- 1The Working Group to Analyze the Emergency Medical Care System in Osaka Prefecture, Osaka, Japan
- 2Department of Traumatology and Acute Critical Medicine, Osaka University Graduate School of Medicine, Suita, Japan
- 3Department of Social and Environmental Medicine, Division of Environmental Medicine and Population Sciences, Osaka University Graduate School of Medicine, Suita, Japan
- 4Osaka Prefectural Government, Osaka, Japan
- 5Department of Emergency Medicine, Tane General Hospital, Osaka, Japan
- 6Rinku General Medical Center, Izumisano, Japan
Background: The novel corona virus (COVID-19) pandemic occurred worldwide. Although an excessive burden was placed on emergency medical institutions treating urgent and severe patients, its impact on patient outcome remains unknown. This study aimed to assess the impact of the COVID-19 pandemic in 2021 on the emergency medical services (EMS) system and patient outcomes in Osaka Prefecture, Japan.
Methods: This was a retrospective descriptive study with a study period from January 1, 2019 to December 31, 2021. We included patients who were transported by ambulance and had cleaned data that was recorded in the ORION system. The study endpoints were the number of patients transported by ambulance and the number of deaths among these patients in each month. To assess the impact of the COVID-19 pandemic on the EMS system, the incidence rate ratio (IRR) and 95% confidence interval (CI) were calculated using 2019 as the reference year. Mortalities were evaluated based on deaths in the emergency department and deaths at 21 days after hospitalization.
Results: The numbers of patients transported by ambulance were 500,194 in 2019, 443,321 in 2020 (IRR: 0.88, 95% CI: 0.87–0.88), and 448,054 in 2021 (IRR: 0.90, 95% CI: 0.89–0.90). In 2019, the number of patients transported by ambulance and who died in the emergency departments was 4,980, compared to 5,485 in 2020 (IRR: 1.10, 95% CI; 1.06–1.44) and 5,925 in 2021 (IRR: 1.19, 95% CI: 1.15–1.24). In 2019, the number of patients who died within 21 days after hospitalization was 11,931, compared to 11,913 in 2020 (IRR; 1.00, 95% CI; 0.98–1.03) and 13,376 in 2021 (IRR; 1.12, 95% CI; 1.09–1.15).
Conclusion: The COVID-19 pandemic decreased the number of ambulance requests and worsened mortality of patients transported by ambulance in Osaka Prefecture during 2021.
Introduction
Novel coronavirus (COVID-19), confirmed in Wuhan, China in December 2019, spread not only in China but throughout the world (1–7). In Japan, the number of COVID-19 patients exceeded 1.7 million as of December 31, 2021 (8). COVID-19 is characterized by symptoms common to ordinary upper respiratory tract infections, such as fever, cough, general malaise, and some patients are even asymptomatic (2, 5, 7, 9). However, the severely ill patients, which account for about 20% of the patients with COVID-19, require intensive care, mainly mechanical ventilation and extracorporeal membrane oxygenation.
As the number of COVID-19 patients increased, especially in the United States and European countries, the number of healthcare workers infected with COVID-19 also increased, and the healthcare system, including emergency medical services (EMS) and intensive care, experienced a critical situation. The healthcare system in Japan is operated from public healthcare insurance, and the EMS system, through which an ambulance can be called, is a public service (10). Since the outbreak of COVID-19, patients with fever have visited specific medical institutions that can treat COVID-19 and have been diagnosed and treated for COVID-19. However, on weekends including holidays and at night when these medical institutions are not open, patients with sudden fever call for an ambulance and are transported to those emergency medical institutions that provide COVID-19 care. Many of these medical institutions include critical care centers that treat severe trauma and out-of-hospital cardiac arrest (OHCA). As a result, an excessive burden was placed on these emergency medical institutions that treat urgent and severe patients, but the impact of this situation on patient outcomes remains unknown.
Osaka Prefecture is the largest metropolitan area in western Japan, with a population of 8.8 million people and approximately a half million calls for ambulances each year (11). Since the first patient with COVID-19 occurred in Osaka Prefecture on January 23, 2020, the cumulative number of COVID-19 patients in Osaka Prefecture as of December 31, 2021 was 203,790 (12). We previously showed the impact of the spread of COVID-19 in 2020 on the EMS system and patient outcomes of those transported by ambulance (13, 14). However, in Japan, there was a marked increase in the number of COVID-19 patients in 2021 compared to 2020, which may have had a further impact. Therefore, the purpose pf this study was to assess the impact of the COVID-19 pandemic in 2021 on the EMS system and patient outcomes using population-based emergency patient registry in Osaka, Japan.
Materials and methods
Study design and settings
This was a retrospective descriptive study with a study period from January 1, 2019 to December 31, 2021. We included patients in this study who were transported by ambulance and who had cleaned data that was recorded in the ORION system. Therefore, we excluded patients who were not registered in the ORION system or had missing data.
In 2020, 8,837,685 people lived in the 1905 km2 area of Osaka Prefecture. Of that population, 4,235,956 people (47.9%) were male and 2,441,984 people (25.4%) were older adults, aged 65 years old or more (10). Because the ORION data is anonymized without specific personal data, such as patient name, date of birth, and address, the requirement of obtaining patients’ informed consent was waived. This study was approved by the Ethics Committee of Osaka University Graduate School of Medicine, Suita, Japan (approval number: 15003). This manuscript was written based on the STROBE statement to assess the reporting of cohort and cross-sectional studies (15).
EMS system and hospitals in Osaka Prefecture and Japan
The EMS system is basically the same as that used in other areas of Japan. In Osaka Prefecture, EMS systems such as ambulance dispatch systems are operated by each local government, and ambulances are dispatched by calling 1-1-9. In 2021, the EMS system was operated by 26 fire departments (298 ambulances) and 26 fire control stations. In 2018, there were 517 medical institutions (105,994 beds) in Osaka Prefecture (16), of which 288 are emergency medical hospitals including 16 critical care centers that are designated to accept patients with life-threatening emergency diseases such as severe trauma and sepsis. Since the introduction of the ORION system, EMS personnel at the scene select the appropriate hospital for emergency patients rather than a dispatcher.
The ORION system
Information on the system configuration of ORION was previously described in detail (17, 18). The EMS personnel at the scene operate the ORION smartphone app for each emergency patient. All of the data input into the cellphone app, such as vital signs and the time of the call to the hospital for acceptance, are also recorded. The cellphone app data are accumulated in the ORION cloud server, and in cooperation with the dispatched EMS personnel, data managers at each fire department directly input or upload the ambulance record of each emergency patient so that it can be connected with the app data. Furthermore, the operators of each hospital also directly input or upload the patient’s data, such as diagnoses and outcomes, after hospital acceptance. The results of the aggregated data in the ORION system are fed back to every fire department and emergency hospital. The Department of Public Health of Osaka Prefecture can also analyze the effects of health policy on the emergency medical system using these collected data. The ORION system has been in place in all fire departments and emergency hospitals in Osaka Prefecture since January 2016.
Data collection and quality control
The ORION system checks for errors in the inputted in-hospital data, and the staff of each emergency hospital can correct them if necessary. Through these tasks, cellphone app data, ambulance records, and the in-hospital data such as diagnosis and prognosis can be comprehensively registered for each patient transported by an ambulance. The registered data is cleaned by the Working Group to analyze the emergency medical care system in Osaka Prefecture (17). Among the collected and cleaned data, we excluded inconsistent data that did not contain all of the cellphone app data, ambulance records, and in-hospital data such as diagnosis and prognosis. In addition, we also excluded patients whose sex as registered by the fire department did not match that registered by the hospital or whose sex was missing. We also excluded patients whose age input by the fire department and that by the hospital differed by 3 years or more. When this difference was present, we defined the age input by the hospital as the patient’s true age.
Endpoints
The primary endpoints of this study were the number of patients transported by ambulance and the number of deaths among these patients for each month. These endpoints were calculated using the ORION dataset. In addition, the principal diagnoses of the patients who died were classified according to the ICD-10.
Statistical analysis
Firstly, we revealed patient characteristics as descriptive study. Categorical variables were described by real numbers and percentages, while continuous variables were described by medians and interquartile range (IQR). Age groups were categorized as children (0–14 years), adults (15–64 years), and older adults (65 years and older). The reasons for the ambulance call were divided into “fire accident,” “natural disaster,” “water accident,” “traffic accident involving car, ship, or aircraft,” “injury, poisoning, and disease due to industrial accident,” “disease and injury due to sports,” “other injury,” “trauma due to assault,” “acute disease,” “interhospital transport” and “other.”
Secondary, to assess the impact of the COVID-19 pandemic on the EMS system, the incidence rate ratio (IRR) and 95% confidence interval (CI) were calculated using 2019 as the reference year. Next, the number of the dead among these patients by reason for the ambulance call for each month of the above years was calculated, and the IRR and 95% CI were calculated in the same way. The IRR was calculated based on the population of Osaka Prefecture determined by the census in 2020 (11). Mortalities were evaluated based on deaths in the emergency department and deaths at 21 days after hospitalization.
In addition, IRRs and 95% CIs were calculated for subgroup analysis limited to patients who called for an ambulance because of “acute disease.” The age groups were classified as children (0–19 years), adults (20–64 years), and older adults (65 years and older). As in the main analysis, the number of the dead among these patients was calculated on a monthly basis, and the IRR and 95% CI were calculated in the same way. Finally, the odds ratios (ORs) and 95% CIs were calculated to evaluate the percentage of mortality by reason for ambulance call. Statistical analyses were implemented using STATA version 16.0MP (STAT Corp., College Station, TX, United States).
Results
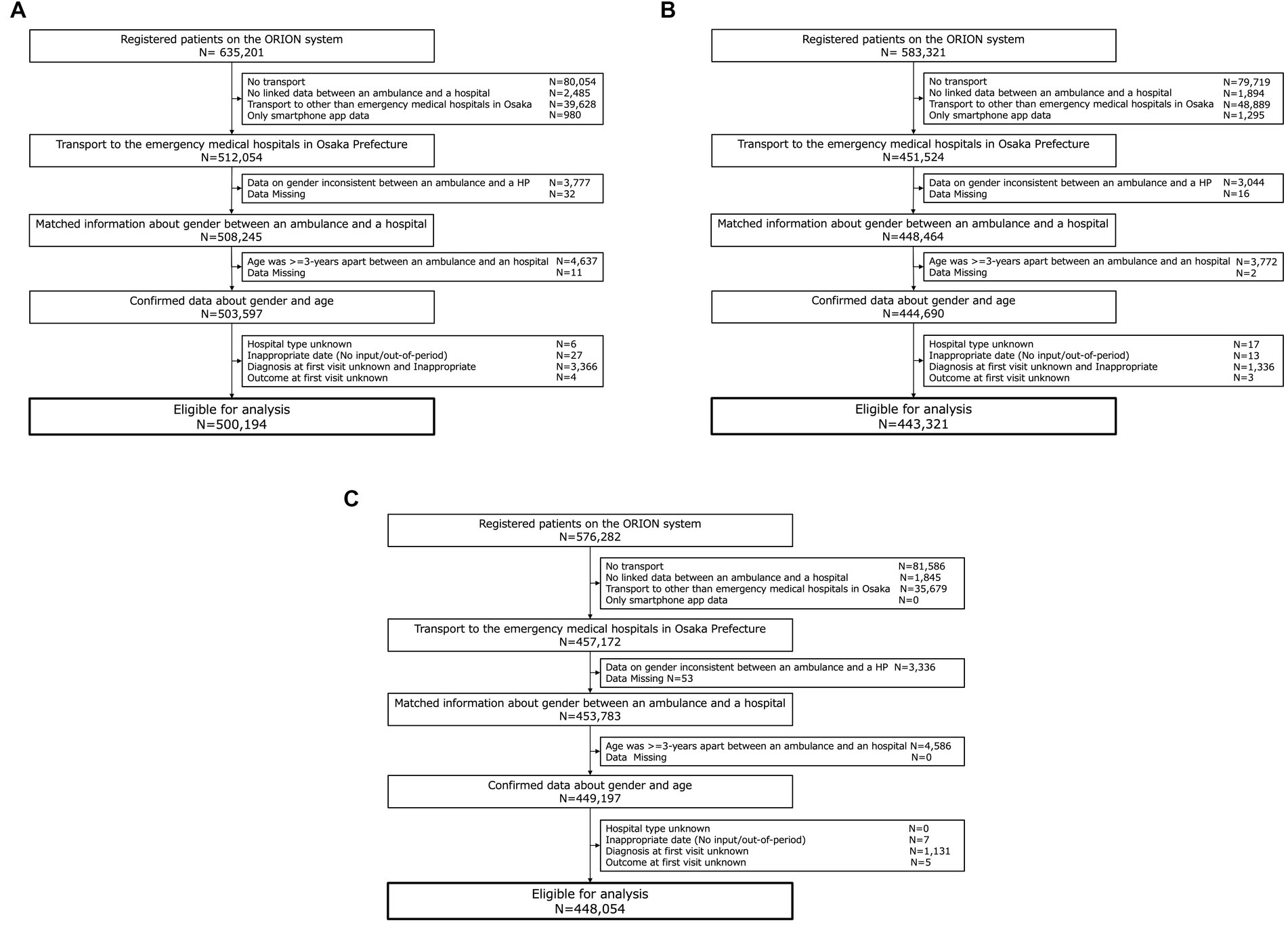
In this study, we included 1,381,581 data-cleaned patients who registered in the ORION system. Of these patients, 500,206 patients were in 2019, 443,321 patients were in 2020, and 448,054 patients were in 2021 (Figure 1). Figure 2 shows the incidence of COVID-19 patients in Osaka and the incidence of patients transported by ambulance during study periods.
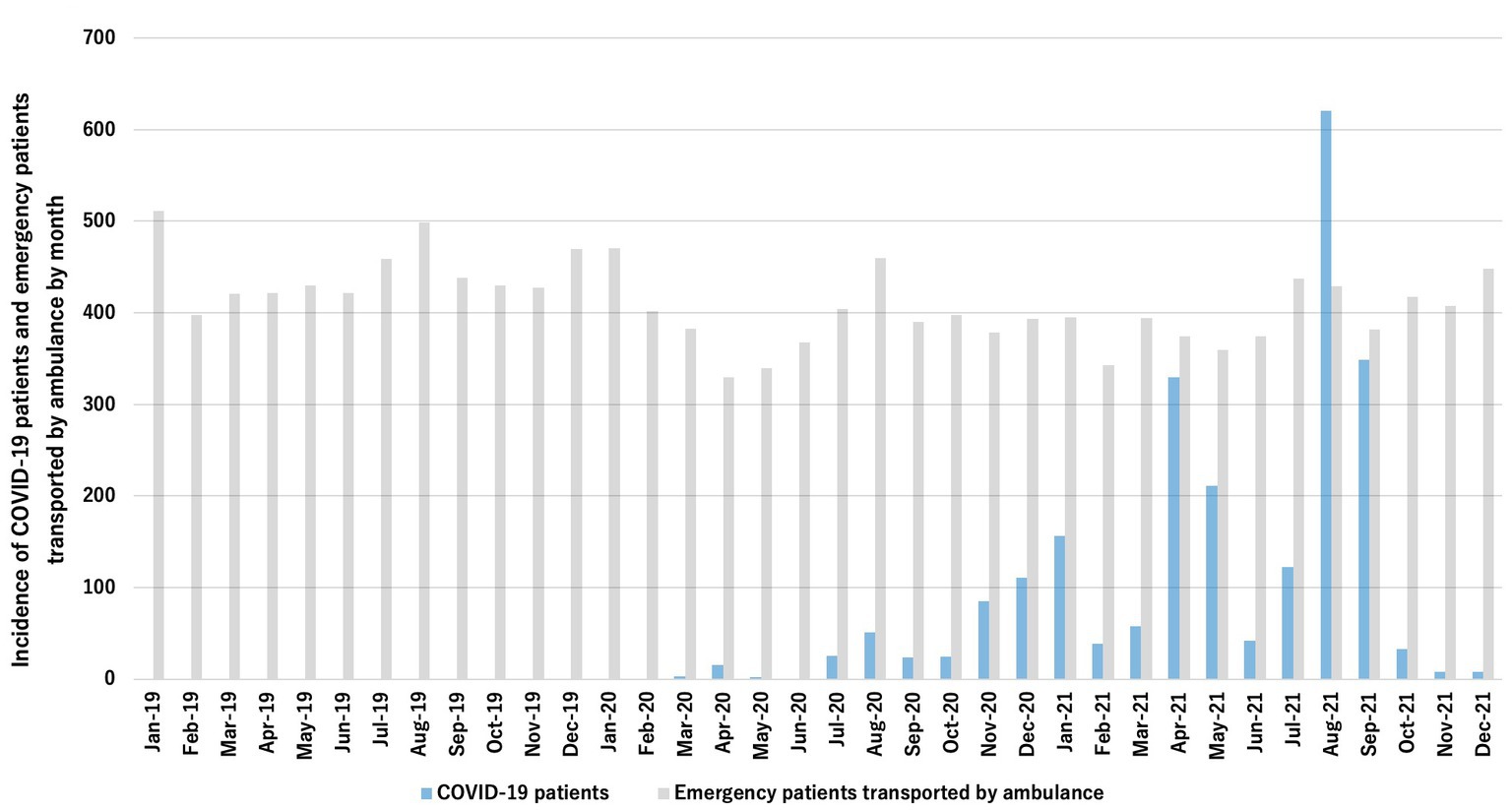
Figure 2. Incidence of emrgency patients transported by ambulance and COVID-19 patients per 100,000 residents.
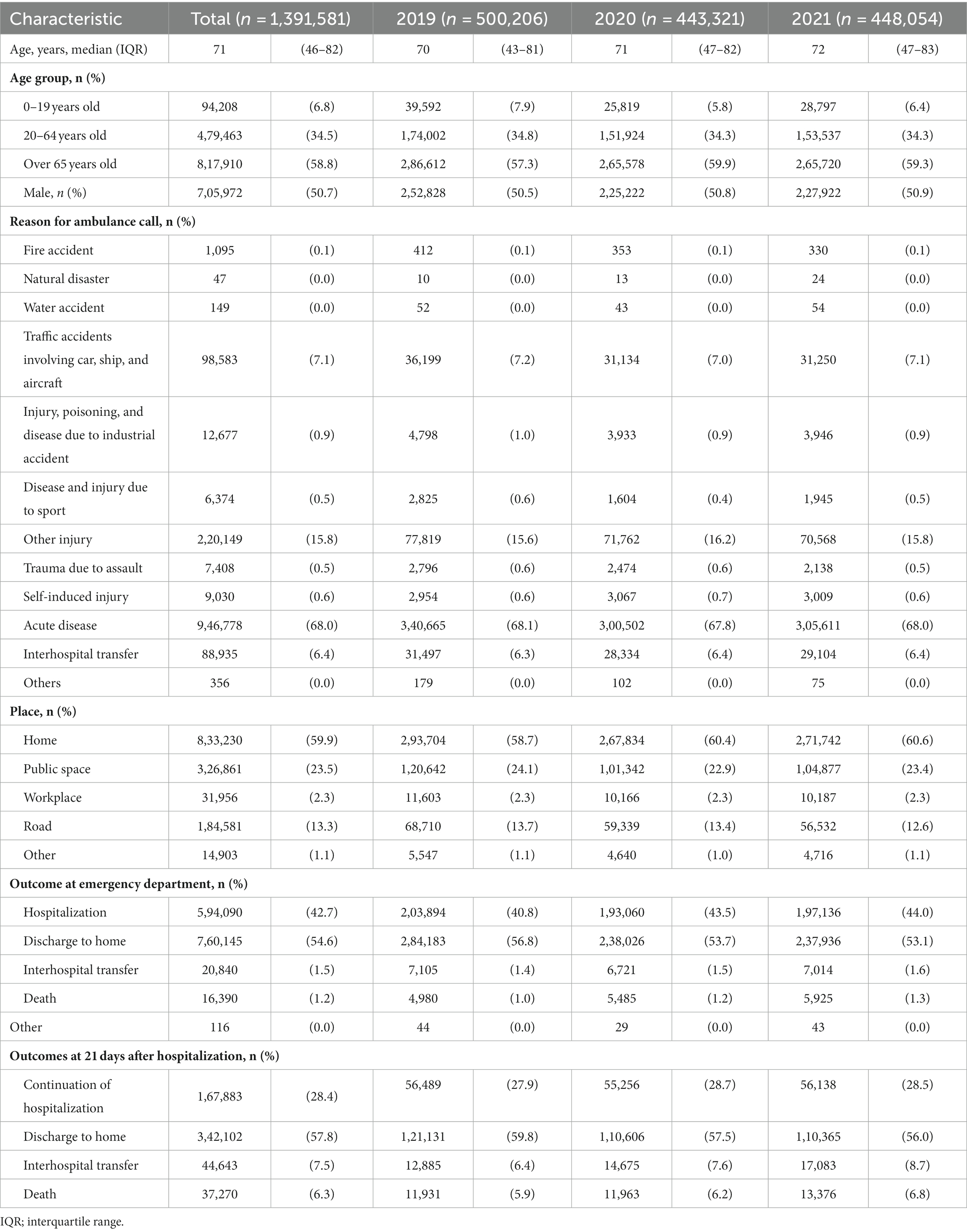
Table 1 shows the patient characteristics in this study. The median of age was 71 years [interquartile range (IQR): 46–82], and 705,972 patients (50.7%) were male. The most common reason for ambulance call was “acute disease” in 946, 778 patients (68.0%), followed by “other injury” (220,149, 15.8%) and “traffic accident” (98,583, 7.1%). The outcome of these patients at the emergency departments were hospitalization in 594,090 (42.7%), discharge home in 760,145 (54.6%), interhospital transfer in 20,840 (1.5%), and death in 16,390 (1.2%). Among the hospitalized patients, the outcomes at 21 days after hospitalization were 167,883 (28.4%) for continuation of hospitalization, 342,102(57.8%) for discharge home, 44,643 (7.5%) for interhospital transfer, and 37,270 (6.3%) for death.
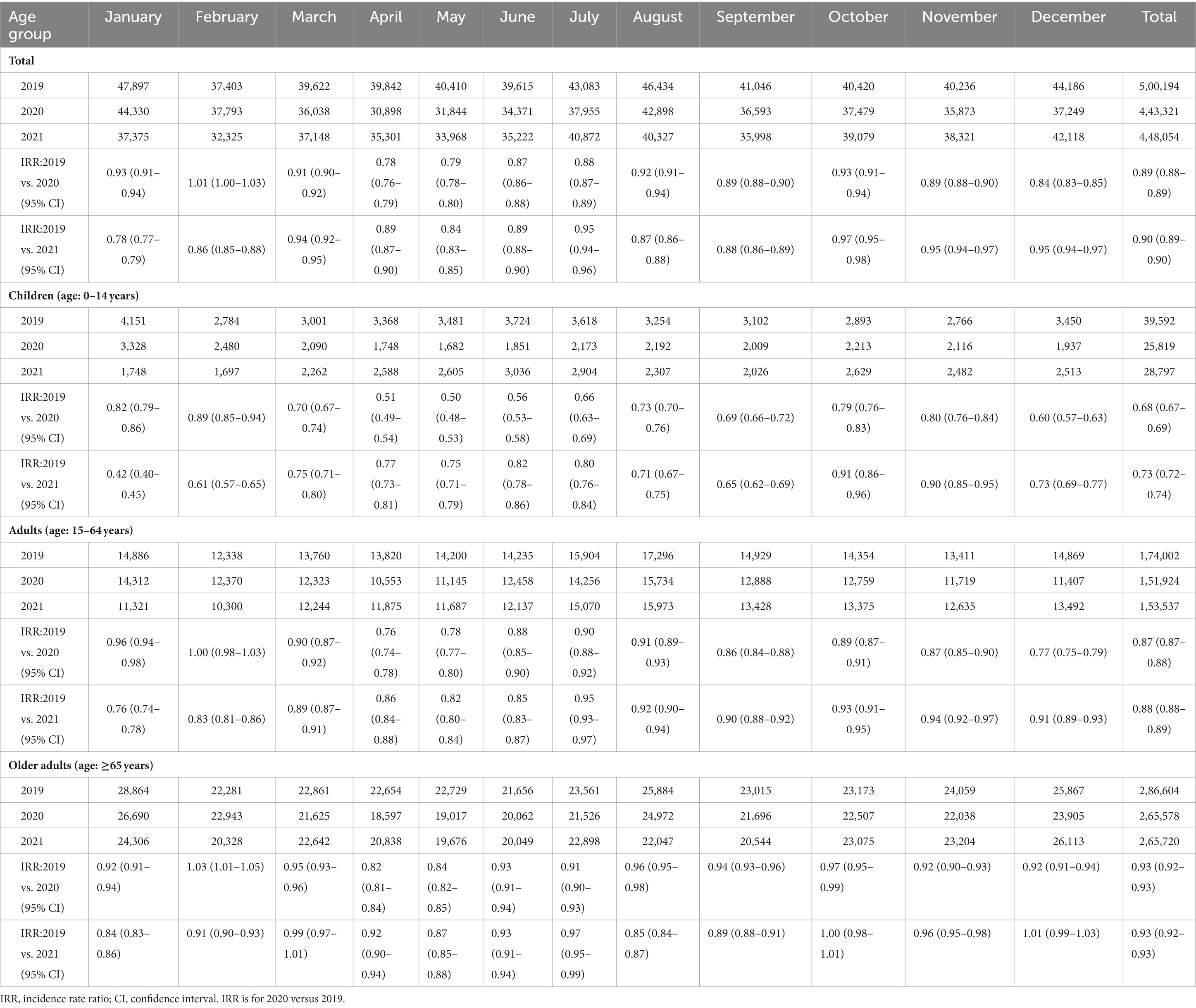
Table 2 shows the number of patients transported by ambulance in 2019, 2020, and 2021 by reason for ambulance call and IRRs and 95% CIs. The numbers of patients transported by ambulance were 500,194 in 2019, 443,321 in 2020 (IRR: 0.88, 95% CI: 0.87–0.88), and 448,054 in 2021 (IRR: 0.90, 95% CI: 0.89–0.90). The most common reason for an ambulance call in 2020, 2021, and 2019 was “acute disease,” with the following numbers: 340,655 in 2019, 300,502 in 2020, and 305,611 in 2021. The lowest IRR during the study period for reason for ambulance call was for “disease and injury due to sport” in both 2020 (IRR: 0.57, 95% CI: 0.53–0.60) and 2021 (IRR: 0.69, 95% CI: 0.65–0.73). In terms of the IRR for number of patients transported by ambulance by month, April had the lowest IRR in 2020 (IRR: 0.78, 95% CI: 0.76–0.79), and January had the lowest IRR in 2021 (IRR: 0.78, 95% CI: 0.77–0.79).
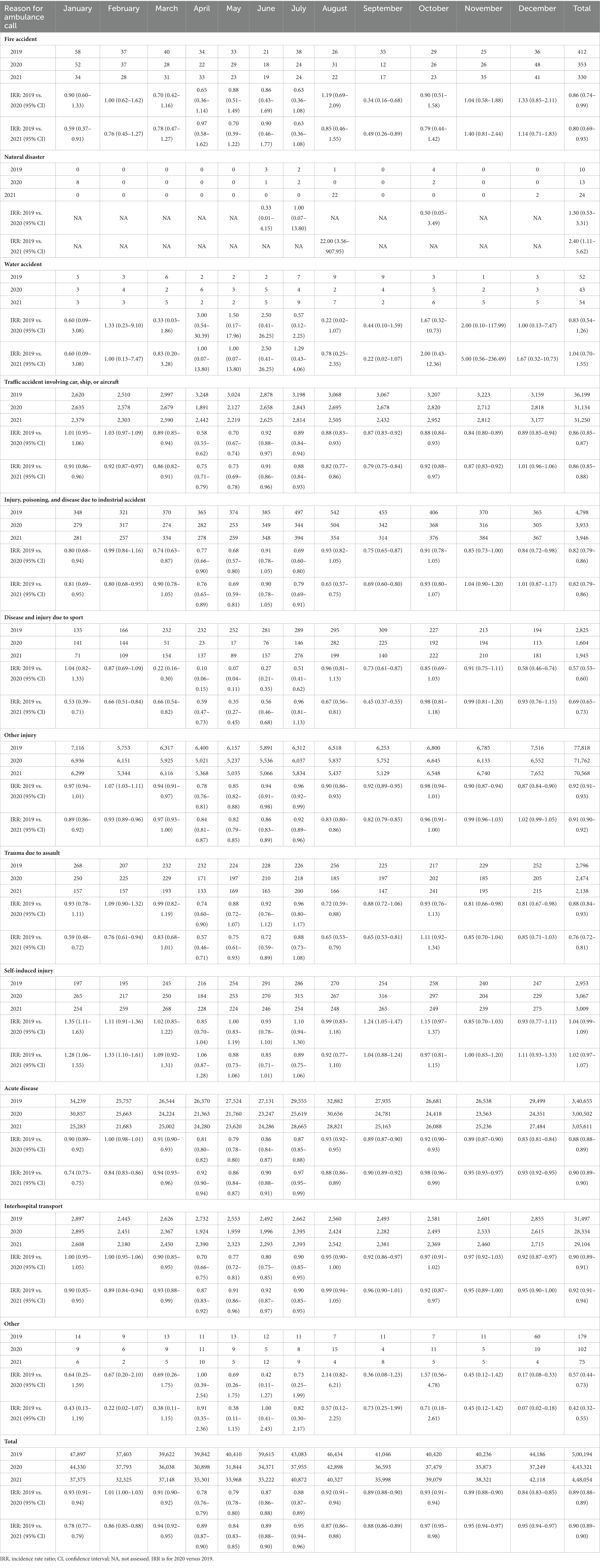
Table 2. Number of emergency patients registered in the Osaka emergency information research intelligent operation network system.
Table 3 shows the number of patients transported by ambulance, IRRs and 95% CIs by age group for each year. For children, the number of patients transported by ambulance decreased throughout the year in 2020 and 2021, with the lowest IRR in January 2021 (IRR: 0.42, 95% CI: 0.40–0.45). For adults, the IRRs were lowest in April 2020 (IRR: 0.76, 95% CI: 0.74–0.78) and January 2021 (IRR: 0.76, 95% CI: 0.74–0.78). Among older adults, the IRR was lowest in April 2020 (IRR: 0.84, 95% CI: 0.82–0.85), whereas the numbers of patients transported by ambulance in March 2021 (IRR: 0.99, 95% CI: 0.97–1.01), October 2021 (IRR: 1.00, 95% CI: 0.98–1.01), and December 2021 (IRR: 1.01, 95% CI: 0.99–1.03) were similar to those in 2019 before the COVID-19 pandemic.
Table 4 shows the number of patients who were transported by ambulance and died in the emergency departments for each year. In 2019, the number was 4,980, compared to 5,485 in 2020 (IRR: 1.10, 95% CI: 1.06–1.44) and 5,925 in 2021 (IRR: 1.19, 95% CI: 1.15–1.24). In 2020, August had the highest IRR (IRR: 1.34, 95% CI: 1.16–1.54) and in 2021, May had the highest IRR (IRR: 1.46, 95% CI: 1.27–1.67).
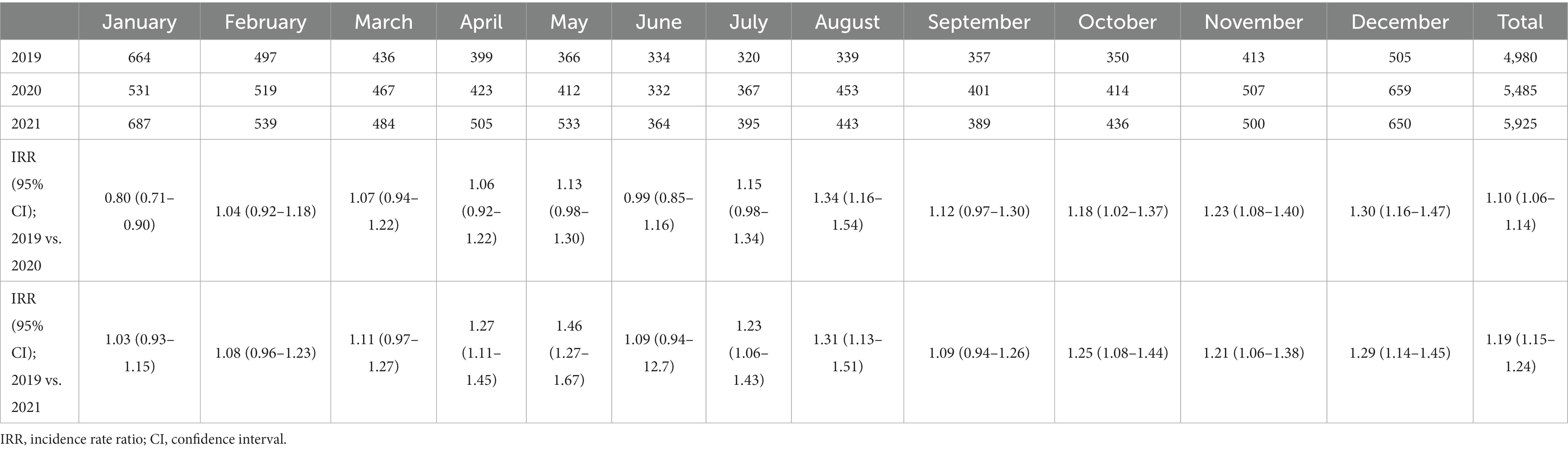
Table 4. Number of deaths in the emergency department after hospital arrival registered in the ORION system.
Table 5 shows the number of patients who died within 21 days after hospitalization and the IRR for each year. In 2019, the number was 11,931, compared to 11,963 in 2020 (IRR: 1.00, 95% CI: 0.98–1.03) and 13,376 in 2021 (IRR: 1.12, 95% CI: 1.09–1.15). In the analysis by month, the number of dead patients did not increase or decrease in 2020, whereas in 2021, the number increased in March (IRR: 1.12, 95% CI: 1.03–1.22), April (IRR: 1.37, 95% CI: 1.26–1.49), May (IRR: 1.29, 95% CI: 1.18–1.41), August (IRR: 1.21, 95% CI: 1.11–1.33), and October (IRR: 1.12, 95% CI: 1.02–1.22). There were no reasons for ambulance calls that showed a statically significant impact between 2019 and 2020, and no statistically significant differences were identified between 2019 and 2020.
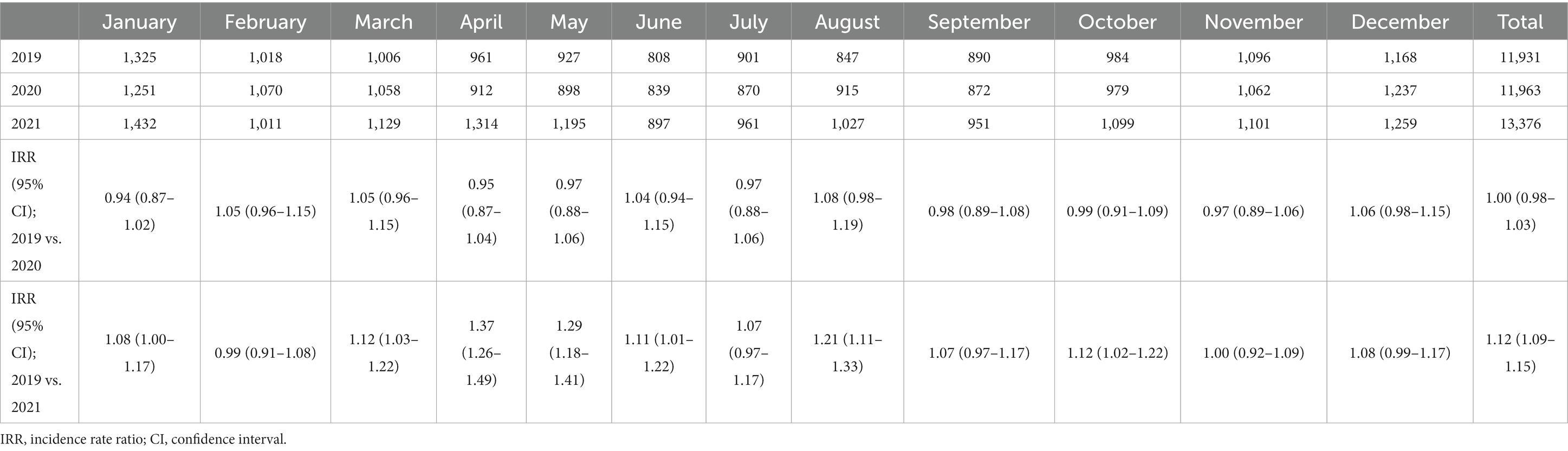
Table 5. Number of deaths among hospitalized patients in the emergency department after hospital arrival registered in the ORION system.
Table 6 shows the number of deaths in the emergency department by reason for ambulance call. Mortality increased statistically for “acute disease,” from 1.2% (4,166/340,665) in 2019 to 1.5% (4,615/300,502, OR: 1.26, 95% CI: 1.21–1.31) in 2020 and 1.7% (5,049/305,611, OR: 1.36, 95% CI: 1.30–1.41) in 2021. As well, mortality increased statistically for “fire accident,” from 3.9% (16/412) in 2019 to 8.2% (27/330, OR 2.21, 95% CI: 1.12–4.46) in 2021.
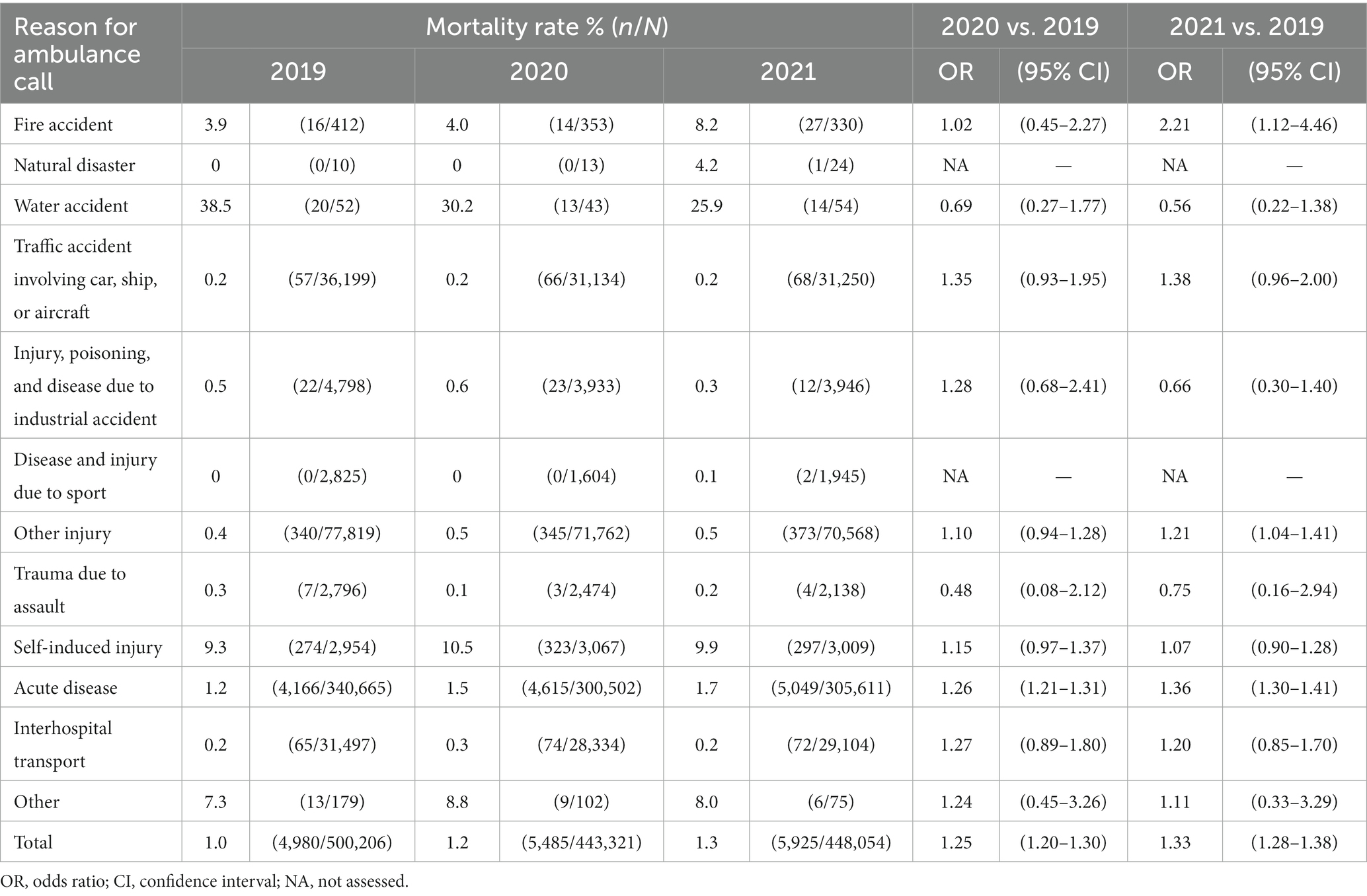
Table 6. Proportion of deaths in the emergency department registered in the ORION system during the study period.
Table 7 shows the number of deaths within 21 days after hospitalization by reason for ambulance call. Mortality increased statistically for “acute disease” and “interhospital transport.” In patients with ambulance calls for “acute disease,” the morality rates were 6.9% (9,827/142,147) in 2019, 7.3% (9,856/135,151, OR: 1.06, 95% CI: 1.03–1.09) in 2020, and 7.9% (11,067/139,757, OR: 1.16, 95% CI: 1.13–1.19). In patients with ambulance calls for “interhospital transport,” the morality rates were 4.7% (1,215/25,884) in 2019, 5.4% (1,300/24,102, OR: 1.16, 95% CI: 1.07–1.26) in 2020, and 5.8% (1,398/23,938, OR: 1.21, 95% CI: 1.11–1.31).
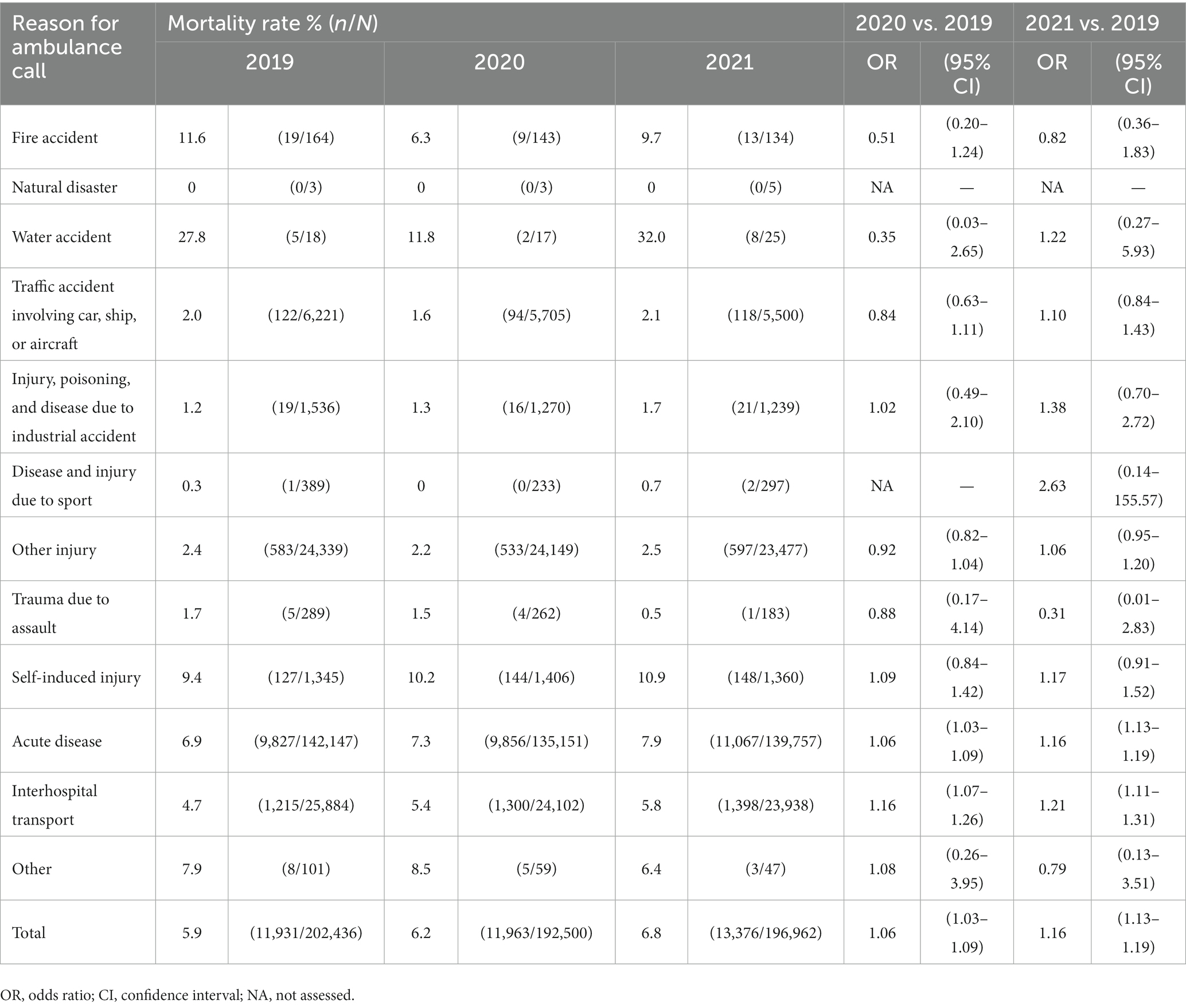
Table 7. Number of deaths among hospitalized patients registered in the ORION system during the study period.
Discussion
This study revealed the outcomes of patients transported by ambulance in Osaka Prefecture from 2019 to 2021. The number of patients transported by ambulance decreased in 2020 and also in 2021 compared to 2019. However, the number of deaths among patients transported by ambulance in 2020 was the same as that in 2019, whereas not only deaths in the emergency department but also deaths among patients transported by ambulances after hospitalization increased in 2021. This population-based descriptive study of the impact of the COVID-19 pandemic will be useful for planning health care systems and policies.
The number of patients transported by ambulance in 2021 was about the same as that in 2020 and was decreased compared to that in the pre-pandemic period. In particular, the number of the patients transported due to traffic accidents and industrial accidents decreased, whereas that of the patients transported due to sports increased slightly. This trend was also observed in other countries (19–26). A study in northwestern Italy reported a decrease in emergency room visits due to the COVID-19 pandemic but an increase in emergency room visits by ambulance (25). A study by Bosson et al. assessing the relationship between hospital admission due to COVID-19 and EMS transports for time-sensitive emergencies in Los Angeles revealed that the number of patients transported by ambulance for traffic accidents decreased during the COVID-19 pandemic, whereas the number of patients transported by ambulance for stroke, ST-segment elevation myocardial infarction, and OHCA increased (24). Thus, the number of these patients may have decreased during the COVID-19 pandemic due to the restriction of socioeconomic activities caused by the lockdown (24). Furthermore, the number of patients transported by ambulance for acute diseases also decreased in 2021 compared to the pre-COVID-19 pandemic period. The impact of the COVID-19 pandemic on changes in patient behavior has been reported in various ways (27, 28). In France, the COVID-19 pandemic reduced initiation of treatment with cardiovascular and antidiabetic drugs (27). In Japan, the COVID-19 pandemic reduced outpatient visits for epilepsy, Parkinson’s disease, and Alzheimer’s disease slightly but significantly in April 2020 (28). This study also found that the COVID-19 pandemic changed patient behavior, such as calling for an ambulance, and that it had not returned to pre-COVID-19 pandemic levels in 2021. The COVID-19 vaccination coverage in Japan was 80% in 2021, and the effect of preventive measures against COVID-19, such as vaccine dissemination, remains clear. We will continue to evaluate changes in patient behavior, such as for ambulance calls, as vaccination coverage increases.
The mortality of patients transported by ambulance in 2020 compared to 2019 did not change, but mortality in 2021 increased. Several studies have reported that patient outcomes were affected by the COVID-19 pandemic (29–31). Surek et al. (29) found that hospitalizations for acute cholecystitis and uncomplicated appendicitis were markedly reduced during the COVID-19 pandemic, whereas hospitalizations for complicated appendicitis and acute mechanical intestinal obstruction increased, as did the mortality from emergency surgery. A study of OHCA in South Korea found that the time from arrival at the scene to the start of resuscitation activities and transport time were prolonged by the need to secure isolation wards and by the increased requirement for personal protective equipment in the prehospital situation (31). In Japan, bystander cardio-pulmonary resuscitation for OHCA patients decreased during the COVID-19 pandemic (30). Thus, factors such as delays in patient access to medical care, decreased treatment performance due to the wearing of infection protection equipment by healthcare workers, and lower rates of prehospital first aid may have affected patient outcomes. These factors were brought about by the need to prevent COVID-19 infection, and widespread use of vaccine may ameliorate these factors. Therefore, we intend to evaluate these effects in the future.
There are several limitations in this study. First, we analyzed IRR on a population basis and did not adjust for various confounding factors. Second, the ORION registry registered patient data from all fire departments and medical institutions only in Osaka Prefecture, so the prognosis of patients transported to medical institutions outside of Osaka Prefecture was not known. Third, we utilized data from a particular region in Japan, which may not be widely applicable elsewhere due to variations in COVID-19 infection rates and insurance systems across different nations. Finally, as this is an observational study, there may be unknown confounding factors.
In conclusion, the COVID-19 pandemic decreased the number of ambulance requests and increased the mortality of patients transported by ambulance in Osaka Prefecture during 2021. The EMS system may have been affected by an increase in special demands, such as the pandemic of infectious diseases.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: data cannot be shared publicly because of the Protection Ordinance for Personal Information in Osaka Prefecture. Requests to access these datasets should be directed to YK, b3Jpb24xM0BocC1lbWVyZy5tZWQub3Nha2EtdS5hYy5qcA==.
Author contributions
YK: Conceptualization, Writing – original draft, Data curation, Investigation, Methodology, Project administration, Resources, Visualization, Writing – review & editing. KT: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Software, Visualization, Writing – review & editing. HD: Conceptualization, Methodology, Resources, Writing – review & editing. JM: Conceptualization, Data curation, Methodology, Resources, Writing – review & editing. SN: Conceptualization, Data curation, Resources, Writing – review & editing. JT: Conceptualization, Data curation, Methodology, Resources, Writing – review & editing. TH: Conceptualization, Data curation, Resources, Writing – review & editing. TK: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Software, Validation, Writing – original draft, Writing – review & editing. JO: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Writing – review & editing. TM: Conceptualization, Data curation, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Fire and Disaster Prevention Technologies Program (Grant No. 21584490). The funder of this study had no role in study design, data collection, analyses, and interpretation of data, or writing and submission of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Huang, C, Wang, Y, Li, X, Ren, L, Zhao, J, Hu, Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
2. Götzinger, F, Santiago-García, B, Noguera-Julián, A, Lanaspa, M, Lancella, L, Calò Carducci, FI, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. (2020) 4:653–61. doi: 10.1016/S2352-4642(20)30177-2
3. Wang, C, Horby, PW, Hayden, FG, and Gao, GF. A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. doi: 10.1016/S0140-6736(20)30185-9
4. Piroth, L, Cottenet, J, Mariet, AS, Bonniaud, P, Blot, M, Tubert-Bitter, P, et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respir Med. (2020) 9:251–9. doi: 10.1016/S2213-2600(20)30527-0
5. Swann, OV, Holden, KA, Turtle, L, Pollock, L, Fairfield, CJ, Drake, TM, et al. Clinical characteristics of children and young people admitted to hospital with COVID-19 in United Kingdom: prospective multicentre observational cohort study. BMJ. (2020) 370:m3249. doi: 10.1136/bmj.m3249
6. Suleyman, G, Fadel, RA, Malette, KM, Hammond, C, Abdulla, H, Entz, A, et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit. JAMA Netw Open. (2020) 3:e2012270. doi: 10.1001/jamanetworkopen.2020.12270
7. Wu, Z, and McGoogan, JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
8. Ministry of Health, Labour and Welfare. The open datasets of patients with novel coronavirus. Available at: (Accessed February 5, 2023). (in Japanese https://www.mhlw.go.jp/stf/covid-19/open-data.html)
9. Takeuchi, T, Imanaka, T, Katayama, Y, Kitamura, T, Sobue, T, and Shimazu, T. Profile of patients with novel coronavirus disease 2019 (COVID-19) in Osaka refecture, Japan: a population-based descriptive study. J Clin Med. (2020) 9:2925. doi: 10.3390/jcm9092925
10. Osaka Prefectural Government. The census of Osaka Prefecture in 2020. Available at: (Accessed February 5, 2023). (in Japanese) https://www.pref.osaka.lg.jp/attach/42622/00426107/R2kokutyo_osakahu_kakuhou_toukeihyo.pdf
11. Osaka Prefectural Government. The latest infection trend of COVID-19 in Osaka Prefecture. Available at: (Accessed February 5, 2023). (in Japanese) https://covid19-osaka.info
12. Osaka Prefectural Government. The 7th medical plan in Osaka Prefecture, emergency medical section. Available at: (Accessed February 5, 2023). (in Japanese) https://www.pref.osaka.lg.jp/attach/2502/00281086/0606.pdf
13. Katayama, Y, Tanaka, K, Kitamura, T, Takeuchi, T, Nakao, S, Nitta, M, et al. Incidence and mortality of emergency patients transported by emergency medical service personnel during the novel corona virus pandemic in Osaka Prefecture, Japan: a population-based study. J Clin Med. (2021) 10:5662. doi: 10.3390/jcm10235662
14. Katayama, Y, Kiyohara, K, Kitamura, T, Hayashida, S, and Shimazu, T. Influence of the COVID-19 pandemic on an emergency medical service system: a population-based, descriptive study in Osaka, Japan. Acute Med Surg. (2020) 7:e534. doi: 10.1002/ams2.534
15. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, and Vandenbroucke, JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. (2007) 370:1453–7. doi: 10.1016/S0140-6736(07)61602-X
16. Osaka Prefectural Government. Medical facility survey in Osaka. Available at: (Accessed February 12, 2023). (in Japanese) https://www.pref.osaka.lg.jp/kenisomu/syuyoufukusidate/hoken1-0.html
17. Okamoto, J, Katayama, Y, Kitamura, T, Sado, J, Nakamura, R, Kimura, N, et al. Profile of the ORION (Osaka emergency information research intelligent operation network system) between 2015 and 2016 in Osaka, Japan: a population-based registry of emergency patients with both ambulance and in-hospital records. Acute Med Surg. (2019) 6:12–24. doi: 10.1002/ams2.371
18. Katayama, Y, Kitamura, T, Kiyohara, K, Iwami, T, Kawamura, T, Izawa, J, et al. Improvements in patient acceptance by hospitals following the introduction of a smartphone app for the emergency medical service system: a population-based before-and-after observational study in Osaka City, Japan. JMIR Mhealth Uhealth. (2017) 5:e134. doi: 10.2196/mhealth.8296
19. Perlini, S, Canevari, F, Cortesi, S, Sgromo, V, Brancaglione, A, Contri, E, et al. Emergency department and out-of-hospital emergency system (112-AREU 118) integrated response to coronavirus disease 2019 in a northern Italy centre. Intern Emerg Med. (2020) 15:825–33. doi: 10.1007/s11739-020-02390-4
20. Fagoni, N, Perone, G, Villa, GF, Celi, S, Bera, P, Sechi, GM, et al. The Lombardy emergency medical system faced with COVID-19: the impact of out-of-hospital outbreak. Prehosp Emerg Care. (2021) 25:1–7. doi: 10.1080/10903127.2020.1824051
21. Spina, S, Marrazzo, F, Migliari, M, Stucchi, R, Sforza, A, and Fumagalli, R. The response of Milan’s emergency medical system to the COVID-19 outbreak in Italy. Lancet. (2020) 395:e49–50. doi: 10.1016/S0140-6736(20)30493-1
22. Saberian, P, Conovaloff, JL, Vahidi, E, Hasani-Sharamin, P, and Kolivand, PH. How the COVID-19 epidemic affected prehospital emergency medical services in Tehran. Iran West J Emerg Med. (2020) 21:110–6. doi: 10.5811/westjem.2020.8.48679
23. Stella, F, Alexopoulos, C, Scquizzato, T, and Zorzi, A. Impact of the COVID-19 outbreak on emergency medical system missions and emergency department visits in the Venice area. Eur J Emerg Med. (2020) 27:298–300. doi: 10.1097/MEJ.0000000000000724
24. Bosson, N, Rollman, JE, Kloner, RA, Shavelle, DM, Saver, JL, Niemann, JT, et al. The correlation between COVID-19 hospitalizations and emergency medical services responses for time-sensitive emergencies during the COVID-19 pandemic. Prehosp Emerg Care. (2023) 27:321–7. doi: 10.1080/10903127.2022.2112792
25. Bardin, A, Buja, A, Barbiellini Amidei, C, Paganini, M, Favaro, A, Saia, M, et al. Elderly people's access to emergency departments during the COVID-19 pandemic: results from a large population-based study in Italy. J Clin Med. (2021) 10:5563. doi: 10.3390/jcm10235563
26. Janke, AT, Jain, S, Hwang, U, Rosenberg, M, Biese, K, Schneider, S, et al. Emergency department visits for emergent conditions among older adults during the COVID-19 pandemic. J Am Geriatr Soc. (2021) 69:1713–21. doi: 10.1111/jgs.17227
27. Mathieu, C, Pambrun, E, Bénard-Laribière, A, Noize, P, Faillie, JL, Bezin, J, et al. Impact of the COVID-19 pandemic and its control measures on cardiovascular and antidiabetic drugs use in France in 2020: a nationwide repeated cohort study. Eur J Epidemiol. (2022) 37:1049–59. doi: 10.1007/s10654-022-00912-2
28. Sato, K, Mano, T, Niimi, Y, Iwata, A, Toda, T, and Iwatsubo, T. The impact of COVID-19 pandemic on the utilization of ambulatory care for patients with chronic neurological diseases in Japan: evaluation of an administrative claims database. Biosci Trends. (2021) 15:219–30. doi: 10.5582/bst.2021.01194
29. Surek, A, Ferahman, S, Gemici, E, Dural, AC, Donmez, T, and Karabulut, M. Effects of COVID-19 pandemic on general surgical emergencies: are some emergencies really urgent? Level 1 trauma center experience. Eur J Trauma Emerg Surg. (2021) 47:647–52. doi: 10.1007/s00068-020-01534-7
30. Nishiyama, C, Kiyohara, K, Iwami, T, Hayashida, S, Kiguchi, T, Matsuyama, T, et al. Influence of COVID-19 pandemic on bystander interventions, emergency medical service activities, and patient outcomes in out-of-hospital cardiac arrest in Osaka City, Japan. Resusc Plus. (2021) 5:100088. doi: 10.1016/j.resplu.2021.100088
Keywords: COVID-19, pandemic, emergency medicine, EMS system, public health, epidemiology
Citation: Katayama Y, Tanaka K, Domi H, Masui J, Nakao S, Tachino J, Hirose T, Kitamura T, Oda J and Matsuoka T (2024) Outcome of emergency patients transported by ambulance during the COVID-19 pandemic in Osaka Prefecture, Japan: a population-based descriptive study. Front. Public Health. 11:1322236. doi: 10.3389/fpubh.2023.1322236
Edited by:
Ozgur Karcioglu, Taksim Training and Research Hospital, Beyoglu, TürkiyeReviewed by:
Roberto Primi, San Matteo Hospital Foundation (IRCCS), ItalyEduardo Gutiérrez-Abejón, Universidad de Valladolid, Spain
Copyright © 2024 Katayama, Tanaka, Domi, Masui, Nakao, Tachino, Hirose, Kitamura, Oda and Matsuoka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yusuke Katayama, b3Jpb24xM0BocC1lbWVyZy5tZWQub3Nha2EtdS5hYy5qcA==
 Yusuke Katayama
Yusuke Katayama Kenta Tanaka3
Kenta Tanaka3 Jotaro Tachino
Jotaro Tachino Tetsuhisa Kitamura
Tetsuhisa Kitamura Jun Oda
Jun Oda