- 1Pandemic Sciences Institute, University of Oxford, Oxford, United Kingdom
- 2Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa
There is a complex interplay between infectious disease outbreaks and the stigmatization of affected persons and communities. Outbreaks are prone to precipitating stigma due to the fear, uncertainty, moralisation, and abatement of freedoms associated with many infectious diseases. In turn, this stigma hampers outbreak control efforts. Understanding this relationship is crucial to improving coordinated outbreak response. This requires valid and reliable methods for assessing stigma towards and within impacted communities. We propose adopting a cross-outbreak model for developing the necessary assessment tools. A stigma-informed approach must then be integrated into outbreak preparedness and response efforts to safeguard public health and promote inclusivity and compassion in future outbreaks.
Infectious disease outbreaks have long been accompanied by an insidious companion – stigma. The legacy of this association traces back to antiquity, encompassing leprosy (now known as Hansen’s disease), and reverberates through contemporary events such as the global outbreak of mpox (formerly known as monkeypox). Notably the renaming of both these diseases was driven by the imperative to disentangle them from this accompanying stigma (1, 2).
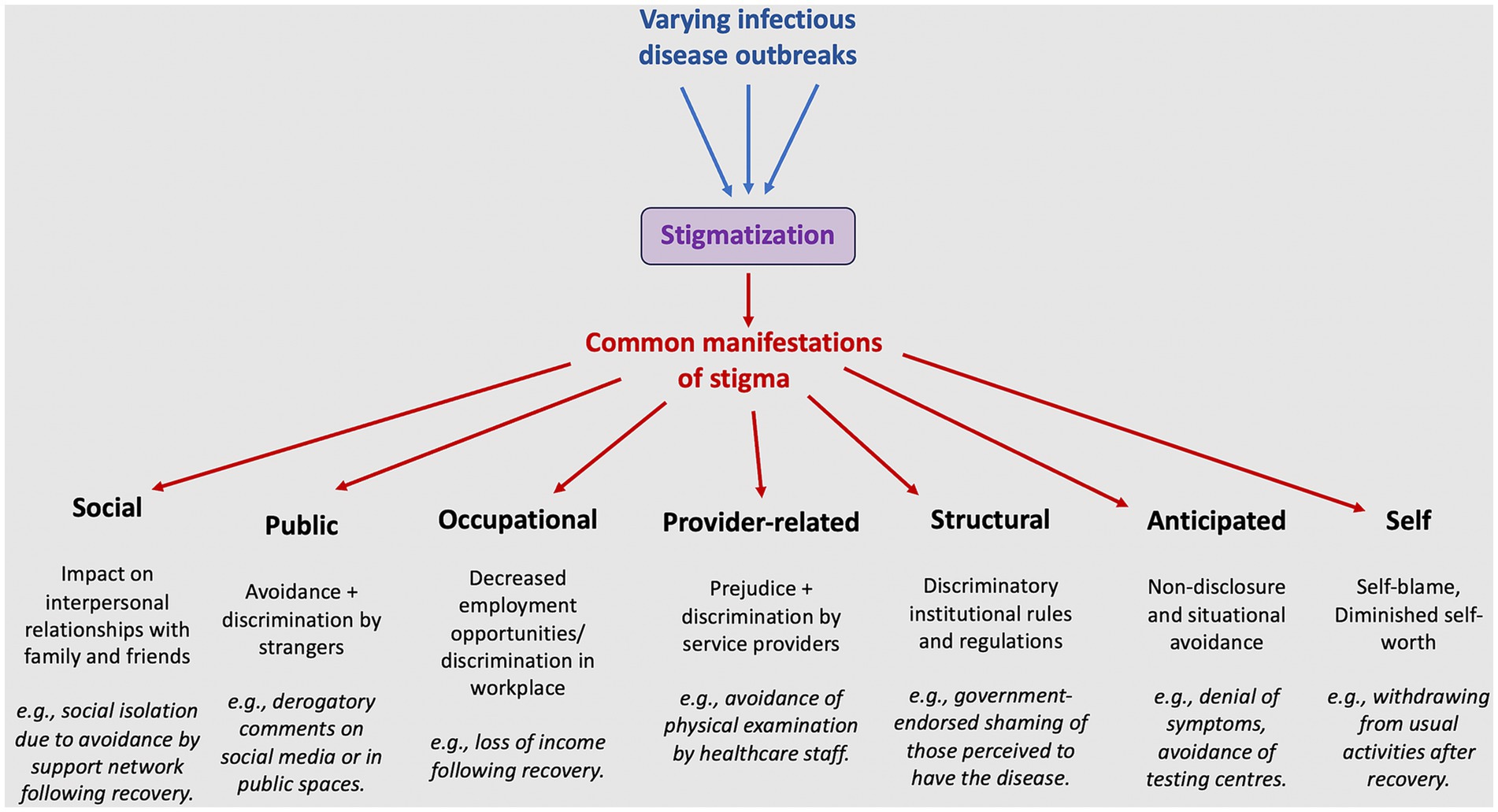
Stigma occurs when an individual or group is denied full social acceptance due to an attribute deemed discrediting by their community or society (3, 4). This umbrella term includes negative thoughts and feelings about affected individuals (i.e., prejudice) and negative treatment including exclusion (i.e., discrimination) (4–6). Stigma plays a prominent role in infectious disease outbreaks for a variety of reasons – the diseases are communicable, often unfamiliar, sometimes severe, and public health interventions can involve a lack of privacy and incursion on civil liberties.
Communities respond to outbreaks with spontaneous actions that can either precipitate or counteract the emergence of stigma. This ranges from exclusion or discrimination of individuals, as witnessed in the ostracization of people of Asian appearance in the initial stages of the COVID-19 outbreak (7), to mobilisation of support groups, such as those established by Ebola survivors in the Democratic Republic of the Congo (8), Sierra Leone (9), and Uganda (10). However, what often remains inadequately considered is the extent to which outbreak control activities might inadvertently precipitate stigma. This is despite the fact that outbreak control measures that could unintentionally foster stigma are seemingly ubiquitous.
Contact tracing, as conducted for COVID-19, often results in linear assignment of blame to affected individuals (11). Public health messaging that relies on instilling fear to drive behavior change can unintentionally foster stigma (12, 13). This is similarly true for messaging that moralizes diseases and health-related behavior (11, 12, 14). For instance, in Mexico, government communication on preventing Dengue has emphasised household cleanliness, leading those who get the disease to be perceived as unclean (15). Risk communication that singles out specific demographics or regions, as observed with COVID-19 (16), SARS (17), and mpox (18), may contribute to intersectional stigma for high risk groups. Hazmat suits and other personal protective equipment can create a sense of otherness for both patients and healthcare workers across outbreak settings (13, 19, 20). Additionally, the prohibition of traditional burial practices, a common measure for infection control in Ebola (21) and Nipah virus outbreaks (22), is viewed as disrespectful and stigmatizing in certain communities. A systematic review of the psychological impacts of enforced quarantine during COVID-19 reported enduring stigma as a recurring theme (23).
While this does not discredit the control measures per se – many outbreak interventions require a delicate dance of accepting some collateral harms and risks – these untoward consequences must be measured more robustly and reduced where possible. This is important for the well-being of affected populations and for optimising outbreak control.
Outbreak-associated stigma substantially impacts social, physical, and psychological well-being (24). This is particularly true when the stigma becomes internalized, also known as self-stigma, resulting in feelings of self-blame, guilt, and low self-confidence (25). These symptoms can reduce self-efficacy, motivation, and perceived control over negative events, including the spread of an outbreak, thereby diminishing the importance placed on preventive measures such as physical distancing (26).
Several studies have demonstrated that Ebola and COVID-19 stigma have strong associations with symptoms of depression, anxiety, insomnia, and post-traumatic stress disorder (PTSD) (27–31). Since these associated mental health conditions are often also stigmatized, this can add to the burden of stigma for affected individuals (32). A Poisson regression model, examining impact of the 2003 SARS epidemic, revealed an excess of older adult suicides at the peak of the epidemic, with the statistic not returning to baseline for at least 2 years (33). This trend has been observed before, during the 1918–19 influenza pandemic (34), and subsequently, with Ebola survivor suicide attempts six times higher than those of other community members in one cohort (35). In some cases, these mental health impacts have continued to affect survivors more than 20 years after the relevant outbreak (36).
This negative impact is not restricted to those who are diagnosed with an outbreak disease, but also those in close proximity with them (including family members and other community members), healthcare workers, and those thought to be associated with the disease (e.g., due to appearance or related symptoms) (37). Notably, in the Democratic Republic of the Congo, nearly half (46%) of individuals in cities and villages affected by the 2019 Ebola outbreak exhibited severe psychological distress symptoms seven months after the outbreak (37). In a population-based sample of adults in Michigan, the prevalence of depressive and anxiety symptoms was higher among respondents who perceived more COVID-19 stigma (31). Higher levels of outbreak-related anxiety in community members may consequently worsen bullying of those with the disease (38). These repercussions of stigma for affected populations perpetuate health and social inequities (24).
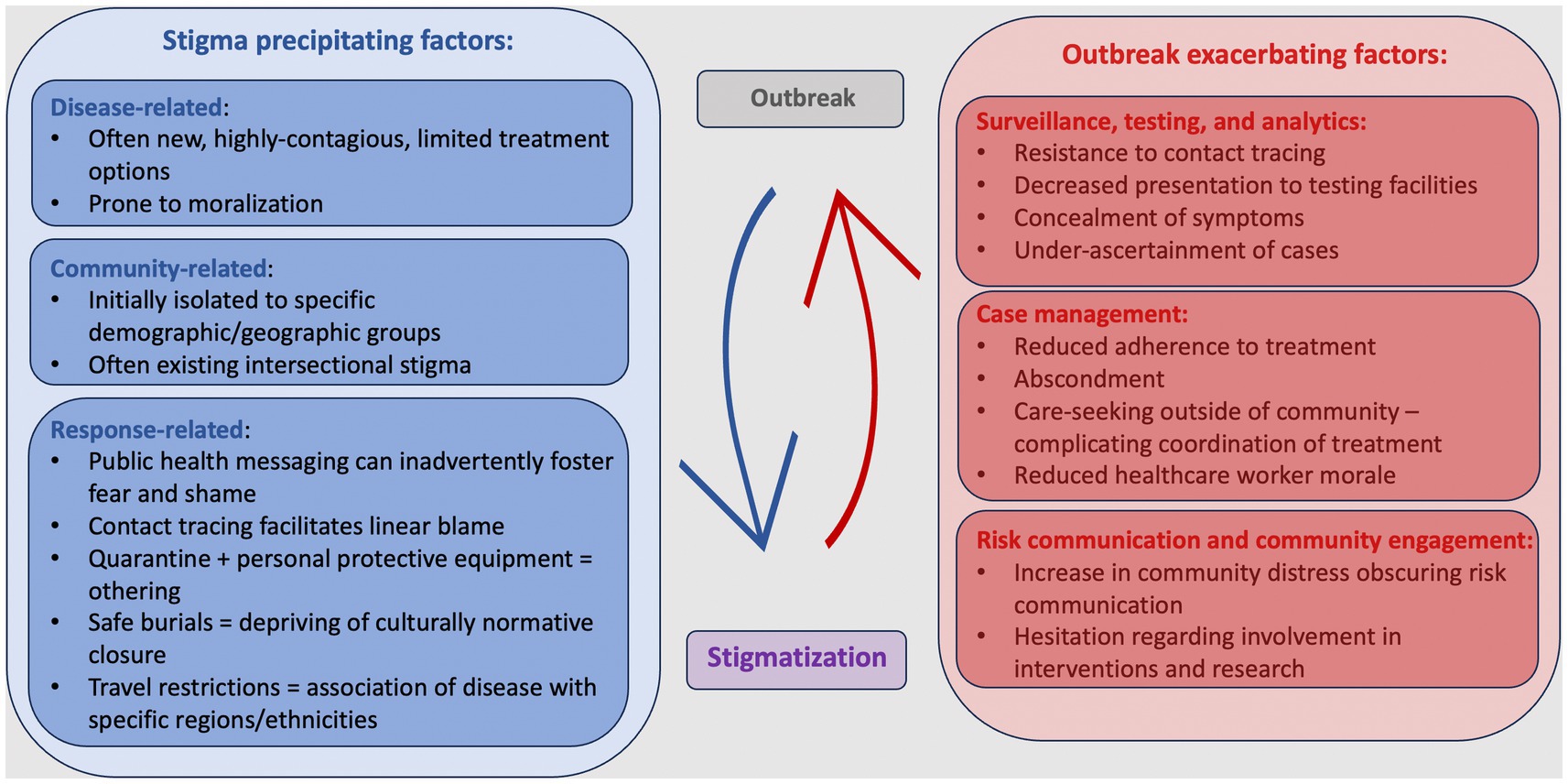
The adverse effects of stigma also impact outbreak control permeating every aspect of outbreak response (Figure 1). These insidious effects can be identified across geographical settings and diseases. For instance, during the Ebola outbreak in West Africa, contact tracers encountered community resistance and non-disclosure of contacts, hindering timely interventions (39). Similarly, in the COVID-19 pandemic, testing efforts suffered from denial, symptom concealment, and avoidance of testing facilities, leading to underestimation of cases and undetected spread (40, 41). As a further example of this, Ebola survivors from Sierra Leone reported they took an average of 3.36 days to seek treatment after symptom onset (41).
In many outbreaks stigma poses a significant challenge to case management by reducing adherence to care and treatment (15, 21). Lack of trust in responders can also risk healthcare worker safety. A cross-sectional study of over 7,000 participants in 173 countries found that healthcare workers were at an increased risk of COVID-19 related bullying and harassment (42). In turn, healthcare worker fear and diminished morale may result in hesitation to treat individuals thought to have an outbreak disease (17, 21). This occurred during the SARS outbreak in Hong Kong, where occupants of a high risk residential complex reported being denied healthcare services at clinics (17).
Infection prevention faces hurdles with stigma fostering avoidance of preventative measures, vaccine hesitancy, and disease denialism. The recent mpox outbreak is an example of this, stigma related to the required disclosure of sexual preferences for vaccination has discouraged vaccine uptake in many countries (23). Epidemiological analytics suffer from under-ascertainment of cases when individuals do not disclose their infections. Risk communication is clouded by social anxieties and decreased interaction with the health system limits educational opportunities, as was found to be the case with Lassa fever in Nigeria (43) and Zika virus disease in Spain (44). Research which is scientifically robust and ethically valid may still fail due to scepticism and fear.
The HIV/AIDS pandemic provides compelling empirical evidence of how stigma can impact infectious disease detection, service uptake, and clinical outcomes (45, 46). For instance, recent data from UNAIDS reveals that addressing stigma and discrimination related to HIV could prevent 2.5 million new HIV infections and avert 1.7 million AIDS related deaths by 2025 (45).
This evidence underscores the need to prioritize addressing stigma in disease control efforts, and has spurred international and national commitments to address HIV stigma (46–48). Notably, the 2021 UN Political Declaration on HIV and AIDS (48) and Global AIDS Strategy (2021–2026) (47) introduced the 10-10-10 targets to achieve HIV control. These targets require countries to undertake reforms to ensure that less than 10% of people living with HIV and key populations will experience HIV-related or intersectional stigma (47, 48). Additionally, the targets aim to reduce structural discrimination such that less than 10% of countries have legal and policy frameworks that limit access to HIV-related services (47, 48).
As a result of these commitments, HIV stigma is now carefully monitored across a wide range of settings (49). Robust assessment tools have been developed for this purpose. For example, the People Living with HIV (PLHIV) stigma index evaluates the effect of HIV stigma on public health in a standardised manner globally. It has subsequently been used for public health and advocacy purposes in more than 100 countries with over 100,000 participants (50). A cross-culturally validated and widely used stigma measure for emerging disease outbreaks could similarly enhance our ability to reveal and mitigate stigma in emerging infectious disease outbreaks.
We advocate for rapid and repeated assessment of stigma as an equally important component of emerging outbreak response. This is critical not only to inform and evaluate strategies for stigma reduction, but also to provide reliable guidance to responders on how to limit the propagation of stigma (51). While outbreak-specific tools exist for assessing stigma (17, 30, 43, 52–58), this assessment currently tends to occur late in the course of an emerging outbreak, limiting the potential impact of this work. This delay is often due to the lead time required for the creation of new stigma assessment tools each time an outbreak occurs.
Cross-outbreak research on stigma could facilitate faster assessment of stigma and mitigation of stigma’s adverse effects on the mental health of affected individuals as well as outbreak control. This is because it allows us to begin creating and validating tools to assess and address stigma associated with future outbreaks, even before the specific details of the next outbreak are known. This approach adopts the concept of “disease X” as an exemplar – a placeholder name widely adopted in vaccine development and clinical research to represent an as yet unknown emerging pathogen that should be included in pandemic preparedness (59).
The development of cross-outbreak stigma research tools has pragmatic benefits: many of these diseases are rare, occur sporadically, and emerge at unexpected times and locations. While high impact, their duration is often brief. A stigma tool designed reactively to an outbreak is often too late to facilitate timely intervention, or of limited validity if developed quickly (60). Local outbreak response efforts usually do not have the capacity to create such a tool in resource-limited settings, or indeed amongst competing demands even in high-resource settings.
Importantly, the development of stigma research tools that can be used across emerging infectious diseases is also feasible. This is due to notable similarities in the manifestations of stigma across different settings and diseases (Figure 2) (61). Consequently, we propose adopting this cross-outbreak model to proactively design evidence-based outbreak stigma assessment and intervention tools with broad applicability. These tools can then be readily tailored to suit local contexts.
An approach that considers and intentionally minimises stigma should be embedded in outbreak preparedness and response efforts. It is imperative to ensure that stigma does not hinder our ability to safeguard public health, protect affected communities, and promote a culture of inclusivity and compassion in the face of future outbreaks.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AP: Conceptualization, Writing – original draft, Writing – review & editing. PO: Supervision, Writing – review & editing. AR: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Deps, P, and Cruz, A. Why we should stop using the word leprosy. Lancet Infect Dis. (2020) 20:e75–8. doi: 10.1016/S1473-3099(20)30061-X
2. World Health Organization. WHO recommends new name for Monkeypox disease (2022). Available from: https://www.who.int/news/item/28-11-2022-who-recommends-new-name-for-monkeypox-disease. (Accessed: November 2023).
4. Corrigan, PW. The stigma of disease and disability: Understanding causes and overcoming injustices, vol. xi. First ed. Washington, DC: American Psychological Association (2014). 319 p.
5. Weiss, MG. Stigma and the social burden of neglected tropical diseases. PLoS Negl Trop Dis. (2008) 2:e237. doi: 10.1371/journal.pntd.0000237
6. Link, BG, and Phelan, JC. Conceptualizing stigma. Annu Rev Sociol. (2001) 27:363–85. doi: 10.1146/annurev.soc.27.1.363
7. Hahm, HC, Xavier Hall, CD, Garcia, KT, Cavallino, A, Ha, Y, Cozier, YC, et al. Experiences of Covid-19-related anti-Asian discrimination and affective reactions in a multiple race sample of U.S. Young adults. BMC Public Health. (2021) 21:11559. doi: 10.1186/s12889-021-11559-1
8. Bahati, KS. Congo’s Ebola survivors unite to combat stigma and misinformation (2021). Available from: https://longreads.trust.org/item/Ebola-survivors-DRC-combat-stigma-misinformation. (Accessed: November 2023).
9. Bond, N, Sesay, S, Kamara, A, Bates, J, Teigen, J, and Stowlow, J. Ebola survivor corps: employing Ebola survivors as health educators and advocates in communities affected by Ebola in northern Sierra Leone. Lancet Glob Health. (2019) 7:S48. doi: 10.1016/s2214-109x(19)30133-0
10. USAID. Restoring Hope and dignity of Ebola survivors in Uganda. U.S. Agency for International Development, (2023). Available from: https://medium.com/usaid-2030/restoring-the-hope-and-dignity-of-ebola-survivors-in-uganda-41cd96844eca (Accessed: November 2023).
11. Trinh, DH, McKinn, S, Nguyen, AT, Fox, GJ, Nguyen, AT, and Bernays, S. Uneven stigma loads: community interpretations of public health policies, 'Evidence' and inequities in shaping Covid-19 stigma in Vietnam. SSM Popul Health. (2022) 20:101270. doi: 10.1016/j.ssmph.2022.101270
12. Kraaijeveld, SR, and Jamrozik, E. Moralization and Mismoralization in public health. Med Health Care Philos. (2022) 25:655–69. doi: 10.1007/s11019-022-10103-1
13. Moodley, P, and Lesage, SS. A discourse analysis of Ebola in south African newspapers (2014–2015). S Afr J Psychol. (2020) 50:158–69. doi: 10.1177/0081246319868656
14. Brewis, A, and Wutich, A. Why we should never do it: stigma as a behaviour change tool in Global Health. BMJ Glob Health. (2019) 4:e001911. doi: 10.1136/bmjgh-2019-001911
15. Arellano, C, Castro, L, Díaz-Caravantes, RE, Ernst, KC, Hayden, M, and Reyes-Castro, P. Knowledge and beliefs about dengue transmission and their relationship with prevention practices in Hermosillo, Sonora. Front Public Health. (2015) 3:142. doi: 10.3389/fpubh.2015.00142
16. Xu, J, Sun, G, Cao, W, Fan, W, Pan, Z, Yao, Z, et al. Stigma, discrimination, and hate crimes in Chinese-speaking world amid Covid-19 pandemic. Asian J Criminol. (2021) 16:51–74. doi: 10.1007/s11417-020-09339-8
17. Lee, S, Chan, LYY, Chau, AMY, Kwok, KPS, and Kleinman, A. The experience of Sars-related stigma at Amoy gardens. Soc Sci Med. (2005) 61:2038–46. doi: 10.1016/j.socscimed.2005.04.010
18. März, JW, Holm, S, and Biller-Andorno, N. Monkeypox, stigma and public health. Lancet Regional Health. (2022) 23:100536. doi: 10.1016/j.lanepe.2022.100536
19. Dua, D, Laxmi, R, Mehra, A, Sahoo, S, and Grover, S. Acute stress reaction related to use of personal protective equipment in health-care workers. Indian J Psychiatry. (2020) 62:599–600. doi: 10.4103/psychiatry.IndianJPsychiatry_409_20
20. Liam Stack, JG, and Otterman, Sharon. Pain, fear, stigma: What people who survived Monkeypox want you to know. (2022)
21. Nuriddin, A, Jalloh, MF, Meyer, E, Bunnell, R, Bio, FA, and Jalloh, MB. Trust, fear, stigma and disruptions: community perceptions and experiences during periods of low but ongoing transmission of Ebola virus disease in Sierra Leone, 2015. BMJ Glob Health. (2018) 3:e000410. doi: 10.1136/bmjgh-2017-000410
22. Radhakrishnan, C, Sankar, UV, Rajendran, VR, Devi, A, and Jayasree, V. Psychosocial impacts of quarantine among survivors of the Nipah virus infection: a qualitative study. J Global Health Rep. (2021) 5:5. doi: 10.29392/001c.28993
23. Mazzagatti, R, and Riva, MA. Monkeypox vaccine-related stigma. Publ Health Practice. (2022) 4:100336. doi: 10.1016/j.puhip.2022.100336
24. Stangl, AL, Earnshaw, VA, Logie, CH, van Brakel, W, and C Simbayi, L. The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. (2019) 17:31. doi: 10.1186/s12916-019-1271-3
25. Yuan, Y, Zhao, Y-J, Zhang, Q-E, Zhang, L, Cheung, T, and Jackson, T. Covid-19-related stigma and its sociodemographic correlates: a comparative study. Glob Health. (2021) 17:54. doi: 10.1186/s12992-021-00705-4
26. Park, J, Lee, S, Sul, S, and Chung, D. Depression symptoms mediate mismatch between perceived severity of the Covid-19 pandemic and preventive motives. Front Psychol. (2021) 12:12. doi: 10.3389/fpsyg.2021.650042
27. Cenat, JM, Rousseau, C, Bukaka, J, Dalexis, RD, and Guerrier, M. Severe anxiety and Ptsd symptoms among Ebola virus disease survivors and healthcare Workers in the Context of the Covid-19 pandemic in eastern Dr Congo. Front Psych. (2022) 13:767656. doi: 10.3389/fpsyt.2022.767656
28. Cenat, JM, Noorishad, PG, Kokou-Kpolou, CK, Dalexis, RD, Hajizadeh, S, Guerrier, M, et al. Prevalence and correlates of depression during the Covid-19 pandemic and the major role of stigmatization in low- and middle-income countries: a multinational cross-sectional study. Psychiatry Res. (2021) 297:113714. doi: 10.1016/j.psychres.2021.113714
29. Cenat, JM, Noorishad, PG, Dalexis, RD, Rousseau, C, Derivois, D, Kokou-Kpolou, CK, et al. Prevalence and risk factors of depression symptoms among rural and urban populations affected by Ebola virus disease in the Democratic Republic of the Congo: a representative cross-sectional study. BMJ Open. (2022) 12:53375. doi: 10.1136/bmjopen-2021-053375
30. Nochaiwong, S, Ruengorn, C, Awiphan, R, Kanjanarat, P, Ruanta, Y, and Phosuya, C. Covid-19 public stigma scale (Covid-Pss): development, validation, psychometric analysis and interpretation. BMJ Open. (2021) 11:48241. doi: 10.1136/bmjopen-2020-048241
31. Soomin Ryu, JLH, Guro, Paula, Patel, Akash, Michael, R, and NLF, Elliott. Michigan Covid-19 recovery surveillance study data report 6: Covid-19 stigma and mental health in Michigan (2023). Available from: https://sph.umich.edu/mi-cress/reports/apr_2023_report.html. (Accessed: December 2023).
32. Thornicroft, G, Sunkel, C, Alikhon Aliev, A, Baker, S, Brohan, E, El Chammay, R, et al. The lancet commission on ending stigma and discrimination in mental health. Lancet. (2022) 400:1438–80. doi: 10.1016/s0140-6736(22)01470-2
33. Cheung, Y, Chau, PH, and Yip, PS. A revisit on older adults suicides and severe acute respiratory syndrome (Sars) epidemic in Hong Kong. Int J Geriatr Psychiatr. (2008) 23:1231–8. doi: 10.1002/gps.2056
34. Wasserman, IM. The impact of epidemic, war, prohibition and media on suicide: United States, 1910-1920. Suicide Life Threat Behav. (1992) 22:240–54. doi: 10.1111/j.1943-278X.1992.tb00231.x
35. Lieberman Lawry, L, Stroupe Kannappan, N, Canteli, C, and Clemmer, W. Cross-sectional study of mental health and sexual Behaviours for Ebola survivors in Beni, Butembo and Katwa health zones of the Democratic Republic of Congo. BMJ Open. (2022) 12:52306. doi: 10.1136/bmjopen-2021-052306
36. Kelly, JD, Hoff, NA, Spencer, D, Musene, K, Bramble, MS, McIlwain, D, et al. Neurological, cognitive, and psychological findings among survivors of Ebola virus disease from the 1995 Ebola outbreak in Kikwit, Democratic Republic of Congo: a cross-sectional study. Clin Infect Dis. (2019) 68:1388–93. doi: 10.1093/cid/ciy677
37. Cénat, JM, McIntee, S-E, Guerrier, M, Derivois, D, and Rousseau, C. Psychological distress among adults from the urban and rural areas affected by the Ebola virus disease in the Democratic Republic of the Congo. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:57–62. doi: 10.1007/s00127-020-01904-x
38. Haddad, C, Sacre, H, Bou Malhab, S, Malaeb, D, Saadeh, D, Abou Tayeh, C, et al. A cross-sectional study of Covid-19-related bullying in a sample of Lebanese adults: scale validation, correlates, and mediating effect of fear and anxiety. BMC Psychol. (2021) 9:137. doi: 10.1186/s40359-021-00643-1
39. Olu, OO, Lamunu, M, Nanyunja, M, Dafae, F, Samba, T, Sempiira, N, et al. Contact tracing during an outbreak of Ebola virus disease in the Western area districts of Sierra Leone: lessons for future Ebola outbreak response. Front Public Health. (2016) 4:130. doi: 10.3389/fpubh.2016.00130
40. Alwan, NA. Surveillance is underestimating the burden of the Covid-19 pandemic. Lancet. (2020) 396:e24. doi: 10.1016/s0140-6736(20)31823-7
41. Karafillakis, E, Jalloh, MF, Nuriddin, A, Larson, HJ, Whitworth, J, and Lees, S. ‘Once there is life, there is Hope’ Ebola Survivors' experiences, Behaviours and attitudes in Sierra Leone, 2015. BMJ Glob Health. (2016) 1:e000108. doi: 10.1136/bmjgh-2016-000108
42. Dye, TD, Alcantara, L, Siddiqi, S, Barbosu, M, Sharma, S, and Panko, T. Risk of Covid-19-related bullying, harassment and stigma among healthcare workers: an analytical cross-sectional global study. BMJ Open. (2020) 10:e046620. doi: 10.1136/bmjopen-2020-046620
43. Usifoh, SF, Odigie, EA, Ighedosa, SU, Uwagie-Ero, EA, and Aighewi, IT. Lassa fever-associated stigmatization among staff and students of the University of Benin, Nigeria. J Epidemiol Global Health. (2019) 9:107–15. doi: 10.2991/jegh.k.190514.001
44. Marbán-Castro, E, Villén-Gonzalvo, A, Enguita-Fernàndez, C, Marín-Cos, A, and Menéndez, C. Uncertainties, fear and stigma: perceptions of Zika virus among pregnant women in Spain. Int J Environ Res Public Health. (2020) 17:6643. doi: 10.3390/ijerph17186643
45. UNAIDS. Global aids update 2022: In Danger. Geneva: Joint United Nations Programme on HIV/AIDS, (2022). Available from: https://www.unaids.org/sites/default/files/media_asset/2022-global-aids-update_en.pdf. (Accessed: November 2023).
46. Global Partnership for Action to eliminate all forms of HIV-related stigma and discrimination. Geneva: UNAIDS, (2018). Available from: https://www.unaids.org/en/topic/global-partnership-discrimination. (Accessed: November 2023).
47. Global AIDS Strategy 2021–2026. End inequalities. End aids. Geneva: Joint United Nations Programme on HIV/AIDS, (2021). Available from: https://www.unaids.org/en/Global-AIDS-Strategy-2021-2026. (Accessed: November 2023).
48. A/res/75/284. Political declaration on HIV and AIDS: Ending inequalities and getting on track to end aids by 2030. New York: United Nations General Assembly (2021). Available from: https://undocs.org/A/RES/75/284 (Accessed: November 2023).
49. Global AIDS Monitoring. Geneva: UNAIDS, (2021). Available from: https://www.unaids.org/en/global-aids-monitoring (Accessed November 2023).
50. PLHIV. About the stigma index. Available from: https://www.stigmaindex.org/about-the-stigma-index/. (Accessed: November 2023).
51. James, PB, Lane, R, and Bah, AJ. Social sciences in emerging infectious disease. P Liamputtong, (Ed.) Handbook of social sciences and global public health. Cham: Springer International Publishing (2023). 1–12
52. Dar, SA, Khurshid, SQ, Wani, ZA, Khanam, A, Haq, I, and Shah, NN. Stigma in coronavirus Disease-19 survivors in Kashmir, India: a cross-sectional exploratory study. PLoS One. (2020) 15:152. doi: 10.1371/journal.pone.0240152
53. Nair, S, Joshi, A, Aggarwal, S, Adhikari, T, Mahajan, N, and Diwan, V. Development and Validation of scales to assess stigma related to Covid-19 in India. Indian J Med Res. (2022) 155:156–64. doi: 10.4103/ijmr.ijmr_2455_21
54. Haddad, C, Bou Malhab, S, Malaeb, D, Sacre, H, Saadeh, D, Mourtada, V, et al. Stigma toward people with Covid-19 among the Lebanese population: a cross-sectional study of correlates and mediating effects. BMC Psychol. (2021) 9:646. doi: 10.1186/s40359-021-00646-y
55. Li, T, Bu, H, and Duan, W. A brief measure of perceived courtesy and affiliate stigma on Covid-19: a study with a sample from China. Pers Individ Dif. (2021) 180:993. doi: 10.1016/j.paid.2021.110993
56. Overholt, L, Wohl, DA, Fischer, WA, Westreich, D, and Tozay, S. Stigma and Ebola survivorship in Liberia: results from a longitudinal cohort study. PLoS One. (2018) 13:6595. doi: 10.1371/journal.pone.0206595
57. Kelly, JD, Weiser, SD, Wilson, B, Cooper, JB, Glayweon, M, and Sneller, MC. Ebola virus disease-related stigma among survivors declined in Liberia over an 18-month, post-outbreak period: an observational cohort study. PLoS Negl Trop Dis. (2019) 13:e0007185. doi: 10.1371/journal.pntd.0007185
58. Gregorio, ER, Medina, JRC, Lomboy, M, Talaga, ADP, and Hernandez, PMR. Knowledge, attitudes, and practices of public secondary school teachers on Zika virus disease: a basis for the development of evidence-based Zika educational materials for schools in the Philippines. PLoS One. (2019) 14:4515. doi: 10.1371/journal.pone.0214515
59. World Health Organization. Prioritizing diseases for Research and Development in emergency contexts. Available from:https://www.who.int/activities/prioritizing-diseases-for-research-and-development-in-emergency-contexts. (Accessed: November 2023).
60. Boateng, GO, Neilands, TB, Frongillo, EA, Melgar-Quinonez, HR, and Young, SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. (2018) 6:149. doi: 10.3389/fpubh.2018.00149
Keywords: infectious disease outbreaks, emerging infectious diseases, stigma, epidemic, pandemic preparedness
Citation: Paterson A, Olliaro PL and Rojek A (2023) Addressing stigma in infectious disease outbreaks: a crucial step in pandemic preparedness. Front. Public Health. 11:1303679. doi: 10.3389/fpubh.2023.1303679
Edited by:
Gonzalo Haro, Universidad CEU Cardenal Herrera, SpainReviewed by:
Sanjana Mukherjee, Georgetown University, United StatesCopyright © 2023 Paterson, Olliaro and Rojek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amy Paterson, YW15LnBhdGVyc29uQG5kbS5veC5hYy51aw==
 Amy Paterson
Amy Paterson Piero L. Olliaro
Piero L. Olliaro Amanda Rojek1
Amanda Rojek1