
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 16 January 2024
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1323335
Introduction: Health literacy is linked to the health status of older adults and is a critical component in achieving active aging. This study to characterize the current health literacy status among older adults in combined medical and nursing care institutions, as well as the factors that influenced this status.
Methods: This cross-sectional study used a convenience sampling method to select 740 older adults who were in 16 combined medical and nursing care institutions in Chengdu, China, from July 2022 to June 2023, using the Health Literacy Management Scale, the Social Support Rating Scale, and the Short Form-36 Health Survey.
Results: The results showed a health literacy score of 75.25 ± 12.33, the percentage of older adults with basic health literacy was 6.33%, a social support score of 37.37 ± 6.10, and a health-related quality of life score of 55.34 ± 15.48. Factors influencing health literacy included age, educational level, previous occupation, family size, monthly per capita household income, and health-related quality of life.
Discussion: Health literacy is an essential factor in improving the health status of older adults. Relevant departments should therefore improve health education and health promotion interventions for older adults in combined medical and nursing care institutions to improve health literacy.
According to China's National Bureau of Statistics, at the end of 2021, the number of people in China over 60 years of age was 267 million, accounting for 18.9% of the population (1). It is expected that around 2035, China's older adults population ≥60 years of age will exceed 400 million, entering a demographic stage with a large percentage of older adults (2). China's per capita healthy life expectancy in 2021 was 78.2 years (3). However, older adults generally suffer from a variety of chronic diseases. In China, there are more than 40 million disabled and semi-disabled older adults (4), so their health condition is not optimistic. Their demand for health services is urgent and imposes a heavy burden on medical and healthcare systems. The 14th Five-Year Plan for the Health of the older adults (5) states that strengthening health education for older adults and improving their health literacy were the primary goals for their health over the past 5 years.
The main ways for older adults in China to age are in communities or institutions. However, with the aging of China's population, the traditional family model of old age care is decreasing, and institutional care is gradually becoming an essential part of the old age care model (6). As most older adults in nursing care institutions have a lower level of education, declining physical function, a heavier burden of disease, and a poorer ability to perform their daily life tasks, there has been a significant increase in the demand for healthcare services for older adults in nursing care institutions, in addition to their material needs.
Health literacy is the ability of individuals to access, process, and understand basic health information and services, and to use them to make appropriate healthcare decisions (7, 8). The results of the 2020 report on monitoring the health literacy of Chinese residents showed that the health literacy level of older adults in the 65–69 year age group was 8.49%, which was the lowest level, when compared with other age groups (9). Compared with the health literacy level of 5.60% in the 65–69 year age group in the 2012 Health Literacy Monitoring Report of Chinese Residents (10), the health literacy level of older adults has shown a steady improvement. The “Healthy China 2030” plan states that health literacy levels should be raised through health education and the promotion of healthy lifestyles (11). The Chinese Government has also stated that health literacy is an essential determinant of health. Improving health literacy is therefore one of the most fundamental, cost-effective, and efficient measures for upgrading health.
Older adults are a vulnerable group when considering health literacy (12, 13). Inadequate health literacy will lead to an increase in the length of hospitalization, higher healthcare expenditures, lower utilization of health services, and poorer adherence to healthcare, which in turn will affect the physical health of older adults (14, 15). In particular, for older adults living in nursing care institutions, the living environment is more closed, with less access to external information, and most of them suffer from chronic diseases (16) and lack appropriate health knowledge and information. There is therefore an urgent need to improve their health literacy to achieve positive and healthy aging. Health literacy is a strong predictor of health status in older adults (17, 18). From an individual perspective, improved health literacy enables older adults to better self-manage their health, and thus improve their health and health-related quality of life (19); and from a socio-economic perspective, improved health literacy partially reduces the pressure and financial burden on the National Health Service (20).
Several studies have reported that health literacy significantly influences health outcomes, and has a crucial role in an individual's physical and mental health (16, 21). Individuals with lower health literacy devote less attention to their health status and are more inclined to have unhealthy behaviors, which in turn leads to a lower quality of life (22). In addition, some studies have shown that social support is an influential factor linking health literacy and quality of life. Good social support enhances an individual's health-promoting behaviors and improves their quality of life (23).
The purpose of this study was therefore to investigate the health literacy of older adults in combined medical and nursing care institutions, and to identify influential factors, to provide a reference basis for the subsequent development of health literacy intervention strategies, and to improve the overall health-related quality of life of the older adults in combined medical and nursing care institutions.
This was a cross-sectional study, and a convenience sampling method was used to select older adults in 16 combined medical and nursing care institutions in Chengdu City from July 2022 to June 2023. Inclusion criteria included the following: age ≥ 60 years, length of stay ≥90 days, clear consciousness and regular language expression, and informed consent. Exclusion criteria included the following: a cognitive or mental disorder, and a visual or hearing impairment. The sample size was calculated using the following formula (24). According to the 2020 report on monitoring the health literacy of Chinese residents, the health literacy level of Chinese seniors was 8.49%. Therefore, this study set P = 0.0849, α = 0.05, Z1−α/2 = 1.96, and δ = 0.03. Based on this formula, the sample size was calculated to be 332, and the minimum sample size was estimated to be 399, considering the 20% sample non-response percentage. To make the results more representative, 740 questionnaires were distributed, 13 questionnaires with incomplete information was excluded, and 727 valid questionnaires (98.24%) were recovered for analysis.
This study used a questionnaire survey method conducted on-site by uniformly trained investigators using a one-on-one approach. Prior to the survey, the purpose and content of the study were explained to older adults, and the questionnaire was independently completed by the older adults. Those who were unable to complete the questionnaire had the questionnaire entries read by the investigator, who completed the questionnaire on their behalf, based on their responses. The survey took 15–20 min to complete, and all questionnaires were collected immediately and checked for completeness. This study was approved by the Chengdu Medical College Ethics Committee (CMCEC-2022NO.42). The participants provided their written informed consent to participate in the study.
The data included was designed by the investigators, and included sex, age, marital status, educational level, previous occupation, family size, monthly per capita household income, smoking status, and alcohol consumption.
There is currently no general health literacy scale for older adults in China (25). Due to the prevalence of chronic diseases among older adults in China, this study used the Health Literacy Management Scale to measure the health literacy level of older adults in nursing care institutions. The scale was compiled by Haolin Sun (26), including four dimensions of ability to access information, ability to communicate and interact, willingness to improve health, and willingness to support financially, with a total of 24 entries, using a five-level Likert scale, with scores from 1 to 5 representing “very difficult” to “not difficult at all,” and a total score of 24–120, with a higher score indicating a higher level of health literacy. A questionnaire score of 80% or more of the total score was considered to have basic health literacy, and its number as a percentage of the total number of people surveyed was the level of health literacy. The Cronbach α coefficient for this scale was 0.908.
The Social Support Rating Scale was designed by Xiao (27), including three dimensions of objective social support, subjective social support, and availability of social support, with a total of 10 entries and a total score of 12–66 points, with higher scores indicating higher levels of social support. The Cronbach α coefficient for this scale study was 0.765.
Short Form-36 Health Survey, the Quality of Survival Evaluation Scale or the Health Survey Short Form (28), is a measurement scale developed by the Bureau of Medicine Research Group. The Chinese version of the scale (29) consisted of a reported health transition, eight dimensions of physical functioning, physical role, bodily pain, general health, vitality, social functioning, emotional role, and mental health, totaling 36 entries. According to the weight of each entry, the sum of the scores of each entry in each dimension was separately calculated, and the crude score of each dimension was calculated. Finally, the crude score was converted to a standard score from 0 to 100. The conversion formula was the following: standard score = (actual score – lowest score of the entry)/(highest score of the entry – lowest score of the entry) × 100. The standardized score ranged from 0 to 100, with higher scores representing a better health-related quality of life. The Cronbach α coefficient for this scale was 0.852.
Data were entered using Epidata 3.1 software and statistically analyzed using SPSS 26.0 statistical software for Windows (SPSS, Chicago, IL, USA). Quantitative information was expressed as ( ± S) for normal distributions and M (P25, P75) for parametric distributions, and count information was expressed as the frequency and percentage. One-way analysis was performed using the independent samples t-test and one-way analysis of variance. The relationships between health literacy, social support, and health-related quality of life were determined using Pearson's correlation analysis. A multivariate stepwise linear regression analysis was conducted with variables that were meaningful in the univariate analysis as independent variables, to identify factors influencing the health literacy of older adults in combined medical and nursing care institutions. The test level α was set at 0.05 unless otherwise stated.
The results of this study showed that the health literacy scores of older adults in combined medical and nursing care institutions was 75.25 ± 12.33, the percentage of older adults with basic health literacy was 6.33%, and the social support score was 37.37 ± 6.10. The health-related quality of life score was 55.34 ± 15.48. The scores of each dimension of the scale are listed in Table 1.
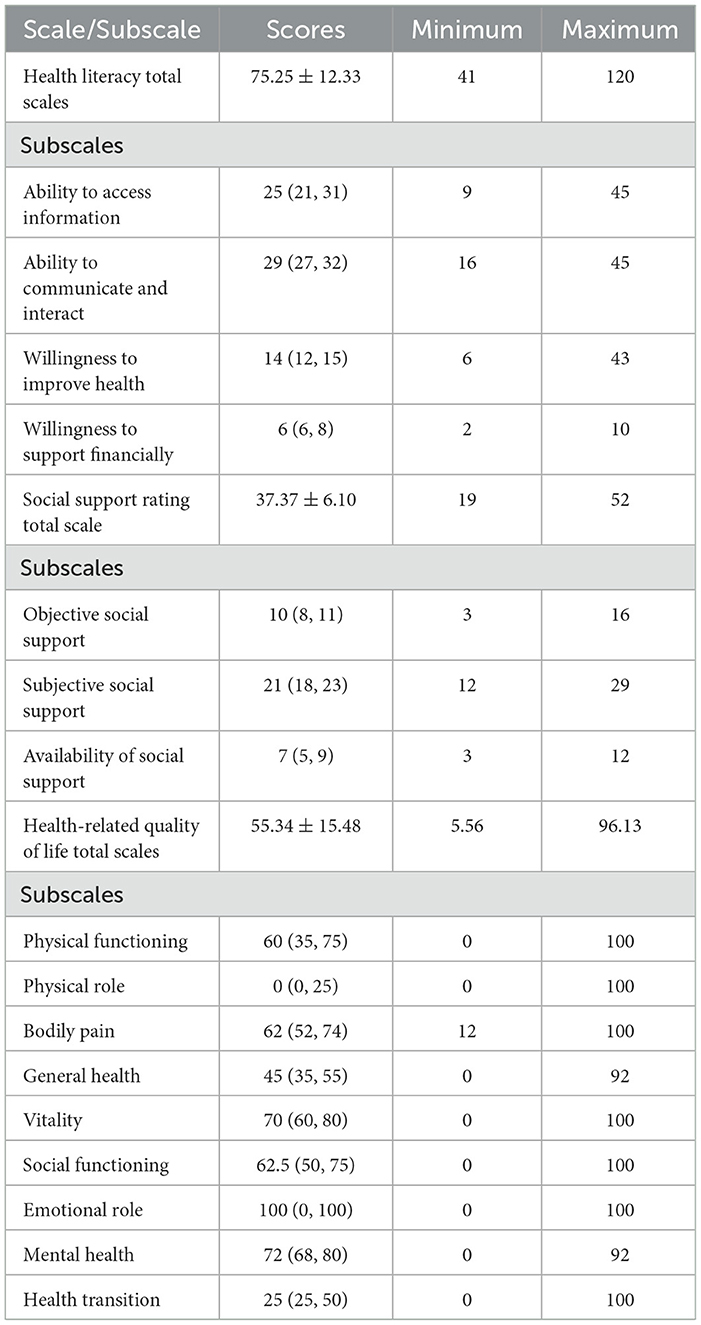
Table 1. Health literacy, social support, and health-related quality of life scores for older adults in combined medical and nursing care institutions.
The univariate analysis of this study showed that there were statistically significant differences between the nine variables of different sexes, age, marital status, educational levels, previous occupation, family size, monthly per capita household income, smoking status, and alcohol consumption, when compared to health literacy scores (P < 0.05), as shown in Table 2.

Table 2. A one-factor analysis of health literacy scores of older adults in combined medical and nursing care institutions.
The results of Pearson's correlation analyses showed that the total health literacy scores, the total social support scores, and the total health-related quality of life scores of older adults in combined medical and nursing care institutions were positively correlated (P < 0.05). See Table 3 for details.
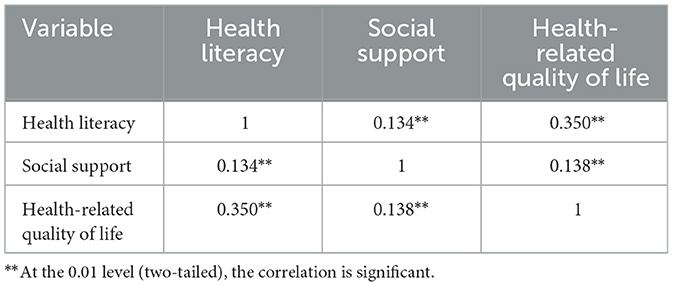
Table 3. Correlation analysis of health literacy, social support, and health-related quality of life scores of older adults in combined medical and nursing care institutions.
The total health literacy score of older adults in combined medical and nursing care institutions was used as the dependent variable, and the statistically significant variables in the univariate and correlation analyses were used as the independent variables in the multiple linear stepwise regression analyses. The results showed that age, educational level, previous occupation, family size, monthly per capita household income, and health-related quality of life influenced health literacy among older adults in combined medical and nursing care institutions, which explained 40.2% of the total variation. The assignments of the independent variables are shown in Table 4, and the results of the linear regression analyses are shown in Table 5.
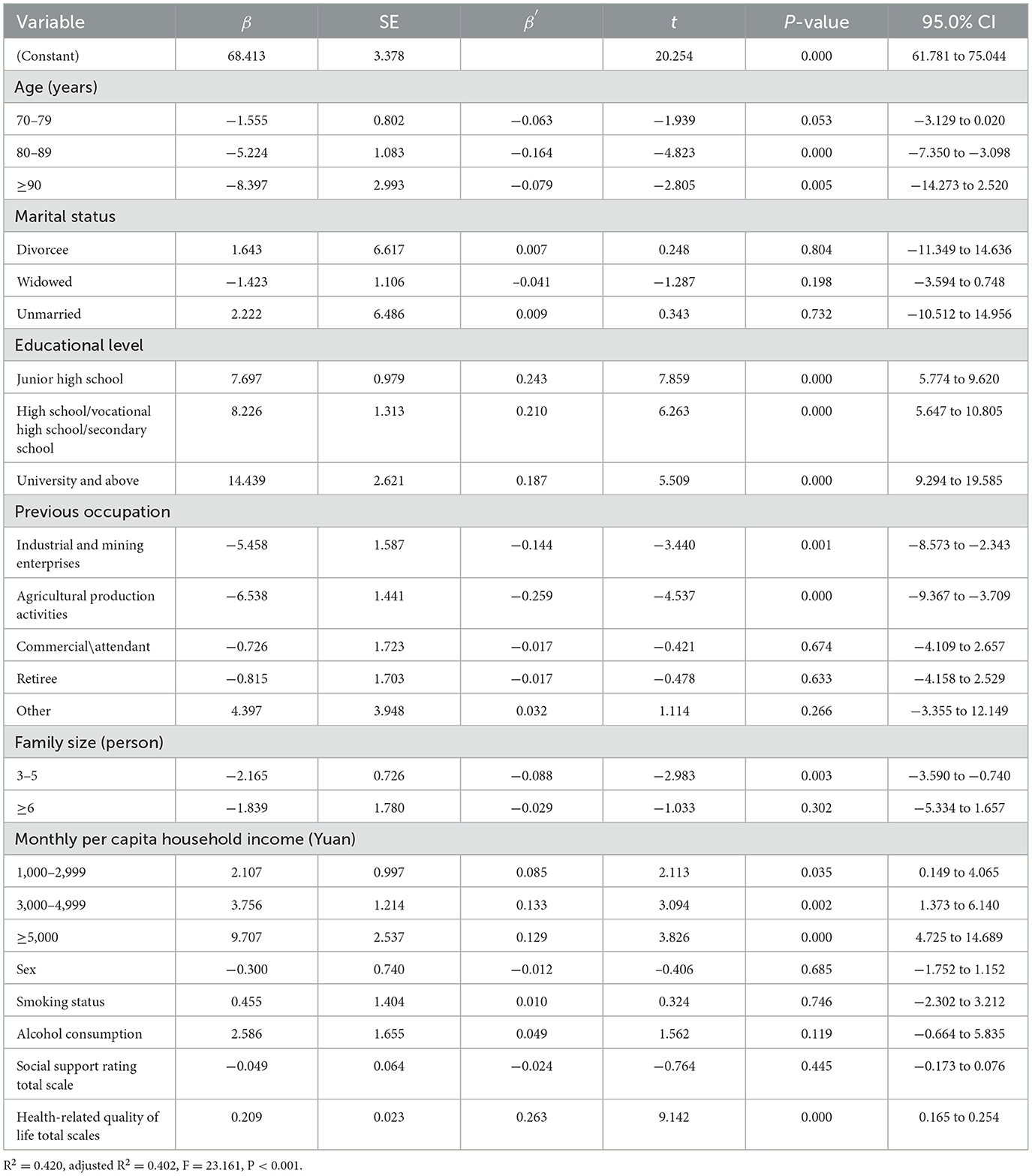
Table 5. Multiple linear regression analysis of the factors influencing health literacy of older adults in combined medical and nursing care institutions.
In this study, the health literacy score of older adults in combined medical and nursing care institutions was 75.25 ± 12.33, which was higher than those of older adults in Yinchuan City, China (30) and Urumqi City, China (19). The reasons may be related to geographical differences, the level of economic development, and older adult's use of health-related resources. Only 6.33% of the older adults in this study had basic health literacy, and the scores for the dimensions of health literacy were, in descending order, ability to communicate and interact, ability to access information, willingness to improve health, and willingness to support financially. Although older adults had a certain degree of health information acquisition, communication, and interaction, there may have been cognitive and economic problems, resulting in a particular gap in transforming health knowledge into health behavior. Therefore, we recommend that the relevant staff of nursing care institutions work together with medical institutions to conduct health education and promotion activities, popularize health knowledge. Furthermore, they should disseminate health knowledge and skills through scientific and authoritative channels, enhance the grasp and understanding of health knowledge among older adults, and help older adults scientifically recognize health problems and implement health behaviors so that they will be willing to improve their existing health problems and enhance their health literacy.
The results of this study showed that the health literacy level of older adults 80–89 years of age vs. those aged ≥90 years of age was lower than that of younger adults 60–69 years of age. Consistent with the findings of Fry et al. (31), with age, the cognitive level of older adults gradually declined, and comprehension decreased, leading to a decrease in the ability of older adults to acquire and master health information and, thus, a decrease in health literacy. It is recommended that when health education is conducted for older adults of different ages, the distribution of brochures, the broadcasting of videos, and the use of a variety of methods in health lectures be chosen to disseminate health-related information in an easy-to-understand manner. Furthermore, health education activities should be conducted to improve the level of health literacy among older adults of advanced ages.
This study showed that as the educational level increased, the health literacy level of older adults increased, which is consistent with the results of previous studies (13, 32). The higher the educational level, and the better the knowledge base of older adults, the better their ability and initiative in acquiring, processing, and understanding information, and the stronger their sense of self-care, the more they will take the initiative to obtain various health information. In contrast, older adults with lower educational levels are slower to accept new things, have poorer self-understanding, have limited awareness of disease prevention, and find it challenging to acquire scientific and adequate health knowledge and skills, resulting in lower health literacy (33, 34). In this survey, the literacy level of older adults was usually low, with 67.7% of older adults having a literacy level of primary and below. These results suggest that the relevant local authorities should pay attention to older adults with a lower literacy level, and conduct long-term corresponding health education for older adults at different literacy levels. Methods such as the teach-back method should be used to promote older adults' understanding of the relevant health information, to improve their health literacy level.
This study showed that older adults who had worked in industrial and mining enterprises and those who had been engaged in agricultural production activities had lower levels of health literacy than those who had worked in offices. Work in industrial and mining enterprises and agricultural production activities involves manual labor, while work in an office involves mental activities. Previous studies (35, 36) have reported that occupation as a manual laborer is a risk factor for the health literacy of older adults in China. The health literacy level of manual laborers is significantly lower than that of office worker laborers, which may be related to the fact that manual laborers have fewer chances to receive health-related training than those who are office workers, as they become older adults (37, 38). Their income level decreases, and they focus more on sustaining their livelihoods, ignoring their physical health, which, in turn, influences the status of their health literacy. Therefore, the relevant government agencies should pay attention to older adults engaged in manual work, increase publicity on health education, and conduct health promotion and health science activities through multiple channels and in multiple ways to improve their health literacy.
This study showed that older adults with a family size of 3–5 members were less health literate than those with a family size of 1–2 members. Consistent with the results of a study in Jiangsu Province, China (39), the reason for this may involve the socio-cultural context of China; older adults tend to live with their children or grandchildren. As the number of family members increases, their attention is more focused on their children or grandchildren (40). They pay less attention to their health, and their health literacy needs to be addressed. Therefore, volunteers are encouraged to enter nursing care institutions and interact with older adults, to increase their health knowledge, learn health skills, and improve their health literacy.
This study showed that the health literacy level of older adults increased as the monthly per capita household income increased, which is consistent with the findings of Kim (41) involving older adults in Korea. The higher the monthly per capita household income, the better the economic base, the more social resources they can obtain, the better the health-related quality of life, the more attention they will pay to their health status, the more health information they will obtain, and thus the better the level of health literacy (42, 43). The relevant departments are therefore encouraged to pay more attention to the health literacy of older adults with lower monthly per capita household income, to improve the ability of older adults with financial difficulties to obtain and understand health-related information, and to enhance their health literacy levels.
This study showed that health-related quality of life considerably influences the health literacy of older adults in nursing care institutions. We found that the higher the health-related quality of life of older adults in nursing care institutions, the higher the level of health literacy. This finding is consistent with the results of the study by Liu et al. (17). Older adults who perceived themselves to be in better health and were more health-conscious had a greater awareness of physical healthcare and health information needs, and were more likely to seek health knowledge and skills and practice them in their daily lives to promote healthy lifestyles and behavior and improve health-related quality of life (44, 45). Therefore, healthcare providers should identify people with low levels of health literacy and develop programs for different health conditions based on individual circumstances. They should also reduce jargon in communication to promote their patients' understanding of relevant health knowledge to improve the health-related quality of life and health outcomes.
The results of this study showed that the health literacy of older adults in combined medical and nursing care institutions was positively correlated with social support (P < 0.05), suggesting that the higher the level of social support, the higher the level of health literacy. Some studies have reported that social support had an essential influence on health literacy and overall health status, and that higher levels of social support positively influenced health literacy and health status (46, 47). In our study, health literacy was positively associated with the health-related quality of life (P < 0.05), similar to the findings of Zheng et al. (48). Multiple linear stepwise regression results also showed that the higher the health-related quality of life, the higher the relative level of health literacy among older adults. Older adults with lower levels of health literacy may need more access to healthcare resources. They may need to more clearly articulate their needs when communicating with professionals, such as doctors, to seek additional healthcare services, ultimately leading to increased health-related quality of life (49). Therefore, to improve the health literacy of older adults, the positive impact of social support and health-related quality of life should be emphasized. When faced with older adults with a low level of health literacy, workers should patiently communicate in an easy-to-understand manner, guiding them to use the social support system they already have to improve their health and health literacy.
This study had some limitations. First, in the selection of the research subjects, this study only investigated some of the older adults in combined medical and nursing care institutions in Chengdu City, China, which could only partially reflect the actual health literacy level of all older adults in China. Because health literacy levels are closely related to the level of regional economic development, it is therefore necessary to include a broader range of older adults in future studies so that the results of this study can be based on a representative sample. Second, in terms of research methodology, this study conducted a cross-sectional survey using a questionnaire survey method without any interventions and control of relevant factors, so subsequent prospective cohort studies should be conducted on the basis of this study to further determine effective measures to improve the health literacy of older adults in combined medical and nursing care institutions.
To summarize, the health literacy level of older adults in combined medical and nursing care institutions was low, fewer older adults have basic health literacy, and the health outlook could be improved. Combined medical and nursing care institutions and relevant departments should pay closer attention to factors affecting the health literacy of older adults. Furthermore, they should help older adults correctly understand aging, establish a positive outlook on aging, and conduct health education activities for older adults using online and offline methods (such as conducting health education bulletin boards, broadcasting health education promotional videos, and holding health clinics, etc.). Doing so will promote the enhancement of health literacy in the form of a tripartite linkage between the government, society, and institutions to better realize positive and healthy aging.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
ST: Conceptualization, Writing – original draft. SS: Conceptualization, Writing – original draft. SW: Methodology, Writing – review & editing. TP: Formal analysis, Writing – review & editing. LC: Methodology, Writing – review & editing. MY: Investigation, Writing – original draft. JM: Investigation, Writing – original draft. HL: Conceptualization, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by National Key Research and Development Program of China (2018YFC2002401) and Foundation of Chengdu Medical College (CYSYB20-07).
We would also like to thank all the investigators for their assistance with data collection and all the respondents for their cooperation.
TP was employed by Sichuan Yibeikang Technology Co., LTD.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. National Bureau of Statistics Information Disclosure [EB/OL]. (2022). Available online at: http://www.stats.gov.cn/xxgk/jd/sjjd2020/202201/t20220118_1826609.html (accessed August 27, 2023).
2. Transcript Transcript of the Press Conference of the National Health Commission on September 20 2022, [EB/OL],. (2022). Available online at: http://www.nhc.gov.cn/xcs/s3574/202209/ee4dc20368b440a49d270a228f5b0ac1.shtml (accessed August 27, 2023).
3. Life Expectancy Per Capita in China to Increase to 78,.2 Years by 2021 [EB/OL] (2022). Available online at: https://www.gov.cn/xinwen/2022-07/12/content_5700668.htm?eqid=bb8caf9a00009d2400000006647470fe (accessed December 11, 2023).
4. Dang J, Wang L. China Report of the Development on Ageing Industry (2021–2022). Social Sciences Academic Press (2023).
5. Notice on the Issuance of the “14th Five-Year Plan” for Healthy Aging [EB/OL]. (2022). Available online at: http://www.nhc.gov.cn/lljks/pqt/202203/c51403dce9f24f5882abe13962732919.shtml (accessed September 18, 2023).
6. Shao C, Qin B, Zhao W. Mental health status and influencing factors of the elderly in Deyang City nursing institutions. Chin J Gerontol. (2019) 39:2807–9. doi: 10.3969/j.issn.1005-9202.2019.11.076
7. Liu C, Wang D, Liu C, Jiang J, Wang X, Chen H, et al. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam Med Community Health. (2020) 8:e000351. doi: 10.1136/fmch-2020-000351
8. Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. (2012) 12:1–13. doi: 10.1186/1471-2458-12-80
9. Questions Answers on Health Literacy of Chinese Residents [EB/OL]. (2021). Available online at: https://www.gov.cn/xinwen/2021-04/01/5597287/files/fa3930ea661d4feba05a0dd66288e52c.pdf (accessed September 18, 2023).
10. Health Literacy Monitoring Report of Chinese Residents [EB/OL]. (2013). Available online at: http://www.nhc.gov.cn/ewebeditor/uploadfile/2014/12/20141216160546459.pdf (accessed December 11, 2023).
11. Outline of the “Healthy China 2030” Plan [EB/OL]. (2016). Available online at: https://www.gov.cn/zhengce/2016-10/25/content_5124174.htm (accessed December 11, 2023).
12. Geboers B, de Winter AF, Spoorenberg SLW, Wynia K, Reijneveld SA. The association between health literacy and self-management abilities in adults aged 75 and older, and its moderators. Qual Life Res. (2016) 25:2869–77. doi: 10.1007/s11136-016-1298-2
13. Ma T, Meng H, Ye Z, Jia C, Sun M, Liu D. Health literacy mediates the association between socioeconomic status and productive aging among elderly Chinese adults in a newly urbanized community. Front Public Health. (2021) 9:647230. doi: 10.3389/fpubh.2021.647230
14. Huang Y, Qi F, Wang R, Jia X, Wang Y, Lin P, et al. The effect of health literacy on health status among residents in Qingdao, China: a path analysis. Environ Health Prev Med. (2021) 26:78. doi: 10.1186/s12199-021-01001-8
15. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005
16. Fabbri M, Murad MH, Wennberg AM, Turcano P, Erwin PJ, Alahdab F, et al. Health literacy and outcomes among patients with heart failure: a systematic review and meta-analysis. JACC Heart Fail. (2020) 8:451–60. doi: 10.1016/j.jchf.2019.11.007
17. Liu Y-B, Xue L-L, Xue H-P, Hou P. Health literacy, physical and mental health, and activities of daily living among older chinese adults in nursing homes. Asia Pac J Public Health. (2018) 30:592–9. doi: 10.1177/1010539518800368
18. Xu L, Xie L, Li X, Wang L Gao Y-m. A meta-analysis of factors influencing health literacy among Chinese older adults. J Public Health. (2022) 30:1889–900. doi: 10.1007/s10389-021-01638-3
19. Liu Y, Hou P, Xue H, Mao X, Li Y. Social support, health literacy, and health care utilization among older adults. Asia Pac J Public Health. (2019) 31:359–66. doi: 10.1177/1010539519851674
20. Xie Y, An W, Zheng C, Zhao D, Wang H. Multidimensional health literacy profiles and health-related behaviors in the elderly: a cross-sectional survey. Int J Nurs Sci. (2022) 9:203–10. doi: 10.1016/j.ijnss.2022.02.007
21. Mai J, Yibo W, Ling Z, Lina L, Xinying S. Health literacy and personality traits in two types of family structure-a cross-sectional study in China. Front Psychol. (2022) 13:835909. doi: 10.3389/fpsyg.2022.835909
22. Park NH, Song MS, Shin SY, Jeong JH, Lee HY. The effects of medication adherence and health literacy on health-related quality of life in older people with hypertension. Int J Older People Nurs. (2018) 13:e12196. doi: 10.1111/opn.12196
23. Alshraifeen A, Al-Rawashdeh S, Alnuaimi K, Alzoubi F, Tanash M, Ashour A, et al. Social support predicted quality of life in people receiving haemodialysis treatment: a cross-sectional survey. Nurs Open. (2020) 7:1517–25. doi: 10.1002/nop2.533
24. Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. (2013) 35:121–6. doi: 10.4103/0253-7176.116232
25. Ou Y, Wang X, Yang C, Tan YZ. Progress of research on health literacy assessment tools for the elderly. Nurs J Chin PLA. (2018) 35:39–43. doi: 10.3969/j.issn.1008-9993.2018.02.008
26. Sun HL. Development and Preliminary Application of Scale on Health Literacy for Patients with Chronic Disease. Shanghai: Fudan University (2012).
27. Xiao S. Theoretical basis and research applications of the Social Support Rating Scale. J Clin Psychiatry. (1994) 4:98–100.
28. Santos M, Sousa C, Pereira M, Pereira MG. Quality of life in patients with multiple sclerosis: a study with patients and caregivers. Disabil Health J. (2019) 12:628–34. doi: 10.1016/j.dhjo.2019.03.007
29. Wang H, Li L, Shen Y. Study on the Chinese version of SF-36 scale for the quality of life of Hangzhou city residents. Chin J Prev Med. (2001) 35:69–71. doi: 10.3760/j:issn:0253-9624.2001.06.023
30. Chen Y, Mei Y, Yan S, Wang W. Correlation between health literacy and cognitive function of elderly people in Yinchuan nursing facilities. Chin J Gerontol. (2020) 40:4883–6. doi: 10.3969/j.issn.1005-9202.2020.22.053
31. Fry JM, Antoniades J, Temple JB, Osborne RH, Cheng C, Hwang K, et al. Health literacy and older adults: findings from a national population-based survey. Health Promot J Austr. (2023). doi: 10.1002/hpja.779. [Epub ahead of print].
32. Furuya Y, Kondo N, Yamagata Z, Hashimoto H. Health literacy, socioeconomic status and self-rated health in Japan. Health Promot Int. (2015) 30:505–13. doi: 10.1093/heapro/dat071
33. Ayaz-Alkaya S, Ozturk FO. Health literacy levels of women and related factors in Turkey. J Nurs Res. (2021) 29:e180. doi: 10.1097/JNR.0000000000000452
34. Mei X, Zhong Q, Chen G, Huang Y, Li J. Exploring health literacy in Wuhan, China: a cross-sectional analysis. BMC Public Health. (2020) 20:1417. doi: 10.1186/s12889-020-09520-9
35. Li P, Zhang C, Niu H, Yu Q, Li X, Ban X. Influencing factors of health literacy of the elderly in China: a meta analysis. Occup Health. (2023) 39:837–41. doi: 10.13329/j.cnki.zyyjk.2023.0172
36. Qian X, Fan X, Li R, Li W, Guo X, Ren Z, et al. Chronic disease prevention literacy and its influencing factors among middle-aged and elderly people in Jilin Province. Chin J Gerontol. (2020) 40:1331–3. doi: 10.3969/j.issn.1005-9202.2020.06.065
37. Xu Q, Mei Q, Feng H, Zhu YY, He TF. Changing trend and influencing factors of health literacy among residents in Ningbo from 2015 to 2019. Prev Med. (2021) 33:35–40. doi: 10.19485/j.cnki.issn2096-5087.2021.01.008
38. Xu L, Xiong Y, Li H, Zhou W, Liu J, Jiao Y, et al. Analysis on the status of health literacy and its influencing factors among residents aged 15-69 years old in Haidian District of Beijing City in 2018. J Hyg Res. (2020) 49:738–43. doi: 10.19813/j.cnki.weishengyanjiu.2020.05.007
39. Hu J, Guo H, Li Y, Qu C, Chen Y, Li X, et al. Health literacy and its influencing factors among residents aged 60-69 years in Jiangsu province. Chin J Public Health. (2016) 32:1156–8. doi: 10.11847/zgggws2016-32-09-06
40. Lan W, Wan D, Liu X, Gu L, Long G, Peng Z, et al. Analysis on the influencing factors of differences in health literacy levels among different gender populations in Fuzhou City. Chin J Health Educ. (2023) 39:175–81. doi: 10.16168/j.cnki.issn.1002-9982.2023.02.016
41. Kim SH. Health literacy and functional health status in Korean older adults. J Clin Nurs. (2009) 18:2337–43. doi: 10.1111/j.1365-2702.2008.02739.x
42. Yigitalp G, Bayram DV, Cifci S. Health literacy, health perception and related factors among different ethnic groups: a cross-sectional study in southeastern Turkey. BMC Public Health. (2021) 21:1109. doi: 10.1186/s12889-021-11119-7
43. Li Z, Tian Y, Gong Z, Qian L. Health literacy and regional heterogeneities in China: a population-based study. Front Public Health. (2021) 9:603325. doi: 10.3389/fpubh.2021.603325
44. Liu S, Zhao H, Fu J, Kong D, Zhong Z, Hong Y, et al. Current status and influencing factors of digital health literacy among community-dwelling older adults in Southwest China: a cross-sectional study. BMC Public Health. (2022) 22:996. doi: 10.1186/s12889-022-13378-4
45. Zhang Q, Huang F, Zhang L, Li S, Zhang J. The effect of high blood pressure-health literacy, self-management behavior, self-efficacy and social support on the health-related quality of life of Kazakh hypertension patients in a low-income rural area of China: a structural equation model. BMC Public Health. (2021) 21:1114. doi: 10.1186/s12889-021-11129-5
46. Lee SY, Arozullah AM, Cho YI. Health literacy, social support, and health: a research agenda. Soc Sci Med. (2004) 58:1309–21. doi: 10.1016/S0277-9536(03)00329-0
47. Vayro C, Brownlow C, Ireland M, March S. A thematic analysis of the personal factors influencing mental health help-seeking in farmers. J Rural Health. (2023) 39:374–82. doi: 10.1111/jrh.12705
48. Zheng M, Jin H, Shi N, Duan C, Wang D, Yu X, et al. The relationship between health literacy and quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes. (2018) 16:201. doi: 10.1186/s12955-018-1031-7
Keywords: combined medical and nursing care, nursing care institutions, older adults, health literacy, influencing factors
Citation: Tao S, Sun S, Wu S, Peng T, Cao L, Yan M, Ma J and Li H (2024) Current status and influencing factors of health literacy among older adults in combined medical and nursing care institutions: a cross-sectional study. Front. Public Health 11:1323335. doi: 10.3389/fpubh.2023.1323335
Received: 23 October 2023; Accepted: 26 December 2023;
Published: 16 January 2024.
Edited by:
Toni P. Miles, Rosalynn Carter Institute for Caregivers, United StatesReviewed by:
Wei Luan, Shuguang Hospital Affiliated to Shanghai University of TCM, ChinaCopyright © 2024 Tao, Sun, Wu, Peng, Cao, Yan, Ma and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Li, MTAyMDE5MDIzQGNtYy5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.