- 1University of Waikato, Hamilton, New Zealand
- 2School of Tourism Management, Sun Yat-sen University, Zhuhai, Guangdong, China
- 3Key Laboratory of Sustainable Tourism Smart Assessment Technology, Ministry of Culture and Tourism of China, Zhuhai, Guangdong, China
- 4Rauawaawa Kaumātua Charitable Trust, Hamilton, New Zealand
- 5Te Runanga o Ngati Manawa, Murupara, New Zealand
- 6Te Hiku Hauora, Kaitaia, New Zealand
- 7Turanga Health, Gisborne, New Zealand
- 8Te Matawai, Wellington, New Zealand
- 9Massey University, Palmerston North, New Zealand
- 10Auckland University of Technology, Auckland, New Zealand
- 11University of Otago, Dunedin, New Zealand
- 12University of Queensland, Brisbane, QLD, Australia
Background: The study offers baseline data for a strengths-based approach emphasizing intergenerational cultural knowledge exchange and physical activity developed through a partnership with kaumātua (Māori elders) and kaumātua service providers. The study aims to identify the baseline characteristics, along with correlates of five key outcomes.
Methods: The study design is a cross-sectional survey. A total of 75 kaumātua from six providers completed two physical functioning tests and a survey that included dependent variables based in a holistic model of health: health-related quality of life (HRQOL), self-rated health, spirituality, life satisfaction, and loneliness.
Results: The findings indicate that there was good reliability and moderate scores on most variables. Specific correlates included the following: (a) HRQOL: emotional support (β = 0.31), and frequent interaction with a co-participant (β = 0.25); (b) self-rated health: frequency of moderate exercise (β = 0.32) and sense of purpose (β = 0.27); (c) spirituality: sense of purpose (β = 0.46), not needing additional help with daily tasks (β = 0.28), and level of confidence with cultural practices (β = 0.20); (d) life satisfaction: sense of purpose (β = 0.57), frequency of interaction with a co-participant (β = −0.30), emotional support (β = 0.25), and quality of relationship with a co-participant (β = 0.16); and (e) lower loneliness: emotional support (β = 0.27), enjoyment interacting with a co-participant (β = 0.25), sense of purpose (β = 0.24), not needing additional help with daily tasks (β = 0.28), and frequency of moderate exercise (β = 0.18).
Conclusion: This study provides the baseline scores and correlates of important social and health outcomes for the He Huarahi Tautoko (Avenue of Support) programme, a strengths-based approach for enhancing cultural connection and physical activity.
Introduction
As the Indigenous peoples of Aotearoa New Zealand (Aotearoa), Māori comprise 17% of the population and 7% of this total are 65 and older (1). Māori face significant and stark social and health inequities relative to non-Māori populations in Aotearoa New Zealand (2, 3). For example, Māori have a life expectancy that is seven years lower than other New Zealanders and yet the major causes of mortality are preventable and treatable (4). Further, “Māori experience systematic disparities in health outcomes, determinants of health, health system responsiveness, and representation in the health sector workforce” (p. 10) (5). These health and social inequities are heightened for kaumātua (elders) who also face additional challenges including social isolation and loneliness, end-of-life concerns, and chronic health conditions (6, 7).
These health and social inequities have not decreased over the last 50 years and are largely explained by a variety of structural determinants (8). These include inequalities in social determinants (e.g., housing, income, and education), institutional discrimination from the effects of colonization, and insufficient access to health services (4, 9, 10). A key component of the explanatory factors is Te Tiriti o Waitangi (Treaty of Waitangi), which is the written agreement for the founding of Aotearoa. It is a disputed document that has different versions in English and Māori, but guaranteed Māori rights. Historically, the Treaty was not followed until 1975 with the Treaty of Waitangi Act (8). More recently, Te Tiriti has five principles: (a) Recognition and protection of tino rangatiratanga (self-determination); (b) Equity—equal access to health care and equitable outcomes; (c) Active protection—governmental protection of the first two principles; (d) Partnership—government partnering with Māori; and (e) Options—providing options for services that are grounded in te Ao Māori (Māori worldview) (2).
Today's kaumātua grew up prior to the Treaty of Waitangi Act and lived in a society that was more racist than in present and were affected by an education system that banned and punished people for embracing tikanga Māori (cultural protocols) and speaking Te Reo Māori (language) (11, 12). This colonial historical trauma contributed to health inequities through cultural dissonance or feeling of separation from their own culture (13–15). Further, kaumātua have not been recognized for their contributions to a dominant society even while Māori culture upholds elders as, “carriers of culture, anchors for families, models for lifestyle, bridges to the future, guardians of heritage, and role models for younger generations” (p. 14) (16).
The treaty principles, colonial history, and existing inequities are reasons why numerous researchers have found a need and advocate for services and programmes that are culturally appropriate and safe and that address structural determinants and structural change (7, 17, 18). However, much of the predominant narrative and specific actions to alleviate inequities are grounded in a deficit approach (19–21). The deficit approach emphasizes Indigenous communities as ‘difficulties' to be fixed relative to mainstream populations. The deficit-model approach sometimes blames Māori for the challenges they face and does not consider structural and systemic elements including loss of cultural connection resulting from colonization (8, 22, 23).
In contrast, this study offers a strength-based approach grounded in tikanga Māori and Te Ao Māori to guide solutions and this particular research. Specifically, the study focuses on kaumātua mana motuhake (actualization, autonomy, and independence) at an individual and collective level (24). He Huaraki Tautoko (Avenue of Support) is a collaboratively developed programme about intergenerational cultural knowledge exchange that also involves physical activity (24). Physical activity is correlated with various health benefits for older adults, from improved mental wellbeing (25), to a reduction in morbidity, mortality and falls (26). Particular physical activities can also be a means of strengthening cultural connection among Māori (27), while cultural activities and practices can be a driver that leads to “incidental” physical activity (28). He Huarahi Tautoko was constructed by researchers and six community providers along with their kaumātua through a participatory process. It is based on kaumātua as carriers of mātauranga (Māori knowledge systems) and involved sharing with each other along with a member of their whānau (extended family) through wānanga (learning sessions). The mātauranga included Te Reo Māori, whakapapa (genealogy), purākau (Māori lore), waiata (songs), and karakia (prayers). This cultural knowledge was selected as there is a link between cultural continuity and positive health outcomes (29–31), especially in the context of kaumātua who have a history of cultural dissonance due to colonial policies and practices. Further, this exchange of mātauranga was grounded in physical activities such as walks to significant cultural landmarks, gardening (e.g., traditional food preparation), and other cultural practices (dancing, cleaning the marae or community meeting house). Physical activity was important to enhance physical functioning and mental wellbeing. This project is a component of the Kaumātua Mana Motuhake Poi (KMMP) programme funded by the Aging Well National Science Challenge (https://www.ageingwellchallenge.co.nz/) (24).
The cultural knowledge and physical elements are important as part of a holistic model of health important for Māori communities. There are various models of Māori health that focus on a holistic perspective with perhaps the most popular being te whare tapa whā (four walls of a house) (13, 32). Te whare tapa whā was chosen by this research partnership to guide this project and includes four elements: te taha whānau, te taha hinengaro, te taha wairua, and te taha tinana (social, psychological/mental, spiritual and physical health respectively).
There are two aims of this study. The first aim is to present the baseline study from the He Huarahi Tautoko project to establish the initial comparison point and the psychometric characteristics for the measures. The second aim is to identify correlates for five outcomes related to te whare tapa whā and mana motuhake: health-related quality of life (HRQOL) and self-rated health for physical and mental wellbeing, loneliness for social health, spiritual wellbeing for spiritual health, and life satisfaction for mana motuhake. Examining the correlates of these health and wellbeing outcomes provides indicators for researchers and practitioners developing programmes and services to address health equity for kaumātua. They can also reinforce whether the He Huarahi Tautoko project is addressing key attributes.
Methods
The larger study has a mixed methods pre-test and two post-test, staggered design; four providers receive the programme initially and two providers receive it later (24). A cross-sectional survey for the baseline measures was the study design for this specific study. The research is grounded in Kaupapa Māori (33, 34) and a participatory research approach, He Pikinga Waiora [enhancing wellbeing (35)]. Kaupapa Māori emphasizes Te Ao Māori and tikanga (36), relies on self-determination and uses mātauranga Māori and Māori epistemology (37). He Pikinga Waiora centers Kaupapa Māori, while also including a partnership model amongst researchers and communities. A partnership of six Māori social-health service providers and university researchers from four universities comprised the research team. The project is registered with the Australia New Zealand Clinical Trial Registry (ACTRN12621000541808).
Participants
Participants were 75 kaumātua from six Māori social-health service providers across Aotearoa. We originally planned to identify a sampling frame and randomly sample participants from each provider. However, the initial planning was prior to the COVID pandemic, and we began the programme in between lockdowns for the pandemic. Kaumātua were hesitant to participate in group interactions post-lockdowns as they comprised one of the most impacted populations by the virus. Thus, the providers made the determination that they should invite all willing kaumātua to participate and it became a purposive sample. We had originally sought to recruit 15 kaumātua from each provider. Four were able to do this and two providers were only able to recruit eight and seven participants. There were 45 women and 16 men (14 did not specify) with an average age of 69.80 (SD = 7.26).
Measures
Measures were organized around our holistic models of hauora (health) and mana motuhake. For hauora, we included the following scales: self-reported health (38, 39), HRQOL (40, 41), spirituality (42), loneliness (two items from Waldergrave et al. (43) and one item from Hayman et al. (6)), perceived and desired social support (44), relationship quality with the person participating with them in the programme (45), cultural connection (29), cultural practices (10 items created for this study), self-reported exercise hours per week (46), and physical functioning (time to complete five chair stands and time to walk 3 meters) (47, 48). We also included life satisfaction (49) and sense of purpose (50) for mana motuhake. The measures included two different types of scales: (1) 11-point semantic differential scales and (2) Likert-type scales ranging from 3–6 points. The Appendix includes the items from the survey.
There were 39 items. Participants could complete the questionnaire on their own in a paper/pencil format or have a Māori community researcher administer the survey via an interview. The survey was written with English and Māori versions (back-to-back); it was originally written in English and then translated and back-translated to ensure equivalence of Māori to English. A large font and sufficient spacing were used for ease of reading for kaumātua. Participants received a $50 voucher for completing the survey. The University of Waikato's Human Research Ethics Committee, HREC (Health) 2020#93 approved the research protocols. The data collection procedures followed a culturally appropriate approach employed in prior projects (51, 52) to provide cultural safety.
Data analysis
Cronbach's alpha was used to assess reliability. Items from scales with low reliability were retained as individual items. Descriptive statistics included means, standard deviation and bivariate correlations. Multiple linear regression models (forward method) were employed to were run to determine the correlates of self-rated health, HRQOL, spiritual wellbeing, loneliness, and life satisfaction. The remaining items/scales were included as independent variables if they had a bivariate correlation with an outcome variable (p ≤ 0.10).
Results
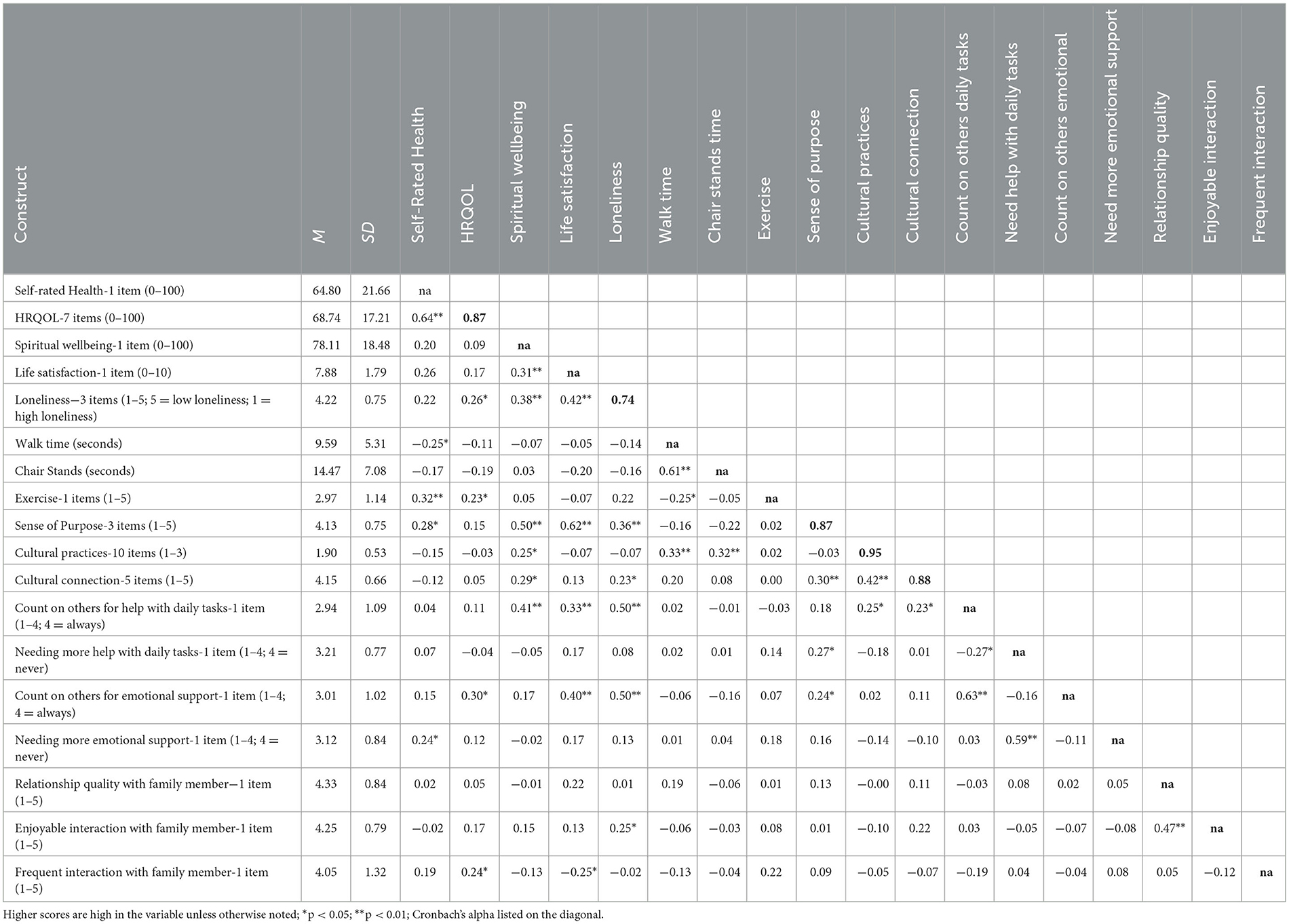
Descriptive statistics and Cronbach's alphas are displayed in Table 1. Spiritual wellbeing, HRQOL, and self-rated health were rescored to a 100-point response scale following prior approaches (53). Other response scores are based on the original response scale described in Table 1. The reliability for the relationship quality (α = 0.21) and social support (α = 0.37) were too low to warrant scales and thus the individual items were included for analysis.
The correlates for the outcomes are included in Table 2. The model for self-rated health included exercise and sense of purpose as positive correlates, F(2, 74) = 7.978, p = 0.001, adj R 2= 0.16. The model for HRQOL included perceived emotional support and frequent interaction with their whānau member as positive correlates, F(2, 74) = 6.521, p = 0.002, adj R2 = 0.13. The model for spiritual wellbeing included sense of purpose, not needing additional help with daily tasks, and cultural practices as positive correlates, F(3, 73) = 15.643, p < 0.001, adj R 2= 0.37. The regression model for life satisfaction was significant, F(4, 72) = 23.203, p < 0.001, adj R2 = 0.54. Life satisfaction had a positive association with sense of purpose, perceived emotional support, and relationship quality with their whānau member; it was negatively related with frequency of interaction with their whānau member. Finally, the regression model for loneliness was significant, F(5, 71) = 12.291, p < 0.001, adj R2 = 0.43. Low level of loneliness was positively associated with perceived emotional support, enjoyable interaction with their whānau member, sense of purpose, not needing additional help with daily tasks, and exercise.
Discussion
The purpose of this study was to establish the psychometric characteristics and baseline scores for the measures in the He Huarahi Tautoko project. Descriptive statistics indicated the following: (a) high levels of life satisfaction, spiritual wellbeing, sense of purpose, and cultural connection; (b) moderate to good levels of self-rated health, HRQOL, engagement with cultural practices, and social support; and (c) low levels of loneliness and exercise frequency. There are limited direct comparisons to other populations or other studies with kaumātua in Aotearoa on these scales. The results are very similar to a recent study of kaumātua in a different project (54) illustrating why it is important to not presume deficits or using a deficit approach when working with kaumātua specifically or Māori more generally (22, 23). Further, the responses demonstrate possibilities for improvement on the scales so the He Huarahi Tautoko project can positively affect these variables.
Sense of purpose had a positive association for loneliness, life satisfaction, self-rated health, and spiritual wellbeing. Sense of purpose was operationalised as making plans, developing a sense of direction, and having goals (50). Having a sense of purpose has found to be a significant correlate for physical activity, maintaining a healthy BMI, and avoiding sleep problems in the Health and Retirement Study (USA) (55). A sense of purpose can center on a variety of factors such as caring for family, contributing to the community, or continuing to work. For kaumātua, a key aspect of sense of purpose consists of contributing to the cultural knowledge and tikanga of the community (16). Given the historical cultural dissonance experienced by kaumātua due to colonization (11, 15), the He Huarahi Tautoko project is timely and important.
Social factors such as emotional support, tangible support, and relationship quality with their family member who is participating with them in the study were key correlates for HRQOL, life satisfaction, spiritual wellbeing, and low levels of loneliness. Prior research shows social support has a positive relationship for various wellbeing and health outcomes for Indigenous and non-Indigenous populations (29, 56–60). For older people, high-quality social relationships are important for enhancing quality of life and life expectancy (61–64). The importance of social relationships was highlighted by the COVID pandemic as many kaumātua were isolated during lockdown periods (7).
Frequency of moderate to vigorous exercise was a correlate for self-rated health and low levels of loneliness. A large amount of extant literature identifies a positive association of exercise and physical activity with wellbeing, mental health, health outcomes, and cognitive functioning (65–67). The relationship with low levels of loneliness is likely due to the preference of older adults to exercise with others as a way to avoid isolation and maintain connections with others (68).
Self-rated proficiency in cultural practices was associated positively with spiritual wellbeing. Cultural practices were operationalised as knowledge and confidence in using and sharing tikanga and Te Reo Māori as well as with roles in the community. Te Ao Māori is grounded in a cultural and spiritual connection which is important for many kaumātua (16). The results of this current study are consistent with these perspectives and reinforce the aim of He Huarahi Tautoko to enhance self-rated proficiency of cultural practices. As noted earlier, the cultural dissonance experienced by kaumātua due to colonization and State policies reinforce the need for culturally resonant programmes to enhance learning about Te Reo Māori and tikanga Māori (15, 69).
There are some implications from this study for Indigenous aging and enhancing cultural practices and physical activity. This study emphasizes a holistic perspective of health including cultural, social, and spiritual elements as well as physical and mental components. Aging well for kaumātua follows Māori models of health (32) and the project this study is based on integrates these elements into the programmes for addressing cultural practices and physical activity.
Further, this study focuses on mana motuhake, which is important in the context of colonial history and not following the Treaty of Waitangi. The cultural dissonance that was created through these historical practices has negatively impacted current kaumātua (11). In addition, much of the framing around inequities that have resulted from this history is based on a deficit perspective that also has negative impacts for kaumātua (19, 69). Mana motuhake emphasizes autonomy, status, and independence of kaumātua to recognize their own concerns and thereby solutions for addressing their wellbeing. Kaumātua are acknowledged as having experience and knowledge and the keepers of Māori tikanga; thus they should be afforded the opportunity to participate in creating solutions to address health and social inequities (2).
The He Huarahi Tautoko programme was developed through a participatory process with kaumātua and kaumātua service providers that addresses key features they deem important (i.e., cultural knowledge exchange and physical activity). This programme was developed to support kaumātua mana motuhake through exchange of mātauranga with each other and with members of their own whānau. The programme addresses key aspect of health, wellbeing, physical function, and culture that are important for kaumātua. The programme is culturally grounded and culturally safe (70), which helps to ameliorate some of the negative harms created from the colonial history.
Although there are key strengths of the study and the larger project, there are a couple of limitations as well. The study uses self-reported measures which are subject to perceptual bias. However, mana motuhake suggests that kaumātua are able to describe their own wellbeing. In addition, we do include physical functioning tests to complement the self-report measures. Further, the study is a purposive sample and thus generalization to the larger population is not appropriate. There may be inherent recruitment bias as a result of the non-random participant selection.
Conclusion
This study offered the baseline and psychometric characteristics from the He Huarahi Tautoko project, which is a programme that aims to enhance physical activity and cultural knowledge exchange for kaumātua in Aotearoa New Zealand. These results provide a baseline for later evaluation of the programme. Further, the study findings include key correlates of five wellbeing indicators grounded in the te whare tapa whā model: sense of purpose, social support and relationship quality, exercise frequency, and proficiency with Māori cultural practices. This current study illustrates key issues for kaumātua wellbeing; the He Huarahi Tautoko programme is a culturally-resonant approach that is strengths-based (rather than deficit based) to address wellbeing.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics statement
The studies involving humans were approved by the Human Research Ethics Committee (Health), University of Waikato. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JO: Conceptualization, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing—original draft. YZ: Conceptualization, Formal analysis, Methodology, Validation, Writing—review & editing. SN: Conceptualization, Funding acquisition, Investigation, Methodology, Supervision, Writing—review & editing. PM: Conceptualization, Funding acquisition, Investigation, Methodology, Supervision, Writing—review & editing. HH: Data curation, Investigation, Writing—review & editing. MV: Data curation, Investigation, Writing—review & editing. TT: Data curation, Investigation, Writing—review & editing. JU: Data curation, Investigation, Writing—review & editing. RW: Data curation, Investigation, Validation, Writing—review & editing. GB: Data curation, Investigation, Writing—review & editing. SK: Data curation, Investigation, Writing—review & editing. PR: Conceptualization, Methodology, Supervision, Writing—review & editing. BE: Conceptualization, Methodology, Supervision, Writing—review & editing. IW: Conceptualization, Methodology, Supervision, Writing—review & editing. A-MJ: Conceptualization, Methodology, Supervision, Writing—review & editing. TP: Conceptualization, Methodology, Supervision, Writing—review & editing. RR: Conceptualization, Funding acquisition, Methodology, Supervision, Writing—review & editing. MS: Conceptualization, Funding acquisition, Methodology, Writing—review & editing. MC: Conceptualization, Funding acquisition, Methodology, Writing—review & editing. BH: Conceptualization, Funding acquisition, Methodology, Writing—review & editing.
Funding
The project was funded by the Ageing Well National Science Challenge, New Zealand's Ministry of Business, Innovation and Employment (18566SUB1953); BH (PI), JO and RR (Co-PIs). The authors maintain sole responsibility for the research design, data collection, data analysis, and interpretation of the findings.
Acknowledgments
We thank the participants for sharing their insights. We also thank the community organizations who implemented the study; without their leadership and hard work, this study would not be possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1307685/full#supplementary-material
References
1. Statistics New Zealand. Māori Population Estimates. Available online at: https://www.stats.govt.nz/information-releases/maori-population-estimates-at-30-june-2020?gclid=CjwKCAjwi9-HBhACEiwAPzUhHLfizQ72e2yCEm976HxDWS8H2e6t2_04SerOx7XnYk3u8O-75F_kjxoCHTMQAvD_BwE (accessed June 30, 2020).
2. Ministry of Health. Wai 2575 Māori Health Trends Report. Wellington, NZL: Ministry of Health (2019).
3. Ministry of Health. Annual Update of Key Results 2019/20: New Zealand Health Survey. Wellington, NZL: Ministry of Health (2020).
4. Walsh M, Grey C. The contribution of avoidable mortality to the life expectancy gap in Māori and Pacific populations in New Zealand—a decomposition analysis. NZ Med J. (2019) 132:1492.
5. Russell L, Smiler K, Stace H. Improving Māori Health and Reducing Inequalities Between Māori and non-Māori: Has the Primary Health Care Strategy Worked for Māori? An Evaluation of the Period 2003-2010. Wellington: Health Research Council of New Zealand (2013).
6. Hayman KJ, Kerse N, Dyall L, Kepa M, Teh R, Wham C, et al. Life and living in advanced age: A cohort study in New Zealand -Te Puawaitanga o Nga Tapuwae Kia Ora Tonu, LiLACS NZ: study protocol. BMC Geriatr. (2012) 12:33. doi: 10.1186/1471-2318-12-33
7. Dawes T, Lapsley H, Muru-Lanning M. Hauora Kaumātua: a review essay on kaumātua wellbeing. Kotuitui. (2022) 17:429–44. doi: 10.1080/1177083X.2022.2067482
8. Brown H, Bryder L. Universal healthcare for all? Maori health inequalities in Aotearoa New Zealand, 1975–2000. Soc Sci Med. (2023) 319:115315. doi: 10.1016/j.socscimed.2022.115315
9. Harris R, Cormack D, Tobias M, Yeh L-C, Talamaivao N, Minster J, et al. The pervasive effects of racism: experiences of racial discrimination in New Zealand over time and associations with multiple health domains. Soc Sci Med. (2012) 74:408–15. doi: 10.1016/j.socscimed.2011.11.004
10. Reid P, Cormack D, Paine S. Colonial histories, racism and health: the experience of Maori and Indigneous peoples. Public Health. (2019) 172:119–24. doi: 10.1016/j.puhe.2019.03.027
11. Simon J. Ideology in the Schooling of Maori Children. Ashburn, VA: Department of Education, Massey University (1986).
12. Hokowhitu B: Te tāminga o te mātauranga Māori: Colonisation in education. In: T Ka'ai, J Moorfield, M Reilly, editors Ki te whaiao: An Introduction to Māori Society. Auckland: Pearson Education (2003), 190–200.
13. Durie M. Understanding health and illness: research at the interface between science and indigenous knowledge. Int J Epidemiol. (2004) 33:1138–43. doi: 10.1093/ije/dyh250
14. Oster R, Grier A, Lightning RM M, Toth E. Cultural continuity, traditional Indigenous language, and diabetes in Alberta First Nations: a mixed methods study. Int J Equity Health. (2014) 13:92. doi: 10.1186/s12939-014-0092-4
15. Pihama L, Reynolds P, Smith C, Reid J, Smith L, Tenana R. Positioning historical trauma theory within Aotearoa New Zealand. Alternative. (2014) 10:248–62. doi: 10.1177/117718011401000304
16. Taskforce on Whānau Ora Initiatives. Whānau ora: Report of the Taskforce on Whanau-Centred Initiatives. Wellington: Ministry of Health (2010).
17. Palmer S, Gray H, Huria T, Lacey C, Beckerrt L, Pitama S. Reported Māori consumer experiences of health systems and programs in qualitative research: a systematic review with meta-synthesis. Int J Equity Health. (2019) 18:163. doi: 10.1186/s12939-019-1057-4
18. Graham R, Masters-Awatere B. Experiences of Māori of Aotearoa New Zealand's public health system: a systematic review of two decades of published qualitative research. Aust NZ J Public Health. (2020) 44:193–200. doi: 10.1111/1753-6405.12971
19. Elers P. Māori health: issues relating to health care services. Te Kaharoa. (2014) 7:1–15. doi: 10.24135/tekaharoa.v7i1.51
20. Hirini PR, Flett RA, Kazantzis N, Long NR, Millar MA, MacDonald C. Health care needs for older Māori: a study of Kaumātua and kuia. Soc Policy J NZ. (1999) 13:136–53.
21. Smith LT. Decolonizing methodologies: Research and Indigenous Peoples. London: Zed Books Ltd. (2021).
22. Hokowhitu B. Indigenous Bodies, Ordinary Lives. In: D Robinson, L Randall, editors Social Justice in Physical Education: Critical Reflections and Pedagogies for Change. Toronto: Canadian Scholar's Press (2016), 164–82.
23. Jones R, Crowshoe L, Reid P, Calam B, Curtis E, Green M. Educating for indigenous health equity: an international consensus statement. Acad Med. (2019) 94:512–9. doi: 10.1097/ACM.0000000000002476
24. Hokowhitu B, Oetzel JG, Simpson ML, Nock S, Reddy R, Meha P, et al. Kaumātua Mana Motuhake Poi: a study protocol for enhancing wellbeing, social connectedness and cultural identity for Māori elders. BMC Geriatr. (2020) 20:377. doi: 10.1186/s12877-020-01740-3
25. Callow D, Arnold-Nedimala N, Jordan L, Pena G, Won J, Woodward J, et al. The mental health benefits of physical activity in older adults survive the COVID-19 pandemic. Am J Geriatr Psychiatry. (2020) 28:1046–57. doi: 10.1016/j.jagp.2020.06.024
26. Thomas E, Battaglia G, Patti A, Brusa J, Leonardi V, Palma A, et al. Physical activity programs for balance and fall prevention in elderly: a systematic review. Med. (2019) 98:e16218. doi: 10.1097/MD.0000000000016218
27. Pihama L, Tipene J, Skipper H. Ngā Hua a Tāne Rore: The Benefits of Kapa Haka. Wellington: NZL (2014).
28. Warbrick I, Dickson A, Prince RJ, Heke I. The biopolitics of Māori biomass: towards a new epistemology for Māori health in Aotearoa/New Zealand. Crit Public Health. (2016) 26:394–404. doi: 10.1080/09581596.2015.1096013
29. Dyall L, Kepa M, Teh R, Mules R, Moyes S, Wham C, et al. Cultural and social factors and quality of life of Maori in advanced age. Te puawaitanga o nga tapuwae kia ora tonu - Life and living in advanced age: a cohort study in New Zealand (LiLACS NZ). N Z Med J. (2014) 127:62–79.
30. Brown A. Kurunpa [Spiriti]: Exploring the Psychosocial Determinants of Coronary Heart Disease among Indigenous Men in Central Australia. Brisbane, QLD: University of Queensland (2009).
31. Carter KT B, Soeberg M. Trends in survival and life expectancy by aity, income and smoking in New Zealand: 1980s to 2000s. NZ Med J. (2010) 123:13–24.
32. Rochford T. Whare tapa wha: a Māori model of a unified theory of health. J Prim Prev. (2004) 25:41–57. doi: 10.1023/B:JOPP.0000039938.39574.9e
33. Tuhiwai-Smith L. Decolonizing Methodologies: Research and Indigenous Peoples. London: Zed Books (1999).
34. Smith GH. The Development of Kaupapa Māori: Theory and Praxis. Auckland: University of Auckland (1997).
35. Oetzel J, Scott N, Hudson M, Masters-Awatere B, Rarere M, Foote J, et al. Implementation framework for chronic disease intervention effectiveness in Māori and other indigenous communities. Global Health. (2017) 13:69. doi: 10.1186/s12992-017-0295-8
38. Achat HM, Thomas P, Close GR, Moerkerken LR, Harris MF. General health care service utilisation: where, when and by whom in a socioeconomically disadvantaged population. Aust J Prim Health. (2010) 16:132–40. doi: 10.1071/PY09066
39. Dulin PL, Stephens C, Alpass F, Hill RD, Stevenson B. The impact of socio-contextual, physical and lifestyle variables on measures of physical and psychological wellbeing among Māori and non-Māori: the New Zealand Health, work and retirement study. Ageing Soc. (2011) 31:1406–24. doi: 10.1017/S0144686X10001479
40. Ware J, Kosinski M, Dewey JE, Gandek B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey. Lincoln, RI: QualityMetric Inc (2001).
41. Wu A, Revicki D, Jacobsen D, Malitz F. Evidence for reliability, validity and usefulness of the medical outcomes study HIV health survey (MOS-HIV). Qual Life Res. (1997) 6:481–93.
42. Statistics New Zealand. Te Kupenga 2013: A survey of Māori Well-Being. Auckland: Statistics New Zealand (2013).
43. Waldegrave C, Cunningham C, Love C, Nguyen G. Co-creating culturally nuanced measures of loneliness with Māori elders. Innov Aging. (2020) 4:610. doi: 10.1093/geroni/igaa057.2064
44. Dyall L, Kerse N, Hayman K, Keeling S. Pinnacle of life-Māori living to advanced age. NZ Med J. (2011) 124:75.
45. Aquilino W. Two views of one relationship: Comparing parents' and young adults children's repjorts of the quality of intergenerational relations. J Marriage Fam. (1999) 61:858–70. doi: 10.2307/354008
46. Saint-Maurice P, Coughlan D, Kelly S, Keadle S, Cook M, Carlson S, et al. Association of leisure-teim physical activity across the adult life course with all-cause and cause-specific mortality. JAMA Netw Open. (2019) 2:e190355. doi: 10.1001/jamanetworkopen.2019.0355
47. Guralnik J, Simonsick E, Ferrucci L, Glynn R, Berkman L, Blazer D, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. (1994) 49:M85–94. doi: 10.1093/geronj/49.2.M85
48. Freiberger E, de Vreede P, Schoene D, Rydwik E, Mueller V, Frandin K, et al. Performance-based physical function in older community-dwelling persons: a systematic review of instruments. Age Ageing. (2012) 41:712–21. doi: 10.1093/ageing/afs099
50. Windsor T, Curtis R, Luszcz, MA. Sense of purpose as a psychological resource for aging well. Dev Psychol. (2015) 51:975–86. doi: 10.1037/dev0000023
51. Oetzel J, Simpson M, Berryman K, Reddy R. Differences in ideal communication behaviours during end-of-life care for Māori carers/patients and palliative care workers. Palliat Med. (2015) 29:764–6. doi: 10.1177/0269216315583619
52. Team RKCTRP. Māori Health Literacy and Communication in Palliative Care: Rauawaawa Kaumātua Charitable Trust Team. Māori Health Literacy and Communication in Palliative Care: Kaumātua-Led Models. Aotearoa: Ministry of Health and the Health Research Council (2012).
53. Rand Health. 36-item Short Form Survey (SF-36) Scoring Instructions: RAND Health. Available online at: https://www.rand.org/health/surveys_tools/mos/36-item-short-form/scoring.html (accessed September 1, 2023).
54. Oetzel JG, Ruru S, Zhang Y, Simpson ML, Nock S, Meha P, et al. Enhancing well-being and social connectedness for māori elders through a peer education (tuakana-teina) programme: a cross-sectional baseline study. Front Public Health. (2021) 9:775545. doi: 10.3389/fpubh.2021.775545
55. Kim E, Shiba K, Boehm J, Kubzansky L. Sense of purpose in life and five health behaviors in older adults. Prev Med. (2020) 139:106172. doi: 10.1016/j.ypmed.2020.106172
56. Adams K, Paasse G, Clinch D. Peer-support preferences and readiness-to-change behaviour for chronic disease prevention in an urban indigenous population. Aust Soc Work. (2011) 64:55–67. doi: 10.1080/0312407X.2010.541269
57. Brownell MD, Nickel NC, Enns JE, Chartier M, Campbell R, Phillips-Beck W, et al. Association between home visiting interventions and First Nations families' health and social outcomes in Manitoba, Canada: protocol for a study of linked population-based administrative data. BMJ Open. (2017) 7:e017626. doi: 10.1136/bmjopen-2017-017626
58. Chappell NL, Funk LM. Social support, caregiving, and aging. Can J Aging. (2011) 30:355–70. doi: 10.1017/S0714980811000316
59. Cohrdes C, Mensink GB, Hölling H. How you live is how you feel? Positive associations between different lifestyle factors, cognitive functioning, and health-related quality of life across adulthood. Q Life Res. (2018) 27:3281–92. doi: 10.1007/s11136-018-1971-8
60. Koutsogeorgou E, Davies JK, Aranda K, Zissi A, Chatzikou M, Cerniauskaite M, et al. Healthy and active ageing: social capital in health promotion. Health Educ J. (2014) 73:627–41. doi: 10.1177/0017896913509255
61. Gerino E, Rollè L, Sechi C, Brustia P. Loneliness, resilience, mental health, and quality of life in old age: a structural equation model. Front Psychol. (2003) 8:2003. doi: 10.3389/fpsyg.2017.02003
62. McGarrigle C, Layte R. OP46 The role of social support and the importance of the quality of the relationship in reducing depression, loneliness and reduced quality of life with disability in older ages evidence from the irish longitudinal study on ageing. J Epidemiol Commun Health. (2015) 69:A29. doi: 10.1136/jech-2015-206256.45
63. Oetzel JG, Hokowhitu B, Simpson M, Reddy R, Cameron MP, Meha P, et al. Correlates of health-related quality of life for māori elders involved in a peer education intervention. J Health Commun. (2019) 24:1–11. doi: 10.1080/10810730.2019.1637483
64. Szabo A, Allen J, Alpass F, Stephens C. Loneliness, socio-economic status and quality of life in old age: the moderating role of housing tenure. Ageing Soc. (2019) 39:998–1021. doi: 10.1017/S0144686X17001362
65. Tulloch A, Bombell H, Dean C, Tiedsemann A. Yoga-based exercise improves health-related qualityof life and mental well-being in older people: a systematic review of randomised controlledt rials. Age Ageing. (2018) 47:537–44. doi: 10.1093/ageing/afy044
66. Gennuso K, Gangnon R, Matthews C, Thraen-Borowski K, Colbert L. Sedentary behavior, physcial activity, and markers of health in older adults. Med Sci Sports Exerc. (2018) 45:1493–500. doi: 10.1249/MSS.0b013e318288a1e5
67. Tseng C-N, Gau B-S, Lou M-F. The effectiveness of exercise on improving cognitive function in older people: a systematic review. J Nurs Res. (2011) 19:119–30. doi: 10.1097/JNR.0b013e3182198837
68. Hwang J, Wang L, Siever J, Del Medico T, Jones C. Loneliness and social isolation among older adults in a community exercise program: a qualitative study. Ageing Mental Health. (2018) 23:736–42. doi: 10.1080/13607863.2018.1450835
69. Hirini P, Flett R, Long N, Millar M. Traumatic events and New Zealand Māori. NZ J Psychol. (2005) 34:20–7.
70. Ramsden I. Cultural Safety: Implementing the Concept—the Social Force of Nursing and Midwifery. In: PT Whaiti, A McCarthy, M Durie, editors Mai I Rangiatea. Auckland: Auckland University and Bridget Williams Books (2002).
Glossary
Keywords: older Māori health, indigenous aging, physical activity, health equity, health-related quality of life
Citation: Oetzel JG, Zhang Y, Nock S, Meha P, Huriwaka H, Vercoe M, Tahu T, Urlich J, Warbrick R, Brown G, Keown S, Rewi P, Erueti B, Warbrick I, Jackson A-M, Perry T, Reddy R, Simpson ML, Cameron MP and Hokowhitu B (2023) Enhancing health outcomes for Māori elders through an intergenerational cultural exchange and physical activity programme: a cross-sectional baseline study. Front. Public Health 11:1307685. doi: 10.3389/fpubh.2023.1307685
Received: 05 October 2023; Accepted: 14 November 2023;
Published: 12 December 2023.
Edited by:
Vahid Rashedi, University of Social Welfare and Rehabilitation Sciences, IranReviewed by:
Amy Silva-Smith, University of Colorado Colorado Springs, United StatesNatalia Sharashkina, Pirogov Russian National Research Medical University, Russia
Copyright © 2023 Oetzel, Zhang, Nock, Meha, Huriwaka, Vercoe, Tahu, Urlich, Warbrick, Brown, Keown, Rewi, Erueti, Warbrick, Jackson, Perry, Reddy, Simpson, Cameron and Hokowhitu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yingsha Zhang, emhhbmd5c2g2N0BtYWlsLnN5c3UuZWR1LmNu
†These authors have contributed equally to this work
‡These authors have contributed equally to this work and share last authorship
 John G. Oetzel
John G. Oetzel Yingsha Zhang
Yingsha Zhang Sophie Nock1†
Sophie Nock1† Bevan Erueti
Bevan Erueti Mary Louisa Simpson
Mary Louisa Simpson Brendan Hokowhitu
Brendan Hokowhitu