosa Lazo of IDEO.org for their review of this case study, and we express our gratitude to the IDEO.org teams who were involved in the design of Mothers x Mothers. The Design Team included Hitesh Singhal, Claudia Sosa Lazo, and Juan Pablo Patino. The Program Team included Ridhi Arun, Michelle Kreger, Cady Shadwick, Mary Katica, and Courtney Chang.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
1. Rodriguez, NM . Community health workers in the united states: time to expand a critical workforce. Am J Public Health. (2022) 112:697–9. doi: 10.2105/AJPH.2022.306775
2. Glenton, C, Javadi, D, and Perry, HB. Community health workers at the dawn of a new era: 5. Roles and tasks. Health Res Policy Syst. (2021) 19:748. doi: 10.1186/s12961-021-00748-4
3. Javanparast, S, Windle, A, Freeman, T, and Baum, F. Community health worker programs to improve healthcare access and equity: are they only relevant to low- and middle-income countries? Int J Health Policy Manag. (2018) 7:943–54. doi: 10.15171/ijhpm.2018.53
4. Perry, HB, Zulliger, R, and Rogers, MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annu Rev Public Health. (2014) 35:399–421. doi: 10.1146/annurev-publhealth-032013-182354
5. Hodgins, S, Kok, M, Musoke, D, Lewin, S, Crigler, L, LeBan, K, et al. Community health workers at the dawn of a new era: 1. Introduction: tensions confronting large-scale CHW programmes. Health Res Policy Syst. (2021) 19:752. doi: 10.1186/s12961-021-00752-8
6. Valeriani, G, Sarajlic Vukovic, I, Bersani, FS, Sadeghzadeh Diman, A, Ghorbani, A, and Mollica, R. Tackling ethnic health disparities through community health worker programs: a scoping review on their utilization during the COVID-19 outbreak. Popul Health Manag. (2022) 25:517–26. doi: 10.1089/pop.2021.0364
7. Community Health Workers . National Resource Center for Refugees, Immigrants, and Migrants (NRC-RIM). (2022). Available at: https://nrcrim.org/community-health-workers (Accessed on December 7, 2022).
8. Holeman, I, and Kane, D. Human-centered design for global health equity. Inf Technol Dev. (2020) 26:477–505. doi: 10.1080/02681102.2019.1667289
9. Johnson, T, Das, S, and Tyler, N. Design for health: human-centered design looks to the future. Glob Health Sci Pract. (2021) 9:S190–4. doi: 10.9745/GHSP-D-21-00608
10. Perry, HB, Chowdhury, M, Were, M, LeBan, K, Crigler, L, Lewin, S, et al. Community health workers at the dawn of a new era: 11. CHWs leading the way to “Health for All”. Health Res Policy Syst. (2021) 19:755. doi: 10.1186/s12961-021-00755-5
11. Hoffman, SJ, Garcia, Y, Altamirano-Crosby, J, Ortega, SM, Yu, K, Abudiab, SM, et al. “How can you advocate for something that is nonexistent?” (CM16-17) Power of community in a pandemic and the evolution of community-led response within a COVID-19 CICT and testing context. Front Public Health. (2022) 10:901230. doi: 10.3389/fpubh.2022.901230
12. Wilson, L, Rubens-Augustson, T, Murphy, M, Jardine, C, Crowcroft, N, Hui, C, et al. Barriers to immunization among newcomers: A systematic review. Vaccine. (2018) 36:1055–62. doi: 10.1016/j.vaccine.2018.01.025
13. Cassady, D, Castaneda, X, Ruelas, MR, Vostrejs, MM, Andrews, T, and Osorio, L. Pandemics and vaccines: perceptions, reactions, and lessons learned from hard-to-reach Latinos and the H1N1 campaign. J Health Care Poor Underserved. (2012) 23:1106–22. doi: 10.1353/hpu.2012.0086
14. Kalocsányiová, E, Essex, R, and Fortune, V. Inequalities in COVID-19 messaging: a systematic scoping review. Health Commun. (2022) 38:1–10. doi: 10.1080/10410236.2022.2088022
15. Tensmeyer, NC, Dinh, NNL, Sun, LT, and Meyer, CB. Analysis of language translations of state governments’ coronavirus disease 2019 vaccine websites. Health Equity. (2022) 6:738–49. doi: 10.1089/heq.2021.0189
16. Salib, Y, Amodei, J, Sanchez, C, Castillo Smyntek, XA, Lien, M, Liu, S, et al. The COVID-19 vaccination experience of non-English speaking immigrant and refugee communities of color: a community co-created study. Community Health Equity Res Policy. (2022) 44:177–88. doi: 10.1177/2752535X221133140
17. Wells, KJ, Dwyer, AJ, Calhoun, E, and Valverde, PA. Community health workers and non-clinical patient navigators: a critical COVID-19 pandemic workforce. Prev Med. (2021) 146:106464. doi: 10.1016/j.ypmed.2021.106464
18. Refugee Women’s Network . Refugee Women’s Network. (2022). Available at: https://refugeewomensnetworkinc.org/ (Accessed on Oct 17, 2022).
19. U.S. Census Bureau QuickFacts . Clarkston city, Georgia. (2022). Available at: https://www.census.gov/quickfacts/fact/table/clarkstoncitygeorgia/PST120221 (Accessed on Oct 17, 2022).
20. United States Census Bureau . DP02: SELECTED SOCIAL … - Census Bureau Table. (2022). Available at: https://data.census.gov/table?q=Foreign+Born&tid=ACSDP1Y2021.DP02 (Accessed on Dec 20, 2022).
21. Feinberg, I, O’Connor, MH, Owen-Smith, A, and Dube, SR. Public health crisis in the refugee community: little change in social determinants of health preserve health disparities. Health Educ Res. (2021) 36:170–7. doi: 10.1093/her/cyab004
22. National Association of County and City Health Officials . The National Association of County and City Health Officials Announces $5 Million in Grants to Improve Public Health Connection to Refugee, Immigrant, and Migrant Communities - NACCHO. (2023). Available at: https://www.naccho.org/blog/articles/the-national-association-of-county-and-city-health-officials-announces-5-million-in-grants-to-improve-public-health-connection-to-refugee-immigrant-and-migrant-communities (Accessed on Jan 4, 2023).
23. National Resource Center for Refugees . Mothers x Mothers | National Resource Center for Refugees, Immigrants, and Migrants (NRC-RIM). (2024). Available at: https://nrcrim.org/covid-19/special-topics/mothers-x-mothers (Accessed on June 14, 2024).
24. McLeish, J, and Redshaw, M. Mothers’ accounts of the impact on emotional wellbeing of organised peer support in pregnancy and early parenthood: a qualitative study. BMC Pregnancy Childbirth. (2017) 17:28. doi: 10.1186/s12884-017-1220-0
25. Law, KH, Jackson, B, Tan, XH, Teague, S, Krause, A, Putter, K, et al. Strengthening peer mentoring relationships for new mothers: a qualitative analysis. J Clin Med. (2022) 11:6009. doi: 10.3390/jcm11206009
26. Shakya, P, Kunieda, MK, Koyama, M, Rai, SS, Miyaguchi, M, Dhakal, S, et al. Effectiveness of community-based peer support for mothers to improve their breastfeeding practices: a systematic review and meta-analysis. PLoS One. (2017) 12:e0177434. doi: 10.1371/journal.pone.0177434
27. Ugarte, DA, and Young, S. Effects of an online community peer-support intervention on COVID-19 vaccine misinformation among essential workers: mixed-methods analysis. West J Emerg Med. (2023) 24:264–8. doi: 10.5811/westjem.2023.1.57253
28. Harris, J, Springett, J, Croot, L, Booth, A, Campbell, F, Thompson, J, et al. Can community-based peer support promote health literacy and reduce inequalities? a realist review. Southampton (UK): NIHR Journals Library; (2015), 3, 1–192.
29. IDEO.org . (2022). Mothers x Mothers | Project. Available at: https://www.ideo.org/project/mothers-x-mothers (Accessed on Nov 28, 2022).
30. US Department of Labor . General Facts on Women and Job-Based Health. US: U.S. Department of Labor Employee Benefits Security Administration (2016).
31. Lee, CHJ, Overall, NC, and Sibley, CG. Maternal and paternal confidence in vaccine safety: Whose attitudes are predictive of children’s vaccination? Vaccine. (2020) 38:7057–62. doi: 10.1016/j.vaccine.2020.09.020
32. Suran, M . Why parents still hesitate to vaccinate their children against COVID-19. JAMA. (2022) 327:23–5. doi: 10.1001/jama.2021.21625
33. Ruiz, JB, and Bell, RA. Parental COVID-19 vaccine hesitancy in the United States. Public Health Rep. (2022) 137:1162–9. doi: 10.1177/00333549221114346
34. Goldman, RD, and Ceballo, R. Group the IC 19 PAS (COVIPAS). Parental gender differences in attitudes and willingness to vaccinate against COVID-19. J Paediatr Child Health. (2022) 58:1016–21. doi: 10.1111/jpc.15892
35. Schleiff, MJ, Aitken, I, Alam, MA, Damtew, ZA, and Perry, HB. Community health workers at the dawn of a new era: 6. Recruitment, training, and continuing education. Health Res Policy Syst. (2021) 19:757. doi: 10.1186/s12961-021-00757-3
36. Sullivan, E, and Morales, C. Texas, Indiana and Georgia are making all adults eligible for Covid-19 vaccination. The New York Times. (2021); Available at: https://www.nytimes.com/2021/03/23/us/texas-covid-vaccine-eligible.html (Accessed on 2024 Jul 19).
Keywords: community health workers (CHWs), human-centered design (HCD), COVID-19, peer support (PS), refugees and immigrants, mothers, COVID-19 vaccine acceptance, family health
Citation: de Acosta D, Moore T, Alam F, Hoffman SJ, Keaveney M, Mann E and Dawson-Hahn E (2024) “It spreads like wildfire”: mothers’ gatherings for vaccine acceptance. Front. Public Health. 12:1198108. doi: 10.3389/fpubh.2024.1198108
Edited by:
Steward Mudenda, University of Zambia, ZambiaReviewed by:
Sarah Denford, University College, Bristol, United KingdomNathan Mugenyi, Mbarara University of Science and Technology, Uganda
Copyright © 2024 de Acosta, Moore, Alam, Hoffman, Keaveney, Mann and Dawson-Hahn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Diego de Acosta, ZGVhY28wMTFAdW1uLmVkdQ==
 Diego de Acosta
Diego de Acosta Temple Moore
Temple Moore Fariha Alam
Fariha Alam Sarah J. Hoffman
Sarah J. Hoffman Megan Keaveney
Megan Keaveney Erin Mann
Erin Mann Elizabeth Dawson-Hahn
Elizabeth Dawson-Hahn